Can tramadol cause headache. Tramadol Side Effects: Understanding Headaches and Other Common Reactions
Can tramadol cause headaches. What are the most common side effects of tramadol. How to manage tramadol-induced headaches. What are the serious side effects of tramadol that require immediate medical attention.
Common Side Effects of Tramadol: What to Expect
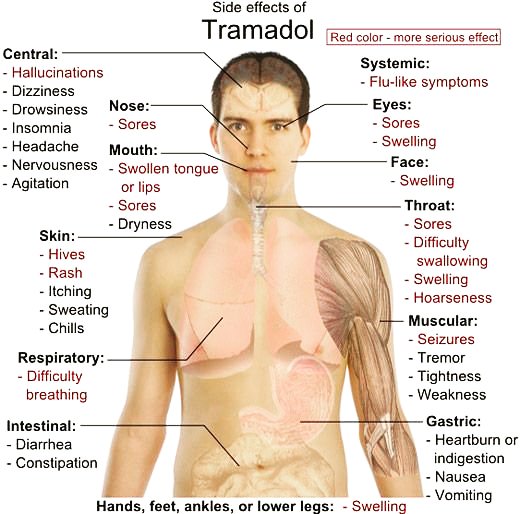
Tramadol, like all medications, can cause side effects in some individuals. While not everyone experiences adverse reactions, it’s crucial to be aware of potential issues that may arise. The most common side effects of tramadol occur in more than 1 in 100 people and include:
- Headaches
- Feeling sleepy, tired, dizzy, or “spaced out”
- Nausea or vomiting
- Constipation
- Dry mouth
- Excessive sweating
- Low energy
It’s important to note that very common side effects, occurring in more than 1 in 10 people, include feeling sick and dizzy. If you experience any of these side effects and they persist or become bothersome, it’s advisable to consult your doctor or pharmacist.

Tramadol and Headaches: Causes and Management
Headaches are a common side effect of tramadol use. They typically occur during the initial stages of treatment and often subside within the first week. How can you manage tramadol-induced headaches?
- Ensure adequate rest and hydration
- Avoid alcohol consumption while taking tramadol
- Consider over-the-counter painkillers (consult a pharmacist for recommendations)
If headaches persist beyond a week or become severe, it’s crucial to inform your doctor. They may need to adjust your dosage or consider alternative pain management options.
Can tramadol cause chronic headaches?
While tramadol can cause headaches as a side effect, chronic headaches are not typically associated with its use. If you experience persistent headaches while taking tramadol, it’s essential to consult your healthcare provider to rule out other underlying causes or potential medication interactions.
Dealing with Nausea and Vomiting from Tramadol
Nausea and vomiting are common side effects of tramadol that can be particularly distressing. To manage these symptoms:

- Stick to simple, bland meals and avoid rich or spicy foods
- Try taking tramadol after eating a meal or snack
- Stay hydrated by sipping water frequently
- Consult a pharmacist if you show signs of dehydration
If nausea and vomiting persist, your doctor may prescribe anti-nausea medication or adjust your tramadol dosage. It’s important to note that severe vomiting or diarrhea lasting more than 24 hours may affect the efficacy of contraceptive pills, so additional precautions may be necessary.
Does tramadol-induced nausea improve over time?
Many people find that nausea and vomiting associated with tramadol use improve as their body adjusts to the medication. This adaptation period typically lasts a few days to a week. However, if symptoms persist or worsen, it’s crucial to consult your healthcare provider for further guidance.
Managing Constipation: A Common Tramadol Side Effect
Constipation is a frequent side effect of tramadol use. To alleviate this issue:
- Increase fiber intake through fruits, vegetables, and cereals
- Drink plenty of water and non-alcoholic fluids
- Engage in gentle exercise, such as swimming or short walks
If lifestyle changes don’t provide relief, your doctor may recommend or prescribe laxatives or stool softeners to manage tramadol-induced constipation.

How long does tramadol-induced constipation typically last?
The duration of constipation caused by tramadol can vary among individuals. Some people may experience it throughout their treatment, while others find it improves over time. Consistent management through diet, hydration, and exercise can help alleviate symptoms. If constipation persists or causes significant discomfort, consult your healthcare provider for personalized advice.
Fatigue and Dizziness: Coping with Tramadol’s Sedative Effects
Feeling sleepy, tired, dizzy, or “spaced out” are common side effects of tramadol, particularly during the initial stages of treatment. These effects typically subside within one to two weeks as your body adjusts to the medication. To manage these symptoms:
- Avoid alcohol consumption, which can exacerbate feelings of fatigue
- Refrain from driving or operating heavy machinery until you know how tramadol affects you
- Ensure adequate rest and sleep
If fatigue and dizziness persist beyond two weeks or significantly impact your daily life, consult your doctor. They may need to adjust your dosage or consider alternative pain management strategies.

Can tramadol cause long-term fatigue?
While fatigue is a common side effect of tramadol, it typically improves as your body adjusts to the medication. Long-term fatigue is not a usual outcome of tramadol use. If you experience persistent fatigue that doesn’t improve over time, it’s important to discuss this with your healthcare provider, as it may indicate an underlying issue or the need for medication adjustment.
Serious Side Effects of Tramadol: When to Seek Medical Attention
While less common, tramadol can cause serious side effects in some individuals. It’s crucial to be aware of these potential reactions and seek immediate medical attention if they occur. Serious side effects of tramadol include:
- Severe dizziness, fatigue, and low energy (possible signs of low blood pressure)
- Hallucinations (seeing or hearing things that aren’t there)
- Confusion
- Extreme drowsiness
- Difficulty urinating or inability to urinate
- Seizures or fits
- Breathing difficulties or shallow breathing
If you experience any of these symptoms, contact your doctor immediately or call emergency services. In cases of severe allergic reactions (anaphylaxis), seek immediate emergency care.

How common are serious side effects from tramadol?
Serious side effects from tramadol are relatively rare, occurring in less than 1 in 100 people. However, their potential severity makes it crucial to be vigilant and seek prompt medical attention if any concerning symptoms arise. Your healthcare provider can help assess the risks and benefits of tramadol use based on your individual health profile.
