Can Cirrhosis Heal: Understanding Symptoms, Causes, and Treatment Options
What are the primary causes of cirrhosis. How does cirrhosis progress over time. What symptoms indicate the development of cirrhosis. Can early-stage cirrhosis be reversed. What treatment options are available for cirrhosis patients. How does alcohol consumption contribute to liver damage. Why is non-alcoholic fatty liver disease becoming more prevalent.
Understanding Cirrhosis: A Progressive Liver Condition
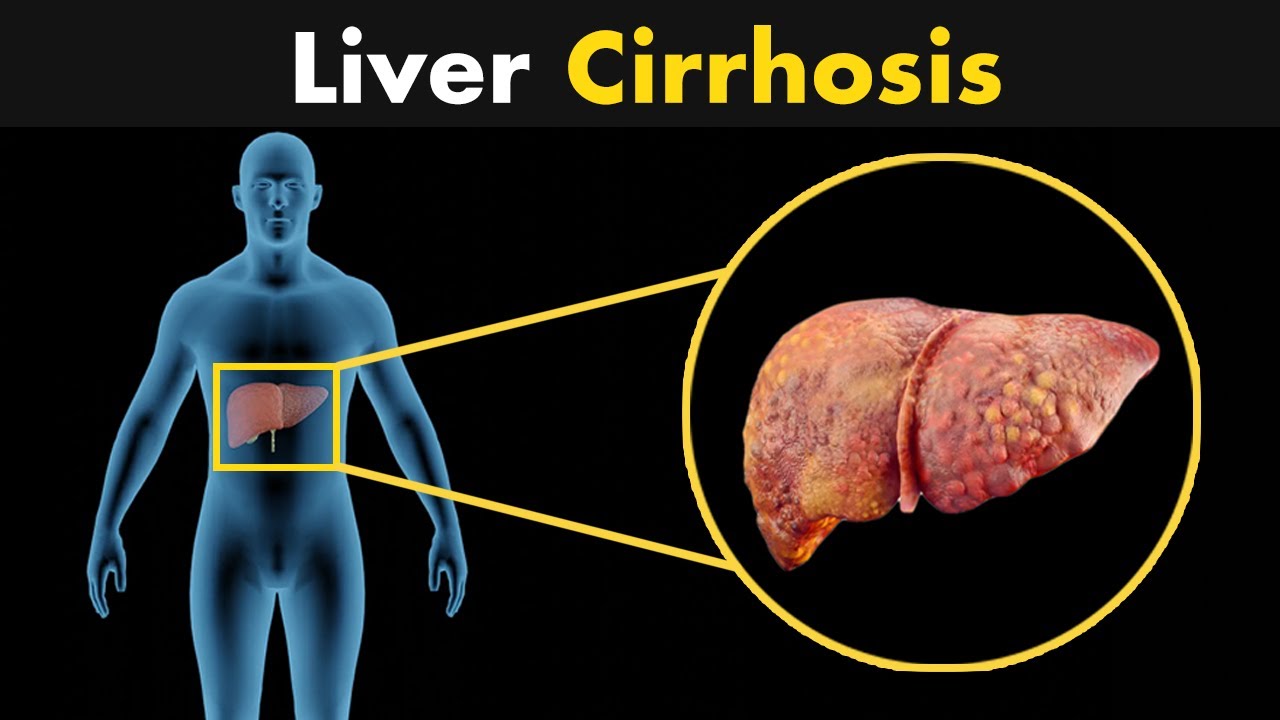
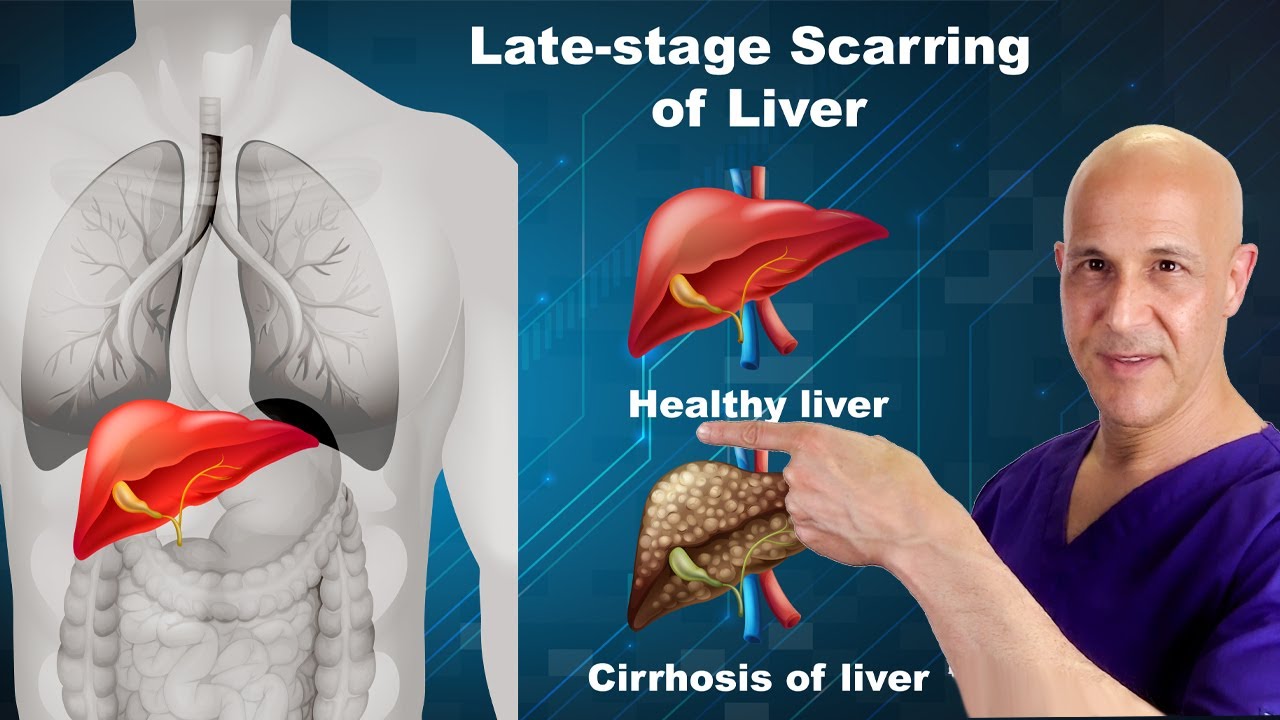
Cirrhosis is a serious liver condition characterized by the gradual replacement of healthy liver tissue with scar tissue. This progressive disease develops over many years, ultimately affecting the liver’s ability to function properly. As scar tissue accumulates, it impedes blood flow through the liver, leading to various complications and potentially life-threatening situations.
The severity of cirrhosis is often categorized using the Child-Pugh score, which classifies liver function into three categories:

- Category A: The liver is functioning well despite some damage
- Category B: Moderate liver damage is present
- Category C: Advanced or severe liver damage, also known as end-stage liver disease
Additionally, cirrhosis can be classified as compensated or decompensated. In compensated cirrhosis, the liver can still function effectively despite the damage, often without noticeable symptoms. Decompensated cirrhosis, on the other hand, occurs when the liver can no longer function properly, leading to more apparent symptoms and complications.
Major Causes of Cirrhosis: From Viral Infections to Lifestyle Factors
Several factors can contribute to the development of cirrhosis. Understanding these causes is crucial for prevention and early intervention. What are the primary causes of cirrhosis? The most common include:
- Viral hepatitis (particularly hepatitis B and C)
- Long-term excessive alcohol consumption
- Non-alcoholic fatty liver disease (NAFLD)
- Exposure to toxins, including certain medications
- Hereditary and genetic conditions
- Autoimmune diseases affecting the liver
- Metabolic syndrome and obesity
Viral Hepatitis: A Global Concern
Hepatitis B and C are the leading causes of cirrhosis worldwide. These viral infections can be contracted through exposure to infected blood, such as through needlestick injuries or sharing needles. While vaccines are available to protect against hepatitis B, there is currently no vaccine for hepatitis C.

In some cases, autoimmune hepatitis can also lead to cirrhosis. This occurs when the body’s immune system mistakenly attacks healthy liver cells, causing inflammation and damage over time.
Alcohol-Related Liver Disease: A Major Contributor
In the United States, alcohol consumption is the primary cause of liver disease. How does alcohol consumption contribute to liver damage? The liver is responsible for breaking down toxins, including alcohol. However, when alcohol levels are consistently high, the liver becomes overwhelmed and unable to process it effectively, resulting in damage to liver cells.
