Asthma worse in morning. Nocturnal Asthma: Causes, Symptoms, and Effective Treatment Strategies
Why does asthma worsen at night. How can nocturnal asthma disrupt sleep patterns. What are the primary triggers for nighttime asthma attacks. Which treatment options are most effective for managing nocturnal asthma symptoms. How does body position affect asthma during sleep. Can lifestyle changes help alleviate nighttime asthma symptoms. What role do hormones play in exacerbating nocturnal asthma.
Understanding Nocturnal Asthma: A Comprehensive Overview
Nocturnal asthma, also known as nighttime asthma, is a condition characterized by the worsening of asthma symptoms during sleep. This phenomenon can significantly impact an individual’s quality of life, leading to sleep disturbances, daytime fatigue, and increased difficulty in managing overall asthma symptoms. Despite its prevalence, nocturnal asthma is often underestimated by healthcare professionals, making it crucial for patients to understand its causes, symptoms, and available treatment options.

Key Symptoms of Nocturnal Asthma
- Chest tightness
- Shortness of breath
- Persistent coughing
- Wheezing
These symptoms typically intensify during the night, making it challenging for individuals to achieve restful sleep. The severity of nocturnal asthma should not be underestimated, as studies have shown that a significant number of asthma-related deaths occur during nighttime hours.
The Science Behind Nocturnal Asthma Exacerbation
While the exact mechanisms underlying the worsening of asthma symptoms at night are not fully understood, several factors have been identified as potential contributors. These include increased exposure to allergens, cooling of the airways, the effects of a reclining position, and hormonal fluctuations that follow a circadian pattern.
Circadian Rhythm and Asthma
Research suggests that asthma symptoms tend to worsen approximately four to six hours after falling asleep, regardless of when the sleep period occurs. This pattern indicates the presence of an internal trigger related to the body’s natural circadian rhythm. For instance, individuals working night shifts may experience asthma attacks during their daytime sleep, further supporting the role of internal biological processes in nocturnal asthma.

Environmental and Physiological Triggers of Nighttime Asthma
Several environmental and physiological factors can contribute to the exacerbation of asthma symptoms during sleep. Understanding these triggers is essential for developing effective management strategies.
Increased Mucus Production and Sinusitis
During sleep, airways tend to narrow, potentially leading to increased airflow resistance. This narrowing can trigger coughing, which in turn may cause further tightening of the airways. Additionally, increased drainage from the sinuses can trigger asthma symptoms in individuals with highly sensitive airways. The co-occurrence of sinusitis and asthma is relatively common and can significantly impact nighttime breathing.
The Impact of Sleeping Position
Lying in a reclining position can predispose individuals to nighttime asthma problems. This may be due to several factors, including:
- Accumulation of secretions in the airways
- Increased blood volume in the lungs
- Decreased lung volumes
- Increased airway resistance
These physiological changes associated with the reclining position can create an environment conducive to asthma symptom exacerbation.

The Role of Environmental Factors in Nocturnal Asthma
Environmental conditions in the bedroom can significantly influence the severity of nighttime asthma symptoms. Two key factors to consider are air temperature and allergen exposure.
Air Conditioning and Airway Cooling
Breathing colder air at night or sleeping in an air-conditioned room can lead to heat loss from the airways. This cooling effect, along with moisture loss, is known to be an important trigger for exercise-induced asthma and is also implicated in nocturnal asthma. The temperature and humidity levels in the sleeping environment should be carefully managed to minimize their impact on asthma symptoms.
Allergen Exposure and Late Phase Response
Exposure to allergens or asthma triggers in the evening can lead to a phenomenon known as the late phase response. This reaction occurs in approximately 50% of individuals who experience an immediate allergic reaction and is characterized by:
- Increased airway responsiveness
- Development of bronchial inflammation
- A more prolonged period of airway obstruction
Studies have shown that allergen exposure in the evening, as opposed to the morning, is more likely to result in a late phase response of greater severity. This highlights the importance of minimizing allergen exposure in the bedroom and during evening hours.

Gastroesophageal Reflux Disease (GERD) and Its Impact on Nocturnal Asthma
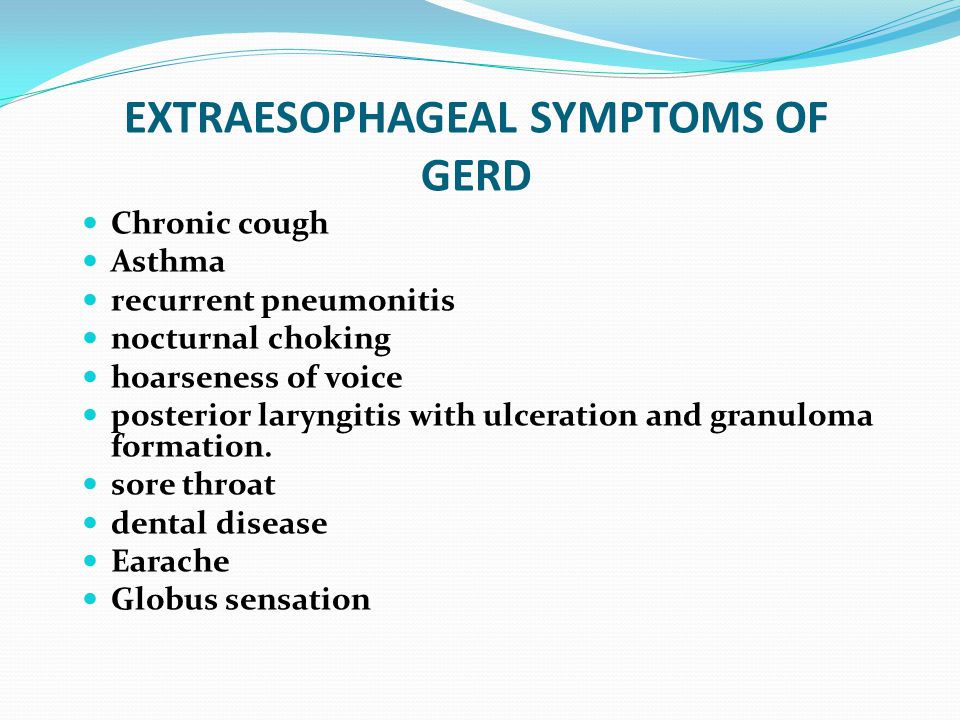
Gastroesophageal reflux disease (GERD) is a common condition that can significantly exacerbate nighttime asthma symptoms. The reflux of stomach acid through the esophagus to the larynx can stimulate bronchial spasms, leading to increased asthma symptoms. This problem is often worse when lying down or when taking certain asthma medications that may relax the valve between the stomach and esophagus.
Mechanisms of GERD-Induced Asthma Exacerbation
GERD can contribute to nocturnal asthma through several mechanisms:
- Irritation of the lower esophagus, leading to constriction of the airways
- Aspiration of stomach acid into the trachea, airways, and lungs
- Triggering of severe reactions involving airway irritation, increased mucus production, and airway tightening
Proper management of both GERD and asthma with appropriate medications can often alleviate nighttime asthma symptoms, underscoring the importance of addressing these conditions concurrently.
The Hormonal Influence on Nocturnal Asthma
Hormones that circulate in the blood follow well-characterized circadian rhythms, which can significantly impact asthma symptoms. One such hormone is epinephrine, which plays a crucial role in maintaining bronchial function.
Epinephrine and Histamine Balance
Epinephrine helps keep the muscles in the walls of bronchi relaxed, ensuring that airways remain wide. It also suppresses the release of substances like histamines, which can cause mucus secretion and bronchospasm. However, epinephrine levels and peak expiratory flow rates are typically lowest at around 4:00 a.m., coinciding with peak histamine levels. This hormonal imbalance may predispose individuals to nocturnal asthma during sleep.
Effective Treatment Strategies for Nocturnal Asthma
While there is no cure for nighttime asthma, various treatment options can effectively manage symptoms and improve quality of life for affected individuals.
Pharmacological Interventions
Daily asthma medications, particularly inhaled steroids, have proven highly effective in reducing inflammation and preventing nocturnal symptoms. These medications work by addressing the underlying inflammatory processes that contribute to asthma exacerbation.
Lifestyle Modifications
In addition to medical treatments, several lifestyle changes can help manage nocturnal asthma:
- Elevating the head of the bed to reduce GERD symptoms
- Using hypoallergenic bedding to minimize allergen exposure
- Maintaining a consistent sleep schedule to support natural circadian rhythms
- Avoiding known asthma triggers in the bedroom environment
By implementing these strategies in conjunction with appropriate medical interventions, individuals with nocturnal asthma can significantly improve their symptoms and overall quality of life.
The Importance of Proper Diagnosis and Monitoring
Accurate diagnosis and ongoing monitoring are crucial for effective management of nocturnal asthma. Healthcare providers may recommend the use of peak flow meters to track lung function throughout the day and night, helping to identify patterns and guide treatment decisions.
Personalized Treatment Plans
Given the complex nature of nocturnal asthma and its various triggers, treatment plans should be tailored to each individual’s specific needs and circumstances. Regular follow-ups with healthcare providers can ensure that treatment remains effective and can be adjusted as needed to address changing symptoms or environmental factors.

In conclusion, nocturnal asthma presents unique challenges for affected individuals, but with proper understanding, management, and treatment, its impact on daily life can be significantly reduced. By addressing both the physiological and environmental factors that contribute to nighttime asthma symptoms, patients can work towards achieving better sleep, improved daytime functioning, and overall enhanced quality of life. As research in this field continues to evolve, new insights and treatment options may emerge, offering hope for even more effective management strategies in the future.
Nocturnal Asthma (Nighttime Asthma) Prevention & Treatment
Nocturnal asthma, with symptoms like chest tightness, shortness of breath, cough, and wheezing at night, can make sleep impossible and leave you feeling tired and irritable during the day. These problems may affect your overall quality of life and make it more difficult to control your daytime asthma symptoms.
Nocturnal or nighttime asthma is very serious. It needs a proper asthma diagnosis and effective asthma treatment.
Nighttime Asthma and Sleep Disturbance
The chances of experiencing asthma symptoms are higher during sleep. Nocturnal wheezing, cough, and trouble breathing are common yet potentially dangerous. Many doctors often underestimate nocturnal asthma or nighttime asthma.
Studies show that most deaths related to asthma symptoms such as wheezing happen at night.
Nocturnal Asthma Causes
The exact reason that asthma is worse during sleep are not known, but there are explanations that include increased exposure to allergens; cooling of the airways; being in a reclining position; and hormone secretions that follow a circadian pattern. Sleep itself may even cause changes in bronchial function.
Sleep itself may even cause changes in bronchial function.
Increased Mucus or Sinusitis
During sleep, the airways tend to narrow, which may cause increased airflow resistance. This may trigger nighttime coughing, which can cause more tightening of the airways. Increased drainage from your sinuses can also trigger asthma in highly sensitive airways. Sinusitis with asthma is quite common.
Internal Triggers
Asthma problems may occur during sleep, despite when the sleep period is taking place. People with asthma who work on the night shift may have breathing attacks during the day when they are sleeping. Most research suggests that breathing tests are worse about four to six hours after you fall asleep. This suggests there may be some internal trigger for sleep-related asthma.
Reclining Position
Lying in a reclining position may also predispose you to nighttime asthma problems. Many factors may cause this, such as accumulation of secretions in the airways (drainage from sinuses or postnasal drip), increased blood volume in the lungs, decreased lung volumes, and increased airway resistance.
Air Conditioning
Breathing colder air at night or sleeping in an air‑conditioned bedroom may also cause loss of heat from the airways. Airway cooling and moisture loss are important triggers of exercise‑induced asthma. They are also implicated in nighttime asthma.
GERD
If you are frequently bothered with heartburn, the reflux of stomach acid up through the esophagus to the larynx may stimulate a bronchial spasm. It’s worse when lying down or if you take medications for asthma that relax the valve between the stomach and esophagus. Sometimes, acid from the stomach will irritate the lower esophagus and lead to constriction of your airways. If stomach acid backs up to your throat, it may drip down to the trachea, airways and lungs, leading to a severe reaction. This can involve airway irritation, increased mucus production, and airway tightening. Taking care of GERD and asthma with appropriate medications can often stop nighttime asthma.
