Condition of hardening of the arteries. Atherosclerosis: Causes, Symptoms, and Treatment of Arterial Hardening
What is atherosclerosis. How does plaque buildup affect arteries. What are the main risk factors for developing atherosclerosis. How is atherosclerosis diagnosed and treated. Can atherosclerosis be prevented or reversed.
Understanding Atherosclerosis: The Silent Threat to Your Arteries
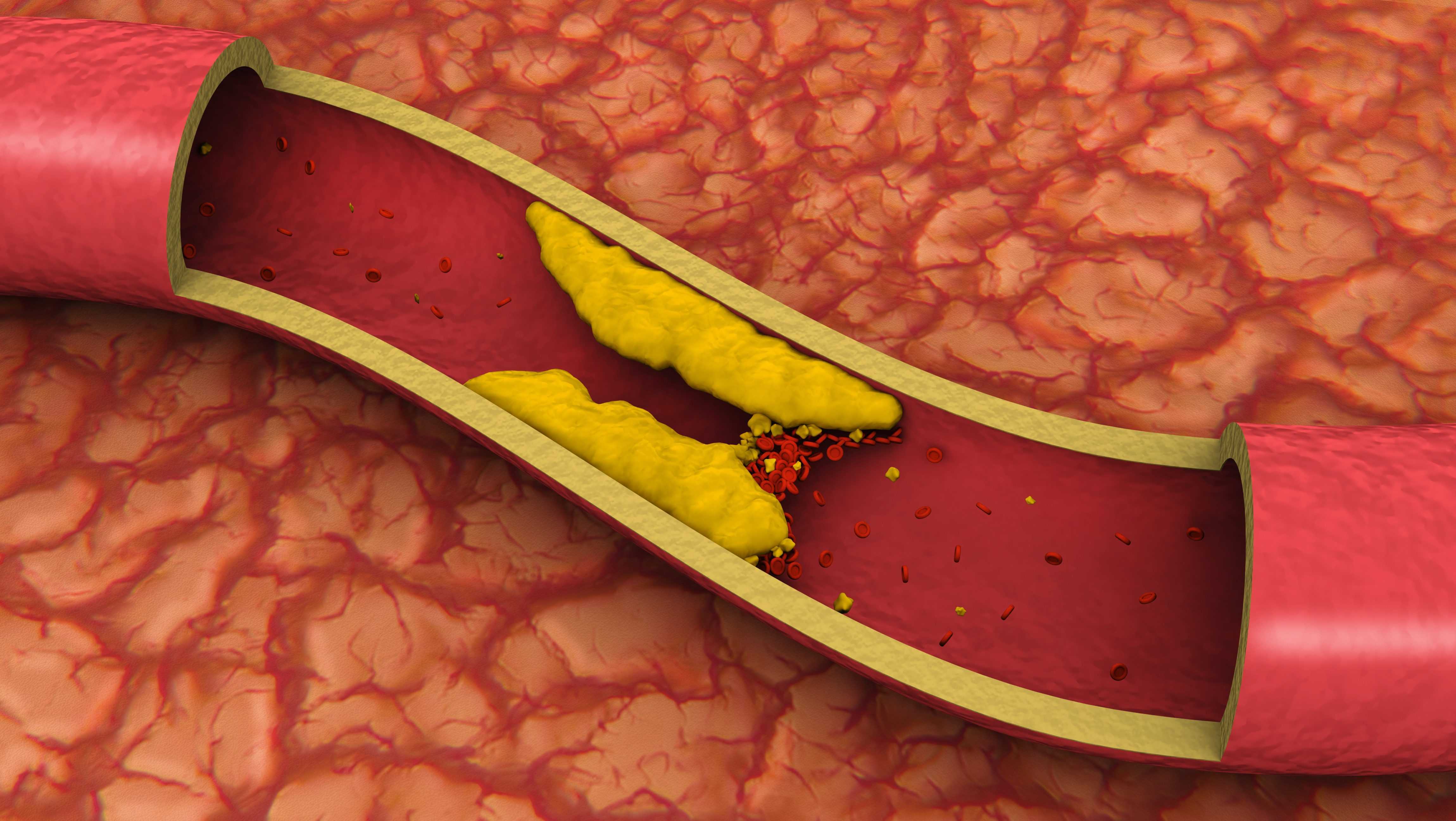
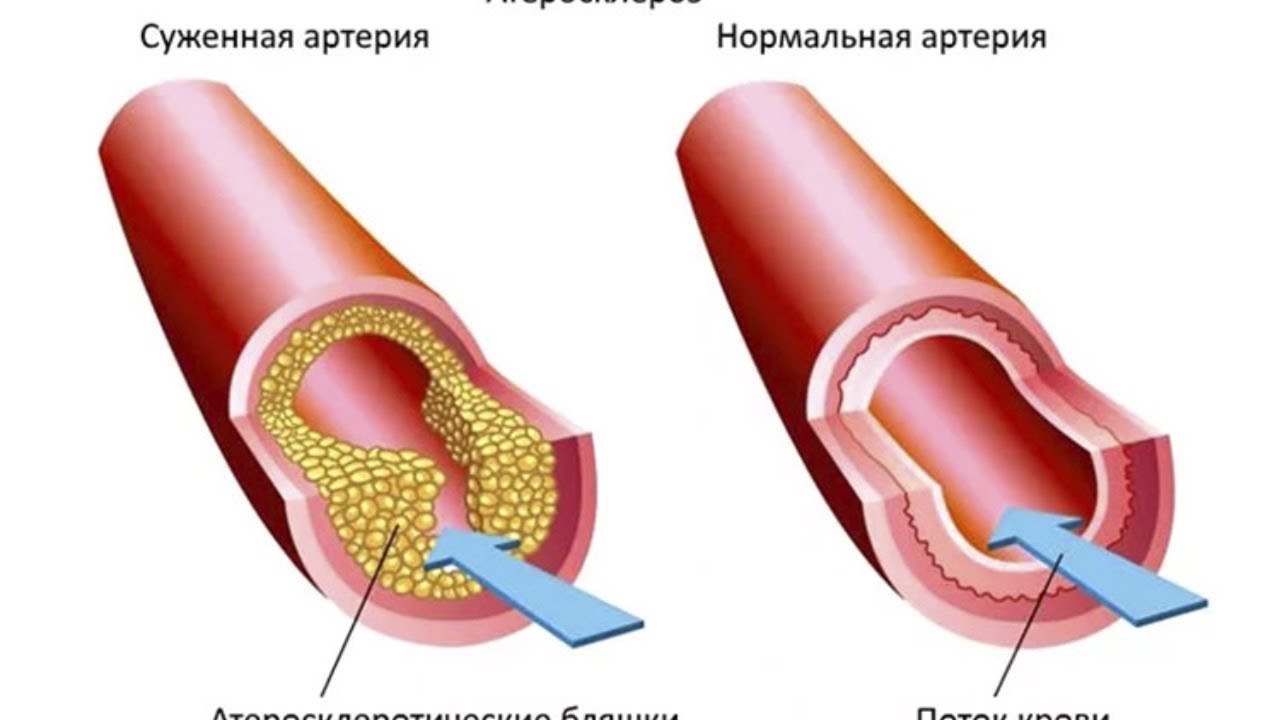
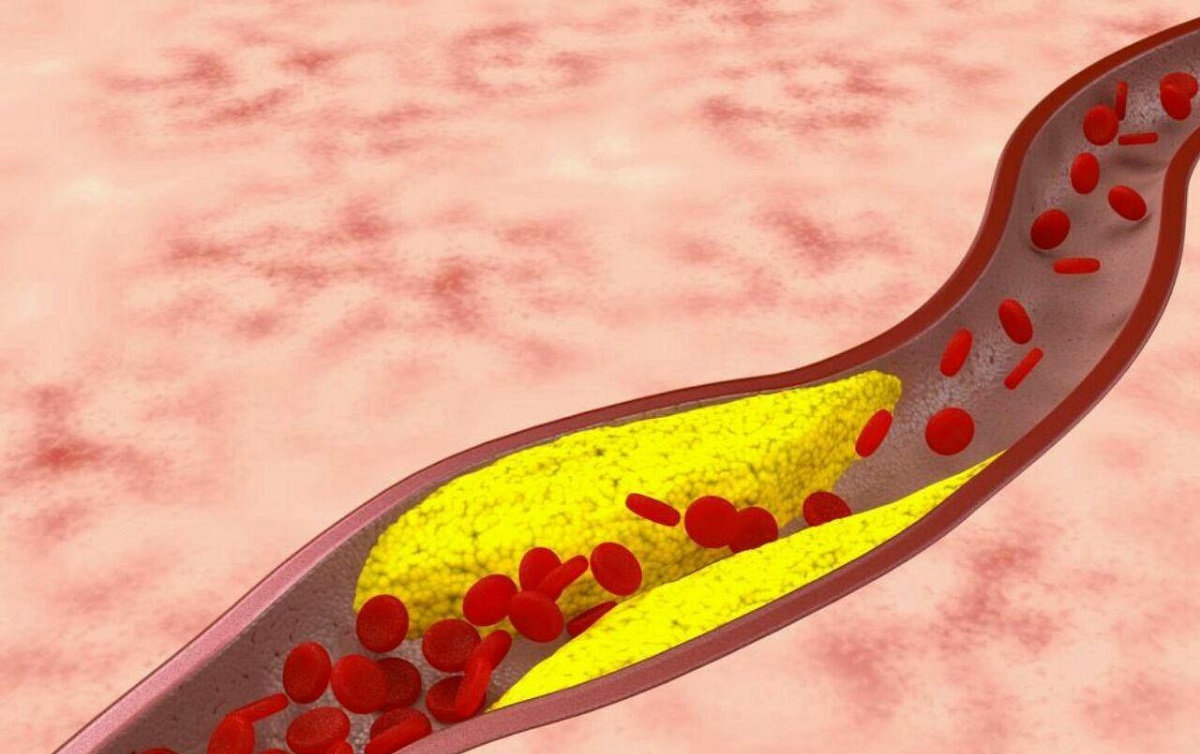
Atherosclerosis is a condition characterized by the hardening and narrowing of arteries due to the buildup of plaque. This process can significantly impair blood flow throughout the body, potentially leading to serious cardiovascular complications. But what exactly causes this condition, and how does it progress over time?
The Anatomy of Atherosclerosis
Arteries are blood vessels responsible for carrying oxygenated blood from the heart to various parts of the body. The inner lining of these arteries, known as the endothelium, plays a crucial role in maintaining smooth blood flow. When this lining becomes damaged, it sets the stage for atherosclerosis to develop.

