Ankle surgery arthroscopy. Ankle Arthroscopy: A Comprehensive Guide to Understanding the Procedure and Its Benefits
What is ankle arthroscopy? How does it work? What are the benefits and risks of this surgery? Get answers to these questions and more in this comprehensive guide.
Understanding Ankle Arthroscopy: The Basics
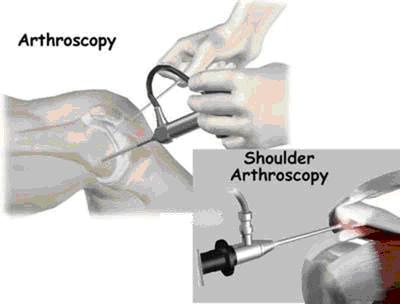
Ankle arthroscopy is a minimally invasive surgical procedure that allows doctors to examine and repair the tissues inside or around the ankle joint. It involves the use of a tiny camera, called an arthroscope, which is inserted through small incisions in the skin. This allows the surgeon to view the inside of the ankle on a video monitor and perform any necessary repairs or treatments without the need for larger open surgery.
When is Ankle Arthroscopy Recommended?
Ankle arthroscopy may be recommended to address a variety of ankle-related issues, including:
- Ankle pain
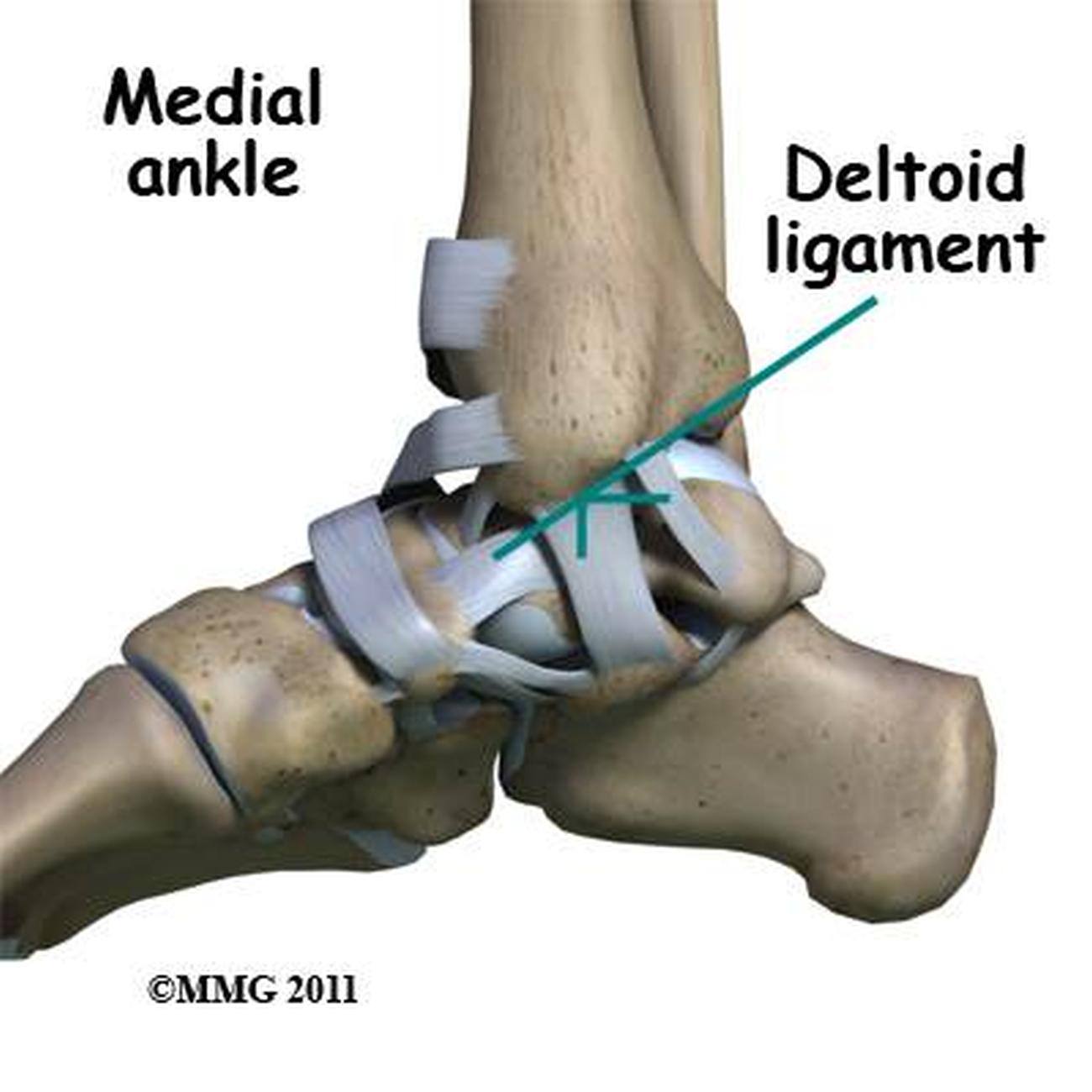
- Ligament tears
- Ankle impingement (where tissues become swollen and sore from overuse)
- Scar tissue formation
- Arthritis
- Cartilage injuries
- Loose bone or cartilage fragments within the ankle joint

The Ankle Arthroscopy Procedure: What to Expect
During the procedure, the surgeon will make one or more small incisions in the skin around the ankle and insert the arthroscope. This allows them to inspect the entire ankle joint and make any necessary repairs or remove any damaged tissue. The surgeon may need to make additional small incisions to insert other tools for the repair work. At the end of the surgery, the incisions are closed with stitches and covered with a dressing.
Advantages of Ankle Arthroscopy
Compared to traditional open ankle surgery, ankle arthroscopy offers several key advantages:
- Smaller incisions, resulting in less scarring and faster healing
- Reduced pain and discomfort during recovery
- Quicker return to normal activities and function
- Lower risk of complications, such as infection or nerve damage
Preparing for Ankle Arthroscopy
Before the surgery, patients may be asked to temporarily stop taking certain medications, such as blood thinners, to reduce the risk of complications. Patients with other medical conditions, such as diabetes or heart disease, may need to see their primary care provider for additional evaluation and clearance before the procedure. It’s important to follow all pre-operative instructions provided by the healthcare team.
Recovery and Aftercare
After the ankle arthroscopy procedure, patients typically go home the same day once they have recovered from the anesthesia. They may need to use crutches or a walker to keep weight off the ankle during the initial recovery period. Patients will also be given instructions on how to care for the incisions, manage pain, and when to follow up with the surgeon.
