Body covered in hives. 5 Common Triggers of Sudden-Onset Hives: Understanding Urticaria and Its Treatment
What are the most common triggers for sudden-onset hives. How can you identify and manage hive outbreaks. What treatment options are available for urticaria. How do antihistamines help in relieving hive symptoms. When should you seek medical attention for hives.
Understanding Hives: Causes and Prevalence
Hives, medically known as urticaria, are a common skin condition affecting approximately 20% of the population at some point in their lives. These red, bumpy, or slightly raised welts can appear anywhere on the body, including the face, torso, back, arms, and legs. Hives can vary in size and may be isolated or connect to cover large portions of the body.
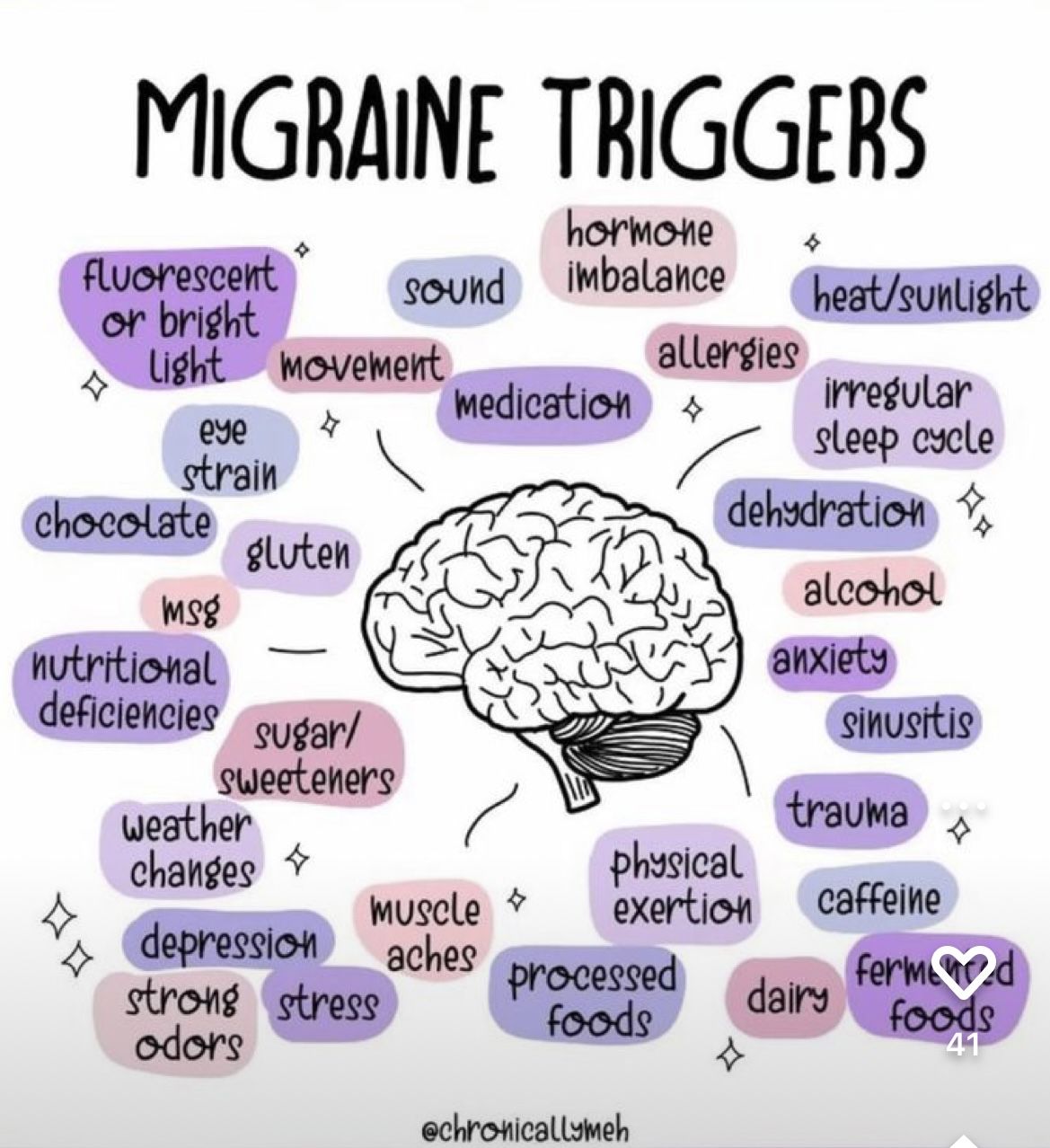
The primary cause of hives is typically an allergic reaction, although other factors such as stress, anxiety, or exercise can also trigger outbreaks. Hives occur when mast cells release histamine into the bloodstream, causing tiny pools of fluid to collect under the skin and form spots and welts of varying sizes.

Acute vs. Chronic Hives
Hives are categorized based on their duration:
- Acute hives: Last less than six weeks
- Chronic hives: Persist for more than six weeks
In this article, we’ll focus primarily on sudden-onset or acute hives and their common triggers.
5 Common Triggers of Sudden-Onset Hives
Identifying the trigger for a hive outbreak can sometimes be straightforward, while other times it may require some detective work. Here are five common triggers of sudden-onset hives:
1. Food Allergies
Certain foods are known to frequently cause allergic reactions that manifest as hives. The most common culprits include:
- Citrus fruits
- Milk
- Eggs
- Peanuts
- Shellfish
Can food allergies develop later in life? Yes, it’s possible to develop food allergies at any age, even if you’ve consumed the food without issues in the past. If you suspect a food allergy, consider keeping a food diary and consult with an allergist for proper testing and diagnosis.
2. Insect Bites and Stings
Allergic reactions to insect bites or stings can trigger hives. The most common culprits include:
- Wasps
- Yellow jackets
- Hornets
- Honeybees
An allergic reaction to an insect bite typically results in swelling and welts that extend beyond the immediate area of the bite.
3. Animal Allergies
Contrary to popular belief, animal allergies are not caused by the animal’s fur but by pet dander – tiny flakes of skin shed by cats, dogs, rodents, and birds. These allergies can manifest as hives in sensitive individuals.
Are hypoallergenic pets truly allergen-free? While no pet is completely hypoallergenic, some breeds produce less dander and may be better tolerated by allergy sufferers. However, individual reactions can vary, so it’s best to spend time with a specific animal before committing to pet ownership if you have allergies.
4. Pollen Exposure
For individuals with seasonal allergies, exposure to pollen can trigger not only typical hay fever symptoms but also hive outbreaks. Pollen from trees, grasses, and weeds can all be potential triggers.
5. Temperature Extremes
Both heat and cold can provoke hive outbreaks, especially in people with sensitive skin. This condition is known as physical urticaria and can be triggered by:

- Direct sunlight exposure
- Extreme cold temperatures
- Sudden temperature changes
Identifying Your Hive Triggers
Determining the specific trigger for your hive outbreak is crucial for effective management and prevention. Here are some strategies to help identify your triggers:
- Keep a detailed diary of your activities, food intake, and environmental exposures
- Note the timing and duration of hive outbreaks
- Consider any recent changes in your routine or environment
- Consult with an allergist for professional evaluation and testing
Is allergy testing always necessary for hive management? While not always required, allergy testing can be beneficial in identifying specific triggers, especially if the cause of your hives remains elusive after careful observation and diary-keeping.
Treatment Options for Sudden-Onset Hives
The primary goal in treating sudden-onset hives is to provide relief from symptoms and prevent future outbreaks. Here are some common treatment approaches:

Avoidance of Triggers
The first step in managing hives is to avoid known triggers whenever possible. This may involve dietary changes, modifications to your environment, or adjustments to your daily routines.
Antihistamines
Antihistamines are the mainstay of treatment for hives. They work by blocking the effects of histamine, reducing itching and minimizing the rash. Common over-the-counter antihistamines include:
- Cetirizine
- Fexofenadine
- Loratadine
How long does it take for antihistamines to work on hives? Most modern antihistamines start working within 1-2 hours of ingestion. However, it may take a few days of regular use to achieve maximum effectiveness in controlling hive outbreaks.
Corticosteroids
For severe cases of hives, your doctor may prescribe a short course of corticosteroid tablets, such as prednisolone. These medications suppress the immune system, reducing the severity of symptoms.
Topical Treatments
Calamine lotion or cool compresses can provide temporary relief from itching and discomfort associated with hives.

When to Seek Medical Attention for Hives
While most cases of sudden-onset hives resolve on their own or with over-the-counter treatments, there are situations where medical attention is necessary:
- Hives persist for more than six weeks
- Symptoms worsen or don’t respond to over-the-counter treatments
- You experience difficulty breathing or swallowing
- Hives are accompanied by fever, joint pain, or other systemic symptoms
Can hives be a sign of a more serious condition? In rare cases, hives can be a symptom of an underlying medical condition or a severe allergic reaction. If you experience recurrent or chronic hives, it’s important to consult with a healthcare professional for a comprehensive evaluation.
Living with Hives: Coping Strategies and Lifestyle Adjustments
Managing hives often requires a combination of medical treatment and lifestyle adjustments. Here are some strategies to help you cope with hives and minimize their impact on your daily life:
Stress Management
Since stress can trigger or exacerbate hive outbreaks, implementing stress-reduction techniques can be beneficial. Consider:
- Regular exercise
- Meditation or mindfulness practices
- Deep breathing exercises
- Adequate sleep and rest
Skin Care
Proper skin care can help reduce irritation and discomfort associated with hives:
- Use gentle, fragrance-free skincare products
- Avoid hot showers or baths, opting for lukewarm water instead
- Pat your skin dry instead of rubbing
- Wear loose-fitting, breathable clothing
Diet Modifications
If food allergies are suspected, working with an allergist or nutritionist to develop an elimination diet can help identify triggers. Once identified, avoiding these foods can prevent future outbreaks.
