Bumps and rashes on skin: The request could not be satisfied
Bumps on elbows: 8 causes and treatments
A bump on the elbow can occur for numerous reasons, such as skin irritation, arthritis, or an injury. People can treat most elbow bumps with over-the-counter medication or rest.
Underlying medical conditions, such as arthritis, can cause permanent tissue damage if left untreated, however.
In this article, we cover eight possible causes of bumps on the elbows. We also discuss symptoms, diagnosis, and treatment options for each.
Eczema, also known as atopic dermatitis, refers to an inflammatory skin condition that causes red, itchy rashes on the skin. These rashes may appear as small bumps.
Although eczema can affect any area of skin, it commonly appears on the:
- inside of the arms
- behind the knees
- hands
- feet
- face
It can also affect the elbows, but this is more typical in infants with eczema. According to the National Institute of Allergy and Infectious Diseases, eczema affects an estimated 30% of people in the United States.
A combination of genetic and environmental factors can cause a person to develop eczema. Eczema can develop alongside food and respiratory allergies and asthma.
People with eczema have more sensitive skin, and the condition can flare when they use certain products, especially those with fragrances.
A doctor can diagnose eczema by reviewing a person’s medical history and examining the affected skin. A doctor may recommend further testing to rule out other potential skin conditions.
Treatment
Unfortunately, there is currently no cure for eczema. However, prescription topical corticosteroids are the primary means of treating the rash and its symptoms.
Phototherapy, typically in the form of Narrowband UVB therapy, uses ultraviolet light for another treatment. The light interacts with the immune system to reduce inflammation and improve the rash and the symptoms.
People can manage their eczema symptoms with the following tips:
- Avoid potential triggers, such as allergens in foods, scented products, and harsh chemicals.

- Keep the skin moisturized with a gentle, fragrance-free cream or plain Vaseline.
- Do not take long showers or baths.
- Bathe with warm, not hot, water.
Learn more about remedies for eczema here.
Psoriasis is a disorder resulting from immune dysregulation that causes chronic inflammation of the skin. People who have plaque psoriasis develop pink or white scaly plaques on areas, typically, the:
- elbows
- knees
- lower back
- face
- scalp
Some other symptoms of psoriasis include:
A doctor can usually diagnose psoriasis from the skin’s appearance.
Treatment
Treatments for psoriasis vary depending on the location and severity of the condition, and if psoriatic arthritis is present. These treatments can include:
- over-the-counter or prescription topical ointments, especially topical corticosteroids and Vitamin D analogs
- phototherapy with ultraviolet light
- immunosuppressant drugs, such as methotrexate or cyclosporine
- biologic medicines, such as Humira, Cosentyx, Stelara, or Taltz
- an oral retinoid known as Acitretin
Learn more about possible home remedies for psoriasis here.:max_bytes(150000):strip_icc()/milia-38ca74189916485ebbf744fb5df80833.jpg)
Rheumatoid arthritis (RA) is another autoimmune disorder that causes painful swelling in the joints, such as the:
- elbows
- wrists
- fingers
- knees
- ankles
- toes
If a person does not receive treatment, inflammation can cause tissue damage and affect the shape of the joints. People who have RA can develop rheumatoid nodules, which are firm, round bumps under the skin.
Symptoms of RA include:
- swelling, tenderness, or stiffness of the joints
- fatigue
- weight loss
- low grade fever
- firm lumps or nodules under the skin
- anemia or low red blood cell count
A doctor can diagnose RA by examining the joints and performing tests, such as:
Treatment
There is no cure for RA. However, people can use medication and lifestyle changes to reduce joint pain, slow progression, and reduce swelling.
Disease-modifying antirheumatic drugs (DMARDs), such as methotrexate and hydroxychloroquine, can reduce inflammation and slow down disease progression. These medications may help prevent joint damage.
These medications may help prevent joint damage.
Also, people can work with their treatment team to develop a personalized exercise routine. Stretches and low impact exercise can help avoid loss of mobility.
Learn more about how RA affects the body here.
The National Institute on Aging state that osteoarthritis is the most common form of arthritis among older adults.
Osteoarthritis affects over 30 million adults in the U.S., according to the Centers for Disease Control and Prevention (CDC).
The loss of cartilage, which is the tissue located where two bones meet to form a joint, characterizes the condition.
Cartilage acts as a cushion and provides lubrication for the joints. However, the repetitive use of joints over a lifetime can damage the cartilage, which may lead to joint pain and swelling.
Osteoarthritis can affect the:
- elbows
- hands
- knees
- hips
- spine
Symptoms of osteoarthritis include:
- pain and stiffness in the joints
- tender joints
- decreased mobility
- crepitus, or the grinding or cracking sound when moving a joint
Doctors can diagnose osteoarthritis with imaging tests, such as X-rays and MRIs.
A doctor might aspirate an affected joint, which involves collecting and analyzing fluid from the area. The results of this test can help rule out other medical conditions that cause joint inflammation and pain.
Treatment
Treatments for osteoarthritis include medication and surgery to reduce swelling in the joints as well as lifestyle changes, such as:
- weight loss
- physical therapy
- regular exercise
- eating a well-balanced diet with fruits and vegetables
- taking omega-3 fatty acid supplements
Learn more about foods to eat and avoid for osteoarthritis here.
Olecranon bursitis causes swelling and redness at the tip of the elbow. It occurs when a fluid filled sac in the elbow called the olecranon bursa becomes inflamed. People usually develop this condition in response to an infection or after an elbow injury.
Symptoms of olecranon bursitis include:
- swelling at the tip of the elbow
- a round, painless lump on the elbow, also known as a swollen bursa
- warmth, pain, or swelling of the bursa indicating inflammation, including infection
A doctor will likely run one or more imaging tests to diagnose an inflamed bursa and rule out other causes. Blood tests may aid diagnosis by evaluating specific forms of arthritis or any infection.
Blood tests may aid diagnosis by evaluating specific forms of arthritis or any infection.
Treatment
An uninfected bursa will likely heal with rest and anti-inflammatory medicine. An infected bursa will need antibiotics. Doctors may also use steroid injections to reduce inflammation. They will consider surgical intervention on a case-by-case basis.
Learn more about bursitis in general here.
Lateral epicondylitis, commonly known as “tennis elbow,” is a medical condition, the characteristic of which is inflammation of the tendons that connect the muscles in the forearm to the elbow.
People develop this condition from performing repetitive motions that involve the elbow. People who have lateral epicondylitis may notice the following symptoms:
- pain in the outer elbow that worsens when using the forearm
- decreased grip strength
Activities that may cause pain in the elbow include:
- shaking hands
- making a fist
- turning a doorknob
- gripping an object, such as a tennis racket or ball
A doctor can diagnose lateral epicondylitis with the following:
- a physical examination of the elbow
- imaging tests, such as an MRI or X-ray
Treatment
Treatments for tennis elbow include rest, ice therapy, and over-the-counter anti-inflammatory medication.
Wearing a brace on the forearm will give the tendons a chance to heal, helping to reduce painful symptoms and prevent further injury.
People who experience symptoms despite trying the treatments listed above may require surgery or physical therapy.
Learn more about exercises that may help with tennis elbow here.
A lipoma is a soft, noncancerous fatty growth underneath the skin. An experienced clinician can usually easily identify a lipoma on physical exam.
Doctors may associate lipomas with certain disorders, family history, or trauma. They can be small or grow to a considerable size.
Signs and symptoms of a lipoma:
- Lipomas are usually asymptomatic. If painful to the touch, they may be a specific variant known as an angiolipoma.
- They are typically a slow growing soft, squishy movable mass underneath the skin.
Treatment
Lipomas do not require treatment since they are noncancerous. However, if a person wants treatment, surgical removal is usually the first choice. A doctor may consider surgery if the lesion is:
A doctor may consider surgery if the lesion is:
- growing to an undesirable size
- interfering with daily life
- cosmetically concerning
- causing symptoms
- a definitive diagnosis is necessary, or diagnosis is in question
Removal of a lipoma will leave a scar, which will depend on its size and the experience of the surgeon.
It is important to discuss with a surgeon the possible size of the scar before removal, as well as complications, such as keloid formation that can be more symptomatic than the lipoma itself. Recurrence is common if any part of the lipoma is left under the skin.
Dermatitis herpetiformis is a chronic autoimmune condition that causes itchy, red, fluid filled bumps on the skin on areas such as the:
- elbows
- knees
- buttocks
- lower back
- scalp
Often only small scratches in the skin will be evident in these areas since the blisters are very fragile, and a person can easily destroy them by scratching.
People can develop dermatitis herpetiformis as a result of genetic and environmental factors. Gluten is a common environmental trigger that experts associate with this condition.
Doctors commonly associate dermatitis herpetiformis with Celiac disease. Individuals with this disorder should see a gastroenterologist to evaluate for intestinal disease.
A doctor can diagnose dermatitis herpetiformis by analyzing a skin sample for the presence of antibody proteins. Antibody proteins appear on areas of skin the condition affects in 92% of people who have dermatitis herpetiformis.
Treatment
Effective treatments for this condition include:
- topical and oral dapsone
- gluten-free diet
- topical corticosteroids
Learn more about gluten-free foods for different diets here.
People may want to speak with a doctor about bumps on the elbow if they experience:
- a red, itchy, or painful rash
- swelling or warmth in the elbow
- pain when moving the wrist or forearm
Early diagnosis can lead to better treatment outcomes, and it is vital that people do not wait for their symptoms to worsen before seeking treatment.
In some cases, bumps and changes on the elbow may be impossible to prevent. However, people, especially those with eczema, can take general measures to care for their skin by using the following skin care tips:
- Keep the elbows moisturized with gentle, unscented creams, and ointments.
- Apply cream or ointment to the elbows and cover with a sock or cotton shirt for an overnight treatment.
- Bathe the elbows in warm, not hot, water to avoid drying out the skin.
- Avoid skin products that contain harsh chemicals and added fragrances.
Skin conditions, joint inflammation, and injuries to the tendons in the forearm can all cause bumps or changes on the elbow. Usually, a bump or rash on the elbow indicates an underlying medical condition or injury.
People should pay close attention to their symptoms. They can see a doctor if they experience pain or swelling in their elbow that does not get better with rest, ice therapy, or over-the-counter, anti-inflammatory medication.
Coronavirus and pregnancy: What to know
COVID-19 is a concern for everybody, but pregnant women and others anticipating the birth of a baby may worry about how the novel coronavirus could affect their health and the health of the baby.
Coronavirus disease 2019 (COVID-19) is a new disease that results from infection with the novel coronavirus SARS-CoV-2.
As it has only appeared recently, experts have not yet collected enough data to know exactly how the virus affects the health of pregnant women, fetuses, or newborns.
However, several official organizations have released guidance on how pregnant women and those with newborns should proceed during the COVID-19 pandemic.
This article looks at what we currently know about the effects of COVID-19 on pregnancy, giving birth, and the period after delivery.
Share on PinterestMore research is necessary to understand the effect that COVID-19 may have on the health of a fetus or newborn.
According to the Centers for Disease Control and Protection (CDC), pregnant people are at an increased risk for severe illness from COVID-19 when compared to non-pregnant people, although the overall risk remains low.
They may also be at increased risk for other poor outcomes, such as preterm birth.
Due to this, the CDC and the World Health Organization (WHO) both recommend that women should take care to reduce their risk of getting sick during pregnancy.
The WHO currently classify pregnant women as a vulnerable population, along with older adults and pediatric patients.
If women suspect that they have COVID-19 while pregnant, they should talk to their doctor as soon as possible. According to the ACOG, pregnant women with suspected COVID-19 should receive priority testing.