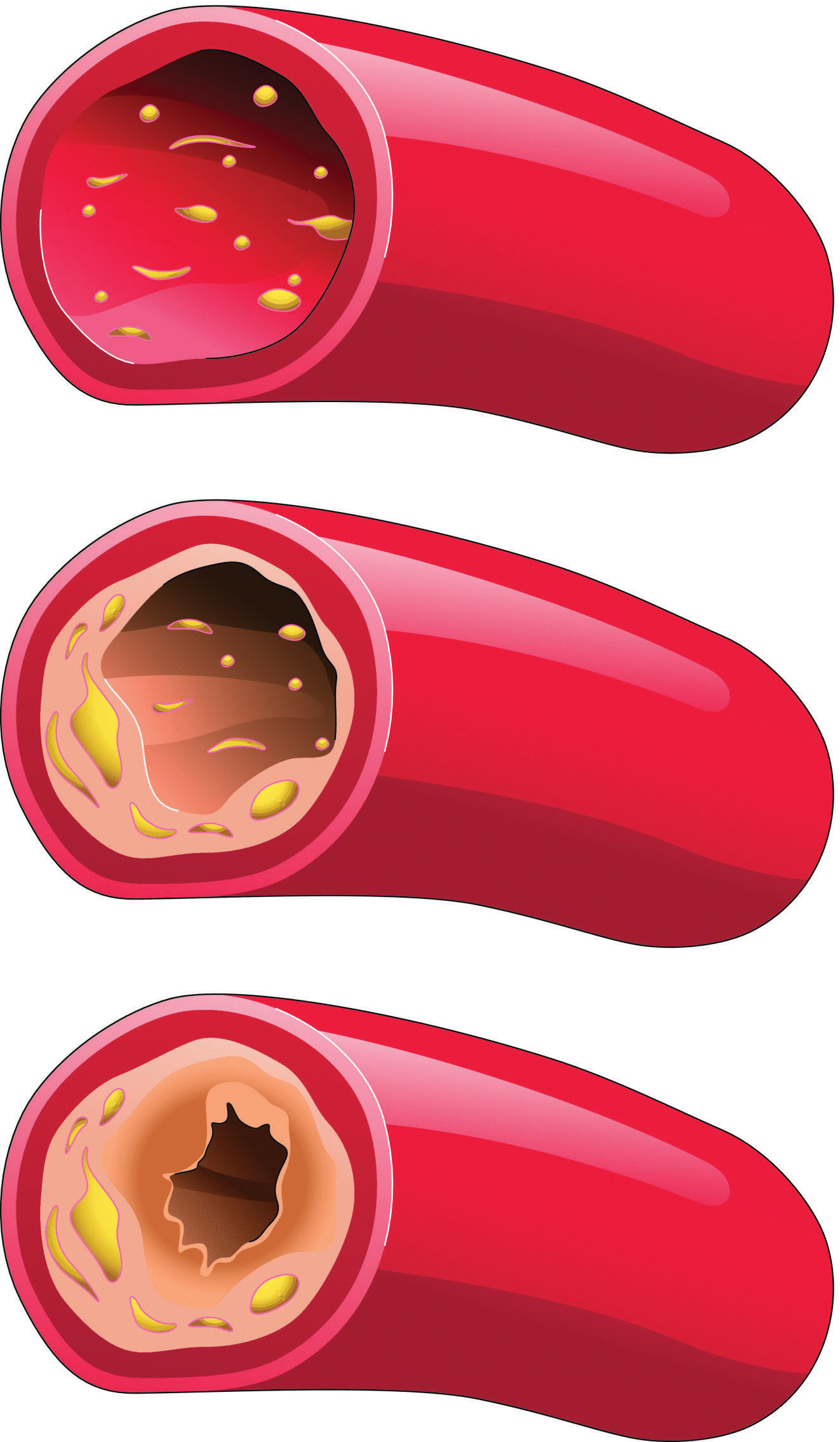
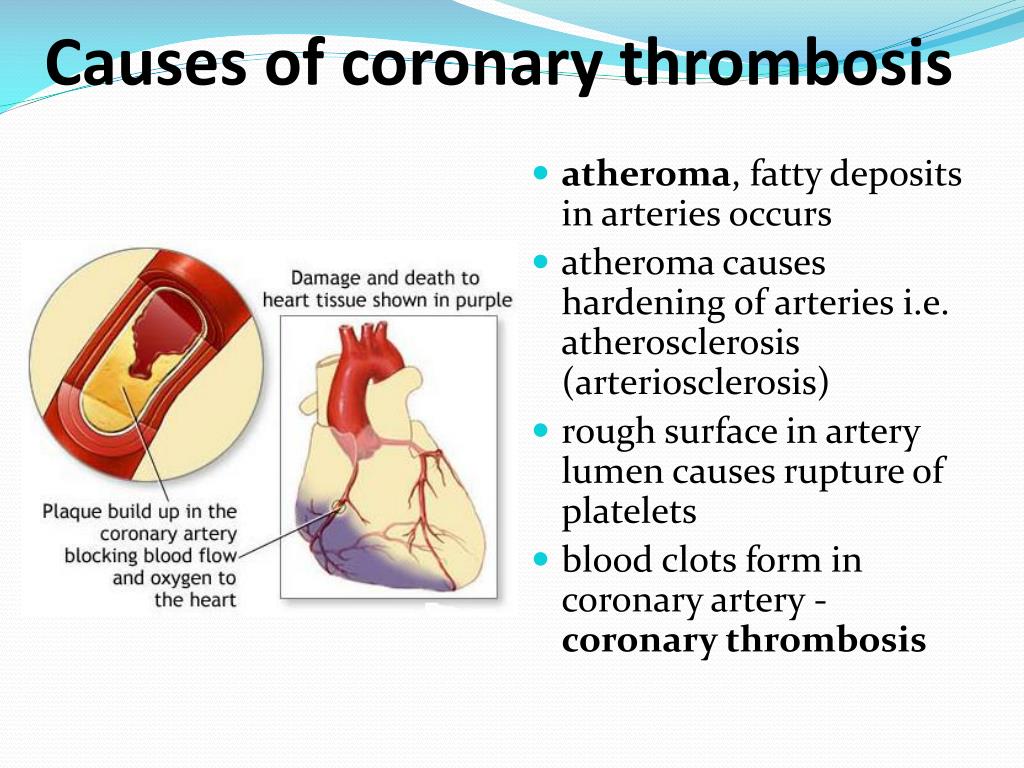
Plaque, composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin, begins to accumulate along the artery walls. As this buildup progresses, it narrows the arterial channel, reducing blood flow and oxygen supply to vital organs and tissues.