Tramadol and Allergic Reactions: Recognizing Anaphylaxis
Although rare, severe allergic reactions (anaphylaxis) to tramadol can occur. It’s vital to recognize the signs of anaphylaxis and seek immediate emergency care if they develop. Symptoms of a severe allergic reaction to tramadol may include:
- Sudden swelling of the lips, mouth, throat, or tongue
- Rapid or difficult breathing
- Tightness in the throat or difficulty swallowing
- Skin, tongue, or lip discoloration (blue, grey, or pale)
- Sudden confusion, drowsiness, or dizziness
- Fainting or unresponsiveness
- In children: limpness, floppiness, or uncharacteristic unresponsiveness
A swollen, raised, itchy, blistered, or peeling rash may also accompany these symptoms. If you suspect anaphylaxis, call emergency services immediately, as prompt treatment is crucial.
Can allergic reactions to tramadol develop over time?
While rare, it is possible for individuals to develop allergic reactions to tramadol even after using it without issues for some time. This phenomenon, known as drug sensitization, can occur with various medications. If you notice any new or concerning symptoms after taking tramadol, regardless of how long you’ve been using it, it’s important to seek medical advice promptly.
Monitoring and Reporting Tramadol Side Effects
While this article covers many common and serious side effects of tramadol, it’s not an exhaustive list. Always refer to the leaflet inside your medication packet for comprehensive information. It’s crucial to monitor your body’s response to tramadol and report any concerning side effects to your healthcare provider.
In many countries, there are systems in place for patients and healthcare professionals to report medication side effects. These reports help regulatory agencies and pharmaceutical companies monitor drug safety and make informed decisions about medication use and labeling.

How can patients report tramadol side effects?
Patients can typically report side effects through their healthcare provider, pharmacist, or directly to the relevant national drug regulatory agency. In the UK, for example, the Yellow Card Scheme allows patients and healthcare professionals to report suspected side effects. Similar systems exist in other countries, such as the FDA’s MedWatch program in the United States. Check with your local health authorities for specific reporting mechanisms in your area.
Balancing Pain Management and Side Effects: Personalized Tramadol Use
Managing chronic pain often involves finding a balance between effective pain relief and minimizing side effects. Tramadol can be an effective pain management tool for many individuals, but its use should be tailored to each patient’s needs and tolerances. Your healthcare provider will consider factors such as:
- The severity and type of pain you’re experiencing
- Your overall health and medical history
- Potential drug interactions with other medications you’re taking
- Your individual response to tramadol, including any side effects
Open communication with your healthcare provider is key to achieving optimal pain management while minimizing adverse effects. Don’t hesitate to discuss any concerns or side effects you experience while taking tramadol.

Can tramadol dosage be adjusted to reduce side effects?
Yes, in many cases, adjusting the tramadol dosage can help reduce side effects while maintaining pain relief. Your doctor may recommend starting with a lower dose and gradually increasing it to find the optimal balance between pain management and side effect minimization. Never adjust your tramadol dosage without consulting your healthcare provider, as improper use can lead to serious health risks, including dependence and withdrawal symptoms.
Alternative Pain Management Options: When Tramadol Isn’t Suitable
For some individuals, the side effects of tramadol may outweigh its benefits, or other factors may make it an unsuitable choice. In these cases, alternative pain management strategies may be considered. Some options include:
- Other opioid medications
- Non-opioid pain relievers (e.g., NSAIDs, acetaminophen)
- Antidepressants or anticonvulsants for certain types of pain
- Topical pain relievers
- Physical therapy and exercise
- Cognitive-behavioral therapy
- Complementary therapies (e.g., acupuncture, massage)
The most appropriate pain management strategy will depend on the individual’s specific condition, overall health, and personal preferences. A comprehensive pain management plan often involves a combination of pharmacological and non-pharmacological approaches.

How do healthcare providers determine the best pain management strategy?
Healthcare providers consider multiple factors when developing a pain management plan, including the type and severity of pain, the patient’s medical history, potential drug interactions, and individual preferences. They may use pain assessment tools, conduct physical examinations, and review medical records to make informed decisions. The process often involves trial and error to find the most effective approach with the least side effects. Regular follow-ups and open communication between patients and healthcare providers are crucial for optimizing pain management strategies over time.
Long-term Use of Tramadol: Considerations and Precautions
While tramadol can be an effective pain management tool, long-term use requires careful consideration and monitoring. Prolonged use of tramadol may lead to:
- Tolerance, where higher doses are needed to achieve the same pain relief
- Physical dependence, leading to withdrawal symptoms if the medication is stopped abruptly
- Potential for addiction in some individuals
- Increased risk of certain side effects
Healthcare providers carefully weigh the benefits and risks of long-term tramadol use for each patient. Regular check-ups and open communication about pain levels, side effects, and overall well-being are essential for those on long-term tramadol therapy.

Can long-term tramadol use cause permanent health effects?
While most side effects of tramadol are reversible upon discontinuation of the medication, long-term use can potentially lead to certain health issues. These may include hormonal imbalances, increased risk of fractures in older adults, and rarely, serotonin syndrome when combined with certain other medications. However, many individuals use tramadol long-term without significant adverse effects. The key is regular monitoring and open communication with healthcare providers to address any concerns promptly.
Tramadol Interactions: Understanding Potential Risks
Tramadol can interact with various medications, supplements, and substances, potentially altering its effectiveness or increasing the risk of side effects. Some important interactions to be aware of include:
- Other opioid pain medications
- Certain antidepressants, particularly MAOIs and SSRIs
- Sedatives and tranquilizers
- Alcohol
- Some antifungal medications
- Certain antibiotics
- St. John’s Wort and other herbal supplements
It’s crucial to inform your healthcare provider about all medications, supplements, and substances you’re using to avoid potential harmful interactions. This includes over-the-counter medications and herbal remedies.

How can patients minimize the risk of tramadol interactions?
To minimize the risk of harmful interactions while taking tramadol:
- Maintain an up-to-date list of all medications, supplements, and substances you use
- Share this list with all healthcare providers involved in your care
- Consult your doctor or pharmacist before starting any new medication or supplement
- Avoid alcohol consumption while taking tramadol
- Read medication labels carefully and follow dosing instructions precisely
By being proactive and transparent about your medication use, you can help ensure the safe and effective use of tramadol as part of your pain management plan.
Side effects of tramadol – NHS
Like all medicines, tramadol can cause side effects, although not everyone gets them. Talk to your doctor or pharmacist if the side effects listed below bother you or do not go away.
Very common side effects
Very common side effects of tramadol happen in more than 1 in 10 people and include:
- feeling sick
- feeling dizzy
Common side effects
These common side effects of tramadol happen in more than 1 in 100 people. There are things you can do to help cope with them.