A study from the United Kingdom found that more than half of the pregnant women hospitalized with COVID-19 between March 1 and April 14 were Black or from ethnic minority groups. Experts are discussing this in the context of widespread discrimination and systemic racism in healthcare. Read more here.
During pregnancy, women are also more at risk of getting sick from other respiratory viruses, including influenza.:max_bytes(150000):strip_icc()/Keratosis_pilaris-599da3f5b501e80011214389.jpg) These infections can have adverse effects on the woman and baby.
These infections can have adverse effects on the woman and baby.
These are unsettling times, and it is natural to feel stressed. Taking time for self-care and activities that relieve stress can have important benefits for both the woman and the baby.
It is possible for newborns to have COVID-19, and some babies have tested positive for the SARS-CoV-2 virus shortly after birth. Doctors do not know if they caught the virus before, during, or after delivery.
To date, research has not found the virus in amniotic fluid when the woman has COVID-19. The babies may, therefore, have contracted the virus after birth, but experts are still unsure.
In most cases, newborns with COVID-19 have had mild or no symptoms and made a full recovery. There are also a few reported cases of severe illness in newborns, though.
In a few cases, early birth and other pregnancy or birth problems have occurred in women with COVID-19. However, experts do not know if these problems were related to the virus.
The CDC say that the safest place to give birth is under the supervision of trained healthcare staff, even during the pandemic.
Women who suspect that they have COVID-19 soon before their due date can contact their hospital in advance to find out about their protocol. Many hospitals have separate entrances for people who have COVID-19.
Some hospitals in the United States are limiting the number of visitors, with the aim of protecting patients and staff from the virus. These policies may affect who can attend ultrasound scans, enter the delivery room, or be present during labor.
However, some hospitals have relaxed their restrictions and no longer have these rules in place. People can call the hospital in advance to find out their current guidelines.
In some cases, if a pregnant woman has confirmed or suspected COVID-19, a doctor might recommend temporarily separating the woman and newborn after delivery to reduce the risk of the newborn catching the virus.
The CDC say that the woman and her healthcare team should decide together whether to take this precaution based on the level of risk and the woman’s wishes.
Those who choose not to separate from the baby should take extra precautions. These include regular hand washing and wearing a cloth face covering when within 2 meters of the newborn.
The WHO still encourage mothers with COVID-19 to hold and breastfeed their babies because this close connection is essential for newborns. They also encourage mothers to share a room with their babies. However, these women must follow strict safety procedures.
The hospital staff will care for pregnant women with COVID-19 according to the procedures that the facility has in place for other people with COVID-19. These may involve staying in private rooms, away from other people.
One of the biggest questions that new mothers with COVID-19 may have is whether they should breastfeed their babies.
Breast milk has many benefits for newborns — not only is it rich in nutrients, but it is also a great source of antibodies and hormones that protect newborns from diseases and help them grow strong.
Experts generally recommend that women breastfeed as much as possible, but those with COVID-19 might worry about passing the virus on to the infant.
However, the CDC state that evidence suggests that SARS-CoV-2 is not present in the breast milk of women with COVID-19.
Despite this, women with COVID-19 should take precautions to ensure that they do not transmit the virus to the baby when breastfeeding. Women who plan to breastfeed should wear a face mask and disinfect their hands before touching the baby.
If a woman with COVID-19 plans to pump her breast milk, she should disinfect her hands and the pump before and after each use. Where possible, someone who does not have the disease should do the actual feeding.
COVID-19 is a new disease, and there are limited data about how it affects pregnant women, fetuses, newborns, and the future health status of these individuals.
The limited data available suggest that SARS-CoV-2 does not pass to babies in the womb, in amniotic fluid, or in breast milk.
Anyone concerned about how COVID-19 might affect their health or their child’s heath can talk to their healthcare provider for up-to-date information and reassurance.
Hay fever (allergic rhinitis): Symptoms, causes, and treatment
Hay fever, or allergic rhinitis, is a common condition with symptoms similar to those of a cold. There may be sneezing, congestion, runny nose, and sinus pressure.
It is caused by an allergic response to airborne substances, such as pollen. The time of year it happens depends on what substance, or allergen, the person reacts to.
Despite its name, hay fever does not mean that the person is allergic to hay and has a fever. Hay is hardly ever an allergen, and fever is not a symptom.
Allergic rhinitis is the fifth most common disease in the United States (U.S.).
This article is about hay fever, or allergic rhinitis. You can read about non-allergic rhinitis here.
Symptoms can start at different times of the year, depending on what substance the patient is allergic to.
A person who is allergic to a common pollen will have more severe symptoms when the pollen count is high.
Common symptoms include:
- sneezing
- watery eyes
- itchy throat
- a blocked, itchy, or runny nose
Severe symptoms may include:
- sweats
- headaches
- loss of smell and taste
- facial pain caused by blocked sinuses
- itchiness spreading from the throat to the nose and ears
Some people may experience tiredness or fatigue, irritability, and insomnia.
People with asthma may experience more wheezing and breathlessness at times when hay fever symptoms are common.
A range of over-the-counter (OTC) treatments can help manage hay fever. Sometimes, a combination of two or three is best. A physician can advise about options.
Medications
These include:
Antihistamine sprays or tablets: Commonly available OTC, these stop the release of the chemical histamine. They usually effectively relieve symptoms of a runny nose, itching, and sneezing, but they will not unblock congested sinuses. Older antihistamines can cause drowsiness.
They usually effectively relieve symptoms of a runny nose, itching, and sneezing, but they will not unblock congested sinuses. Older antihistamines can cause drowsiness.
Eye drops: These reduce itching and swelling in the eyes. They are usually used alongside other medications. Eye drops often contain cromoglycate.
Nasal corticosteroids: These sprays treat the inflammation caused by hay fever. They offer a safe and effective long-term treatment. It may take a week for benefits to show.
Examples include fluticasone (Flonase), fluticasone (Veramyst), mometasone (Nasonex) and beclomethasone (Beconase).
There may be an unpleasant smell or taste, or nose irritation.
Oral corticosteroids: Severe hay fever symptoms may respond well to prednisone tablets, prescribed by a doctor. These are for short-term use only. Long-term use is linked to cataracts, muscle weakness, and osteoporosis.
Immunotherapy: Immunotherapy can provide long-term relief by gradually desensitizing the immune system to the allergens that trigger the symptoms.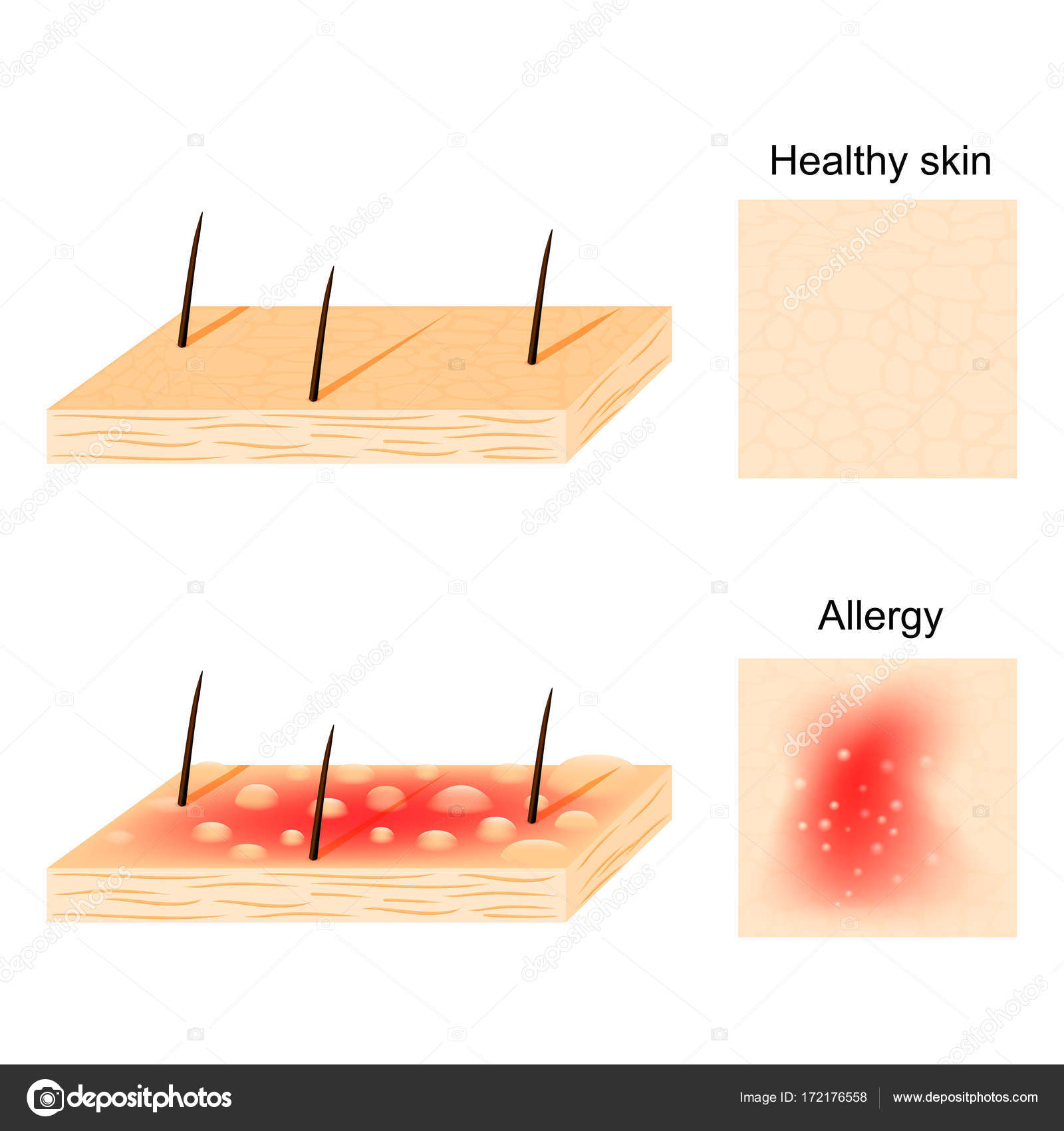 It is usually received in the form of allergy shots or sublingual drops for people whose symptoms are serious and have not cleared up following other treatments.
It is usually received in the form of allergy shots or sublingual drops for people whose symptoms are serious and have not cleared up following other treatments.
Immunotherapy may lead to lasting remission of allergy symptoms, and it may help prevent the development of asthma and new allergies.
Injections are given by a doctor, but sublingual immunotherapy, or medication that is dissolved under the tongue, can be taken at home.
Alternative therapies
Alternative therapies that claim to treat hay fever include acupuncture, but study results have not confirmed significant improvements.
No herbal remedies are recommended.
During pregnancy, it is important to speak to a doctor before taking any medication, to prevent potential adverse effects on fetal development.
Diagnosis
To specify the correct treatment, a doctor will look at the symptoms and ask about personal and family medical history.
A blood or skin test can identify which substance the patient is allergic to.
In a skin test, the skin is pricked with a minute amount of a known allergen.
A blood test will show the level of IgE antibodies. This will be high if an allergy is present. The test takes about 20 minutes.
Zero IgE antibodies indicate no sensitivity, while 6 indicates very high sensitivity.
Another skin-prick test involves injecting an allergen under the skin and checking for a reaction around 20 minutes later.
Hay fever is an allergic reaction to airborne substances, such as pollen.
An allergy happens when the immune system mistakes a harmless substance for a harmful one, and the body releases chemicals to fight it.
This reaction is what causes the symptoms.
Allergens are often common substances that the immune system in most people either does not react to, or reacts only mildly.
However, some people require treatment, because their symptoms make it difficult to complete their daily tasks.
Treatment may not eliminate symptoms, but it can reduce their impact.
An individual cannot prevent the development of an allergy, but people who experience hay fever may find some strategies useful for minimizing the impact.
