Sphincter Muscle Cramp: Understanding Symptoms, Causes, Diagnosis, and Treatment Options
What are the symptoms of sphincter muscle cramp. How is proctalgia fugax diagnosed. What treatment options are available for chronic proctalgia fugax. Can stress trigger sphincter muscle spasms. How does proctalgia fugax differ from levator syndrome.
What is Sphincter Muscle Cramp and Proctalgia Fugax?
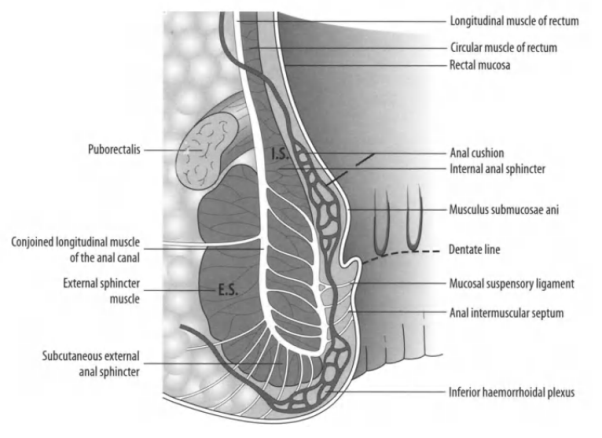
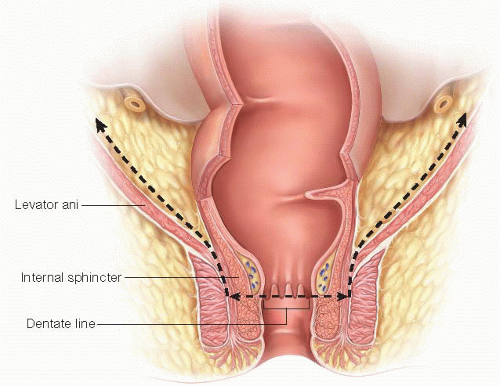
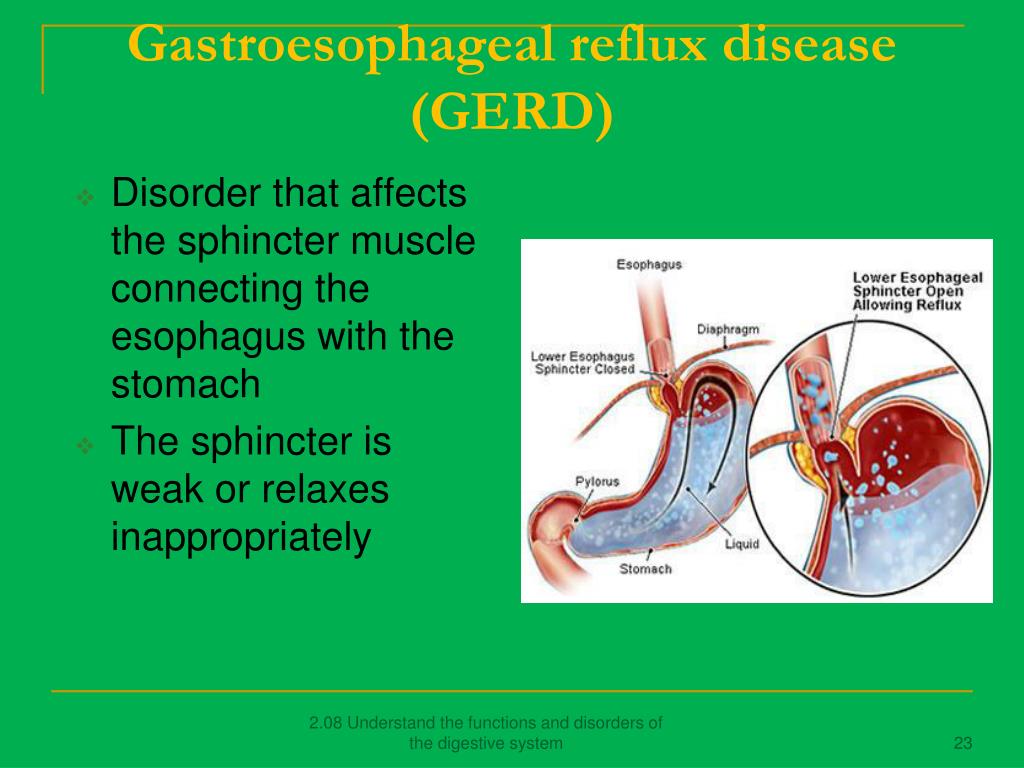
Sphincter muscle cramp, also known as proctalgia fugax, is a condition characterized by sudden, intense pain or cramping in the buttocks and rectal area. This discomfort is caused by spasms or contractions of the pelvic floor muscles, anal sphincter muscles, or rectum muscles. Proctalgia fugax is often unpredictable, making it challenging for doctors to diagnose and researchers to study effectively.
The rectum, which is the final segment of the large intestine ending at the anus, plays a crucial role in removing solid waste from the body. When the muscles in this area experience involuntary contractions, it can lead to the uncomfortable symptoms associated with proctalgia fugax.
Recognizing the Symptoms of Proctalgia Fugax
Proctalgia fugax is characterized by temporary rectal pain that can vary in intensity and duration. The primary symptoms include:
- Sudden, intense pain in the rectum and buttocks
- Cramping sensations lasting from a few seconds to several minutes
- Pain severe enough to wake you from sleep or interfere with daily activities
- Absence of pain or discomfort between episodes
In cases of chronic proctalgia fugax, episodes may last longer than 20 minutes and occur more frequently. Additional long-term symptoms can include:
- Discomfort from prolonged sitting
- Painful bowel movements
Is proctalgia fugax a serious condition?
While proctalgia fugax can be extremely uncomfortable and disruptive, it is generally not considered a serious medical condition. However, if you experience persistent or severe symptoms, it’s important to consult with a healthcare professional to rule out other potential underlying causes and receive appropriate treatment.
Differentiating Proctalgia Fugax from Levator Syndrome
Proctalgia fugax is a form of levator syndrome, but there are key differences between the two conditions:
- Duration: Proctalgia fugax is typically temporary, while other types of levator syndrome can last for several days.
- Pain location: Proctalgia fugax pain is primarily felt in the rectum, whereas levator syndrome pain can be more widespread, affecting the pelvic floor, thighs, and buttocks.
- Pain position: Levator syndrome symptoms are usually felt higher in the pelvis compared to proctalgia fugax.
- Effect of posture: Levator syndrome symptoms often worsen when sitting and improve when standing or lying down.
How can I distinguish between proctalgia fugax and other anorectal conditions?
To differentiate proctalgia fugax from other anorectal conditions, pay attention to the duration and location of the pain, as well as any accompanying symptoms. While proctalgia fugax typically causes brief, intense episodes of rectal pain, other conditions like hemorrhoids or anal fissures may cause more persistent discomfort or bleeding. If you’re unsure about your symptoms, consult a healthcare professional for an accurate diagnosis.
Exploring the Causes of Proctalgia Fugax
The exact causes of proctalgia fugax can be challenging to pinpoint, as they may vary from person to person. Some potential triggers and contributing factors include:
- Stress and anxiety
- Sexual activity
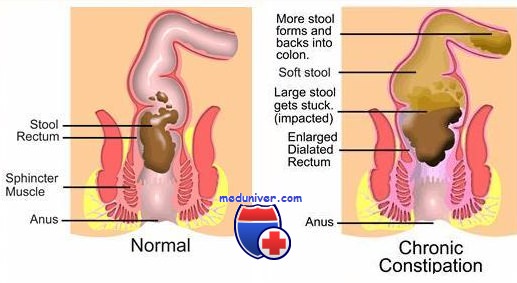
- Constipation
- Abnormal bowel movements
- Menstruation
Research has shown a possible connection between stress and proctalgia fugax, with some individuals experiencing spasms shortly after feeling stressed. Similarly, studies have indicated a relationship between stress and levator syndrome, with many affected individuals also experiencing psychosocial distress, including depression and anxiety.
Can dietary factors contribute to proctalgia fugax?