Headaches
Make sure you rest, and drink plenty of fluids. It’s best not to drink alcohol with tramadol as you’re more likely to get side effects, like feeling sleepy. Ask your pharmacist to recommend a painkiller. Headaches should usually go away after the first week of taking tramadol. Talk to your doctor if they last longer than a week or are severe.
Ask your pharmacist to recommend a painkiller. Headaches should usually go away after the first week of taking tramadol. Talk to your doctor if they last longer than a week or are severe.
Feeling sleepy, tired, dizzy or “spaced out”
These side effects should wear off within a week or two as your body gets used to tramadol. Talk to your doctor if they carry on for longer. Do not drink any alcohol as this will make you feel more tired.
Feeling or being sick (nausea or vomiting)
Stick to simple meals and do not eat rich or spicy food. It might help to take your tramadol after you’ve eaten a meal or snack. If you’re being sick, try small frequent sips of water. Speak to a pharmacist if you have signs of dehydration, such as peeing less than usual or having dark, strong-smelling pee.
If tramadol continues to make you sick, or feel sick, tell your doctor. They may be able to prescribe a medicine which can also protect your stomach.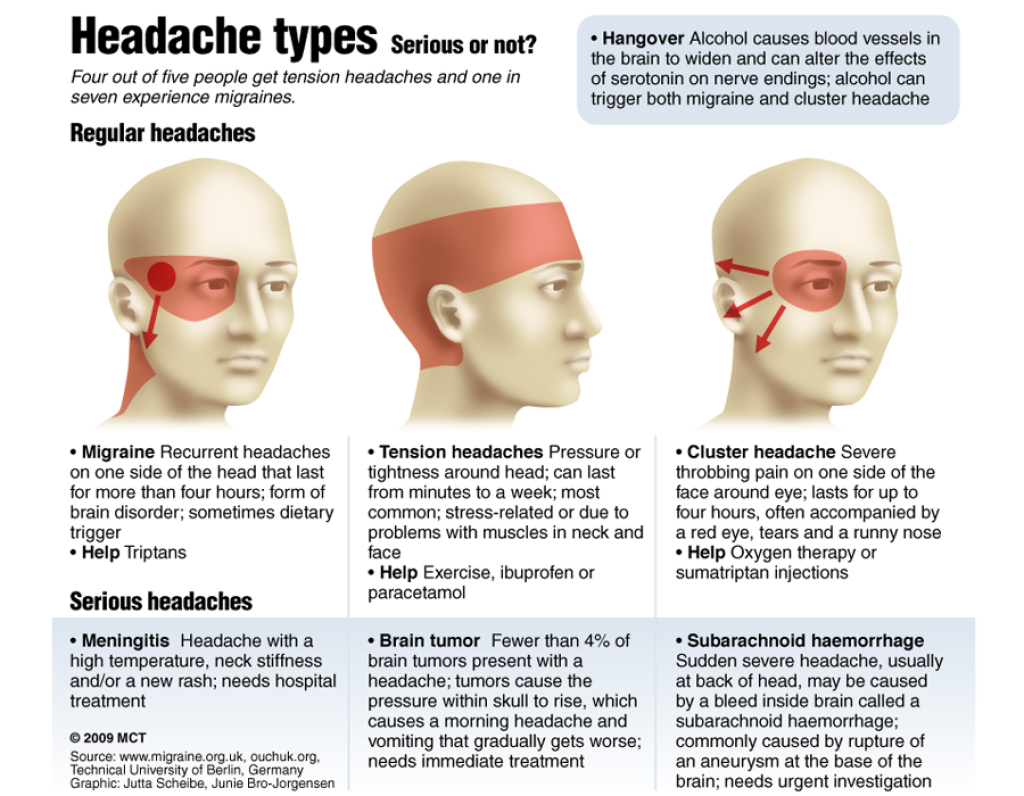 If tramadol makes you vomit or have severe diarrhoea for more than 24 hours, your contraceptive pills may not protect you from pregnancy. Check the pill packet to find out what to do.
If tramadol makes you vomit or have severe diarrhoea for more than 24 hours, your contraceptive pills may not protect you from pregnancy. Check the pill packet to find out what to do.
Constipation
Try to get more fibre into your diet such as fresh fruit and vegetables and cereals. Also try to drink several glasses of water, or another non-alcoholic drink, every day. If you can, it may also help to do some gentle exercise like swimming or going for a short walk.
Speak to your doctor about medicine to help prevent or treat constipation caused by tramadol if your symptoms do not go away.
Dry mouth
Try chewing sugar-free gum or sucking sugar-free sweets. Your doctor may also prescribe an artificial saliva substitute to keep your mouth moist. This comes as a spray, gel or lozenge.
Sweating
Try wearing loose clothing, using a strong anti-perspirant and using a fan, if possible. If this does not help and you find it unbearable, speak to your doctor as you may need to be treated with a different type of painkiller.
If this does not help and you find it unbearable, speak to your doctor as you may need to be treated with a different type of painkiller.
Low energy
Speak to your doctor as they may be able to adjust your dose or give you a different painkiller.
Serious side effects
Serious side effects happen in less than 1 in 100 people.
Call your doctor or call 111 now if you:
- feel dizzy, tired and have low energy – these can be a sign of low blood pressure
- have hallucinations (seeing or hearing things that are not there)
- feel confused
- feel very sleepy
- have trouble peeing or you cannot pee at all
Immediate action required: Call 999 or go to A&E now if you or your child:
- have a seizure or fit
- have breathing difficulties or short shallow breathing
Serious allergic reaction
In rare cases, it’s possible to have a serious allergic reaction (anaphylaxis) to tramadol.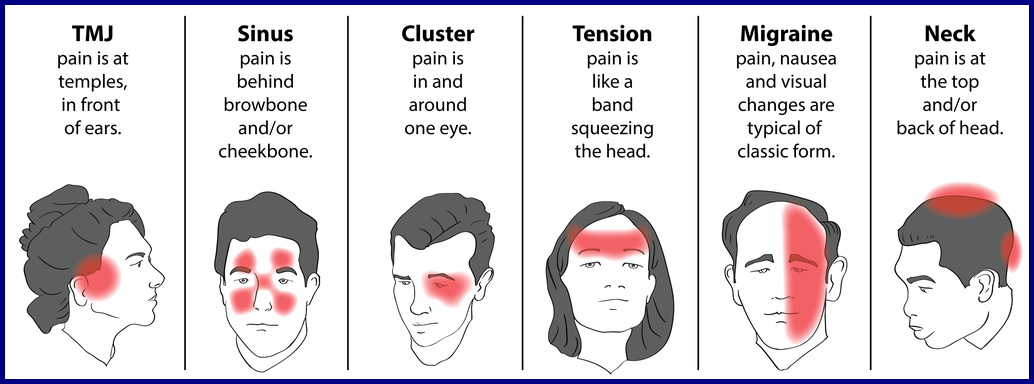
Immediate action required: Call 999 now if:
- your lips, mouth, throat or tongue suddenly become swollen
- you’re breathing very fast or struggling to breathe (you may become very wheezy or feel like you’re choking or gasping for air)
- your throat feels tight or you’re struggling to swallow
- your skin, tongue or lips turn blue, grey or pale (if you have black or brown skin, this may be easier to see on the palms of your hands or soles of your feet)
- you suddenly become very confused, drowsy or dizzy
- someone faints and cannot be woken up
- a child is limp, floppy or not responding like they normally do (their head may fall to the side, backwards or forwards, or they may find it difficult to lift their head or focus on your face)
You or the person who’s unwell may also have a rash that’s swollen, raised, itchy, blistered or peeling./ativan-withdrawal-symptoms-4588394_final-6bb2e0e1202b4092ba7297c475a8509f.png)
These can be signs of a serious allergic reaction and may need immediate treatment in hospital.