Here are some tips:
- Be aware of the pollen count during susceptible months. Information is available through the internet and other media. Pollen count tends to be higher on humid and windy non-rainy days and during the early evening.
- Keep windows and doors shut when the pollen count is high.
- Avoid mowing the lawn during susceptible months, choose low-pollen days for gardening, and keep away from grassy areas when pollen counts are high.
- Regularly splash the eyes with cool water, to sooth them and clear them of pollen.
- Shower and change your clothes after coming indoors, when pollen counts are high.
- Use wrap-around glasses to protect the eyes from pollen.
- Wear a hat to prevent pollen from collecting in the hair and then sprinkling down onto the eyes and face.
- Have your car fitted with a pollen filter, and drive with the windows closed at high-count times.
- Do not have flowers inside your home.
- Keep all surfaces, floors, and carpets as dust free as possible.
- Choose a vacuum cleaner with a good filter.
- Use “mite-proof” bedding.
- Use a dehumidifier to prevent mold.
- Keep away from cigarette smoke, and quit, if you are a smoker.
- Wash pets when they come indoors on a high pollen count day, or smooth their fur down with a damp cloth.
- Smear Vaseline around the inside edges of your nostrils, as it helps stop pollen from getting through.
- Ask a physician for a plan, if you know your susceptible time is just around the corner.
Hay fever occurs when the immune system mistakes a normally harmless airborne substance for a threat.
The body produces an antibody called immunoglobulin E (IgE) to attack the threat, and it releases the chemical histamine. Histamine causes the symptoms.
Seasonal hay fever triggers include pollen and spores that only cause symptoms at certain times of the year.
Examples of hay fever triggers include:
- tree pollen in the spring
- grass pollen in late spring and summer
- weed pollen, especially during fall
- fungi and mold spores, more common in warm weather
Other triggers include pet hair or dander, dust mites, mold, and cockroach dust. Irritants that can lead to symptoms of hay fever are cigarette smoke, perfumes, and diesel exhaust fumes.
Risk factors
Some factors increase the risk of hay fever.
Genetic factors: If a close family member has hay fever or another allergy, the risk is higher.
Other allergies or asthma: People with other allergies or asthma are more likely to have hay fever as well.
Gender and age: Before adolescence, hay fever is more common among boys, but after adolescence, females are more affected.
Birth date: People born during the high pollen season have a slightly higher risk of developing hay fever.
Second-hand smoke: Exposure to cigarette smoke during the early years of life increases the risk of hay fever.
Other factors include being the firstborn, coming from a smaller family or a higher-income family. These last three risk factors may be linked to childhood infections.
An infant who has had fewer childhood infections may have a higher risk of autoimmune problems later in life.
There is currently no cure for hay fever. However, symptoms can be managed during the times of the year that have a high pollen count.
For treatment to work in the first year, treatment should be commenced 3 months before the season in which pollen spreads.
Continued treatment can have the effect of reducing symptoms, improving immunity to the allergen, and enhancing the quality of life. Three years of treatment has been shown to lead to long-term desensitization against pollen.
However, if symptoms do not improve significantly after one year, treatment should be discontinued as it is unlikely to work.
Hay fever can become more serious, moving into the lungs and developing into allergic asthma. People with a pollen allergy can also become more likely to develop other allergies, such as food intolerances.
Severe hay fever can also make the mucous membranes of the nose more sensitive to other irritants, such as cigarette smoke or dry air. This can lead to sinusitis.
Skin Allergies | Causes, Symptoms & Treatment
What does a skin allergy look like?
There are several different types of skin allergy reactions that allergists treat.
Eczema (also commonly called atopic dermatitis) typically results in dry, sensitive skin. You may experience red itchy patches. Eczema can come and go over time, and flare-ups may crack, ooze, and itch severely. It is very itchy and can vary in severity from mild (just dry skin ) to severe (red, scaly, thick, fissured and oozing skin)
Hives (also known as urticaria) are raised itchy bumps. Typically hives appear reddish, and will “blanch” (or turn white) in the center when pressed.
Contact dermatitis is typically caused by exposure to an allergen or irritant. If you have red itchy bumps on your skin, especially at the site of contact with some potential irritant or allergen, you may be experiencing contact dermatitis.
If you suspect you have any of these conditions, your allergist can conduct an examination and do testing to help determine the cause of your skin reaction and can recommend treatment to help relieve your symptoms.
How can I relieve the itching from my skin rash?
Avoid scratching! Scratching your rash or hives can create more irritation and can lead to infection. Frequent baths followed immediately with adequate moisturization may help ease your discomfort.
Allergists are specially trained to help treat your condition. Your allergist may prescribe a cream or oral medication to help alleviate your discomfort. Antihistamines and moisturizing ointments can also help ease irritation and dryness. Recently, new medications have been approved, including an ointment for mild to moderate atopic dermatitis and a biologic for moderate to severe atopic dermatitis. You can discuss these options with your allergist.
I haven’t changed anything about my usual routine – what could be causing my skin rash or hives?
There are many possible causes for your skin rash. Some types of rashes are caused by allergies, others may be caused by infections, skin conditions such as eczema or rosacea, or even just dry or damaged skin. Your allergist can help diagnose the cause of your symptoms and prescribe treatment to help you take control and find relief.
Should I stay out of the sun until my rash or hives are gone?
If your skin is already irritated or sensitive, exposure to UV rays and possible sunburn could cause you more discomfort. Take control of your condition by covering up and minimizing your time in direct sunlight.
In addition, some types of skin rash can be caused by the sun. Photoallergic contact dermatitis occurs when your skin has a reaction to an irritant or allergen after exposure to the sun. Cosmetics, sunscreen, shaving lotion, and perfume can trigger this kind of reaction.
Consult with your allergist to determine the cause of your skin reaction and the best course of treatment.
Could my skin reaction be caused by a food allergy?
Yes! A reaction to a food allergen can cause you to have a skin reaction like hives.
There are many possible causes for hives and rashes, so consult with your allergist to determine the cause of your symptoms and the best course of treatment.
18 Common Skin Rash Pictures
Your skin is your body’s largest organ, so it’s not surprising that plenty can (and does) go wrong with it. Skin rashes are a common issue that can impact pretty much anyone, no matter your age, hygiene, or medical history.
“A rash is essentially inflammation in the skin that can be caused by either an external exposure or an internal factor,” says Joshua Zeichner, M.D., director of cosmetic and clinical research in dermatology at Mount Sinai Hospital in New York City. Basically, a rash is your skin’s way of telling you something is up, whether you’ve been exposed to an irritant or you have an underlying medical condition.
The unifying feature of all rashes is inflammation, Dr. Zeichner explains. That inflammation could be minor or could greatly impact the color, texture, or feeling of your skin—it all depends on the type and severity of your rash. (Note: Some of the chronic skin conditions listed below, like acne and rosacea, might not be considered rashes by all dermatologists, but their symptoms and treatments are similar enough to other rashes to include them.)
What causes skin rashes?
Again, when it comes to the root causes of rashes, they tend to fall into two main categories: outside-in and inside-out, explains Dr. Zeichner. A few distinct features make their identification and treatment unique.
Outside-in rashes, like contact dermatitis and ringworm, are due to direct exposure to an outside irritant, allergen, or organism. Irritants (substances like household cleaners and chemicals that can affect anyone) and allergens (substances like latex and poison ivy that only affect those with specific allergies) can both trigger rashes such as contact dermatitis. Organisms living on the skin, meanwhile, cause conditions like ringworm and scabies.
Inside-out rashes stem from genetics, allergies, or infections. Genetic rashes, like eczema or psoriasis, appear because your skin or immune system is triggered to produce them. Allergic rashes, like a drug rash, occur when you ingest an allergen, including certain foods or medications. And viral infections, like measles, can also result in rashes.
Many of these rashes can be resolved with proper treatment, except in the case of inside-out rashes caused by genetics. “Our bodies are genetically programmed to work a certain way, and while we can keep symptoms under control, we don’t necessarily have a permanent cure,” Dr. Zeichner explains.
How to identify common skin rashes and their symptoms
Size and location are the first things to notice when trying to identify a rash. “Something that’s localized with distinct borders will typically be an outside-in job,” Dr. Zeichner says, while inside-out ones “can lead to red, angry rashes throughout the entire body.” The next clues to look for are the shape, color, and texture of the rash.
“If your over-the-counter products aren’t working, you’re suffering from a rash for a week or so, and it’s not improving, you should touch base with a board-certified dermatologist,” Dr. Zeichner says. “This is what we are trained to do, and treatment depends on proper diagnosis.” Be sure to tell your doctor how long you’ve had the rash and any other symptoms you’ve been experiencing (such as a fever or difficulty breathing).
Ahead, you’ll find pictures of common skin rashes, plus symptoms to lookout for. It’s important to note that rashes can look different depending on your skin tone. Some conditions might not cause discoloration on darker skin so if you’re unsure, see a dermatologist who can make the proper diagnosis.
1
Eczema
What it looks like: Medically known as atopic dermatitis, eczema is an umbrella term for a range of skin conditions characterized by red, splotchy, flaky, dry, cracked, or crusty skin that can emit clear fluid when scratched. It’s usually clustered around the insides of elbows and knees, but can appear anywhere on the skin.
Other symptoms to note: Eczema is usually itchy and most common in young people, although many adults also have eczema-prone skin. An estimated 30% of Americans, mostly children and adolescents, suffer from eczema, per the National Institutes of Health. Cold, dry weather and overexposure to water can exacerbate the condition, according to Dr. Zeichner.
2
Contact Dermatitis
What it looks like: Contact dermatitis has the same symptoms mentioned above, and can be a red rash that appears scaly or blistered, depending on its cause and severity. This rash often has a distinct border.
Other symptoms to note: Contact dermatitis appears following exposure to an irritant or allergen, and it’s the most common rash caused by external factors, Dr. Zeichner says. (This can include certain chemicals, acids, botanicals, metals, and more.) Allergens usually cause a shiny, blistered, itchy rash, while irritants tend to cause a dry, scaly, less itchy rash. It can appear hours to days after exposure.
3
Ringworm
What it looks like: Ringworm is a common skin infection caused by a fungus. It gets its name from its circular rash, which is often red, swollen, and cracked.
Other symptoms to note: This rash is itchy and can cause hair loss when it occurs on the scalp. The same fungus also causes athlete’s foot and jock itch. Ringworm is contagious, so avoid touching people and pets or sharing objects like towels with others during flareups.
4
Rosacea
What it looks like: Rosacea causes redness and thick skin on the face, usually clustered in the center. Easy flushing, a stinging sensation, and small, pus-filled pimples are other common signs of the condition, which is often confused with acne breakouts.
Other symptoms to note: With rosacea, skin might feel rough, bumpy, or warm to the touch. Redness usually appears on the forehead, nose, cheeks, and chin. Red, itchy, sensitive eyes are also associated with the condition. Triggers include “spicy food, hot beverages, alcohol, extremes in temperature, and physical and emotional stress,” Dr. Zeichner explains.
5
Psoriasis
What it looks like: Psoriasis causes patches of thickened skin, most often with silver, scaly flakes. It’s usually found around the elbows, feet, knees, palms, and scalp.
Other symptoms to note: Telltale scales set psoriasis apart from other rashes. Per the CDC, up to 20% of people with psoriasis also experience psoriatic arthritis. Psoriasis is not contagious; it’s due to “overactivity of the immune system resulting in skin inflammation,” Dr. Zeichner explains.
Right image credit: Tim Kubacki
6
Hives
What it looks like: Also called urticaria, hives are raised welts in the skin that appear red or discolored. They range in size from small bumps to larger patches.
