Can yeast infections cause headaches. Yeast Infection Complications: Can They Cause Headaches and Other Symptoms?
Can yeast infections lead to headaches. What are the common complications of yeast infections. How do yeast infections affect overall health. What are the signs of a severe yeast infection. When should you seek medical attention for a yeast infection.
Understanding Yeast Infections and Their Potential Complications
Yeast infections, primarily caused by the fungus Candida albicans, are a common form of vaginitis affecting millions of women worldwide. While typically associated with vaginal discomfort, itching, and discharge, yeast infections can potentially lead to more serious complications if left untreated or if they become chronic.
One of the questions that often arises is whether yeast infections can cause headaches. Let’s explore this and other potential complications associated with yeast infections.
The Link Between Yeast Infections and Headaches
Can yeast infections directly cause headaches? There is no direct scientific evidence linking yeast infections to headaches. However, some individuals report experiencing headaches during a yeast infection. This could be due to several factors:

- Stress and discomfort associated with the infection
- Immune system response to the infection
- Possible systemic effects of severe or chronic yeast infections
It’s important to note that if you’re experiencing persistent headaches along with symptoms of a yeast infection, it’s advisable to consult a healthcare professional. These symptoms could be indicative of other underlying conditions or a more severe form of infection.
Common Symptoms and Complications of Yeast Infections
While headaches are not typically listed as a primary symptom of yeast infections, there are several well-documented symptoms and potential complications:
Typical Symptoms:
- Vaginal itching and irritation
- Burning sensation, especially during urination or intercourse
- Redness and swelling of the vulva
- Thick, white, odorless discharge resembling cottage cheese
Potential Complications:
- Recurrent infections
- Skin rashes or infections in other parts of the body
- Increased risk of sexually transmitted infections
- Complications during pregnancy
How often do yeast infections recur? Studies suggest that about 75% of women will experience at least one yeast infection in their lifetime, with 40-45% experiencing two or more.
Systemic Yeast Infections: When Candida Spreads
In rare cases, particularly in individuals with weakened immune systems, yeast infections can become systemic, affecting multiple parts of the body. This condition, known as invasive candidiasis, can lead to more severe symptoms and complications.
What are the symptoms of a systemic yeast infection?
- Fever and chills
- Fatigue
- Body aches
- Nausea
- In severe cases, organ dysfunction
While headaches could potentially be a symptom of systemic candidiasis, it’s crucial to seek immediate medical attention if you suspect this condition, as it can be life-threatening if left untreated.
The Impact of Chronic Yeast Infections on Overall Health
Chronic or recurrent yeast infections can have a significant impact on a person’s overall health and well-being. Beyond the physical discomfort, they can lead to:
- Emotional distress and anxiety
- Sexual dysfunction
- Reduced quality of life
- Potential complications in other areas of health
How do chronic yeast infections affect mental health? The persistent discomfort and recurrence of symptoms can lead to stress, anxiety, and even depression in some individuals. This psychological impact underscores the importance of proper diagnosis and treatment.
Diagnosing and Treating Yeast Infections
Accurate diagnosis is crucial for effective treatment of yeast infections. While over-the-counter treatments are available, it’s important to consult a healthcare provider if:
- It’s your first yeast infection
- Symptoms persist after over-the-counter treatment
- You experience recurrent infections
- You’re pregnant
- You have additional symptoms like fever or abdominal pain
What methods are used to diagnose yeast infections? Healthcare providers typically use a combination of:
- Physical examination
- Review of symptoms
- Microscopic examination of vaginal secretions
- In some cases, culture tests
Treatment usually involves antifungal medications, either in topical or oral form, depending on the severity and type of infection.
Preventing Yeast Infections and Complications
Prevention is key in managing yeast infections and avoiding potential complications. Some strategies include:
- Maintaining good hygiene
- Wearing breathable, cotton underwear
- Avoiding douches and scented feminine products
- Managing diabetes and other underlying health conditions
- Taking probiotics
How effective are probiotics in preventing yeast infections? While research is ongoing, some studies suggest that certain probiotic strains, particularly Lactobacillus species, may help prevent recurrent yeast infections by maintaining a healthy vaginal microbiome.

When to Seek Medical Attention for Yeast Infection Symptoms
While many yeast infections can be treated with over-the-counter medications, there are situations where medical attention is necessary. Seek help if:
- Symptoms persist or worsen after self-treatment
- You have recurrent infections (4 or more in a year)
- You’re pregnant
- You have diabetes or a weakened immune system
- You develop additional symptoms like fever, chills, or pelvic pain
Is it possible to mistake other conditions for a yeast infection? Yes, several other conditions, including bacterial vaginosis and certain sexually transmitted infections, can present with similar symptoms. This is why professional diagnosis is important, especially for recurrent or severe symptoms.
The Role of Diet and Lifestyle in Managing Yeast Infections
While the direct link between diet and yeast infections is still a subject of research, some lifestyle factors may influence the frequency and severity of infections:
Dietary Considerations:
- Limiting sugar and refined carbohydrates
- Incorporating probiotic-rich foods
- Staying hydrated
Lifestyle Factors:
- Managing stress
- Getting adequate sleep
- Avoiding tight-fitting synthetic clothing
- Practicing safe sex
Can certain foods prevent or treat yeast infections? While no specific diet has been proven to prevent or cure yeast infections, a balanced diet that supports overall immune function may help reduce the risk of recurrent infections.
Understanding the Connection Between Yeast Infections and Other Health Conditions
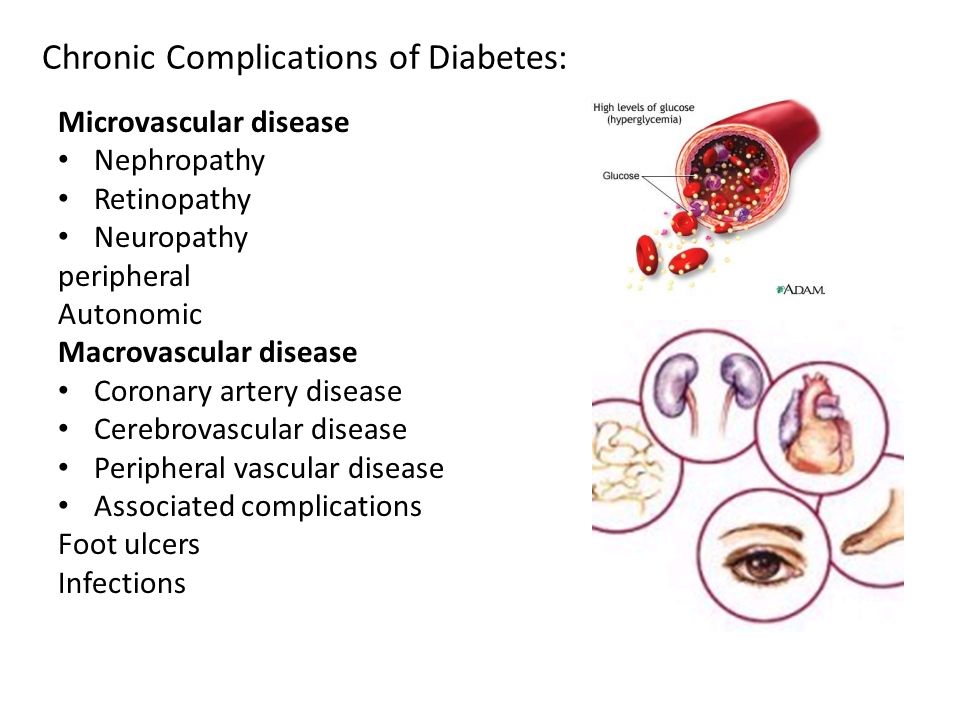
Yeast infections can sometimes be indicative of or influenced by other health conditions. Some conditions that may increase the risk of yeast infections include:
- Diabetes
- HIV/AIDS
- Pregnancy
- Hormonal imbalances
- Certain medications (e.g., antibiotics, corticosteroids)
How does diabetes affect the risk of yeast infections? High blood sugar levels can create an environment conducive to yeast overgrowth. Additionally, diabetes can affect immune function, making it harder for the body to fight off infections.
The Impact of Yeast Infections on Sexual Health and Relationships
Yeast infections can have a significant impact on sexual health and intimate relationships. Some considerations include:
- Discomfort during intercourse
- Temporary abstinence during treatment
- Potential transmission to sexual partners
- Emotional impact on self-esteem and intimacy
Can yeast infections be sexually transmitted? While yeast infections are not typically classified as sexually transmitted infections, they can be passed between sexual partners. It’s important for both partners to be treated if one is diagnosed with a yeast infection to prevent reinfection.
Emerging Research and Future Directions in Yeast Infection Management
The field of yeast infection research is constantly evolving, with new insights into prevention, diagnosis, and treatment emerging. Some areas of current research include:
- Development of new antifungal medications
- Exploration of alternative treatments, including natural remedies
- Improved diagnostic techniques for faster, more accurate detection
- Understanding the role of the microbiome in preventing yeast overgrowth
What new treatments for yeast infections are on the horizon? Researchers are exploring various avenues, including new antifungal compounds, probiotic therapies, and even vaccines targeting Candida albicans. However, these are still in developmental stages and require further research before becoming widely available.
Conclusion: Managing Yeast Infections for Overall Health
While yeast infections are common and generally not serious, they can lead to complications if left untreated or if they become chronic. Understanding the symptoms, potential complications, and when to seek medical attention is crucial for maintaining vaginal and overall health.

Although headaches are not typically a direct symptom of yeast infections, the stress and discomfort associated with these infections could potentially contribute to headache occurrence in some individuals. If you’re experiencing persistent or severe symptoms, including headaches, along with signs of a yeast infection, it’s important to consult a healthcare provider for proper diagnosis and treatment.
By staying informed, practicing good hygiene, and seeking timely medical care when needed, you can effectively manage yeast infections and minimize their impact on your health and quality of life. Remember, your health is a priority, and addressing concerns promptly is key to preventing more serious complications.
Vaginitis – Symptoms and causes
Overview
Vaginitis is an inflammation of the vagina that can result in discharge, itching and pain. The cause is usually a change in the normal balance of vaginal bacteria or an infection. Reduced estrogen levels after menopause and some skin disorders can also cause vaginitis.
The most common types of vaginitis are:
- Bacterial vaginosis, which results from a change of the normal bacteria found in your vagina to overgrowth of other organisms
- Yeast infections, which are usually caused by a naturally occurring fungus called Candida albicans
- Trichomoniasis, which is caused by a parasite and is commonly transmitted by sexual intercourse
Treatment depends on the type of vaginitis you have.
Products & Services
Show more products from Mayo Clinic
Symptoms
Vaginitis signs and symptoms can include:
- Change in color, odor or amount of discharge from your vagina
- Vaginal itching or irritation
- Pain during intercourse
- Painful urination
- Light vaginal bleeding or spotting
If you have vaginal discharge, which many women don’t, the characteristics of the discharge might indicate the type of vaginitis you have. Examples include:
- Bacterial vaginosis. You might develop a grayish-white, foul-smelling discharge. The odor, often described as a fishy odor, might be more obvious after sexual intercourse.
- Yeast infection. The main symptom is itching, but you might have a white, thick discharge that resembles cottage cheese.
- Trichomoniasis. An infection called trichomoniasis (trik-o-moe-NIE-uh-sis) can cause a greenish-yellow, sometimes frothy discharge.
When to see a doctor
See your doctor if you develop unusual vaginal discomfort, especially if:
- You have a particularly unpleasant vaginal odor, discharge or itching.
- You’ve never had a vaginal infection. Seeing your doctor can establish the cause and help you learn to identify the signs and symptoms.
- You’ve had vaginal infections before.
- You’ve had multiple sex partners or a recent new partner. You could have a sexually transmitted infection. Some sexually transmitted infections have signs and symptoms similar to those of a yeast infection or bacterial vaginosis.
- You’ve completed a course of over-the-counter anti-yeast medication and your symptoms persist.
- You have a fever, chills or pelvic pain.
Wait-and-see approach
You probably don’t need to see your doctor every time you have vaginal irritation and discharge, particularly if:
- You’ve previously had a diagnosis of vaginal yeast infection and your signs and symptoms are the same as before
- You know the signs and symptoms of a yeast infection, and you’re confident that’s what you have
Causes
The cause depends on what type of vaginitis you have:
Bacterial vaginosis. This most common cause of vaginitis results from a change of the normal bacteria found in your vagina, to overgrowth of one of several other organisms. Usually, bacteria normally found in the vagina (lactobacilli) are outnumbered by other bacteria (anaerobes) in your vagina. If anaerobic bacteria become too numerous, they upset the balance, causing bacterial vaginosis.
This type of vaginitis seems to be linked to sexual intercourse — especially if you have multiple sex partners or a new sex partner — but it also occurs in women who aren’t sexually active.
- Yeast infections. These occur when there’s an overgrowth of a fungal organism — usually C. albicans — in your vagina. C. albicans also causes infections in other moist areas of your body, such as in your mouth (thrush), skin folds and nail beds. The fungus can also cause diaper rash.
Trichomoniasis. This common sexually transmitted infection is caused by a microscopic, one-celled parasite called Trichomonas vaginalis. This organism spreads during sexual intercourse with someone who has the infection.
In men, the organism usually infects the urinary tract, but often it causes no symptoms. In women, trichomoniasis typically infects the vagina, and might cause symptoms. It also increases a women’s risk of getting other sexually transmitted infections.
- Noninfectious vaginitis. Vaginal sprays, douches, perfumed soaps, scented detergents and spermicidal products may cause an allergic reaction or irritate vulvar and vaginal tissues. Foreign objects, such as tissue paper or forgotten tampons, in the vagina can also irritate vaginal tissues.
- Genitourinary syndrome of menopause (vaginal atrophy). Reduced estrogen levels after menopause or surgical removal of your ovaries can cause the vaginal lining to thin, sometimes resulting in vaginal irritation, burning and dryness.
Risk factors
Factors that increase your risk of developing vaginitis include:
- Hormonal changes, such as those associated with pregnancy, birth control pills or menopause
- Sexual activity
- Having a sexually transmitted infection
- Medications, such as antibiotics and steroids
- Use of spermicides for birth control
- Uncontrolled diabetes
- Use of hygiene products such as bubble bath, vaginal spray or vaginal deodorant
- Douching
- Wearing damp or tightfitting clothing
- Using an intrauterine device (IUD) for birth control
Complications
Women with trichomoniasis or bacterial vaginosis are at a greater risk of acquiring sexually transmitted infections because of the inflammation caused by these disorders. In pregnant women, symptomatic bacterial vaginosis and trichomoniasis have been associated with premature deliveries and low birth weight babies.