Late Phase Response
If you are exposed to an allergen or asthma trigger, the chances are great that airway obstruction or allergic asthma will occur shortly afterward. This acute asthma attack ends within one hour. About 50% of those who experience an immediate reaction also have a second phase of airway obstruction within three to eight hours of exposure to the allergen. This phase is called the late phase response, and it is characterized by an increase in airway responsiveness, development of bronchial inflammation, and a more prolonged period of airway obstruction.
This acute asthma attack ends within one hour. About 50% of those who experience an immediate reaction also have a second phase of airway obstruction within three to eight hours of exposure to the allergen. This phase is called the late phase response, and it is characterized by an increase in airway responsiveness, development of bronchial inflammation, and a more prolonged period of airway obstruction.
Many studies report that when allergen exposure occurs in the evening instead of in the morning, you are more susceptible to having a late phase response and are more likely to have one of greater severity.
Hormones
Hormones that circulate in the blood have well‑characterized circadian rhythms that are seen in everybody. Epinephrine is one such hormone, which exerts important influences on the bronchial tubes. This hormone helps keep the muscle in the walls of bronchi relaxed so the airway remains wide. Epinephrine also suppresses the release of other substances, such as histamines, which cause mucus secretion and bronchospasm. Your epinephrine levels and peak expiratory flow rates are lowest at about 4:00 a.m., while histamine levels tend to peak at this same time. This decrease in epinephrine levels may predispose you to nocturnal asthma during sleep.
Your epinephrine levels and peak expiratory flow rates are lowest at about 4:00 a.m., while histamine levels tend to peak at this same time. This decrease in epinephrine levels may predispose you to nocturnal asthma during sleep.
How Is Nocturnal Asthma Treated?
There is no cure for nighttime asthma, but daily asthma medications, such as inhaled steroids, are very effective at reducing inflammation and preventing nocturnal symptoms. Since nocturnal asthma or nighttime asthma may occur anytime during the sleep period, asthma treatment must be sufficient to cover these hours. A long-acting bronchodilator delivered in an asthma inhaler can be effective in preventing bronchospasm and symptoms of asthma. If you suffer from nocturnal asthma, you may also benefit from a long-acting inhaled corticosteroid. If you suffer with GERD and asthma, ask your doctor about medication that reduces acid production in the stomach. Avoidance of potential allergy triggers such as dust mites, animal dander, or feathers in a down comforter may also be very helpful in preventing allergies and asthma and nocturnal asthma attacks./GettyImages-101930209-5a53da6cbeba33003758be9f.jpg)
In addition, using your peak flow meter, you can monitor how your lung function is altered throughout the day and night. Once you notice this altered pattern of lung function, talk with your doctor about a plan to resolve your nighttime asthma symptoms. According to your type of asthma and asthma severity (mild, moderate, or severe), your doctor can prescribe treatment to help you resolve your nighttime asthma symptoms so you can sleep like a baby.
Physiological patterns in early morning asthma.
Thorax. 1977 Aug; 32(4): 418–423.
This article has been cited by other articles in PMC.
Abstract
Sixteen asthmatic patients who regularly showed early morning falls in peak expiratory flow rate of more than 25% were studied at 06.00 hours and 14.00 hours. At 06.00 hours considerable deterioration in static lung volumes and airways resistance occurred which was typical of an attack of acute asthma. Blood gas analysis showed less variation, with mild hypoxia and a wide alveolar-arterial oxygen tension gradient throughout the study. Diurnal variation was also seen in the response of maximal mid expiratory flow rates to the inhalation of helium/oxygen mixture in seven patients, but another seven were consistently non-responders. The overall pattern of results suggests that the calibre of both large and small airways decreased at night but improvement was more complete in large airways during the day. Despite these findings patients had few symptoms at 06.00 hours when most of them showed marked reversibility after inhaling aerosol salbutamol. This phenomenon might account for the sudden nature of some asthma deaths as these often occur in the early morning. If this is the case, the minority of patients whose early morning decline in lung function was not immediately reversible would appear to be at greatest risk.
Diurnal variation was also seen in the response of maximal mid expiratory flow rates to the inhalation of helium/oxygen mixture in seven patients, but another seven were consistently non-responders. The overall pattern of results suggests that the calibre of both large and small airways decreased at night but improvement was more complete in large airways during the day. Despite these findings patients had few symptoms at 06.00 hours when most of them showed marked reversibility after inhaling aerosol salbutamol. This phenomenon might account for the sudden nature of some asthma deaths as these often occur in the early morning. If this is the case, the minority of patients whose early morning decline in lung function was not immediately reversible would appear to be at greatest risk.
Full text
Full text is available as a scanned copy of the original print version. Get a printable copy (PDF file) of the complete article (905K), or click on a page image below to browse page by page. Links to PubMed are also available for Selected References.
Links to PubMed are also available for Selected References.
Images in this article
Click on the image to see a larger version.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bass H. The flow volume loop: normal standards and abnormalities in chronic obstructive pulmonary disease. Chest. 1973 Feb;63(2):171–176. [PubMed] [Google Scholar]
- Benatar SR, Clark TJ, Cochrane GM. Clinical relevance of the flow rate response to low density gas breathing in asthmatics. Am Rev Respir Dis. 1975 Feb;111(2):126–134. [PubMed] [Google Scholar]
- Bouhuys A, Van de Woestijne KP. Respiratory mechanics and dust exposure in byssinosis. J Clin Invest. 1970 Jan;49(1):106–118. [PMC free article] [PubMed] [Google Scholar]
- Chan-Yeung M, Abboud R, Tsao MS, Maclean L. Effect of helium on maximal expiratory flow in patients with asthma before and during induced bronchoconstriction.
 Am Rev Respir Dis. 1976 Apr;113(4):433–443. [PubMed] [Google Scholar]
Am Rev Respir Dis. 1976 Apr;113(4):433–443. [PubMed] [Google Scholar] - Cochrane GM, Clark JH. A survey of asthma mortality in patients between ages 35 and 64 in the Greater London hospitals in 1971. Thorax. 1975 Jun;30(3):300–305. [PMC free article] [PubMed] [Google Scholar]
- Despas PJ, Leroux M, Macklem PT. Site of airway obstruction in asthma as determined by measuring maximal expiratory flow breathing air and a helium-oxygen mixture. J Clin Invest. 1972 Dec;51(12):3235–3243. [PMC free article] [PubMed] [Google Scholar]
- DUBOIS AB, BOTELHO SY, BEDELL GN, MARSHALL R, COMROE JH., Jr A rapid plethysmographic method for measuring thoracic gas volume: a comparison with a nitrogen washout method for measuring functional residual capacity in normal subjects. J Clin Invest. 1956 Mar;35(3):322–326. [PMC free article] [PubMed] [Google Scholar]
- Hutcheon M, Griffin P, Levison H, Zamel N. Volume of isoflow. A new test in detection of mild abnormalities of lung mechanics.
 Am Rev Respir Dis. 1974 Oct;110(4):458–465. [PubMed] [Google Scholar]
Am Rev Respir Dis. 1974 Oct;110(4):458–465. [PubMed] [Google Scholar] - Hyatt RE, Black LF. The flow-volume curve. A current perspective. Am Rev Respir Dis. 1973 Feb;107(2):191–199. [PubMed] [Google Scholar]
- HYATT RE, SCHILDER DP, FRY DL. Relationship between maximum expiratory flow and degree of lung inflation. J Appl Physiol. 1958 Nov;13(3):331–336. [PubMed] [Google Scholar]
- Ingram RH, Jr, Schilder DP. Effect of thoracic gas compression on the flow-volume curve of the forced vital capacity. Am Rev Respir Dis. 1966 Jul;94(1):56–63. [PubMed] [Google Scholar]
- McDermott M. Diurnal and weekly cyclical changes in lung airways resistance. J Physiol. 1966 Oct;186(2):90P–92P. [PubMed] [Google Scholar]
- Macdonald JB, Seaton A, Williams DA. Asthma deaths in Cardiff 1963-74: 90 deaths outside hospital. Br Med J. 1976 Jun 19;1(6024):1493–1495. [PMC free article] [PubMed] [Google Scholar]
- McFadden ER, Jr, Linden DA. A reduction in maximum mid-expiratory flow rate.
 A spirographic manifestation of small airway disease. Am J Med. 1972 Jun;52(6):725–737. [PubMed] [Google Scholar]
A spirographic manifestation of small airway disease. Am J Med. 1972 Jun;52(6):725–737. [PubMed] [Google Scholar] - Mead J, Turner JM, Macklem PT, Little JB. Significance of the relationship between lung recoil and maximum expiratory flow. J Appl Physiol. 1967 Jan;22(1):95–108. [PubMed] [Google Scholar]
- BLAKEMORE WS, FORSTER RE, MORTON JW, OGILVIE CM. A standardized breath holding technique for the clinical measurement of the diffusing capacity of the lung for carbon monoxide. J Clin Invest. 1957 Jan;36(1 Pt 1):1–17. [PMC free article] [PubMed] [Google Scholar]
- Peress L, Sybrecht G, Macklem PT. The mechanism of increase in total lung capacity during acute asthma. Am J Med. 1976 Aug;61(2):165–169. [PubMed] [Google Scholar]
- Rees HA, Millar JS, Donald KW. A study of the clinical course and arterial blood gas tensions of patients in status asthmaticus. Q J Med. 1968 Oct;37(148):541–561. [PubMed] [Google Scholar]
- Reinberg A, Gervais P. Circadian rhythms in respiratory functions, with special reference to human chronophysiology and chronopharmacology.
 Bull Physiopathol Respir (Nancy) 1972 May-Jun;8(3):663–677. [PubMed] [Google Scholar]
Bull Physiopathol Respir (Nancy) 1972 May-Jun;8(3):663–677. [PubMed] [Google Scholar] - Soutar CA, Costello J, Ijaduola O, Turner-Warwick M. Nocturnal and morning asthma. Relationship to plasma corticosteroids and response to cortisol infusion. Thorax. 1975 Aug;30(4):436–440. [PMC free article] [PubMed] [Google Scholar]
- Woolcock AJ, Read J. Lung volumes in exacerbations of asthma. Am J Med. 1966 Aug;41(2):259–273. [PubMed] [Google Scholar]
Articles from Thorax are provided here courtesy of BMJ Publishing Group
Facts, Causes, Symptoms, Triggers, and FAQs
Nocturnal Asthma Facts
- A type of asthma that gets worse at night is called nocturnal asthma.
- Environmental allergens, stress, hormonal factors, obesity, sinusitis, and more contribute to the worsening of asthma at night.
- People with nocturnal asthma develop symptoms such as wheezing, chest tightness, breathing difficulty, and coughing.

- Nocturnal asthma symptoms are common regardless of which type of asthma you have – including allergic and non-allergic asthma, exercise-induced asthma, or occupational asthma.
- The average sleep quality score for nocturnal asthma patients are lower. For children, it gets as low as 51.
- In Orange County alone, 15.9% of asthma cases were reported in 2015-2017.
What is Nocturnal Asthma?
Asthma is a long-term, chronic respiratory disease, caused by the inflammation of the airways. When this condition worsens overnight, we call it nocturnal asthma or nighttime asthma. Regardless of the type of asthma you have, including allergic, non-allergic, occupational, and exercise-induced asthma, nocturnal asthma can occur more than once a month.
Over the past decade, the prevalence of asthma in adults and children has increased in the United States. The California Health Interview Survey states that 15. 9% of asthma cases were reported in Orange County in 2015-2017. Although there is no cure for asthma, the symptoms (whether worse during daytime or nighttime) can be managed through long-term medications and short-term quick-relief inhalers. A few home remedies and other tips (we”ll look into those later in this blog) can also help patients with nocturnal asthma sleep better.
9% of asthma cases were reported in Orange County in 2015-2017. Although there is no cure for asthma, the symptoms (whether worse during daytime or nighttime) can be managed through long-term medications and short-term quick-relief inhalers. A few home remedies and other tips (we”ll look into those later in this blog) can also help patients with nocturnal asthma sleep better.
What Factors Contribute to Night Time Asthma Attack?