Alcohol-related liver disease progresses through three stages:
- Alcohol-related fatty liver (steatosis): Small fat droplets accumulate in the liver
- Alcohol-related hepatitis: Inflammation occurs in liver cells, causing swelling
- Cirrhosis: Irreversible damage that can lead to life-threatening complications
Individuals who consume 30-50 grams of alcohol per day for five years are at risk of developing alcohol-related liver disease. For context, males who consume more than 21 units per week and females who consume more than 14 units per week are at risk of steatosis due to alcohol consumption.
Non-Alcoholic Fatty Liver Disease: An Emerging Concern
Why is non-alcoholic fatty liver disease becoming more prevalent? NAFLD is diagnosed when fat accumulates in over 5% of liver cells without another apparent cause, such as alcohol consumption. This condition is closely linked to the rising rates of obesity, diabetes, and metabolic syndrome.
NAFLD encompasses two main conditions:
- Non-alcoholic fatty liver (NAFL): Characterized by fatty deposits in the liver
- Non-alcoholic steatohepatitis (NASH): Involves inflammation and cell damage in addition to fat accumulation
Individuals with metabolic syndrome, polycystic ovary syndrome (PCOS), or certain genetic conditions are at higher risk of developing NAFLD. The increasing prevalence of these conditions in modern society contributes to the growing rates of NAFLD and, consequently, cirrhosis.
Recognizing the Signs and Symptoms of Cirrhosis
What symptoms indicate the development of cirrhosis? In its early stages, cirrhosis often presents no noticeable symptoms. However, as the disease progresses and scar tissue accumulates, various signs and symptoms may emerge:

Early Symptoms of Cirrhosis
- Fatigue
- Nausea
- Loss of appetite
- Weight loss and muscle mass reduction
- Small, red blood vessel patches on the upper trunk and palms
Advanced Symptoms of Cirrhosis
- Swelling in the legs and abdomen (edema and ascites)
- Enlarged spleen
- Increased susceptibility to infections
- Confusion or difficulty concentrating
- Jaundice (yellowing of the skin and eyes)
- Dark-colored urine
- Tarry stools
- Persistent itching
- Internal bleeding
- Decreased libido
As cirrhosis advances, the liver attempts to heal itself by forming regenerative nodules. These lumps appear as the organ tries to repair the damage, but they can further compromise liver function.
Diagnosing Cirrhosis: Tools and Techniques
How do medical professionals diagnose cirrhosis? Diagnosing cirrhosis often involves a combination of medical history, physical examination, and various tests. Some common diagnostic tools include:
- Blood tests to assess liver function and look for signs of infection
- Imaging studies such as ultrasound, CT scan, or MRI to visualize the liver
- Liver biopsy to examine liver tissue for signs of damage and scarring
- Elastography, a non-invasive test that measures liver stiffness
- Endoscopy to check for varices (enlarged blood vessels) in the esophagus or stomach
The Child-Pugh score, mentioned earlier, is often used to grade the severity of cirrhosis. This scoring system takes into account various factors, including:
- Bilirubin levels
- Albumin levels
- Prothrombin time
- Presence of ascites
- Presence of hepatic encephalopathy
Based on these factors, cirrhosis is classified into categories A, B, or C, with category C representing the most severe form of the disease.
Treatment Options for Cirrhosis: Managing Symptoms and Slowing Progression
Can cirrhosis be treated effectively? While cirrhosis is generally considered irreversible, various treatment options can help manage symptoms, slow disease progression, and improve quality of life. The specific treatment approach depends on the underlying cause and severity of the condition.
Lifestyle Changes and Supportive Care
For many cirrhosis patients, lifestyle modifications play a crucial role in managing the condition:
- Abstaining from alcohol consumption
- Adopting a healthy, balanced diet
- Maintaining a healthy weight
- Regular exercise, as tolerated
- Avoiding medications that may further damage the liver
- Getting vaccinated against hepatitis A and B
Medications and Medical Interventions
What treatment options are available for cirrhosis patients? Depending on the underlying cause and symptoms, various medications and interventions may be prescribed:

- Antiviral medications for hepatitis B or C
- Diuretics to reduce fluid buildup
- Beta-blockers to lower portal hypertension
- Lactulose or rifaximin for hepatic encephalopathy
- Antibiotics for infections
- Medications to control itching
- Nutritional supplements to address deficiencies
In some cases, more invasive procedures may be necessary:
- Endoscopic treatments for esophageal varices
- Paracentesis to remove excess abdominal fluid
- Transjugular intrahepatic portosystemic shunt (TIPS) for severe portal hypertension
Liver Transplantation
For patients with end-stage liver disease or severe complications, liver transplantation may be the best option. This procedure involves replacing the damaged liver with a healthy liver from a donor. While liver transplantation can be life-saving, it comes with its own set of challenges, including the need for lifelong immunosuppressive medications.
Preventing Cirrhosis: Strategies for Liver Health
Can cirrhosis be prevented? While not all cases of cirrhosis can be prevented, many risk factors are modifiable. Here are some strategies to promote liver health and reduce the risk of developing cirrhosis:

- Limit alcohol consumption or abstain entirely
- Maintain a healthy weight through diet and exercise
- Get vaccinated against hepatitis B
- Practice safe sex and avoid sharing needles to prevent hepatitis B and C transmission
- Use medications as directed and avoid unnecessary over-the-counter drugs
- Protect yourself from exposure to toxic chemicals
- Manage underlying conditions such as diabetes and high cholesterol
- Undergo regular health check-ups to detect liver problems early
Living with Cirrhosis: Coping Strategies and Support
A cirrhosis diagnosis can be challenging, but with proper management and support, many patients can maintain a good quality of life. Here are some coping strategies for individuals living with cirrhosis:
- Educate yourself about the condition and treatment options
- Adhere to your treatment plan and attend regular check-ups
- Join support groups to connect with others facing similar challenges
- Manage stress through relaxation techniques or counseling
- Communicate openly with your healthcare team about any concerns or new symptoms
- Plan for the future, including advance care planning if necessary
Living with cirrhosis may require significant lifestyle adjustments, but many patients find that these changes can lead to improved overall health and well-being.
Research and Future Directions in Cirrhosis Treatment
What advancements are being made in cirrhosis treatment? Ongoing research in the field of hepatology continues to uncover new potential treatments and management strategies for cirrhosis. Some areas of active investigation include:
- Antifibrotic therapies to slow or reverse liver scarring
- Gene therapies for inherited liver diseases
- Improved antiviral treatments for hepatitis B and C
- Novel approaches to managing complications like portal hypertension
- Advancements in liver transplantation techniques and immunosuppression
- Development of artificial liver support devices
- Stem cell therapies for liver regeneration
While many of these approaches are still in the experimental stages, they offer hope for improved outcomes for cirrhosis patients in the future.
In conclusion, cirrhosis is a complex and potentially severe liver condition that requires careful management and ongoing medical attention. By understanding the causes, symptoms, and available treatments, individuals can take proactive steps to protect their liver health and improve their prognosis if diagnosed with cirrhosis. Early detection and intervention are key to managing this progressive disease effectively.
Causes, symptoms, and treatments of liver scarring
Cirrhosis is a progressive condition where scar tissue gradually replaces healthy liver cells. In time, this can affect liver function.
Cirrhosis is a progressive disease that develops over many years. As scar tissue builds up, it can affect blood flow through the liver, leading to liver dysfunction.
Various factors can lead to liver damage and cirrhosis, such as:
- viral infections
- alcohol consumption
- toxins, including medications
- hereditary and genetic conditions
- some autoimmune diseases
- metabolic syndrome, including obesity, which leads to widespread inflammation
This article looks at why cirrhosis happens and how to recognize it, as well as the treatments, complications, and outlook.
With early cirrhosis, there are often no symptoms. But, as scar tissue accumulates, it undermines the liver’s ability to function properly.
A person may notice:
- fatigue
- nausea
- loss of appetite
- weight loss and loss of muscle mass
- patches of small, red blood vessels on the upper trunk and the palms of the hands
As the disease progresses, they may experience:
- swelling in the legs and abdomen due to a buildup of fluid
- an enlarged spleen
- infections
- confusion
- jaundice, where the whites of the eyes take on a yellow tinge
- dark-colored urine
- tarry stools
- itching
- internal bleeding
- low sex drive
In time, fibrous scar tissue replaces healthy liver tissue. Regenerative nodules may also form. These are lumps that appear as the liver tries to heal the damage.