Other side effects
These are not all the side effects of tramadol. For a full list, see the leaflet inside your medicine packet.
Information:
You can report any suspected side effect using the Yellow Card safety scheme.
Visit Yellow Card for further information.
Page last reviewed: 19 January 2022
Next review due: 19 January 2025
What are the side effects of tramadol? An overview
Tramadol is a prescription pain medication that can help with moderate to severe pain. Tramadol side effects can include dizziness, nausea, sweating, and heartburn.
Doctors only prescribe tramadol to people over 12 years old. Adolescents with certain risk factors should speak with their doctors about the risks of taking tramadol.
Some people take tramadol for premature ejaculation and restless legs syndrome, but the Food and Drug Administration (FDA) have not approved these uses of it.
As an opioid drug, tramadol acts on the brain to relieve pain. However, tramadol is not as effective as morphine, which is another opioid. Because of its opioid activity, people can become dependent on tramadol.
In this article, we discuss the side effects of tramadol. We will also take a look at tramadol dependence.
Ultram and Ultram ER are the brand names of the drug tramadol. They are available in the form of immediate and extended release tablets. Tramadol is also combined with acetaminophen in the drug Ultracet.
The following table lists the available dosages of tramadol in milligrams (mg).
| Brand name | Active ingredient and dosage | Type of release |
| Ultram | tramadol 50 mg | immediate release |
| Ultram ER | tramadol 100 mg tramadol 200 mg tramadol 300 mg | extended release |
| Ultracet | acetaminophen 325 mg tramadol 37.  5 mg 5 mg | immediate release |
Tramadol acts on two compounds associated with the sensation of pain: serotonin and norepinephrine. Tramadol helps relieve pain by decreasing the amount of these two compounds in brain cells.
Liver enzymes break down tramadol into another compound called O-desmethyltramadol, which binds to the opioid receptor. This is the same receptor that morphine binds to, but tramadol is not as strong as morphine; its efficacy is “about one-tenth that of morphine.”
The FDA classify tramadol as a schedule IV drug because of its potential for misuse and addiction. It belongs to the same schedule as Xanax, Soma, and Valium.
Doctors should choose the lowest effective dosage for the shortest period and educate people on the possible risks of taking tramadol.
Tramadol can cause side effects in some people. They occur more often when people first start taking tramadol and can wear off over time.
Common side effects
Share on PinterestSide effects of tramadol include dizziness, nausea, and headaches.
The most common side effects of tramadol affect the abdominal tract and the brain.
The following list provides common side effects that occur in 5% or more of people who take tramadol:
- dizziness and vertigo
- nausea
- constipation
- headache
- drowsiness
- vomiting
- itchiness
- stimulation of the central nervous system
- weakness
- sweating
- heartburn
- dry mouth
- diarrhea
Less common side effects
People may experience other side effects that occur with an incidence of less than 5%, such as:
- whole body discomfort
- allergic reactions
- suicidal tendencies
- weight loss
- rapid heartbeat
- drop in blood pressure upon standing up
- confusion
- disturbance in coordination
- constriction of the pupil
- fainting
- rash
- hives
- visual disturbance
- menopausal symptoms
- retention of urine
- difficulty breathing
- frequent urination
- serotonin syndrome
Serious side effects
Serious side effects may also occur in some people.:max_bytes(150000):strip_icc()/pinched-nerve-headache-treatment-1719581-5c04ae4146e0fb0001cc18461-0c080f4cb6234cd1887540cd7c5011b9.png)
Some serious side effects include:
- respiratory depression
- serotonin syndrome
- heart rhythm problems called QT prolongation
The following sections discuss these serious side effects.
Respiratory depression
Respiratory depression is a serious side effect that may occur in people taking tramadol. If a person has difficulty breathing while taking tramadol, they must seek emergency medical attention.
People can experience respiratory depression with usual dosages of tramadol. Respiratory depression usually occurs when the person starts taking tramadol or when they increase their dosage.
People who overdose on tramadol are at an even greater risk of respiratory depression. Combining certain drugs with tramadol can also increase the risk of respiratory depression.
Some people are more at risk than others. Some people’s bodies break down tramadol into O-desmethyltramadol much more quickly and completely. This can result in higher levels of this compound in the bloodstream and lead to respiratory depression.
This can result in higher levels of this compound in the bloodstream and lead to respiratory depression.
Adolescents aged 12–18 years may have additional risk factors for respiratory depression:
- obstructive sleep apnea
- obesity
- severe lung disease
- neuromuscular disease
Some adolescents may be taking other medicines that put them at greater risk of respiratory depression. In these situations, tramadol can cause life threatening respiratory depression.
Serotonin syndrome
Serotonin syndrome develops when there is too much serotonin accumulating in the body. This can cause mild to fatal symptoms.
In rare cases, people can experience serotonin syndrome when taking tramadol alone or with other drugs.
The symptoms of serotonin syndrome may include:
- agitation
- hallucinations
- coma
- rapid heartbeat
- fluctuating blood pressure
- high body temperature
- muscle rigidity
- nausea
- vomiting
- diarrhea
Heart rhythm problems
QT prolongation is a serious condition affecting the heart rhythm. On an electrocardiogram of the heart, the QT interval represents a portion of the electrical activity during the heartbeat.
On an electrocardiogram of the heart, the QT interval represents a portion of the electrical activity during the heartbeat.
