Arthritis whole body. Comprehensive Guide to the Impact of Rheumatoid Arthritis on the Whole Body
How does rheumatoid arthritis affect the eyes, mouth, hands, feet, and major organs? Discover the symptoms, causes, and treatment options to protect your body from this autoimmune disease.
Rheumatoid Arthritis: A Systemic Condition
Rheumatoid arthritis (RA) is an autoimmune inflammatory condition that primarily affects the joints, causing pain, stiffness, and swelling. However, RA is not just a localized joint disease – it is a systemic condition that can impact the entire body, damaging major organs and even leading to a shortened life span if left untreated.
The key to managing RA and preventing long-term complications is early intervention with medication. According to Dr. Jonathan Greer, a rheumatologist in Boynton Beach, Florida, “The earlier you begin medication, the better your chances of halting joint damage, protecting your organs, and living a longer life without pain and disability.”
The Eyes: Protecting Vision from Rheumatoid Arthritis
Rheumatoid arthritis can affect the eyes in several ways. Inflammation around the eyes can lead to dry eye syndrome or episcleritis, a redness in the white part of the eye. These conditions can generally be managed with over-the-counter or prescription eye drops.

A more serious eye condition is scleritis, where a deeper part of the white area, the sclera, is affected. Untreated scleritis can lead to vision loss. Uveitis, an inflammation of the eye’s middle layer, the uvea, can also develop, causing floaters, blurred vision, and pain. Untreated uveitis can put a person at risk of glaucoma, which can damage the optic nerve and cause blindness.
Treatment for scleritis and uveitis typically involves corticosteroid eye drops, and in some cases, oral or injected corticosteroids may be necessary. It’s important to note that up to 30% of people with RA also develop another autoimmune disease, Sjögren’s syndrome, which can further affect tear glands and lead to very dry eyes.
The Mouth: Maintaining Oral Health with Rheumatoid Arthritis
Research shows that people with rheumatoid arthritis may be more prone to developing periodontal disease, which usually starts with a gum infection. They are also more likely to experience dry mouth, which can increase the risk of tooth decay. Interestingly, the relationship may also work the other way around – poor oral health may contribute to the onset or worsening of RA.

Evidence suggests that bacteria in the mouth can create autoantibodies that attack the lining of the joints. Damaged gum tissue can also allow these bacteria to travel from the mouth into the bloodstream and affect other parts of the body. To maintain good oral health and manage RA, it’s recommended to schedule frequent dental checkups, every three months if possible, to catch and treat any issues early.
Hands and Feet: Preventing Deformities and Nerve Damage
Since rheumatoid arthritis primarily affects the joints, it’s no surprise that the hands and feet are commonly impacted. Without early treatment with disease-modifying antirheumatic drugs (DMARDs), RA can cause various deformities and distortions in the hands, such as locking joints, ulnar deviation (a weakening of tendons and ligaments that causes fingers to curve toward the pinkie), swan-neck deformities, and even ruptured tendons.
These effects can make basic daily tasks, such as writing, holding objects, and unscrewing lids, extremely difficult. The hands may also be affected by muscle cramping, which can be relieved with gentle movements and warm compresses. Additionally, the inflammation of RA can affect the median nerve, causing numbness or carpal tunnel syndrome.

In the feet, uncontrolled inflammation may lead to joint deformities, including hammertoes and bunions, as well as nerve pain and inflammation of the tendons. Proper foot care and the use of orthotics or other supportive devices can help manage these issues.
Protecting Major Organs from Rheumatoid Arthritis
Rheumatoid arthritis is not just a joint disease – it can also impact major organs, including the heart, lungs, and kidneys. The inflammation associated with RA can lead to conditions such as pericarditis (inflammation of the heart’s outer lining), myocarditis (inflammation of the heart muscle), and vasculitis (inflammation of the blood vessels).
Lung involvement in RA can manifest as interstitial lung disease, which can cause scarring and stiffening of the lung tissue, making it difficult to breathe. Kidney problems, such as glomerulonephritis (inflammation of the kidney’s filtering units), can also occur due to the systemic nature of rheumatoid arthritis.
Early detection and management of these organ-related complications are crucial, as they can significantly impact a person’s overall health and life expectancy. Regular monitoring by a rheumatologist and other specialists is essential for individuals living with rheumatoid arthritis.

Addressing the Whole-Body Impact of Rheumatoid Arthritis
Rheumatoid arthritis is a complex, multifaceted condition that goes beyond just affecting the joints. It is a systemic disease that can impact the eyes, mouth, hands, feet, and major organs, leading to a range of complications if left untreated.
By understanding the wide-ranging effects of RA and seeking early intervention with appropriate medications and therapies, individuals with this autoimmune disorder can better protect their overall health and quality of life. Regular checkups with rheumatologists, ophthalmologists, dentists, and other specialists are crucial for comprehensive management of this condition.
Preventing and Managing Rheumatoid Arthritis Complications
What are some key steps to prevent and manage the complications of rheumatoid arthritis?
The most important step is to begin treatment with disease-modifying antirheumatic drugs (DMARDs) as early as possible. Early intervention can help halt joint damage, protect major organs, and improve long-term outcomes.
Regular eye exams with an ophthalmologist are critical for detecting and managing eye-related conditions, such as dry eye, scleritis, and uveitis. Maintaining good oral hygiene and scheduling frequent dental checkups can help prevent and manage gum disease and tooth decay.
For the hands and feet, using assistive devices, such as splints or orthotics, can help maintain function and prevent deformities. Gentle exercises and warm compresses can also help manage muscle cramping and other issues.
Monitoring for and addressing any organ-related complications, such as heart, lung, or kidney problems, through regular checkups and appropriate treatment is essential for protecting overall health and longevity.
By taking a comprehensive, proactive approach to managing rheumatoid arthritis, individuals can minimize the risk of long-term complications and maintain the best possible quality of life.
How Rheumatoid Arthritis Affects the Whole Body
Rheumatoid arthritis (RA), an autoimmune inflammatory condition that causes pain, stiffness, and swelling, is most noted for its effects on the body’s joints. But rheumatoid arthritis is also a systemic disease, meaning it can affect the whole body, damage major organs, and even lead to a shortened life span.
The earlier you begin medication, the better your chances of halting joint damage, protecting your organs, and living a longer life without pain and disability, says Jonathan Greer, MD, a rheumatologist in Boynton Beach, Florida.
Here’s everything you need to know to protect various parts of your body if you have RA.
How Rheumatoid Arthritis Can Affect Your Eyes
Because of inflammation around the eyes, some people with rheumatoid arthritis may get either dry eye syndrome or episcleritis, a redness in the white part of the eye. These can generally be managed with over-the-counter or prescription drops, according to Johns Hopkins Medicine.
A more serious eye condition is scleritis, in which a deeper part of the white area, the sclera, is affected. Untreated, scleritis can lead to vision loss.
Uveitis can develop when the eye’s middle layer, the uvea, is inflamed. This brings on floaters (cobwebs or black spots in the field of vision), blurred vision, and pain, says Ana-Maria Orbai, MD, a rheumatologist and an assistant professor of medicine at the Johns Hopkins University School of Medicine in Baltimore.
Untreated uveitis can put a person at risk of glaucoma, a disease that causes pressure to build up in the eye that can ultimately damage the optic nerve and cause blindness. (This can also happen to people who take steroid medications for RA over a long period of time.) Treatment for both scleritis and uveitis involves corticosteroid eye drops, though this may not be enough to treat uveitis beyond the front of the eye, in which case oral and injected corticosteroids may be needed, according to the Mayo Clinic.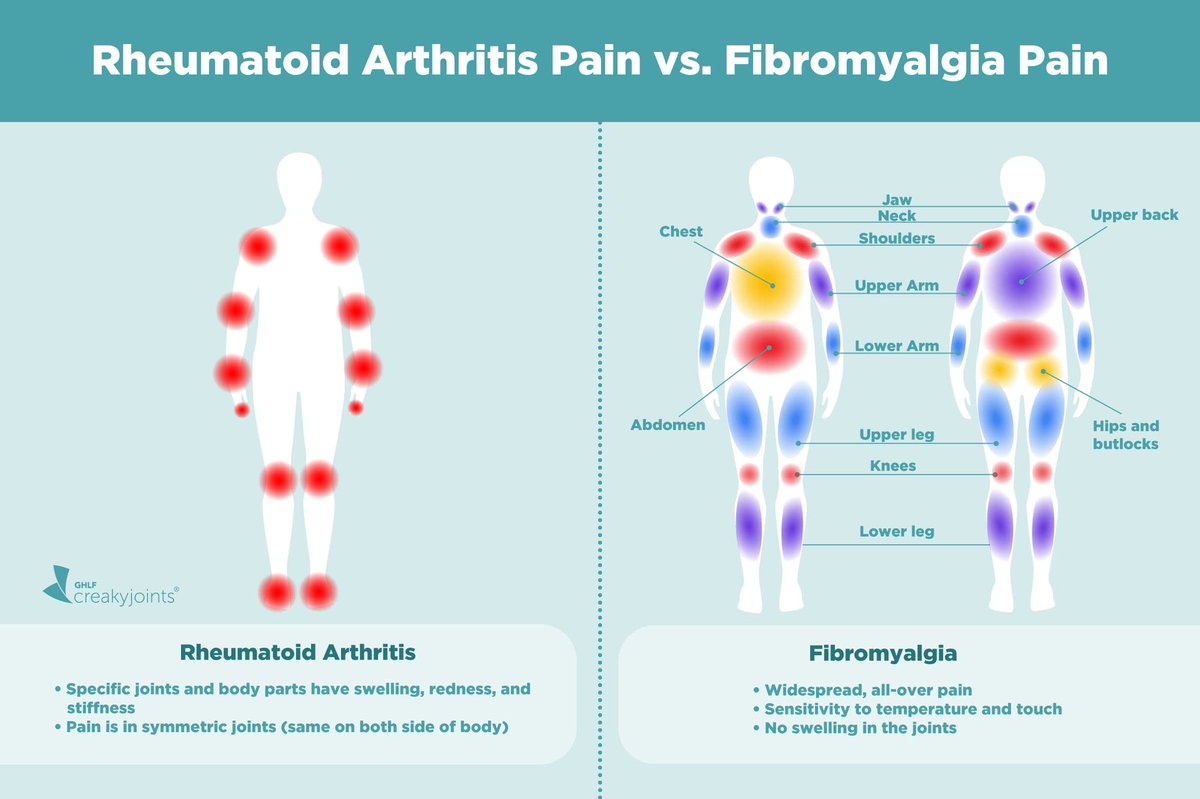
It’s also important to note that up to 30 percent of people with RA develop another autoimmune disease, Sjögren’s syndrome. This disease affects tear glands (as well as salivary glands), causing very dry eyes along with other symptoms.
Because of the risk of these eye diseases, regular eye exams by an ophthalmologist are critical to diagnosing these conditions early, which is why everyone living with RA should see this specialist every year.
RELATED: Rheumatoid Arthritis and Your Eyes: What to Know
How Rheumatoid Arthritis May Affect Your Mouth
Research shows that people who have rheumatoid arthritis may be more likely to develop periodontal disease, which usually starts with a gum infection.
They are also more likely to have dry mouth, which can predispose them to tooth decay. (This is especially true for people with coexisting Sjögren’s syndrome.)
The flip side of this may be true too: Poor oral health may lead to the onset or worsening of RA. Evidence suggests that bacteria in the mouth create autoantibodies that can attack the lining of the joints; according to the Arthritis Foundation, damaged gum tissue allows these bacteria to travel from the mouth into the bloodstream and affect other parts of the body.
Evidence suggests that bacteria in the mouth create autoantibodies that can attack the lining of the joints; according to the Arthritis Foundation, damaged gum tissue allows these bacteria to travel from the mouth into the bloodstream and affect other parts of the body.
Researchers have been working to better understand the mechanism behind this, but the takeaway is that treating gum disease and preventing unnecessary gum infections is good for your RA, as well. Schedule frequent dental checkups to catch minor issues before they become major problems. Some rheumatologists recommend a visit every three months, instead of the usual six, if you can afford it or your insurance covers it.
Rheumatoid Arthritis and Your Hands and Feet
Since RA is a condition of the joints, it’s obvious that it affects a person’s hands and feet. But beyond joint pain, RA can cause other distortions and deformities if it is not treated as early as possible with disease-modifying antirheumatic drugs (DMARDs).
Some of the most common symptoms affecting the hands include locking joints, ulnar deviation (also called ulnar drift — a weakening of tendons and ligaments that cause fingers to curve toward the pinkie), swan-neck deformities (distortions of the joints causing unusual bending and straightening), and even ruptured tendons, according to research published in the European Journal of Orthopaedic Surgery and Traumatology in 2020. All these effects can make basic life tasks such as writing, holding objects, and unscrewing lids difficult.
The hands can also be affected by muscle cramping, which can be relieved by gentle movements and warm compresses. More concerning, the inflammation of RA can affect the median nerve (which runs from the wrist to the fingers), causing numbness or carpal tunnel syndrome, notes CreakyJoints. See your doctor if you experience any of these.
In the feet, uncontrolled inflammation may lead to painful conditions like hammertoes (abnormal bending of the toes), bunion (a bony nodule on the outside edge of the big toe), a collapsed arch, and flatfoot deformity, notes the American Academy of Orthopaedic Surgeons.
RELATED: How to Relieve Rheumatoid Arthritis Related Foot Pain
In addition to seeing your rheumatologist and, if necessary, a podiatrist, you may also consult an occupational or physical therapist. These experts help you learn ways of moving that are less painful and that strengthen muscles, says Rebecca Manno, MD, a rheumatologist and adjunct assistant professor of medicine at the Johns Hopkins University School of Medicine in Baltimore.