Prevention
Good hygiene may prevent some types of vaginitis from recurring and may relieve some symptoms:
- Avoid baths, hot tubs and whirlpool spas.
- Avoid irritants. These include scented tampons, pads, douches and scented soaps. Rinse soap from your outer genital area after a shower, and dry the area well to prevent irritation. Don’t use harsh soaps, such as those with deodorant or antibacterial action, or bubble bath.
- Wipe from front to back after using the toilet. Doing so avoids spreading fecal bacteria to your vagina.
Other things you can do that may help prevent vaginitis include:
- Don’t douche. Your vagina doesn’t require cleansing other than normal bathing. Repetitive douching disrupts the normal organisms that reside in the vagina and can actually increase your risk of vaginal infection. Douching won’t clear up a vaginal infection.
- Use a latex condom. Both male and female latex condoms may help you avoid infections spread by sexual contact.
- Wear cotton underwear. Also wear pantyhose with a cotton crotch. If you feel comfortable without it, skip wearing underwear to bed. Yeast thrives in moist environments.
Nov. 13, 2019
Show references
- Sobel J. Approach to women with symptoms of vaginitis. http://www.uptodate.com/home. Accessed Aug. 11, 2016.
- Vaginitis. American College of Obstetricians and Gynecologists—FAQS.. http://www.acog.org/Patients/FAQs/Vaginitis. Accessed Aug. 11, 2016.
- Vaginitis. Centers for Disease Control and Prevention. http://search.cdc.gov/search?query=vaginitis&utf8=%E2%9C%93&affiliate=cdc-main. Accessed Aug. 12, 2016.
- Overview of vaginitis. Merck Manual Professional Version. http://www.merckmanuals.com/professional/gynecology-and-obstetrics/vaginitis,-cervicitis,-and-pelvic-inflammatory-disease-pid/overview-of-vaginitis. Accessed Aug. 11, 2016.
Related
Products & Services
Show more products and services from Mayo Clinic
What Is Candida? 6 Things To Know About Yeast Overgrowth
We’d like to think that we’re the only ones living in our bodies, but there are thousands of organisms living in us at any given time. One such organism is a fungus called Candida. While having some Candida growing in your body is normal, overgrowth of Candida can lead to a surprisingly diverse number of health problems.
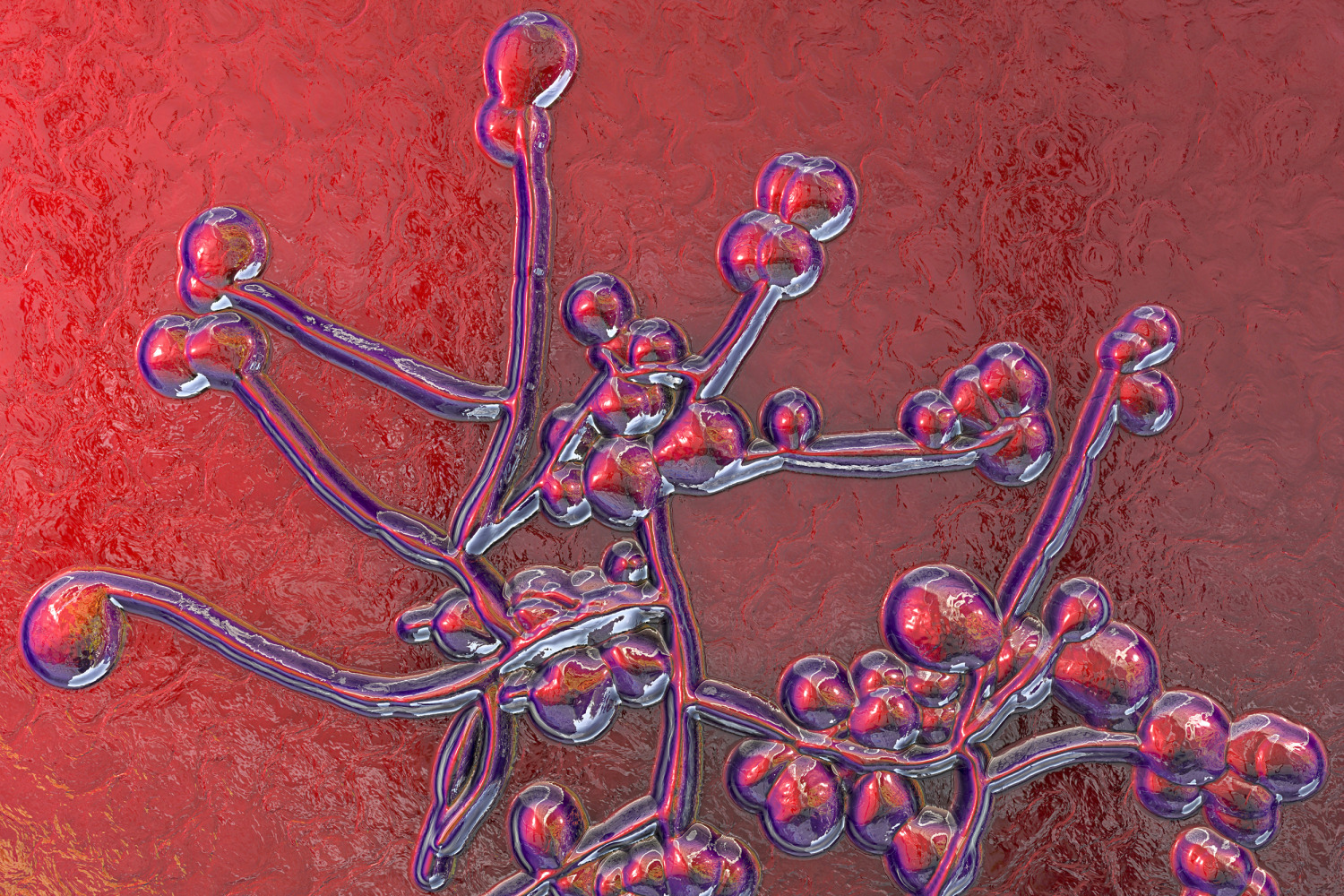
In normal quantities, Candida can actually help with your digestion and nutrient absorption, Dr. Josh Axe, founder of Ancient Nutrition and DrAxe.com, tells Bustle. The problem occurs when you have an excess of it, which may happen due to imbalances in your body’s microbiome or pH levels. Candida overgrowth can occur in the sinuses, mouth, GI tract, and bladder, integrative medicine doctor Susan Kolb, MD tells Bustle. There, the Candida produces biotoxins like aldehydes and alcohol that can lead to fatigue, muscle aches, brain fog, dizziness, dysuria, chronic sinusitis, and itching. Excess Candida can also break down your intestinal lining, leading to Leaky Gut Syndrome, says Axe.
The most common Candida species to cause infections is Candida albicans, he adds. Usually, these infections are not serious and are limited to the mouth, vagina, and GI tract. But if the immune system isn’t functioning properly, it can infect the blood or the membranes around the brain or heart. If it gets into the blood, it can cause life-threatening septic shock, Amesh A. Adalja, MD, senior scholar at the Johns Hopkins Center for Health Security, tells Bustle. “Candida can also cause eye infections, seed prosthetic joints, cause heart valve infections, and cause infections of the esophagus,” he says.
Here are a few facts about Candida to be aware of for the sake of your health.
1
It Can Overgrow For Many Reasons
RK-studio/Shutterstock
Excessive consumption of sugar and/or carbohydrates, stress, and excessive estrogen can all contribute to Candida overgrowth, says Kolb. Some women even find that hormonal birth control can trigger Candida growth, says Axe. Corticosteroid inhalants used for asthma have been linked to oral Candida overgrowth, and those with diabetes or inflammatory and autoimmune conditions that suppress the immune system are at greater risk.
Candida may also overgrow in response to use of antibiotics, which may kill off bacteria that it competes with, says Adalja. People with gluten intolerance and celiac disease also have a higher risk for Candida overgrowth, rheumatologist Alexander Shikhman, MD, PhD tells Bustle.
2
It Can Lead To Acute Infections
Alexxndr/Shutterstock
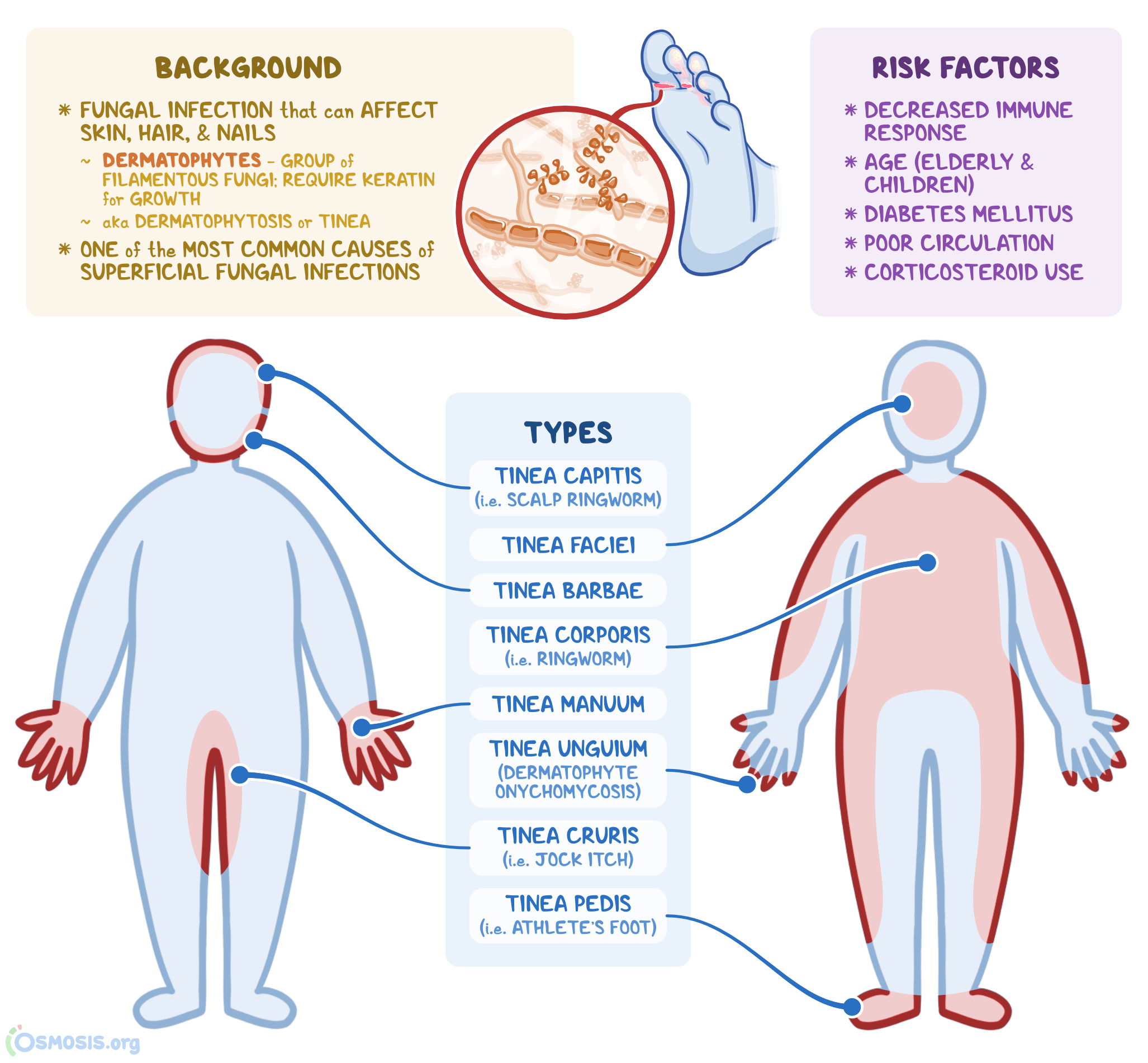
Candida is the microbe responsible for oral thrush (a mouth infection that causes a white coating on the tongue), vaginal yeast infections, and some skin rashes, says Shikhman. Candida-induced skin rashes will look like “red, inflamed areas typically in warm areas such as underarms,” he says.
3
It Can Also Cause Subtler Chronic Health Issues
WAYHOME studio/Shutterstock
Even without an acute infection, Candida can cause what’s sometimes known as Candida Overgrowth Syndrome, says Axe. The symptoms of this condition can include chronic fatigue, mood disorders, chronic and recurrent infections, digestive issues, brain fog, and hormonal imbalances. It can also cause sweet cravings, acne, migraines, and eczema, says Shikhman.
4
You Can Test For It
Monkey Business Images/Shutterstock
“Most people do not know they have Candidiasis, as most doctors are not educated in the symptoms,” says Kolb. “Some learn of the condition by research on the internet or because of an integrative or holistic health practitioner. It is considered overgrowth when one has symptoms or is ill. Most doctors will treat based on the symptoms if they have experience, but testing is possible.” Candida can be picked up on a stool or urine test or a blood test that checks for antibodies against Candida.
5
Dietary Changes Can Reduce It
Rawpixel/Shutterstock
Health care providers will often recommend a “Candida cleanse” for those with Candida Overgrowth Syndrome. This involves eliminating starch, sugar, alcohol, and most fruit from your diet and focusing on vegetables, proteins, and healthy fats. You can also add coconut oil, milk thistle, clove oil, oregano oil, myrrh oil, and lavender oil to your diet to kill off Candida and stop it from spreading, says Axe.
6
Supplements And/Or Medications May Also Be Necessary
Tiko Aramyan/Shutterstock
Treatment for Candida depends on what your symptoms are, but Shikhman breaks Candida treatment into five general goals: stop feeding the yeast (with a low carb diet and Betaine HCL), digest your food completely (with digestive enzymes), normalize your gut microbiome (with prebiotics and probiotics), reduce yeast in your gut (with Pau D’Arco, Black Walnut Hulls, Caprylic Acid, and/or Monolaurin), and stop biofilm formation (with Serrazimes and/or Bromelain).
Kolb treats GI Candida overgrowth with a medication called Nystatin oral solution or herbal remedies like Pau D’Arco. Those who experience symptoms like Fibromyalgia as a result of Candida-induced magnesium deficiency may benefit from Mg Malic acid, and those with memory problems can take molybdenum, she says.
If you’re experiencing signs of Candida overgrowth, Shikhman recommends working with a doctor to establish a low-carb diet and supplement plan. “If you have uncontrollable bloating, diarrhea, skin rashes, or a vaginal yeast infection, it is time to see a doctor.”