Some drugs, such as tramadol, can cause QT prolongation. When a person has a prolonged QT interval, they may experience serious heart problems. They may have an irregular heartbeat, which can become life threatening.
In most cases of QT prolongation related to tramadol, a person has taken tramadol with other drugs that prolong the interval.
Although the combination of QT-prolonging drugs can be dangerous, some people are born with long QT syndrome. These people should let their doctor know about their condition before taking tramadol.
People who overdose on tramadol also have an increased risk of QT prolongation.
Tramadol can interact with several medications, such as benzodiazepines and serotonergic drugs.
Benzodiazepines
Benzodiazepines are drugs that reduce anxiety and relax the muscles. People use them to treat anxiety and insomnia.
If someone is already taking a benzodiazepine medication such as lorazepam or alprazolam, also taking tramadol can result in sedation, respiratory depression, coma, and even death.
Serotonergic drugs
Serotonergic drugs affect serotonin levels in the body. People use them to treat depression.
People who are taking serotonergic drugs should use tramadol carefully because of the risk of serotonin syndrome.
The following table lists serotonergic drug classes:
| Drug class | Drugs |
| selective serotonin reuptake inhibitors (SSRIs) | citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline |
| serotonin and norepinephrine reuptake inhibitors (SNRIs) | venlafaxine, duloxetine, desvenlafaxine |
| tricyclic antidepressants | amitriptyline, imipramine, clomipramine |
| triptans | almotriptan, eletriptan, frovatriptan, rizatriptan, sumatriptan |
| 5-HT3 receptor antagonists | granisetron, ondansetron |
| monoamine oxidase inhibitors (MOIs) | phenelzine, selegiline |
People taking tramadol should report any side effects to their doctor.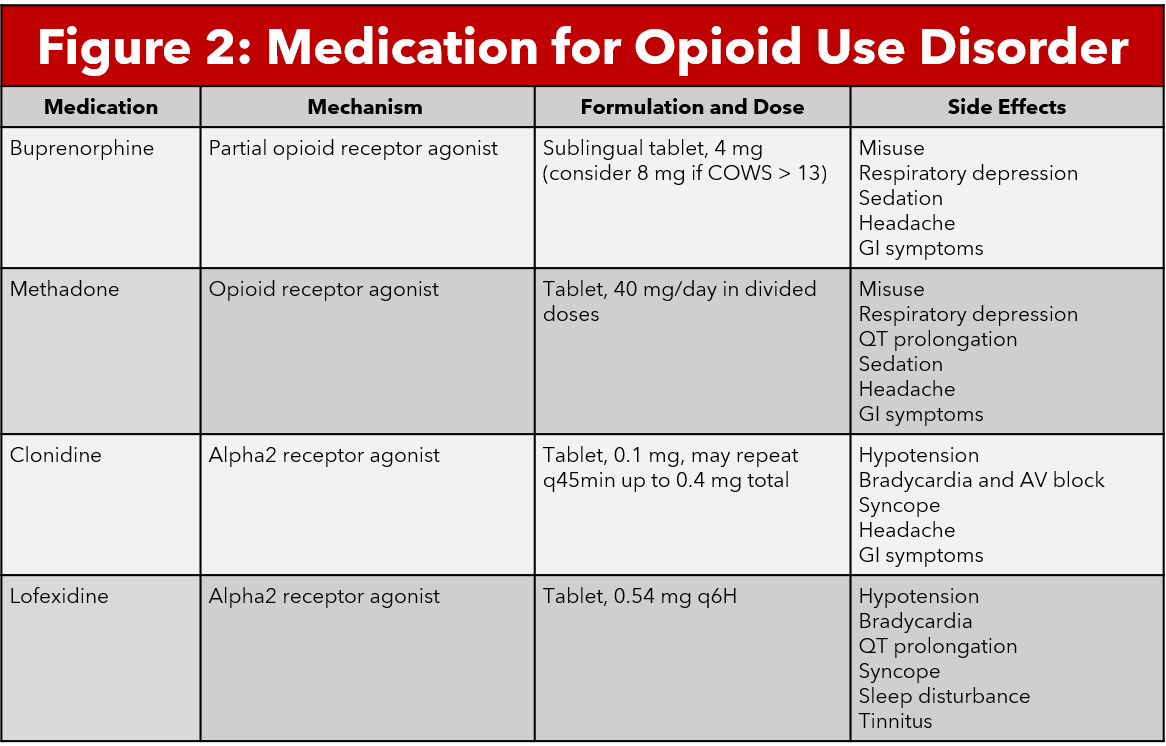 By discussing the benefits and risks of the medication, a doctor can help a person find the most appropriate medicine at the lowest effective dosage.
By discussing the benefits and risks of the medication, a doctor can help a person find the most appropriate medicine at the lowest effective dosage.
Severe allergic reactions require emergency medical attention.
Anyone having difficulty breathing or experiencing any symptoms of serotonin syndrome must seek immediate medical care.
Share on PinterestPeople may become dependent on tramadol when taking it for more than a few weeks or months.
According to a World Health Organization (WHO) report on tramadol, clinical data in adults suggests that the drug has a low potential for dependence.
People may, however, become dependent on tramadol when taking it for more than a few weeks or months. People with a history of drug misuse are more at risk of developing a dependence on tramadol.
In one case study, a 39-year-old male with no history of substance misuse went to the emergency room to get help for tramadol addiction. His tramadol treatment began about 2 years earlier. He was taking up to 600 mg per day and was unable to stop taking it without experiencing withdrawal symptoms.
He was taking up to 600 mg per day and was unable to stop taking it without experiencing withdrawal symptoms.
So, in rare cases, tramadol dependence can affect people without a history of drug misuse.
Tramadol is an opioid pain medication. It also acts on brain chemicals called serotonin and norepinephrine to relieve moderate to severe pain.
Tramadol is not safe for everyone. Children under 12 years old should not take tramadol, and those aged 12–18 should use caution when taking it.
Some people may experience mild to severe side effects when taking tramadol. Some drug interactions can occur with tramadol, and the effects can be severe.
Although it has a low potential for dependence, the Drug Enforcement Administration (DEA) control the distribution of tramadol.
Tramadol for osteoarthritis | Cochrane
This translation is out of date. Please click here for the latest English version of this review.
This summary of the Cochrane Review presents what we know from research on the effects of tramadol on osteoarthritis. The review shows that:
The review shows that:
There is gold level evidence that for the treatment of osteoarthritis, taking tramadol for up to three months can reduce pain, stiffness, and improve function and overall well-being. Tramadol can cause side effects such as nausea, vomiting, dizziness, constipation, fatigue and headache.