The factors that contribute to nocturnal asthma include:
- Environmental allergens
- Cold air
- Hormonal factors
- Stress
- GERD (Gastroesophageal Reflux Disease)
- The supine sleeping position
- Obstructive sleep apnea
- Sinusitis
- Obesity
- Increased mucus production
What Are the Symptoms of Nocturnal Asthma?
The symptoms of nocturnal asthma and regular asthma are the same, but a few may get worse at night, which include:
- Shortness of breath
- Wheezing
- Chest tightness
- Coughing
In addition, people and especially children may develop other sleep issues, including:
- Excessive daytime sleepiness
- Sleep-maintenance insomnia
- Sleep-disordered breathing like sleep apnea
- Parasomnias like sleepwalking
What to Do During an Asthma Attack Without an Inhaler at Night?
Follow these tips to survive a night-time asthma attack without an inhaler:
- Sit straight to keep your airways open
- Stay calm, as stress or panic can worsen your symptoms
- Take long, deep breaths to reduce symptoms
- Asthma can be triggered by dust, cigarette smoke, and other allergens.
 Stay away from triggers and go to any area with clean air.
Stay away from triggers and go to any area with clean air. - A cup of coffee can open up your airways and provide you some relief
- Seek emergency medical attention if symptoms persist
Tips to Sleep Better with Severe Asthma At Night
Nocturnal asthma is associated with poor sleep quality. This condition of sleeplessness and its effects are worse for children. The average total sleep quality score of children affected by asthma is 51, which is above the clinical cut off of 41, but it indicates the pervasive sleep disturbances among this population.
Here are a few tips that can help you sleep better with asthma at night:
-
Keep Your Bedroom Clean
Pet dander, dust mites, and other indoor allergens can trigger or worsen asthma symptoms. Clean your bedroom regularly to improve the indoor air quality and keep these factors out.
Related Blog: 4 Ways How Poor Air Quality Can Negatively Affect Your Health
-
Wash Your Bed Covers and Blankets
Wash your bedding in hot water every week.
 The water should be at least 130 degrees Fahrenheit so that it can kill dust mites and other allergens in your bedding.
The water should be at least 130 degrees Fahrenheit so that it can kill dust mites and other allergens in your bedding. -
Use Dust-Proof Pillow Covers and Mattress
Zippered pillow covers are tightly woven to keep allergens and dust mites out of your bed covers. Dust and allergens are more common during summertime you keep your windows open that allows the dust to enter your room. Learn more about 14 ways to prevent summertime asthma attacks
-
Use Humidifier
Cold air can trigger or worsen asthma symptoms at night. During winter, you can use a humidifier to increase your bedroom’s air quality. Dust mites usually develop in low humidity. By increasing humidity, you can keep the dust mites out of your room.
-
Avoid Sleeping with Pets
Pet dander can trigger asthma symptoms, so don’t sleep with pets. Make sure to close your bedroom door to keep your pet and their dander out.

-
Consider Your Sleeping Position
If you have acid reflux, cold or sinus infection, lying flat can trigger an asthma attack. You can sleep keeping your head propped slightly up with a pillow to avoid a night-time asthma attack.
-
Undergo Sleep Apnea Test
People with asthma may experience sleep apnea, which are frequent pauses in breathing during sleep. Sleep apnea can worsen asthma symptoms. Undergo a test to diagnose sleep apnea and take treatments if required.
Nocturnal Asthma FAQs
Can You Die in Your Sleep From Severe Asthma?
Asthma causes sleep disturbances and usually wakes up people from sleep, so it is unusual to die because of asthma during sleeping, unless heavily sedated for some other reason. However, asthma can be fatal if you are not seeking proper medical attention to treat worsening symptoms.
Does Steam or Vaporizer Reduce Chances of an Asthma Attack at Night?
Generally, steam or vaporizer can liquefy mucus when breathing problems are caused by an allergy or cold. This can help a person feel better. On the other hand, asthma is caused by chronic inflammation of the airways, making it difficult to breathe. Steam or vaporizer can cause irritations and worsen breathing problems.
This can help a person feel better. On the other hand, asthma is caused by chronic inflammation of the airways, making it difficult to breathe. Steam or vaporizer can cause irritations and worsen breathing problems.
Does Melatonin Improve Sleep in Asthma?
Researchers have revealed that the hormone melatonin plays a vital role in improving the sleep cycle in asthma patients. Melatonin helps in regulating human circadian rhythms and is believed to have sleep-inducing activity. Additionally, melatonin studies suggest that it affects smooth muscle tone and inflammation too. Both of which helps in improving the sleep cycle for asthma patients at night.
Does Honey Treatment Help in Improving Sleep with Asthma?
Coughing is one of the symptoms of nocturnal asthma, which can be reduced by taking two teaspoons of honey with warm water or cinnamon before you go to bed. Honey can increase saliva production, which can ease your cough by lubricating your airways and reduce inflammation in the bronchial tubes that causes breathing difficulty.
Does a CPAP Help in Asthma Attack at Night?
If there is an issue of carbon dioxide retention during an asthma attack, your doctor is more likely to recommend a BiPAP (Bilevel Positive Airway Pressure), as opposed to a CPAP (Continuous Positive Air Pressure). However, many patients with mild asthma have reported of using a CPAP machine without any problems.
Visit your doctor as soon as you suspect that you have asthma or asthma-like symptoms. Seeking immediate medical attention from an urgent care near you can also help you control an asthma attack and manage the symptoms. Visit our Woodbridge Walk-In Urgent Care in Irvine, Fountain Valley Urgent Care, or Costa Mesa Urgent Care to get seen.
Also Read: Signs of Acute Bronchitis and How to Heal It
Family Care Centers Medical Group
Family Care Centers Medical Group has provided quality primary care and
urgent care services to the residents of Orange County since 1982.
Our team of experienced and dedicated healthcare professionals is committed to providing
exceptional medical care in a caring and compassionate environment. At our urgent care centers at
Irvine,
Fountain Valley, and
Costa Mesa,
we offer immediate attention to minor medical emergencies, including cuts, bruises, scrapes, sprains, strains, broken bones, sore throats,
flu, and workplace injuries. Our primary care doctors at Irvine,
Fountain Valley, and Costa Mesa centers are ready to take care of all your primary healthcare needs,
like the flu shot, physical examination, and treatment for acute or chronic illnesses.
Nocturnal Asthma: Here’s Why Your Asthma Gets Worse at Night
Having your sleep interrupted is annoying at best and, especially if it happens often, meltdown-inducing at worst. But when you wake up in the middle of a coughing fit or because you feel like you’re breathing through a straw, the whole experience can take a terrifying turn.
But when you wake up in the middle of a coughing fit or because you feel like you’re breathing through a straw, the whole experience can take a terrifying turn.
Unfortunately, that’s what some people with asthma have to deal with. “It is very common for asthma to get worse at night,” pulmonologist Ryan Thomas, M.D., director of the Multidisciplinary Severe Asthma Team at Michigan State University, tells SELF. This phenomenon, which experts sometimes refer to as nocturnal asthma, can make it far too difficult to get the amount of rest you need. It can also be a sign that you need to take steps to subdue your asthma before it gets even worse.
It’s important to cover some asthma basics before we dive into the rude awakening portion.
Your airways, which extend between your nose and mouth and your lungs, carry air in and out of your body, according to the National Heart, Lung, and Blood Institute (NHLBI). Pretty key job, huh? But if you have asthma, those airways can get all puffy and inflamed when you’re exposed to triggers like animal dander (particles of skin and saliva that they’ve shed), pollen, mold, cold air, cigarette smoke, exercise, and respiratory infections like the flu, the NHLBI says. That swelling can then cause the muscles around your airways to tighten, and your airways may also expel more mucus than they usually do. The end result is the opposite of breathing easy: You might experience asthma symptoms like wheezing (a whistling sound when you breathe), coughing, shortness of breath, and chest pain or tightness.
That swelling can then cause the muscles around your airways to tighten, and your airways may also expel more mucus than they usually do. The end result is the opposite of breathing easy: You might experience asthma symptoms like wheezing (a whistling sound when you breathe), coughing, shortness of breath, and chest pain or tightness.
It’s possible that your asthmatic reaction to a trigger will be mild and go away on its own, but if your symptoms get worse and don’t respond to treatment, you can have what’s known as an asthma attack or asthma exacerbation, which can be life-threatening.
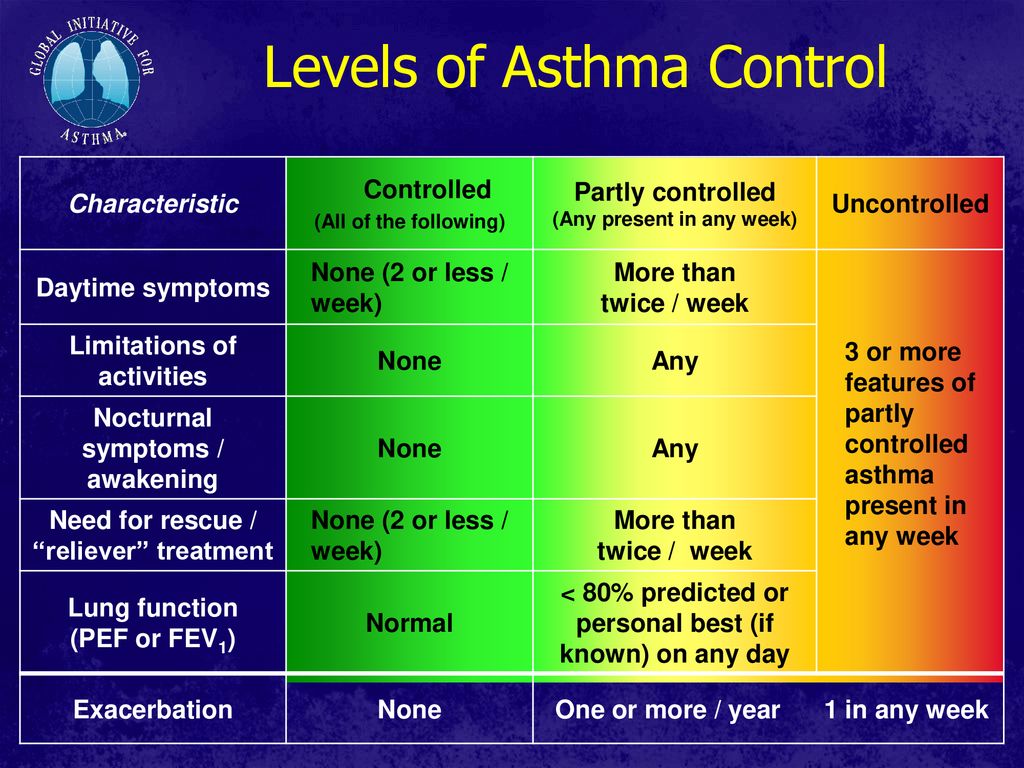
Depending on its severity, your asthma can fall into one of four categories. Some of this classification hinges on how your asthma acts at night.
Mild intermittent asthma means you have minor symptoms up to two days a week and up to two nights a month, according to the Mayo Clinic. Mild persistent asthma takes it up a notch, so you have symptoms more than twice a week but not more frequently than once in a day. Moderate persistent asthma involves symptoms at least once a day, along with more than one night a week. Finally, severe persistent asthma means you’re having signs of asthma throughout the day on most days, along with frequently at night.
Moderate persistent asthma involves symptoms at least once a day, along with more than one night a week. Finally, severe persistent asthma means you’re having signs of asthma throughout the day on most days, along with frequently at night.
No matter your asthma classification, you might notice that when you experience symptoms, they’re more likely to strike at night, or that they seem to be worse after the sun has set than they are during the daytime. There are a few reasons this may happen.
Doctors aren’t 100 percent sure why asthma can flare up at night, but there are some theories, including how prevalent triggers may be in your bedroom, hormonal fluctuations, and more.
Certain asthma triggers are more likely to pop up where you sleep. For instance, dust mites, which are microscopic creatures that feed on your old skin cells, are a common asthma trigger, according to the Mayo Clinic. If these gross little dudes incite your asthma, spending hours in your bed as you sleep raises the risk that you’ll have symptoms, Timothy McGee, D. O., a pulmonologist at Northwestern Medicine Central DuPage Hospital, tells SELF. That’s because dust mites adore living in areas like your bed, as that’s the exact type of warm, humid environment in which they thrive. Plus, there’s a ton of food for them there. (Remember, that food is your old skin cells.)