What Is It, Symptoms & Treatment
Overview
What is fungal sinusitis?
Fungal sinusitis (fungal rhinosinusitis) is a sinus infection that results from a fungus. Several types of fungal sinus infections cause similar symptoms. These may include nasal congestion and sinus pain (in the cheeks, forehead and between the eyes).
Providers treat most cases of fungal sinusitis with sinus surgery, and extreme forms may require additional anti-fungal treatment. But people with healthy immune systems may not need treatment. Some fungal sinus infections clear up without intervention.
People who have conditions that weaken the immune system (such as diabetes and leukemia) are much more likely to get fungal sinusitis. They also have a higher risk of complications. Some types of fungal sinusitis can destroy the lining of the nose, spread to the brain and lead to death.
What is a fungus?
A fungus is a living organism. It can’t make its own food, so it takes its nutrients from decomposing matter in the soil, water or plants where it lives. Fungi live in the air, on surfaces, and on humans and other animals.
Scientists classify fungi in groups. They include mold, yeasts and mildew. Some fungi are big enough to see (like mushrooms), and some are so small you can only see them with a microscope.
There are more than 100,000 species of fungi. They live all around us, and most aren’t dangerous. But some fungi can invade the body and multiply, leading to serious health problems. Different types of fungi cause infections in many parts of the body. Some examples are yeast infections, thrush and toenail fungal infections.
What are the sinuses?
The sinuses are hollow, interconnected spaces (cavities) inside your skull. They extend across your forehead, behind your nose, between your eyes and under your cheekbones. Sinus walls have a layer of mucus that traps bacteria and keeps the air inside moist.
Sinuses need to drain frequently. If there’s a blockage or inflammation, the sinuses don’t work like they should.
What are the types of fungal sinusitis?
Providers classify fungal sinus infections as invasive and noninvasive. Invasive infections can spread to other areas, such as the eyes and brain. Noninvasive sinus infections, the more common type, only affect the nose and sinus areas.
The types of noninvasive fungal sinusitis are:
- Allergic fungal rhinosinusitis: This is the most common type of fungal sinus infection. It results from an allergic reaction to fungi inside the nose. Untreated, the sinuses fill up with thick mucus and nasal polyps can form. People with asthma or allergic rhinitis (hay fever) are more likely to develop this condition.
- Fungal ball (mycetoma): Fungi build up in the sinuses and form a clump or ball. The fungal ball can get bigger and block the sinuses. Providers use surgery to remove fungal balls and clean out the sinuses.
- Saprophytic fungal sinusitis: This type of infection doesn’t actually affect the nose tissue. Instead, fungus grows on crusts of mucus inside the nose. When providers remove the crusts, they remove the fungus, too.
Untreated, invasive sinus infections are life-threatening. The infection can destroy tissue inside the nose and move into the skull and brain. The types of invasive fungal sinusitis are:
- Acute fulminant invasive rhinosinusitis: This life-threatening condition is more common in people who have a compromised immune system. Their immune system may be weak due to cancer, chemotherapy or after an organ transplant. Fungi destroy blood vessels inside the nose. Without a blood supply, the tissue begins to die. The infection can quickly spread to the eyes and brain, leading to blindness and death. Providers also call this condition acute invasive fungal sinusitis and mucormycosis.
- Chronic invasive rhinosinusitis: People with diabetes are more likely to have this type of sinusitis. It’s similar to acute fulminant invasive rhinosinusitis, but it doesn’t spread as quickly.
- Granulomatous invasive fungal sinusitis (GIFS): This rare type of fungal sinusitis happens when the body launches an immune response to fungi. The person’s immune system attacks the lining of the nose and destroys the nasal tissue. Providers aren’t sure why the immune response happens.
How common is fungal sinusitis?
Some types of fungal sinusitis are more common than others. Women are much more likely to develop fungal balls than men. Allergic fungal sinusitis is more common in warm, humid climates. GIFS is very rare in the United States. It’s much more common in India, Sudan and Pakistan.
Fungal sinus infections have increased over the last few decades. This may be because healthcare providers are prescribing more antibiotics and immunosuppressant drugs. This increase could also be due to a rise in the number of diseases that weaken the immune system.
People with weakened immune systems are more likely to develop fungal sinus infections. Severe infections are more common among people who:
- Are HIV positive.
- Have cancer, including leukemia or lymphoma, or are getting chemotherapy treatments.
- Have severe or uncontrolled diabetes.
- Take drugs to suppress the immune system (such as after an organ transplant).
Symptoms and Causes
What are the symptoms of fungal sinusitis?
Symptoms of fungal sinusitis include:
- Decreased sense of smell or a bad smell in the nose.
- Fever.
- Inflammation (swelling) in the nose and sinuses.
- Nasal congestion and runny nose.
- Pain, tenderness and pressure in the sinus area. It may hurt when you touch your cheeks or forehead.
- Sinus headache.
People with weakened immune systems have a higher risk of serious symptoms of fungal sinusitis. These include:
- Behavioral changes and neurological problems (trouble with thinking and reasoning).
- Changes in skin color (the skin may turn very pale or black).
- Facial numbness.
- Proptosis (eyeballs that protrude, or stick out, from the eye sockets).
- Severe swelling in the cheeks or eyes.
- Vision changes, vision loss and blindness.
What causes fungal sinusitis?
Several types of fungi can cause a sinus infection. Most fungal sinus infections result from mold or yeast. Tiny fungi can enter the sinuses when someone breaths them in.
Many types of fungus live on or inside the body all the time. They’re usually only dangerous to people who have a weakened immune system.
Diagnosis and Tests
How do healthcare providers diagnose fungal sinusitis?
To diagnose a fungal sinus infection, your provider will do a physical exam. They will ask about your symptoms, health history and medications. Then, your provider may remove some mucus or tissue from your sinuses and send it to a lab. The lab tests for fungus.
Your provider may also order a CT scan. This imaging study uses X-rays and a computer to see detailed images of your sinuses. It helps your provider locate the infection or check for a fungal ball. It also helps them develop an effective treatment plan.
An endoscopy can also help your provider diagnose and evaluate a fungal sinus infection. During this procedure, your provider inserts a long, thin tube with a camera into your nose. The camera shows images of your nose and sinuses. Your provider views these images on a monitor.
Management and Treatment
How do providers treat fungal sinusitis?
Fungal sinusitis treatments vary. People with healthy immune systems may not need treatment for some types of fungal sinus infections. Invasive fungal sinus infections require immediate treatment.
Treatments include:
- Antifungal medications: Some types of infection require medications to kill the fungus. Providers usually prescribe these drugs along with surgery.
- Corticosteroid medications: Your provider may prescribe steroids to reduce inflammation and relieve sinus pressure.
- Nasal wash: To treat saprophytic fungal sinusitis, providers remove crusts of mucus and wash out the sinuses. They usually use a saline solution (a mix of water and salt) to cleanse the sinus cavities.
- Surgery: Depending on the type of infection, your provider may do traditional surgery or minimally invasive endoscopic surgery. They insert a long, flexible tube with a camera into your nose and use tiny tools to remove the fungus, fungal ball and any damaged tissue.
Prevention
Can I prevent fungal sinusitis?
You may not be able to prevent a fungal sinus infection. If you’re at a higher risk for fungal sinus infections, talk to your provider. They may recommend regular checkups to monitor your health and treat infections quickly. Talk to your provider if you:
- Have had a fungal sinus infection in the past.
- Have a health condition that weakens your immune system.
- Take immunosuppressant drugs or are getting chemotherapy treatments for cancer.
Outlook / Prognosis
What is the outlook for people with fungal sinusitis?
With treatment, most noninvasive fungal sinus infections go away without serious complications. Some types of infection may come back after treatment.
Untreated, invasive fungal sinus infections can spread to the eyes and brain. They can lead to tissue loss, blindness and death.
Acute fulminant invasive fungal sinusitis is fatal about 50% of the time. This infection worsens very quickly, so it’s essential to get treatment as soon as possible. After treatment, some people have nerve damage, chronic pain or facial abnormalities due to lost tissue.
Living With
When should I see my healthcare provider about fungal sinusitis?
If you have symptoms of a sinus infection, see your provider for an evaluation. It’s also important to call your provider if you have sinus problems that don’t seem to go away (chronic sinusitis).
If you have a condition that weakens your immune system or you take immunosuppressant drugs and you notice sinus infection symptoms, get help immediately. People who have weakened immune systems are at a higher risk of death from a fungal sinus infection. Some infections spread quickly, so it’s essential to seek treatment right away.
A note from Cleveland Clinic
If you have symptoms of a sinus infection, see your provider. They will determine what’s causing your symptoms and recommend the most appropriate treatment. If you have these symptoms and you take immunosuppressant medications or have a condition that weakens your immune system, get help right away. Invasive fungal sinus infections are very dangerous and can worsen quickly. They may be fatal without prompt treatment. If you have a compromised immune system, talk to your provider about getting regular checkups to monitor your health.
What is Candida die-off? What causes it? What to expect & more
Once a candida infection (candidiasis) has been diagnosed and accurately treated with antifungal medications, large amounts of fungal and yeast cells are killed off rapidly and candida die-off may occur. This is referred to as the Jarisch–Herxheimer reaction (JHR) or Herxheimer reaction and may also be referred to as a HERX reaction or healing crisis.
The Herxheimer reaction is an immune system response to the recovery and detoxification process known as the immune cascade23. It was first noted during the 15th century in patients who were undergoing treatment for acute infections such as syphilis and were receiving mercury treatment (which is a weak antibiotic).
Since then, the Herxheimer reaction has been noted during the treatment of other infections caused by spiral bacteria. These include tick and louse borne relapsing fever and Lyme disease24. The reaction usually occurs a few hours after antibiotics are given and symptoms include headaches, fever, fatigue and low blood pressure. It is essentially a short-term response, that takes place over a few days to a couple of weeks, as the body detoxifies.
Anecdotal evidence suggests that the elimination of yeast from a person’s diet or undergoing a ‘Candida Cleanse’ or diet may cause candida die-off that leads to the symptoms described above. There is, however, no strong scientific data to support this theory.
What to expect during candida die-off
While candida die-off may occur after the successful treatment of candidiasis, most people aren’t aware of this fact. This often leads to confusion and anxiety as sufferers expect symptom improvement and to feel better during and following treatment. Instead they end up feeling worse, which may result in the premature abandonment of successful treatment.
As alarming as the sudden development or worsening of symptoms can be, the reaction is temporary and harmless and will usually run its course and resolve without causing further complications.
It is, however, important to note that not all worsening of candida symptoms is attributed to the Herxheimer reaction as a result of candida die off. If a candida infection has not been adequately treated, worsening symptoms may be a sign of infection progression. This is why working with a medical doctor to treat candida is advised.
Candida die off explained
The regular process of cell elimination of candida cells (i.e. the process that occurs naturally in the body when there is no overgrowth or infection) is vastly different to the pace of cell elimination associated with the effective treatment of a candida infection.
When candida yeast cells die, they release a noxious (harmful) substance that contains roughly 79 different toxins. When large numbers of these pathogenic (disease-causing) micro-organisms are killed off quickly, the cell death that occurs leads to a simultaneous release of toxins. This flood of endotoxins causes the kidneys and liver to work overtime to try and remove them, and intensifies the symptoms experienced by the sufferer.
Some of these toxins include:
- Uric acid
- Ethanol
- Acetaldehyde
The neurotoxin acetaldehyde has a wide range of detrimental effects on a person’s health. It can kill brain cells and therefore impairs the functioning of the brain. The endocrine, respiratory and immune systems may all be affected. In addition, the red blood cells can also be damaged as their ability to transport oxygen through the body is hindered as the toxin attacks the membranes of the cells which can lead to symptoms such as fatigue and brain fog.
These toxins can also trigger allergic reactions which can lead to inflammation as the body’s ability to recognise non-threatening organisms is impaired, resulting in certain substances or foods being identified as antigens. The immune system will, in turn, create antibodies as a means of fighting off the invaders, which leads to inflammation and candida die-off symptoms.
Candida die-off symptoms
The symptoms of Candida die off vary between individuals and each person will have their own unique degree of the symptoms depending on the severity of the candida infection as well as personal health status.
The symptoms of Herxing are often compared with the symptoms of seasonal allergies or the common cold, although they do tend to differ from person to person and can be more severe.
The by-products of the toxins involved will often cause inflammation which can lead to blocked sinuses and other sinus infections. As mentioned, toxins such as acetaldehyde can lead to headaches, brain fog, nausea and fatigue. The liver will also be working at maximum capacity to filter the toxins out of the body which can result in pain within the abdomen.
It is best to always keep a medical doctor informed on the progress of recovery.
The below is a list of the most common candida die off symptoms (i.e. the Herxheimer reaction):
- Chronic fatigue
- Brain Fog
- Moderate to more severe headaches
- Muscle and joint pain
- Low grade Fever
- Elevated heart rate
- Sweating
- Swollen lymph nodes or glands
- Inflammation
- Flatulence, bloating, gas, diarrhoea and/or constipation
- Dry mouth and oral thrush
- Sore or itchy throat
- Sleep issues
- Psychological issues such as irritability, anxiety, depression and mood swings
Less common symptoms may include:
- Skin rash
- Lethargy
- Intense craving for sugar and sweets
In addition to these symptoms, the pre-existing symptoms of the current candida infection may progress, this is known as the healing reaction. In addition, the symptoms caused by toxins can be exacerbated due to the body having to use more energy to replace the damaged cells and defective tissue that the toxins and candida have caused during the infection.
If, however, you experience the following after antifungal treatment, seek emergency medical care immediately as this may be a sign of an allergic reaction:
- Difficulty breathing
- Swelling of the tongue, throat and/or face
- A severe skin rash that appears suddenly and looks like blistering or peeling
- Vomiting
- Weak pulse
- Fainting (loss of consciousness)
How long does candida die off last?
The exact amount of time a person will suffer from candida die off or ‘herxing’ is based on the severity of their infection and reaction to treatment. Some reactions resolve spontaneously within a few days and others take a little longer.
Once the treatment administered has effectively cleared the candida infection, symptoms generally resolve. Despite popular belief, candida die-off is not an ongoing issue. The only time the Herxheimer reaction may recur is if a new infection developed and was treated. As such, if you experience ongoing symptoms that are similar to those described, visit your doctor to determine whether something else is going on.
Can candida die off be prevented or treated?
To prevent the Herxheimer reaction, a doctor may suggest starting on a low dose of antifungal medications and probiotics and then slowly increasing it over time. Any symptoms that may arise will be treated accordingly, generally with over-the-counter medications.