Reducing Swelling and Pain
To help reduce swelling and pain after the procedure, patients are often advised to:
- Keep the ankle elevated above the level of the heart for 2-3 days
- Apply cold packs to the ankle
- Take pain medication as directed by the healthcare provider
Returning to Normal Activities
The timeline for returning to normal activities and weight-bearing on the ankle will vary depending on the specific procedure performed and the individual patient’s healing process. Patients will typically need to use crutches or a boot/splint for a period of time before gradually transitioning back to regular footwear and activities. It’s important to follow the surgeon’s post-operative instructions closely to ensure a successful recovery.

Risks and Potential Complications
As with any surgical procedure, there are some risks associated with ankle arthroscopy, including:
- Allergic reactions to anesthesia or medications
- Breathing problems
- Bleeding, blood clots, or infection
- Failure of the surgery to relieve symptoms or heal properly
- Weakening of the ankle
- Injury to tendons, blood vessels, or nerves
Patients should discuss these potential risks with their surgeon and follow all pre- and post-operative instructions to minimize the likelihood of complications.
Conclusion
Ankle arthroscopy is a minimally invasive surgical procedure that allows doctors to diagnose and treat a variety of ankle-related issues with less pain and faster recovery times compared to traditional open surgery. By understanding the benefits, risks, and what to expect during the procedure and recovery, patients can make informed decisions about their ankle health and care.
Ankle arthroscopy: MedlinePlus Medical Encyclopedia
Ankle arthroscopy is surgery that uses a tiny camera and surgical tools to examine or repair the tissues inside or around your ankle. The camera is called an arthroscope. The procedure allows the doctor to detect problems and make repairs to your ankle without making larger cuts in the skin and tissue. This means that you may have less pain and recover more quickly than open surgery.
You may receive general anesthesia before this surgery. This means you will be asleep and unable to feel pain. Or, you will have regional anesthesia. Your leg and ankle area will be numbed so that you do not feel any pain. If you receive regional anesthesia, you will also be given medicine to make you very sleepy during the operation.
During the procedure, the surgeon does the following:
- Inserts the arthroscope into your ankle through a small incision. The scope is connected to a video monitor in the operating room. This allows the surgeon to view the inside of your ankle.

- Inspects all the tissues of your ankle. These tissues include cartilage, bones, tendons, and ligaments.
- Repairs any damaged tissues. To do this, your surgeon makes 1 to 3 more small incisions and inserts other instruments through them. A tear in a muscle, tendon, or cartilage is fixed. Any damaged tissue is removed.
At the end of the surgery, the incisions will be closed with stitches and covered with a dressing (bandage). Most surgeons take pictures from the video monitor during the procedure to show you what they found and what repairs they made.
Your surgeon may need to do open surgery if there is a lot of damage. Open surgery means you will have a large incision so that the surgeon can get directly to your bones and tissues.
Arthroscopy may be recommended for these ankle problems:
- Ankle pain. Arthroscopy allows the surgeon to explore what is causing your ankle pain.
- Ligament tears. A ligament is a band of tissue that connects bone to bone.
 Several ligaments in the ankle help keep it stable and allow it to move. Torn ligaments can be repaired with this type of surgery.
Several ligaments in the ankle help keep it stable and allow it to move. Torn ligaments can be repaired with this type of surgery. - Ankle impingement. Tissues in your ankle can become swollen and sore from overuse. This makes it hard to move the joint. Arthroscopy can remove the tissue so you can move your joint.
- Scar tissue. This can form after an injury to the ankle. This surgery can remove scar tissue.
- Arthritis. Arthroscopy can be used to help reduce pain and improve movement.
- Cartilage injuries. This surgery can be used to diagnose or repair cartilage and bone injuries.
- Loose fragments. These are pieces of bone or cartilage inside the ankle that can cause the joint to lock up. During arthroscopy these fragments can be removed.
Risks of anesthesia and surgery in general are:
- Allergic reactions to medicines
- Breathing problems
- Bleeding, blood clot, or infection
Risks of ankle arthroscopy are:
- Failure of surgery to relieve symptoms
- Failure of repair to heal
- Weakness of the ankle
- Injury to tendons, blood vessels, or nerves
Tell your health care provider what medicines you are taking. This includes medicines, supplements, or herbs you bought without a prescription.
This includes medicines, supplements, or herbs you bought without a prescription.
During the 2 weeks before your surgery:
- You may be asked to temporarily stop taking blood thinners. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), and other medicines.
- Ask your provider which medicines you should still take on the day of your surgery.
- If you have diabetes, heart disease, or other medical conditions, your surgeon will ask you to see your doctor who treats you for these conditions.
- Tell your provider if you have been drinking a lot of alcohol, more than 1 or 2 drinks a day.
- If you smoke, try to stop. Ask your provider or nurse for help. Smoking can slow wound and bone healing.
- Tell your surgeon if you develop a cold, flu, fever, herpes breakout, or other illness before your surgery. If you do get sick, the procedure may need to be postponed.
On the day of surgery:
- Follow instructions about when to stop eating and drinking before the procedure.

- Take any drugs you’re asked to take with a small sip of water.
- Follow instructions on when to arrive at the hospital. Arrive on time.
You can usually go home the same day after you recover from the anesthesia. You should have someone drive you home.
Follow any discharge instructions you’re given. These may include:
- Keep your ankle elevated above your heart for 2 to 3 days to help reduce swelling and pain. You can also apply a cold pack to reduce swelling.
- Keep your bandage clean and dry. Follow instructions for how to change the dressing.
- You can take pain relievers, if needed, as long as your doctor says it is safe to do so.
- You will need to use a walker or crutches and keep weight off your foot unless your provider says it is OK to put weight on your foot.
- You may need to wear a splint or boot for a few weeks or longer to keep the ankle stable as it heals.
Arthroscopy uses small cuts in the skin. Compared to open surgery, you may have:
Compared to open surgery, you may have:
- Less pain and stiffness
- Fewer complications
- Faster recovery
The small cuts will heal quickly, and you may be able to resume your normal activities in a few days. But, if a lot of tissue in your ankle had to be repaired, it may take several weeks to heal. How quickly you heal depends on how complicated the surgery was.
You may be shown how to do gentle exercises as you heal. Or, your surgeon may recommend that you see a physical therapist to help you regain the full use of your ankle.
Ankle surgery; Arthroscopy – ankle; Surgery – ankle – arthroscopy; Surgery – ankle – arthroscopic
Murphy GA. Arthroscopy of the foot and ankle. In: Azar FM, Beaty JH, eds. Campbell’s Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 50.