O., a pulmonologist at Northwestern Medicine Central DuPage Hospital, tells SELF. That’s because dust mites adore living in areas like your bed, as that’s the exact type of warm, humid environment in which they thrive. Plus, there’s a ton of food for them there. (Remember, that food is your old skin cells.)
Why Does Asthma Get Worse at Night?
In 1698, British doctor John Floyer wrote a treatise on asthma, the first major work focused on the disease. Not all of it aged well. He warned that those who were sad or angry were more likely to experience attacks, as sadness would stop the “Motion of Humors.” He also recommended a few cures including regular, gentle vomiting.
In an asthma attack, the air passageways in a person’s lungs start to close, making it hard for them to breathe and causing tightness in the chest, coughing, and wheezing. But Floyer’s piece also noted another important symptom: His own asthma was almost always more severe at night, sometimes waking him up at 1 or 2 in the morning.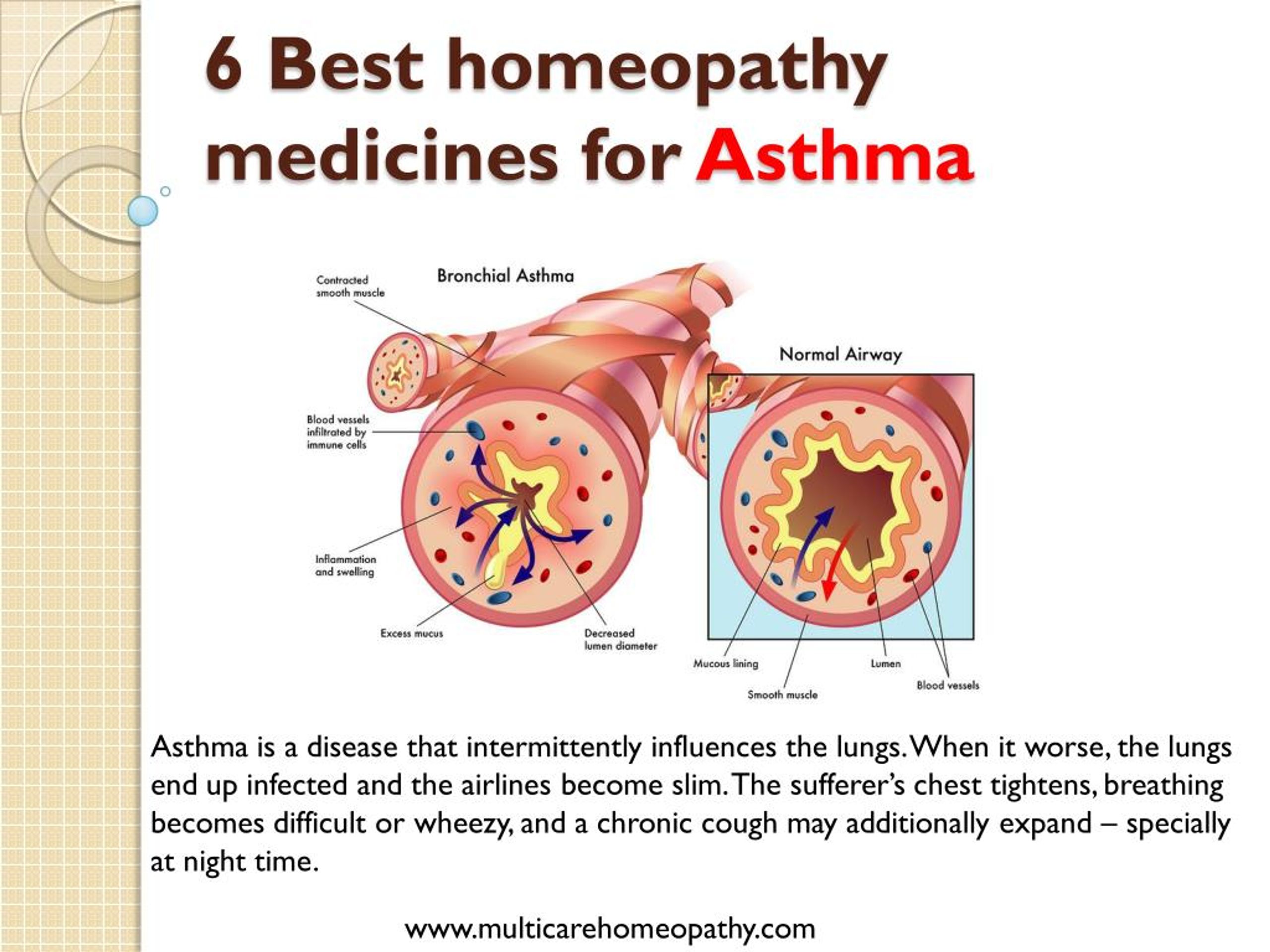 Hundreds of years later, scientists were finding evidence that backed him up: A study from 2005 showed that nearly 75 percent of people with asthma experience worse attacks at night. A famous mortality survey of London hospitals in the 1970s showed that early morning and nighttime attacks were more likely to be fatal.
Hundreds of years later, scientists were finding evidence that backed him up: A study from 2005 showed that nearly 75 percent of people with asthma experience worse attacks at night. A famous mortality survey of London hospitals in the 1970s showed that early morning and nighttime attacks were more likely to be fatal.
Yet no one is sure why asthma gets worse at night, says Steven Shea, director of the Oregon Institute of Occupational Health Sciences at Oregon Health and Science University. “Most people sleep at night, so maybe it’s the sleep that causes your asthma to get worse at night,” he says. Or it may be caused by body position or mites or allergens in the bedding. Or, Shea adds, “maybe it’s the internal body clock.”
That body clock is also called the circadian system. Among other important functions, it regulates hormones, heartbeat, and the immune system over a cycle that lasts about 24 hours. While this system is internal, it’s heavily influenced by outside factors like light and dark, mealtimes, and work schedules.
Historically, it’s been impossible to isolate the role of the circadian system from people’s behavior and environmental risks “because they go hand in hand,” says Frank Scheer, director of the Medical Chronobiology Program at Brigham and Women’s Hospital. “You cannot know what is actually driving changes in pulmonary function.” But in a paper published this month in Proceedings of the National Academy of Sciences, a team led by Scheer and Shea finally found a way to divorce the circadian system from all the external factors that might contribute to asthma.
First, they had their 17 study participants, all of whom had previously been diagnosed with asthma, track their pulmonary function at home during their daily lives. Four times a day, the participants used a handheld spirometer to test how much air they could push out of their lungs in one second, a measurement called FEV1. (The more, the better.) They also recorded their symptoms and noted when they had to use their rescue inhalers.
Then, things got significantly more involved. The same set of participants were put through two different experiments while living in dimly lit rooms at the Center for Critical Inquiry at Brigham and Women’s Hospital. In one experiment, called the “constant routine protocol,” participants sat in bed for 38 hours without being allowed to sleep. They couldn’t get up to use the bathroom or do any strenuous activities. Every two hours, they ate the same snack, a small peanut butter and jelly or tuna fish sandwich. They were allowed to listen to books on tape, chat with the nurses, or play card games, but they couldn’t move around or get excited or angry.
Asthma symptoms & treatments – Illnesses & conditions
Reliever inhalers
Reliever inhalers – usually blue – are taken to relieve asthma symptoms quickly.
The inhaler usually contains a medicine called a short-acting beta2-agonist, which works by relaxing the muscles surrounding the narrowed airways. This allows the airways to open wider, making it easier to breathe again.
Reliever inhalers do not reduce the inflammation in the airways, so they do not make asthma better in the long term – they are intended only for the relief of symptoms.
Examples of reliever medicines include salbutamol and terbutaline. They are generally safe medicines with few side effects, unless overused.
However, they should rarely, if ever, be necessary if asthma is well controlled, and anyone needing to use them three or more times a week should have their treatment reviewed.
Everyone with asthma should be given a reliever inhaler, also known simply as a ‘reliever’.
Read further information:
Preventer inhalers
Preventer inhalers – usually brown, red or orange – work over time to reduce the amount of inflammation and sensitivity of the airways, and reduce the chances of asthma attacks occurring.
They must be used regularly (typically twice or occasionally once daily) and indefinitely to keep asthma under control.
You will need to use the preventer inhaler daily for some time before you gain the full benefit./a-young-man-is-using-an-asthma-inhaler-924327182-5aff16fe119fa8003717596c.jpg) You may still occasionally need the blue reliever inhaler to relieve your symptoms, but your treatment should be reviewed if you continue to need them often.
You may still occasionally need the blue reliever inhaler to relieve your symptoms, but your treatment should be reviewed if you continue to need them often.
The preventer inhaler usually contains a medicine called an inhaled corticosteroid. Examples of preventer medicines include beclometasone, budesonide, fluticasone, ciclesonide and mometasone.
Preventer treatment should be taken regularly if you have anything more than occasional symptoms from your asthma, and certainly if you feel the need to use a reliever inhaler more than twice a week.
Some inhaled corticosteroids can occasionally cause a mild fungal infection (oral thrush) in the mouth and throat, so make sure you rinse your mouth thoroughly after inhaling a dose. The use of a spacer device also reduces this risk.
Smoking can reduce the effects of preventer inhalers.
Read further information:
Other treatments and ‘add-on’ therapy
Long-acting reliever inhalers
If your asthma does not respond to initial treatment, the dose of preventer inhaler you take may be increased in agreement with your healthcare team.
If this does not control your asthma symptoms, you may be given an inhaler containing a medicine called a long-acting reliever (long-acting bronchodilator/long-acting beta2-agonist, or LABA) to take as well.
These work in the same way as short-acting relievers. Although they take slightly longer to work, their effects can last for up to 12 hours. This means that taking them regularly twice a day provides 24-hour cover.
Regular use of long-acting relievers can also help reduce the dosage of preventer medication needed to control asthma. Examples of long-acting relievers include formoterol and salmeterol, and recently vilanterol, which may last up to 24 hours.
However, like short-acting relievers, long-acting relievers do not reduce the inflammation in the airways. If they are taken without a preventer, this may allow the condition to get worse while masking the symptoms, increasing the chance of a sudden and potentially life-threatening severe asthma attack.
You should therefore always use a long-acting reliever inhaler in combination with a preventer inhaler, and never by itself.
In view of this, most long-acting relievers are prescribed in a ‘combination’ inhaler, which contains both an inhaled steroid (as a preventer) and a long-acting bronchodilator in the one device.
Examples of combination inhalers include Seretide, Symbicort, Fostair, Flutiform and Relvar. These are usually (but not always) purple, red and white, or maroon.
Other preventer medicines
If regular efficient administration of treatment with a preventer and a long-acting reliever still fails to control asthma symptoms, additional medicines may be tried. Two possible alternatives include:
- leukotriene receptor antagonists – tablets that block part of the chemical reaction involved in the swelling (inflammation) of the airways
- theophyllines – tablets that help widen the airways by relaxing the muscles around them, and are also relatively weak anti-inflammatory agents
Oral steroids
If your asthma is still not under control, you may be prescribed regular steroid tablets. This treatment is usually monitored by a respiratory specialist (an asthma specialist).
This treatment is usually monitored by a respiratory specialist (an asthma specialist).
Oral steroids are powerful anti-inflammatory preventers, which are generally used in two ways:
- to regain control of asthma when it is temporarily upset – for example, by a lapse in regular medication or an unexpected chest infection; in these cases, they are typically given for one or two weeks, then stopped
- when long-term control of asthma remains a problem, despite maximal dosages of inhaled and other medications – in these cases, oral steroids may be given for prolonged periods, or even indefinitely, while maintaining maximum treatment with inhalers as this maximises the chance of being able to stop the oral steroids again in the future
Long-term use of oral steroids has serious possible side effects, so they are only used once other treatment options have been tried, and after discussing the risks and benefits with your healthcare team.
Omalizumab (Xolair)
Omalizumab, also known as Xolair, is the first of a new category of medication that binds to one of the proteins involved in the immune response and reduces its level in the blood. This lowers the chance of an immune reaction happening and causing an asthma attack.