While there is limited research on the direct impact of diet on proctalgia fugax, maintaining a healthy diet rich in fiber may help prevent constipation and reduce the strain on anorectal muscles during bowel movements. This, in turn, could potentially lower the risk of proctalgia fugax spasms. However, more research is needed to establish a definitive link between dietary factors and the condition.
Diagnostic Approaches for Proctalgia Fugax
Diagnosing proctalgia fugax can be challenging due to the quick and random nature of the spasms. There are no specific tests for the condition, but healthcare professionals typically focus on ruling out other possible causes of anorectal pain. The diagnostic process may include:
- Symptom history: Keeping an accurate record of when spasms occur, their duration, severity, and any preceding events can help your doctor make a more informed diagnosis.
- Physical examination: Your doctor may perform a physical exam to check for areas of tenderness in the rectum or pain when the area is touched. This can help identify potential causes of proctalgia fugax and rule out other conditions.
- Differential diagnosis: Your healthcare provider will consider other anorectal conditions that may cause similar symptoms, such as:
- Hemorrhoids
- Ulcers or abscesses
- Anal fissures
- Inflammatory bowel disease
What diagnostic tests might be used to rule out other anorectal conditions?
While there are no specific tests for proctalgia fugax, your doctor may recommend various diagnostic procedures to rule out other anorectal conditions. These may include:
- Digital rectal examination
- Anoscopy or proctoscopy
- Colonoscopy
- Imaging studies such as MRI or CT scans
The choice of diagnostic tests will depend on your specific symptoms and medical history.
Treatment Options for Proctalgia Fugax
Treatment for proctalgia fugax primarily focuses on managing symptoms and alleviating pain and discomfort. Since episodes are typically short-lived and irregular, treatment approaches may vary based on individual symptoms and severity. Some common treatment options include:
At-home treatments:
- Over-the-counter antispasmodic drugs
- OTC muscle relaxers and pain relievers
- Warm baths
- Heating pads and ice packs
- Increasing fiber intake to promote softer bowel movements
Medical interventions:
- Botox injections around the anorectal area to relax muscles
- Other types of injections to stop muscle spasms in severe cases
How effective are at-home treatments for managing proctalgia fugax symptoms?
At-home treatments can be effective for many individuals experiencing proctalgia fugax. Simple measures like warm baths, heating pads, and over-the-counter pain relievers may provide relief during episodes. Increasing fiber intake can also help prevent constipation and reduce strain on anorectal muscles. However, the effectiveness of these treatments can vary from person to person, and it’s important to consult with a healthcare professional before starting any new treatment regimen.

Lifestyle Modifications and Prevention Strategies
While it may not always be possible to prevent proctalgia fugax entirely, certain lifestyle modifications may help reduce the frequency and severity of episodes:
- Stress management: Practice relaxation techniques, such as deep breathing exercises, meditation, or yoga to help reduce stress and anxiety.
- Dietary changes: Increase fiber intake to promote regular, soft bowel movements and reduce strain on anorectal muscles.
- Exercise: Regular physical activity can help improve overall muscle tone and reduce stress levels.
- Proper hydration: Drink plenty of water to help prevent constipation and maintain healthy bowel function.
- Toilet habits: Avoid straining during bowel movements and limit time spent sitting on the toilet.
Can pelvic floor exercises help prevent or manage proctalgia fugax?
Pelvic floor exercises, also known as Kegel exercises, may potentially help some individuals manage proctalgia fugax by improving muscle control and strength in the pelvic area. However, the effectiveness of these exercises for proctalgia fugax specifically has not been extensively studied. It’s best to consult with a pelvic floor physical therapist or healthcare provider before starting any new exercise regimen to ensure it’s appropriate for your individual situation.
When to Seek Medical Attention
While proctalgia fugax is generally not a serious condition, there are certain circumstances where medical attention is warranted:
- Persistent or worsening symptoms
- Pain that interferes significantly with daily activities or sleep
- Presence of other concerning symptoms, such as rectal bleeding or changes in bowel habits
- Suspicion of other underlying anorectal conditions
If you experience any of these situations, it’s important to consult with a healthcare professional for a proper evaluation and appropriate treatment plan.
How can I prepare for a medical appointment regarding proctalgia fugax?
To make the most of your medical appointment, consider the following preparations:
- Keep a detailed symptom diary, noting the frequency, duration, and severity of episodes
- Record any potential triggers or factors that seem to worsen or alleviate symptoms
- Make a list of all medications and supplements you’re currently taking
- Prepare questions about your condition, potential treatments, and lifestyle modifications
- Be ready to discuss your medical history and any family history of anorectal conditions
This information will help your healthcare provider make a more accurate diagnosis and develop an effective treatment plan.
Symptoms, Causes, Diagnosis, and Treatment
Written by WebMD Editorial Contributors
Medically Reviewed by Dan Brennan, MD on April 28, 2021
- Symptoms
- Proctalgia Fugax vs. Levator Syndrome
- Causes
- Diagnosis
- Treatment
Pain is part of life. Headaches, stiff knees, and sudden back pain may make you feel uncomfortable. Similarly, you may have pain in your buttocks.
Proctalgia fugax is pain or cramping felt around your buttocks and rectum. The rectum is the last part of the large intestine, ending in the anus, which removes solid waste from the body.
This pain is the result of spasms or cramps of your pelvic floor muscles, anal sphincter muscles, or rectum muscles. Because proctalgia fugax is unpredictable, it is difficult for doctors to diagnose or researchers to study.
Proctalgia fugax is temporary rectal pain. You may have intense pain for a short time. Cramps in your rectum may last from a few seconds to several minutes.
Severe episodes of proctalgia fugax can be painful enough to wake you up from your sleep or keep you from going to work or school. Between episodes, you probably won’t have any pain or discomfort. If you do have pain that isn’t coming from another spasm, another anorectal condition may be causing it, so talk to your doctor to rule out other conditions.
Chronic proctalgia fugax. Episodes of chronic proctalgia fugax usually last for more than 20 minutes and happen more often than occasionally. Other long-term symptoms include discomfort from sitting for too long and painful bowel movements.
Proctalgia fugax is a form of levator syndrome (also called levator ani syndrome). Both include spasms of muscles in the pelvic area. Proctalgia fugax is temporary, but other types of levator syndrome can last for several days.
Another major difference is the location of the pain. Pain from proctalgia fugax is felt mainly in the rectum. Pain due to levator syndrome is felt in the pelvic floor — specific or vague areas — and in the thighs and buttocks.
Symptoms of levator syndrome are usually felt higher in the pelvis than the symptoms of proctalgia fugax. You may notice that symptoms worsen when sitting and improve when standing or lying down.
Finding the cause of proctalgia fugax may be difficult. The causes vary from person to person and need different approaches for treatment. Other conditions in the anorectal area may cause spasms that seem similar to proctalgia fugax but are diagnosed and treated as separate issues. Sometimes an underlying condition causes proctalgia fugax, and treating that condition will relieve the symptoms of proctalgia fugax.
Stress. Proctalgia fugax may be related to stress and anxiety. In some cases, people with proctalgia fugax felt stressed just before the spasms.
Studies have shown a similar relationship between stress and levator syndrome. Many people with levator syndrome have psychosocial distress, including depression and anxiety.