Other symptoms to note: Hives are most of often the result of exposure to allergens, and they could be a sign of a serious allergic reaction. Hives might not cause any discoloration on darker skin, so be alert for raised patches or welts—those could be a sign of urticaria.
7
Acne
What it looks like: Acne causes red, discolored bumps on the skin, along with whiteheads, blackheads, and cysts.
Other symptoms to note: Acne is the most common skin condition affecting Americans, Dr. Zeichner says, so you likely have experience with pimples already. The causes vary, but are often rooted in excess oil and bacteria on the face, chest, or back, which can be triggered by hormonal issues, stress, certain foods, and irritating products.
8
Shingles
What it looks like: Also known as herpes zoster, shingles is a blistering rash. It often appears in a stripe or in the top quadrant of the head, but only on one side of the body.
Other symptoms to note: Blisters are painful and are sometimes accompanied by fever, headache, and chills. Local tingling or pain is common before the blisters appear. Shingles can affect the eye and even cause vision loss. The condition is caused by the same virus as chickenpox.
Bottom image credit: Preston Hunt
9
Seborrheic Dermatitis
What it looks like: Seborrheic dermatitis is a form of eczema that is characterized by scaly, oily or greasy patches of skin, usually on the scalp.
Other symptoms to note: This condition is itchy and can cause dandruff and buildup on the scalp. It’s also common on other oily areas, like the face and chest, and can be difficult to treat. Dr. Zeichner explains that although the exact cause of seborrheic dermatitis is unknown, the body overreacts to yeast on oily parts of the skin, causing the thick, flaky buildup.
Top image credit: Amras666
10
Perioral Dermatitis
What it looks like: Like seborrheic dermatitis, perioral dermatitis causes red, inflamed skin and small pustules around the nose and mouth.
Other symptoms to note: Flareups can be itchy and uncomfortable, and are often confused with acne. There is no known cause of perioral dermatitis, but overuse of topical corticosteroids is associated with the condition.
11
Scabies
What it looks like: Scabies is a discolored, splotchy rash that can appear pimple-like on any affected parts of the skin. Patients might also notice tiny lines on the skin where the mites have burrowed.
Other symptoms to note: Scabies is very itchy, and usually more intense at night. Unlike the other rashes on this list, this one is caused by an infestation of mites. It’s very contagious and spreads easily through skin-to-skin contact in crowded spaces.
Top image credit: Cixia
Bottom image credit: Tim Kubacki
12
Drug Rash
What it looks like: Drug rashes are usually speckled, itchy, and red, and can cover large areas of skin. They can appear days to weeks after taking a medication.
Other symptoms to note: Drug rashes can be a side effect of or a reaction to a new medication; almost any medication can cause a drug rash, but antibiotics and NSAIDs are the most common culprits. The rash might not be anything to worry about, but it could be a sign of a serious allergic reaction, especially if combined with difficulty breathing. Contact your doctor immediately if you experience these symptoms.
13
Lichen Planus
What it looks like: Purplish legions on the inner arms, legs, wrists, or ankles can signify lichen planus, a skin rash triggered by an overreaction of the immune system.
Other symptoms to note: The legions are usually itchy and may cause skin discoloration as they heal. Lichen planus does not have one single cause—illnesses, allergies, and stress can all trigger breakouts. It is not contagious.
Right image credit: James Heilman, M.D.
14
Measles
What it looks like: Measles causes flat, red spots that cover huge swaths of skin. The rash often appears on the face near the hairline, then spreads down to the feet.
Other symptoms to note: The rash is accompanied by flu-like symptoms, including high fever, cough, and runny nose. Conjunctivitis (pink eye) is also common. Young people could face severe complications from measles, so contact your healthcare provider if you suspect exposure to the illness. Measles is spread when an infected person coughs or sneezes, and it’s one of the most contagious diseases, per the CDC.
Top image credit: Mike Blyth
15
Hand, Foot, and Mouth Disease
What it looks like: Hand, foot, and mouth disease is named for its characteristic flat, red spots that appear on the palms, soles of the feet, and around the mouth.
Other symptoms to note: Spots may blister over time. Cold-like symptoms, including fever and loss of appetite, might also appear. It’s usually not serious, but it’s very contagious and can spread quickly through skin contact or respiratory transmission among people of any age, especially in schools.
16
Tick Bite
What it looks like: The most recognizable reaction on this list is the bullseye rash—a large, red, target-like rash that signals the early stages of Lyme disease from the bite of an infected blacklegged tick. However, many tick bites do not cause a bullseye rash; it appears in about 70 to 80% of Lyme patients.
Other symptoms to note: You might actually find a tick attached to you before a rash appears, which is usually itchy. The bullseye rash in particular is a telltale sign of Lyme disease, even though some patients never get one, so monitor your symptoms and let your doctor know as soon as you notice one.
17
Lupus
What it looks like: Lupus, a chronic autoimmune disease that causes inflammation throughout the body, often presents with a red, butterfly-shaped rash across the cheeks and nose. It is usually worsened by exposure to the sun.
Other symptoms to note: Although the rash does not leave scarring, it could cause discoloration after it disappears. The butterfly rash is distinct from the sores and scaly lesions also caused by lupus. Each case varies, but topical treatments and lifestyle changes can help the rash fade.
This content is created and maintained by a third party, and imported onto this page to help users provide their email addresses. You may be able to find more information about this and similar content at piano.io
12 Common Summertime Skin Rashes in Children
Sunny days and starlit evenings spent playing, splashing, and exploring can leave kids with more than warm summertime memories. Balmy weather also can lead to itchy, irritated skin.
Check out the list from the American Academy of Pediatrics (AAP) to see how you can help prevent, identify, and soothe these common summertime skin rashes.
1. Heat Rash
Heat rash (also known as prickly heat or miliaria) is seen most often in babies and young children when sweat gland pores become blocked and perspiration can’t escape. The rash looks like patches of small pink or red bumps or blisters under clothing or spots where skin tends to fold—on the neck, elbows, armpits, or thighs—although heat rash can occur on other covered areas.
What parents can do:
Keep kids cool. Dress your child in clothing that keeps the skin cool and dry. If possible, use fans and air conditioning to avoid overheating.
Pay attention to hot spots. Wash areas of the skin that stay wet with sweat, urine, or drool with cool water. Pat them dry.
Keep skin bare. Leave areas open to air without clothing. Do not apply skin ointments.
2. Poison Ivy & Other Plant Rashes
Many children get a burning, intensely itchy rash where their skin touches plants—such as poison ivy, poison oak, sumac—containing a sticky oil called urushiol. An allergic skin reaction causes redness, swelling and blisters. Other plants—such as wild parsnip, giant hogweed, and citrus—contain chemicals that make skin hypersensitive to sunlight and cause a phytophotodermatitis rash.
What parents can do:
Prevent exposure. Teach your child what these plants look like and how to avoid them. Both poison ivy and poison oak have shiny green leaves that grow three to a stem, so you might share the rhyme: “Leaves of three, let them be.” The sumac shrub has stems that contain 7-13 leaves arranged in pairs, while wild parsnip and giant hogweed have clusters of small, flat-topped yellow and white flowers. If you have younger children, inspect the parks they play in and have rash-causing plants removed.
Wash and trim. If your child comes into contact with these plants, wash all of his or her clothes and shoes in soap and water. Also, wash the area of the skin that was exposed with soap and water for at least 10 minutes after the plant or the oil is touched. To discourage scratching and further damage to the skin, keep your child’s fingernails trimmed. This will also prevent the rash from spreading if there is still a small amount of oil under the fingernails.
Soothing salves. If the rash is mild, apply calamine lotion to cut down on the itching. Avoid ointments containing anesthetics or antihistamines—they can cause allergic reactions themselves. Another good option to reduce skin inflammation is 1% hydrocortisone cream.
Talk with your pediatrician. While mild cases can be treated at home, talk with your pediatrician if your child is especially uncomfortable, the rash is severe and/or isn’t going away, if the rash is on your child’s face or groin area, or if you notice signs of infection (i.e., fever, redness, swelling beyond the poison ivy or oak lesions).
3. Eczema
Eczema (also called atopic dermatitis or AD) is a chronic condition common in children that causes patches of dry, scaly red skin and tends to flare up during colder months when there’s less moisture in the air. But dryness caused by air conditioning and pressurized planes during summer travel can cause problems, too. Overheating, sweating and chlorine in swimming pools also can trigger eczema.
What parents can do:
Moisturize. Apply fragrance-free creams or ointments at least once a day or more often if needed. After a bath or swimming, gently pat your child’s skin with a towel and then apply moisturizer to his or her damp skin.
Dress wisely. Choose clothing made of soft, breathable fabrics like cotton when possible. Wash clothes in a detergent free of irritants such as perfumes and dyes.
Don’t scratch. Keep your child’s fingernails short and smooth, and remind him or her not to scratch. Scratching can make the rash worse and lead to infection.
Talk with your pediatrician. Ask your child’s pediatrician if allergies, sometimes triggered by trees and plants that bloom during summer, could be a cause of the eczema. Your child’s pediatrician may recommend medicines to help your child feel better and to keep the symptoms of eczema under control.
4. Insect Bites & Stings
Insects such as bees, wasps, mosquitos, fire ants, and ticks can cause itching and minor discomfort where they prick the skin. For some children, insect bites and stings can cause a severe allergic reaction called anaphylaxis—which includes a rash or hives and life-threatening symptoms such as airway swelling. (For children with a known allergy to insect bites and stings, it is important to have anaphylaxis emergency care plan in place). Other times, diseases spread by insects such as Lyme Disease, Rocky Mountain Spotted Fever, and Zika Virus can cause rashes and other health problems.
What parents can do:
Avoidance. When spending time outdoors, avoid scented soaps and shampoos and brightly colored clothing—they can attract insects. If possible, steer clear of areas where insects nest and gather (i.e., stagnant pools of water, uncovered food, and blooming flowers).
Use insect repellent. Products with DEET can be used on the skin, but look for family-friendly products that contain concentrations of no more than 30% DEET. Wash the insect repellent off with soap and water when your child returns indoors.
Cover up. When in wooded areas or in or near tall grass, stay on cleared trails as much as possible. Have your child wear a long-sleeved shirt, pants, and hat. Avoid wearing sandals in an area where ticks may live.
Look closely. Wear light-colored clothing to make it easier to spot ticks. After coming indoors, check for ticks on your child’s skin—they often hide behind the ears or along the hairline.
Remove stingers and ticks. To remove a visible stinger from skin, gently scrape it off horizontally with a credit card or your fingernail. If you find a tick, gently grasp it with fine-tipped tweezers as close to the skin as possible. Without squeezing the tick’s body, slowly pull it away from the skin. See How To Remove A Tick for more information.
Clean the skin. After the stinger or tick is out, clean the bitten area with rubbing alcohol or other first aid ointment.
Treat swelling. Apply a cold compress or an ice pack to any swelling for at least 10 minutes.
Help relieve the itch. Applying ice, along with calamine lotion or 1% hydrocortisone cream, can also help relieve itching.
5. Impetigo
Impetigo is a bacterial skin infection that’s more common during hot, humid weather. It causes a rash that may have fluid-filled blisters or an oozing rash covered by crusted yellow scabs. Impetigo is more likely to develop where there is a break in the skin, like around insect bites.
What parents can do:
Clean and cover. Clean the infected area with soap and water. Cover the infected area loosely to help prevent contact that would spread the infection to others or to other parts of the body. Wash your own hands well after treating your child’s sores.
Avoid scratching. Trim your child’s fingernails and discourage scratching. A child can spread the infection to other parts of his or her body by scratching. You can cover the rash loosely with a bandage to discourage your child from touching the rash, but make sure air can flow through so the skin can heal.