If severe symptoms associated with Candida die off occur at any time during treatment, the treating doctor may suggest reducing the dosage again or stopping the medication completely and trying another one.
Tips for coping with Candida die-off
There are a few things other things that can be done to help ease candida die-off symptoms at home should they occur. These should, however, be discussed with and approved by your doctor.
Medications to treat Herxheimer reaction symptoms
Over-the-counter medications may be recommended to help alleviate the symptoms associated with the Herxheimer reaction caused by candida die off. These include:
- Medications to reduce headaches and fever such as paracetamol or acetaminophen based products.
- Non-steroidal anti-inflammatory medications (NSAIDs) like ibuprofen or naproxen to relieve headaches and muscle aches.
- Antihistamines to alleviate any rashes or itching if these occur.
Home remedies and supplement for candida die off symptoms
The following home remedies may also be considered when managing symptoms at home:
- Drink enough water to help flush out toxins – Drinking water may help your body in eliminating toxins a bit faster as urine helps in transporting toxins out of the body. Hot showers, saunas and skin brushes (help to increase the circulation of lymphatic system) can also aid in detoxing the body.
- Eat enough fibre to keep your bowel moving
- Decrease stress levels – Stress can often weaken the body’s ability to recover and fight off the fungal infections. Stressing also increases levels of the hormone cortisol which can impact the immune system’s ability to function at full capacity.
- Rest – Resting and ensuring that you get adequate sleep enables the body to devote energy to healing.
- Use compresses – Warm or cold compresses can be used to muscle aches while cool ones can be used to reduce fever.
- Take oatmeal baths to relieve itching or rashes should they occur
- Epsom salt baths can help with detoxification and muscle aches.
- Liver-support supplements– Milk thistle or molybdenum helps the liver to expel the toxins from the body. Molybdenum is especially helpful in those who are suffering from Candida die-off. This aids the body in the production of the enzymes needed to convert acetaldehyde into the acid known as acetic acid, this can then be converted into either helpful enzyme needed for digestion or be easily expelled from the body.
- Increase antioxidants – Vitamins C & A are powerful antioxidants that support liver detoxification and can help to reduce toxin-related oxidative reactions.
References
23. Jarisch-Herxheimer reaction. BMJ. 1967;1(5537):384-384. doi:10.1136/bmj.1.5537.384
24. Butler T. The Jarisch–Herxheimer Reaction After Antibiotic Treatment of Spirochetal Infections: A Review of Recent Cases and Our Understanding of Pathogenesis. Am J Trop Med Hyg. 2016;96(1):46-52. doi:10.4269/ajtmh.16-0434
25. Kieffer D, Martin R, Adams S. Impact of Dietary Fibers on Nutrient Management and Detoxification Organs: Gut, Liver, and Kidneys. Advances in Nutrition: An International Review Journal. 2016;7(6):1111-1121. doi:10.3945/an.116.013219
Fungal Ear Infection | Causes, Symptoms and Treatment
What are the symptoms of a fungal ear infection?
An explanation of the different types of ear infection and which parts of the ear are involved can be found in the separate leaflet called Ear Infection (Otitis Media).
This leaflet is about infection of the ear canal (otitis externa) with a fungus. Other causes of otitis externa can be found in the separate leaflet called Otitis Externa and Painful, Discharging Ears.
Typically, the ear starts to look red and the skin on the outer part of the ear becomes scaly. It may start to itch and become quite uncomfortable. You may notice discharge beginning to leak out of the ear.
The itching is often worse with fungal infections than with other types of ear infection. Apart from this the symptoms of a fungal ear infection are often identical to ear infections caused by germs (bacteria). This means your doctor may prescribe antibiotic ear drops to start with and may only suspect a fungal infection when the treatment doesn’t work.
Who gets a fungal ear infection?
Fungal infection of the ear is more common in people living in tropical and subtropical countries. It’s also more common in people who do a lot of water sports such as SCUBA diving and surfing. It occurs more often in the summer than the winter.
About 1 in 8 people with infections of the outer part of the ear (otitis externa) have fungal infections.
What causes a fungal ear infection?
Earwax (cerumen) protects the lining of the ear from fungus so anything that reduces the amount of wax (such as sea water splashing into the ear canal and overuse of cotton buds) will allow a fungal infection to take hold. Eczema of the skin inside the ear can be another risk factor.
The outside temperature plays a significant part. Fungi grow faster in the heat, so it’s more common in warmer climates. In the UK it occurs more often in summer than in winter.
9 out of 10 fungal infections are due to a fungus belonging to the Aspergillus species and the rest are caused by a fungus of the Candida species.
How is a fungal ear infection diagnosed?
It you’ve just come back from SCUBA diving in Hawaii, your doctor may well suspect a fungal cause for your ear infection. Otherwise, because a fungal infection looks just like an infection from germs (bacteria), it’s unlikely to be the first thing your doctor thinks of. Most likely, a fungal infection will only be suspected if your infection does not improve with antibiotic drops prescribed for a bacterial infection.
Will I need any tests for a fungal ear infection?
Your doctor will probably treat your ear first and take an ear swab if the condition doesn’t get better. Taking an ear swab is a fairly simple procedure and involves the doctor (or nurse) putting a swab that looks very similar to a cotton bud in your ear and swishing it around. This shouldn’t be painful unless your ear is very tender and inflamed from the infection. Even then, gentle swabbing should only cause mild discomfort.
When should I see a doctor about a fungal ear infection?
Fungal ear infections usually cause a fair amount of discomfort and discharge so most people want to see a doctor soon after the condition starts. There are some eardrops available from pharmacies, but the best they can do is reduce the inflammation a bit. In fungal infections, they don’t usually have much effect.
See a doctor sooner rather than later if:
- You are in a lot of pain.
- Your ear produces a lot of discharge.
- You feel generally unwell or develop unusual symptoms such as dizziness.
- You have a high temperature.
- The outer part of your ear looks very mucky.
- Your hearing becomes muffled.
- You’ve bought some treatment from the chemist which hasn’t worked.
How is a fungal ear infection treated?
If the inside of your ear looks really messy, the doctor may suggest a clean-up. This has the odd name of aural toilet. It can be done by a doctor or more usually a nurse. It involves gently clearing the ear of discharge using swabs, a suction tube or syringe. This may need to be done several times a week in the first instance. Aural toileting eases discomfort and also helps ear drops to get to the right place. However, it may be a bit uncomfortable while you’re having it done, and you may need to take some painkillers.
Don’t fiddle with your ear, keep it dry and try to resist scratching inside, however itchy it may be, as this will stop the infection from clearing up. It’s not usually advisable to put a cotton wool plug in the ear unless you get a lot of discharge and you need to keep it under control for the sake of appearances.
Avoid swimming until the condition clears up.
Your doctor may prescribe 5% aluminium acetate ear drops. This is also known as Burow’s solution. It’s not an antifungal but is used to calm down inflammation and help remove any muck in your ear.
A similar preparation that helps with inflammation is 2% acetic acid. This is available on prescription or can be bought from the chemist in the form of EarCalm® spray.
There are a number of antifungal ear drops available which may be useful, such as clotrimazole 1% ear drops or an antifungal/steroid combination such as flumetasone pivalate 0.02% plus clioquinol 1% ear drops. There’s no real evidence that one is better than another.
If you’ve tried antifungal drops for a couple of weeks and you’re still having problems, stop the treatment and go back and see your doctor. You may need further investigation and/or referral to a specialist. Hospital doctors have special ways of getting the ear clean and dry, such as inserting a pack made from ribbon gauze, a wick made of sponge that hangs out of the ear and drains it or suction using a tiny tube (microsuction).
What is the outlook for a fungal ear infection?
Providing you’re otherwise fit and well and your immune system is working properly, the infection should respond fairly quickly to antifungal treatment. However, if you have a long-term condition that makes you prone to getting repeated infections (such as diabetes or AIDS) it may well come back or become persistent. Also if you’re exposed to whatever it was that caused the infection in the first place (for example, you go straight back to water sports again), it’s likely to return.
The problem with fungal infections (and other types of otitis externa) is that once the ear canal is infected the defence system protecting the ear may not return to normal and a vicious cycle is set up. This explains why frequently poking around inside your ear with a cotton bud (some people call it ‘cleaning out the ear’) prolongs the condition.
Is Hidden Fungus Making You Ill?
A hidden fungus may be making you ill. A 35-year-old recently walked into my office suffering from a whole list of health problems (which is why I often call myself a “whole-listic doctor”). She had chronic fatigue, recurrent yeast vaginal infections, itchy ears, dandruff, patchy itchy skin rashes, irritable bowel syndrome, muscle twitching, acne rosacea, malabsorption, headaches and more.
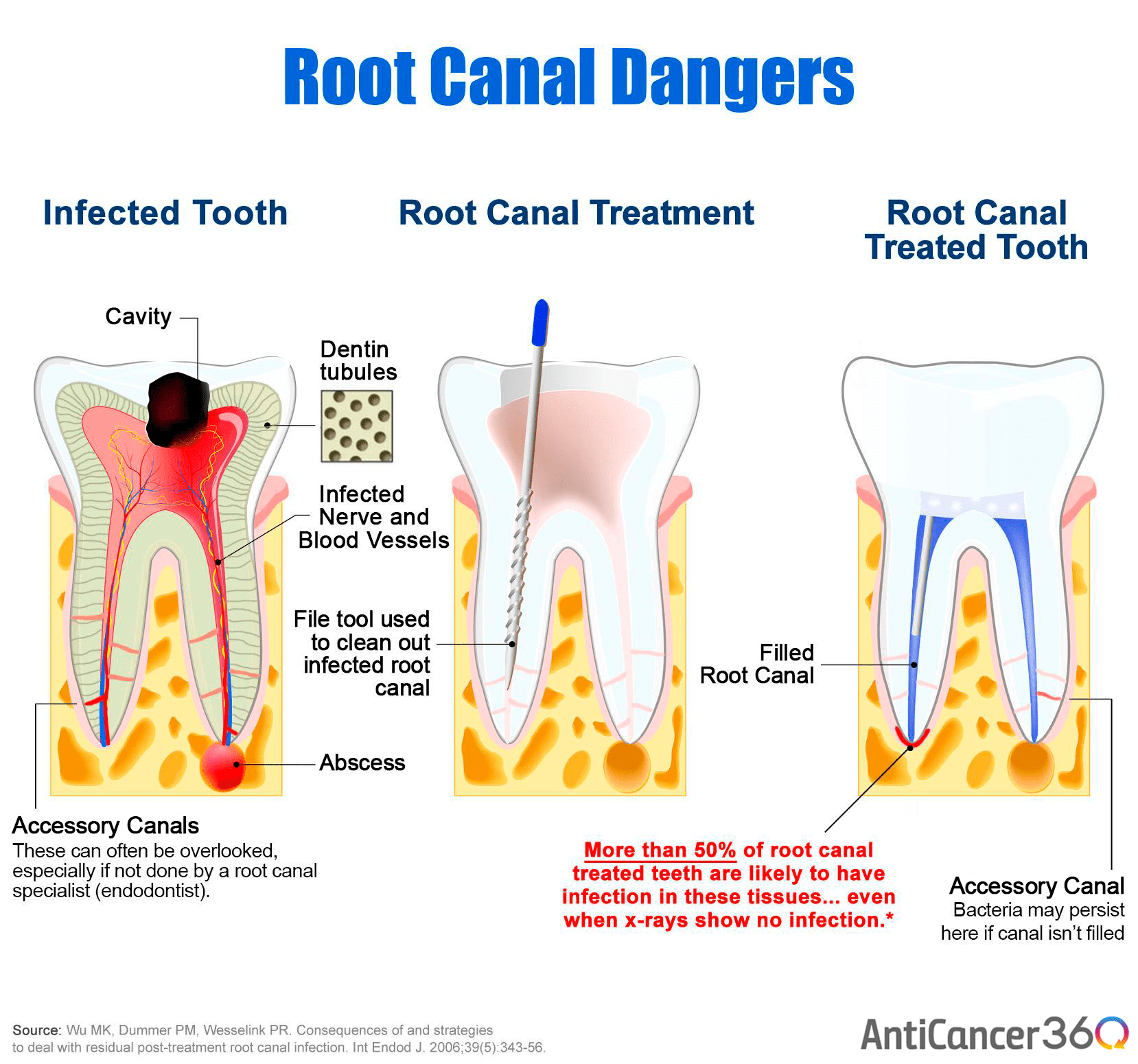
These symptoms can have multiple causes, but in her case all of these problems were related. They were symptoms of an overgrowth of yeast in and on her body. This patient had such a fungus problem that she was practically a walking mushroom!
The cause was clear. She had taken many, many courses of antibiotic over the years. She had been diagnosed with a mostly benign condition called mitral valve prolapse–a problem I believe is over diagnosed and over treated–and “needed” antibiotics every time she went to the dentist. In addition, she had many urinary tract infections for which she took many more courses of antibiotics.
Frequent use of antibiotics disrupts the normal balance between healthy bugs in the gut (lactobacillus, bifidobacter, e. coli) and other potentially dangerous bugs, including yeasts, bacteria and occasionally parasites. These bad bugs are usually present in small numbers in the digestive system. But when the good bugs are killed by antibiotics (i) or not fed with adequate fiber, or the bad guys are fueled with too much sugar, or the gut’s delicate ecosystem (ii) is damaged by too much stress, then yeasts and other noxious agents take over.
This can result in many chronic illnesses and symptoms including allergies, chronic inflammation, joint problems, mood and brain disorders, digestive symptoms and more.
In today’s post I will explain why yeast overgrowth is such a common problem, why conventional medicine tends to overlook it, and provide you with a comprehensive plan to reduce and remove yeast and rebalance your gut’s delicate ecosystem, which sits at the center of your health.
Yeast: A Common But Often Unrecognized Problem
Yeast overgrowth is quite common, but many people don’t know they have it and conventional doctors tend to ignore it. In medical school, we are taught that you either have a disease or you don’t. It’s black and white. However, our bodies weren’t designed with an “on” or “off” switch for disease. All diseases occur in shades of gray along a continuum of imbalance along spectrum of disease.
Medical students learn about fungal and yeast problems, but only in a limited way. They know that AIDS patients have severe yeast and fungal infections and need long-term anti-fungal treatment. People with diabetes tend to grow yeast because yeast likes sugar. Babies get thrush and need antifungal treatment. Women get vaginal Candida yeast infections. All of these are well-accepted and treatable problems. Unfortunately more subtle problems related to yeast are usually ignored and not linked to patient’s complaints. If a subject is not taught in medical school, it is assumed not to be real. Medical history proves this is a dangerous assumption.