Smyth NA, Kaplan JR, Aiyer AA, Campbell JT, Triche R, Cerrato R. Ankle arthroscopy. In: Miller MD, Thompson SR, eds. DeLee, Drez, & Miller’s Orthopaedic Sports Medicine. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 115.
5th ed. Philadelphia, PA: Elsevier; 2020:chap 115.
Updated by: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Ankle Arthroscopy | FootCareMD
Ankle arthroscopy is a minimally invasive surgical procedure that orthopaedic surgeons use to treat problems in the ankle joint. Ankle arthroscopy uses a thin fiber-optic camera (arthroscope) that can magnify and transmit images of the ankle to a video screen. The arthroscope is inserted into the ankle joint
through a tiny incision, and enables the surgeon to see inside the joint. While looking into the joint with the arthroscope, your surgeon can insert surgical instruments through a separate tiny incision to perform work on the ankle. Ankle arthroscopies
can reduce ankle pain and improve overall function.
Osteochondral defect (OCD), also called osteochondral lesions or osteochondritis dissecans: These are areas of damaged cartilage and bone in the ankle joint. OCDs usually are caused by injuries to the ankle such as fractures and sprains. Common symptoms include ankle pain and swelling. Patients may complain of catching or clicking in the
ankle. The diagnosis is made with a combination of a physical exam and imaging studies. Imaging may include X-rays, MRI, or CT scan. The treatment is based on the size, location, and stability of the OCD. The patient’s age, symptoms, and activities
also are considered. Surgery often consists of scraping away the damaged cartilage and drilling small holes in the bone to promote healing. Bone grafting and cartilage transplant procedures also can be performed.
Loose bodies: Cartilage, bone, and scar tissue can become free floating in the joint and form what is referred to as “loose bodies.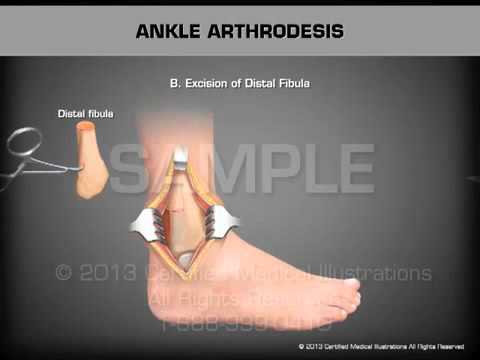 ” Loose bodies can be painful and can cause problems such as clicking and catching. Locking of the ankle
” Loose bodies can be painful and can cause problems such as clicking and catching. Locking of the ankle
joint may occur. They are often associated with osteochondral defects/lesions.
Ankle arthroscopy can be used to find and remove the loose bodies.
Ankle instability: Ligaments of the ankle
can become stretched out, which can lead to a feeling that the ankle “gives out.” These ligaments can be tightened with surgery. Arthroscopic techniques may be an option for treating moderate instability.
Synovitis: The soft tissue lining of the ankle joint (synovial tissue) can become inflamed. This causes pain and swelling. It can be caused by injury and overuse. Inflammatory arthritis (rheumatoid arthritis) and osteoarthritis also can
cause synovitis. Ankle arthroscopy can be used to surgically remove inflamed tissue that does not respond to nonsurgical treatment.
Ankle fractures: Ankle arthroscopy may be used along
with open techniques of fracture repair. This can help the surgeon ensure normal alignment of bone and cartilage. It also may be used during ankle fracture repair to look for cartilage injuries inside the ankle.
This can help the surgeon ensure normal alignment of bone and cartilage. It also may be used during ankle fracture repair to look for cartilage injuries inside the ankle.
Ankle arthritis: Ankle fusion is a treatment option for many patients with end-stage ankle arthritis. Ankle arthroscopy offers a minimally invasive way to perform
ankle fusion. Results can be equal to or better than open techniques.
Infection: Infection in the joint space cannot be treated with antibiotics alone. It often requires an urgent surgery to wash out the joint. This can be done with arthroscopy.
Unexplained ankle symptoms: Occasionally patients develop symptoms that cannot be explained by other diagnostic techniques. Arthroscopy provides the opportunity to look directly into the joint. The surgeon can then identify problems that
may be treated with surgery.
Elective arthroscopy is not appropriate for some patients.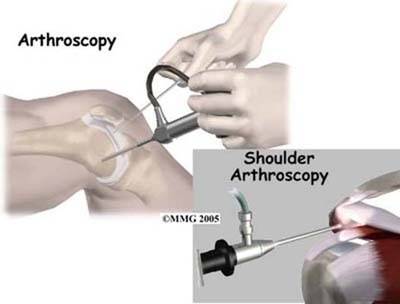 Patients with severe ankle arthritis usually do not benefit from arthroscopic surgery. Patients with active infections or other medical problems may not be appropriate surgical candidates.
Patients with severe ankle arthritis usually do not benefit from arthroscopic surgery. Patients with active infections or other medical problems may not be appropriate surgical candidates.
Treatment
Your foot and ankle orthopaedic surgeon will mark the operative leg
prior to surgery. You will be transported to the operating room and given anesthesia. A tourniquet is commonly applied to the leg. The leg is thoroughly cleaned. The surgeon will sometimes use a device to stretch the ankle joint and make it easier
to see inside.
At least two small incisions (“portals”) are made in the front and/or back of the ankle. These portals become the entry sites into the ankle for the arthroscopic camera and instruments. Sterile fluid flows into the joint to expand it and allow for better
visualization. The camera and instruments can be exchanged between portals to perform the surgery. Both motorized shavers and hand operated instruments are used. After the surgery is complete, sutures are placed to close the portals.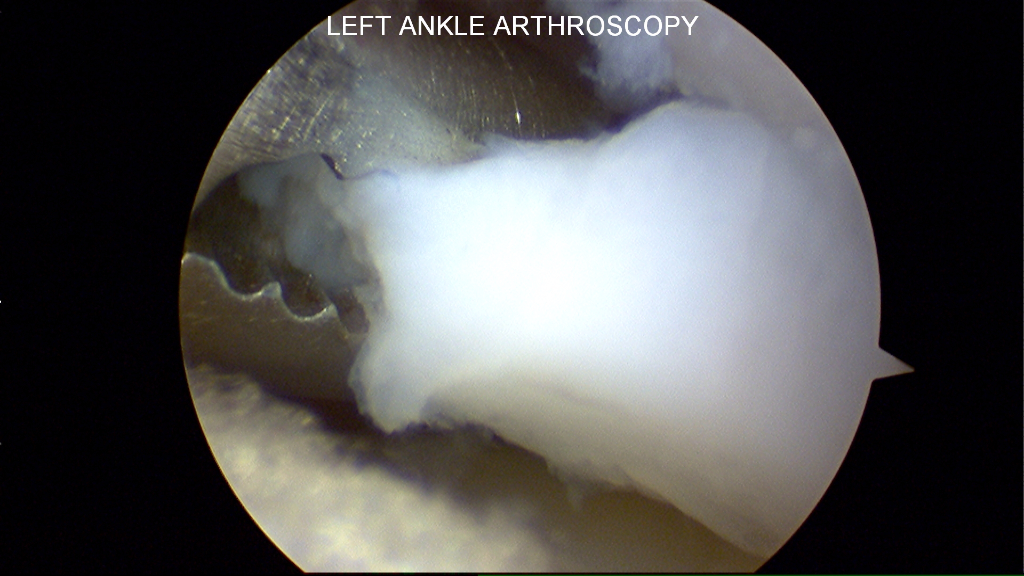 A sterile dressing
A sterile dressing
is placed over the sutures. A splint or boot is often used.