This lowers the chance of an immune reaction happening and causing an asthma attack.
It is licensed for use in adults and children over six years of age with asthma.
The National Institute for Heath and Care Excellence (NICE) recommends that omalizumab can be used in people with allergy-related asthma who need continuous or frequent treatment with oral corticosteroids.
Omalizumab is given as an injection every two to four weeks. It should only be prescribed in a specialist centre. If omalizumab does not control asthma symptoms within 16 weeks, the treatment should be stopped.
Read further information:
Bronchial thermoplasty
Bronchial thermoplasty is a relatively new procedure that can be used in some cases of severe asthma. It works by destroying some of the muscles surrounding the airways in the lungs, which can reduce their ability to narrow the airways.
The procedure is carried out either with sedation or under general anaesthetic. A bronchoscope (a long, flexible tube) containing a probe is inserted into the lungs through the mouth or nose so it touches the airways.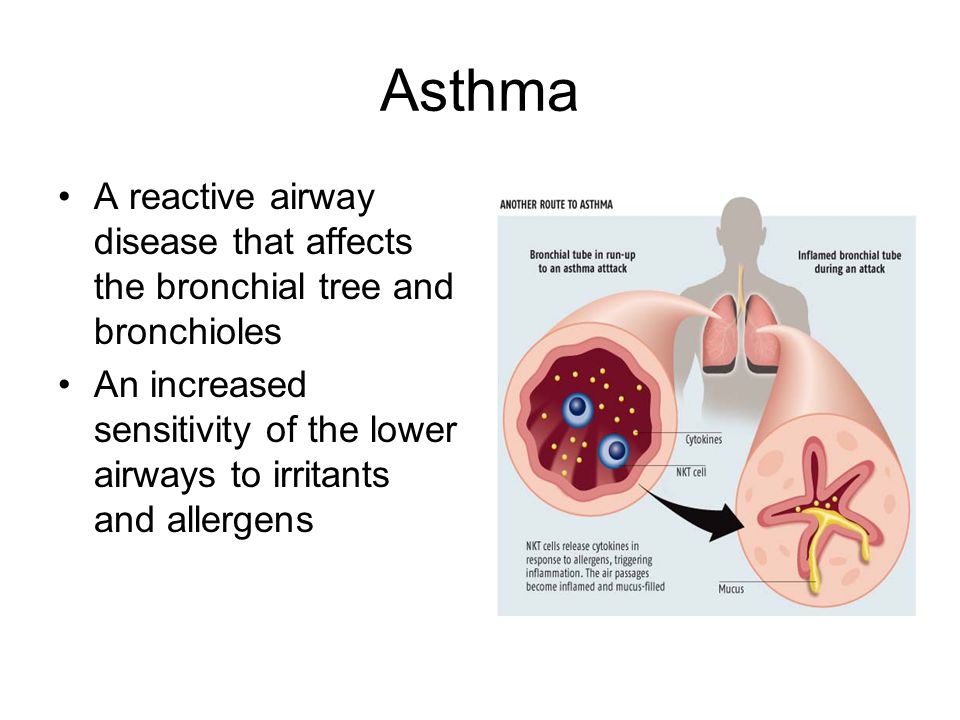
The probe then uses controlled heat to damage the muscles around the airways. Three treatment sessions are usually needed, with at least three weeks between each session.
There is some evidence to show this procedure may reduce asthma attacks and improve the quality of life of someone with severe asthma.
However, the long-term risks and benefits are not yet fully understood. There is a small risk it will trigger an asthma attack, which sometimes requires hospital admission.
You should discuss this procedure fully with your clinician if the treatment is offered.
Read further information:
Side effects of treatments
Side effects of relievers and preventers
Relievers are a safe and effective medicine, and have few side effects as long as they are not used too much. The main side effects include a mild shaking of the hands (tremors), headaches and muscle cramps. These usually only happen with high doses of reliever inhaler and usually only last for a few minutes.
Preventers are very safe at usual doses, although they can cause a range of side effects at high doses, especially with long-term use.
The main side effect of preventer inhalers is a fungal infection of the mouth or throat (oral candidiasis). You may also develop a hoarse voice and sore throat.
Using a spacer can help prevent these side effects, as can rinsing your mouth or cleaning your teeth after using your preventer inhaler.
Your doctor or nurse will discuss with you the need to balance control of your asthma with the risk of side effects, and how to keep side effects to a minimum.
Side effects of add-on therapy
Long-acting relievers may cause similar side effects to short-acting relievers. You should be monitored at the beginning of your treatment and reviewed regularly. If you find there is no benefit to using the long-acting reliever, it should be stopped.
Theophylline tablets have been known to cause side effects in some people, including nausea, vomiting, tremors and noticeable heartbeats (palpitations).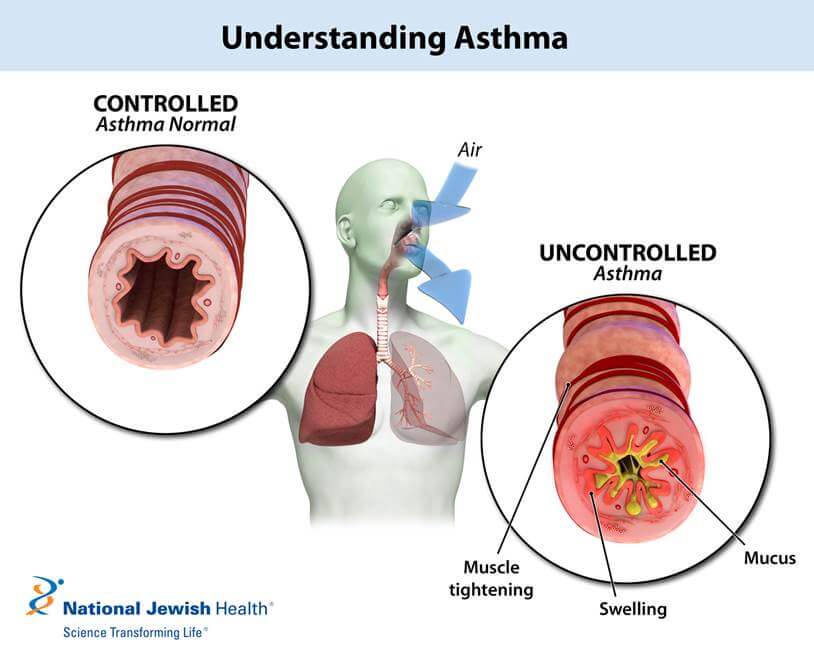 These can usually be avoided by adjusting the dose according to periodic measurement of the theophylline concentration in the blood.
These can usually be avoided by adjusting the dose according to periodic measurement of the theophylline concentration in the blood.
Side effects of leukotriene receptor agonists can include tummy (abdominal) pain and headaches.
Side effects of steroid tablets
Oral steroids carry a risk if they are taken for more than three months or if they are taken frequently (more than three or four courses of steroids a year). Side effects can include:
With the exception of increased appetite, which is very commonly experienced by people taking oral steroids, most of these unwanted effects are uncommon.
However, it is a good idea to keep an eye out for them regularly, especially side effects that are not immediately obvious, such as high blood pressure, thinning of the bones, diabetes and glaucoma.
You will need regular appointments to check for these.
Read further information:
Asthma attacks
A personal asthma action plan will help you recognise the initial symptoms of an asthma attack, know how to respond, and when to seek medical attention.
In most cases, the following actions will be recommended:
- Take one to two puffs of your reliever inhaler (usually blue) immediately.
- Sit down and try to take slow, steady breaths.
- If you do not start to feel better, take two puffs of your reliever inhaler (one puff at a time) every two minutes (you can take up to 10 puffs) – this is easier using a spacer, if you have one.
- If you do not feel better after taking your inhaler as above or if you are worried at any time, phone 999.
- If an ambulance does not arrive within 10 minutes and you are still feeling unwell, repeat step three.
If your symptoms improve and you do not need to phone 999, you still need to see a doctor or asthma nurse within 24 hours.
If you are admitted to hospital, you will be given a combination of oxygen, reliever and preventer medicines to bring your asthma under control.
Your personal asthma action plan will need to be reviewed after an asthma attack, so reasons for the attack can be identified and avoided in future.
Read further information:
Personal asthma action plan
As part of your initial assessment, you should be encouraged to draw up a personal asthma action plan with your GP or asthma nurse.
If you’ve been admitted to hospital because of an asthma attack, you should be offered an action plan (or the opportunity to review an existing action plan) before you go home.
The action plan should include information about your asthma medicines, and will help you recognise when your symptoms are getting worse and what steps to take. You should also be given information about what to do if you have an asthma attack.
Your personal asthma action plan should be reviewed with your GP or asthma nurse at least once a year, or more frequently if your symptoms are severe.
As part of your asthma plan, you may be given a peak flow meter. This will give you another way of monitoring your asthma, rather than relying only on symptoms, so you can recognise deterioration earlier and take appropriate steps.
Read further information:
What is good asthma care?
Your doctor or nurse will tailor your asthma treatment to your symptoms. Sometimes you may need to be on higher levels of medication than at others.
You should be offered:
- care at your GP surgery provided by doctors and nurses trained in asthma management
- full information about your condition and how to control it
- involvement in making decisions about your treatment
- regular checks to ensure your asthma is under control and your treatment is right for you (this should be at least once a year)
- a written personal asthma action plan agreed with your doctor or nurse
It is also important that your GP or pharmacist teaches you how to properly use your inhaler, as this is an important part of good asthma care.
Occupational asthma
If it is possible you have asthma associated with your job (occupational asthma), you will be referred to a respiratory specialist to confirm the diagnosis.
If your employer has an occupational health service, they should also be informed, along with your health and safety officer.
Your employer has a responsibility to protect you from the causes of occupational asthma. It may sometimes be possible to substitute or remove the substance triggering your occupational asthma from your workplace, to redeploy you to another role within the company, or to wear protective breathing equipment.
However, you may need to consider changing your job or relocating away from your work environment, ideally within 12 months of your symptoms developing.
Some people with occupational asthma may be entitled to Industrial Injuries Disablement Benefit.
Read further information:
Complementary therapies
A number of complementary therapies have been suggested for the treatment of asthma, including:
- breathing exercises
- traditional Chinese herbal medicine
- acupuncture
- ionisers – devices that use an electric current to charge (ionise) molecules of air
- manual therapies – such as chiropractic
- hypnosis
- homoeopathy
- dietary supplements
However, there is little evidence that any of these treatments, other than breathing exercises, are effective.
There is some evidence that breathing exercises can improve symptoms and reduce the need for reliever medicines in some people. These include breathing exercises taught by a physiotherapist, yoga and the Buteyko method (a technique involving slowed, controlled breathing).
Read further information:
Asthma: Symptoms, Types & Treatment
Overview
What’s asthma?
Asthma is a disease that affects your lungs’ airways. It is a chronic (ongoing) condition. A chronic condition doesn’t go away and needs ongoing medical management.
Asthma affects more than 24 million people in the United States. This total includes roughly 5.5 million children. Asthma can be life-threatening if you don’t get treatment.
What’s an asthma attack?
When you breathe normally, muscles around your airways are relaxed, letting air move easily. During an asthma attack, three things can happen:
- Bronchospasm: The muscles around the airways constrict (tighten). When they tighten, it makes the airways narrow. Air cannot flow freely through constricted airways.
- Inflammation: The airway linings become swollen. Swollen airways don’t let as much air in or out of the lungs.
- Mucus production: During the attack, your body creates more mucus. This thick mucus clogs airways.
What types of asthma are there?
Healthcare providers identify asthma as intermittent (comes and goes) or persistent (lasting). Persistent asthma can be mild, moderate or severe. Healthcare providers base asthma severity on how often you have attacks. They also consider how well you can do things during an attack.
Asthma can be:
- Allergic: Some people’s allergies can cause an asthma attack. Molds, pollens and other allergens can cause an attack.
- Non-allergic: Outside factors can cause asthma to flare up. Exercise, stress, illness and weather may cause a flare.
Who can get asthma?
Anyone can develop asthma at any age. People with allergies or people exposed to tobacco smoke and secondhand smoke are more likely to develop asthma.