On the other hand, many alternative practitioners over diagnose yeast problems. However, there are many people who do have yeast problems, and most of them don’t know it.
There is not enough research on this topic. But the collective intelligence of many doctors working in this field for decades with thousands of patients has helped us learn how to appropriately diagnose and treat this often misdiagnosed problem.
We know that yeast overgrowth can be triggered by a number of things. These include a high-sugar, high-fat, low-fiber diet, impaired immunity, use of drugs like antibiotics, birth control pills, estrogen, and steroids like prednisone, and psychological stress.
Although symptoms of yeast overgrowth are similar to those of many other conditions, you may have a yeast problem if you have these problems (iii)
• Chronic fatigue
• Loss of energy
• General malaise
• Decreased libido
Gastrointestinal Symptoms
• Thrush
• Bloating and gas
• Intestinal cramps
• Rectal itching
• Altered bowel function such as diarrhea (iv) or constipation
• Yeast infections
• Frequent bladder infections
• Interstitial cystitis (irritable bladder)
• Menstrual irregularities like pain, bleeding, etc.
• Premenstrual syndrome
• Thyroid dysfunction
Nervous System Complaints
• Depression
• Irritability
• Inability to concentrate
• Allergies
• Chemical sensitivities
• Low immune function
• Chronic yeast infections
• Chronic antibiotic use for infections or acne
• Oral birth control pill usage
• Oral steroid hormone usage
• Sensitivity to foods, chemicals, or other allergens
• Eczema
• Psoriasis
• Irritable bowel syndrome
• Craving for foods rich in carbohydrates or yeast
• Toenail fungus
Many tests we use for diagnosis of yeast problems are not definitive or foolproof. It is often a diagnosis that must be made from a patient’s story, symptoms, and physical findings on examination. Blood antibody levels for yeasts, stool tests, and organic acid urine tests (v) for yeast metabolites can be helpful if they come out positive but don’t rule yeast out if they’re negative.
The best method for diagnosis is a good history for risk factors like antibiotic use and symptoms of chronic yeast problems. The symptoms of yeast overgrowth vary from person to person and the response to treatments will vary. Some people may need aggressive treatment, while others many need only simple changes to make a significant difference in their health.
I recommend a systematic approach to yeast overgrowth. Taking the following steps can help overcome this common but under diagnosed ailment.
Overcoming Yeast Overgrowth
1. Address predisposing factors. Don’t take antibiotics, steroids, or hormones unless absolutely medically necessary.
2. Eat a diet that doesn’t feed yeast in the gut (low sugar and refined carbohydrates, and low mold and yeast in food (see below).
3. Use probiotics to repopulate the gut with healthy bacteria
4. Take antifungal herbs and medications when indicated
5. Identify potential environmental toxic fungi and molds in your home or workplace
The Yeast Control Eating Program
A simple five-day elimination of yeast and molds in your diet, followed by a challenge or binge of yeasty foods will often relieve and then trigger your symptoms. This can be a good diagnostic tool to see if a long-term yeast control diet would be helpful for you. Remember, different people with different sensitivities may require varying degrees of dietary restrictions. Often, the process of healing requires listening to your body and its signals and sensitivities. Nowhere is this better illustrated than in the management of yeast problems. Follow these guidelines as the first step to assess your yeast problem:
• Eliminate all yeast promoting or yeasty and moldy substances from your diet.
• Try to be totally strict during this time to get the best results.
• Keep a food diary and track what you are eating. You should try to vary your meals and make sure you are not eating a lot of any one food.
• Avoid the test foods for five full days.
• On the sixth day, eat large amounts of the foods you have been avoiding and monitor your reaction. If you get a recurrence of symptoms, you have identified your problem. If not, then yeast may not be a problem
• Remember that sometimes a dietary change may not reduce the yeast overgrowth enough to resolve your symptoms. Then you may need to proceed to the next steps — medication or non-prescription treatments.
• If you feel great off the yeasty foods, you might not want to do the challenge. It could make you feel very ill. Continue to follow a yeast control eating program for at least three months and continue with the other recommendations here.
Additional Steps You Can Take to Reduce or Control Yeast Overgrowth
Often, I find that patients need extra help and should take antifungal herbs, medications, and probiotics.
Take at least 10 to 20 billion live organisms a day of lactobacillus and bifidobacter species. (vi) A special “yeast against yeast” probiotic called saccharomyces boulardii (vii) can be very safe and effective in controlling yeast.
Non-prescription Anti-fungals
Using antifungal therapies such as herbs and other naturally occurring compounds can be very helpful in controlling yeast. The dose for all of the following herbal remedies is generally two pills with meals, three times a day for two to three months. You might need less or more based on your response and symptoms. Sometimes these remedies can be combined for better effect. To find the right combinations and doses for you and identify quality products, consult with a qualified practitioner trained in functional medicine (www.functionalmedicine.org) Some of the best antifungal compounds include the following:
• Oregano — Oil of oregano has many antibacterial and antifungal properties.
• Garlic — Fresh, crushed garlic is a potent antimicrobial and immune booster.
• Citrus seed extract — The phytochemicals in citrus seeds have been found to have potent antimicrobial properties.
• Berberine — This potent yellow plant extract comes from goldenseal and barberry
• Tannins — These are the astringent compounds found in tea and the bark of trees.
• Undecylenate — This chemical compound is a potent antifungal.
• Isatis tinctoria — This Chinese herb can be a useful adjunct to treating intestinal imbalances.
• Caprylic acid — This is another useful compound for treating yeast.
Sometimes, nutrition and supplements just aren’t enough to clear up stubborn yeast overgrowth. That’s where prescription medications can help. (viii) They’re often needed to treat more resistant cases of yeast for either the short or long term — and in some cases can be miraculous in their results.
Nystatin is the most common antifungal drug and is often used to treat thrush in babies. It is not absorbed by the intestinal tract and has no systemic effects. Unfortunately, many fungal organisms are resistant to nystatin and you may need stronger medications. I say “unfortunately” because these drugs are generally processed by the liver and occasionally can cause reversible elevation of liver function tests. They also may have serious interactions with other medications.
People with liver or heart diseases often cannot take these drugs. If you do take Diflucan, Sporonox or Lamasil, you have to have your liver function checked every six weeks. For all of these reasons, you should only take prescription antifungals under the supervision of an experienced and qualified practitioner. These medications can often be life-saving treatments for many conditions unresponsive to conventional treatments.
Killing off yeast is a good thing. However you should be aware that in some people the dead yeast release enough byproducts to cause a “die off” reaction that may make you feel worse before you feel better. This reaction goes away may take up to a week to completely resolve. You can minimize its effects by following the yeast control eating program for a week or so before you start taking any antifungal preparations.
I also recommend taking two to three activated charcoal capsules every four to six hours during the day. Taking a soluble fiber supplement that contains guar gum, alginates, psyllium seed, or pectin to bind to yeast toxins before bed can also be helpful in reducing the “die off” reaction.
Now you know that fungi, yeasts, and mold can make you sick — but there’s good news, too. You can treat the problem. I hope you’ll use the tools I’ve given you in this blog to start getting well and feeling healthy now.
Now I’d like to hear from you…
Do you suffer from the symptoms described here? Have you been diagnosed with yeast overgrowth?
How do certain foods seem to affect your symptoms?
Are you seeing a doctor for yeast problems?
What’s been your experience in dealing with and treating yeast?
Please let me know your thoughts by leaving a comment below.
(i) Kourbeti, I.S., Alegakis, D.E., Maraki, S., and G. Samonis. (2010). Impact of prolonged treatment with high-dose ciprofloxacin on human gut flora: A case report. J Med Case Reports. 4: 111.
(ii) Hawrelak, J.A. and S.P. Myers. (2004). The causes of intestinal dysbiosis: A review. Altern Med Rev. 9(2): 180-97. Review.
(iii) Pizzorno and Murray. 1999. Textbook of Natural Medicine. Churchill Livingstone.
(iv) Krause, R., Schwab, E., Bachhiesl, D., et al.(2001). Role of Candida in antibiotic-associated diarrhea. J Infect Dis. 184(8): 1065-9.
(v) Tana, C., Umesaki, Y., Imaoka, A., et al. (2010). Altered profiles of intestinal microbiota and organic acids may be the origin of symptoms in irritable bowel syndrome. Neurogastroenterol Motil. 22(5): 512-9.
(vi) Hatakka, K., Ahola, A.J., Yli-Knuuttila, H., et al. (2007). Probiotics reduce the prevalence of oral candida in the elderly–a randomized controlled trial. J Dent Res. 86(2): 125-30.
(vii) Pothoulakis, C. (2009). Review article: anti-inflammatory mechanisms of action of Saccharomyces boulardii. Aliment Pharmacol Ther. 30(8): 826-33. Epub 2008 Jul 23. Review.
(viii) Rimek, D., Redetzke, K., and R. Kappe. (2006). Impact of antifungal prophylaxis on the gastrointestinal yeast colonisation in patients with haematological malignancies. Mycoses. 49 Suppl (2):18-23.
Mark Hyman, M.D. is a practicing physician, founder of The UltraWellness Center, a four-time New York Times bestselling author, and an international leader in the field of Functional Medicine. You can follow him on Twitter, connect with him on LinkedIn, watch his videos on YouTube, become a fan on Facebook, and subscribe to his newsletter.
11 Candida Symptoms & How to Eliminate Them
Last updated July 16, 2021 by Lisa Richards, CNC Reviewed by Dr Eric Wood, ND.
Candida overgrowth is a chronic health condition that affects millions of people each year. It can appear on various parts of the body, but is often related to an imbalance in the microorganisms living in the gut. The symptoms of Candida can be difficult to treat unless this gut imbalance is addressed.
If your doctor is unaware of the importance of gut health, he or she may treat the symptoms rather than the cause. Fatigue might be written off as depression, and digestive problems might be blamed on IBS. The underlying cause, an imbalance in the gut flora, might not be recognized or treated.
Just like other syndromes and chronic conditions, the symptoms of Candida can flare up in different places. There are tests for Candida overgrowth but in many cases, patients do much of the diagnostic work themselves.
Looking at the various Candida symptoms that you’re experiencing can give a good indication of whether you have a deeper issue with your gut flora.
What is Candida?
Candida overgrowth, sometimes known as Candidiasis or just Candida, is a fungal infection caused by an overgrowth of one or more Candida species.
Sign up to our free, 8-part email course today, and learn how to create your own, personalized Candida treatment plan 🙂
This is frequently caused by some kind of disruption to the delicate balance of microorganisms in your intestines, otherwise known as your gut flora. A change in the environment allows the colonies of Candida in your gut to multiply and overwhelm the ‘good bacteria’ that live there.
As the population of Candida grows, the multitude of toxic byproducts that it releases begin to cause symptoms like fatigue, brain fog, digestive problems, and headaches. These byproducts include acetaldehyde, ammonia, and uric acid.
When the Candida yeast switches to its more virulent fungal form, it grows long branches (hyphae) that can extend into your soft tissue. These can break through the membrane that surrounds your intestinal tract and release those same waste products. This prompts a reaction from your immune system that can cause allergies and other health problems, including increasing your risk for various autoimmune illnesses.
There are many different types of Candida yeast. Some, like Candida auris, are very rare but life-threatening. The most common infection is Candida albicans, although other subspecies like Candida glabrata and Candida parapsilosis are also common.
What Causes Candida?
A high-sugar diet and antibiotics are the most common causes of Candida, but they are certainly not the only ones. You might be surprised to discover some of the other risk factors that can lead to a Candida overgrowth.
The first stage in addressing your Candida overgrowth is identifying the major risk factors for Candida and eliminating them from your lifestyle.
If you’re wondering what causes Candida, here is a list of the 7 most common triggers:
- A High-Sugar Diet
- Antibiotics
- Chronic Stress
- The Contraceptive Pill
- Heavy metal toxicity
- Chemical Exposure
- Diabetes
The 11 Most Common Candida Symptoms
Candida overgrowth symptoms can include fatigue, brain fog, digestive issues, sinus infections, recurring yeast infections, mild depression, joint pain, and much more.
The consensus is that many more people are suffering from Candida overgrowth than those few who are diagnosed correctly. You may find yourself suffering from any or all of the symptoms below if you have Candida. All of them can be linked to an imbalance in the gut flora.
Here are 11 of the most common Candida overgrowth symptoms that you may be experiencing. You may have just a handful of these, or you might recognize most of the list. Let’s start by taking a look at these symptoms in more detail.
1. Chronic Fatigue
Do you feel like you’re tired all the time? A gut imbalance like Candida overgrowth could be to blame. A pathogen like Candida albicans can affect your energy levels in at least three different ways.
Candida Overgrowth Reduces Nutrient Absorption
When an external factor like antibiotics disturbs the balance in your gut flora, one of the most immediate effects is on the way that you absorb nutrients. Your gut is the place where much of the digestive ‘heavy lifting’ takes place. It’s here that nutrients are broken down, processed, and absorbed.
If Candida (or another pathogen) has expanded its colonies to the point where it affects this balance, your nutrient absorption can suffer.
Foods can pass through your gut without being properly broken down, and you lose the opportunity to absorb the nutrients they contain. Over time, this can lead to fatigue as your body simply doesn’t get the fuel that it needs.
In fact, researchers have noted that Candida overgrowth is associated with deficiencies in important nutrients like essential fatty acids, magnesium, iron, vitamin A, and vitamin B6. Low levels in any of these nutrients, especially magnesium, can lead to fatigue (1, 2).
Candida Produces Toxic Byproducts
Candida’s metabolic processes produce a wide variety of chemicals, many of which are toxic to us. These include a neurotoxin named acetaldehyde, which is coincidentally the same chemical that causes hangovers (3).
In a healthy individual, the small amounts of acetaldehyde produced by Candida are easily processed by the liver. In a person with a Candida overgrowth, this is not necessarily the case. The liver becomes overworked as it struggles to process larger amounts of acetaldehyde.
This build-up of acetaldehyde, ethanol, and other toxins can slow down various processes in your body. And don’t forget that the liver is responsible for energy storage too.
In extreme cases, a yeast overgrowth in the gut can lead to a condition named Auto-Brewery Syndrome, or gut fermentation syndrome. In fact, a New York woman was arrested for drunk driving, only to have her conviction overturned for this very reason (4).
The Adrenal Fatigue Connection
This leads us on to the last reason why Candida can lead to fatigue. Things like an overworked liver, a weakened immune system, and chronic fatigue can put pressure on other organs. Burnout and adrenal fatigue are often seen at the same time as Candida.