The Double Threat of Plaque
Plaque buildup poses two significant risks:
- Rupture: A piece of plaque can break off and travel through the bloodstream, potentially causing a blockage elsewhere.
- Thrombus formation: Narrowed arteries may lead to blood clot formation, which can adhere to the vessel wall and further obstruct blood flow.
In either scenario, the result can be a complete blockage of the affected artery, leading to serious health consequences depending on the location.
The Root Causes of Atherosclerosis: Unraveling the Mystery
While the exact cause of atherosclerosis remains somewhat elusive, researchers have identified several factors that contribute to its development and progression. Understanding these factors is crucial for both prevention and management of the condition.

Key Contributors to Atherosclerosis
- Elevated cholesterol and triglyceride levels
- High blood pressure
- Cigarette smoking
- Diabetes
- Obesity
- Chronic inflammation
Among these factors, smoking plays a particularly significant role in accelerating atherosclerosis progression, especially in the aorta, coronary arteries, and leg arteries. It not only increases the likelihood of fatty deposit formation but also speeds up plaque growth.
The Lifelong Progression of Atherosclerosis
Atherosclerosis is not a condition that develops overnight. Rather, it’s a slow, lifelong process that can begin as early as childhood. The rate of progression often accelerates with age, making it crucial to adopt preventive measures early in life.
Recognizing the Signs: Symptoms of Atherosclerosis
One of the challenges in dealing with atherosclerosis is that it often develops silently over many years without noticeable symptoms. However, as the condition progresses, certain signs may become apparent.
Common Symptoms Based on Affected Arteries
- Coronary arteries: Chest pain (angina) or shortness of breath
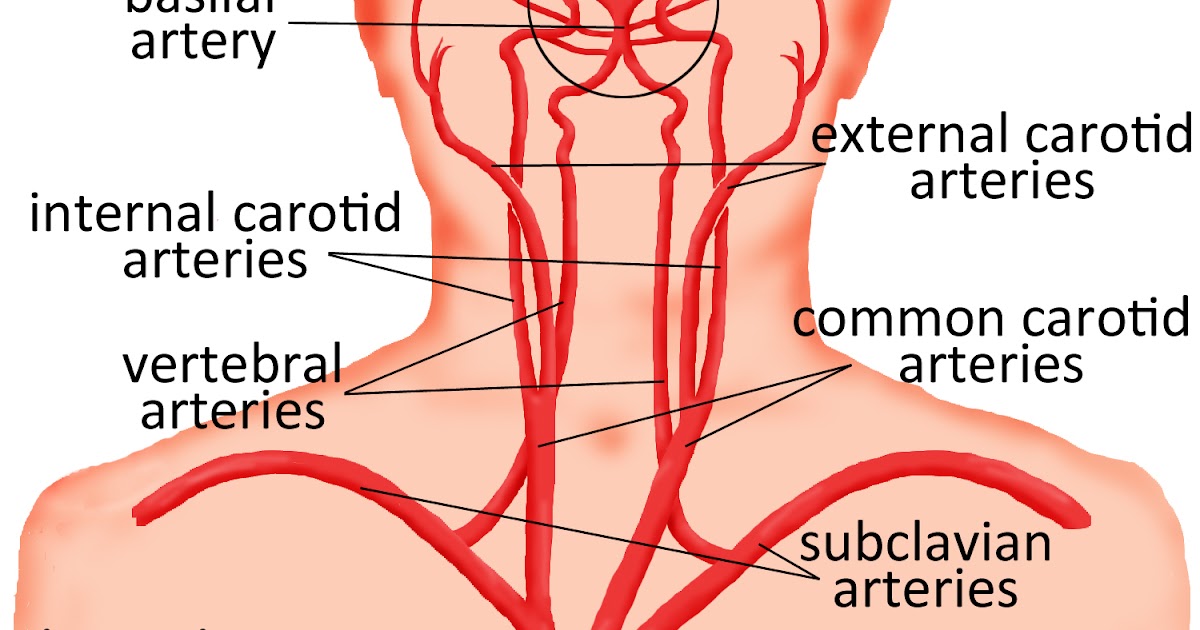
- Carotid arteries: Sudden weakness, numbness, or slurred speech
- Peripheral arteries: Pain or cramping in the legs, especially during physical activity
- Renal arteries: High blood pressure or decreased kidney function
It’s important to note that symptoms often don’t appear until an artery is severely narrowed or blocked. In some cases, a heart attack or stroke may be the first sign of underlying atherosclerosis.