The following activities may cause proctalgia fugax:
- Sexual activity
- Constipation
- Abnormal bowel movement
- Menstruation
Proctalgia fugax is difficult to diagnose because of how quick and random the spasms can be.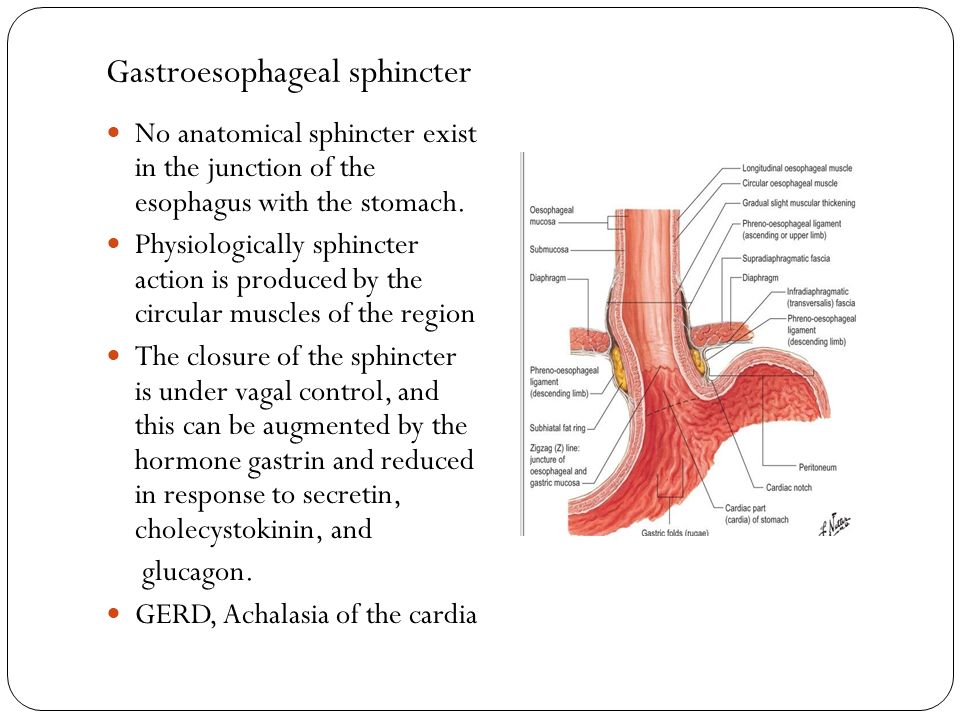 There are no tests for proctalgia fugax. But your doctor will rule out other possible causes for your anorectal pain.
There are no tests for proctalgia fugax. But your doctor will rule out other possible causes for your anorectal pain.
Other anorectal conditions your doctor may check for are:
- Hemorrhoids
- Ulcers, abscesses, or other abnormal growths
- Anal fissures, or small tears
- Inflammatory bowel disease
History. Your doctor may make a diagnosis based on your symptom history. Keep an accurate record of when the spasms happen, how long they last, how severe they are, and what happened before the spasms to help your doctor make a better diagnosis.
Physical exam. Your doctor may do a physical exam to check for places of tenderness in the rectum, or pain when the area is touched. Tenderness in the rectum or its nerves can be the cause of proctalgia fugax. A similar physical exam is performed to rule out any other conditions that cause anorectal pain.
Most treatment options for proctalgia fugax depend on the symptoms. Treatments aim to ease pain and discomfort. This is mainly because the episodes are short, irregular, and without a clear cause.
Treatments aim to ease pain and discomfort. This is mainly because the episodes are short, irregular, and without a clear cause.
At-home treatment. Before trying treatment options, check with your doctor to rule out other causes. You can take care of your symptoms on your own with the following methods:
- Over-the-counter (OTC) antispasmodic drugs
- OTC muscle relaxers and pain relievers
- Warm baths
- Heating pads and ice packs
Another at-home method that may help you avoid proctalgia fugax is to eat more fiber. Fiber will allow you to have softer bowel movements. These will keep your anorectal muscles from working too hard and may lower the risk of proctalgia fugax spasms.
Injections. For more severe pain, your doctor may recommend a variety of injections to stop muscle spasms. A Botox injection around the anorectal areas will relax the muscles. An epidural injection or a local anesthetic will numb the pelvic areas to ease muscle spasms.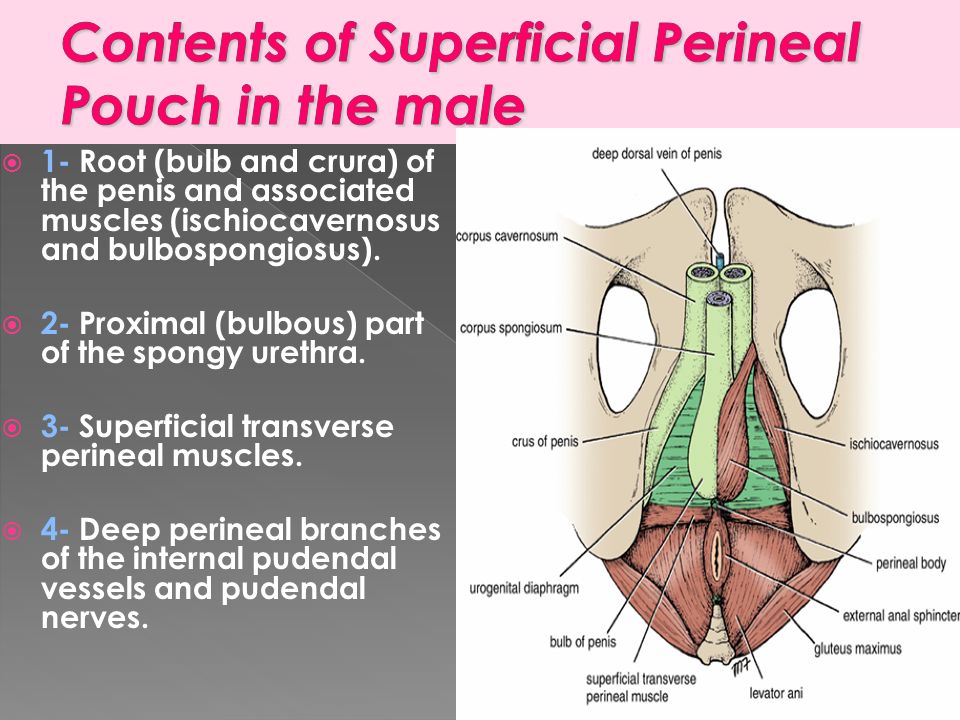
Electrical stimulation. For severe proctalgia fugax, electrical stimulation of the anorectal muscles may provide relief. This treatment option involves inserting a small, finger-sized probe into the rectum and using a low voltage current to relax spastic muscles through vibration.
Top Picks
Proctalgia Fugax: Causes, Symptoms, and Treatments
Proctalgia fugax is anal pain with no specific cause. It occurs from intense muscle spasms in or around the canal of the anus. It can be severe enough to impact your day-to-day life.
It can be severe enough to impact your day-to-day life.
Anyone can experience proctalgia fugax. But it doesn’t usually affect anyone prior to the start of puberty and seems to affect more women than men, according to one 2017 review.
The symptoms of proctalgia fugax are:
- muscle spasms in or around the lower rectum area or in or around the canal of the anus
- pain that happens suddenly and usually without warning
- pain that lasts for only a few seconds, although it can last up to 30 minutes in some cases
These episodes may be severe enough to keep you home from work. They may limit your other activities until the episode is over.
The pain will usually stop on its own. People with proctalgia fugax don’t have any anal pain between spasms. There can be long periods of time between spasms.
The pain or spasms that occur at night may be painful enough to wake you from sleep. They can also occur during the day.
Proctalgia fugax isn’t known to have specific triggers. But a 2005 study suggested that it may be caused by an issue with the pudendal nerves. It often happens after an injection procedure for hemorrhoids called sclerotherapy or after a vaginal hysterectomy.
But a 2005 study suggested that it may be caused by an issue with the pudendal nerves. It often happens after an injection procedure for hemorrhoids called sclerotherapy or after a vaginal hysterectomy.
Other possible triggers may be:
- sexual activity
- menstruation
- constipation
- defecation
- stress
Despite some evidence that there are some possible triggers like those listed above, it’s also common for proctalgia fugax to occur without anything triggering it.
Proctalgia fugax is normally diagnosed after other possible causes of anal pain and spasms have been ruled out. In order to rule out other conditions that may be causing the pain, your doctor may:
- conduct a physical exam
- ask questions about the pain severity, duration, etc.
- check for hemorrhoids, fissures, an abscess, and other diseases or conditions that might cause anal pain
Once other conditions have been ruled out as the cause of your pain, your doctor will be able to diagnose proctalgia fugax.
Anal pain is classified according to three types. Each of the three types has unique characteristics.