Regenerative nodules may also form. These are lumps that appear as the liver tries to heal the damage.
Doctors grade cirrhosis in various ways, such as the Childs-Pugh score.
Using scores from various tests, it puts the liver into one of three categories:
- A: The liver is working well.
- B: There is moderate damage.
- C: Damage is advanced or severe.
The score helps give an idea of the person’s outlook. Category C, or end-stage liver disease, is potentially fatal.
Cirrhosis can also be either compensated or decompensated.
With compensated cirrhosis, the liver can function effectively despite the damage. People with compensated cirrhosis often have no symptoms.
With decompensated cirrhosis, the liver cannot function effectively, and symptoms may be noticeable.
Common causes of cirrhosis are:
- hepatitis, a viral infection
- long-term high alcohol consumption
- non-alcohol-related steatosis, a type of fatty liver disease
- exposure to toxins
- genetic diseases
Hepatitis
Globally, hepatitis B and C are the leading causes of cirrhosis.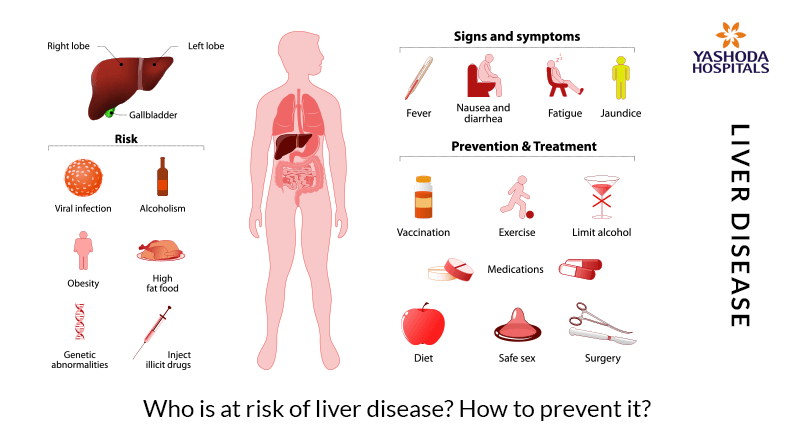 People can get either type after exposure to blood that contains the virus, for example, through needlestick injuries or sharing needles.
People can get either type after exposure to blood that contains the virus, for example, through needlestick injuries or sharing needles.
Vaccines can protect against hepatitis B but not hepatitis C.
In autoimmune hepatitis, the person has an autoimmune disease. In this type of disease, the immune system mistakenly attacks healthy cells. Sometimes, an autoimmune disease can affect the liver, leading to hepatitis and cirrhosis.
Alcohol-related fatty liver disease
The liver breaks down toxins, including alcohol. But, if toxin levels are too high, the liver will be unable to process them effectively, and damage to liver cells will result.
There are three stages of alcohol-related liver disease:
- Alcohol-related fatty liver or steatosis: Small fat droplets accumulate in the liver.
- Alcohol-related hepatitis: There is inflammation in the liver cells, causing swelling. At this stage, stopping alcohol consumption may repair the liver.
- Cirrhosis: Irreversible damage can lead to potentially life threatening complications.

People who consume 30–50 grams (g) of alcohol per day for 5 years have a risk of alcohol-related liver disease. Males who consume more than 21 units per week and females who consume more than 14 units per week are at risk of steatosis due to alcohol consumption.
In the U.S., alcohol consumption is the leading cause of liver disease.
Non-alcohol-related fatty liver disease
Doctors diagnose non-alcohol-related fatty liver disease (NAFLD) when fat accumulates in over 5% of liver cells, and there is no other explanation.
NAFLD included non-alcohol-related fatty liver (NAFL) and non-alcohol-related steatosis (NASH). In NAFL, there are fatty deposits. In NASH, inflammation and cell damage are also present.
NAFLD is more likely to affect people with:
- metabolic syndrome, including obesity, diabetes, high cholesterol, and high blood pressure
- polycystic ovary syndrome (PCOS)
- genetic conditions, such as Wilson’s disease, when copper accumulates in the liver and other parts of the body
- conditions involving a nutritional imbalance, such as kwashiorkor
Other conditions
Other diseases and conditions that can contribute to cirrhosis include:
- cystic fibrosis
- primary sclerosing cholangitis, or hardening and scarring of the bile ducts
- galactosemia, or inability to process sugars in milk
- schistosomiasis, a parasitic disease
- biliary atresia, which affects the formation of bile ducts before birth
- glycogen storage disease, when the body has problems storing and releasing the energy release that is vital for cell function
- hemochromatosis, when iron accumulates in the liver and other parts of the body
- Budd-Chiari syndrome, when blood clots in the hepatic vein lead to liver enlargement and the development of new blood vessels
- cancer of the bile ducts or pancreas, which can lead to blockages in the bile ducts
Symptoms rarely appear in the early stages, so diagnosis often occurs when testing for another condition or disease.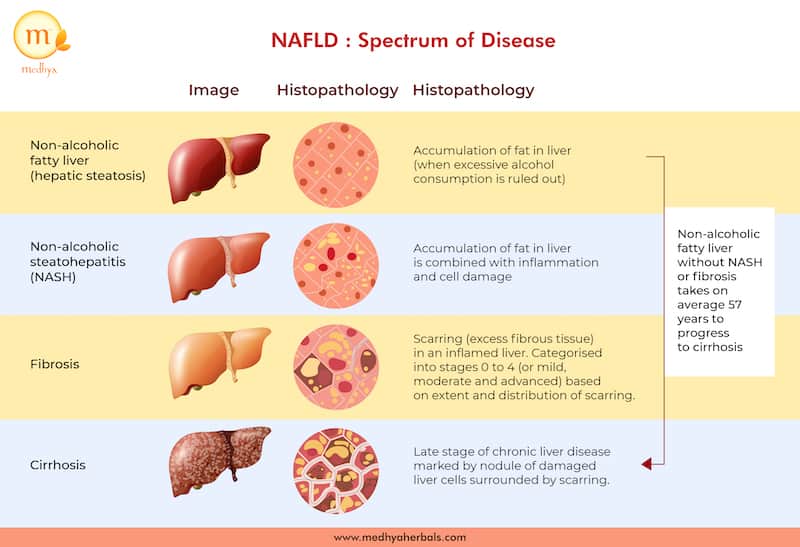
If a doctor suspects cirrhosis, they will:
- carry out a physical examination, including checking for swelling in the upper abdomen
- ask the person about their personal and family medical history
- ask about their lifestyle, including dietary habits and alcohol consumption
They may also recommend the following tests:
- blood tests to check liver function
- imaging tests such as an ultrasound, CT, or MRI scan to look for signs of enlargement, scarring, or nodules
- a biopsy, which takes a tissue sample for testing in a laboratory
Cirrhosis can affect a range of body organs, including the:
- gastrointestinal system
- blood and cardiovascular system
- kidneys
- lungs
- skin and nails
- hormones
It can lead to several other conditions, some of which are life threatening.
Ascites or edema
Ascites is a buildup of fluid in the abdomen, and edema is a buildup of fluid in the legs. A low-salt diet and diuretics, or water pills, can help manage fluid levels. In severe cases, a doctor may need to drain the fluid repeatedly.
A low-salt diet and diuretics, or water pills, can help manage fluid levels. In severe cases, a doctor may need to drain the fluid repeatedly.
Varices and portal hypertension
Large, swollen veins develop in the esophagus and stomach. They can put pressure on a blood vessel called the portal vein, which carries blood from the spleen and bowel to the liver, leading to portal hypertension. Varices can rupture, causing bleeding and clots.
Hepatic encephalopathy
This refers to high levels of toxins in the blood where the liver can no longer filter them effectively.
Hepatocellular carcinoma
This is the most common type of liver cancer and can result from cirrhosis due to hepatitis B or C infection. Research from 2013 suggests it is becoming more common in the U.S. and globally and has a high fatality rate.
Hepatopulmonary syndrome
Hepatopulmonary syndrome (HPS) refers to a combination of:
- liver disease
- dilated blood vessels in the lungs
- problems with the exchange of gases in the lungs
HPS is a potentially life threatening condition.
Coagulation disorders
Cirrhosis can cause problems with blood clotting, leading to bleeds and clots that can sometimes be fatal.
There is no cure for cirrhosis, and it can be life threatening.