Recovery
You can expect some pain and swelling following surgery. Your may need to keep your leg elevated. You may need to take oral pain medication for several days. You may be able to walk on the leg immediately, or you may need to wait several months before putting
weight on the leg. This will depend on the type of surgery performed and the recommendations of your surgeon.
If needed, sutures are removed 1-2 weeks after surgery. Your surgeon will determine when activities such as range-of-motion and ankle
exercises are allowed. Physical therapy may also be recommended.
Risks and Complications
All surgeries come with possible complications, including the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots.
Potential complications specific to ankle arthroscopy include injury to nerves and blood vessels around the ankle. Numbness or tingling over the top of the foot can occur approximately 10% of the time. This typically resolves over time.
Numbness or tingling over the top of the foot can occur approximately 10% of the time. This typically resolves over time.
When can I safely return to driving?
You will likely be cleared for driving when you are able to bear weight without limitation and are no longer taking narcotic pain medication.
When can I expect to return to work and sports?
Your return to work and sports depends on what kind of surgery was done. You may be able to return work several days after surgery if you can safely complete your job duties. While some simple surgeries may allow return to sports after about 4-6 weeks,
other surgeries may take much longer (4-6 months).
Is ankle arthroscopy effective?
80-90% of patients undergoing ankle arthroscopy for common problems achieve good or excellent results.
Original article by Sarang Desai, DO
Contributors/Reviewers: Robert Gorman, MD; Robert Leland, MD; Elizabeth Cody, MD
The American Orthopaedic Foot & Ankle Society (AOFAS) offers information on this site as an educational service. The content of FootCareMD, including text, images, and graphics, is for informational purposes only. The content is not intended to substitute
The content of FootCareMD, including text, images, and graphics, is for informational purposes only. The content is not intended to substitute
for professional medical advice, diagnoses or treatments. If you need medical advice, use the “Find a Surgeon” search to locate a foot and ankle orthopaedic surgeon in your area.
Ankle Arthroscopy | Blog ММЦ Clinic №1 Lublino, Moscow
Call
Call me back
Home
Blog
Ankle arthroscopy: preparation for surgery
10/23/2020
Ankle arthroscopy is a method that allows you to simultaneously detect and cure pathology. Minimal interference in the coordinated work of the body contributes to a quick recovery after surgery and reduces the risk of relapse to a minimum.
Features of the ankle joint
The ankle joint is a complex and highly mobile articulation of the bones of the leg and foot. It consists of the tibia, fibula, and talus bones, muscles, ligaments, and blood vessels. The ankle joint can move only in the frontal plane, that is, it can perform flexion and extension of the foot.
The ankle joint can move only in the frontal plane, that is, it can perform flexion and extension of the foot.
It would seem that the feet, on which the entire mass of the human body with additional loads (bags, bars, boxes) presses daily, should be made of strong material. But no: the bones of the foot at the base are very thin, so they are easy to injure with the wrong shoes, careless movement, non-compliance with safety measures in sports (for example, insufficient warming up of the muscles before further work). And if everyone’s weight is different, then the anatomy of the joint and bones is almost the same.
The most common injuries of the ankle joint are bruises and sprains, as a result of an unsuccessful fall or direct force impact when bruised.
Damaged areas painfully react to palpation, are characterized by swelling, hemorrhage (bruising) and limitation of mobility. Stronger pain sensations are dislocations and subluxations, which lead to limited mobility and may be the result of fractures.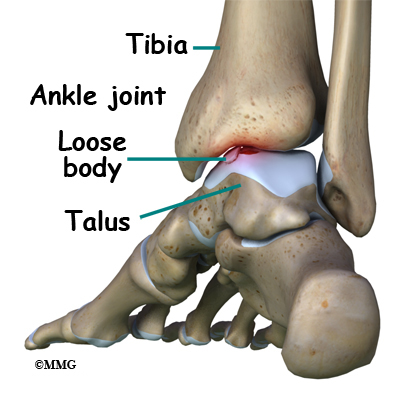 However, they rarely become the reason for doing arthroscopy, only in cases where other diagnostic methods do not work, and the treatment does not bring healing.
However, they rarely become the reason for doing arthroscopy, only in cases where other diagnostic methods do not work, and the treatment does not bring healing.
When arthroscopy is indicated
Ankle arthroscopy is indicated for severe injuries, failure of conservative treatment, failure of taping or elastic bandages for a long time. The procedure is prescribed by the surgeon. The reason for the operation may be:
- development of deforming arthrosis of the joint or its chronic, advanced stage;
- damage to cartilage tissue, its exfoliation;
- unstable state of the joints;
- pain of unknown etiology;
- synovitis of various nature;
- chondromatosis;
- arthritis;
- impingement syndrome.