Rashes, Ulcers, and Bumps: How RA Affects Your Skin
A skin rash or ulcers on the arms and legs sometimes occur in people with rheumatoid arthritis, especially if the disease has gone untreated for a long time, Dr. Greer says.
Up to 25 percent of people with RA develop rheumatoid nodules — knots of inflammatory tissue just under the skin near a joint. Most often appearing on the elbows, hands, and feet, they can be treated with a steroid injection if they become bothersome.
The conditions that affect the skin tend to resolve once RA is controlled with DMARD medications.
Rheumatoid Arthritis and Your Heart and Circulatory System
Higher levels of inflammation in people with rheumatoid arthritis increase the risk of heart disease, especially heart attacks and strokes, Greer says. Inflammation increases the buildup of plaque in the arteries, which narrows blood vessels and slows blood flow, notes the Arthritis Foundation, upping the chances of stroke and heart attack.
These heart conditions are also more deadly in those with RA. In people with systemic inflammatory diseases, heart attacks in those under 50 were found to be twice as likely to be fatal compared with heart attacks in people without an inflammatory condition, according to a study published in the European Journal of Preventive Cardiology in March 2021.
To lower your risk, you’ll want to get your RA under control and also reduce heart risk factors, such as high blood pressure and high cholesterol. A healthy diet like the Mediterranean diet can lower your risk of heart disease.
Another way to assist your heart and improve your RA: Don’t smoke; and if you do smoke, quit as soon as possible; in addition, avoid exposure to secondhand smoke.
Finally, know that certain RA medications themselves – including NSAIDs and steroids, per the Arthritis Foundation – have been linked to heart problems; JAK inhibitors may raise cholesterol levels, notes CreakyJoints. But these side effects are are not a reason to skip drug treatment. “The negative effects of not treating RA with medication are much, much worse than the side effects of RA drugs,” cautions Greer.
RA Can Trigger Anemia and Fatigue
A large percentage of people living with RA experience anemia, a shortage of red blood cells or the iron-rich hemoglobin in the red blood cells. Red blood cells carry oxygen from your lungs to all the cells in the body and organs, so when your organs aren’t getting enough O2, you can experience weakness, fatigue, headaches, shortness of breath, dizziness, and more.
There are different types of anemia, and a common type in RA patients is called anemia of chronic disease. RA’s inflammatory molecules may interfere with the body’s ability to use iron, which in turn leads to anemia. Iron supplementation can help, but the best treatment is to keep the inflammation of RA under control with DMARD medication.
Another cause of fatigue: Autoimmune disorders like RA can trigger the release of inflammatory cytokines (proteins) in the blood, and the body undergoes stress as it tries to manage this, which leads to fatigue, notes the Arthritis Foundation. In addition, the depression and pain that may come along with RA continually sap energy.
RELATED: The Link Between Rheumatoid Arthritis and Anemia
Fever: A Full-Body Effect of Rheumatoid Arthritis
According to the American College of Rheumatology, low-grade fever is one of many common rheumatoid arthritis experiences. The Centers for Disease Control and Prevention (CDC) considers an adult to have a fever when their temperature is at least 100. 4 degrees F (37.8 degrees C), with symptoms of feverishness or chills.
4 degrees F (37.8 degrees C), with symptoms of feverishness or chills.
Fever can occur as a result of your body’s autoimmune response. Once you start treating your RA, systemic symptoms like fever should improve, notes CreakyJoints, but some people may still develop low-grade fevers on occasion, depending on their disease activity.
How Rheumatoid Arthritis Impacts Organs
In addition to heart problems, RA can increase your risk of damage to other organs, such as the lungs and kidneys.
Rheumatoid Arthritis and Your Lungs
The most common RA-related lung complication is interstitial lung disease (ILD), a condition that causes inflammation and scarring of the lung tissue. This illness can be hard to detect but occurs when lung tissue becomes inflamed and eventually scarred.
It’s unclear exactly how many people with RA develop it, but French researchers presenting an abstract at the American College of Rheumatology (ACR) annual conference in 2020 found that the prevalence of subclinical (symptomless) ILD was 18 percent in people who had RA for a dozen years. Other research has detected ILD in up to 60 percent of patients with RA, with 10 percent of cases being clinically significant. People with RA are nine times more likely to develop ILD than the general population, according to a review published in May 2022 in Frontiers in Medicine.
Other research has detected ILD in up to 60 percent of patients with RA, with 10 percent of cases being clinically significant. People with RA are nine times more likely to develop ILD than the general population, according to a review published in May 2022 in Frontiers in Medicine.
This scarring makes it harder for oxygen in the lungs to enter the bloodstream and travel to other organs. The condition can cause breathlessness and coughing, but it can also be asymptomatic. If untreated, it can progress to pulmonary fibrosis, in which tissues are permanently scarred.
Research also shows that RA sufferers are at double the risk of chronic obstructive pulmonary disease, or COPD (which includes emphysema and chronic bronchitis), in which the air sacs can’t expand as easily and become clogged with mucus. There is no cure for COPD, although inhalers and steroids can help open airways.
Pleural effusion is another condition with increased risk. Here, the pleura — the tissue surrounding the lungs — becomes inflamed, which can lead to fluid buildup between the lung and the chest wall, according to the Arthritis Foundation.
People with RA may also develop nodules in the lungs, though they may not be bothered by them. (Nodules can also form on the throat and vocal cords, causing difficulty speaking.)
Being proactive and diligent about your RA treatment can address inflammation and minimize the risk for lung problems. And of course, if you smoke, quit.
Rheumatoid Arthritis and Kidney Function
People with RA have a greater risk of developing chronic kidney disease, though as RA treatment has improved — including the use of biologic medications and a decrease in chronic NSAID use — kidney problems have been reduced, according to an article published in Rheumatic Diseases Clinics of North America in November 2018.
Amyloidosis, a condition caused by the abnormal buildup of certain proteins that can impair kidney function, may occur in association with RA — usually in the later stages or if someone’s disease isn’t well-controlled with medication. The symptoms can be vague, such as weakness or swelling, and can include an enlarged spleen and gastrointestinal issues.
To screen for amyloidosis, rheumatologists will periodically check your kidney function.
To maintain healthy kidneys, you should also take care not to overuse nonsteroidal anti-inflammatory painkillers (NSAIDs), like ibuprofen and naproxen, as they can damage the kidneys, too.
RELATED: Protect Your Kidneys When You Have RA
Mental Health: Rheumatoid Arthritis and Depression
The fear that comes with living with any chronic illness, as well as dealing with daily pain and limited mobility, can take a toll on emotional wellness. But when it comes to RA, depression can be more than just an emotional response to the disease. “There is a clear link between RA and depression,” says Daniel Solomon, MD, MPH, the chief of the clinical sciences section in the division of rheumatology at Brigham and Women’s Hospital in Boston. “We don’t yet understand how much of the depression is from a reaction to the disease and how much is the inflammation of the disease, but they both contribute somehow. ”
”
What experts do know is that treatment for RA’s inflammation quells the inflammation associated with depression. The opposite may also be true: Treatment for depression (with talk therapy or medication, for example) may lessen the pain of the disease. As the Arthritis Foundation notes, while pain can incite depression, depression can also worsen pain. According to research presented at the 2021 annual congress of the European Alliance of Associations for Rheumatology (EULAR), catastrophizing about pain makes it worse, and it can actually impede RA remission.
RELATED: The Link Between RA, Depression, and Anxiety
Rheumatoid Arthritis Can Threaten Bone Health
RA can increase your risk of osteoporosis, a disease in which bones become less dense and more fragile, increasing the likelihood they will break.
According to a study in the August 2021 issue of Cureus, there are several reasons for this association: chronic joint inflammation, genetics, the role of estrogen, and the fact that certain RA medications, such as corticosteroids, can speed bone loss.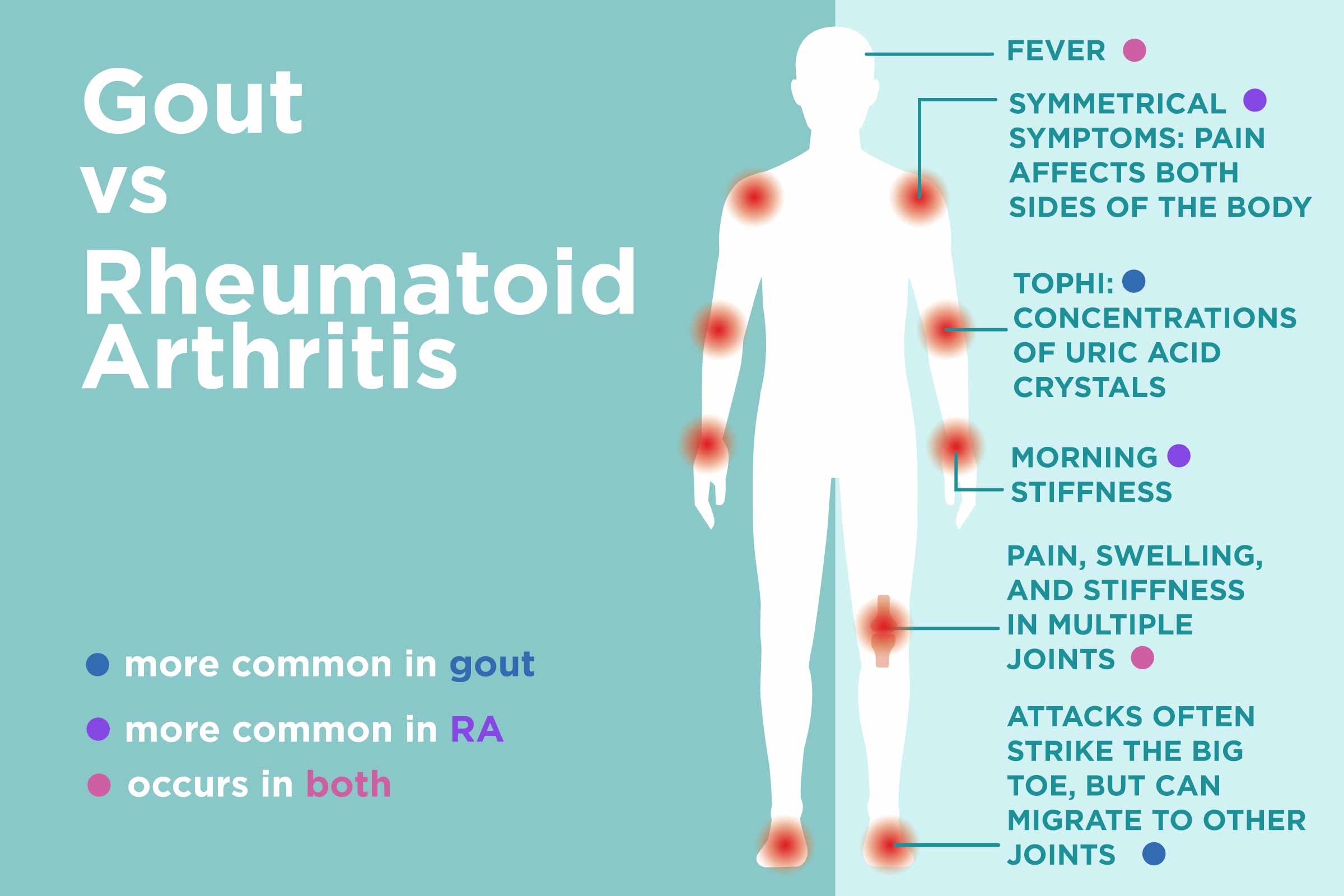 Bone loss is most prevalent in areas that immediately surround joints affected by rheumatoid arthritis, notes the National Institutes of Health (NIH). Fractures most commonly occur at the spine, wrist, and hip, per the American College of Rheumatology (ACR), which notes that spine and hip fractures may lead to chronic pain, disability, and even death.
Bone loss is most prevalent in areas that immediately surround joints affected by rheumatoid arthritis, notes the National Institutes of Health (NIH). Fractures most commonly occur at the spine, wrist, and hip, per the American College of Rheumatology (ACR), which notes that spine and hip fractures may lead to chronic pain, disability, and even death.
The best way to protect bones when you have rheumatoid arthritis? Eat calcium-rich and vitamin D–rich foods like eggs and fish, as well as D-fortified foods; do weight-bearing exercises (walking, stair-stepping) that your doctor approves; if you smoke, quit; and get a bone mineral density test so your doctor can consider whether you need medication.
RELATED: What to Eat and What to Avoid for Osteoporosis Prevention
How to Relieve Rheumatoid Arthritis Foot Pain
Rheumatoid arthritis can cause symptoms in the feet such as joint pain, ankle swelling, stiffness, and a burning sensation. Learn how to prevent and relieve…
Learn how to prevent and relieve…
By Susan L Sullivan
How Massage Therapy Helps Ease Rheumatoid Arthritis Pain
Rheumatoid arthritis symptoms such as pain and stiffness can be reduced by moderate pressure massage and other types of massage therapy. Learn more about…
By Madeline R. Vann, MPH
What Does Arthritis Pain Feel Like?
There are two arthritis types: inflammatory (rheumatoid arthritis) versus mechanical (osteoarthritis). Both involve the joints but other symptoms and …
By Diana Rodriguez
Can Mindfulness Meditation Ease Rheumatoid Arthritis Pain?