Diagnosing Atherosclerosis: From Simple Tests to Advanced Imaging
Early detection of atherosclerosis is crucial for effective management and prevention of complications. Healthcare providers employ a variety of diagnostic tools and techniques to assess the presence and severity of the condition.
Common Diagnostic Approaches
- Physical examination: Checking for weak or absent pulses, abnormal sounds over arteries, or signs of aneurysms
- Blood tests: Assessing cholesterol levels, blood sugar, and markers of inflammation
- Electrocardiogram (ECG): Detecting irregularities in heart rhythm and signs of previous heart attacks
- Stress tests: Evaluating heart function during physical exertion
- Imaging studies: Using techniques like ultrasound, CT scans, or angiograms to visualize arteries and detect plaque buildup
The choice of diagnostic tools often depends on the suspected location of atherosclerosis and the presence of specific symptoms or risk factors.
The Impact of Plaque: Understanding Atherosclerosis Progression
As atherosclerosis advances, the accumulation of plaque in the arteries can lead to various complications, depending on the location and extent of the buildup.
Potential Consequences of Plaque Buildup
- Coronary heart disease: Reduced blood flow to the heart muscle
- Carotid artery disease: Impaired blood supply to the brain
- Peripheral artery disease (PAD): Decreased circulation in the extremities, particularly the legs
- Chronic kidney disease: Compromised renal function due to restricted blood flow
In severe cases, complete blockage of an artery can result in life-threatening events such as heart attacks, strokes, or tissue death (gangrene) in the affected area.
The Role of Inflammation in Atherosclerosis
Recent research has highlighted the significant role of inflammation in the development and progression of atherosclerosis. Chronic inflammation can damage the arterial lining, making it more susceptible to plaque formation and accelerating the disease process.
Treatment Strategies: Combating Atherosclerosis on Multiple Fronts
While atherosclerosis is a chronic condition, various treatment options are available to manage symptoms, slow disease progression, and reduce the risk of complications.
Lifestyle Modifications
- Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins
- Engaging in regular physical activity
- Quitting smoking and limiting alcohol consumption
- Managing stress through relaxation techniques or counseling
Medications
- Cholesterol-lowering drugs (statins)
- Blood pressure medications
- Antiplatelet agents to prevent blood clots
- Medications to control blood sugar in diabetic patients
Surgical Interventions
In severe cases or when medications are insufficient, surgical procedures may be necessary:
- Angioplasty and stent placement to open blocked arteries
- Endarterectomy to remove plaque from arteries
- Bypass surgery to create alternative routes for blood flow
The choice of treatment depends on various factors, including the severity of atherosclerosis, overall health status, and individual risk factors.
Prevention: The Key to Managing Atherosclerosis Risk
While some risk factors for atherosclerosis, such as age and family history, cannot be changed, many others can be modified through lifestyle choices and medical interventions.
Effective Prevention Strategies
- Maintaining a healthy weight
- Exercising regularly (aim for at least 150 minutes of moderate-intensity activity per week)
- Following a balanced, nutrient-rich diet
- Quitting smoking and avoiding secondhand smoke
- Managing chronic conditions like diabetes, high blood pressure, and high cholesterol
- Limiting alcohol consumption
- Reducing stress through relaxation techniques or mindfulness practices
Regular health check-ups and screenings can also help detect early signs of atherosclerosis, allowing for timely intervention and management.
Living with Atherosclerosis: Navigating the Challenges
A diagnosis of atherosclerosis can be daunting, but with proper management and lifestyle adjustments, many individuals can lead fulfilling lives while minimizing the risk of complications.
Coping Strategies for Atherosclerosis Patients
- Educate yourself about the condition and stay informed about new developments in treatment and management
- Adhere to prescribed medications and follow-up appointments with healthcare providers
- Join support groups or seek counseling to address emotional challenges associated with chronic illness
- Engage in cardiac rehabilitation programs to improve cardiovascular health and overall well-being
- Explore stress-reduction techniques such as meditation, yoga, or tai chi
- Maintain a positive outlook and focus on achievable goals for health improvement
By taking an active role in their care and making sustainable lifestyle changes, individuals with atherosclerosis can significantly improve their quality of life and reduce the risk of future cardiovascular events.
The Future of Atherosclerosis Management: Emerging Treatments and Research
As our understanding of atherosclerosis continues to evolve, researchers are exploring innovative approaches to prevent, detect, and treat this complex condition.
Promising Areas of Research
- Gene therapy to target specific genetic factors contributing to atherosclerosis
- Nanotechnology for targeted drug delivery to affected arteries
- Stem cell therapies to regenerate damaged arterial tissue
- Advanced imaging techniques for earlier and more precise detection of plaque buildup
- Novel anti-inflammatory drugs to address the underlying causes of atherosclerosis
While many of these approaches are still in the experimental stages, they offer hope for more effective and personalized treatments in the future.
The Role of Artificial Intelligence in Atherosclerosis Management
Artificial intelligence (AI) and machine learning algorithms are increasingly being applied to improve the diagnosis and prediction of atherosclerosis progression. These technologies can analyze vast amounts of patient data to identify patterns and risk factors that may not be apparent through traditional methods.