How long a person will survive with cirrhosis depends on various factors, including:
- the cause
- the severity of the scarring
- their age and overall health
- how they treat the condition
As the disease progresses, the prognosis worsens. People with compensated cirrhosis, when the liver can still function, have a 47% chance of surviving another 10 years compared with people who do not have cirrhosis. Once cirrhosis starts to affect liver function, the chance of surviving another 10 years falls to around 16%.
People who consumed alcohol before their diagnosis and then quit have a better outlook, especially if they stopped in the earlier stages.
In the United States, 4.5 million people, or 1.8% of the adult population, have liver disease. Cirrhosis accounts for 15.8 deaths in every 100,000.
Cirrhosis accounts for 15.8 deaths in every 100,000.
Cirrhosis is not always avoidable, but some tips can help lower the risk:
- Follow a varied diet that is low in processed foods and added fats.
- Keep within the recommended guidelines for the consumption of alcohol.
- Use diet and exercise to maintain a suitable weight and avoid obesity.
- Use a condom during sex to lower the risk of hepatitis.
- Never share needles and take care when dealing with blood.
- Avoid alcohol if any stage of liver disease is present.
- Ask about vaccinations for hepatitis B if you are at risk.
Here are some answers to questions people often ask about cirrhosis.
What are the stages of cirrhosis?
There are different ways to describe the progression of cirrhosis. The Child-Pugh system describes three stages, based on test results.
In this system:
- Stage A: The liver is working well.
- Stage B: There some impact on liver function.

- Stage C: Liver function is severely affected.
Doctors also refer to compensated cirrhosis, where damage is present, but the liver is functioning; and decompensated cirrhosis, where damage affects liver function.
Can a person survive cirrhosis?
The outlook will depend on various factors, including the cause of cirrhosis and the stage at diagnosis.
A person who receives a diagnosis in the early stage can continue to live a healthy life, but they may need to take measures, such as avoiding alcohol and maintaining a suitable weight. Once cirrhosis starts to affect liver function, the impact on a person’s outlook becomes more severe.
What are the early warning signs of cirrhosis?
Often, a person will not notice any symptoms until a later stage, when cirrhosis begins to affect liver function.
As it progresses, cirrhosis can cause a wide range of symptoms, including fatigue, nausea, low appetite, jaundice, swelling, and itchy skin.
Cirrhosis results when tissue damage causes scarring in the liver. Possible causes include a hepatitis infection, high consumption of alcohol, some genetic conditions, and inflammation that occurs with obesity and metabolic disorder.
In the early stages, damage is present and scarring start to appear, but the liver continues to function. In time, scarring becomes widespread. Eventually, the liver is unable to function.
Some ways of reducing the risk include limiting alcohol consumption, maintaining a moderate body weight, and taking measures to prevent infection with hepatitis B and C.
For people with early-stage cirrhosis, lifestyle changes — such as avoiding alcohol consumption, protecting against infection, and managing body weight — can improve their outlook.
When cirrhosis starts to affect liver function, it can become life threatening. For this reason, it is best to take measures to prevent cirrhosis where possible.
Read this article in Spanish.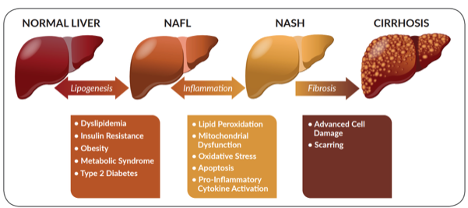
Infusion of Anti-Fibrotic Vascular Cells to Cure Liver Cirrhosis | Newsroom
October 23, 2017
Portal Venogram. Imaging-guided catheter-directed intra-portal infusion of endothelial cell therapy. Drs. Kyungmouk Steve Lee and David C. Madoff, Weill Cornell Medicine.
A new therapy that uses blood-vessel-lining cells to regenerate damaged tissue has the potential to treat liver cirrhosis, Weill Cornell Medicine scientists demonstrate in new research.
The small-scale animal study, published in the October issue of Radiology, was a test of the basic feasibility of the cell delivery technique and not designed to prove safety or effectiveness. Still, the researchers found that the interventional therapy—a single, image-guided infusion of blood vessel cells called endothelial cells derived from liver tissue—was followed by an apparent lessening of liver damage in pigs that had liver cirrhosis before the treatment. If the scientists can replicate the findings in humans, it could offer an alternative treatment for liver cirrhosis, which affects more than 600,000 people in the United States alone.
“There was a reduction in markers of cirrhosis and related injury to structures in the liver, and we didn’t see any bleeding, clotting or other harm from the technique itself,” said first author Dr. Kyungmouk Steve Lee, an assistant professor of radiology at Weill Cornell Medicine and an interventional radiologist at NewYork-Presbyterian/Weill Cornell Medical Center.
Reduction of liver fibrosis after endothelial cell therapy. These images show improvement in liver fibrosis after imaging-guided catheter-directed intra-portal infusion of endothelial cells in a cirrhotic model. Image credit: Drs. Kyungmouk Steve Lee and David C. Madoff, Weill Cornell Medicine
Liver cirrhosis, which features chronic inflammation and fibrosis—an accumulation of fibrous, scar-like tissue—is most commonly caused by chronic heavy drinking and chronic viral infection by the Hepatitis B and C viruses. Most patients are unaware of their condition, which typically progresses to liver failure or liver cancer, and the only truly effective treatment is a liver transplant. “The difference in the appearance of liver cells in the treated versus untreated animals was impressive,” said senior author Dr. David Madoff, vice chair for academic affairs in the Department of Radiology and a professor of radiology at Weill Cornell Medicine, and an interventional radiologist at NewYork-Presbyterian/Weill Cornell Medical Center.
“The difference in the appearance of liver cells in the treated versus untreated animals was impressive,” said senior author Dr. David Madoff, vice chair for academic affairs in the Department of Radiology and a professor of radiology at Weill Cornell Medicine, and an interventional radiologist at NewYork-Presbyterian/Weill Cornell Medical Center.
Scientists have been exploring the potential of stem cell and other cell therapies to regenerate fibrosis-damaged organs including cirrhotic livers. One problem with this strategy is that inflammatory and other disease processes within a damaged organ tend to create an inhospitable environment—or “niche”—for transplanted cells and even for resident stem cells. Study co-author Dr. Shahin Rafii and colleagues have shown in prior work, however, that vessel-lining endothelial cells can produce special organ-specific growth factors, known as angiocrine factors, that restore a healthier niche and promote regeneration without provoking scarring.
“In the case of liver cirrhosis, blood vessels in the liver are damaged and fail to supply angiocrine factors that promote regeneration. So the idea underlying this endothelial cell therapy is to rejuvenate that vascular niche,” said Dr. Rafii, director of the Ansary Stem Cell Institute, the Arthur B. Belfer Professor of Genetic Medicine and chief of the Division of Regenerative Medicine at Weill Cornell Medicine. Dr. Rafii is a co-founder and consultant with equity in Angiocrine Bioscence, a cellular therapy company. “Accordingly, the remaining hepatocyte progenitors in the liver can get the proper signals from angiocrine factors they need to suppress fibrosis and regenerate liver tissue.”
For the study, the investigators harvested small quantities of endothelial cells from the liver vessels of eight pigs, and multiplied the cells to large quantities in the laboratory. After inducing cirrhosis in each pig’s liver, the researchers then treated half of the pigs in an interventional radiology suite by infusing the liver-specific endothelial cells into a large vein that runs into the liver, using a small catheter inserted through the skin and guided by ultrasound and live x-ray imaging.
Although the number of pigs in the study wasn’t large enough to determine the therapeutic effectiveness of the technique, examination of the pigs’ livers three weeks after treatment revealed some striking differences between treated and untreated animals. When the investigators examined samples of cells and tissues taken from the treated pigs’ livers under the microscope, they found that the organ appeared much more like the livers of healthy pigs, in contrast to the untreated livers.
“These were very encouraging results,” said Dr. Madoff, who is a member of the clinical advisory board with equity in Angiocrine.
The Weill Cornell Medicine researchers now hope to conduct larger trials of the endothelial cell therapy in pigs and, if they are successful, progress to clinical trials in humans. In principle, the investigators said, the cell therapy could be used to treat not just cirrhosis but other forms of liver injury as well.
Dr. David Madoff, Dr. Kyungmouk Steve Lee, Dr. Shahin Rafii, Research, News from WCM
Shahin Rafii, Research, News from WCM
The effect of alcohol on the liver | Essentiale
- home
- Articles
- Effect of alcohol on the liver
How much do you think Russians drink and how does this domestic “tradition” compare with the behavior of residents of other countries?