The procedure can be both diagnostic and therapeutic. Diagnosis using an arthroscope allows you to assess the condition of the joint and its structures, determine the existing pathologies and the state of their development, make tissue sampling for analysis, and clarify the existing conclusion.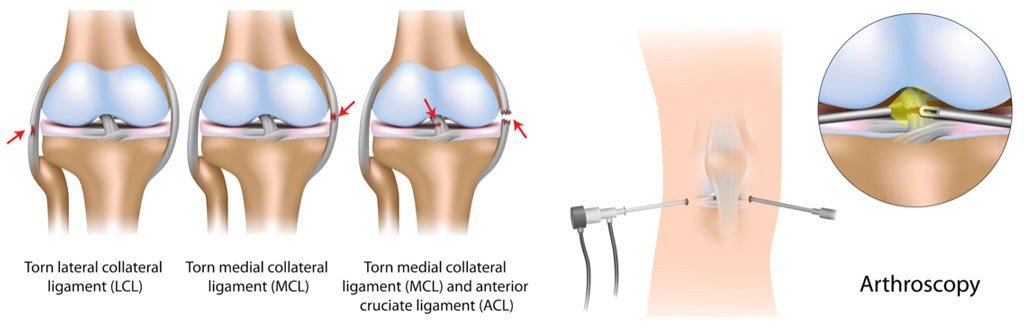
Surgical intervention is needed to excise individual fragments, remove adhesions, tissue or bone growths, synovial membrane (full or partial), replace damaged areas, match pieces of destroyed bones.
Preparation for surgery and contraindications
The first consultation is given by an orthopedic surgeon. He examines the sore spot and prescribes additional diagnostics: X-ray, MRI, ECG, fluorography. There are contraindications for ankle arthroscopy, so it is important for the doctor to know everything about your health.
Contraindications are divided into two groups: relative and absolute. Relative contraindications imply prior treatment. For example, hidden damage to the ligaments and joint capsule or hemorrhage into the joint cavity. This group also includes somatic disorders. For women, there is an additional point – the operation is not possible during menstruation.
List of absolute contraindications:
- anesthesia intolerance;
- infection of the cavity;
- purulent infection;
- infectious diseases of the skin;
- pathologies of the cardiovascular system, diabetes mellitus;
- progressive dystrophic pathology of cartilage tissue;
- HIV, hepatitis;
- herpes;
- colds.

To detect contraindications, you need to consult a general practitioner who will make a conclusion based on a general and biochemical analysis of blood, urine, a test for the presence of hepatitis and HIV, and the testimony of an anesthesiologist. People who have had a heart attack or stroke should visit a neurologist or cardiologist.
You will have to prepare for the operation not only mentally, but also physically. A light diet is recommended a few days before the operation, no alcohol for 10-15 days and no food for 12 hours before anesthesia is administered. You need to take care of the crutches in advance, because in the first postoperative days, the load on the diseased joint is excluded.
How the operation works
Ankle arthroscopy is performed under either local or general anesthesia, depending on how large the area to be operated on and the complexity of the problem. The operation time also depends on this – from 30 minutes to 3 hours.
The lower leg is fixed with a stand at the required height and several access incisions are made for the introduction of instruments. As with shoulder surgery, saline is injected to improve the visibility of the device. The surgeon’s assistant stretches the joint space around the ankle so the doctor can insert the arthroscope.
The image from the device is broadcast on a large screen, thanks to which it is possible to examine the joint and periarticular space in detail.
At the end of the operation, the joint cavity is cleaned of excess fluid introduced at the beginning and filled with a therapeutic solution. The incisions are closed with sutures and a sterile dressing.
Possible complications
Complications can be observed in very rare cases and even more due to an incorrect diagnosis or very late and poor-quality treatment. For example, if for some reason the seams parted, forming an open wound. An infection can easily get into the wound and cause an inflammatory process. But in order for this to happen, you probably need to escape from the hospital on the day of the operation.
But in order for this to happen, you probably need to escape from the hospital on the day of the operation.
Of the really existing threats, one can name an abnormal accretion of the ankle. This leads to the development of arthrosis and joint deformity. The process is accompanied by regular swelling, as blood circulation is disturbed and, as a result, lameness appears. Another scenario: hemorrhages in the joint cavity, sprains and the effects of anesthesia (nausea, dizziness). All sensations should be reported to the doctor.
Complications occur in 0.1% of cases out of a hundred. But the most important thing to remember is that the tendons, nerves and blood vessels remain intact. And it is very easy to avoid any complications: you must strictly follow the recommendations of the attending physician, especially in the first weeks of rehabilitation.
Rehabilitation
Minimally invasive procedure allows you to quickly return to normal life. This is facilitated by therapeutic physical education. Exercise helps strengthen muscles and restore blood flow. The rehabilitation plan is purely individual, it is compiled by the attending physician, giving a gradual load on the joint and prescribing the necessary medications.
Exercise helps strengthen muscles and restore blood flow. The rehabilitation plan is purely individual, it is compiled by the attending physician, giving a gradual load on the joint and prescribing the necessary medications.
It is possible to return to full-fledged sports activities after 3-6 months, and any risks of relapse can be excluded only after a year. You yourself can contribute to effective recovery by regularly consulting with a specialist and exercising at home.
Benefits of ankle arthroscopy
Arthroscopy is a minimally invasive procedure. There is minimal surgical intervention, which allows you to keep the connective tissue intact. Therefore, after arthroscopy, there are no scars, and the terms of complete rehabilitation of the patient are much shorter than after open surgery.