Mindfulness-based stress reduction (MBSR) programs may help people with rheumatoid arthritis. Learn how it helps reduce perception of pain and other RA…
By Meryl Davids Landau
Rheumatoid Arthritis Diagnosis
To diagnose rheumatoid arthritis, doctors take many steps. There is no single test that can definitively diagnose RA. Learn about the process for this…
There is no single test that can definitively diagnose RA. Learn about the process for this…
By Joseph Bennington-Castro
Top Assistive Devices for Rheumatoid Arthritis
Rheumatoid arthritis can make it tough to dress, cook, and clean, but simple devices can make everyday tasks easier without stressing your joints.
By Connie Brichford
How Rheumatoid Arthritis Affects the Lungs
Besides damaging joints, rheumatoid arthritis can hurt the lungs. Learn about interstitial lung disease (RA-ILD) and lung protection.
By Connie Brichford
8 Ways to Prevent Rheumatoid Arthritis Joint Damage
Rheumatoid arthritis can leave joints feeling painful and stiff. Find out how exercise, a healthy diet, and other healthy habits can help.
By Diana Rodriguez
7 Top Cities for People With Rheumatoid Arthritis
Abundant sunshine, good transportation, and a low-stress lifestyle are just a few key qualities that help determine which cities are rheumatoid arthritis.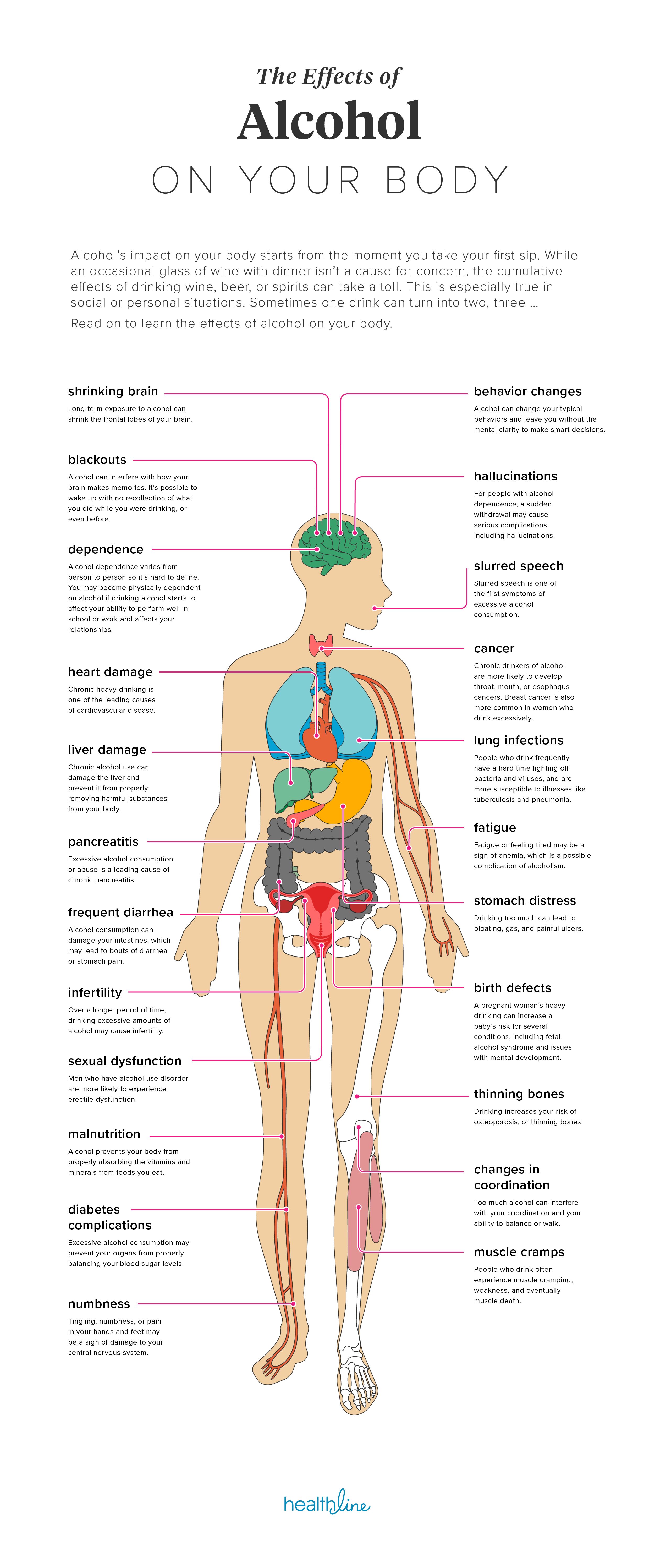 ..
..
By Beth W. Orenstein
Fibromyalgia | Causes, symptoms, treatment
-
What is fibromyalgia?
-
Symptoms
-
Who gets fibromyalgia?
-
Causes
-
Diagnosis
-
What does the future hold for me?
-
Treatments
-
Physical therapies
-
Psychological therapies
-
Drug treatments
-
How can I help myself?
-
Research and new developments
-
Lynn’s story
Get help
What is fibromyalgia?
Fibromyalgia is a long-term condition that causes pain and tenderness all over your body.
Unlike arthritis, this isn’t because you have problems with your joints, bones or muscles. It’s thought to be caused by your nervous system in your brain and spine not being able to control or process pain signals from other parts of your body.
The condition is also linked to:
- poor sleep
- feeling you can’t concentrate or remember things
- extreme and constant tiredness that doesn’t improve with sleep or rest – which is known as fatigue.
There can be many other symptoms that affect different parts of your body.
Symptoms
The main symptoms of fibromyalgia are:
- pain – you may feel as though you’ve got pain that spreads throughout your entire body, with certain parts – such as your neck and back – feeling particularly painful
- tiredness, fatigue and generally feeling like you have no energy
- sleeping badly – waking up feeling unrested
- aching and stiffness, which often feels worse during or after you’ve been active.

It’s common for your condition to flare-up, making your symptoms suddenly worse.
Fibromyalgia can also cause:
- forgetfulness or poor concentration
- stress, worry or low mood
- tingling, numbness or swelling of your hands and feet
- headaches
- restless legs syndrome – a tingling, uncomfortable feeling in your legs, especially at night
- irritability, or feeling low or weepy
- feeling like you urgently need to wee, especially at night
- painful menstrual periods
- diarrhoea, constipation and stomach pain – sometimes separately diagnosed as irritable bowel syndrome (IBS)
- increased sensitivity to things like cold, sound, knocks and bumps
- tender or overly sensitive joints and muscles.
The pain may feel like it’s affecting your whole body, or it may be particularly bad in just a few areas. Some people say their pain gets worse in extreme temperatures, such as very hot, cold or damp weather.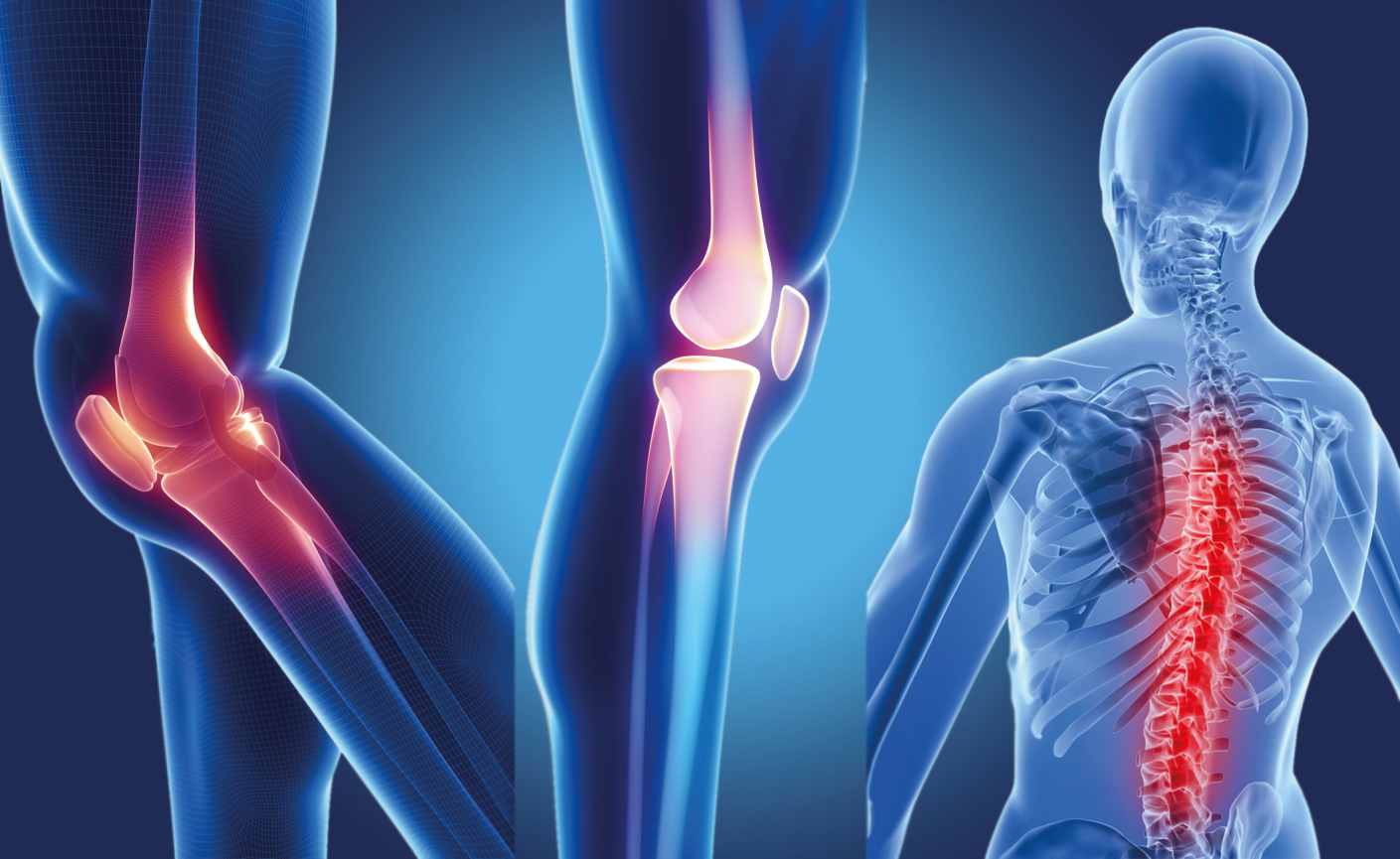
People often say that besides the pain, fatigue is the worst part of fibromyalgia. This can be linked to a difficulty to think clearly or remember things properly, which is sometimes called fibro fog or brain fog.
Who gets fibromyalgia?
It’s estimated that somewhere between 1.8 million and 2.9 million people in the UK have fibromyalgia.
It most commonly develops between the ages of 25 and 55, although children can also get it. It appears that more women are diagnosed with fibromyalgia than men.
Does it run in families?
We don’t know for sure whether fibromyalgia can run in families.
It’s thought that people can inherit genes that make them more likely to get fibromyalgia, and the condition can then be triggered by an injury, physical or psychological trauma, or stress.
Causes
We don’t currently know the exact reason why people get fibromyalgia. But there does seem to be a common link with things such as arthritis, a traumatic event, and mental health and well-being.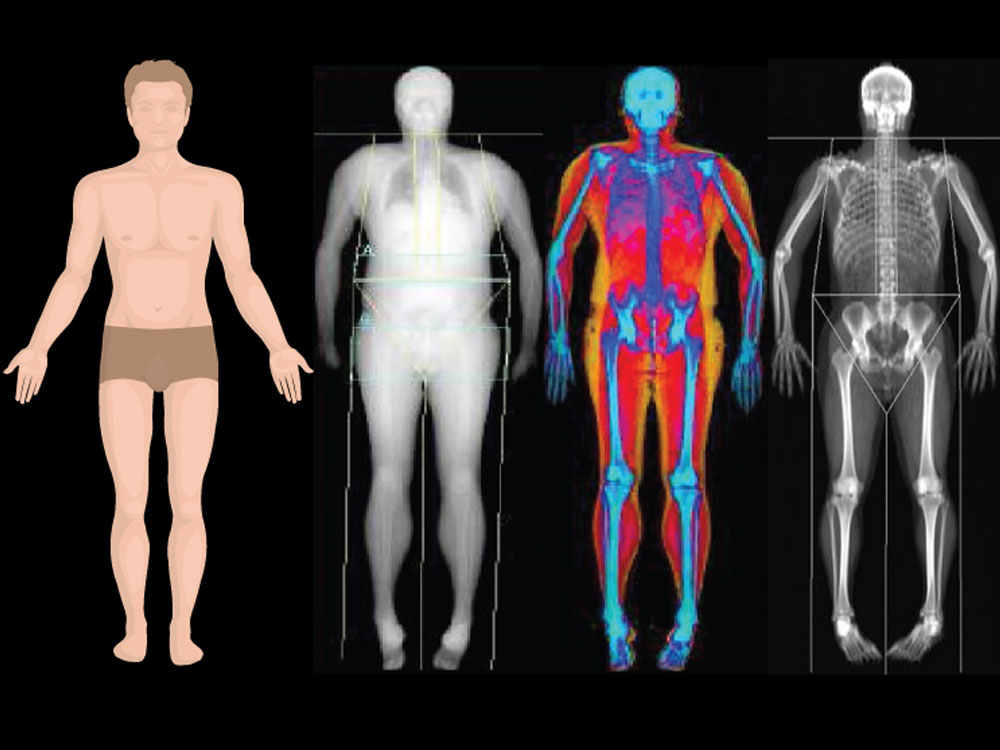
Fibromyalgia isn’t caused by damage or an injury to the body. But it does increase the sensitivity of your nerve endings, which means you could feel pain from a small amount of pressure or minor knocks.
One theory is that the condition is caused by problems with a person’s central nervous system – which controls all the sensations and movements the body makes.