Over the past 5 years, Russians have begun to drink less (from 15.1 liters to 12.8 liters of absolute alcohol per person per year).
But what is 12.8 liters – is it a lot or a little? It turns out there are quite a few. If you look at the statistics of 32 European countries, Russia is in 8th place (2017 data). I’m glad it’s not the first. However, in terms of inclinations towards a healthy lifestyle, you will agree that we still have room to “grow”.
If you look at the statistics of 32 European countries, Russia is in 8th place (2017 data). I’m glad it’s not the first. However, in terms of inclinations towards a healthy lifestyle, you will agree that we still have room to “grow”.
Who consumes the most alcohol in Europe? It turned out that these are residents of Lithuania, taking 18.2 liters of alcohol per year. In terms of 0.5 l bottles of beer with a strength of 5%, this is 728 bottles (or a liter of beer every day). 1
It is no secret that the abuse of strong drinks is a harmful practice. And the first organ to take a hit, (this is not news!), Is the liver. Alcoholic liver disease is the name of the disease. Ask what happens in the liver in this disease?
Men and women who consume more than 40 and 20 grams of ethanol daily, respectively, are at risk of developing fatty liver disease. 2
What is fatty liver disease?
Depending on the amount of alcohol consumed, it takes from 5 to 10-12 years to develop diseases.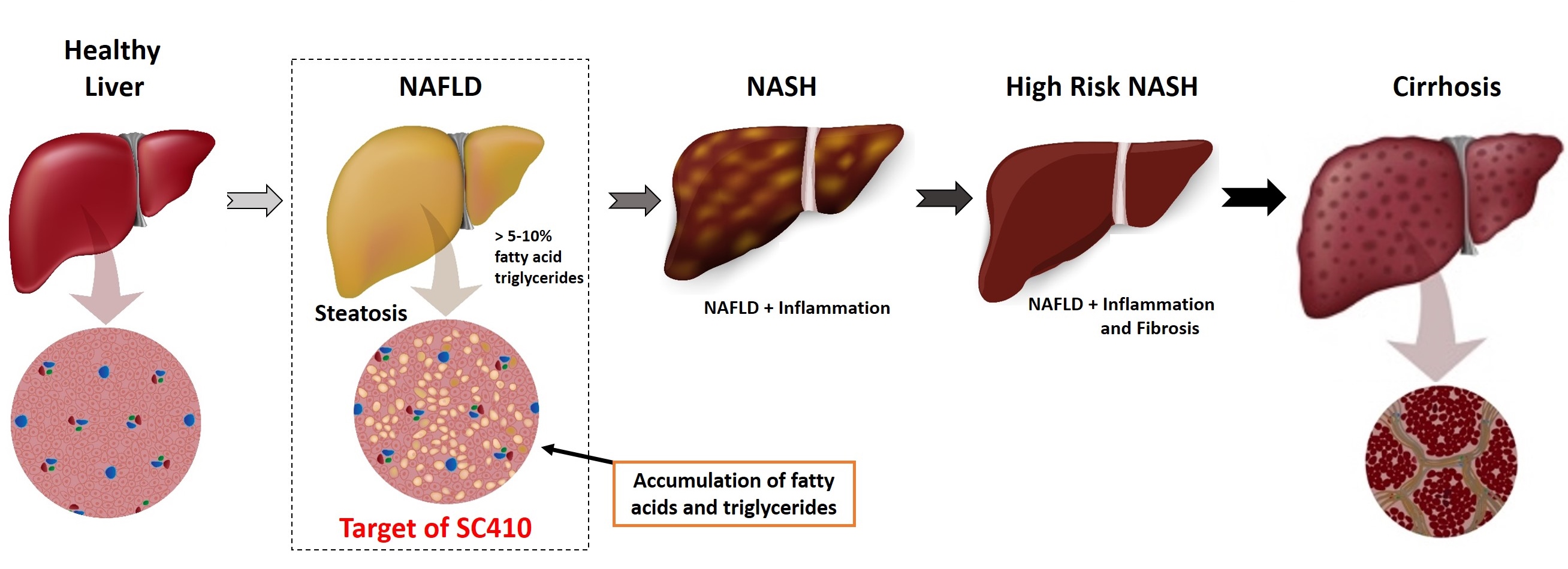 Under the influence of alcohol, hepatocytes are damaged and die, redox processes are disturbed, the toxic breakdown product of alcohol, acetaldehyde, accumulates, inflammation develops, and the replacement of liver cells with connective tissue begins. The liver increases in size, its function may be impaired. Synthesis of connective tissue marks fibrosis, which in turn evolves into cirrhosis of the liver – the main reason for the transplantation of this organ. 3
Under the influence of alcohol, hepatocytes are damaged and die, redox processes are disturbed, the toxic breakdown product of alcohol, acetaldehyde, accumulates, inflammation develops, and the replacement of liver cells with connective tissue begins. The liver increases in size, its function may be impaired. Synthesis of connective tissue marks fibrosis, which in turn evolves into cirrhosis of the liver – the main reason for the transplantation of this organ. 3
How to restore the liver after alcohol?
Questions that sooner or later confront every person who abuses alcohol:
• How to maintain health?
• What if you already have a lot of experience behind you?
• Are the effects reversible?
First you need to stop or limit the amount of alcohol consumed. As soon as possible. The treatment of fatty liver disease is a process that requires lifestyle changes, discipline, perseverance and work with a doctor, following his recommendations. 4
4
If you completely avoid alcohol, have a balanced diet, regularly see a doctor and follow his recommendations in the early stages of the disease, the prognosis can be favorable. 5
Among the therapeutic possibilities is the use of essential phospholipids. Essential phospholipids are incorporated into damaged liver cell membranes and promote their regeneration. This action is directed against inflammation and helps to delay the formation of connective tissue 6 . However, it is important to remember that the treatment of fatty liver disease requires an integrated approach with lifestyle changes with regular monitoring and coordination of therapy with a doctor.
you may also find
useful
Influence
alcohol on the liver
Men and women,
daily consumption of more than 40 and 20 grams of ethanol, respectively, are at risk
development of alcoholic fatty liver disease
Chronic
viral hepatitis
Chronic viral
Hepatitis is an infectious disease that can be caused by a number of specific viruses.
Read more about the diagnosis in our material
Phospholipids
Phospholipids are
“building blocks” that make up liver cells. However, under the influence of negative
factors or against the background of liver diseases, the phospholipid balance may be disturbed …
World’s #1 Liver Treatment*
Ask for availability
*Based on sales for 2021 according to Nicholas Hall Europe LLC data for 2021 in 63 countries. The full text of the confirmation letter can be read on the official website of Essentiale ® Forte N. https://essentiale.ru/products/numberone
*Based on sales for 2021 according to Nicholas Hall Europe LLC data for 2021 in 63 countries. The full text of the confirmation letter can be read on the official website of Essentiale ® Forte N. https://essentiale.ru/products/numberone
https://essentiale.ru/products/numberone
Show sources
1.
http://www.eurocare.org/library/updates/lithuania_the_heaviest_drinking_country_in_the_world – – Accessed 02/20/2018.
2.
https://www.novayagazeta.ru/news/2016/05/20/121858-potreblenie-alkogolya-v-rossii-snizilos-na-tret – accessed on 20.02.2018.
3.
Diagnosis and treatment of non-alcoholic fatty liver disease Edited by Academician of the Russian Academy of Sciences, Professor V.
 T. Ivashkin Moscow 2015
T. Ivashkin Moscow 20154.
V.T. Ivashkin et al. Clinical guidelines of the Russian Society for the Study of the Liver for the management of adult patients with alcoholic liver disease, RJGGK, 2017;27(6), 20-40.
5.
S Dam-Larsen et al, Long term prognosis of fatty liver: risk of chronic liver disease and death, Gut. May 2004; 53(5): 750–755.
6.
Instructions for medical use of the drug Essentiale Forte N (Reg.
 ud. P N011496/01).
ud. P N011496/01).MAT-RU-2200075-1.0-02/2022
what it is, how it is used
The state of the liver plays a vital role in human health. This body weighing more than a kilogram performs many tasks. In one liver cell, hepatocyte, about 500 different biochemical processes take place 1 . In the liver, the breakdown and / or detoxification of harmful substances is carried out, as well as their removal from the body. In addition, the organ synthesizes the most important components of biological membranes – phospholipids 2 .