The reason is that many of your body’s resources are being diverted to process Candida toxins, fight the Candida overgrowth, and maintain your energy levels.
Over time, this can deplete the hormonal precursors that are needed to produce crucial hormones like pregnenolone, cortisol, and DHEA. As your levels of these hormones drop, it can start to affect your energy levels, your libido, and much more.
2. Brain Fog
We’ve already touched on the reason why a Candida overgrowth can lead to symptoms like brain fog, confusion, difficulties with memory, and poor concentration. A chemical named acetaldehyde, one of the toxic metabolites produced by Candida albicans, is to blame (5).
Acetaldehyde is one of many chemicals produced by Candida (by one count, there are at least 79). Others include ammonia and uric acid. But it’s acetaldehyde that is likely to have the greatest effect on your wellbeing.
If your head is permanently ‘foggy’, you struggle to stay focused, and you are more forgetful than you used to be, acetaldehyde could be the culprit (6).
Get your free, 8-part guide to beating Candida, and join more than 100,000 people getting weekly updates and recipes!
During a Candida overgrowth, there may be too much acetaldehyde in your bloodstream for your liver to process efficiently. This allows it to circulate to your nervous system and brain.
Here are 3 ways in which acetaldehyde can affect your mental focus:
- Red blood cells that combine with acetaldehyde can carry less oxygen to the brain and travel more slowly through blood vessels (7).
- Acetaldehyde can cause a deficiency in vitamin B1, which is crucial for brain health (8).
- Acetaldehyde can damage nerve cells in a similar way to chronic alcoholism or Alzheimer’s (9).
3. Digestive Issues
This Candida symptom takes us right to the heart of Candida overgrowth. It is, after all, a gut-related condition. The changes in your digestive tract are what ultimately leads to all of the other symptoms on this list.
Whatever caused your Candida, whether it was a course of antibiotics or a sustained high-sugar diet, during a Candida overgrowth your gut flora will become imbalanced. As well as weakening your immunity, this can really affect the way that your body digests food.
Those ‘good bacteria’ that normally reside in your gut are a crucial part of your digestive system, responsible for the processing of starches, fibers, and some sugars.
When a healthy gut microbiome is overwhelmed by an opportunistic pathogen like Candida albicans, the small and large intestine can start to function suboptimally.
Digestive issues related to Candida can include:
- Diarrhea
- Gas
- Bloating
- Constipation
- Cramps
- Nausea
In the past few years, researchers have drawn links between Candida overgrowth and other diseases of the gut. These include Crohn’s disease, ulcerative colitis, gastric ulcers, and duodenal ulcers (10).
4. Recurring Yeast Infections
Recurring yeast infections are perhaps the most obvious sign of a Candida overgrowth.
Repeated vaginal yeast infections are a clear sign that something is wrong with your microbiome. If they keep coming back, it’s likely that some kind of gut imbalance is to blame.
More than 75% of women will get a vaginal yeast infection during their lives. And almost 40% will have two or more yeast infections (11).
Symptoms of a vaginal yeast infection will vary from person to person, but they can include:
- Itching
- Pain during intercourse
- Swelling
- White discharge
There’s a characteristic of yeast infections that is very important to note. Even if you clear up the localized yeast infection, Candida albicans has the ability to grow and spread to different areas around your body.
So even though your vaginal infection might have disappeared, the same area may continue to be reinfected until you eliminate your intestinal Candida overgrowth.
UTIs Can Be A Candida Symptom Too
Did you know that urinary tract infections (UTIs) can also be caused by Candida albicans? It typically happens in the very young, very old, or those who are immuno-compromised (12).
If you are under great stress, or your immunity has been weakened for some other reason, your UTI might have been caused by Candida. Symptoms of a UTI include dark urine, pain in the lower abdomen, pain when you urinate, and feeling like you need to urinate when you really don’t.
Male Yeast Infections
Male yeast infections might be less common, but they certainly happen. Symptoms of a penile yeast infection can include a thick, smelly discharge from the foreskin, pain in pulling back the foreskin, an itchy rash around the genital area, redness, and pain when urinating or during sex.
5. Oral Thrush
The mouth is another part of the digestive tract that is particularly vulnerable to Candidiasis. Oral thrush is incredibly common, and in its mild form is frequently undiagnosed until it becomes quite bad. An intestinal Candida infection often occurs at the same time as oral thrush.
The same environmental changes that cause an intestinal overgrowth can also lead to an oral Candida infection. If you take antibiotics or eat a high-sugar diet, they will change the environment in both your gut and your mouth, making both locations more appealing for the Candida fungus.
How do you know if you have the symptoms of oral thrush? You’ll notice white bumps or lesions on your tongue, throat or elsewhere in your mouth (13).
Oral thrush symptoms include:
- White bumps or lesions on your tongue or throat
- Redness inside your mouth or on your gums
- Painful and inflamed areas inside your mouth
- Difficulty swallowing
In a milder form or oral thrush, you might see only a thin, white covering on your tongue. This covering can be removed with a tongue scraper, but soon returns.
Oral thrush can happen to anyone, especially if they follow the wrong diet, but it is most common among the elderly, newborn children, and anyone with a compromised immune system (15). Dentures are a possible cause, along with poor oral hygiene (16).
6. Sinus Infections
Doctors used to assume that almost all chronic sinus infections were caused by bacteria. Newer research suggests that this is not the case. Although acute (short-term) sinus infections are mostly caused by bacteria, many of the longer-term, chronic sinus infections may be fungal infections.
In fact, a Mayo Clinic study looked at 210 patients with chronic sinusitis and found fungal infections in 96% of them (17).
It seems pretty clear that sinus infections might be a Candida symptom, but here’s the big problem. The most common treatment for chronic sinus infections is antibiotics. And antibiotics are pretty much useless for a fungal infection.
Even worse, antibiotics can kill off many of the ‘good bacteria’ that are competing with the fungus, thereby allowing the fungal infection to spread.
If you suffer from chronic sinus infections, improving your diet and rebalancing your gut bacteria may be a far better solution than antibiotics.
7. Food Sensitivities
This is a good time to mention intestinal permeability, or what we know as Leaky Gut Syndrome. This condition is caused when the fungal Candida grows long branches (hyphae) that penetrate the walls of your intestines.
If left unchecked, this results in a highly permeable intestinal membrane which allows food particles and metabolites to escape the intestinal lumen and enter the bloodstream behind the wall.
These particles and bacteria are then identified as foreign substances by your immune system. In the case of bacteria, they may be quickly neutralized. However, your immune system’s reaction to escaped food particles can potentially lead to food sensitivities (18).
As these foods enter the bloodstream, an area where they really don’t belong, your body begins to treat them as threats to your health. When you eat those foods again, your immune system might react to them.
8. Fungal Infections On The Skin And Nails
Just as there are microorganisms inside your gut, there are bacteria on your skin that protect you and prevent pathogens like Candida albicans from spreading in an uncontrolled way. These protective microorganisms are often known as the skin flora or skin microbiota.
The same conditions that lead to an intestinal overgrowth (a high-sugar diet, weakened immune system, etc) can also change the environment on your skin and allow Candida to overwhelm the local flora. Warm, moist areas like the armpits and groin are particularly vulnerable.
This can result in Candida symptoms like the following fungal infections:
- Fingernail infections
- Toenail infections
- Skin rashes
- Athlete’s foot
Topical creams can help with these superficial yeast infections (19). Natural antifungals can also help, with coconut oil being a good, mild example.
As with oral thrush, changing the environmental conditions is the key to eliminating superficial fungal infections in the long run. The same therapies that can reverse an intestinal Candida overgrowth (i.e. probiotics, antifungals, and a low sugar diet) can also help to eliminate fungal skin infections for good.
9. A Weak Immune System
When it comes to a Candida albicans infection, your immune system can play the role of both cause and effect. A weakened immune system is typically what allows an intestinal Candida overgrowth to happen in the first place. But Candida can also play a role in weakening your immune system, all by itself.
Here are three ways this happens:
- An imbalanced gut flora
Your intestines are one of the most significant parts of your immune system. Researchers have found that the bacteria and yeast in your gut ‘prime’ your immune system and keep it ready to fight off pathogens like Candida (20). Without the correct balance of microorganisms in your gut flora, your immune system can be significantly weakened. - Leaky Gut Syndrome
This Candida-related condition, often known as intestinal permeability, provokes inflammation and a strong immune response. The inflammation and food sensitivities that it causes put pressure on your overloaded immune system (21). - Adrenal Fatigue / HPA Axis dysfunction
Lastly, Candida can overwork the adrenal glands and disrupt the HPA axis. These important organs (hypothalamus-pituitary-adrenals) play a role in regulating your immune system, among other things (22). Health problems like chronic fatigue and nutrient malabsorption can lead to hormonal imbalances that weaken and disrupt the HPA axis. A lengthy Candida infection can affect levels of hormones and neurotransmitters like cortisol that regulate the immune system.
Does any of this sound like your experience? If you find that you are regularly suffering from colds and flu, and you don’t know why, a gut imbalance like Candida might be the cause.
Join 100,000+ people on our mailing list, and get your free, 8-part guide to beating Candida 🙂
10. Joint Pain
We’ve already discussed acetaldehyde, but this is far from the only Candida metabolite that can cause unpleasant symptoms. Uric acid is another toxic byproduct of Candida albicans, and it can lead to joint pain in various parts of the body.
If it builds up to sufficient levels, uric acid can lead to gout, a form of arthritis associated with pain, stiffness, and swelling in your joints (23).
These attacks can happen relatively suddenly and can occur repeatedly until the underlying problem is addressed. Longer term, high levels of uric acid can do damage to your tendons and joints.
There is also a particular kind of arthritis that is more directly linked to Candida. If a Candida infection is left untreated for too long, there is a chance that it may enter the bloodstream and appear in joints like the knees and hips. This is known as Candida arthritis (24).
11. Low Mood
So far, we’ve discussed a wide range of symptoms that include tiredness, joint pain, brain fog, and more. If you are experiencing a few of these different symptoms, it could be affecting your mood. But there is also a more direct link between Candida and depression.
- Suppressed Serotonin Production
An intestinal Candida overgrowth can suppress production of serotonin, one of the neurotransmitters that boost your mood. Most serotonin is produced in the gut, so a major gut problem is likely to throw this production out of balance (25). - Reduced Dopamine Levels
Dopamine is another neurotransmitter that affects your mood, and low dopamine levels are strongly associated with depression. Candida has a role to play here too, as one of its metabolites (acetaldehyde) binds with dopamine. This, incidentally, is also one of the reasons why alcoholics tend towards depression (26). - Low B12
Lastly, an overworked liver can reduce your ability to store and use vitamin B12. This important vitamin helps your brain and nervous system to function properly, and low levels have been linked to depression and mental illness.
Less Common Symptoms Of Candida
The symptoms listed above might be the most common signs of a Candida problem, but they are far from the only ones. A chronic gut imbalance can affect your hormone and neurotransmitter levels, your immune system, your liver, and much more.
The signs of Candida overgrowth can also include any of the symptoms listed below. If you recognize a few of these, along with some of the more common symptoms listed above, it might be time to evaluate whether poor gut health might be causing your health issues. If you have a wide selection of seemingly-unrelated symptoms, Candida albicans might be to blame.
- Acid reflux
- Acne
- Allergies
- Asthma
- Bleeding gums
- Bloating
- Body odor
- Constipation
- Cracked tongue
- Cravings for sugary snacks
- Crying spells
- Diarrhea
- Dizziness
- Flatulence
- Flu-like symptoms
- Fungal skin rash
- Halitosis
- Inability to focus
- Inability to lose weight
- Indigestion
- Insomnia
- Irritability
- Itchy anus
- Itchy eyes
- Low libido
- Mucus in stool
- Muscle aches and stiffness
- Nausea
- Panic attacks
- Persistent extreme fatigue
- Poor coordination
- Poor memory
- Psoriasis
- Sensitivities to fragrances and chemicals
- Sensitivity to light
- Stomach cramps
- Water retention
Check out our Candida Questionnaire to see if you might have excess Candida in your gut or elsewhere.
How To Treat Your Candida Symptoms
Your Candida treatment will largely depend on what symptoms you are experiencing. Remember, though, that these symptoms are often related to an underlying intestinal Candida infection. You can treat the symptoms of Candida, but they will keep coming back until you rebalance your gut.
Any treatment of Candida symptoms should be combined with a full Candida protocol, including an anti-Candida diet, to fix the problems in your gut.
Restoring balance to your gut microbiome
If you want long-lasting relief from your Candida overgrowth symptoms, you need to address what’s going on in your gut. The best way to do that is by addressing it in multiple ways. Here are the three elements that you need to include as you treat your Candida and restore your gut health.
- Diet
Diet is the most common cause of an intestinal Candida infection. A high-sugar diet, full of inflammatory, low-nutrient foods, is exactly what Candida albicans needs to thrive (31). By adopting a low-sugar, anti-inflammatory diet, you can reduce inflammation in your gut and deprive the Candida of what it needs to survive. Take a look at our list of foods to eat for some ideas. Here are some basic principles of the Candida diet.- Avoid added sugars
- Eat non-starchy vegetables
- Eat low-sugar fruits
- Eat lots of fermented foods
- Minimize your caffeine
- Eat gut-healing foods
- Enjoy healthy proteins and fats
- Stay away from gluten
- Minimize or avoid alcohol
- Maximize your nutrition
- Drink lots of water
- Probiotics
Probiotics help to maintain acidity in the gut and crowd out the Candida yeast by competing with it for resources. Research has also shown that ‘good bacteria’ in the gut will help to boost your immunity (32). These are all important factors in fighting a Candida overgrowth. You can try probiotic supplements or probiotic foods. - Antifungals
Natural antifungals help to break down the biofilms that Candida uses to protect itself. When used in combination with probiotics and a low-sugar diet, they work alongside your immune system to restrict and reverse the growth of Candida albicans. Good examples are caprylic acid and oregano oil.
Treating Localized Candida Infections
Once you’ve sorted out your gut health, you can take a look at some natural ways to treat localized infections. Examples of these infections are vaginal yeast infections or nail fungus.
How To Treat Vaginal Candida Infections
Here are some natural treatments that you can use to treat vaginal yeast infections. If you suffer from recurring yeast infections, remember that fixing your gut health is a good way to prevent them.