Proctalgia fugax: As described above, this type is characterized by intermittent pains in the rectum that can last up to 30 minutes.
Levator ani syndrome: This type features pain or tenderness in the pelvic area and rectum that’s more lasting and may result in discomfort sitting for long periods. People with this condition experience pain in the rectum during a digital rectal exam.
Unspecified functional anorectal pain: This type features pain or tenderness in the pelvic area and rectum similar to levator ani syndrome, but no pain during a digital rectal exam.
There are several treatment options, but getting relief from the symptoms is different for each person. Since there isn’t a specific cause, treatment focuses on managing the symptoms. If a trigger has been identified, then that trigger should also be managed./2549387-article-causes-of-calf-pain-5a70fb720e23d90036a5fa54.png)
At-home treatments
Home treatments focus on relieving the pain from the spasms. Options include:
- warm baths or sitz baths
- relaxation techniques
- over-the-counter pain medications
- ointments prescribed by a doctor, like glyceryl trinitrate or topical diltiazem
Injections
If your spasms are severe, you may be a candidate for Botox injections in the area.
Electrical stimulation
This treatment works by the use of a probe inserted into the anus that carries electric stimulation. This can help to block the transmission of pain signals to the brain.
Biofeedback
This treatment uses attached electrodes to guide you in feeling what happens when the pelvic floor is tensed and relaxed. It can help you learn how to relax the pelvic floor muscles to relieve discomfort.
While proctalgia fugax doesn’t have a specific cause, there are some conditions that may be associated or that commonly occur at the same time.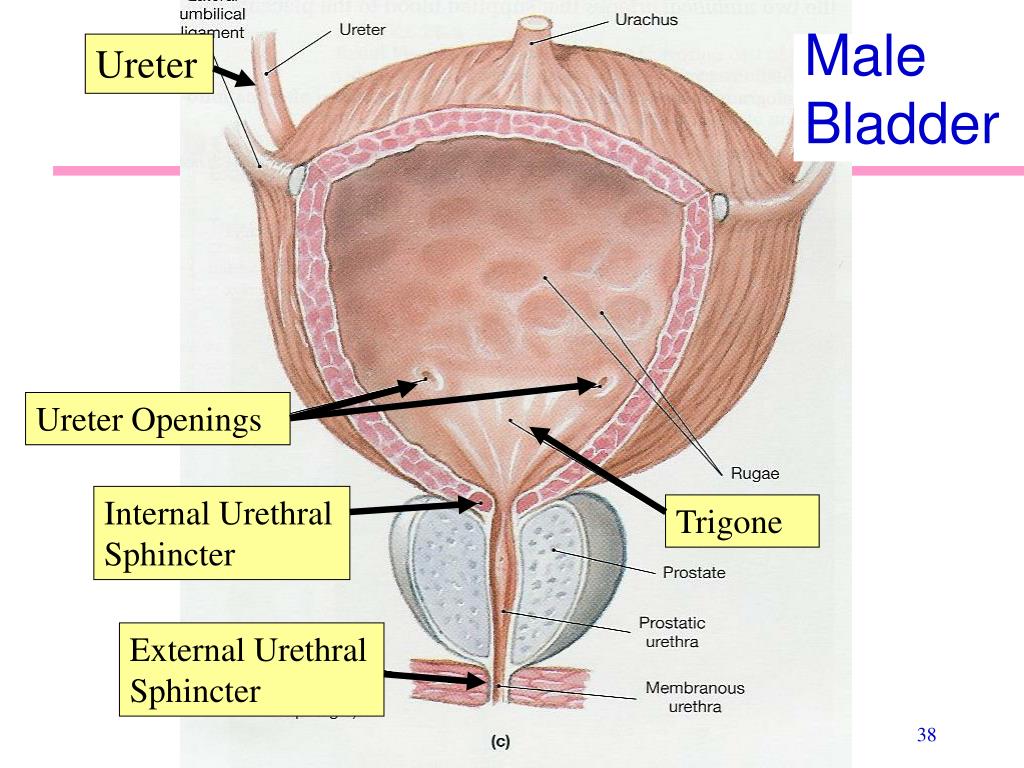 Some of these include menstruation and constipation.
Some of these include menstruation and constipation.
Many times, an episode of these painful anal spasms can be associated with psychological issues like anxiety, depression, or stress.
Other conditions that may have an association with proctalgia fugax are anal fissures and abscesses, as well as rectal cancer.
If you have anal pain of any kind, it’s important that you discuss it with a medical professional. This pain can be a symptom of a disease or condition that needs to be addressed.
But if no other condition or disease is found to be causing the pain, and you’re diagnosed with proctalgia fugax, there are treatments that can help manage the episodes.
If the pain and spasms seem to be related to times when you have an increase in stress or feel depressed, counseling or therapy may be recommended.
Anal sphincter spasm – causes, symptoms, diagnosis and treatment
Anal sphincter spasm is a pathological condition in which involuntary painful contractions of the smooth muscles surrounding the anus are observed.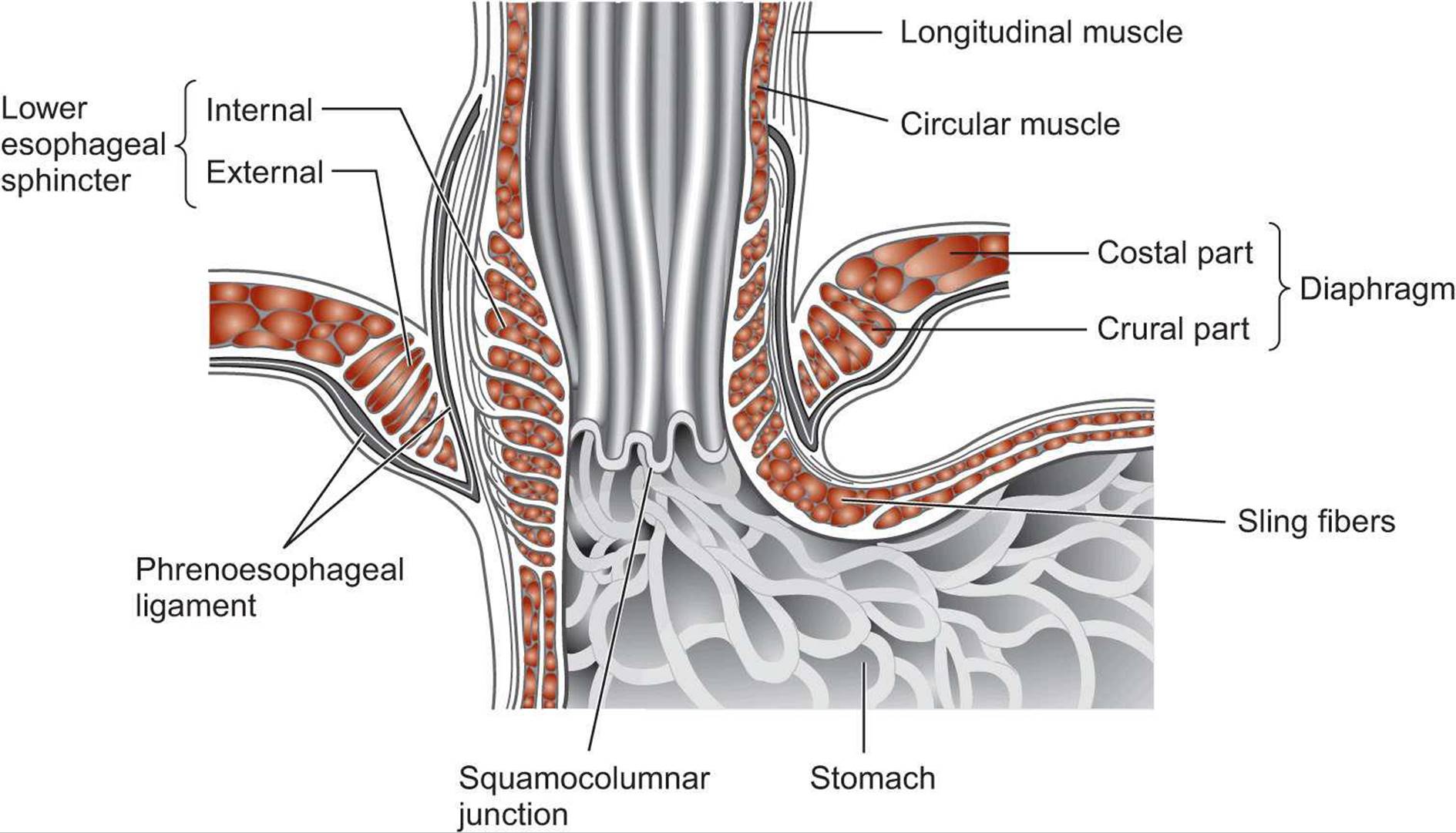 It can develop with some injuries and diseases of the rectum and anus, disorders of innervation, autonomic disorders and emotional instability. Spasm of the anal sphincter is accompanied by pain radiating to the coccyx, abdomen, perineum, etc. It is diagnosed on the basis of complaints, anamnesis, rectal examination, sigmoidoscopy, colonoscopy and irrigoscopy. Treatment – diet, antispasmodics, analgesics, physiotherapy, surgery.