During the diagnosis, the surgeon can not only examine the diseased area, but also immediately perform the operation, thereby eliminating the repetition of the procedure and reducing the load on the body associated with anesthesia.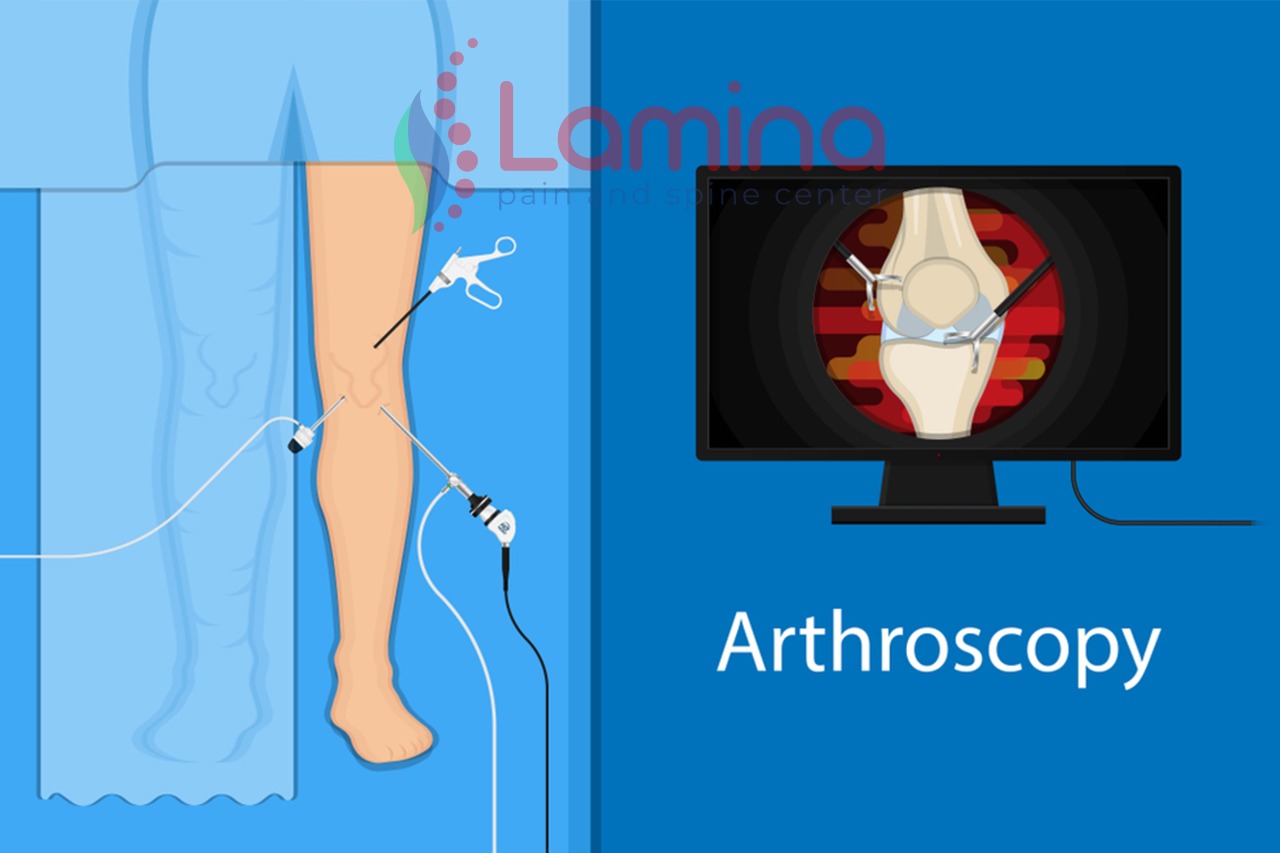
The price of ankle joint arthroscopy depends on the complexity of the operation and the number of items needed for rehabilitation: crutches, bandages, medicines, additional procedures. You can clarify the details directly at a meeting with a doctor or in the feedback form.
On the Internet you can find very conflicting reviews about ankle arthroscopy. Negative experience is often associated with the incompetence of the doctor or the patient’s disdain for the recommendations. Most note a short rehabilitation period and a positive result even with severe injuries.
Author of the article
Bagirov Akshin Beyukovich
Traumatologist-orthopedist, MD
Enter your details and we will contact you as soon as possible
I agree to the processing of personal data. Conditions for the processing of personal data.
Send
We will call you back as soon as possible
LETTER TO THE CHIEF DOCTOR
Send
Thank you for your message
have surgery at the Sports Injury Center
Kazarinova Marina
I want to express my sincere gratitude to the team of doctors of the Department of Traumatology-2 of the Federal Scientific and Practical Center of the Federal Medical and Biological Agency of Russia and personally to the operating surgeon Mukhanov V. V. Thanks to a successful knee surgery, I was able to return to my usual rhythm of life after a couple of months. It took me a long time to decide on an operation. But it turned out that my doubts and preoperative worries were in vain. It was even fascinating to watch the well-coordinated work of professionals during the operation, to watch on the screen how Viktor Viktorovich performs confident manipulations inside the knee, explaining his every step. Staying in the hospital also left the most pleasant impressions, the hospital is equipped with modern equipment, the nurses are attentive and friendly. Special THANKS to the attending physician Karpashevich A.A. for your kindness and help! Thank you for helping people cope with their big and small ailments! Thanks for doing a good job! And yet, intra-articular injections – it does not hurt if you are in the safe hands of Viktor Viktorovich 🙂
V. Thanks to a successful knee surgery, I was able to return to my usual rhythm of life after a couple of months. It took me a long time to decide on an operation. But it turned out that my doubts and preoperative worries were in vain. It was even fascinating to watch the well-coordinated work of professionals during the operation, to watch on the screen how Viktor Viktorovich performs confident manipulations inside the knee, explaining his every step. Staying in the hospital also left the most pleasant impressions, the hospital is equipped with modern equipment, the nurses are attentive and friendly. Special THANKS to the attending physician Karpashevich A.A. for your kindness and help! Thank you for helping people cope with their big and small ailments! Thanks for doing a good job! And yet, intra-articular injections – it does not hurt if you are in the safe hands of Viktor Viktorovich 🙂
Shulyatieva Varvara
theater and film actress
№
About professionals and good people. Knowing Viktor Viktorovich and Alexander Aleksandrovich for several years now, I speak with confidence about the trust in these Doctors. The combination of knowledge and practice, as well as attentiveness and individual approach to each patient, is the main magic of these doctors. They are transcendent, have intuition and an amazing ability to logically connect absolutely disparate semiotics in the human body, which is important for making a diagnosis. Doctors are gifted with the power of desire and positive energy, which contributes to the rapid rehabilitation of the patient. The selection of the team corresponds to the level, the doctors are neat and detailed.
Knowing Viktor Viktorovich and Alexander Aleksandrovich for several years now, I speak with confidence about the trust in these Doctors. The combination of knowledge and practice, as well as attentiveness and individual approach to each patient, is the main magic of these doctors. They are transcendent, have intuition and an amazing ability to logically connect absolutely disparate semiotics in the human body, which is important for making a diagnosis. Doctors are gifted with the power of desire and positive energy, which contributes to the rapid rehabilitation of the patient. The selection of the team corresponds to the level, the doctors are neat and detailed.