Statistics show women tend to have asthma more than men, and asthma affects Black Americans more frequently than other races.
When a child develops asthma, healthcare providers call it childhood asthma. If it develops later in life, it’s adult-onset asthma.
Children do not outgrow asthma. They may have fewer symptoms as they get older, but they could still have an asthma attack. Your child’s healthcare provider can help you understand the risks.
Symptoms and Causes
What causes asthma?
Healthcare providers don’t know why some people have asthma while others don’t. But certain factors present a higher risk:
- Allergies: Having allergies can raise your risk of developing asthma.
- Environmental factors: Infants can develop asthma after breathing in things that irritate the airways. These substances include allergens, secondhand smoke and some viral infections. They can harm infants and young children whose immune systems haven’t finished developing.
- Genetics: People with a family history of asthma have a higher risk of developing the disease.
- Respiratory infections: Certain respiratory infections, such as respiratory syncytial virus (RSV), can damage young children’s developing lungs.
What are common asthma attack triggers?
An asthma attack happens when someone comes in contact with substances that irritate them. Healthcare providers call these substances “triggers.” Knowing what triggers your asthma makes it easier to avoid asthma attacks.
For some people, a trigger can bring on an attack right away. Sometimes, an attack may start hours or days later.
Triggers can be different for each person. But some common triggers include:
- Air pollution: Many things outside can cause an asthma attack. Air pollution includes factory emissions, car exhaust, wildfire smoke and more.
- Dust mites: You can’t see these bugs, but they are in many homes. If you have a dust mite allergy, they can cause an asthma attack.
- Exercise: For some people, exercising can cause an attack.
- Mold: Damp places can spawn mold. It can cause problems for people with asthma. You don’t even have to be allergic to mold to have an attack.
- Pests: Cockroaches, mice and other household pests can cause asthma attacks.
- Pets: Your pets can cause asthma attacks. If you’re allergic to pet dander (dried skin flakes), breathing in the dander can irritate your airways.
- Tobacco smoke: If you or someone in your home smokes, you have a higher risk of developing asthma. The best solution is to quit smoking.
- Strong chemicals or smells.
- Certain occupational exposures.
What are asthma symptoms?
People with asthma usually have obvious symptoms. These symptoms resemble many respiratory infections:
With asthma, you may not have all of these symptoms. You may have different signs at different times. And symptoms can change between asthma attacks.
Diagnosis and Tests
How do healthcare providers diagnose asthma?
Your healthcare provider will review your medical history, including information about your parents and siblings. Your provider will also ask you about your symptoms. Your provider will need to know any history of allergies, eczema (a bumpy rash caused by allergies) and other lung diseases.
Your healthcare provider may order a chest X-ray, blood test or skin test. Your provider may order spirometry. This test measures airflow through your lungs.
Management and Treatment
What asthma treatment options are there?
You have options to help manage your asthma. Your healthcare provider may prescribe medications to control symptoms. These include:
- Anti-inflammatory medicines: These medicines reduce swelling and mucus production in your airways. They make it easier for air to enter and exit your lungs. Your healthcare provider may prescribe them to take every day to control or prevent your symptoms.
- Bronchodilators: These medicines relax the muscles around your airways. The relaxed muscles let the airways move air. They also let mucus move more easily through the airways. These medicines relieve your symptoms when they happen.
- Biologic therapies for asthma when symptoms persist despite being on proper inhaler therapy.
You can take asthma medicines in several different ways. You may breathe in the medicines using a metered-dose inhaler, nebulizer or other inhaler. Your healthcare provider may prescribe oral medications that you swallow.
What is asthma control?
The goal of asthma treatment is to control symptoms. Asthma control means you:
- Can do the things you want to do at work and home.
- Have no (or minimal) asthma symptoms.
- Rarely need to use your reliever medicine (inhaler).
- Sleep without asthma interrupting your rest.
How do you monitor asthma symptoms?
Monitoring your asthma symptoms is an essential piece of managing the disease. Your healthcare provider may have you use a peak flow (PF) meter. This device measures how fast you can blow air out of your lungs. It can help your provider make adjustments to your medication. It also tells you if your symptoms are getting worse.
Prevention
How can I prevent an asthma attack?
If your healthcare provider says you have asthma, you will need to know what triggers an attack. If you know the triggers, you can try to avoid them to avoid an attack. You cannot prevent getting asthma, though.
Outlook / Prognosis
What’s the outlook for someone with asthma?
A person with asthma can live a very productive life, including participating in sports and other activities. Your healthcare provider can help you manage symptoms, learn your triggers and prevent or manage attacks.
Living With
What is an asthma action plan?
Your healthcare provider will work with you to develop an asthma action plan. This plan tells you how and when to use your medicines. It also tells you what to do if your asthma gets worse and when to seek emergency care. Understand the plan and ask your healthcare provider about anything you don’t understand.
What should I do if I have a severe asthma attack?
A severe asthma attack needs immediate medical care. The first step is your rescue inhaler. A rescue inhaler uses fast-acting medicines to open up your airways. It’s different than your normal maintenance inhaler, which you use every day. You should only use the rescue inhaler in an emergency.
If your rescue inhaler doesn’t help or you don’t have it with you, go to the emergency department if you have:
- Anxiety or panic.
- Bluish fingernails, bluish lips (in light-skinned people) or gray or whitish lips or gums (in dark-skinned people).
- Chest pain or pressure.
- Coughing that won’t stop or severe wheezing when you breathe.
- Difficulty talking.
- Pale, sweaty face.
- Very quick or rapid breathing.
A note from Cleveland Clinic
Many people live fulfilling lives with asthma. Some professional athletes with asthma have set records in their sport. Your healthcare provider can help you find the best way to manage your asthma. Talk to your healthcare provider about how to control your symptoms.
90,000 Bronchial asthma and COPD
COPD is a collective concept that unites a group of chronic diseases of the respiratory system: chronic obstructive bronchitis (COB), pulmonary emphysema (EL), severe bronchial asthma (BA).
COPD is also considered as a symptom complex with signs of terminal respiratory failure: FEV1 <1.5 l or 30% of the proper value, i.e. the progression of the disease, leading to the loss of a reversible component of bronchial obstruction, cor pulmonale.The most common (about 90%) cause of COPD is COP, about 1% is pulmonary emphysema (due to α1-antitrypsin deficiency), about 10% is due to severe asthma.
Bronchial asthma – a chronic inflammatory disease of the respiratory tract, in which mast cells, eosinophils and T-lymphocytes take part. In susceptible individuals, this inflammation leads to recurrent episodes of wheezing, shortness of breath, chest tightness, and coughing, especially at night and / or in the early morning.These symptoms are usually accompanied by widespread but variable obstruction of the bronchial tree, which is at least partially reversible spontaneously or under the influence of treatment. Inflammation also causes a concomitant increase in airway response to various stimuli (c) GINA (Global Initiative for Asthma).
Distribution of bronchial asthma.
- Bronchial asthma affects more than 300 million people.
- The incidence of bronchial asthma in different countries ranges from 1% to 18% of the population (in Russia – 6.2%).
- The maximum spread of bronchial asthma is observed in countries with a warm and damp climate, the minimum in the desert zone and in the Arctic.
- Currently, there is an increase in the severity of the course of bronchial asthma.
Factors influencing the development and severity of asthma:
| Endogenous: | Exogenous: |
|
|
Mechanism of development of bronchial asthma:
- Pathology
Inflammation of the respiratory tract
Remodeling of the bronchial wall
- Pathophysiology
Narrowing of the airway
Airway hyperresponsiveness
- Special mechanisms
Acute illness
Night asthma
Clinical picture.
The main symptoms of bronchial asthma are episodes of shortness of breath, wheezing, coughing and chest congestion. Of significant importance are: the appearance of symptoms after contact with an allergen, seasonal variability of symptoms, the presence of relatives with bronchial asthma or other atopic diseases.
The main groups of drugs used for the treatment of asthma:
β2 – adrenergic agonists ( short-acting – fenoterol, medium – salbutamol, long-acting – salmeterol, formoterol).
Effects : Relaxation of the smooth muscles of the airways, suppression of the release of mediators from mast cells, increased mucociliary clearance, prevention of bronchospasm.
M-anticholinergics – Ipratropium bromide (atrovent).
Methylxanthines (short-acting – Theophylline, Eufillin, long-acting – Teopek, Theophyllon).
Effects : bronchodilation, membrane stabilizing effect, improvement of bronchial patency, positive foreign, chrono-, dromo- and batmotropic effects, stimulation of the respiratory center, psychoemotional arousal.
Stabilizers of mast cell membranes ( sodium cromoglycate (intal), sodium nedocromil, ketotifen).
Used for basic therapy of mild bronchial asthma, prevention of bronchospasm caused by physical exertion, inhalation of tobacco smoke, cold air
Antileukotriene drugs ( leukotriene receptor antagonists – (Zafirlukast, Montelukast), 5-hydroxyLOG inhibitors (Zileuton)
Glucocorticosteroids
Regulate gene expression, change the spectrum and amount of synthesized proteins, have an anti-inflammatory effect (PLA2, stabilization of lysosomal membranes), affect the activity of fibroblasts, reduce the migration of monocytes to the inflammation focus, suppress the enzyme hyaluronidase.
Also for the treatment of bronchial asthma, PUFA (polyunsaturated fatty acids) are used as a false substrate.
90,000 Asthma medicines: an overview of our arsenal to defeat the disease
Let’s take a look at the goals of treatment and the modern arsenal of anti-asthma drugs. So let’s start with the real goals of asthma therapy. Briefly, they boil down to the formula: achieving asthma control . And this is true for a patient of any age, with any initial severity of the condition.
Controlled asthma should behave in such a way as not to be reminded of any symptoms for as long as possible. And the experience of recent years suggests that this lofty goal can be achieved in most patients. Only for this it is necessary for the whole family to work together (with the attending physician). But passive expectation of miracles (for example, complete and final healing or that the child will “outgrow” his illness) is not recommended.
So, for cooperation, we need a common language and self-control tools: a diary of symptoms and peak flowmetry, regular completion of the AST and / or ACQ questionnaires.Unknown words? Refer to the articles in the same section on our website or to your doctor. And within the framework of this small article I will tell you about two groups of anti-asthma drugs. These are BASIC THERAPY (1) and AMBULANCE (2) *.
1. BASIC THERAPY MEANS *
The doctor usually prescribes immediately for a long period (months!) With an anti-inflammatory purpose, for daily use, regardless of the presence / absence of asthma manifestations at the moment, for the prevention and not removal of bronchial obstruction.These drugs are the main hopes for achieving asthma control. Moreover, the duration of their use is not limited, there is no concept of “undergoing a course of treatment”: drug support can be used as long as it is needed. So, the BASIC ones include:
- Inhaled glucocorticosteroids = ICS (“hormones” in the language of beginners): Beclomethasone (Beklazon, Bekotid, Klenil-Jet), Budesonide (Pulmicort, Budenit-Sterineb, Tafen-novolizer) (Fledshiekazidone in Russia), and Flixotkazidone in 2013 G.-Mometasone (Astmanex) and Ciclesonide (Alvesco). Today, ICS is a well-studied and “honored” group of drugs. Their arrival in practice about 40 years ago became a real revolution in approaches to the treatment of asthma, because it made it possible to avoid the systemic (oral or intravenous) administration of steroids, but to treat directly the inflamed bronchi! It is no exaggeration to say that ICS is the cornerstone of basic anti-inflammatory therapy for asthma in patients of any age and severity from mild to severe.This group is the first choice for asthma treatment worldwide.
- Antileukotriene drugs = ALTR : Montelukast (Singular, Montelar) and Zafirlukast (Akolat). At present, their features, effects are being actively studied, experience is accumulating for various asthma variants (including physical effort asthma in professional athletes – drugs are allowed by the WADA anti-doping rules), the age threshold for use has been lowered (Montelukast has been used in Russia since 2 years).The most curious feature of the whole group is the tablet form, not the inhaler. Therefore, neither the old nor the little ones have any technical difficulties with taking the medicine. An interesting effect of this group of drugs is the possibility of both independent use and combinations with ICS therapy, which is especially relevant during periods of the “surge” of respiratory viral infections.