Are there any foods that can help reduce hive symptoms? While no specific foods are proven to cure hives, some people find relief by incorporating anti-inflammatory foods into their diet, such as omega-3 rich fish, leafy greens, and berries. However, it’s important to note that individual responses may vary.
Environmental Control
For those with environmental triggers such as pollen or pet dander, implementing measures to reduce exposure can be helpful:

- Use air purifiers with HEPA filters
- Keep windows closed during high pollen days
- Regularly clean and vacuum your living space
- Consider using allergy-proof bedding
The Future of Hive Treatment: Emerging Therapies and Research
While current treatments for hives are effective for many patients, ongoing research is exploring new therapies for those with chronic or treatment-resistant hives. Some promising areas of research include:
Biological Therapies
Monoclonal antibodies, such as omalizumab, have shown promise in treating chronic spontaneous urticaria. These targeted therapies work by blocking specific pathways in the immune system involved in hive formation.
Immunomodulators
Medications that modify the immune response, such as cyclosporine and methotrexate, are being studied for their potential in managing severe or chronic hives.
Personalized Medicine
Advances in genetic testing and biomarker identification may lead to more personalized treatment approaches, allowing doctors to tailor therapies based on an individual’s specific immune profile.

How close are we to a cure for chronic hives? While a definitive cure for all types of hives remains elusive, ongoing research is continually improving our understanding of the condition and developing more effective treatments. For many patients, current therapies can provide significant relief and improved quality of life.
Understanding the Psychological Impact of Hives
Living with hives, especially chronic or recurrent cases, can have a significant psychological impact. It’s important to address both the physical and emotional aspects of the condition:
Emotional Challenges
Hives can lead to various emotional challenges, including:
- Anxiety about potential outbreaks
- Depression related to chronic symptoms
- Self-consciousness about visible skin changes
- Frustration with treatment efficacy or side effects
Coping Strategies
To address the psychological impact of hives, consider the following strategies:
- Join support groups or online communities for individuals with hives
- Practice self-compassion and positive self-talk
- Engage in activities that boost self-esteem and promote relaxation
- Consider counseling or therapy if emotional distress becomes overwhelming
Can stress-reduction techniques alone improve hive symptoms? While stress management is an important aspect of hive management, it’s typically most effective when combined with appropriate medical treatment. However, reducing stress can help minimize trigger factors and improve overall well-being for many individuals with hives.

Understanding and managing hives requires a comprehensive approach that addresses both the physical symptoms and the underlying triggers. By working closely with healthcare professionals and implementing appropriate lifestyle modifications, most individuals with hives can achieve effective symptom control and improved quality of life. As research continues to advance our understanding of this complex condition, new and more targeted treatments offer hope for even better outcomes in the future.
5 Common Triggers of Sudden-Onset Hives: AIR Care: Asthma, Allergy, and Immunology
Hives, called urticarial by the medical community, are common, uncomfortable, and unsightly. Hives affect about 20% of the population in this country at some point in their lives.
These red, bumpy, or slightly raised welts can occur anywhere on your body including your face, torso, back, arms, and legs. Hives can be small or large. They can be isolated or connect to each other and cover an entire portion of your body. They are usually itchy. Sometimes they’re painful or sting.
They often disappear within a day only to return, lasting for a few days or a few weeks. If they last longer than six weeks, they’re considered chronic hives, rather than sudden-onset hives.
What causes hives?
An allergic reaction usually triggers hives, but they can also be caused by other situations such as stress, anxiety, or exercise. Hives are a reaction to the release of mast cells into the bloodstream, which unleashes the chemical histamine. The release of histamine causes tiny pools of fluid to collect under the skin, forming spots and welts of varying sizes.
Sometimes the cause for a hive outbreak is easy to figure out. Sometimes you and your allergist need to do some detective work. Unfortunately, sometimes the cause of hives is never determined.
Common triggers of sudden-onset hives
Fortunately, there are several common triggers of hives that can help you pinpoint whatever is triggering your itchy, blotchy hive outbreak. The most common triggers include:
Certain foods
Common foods that lead to an allergic reaction of hives include citrus fruits, milk, eggs, peanuts, and shellfish
Insect bites and stings
Most insect stings and bites come from wasps, yellow jackets, hornets, and honeybees. An allergic reaction to an insect bite means that you experience swelling and welts that extend outside the area of the bite itself.
Animals
An allergy to animals is not to the animal itself, or even the animal’s fur, as many people think. The allergy stems from pet dander, which is tiny flecks of skin shed by cats, dogs, rodents, and birds.
Pollen
If you’re one of the many people who suffer from seasonal allergies, then, unfortunately, exposure to pollen can not only bring on red, watery eyes and a stuffy nose; for some, it can also bring on an outbreak of hives.
Heat or cold temperature exposure
Direct sunlight or cold temperatures can bring on an outbreak of hives, especially for people with sensitive skin.
Treatment for hives
The first step to minimize hives is to steer clear of your triggers. Since that’s not always easy to do, especially if you like to spend time outside, then antihistamines can help provide relief from the itching and discomfort associated with hives.
Whatever your symptoms or triggers are, Dr. Richard Herrscher can help you develop a personalized treatment plan to combat hives and symptoms of hives.
For more information on triggers and treatments for sudden onset hives, call Dr. Herrscher at AIR Care with offices in Dallas and Plano, Texas. You can also make an appointment online through this website.
Urticaria (hives) | NHS inform
Most cases of urticaria don’t need treatment, because the symptoms are usually mild and often get better within a few days.
Short-term (acute) urticaria
If your symptoms are troublesome or persistent, antihistamines are available over the counter from pharmacies.
See your GP or speak to your pharmacist if your symptoms get worse. If your symptoms are very severe, your GP may prescribe other medications, such as a short course of corticosteroid tablets.
Go back to your GP if your symptoms get worse or if the treatment hasn’t worked after 2 weeks.
Antihistamines
Antihistamines block the effects of histamine, helping to stop the itchiness and reduce the rash. Examples of antihistamines include:
- cetirizine
- fexofenadine
- loratadine
For most people, modern antihistamines don’t cause drowsiness, although there are some exceptions. See how you react to the antihistamine before driving or operating heavy machinery. Antihistamines may also cause drowsiness if taken with alcohol. Always read the information leaflet that comes with the medication.
Antihistamines aren’t usually prescribed to pregnant women, as it’s not known whether they’re entirely safe. However, chlorphenamine may be recommended if it’s believed that the benefits outweigh the risks. There’s no evidence that chlorphenamine harms unborn babies.
Corticosteroid tablets
You may be prescribed a short course of high-dose corticosteroid tablets, such as prednisolone, if your symptoms are severe.
Corticosteroids suppress your immune system, which lessens the symptoms of urticaria. A course of prednisolone lasting between 3 and 5 days is usually recommended.
Taking steroid tablets on a long-term basis isn’t usually recommended, because it can lead to a wide range of side effects and complications, such as:
Long-term (chronic) urticaria
Treatment for chronic urticaria involves trying to control your symptoms and avoiding any triggers that make them worse.
If you have chronic urticaria and angioedema, you may be referred to a skin specialist (dermatologist). This is because angioedema is potentially more serious and can cause breathing difficulties.
You should also be referred to a dermatologist if you just have chronic urticaria and the symptoms continue, despite treatment.
Antihistamines
Chronic urticaria is treated with antihistamines. You may have to take them regularly for as long as your symptoms last.
An increased dose may be recommended if your symptoms don’t respond to treatment. Increasing the dose can often help to control symptoms that previously didn’t respond to treatment. However, this should only be carried out under the instruction of the doctor in charge of your care.
Menthol cream
Menthol cream can be used as an alternative or in addition to antihistamines because it helps to relieve itchiness. Your GP can prescribe this.
Corticosteroid tablets
Occasionally, more serious episodes of urticaria can be treated with short doses of corticosteroid tablets, such as prednisolone. Possible side effects of corticosteroid tablets include:
Long-term use of corticosteroids for chronic urticaria isn’t recommended for the reasons mentioned above.
h3 antihistamines
The type of antihistamines you can get from the pharmacist are known as h2 antihistamines. However, there are several other types of antihistamines, including h3 antihistamines.
h3 antihistamines can sometimes be useful for treating chronic urticaria, because they narrow blood vessels, which can reduce the skin’s redness.
h3 antihistamines can be used as an alternative to h2 antihistamines or in combination with them. Side effects of h3 antihistamines are uncommon, but include:
Don’t drive or use tools or machinery if you feel dizzy after taking a h3 antihistamine.
Leukotriene receptor antagonists
Leukotriene receptor antagonists are a type of medication that can help to reduce redness and swelling of the skin.
They can be a useful long-term alternative to using corticosteroid tablets, because they don’t carry the same risk of causing wide-ranging side effects.
The side effects of leukotriene receptor antagonists are rare and relatively minor. They include headaches and nausea (feeling sick).
Ciclosporin
In around two-thirds of cases, a powerful medication called ciclosporin has proved effective in treating urticaria.
Ciclosporin works in a similar way to corticosteroids. It suppresses the harmful effects of the immune system and is available in capsule form or as a liquid.