It can develop with some injuries and diseases of the rectum and anus, disorders of innervation, autonomic disorders and emotional instability. Spasm of the anal sphincter is accompanied by pain radiating to the coccyx, abdomen, perineum, etc. It is diagnosed on the basis of complaints, anamnesis, rectal examination, sigmoidoscopy, colonoscopy and irrigoscopy. Treatment – diet, antispasmodics, analgesics, physiotherapy, surgery.
General information
Anal sphincter spasm is a fairly common pathological condition that occurs as a result of disorders of innervation and autonomic regulation, traumatic injuries, operations, chronic diseases or severe emotional instability. The main symptom of anal sphincter spasm is pain in the anus (proctalgia) of varying duration and intensity. Mostly middle-aged people suffer, the disease is equally common in patients of both sexes.
Spasm of the anal sphincter tends to be prolonged. It negatively affects the quality of life, accompanied by emotional and mental exhaustion. Cancerophobia is possible, due to the initial mental instability and the tendency of many patients to neurotic reactions. Treatment of anal sphincter spasm is mainly carried out by specialists in the field of clinical proctology. In the presence of severe mental disorders, the participation of a psychologist or psychotherapist is required.
Cancerophobia is possible, due to the initial mental instability and the tendency of many patients to neurotic reactions. Treatment of anal sphincter spasm is mainly carried out by specialists in the field of clinical proctology. In the presence of severe mental disorders, the participation of a psychologist or psychotherapist is required.
Anal sphincter spasm
Causes
Anal sphincter spasm belongs to the category of polyetiological diseases and can be primary or secondary. In the absence of organic changes, they speak of a primary disorder. The cause of the development of the primary spasm of the anal sphincter is viscero-neurotic disorders and mental instability. The disease is often detected in individuals with a pronounced hysterical component, neurasthenia, increased emotional lability and vegetative-vascular dystonia.
Secondary spasm of the anal sphincter occurs against the background of conditions accompanied by the appearance of organic changes and functional disorders in the anus and lower rectum.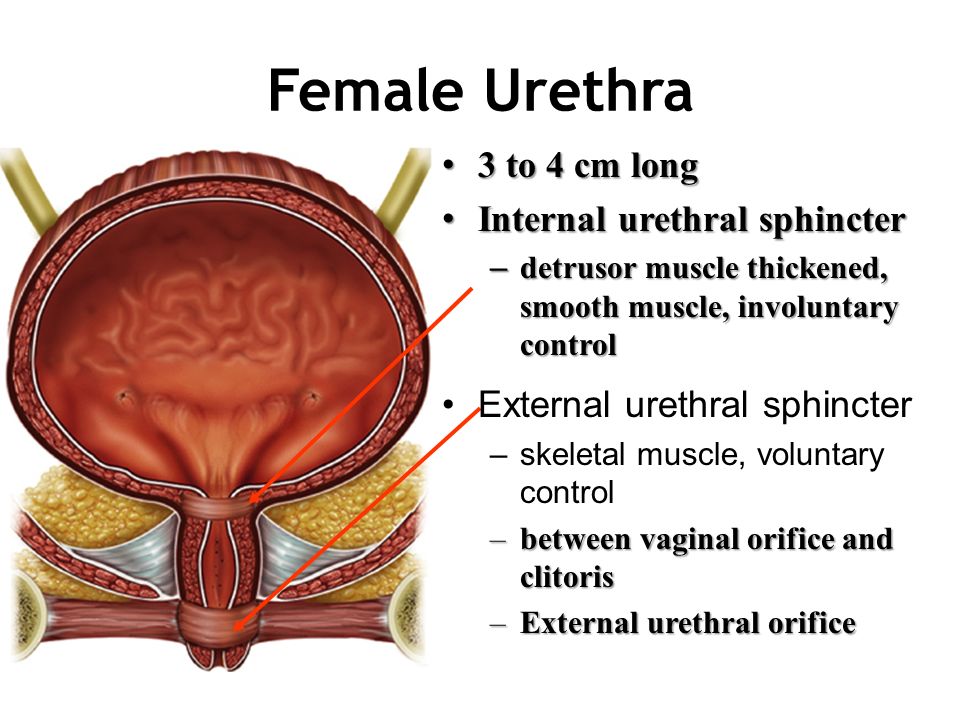 Among the common causes that cause the development of this pathology are chronic diseases of the anus, such as hemorrhoids and anal fissure. In addition, spasm of the anal sphincter can be provoked by inflammatory processes in the lower intestine (Crohn’s disease, ulcerative colitis), benign and malignant tumors of the rectum, constipation, trauma to the sacrum and coccyx, complicated childbirth, surgical interventions and adhesions in the pelvic area.
Among the common causes that cause the development of this pathology are chronic diseases of the anus, such as hemorrhoids and anal fissure. In addition, spasm of the anal sphincter can be provoked by inflammatory processes in the lower intestine (Crohn’s disease, ulcerative colitis), benign and malignant tumors of the rectum, constipation, trauma to the sacrum and coccyx, complicated childbirth, surgical interventions and adhesions in the pelvic area.
Pathogenesis
There are a large number of nerve endings and blood vessels in the posterior wall of the rectum. Violations of the normal functioning of this part of the intestine are accompanied by the appearance of many nerve impulses that cause a reflex contraction of the smooth muscles surrounding the external and internal sphincters of the anus. With intense stimulation of this reflexogenic zone, individual contractions can turn into spasms of the anal sphincter of various durations. Such spasms, in turn, entail a violation of the blood supply to the rectum and surrounding tissues, cause even more irritation of the nerve endings and exacerbate muscle contraction, which provokes the emergence of a “vicious circle”.
Symptoms
The characteristic manifestations of anal sphincter spasm are pains of varying duration and intensity, radiating to the coccyx, perineum, hip joints or lower abdomen. Pain during spasm is paroxysmal, may appear during defecation or occur without apparent connection with the state of the rectum (empty or not emptied) and other circumstances. There is a low effectiveness of analgesics, while the pain syndrome often disappears or weakens after the completion of a bowel movement or taking a warm bath.
Spasm of the anal sphincter can be provoked not only by the act of defecation, but also by chronic stress, acute emotional and psychological stress, overwork, heavy physical exertion and some neurological diseases. At the same time, spasm of the anal sphincter often itself becomes an impetus for the occurrence of prolonged stress, increased emotional instability and the development of mental disorders of a neurotic level.
Depending on the type of pain syndrome, there are two forms of anal sphincter spasm: with prolonged and short-term proctalgia. With short-term proctalgia, the pain is strong, pulling or stabbing. Due to the high intensity of the pain syndrome and its irradiation to neighboring anatomical regions, patients suffering from anal sphincter spasm often find it difficult to determine the localization of pain and may regard this symptom as a manifestation of diseases of the reproductive or urinary system. With prolonged proctalgia, pain is usually less intense, poorly relieved by analgesics.