The benefits of tramadol are negligible and the side effects may cause people to stop taking it, which may limit the benefit of tramadol in the treatment of osteoarthritis.
What is osteoarthritis and what drugs are used to treat it?
Osteoarthritis (OA) is the most common form of arthritis and can affect the hands, hips, shoulders, and knees. In OA, the cartilage that protects the ends of bones breaks down and causes pain and swelling. There are two main types of drug treatment for OA. Painkillers (such as acetaminophen/paracetamol and opioids) are used to relieve pain, but they do not affect swelling. Non-steroidal anti-inflammatory drugs (NSAIDs such as ibuprofen and COX-II inhibitors) are used to reduce pain and swelling. Tramadol is one of the opioids most used in OA. It does not cause bleeding from the stomach and intestines, and does not cause kidney problems that can occur with other painkillers. It also does not affect the cartilage at the ends of bones. But tramadol does not reduce swelling and may not be effective with long-term use. Therefore, it is important to know the benefits and harms of tramadol.
Tramadol is one of the opioids most used in OA. It does not cause bleeding from the stomach and intestines, and does not cause kidney problems that can occur with other painkillers. It also does not affect the cartilage at the ends of bones. But tramadol does not reduce swelling and may not be effective with long-term use. Therefore, it is important to know the benefits and harms of tramadol.
What are the results of this review?
People in the studies took about 200 mg of tramadol per day, or a placebo (fake pill or powder), or an NSAID, or other pain medication. People took the medicines for one week to three months.
Benefits of tramadol
in people with osteoarthritis:
tramadol can reduce pain more than placebo
– tramadol can reduce pain by more than 8.5 points on a scale of 0 to 100
tramadol may improve overall well-being more than placebo
– 50 out of 100 people may improve with placebo
– 69 out of 100 people may improve with tramadol
tramadol may reduce stiffness somewhat and improve function more than placebo
– function may improve by 0. 32 points on a scale of 0 to 10 with tramadol
32 points on a scale of 0 to 10 with tramadol
It is not known whether tramadol improves osteoarthritis symptoms more than other drugs. It is also unknown if tramadol is still effective with long-term use. This is due to the fact that the observations in the studies were short.
Harm of tramadol
in people with osteoarthritis:
tramadol may cause minor side effects in more people than placebo, such as nausea, vomiting, dizziness, constipation, fatigue, and headache
– 18 out of 100 people may have minor side effects when placebo
– 39 out of 100 people may have minor side effects when taking tramadol
tramadol can cause serious side effects that would cause people to stop taking it
– 8 out of 100 people had serious side effects with placebo
– 21 out of 100 people had serious side effects with tramadol
It is not known if tramadol causes more side effects than other osteoarthritis medications.
If you found this evidence helpful, please consider donating to Cochrane. We are a charity that produces accessible evidence to help people make health and care decisions.
Donate
Translation notes:
Translation notes: Translation: Aleksandrova Elvira Grigoryevna. Editing: Gamirova Rimma Gabdulbarovna, Ziganshina Lilia Evgenievna. Russian translation project coordination: Kazan Federal University. For questions related to this transfer, please contact us at: [email protected]
Tramadol tablets for oncology – instructions for use, reviews, reaction in cancer patients to the drug
Tramadol is an effective pain reliever that belongs to soft drugs. It is difficult to get a prescription for it, but it is often impossible for cancer patients to do without this drug.
Oncology and pain syndrome
Drug therapy of pain syndrome in oncology is carried out in accordance with some fundamental principles: pain in 90% of patients;

Description and pharmacological effects of Tramadol
Tramadol is a weak opioid analgesic similar to morphine, only weaker. This compound is a derivative of cyclohexanol. Once in the body, it binds to opioid prescriptions and blocks the transmission of pain impulses to the spinal cord. In addition, this drug has a sedative (sedative) and antitussive effect. Thus, after the introduction of Tramadol, the patient not only ceases to experience pain, but also calms down, can sleep normally.
Indications for the use of Tramadol
Tramadol is prescribed for various conditions that are accompanied by very severe pain, with the ineffectiveness of drugs from the NSAID group:
- injuries;
- oncological diseases;
- myocardial infarction;
- postoperative period;
- neuralgia.
Tramadol in oncological practice
Tramadol according to the rules of the “anaesthesia ladder” recommended by WHO, is prescribed in the second line – after the use of nonsteroidal drugs (NSAIDs).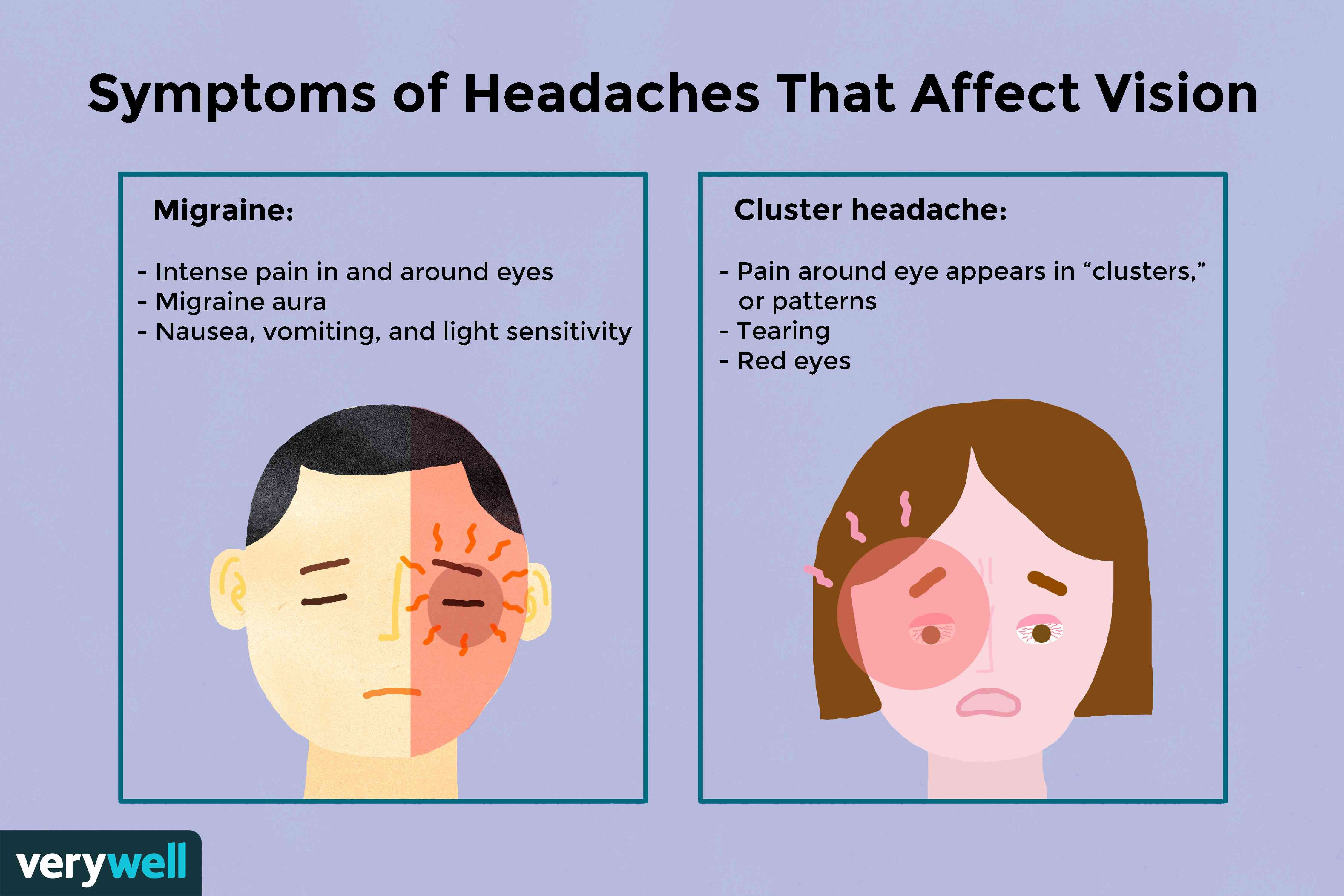
Long-term use of opiates is addictive. But cancer patients should not be afraid of this side effect – provided that they are used strictly according to indications, adequate dosage and regimen.