Side effects of ciclosporin include:
There are also a number of other side effects that can occur when taking ciclosporin, and you should discuss these thoroughly with your doctor before starting.
Side effects, such as high blood pressure and high cholesterol, are a particular cause for concern, because they can increase your risk of heart disease and stroke.
Even if you still respond to treatment, it may be recommended that the medication is withdrawn after a few months.
Omaluzimab
For urticaria that hasn’t responded to antihistamines, there are newer medications becoming available, such as omalizumab. Omalizumab is given by injection and is thought to reduce a type of antibody that can play a part in urticaria.
Diet
There’s some uncertainty over the role of diet in people with long-term urticaria. There are 2 groups of chemicals in foods that may trigger urticaria in some people –vasoactive amines and salicylates.
The Allergy UK website has more information on:
Avoiding or cutting down on foods that contain these chemicals may improve your symptoms. You could also keep a food diary to see whether avoiding certain foods helps you.
However, you should talk to a dietitian before restricting your diet. They can make sure you’re not avoiding foods unnecessarily and that your diet is healthy.
Avoiding triggers
If you know what triggers your urticaria or makes it worse, avoiding the trigger may keep your symptoms under control.
Triggers such as alcohol and caffeine can be easily avoided. If you think that a certain medication may be triggering your symptoms, contact the doctor who prescribed it, because alternatives may be available.
Avoiding stress can be more difficult, particularly if your symptoms negatively affect your quality of life.
If you have severe urticaria or urticaria that keeps coming back, you may find that relaxation techniques, such as meditation or hypnosis, reduce your stress levels and the severity of your symptoms.
What Causes Hives | Breaking Out in Hives for No Apparent Reason
Itchy, red hives happen when the body releases a chemical called histamine to fight a threat (real or imagined). An allergic reaction to food, an infection, and stress can all trigger hives, also called urticaria. There are seemingly endless triggers, and they can cause hives to break out within a few minutes or a few hours. Tracing hives back to the trigger is the first step toward effective treatment. This is relatively easy in some cases and more difficult in others.
For those with acute hives–hives that last 24 hours or less–identifying and avoiding triggers may be all it takes to keep hives at bay. For people with chronic hives that last longer than six weeks, triggers may be less obvious, and it might not come down to one specific cause. Understand the full range of potential triggers to help you narrow the field as you work with your doctor–a dermatologist or allergist–to find relief.
First, Keep in Mind: There Might Not Be an Identifiable Cause
One thing to note: unfortunately, not all hives triggers can be identified. Some people live with hives for months or years without knowing the trigger. This type of hives is called “idiopathic,” which translates to “cause unknown.” People with chronic idiopathic urticaria are often unable to identify a cause. Not finding an answer can be upsetting, but that doesn’t mean relief is out of reach.
Treatment with antihistamines can be just an effective for those with an unknown trigger as those with a known trigger. In both cases, corticosteroids may also be given in short courses. Newer treatments are also available specifically for chronic idiopathic urticaria. Biologic therapies work with the body’s immune system to block unknown triggers, and immunosuppressive drugs stop the body from responding with hives. The good news is, scientists are working hard to determine the underlying cause of chronic hives, and we will know more in coming years.
Thanks to this research, your doctor has more tools than ever to help you cope with hives, whether they’re a brief inconvenience or a longer-term condition. You have every reason to feel confident you can manage it together.
If you break out in hives every time you take penicillin or eat a Brazil nut, consider yourself “lucky.” You’ve likely found your trigger. Treatment may be as simple as avoiding your trigger as much as possible. Your doctor may also prescribe an antihistamine medication to make you more comfortable until the hives clear.
In cases where the trigger isn’t as straightforward, your doctor may ask you to keep a diary of foods you eat, medications you take, and things you touch to help reveal a connection. Keep these common culprits in mind:
Foods such as peanuts, shellfish, milk, eggs, and citrus fruits
Medication, including antibiotics, aspirin, ibuprofen, codeine, some high blood pressure medicines, and allergy shots
Insect stings and bites
Pollen
Animal dander
Plants such as poison ivy
Materials such as latex
Your doctor may recommend that an allergist perform a “skin prick” test or blood test to confirm the suspected trigger. A carefully supervised food or medication “challenge” may also be considered. This involves consuming or interacting with small amounts of a suspected trigger to see if it causes hives.
If your reaction to your trigger tends to be severe, such as having trouble breathing, your doctor may prescribe an epinephrine (adrenaline) auto-injector in case of a future emergency.
When it comes to hives, even the common cold can be a culprit. You may experience hives when you have a cold or another type of infection. Bacterial infections that can trigger hives include strep throat and urinary tract infection. Viral infections that can trigger hives include infectious mononucleosis and hepatitis.
A blood transfusion or an underlying illness such as lupus, thyroid disease, or vasculitis can also be a hives trigger. Vasculitis is an inflammation of the blood vessels that tends to be more painful than itchy and appear more like a bruise than a welt. Your doctor will take a complete medical history to help rule out underlying illness as a cause of your hives. To help diagnose vasculitis, a skin biopsy may also be obtained.
Hives can be caused by something you’re feeling—or doing—rather than by something you’re ingesting. Anxiety, for example, can trigger hives by raising your body temperature (cholinergic urticaria). If you and your doctor think you may have stress-induced hives, stress-management techniques such as meditation or yoga can help. You may also benefit from psychotherapy or antidepressant medications.
Take a look at your lifestyle, too. Do hives tend to appear after you’ve been in the sun? What about after exercising, or the reverse—sitting for a long period of time? You can likely exert some control over these common causes:
Temperatures changes, such as when you take a hot shower or swim in cold water
Too much sunlight (solar urticaria)
Exercise or sweating
Contact with chemicals
Pressure on the skin, from sitting too long or wearing tight clothing
Even if the cause of your hives is elusive, many people find relief with different treatments available. Work with your doctor to try to identify a trigger or triggers, and if you can’t, follow your treatment plan and keep an open line of communication with your doctor should you need to address any concerns.
Hives / Urticaria | ColumbiaDoctors
What are hives, or urticaria?
Hives or urticaria are a type of rash consisting of itchy, swollen, red welts. The itching may be mild or severe. Foods, medications, infections, exercise, scratching, alcoholic beverages, emotional stress and many other factors may worsen hives. The condition affects an estimated 20 percent of the population at one time or another in their lives.
How long can hives last?
Hives can last a variable amount of time. Usually, eruptions may last for a few minutes, sometimes several hours, and even several weeks to months. Most individual hives last no more than 24 hours.
What are the different types of hives?
Acute episodes of urticaria last for six weeks or less. Acute urticaria can be due to infections foods, medications, insect stings, blood transfusions and infections. The most common cause of hives is infections. Foods such as eggs, nuts and shellfish are common causes of urticaria. Medications such as aspirin and antibiotics (especially penicillin and sulfa) also are common causes of hives. Infections causing hives include the common cold, and other viral infections. In most of these cases, when the reason for hives is removed or avoided, the hives resolve.
Chronic episodes of urticaria last more than six weeks. In most cases, the cause of chronic hives will not be identified despite testing. Half of the patients have antibodies (proteins) that attack the mast cell (allergy cell). This triggers chemicals such as histamine to be released which causes the hives and itching. Even though hives are associated with other autoimmune conditions such as thyroid disease, treating the other condition doesn’t cure the hives. Rarely, chronic urticaria has been associated with cancer. In most cases of chronic urticaria, the hives will gradually disappear over time.
Physical urticaria is due to one or more “physical” causes. The most common reason for long-lasting hives is dermographism. These hives appear within a few minutes of scratching along an area of skin. Most often, the rash is linear, following the path taken by the act of scratching. Delayed pressure urticaria is swelling that appears on areas of constant pressure from belts and constricting clothing such as sock bands. Cold urticaria (from exposure to low temperature followed by re-warming) can be severe and life threatening if there is a generalized body cooling, for example after a plunge into a swimming pool. Cholinergic urticaria is due to an increase in body temperature with sweating, exercise, hot showers, and/or anxiety. Sun-induced urticaria may occur within a few minutes after exposure to the sun.
What causes hives?
In some cases, the cause is clear. A person ingests nuts or fish, and then develops hives within a few minutes or possibly a couple of hours. Some cases require a more detailed history from an Allergist to help figure out the cause. A single episode of uncomplicated hives does not usually need extensive testing. If the reaction involves respiratory symptoms, such as coughing, shortness of breath, throat closing or tongue swelling, then the patient should be immediately brought to the emergency department. If allergy is suspected, a diary of foods eaten within a few hours before the hives started may be extremely helpful.
Chronic urticaria should be evaluated by an Allergist/Immunologist. This specialist will take a detailed personal medical history, familys’ medical history, and medication history. In some cases you may require tests to analyze blood and urine. It is rare for a food to cause chronic hives. The specific cause of hives is rarely identified.
What medications treat hives?
There are many different antihistamines that are used to treat hives. Some cause drowsiness, others don’t. Very commonly patients are given a few antihistamines at a time to treat the hives. Sometimes medications such as steroids, antileukotrienes, and cyclosporine are needed to control hives.
Importance of medical follow-up
Whatever medication is used does not “cure” the hives, but helps to control outbreaks. When the medications are discontinued the hives can return. Patients should have us monitor their progress every one to two months initially.