What is a cell membrane?
Cells are the basic building blocks of the human body. They, in turn, cannot exist without fats and phospholipids, which form the outer membrane, the “wall” of the cell, which holds the cytoplasm inside it.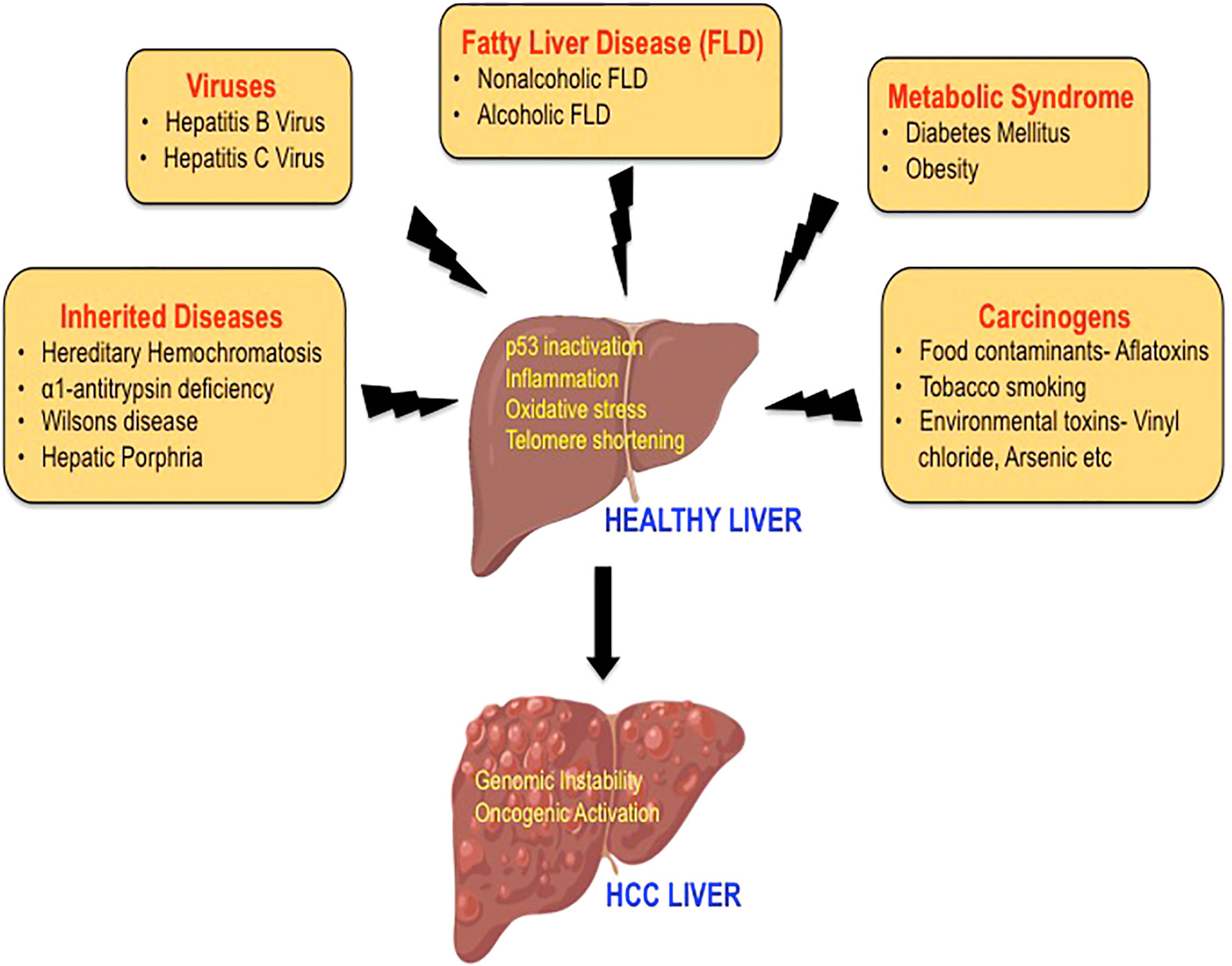 The membrane consists of two layers of phospholipids, which consist of a hydrophilic “head”, attracted to water, and a hydrophobic, that is, water-resistant “tail”. The “heads” of the two rows of phospholipids face outwards, towards the liquid, and the “tails” are fastened together, providing high strength to the cell walls 2 .
The membrane consists of two layers of phospholipids, which consist of a hydrophilic “head”, attracted to water, and a hydrophobic, that is, water-resistant “tail”. The “heads” of the two rows of phospholipids face outwards, towards the liquid, and the “tails” are fastened together, providing high strength to the cell walls 2 .
Phospholipids perform a structural function, supporting the cell scaffold, participate in molecular transport, enzymatic and other equally important processes. Any disruption to their activities can have the most serious consequences 2 .
Hepatocytes are the “bricks” of the liver
Liver cells, hepatocytes, make up to 70 – 85% of the organ mass. They are primarily responsible for the activity of the liver, participating in processes such as:
- Protein synthesis and storage
- Breakdown of carbohydrates
- Synthesis of cholesterol, bile salts and phospholipids
- Detoxification, breakdown and excretion of substances
- Initiation of education and, in fact, the production of bile.

The cell wall of hepatocytes, like any other cells, consists of phospholipids, which ensure its full functioning. However, unfortunately, she is vulnerable. The impact of negative factors, for example, certain drugs, toxic substances, and especially alcohol, and even an unbalanced diet, leads to disruption of intracellular metabolism and death of hepatocytes. How various liver diseases develop0019 1 .
When does the liver “naughty”?
Liver problems are primarily associated with chronic intoxication, which, in turn, can be caused by various diseases and conditions. These include chronic alcohol intake, type 2 diabetes mellitus, environmental intoxication, “chemization” of food and everyday life, the adverse effects of drugs, and other factors. All of them contribute to the development of oxidative stress due to disruption of the adequate functioning of antioxidant mechanisms. Gradually, against the background of chronic negative influence, the destruction of cell membranes, proteins and DNA occurs, the work of the cell is disrupted.
The result of long-term intoxication is a triad: lipid peroxidation (oxidative degradation occurring under the action of free radicals), accumulation of more than 5% of fat in the liver cells of the organ mass (steatosis) and chronic inflammation 1 .
Essential means necessary
Essential phospholipids (EPL) are widely used to treat liver damage of various origins. Their fundamental difference from conventional phospholipids is the presence of an additional molecule of linoleic acid. This allows EPL to easily compensate for defects in the cell membrane, which increases its flexibility and normalizes functions. It is the presence of linoleic acid that is considered the most important difference between EPL and classical phospholipids, such as lecithin, which underlies the therapeutic benefits of essential phospholipids 2 .
In a sense, the appointment of EPL can be called membrane therapy, because their activity is associated precisely with cell walls.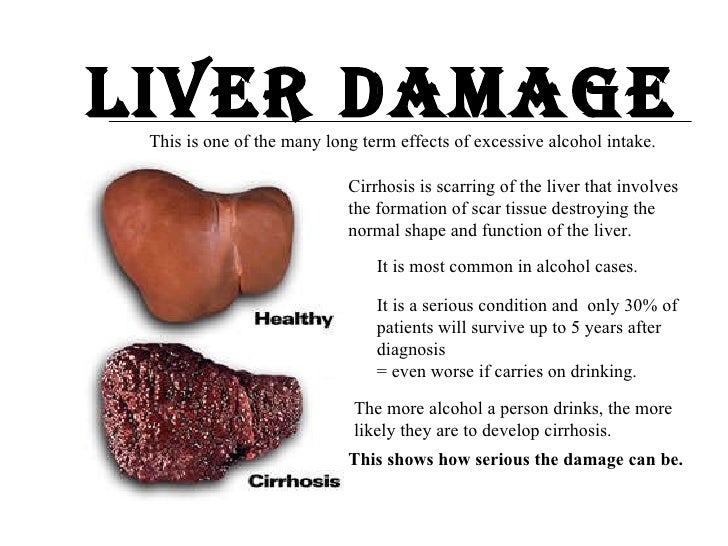 Such treatment became possible thanks to soybeans, from which the valuable substance 3 is obtained.
Such treatment became possible thanks to soybeans, from which the valuable substance 3 is obtained.
Soybeans: from ancient times to the present day
An annual plant of the legume family has been used by humans for thousands of years. There are mentions of him in the books of the time of Emperor Sheng Nung, who reigned in 2838 BC 1 . Then soybeans were considered one of the five “holy grains”, without which life on earth was impossible.