Studies have shown that parts of the brain that register pain react differently if you have fibromyalgia. This means you feel pain when other people just feel uncomfortable or stiff.
People with fibromyalgia often don’t get enough deep sleep. Research shows that lack of good quality sleep can make pain worse, and maybe even cause pain.
Pain, unhappiness, depression and stress can all make you sleep badly.
Symptoms often start after an illness, accident, or a time of emotional stress and anxiety.
When you’re low or depressed, your pain can also feel worse. At the same time, your pain can make you feel more stressed.
Unlike conditions, such as arthritis, the pain you feel with fibromyalgia isn’t caused by visible inflammation or damage to your body.
This doesn’t mean the symptoms of fibromyalgia are unreal or ‘all in your mind’. However, anxiety, physical or mental trauma, and sleep disturbance are all thought to play a part in the condition.
Diagnosis
Fibromyalgia can sometimes be difficult to diagnose, as the symptoms vary from person to person.
There are some common symptoms your doctor will look for to help diagnose fibromyalgia, including:
- severe pain that has lasted three months or more
- fatigue
- regularly waking up feeling unrefreshed
- problems with your memory and understanding.
It may help your doctor understand the problems you’re having if you make a list of any physical or psychological problems you’ve experienced. They will probably then carry out a physical examination.
There aren’t any specific blood tests, x-rays or scans to confirm a diagnosis of fibromyalgia. But you might have blood tests to check for other conditions.
But you might have blood tests to check for other conditions.
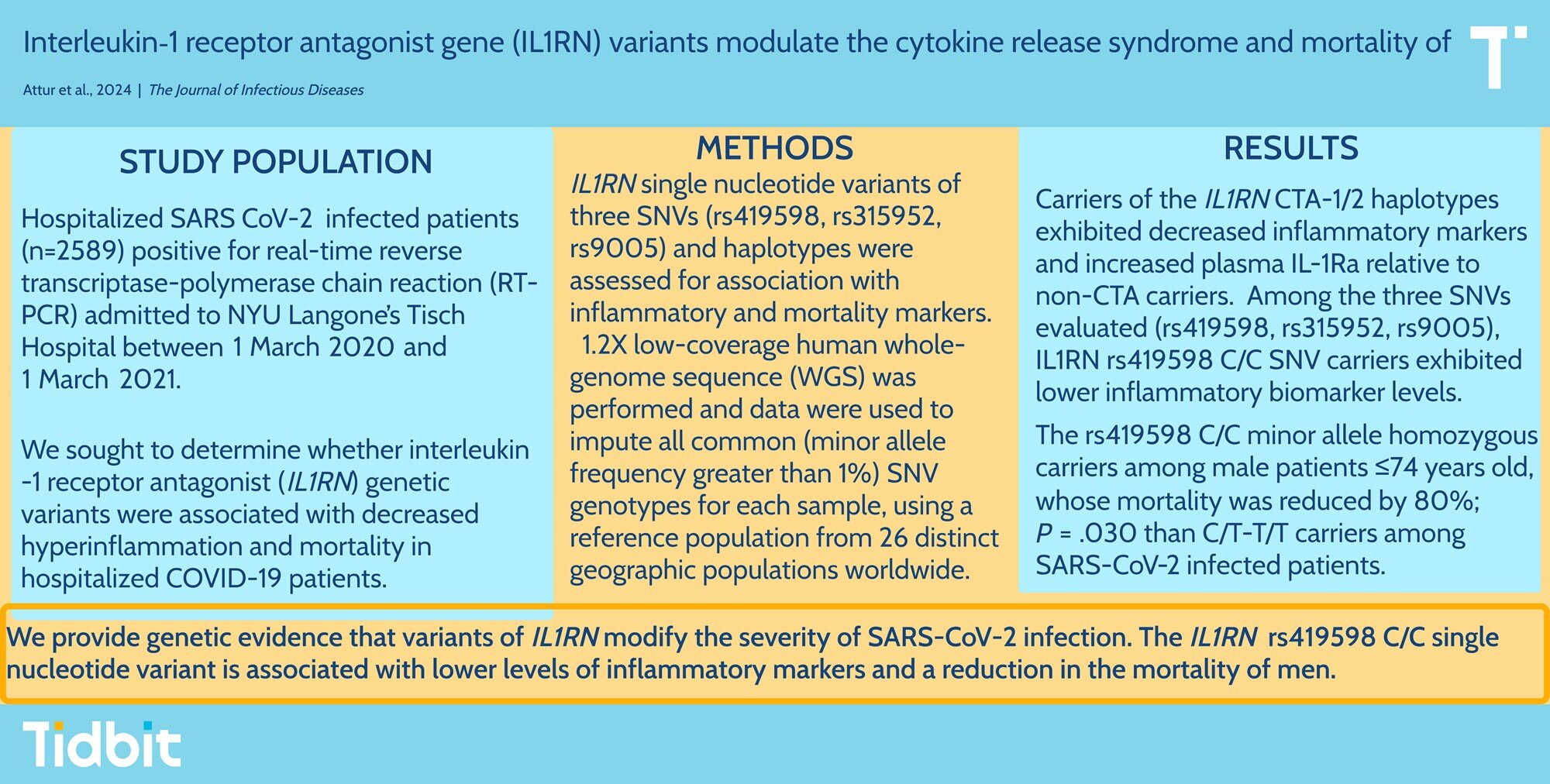
Many symptoms of fibromyalgia are similar to those of other conditions, such as rheumatoid arthritis, Sjögren’s syndrome (sher-grenz sin-drome) and an underactive thyroid gland.
Some people may be diagnosed and treated for one of these other conditions. It is also possible to have one of these conditions as well as fibromyalgia.
Your doctor may also suggest a referral to:
- a rheumatologist – a doctor who specialises in conditions affecting the bones, joints and muscles. They may confirm your diagnosis.
- a physiotherapist – who can suggest exercises and relaxation techniques
- a clinical psychologist or counsellor – who may use methods such as cognitive behavioural therapy (CBT) and mindfulness
- an occupational therapist – who can advise you on the best way to carry out daily activities and work around your condition
- a community or hospital-based specialist pain clinic, or chronic fatigue service – who can help you manage your symptoms.

What does the future hold for me?
Because fibromyalgia’s symptoms vary from person to person, it’s difficult to predict how long you will have the condition and the impact it will have on your life.
Although there’s currently no cure, there are treatments, therapies and self-management techniques that can improve your quality of life.
Fibromyalgia doesn’t seem to cause long-term damage to your body. But it’s important to keep your muscles and joints strong through activity.
Gradually increasing how much exercise you do can also improve your symptoms.
Treatments
There are a number of ways your symptoms can be managed.
In many cases, fibromyalgia can be diagnosed and treated by your GP, without the need to see a specialist.
They can advise you on treatments and therapies that tackle specific symptoms. These may include drug treatments. However, physical and psychological therapies can often be a more effective way of managing fibromyalgia than medication.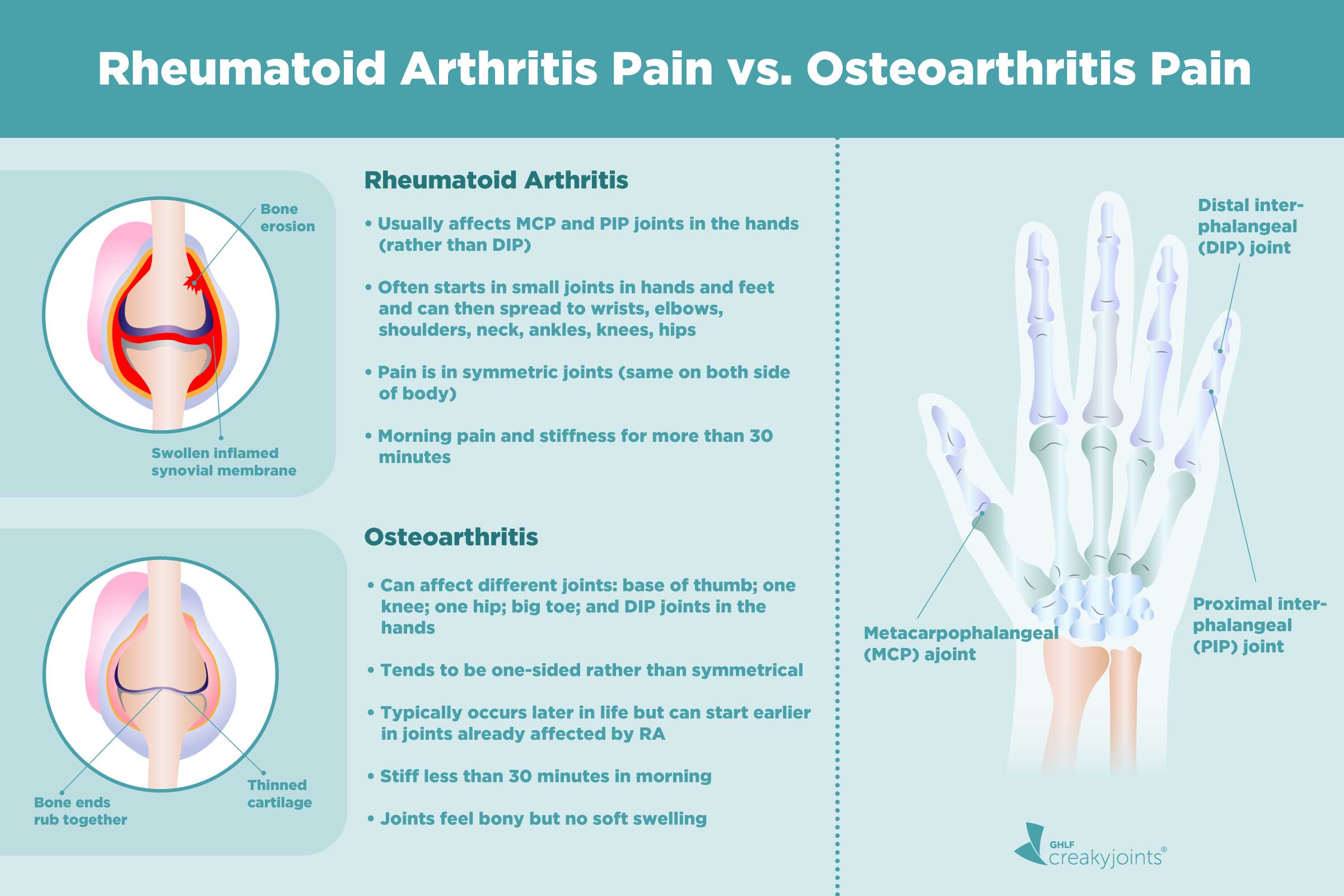
There are also many things you can do for yourself that can change the way your condition impacts upon your life.
Physical therapies
Depending on how your fibromyalgia is affecting you, your doctor may refer you to a physiotherapist or occupational therapist.
Physiotherapy
Physiotherapy can help relieve the pain of fibromyalgia.
Physiotherapists are trained specialists who can help you stay active and independent. They will show you the best exercises to strengthen your muscles, without hurting yourself or putting your body under too much strain.
They can show you how something as simple as improving your posture can help your pain. They may also advise you on relaxation techniques which can be just as important as exercise when you’re dealing with fibromyalgia.
Your doctor can refer you to an NHS physiotherapist. In some areas you can refer yourself, but this may take a while.
It can be quicker to see a physiotherapist privately, but you would pay for the appointment. To find a private physiotherapist, visit the Chartered Society of Physiotherapy website.
To find a private physiotherapist, visit the Chartered Society of Physiotherapy website.
Occupational therapy
Occupational therapy can help you manage your everyday activities around your fibromyalgia, without increasing your pain or overwhelming yourself.
Your occupational therapist may suggest new ways you can get things done. They may also teach you some relaxation techniques.
If you still find some activities difficult after you’ve made these changes, they may suggest equipment, known as aids and adaptations, to help you.
Your doctor can refer you to an occupational therapist or you can see one privately, for a fee.
To find a private occupational therapist, visit the Royal College of Occupational Therapists website.
If you’re having problems at work, your employer may have an occupational health team that could help you. Otherwise, you can contact a Jobcentre Plus office to ask for advice.
Acupuncture
Your doctor may recommend a course of acupuncture from a trained NHS healthcare professional, such as a physiotherapist, to help with your pain. You may be able to receive this treatment at a local health centre or GP surgery.
You may be able to receive this treatment at a local health centre or GP surgery.
Acupuncture uses fine needles, inserted into several specific parts of the body to relieve pain. There is evidence to support its use in the short-term treatment of fibromyalgia. Though a course of treatments may only help for up to three months, it may help you start managing your condition.
Doctors will not recommend treatment with devices such as TENS machines, ultrasound or interferential therapy, because there is currently little evidence to support their use in treating fibromyalgia.
Pain clinics and pain management programmes
Pain clinics bring together the skills of a wide range of professionals, such as:
- specialist pain consultants
- physiotherapists
- occupational therapists
- psychologists
- social workers
- employment advisors.
They can provide specific treatments or rehabilitation therapies that could reduce the effects of fibromyalgia.
A pain specialist may suggest you join a pain management programme, which brings together people with different long-term pain conditions. Pain management won’t take away your pain, but it can help you manage it better and reduce its impact on your life.
These sessions are often led by psychologists who specialise in helping people find ways to live with their pain. They are usually held in an outpatient clinic and run over several days or weeks.
Psychological therapies
Pain is never just a physical experience, especially if it lasts a long time. Pain can affect your mood and behaviour.
Psychological approaches to pain management try to address the emotional effects of your pain and the things that can make your pain worse. They help you look at how your pain affects your thoughts and habits, and how your emotions can affect your pain.