- Cromones : Sodium Cromoglycate (Intal, Cromhexal), Sodium Nedocromil (Tyled). Interest in them is retained by the domestic pediatric school – with mild asthma in young children, at the stage of reducing therapy and for the prevention of bronchospasm during physical exertion, with the so-called cough variant of asthma.
- Combinations of ICS with long-acting bronchodilators (ICS + LABA): Seretid, Symbicort, Tevacomb, Foradil-kombi, Foster. Fixed combinations “2 in one” for basic therapy are today the main tool for achieving control over moderate to severe and severe asthma, in the presence of nocturnal symptoms, pronounced hyperreactivity of the bronchi, the impossibility of completely eliminating the action of provoking factors. These medicines are intended to be taken on a daily basis exactly twice a day (morning and evening), as they act just within 10-12 hours after inhalation.Often one drug is produced in different dosages and / or forms, which is very convenient when moving to the next level of therapy (and believe me, the doctor always dreams of a “step down”, that is, reducing the volume of drug therapy).
2. AMBULANCE DRUGS *
Bronchodilators, bronchodilators, bronchospasmolytics, bronchodilators. In contrast, they are used to quickly relieve asthma symptoms in an exacerbation / attack, that is, as needed, rather than routinely.There are not so many drugs in this group: Salbutamol (Ventolin, Salamol), Fenoterol (Berotek), Combined drugs Berodual and Ipramol-Sterineb, as well as pills and injections of Euphyllin. In a few minutes after taking these drugs, they relax the spasmodic smooth muscles of the bronchi, due to which the patency of the airways is restored, air again freely enters the bronchi during inhalation and exhaled during exhalation. But bronchodilators cannot influence other mechanisms of bronchial obstruction – edema of the mucous membrane, mucus secretion, thickening of the bronchial wall due to inflammation and rearrangement at the cellular level.And they do not have a prophylactic effect, with the exception of the ability to prevent bronchospasm caused by exercise (exercise asthma). The effect – expansion of the bronchi under the action of bronchodilators – lasts about 3-6 hours. Thus, the more often the patient has to use the ambulance medication, the worse his asthma is controlled.
True, there is also a group of bronchodilators for routine therapy – they do not begin to act so quickly, but they work not 3-6 hours, but all 8-12 hours, and therefore usually the doctor prescribes them 2 times a day for admission for some time (from 5 days to several weeks) and always in combination with ICS – these are: Salmeterol (Serevent), Formoterol (Foradil, Oxis, Atimos), Clenbuterol, Ipratropium (Atrovent, Ipratropium-Sterineb), prolonged theophyllins (Teopek tablets, Theotard, etc.).
As you can see, no universal or ideal medicine has yet been found. New groups of funds are also being investigated and implemented. Each drug, even if assigned to one group, has its own nuances of use, often – its own device for inhalation (metered aerosol or powder inhalers, nebulizer), features of action, advantages and disadvantages.
To tell about everything at once is simply unrealistic, and probably not necessary. After all, we finally got to the most interesting.What is the basis for the choice of a specific medicine for a specific patient?
Clinical guidelines for asthma treatment (international – GINA, Russian – National program) recommend a certain stage of therapy, depending on whether asthma control is achieved. Accordingly, over time, both “steps down” (that is, reducing doses, the number of drugs used) and “steps up” in steps (that is, increasing therapy) are possible.
It is necessary to take into account the previous individual experience of the patient himself (tolerance, adverse events, opinion about the effectiveness), the correct use and convenience of the inhalation device, possible age and safety restrictions (in children, in pregnant women and nursing mothers), concomitant diseases and their medication treatment at this time …
So the choice will be made by your attending physician in the process of dialogue with you. And the more active and honest your position is, the faster you will be able to find your real drug. Be sure to ask the doctor to check the inhalation technique (especially when switching to a new type of device for you or if you have never done it before), grab the diary questionnaire (show your knowledge of self-control!) And discuss the questions that have arisen.
I wish all asthmatics complete control!
* When writing the names of drugs, I give first the internationally patented name, and in brackets – the commercial names.
Yulia Arturovna Yasnova, allergist-immunologist, Center “Paracelsus”
| Eligibility | Sampling method: Improbability sample Criteria: Inclusion criteria: 1. Age 0-14 years, clinical diagnosis of asthma according to Chinese pediatric practice. recommendations for the diagnosis and treatment of asthma 2.Home nebulization therapy for at least 3 months. 3. Guardians must sign an informed consent form; Subjects who can make decisions he / she must also sign an informed consent form. Diagnosis of Pediatric Asthma: A patient who meets criteria 1 to 4 or criterion 4 plus any element of criterion 5 may be diagnosed as childhood asthma. 1. Recurrent respiratory symptoms (wheezing, coughing, shortness of breath, chest tightness), usually worse at night / early morning, aggravated by exercise, viral infection, smoke, dust, pets, mold, dampness, changes in weather, laughing, crying, allergens.2. A musical high-pitched sibilant sound can be detected on both sides of the lung by auscultation of the chest. Wheezing usually occurs when you exhale. 3. The above symptoms / signs can be eliminated automatically or with anti-asthma treatment. 4. Exclusion of other diseases that can also cause wheezing, coughing, shortness of breath, chest. tightness. 5. Atypical symptoms / signs without wheezing or wheezing sounds (at least meet one of the following criteria): 1) Bronchial challenge test results are positive.2) Demonstration of reversibility of airflow limitation: i. The test result for bronchial dilatation is positive. II. Effective anti-asthma treatment to improve lung function. 3) The ratio of daily PEF variation (consistently more than two weeks) is more than 13%. Exclusion criterion: 1. Allergy to any cortical steroid inhaler 2. Introducing differential diagnosis of asthma such as congenital heart disease, gastroesophageal reflux, bronchopulmonary dysplasia, bronchiolitis obliterans, etc.3. Parents / guardians have problems expressing, understanding, writing and reading Chinese to be judged by an investigator 4. Subjects are participating in other ongoing clinical trials. 5. Subjects with other diseases that may affect the results of the study, as assessed by investigators Floor: All Minimum age: No data Maximum age: 14 years Healthy volunteers: No |
|---|
Allergic bronchial asthma – Pulmonology – 10.07.2020
anonymous, Woman, 28 years old
Good afternoon, Olga Voldemarovna. To you with such a question, now there is no way to get to the doctors because of the coronavirus pandemic, in the city there is quarantine, many are sick. It all started in February with excessive sneezing, then for the first time I felt a small lump in the nasopharynx, bought vasoconstrictor drops, everything went away instantly. A week later, my head began to hurt and my ears began to fill up. I turned to the ENT, took a picture: there was sinusitis, frontal sinusitis, ethmoiditis, non-purulent eustachitis, monocytes were slightly increased in the blood – 9.5. Were treated with metrid, flemoxin, lavage, vasoconstrictor for 8 days, physio. At that moment, my breathing was absolutely all right. After treatment, I felt that a lump in the nasopharynx began to grow and began to flow down the throat. At that time it did not bother me at all, but literally a couple of days later I fell ill again. There was a very strong pharyngitis, the throat was terrible, the temperature was 38 one day, then it went down, the sinusitis at that time was cured, the flowing went away, as it turned out, not for long.The therapist put me on washing my throat with salt, plus my nose became swollen again, another vasoconstrictor for 5 days. The cough at that time was strong for several days, I wanted to cough constantly and at night, there was a tickling in the throat and chest. I was prescribed cefazolin, on the third day I felt as if I could not breathe, as if I was under water. I called an ambulance: they said there were no problems with breathing, do not wind yourself up, but the back wall of the throat is covered with plaque, you are suffocating because of this. The chest was very painful at that time, I did an X-ray, they did not reveal anything, it was clean, I donated blood, only platelets 345 were increased, the leukocyte formula was normal.Then the flow into the nasopharynx resumed again, and a barking cough began, somewhere in the trachea and larynx region. Mucus flowed like a river, I stood every morning over the sink, expectorating thick colored mucus, this is exactly mucus. The sputum is thinner, after expectoration it became easier, but not for long, the mucus accumulated again, it tickled very strongly in the chest, I wanted to scratch the inside with a comb, when coughing, the nasopharynx was always added, there was always some kind of lump. I started to drink sumamed as prescribed by ENT for 7 days, there was no effect at all.In May I ran to the first clinic, because it became impossible, I started suffocating, I was ready to lose consciousness, everything seemed to swell in my chest, it felt sore in my throat, the pulmonologist’s saturation was 95, he began to treat me for obstructive bronchitis with regular antibiotics and euphyllin with dexamethasone. IgE was 30, in sputum streptococcus salivarius, Soe’s blood was 13, but I was told this was within normal limits, there was increased bilirubin in the urine. After dexamethasone, it seemed a little released, but still every morning I was spitting up white sputum along with thick mucus from the nasopharynx, the effect was temporary.Suffocations began to haunt me again. I want to add that all these 2 months everything was accompanied by a sore throat. I ran to do CT scan and sinuses in May, donate blood again, everything is clean on CT, I attach a photo of the conclusion, eosinophilic cationic protein was 13, fadiatop was negative 0.03, CRP – 0.4, procalcitonin – 0.024. The spirogram showed obstruction, but the indicators were all above 80, there was no reaction to Ventolin. I ran to another pulmonologist, coughing and gasping for breath, and said that there was nothing on his part. As a result, I turned to an allergist, she prescribed me bufomix, montelukast, nasobek, she does not exclude asthma, exhalation is lengthened, breathing is hard, dry wheezing.Bufomix was used for a month, the suffocation was gone, but the mucus in the nasopharynx did not want to pass from the word at all, I spread my nose on the side, but the mucus became more, I choke on it, I no longer have to cough up the cough, the cough gradually disappeared, but pulled it out from somewhere from the throat, until nausea and almost vomiting. It is unpleasant, and the feeling is like worms in the throat. Lore, in his part, excludes deviations. What kind of mucus is it in lumps and can it be in large quantities? Is there such an allergy? I was already worn out. To tears. It’s good at home in quarantine while sitting, it will be impossible at work.Is it posterior rhinitis in combination with asthma or is it some kind of terrible pathology, some kind of disorder in the body? I’m already afraid for all sorts of herpes and cytomegalovirus. I also passed on them. By the way, it all started with the nose. Does the throat hurt with asthma? Before that, there were no problems with breathing at all, only at all times, frequent yawning, a desire to take a deep breath. Help please, I am suffering with this mucus. Best regards, Zarina.
Photo attached to the question
The doctor told how to live with glaucoma and not go blind
– Sergey Yurievich, glaucoma is one of the leading pathologies of the organ of vision in the world.How would you describe the situation with it in Russia?
– There are five main causes of blindness in the world: cataracts, glaucoma, ocular complications of diabetes mellitus, age-related macular degeneration and high complicated myopia – myopia, leading to myopic retinal degeneration and other problems. Of these, only cataracts are a reversible cause of blindness. All other diseases lead to permanent loss of vision. The statistics on glaucoma are disappointing: within 20 years of follow-up, 22% of glaucoma patients go blind in both eyes and 54% in one eye.
The number of glaucoma patients in the world is difficult to determine precisely. We can track the number of these patients relatively well in countries such as Sweden, Denmark and a number of other countries that have a corresponding registry. It is much more difficult with the large states of Asia, Africa and Latin America. In Russia in 2017 there were more than 1 million 328 thousand registered patients with glaucoma. It should be understood that this is about half of the real number of patients with glaucoma.
Glaucoma is the lot of the elderly.In older age groups, the prevalence of glaucoma is several times higher. So, among 40-year-old patients with glaucoma about 1.5%, after 70 years – more than 10%, after 80 – already 14-16%, and after 90 – more than 20%. It should be noted that in our clinic the average age of patients is 72 years. So “adult” ophthalmology is a gerontological specialty, since cataracts, macular degeneration, and a number of other diseases manifest themselves over the years.
Unfortunately, we cannot cure patients with glaucoma, however, modern medicine is able to provide patients who have this diagnosis in a timely manner, the safety of visual functions for the rest of their lives.Naturally, with adequate treatment, the principles of which the patient must follow.
– What, in your opinion, is the reason for such an increase in the incidence?