As research progresses, the integration of AI-driven tools with conventional diagnostic and treatment approaches may lead to more precise and tailored strategies for managing atherosclerosis.
Global Impact: Atherosclerosis as a Public Health Concern
Atherosclerosis and its associated cardiovascular diseases represent a significant global health burden. Understanding the broader implications of this condition is crucial for developing effective public health strategies.
The Economic Burden of Atherosclerosis
The costs associated with atherosclerosis extend beyond individual health impacts. Healthcare systems worldwide face substantial financial strain due to the treatment and management of atherosclerosis-related conditions. This economic burden includes direct medical costs, lost productivity, and the long-term care needs of affected individuals.
Disparities in Atherosclerosis Prevalence and Care
Research has shown that the prevalence and outcomes of atherosclerosis can vary significantly across different populations. Factors such as socioeconomic status, access to healthcare, and cultural dietary patterns can influence both the risk of developing atherosclerosis and the quality of care received.

Addressing these disparities requires a multifaceted approach, including:
- Improving access to preventive care and early screening programs
- Developing culturally sensitive health education initiatives
- Implementing policies to promote healthy lifestyles across all communities
- Enhancing research efforts to understand population-specific risk factors and treatment responses
By recognizing atherosclerosis as a global health challenge, we can work towards more comprehensive and equitable solutions that benefit individuals and societies worldwide.
Empowering Patients: The Role of Self-Management in Atherosclerosis Care
While medical interventions play a crucial role in managing atherosclerosis, patient engagement and self-management are equally important for achieving optimal outcomes.
Key Components of Effective Self-Management
- Medication adherence: Understanding the importance of prescribed medications and taking them as directed
- Regular monitoring: Keeping track of blood pressure, cholesterol levels, and other relevant health markers
- Lifestyle modifications: Consistently implementing dietary changes, exercise routines, and stress management techniques
- Symptom awareness: Recognizing and promptly reporting new or worsening symptoms to healthcare providers
- Proactive communication: Engaging in open dialogue with healthcare teams and asking questions about treatment options and progress
Empowering patients with the knowledge and tools to actively participate in their care can lead to improved health outcomes and a greater sense of control over the condition.

The Impact of Technology on Self-Management
Advancements in digital health technologies are revolutionizing the way patients manage chronic conditions like atherosclerosis. Mobile apps, wearable devices, and telemedicine platforms offer new opportunities for:
- Real-time monitoring of vital signs and symptoms
- Medication reminders and adherence tracking
- Virtual consultations with healthcare providers
- Access to educational resources and support communities
- Personalized lifestyle recommendations based on individual data
By leveraging these tools, patients can take a more active role in their care, potentially improving outcomes and reducing the need for frequent in-person medical visits.
As our understanding of atherosclerosis continues to grow, so does our ability to prevent, manage, and treat this complex condition. Through a combination of medical advancements, lifestyle interventions, and patient empowerment, we can work towards reducing the global burden of atherosclerosis and improving cardiovascular health for generations to come.

What is Atherosclerosis? | American Heart Association
Atherosclerosis and cholesterol
Plaque (fatty deposits) build up in your arteries is called atherosclerosis. These deposits are made up of cholesterol, fatty substances, cellular waste products, calcium and fibrin (a clotting material in the blood). Atherosclerosis is a type of arteriosclerosis. Arteriosclerosis means hardening (sclerosis) of the arteries.
As plaque builds up, the wall of the blood vessel thickens. This narrows the channel within the artery – reducing blood flow. That lessens the amount of oxygen and other nutrients reaching the body.
Watch an animation about atherosclerosis.
Where plaque develops, and the type of artery affected, varies with each person. Plaque may partially or totally block blood flow through large- or medium-sized arteries in the heart, brain, pelvis, legs, arms or kidneys. This can lead to conditions such as:
- Coronary heart disease (plaque in arteries in or leading to the heart)
- Angina (chest pain from reduced blood flow to the heart muscle)
- Carotid artery disease (plaque in neck arteries supplying blood to the brain)
- Peripheral artery disease, or PAD (plaque in arteries of the extremities, especially the legs)
- Chronic kidney disease
Plaque presents a double threat
Plaque itself can pose a risk. A piece of plaque can break off and be carried by the bloodstream until it gets stuck. And plaque that narrows an artery may lead to a blood clot (thrombus) that sticks to the blood vessel’s inner wall.
A piece of plaque can break off and be carried by the bloodstream until it gets stuck. And plaque that narrows an artery may lead to a blood clot (thrombus) that sticks to the blood vessel’s inner wall.
In either case, the artery can be blocked, cutting off blood flow.
If the blocked artery supplies the heart or brain, a heart attack or stroke occurs. If an artery supplying oxygen to the extremities (often the legs) is blocked, gangrene, or tissue death, can result.
Atherosclerotic cardiovascular disease (ASCVD) involves plaque buildup in arterial walls which includes conditions such as acute coronary syndrome and peripheral artery disease, and can cause a heart attack, stable or unstable angina, stroke, transient ischemic attack (TIA) or aortic aneurysm.
Download Reduce Your Risk of ASCVD (PDF) | Spanish (PDF)
How it starts and how it progresses
Atherosclerosis is a slow, lifelong progression of changes in the blood vessels that may start in childhood and get worse faster as you age.
The cause of atherosclerosis isn’t completely known.