Therapies such as cognitive behavioural therapy (CBT), which is a talking therapy, try to reduce the overwhelming effect of problems such as stress, unhappiness and pain.
They aim to help you understand how you react to different problems by breaking them down into smaller, more manageable, chunks. This should help you change the way you react to them and the effect they have on you.
Making small changes to the way you react to a situation or problem can often improve both your emotional and physical health.
Psychological therapies can also include relaxation techniques and other ways to reduce your stress.
They encourage you not to be too hard on yourself, even when you feel frustrated, and to accept that sometimes there are limits to what you can do.
A number of healthcare professionals often have training in CBT, so you may not have to see a psychologist.
For more information about psychological therapies and CBT, the British Association for Behavioural & Cognitive Psychotherapies (BABCP) keeps a register of all accredited therapists in the UK.
Drug treatments
Drugs can’t treat fibromyalgia, but they can help reduce your symptoms.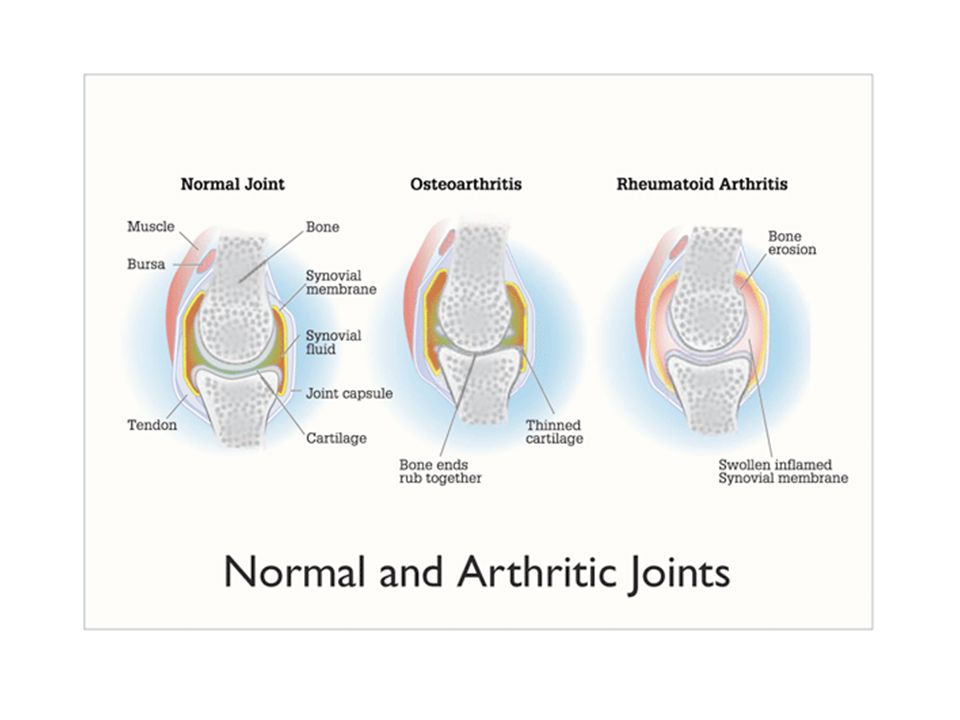 Your doctor may only recommend drug treatment once you’ve tried options such as exercise, psychological therapy or acupuncture.
Your doctor may only recommend drug treatment once you’ve tried options such as exercise, psychological therapy or acupuncture.
Before prescribing drugs to treat your pain, your doctor will discuss the benefits and risks of starting drug treatment. If you are aged over 18, it’s likely they will first try you on an antidepressant, such as:
- amitriptyline
- citalopram
- duloxetine
- fluoexetine
- paroxetine
- sertraline.
Antidepressants are regularly used to treat sleep problems and pain, as well as depression. When they are used to treat pain, they’re usually prescribed at a lower dose than when they are used to treat depression. However, they can still help if your condition effects your mood.
Antidepressants are now recommended by the National Institute of Health and Care Excellence (NICE) as the first choice of drug treatment for unexplained long-term, widespread pain, such as fibromyalgia.
You might need to take them for a few months before you feel their full benefits. Your doctor will gradually increase the dose to a level that works for you.
Your doctor will gradually increase the dose to a level that works for you.
Some antidepressants can make you feel sleepy, so avoid taking them before you drive, cycle or use heavy machinery. You usually need to take them about two hours before bedtime.
All drugs have potential side effects. It’s important to talk to your doctor about how to get the best balance between pain relief and any unpleasant effects. If you feel like a treatment isn’t helping you, talk to your doctor.
In the past people with fibromyalgia have been prescribed a variety of different types of drugs, such as:
- gabapentin and pregabalin, which target nerve pain
- opioid painkillers, such as codeine, tramadol, and morphine
- compound painkillers, including co-codamol and co-dydramol
- paracetamol
- non-steroidal anti-inflammatory (NSAIDs), such as ibuprofen and naproxen
- steroid injections.
If you are currently prescribed one of these drugs, your doctor is likely to want to discuss whether your condition could be treated differently in the future.
How can I help myself?
Exercise
If you’re in pain, your instinct may be to avoid exercise or moving around too much. But keeping active is a really important part of the treatment for fibromyalgia and can prevent other health problems.
Your symptoms and general health can be improved by a combination of aerobic exercise and movements that improve your flexibility and strength.
Exercise has been proven to improve fatigue and our ability to control pain.
At first, you may find that your pain and tiredness become worse, particularly if you’re starting to exercise muscles that haven’t been used for a while. Try to do the same amount of exercise each day, so you build up your muscle strength and your stamina.
Then, after doing your routine of exercises for a couple of weeks, slowly increase the amount you do, and this will improve your fitness, stamina and flexibility.
Aerobic exercises
Aerobic exercise is anything that makes you a little out of breath and your heart beat faster.
Swimming is recommended for people with fibromyalgia. Taking a brisk walk and cycling can also help.
At home, you could step up and down your bottom step several times, or march on the spot to get your heart beating faster.
Strengthening exercises
Strengthening exercises help develop and build the muscles that move and protect your joints. They may be difficult at first but should become easier with practice.
Aim to do at least one session a day, either at home or in a gym. Ask a GP or physiotherapist for examples of strengthening exercises you could do at home.
You can also buy specially designed equipment, such as ankle weights. Begin with lighter weights, then move on to heavier ones, if you feel able to.
Strengthening equipment in a gym allows you to work your muscles by pushing or pulling against a resistance, such as weights or elastic ropes. You can ask an instructor for advice about using the equipment, if you’re not sure.
Stretching exercises
Stretching, or range of movement, exercises can increase your flexibility. You can do these anywhere. There are plenty of examples of exercises online, or you could ask a physiotherapist. Some people with fibromyalgia have found Tai chi and yoga help.
You can do these anywhere. There are plenty of examples of exercises online, or you could ask a physiotherapist. Some people with fibromyalgia have found Tai chi and yoga help.
Diet and nutrition
There’s no particular diet that’s been proven to help fibromyalgia. However, it’s recommended that you keep to a healthy weight by eating a balanced diet that is low in saturated fats, sugar and salt, and has plenty of fruit and vegetables. It’s also good to drink six to eight glasses of water every day.
Complementary treatments
Some people with fibromyalgia find that complementary treatments help their symptoms.
Massage can also be helpful for some people with fibromyalgia. However, the effects don’t often last that long.
If you want to try a complementary treatment, speak to your doctor first, in case it affects any other treatment you’re on.
It’s important to go to a legally registered therapist, or one who has a set ethical code and is fully insured.
If you decide to try therapies or supplements, you should be critical of what they’re doing for you and only continue if they’re helping.
Sleep
Poor sleep appears to be a significant cause of fibromyalgia, so getting enough good-quality sleep is an important part of your treatment. Not only will it help with tiredness and fatigue, it may also improve your pain.
Sleeping tablets are not normally recommended, as the body can become tolerant to them, which can lead to the effects wearing off and even addiction. But regular activity, particularly aerobic exercise, and cognitive behavioural therapy (CBT) have proven effective for people with disrupted sleep patterns.
It can also help to change your habits around bedtime. To help you get a better night’s sleep:
- Make sure your bedroom is dark, quiet and a comfortable temperature.
- Try a warm bath before bedtime to help ease pain and stiffness.
- Develop a regular routine, where you go to bed and get up at a similar time each day.

- You may like to try listening to some soothing music before going to bed.
- Some gentle exercises may help reduce muscle tension, but it’s probably best to avoid energetic exercise too close to bedtime.
- Keep a notepad by your bed – if you think of something you need to do the next day, write it down and then put it out of your mind.
- Avoid caffeine in the eight hours before you go to bed.
- Don’t drink alcohol close to bedtime.
- Avoid eating main meals close to bedtime.
- If you smoke, try to stop smoking, or at least don’t smoke close to bedtime.
- Try not to sleep during the day.
- Avoid watching TV and using computers, tablets or smartphones in your bedroom.
- Don’t keep checking the time during the night.
What else can I do?
Because fibromyalgia varies from person to person, we suggest you try some of the following tips to find out what works for you:
- Learn about fibromyalgia – understanding your condition can help reduce your fears and anxiety.
 It also means you’re fully aware of treatment and self-management approaches that can help you.
It also means you’re fully aware of treatment and self-management approaches that can help you. - Find a support group in your area or an online forum for people with fibromyalgia. Talking about your experiences with other people who understand can help.
- Encourage your family and friends to learn more about your condition and to talk to you about it. You could show them this information. It’s especially important they understand how your pain affects you, even if you look well.
- Find ways to talk about your feelings, such as anxiety, low mood or anger. Counselling or CBT can help – your GP will be able to refer you.
- For ‘fibro fog’, some people find mental exercises like crosswords or jigsaw puzzles help. Do as much as you can to stimulate your brain.
- Pick your best time of day to do anything needing concentration. Explain to others if fibromyalgia affects your memory.
- Learn to pace yourself by breaking tasks into smaller chunks, giving yourself time to rest in between.

- Stress and unhappiness can make fibromyalgia pain feel worse – addressing what’s making you feel that way could help.
- Ask for help from people at your workplace, such as a friend, colleague or manager.
- Working shorter hours, as well as adapting your desk, chair, computer and other working areas for comfort, can all help.
- Ask an occupational therapist, your local Jobcentre Plus office or Citizens Advice service for advice. They can work with both you and your employer.
- Applying heat with a hot water bottle, or having a hot bath or shower, can help pain and improve morning stiffness.
- If you have a dry mouth, try a toothpaste containing sodium bicarbonate.
- Some people have found meditation helps improve their pain.
- Try the treatments your doctor offers and discuss which ones are helpful.
Related information
-
Exercise
Find out more about exercising with arthritis and what types of exercises are beneficial for certain conditions.

Research and new developments
Versus Arthritis is funding a number of research studies into the causes, effects and treatment of fibromyalgia. Some examples include:
- A study at the University of Cambridge is looking at why things that wouldn’t normally be painful, such as sound, light and gentle touch become painful for people with fibromyalgia, and whether brain signals that process pain differ in people with fibromyalgia.
- Research underway at the University of Sussex is examining how the bodies’ natural fight and flight response to stress might be altered in people who have fibromyalgia. This work is also looking at the role inflammation might have in this process.
- We are funding work at the University of Liverpool investigating how the brain processes pain signals. It has been found that in people with long-term pain such as fibromyalgia there are differences in the structure and activity in the parts of the brain that process pain signals.
 Using mathematical modelling, this work could help to match people up with the best treatment option for them.
Using mathematical modelling, this work could help to match people up with the best treatment option for them. - We are also investigating how to improve healthcare services for people with fibromyalgia. Research being carried out at the University of Aberdeen is looking at how long it took people with fibromyalgia to get diagnosed and where in the system improvements can be made.
The Pain Centre Versus Arthritis
In partnership with the University of Nottingham and local NHS Trusts, Versus Arthritis supports the world’s first national centre for research into pain.
The aims of the centre are to improve our understanding of pain and ways to stop it, through existing and new treatments.
The centre has experts in rheumatology, neuroimaging, psychology, neuropharmacology, neurosciences and orthopaedic surgery.
Lynn’s story
Lynn White was diagnosed with fibromyalgia in her early 40s. Now at 52, she wants people to know they can keep on top of their condition with treatment, self-care and the occasional treat.
‘I had the symptoms for years before I found out I had fibro. I knew I wasn’t right. I’d feel awful.
‘I’d get terribly low and I was in pain everywhere. But you just get on with things don’t you. I didn’t want to make an issue out of it. My daughter has JIA and Sjogren’s syndrome and she was so ill, I couldn’t think about how I was feeling.
‘When I eventually saw a rheumatologist, she just pressed my trigger points – I went through the roof. Tears were pouring down my face.
‘Knowing I had fibro made such a difference. When you can name it, you can start dealing with it.
‘I have to look after myself. I try to pace myself. I exercise with a personal trainer too, that makes all the difference.
‘Exercise is so important. But don’t just go and exercise, you need to see a physiotherapist or a gym instructor. Doing the wrong exercises can be as harmful as doing nothing. Make yourself keep walking, because when you stop it’s so difficult to get going again.
‘I have acupuncture, laser and heat treatments. They’re brilliant and really help. If I don’t go it takes weeks to get back on track.
They’re brilliant and really help. If I don’t go it takes weeks to get back on track.
‘I get as much sleep as I can. In the morning I’m still tired and my legs feel like lead, but I must get on and walk the dogs. Heat pads on my waist really help me walk. I always feel much better out in the fresh air.
‘I watch my diet, because once the weight goes on it doesn’t shift, that makes me feel worse.