With short-term proctalgia, the pain is strong, pulling or stabbing. Due to the high intensity of the pain syndrome and its irradiation to neighboring anatomical regions, patients suffering from anal sphincter spasm often find it difficult to determine the localization of pain and may regard this symptom as a manifestation of diseases of the reproductive or urinary system. With prolonged proctalgia, pain is usually less intense, poorly relieved by analgesics.
In secondary spasm of the anal sphincter, which has arisen against the background of hemorrhoids, anal fissure and other diseases, as a rule, there is a clear connection between proctalgia and the act of defecation. Pain appears when urging to stool, increases with straining and persists for several hours (sometimes up to a day or more) after the end of defecation. Persistent pain negatively affects the quality of life of patients suffering from anal sphincter spasm, and can cause fear of defecation, due to which patients “postpone” going to the toilet.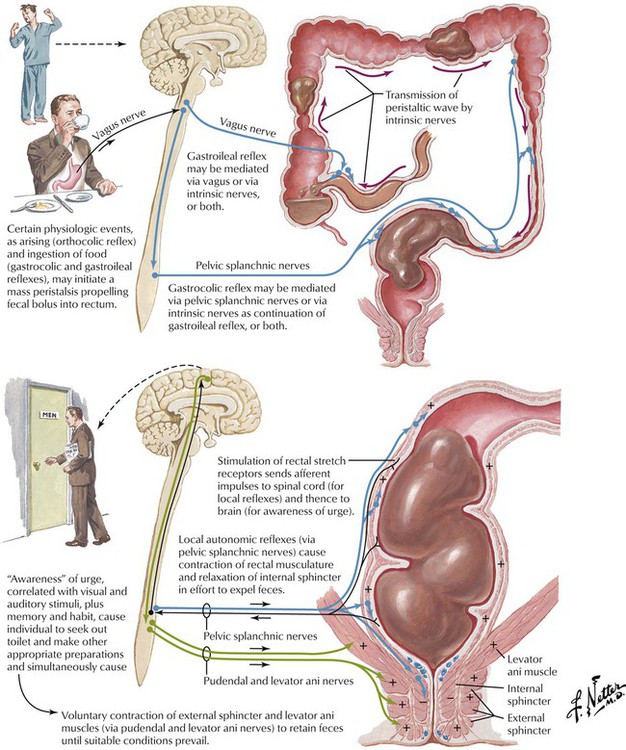 This further exacerbates the resulting violations.
This further exacerbates the resulting violations.
In case of primary spasm of the anal sphincter, the connection with the act of defecation can be traced less clearly. Pain often appears at night or in the morning. Patients develop insomnia. The causelessness of the appearance of pain syndrome, sleep disturbances, initial emotional instability and predisposition to neurotic disorders create a psycho-emotional mood that contributes to the onset of cancerophobia and hypochondria disorders.
Diagnosis
When diagnosing anal sphincter spasm, a thorough collection of complaints, clarification of the history of life and disease is of great importance. When collecting complaints, a proctologist draws attention to the nature of the pain syndrome, its connection with the act of defecation and the time of day. When clarifying the anamnesis of the life of patients with suspected spasm of the anal sphincter, they focus on the presence of chronic pathology of the large intestine and the anus, previous operations and injuries of this anatomical region, vegetative-vascular dystonia, neurotic disorders and emotional lability.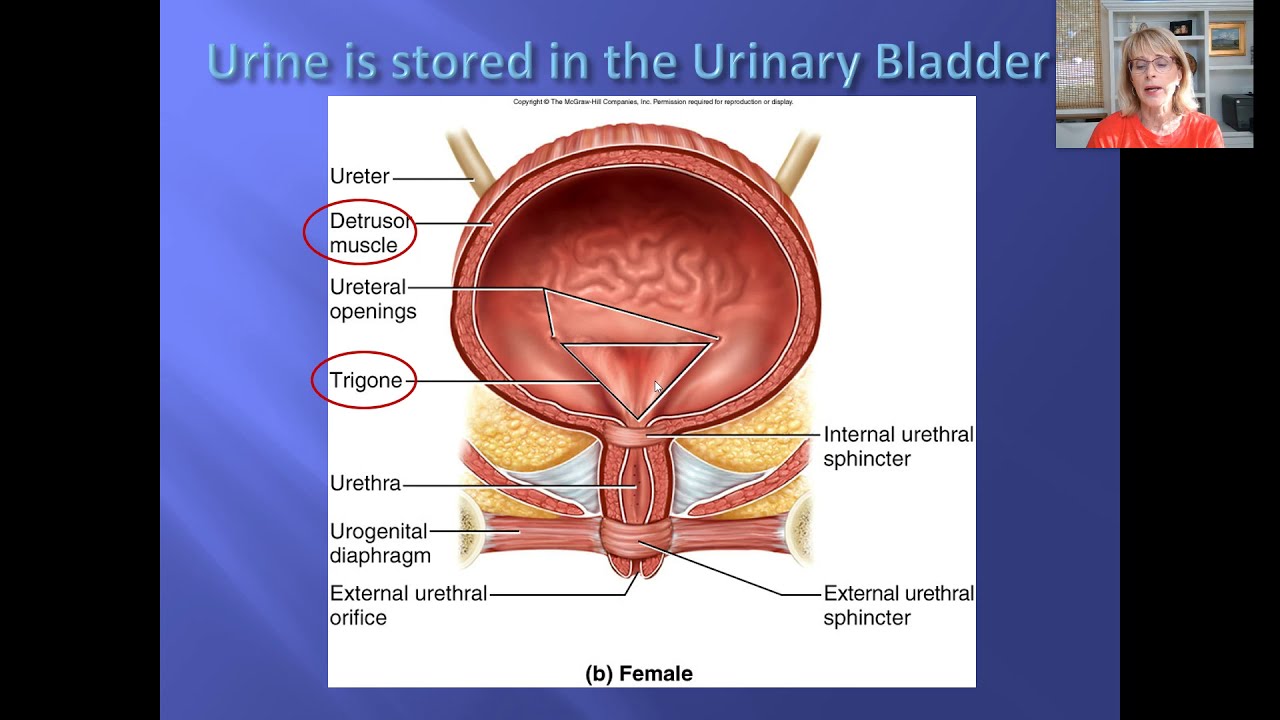
In a number of cases, it is possible to establish that, despite the absence of diagnosed vegetative and mental disorders, in the life history of patients suffering from anal sphincter spasm, recurring spasms of smooth muscles of various organs are traced, for which patients in the past turned to gastroenterologists, pulmonologists, otolaryngologists and other specialists. The examination plan for suspected anal sphincter spasm includes rectal examination and sigmoidoscopy. If you suspect the presence of pathological changes in the upper sections of the large intestine, barium enema and colonoscopy are prescribed. With severe psychoemotional disorders, patients are referred for a consultation with a psychologist or psychotherapist.
Treatment of anal sphincter spasm
Treatment may include diet, drug therapy, physical therapy, and surgery. Therapeutic tactics are determined individually, taking into account the cause of development, the severity and duration of the disease, the somatic and psychological state of the patient.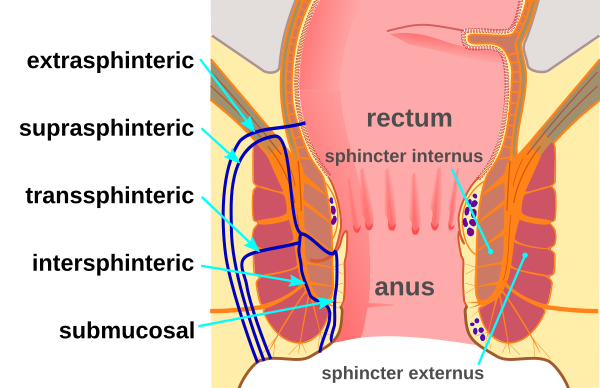 The patient is advised to give up fatty and spicy foods that irritate the intestinal wall, they are advised to carefully observe the rules of personal hygiene and avoid injuring the perianal area with coarse toilet paper.
The patient is advised to give up fatty and spicy foods that irritate the intestinal wall, they are advised to carefully observe the rules of personal hygiene and avoid injuring the perianal area with coarse toilet paper.