Hives (urticaria) – Australasian Society of Clinical Immunology and Allergy (ASCIA)
Hives (the common term for urticaria), are pink or red itchy rashes, that may appear as blotches or raised red lumps (wheals), on the skin. They range from the size of a pinhead to that of a dinner plate. When hives first start to appear, they can be mistaken for mosquito bites. Swellings usually disappear within minutes to hours in one spot, but may come and go for days or weeks at a time, sometimes longer. In most cases hives are not due to allergy and they can be effectively treated with a non-drowsy antihistamine. When hives occur most days for more than six weeks this is defined as chronic (ongoing) urticaria, which may require additional medication.
ASCIA PCC Hives Urticaria 2021131.12 KB
Hives occur in the skin and are common
Up to 20% of people will develop hives at some time during their life. In most cases, hives are not due to allergy. Underneath the lining of the skin and other body organs (including the stomach, lungs, nose and eyes) are mast cells. Mast cells contain chemicals including histamine. When these are released into the skin they irritate nerve endings to cause local itch and irritation and make local blood vessels expand and leak fluid, triggering redness and swelling.
Can hives occur anywhere else?
Hives can also cause deeper swellings in the skin and mucosa, this is called angioedema. These swellings are often bigger, last longer, may itch less, sometimes hurt or burn and respond less well to antihistamines. Large swellings over joints, for example, can cause pain that feels like arthritis, even if the joint is not involved. Angioedema most frequently affects the face and lips. Although hives and facial swelling can be uncomfortable and cosmetically embarrassing, they are not usually dangerous. Information on angioedema is available on the ASCIA website.
Hives are rarely due to a serious underlying disease
Whilst a clear cause of hives in not obvious in many cases, causes may include:
- Infection from a virus is the most common cause of hives in children, especially if they last for more than 24 hours.
- Contact allergy to plants or animals may cause localized hives.
- Allergic reactions to food, medicines or insect stings can appear as hives. They usually occur within one to two hours of exposure and disappear in most cases within six to eight hours.
An allergic cause for hives should be suspected if episodes are rare, short-lived and occur under specific circumstances, for example:
- Only when exercising.
- Always within two hours of a meal.
- When symptoms involving other organs occur around the same time, such as stomach pain, vomiting, difficulty breathing or dizziness.
- If hives occur with swelling of the tongue or throat, difficulty breathing or low blood pressure, anaphylaxis should be suspected. Urgent administration of adrenaline and medical assessment is required. Information about anaphylaxis is available on the ASCIA website.
Ongoing hives lasting days at a time are almost never allergic in origin, with the exception of some cases of allergy to medicines. Stress is a very rarely the cause of hives but may make the symptoms worse.
In some people hives are caused by physical triggers, including cold (such as cold air, water or ice), heat, sunlight (solar), vibration, rubbing or scratching of the skin (dermatographism), and delayed pressure (such as after carrying heavy bags. In other people, exercise (sweating), stress, alcohol, spicy food or coffee may cause symptoms.
Chronic urticaria is defined when hives occur most days for more than six weeks
Symptoms of chronic urticaria usually resolve, although this can take months or several years. Most people with chronic urticaria manage with appropriate doses of non-drowsy antihistamines. People with severe symptoms interfering with quality of life may be referred to a clinical immunology/allergy specialist or dermatologist for assessment and consideration of additional medications.
Most people with hives do not need tests
Tests are sometimes done when hives go on for long periods, or when unusual symptoms are occurring around the same time. This is to exclude other diseases, which may appear as hives first, and other conditions later. If hives are associated with high fever, bruising, bleeding into the skin, purple lumps that last for several days, or sore joints, a doctor’s appointment should be arranged promptly.
Allergy testing is performed when the history suggests an allergic cause.
Treatment of hives
Whilst most hives resolve within a couple of weeks without any specific treatment, the following treatments may be useful:
- Avoid aggravating factors such as avoiding excessive heat, spicy foods or alcohol.
- Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided as they often make symptoms worse.
- Medications like non-drowsy antihistamines are often used to reduce the severity of the itch. Severe throat swelling requires early use of adrenaline and attention by your doctor or treatment in hospital.
- Severe chronic urticaria sometimes requires a trial of medicines which reduce inflammation, often called immune modulators or immunosuppressive medications. Recurrent courses of cortisone/steroid tablets need to be avoided due to a significant risk of side effects.
- Special diets appear to have a limited role to play in the management of hives. Unfortunately, it is difficult to predict who will, or will not respond to diet on the basis of history or allergy testing. A temporary elimination diet under close medical supervision, followed by challenges may be useful in a small number of cases.
For patient support organisations go to www.allergy.org.au/patients/patient-support-organisations
© ASCIA 2021
ASCIA is the peak professional body of clinical immunology/allergy specialists in Australia and New Zealand.
ASCIA resources are based on published literature and expert review, however, they are not intended to replace medical advice. The content of ASCIA resources is not influenced by any commercial organisations.
For more information go to www.allergy.org.au
To donate to immunology/allergy research go to www.allergyimmunology.org.au/donate
Updated March 2021
Hives (mate kārawa) | Health Navigator NZ
Hives (mate kārawa) are an itchy rash that can appear anywhere on your body. This rash is sometimes called weals or wheals. It comes and goes and can last from hours or days (acute) to months (chronic).
Key points
- Hives are common, with 1 out of 5 people getting them at some stage in their life.
- Hives can be triggered by lots of things and the cause can only be identified about half the time.
- Treatment involves avoiding known triggers and taking antihistamines.
- Angioedema is similar to hives, but the swelling is beneath your skin.
Are hives serious?
Hives usually settle within a day and cause no harm. However, they can sometimes be a sign of a serious allergic reaction, drug reaction or even life-threatening anaphylaxis.
|
Seek medical help immediately by calling 111 in New Zealand if you have:
|
|---|
|
Image source: DermNet NZ
What causes hives?
Hives form when your immune system releases a chemical called histamine. Histamine release can be triggered by lots of things and the cause is not always clear.
- Infection from a virus is the most common cause of hives in children, especially if they last for more than 24 hours.
- Direct contact with plants or animals may cause hives in just one area of your body.
- Allergic reactions to food, medicines or insect stings can appear as hives. They usually occur within 1–2 hours of exposure and disappear in most cases within 6-8 hours.
- Hives can be caused by physical triggers, including cold (such as cold air, water or ice), heat, sunlight (solar), vibration, rubbing or scratching your skin (dermatographism) and delayed pressure (such as after carrying heavy bags).
- Rarely, exercise, sweating, alcohol, spicy food or coffee may cause hives.
- Stress rarely causes hives but may make symptoms worse.
Identifying the cause of hives is tricky. They are probably due to an allergic reaction if there are patterns to when they appear, eg:
- always within 2 hours of a meal
- other symptoms occur around the same time, such as stomach pain, vomiting, difficulty breathing or dizziness.
Ongoing hives lasting days at a time are almost never due to allergy, with the exception of some cases of allergy to medicines.
Serious allergic reaction
Sometimes hives may be a sign of a serious, life-threatening allergic reaction which requires immediate medical attention. If hives occur with swelling of your tongue or throat, difficulty breathing or low blood pressure, anaphylaxis should be suspected. You will need urgent administration of adrenaline (Epipen®) and medical assessment.
What are the different types of hives?
There are 2 main types of hives:
- Acute urticaria (hives) – these last less than 6 weeks. It often goes away within hours to days.
- Chronic urticaria (hives) – this is when hives occur most days for more than 6 weeks.
This page focuses on acute cases of hives. Read about chronic hives.
What are the symptoms of hives?
The key symptoms of hives are weals (raised, itchy swellings) that:
- are round or form rings, a map-like pattern or giant patches
- may change shape
- are a few millimetres or several centimetres in diameter
- coloured white or red
- with or without a red flare
- may last a few minutes or several hours
- can affect any part of your body
- may be widespread across your skin.
How are acute hives diagnosed?
For most cases of acute hives, you don’t need to see a doctor.
- If you notice a trigger causes you to get hives, try to avoid it.
- Avoid anything that may worsen hives, such as heat, tight clothes and alcohol.
- Most people with acute hives do not need tests, unless they go on for a long time or you have unusual symptoms around the same time.
- If the suspected cause is allergy, skin or blood tests may be done.
How are hives treated?
Cool cloth, bath or shower
If the reaction is mild, simple measures such as a cool bath or shower may be all that is needed.
Antihistamines
Since the skin reaction is caused by histamine release, most people benefit from taking antihistamines such as loratadine or cetirizine to ease the itch. They can be bought from a pharmacy or prescribed by a doctor or nurse practitioner.
Please note these medicines may cause drowsiness, so take care when driving or operating machinery.
Avoid the causes/triggers
If the cause is a specific food, food additive, shellfish, cosmetic or anything else, avoiding these foods or substances will reduce the risk of hives coming back again.
Also avoid anything that can make hives worse such as excessive heat, spicy foods or alcohol.
Aspirin and other NSAIDs should be avoided as they often make symptoms worse.
Severe cases
If the rash is widespread or you have any swelling of your mouth or airways, seek medical help urgently. You may need need adrenaline, steroid medicine and admitting to hospital to identify the cause and prevent life-threatening reactions.
Diet
Special diets aren’t usually useful in the management of hives.
Learn more
Images of urticaria & angioedema DermNet NZ
Allergies & hives (urticaria & angioedema) WebMD
References
- Hives (urticaria) Australasian Society of Clinical Immunology and Allergy (ASCIA), 2019
- Acute urticaria DermNet NZ
- Diagnosing urticaria NHS, UK
Reviewed by
| Dr Sharon Leitch is a general practitioner and clinical research training fellow in the Department of General Practice and Rural Health at the University of Otago. Her area of research is patient safety in primary care and safe medicine use. |
Back to top
Credits: Health Navigator Editorial Team. Reviewed By: Dr Sharon Leitch
Last reviewed: 22 Feb 2020
What are chronic hives?