‘If I’m going out, I try not to do too much the day before and after. Sometimes, I really don’t feel up to it, but my friends really understand.
‘I have down days, but I deal with it. It helps to stay positive. It would be very easy to get down.
‘I make sure I treat myself with a massage or a facial. It’s not indulgent, it helps. It’s so important to relax your body, mind and muscles and I know I’ll sleep well that night.
‘Little things really do make a difference. I still have days I don’t feel great, but I know I have to get on with things.’
Arthritis: Causes, Symptoms, Stages
Leading rheumatologists and orthopedists visit the IMMA network of medical clinics. Many years of experience in successfully diagnosing and treating arthritis, both in the early and late stages, allows us to quickly determine or exclude articular disease.
Many years of experience in successfully diagnosing and treating arthritis, both in the early and late stages, allows us to quickly determine or exclude articular disease.
According to WHO, arthritis is the most common disease of the musculoskeletal system worldwide. For every thousand people, there are 10 officially registered cases. Arthritis affects both young and old people equally. If only 20 years ago, leading rheumatologists confidently stated that the disease is most often diagnosed in women over 40, now the trend has changed. The boundaries of age and gender are gradually blurred. Arthritis develops rapidly in children and adolescents.
Classification of arthritis by types and causes
Arthritis is a collective definition of a broad group of pathologies affecting the joints and surrounding connective tissue. It can be either a separate disease (spondylitis) or a complication of other diseases (for example, rheumatism). It occurs in chronic, subacute and acute forms, with damage to one or more joints.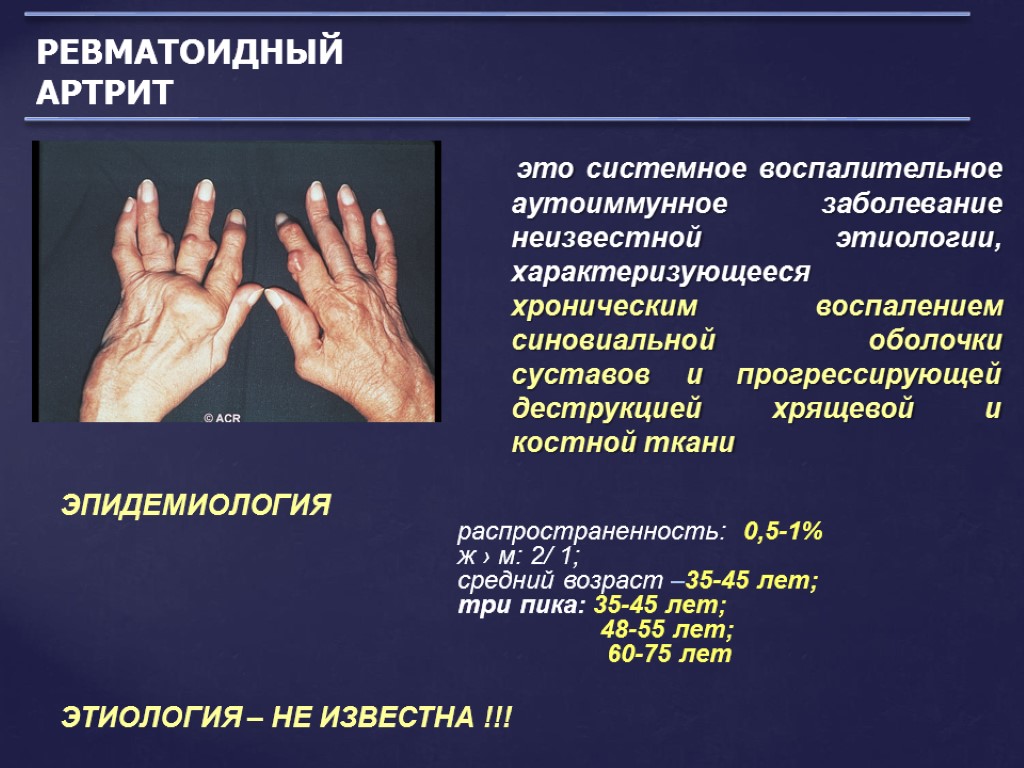
In MCD, arthritis is divided into several groups, depending on the etiology:
- inflammatory, developing as a result of pathological processes in the joint capsule – gout, rheumatoid, infectious, reactive.
- degenerative, against the background of cartilage tissue damage – osteoarthritis, traumatic arthrosis;
- primary, caused by specific infectious diseases such as tuberculosis, gonorrhea, chlamydia, etc.
- secondary, as complications of concomitant diseases of the central nervous system, cardiovascular system, gastrointestinal tract, oncological pathologies, etc.
Currently, it is not known exactly which factors play a decisive role in the development of arthritis. Medicine gives an exact definition only for some groups. All types of arthritis cause their own reasons for the development of pathology. Of the many, it is possible to single out the main ones that most often provoke pathological processes:
- Infectious, viral – all diseases that in their pathogenesis have complications on the joints.

- Traumatic – past (present) fractures, bruises, open wounds that affect the periarticular tissue.
- Hereditary – risks increase if close blood relatives have been diagnosed with arthritis.
- Immune – malnutrition, lack of vitamins and microelements, adverse environmental conditions disrupt the defense system, thereby activating degenerative processes.
- Allergic – the reaction of the body to irritants can be ambiguous and provoke the appearance of arthritis.
- External – reaching the age of 45, female sex, surgery, pregnancy, childbirth, multiple abortions, vaccinations are additional causes of the disease.
Important! The types and many factors of arthritis make every person vulnerable. Any infection or injury can be the beginning of negative processes. Age and gender characteristics in this case play a conditional role – the internal statistics of clinical institutions state that the disease is diagnosed in both adults and children in almost equal proportions.
Children’s arthritis
Every year the number of children diagnosed with arthritis is steadily increasing. In pediatrics, 7-16 cases are recorded for every hundred people. At the same time, girls are 3 times more sick than boys. The causes of rapid growth and arthritis in childhood are under investigation. Most rheumatologists agree on only one factor – immune disorders, during which the defense system begins abnormal activity against its own body.
Infections (influenza, acute respiratory viral infections, chicken pox, measles, etc.), which are severe and are accompanied by a prolonged fever, can lead to joint complications. After 2-3 weeks, after therapeutic measures, against the background of a weakened immune system, the following symptoms occur:
- fever;
- lethargy, drowsiness;
- conjunctivitis;
- swelling in the affected joints;
- frequent urge to urinate.
Important! The main thing is not to miss the primary signs of arthritis and consult a doctor in a timely manner. The signs of childhood arthritis are in many ways similar to infectious pathologies, so many people ignore the initial stages and self-medicate, which only aggravates the clinical picture of the disease.
The signs of childhood arthritis are in many ways similar to infectious pathologies, so many people ignore the initial stages and self-medicate, which only aggravates the clinical picture of the disease.
Symptoms depending on the stage
Arthritis progression has 4 degrees, each of which is characterized by its own symptoms and joint damage:
I stage. Rarely, some stiffness and discomfort may be felt. Usually diagnosed randomly. Ultrasound shows thickening and thickening of the periarticular soft tissues, inflammatory fluid in the joint (synovitis).
Stage II. Inflammation progresses, the joint shell becomes thinner, painful friction occurs between the head of the bone and the articular cavity. There is swelling, redness in the affected area and a local increase in temperature. On radiography – narrowing of the joint space, an increase in periarticular osteoporosis.
Stage III. The joint is significantly deformed, the motor function is limited, the muscles compensate for the impaired functionality, therefore they are in constant tone, which is the cause of frequent convulsions.
Stage IV. The destruction of the joint becomes irreversible. The heads of the bones grow together, defective bone formations are formed at the site of the lesion – contractures, ankylosis. The pains become excruciating, the patient is bedridden.
Arthritis is a chronic disease that currently has no universal treatment options. The disease will always be either in regression or in the process of exacerbation. Therefore, a person who has been diagnosed with arthritis will have to maintain a stable condition throughout his life. At the same time, it is extremely important not to miss the beginning of the exacerbation and take timely measures.
To make an appointment for a consultation and a preventive examination, you can contact the nearest IMMA medical center or use the contacts listed on the website.
Arthritis: Causes, Symptoms, Treatment | doc.ua
Arthritis, as a term in modern medicine, is a general designation used to define many varieties of inflammatory joint diseases. Arthritis of the joints is of two varieties: primary or secondary (caused by an underlying disease, for example, rheumatism). With a simultaneous disease of more than one joint, another term is used to define the disease – polyarthritis.
Arthritis of the joints is of two varieties: primary or secondary (caused by an underlying disease, for example, rheumatism). With a simultaneous disease of more than one joint, another term is used to define the disease – polyarthritis.
Types of arthritis
In its primary form, arthritis is represented by several types of joint diseases. The most common are osteoarthritis, rheumatoid and gouty types of the disease, somewhat less often – septic, juvenile, Still’s disease and spondylitis. In the secondary form, the most common forms of arthritis are purpura, systemic lupus erythematosus, hepatitis, hemochromatosis, psoriatic and reactive arthritis, as well as granulomatosis and borreliosis.
Causes
The main precondition for the secondary form of arthritis is the underlying disease. The cause contributing to the development of the primary form of the disease can be a variety of disorders in the body, for example, problems with the metabolism, nervous or immune systems, as well as infectious disorders and the consequences of injuries.
Infectious arthritis is caused by an autoimmune disease. Due to impaired immune function, an excess of immune complexes attacks the joints. Traumatic and vibration arthritis (for example, knee arthritis), as a rule, become a consequence of mechanical damage to the joints that occurs during injuries or heavy loads.
If the joint is already affected by a mild form of inflammatory arthritis, then its injury can provoke a complication or exacerbation of the disease. Occupational arthritis usually develops on the basis of regular microtraumatization associated with the patient’s profession or activity. For example, arthritis of the joints of the hands and fingers is common among massage therapists, cosmetologists, seamstresses and hairdressers, and people whose work is associated with constant physical exertion often develop arthritis of the spine.
High mechanical loads, traumas and genetic prerequisites provoke not only such local forms as arthritis of the knee joint, but can cause such a common form of the disease as osteoarthritis.
Among the causes contributing to the development of the disease are the presence of excess weight, congenital joint injuries, chronic inflammation and diseases of the nervous system. At a more detailed level of analysis, it can be emphasized that the majority of arthritis patients have various disorders associated with bone nutrition and vascular tone. The symmetry with which the lesion of the diseased joint develops in arthritis speaks of its neurotic nature.
Some types of infectious arthritis are allergic in nature. An example of this type of disease is tuberculosis, dysentery and gonorrhea, as well as nonspecific polyarthritis. Disruptions in the activity of the endocrine system in female menopause lead to the progress of rheumatoid arthritis.
Gout is usually formed on the basis of malnutrition, genetic factors and being overweight. The rheumatoid form of the disease develops on the basis of an autoimmune disorder of immunity, usually stimulated by infection, stress and overwork.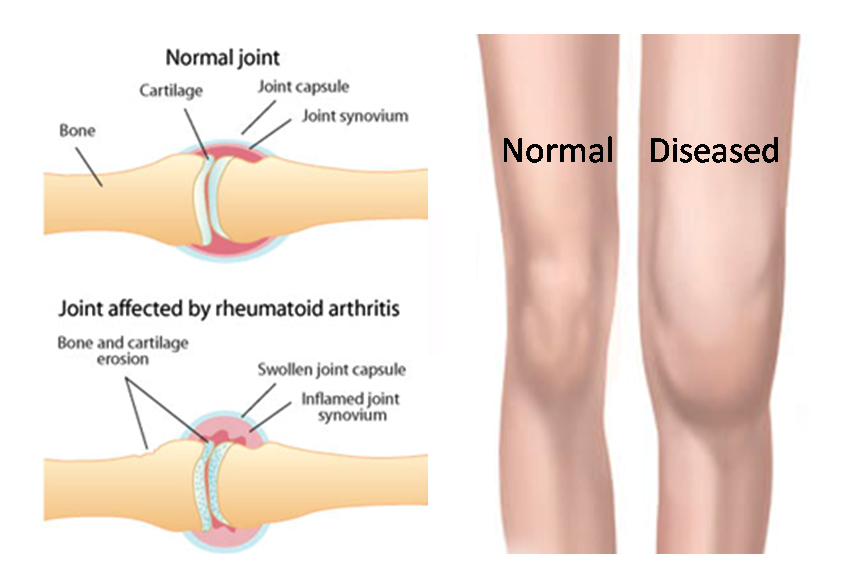
Symptoms
With the development of most types of arthritis, inflammation and swelling of the joint occurs, which visually increases in size and changes the color of the skin to purple-cyanotic. Arthritis is often characterized by significant pain, unnatural crunching, and decreased mobility of the joint, usually with deformity. Sometimes other signs appear, for example, reduced joint mobility in the morning and with relatively long immobility.
Arthritis, the symptoms of which are “sausage” swelling of the finger over the entire area and redness of the skin, can be rheumatoid, gouty or psoriatic. Another common symptom of the disease is “flying” inflammation of the joints, in which a suddenly swollen joint quickly returns to its former shape, but after it, the symptom is alternately observed in other joints. Rheumatoid arthritis, practically does not show symptoms, for example, reddening of the skin in the area of swelling, which complicates its treatment. With gout, redness is observed, but is accompanied by sharp pain.
One of the significant symptomatic definitions of arthritis from arthrosis can be considered a decrease (or disappearance) of pain after warming up the joint in arthritis, while in arthrosis the pain from movements will only increase. The combination of a prolonged increase in temperature to 37 degrees and above with a swelling of the joint may indicate the development of rheumatoid or reactive arthritis, and possibly ankylosing spondylitis. These same varieties of the disease are very likely with obvious prolonged inflammation of the eyes, regular “chills” or profuse sweating – during inflammation of the joints.