Antibacterial therapy if necessary. Antispasmodics and analgesics are prescribed (mainly in the form of suppositories, creams and microclysters). For constipation, laxatives are prescribed. To eliminate spasm of the anal sphincter, thermal procedures, electrosleep, UHF, darsonvalization and other physiotherapeutic techniques are used. If conservative therapy is ineffective, a sphincterotomy is performed with partial excision of the smooth muscles surrounding the anus.
Anal sphincter spasm – causes, symptoms, diagnosis and treatment
Anal sphincter spasm is a pathological condition in which involuntary painful contractions of the smooth muscles surrounding the anus are observed. It can develop with some injuries and diseases of the rectum and anus, disorders of innervation, autonomic disorders and emotional instability. Spasm of the anal sphincter is accompanied by pain radiating to the coccyx, abdomen, perineum, etc. It is diagnosed on the basis of complaints, anamnesis, rectal examination, sigmoidoscopy, colonoscopy and irrigoscopy. Treatment – diet, antispasmodics, analgesics, physiotherapy, surgery.
Spasm of the anal sphincter is accompanied by pain radiating to the coccyx, abdomen, perineum, etc. It is diagnosed on the basis of complaints, anamnesis, rectal examination, sigmoidoscopy, colonoscopy and irrigoscopy. Treatment – diet, antispasmodics, analgesics, physiotherapy, surgery.
General information
Anal sphincter spasm is a fairly common pathological condition that occurs as a result of disorders of innervation and autonomic regulation, traumatic injuries, operations, chronic diseases or severe emotional instability. The main symptom of anal sphincter spasm is pain in the anus (proctalgia) of varying duration and intensity. Mostly middle-aged people suffer, the disease is equally common in patients of both sexes.
Spasm of the anal sphincter tends to be prolonged. It negatively affects the quality of life, accompanied by emotional and mental exhaustion. Cancerophobia is possible, due to the initial mental instability and the tendency of many patients to neurotic reactions.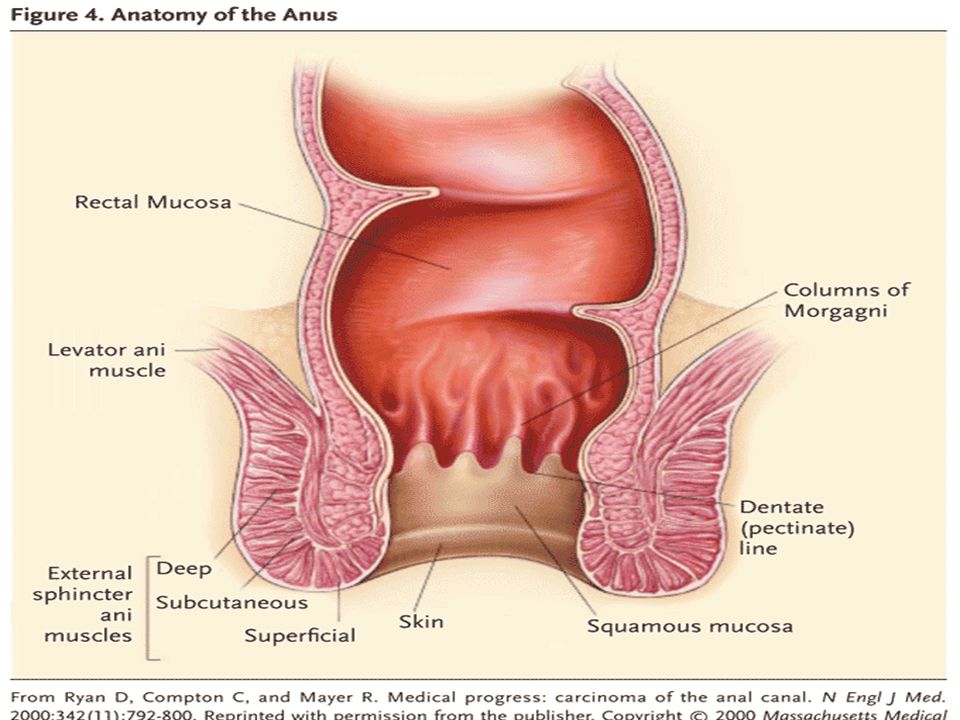 Treatment of anal sphincter spasm is mainly carried out by specialists in the field of clinical proctology. In the presence of severe mental disorders, the participation of a psychologist or psychotherapist is required.
Treatment of anal sphincter spasm is mainly carried out by specialists in the field of clinical proctology. In the presence of severe mental disorders, the participation of a psychologist or psychotherapist is required.
Anal sphincter spasm
Causes
Anal sphincter spasm belongs to the category of polyetiological diseases and can be primary or secondary. In the absence of organic changes, they speak of a primary disorder. The cause of the development of the primary spasm of the anal sphincter is viscero-neurotic disorders and mental instability. The disease is often detected in individuals with a pronounced hysterical component, neurasthenia, increased emotional lability and vegetative-vascular dystonia.
Secondary spasm of the anal sphincter occurs against the background of conditions accompanied by the appearance of organic changes and functional disorders in the anus and lower rectum. Among the common causes that cause the development of this pathology are chronic diseases of the anus, such as hemorrhoids and anal fissure. In addition, spasm of the anal sphincter can be provoked by inflammatory processes in the lower intestine (Crohn’s disease, ulcerative colitis), benign and malignant tumors of the rectum, constipation, trauma to the sacrum and coccyx, complicated childbirth, surgical interventions and adhesions in the pelvic area.
In addition, spasm of the anal sphincter can be provoked by inflammatory processes in the lower intestine (Crohn’s disease, ulcerative colitis), benign and malignant tumors of the rectum, constipation, trauma to the sacrum and coccyx, complicated childbirth, surgical interventions and adhesions in the pelvic area.