Many scientists believe plaque begins when an artery’s inner lining (called the endothelium) becomes damaged. Four possible causes of such damage are:
- Elevated levels of cholesterol and triglycerides in the blood
- High blood pressure
- Cigarette smoking
- Diabetes
Smoking plays a big role in the progression of atherosclerosis in the aorta (the body’s main artery), coronary arteries and arteries in the legs. Smoking makes fatty deposits more likely to form, and it accelerates the growth of plaque.
Written by American Heart Association editorial staff and reviewed by science and medicine advisors. See our editorial policies and staff.
Last Reviewed: Nov 6, 2020
Related Articles
The Skinny on Fats
Watch, Learn and Live
See your cardiovascular system in action with our interactive illustrations and animations.
Symptoms, Causes, Diagnosis, and Treatment
Written by WebMD Editorial Contributors
- What Is Atherosclerosis?
- What Causes Atherosclerosis?
- What Are the Symptoms of Atherosclerosis?
- What Are the Risk Factors for Atherosclerosis?
- How Do You Diagnose Atherosclerosis?
- How Does Plaque Affect Atherosclerosis?
- What Are the Complications of Atherosclerosis?
- How Do You Treat Atherosclerosis?
- More
Atherosclerosis is a hardening and narrowing of your arteries caused by cholesterol plaques lining the artery over time. It can put blood flow at risk as your arteries become blocked.
You might hear it called arteriosclerosis or atherosclerotic cardiovascular disease. It’s the usual cause of heart attacks, strokes, and peripheral vascular disease — what together are called cardiovascular disease.
You can prevent and treat this process.
Arteries are blood vessels that carry blood from your heart throughout your body.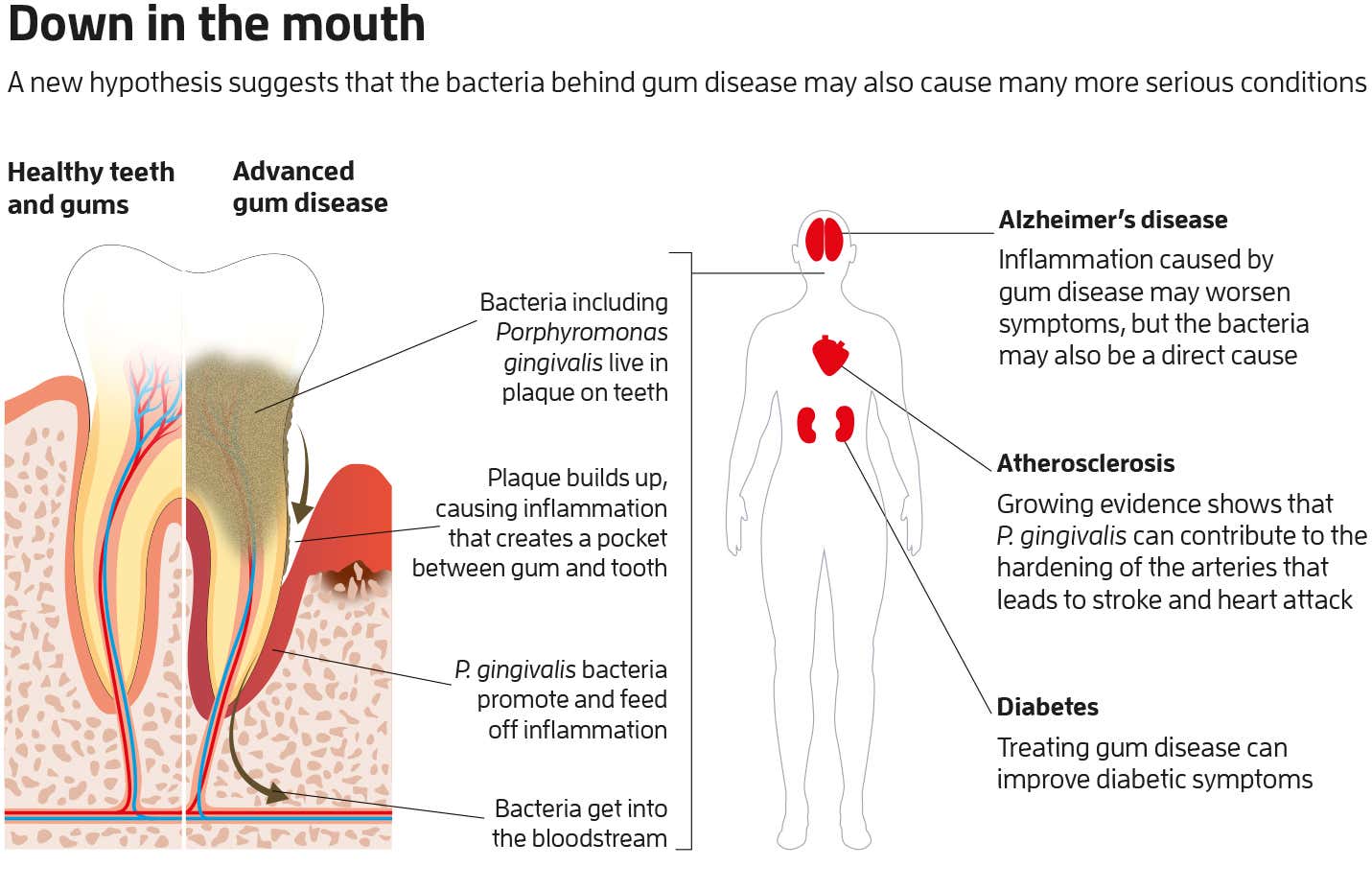 They’re lined by a thin layer of cells called the endothelium. It keeps the inside of your arteries in shape and smooth, which keeps blood flowing.