- Chronic hives (urticaria) are when hives occur most days for more than 6 weeks. They are less common than acute hives, with about 1 in 1000 people affected.
- They are more common in women than men (two-thirds of those with this condition are women).
- Symptoms are the same as in acute hives, but last longer.
- Although chronic hives clear up in most cases, some people will experience longer-term symptoms.
- Treatment includes avoiding any known triggers and taking antihistamines.
What are the different types of chronic hives?
Chronic hives may be spontaneous or inducible (physical). You can have both types at the same time.
Spontaneous chronic urticaria is the diagnosis when the trigger for hives is not known.
Inducible or physical chronic urticaria is a reaction to a known external factor. This includes hives caused by the following:
- stroking your skin (dermographism) – this is the most common type of inducible/physical urticaria
- exposure to cold, cold water and cold objects (cold urticaria)
- sweating (cholinergic urticaria)
- direct contact with a substance such as stinging nettles, foods, preservatives, fragrances, plant and animal products, metals and rubber latex (contact urticaria) – this is different to dermatitis, which develops hours or days later
- pressure to your skin – this can be an immediate or delayed reaction (pressure/delayed pressure urticaria)
- exposure to sunlight or to artificial ultraviolet (UV) light (solar urticaria)
- direct contact of warmth to your skin (heat urticaria)
- exposing your skin to vibration, repetitive stretching or rubbing (vibratory urticaria)
- contact with water (aquagenic urticaria).
Some of these types are quite rare.
What causes chronic or recurrent hives?
While external factors can be identified as triggers for inducible/physical hives, the cause of chronic spontaneous hives is often unknown, but it is likely to be an autoimmune reaction (where your immune system mistakenly attacks your own cells as if they were cells from a germ).
Chronic spontaneous hives have also been associated with:
How are chronic hives diagnosed?
Chronic hives are diagnosed if you have a long history (more than 6 weeks) of daily or regular hives. Your doctor will take a family history and do a physical examination.
Inducible hives are often confirmed by inducing the reaction, such as scratching your skin in dermographism or applying an ice cube in suspected cold urticaria.
Your doctor may ask for blood tests to rule out underlying conditions.
How are chronic hives treated?
Most people with chronic hives manage with appropriate doses of non-drowsy antihistamines such as cetirizine and loratadine. The doses for chronic hives are usually higher than the usually recommended doses. Although referred to as ‘non-sedating’, these medicines may still cause drowsiness especially at higher doses, so take care when driving or operating machinery.
If the cause is a specific food, food additive, shellfish, cosmetic or something else, avoiding those foods or substances will reduce the risk of hives coming back again. Also avoid anything that can make hives worse such as excessive heat, spicy foods or alcohol.
Steroid or antihistamine creams are not helpful and may cause skin changes or skin irritation.
People with severe symptoms interfering with quality of life may be referred to a clinical immunology/allergy specialist or dermatologist for assessment and consideration of additional medications.
What is the outlook for chronic hives?
Although chronic hives clear up in most cases, 15% of people continue to have symptoms at least twice weekly after 2 years.
Learn more
Chronic urticaria NHS, UK
Images of urticaria & angioedema DermNet NZ
References
- Hives (urticaria) Australasian Society of Clinical Immunology and Allergy (ASCIA), 2019
Information for healthcare providers on hives
The content on this page will be of most use to clinicians, such as nurses, doctors, pharmacists, specialists and other healthcare providers.
|
This information is from Urticaria – an overview DermNet, NZ, 2015
Clinical features of urticaria
Urticarial weals can be a few millimetres or several centimetres in diameter, coloured white or red, with or without a red flare. Each weal may last a few minutes or several hours and may change shape. Weals may be round, or form rings, a map-like pattern or giant patches.
Urticaria can affect any site of the body and tends to be distributed widely.
Angioedema is more often localised. It commonly affects the face (especially eyelids and perioral sites), hands, feet and genitalia. It may involve tongue, uvula, soft palate or larynx.
Serum sickness due to blood transfusion and serum sickness-like reactions due to certain drugs cause acute urticaria leaving bruises, fever, swollen lymph glands, joint pain and swelling.
In chronic inducible urticaria, weals appear about 5 minutes after the stimulus and last a few minutes or up to one hour.
Characteristically, weals are:
- Linear in symptomatic dermographism
- Tiny in cholinergic urticaria
- Confined to contact areas in contact urticaria
- Diffuse in cold urticaria—if large areas of skin are affected, they can lead to fainting (potentially dangerous if swimming in cold water).
The weals are more persistent in chronic spontaneous urticaria, but each has gone or has altered in shape within 24 hours. They may occur at certain times of the day.
Clinical pathway
This information is from Auckland HealthPathways Urticaria accessed December 2019
Clinical history
- Establish onset and frequency.
- Determine whether acute (< 6 weeks) or chronic (≥ 6 weeks).
- Ask about obvious triggers.
- An identifiable trigger is more common in acute urticaria.
- A trigger is more likely to be relevant if symptoms start within 30 to 60 minutes of exposure, and resolve on withdrawal of the suspected trigger.
Consider:
- Aggravating factors, eg, heat, cold, tight clothing, NSAIDs, alcohol, stress.
- Any features suggestive of urticarial vasculitis (UV) – a single urticarial lesion that lasts longer than 24 hours and may leave bruising or scarring.
Examination:
- Check for signs and symptoms of severe or life-threatening allergic reaction.
- Well-circumscribed itchy weals with central pallor and surrounding flare that resolve within 24–48 hours without marking the skin.
- Rule out other causes of itchy rash.
Investigations:
- Routine diagnostic measures are not recommended in urticaria.
- Do not request “routine allergy testing” or “allergy panels” – test only if clinical history strongly suggests a specific trigger.
Management
Non-sedating antihistamines are first-line treatment in both acute and chronic urticaria. High doses are often required to control symptoms. Treatment failure is most commonly due to inadequate doses taken irregularly, or for too short a duration.
Other clinical resources
Regional HealthPathways NZ
Access to the following regional pathways is localised for each region and access is limited to health providers. If you do not know the login details, contact your DHB or PHO for more information:
Auckland DHB Clinical Immunology and Allergy : Hives/Urticaria
What is urticaria?
Urticaria (also known as hives) is an itchy rash that can appear like welts, which comes and goes in a seemingly unpredictable fashion.
Sometimes, if you scratch the skin, you may notice it comes up in a raised red line. This is called dermatographism.
Urticaria is actually quite common with one out of three people getting it at some stage in their life.
The skin swelling seen in urticaria is due to the release of chemicals such as histamine from mast cells and basophils in the skin, which causes small blood vessels to leak. The welts can be a few millimetres or several centimetres in diameter, coloured white or red, often surrounded by a red flare, and frequently itchy. Each wheal (or weal) may last a few minutes or several hours, and may change shape. Wheals may be round or form rings, a map-like pattern or giant patches.
The surface wheals may be accompanied by deeper swelling of eyelids, lips, hands and elsewhere. The deeper swelling is called angioedema and may occur with or without urticarial wheals (10%).
Did you know? 80% of cases of hives occurring in adults are not due to allergy
This is particularly true for hives that are recurrent or chronic (occurring on a daily basis). Hives due to allergy more often comes on in sudden discreet attacks after food only. Non-allergic hives can come and go any time of the day, and often occurs overnight or first thing in the morning too.
Causes of chronic or recurrent hives
Recurrent or chronic hives can be caused by different factors. Sometimes one of these factors can cause urticaria by itself, but sometimes a combination of multiple factors is needed.
Also, these factors can be intermittent, causing hives only sometimes. This can make it confusing when trying to identify the cause. Here is a list of some common causes:
- Autoimmune causes – this is where the body’s immune system tends to activate itself and cause the hives. This is quite a common cause of hives. It is important to note that it is very rare that this signifies any significant other autoimmune disease though. A thyroid test should be done however.
- Medications – commonly codeine or non-steroidal anti-inflammatory drugs NSAIDS like ibuprofen, diclofenac, Voltaren, Nurofen and aspirin. Many cough and cold remedies can contain NSAIDs. One in three adults with recurrent hives will intermittently and unpredictably react to NSAIDs and aspirin. If this happens all NSAIDs and aspirin must be avoided. Patients may need an alternative for analgesia, and an Arcoxia challenge can be considered.
- Stress and any extraordinary or emotional recent events in a person’s life may trigger or maintain hives.
- Infections including viruses and bacteria. This often causes hives during or after the infection for a few days.
- Time of menstrual cycle.
- Physical triggers may include pressure, cold, heat, sunlight, exercise and, rarely, water. Dermatographism or “skin writing” is marked by the appearance of weals or welts on the skin as a result of scratching or firm stroking of the skin. Seen in 4–5% of the population, it is one of the most common types of urticaria, in which the skin becomes raised and inflamed when stroked, scratched, rubbed, and sometimes even slapped.
Treatment of chronic or recurrent urticaria (hives)
The first step is diagnosis of the cause, which involves accurate, detailed discussion between doctor and patient, with particular emphasis on the multiple factors listed above. Sometimes, just understanding the role of these multiple factors with intermittent effects, helps a patient understand the nature of hives and can provide a feeling of control over the situation.