- Antifungal baths
Run a hot bath and add a few drops of tea tree oil or oregano oil. Start with a small amount (oregano oil, in particular, is very potent) and gradually increase it over the course of a few days. - Yogurt
Plain probiotic yogurt is full of beneficial bacteria like strains of Lactobacillus and Bifidobacterium. You can apply the yogurt externally, just like you would a cream from the pharmacy. Some people soak a tampon in the yogurt and leave it overnight. - Coconut oil
You can apply coconut oil externally just like any cream. Depending on the room temperature in your house, your coconut oil may start off either solid or liquid. If it’s solid, you can simply warm it in your hands for a few seconds before applying. Just like yogurt, coconut oil can also be applied internally by using a tampon. - Garlic
Some sources recommend using whole garlic cloves to treat vaginal yeast infections (33). If you choose to try this, carefully peel a garlic clove, clean it thoroughly, coat it with coconut oil and insert it in the frontal cavity of the vagina. Do this before you go to bed, then it will dissolve during your sleep and you can remove any remnants in your morning shower. - Boric acid
Boric acid is available from pharmacies in powder form and can be packed into empty gelatin capsules for use as suppositories. - Tea Tree Oil
Research has shown that tea tree oil is able to impair Candida’s ability to adhere to human cell surfaces (27). Use it topically, and be careful as it is very strong.
How To Treat Male Yeast Infections
The natural treatments here are similar to those used for vaginal Candida, although adapted for male yeast infections.
- Antifungal baths
Run a hot bath and add a few drops of tea tree oil or oregano oil. Start with a small amount (oregano oil, in particular, is very potent) and gradually increase it over the course of a few days. - Yogurt
Rub some plain yogurt on the affected area. Make sure that you buy plain yogurt that contains active cultures. - Coconut oil
Rub some coconut oil on the affected area. Extra virgin or virgin coconut oil is best. It contains three natural antifungals, including caprylic acid, and is an effective antifungal (28). - Apple cider vinegar
Purchase some cotton swabs and swab the affected area with apple cider vinegar.
How To Treat Topical Candida Infections
Here are some natural treatments that you can use to treat fungal infections on your skin and nails.
- Topical treatments
Treatments like tea tree oil, oregano oil, or even minced garlic can be very effective when applied topically. For fungal infections, paint tea tree oil or oregano oil on your nails twice a day for 2 months, or until the fungal infection disappears. Fungal nail infections are very difficult to eliminate and may take a few months. - Other strategies
Keep your feet and hands clean and dry, especially the areas around your nails and between your toes. Change your socks every day, and take them off and walk barefoot when you can. The more airflow your feet get, the faster the infection will go!
How To Treat Oral Thrush
The best natural treatment for oral thrush is coconut oil. It contains three different antifungal compounds, including caprylic acid and lauric acid.
Simply put some coconut oil in your mouth, swish it around for a few minutes, then spit it out (29). Do this twice a day for 2 weeks or until your oral thrush is gone.
Note that coconut oil can be a solid or a liquid, depending on the temperature. If it’s winter or you live in a cold climate, you may find that it’s completely solid. Don’t worry! Just place it in your mouth and it will rapidly dissolve into a liquid.
How To Treat Fungal Sinusitis
Here are two natural treatments for fungal sinusitis. Most sinus infections have some kind of fungal component, and you might continue to struggle with them if you use antibiotics to treat them.
- Sinus Rinse
Rinsing your sinuses with a ‘Neti pot’ is a great way to remove fungi and bacteria from your nasal cavity and fight the excess mucus associated with a sinus infection. Tilt your head to the side, pour the saline water into one nostril, and allow it to drain out of the other. It’s easier than it sounds and it can give incredibly fast, lasting sinus pressure relief. - Essential oils
Peppermint and rosemary essential oils are frequently used to combat nasal and sinus discomfort (30). The best way to get these into your sinuses is to steam them. Add a few drops into a glass bowl and then fill it with boiling water. Cover your head with a large towel, lean over the bowl, and breath naturally.
The Bottom Line
There is a long list of Candida symptoms, and these symptoms can appear in many different parts of the body. Infections in various areas such as the gut, genitals, and skin may all be linked.
Treating individual symptoms can be effective in the short-term, but for long-term relief, you may need to change your diet. The Candida diet is a low-sugar, anti-inflammatory diet that could help when combined with probiotics and natural antifungals.
For lots more information on the symptoms of Candida, take a look at our Ultimate Candida Diet treatment plan. It contains a detailed five-step plan to rebalance your gut flora, beat Candida, and get your health back.
Beat your candida in 60 days with this detailed 5-step program
If you’re looking for a more comprehensive Candida treatment plan, check out the Ultimate Candida Diet program, written by Lisa Richards and Dr Eric Wood. This plan is based on the latest research into Candida Related Complex, and contains everything you need to know to beat your Candida overgrowth.
Order Now
90,000 Candida albicans, IgA
Candida albicans is part of the normal intestinal microflora, however, in some cases, the increased growth of these microorganisms leads to imbalance and the development of candidiasis. Microorganisms or cytoplasmic antigens of C. albicans stimulate the development of an immune response, resulting in the production of specific antibodies to the antigens of Candida albicans. At the first stage, the production of immunoglobulins of the IgM class occurs. The increased growth of Candida on the surface of the mucous membranes leads to the synthesis of specific antibodies of class A (IgA).The detection of immunoglobulins IgA, IgM to fungi of the genus Candida can be used to diagnose candidiasis of various etiologies in conjunction with microbiological diagnostics and taking into account the clinical symptoms of the disease.
Synonyms Russian
IgA immunoglobulins, candidiasis, serological tests for candidiasis.
English synonyms
IgA antibodies, candidiasis, Candida antibody.
Research method
Enzyme-linked immunosorbent assay (ELISA).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for the study?
- Do not eat for 2-3 hours before the examination, you can drink clean non-carbonated water.
- Do not smoke within 30 minutes prior to examination.
General information about the study
Candida albicans (C. albicans) is a yeast-like fungus that is a representative of the normal microbiota of the human skin and mucous membranes, which, under certain conditions, causes superficial or invasive (systemic, visceral) candidiasis.The genus Candida includes other species (C. glabrata, C. dubliniensis, C. krusei), but C. albicans is the most common species and has the greatest clinical significance.
When Candida albicans is under the control of the immune system and balanced with other bacteria, it does not pose any problem to the body. But when these fungi get out of control and start to grow, various symptoms appear, including allergies, fatigue, headaches, bloating, indigestion, vaginitis, arthritis, muscle weakness, joint pain, nasal congestion, pain or tightness in the chest. , blurred vision, hypoglycemia, multiple sclerosis, Crohn’s disease, foggy thinking, and many others.
The spread of the disease is facilitated by the widespread use of antibiotics, the use of refined carbohydrates and yeast, impaired immunity due to exposure to environmental toxins, poor nutrition and lifestyle.
Candida albicans in the body produces up to 180 different toxins that can affect the liver, hormonal balance, impair immunity and cause sugar cravings. A healthy immune system maintains a balance of Candida with other microorganisms on the mucous membranes, but under certain conditions they begin to grow and, out of control, enter the circulatory system.
Often, Candida albicans is the cause of oral and genital infections (thrush), as well as candidal onychomycosis (nail fungus).
Several methods are used to diagnose C. albicans, including smear / scraping microscopy after treatment with potassium hydroxide solution KOH, microscopy of a native smear (for vulvovaginitis), culture on the medium (culture method), molecular diagnostics (RT-PCR), detection antigens of the fungus or antibodies to it (serological tests).
Serological tests are based on the detection of various classes of immunoglobulins in the blood, produced during the recognition of microorganism antigens by the human immune system. There are certain patterns in the development of the immune response when interacting with any microorganism, including the yeast-like fungi of the C. albicans species. During primary contact with C. albicans, immunoglobulins of the IgM class are formed earlier than other classes, which reach the highest titer in comparison with immunoglobulins of other classes during primary infection and are used as an indicator of primary infection.Then specific antibodies of the IgG class appear, and the increased growth of Candida on the surface of the mucous membranes leads to the synthesis of specific antibodies of the IgA class.
Many people are “healthy carriers” of C. albicans. Yeast can be found in about 60% of healthy adults in the mouth and in 12% of women in the vagina. Colonization of the skin and mucous membranes of C. albicans is also accompanied by the development of an immune response and the formation of immunoglobulins. Thus, antibodies to C.albicans. Therefore, the test does not allow differentiating “healthy carriage” from a clinically significant disease. Due to the lack of specificity, the antibody assay is used as an adjunct test for the diagnosis of superficial candidiasis and is inferior to methods such as clinical examination and smear / scraping microscopy after KOH treatment.
The study is not specific for candidiasis, but it is specific for the microorganism: the test detects immunoglobulins to C.albicans, but not other yeast-like fungi. Species identification of Candida is very important, as these yeast-like fungi have different sensitivity to antifungal drugs. So, for example, representatives of Candida krusei are characterized by species (innate) resistance to azole antimycotics. It should be noted that there are other, more accurate methods for determining the species specificity of yeast-like fungi (culture method, PCR).
Determination of IgA antibodies enables early diagnosis of infection; allows you to diagnose the active or chronic stage of infection, therefore it can be used to monitor the dynamics of serological changes during the etiotropic pharmacotherapy of candidiasis and the subsequent monitoring of the patient’s recovery, to assess the strength and quality of the body’s immune response to the activation of the fungal pathogen.
What is the research used for?
- For the diagnosis of candidiasis.
When is the study scheduled?
- Differential diagnosis of mixed infections caused by Candida fungi and bacteria;
- Diagnostics of invasive (systemic) forms of candidiasis;
- evaluation of the effectiveness of antifungal therapy;
- Study of the specific immune response to yeast-like fungi of the genus Candida;
- before and after a course of antimycotic therapy for invasive candidiasis (also as an addition to the main methods of diagnosing candidiasis).
What do the results mean?
Reference values
Component | Reference values | Interpretation |
KP * | no antibodies detected | |
0.85 – 1.00 | it is recommended to repeat the | |
≥ 1.00 | antibodies detected |
* Positivity coefficient – CP – concentration of specific antibodies per unit volume.The higher the CP of the sample, the higher the concentration of antibodies.
Negative / doubtful result:
no infection;
weak immune response of the patient;
low antibody level.
Positive result:
acute candidiasis;
chronic candidiasis;
asymptomatic carriage.
In case of obtaining a questionable result, it is recommended to repeat the study in 10-14 days. If the result is questionable again, the result should be considered negative.
Antibodies of the IgA class to C. albicans are produced 2-3 weeks after infection. The level of antibodies is directly proportional to the severity of the infection – an increase in the synthesis of IgA antibodies occurs in the acute phase, and a decrease in the chronic phase.
What can influence the result?
A positive test is often noted in severe vaginitis with pronounced suppression of the normal microflora of the vagina and increased development of opportunistic microbial flora (coccal bacteria, proteus, fungi).
A negative diagnostic result in most cases means that there is no candidemia.
However, it should be remembered that in immunocompetent individuals with severe immunosuppression, the body’s immune response may be so weak that its strength is insufficient for the production of immunoglobulins in response to the generalization of a fungal infection. In such cases, even with its systemic form, antibodies to Candida in the blood may not appear and, accordingly, may not be detected by serological tests.
Prevention and treatment of insomnia, how to fall asleep with insomnia, how to get rid of, what to do and how to deal with it at home
Sleep is the same human need as food and water. If you completely abandon it or reduce the duration to several hours, then after 4-5 days there will be serious health problems. Even replacing nighttime sleep with daytime sleep is harmful for those who have to work day and night. Lack of adequate sleep leads to endocrine disorders, diseases of the cardiovascular and digestive systems, nervous and mental illnesses.Therefore, insomnia, or insomnia, is also harmful to health – a disease in which the process of falling asleep or sleep itself is disturbed.
Causes of insomnia
Insomnia is more common in women than in men. And in pregnant women, it is observed in 75% of cases. Women are susceptible to illness during menopause, when hormonal changes cause a surge in the activity of the thyroid gland in the evening and at night. This is accompanied by tachycardia, sweating, and inability to sleep.
Insomnia has a large number of causes, some of which are related to the person’s lifestyle:
- sleep hygiene disorders – extraneous noise, bright light, constant vibration or uncomfortable bed;
- stressful conditions – severe traumatic situations suffered, unusual sleeping environment, nervous overstrain;
- change of time zones, work at night;
- mental illness – depression, anxiety disorders;
- the effect of psychoactive substances – alcohol abuse, smoking, a large number of drinks with caffeine, drugs from the group of nootropics, antipsychotics, antidepressants;
- pregnancy – insomnia is associated with changes in the nervous system, discomfort and difficulty breathing due to a large abdomen.
Disruptions to sleep at night can be caused by medical conditions. Insomnia is caused by problems with digestion, diseases of the heart and blood vessels, and increased activity of the thyroid gland. Pain and aches in the joints with arthritis or SARS will also prevent you from falling asleep.
In older age, insomnia is associated with age-related changes in the brain, the development of Parkinson’s disease, dementia and other neurological reasons. But regardless of the factors due to which a person cannot sleep, the problem requires treatment.
How to fall asleep quickly with insomnia
Scientists believe that healthy sleep is a reflex mechanism. If a person went to bed and did not fall asleep after 15-20 minutes, do not lie further in it. Otherwise, it will lead to the formation of a new reflex: bed-insomnia.
Independently you can fight acute insomnia, which occurred for the first time. First you need to get rid of the factors that prevent you from falling asleep. To do this, you need to turn off the TV or computer monitor, curtain the windows if the light of lanterns or the moon breaks through the window.
It is bad to fall asleep in a stuffy and hot room. Therefore, if the question arose of how to fall asleep with insomnia, you need to open a window for airing, reduce the supply of heat in heating radiators. At this time, you can go for a leisurely walk in the fresh air. After returning home, drink a glass of warm milk, herbal tea. This is an old method that has proven to be effective for mild disorders.
Milk contains substances that help in the production of melatonin. It is a pineal gland hormone that regulates circadian rhythms, changes in the state of sleep and wakefulness, and controls the functioning of the immune and endocrine systems.Therefore, with insomnia, the risk of infectious diseases and metabolic disorders, problems in the male genital area increases.
Reading helps to fall asleep quickly. But for this you need to choose not an exciting detective story, but literature of a calm orientation, which usually causes drowsiness. If these methods did not help to fall asleep, the violations persist and disturb regularly, examination and consultation with a doctor is necessary.
Prevention of insomnia
In order not to have to look for ways to treat insomnia, it is necessary to take preventive measures:
- go to bed no later than 23 hours;
- refuse to watch TV, use a smartphone 2 hours before bedtime;
- do not eat large amounts of food at night, do not eat heavy meals;
- do not go to rest with a feeling of hunger;
- ventilate the bedroom before going to bed;
- Do not drink alcohol, coffee, strong tea.