Talk with your pediatrician. While mild cases may respond to over-the-counter antibiotics such as bacitracin or bacitracin-polymyxin, impetigo is usually treated with prescription antibiotics—either a skin cream or oral medication. Your pediatrician may order a skin culture (test of your child’s skin) to determine which bacteria are causing the rash.
6. Swimmer’s Itch
Swimmer’s itch (also called clam digger’s itch or cercarial dermatitis) may appear after playing in lakes, oceans, and other bodies of water. The rash is caused by microscopic parasites found in shallow, warmer water near the shoreline where children tend to stay. The parasites burrow into skin, and cause tiny reddish, raised spots on skin not covered by the swimsuit to appear. Welts and blisters may also form.
What parents can do:
Be aware. Don’t swim near or wade in marshy areas where snails are commonly found. Try not to attract birds (by feeding them, for example) where your family swims. Birds may eat the snails and spread the parasites in the water.
Shower or towel dry. Shower or briskly rub the skin with a towel immediately after getting out of the water. The parasites start to burrow when the water on skin begins evaporating. If your skin child’s skin stings with rubbing—and the rash appears under the swimsuit—he or she may instead have Seabather’s Eruption from stinging larvae of sea critters such as jellyfish or sea anemone. Stop rubbing and shower instead.
Don’t scratch. Trim your child’s fingernails and discourage scratching. Home treatments such cool compresses on the affected areas, Epsom salt or oatmeal baths, or baking soda paste may help to relieve the discomfort. If itching is severe, talk with your child’s pediatrician. He or she may suggest prescription-strength lotions or creams to reduce your child’s symptoms.
7. Cutaneous Larva Migrans (Sandworms)
Sandworms may be present in sand contaminated with feces from pets or stray animals. When a child stands or sits in contaminated sand on a beach or in a sandbox, the worms may burrow under the skin, usually around the feet or buttocks. Lines of itchy, reddish rash known as a creeping eruption appear as the worms move under the skin, up to a few centimeters a day. The condition is more common subtropical and tropical areas such as the Caribbean, as well as parts of the southwestern United States.
What parents can do:
Keep shoes on. Don’t let your child play on beaches where people walk their dogs. If your family goes on an outing to a designated pet-friendly beach, make sure your child keeps shoes on and doesn’t sit in the sand without a blanket or towel.
Talk with your pediatrician. Your pediatrician can prescribe anti-parasitic medications such as albendazole or ivermectin to treat the rash. Without treatment, the larvae usually will die off in 5 to 6 weeks. Your pediatrician may suggest a cream to help relieve itching.
8. Folliculitis (Hot Tub Rash)
Folliculitis (hot tub rash) is an itchy, pimply rash that occurs when bacteria in unclean pools and hot tubs gets into hair follicles on the skin. The area where hairs grow from the skin becomes infected and inflamed, sometimes forming small, pus-filled blisters. A similar rash may come from wearing a damp swimsuit that wasn’t washed and dried well after previous use. Hot rub rash typically starts 12-48 hours after being in a hot tub.
What parents can do:
Avoid dirty pools. If you’re unsure whether the acid and chlorine levels are properly controlled in a heated pool, don’t allow your child to go in.
Don’t allow young children in spas or hot tubs. In addition to the risk for drowning and overheating, young children are also at higher risk of bacterial skin infection because they tend to spend more time in the water than teens or adults.
Talk with your pediatrician. Hot tub rash usually clears up without medical treatment. In the meantime, warm compresses and an over-the-counter anti-itch cream recommended by your pediatrician can help your child be more comfortable. If your child’s rash lasts more than a few days, talk with your pediatrician.
9. Molluscum Virus
Molluscum contagiosum is a viral infection that causes pearly bumps on the skin on a child’s chest, back, arms or legs. The dome-shaped bumps, also known as “water warts,” may have a dimple in the center. The poxvirus that causes the bumps is more common in hot, humid climates. Some studies suggest the infection may spread in contaminated swimming pools.
What parents can do:
Wait it out. In most cases, molluscum contagiosum does not need treatment. The bumps usually will go away in 6 to 12 months.
Stop the spread. A child with molluscum contagiosum should not share towels, bedding, or clothing with others to avoid spreading the virus. The bumps are contagious as long as they are present.
Avoid scratching. Scratching the bumps can spread the virus and cause a second, bacterial infection where the skin is open.
10. Juvenile Plantar Dermatosis (Sweaty Sock Syndrome)
A smooth, reddened rash on your child’s feet, sometimes with peeling, cracking skin or scaly skin, could be from a condition called Juvenile Plantar Dermatosis (Sweaty Sock Syndrome). It happens when feet get wet and then dry quickly, again and again—like when shoes are taken on and off coming in and out of the house during summer.
What parents can do:
Breathable footwear. Reduce how often the feet go from wet to dry quickly by having your child wear open or more breathable footwear made of materials like mesh or cotton (i.e., water shoes) and/or thicker more absorbent socks.
Apply ointment. Applying moisturizing ointment or an over-the-counter steroid cream to the affected areas of your child’s foot immediately after taking shoes off or getting out of water can help. If the condition does not improve, or if you notice any sign of infection where your child’s skin is cracking, talk to your pediatrician.
11. Tinea (Ringworm)
Despite having “worm” in its misleading name, tinea (ringworm) is an infection caused by a fungus that thrives in warm, damp conditions. It is similar to athlete’s foot and jock itch and can appear on a child’s scalp or other parts of the body. It’s called ringworm because the rash from the infection tends to form round or oval spots that become smooth in the center as they grow while the border remains red and scaly. The fungus can spread quickly among student athletes, especially during sweaty, summertime practices and games, when they share sports equipment and locker rooms.
What parents can do:
Stop the spread. Check and treat any pets that may have the fungus—look for scaling, itchy, hairless areas on their fur. Family members, playmates, or schoolmates who show symptoms also should be treated. Do not allow your child to share combs, brushes, hair clips, barrettes, or hats. Make sure mats used in sports like wrestling and gymnastics are properly disinfected after use.
Talk with your pediatrician. A single ringworm patch on the body can be treated with an over-the-counter cream recommended by your pediatrician. If there are any patches on the scalp or more than one on the body, or if the rash is getting worse while being treated, your pediatrician may prescribe a stronger medication and special shampoo.
12. Hand, Foot & Mouth Disease
Many parents assume virus season winds down after winter. But some viral illnesses, such as hand, foot, and mouth disease, are more common during summer and early fall. Outbreaks are most common in younger children and can spread in child care centers, preschools, and summer camps. Caused by Enterovirus coxsackie, the illness starts with a fever, sore throat, and runny nose—much like the common cold—but then a rash with tiny blisters may appear on any or all the following places on the body:
In the mouth (inner cheeks, gums, sides of the tongue or back of the mouth)
Fingers or palms of hands
Soles of feet
Buttocks
Symptoms are the worst in the first few days, but they are usually gone within a week. Peeling skin on the fingers, toes, and nails may begin after a week or two, but it is harmless. Parents of children with a history of atopic dermatitis or eczema should be aware that their children may be prone to a more severe outbreak.
What parents can do:
Monitor symptoms. Be sure to call your pediatrician if your child’s fever lasts more than 3 days or if he or she is not drinking fluids. If symptoms are severe, your pediatrician may collect samples from your child’s throat for lab testing.
Ease the pain. For fever and pain, the pediatrician may also recommend acetaminophen or ibuprofen. Liquid mouth-soothing remedies may be useful to alleviate mouth ulcer pain. Do not use regular mouthwashes, because they sting.
Avoid dehydration: Children with hand, foot, and mouth disease need to drink plenty of fluids. Call your pediatrician or go to the ER if you suspect your child is dehydrated. See Signs of Dehydration in Infants & Children for more information.
Inform others. Tell child care providers and playmates’ parents to watch for symptoms of the illness. Children with hand, foot, and mouth disease may spread the virus through the respiratory tract (nose, mouth and lungs) for 1-3 weeks, and in the stool for weeks to months after the infection starts. Once a child’s fever has gone away and he or she is feeling better, there is no need to keep him or her home unless there are still open and oozing blisters. See When to Keep Your Child Home from Child Care for more information.
Remember…
Protecting your child’s skin is a year-round concern, but it’s especially important in the summer months when so much skin is exposed and vulnerable. Fortunately, many summertime rashes clear up quickly on their own. Be sure to talk with your pediatrician about any rash that you’re unsure about—especially if you don’t know what caused it, if it is making your child feel miserable or doesn’t clear up quickly, or if it shows signs of infection or is accompanied by any shortness of breath.
Additional Information:
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
What’s that rash?: with pictures
Have you ever Googled, ‘what’s that rash?’ You may have been looking for yourself, your child or a ‘friend’.
Chances are you’ve had a rash or two in your lifetime. What is a rash? A rash is a temporary flare-up on the skin. It usually appears as red spots or reddening. It can sometimes be dry, scaly or itchy.
Your skin is actually covered in trillions of bugs, these are called microorganisms and together they make up your skin microbiome. When they are balanced and happy so is your skin. Rash conditions like eczema and dermatitis are caused when your skin microbiome is out of balance. Find out more about your skin microbiome by listening to our podcast: My Amazing Body.
There are many types of rashes, including eczema, hives, and heat rash. Some rashes can be temporary, or they might be a chronic condition. Sometimes rashes can be a sign of a serious illness, like measles, so it’s important you seek medical advice if you are concerned about a rash.
We’ve listed some common rashes, their symptoms and how you can treat them. The rashes we mention usually occur on your face and sometimes other parts of the body. If you’ve got a rash ‘downstairs’ it could be a symptom of an STI and we recommend you talk with your GP or get a sexual health check.
Eczema
Eczema is a skin condition that affects children and adults. It is more common in children, in fact, 66 percent of eczema sufferers are diagnosed before aged two. They will usually grow out of eczema by adolescence. It can also be called atopic eczema, atopic dermatitis and allergic eczema.
We don’t really know exactly what causes eczema, but we do know that it can sometimes be genetic. One gene linked to eczema is called filaggrin and people who get eczema often have a defect which reduces their skins ability to repair itself after injury. It also allows allergens to enter the deeper layers of the skin. People who have eczema may also have other conditions like hay fever or asthma.
Some triggers that cause and make eczema worse include:
- dry skin
- scratching the affected area
- viral or bacterial infections
- chemicals from swimming pools
- sand, especially from sandpits
- some types of carpet or grass
- animals or house dust mites
- allergens that you can breathe in, such as pollen
- artificial colours and preservatives
- perfumes, soap and chemicals
- woollen or synthetic fabrics
- heat or very hot rooms
- stress
Eczema causes very itchy, scaly, red patches of skin, usually on cheeks, in elbow creases and behind the knees.
Your doctor will be able to diagnose you with eczema and advise a suitable treatment plan. The most effect way to relieve symptoms and treat eczema is to keep the skin well moisturised by using a non-perfumed moisturiser on your skin every day. It’s also best to avoid itching the area to reduce breaking the skin which can increase the chance of infection.
The skin has special cells that have an immune function. Eczema causes a breakdown in the skin’s barrier function. Sometimes, children with eczema are more prone to developing allergies. Foreign proteins make their way through the damaged skin and activate the immune cells.
For this reason, it is important not to use creams containing food ingredients. e.g. oats, goats’ milk, almond oil. Using creams containing food ingredients can cause an allergy to that food to be developed.
Contact dermatitis
Contact dermatitis is inflammation of the skin. There are two types of contact dermatitis, which occurs when your skin touches something that makes it red and inflamed. Allergic contact dermatitis is when your skin becomes inflamed after coming into contact with an allergen, like plants. If your skin is exposed to an irritant, like cosmetics, for a long period of time this is called irritant contact dermatitis.