Alexander Pavlovsky
Deputy Head of the Yu.A. Gagarin Cosmonaut Training Center, reserve lieutenant general
I want to express my gratitude to the traumatologist Viktor Viktorovich Mukhanov! Patients visit surgeons at critical moments for their health and life.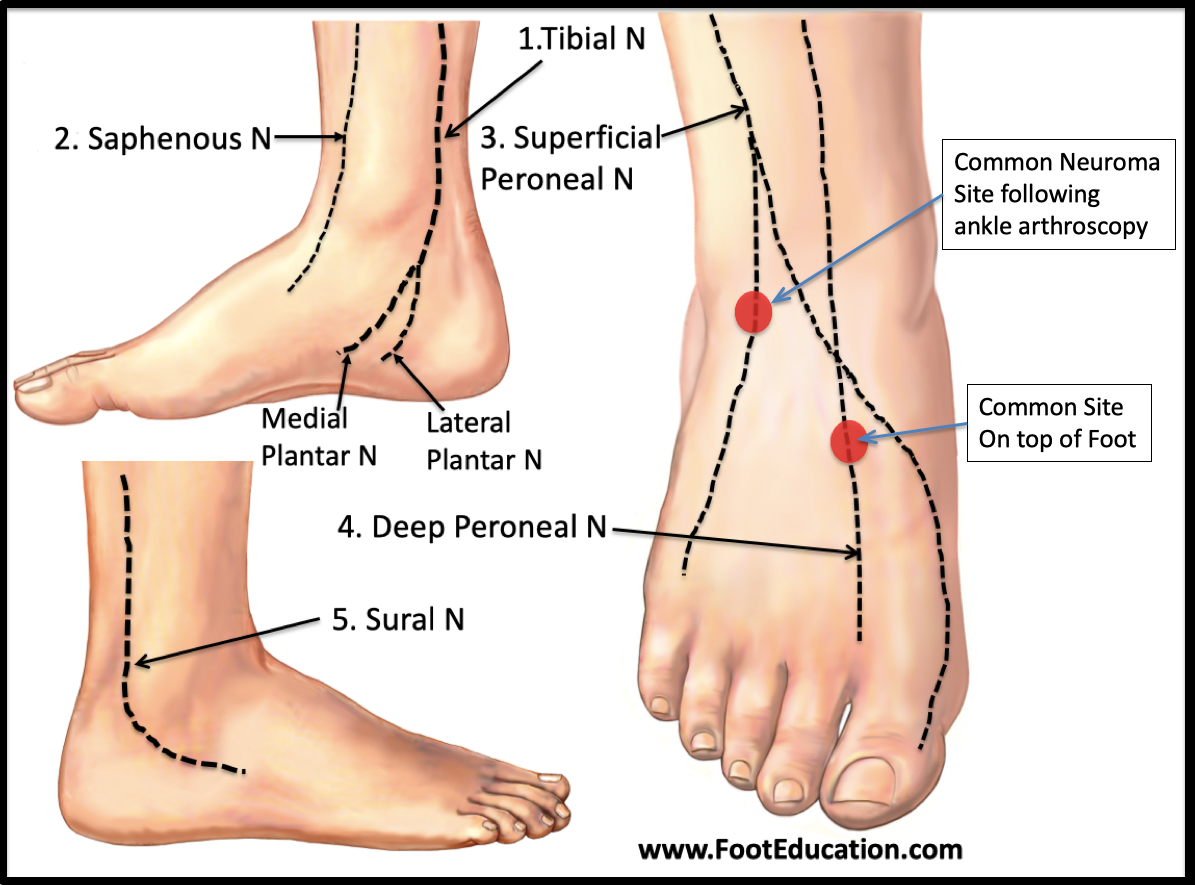 It is in such a situation that the professionalism of the doctor, the correct diagnosis, the sensitive and attentive attitude towards the patient inspires confidence in the successful outcome of the treatment. Viktor Viktorovich performed an operation on me with a diagnosis of subacromial decompression of the left shoulder joint, release of the left shoulder joint. He saved my hand, brought me back to normal life, got rid of the health problems that had plagued me for many months. I want to once again express my gratitude to him for his skillful hands, attention and support during the treatment! Knowing that there are such specialists, I have confidence in the revival of the noble profession of a doctor and the future of our medicine. Special thanks to the leadership of the Federal Scientific and Clinical Center for Specialized Types of Medical Care and Medical Technologies of the FMBA of Russia for forming its team of such highly qualified specialists as Mukhanov V.V., who, in turn, form a positive image of this medical institution.
It is in such a situation that the professionalism of the doctor, the correct diagnosis, the sensitive and attentive attitude towards the patient inspires confidence in the successful outcome of the treatment. Viktor Viktorovich performed an operation on me with a diagnosis of subacromial decompression of the left shoulder joint, release of the left shoulder joint. He saved my hand, brought me back to normal life, got rid of the health problems that had plagued me for many months. I want to once again express my gratitude to him for his skillful hands, attention and support during the treatment! Knowing that there are such specialists, I have confidence in the revival of the noble profession of a doctor and the future of our medicine. Special thanks to the leadership of the Federal Scientific and Clinical Center for Specialized Types of Medical Care and Medical Technologies of the FMBA of Russia for forming its team of such highly qualified specialists as Mukhanov V.V., who, in turn, form a positive image of this medical institution.
Garibov Emin
Russian gymnast, captain of the Russian national gymnastics team
I am the captain of the Russian gymnastics team. Within 2 years, he was recovering from numerous operations performed in Munich on both shoulder joints, due to injuries received during training. But it was not possible to continue treatment abroad, and I was advised by Viktor Viktorovich Mukhanov at the Federal Scientific and Practical Center for Clinical Hospital KB83, who also successfully operated on almost all the leading athletes of Russia. Having extensive experience in communication and treatment with various doctors, I immediately noted great professionalism and competence, after looking only at the photos from the operation, he made an accurate diagnosis and, taking into account the specifics of my sport, as well as the preparation plan for the Rio 2016 Olympic Games, as much as possible He clearly explained all the details of the problem, which inspired confidence in the doctor. Then a course of prp-therapy was prescribed and carried out very effectively. I was very pleased with the work done, as it can be very difficult for athletes to find a truly qualified traumatologist. Now, if anything, only to him!
Then a course of prp-therapy was prescribed and carried out very effectively. I was very pleased with the work done, as it can be very difficult for athletes to find a truly qualified traumatologist. Now, if anything, only to him!
Olesya Karpovich
Russian water polo team
I want to express my deep gratitude to the doctors of the 83rd hospital of the FMBA, trauma department – Mukhanov V.V., Sovetnikov N.N., Karpashevich A.A. and also Budashkina M.V. for high professionalism, sensitive attitude and assistance in rehabilitation! Thanks to all the staff for their hospitality and kindness! Thank you for the opportunity to continue my sports career!!!!!
Petr Khutiev
captain of the Moscow Dragons
Being a rugby player with 35 years of experience, I had to repeatedly get injured and go through the process of treatment and rehabilitation, and I must say that the continuation of my sports career in the last three years became possible only thanks to the excellently translated knee surgery by Viktor Viktorovich Mukhanov , Doctor of the Department of Traumatology and Orthopedics of the Federal Research and Clinical Center of the Federal Medical and Biological Agency of Russia. Excellent staff, comfortable conditions of stay and, of course, a surgical operation and subsequent recovery under the supervision of Viktor Viktorovich made it possible to resume training in 2 months, to go skiing in three months, and to enter the rugby field in four months and become the champion of Moscow in the 2015 season .