Pathogenesis
There are a large number of nerve endings and blood vessels in the posterior wall of the rectum. Violations of the normal functioning of this part of the intestine are accompanied by the appearance of many nerve impulses that cause a reflex contraction of the smooth muscles surrounding the external and internal sphincters of the anus. With intense stimulation of this reflexogenic zone, individual contractions can turn into spasms of the anal sphincter of various durations. Such spasms, in turn, entail a violation of the blood supply to the rectum and surrounding tissues, cause even more irritation of the nerve endings and exacerbate muscle contraction, which provokes the emergence of a “vicious circle”.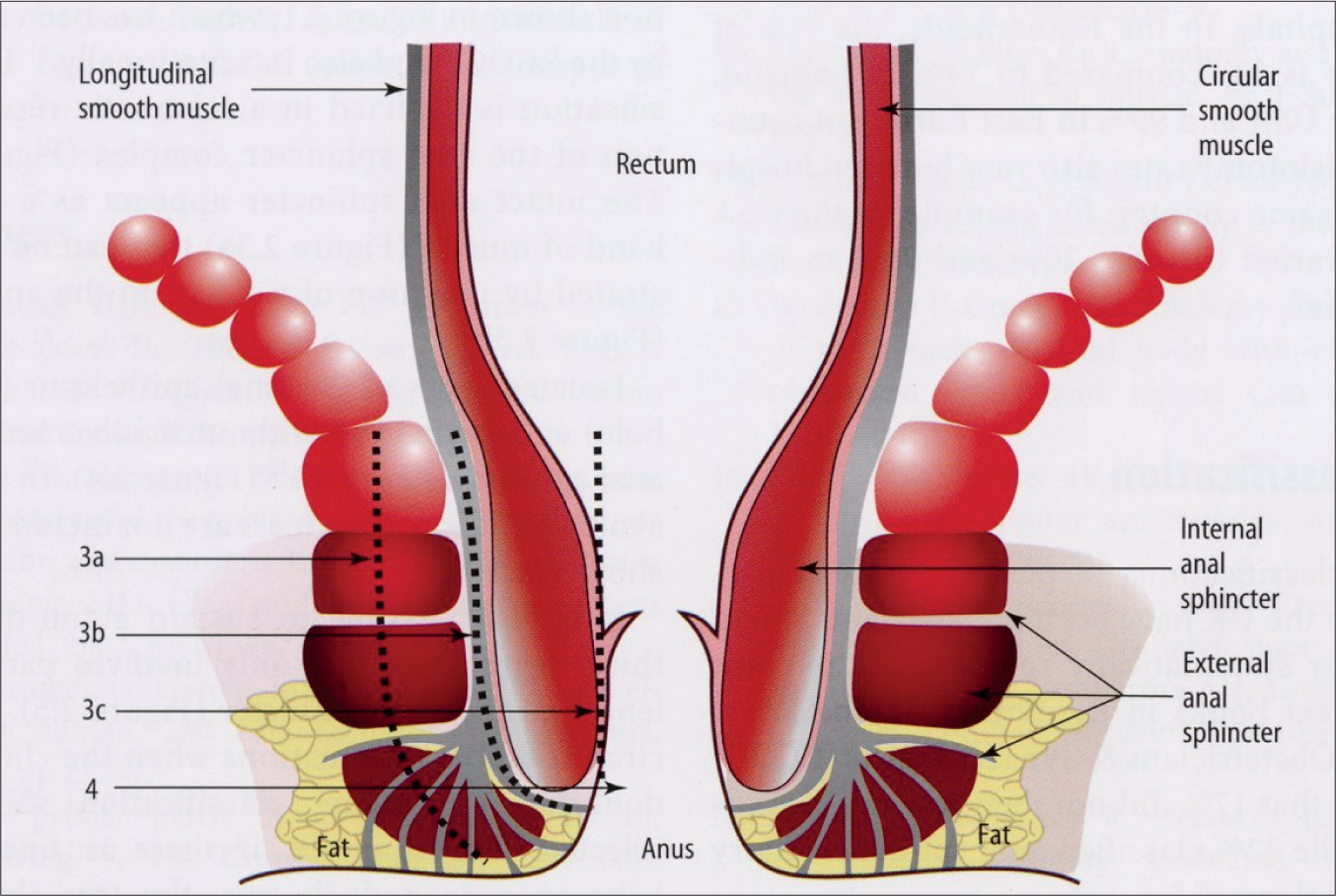
Symptoms
The characteristic manifestations of anal sphincter spasm are pains of varying duration and intensity, radiating to the coccyx, perineum, hip joints or lower abdomen. Pain during spasm is paroxysmal, may appear during defecation or occur without apparent connection with the state of the rectum (empty or not emptied) and other circumstances. There is a low effectiveness of analgesics, while the pain syndrome often disappears or weakens after the completion of a bowel movement or taking a warm bath.
Spasm of the anal sphincter can be provoked not only by the act of defecation, but also by chronic stress, acute emotional and psychological stress, overwork, heavy physical exertion and some neurological diseases. At the same time, spasm of the anal sphincter often itself becomes an impetus for the occurrence of prolonged stress, increased emotional instability and the development of mental disorders of a neurotic level.
Depending on the type of pain syndrome, there are two forms of anal sphincter spasm: with prolonged and short-term proctalgia. With short-term proctalgia, the pain is strong, pulling or stabbing. Due to the high intensity of the pain syndrome and its irradiation to neighboring anatomical regions, patients suffering from anal sphincter spasm often find it difficult to determine the localization of pain and may regard this symptom as a manifestation of diseases of the reproductive or urinary system. With prolonged proctalgia, pain is usually less intense, poorly relieved by analgesics.
With short-term proctalgia, the pain is strong, pulling or stabbing. Due to the high intensity of the pain syndrome and its irradiation to neighboring anatomical regions, patients suffering from anal sphincter spasm often find it difficult to determine the localization of pain and may regard this symptom as a manifestation of diseases of the reproductive or urinary system. With prolonged proctalgia, pain is usually less intense, poorly relieved by analgesics.
In secondary spasm of the anal sphincter, which has arisen against the background of hemorrhoids, anal fissure and other diseases, as a rule, there is a clear connection between proctalgia and the act of defecation. Pain appears when urging to stool, increases with straining and persists for several hours (sometimes up to a day or more) after the end of defecation. Persistent pain negatively affects the quality of life of patients suffering from anal sphincter spasm, and can cause fear of defecation, due to which patients “postpone” going to the toilet.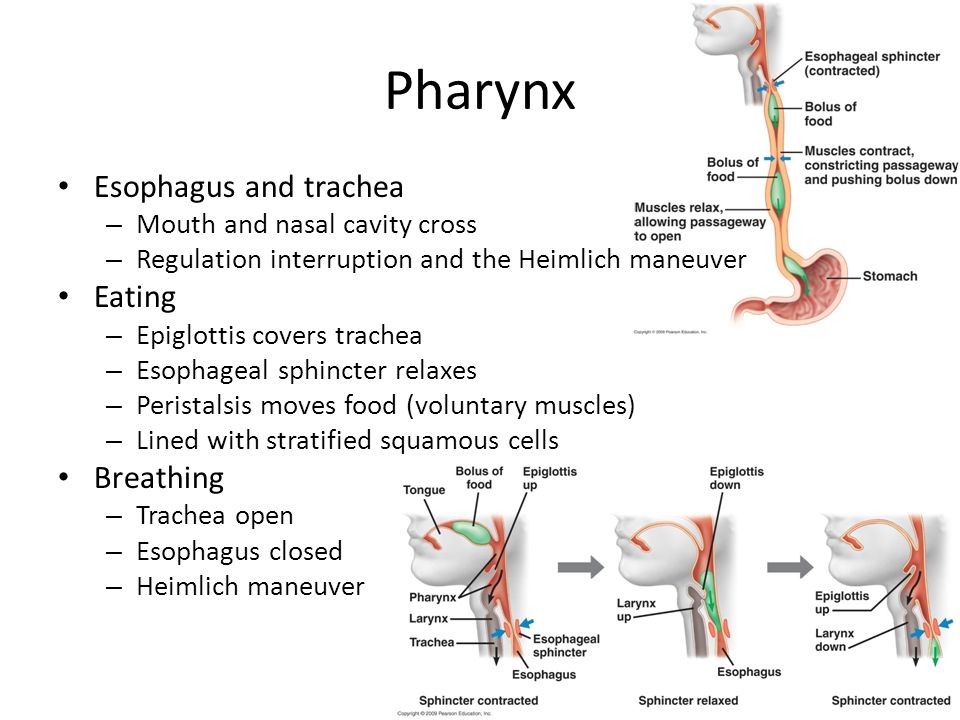 This further exacerbates the resulting violations.
This further exacerbates the resulting violations.
In case of primary spasm of the anal sphincter, the connection with the act of defecation can be traced less clearly. Pain often appears at night or in the morning. Patients develop insomnia. The causelessness of the appearance of pain syndrome, sleep disturbances, initial emotional instability and predisposition to neurotic disorders create a psycho-emotional mood that contributes to the onset of cancerophobia and hypochondria disorders.
Diagnosis
When diagnosing anal sphincter spasm, a thorough collection of complaints, clarification of the history of life and disease is of great importance. When collecting complaints, a proctologist draws attention to the nature of the pain syndrome, its connection with the act of defecation and the time of day. When clarifying the anamnesis of the life of patients with suspected spasm of the anal sphincter, they focus on the presence of chronic pathology of the large intestine and the anus, previous operations and injuries of this anatomical region, vegetative-vascular dystonia, neurotic disorders and emotional lability.
In a number of cases, it is possible to establish that, despite the absence of diagnosed vegetative and mental disorders, in the life history of patients suffering from anal sphincter spasm, recurring spasms of smooth muscles of various organs are traced, for which patients in the past turned to gastroenterologists, pulmonologists, otolaryngologists and other specialists. The examination plan for suspected anal sphincter spasm includes rectal examination and sigmoidoscopy. If you suspect the presence of pathological changes in the upper sections of the large intestine, barium enema and colonoscopy are prescribed. With severe psychoemotional disorders, patients are referred for a consultation with a psychologist or psychotherapist.
Treatment of anal sphincter spasm
Treatment may include diet, drug therapy, physical therapy, and surgery. Therapeutic tactics are determined individually, taking into account the cause of development, the severity and duration of the disease, the somatic and psychological state of the patient.