Pharmacokinetics
Tramadol enters the body in an inactive form and only in the liver is converted into ten inactive metabolites and one active, which reduces pain intensity and disrupts the transmission of pain impulses in the spinal cord.
Of the tablets and drops taken, 68% of the medicine reaches the “sore spot”, all 100% are delivered by blood when injected. The disintegrated drug is excreted by 90% by the kidneys and 10% through the intestines, therefore, with renal failure, it can linger in the blood and tissues for a long time.
After taking a tablet or drops, the analgesic effect will appear after a quarter of an hour, after a maximum of half an hour, and will last almost 6 hours, Tramadol-retard acts up to 12 hours. The drug is highly effective, but over time the body decomposes it more actively, which requires an increase in the dose.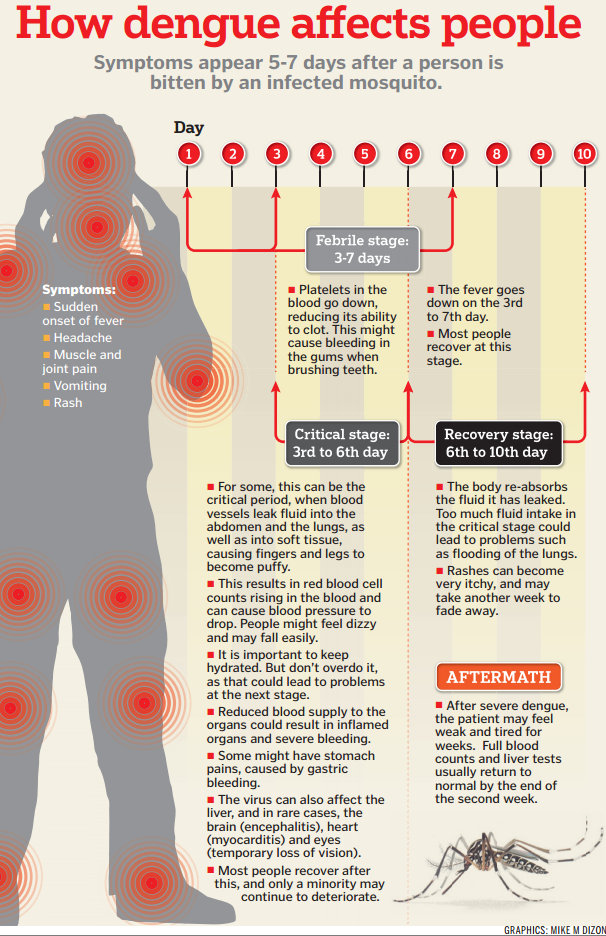 If tramadol does not help at all, then a transition to stronger narcotic analgesics is required.
If tramadol does not help at all, then a transition to stronger narcotic analgesics is required.
How to use the medicine?
Unlike most narcotic analgesics, Tramadol has several dosage forms. You can swallow capsules and tablets, and two types of solutions are also available: in drops for oral administration and in ampoules for injection.
In all cases, oral forms are preferred: injections are painful and, in patients weakened by a long illness, are associated with the possibility of developing an abscess even if complete sterility is observed – immunity works at half strength.
Tramadol drops begin to work very quickly, but they are easy to overdose. It is necessary to drip 20 drops onto a piece of sugar or into water – this is a dose for one dose. The second 20 drops are taken in the absence of pain relief within an hour after the first dose.
Capsule and tablet contains a full single dose. They are taken regardless of food. With unbearable pain syndrome, it is allowed to swallow two at once.
With unbearable pain syndrome, it is allowed to swallow two at once.
Long-acting tablet – Tramadol retard contains a doubled, tripled dose, and the largest one contains 4 single doses at once, which last up to 12 hours, but in especially difficult situations can be taken after 6 hours.
Ampoules contain 1 or 2 ml of solution, i.e. 50 mg or 100 mg of the drug. How often can you inject tramadol? Injections under the skin, into a muscle or vein are repeated no earlier than 4 hours later.
Contraindications
Stop using tramadol:
- if allergic to it;
- in case of alcohol and drug intoxication, overdose of psychotropic drugs;
- is incompatible with antidepressants from the group of MAO inhibitors due to the possibility of developing a severe serotonin syndrome;
- in severe renal failure, when the drug remains in the blood for a long time at a high concentration and an overdose may occur;
- in liver failure, the formation of the active metabolite is impaired.

Oncology and pain syndrome
90% of cancer patients experience pain of varying intensity, but it is not necessarily unbearable. Intolerable excruciating pain usually accompanies metastatic cancer, again, not in everyone, but with severe complications.