Antihistamines
- For patients with recurrent or even daily hives it is best to take regular antihistamines. This can be once daily, but often twice daily is needed. They should be non-sedating such as loratadine or cetirizine. If hives occur mainly at night or early morning, they should be taken before bed. Sometimes higher doses of regular antihistamines are required for urticaria than the doses used in other conditions. In general, these higher doses are well tolerated and side-effects are rare.
Avoid the causes
- Looking at the factors in the list above to see if any of these can be modified.
Does chronic urticaria go away?
For people who have chronic urticaria (hives every day for more than six weeks), this problem always goes away eventually. It does tend to take months to completely resolve. 50% of long term cases resolve by one year and 30% resolve the year after. Milder cases will often go away sooner.
90,000 Skin problems in adults: herpes, urticaria and much more
- Home> News> Common Skin Problems in Adults: Herpes, Hives and More
Do you have itchy spots, cracks or rashes on your skin? Damage to the skin, a change in its texture or color, the appearance of spots can indicate the development of an infection, contact with a skin allergen or irritant, or an exacerbation of a chronic disease. If you have these symptoms, seek medical attention.Some of these can be signs of a serious medical condition.
Shingles
A rash appears on the skin in the form of raised dots above the surface of the skin, which subsequently turn into painful blisters. The rash is accompanied by itching and tingling, and the skin becomes very sensitive. Shingles most commonly affects the skin on the chest and buttocks, but it can also appear on other parts of the body. The exacerbation lasts about two weeks. The rash goes away, but the numbness and itching can last for months, years, or even the rest of your life.Treatment includes the use of topical agents, antiviral drugs, and antidepressants. Timely initiation of therapy helps to avoid serious complications.
Urticaria
Urticaria appears as pale pink blisters that cause severe itching and burning. They vary in size and often blend together. The rash can appear on any part of the body and go away within a few minutes or a few days. Causes of hives include: exposure to extreme temperatures, infections such as sore throat, and allergies to medications, foods, and dietary supplements.It is treated with topical corticosteroids and antihistamines.
Psoriasis
Signs of psoriasis are dense red spots covered with white or silvery scales. Psoriasis is a chronic non-communicable disease. For unknown reasons, the immune system begins to stimulate the accelerated growth of skin cells. Psoriatic plaques typically appear on the elbows, knees, scalp, and lower back. They can pass and come back again throughout your life.Treatment consists of topical steroid ointments and drug therapy.
Herpes
Herpes simplex virus causes small, painful blisters filled with clear fluid on the lips or nose. The exacerbation lasts about 10 days, while the person remains infectious. Causative factors include colds, excessive sun exposure, stress, and hormonal changes such as during menstruation. Herpes can be treated with antiviral ointments and pills.See a doctor if pus appears in the wound, it turns red and you have irritation of the mucous membranes of the eyes.
Ingrown hair
Ingrown hairs occur when the sharp edge of the cut hair curls back after shaving and grows into the skin. This can cause irritation, suppuration and even scarring. To minimize the risk of ingrown hairs, take a hot shower before shaving. Run the razor in the direction of hair growth and do not stretch the skin when shaving.Always use shaving cream or foam. Rinse your skin with cool water and then apply a moisturizer.
Foot fungus
Fungal infection is often accompanied by severe burning and itching. Blisters and ulcers may appear on the legs. Foot fungus is contagious and is spread by direct and indirect contact. In order not to catch an infection, do not wear someone else’s shoes and do not go barefoot in public places (swimming pool, sauna, gym). It is treated with topical antifungal creams and ointments.A doctor may recommend medication for more severe cases. Legs, socks and shoes should be kept clean and dry during treatment.
Moles
Moles, usually brown or black, can be found anywhere on the body. They can appear alone or in groups. Most often, new moles appear before the age of 20. Some of them change slowly over the years. Formations can be flat or raised, solid or pigmented, and sometimes hair grows on them.Once a year, you need to check your moles with a dermatologist. See your doctor immediately if you notice that the mole has begun to grow rapidly, its color or borders have changed, it has become irregular, has an ulcer, bleeding or itching.
Pigment (age) spots
These unsightly brown or gray patches are not actually caused by aging, although they do increase with age. The main cause of their occurrence is exposure to the sun, which is why spots appear more often on open areas of the body – the face, forearms and hands.Whitening creams, exfoliation and dermabrasion can help lighten stains. See a dermatologist to rule out a serious problem like melanoma (skin cancer).
90,000 Research of skin diseases – to pass the analysis to SZCDM
Skin diseases have more than a hundred species and categories. The most dangerous dermatologists call viral and fungal infections of the skin, dermatitis, scabies, melanoma and non-melanoma skin cancer, psoriasis, urticaria, pyoderma, acne, bedsores, alopecia areata.
In the United States and Europe, skin diseases are the 4th largest disability received. Therefore, a variety of rashes, itching, pain, discoloration of the skin, peeling should not be underestimated – for any deviations from the norm, especially if they do not pass for a long time, you need to contact a specialist.
With extensive skin itching, they usually consult a therapist, with localized itching or rashes, a dermatologist. If necessary, they prescribe a referral to narrow specialists – a dermatovenerologist (skin diseases caused by STIs), a trichologist (problems of the scalp), a dermatocosmetologist (aesthetic skin problems).
Often, problems with the skin indicate diseases of other organs, and then dermatologists work together with endocrinologists, hematologists, oncologists, gynecologists, allergists and other specialists.
When skin examinations are prescribed
Normally, the skin is evenly colored, moderately moist, smooth. If any indicator changes, the changes bring obvious discomfort, the symptoms do not go away for a long time, you must consult a doctor.
The skin is heterogeneous, and diseases affect its various layers: psoriasis and scabies – epidermis, furunculosis – dermis, cellulite – subcutaneous fat, etc. the doctor decides what tests the patient needs to take in order to diagnose the disease.
An oral survey reveals the duration of the condition, the reasons – according to the patient’s version, regularity (whether it was like this before or for the first time), symptoms of the general condition, the presence of chronic diseases and diseases in relatives, colleagues, dietary characteristics, living and working conditions, etc.etc.
The specialist makes a visual examination and, if necessary, prescribes tests:
with a variety of rashes in the natural folds of the skin, on the scalp, neck, face;
with small whitish scales in the area of the nasolabial triangle, on the scalp, on the back, under the arms, in other places;
with itching, burning;
with the appearance of plaques covered with scales, usually – on the knee and elbow bends, in places where the joints are exposed, on the palms, soles, on the scalp;
with bruising, edema, ulcers;
when papillomas appear;
when spots of unknown origin are found;
with acne, pimples and other deviations of the skin from the norm;
with some nonspecific symptoms.
Types of skin diseases diagnostics:
Complete blood count:
by leukocytes, leukocyte formula, the presence / absence of an inflammatory process is determined;
for erythrocytes, hemoglobin – leukemia, the presence of internal bleeding;
for basophils and eosinophils – presence / absence / strength of the allergic process.
The blood of a healthy person contains no more than 5% eosinophils. An increase in their proportion raises suspicion of allergies. However, a high number of eosinophils is also characteristic of parasite infestation, therefore additional tests are required.
General urinalysis
Allows you to judge the presence / absence of the inflammatory process, to determine whether there are diseases of the kidneys and other related organs.
Blood biochemistry
With the help of this analysis, the metabolic processes in the body are judged, and the most complete, systemic picture of its work is obtained.
Stool analysis
With the help of this analysis, parasites are identified that can cause an allergic reaction, inflammatory processes of the skin.
Immunogram
With the help of an immunogram, the preliminary diagnosis is confirmed. During the study, the blood is tested for immunoglobulins: if they are elevated, the disease develops.
Microscopy of scrapings
Scrapings are performed if scabies and mycotic (fungal) infections are suspected.For the analysis, scales from the lesion focus, suspicious moves are used, which are placed on a glass slide and examined.
Epicutaneous and intracutaneous skin tests for allergic conditions
In some clinical situations, children and adults need to undergo an allergological examination, for example, for patients with allergic rhinitis, bronchial asthma, atopic dermatitis, food allergies, drug reactions, etc.
In the epicutane method, the allergen is applied to the skin to identify the irritant in cases with a delayed hypersensitive response to the contact allergen.Intracutane (intradermal, intradermal) methods are used to detect an immediate hypersensitive response to drugs, bee venom and some other irritants. Intradermal tests are highly accurate. however, their disadvantage is the large number of false positives.
Mycological, bacteriological, virological, serological tests for dermatoses caused by microorganisms
To identify pathogenic microorganisms, use:
scrapings of scales, nails, hair, which are specially processed and examined under a microscope – this is how pathogenic fungi are determined;
detachable from the urethra, smear – to identify gonococci, other STD pathogens;
smears-prints on Tzank cells from surfaces affected by erosion – to determine acantholytic pemphigus;
skin scrapings – to determine the scabies mite;
tissue juice collected from the bottom of hard chancre – to identify pale treponemas;
cultural studies (crops of pathological biomaterial) – to determine the causative agent of pyoderma, mycoses (including latent forms), STDs and carriage of deomatophytes.
Immunofluorescence tests for autoimmune diseases
Autoimmune skin diseases include cystic dermatoses – Duhring’s dermatitis herpetiformis, pemphigus (true and all its varieties), pemphigoid.
These diseases are based on the body’s immune response directed at the intercellular contacts of the skin. So, pemphigus vulgaris is characterized by the appearance of antibodies to desmosomes, pemphigoid – antibodies to hemidesmosomes.