Complicated arthritis
Complicated arthritis is very dangerous, which makes timely detection of symptoms and competent therapy paramount, despite the difficulty of determining the exact type of disease. There are early stages of complicated arthritis and late stages.
Among the early stages of the complication, phlegmon can be distinguished, which is suppuration without a pronounced membrane, as well as panarthritis – an acute form of purulent arthritis, which is combined with inflammation of the ligamentous complex of the joint and suppuration of tissues close to the joint.
Complicated arthritis in the late stages is an extremely dangerous disease that can form irreversible processes and are difficult to treat. Among the late complicated forms, osteomyelitis, which affects areas of the bone close to the joint, and sepsis, which is blood poisoning, are common. Contracture is also common, leading to a stable limitation of joint mobility, up to the loss of its function, and pathological dislocation, in which the joint is separated (the head is forced out or falls out of the articular bag).
Arthritis in children
Children are inherently very mobile and frequently bump. Therefore, almost no one pays attention to the resulting pain in the joints. Moreover, the child does not understand what exactly hurts: the bruised place, or the bone itself. And it is quite common that the baby is simply afraid to go to the doctor, because he hides the pain. This is one of the main problems, since you can miss the moment of development of arthritis in children, and it will no longer be possible to stop it at an early stage. And this can be very fraught in the future and bring a lot of trouble for health.
And this can be very fraught in the future and bring a lot of trouble for health.
That is, if you see or hear that your child complains of pain in the elbows, knees, hands or fingers, then maybe you should think about what it is – children’s arthritis? This is especially true for families in which there are examples of this disease. Don’t forget, arthritis can be passed down genetically and can strike as early as infancy.
If you are unsure of your findings, it is still worth going to the doctor and doing basic blood tests and x-rays to determine the presence of the disease. Arthritis in children is very secretive and smooth, although the development of the disease occurs much faster than in adults or the elderly. Therefore, blood tests and x-rays will help decide whether it is really children’s arthritis, or just pain at the household level.
It happens that the moment with unpleasant, painful sensations in the joints is missed. Then you can observe reddening of the skin in those places where the joints are under the skin. Redness may be accompanied by swelling, and the area may be hotter than the rest of the body. It is possible that at this stage, your child may begin to chill and rise in temperature – this is how arthritis in children in the second stage manifests itself.
Redness may be accompanied by swelling, and the area may be hotter than the rest of the body. It is possible that at this stage, your child may begin to chill and rise in temperature – this is how arthritis in children in the second stage manifests itself.
It is an increase in temperature and swelling of the joints that is considered the main symptom, but then the treatment is much more complicated and the child suffers from constant pain. It is possible that there is a decrease in joint mobility, due to which your child will not be able to move normally, and also feel pain.
Children’s arthritis is dangerous in itself because it is difficult to recognize and even more difficult to treat. Even if arthritis has been found in your baby, many medications cannot be combined with his weak children’s body. Therefore, the treatment is chosen carefully by the doctor, who takes into account all the features of the child’s body.
Reactive arthritis
Reactive arthritis is a disease of the joints, the source of which is an infectious disease obtained by airborne, sexual, intestinal or other means. The reason is not the infection itself, but the body’s reaction to the disease, for example, diphtheria, we can say that this is a complication after improper treatment, which brings sad results.
The reason is not the infection itself, but the body’s reaction to the disease, for example, diphtheria, we can say that this is a complication after improper treatment, which brings sad results.
The symptoms of reactive arthritis are easily recognizable and identifiable in most cases. However, often treatment is delayed due to the strangeness of the onset of symptoms, for example, not every young person will go to a venereologist due to finger numbness or sudden pain in the tendon. The inflammatory process in reactive arthritis is characterized by swelling, fever, pain, redness. In fact, the infection has already managed to penetrate into the joint and infect nearby tissues, so you should not endure the disease – you need to urgently go to a specialist, otherwise the disease will spread throughout the musculoskeletal system and immobilize you.
Gouty arthritis
Gouty arthritis or gout is a joint disease associated with the deposition of uric acid salts. Most often, gout is the lot of elderly and older men, due to metabolic disorders and a malfunction in the functioning of male sex hormones.
In women, this disease can be observed quite rarely, however, recently, the consumption of fatty and salty foods among the beautiful half has increased dramatically, which led to an inevitable increase in relapses of gout, in addition, taking medications for pressure and hormonal drugs also provoked a significant activity of the disease in women. the female half of society.
Symptoms of gouty arthritis come on suddenly. You can feel a sharp pain in the finger or in a separate part of the leg, pain syndromes are accompanied by a sharp swelling of the inflamed area and redness to redness or crimson hue. It will be extremely difficult to touch a place that has suddenly disturbed you – the pain will remind you of itself immediately. However, the pain will soon subside, but do not think that it will be for a long time – an attack of gouty arthritis may recur the next night or after a few hours. The symptoms of gouty arthritis can be similar to some other diseases, such as arthrosis.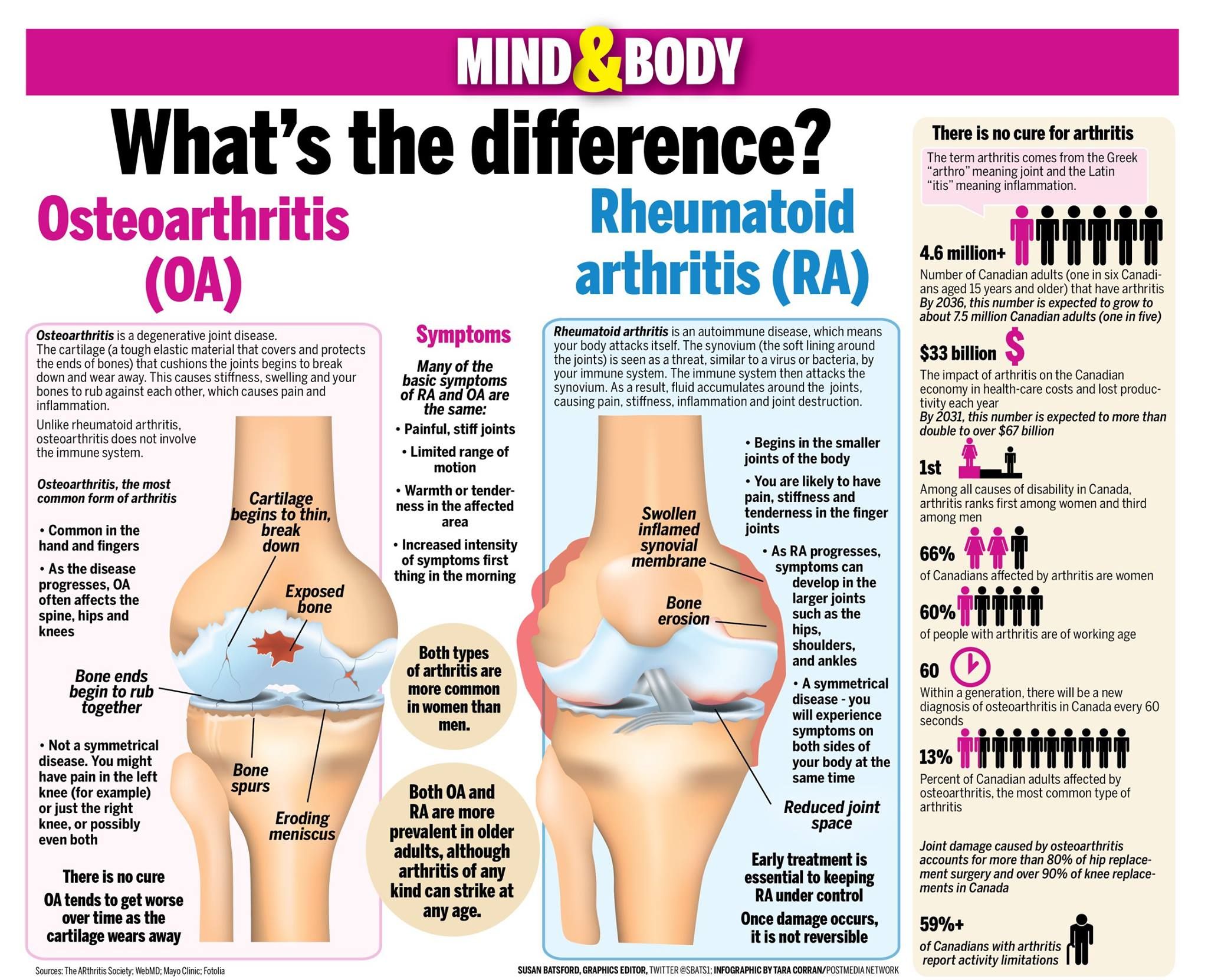 Only the extreme inflammation of the sore spot will tell an experienced specialist about the correct diagnosis. There is also pseudogout-pyelonephritis, where the course of the disease occurs in a similar way, and pyelonephric acid salts are similar to sodium urate. They can only be distinguished under a microscope, they will differ in the structure and refractive index of the crystals.
Only the extreme inflammation of the sore spot will tell an experienced specialist about the correct diagnosis. There is also pseudogout-pyelonephritis, where the course of the disease occurs in a similar way, and pyelonephric acid salts are similar to sodium urate. They can only be distinguished under a microscope, they will differ in the structure and refractive index of the crystals.
Rheumatoid arthritis
Rheumatoid arthritis is a disease (inflammation) of the joints caused by a malfunction of the immune system. As a rule, the process of rheumatoid arthritis begins with an infection in the human body. This manifestation of rheumatism is one of the most common and can have very serious consequences, up to the destruction of the joint, if the disease is neglected.
Quite often one can hear the opinion that such a problem as joint pain associated with rheumatoid arthritis is a problem for older people. But the reality looks a little different: in fact, many young people between the ages of 7 and 15 suffer from rheumatoid arthritis.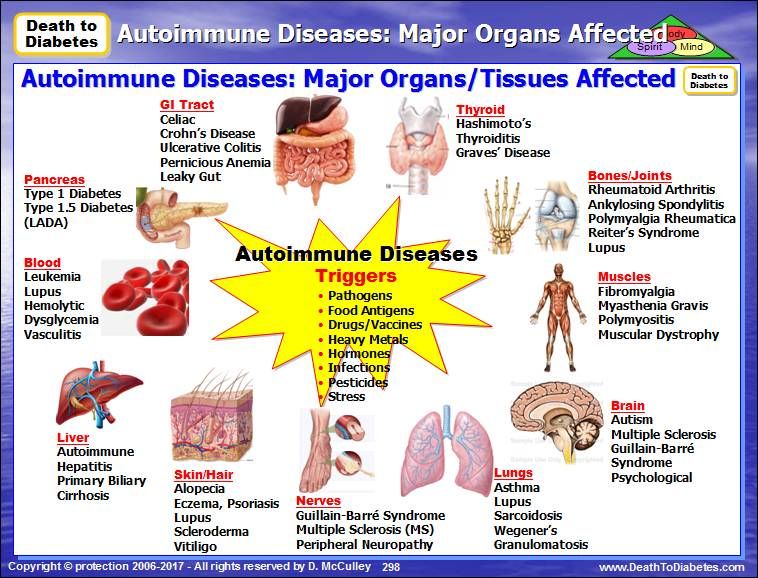
Young people are vulnerable to rheumatoid arthritis because it develops due to streptococcal infection, for which age factors do not matter.
Rheumatoid arthritis has a very unusual development process: those joints that were inflamed and deformed begin to recover over time, the inflammation goes away, and the deformity disappears. As a result, the patient again becomes able to walk normally.
But, despite the relief in the condition, the lesion (inflammation and deformity) passes to other joints of a person suffering from rheumatoid arthritis. Such wave-like symptoms are characteristic of rheumatoid arthritis.
It is worth noting the important fact that a dynamic change in the state of the joints is a clear sign of rheumatism developing in the body. This, in turn, can lead to damage to the visceral organs, in particular, the heart.
Also in this disease, endocarditis and carditis make themselves felt.
During progressive rheumatism, accompanied by dynamically shifting symptoms of arthritis, ESR increases in the blood, leukocytosis appears, the level of immunoglobulins, seromucoid and fibrinogen increases.
Diagnostics
Arthritis is diagnosed by determining the exact nature of the clinical picture, laboratory (tests) and instrumental examinations (X-ray, ultrasound, MRI and CT). A relatively young but effective diagnostic method is arthroscopy, which provides an opportunity for a detailed examination of the joint cavity and analysis of the synovial fluid. However, methods of laboratory or instrumental analysis that make it possible to accurately determine the type of arthritis do not exist today.
Treatment
For the treatment of secondary forms of the disease, first of all eliminate the root cause or, if possible, neutralize the provoking effect of the underlying disease. If extra-articular phenomena in arthritis are not observed, then drug therapy begins with the appointment of nonsteroidal drugs. Such agents include, for example, indomethacin, acetylsalicylic acid, diclofenac and brufen, and the treatment is long and can be carried out for years.