Duration of use
How long tramadol can be taken depends on the purpose for which it is prescribed. For example, after injuries and operations, it is used in a short course for several days, a maximum of weeks. In oncological diseases, the drug is used for a long time. It is important to strictly follow the instructions of the attending physician and immediately report all side effects.
Special instructions
During pregnancy Tramadol is prescribed only in short courses. Otherwise, the fetus may become addictive, and then the newborn child may experience a withdrawal syndrome. During breastfeeding, it is also necessary to take into account that a certain amount of the drug passes into breast milk.
Tramadol should be used with caution in case of impaired liver and kidney function .
Do not use the drug in children under 1 year of age. At the age of 1-14 years, dosages of 1 to 2 mg/kg are used. At the same time, prolonged forms of Tramadol should not be used in children under 14 years of age.
Tramadol should be used with caution in case of hypersensitivity to other opioid analgesics, confusion, drug dependence, convulsions.
The drug is incompatible with alcohol, drugs from the group of MAO inhibitors.
Tramadol reduces attention and reaction speed, therefore, during the course of treatment, you can not drive a car and engage in certain activities.
Side effects
Tramadol at therapeutic doses is well tolerated but may cause nausea , which is usually treated with conventional antiemetics – antiemetics.
In long-term treatment, especially in bedridden patients, constipation is possible , which is fought with enemas and laxatives.
Drowsiness and drowsiness are not always unfavorable for severe patients, they even help to some extent, however, this is a side effect.
The drug is characterized by excitation due to changes in the metabolism of serotonin – the “hormone of joy”.
Some patients find over time that this medicine no longer helps them effectively relieve pain and ask the doctor: “why doesn’t tramadol work?”. First, it is one of the weakest opioids. Secondly, as we mentioned above, with prolonged use, the body “gets used” to it and does not respond as well. If the pain syndrome can no longer be effectively controlled, this is an occasion to reconsider the treatment regimen, to include more powerful drugs in it.
Overdose
The maximum dose of Tramadol per day is not more than 400 mg, that is, four times 40 drops, or 8 capsules and regular tablets, 4 suppositories or 4 painkillers injections of tramadol, 2 ml each.
Exceeding the dose is accompanied by a change in consciousness – workload and even coma, convulsions, respiratory depression against the background of a strong heartbeat and a decrease in blood pressure are not excluded.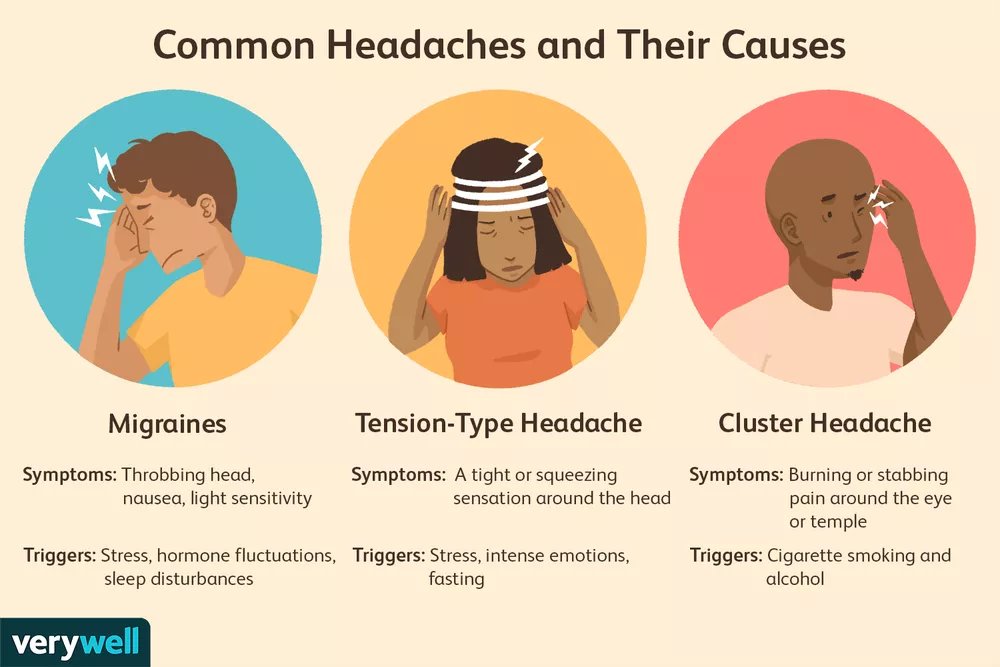 To stop the condition, naloxone is used, convulsions are relieved by an injection of diazepam. Serotonin syndrome is treated with cyproheptadine.
To stop the condition, naloxone is used, convulsions are relieved by an injection of diazepam. Serotonin syndrome is treated with cyproheptadine.
Tramadol analogues
Tramadol and Tramal are the same drug from different manufacturers.
The combination of Tramadol with paracetamol from the group of NSAIDs is available under the names zaldiar, ramleps, tramaceta and forsodol.
How to replace tramadol in oncology? This question is best answered by the attending physician, who knows how the disease proceeds in a particular individual patient.
Only a doctor knows what needs to be done to make the painkiller Tramadol work in full force and with minimal risk to the patient’s health. But it is also important for the patient himself to have information about the drug in order to better understand the goals of treatment, follow the doctor’s prescriptions correctly, and notice side effects in time. Euroonco clinics use only original drugs with proven efficacy, and they are always in stock. Our doctors prescribe treatment in accordance with modern international recommendations.
Our doctors prescribe treatment in accordance with modern international recommendations.
Appointment for a consultation around the clock
+7 (495) 668-82-28
References:
- Abuzarova G.R. /The role of tramadol in oncology and surgery// Abstracts X Ross. National congress “Man and medicine”; M.; 2003.
- Abuzarova G.R., Gallinger E.Yu. Pchelintsev M.V. / Algorithm for pharmacotherapy of chronic pain syndrome in an oncological clinic // Vrach; 2011.-№ 6.
- Pain ed. Yakhno N.N. / Guide for doctors / / Ed. Medpress info; 2009
- Kogonia L.M., Voloshin A.G., Novikov G.A., Sidorov A.V. /Practical recommendations for the treatment of chronic pain syndrome in cancer patients // Malignant tumors: Practical recommendations RUSSCO #3s2, 2018 (vol. 8 ).
- Osipova N.A., Abuzarova G.R. /Treatment of chronic pain in incurable patients at home// Doctor; 2002.-№ 4.
- Novikov G.A., Osipova N.A. /Treatment of chronic pain of oncological genesis//Ed.