Contact dermatitis can cause the skin to become:
- cracked
- red
- blistered
- thickened
- dry
- itchy
The rash should clear slowly if you avoid the substance that is causing the irritation or reaction. You should see a doctor if your rash is uncomfortable or doesn’t clear up. They will be able to assist you with treatment and help find the allergen or irritant.
Heat rash
Heat rash often occurs during summer and is usually harmless. It’s also known as prickly heat or miliaria. Heat rash is caused by a blockage and inflammation of your sweat ducts.
Symptoms can last 2-3 days and can include, tiny red spots or blisters, an itchy or prickling sensation, redness or mild swelling of the area. It is more common in sweaty areas of the body. The armpits, back, under the breast, chest, groin or crooks of your elbows and knees are all areas that can be affected.
To reduce the risk of heat rash you should stay cool during the hotter months, by drinking water regularly, wearing light clothing and staying out of the heat. Heat rash can sometimes be the first sign of a heat-related conditions, like heat stroke or exhaustion, which require urgent attention.
Heat rash will usually go away by itself. You should see you doctor if the rash gets worse or lasts more than 3 days. If the blisters become infected with yellow or green pus, if you have a fever or are feeling generally unwell you should see your doctor.
Hives
Hives, also known as urticaria or nettle rash, is a skin rash that occurs when the body produces histamine. Histamine is a protein your body uses to fight off viruses and bacteria but when you get hives, your body might be reacting to an irritant.
Hives symptoms include a raised bumpy red rash. The bumps can sometimes look more like your normal skin colour and can be quite itchy. The trigger for hives is sometimes unknown but can be caused by an allergic reaction, medication or an infection.
It can sometime take days or weeks for hives to develop but true hives can last just a couple of hours or up to 6 weeks. You should see your doctor is the rash lasts longer that 6 weeks or if you are concerned.
Hives are usually harmless, but sometimes they might be a sign of anaphylaxis. Anaphylaxis requires urgent medical attention. If you or your child is having difficulty breathing, seems to have a swollen tongue or throat or has collapsed, phone Triple Zero (000) for an ambulance immediately.
Rosacea
Rosacea, or acne rosacea, is a non-contagious, common skin inflammation that only affects the face. It causes redness, flushing and sometime pimples on your face, though it is not the same as acne.
The first signs of rosacea can include frequent flushing or blushing of the skin and it usually appears between the ages of 30 and 50 years old. The cause is unknown and there is no cure, and unfortunately symptoms get worse as you age.
Symptoms of rosacea:
- frequent blushing, flushing or redness on your cheek, nose, chin or forehead
- persistent redness that looks similar to a sunburn that does not go away
- small visible blood vessels on your face
- bumps or pimples on your face that might sting or burn
- red or irritated eyes or swollen eyelids
Some people’s rosacea can also be triggered by exposure to sun, hot weather, spicy foods, exercise or certain medications and skincare products. Talk to your doctor or a skin specialist for recommendations to control the symptoms.
If you are concerned about a rash or it is associated with a severe headache, neck stiffness, fever or vomiting and nausea you should see your doctor or call 13 HEALTH (13 43 25 84) for medical advice.
More information
Health Direct
Raising Children
Eczema Association of Australia
My Amazing Body Podcast – The Skin Microbiome
90,000 Plaques on the skin – causes of appearance, in what diseases it occurs, diagnosis and methods of treatment
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-medication. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For a diagnosis and correct prescription of treatment, you should contact your doctor.
Plaques on the skin: causes of appearance, in what diseases occur, diagnostics and methods of treatment.
Definition
A plaque is a pathological element with clear edges that rises above the surface of the skin or merges with it, more than 5 mm in size.
In dermatology, many types of plaques are distinguished – about 70 diseases occur with the formation of these elements, which makes plaque one of the most common rashes.
Varieties of plaques
The plaques are round, oval and irregular in shape.The shape, surface and appearance of this element may change over time.
Due to the occurrence of plaques, it can be both a manifestation of skin diseases and a symptom of diseases of internal organs and systems (autoimmune reactions, liver diseases, oncological processes, allergic reactions).
Plaques are dry, smooth, red, brown, gray-white, etc.
Possible causes of the appearance of plaques
Dry plaques on the skin in adults can be a manifestation of the following diseases:
- Fungal skin lesions accompanied by plaques with severe itching.
- Allergic reactions are characterized by the appearance on the skin of smooth dry plaques, pink spots, blisters, which are very itchy and cause severe discomfort. They can develop both when the skin comes into contact with an allergen, and when it gets on mucous membranes (for example, with urticaria, hay fever, food and contact allergies).
- Psoriasis is a chronic non-infectious skin disease in which scaly dry plaques form on the elbows, knees, scalp, prone to fusion and accompanied by mild itching.
- Dry plaques form on the skin if it is exposed to stress for a long time with the loss of its protective functions.
- Diseases of the digestive tract, accompanied by malabsorption syndrome (impaired absorption of vitamins and trace elements in the small intestine), chronic diseases of the liver and other organs, in which substances that are not normally present in the dermis accumulate in the dermis, also lead to the appearance of dry plaques.
- Solar keratoma is a precancerous condition characterized by the presence of many light grayish plaques on the skin.
The appearance of red plaques on the skin indicates their good blood supply. Possible reasons for this condition may be the following nosologies:
- Medicinal toxidermia is an allergic reaction accompanied by the appearance of elements in the form of plaques on the skin. In severe cases, Lyell’s or Stevens-Johnson’s syndrome, toxic epidermal necrolysis, may develop.
- Duhring’s dermatitis (herpetiformis) is a chronic skin disease without an established etiology, which is characterized by a recurrent appearance on the skin of a rash of various morphology, accompanied by severe itching and burning.
- Fungal mycosis – primary T-cell lymphoma of the skin, malignant lymphoid lesion, primarily of the skin. Itchy, red, eczema-like plaques appear on the skin. In the initial stages, they respond well to treatment with hormonal ointments, but the disease itself requires more complex therapy.
- In children, the appearance of red spots and plaques on the skin is most often associated with an allergic reaction to food.
Brown plaques occur when melanin is deposited in the affected area of the dermis, which causes a brown (dark) color.Possible causes may include the following diseases:
- Becker’s nevus is an abnormality in the development of the dermis, when dark plaques with an uneven surface appear on the skin, on which hair can begin to grow over time.
- Pigmented nevus – “birthmark”, can rise above the skin, has a brown or dark color.
- Melanoma is the most malignant skin tumor characterized by rapid metastasis. It develops mainly from nevi and moles.When the nature of the surface, the boundaries of the mole changes, its size increases, bleeding occurs, you must immediately contact a dermatologist or oncologist to exclude the development of melanoma.
- Basal cell skin cancer is more often localized on the head, face, neck, does not metastasize, and is characterized by slow growth.
- Senile keratoma occurs in elderly people, develops, most likely, due to a lack of vitamins, an abundance of consumed animal fats, sensitivity of the skin to ultraviolet light due to a violation of its protective functions.Typical localization – face, neck, open areas of the body.
- Seborrheic keratoma is a yellowish plaque on the skin that eventually transforms into a dark brown growth that tends to flake off, itch, crack, bleed, and can act as a gateway to infection.
Which doctors should I contact
If plaques form on the skin, it is necessary to consult a dermatologist to determine the causes of the appearance of this element of the rash.
Diagnostics and examinations when plaques appear
To diagnose fungal skin lesions, scraping from the affected area is used for subsequent microscopic examination.
The development of an allergic reaction requires seeking medical help to identify the allergen, prescribe antihistamines, and sometimes hormonal drugs. In allergy clinical cases, along with skin tests, tests are carried out using various sets of common allergens and triggers: a panel for respiratory allergens, food allergens, and their combination.
90,000 HIV symptoms, infection and spread
HIV (Human Immunodeficiency Virus) is the virus that causes AIDS. HIV attacks the immune system by destroying white blood cells that help the body fight infections and disease. Testing is the only reliable way to tell if you have HIV. The following are symptoms that can serve as a warning that you have an infection.
Method 1 of 3: Identifying Early Symptoms
1
Determine if you are experiencing severe fatigue for no reason. Fatigue can be a symptom of a large number of different diseases, and is also manifested as a symptom in HIV-infected people. This symptom should not cause you more concern if it is the only one that you feel, but it is worth considering in the future.
- – Severe fatigue is not a feeling when you just want to sleep. Do you feel tired all the time, and even after a good night’s sleep. Do you go to naps during the day more often than usual and avoid strenuous activity because you feel exhausted.This type of fatigue is cause for concern.
- – If this symptom persists for more than a few weeks or months, you should be tested to rule out HIV.
2
Monitor fever or increased night sweats. These symptoms often occur in the early stages of HIV, during the so-called primary or acute stage of HIV infection. Again, many people do not have these symptoms, but those who did have them usually feel them 2-4 weeks after they acquired HIV.
- – Fever and increased sweating are symptoms of the flu and the common cold. If it is a cold season or a flu epidemic, you may have these diseases.
- – Chills, muscle pain, sore throat and headache are also symptoms of the flu and colds, but can also be signs of early HIV infection.
3
Check for swollen glands in the throat and lymph nodes in the armpits and groin. Lymph nodes swell as a result of infection. This does not happen in everyone who has early HIV, but among those who have these symptoms, these are the most common.
- – In HIV infection, the lymph nodes in the neck usually swell more than the nodes in the armpits and groin.
- – Lymph nodes can swell as a result of other types of infections such as colds and flu, so further testing is needed to make a diagnosis.
4
Pay attention to cases of nausea, vomiting and diarrhea. These symptoms can also be a sign of early HIV infection. Check if these symptoms persist for a long time.
5
Note sores in the mouth and genitals. If sores in the mouth occur along with other symptoms already mentioned, and especially if you usually have not developed such sores before, then this may be a sign of early HIV infection.Genital ulcers are also a sign that you may have been infected with HIV.
Method 2 of 3: Identifying progressive symptoms
1
Do not rule out dry cough. This symptom occurs in the late stages of HIV, sometimes even for many years after infection, when the virus was latent in the body. This seemingly harmless symptom is easy to miss at first, especially if it occurs during the allergenic or flu season or during the cold season.If you have a dry cough and cannot get rid of it with antihistamines or an inhaler, then this could be a sign of HIV.
2
Look for unusual spots (red, brown, pink, or purple) on the skin. People with advanced stages of HIV often have skin rashes, especially on the face and torso. The rash can be inside the mouth or nose. This is a sign that HIV is turning into AIDS.
- – Flaky, red skin is also a sign of advanced stage of HIV.The spots can be in the form of boils and bumps.
- – A rash on the body is usually not accompanied by a cold and fever. Accordingly, if you have such symptoms alternately, consult a doctor immediately.
3
Pay attention to pneumonia. Pneumonia is a common disease in those whose immune systems are weakened for various reasons. People with advanced HIV infection tend to develop pneumonia through exposure to germs, which usually do not cause such a severe reaction.
4
Check for thrush especially in the mouth. The last stage of HIV usually causes thrush in the mouth, called stomatitis. It looks like white or other unusual patches on the tongue or inside the mouth. This is a warning sign that the immune system cannot fight infection effectively.
5
Examine your nails for fungus. Yellow or brown nails with cracks and chips are a common sign of advanced HIV infection.The nails become more susceptible to fungi, which the body can normally fight against.
6
Determine if you are experiencing rapid weight loss for an unknown reason. In the early stages of HIV, it can be caused by severe diarrhea, in the later stages by “atrophy”, a strong reaction of the body to the presence of HIV in the body.
7
Watch out for memory loss, depression, or other neurological problems. In the last stages, HIV affects the cognitive functions of the brain. These symptoms are serious in themselves and should be investigated anyway.
Method 3 of 3: HIV Data
1
Find out if you are at risk. There are several conditions that put you at risk of contracting HIV. If you have such situations, then you are at risk:
- – You have had unprotected anal, vaginal or oral sex.