Today, about 800 species of soybeans are known. They contain 35 – 40% proteins, 20 – 30% carbohydrates, 5 – 10% related substances (vitamins, triterpene saponins, flavonoids, etc.), as well as 12 – 18% fats. The oils that make up the beans are 90 – 95% composed of fatty acid glycerides, in particular, oleic and linoleic. In the process of processing crude oil, it is possible to obtain 30-45% of soy lecithin (phosphatidylcholine), which is the “target product” used in the pharmaceutical industry to create drugs that exhibit a hepatoprotective effect.
Phosphatidylcholines in action
Derived from soybeans, phosphatidylcholines are a typical lipid bilayer consisting of a hydrophilic head and a hydrophobic tail, and are a major structural component of biological membranes. Essential phospholipids easily replace endogenous, that is, “own” phospholipids of the body, which were damaged for one reason or another, integrating into the cell membrane. At the same time, EPL can enter the body both orally, in the form of solid dosage forms (capsules), and intravenously, with a highly purified injection solution 4 .
By the way, the name “essential phospholipids” is registered only for preparations containing at least 75% phosphatylcholine. An example of a drug containing high concentrations of EFL is Essentiale Forte N. 1 capsule of Essentiale Forte N contains 76% phosphatidylcholine 3 .
Membrane protection!
Incorporation of essential phospholipids into damaged hepatocyte membranes ensures the restoration of normal membrane structures, which in turn leads to a complex therapeutic effect. What is the effect of EFL? First of all, they exhibit protective (protective) and regenerative properties in relation to liver cells 1 . In this case, liver damage can be caused by a variety of factors, including toxic, inflammatory, allergic, metabolic and immunological reactions 1 .
What is the effect of EFL? First of all, they exhibit protective (protective) and regenerative properties in relation to liver cells 1 . In this case, liver damage can be caused by a variety of factors, including toxic, inflammatory, allergic, metabolic and immunological reactions 1 .
It has been proven that EPL protect hepatocytes from damage associated with the action of various chemicals, alcohol, drugs, cytostatics used to treat cancer, ionizing radiation, etc. 1 .
EPL and polyunsaturated fatty acids
The mechanism of action of EPL is similar to the action of omega 3-6 polyunsaturated fatty acids (PUFAs), since the former are essentially the natural form of the existence of the latter. Omega 3-6-PUFAs are essential fats that reduce the risk of a number of diseases, including cardiovascular disease and diabetes. They are not synthesized in the body and must be consumed daily in the amount of 2 g of omega-3 and 6 grams of omega-6 PUFAs.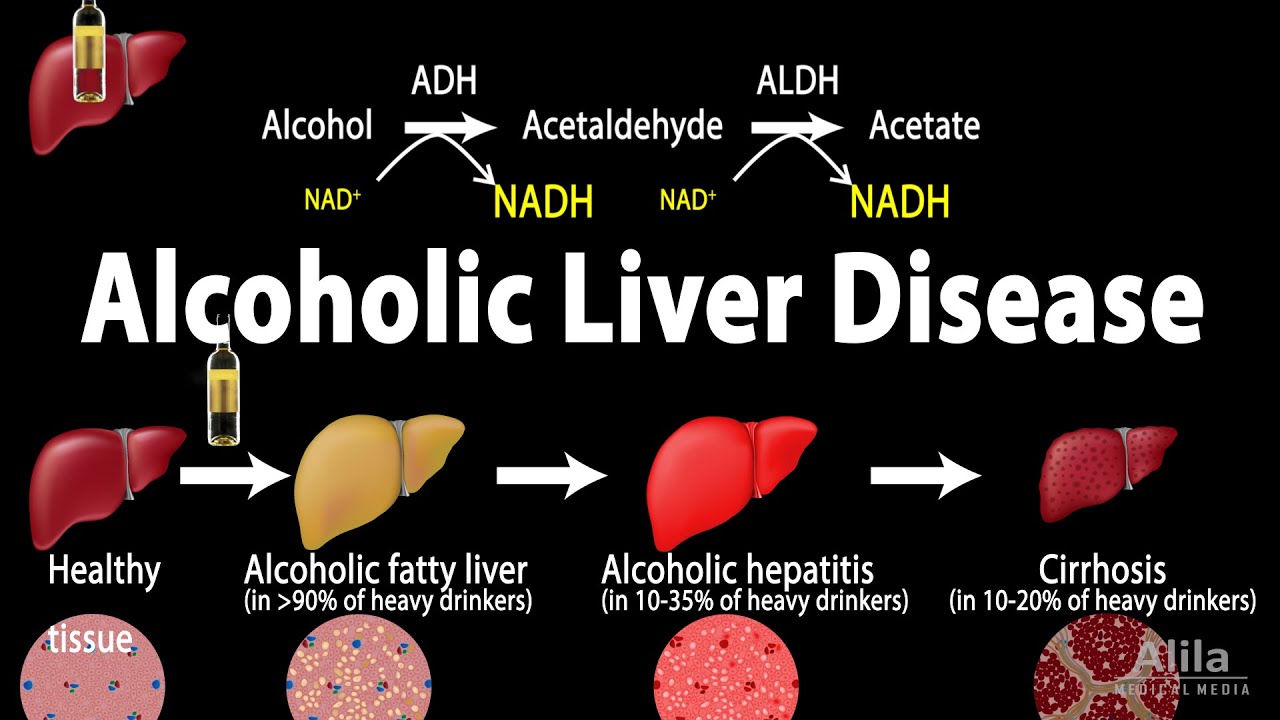 However, red varieties of fish, walnuts, vegetable oils, soybeans, which contain a large amount of these acids, are high in calories, which limits their use 5 .
However, red varieties of fish, walnuts, vegetable oils, soybeans, which contain a large amount of these acids, are high in calories, which limits their use 5 .
Preparations containing EPL, such as Essentiale forte N, can be widely used to compensate for the dietary deficiency of polyunsaturated fatty acids without increasing the caloric content of the diet 6 . And what an important role they play in diseases associated with impaired fat metabolism!
Cholesterol – stop!
Essential phospholipids are involved in the transport of cholesterol in plasma and tissues, as well as the formation of high and low density lipoproteins (HDL and LDL) 7 . Recall that it is with an increase in the level of LDL and triglycerides and a decrease in the content of HDL that one of the most dangerous diseases, atherosclerosis, is associated.
EPL provide the so-called systemic mobilization of cholesterol and its utilization at all stages of metabolism due to a number of processes, including:
- Increased LDL synthesis and mobilization of cholesterol from blood plasma
- Hepatocyte uptake of LDL
- Increased secretion of cholesterol, phospholipids and fats into bile, which consequently reduces their accumulation in the liver.
 8
8
Bile contains bile acids (about 70%) and EPL (phosphatidylcholine, makes up 22% of bile) 9 . In healthy people, EPLs provide cholesterol solubility. If the ratio of bile acids and EPL is disturbed, cholesterol crystals can precipitate, as a result of which cholelithiasis (GSD) develops.
Gallbladder stones: easier to prevent than to treat
It is known that up to 90% of gallstones are predominantly cholesterol, consisting of at least 70% of cholesterol 10 . An increase in the release of cholesterol into bile, leading to stone formation, may occur due to an imbalance in the diet and its saturation with animal fats. Environmental pollution is also considered an important risk factor for cholelithiasis, leading to chronic intoxication of the body and, as a result, an increase in the need for antioxidants and EPL, which are necessary to bind toxic substances. If the reserves of EPL and antioxidants are not replenished, the function of cell membranes is impaired, and the body begins to accumulate cholesterol in order to maintain the structure of the cell wall, triggering the process of stone formation 11, 12 .
The group of increased risk of gallstone disease includes people who abuse alcohol. The prophylactic administration of EPL preparations to those who experience a high load of toxins or alcohol compensates for the deficiency of phospholipids and prevents stone formation 12 .
Non-alcoholic fatty liver disease
An important effect of EPL is achieved due to their ability to improve lipid metabolism. It is especially relevant in the treatment of non-alcoholic fatty liver disease (NAFLD), which occurs due to excessive accumulation of fat in the body. It should be noted that the prevalence of this disease is constantly growing, including among children and adolescents, especially those living in cities 6 . In Russia, only in general practice patients, the prevalence of NAFLD reaches 27% 6 !