The developed disease is well diagnosed using serological tests – antibodies are detected in about 80%. But with the initial forms and lesions of mucous antibodies in the blood there are no, therefore, direct and indirect immunofluorescence examination is used.
Direct immunofluorescence detects IgG and complement on cryostat skin sections. Indirect immunofluorescence reveals high titers of Ig G to desmosomes in the blood and fluid content of blisters – the higher the titers, the more severe the course of the disease.
Angiographic studies for vascular disorders
Vascular skin disorders – angiomas – include densely located blood and lymph vessels. Angiomas are located on and under the skin, changing its color to red and with a clear purple tint.
Distinguish:
hemangiomas – pathological clusters-tumors from blood vessels, colored red or purple.Children’s hemangiomas are especially common, which disappear in 2/3 of children by about 7 years of age, but leave “colored” marks or scars on the skin;
flaming nevi – pink, red, purple flattened spots, by their nature – congenital malformations of the blood vessels;
lymphangiomas – bumps of different sizes on the skin, formed by an accumulation of lymphatic vessels;
pyogenic granulomas – raised, fleshy red, reddish-brown formations, moist or crusted, which are formed by vigorously growing capillaries and edema of adjacent tissue;
spider angiomas – bright red spots with a central blood vessel and capillaries extending from it in the form of spider legs.
If the damage to the skin is only cosmetic, your doctor will advise you on how to get rid of it. But sometimes angiographic studies are required – contrast studies of blood vessels using X-ray, CT, MRI, etc.
Histological examination
Histological studies of the skin confirm or exclude a preliminary diagnosis, serve to determine the stage of the disease, the prevalence of the tumor.All this is necessary for correct diagnosis, prognosis and effective treatment.
A typical element is selected for biopsy, preferably fresh primary. If the rash is widespread, then the biomaterial is taken from such a focus, the removal of which will cause minimal cosmetic, functional defects.
The biopsy is performed under local anesthesia using a scalpel or puncture biopsy, electrosurgery.
Allergy tests
To determine the allergen, experts use different tests:
prick tests (applying drops with an allergen to the skin, then piercing through the drop with a lancet) – to detect sensitization to household, epidermal, pollen, medicinal, fungal and other allergens;
scarification (scratches with special lancets with allergens in cases where a prick test is impossible) – have a high specificity.however, they often give a false positive result;
application, or Patch tests (the allergen is applied to a patch that is glued to the back or shoulder) – to determine contact and atopic dermatitis.
Skin tests are evaluated after 20 minutes, 6 hours, or 24 to 48 hours, depending on the allergen. The test result can be negative, slightly positive, positive, or equivocal.
Additional studies
Serological (study of antibodies and antigens in blood serum)
With a high sensitivity to a certain allergen, the content of IgE antibodies in the blood increases, which in a normal state make up about ~ 0.001% of all immunoglobulins. To find out the irritant, allergen-specific antibodies are determined.
The study of blood serum begins with the determination of the total level of immunoglobulin E (IgE).However, in about 30% of people prone to allergies, total immunoglobulin is normal, and its increased level can also be observed with helminth infestation and some other diseases.
Then a specific irritant is identified by determining specific IgG antibodies, for example, to food, pollen, etc.
Microscopic (examination of smear under a microscope)
Cytological research is carried out with the aim of morphological assessment of the cellular composition, changes in cells (nucleus, cytoplasm, their ratio).Based on the data obtained, preliminary diagnoses of benign, malignant tumors, and other non-neoplastic lesions are made.
Pathological (biopsy)
Skin biopsy is performed for the purpose of microscopic detection of pathology – skin non-cancerous diseases (for example, psoriasis, systemic lupus erythematosus, scleroderma, periarteritis nodosa, amyloidosis, skin tuberculosis, etc.), skin cancer, bacterial skin infections, fungal infections.
The test results are ready in 1-6 weeks. Scars can be a complication of this method, but in some cases a biopsy is simply necessary to obtain an accurate analysis and prescribe an effective treatment.
Cost of services at SZDTSM JSC
At the Northwest Center for Evidence-Based Medicine, you can complete all skin examinations as directed by your doctor.
Experienced specialists work in laboratories, medical centers and laboratory terminals of SZCDM JSC, all departments are equipped with modern laboratory equipment and drugs.we guarantee you high research accuracy, security and confidentiality.
go to analyzes
History
Our institution begins its history in 1988, when the Rostov Regional School of Advanced Training for workers with secondary medical and pharmaceutical education was created in the Rostov region. In accordance with the constantly growing requirements of practical health care to the level and quality of training of specialists, the material and technical base and educational and methodological support of the school were dynamically developing.
In 2004, the ROUPK was renamed into the state educational institution of additional professional education “Center for advanced training of specialists with secondary medical and pharmaceutical education” of the Rostov region, and in 2011 – into the state budgetary educational institution of additional professional education of the Rostov region ” secondary medical and pharmaceutical education “
Currently, the center is a large educational institution in the South of Russia, with an educational building with an area of 1571 sq.m. and a strong material and technical base.
The head of the advanced training center is the Honored Doctor of the Russian Federation L.V. Dimitrova.
The purpose of the center is to provide educational services for advanced training at a modern and high-quality level. More than 8000 specialists in 32 specialties are trained in the center annually.
Conditions for the provision of educational services have been created:
- advanced material and technical base,
- team with high creativity,
- modern pedagogical and health-preserving technologies in teaching.
The modernization of the educational process is actively carried out:
- A unified information environment of the center was formed
- Completed the transition to multimedia technologies
| Multimedia equipment for the lesson (using an interactive whiteboard, document camera, etc.) | In the classroom for emergency medical care, students work with a training computer program for cardiopulmonary resuscitation |
| Computer final testing of students is carried out | Multimedia presentations are in the arsenal of every teacher.Example: the development of N.N. Garlikov. |
The achievement of our center is the introduction of the latest developments in the educational process:
- In the field of safety of the professional environment of medical workers
| Working with a needle breaker and portable autoclave | New in laboratory diagnostics (work with express analyzers) |
- In training students in the section “Ambulance and Emergency Aid”
| Using vacuum splints and cardiac massage with a cardiopump | Performing mechanical ventilation by ambulance paramedics after tracheal intubation using a laryngoscope |
- Nursing
| Mastering the technology of blood collection using vacuum systems | Learning to insert peripheral catheters |
Our contribution to the implementation of the Priority National Project “Health” is in the following areas:
- Formation of a healthy lifestyle
To achieve the best results in this area, a study room “Health” was opened
| The hardware and software complex “Health-Express” is being demonstrated | Work has been organized to combat tobacco smoking |
Contests are held among listeners for the best creative work to promote a healthy lifestyle
| Winner of the competition – the film “Radiant Smile” – the cycle “Dental care for the population” |
- Improving the provision of medical care to victims of road accidents
113 specialists trained to provide assistance to victims on the Federal highway M-4
- Improvement of medical care for patients with cardiovascular diseases
422 specialists trained to work in new vascular centers for minimally invasive surgery and cardiac surgery departments
Particular attention is paid to cooperation with the International Committee of the Red Cross in the North Caucasus
For five years of cooperation, 74 medical workers have studied.The activities of the center in this direction were highly appreciated by Michel Masson, head of the International Committee of the Red Cross in the North Caucasus.
The Center for Advanced Studies has ample opportunities to provide quality educational services for training specialists with secondary medical and pharmaceutical education in accordance with the constantly growing requirements of practical healthcare.
ALERZIN instructions for use, price in pharmacies in Ukraine, analogues, composition, indications | ALERZIN of the company “Egis”
pharmacodynamics .Levocetirizine is the active stable R-enantiomer of cetirizine, which belongs to the group of competitive histamine antagonists. The pharmacological action is due to the blocking of H 1 -histamine receptors. The affinity for H 1 -histamine receptors in levocetirizine is 2 times higher than that of cetirizine. Alerzin affects the histamine-dependent stage of the development of an allergic reaction, reduces the migration of eosinophils, vascular permeability, and limits the release of inflammatory mediators.Alerzin prevents the development and facilitates the course of allergic reactions, has an antiexudative, antipruritic, anti-inflammatory effect, has almost no anticholinergic and antiserotonin effect.
Pharmacokinetics . The pharmacokinetic parameters of levocetirizine have a linear relationship and almost do not differ from those of cetirizine.
Absorption . The drug after oral administration is rapidly and intensively absorbed. The degree of absorption of the drug does not depend on the dose of the drug and does not change with food intake, but C max of the drug decreases and reaches its maximum value later.Bioavailability reaches 100%.
In 50% of patients, the effect of the drug develops 12 minutes after taking a single dose, and in 95% – after 0.5-1 hours. 2 days. C max is 270 ng / ml after a single use and 308 ng / ml – after repeated use at a dose of 5 mg, respectively.
Distribution . There is no information on the distribution of the drug in human tissues, as well as on the penetration of levocetirizine through the BBB.In studies, C max was recorded in the liver and kidneys, and the minimum in the tissues of the central nervous system. The volume of distribution is 0.4 l / kg. Plasma protein binding – 90%.
Biotransformation . In the human body, about 14% of levocetirizine is metabolized. Metabolic processes include oxidation, N- and O-dealkylation, and coupling with taurine. Dealkylation primarily occurs with the participation of cytochrome CYP 3A4, while numerous and / or undefined CYP isoforms are involved in the oxidation process.Levocetirizine does not affect the activity of cytochrome isoenzymes 1A2, 2C9, 2C19, 2D6, 2E1, 3A4 at concentrations significantly exceeding the maximum after taking a dose of 5 mg orally. Given the low degree of metabolism and the lack of the ability to inhibit metabolism, the interaction of levocetirizine with other substances (and vice versa) is unlikely.