The most affected joints are treated with corticosteroids such as hydrocortisone or triamcinolone.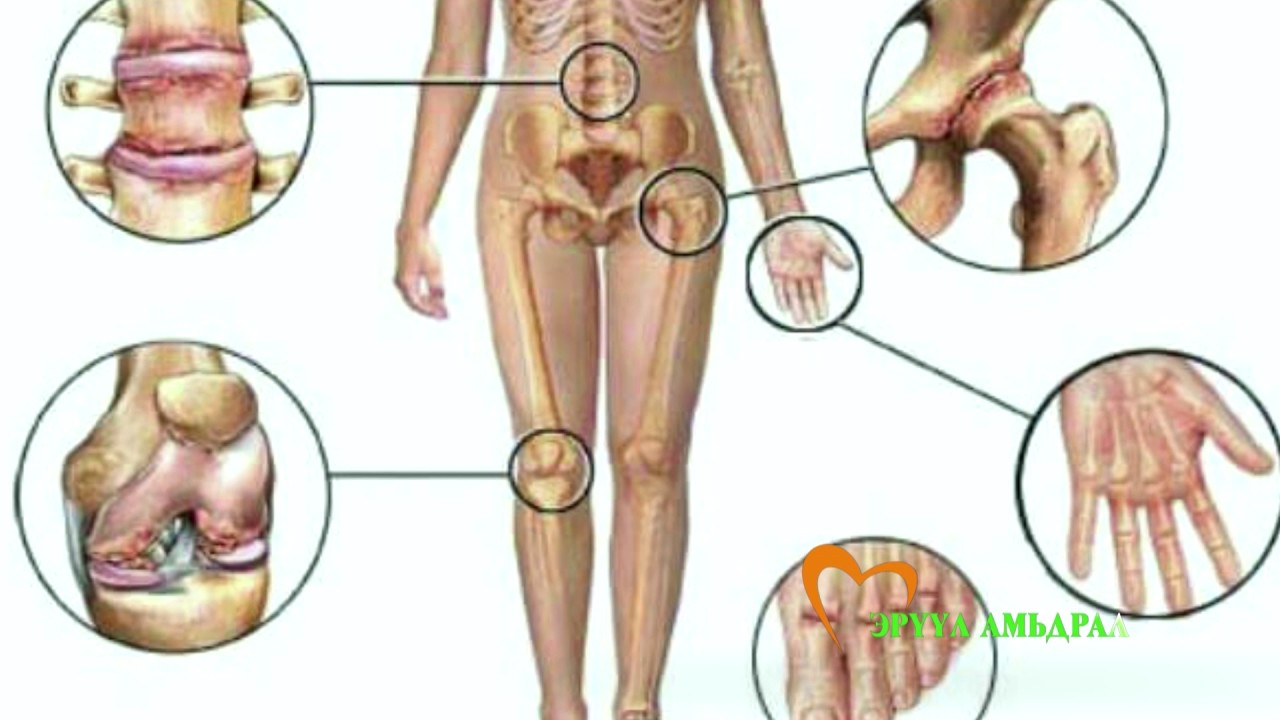 Corticosteroid hormonal preparations are prescribed with extreme caution and only in cases where acute pain is observed that cannot be eliminated by other anti-inflammatory drugs. If febrile phenomena accompanying reactive arthritis are observed, treatment is carried out with the obligatory use of corticosteroid therapy, but they seek to replace non-steroidal drugs as soon as possible.
Corticosteroid hormonal preparations are prescribed with extreme caution and only in cases where acute pain is observed that cannot be eliminated by other anti-inflammatory drugs. If febrile phenomena accompanying reactive arthritis are observed, treatment is carried out with the obligatory use of corticosteroid therapy, but they seek to replace non-steroidal drugs as soon as possible.
Arthritis, the treatment of which, with the use of the above drugs, does not stop the progress of the disease, should be treated with basic drugs, for example, aurotioprol (a preparation of gold, now rarely used), D-penicillamine, chloroquine, levamisole. Basic drug therapy lasts from six months to several years.
In case of arthritis in general, patients are indicated for complex therapy focused on general strengthening of the body and restoration of immunity (spa treatment). The treatment of arthritis is perfectly complemented by physiotherapeutic procedures (therapeutic exercises, massage), in particular, to restore the natural mobility of the articular complex.
How to treat children’s arthritis?
To start treatment, it is necessary to pass all examinations. This is necessary for the doctor to decide on the best way to cure arthritis in a child. During treatment, there may be relapses, so you need to constantly be under the supervision of doctors.
First of all, when the treatment has already begun, the immune parameters are brought back to normal. This is done to improve the protection of the child’s body from viruses and increase the ability to resist them. When the baby develops a strong antiviral barrier, there is hope that the disease will not return.
At the same time, pain must be removed. Since the pain in children’s arthritis is very severe, it is worth relieving this symptom so that the child can feel better. Then it will be easier for the body to fight the disease. Moreover, the pain is accompanied by swelling or swelling of the joints. This is why anti-inflammatory drugs are needed. But at the same time, they should not carry a heavy load on the heart and kidneys, since at such a young age the body cannot work extremely smoothly. Therefore, it is necessary to remove inflammation and anesthetize very carefully.
Therefore, it is necessary to remove inflammation and anesthetize very carefully.
In addition, treatment includes a direct attack on the problem that caused the disease to manifest itself. It is necessary to eliminate the main causative agent of arthritis in order to completely get rid of the disease.
The whole process is very long and labor intensive. In order for the treatment to progress faster, doctors quite often prescribe additional treatments. For example, this is physical therapy. A set of exercises performed by a child helps to strengthen the joints. Swimming can help in this case. If you have a swimming pool in your city, you just need to check with your doctor or trainer how best to visit it and what exercises are best to use in order to speed up the process of getting rid of childhood arthritis. Since the joints move softer during swimming, and the weight of the body decreases, the load also becomes less. Thus, recovery will be much faster.
Physiotherapy may also be included in the complex of treatment.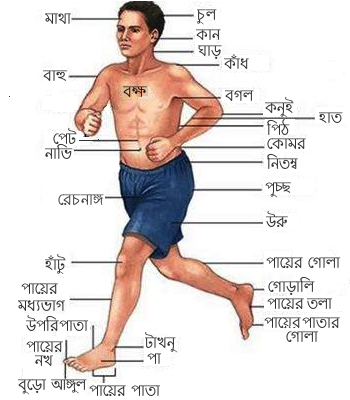 Warming up, stimulating the necessary areas – all this can improve the general condition of the joints, and you will get the desired recovery in the shortest possible time.
Warming up, stimulating the necessary areas – all this can improve the general condition of the joints, and you will get the desired recovery in the shortest possible time.
If the disease has receded, you should not relax. Continue to use vitamins, immune preparations and exercise. While the body and the musculoskeletal system in particular is growing, it is necessary to keep it in good shape in order to avoid relapses and protect the child from the manifestation of the disease in the future.
Diet for arthritis of the joints?
The most basic aspect of the diet is protein. You should be getting almost twice as much as healthy people. Protein will protect your body from the harmful side effects of medications. It will also strengthen bones and cartilage – this is necessary in order to quickly bring the joints back to normal. We can say that the diet for arthritis is based on food with a large capacity of proteins:
- eggs;
- milk;
- cottage cheese;
- oil;
- meat;
- fermented milk products.

All of this should be consumed in huge portions, literally made into main dishes.
Pay attention to the amount of fat you eat. It is desirable that the diet contains only vegetable fats in the form of olive and sunflower oil. After all, it’s like with a faulty mechanism – it needs lubrication. So your joints need it too. Therefore, when choosing a diet for arthritis of the joints, carefully consider the amount of animal fats. Their overabundance can “clog” both your body and blood vessels. In principle, butter is allowed in small quantities, but here you also need to know the measure.
The main things you will need to fill your diet with are fruits, berries and vegetables. They are filled with almost the entire spectrum of known vitamins, so they will keep your body in good shape and help you recover faster. You should distribute your arthritis diet so that fresh, plant-based foods dominate your daily meals.
Treatment of arthritis with folk remedies
Internal treatments
- You will need lemon and celery, about 0.
 5 kg each. Turn them in a meat grinder, then add 500 grams of honey. Stir the mixture thoroughly and infuse in the refrigerator for 4-5 days. Take one tablespoon of the mixture three times a day 15 minutes before meals. After the prepared mixture is over, you should take a two-week break, and then repeat the course.
5 kg each. Turn them in a meat grinder, then add 500 grams of honey. Stir the mixture thoroughly and infuse in the refrigerator for 4-5 days. Take one tablespoon of the mixture three times a day 15 minutes before meals. After the prepared mixture is over, you should take a two-week break, and then repeat the course. - Boil the potatoes in their skins, then mash them thoroughly in the same water in which they were boiled. Let it settle well. Starch will remain at the bottom, but you need to drain the settled broth, it should be taken three times a day for 1/3 cup.
- It is recommended to drink a glass of carrot juice every day for a long time.
- Pour a tablespoon of chopped dry St. John’s wort with a glass of boiling water, insist for half an hour. It should be consumed in a tablespoon 3-4 times a day.
- A decoction of bay leaves is very effective for joint pain, it should be drunk two to three glasses three times a day.
- Pour two tablespoons of dry chopped thistle into 0.
 5 liters of water and boil for 10 minutes, then strain. Take one teaspoon 2-3 times a day.
5 liters of water and boil for 10 minutes, then strain. Take one teaspoon 2-3 times a day. - Ordinary garlic can also relieve joint pain. Peel and finely chop 5 heads of garlic, pour 0.5 vodka and insist in the dark for ten days. You should drink a teaspoon of tincture before each meal. In the event that the tincture turned out to be too strong for you, you can dilute the dose with three tablespoons of boiled water. You should be careful with this recipe if you have an ulcer, gastritis or other stomach problems.
- Grind three heads of garlic on a grater, add the juice squeezed from ten lemons and a teaspoon of chopped horseradish. Infuse the mixture in a warm and dark place for three weeks. In the morning and evening, you need to drink a glass of water, to which a teaspoon of the mixture is added, take until the tincture is over.
- Add a teaspoon of apple cider vinegar to a glass of water and drink before meals. In the event that you have stomach problems, the amount of vinegar must be halved.
 The course lasts for 2-4 weeks.
The course lasts for 2-4 weeks. - You can also dilute apple cider vinegar with water and add honey – two teaspoons of honey and two teaspoons of apple cider vinegar to a glass of water. Take two teaspoons three times a day half an hour before meals. The course lasts a month, then – 20 days break and repetition. This procedure should be carried out three times a year.
External treatments
- Pour 100 grams of propolis with 100 grams of vegetable oil. Heat for half an hour in a water bath, stirring constantly, until the propolis is completely dissolved in the oil. Cool the resulting ointment and rub it into the affected joint.
- Dry the pits of the cherries thoroughly and grind them into a powder. Mix with water or vegetable oil to a mushy state and use to rub the joints.
- Mix chicken yolk, a teaspoon of apple cider vinegar and a teaspoon of turpentine thoroughly and apply to sore joints daily at bedtime.
- It is necessary to mix 200 grams of salt and 100 grams of dry mustard.
 Mix with kerosene to the consistency of thick sour cream and rub so that the ointment is completely absorbed, while the skin remains dry.
Mix with kerosene to the consistency of thick sour cream and rub so that the ointment is completely absorbed, while the skin remains dry. - You will need radish, turnip and horseradish, only 100 grams each, grind into gruel, mix thoroughly and rub the joints with this mixture, make a compress from it. The course lasts a week, the mixture must be prepared immediately before use.
- It helps with joint pain by applying fresh horseradish leaves to it.
- Mix 100 grams of vodka and turpentine, add 3 tablespoons of vegetable oil. In this mixture, you need to moisten the gauze, wring it out and wrap the affected joint with it, wrap it over it with polyethylene or cling film and a woolen scarf. Leave the compress all night, the duration of the course is a week.
It is also recommended to systematically take short baths with Epsom salts – you need a cup of salt for the bath, you need to lie in it for about half an hour. You can boil two kilograms of fresh bran in water for 10 minutes, pour the broth into the bath and add sea salt for a greater effect.
Every person suffering from constant debilitating joint pain should know how to treat arthritis with folk remedies.
It is important to remember that a positive result can only be achieved if you have patience and fully follow all the recommendations. The key to success is a combination of two important points: complexity and consistency. If the prescription indicates that the course of treatment lasts twenty days, it means that it is necessary to take a tincture or make a compress during such a time, no more and no less. Do not forget to consult with your doctor, then traditional medicine combined with herbal medicine will give tangible results. Even with prolonged remission, it is necessary to repeat the treatment in the off-season and in case of a cold. Keep in mind that folk remedies, like any medicine, have their own contraindications and side effects that you cannot predict on your own, because it all depends on your individual characteristics. In various reference books on herbal medicine, you can easily find information about the contraindications of a particular plant that is part of the therapeutic mixture.




 It also means you’re fully aware of treatment and self-management approaches that can help you.
It also means you’re fully aware of treatment and self-management approaches that can help you.

 Using mathematical modelling, this work could help to match people up with the best treatment option for them.
Using mathematical modelling, this work could help to match people up with the best treatment option for them.

 5 kg each. Turn them in a meat grinder, then add 500 grams of honey. Stir the mixture thoroughly and infuse in the refrigerator for 4-5 days. Take one tablespoon of the mixture three times a day 15 minutes before meals. After the prepared mixture is over, you should take a two-week break, and then repeat the course.
5 kg each. Turn them in a meat grinder, then add 500 grams of honey. Stir the mixture thoroughly and infuse in the refrigerator for 4-5 days. Take one tablespoon of the mixture three times a day 15 minutes before meals. After the prepared mixture is over, you should take a two-week break, and then repeat the course. 5 liters of water and boil for 10 minutes, then strain. Take one teaspoon 2-3 times a day.
5 liters of water and boil for 10 minutes, then strain. Take one teaspoon 2-3 times a day. The course lasts for 2-4 weeks.
The course lasts for 2-4 weeks. Mix with kerosene to the consistency of thick sour cream and rub so that the ointment is completely absorbed, while the skin remains dry.
Mix with kerosene to the consistency of thick sour cream and rub so that the ointment is completely absorbed, while the skin remains dry.