Against the background of the disease, a complex of pathological disorders develops, including a decrease in the sensitivity of tissues to insulin, an increase in the content of insulin in the blood. The mass of visceral fat increases, which leads to obesity and arterial hypertension. Patients often develop type 2 diabetes mellitus and hyperlipidemia – an increase in the level of cholesterol and triglycerides in the blood. People suffering from NAFLD should control their calorie intake, minimize trans fats, cholesterol and increase their intake of polyunsaturated lipids (more than 10 grams per day) 7 . Due to the high calorie content of products containing PUFAs, EPL preparations, which have a pronounced therapeutic effect, are of particular importance.
The mass of visceral fat increases, which leads to obesity and arterial hypertension. Patients often develop type 2 diabetes mellitus and hyperlipidemia – an increase in the level of cholesterol and triglycerides in the blood. People suffering from NAFLD should control their calorie intake, minimize trans fats, cholesterol and increase their intake of polyunsaturated lipids (more than 10 grams per day) 7 . Due to the high calorie content of products containing PUFAs, EPL preparations, which have a pronounced therapeutic effect, are of particular importance.
With fatty infiltration of hepatocytes, which is observed in patients with NAFLD, preparations containing essential phospholipids help to reduce 13 cell mitochondrial stress caused by excess fatty acids, reduce the severity of the inflammatory process and normalize fat metabolism due to the correction of dyslipidemia 14 . The appointment of these drugs improves the lipid composition of the blood, indicators of lipid peroxidation and restore the antioxidant defense system as a whole 6 .
It has been clinically proven that essential phospholipids, for example, as part of Essentiale forte N, improve the course and prognosis of fatty liver in NAFLD, increase tissue sensitivity to insulin, normalize the lipid profile (that is, help reduce the level of “bad” cholesterol and triglycerides ) and also reduce the severity of symptoms of digestive disorders.
Alcohol test
An equally important indication for essential phospholipids is alcoholic liver disease (ALD). People who take 40-80 ml of pure ethanol daily for 4-6 years are at high risk of developing the disease 15 . Alcohol is rich in “light” carbohydrate calories, which gradually cause fatty degeneration of internal organs. In addition, it contributes to the development of circulatory disorders of the body. In chronic alcohol intoxication against the background of oxidative stress, hepatocyte necrosis occurs, a chronic inflammatory process and liver fibrosis develop. The mechanism of development of the latter is largely due to the activation of the so-called stellate cells.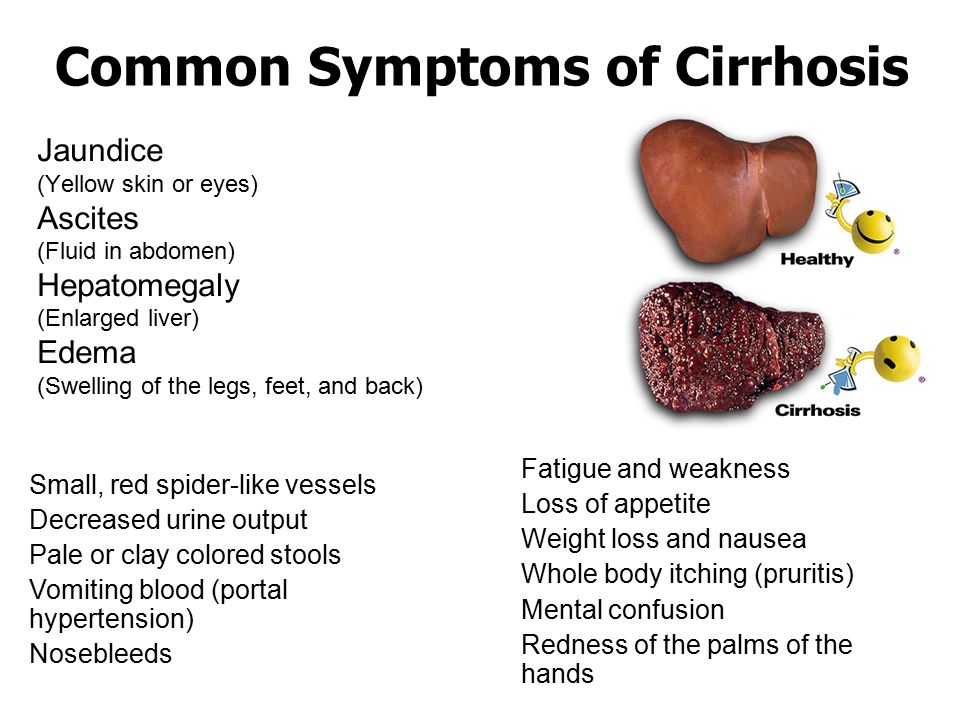



 T. Ivashkin Moscow 2015
T. Ivashkin Moscow 2015 ud. P N011496/01).
ud. P N011496/01).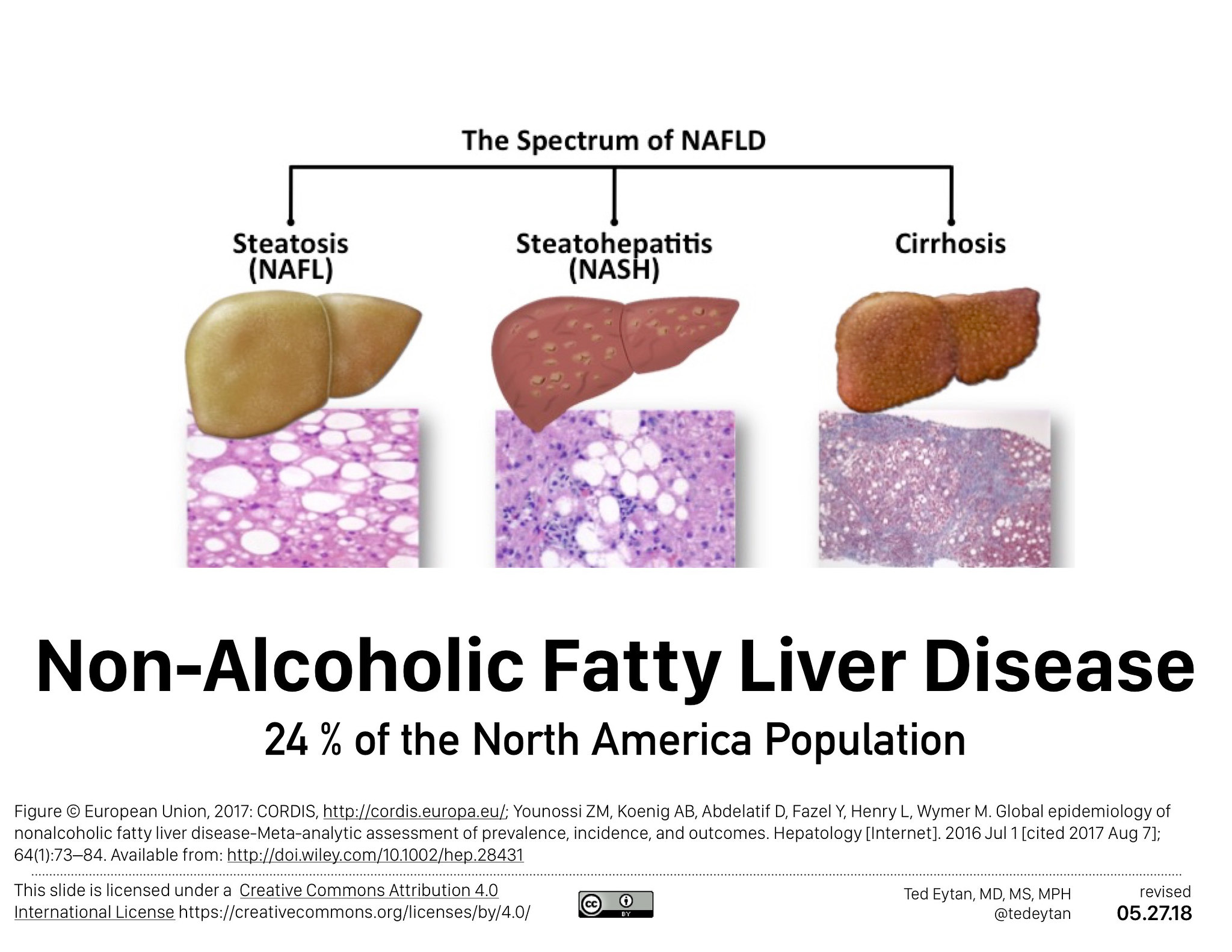
 8
8