Derivation of . Excretion of the drug occurs mainly due to glomerular filtration and active tubular secretion. T ½ from blood plasma in adults is 7.9 ± 1.9 hours.T ½ of the drug is shorter in young children. The total clearance in adults is 0.63 ml / min / kg. Basically, the excretion of levocetirizine and its metabolites from the body occurs in the urine (an average of 85.4% of the administered dose of the drug is excreted). With feces, 12.9% of the taken dose of the drug is excreted.
Special populations
Renal impairment . The apparent clearance of levocetirizine in the body correlates with creatinine clearance (CLcr). Therefore, for patients with moderate and severe renal impairment, it is recommended to select the intervals between doses of levocetirizine taking into account CLcr.With anuria in the final end stage of kidney disease, the total body clearance of patients, compared with the total body clearance in individuals without such disorders, decreases by about 80%. The amount of levocetirizine excreted during a standard 4-hour hemodialysis procedure was <10%.
tablets . Symptomatic treatment of allergic rhinitis (including perennial allergic rhinitis) and urticaria.
Alerzin, tablets .
The drug is prescribed for adults and children over the age of 6 years
Recommended doses
Adults and children over 12 years old: the daily dose is 5 mg (1 tablet) once a day.
Children aged 6–12 years: the recommended daily dose is 5 mg (1 tablet).
For children aged 2 to 6 years, it is impossible to adjust the dose of the drug in the dosage form of film-coated tablets. It is recommended to prescribe levocetirizine in a dosage form suitable for pediatric use.
Method of application
Take a tablet by mouth, with or without food. The tablet must be swallowed whole with a little water. It is recommended to apply the daily dose at one time.
Alerzin, oral drops . The drug is prescribed for adults and children over the age of 2 years
Recommended doses:
- Children aged 2-6 years: The recommended daily dose is 2.5 mg (10 drops).The specified dose is applied at 1.25 mg (5 drops) 2 times a day;
90,080 children aged 6–12 years: the recommended daily dose is 5 mg (20 drops) once a day;
90,080 children over the age of 12 and adults: the recommended daily dose is 5 mg (20 drops) once a day.
Method of application
Drops should be dripped into a spoon or dissolved in a little water and taken orally. When diluting drops, it should be borne in mind (especially when used in children) that the volume of water to which the drops are applied should correspond to the amount of liquid that the patient can swallow.The prepared solution should be taken immediately.
When counting drops, the bottle should be held vertically (upside down). If there is no flow of drops (if the corresponding number of drops has not been received), turn the bottle upright, and then upside down again and continue counting drops.
The drug can be taken with or without food.
Elderly patients
Elderly patients with normal renal function do not require dose adjustment of the drug.
Renal failure
For patients with impaired renal function, the dose calculation should be carried out taking into account CL cr according to the table.
To use this dosing table, it is necessary to estimate the patient’s CL cr in ml / min. CL cr (ml / min) should be estimated from plasma creatinine (mg / dL) using the following formula:
(• 0.85 for women)
Correction of the drug dose for patients with impaired renal function:
| Renal function | CL cr , ml / min | Dose and number of doses |
|---|---|---|
| Normal kidney function | ≥80 | 5 mg once a day |
| Mild disorders | 50-79 | 5 mg once a day |
| Moderate disorders | 30-49 | 5 mg once every 2 days |
| Severe disorders | <30 | 5 mg once every 3 days |
| End-stage kidney disease (patients on dialysis) | <10 | Contraindicated |
For children with impaired renal function, the dose of the drug should be adjusted individually, taking into account renal clearance and body weight.
There are no specific data for use in children with impaired renal function.
Liver failure
Patients exclusively with hepatic insufficiency do not need to adjust the dosage regimen. Patients with hepatic and renal insufficiency should adjust the dosage regimen in accordance with the table above.
Duration of use
Patients with recurrent allergic rhinitis (symptom duration <4 days per week or for less than 4 weeks) should be treated according to illness and history; treatment can be discontinued if symptoms disappear and can be restored if symptoms recur.In the case of persistent allergic rhinitis (duration of symptoms of the disease is> 4 days per week or for more than 4 weeks) during the period of contact with allergens, the patient may be offered continuous therapy. There is clinical experience with levocetirizine for at least 6 months of treatment.
In chronic diseases (chronic allergic rhinitis, chronic urticaria), the duration of treatment is up to 1 year (data are available from clinical studies using cetirizine (racemate)).
Hypersensitivity to levocetirizine, cetirizine, hydroxyzine, any other piperazine derivatives or any other excipient of the drug. Severe chronic renal failure (CL cr <10 ml / min). For the drug in the form of tablets, there are also rare hereditary diseases of galactose intolerance, lactase deficiency or impaired absorption of glucose and galactose.
from the nervous system: drowsiness, headache, fatigue, weakness, asthenia, convulsions, paresthesia, dizziness, fainting, tremor, dysgeusia.
From the side of the psyche: sleep disturbance, agitation, hallucinations, depression, aggression, insomnia, suicidal thoughts.
From the side of the heart: increased heartbeat, tachycardia.
From the side of the organ of vision: visual impairment, blurred vision.
On the part of the organ of hearing and balance: vertigo.
From the liver and biliary tract: hepatitis.
From the kidneys and urinary system: dysuria, urinary retention.
Immune system disorders: hypersensitivity, including anaphylaxis.
From the respiratory system, chest and mediastinal organs: shortness of breath.
From the digestive tract: diarrhea, vomiting, constipation, dry mouth, nausea, abdominal pain.
Skin and subcutaneous tissue disorders: angioedema, persistent drug rash, itching, rash, urticaria.
From the musculoskeletal system: myalgia, arthralgia.
Research results: increase in body weight, deviations of liver function tests from the norm.
Eating and metabolic disorders: increased appetite.
General disorders: edema.
The drug should be discontinued in the event of any of the above side effects and when the cause of their development cannot be unambiguously established.
Methyl parahydroxybenzoate and propyl parahydroxybenzoate in oral drops may cause allergic reactions (possibly delayed).
Description of selected side reactions
Itching has been reported after discontinuation of levocetirizine.
Reporting of adverse reactions
Post-approval reporting of suspected adverse reactions is important. This allows you to continue monitoring the benefit / risk ratio of the drug. Health care providers are asked to report any suspected adverse reactions through the national reporting system.
is used with caution in patients with chronic renal failure (dosage adjustment is necessary) and elderly patients with renal failure (glomerular filtration may decrease). During the use of the drug, you should refrain from drinking alcohol.
If patients have certain factors that provoke urinary retention (for example, spinal cord injury, prostatic hyperplasia), attention should be paid when determining the dose of the drug, since levocetirizine may increase the risk of urinary retention.
Levocetirizine should be used with caution in patients with epilepsy and the risk of seizures, since its use can lead to increased seizures.
Antihistamines suppress the response to an allergic skin test, therefore, before taking it, the drug should be discontinued 3 days before the study (elimination period).
Itching may occur after discontinuation of levocetirizine, even if these symptoms were not present before starting treatment.Symptoms may go away on their own. In some cases, symptoms can be intense and re-treatment may be required. Only if the symptoms disappear can the treatment be restarted.
The drug in the form of tablets is not used in children under the age of 6 years, since this dosage form does not allow the necessary adjustment of the dosage regimen. For this category of patients, it is recommended to prescribe levocetirizine in a dosage form suitable for use in pediatrics.
Use during pregnancy or lactation . Levocetirizine is contraindicated during pregnancy. Levocetirizine passes into breast milk, therefore, if it is necessary to use the drug, breastfeeding should be discontinued.
Fertility . There are no clinical data (including animal studies) on the effect of levocetirizine on fertility.
The ability to influence the reaction rate when driving or working with other mechanisms .You should refrain from driving vehicles or working with other mechanisms during drug treatment.
interaction studies with levocetirizine (including studies with CYP 3A4 inducers) have not been conducted.
Studies with cetirizine (racemate compounds) have shown that concomitant use with antipyrine, azithromycin, cimetidine, diazepam, erythromycin, glipizide, ketoconazole or pseudoephedrine has no clinically significant adverse interactions.Simultaneous use with theophylline (400 mg / day) reduces the total clearance of levocetirizine by 16% (the theophylline kinetics does not change). In the study of repeated administration of ritonavir (600 mg 2 times a day) and cetirizine (10 mg / day), the degree of cetirizine exposure increased by about 40%, while the distribution of ritonavir slightly changed (-11%) before the parallel administration of cetirizine.
There is no data on the enhancement of the effect of sedatives when used in therapeutic doses.However, you should avoid the use of sedatives while taking the drug.
Levocetirizine does not enhance the effect of alcohol, however, in sensitive patients, the simultaneous use of levocetirizine and alcohol or other drugs that depress the central nervous system function can affect the central nervous system.
Food intake does not affect the degree of absorption of the drug, but the simultaneous consumption of food reduces the rate of absorption.
Symptoms: Overdose symptoms may include drowsiness in adults and initial agitation and increased irritability followed by drowsiness in children.
Treatment . There is no specific antidote to levocetirizine. In case of symptoms of an overdose, symptomatic and supportive therapy is recommended. Consideration should be given to the need for gastric lavage shortly after taking the drug.