- – You used needles and syringes with other people.
- – You have been diagnosed with or treated with a sexually transmitted disease (STD), tuberculosis, or hepatitis.
- – You had a blood transfusion between 1978 and 1985, years before blood tests were started, to prevent a transfusion of contaminated blood.
2
Do not wait for symptoms to appear for analysis. Many people with HIV do not know they have it. The virus can remain in the body for more than 10 years until symptoms appear. If you have reason to suspect that you have contracted HIV, do not withdraw from the test due to the absence of symptoms.
3
Get an HIV test. This is the most accurate method in determining HIV. Please contact us at: Izhevsk, st. Truda 17a, tel. (3412) 21-15-94 or to one of our zonal centers located in the cities of Glazov, Votkinsk, Sarapul, Mozhga, as well as in the villages of Uva and Igra.
- – Testing is simple and absolutely FREE.
- – If you have been tested for HIV, do not let fear prevent you from getting your test results. Knowing whether or not you are infected will change either your lifestyle or the way you think.
Councils
- – If you have doubts about doing the analysis or not, do it. This is the only correct and safe action for both you and those around you.
- – HIV is not transmitted by airborne droplets or food. This virus does not live long outside the body.
90,000 Tubercles – globular or flat formations
Among the various formations on the skin, tubercles should be distinguished. Outwardly, they look a little like ordinary acne, but unlike acne, they do not become inflamed and can persist on the skin for a long time.Bumps can appear on various parts of the body: on the face, back, limbs, in the eye area. Bumps on the skin can be spherical or oval in shape, reach various sizes and be caused by different reasons.
Among the factors that provoke the growth of seals under the skin, there are blockages of sebaceous plugs, staphylococcal infection, metabolic disorders, an unhealthy lifestyle, poor environmental conditions, mechanical damage to the skin.
Varieties of bumps on the skin
Small lumps on the skin can be:
- wen – a benign tumor that does not pose a health hazard;
- subcutaneous cyst – mildew;
- molluscum contagiosum.
90,031 subcutaneous comedones;
Bumps on the skin often do not cause pain or discomfort to the patient. Often they represent only a defect in appearance, but sometimes they can become inflamed as a result of constant rubbing with clothing.
When bumps appear on the skin, in no case should you self-medicate, since for treatment you need to establish the cause that caused the pathological formations. Also, you can not try to squeeze out the tubercles, especially since it is difficult to do this. An attempt to open the tubercles on their own can provoke the spread of infection throughout the body and the further appearance of a scar or scar.
Treatment of bumps on the skin
When choosing treatment methods, it is very important to determine the type of tubercles and establish the cause of their appearance. This can only be done by an experienced specialist. When diagnosing, it is necessary to exclude the malignant nature of skin formations.
Treatment of pathological seals on the skin should be aimed at eliminating the cause that causes them. It is often necessary to check the condition of the patient’s internal organs (stomach, intestines, pancreas).
Experienced specialists of our center will determine with maximum accuracy the reasons that provoked the appearance of tubercles and will select the most effective drugs in each case. To get rid of the bumps, various cosmetic procedures for skin care, nutritional correction, mechanical removal using special techniques can be additionally recommended.
Ask a question to a specialist?
Get a free consultation
90,000 Human parasitic diseases.Dirofilariasis. – GBUZ LO “Vsevolozhskaya KMB”
Human parasitic diseases. Dirofilariasis.
Doctor-epidemiologist E.A. Batitskaya
Parasitic diseases (from the Greek parasitos – freeloader; synonym – invasive diseases) is a group of diseases caused by animal parasites. More often, these diseases have a cyclical and long course, immunity after a disease is short-lived.
Parasites are organisms that live off another organism (host), using it as a habitat and a source of nutrients.
Animal parasites include:
· Helminths or parasitic worms (more than 200 species). The diseases caused by them are called helminthiases or helminthic infestations. The most common of them are ascariasis (the causative agent of ascaris), enterobiasis (pinworms), schistosomiasis (blood fluke), teniarinhoz (bovine tapeworm), teniasis (pork tapeworm) and others.
· Protozoa (more than 20 species). Diseases – protozoses. The most common: amebiasis, giardiasis, leishmaniasis, malaria, toxoplasmosis, trypanosomiasis.
· Arthropods (insects and mites). Diseases caused by insects – entomoses, ticks – acariasis. The most common acariasis is scabies.
Most parasites, primarily helminths, have a complex development cycle, that is, the stages of development from larva to sexually mature individuals occur under certain conditions either in the external environment, or with a change of hosts, or with a combination of these factors.
Among the variety of parasites, there are also those that cause quite rare diseases.So, in the structure of rare helminthiases, the largest share falls on dirofilariasis , which is registered in 24 constituent entities of the Russian Federation. Since 2011, 3 cases of this disease have been registered in the Leningrad region, including 1 case in our Vsevolozhsk region. In some regions, dirofilariasis is no longer considered a rare disease: in the Rostov region, from 1 to 12 cases are detected annually. Distributed mainly in the southern regions of the European part of the Russian Federation, Western Siberia and the Far East.
Dirofilariasis occurs when roundworms of the genus Dirofilaria (Dirofilaria) are parasitized in the human body. Dirofilariae are up to 18 cm long. Thin filamentous helminths. Human infection occurs through the bites of blood-sucking mosquitoes infected with dirofilaria larvae. In turn, the source of mosquito infection is usually domestic dogs and cats infected with dirofilariae, less often wild animals. In humans, the disease develops slowly and has a long chronic course.Man is a random, dead-end owner of these worms, since in the human body, female worms do not reach sexual maturity, and it is also believed that most of the larvae die when they enter the human body.
In a city apartment, the transmission of the parasite in the presence of a sick dog or cat can be carried out year-round by “basement” mosquitoes. Mosquitoes fly into apartments through the ventilation system of modern multi-storey buildings with central heating.
Clinic (disease symptoms):
Usually, a few days after being bitten by an infected mosquito, a small millet-sized lump develops at the site of the bite, sometimes accompanied by itching.The skin over the lump often has slight redness, sometimes there is moderate swelling. Thus, the first symptom of the disease is a painful swelling in which itching and burning of varying degrees of intensity are felt. Also, a characteristic symptom of dirofilariasis is the movement of the seal or the helminth itself under the skin, which is noted in 10-40% of those infested.
Other symptoms of the disease may be headache, nausea, weakness, fever, severe pain at the site of localization of helminths with the spread of pain along the nerve trunks.
Dirofilaria under the skin of the upper eyelid Dirofilaria in tissue preparation | Most often, dirofilariasis is recorded with the localization of the pathogen under the skin of the eyelids – about 50% of all registered cases. There have been cases of localization of helminths in the mammary gland, upper and lower extremities. In ocular dirofilariasis, the eyelids, conjunctiva, anterior chamber, sclera, orbit are affected. With lesions of the skin of the eyebrows and eyelids, a Quincke-type edema develops, associated with the parasitization of the female / male dirofilaria in the subcutaneous tissue. Characterized by redness of the eyelid skin, their drooping and blepharospasm – a symmetrical contraction of the circular muscles of the eye. Tight nodules, granulomas, or swelling form under the skin. Some patients notice the presence of dirofilaria in the conjunctiva of the eye, looking in the mirror.Visual acuity usually does not decrease. Sometimes intraocular pressure may rise. |
A case of dirofilariasis with atypical localization of the pathogen – in the mesentery of the large intestine – was registered. Dirofilaria 12 cm long was found during an operation for acute appendicitis. In the Leningrad region, there were cases of localization of helminths in the form of an abscess on the elbow joint, lumbar-scapular region, on the anterior abdominal wall. |
Depending on the localization of the parasite in the human body, patients turn to doctors of various profiles: surgeons, oncologists, ophthalmologists, otolaryngologists, infectious disease specialists, therapists, etc. in relation to dirofilariasis, during the season of mosquito activity. It is the presence of an appropriate epidemic history, specific symptoms and clinical manifestations of the disease that helps to suspect dirofilariasis and, after surgical removal of the helminth, confirm the diagnosis by morphological examination and identification of the pathogen.Sometimes the diagnosis is made on the operating table, when a live helminth comes out on its own or is isolated by the surgeon from the removed tissue when examining it or accidentally cutting the cavity of the affected node or granuloma.
Prevention of dirofilariasis:
Measures to prevent infection of humans and animals with dirofilariae include:
mosquito control,
Identification and deworming of infested domestic dogs and cats,
· Prevention of contact of mosquitoes with pets and humans.
Taking into account the variety of parasitic diseases and, above all, animal parasites, main directions of preventive actions can be identified, which in turn will help to protect themselves not only from parasitic diseases, but also from other infectious diseases of bacterial and viral nature:
– Protect yourself from insect attack,
– Swim in bodies of water permitted for these purposes,
– You should drink boiled or bottled water,
– Avoid raw food, food must be thermally processed, especially meat and fish,
– Fresh vegetables, fruits and berries should be washed well with tap water,
– Observe the rules of personal hygiene, wash your hands before eating, before and after using the toilet,
– Take care of your pets and farm animals – don’t forget the vet.
More information on parasitic diseases can be found on the Internet, I recommend the following site – http://www.linmed.ru/readarticle.php?article_id=64#b
90,000 Allergies in dogs – types of allergies, signs and symptoms, treatment of dogs with food allergies
What to do if a dog has a rash and scabs all over the body
Dogs react differently to the same stimuli.Someone eats chicken with pleasure, and someone starts to itch from it. When this reaction becomes too severe, it is called an allergy. This is when a dog’s body perceives simple things like pollen as dangerous and harmful. Outwardly, this can manifest itself as redness, itching, scabs and rashes on the dog’s skin.
Main types of allergies in dogs:
- Food allergy
- Flea saliva allergy
- Allergy to environmental substances
Now let’s see how they differ, and what to do if your dog has just such an allergy.
Signs of Allergy in Dogs
Symptoms for allergies can be the same regardless of the type. These are mainly skin rashes, itching, redness and swelling. Allergy symptoms are most often found in the armpits, face and ears, paws and abdomen
Allergies in dogs are manifested on the skin, ears, open skin areas, paws and abdomen.
Dog Allergy Symptoms:
- Puffiness
- Discharge from ears, eyes, nose
- Redness and breakouts
- Itching
- Bad smell from wool and leather
How allergies manifest in dogs is not so important.Outwardly, all types of allergies may look the same, and the treatment will be different. Therefore, for any signs of allergies, you need to go to the doctor, and not self-medicate.
It will not work to establish the cause of the allergy without a doctor.
Food allergy in dogs
One of the rarest types of allergies. It appears gradually. Therefore, if a dog develops an allergy at the same time as a new diet, it is most likely not a matter of food.
It takes time for a food allergy to manifest itself.Usually, an allergy occurs to a particular type of protein. Most often for chicken and beef, less often for turkey, calf, duck and rabbit. That is why they are often included in hypoallergenic feeds.
Treatment for food allergies in dogs begins with a change in diet. First of all, it is necessary to establish what type of protein the dog is allergic to. Therefore, the old protein source is removed from the diet and replaced with a new one. For example, they stopped feeding beef and switched to duck. This applies to both natural nutrition and ready-made feed.In severe cases of food allergy, the dog is completely transferred to hypoallergenic food.
You can buy food for dogs with food allergies at your veterinary pharmacy.
Anatoly Albesko, Chief Physician, VetSet
It is possible to differentiate the type of allergy only by excluding the influence of food on its occurrence. Currently, the gold standard for diagnosing food allergy is the application of a diagnostic diet with a limited number of components, then a provocative diet, and again a diet with a limited number of components.