- motherwort grass;
- valerian root;
Daytime sleep will not prevent you from falling asleep in the evening, if you allocate 1-2 hours for it. But if they replace night rest, this will provoke the development of insomnia.
Getting up in the morning is also included in the prevention of insomnia. You need to try to get up at the same time, to increase your tone – do exercises. In order not to disturb the reflex of falling asleep, there is a recommendation not to use the bed for other purposes. You need to go to it only when you feel sleepy and not stay for a long time to eat, read or watch a movie.
How to get rid of insomnia at home
You can fight bad sleep on your own. For milder forms of insomnia, alternative methods of treatment can be used. At home, they make foot baths with dill, after which they take a glass of warm milk with honey and quickly go to bed. In case of increased nervous excitability, prefabricated infusions of medicinal herbs help, for which they use:
90,033 mint leaves.
If the cause of the disturbances is the transferred stress, it is necessary to use methods of struggle that calm the nervous system. At home, you can use various methods of relaxation, master meditation. They complement their effect with aromatherapy. Essential oils of mint, lemon balm, chamomile quickly relieve nervous tension.
Sleep rituals help to effectively fall asleep. If you choose the same time for this, perform a certain list of actions (dinner, airing the room, hygiene before bedtime and other options), then with each such preparation, the body will tune in to fall asleep quickly.
People who are engaged in mental work during the day, hard physical work helps to cure insomnia. This is called the “peasant life effect.” After a heavy load, a person’s production of the hormone adenosine increases. This substance causes a feeling of fatigue, inhibits brain activity, which leads to early falling asleep.
It is difficult to fight insomnia during pregnancy. In the later stages, the deterioration in falling asleep is associated with a deterioration in lung ventilation and excitability of the nervous system.Most drugs are prohibited for use in pregnant women. Therefore, they choose simple ways to improve sleep: a comfortable position on the side of the bed with a raised edge, using a special pillow for pregnant women, airing the room and valerian tablets.
Medicines for insomnia
If home remedies do not cure insomnia, see your doctor. To restore normal sleep patterns, the cause of the disturbance must be addressed. Therefore, the first drugs will be used against the underlying disease.
Drug therapy begins with safe drugs. Your doctor may prescribe melatonin tablets, which are analogous to your own hormone. They treat sleep disorders and do not have many side effects. The development of addiction practically does not happen. But if used improperly, nightmares and headaches may appear. Therefore, the drug should be used after consulting a doctor.
A doctor can prescribe a pill for severe sleep disturbances. But they do not cure a disease if it is associated with stress, sleep hygiene disorders.Therefore, any treatment must be accompanied by preventive measures. Doxylamine-based drugs cure sleep disorders. They are available in the form of tablets, drops for oral administration. But prolonged use of sleeping pills is not recommended due to the risk of addiction.
Doctors consider insomnia as a psychological problem that trainings and cognitive-behavioral psychotherapy help to fight. Insomnia can be cured by using group therapy and hypnosis.These techniques help to eliminate disturbances even with a protracted chronic illness.
& nbsp
Tokareva Lyudmila Georgievna, therapist of medical offices 36.6
& nbsp
CONTRAINDICATIONS ARE AVAILABLE, CONSULT A SPECIALIST BEFORE USE
Untitled page
In the Kuzbass Center for the Prevention and Control of AIDS, together with non-profit organizations, new projects are being implemented to provide comprehensive support and assistance to people living with HIV.
“Rapid HIV Testing”
The main goal of the new Rapid HIV Testing project is to inform about HIV infection, early HIV detection in key populations, including those in the group increased risk including injecting drug users; released from places of imprisonment; partners of people living with HIV, etc. As part of the project, the mobile team of the center for the prevention and control of AIDS travels not only to popular public places (shopping centers, cinemas), but also to rehabilitation and adaptation centers, where they conduct testing and consultations on HIV prevention.Specialists then accompany those who tested positive and form their adherence to treatment – provide social and psychological support, help register with the AIDS Center and start antiretroviral therapy.
It is planned that about 2.5 thousand people will take part in the first stage of the project, which will last until the end of 2021.
“Medical, psychological and social support for people living with HIV”
17% of people with HIV in Kuzbass today do not register for dispensaries and do not take therapy.Involve those who know about their illness, but neglect therapy, skip appointments and risk that HIV, which can be controlled, can develop into AIDS, in clinical examinations and treatment. This is the task of yet another large-scale project. A large team of specialists from the Kuzbass AIDS Center and NGOs will work with non-adherent patients to help them learn to live with HIV. The organizers plan to reach 4.5 thousand people with the events.
In addition, within the framework of the project, the “START-club” will begin to work – a school for patients will be organized here for patients, which will provide psychological trainings, consultations, art therapy classes.
“In the spotlight”
A new stage of the “Spotlight” project will start in August – children (under 10 years old) and their parents living with HIV will join it. In addition, work will continue with other target groups – people over 50, women of fertile age, adolescents. In total, about 500 people will join the project.
“In the spotlight” has been implemented in Kuzbass for four years already – a multi-professional team of doctors, nurses, social workers and a peer consultant provides psychological and social support to people living with HIV.The specialists themselves undergo training and seminars within the framework of the project. Patients are taught about antiretroviral therapy, adherence to treatment, and other aspects of HIV-positive life through Patient School classes, self-help groups, and individual counseling sessions.
The first three projects are being implemented in cooperation with the Kemerovo Charitable Regional Public Foundation “Kuzbass Against Drugs and AIDS”.
“Invisible Families”
The fourth project, “Invisible Families”, is for families living with HIV.It was launched jointly with the Children + charitable foundation for helping children and adolescents with socially significant diseases (Moscow).
The project includes an educational stage for specialists – the foundation will conduct training in effective practices of social and psychological assistance to families living with HIV, using specially developed methods. Experts will apply these practices and knowledge in practice – every month for children and parents there will be meetings, individual psychological consultations, online training.
The project will improve the life situation of children and parents with HIV – at the first stage about 100 people will take part in it.
“Our goal is to help as much as possible those who have faced HIV in their lives. And since HIV is now not only a medical problem, but also a social one, we involve non-profit organizations and foundations in our work. We expect that thanks to new projects it will be possible to introduce new technologies into our work that will help motivate patients to be adherent to treatment and live fully, despite HIV, “commented Tatyana Bulatova, chief regional specialist on HIV infection, chief physician of the Kuzbass Center for Prevention and the fight against AIDS.
Active preventive work on HIV infection is carried out in Kuzbass on a regular basis and yields results. Over the past several years, the share of young people among those diagnosed has significantly decreased; thousands of people every year since 2016 undergo anonymous rapid HIV testing in mobile centers as part of the “Take an HIV test and act safely” campaign. And the literacy of the population is increasing – more than 93.5% of Kuzbass residents, according to research in 2020, know how HIV is transmitted and how to protect themselves and their loved ones, which means that the risk of their infection is reduced.
Information provided by the Kuzbass Center for the Prevention and Control of AIDS.
Page not found |
Page not found |
404.Page not found
Monthly archive
MonTueWedThuFtSaSun
22232425262728
2930
12
12
1
3031
12
15161718192021
25262728293031
123
45678910
12
17181920212223
31
2728293031
1
1234
567891011
12
891011121314
11121314151617
28293031
1234
12
12345
6789101112
567891011
12131415161718
19202122232425
3456789
17181920212223
24252627282930
12345
13141516171819
20212223242526
2728293031
15161718192021
22232425262728
2930
Archives
Tags
Settings
for visually impaired
90,000 Types of fungal diseases of the ENT organs | Medical Center “Doctor 2000”
Mycosis is an infectious and inflammatory disease caused by the pathogenic effect of fungi.
The main causative agents of fungal diseases of the upper respiratory tract are yeast-like fungi (genera Candida, Geotrichum), mold fungi (genera Aspergillus, Penicillium, Scopulariopsis, Mucor, Cephalosporium, Alternaria), pathogenic fungi that cause deep mycoses, sporotrichosis).
Clinical manifestations depend on the localization of the process.
Otomycosis – a fungal disease of the ear.
There are fungal otitis externa and otitis media.
Symptoms of external otitis media:
- Liquid discharge from the ear, crusting, blockages in the external auditory canal;
- Hypersensitivity of the auricle and behind the ear.
90,033 itching, pain, ear congestion;
90,033 headache, fever;
Symptoms of otitis media:
- hearing impairment, ear discharge, recurrent itching;
- local headache on the side of the affected ear and dizziness.
Pharyngomycosis is a fungal disease of the pharynx.
The most common candidiasis, which causes inflammation of the mucous membrane of the pharynx (pharyngitis), palatine tonsils (fungal tonsillitis, chronic fungal tonsillitis).
Mycoses of the nose and paranasal sinuses
Fungal rhinitis most often affects the nasal septum when isolated ulcers with irregular infiltrated edges appear in the anterior or middle third of it. Mycosis of the nasal cavity is more often found in persons of older age groups, which is facilitated by age-related changes in the mucous membrane, which create favorable conditions for the development of fungi.
With lesions of the paranasal sinuses, patients are worried about the complaints characteristic of ordinary sinusitis: nasal discharge, congestion, headache and others.
Laryngomycosis is a fungal disease of the larynx.
Mycoses of the larynx have a chronic course, characterized by a subtle onset of the disease, its gradual development and considerable duration.
Announcements – BUZ RA “Mayminskaya CRH”
Friday,
25
March
2016
Dear residents of the Maiminsky district, from April 24 to 30, 2016, the annual European Immunization Week is held.The aim of European Immunization Week is to increase vaccination coverage by achieving a deeper understanding that every child and adult needs and has the right to be protected from diseases preventable by means of specific prevention. European Immunization Week harnesses the power of advocacy and targeted outreach to raise awareness and ensure the success of immunization programs. During European Immunization Week, the issue of immunization is at the center of attention.All countries are invited to participate in European Immunization Week. What is immunization? Immunoprophylaxis is a method of individual or mass protection of the population from infectious diseases by creating or enhancing artificial immunity with the help of vaccines.
What is vaccination? Vaccination is the most effective and cost effective means of protection against infectious diseases known to modern medicine.Among the microorganisms that are successfully fought with the help of vaccinations: viruses (for example, pathogens of measles, rubella, mumps, poliomyelitis, hepatitis B, rotavirus infection) or bacteria (pathogens of tuberculosis, diphtheria, whooping cough, tetanus, hemophilic infection). There are several types of vaccines. Live vaccines are made on the basis of weakened strains of the microorganism with firmly fixed harmlessness. The vaccine strain after administration multiplies in the body of the vaccinated and causes a vaccinal infection process.In most of the vaccinated, the vaccine infection proceeds without pronounced clinical symptoms and leads to the formation of, as a rule, persistent immunity. An example of live vaccines are vaccines for the prevention of rubella, measles, poliomyelitis, tuberculosis, and mumps. Corpuscular vaccines contain weakened or killed germs (virions). Chemical vaccines are created from components extracted from a microbial cell. Recombinant Vaccines — These vaccines use genetic engineering techniques by inserting the genetic material of a microorganism into the antigen-producing yeast cells.After culturing the yeast, the desired antigen is isolated from it, purified, and a vaccine is prepared. Examples of such vaccines include the hepatitis B vaccine and the human papillomavirus (HPV) vaccine.
What does not vaccination entail? You can get those diseases that you can get vaccinated against; getting sick, you can infect others (including family members).
What vaccinations do we get? Whooping cough, diphtheria and tetanus.It is a triple vaccine that provides protection against all three diseases. The abbreviated name of the vaccine is DPT. Whooping cough is a dangerous and difficult disease, especially in the first year of a child’s life. The disease begins with runny nasal discharge, fever and cough, followed by bouts of indomitable coughing when the child suffocates. During these seizures, the baby’s skin may turn blue from lack of oxygen. Diphtheria is a serious illness that begins with angina and mild fever.A diphtheria film forms on the mucous membranes of the nose, throat, tonsils, it grows and blocks the nose and throat, causing difficulty breathing and attacks of suffocation. A severe attack can result in death. Tetanus is not contagious, but it is still a threat. It is caused by microbes carried from soil or dirt into an open wound (especially if it is a deep “puncture” wound) or in the place of a burn. Once inside the body, the microbes attack the nervous system, causing muscle spasms that make breathing difficult and can even be fatal.Polio attacks the nervous system and paralyzes muscles anywhere in the body. The result can be permanent paralysis if the disease attacks the lower limbs; if it attacks the respiratory muscles, artificial respiration may be required and the baby may even die. Poliomyelitis has been formally defeated, but it can be brought in from other countries. In addition, the polio virus can be shed in a child’s faeces for up to six weeks after vaccination, so unvaccinated adults can become infected by changing the diaper of a recently vaccinated child.Since there are three types of poliomyelitis virus, in order to achieve full protection of the child’s body, vaccination is carried out in three stages. Vaccination against measles, mumps and rubella is carried out by administering one vaccine with a triple effect. Measles is often considered a mild childhood illness, but it is not only uncomfortable for a child, but it can also be dangerous. It begins as a bad cold with cough, runny nasal discharge, watery eyes, and fever.Then reddish rashes appear on the face and on the body. Measles can be complicated by encephalitis (inflammation of the brain), which can cause brain damage, seizures, infections of the eyes and ears, croup, pneumonia, bronchitis, or death. Mumps causes headaches, fever, dry mouth and difficulty swallowing, and swelling under the jaw and ears. Mumps can cause deafness and encephalitis and is the most common cause of viral meningitis in children under 15. Rubella usually begins with a cough, sore throat, and runny nasal discharge, followed by a bright pink rash.Vaccination against rubella is important for all children: both boys and girls can transmit the disease to pregnant women, which is dangerous due to intrauterine fetal death or the development of severe pathology of the child. Women who develop measles or rubella early in pregnancy are advised to terminate the pregnancy.
Tuberculosis can affect the lungs and other parts of the body. Not so long ago, tuberculosis was a serious disease that required months of treatment; it was also one of those diseases that often led to the death of the patient.Prevention measures and universal vaccination have led to the practical eradication of the disease, but since the compulsory vaccination has ceased to be carried out, tuberculosis has again become a common disease.
Influenza is an acute respiratory viral disease that affects the organs of the upper and lower respiratory tract, fever, and headaches. The disease gives dangerous complications: myocarditis, pneumonia, meningitis, otitis media, sinusitis, etc. Everyone should understand the danger of an impending infection and take all measures to preserve their health.The surest way to protect yourself and your loved ones is to get vaccinated.
Take an active part in European Immunization Week! Protect yourself and your loved ones! Get vaccinated! Be healthy!
District infectious disease specialist Latyshkova N.