Excellent staff, comfortable conditions of stay and, of course, a surgical operation and subsequent recovery under the supervision of Viktor Viktorovich made it possible to resume training in 2 months, to go skiing in three months, and to enter the rugby field in four months and become the champion of Moscow in the 2015 season .
Tatyana Churakova
Russian team, water skiing
Dear Viktor Viktorovich, I want to thank you for the operation on the Achilles tendon and all the medical care. personnel of traumatology of FMBA of Russia N-83. Thank you for your professionalism, for your support, it was not at all scary with you. Despite the complexity of your work, you charge with a positive attitude and there is no doubt that something is wrong. I thank God that it was you who did this operation. I fully recovered and started training in full. Thank you.
Soloviev Denis
MSMK in sports aerobics, European champion, winner of the VII World Games, winner of the first European Olympic Games
Good afternoon, on behalf of the athletes of the Russian national aerobics team, I would like to thank the team of doctors and physicians who provided timely medical support to us at the 7th World Games held in the city of Cali (Colombia). And also for carrying out an urgent operation for Polyanskikh Polina Sergeevna. Personally, I want to thank Viktor Viktorovich Mukhanov for the assistance rendered. With gratitude and best wishes – Soloviev Denis Olegovich (MSIC in sports aerobics, European champion, winner of the VII World Games, winner of the first European Olympic Games).
And also for carrying out an urgent operation for Polyanskikh Polina Sergeevna. Personally, I want to thank Viktor Viktorovich Mukhanov for the assistance rendered. With gratitude and best wishes – Soloviev Denis Olegovich (MSIC in sports aerobics, European champion, winner of the VII World Games, winner of the first European Olympic Games).
Zlyvko Alisa
Russian national basketball team
Faced with many doctors, had the experience of unsuccessful operations to restore the ACL. Therefore, I can say with confidence that Viktor Mukhanov is the only doctor to whom I trust my knee! Thanks for the help!
Andrey Shimanov
Russian youth football team
I express my heartfelt gratitude and wholeheartedly thank doctor V.V. Mukhanov for high professionalism, responsiveness, warmth. Please accept my best wishes for health and success in your noble cause.
Gligor Vitaliy
Head of the FMBA of Russia Uiba Vladimir Viktorovich from the Senior Coach of the Russian national team in judo – the sport of the blind
We express our sincere gratitude to the entire team of the Sports Injury Department and personally to the Head of the Department, Doctor of Medical Sciences Sergey Vasilievich Arkhipov and traumatologist Nikolay Nikolaevich Sovetnikov for carrying out the operation and subsequent rehabilitation of members of the Russian national judo team, Paralympic Games Champion, 4-time World Champion and multiple European Champion Kretsul Oleg Vasilyevich and silver medalist of the World Championship Andrey Viktorovich Vankin. We would like to note the high professionalism, attention and care for the athletes on the part of the entire staff of the department, which creates a homely atmosphere and contributes to the speedy recovery of athletes.
Andrey Vankin
Senior coach of the Russian men’s national team in judo-sport for the blind of Russia Andrey Vankin, master of sports.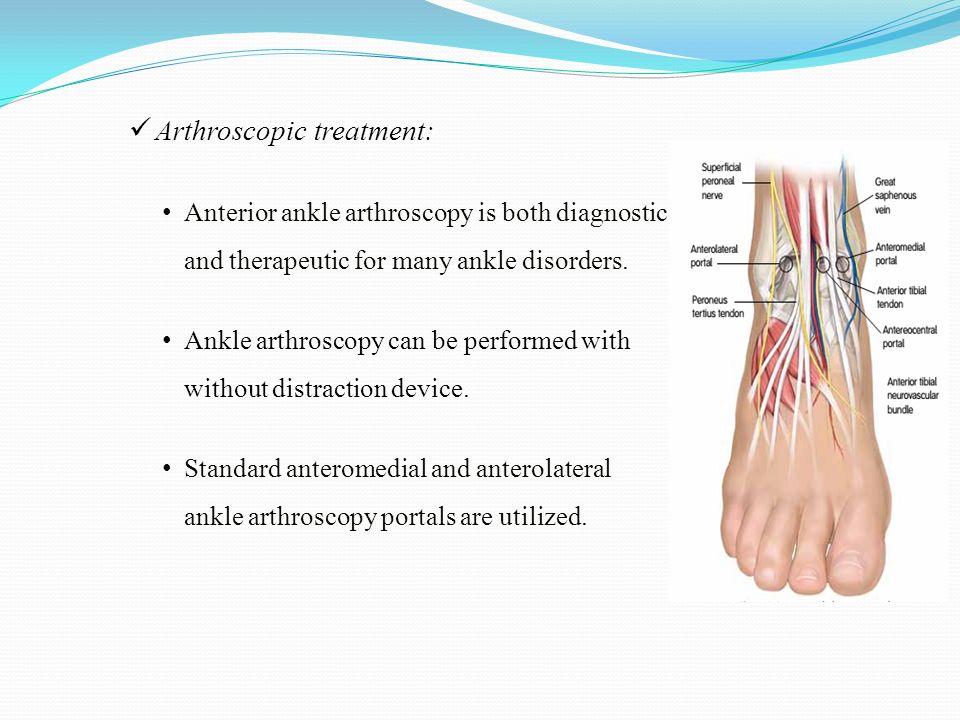 Member of the Russian Paralympic judo team (sport of the blind)
Member of the Russian Paralympic judo team (sport of the blind)
From the bottom of my heart I express my deep gratitude to the entire staff of the traumatology department of hospital No. 83. Frankly, I am amazed at the level of medical care that takes place in your department, for the warm, friendly attitude towards patients.
Special thanks to V. V. Mukhanov.
Fayzzulina Aigul
Master of Sports of Russia
The hospital is wonderful! The service of patients in the traumatology department and the cleanliness maintained in it are beyond praise. A team of highly educated medical specialists, such as Mukhanov V.V. and Budashkina M.V., serving patients of the medical team, was competently selected. nurses, room cleaners, etc. Thank you very much for being there and treating sick people so wholeheartedly and successfully.
Olga Zabrodskaya
member of the Russian Paralympic judo team, master of sports of international class
I would like to express my gratitude to the doctors and junior medical staff of the traumatology department of the 83rd hospital.


 Several ligaments in the ankle help keep it stable and allow it to move. Torn ligaments can be repaired with this type of surgery.
Several ligaments in the ankle help keep it stable and allow it to move. Torn ligaments can be repaired with this type of surgery.