For 6-8 weeks (in rare cases up to 10 weeks), the patient should receive only food with a new source of protein. If during this period the itching has completely disappeared, provocative feeding of the dog with the same diet is carried out (1-2 weeks). Resumption of clinical signs confirms the diagnosis of food allergy. If during the period of the diagnostic diet the intensity of itching has not changed, or if the itching has completely disappeared but has not resumed after the provocative diet, food can be excluded as its cause.
In this case, food allergy (atopic dermatitis) is the most likely cause.
If during the period of the diagnostic diet the itching has decreased, but has not completely disappeared, and after the provocative diet has intensified again, it means that the patient, in addition to food allergies, is likely to have a non-food allergy.
Flea allergy in dogs
Flea saliva contains a foreign protein.It is to this that the allergy occurs, which is often called flea allergy in dogs. When a flea bites a dog, toxic protein enters the bloodstream along with the saliva. Therefore, symptoms may persist even after you have removed fleas from your dog. Flea allergies are more common in summer and autumn. This seasonality is due to the fact that at this time fleas feed more actively before hibernation.
To cure an allergy to flea saliva, you need to remove the very cause – fleas. Collars, special shampoos are used.The veterinarian may prescribe medications. The complexity of this allergy lies in the fact that you may not find fleas on the dog. To start an allergy, one bite on the street is enough. In addition, all dogs itch in different ways: someone will comb it so that the owner will not stand it, and other dogs will not even notice.
How to remove fleas from a dog
It is not difficult to remove fleas from the dog itself. However, everyone forgets that fleas do not live on a dog, but on mats and carpets, and even under a baseboard.To cope with flea allergies, you need to remove the parasites themselves from everywhere. Do not forget to clean not only the dog, but also its sleeping place.
Read more in the article How to remove fleas from a dog
Allergy to environmental substances
The reaction to external stimuli – pollen, dust, mold, even grass – is called atopic dermatitis. After flea allergies, this is the most common type. It usually appears between 10 months and 3 years of age.
Atopic dermatitis cannot be cured; you can only make your dog’s life comfortable enough. Sometimes prevention or relocation helps. For example, if your dog is allergic to dust, frequent cleaning, replacing carpets with parquet floors, or moving to the countryside may reduce symptoms.
Unusual types of atopic dermatitis
- Allergy to the sun. Dogs with such allergies have to walk early in the morning and late in the evening when there is no sunlight.
- Host allergy. The dog reacts to specific substances that are contained in the particles of the owner’s skin and hair.
- Allergy to perfumery. It is especially dangerous if the owner uses this perfume.
Diagnosis of Allergy in Dogs
There is a wide range of methods and research to identify allergies in a dog. It will not be possible to do this in only one way, and a comprehensive study is always needed.This is because different types of allergies can have the same symptoms. Therefore, the task of the veterinarian is to consistently eliminate each of the possible options.
It all starts with taking anamnesis. The doctor asks about how the dog is kept, where he lives and sleeps, what vegetation is at home and near the house, that the dog eats every day. You should know the answers to these questions if you are taking someone else’s dog to the doctor. The visit will be useless without answers.
Allergy Treatment in Dogs
Not all allergies can be cured forever:
- Food allergies in dogs.From the diet, you need to exclude the product to which the allergy appears.
- Allergy to food in dogs. It is necessary to change the feed itself, for example, switch to another brand. You can keep the same brand of feed, but replace the base. For example, go from duck to rabbit.
- Flea saliva allergy. Regularly use flea medications: collars, shampoos, etc.
- Allergy to external stimuli. Eliminate contact with objects that cause allergies.Remove carpets from the house, put boots on the dog’s paws to exclude contact with pollen and grass.
What can you give your dog for allergies
Sometimes you don’t have to give anything. With food allergies, it is enough to exclude a certain type of protein from the diet. For example, go from beef to duck. However, only a doctor can establish this. The same goes for antihistamines. It is not worth giving them the first signs of allergies in dogs, because not all animals even react to them.
If you suspect your dog is allergic, see a dermatologist.
How to prepare for a visit to a dermatologist
It is a big mistake to wash or hide symptoms in a dog. If there are rashes on the skin, do not smear them with brilliant green. If there is discharge, do not wash it off before visiting your doctor. The dermatologist must see the problem overt.
90,000 Skin growths – from wart to melanoma.Looking for the reason in Angio Line
In medical practice, the term “growth” is used instead of the term “neoplasm”.
Neoplasms are divided into benign and malignant.
Benign grows slowly without destroying the surrounding cells. Often their growth stops completely.
Malignant neoplasms deform adjacent tissues, grow chaotically and irregularly, causing complications.
Benign growths:
Warts
The growths are caused by the human papillomavirus as a result of immune diseases or metabolic disorders.Most of them are harmless, only warts larger than 0.5 cm are dangerous, flat or without clear contours and ovoid.
Moles
Formations that have arisen due to excess of the coloring substance in the skin – melanin. Some of them can transform into malignant neoplasms – melanomas. To do this, the mole should look like a knot, dry, hairless, or bleeding.
Fibroids
Formations that look like a nodule that has grown deep into the skin and protrudes from it.The surface of the fibroids is smooth and even, sometimes they turn into a malignant tumor – fibrosarcoma.
Fats
Tumors of the fatty layer that do not change skin color. They are transferred painlessly and easily slide to the side with a finger. Formed on areas of the body that are poor in adipose tissue: thighs, shoulder blades, on the upper back.
Atheromas
Formations resulting from blockage of the sebaceous gland duct.
Painful to the touch, inflamed atheromas secrete purulent contents.
Occur in places of increased sweating.
Hygroma
Cysts that appear in the area of joints and tendons. Hygromas do not change skin color, protrude strongly above the level of the body.
They are usually harmless and painless.
Hemangiomas
Formations from cells of capillary or venous vessels of red and blue-black color.
Malignant growths:
Lymphomas
Tumors formed due to diseases of the lymphatic tissue.They are characterized by enlarged lymph nodes. On the skin they appear in the form of fungal mycosis, Sesari’s syndrome, primary anaplastic form, lymphomatoid papulosis.
Myelomas
Formations arising from blood plasma cells. They are initially formed in the ribs, spine and bones of turtles.
Secondary myeloma can manifest on the skin.
Carcinomas
Cancers from epithelial tissue. Carcinomas grow rapidly, metastasizing to cells and organs.
A type of carcinoma develops on the skin – basilioma . The swelling appears on the neck or face, forming ulcerating nodules. Basilioma most often does not metastasize, but during development it destroys the surrounding tissues.
Another variety, squamous cell carcinoma , forms nodules, cracks, ulcers, plaques on the skin and rapidly increases, metastatic.
A common cause of carcinoma is an abundance of ultraviolet radiation.
Melanomas
Dangerous tumors arising from an excess of melanin.They develop rapidly, metastasizing and affecting internal organs.
Melanoma causes itching, increases in size, hair falls out, ulcerates and bleeds.
At the initial stage, it looks like a mole.
In appearance, only a dermatologist can distinguish the nature of the neoplasm. Do not postpone the trip to him and diagnose.
Be healthy with Angio Line.
How to care for the skin of a newborn.
After leaving the hospital, mother and baby gradually get used to the daily routine.The baby should eat well and be warm – this is the first on the list. It is equally important to care for the baby’s skin, which is very delicate and sensitive to external stimuli. To adapt to a new environment, a baby needs time and parental care. Chemicals, fragrances, dyes in clothes, detergents cause redness, diaper rash or rashes. How to properly care for the skin of a newborn to protect the baby from contact dermatitis, allergies, and other rashes?
Bathing
The baby is born with a protective coating that exfoliates in the first week.During this period, there is no need to bathe the baby or use baby lotions and creams.
A full bath is normal from the first days of a baby’s life, the main thing is to adhere to the rules:
– bathe your baby in a warm room.
– water should be at body temperature: 36-37 degrees to the touch.
– make sure the necessary items for the procedure are within reach. – remove jewelry that could scratch the baby.
– Hold the newborn firmly by raising your head above the water.
– Do not use cotton swabs to clean your nose and ears.
– To wash your baby’s face, use soap-free water.
– Never leave your baby unattended while bathing, even for a moment.
– For the first 2-3 months after birth, give up shampoo and soap, which can cause an allergic reaction in the baby.
– if you do use baby bath products, make sure they are soft, baby-friendly and odorless.
– then carefully wrap the baby in a cotton towel or a special bathrobe-corner for newborns.
– the room in which the baby will be after the bath must be warm, and air conditioners and fans must be turned off to avoid colds.
Umbilical cord care
By the time of discharge from the hospital, this organ, which connected the mother and baby for all 9 months of pregnancy, will begin to dry out.Gradually, the umbilical cord will atrophy and fall off within 1-2 weeks. Until then, the place of its attachment to the belly of the newborn must be kept clean and dry. All that is needed for this is plain water. You cannot pull the keratinized part, even if it begins to fall off. The process will end on its own. To avoid damaging your baby’s delicate skin, buy newborn diapers that have a notch for an unhealed navel on their belt. If you are using a regular diaper, fold the edge so that the fabric does not chafe your tummy.In some cases, the child may need a doctor. See your pediatrician if your child has a temperature rise of 38 ° C or higher at the same time as changes in the navel: the area becomes red and swollen; oozing yellow pus; an unpleasant smell is felt. Many mothers are worried about the appearance of small specks of blood on the baby’s undershirt or diaper, the sleeping place of the child. Minor bleeding is normal.
Diapers and diapers
Change diapers often as soon as you notice that they are wet or dirty.Leaving it on for too long can cause infections. For newborn hygiene, thoroughly clean the genital area after each diaper change. Rinse your baby under warm running water to prevent irritation. Allow the skin to air dry for a few minutes or dry it gently with a soft towel. Use baby wipes less frequently to care for your newborn’s skin. Fragrances and alcohol in them can cause irritation and cause rashes. Make sure you buy diapers in a size that suits your baby.If the baby’s skin in the diaper area is irritated, choose a different brand or temporarily stop using them. … Wash reusable diapers and diapers with a mild, unscented detergent or clean hot water. Most diaper rashes on a newborn’s skin are harmless, but some may be a sign of infection and need care. If the baby’s skin is very red, itchy, painful, contact a pediatrician immediately.
What to do in case of skin problems
In the first months after birth, a baby may develop a rash, irritation, diaper rash, which seem unusual to parents.
Most of the skin problems in a newborn do not need treatment:
– baby acne – small red rash on the face. As a rule, it disappears over time without intervention.
– milia – tiny whiteheads on the baby’s face.
– Erythema is a common patchy rash that can affect newborns. In some, it looks like yellow or white bumps surrounded by a red halo. The rash tends to migrate to different parts of the body.Most often occurs on the second day of life, but may appear at birth or within the first two weeks. There is no cure – erythema gradually goes away on its own.
Eczema
This rash appears as red bumps that may fester. It usually appears on the forehead, cheeks, or scalp, and sometimes spreads to other parts of the body. The risk group includes babies who are allergic from birth or have a genetic tendency to the disease.In case of pathology, it is recommended to use special moisturizers: ointments, creams, oils. You should not bathe a baby for a long time with this disease. When an allergic rash appears, consultation with a pediatrician is required.
Diaper rash
Causes of occurrence:
– late diaper change. The urine or stool in the diaper irritates the newborn’s skin, causing red, weeping spots.
– bacterial or yeast infection. Taking antibiotics can cause the growth of Candida fungi. Usually appears around the genitals and buttocks of the baby. Looks like red spots with a whitish coating.
How to properly care for your skin to prevent diaper rash:
-Do not use reusable diapers frequently.
– Give up talcum powder: it dries out the skin of the newborn.
– Arrange half-hour air baths.
Prickly heat
Heat rash causes overheating of the body. It is usually visible in the folds of the baby’s skin.