– Glaucoma is the general name for nearly 60 different nosological forms, which have a variety of causes. As for the most common open-angle glaucoma, which accounts for 80% of all glaucoma cases, here, as already noted, age-related changes in the body are the cause. This concerns problems with the drainage system of the eye, which can no longer ensure the proper outflow of intraocular fluid that is constantly formed in the eye and is a supplier of nutrients for such avascular formations as the lens, cornea, trabecular meshwork.The amount of liquid produced should correspond to the amount of aqueous humor leaving the eye. In glaucoma, this balance is disturbed, and the amount of fluid produced is greater than the amount of fluid that flows out of the eye, which has a limited volume. Intraocular pressure begins to rise and affect the weakest part of the fibrous capsule of the eye, through which the optic nerve passes. This, as a rule, is joined by age-related problems of blood supply to the optic nerve and retina against the background of concomitant vascular pathology.The result is optic atrophy and irreversible loss of vision.
In addition to an increase in life expectancy, an increase in the number of diagnosed patients with glaucoma may be partially associated with an improvement in the quality of diagnostics. And it’s not that bad.
– What difficulties does an ophthalmologist face in the treatment of glaucoma? Are there any peculiarities typical for Russia?
– 40 years ago, experts believed that a diagnosis of glaucoma was an indication for surgical treatment.Today, about 85% of these patients can be treated conservatively. This is primarily medical treatment with eye drops or drug installations in combination with laser treatment.
Glaucoma surgery is losing popularity primarily because it is associated with a significant number of complications that often lead to visual impairment, despite the normalization of intraocular pressure. Although antihypertensive surgery effectively stops optic nerve atrophy, the accompanying opacity of the lens leads to decreased vision.Here, however, patients should remember that blindness from cataracts is reversible, and more than 20 million lens replacements have been performed in the world for a long time already, while blindness from glaucoma is incurable.
As for the complexities of drug treatment, first of all, they lie in the drugs themselves. So, back in the early 1980s, our choice was limited to pilocarpine, very toxic anticholinesterase drugs, adrenaline and clonidine. An abundance of side effects – both local and general – led to the fact that most of these drugs for lowering intraocular pressure were discontinued.The availability of a variety of glaucoma medications in our clinical practice today is a good thing because there is a choice. On the other hand, it is clear that there is no single effective drug.
Another difficulty is compliance by patients with doctor’s prescriptions, the so-called compliance. I always explain to patients that the main crime they commit, first of all, against themselves, is failure to comply with doctor’s prescriptions. It is known that glaucoma is an eye disease in a diseased body.Against the background of complete health, glaucoma does not happen. Therefore, it affects mainly patients of the older age group, who, as a rule, have a number of concomitant diseases. Most often these are diseases of the cardiovascular system. Often, drugs that are prescribed for the treatment of the main general somatic disease do not go well with those drugs that we use to reduce intraocular pressure. This applies, for example, to beta-blockers, which until recently belonged to the drugs with which the treatment of glaucoma began.Patients with heart failure, bradycardia, atrioventricular block, bronchial asthma, and chronic obstructive pulmonary disease should not receive beta-blockers.
– What should be done to prevent the problem of glaucoma from becoming so acute?
– An increase in the number of patients with glaucoma in absolute numbers is not always a bad thing, because it may indicate that it has begun to be better detected. The problem is asymptomatic disease and unexamined patients.Therefore, an effective screening program and the availability of specialized care are needed. In large cities, it is necessary to expand the network of glaucoma centers and equip them with modern high-tech equipment, which significantly reduces the examination time and provides the possibility of dynamic observation.
I would not place a lot of hope on general practitioners who are unlikely to be able to determine who is suspected of glaucoma and who is not. Sometimes it is difficult for them to distinguish an acute attack of glaucoma from a hypertensive crisis.At the level of the polyclinic unit, it should be possible to check visual acuity, visual field, and measure intraocular pressure. If there is an opportunity and skill – to examine the fundus and assess the condition of the optic nerve head.
Unfortunately, due to the pandemic, the possibilities of specialized medical care have significantly decreased, and many patients who need dispensary supervision were left without it. The possibilities of inpatient care have been sharply reduced. In St. Petersburg, for example, GMPB # 2 has been working as a covid hospital for several months, and together with it the city ophthalmological center located there.
Extraordinary circumstances dictate the need to develop technologies that allow patients to control the level of intraocular pressure on their own. Today, there are tonometers that can be issued to patients, and they can independently conduct tonometry for several days at different times of the day. This is important because, like blood pressure, intraocular pressure is not constant. Sometimes we can simply not determine the moment of increase in intraocular pressure during its rare measurements.
The use of modern medical information systems should improve control over the condition of patients with a high risk of glaucoma progression. It is necessary to create a glaucoma register.
It is important to develop information resources and patient communities both for disseminating information and providing psychological support to patients.
– Many glaucoma medications also contain a beta blocker. What can you expect with a combination of beta blockers prescribed by a cardiologist and an ophthalmologist?
– Interestingly, the ability to lower intraocular pressure was initially seen incidentally in hypertensive patients receiving systemic beta-blocker therapy.It was in the late 1960s, and in 1978, the first eye drops appeared with the beta-blocker timolol, which lowers intraocular pressure by reducing the formation of intraocular fluid. Later it turned out that the systemic use of beta-blockers for the treatment of hypertension is poorly combined with eye drops containing them for the treatment of glaucoma, since the decrease in intraocular pressure is worse. This is the opposite effect with local and systemic use of seemingly very similar drugs.When beta-blockers are prescribed by a cardiologist and an ophthalmologist is inattentive to this, the result is that the decrease in intraocular pressure is less, and there are more side effects. We, of course, continue to use beta-blockers today, but they have long ceased to be among the drugs with which to start treatment of glaucoma.
– How to improve the effectiveness of drug treatment of glaucoma?
– One of the problems with strict adherence to the doctor’s recommendations is that life should not turn into burial.When we had aqueous solutions of pilocarpine, the patient had to instill this drug 6, and in some cases 8 times a day. This treatment is counterproductive. It must be clearly understood that the recommendations must be implemented. Now there are drugs that can be dripped once or twice a day. It’s quite real. Various systems for the delivery of the drug into the eye in the form of a depot are under development, which will ensure the effect of the drug for several months. But this is still a question of a more or less distant future.One of the options for improving the action of antihypertensive drugs is a combination of several known drugs. It is much easier and more convenient to bury drops once or twice a day from one bottle than to drip them in the morning and evening, say, from two bottles.
Most patients do not use drops correctly. They think that the more they drip, the more they get inside the eye. But in fact, this is not so, because the volume of the conjunctival sac, where we put a drop of medicine, is several times less than the volume of the drop.Therefore, only a small fraction of what falls on the surface of the eyeball gets inside and has one or another therapeutic effect.
I always recommend that patients keep their medications in the refrigerator, because a cold drop is better felt whether it has been in it or not. If several medications need to be instilled, there should be at least a 10-15 minute interval between the instillation of the drops so that one medication is not washed out with the other. Otherwise, the last medicine to be buried has a curative effect.
90,000 Asthma may protect against coronavirus infection
Allergic bronchial asthma, according to German, Chinese, American and Russian scientists, may be a protective factor in coronavirus due to a special type of inflammation that allergy sufferers have. However, immunologists say that only people with a certain type of asthma, whose symptoms worsen when exposed to an allergen, have a lower risk of becoming infected. Moreover, if an asthmatic person nevertheless falls ill, then he may be harder to carry the virus.
Patients with allergic asthma can more easily tolerate a new type of coronavirus infection – such people have a special type of inflammation in the lungs that prevents the virus from entering. Academician of the Russian Academy of Sciences Alexander Karaulov said this to the Izvestia newspaper.
“Together with our German, Chinese and American colleagues, we are studying the role of allergic asthma as a protective factor in COVID-19. We have already prepared a scientific review, which was submitted to the press, where we consider in detail the aspects of this theory, ”he said.
According to him, asthma may be a protective factor in coronavirus due to a special type of inflammation that all people with allergies have – Th-2-mediated. Karaulov notes that it is the polarization of the immune response in this direction that possibly protects patients with allergic asthma from a severe form of coronavirus and from death.
Pediatrician-immunologist, doctor of medical sciences, professor Andrei Prodeus, in turn, explained to Gazeta.Ru that asthma itself is not a protective factor.
“There is evidence that in people who have allergies and allergic asthma, the number of Th-2 receptors, the very ones through which the virus can enter cells, their number is less. That is, it is more difficult for a virus to infect a person who has such an allergic disease, ”the doctor said.
He recalled that asthma is actually a chronic-allergic inflammation, which is manifested by bronchial edema and hypersecretion of mucus – that is, a large amount of sputum in the bronchi – as well as bronchial obstruction, that is, narrowing of the bronchial lumen as a result of a reaction to an allergic irritant.
“Accordingly, it becomes more difficult for a person to exhale air, that is, his vital capacity of the lungs also decreases, and it becomes more difficult for him to inhale and exhale. Asthma is a chronic, allergic disease, ”stressed Prodeus.
Moreover, the expert noted that at the moment it is impossible to talk about the accuracy of these studies. According to him, there is evidence that people with bronchial asthma have a slightly lower risk of getting infected when they meet with a patient with coronavirus infection.
“Another thing, you need to understand that if a person with asthma gets sick, then he can get sick worse, because his inflammatory process can be more pronounced. It is more difficult for him to get infected, but he can get sick harder. Such scientific data absolutely exist, I am familiar with them, “the interlocutor of Gazeta.Ru concluded.
Immunologist-allergist Maria Polner called for a detailed study of the effect of asthma on a person’s vulnerability to coronavirus.
“They share the Th-2 endotype of asthma, which includes allergic asthma.With this type, symptoms may appear / worsen upon contact with an allergen (dust, animals, pollen). And Th-2 asthma, in which neutrophilic inflammation plays a key role and the propensity to actively produce cytokines such as inteleukin-17 (Th27 is the endotype of asthma), interleukin 1, interleukin 6 and TNF, ”Polner clarified.
This form of asthma, as a rule, is associated with a more severe course of the disease and the achievement of poorer control over it. The same cytokines, according to the specialist, are involved in the “cytokine storm” in cases of coronavirus disease.
“Accordingly, with non-Th3 asthma there is a risk of a more severe course of COVID-19. As for the Th3 type of asthma, it is premature to say that it protects against severe asthma, but studies have already shown that this type of asthma does not increase the risks of severe asthma “, – explained the interlocutor of Gazeta.Ru
At the same time, the Ministry of Health previously warned Russians that, in addition to the elderly, people with certain chronic diseases, such as heart disease, diabetes, and asthma, fall into the risk group for a severe course of coronavirus infection.
The pulmonologist of the Russian National Research Medical University named after V.I. N.I. Pirogova Anna Sergeeva. In her opinion, such statements should not be made until there is a 100% guarantee for people suffering from allergic asthma.
“In such patients, the lungs already have inflammatory processes, moreover, they are chronic, therefore, it is categorically impossible to say that they will supposedly be easier to tolerate the coronavirus. Immunity is such a thing that for someone it can work in defense, while for someone, on the contrary, it can only harm, having met with an unknown virus, “Sergeeva said in a conversation with Gazeta.

 Am Rev Respir Dis. 1976 Apr;113(4):433–443. [PubMed] [Google Scholar]
Am Rev Respir Dis. 1976 Apr;113(4):433–443. [PubMed] [Google Scholar] A spirographic manifestation of small airway disease. Am J Med. 1972 Jun;52(6):725–737. [PubMed] [Google Scholar]
A spirographic manifestation of small airway disease. Am J Med. 1972 Jun;52(6):725–737. [PubMed] [Google Scholar] Bull Physiopathol Respir (Nancy) 1972 May-Jun;8(3):663–677. [PubMed] [Google Scholar]
Bull Physiopathol Respir (Nancy) 1972 May-Jun;8(3):663–677. [PubMed] [Google Scholar]
 Stay away from triggers and go to any area with clean air.
Stay away from triggers and go to any area with clean air. The water should be at least 130 degrees Fahrenheit so that it can kill dust mites and other allergens in your bedding.
The water should be at least 130 degrees Fahrenheit so that it can kill dust mites and other allergens in your bedding.