They’re lined by a thin layer of cells called the endothelium. It keeps the inside of your arteries in shape and smooth, which keeps blood flowing.
Atherosclerosis begins with damage to the endothelium. Common causes include:
- High cholesterol
- High blood pressure
- Inflammation, like from arthritis or lupus
- Obesity or diabetes
- Smoking
That damage causes plaque to build up along the walls of your arteries.
When bad cholesterol, or LDL, crosses a damaged endothelium, it enters the wall of your artery. Your white blood cells stream in to digest the LDL. Over the years, cholesterol and cells become plaque in the wall of your artery.
Plaque creates a bump on your artery wall. As atherosclerosis gets worse, that bump gets bigger. When it gets big enough, it can create a blockage.
That process goes on throughout your entire body. It’s not only your heart at risk. You’re also at risk for stroke and other health problems.
Atherosclerosis usually doesn’t cause symptoms until you’re middle-age or older. As the narrowing becomes severe, it can choke off blood flow and cause pain. Blockages can also rupture suddenly. That causes blood to clot inside an artery at the site of the rupture.
You might not have symptoms until your artery is nearly closed or until you have a heart attack or stroke. Symptoms can also depend on which artery is narrowed or blocked.
Symptoms related to your coronary arteries include:
- Arrhythmia, an unusual heartbeat
- Pain or pressure in your upper body, including your chest, arms, neck, or jaw. This is known as angina.
- Shortness of breath
Symptoms related to the arteries that deliver blood to your brain include:
- Numbness or weakness in your arms or legs
- A hard time speaking or understanding someone who’s talking
- Drooping facial muscles
- Paralysis
- Severe headache
- Trouble seeing in one or both eyes
Symptoms related to the arteries of your arms, legs, and pelvis include:
- Leg pain when walking
- Numbness
Atherosclerosis starts when you’re young.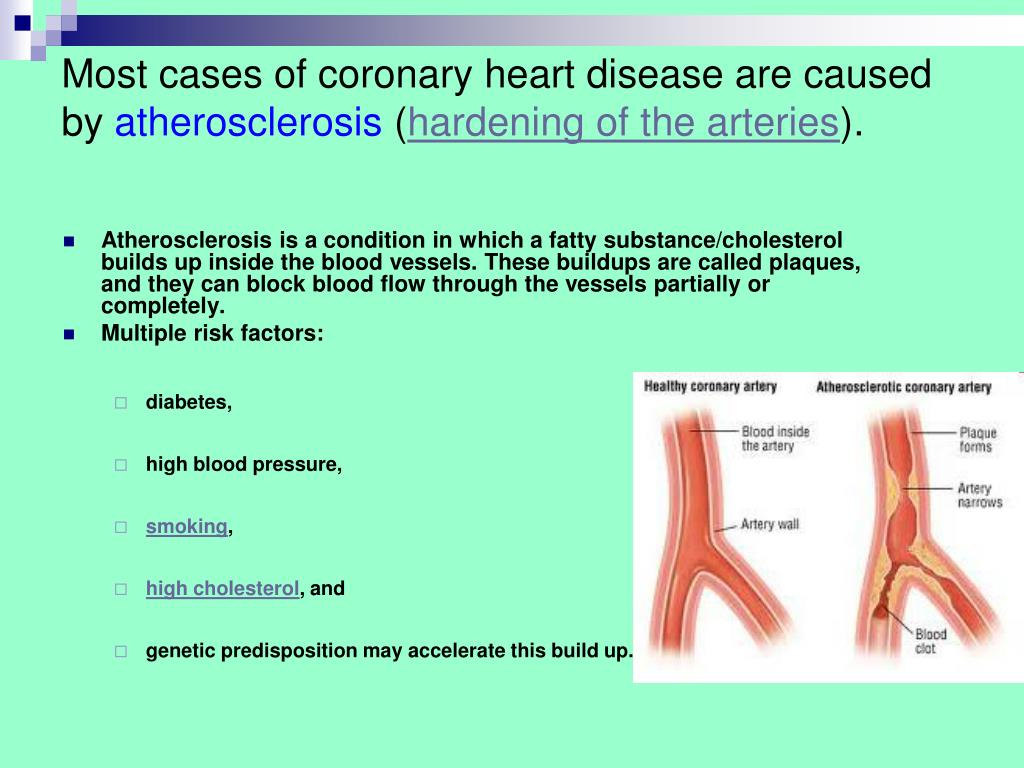 Research has found that even teenagers can have signs.
Research has found that even teenagers can have signs.
If you’re 40 and generally healthy, you have about a 50% chance of getting serious atherosclerosis in your lifetime. The risk goes up as you get older. Most adults older than 60 have some atherosclerosis, but most don’t have noticeable symptoms.
These risk factors are behind more than 90% of all heart attacks:
- Abdominal obesity (“spare tire”)
- Diabetes
- High alcohol intake (more than one drink for women, one or two drinks for men, per day)
- High blood pressure
- High cholesterol
- Not eating fruits and vegetables
- Not exercising regularly
- Smoking
- Stress
Rates of death from atherosclerosis have fallen 25% in the past 3 decades. This is because of better lifestyles and improved treatments.
Your doctor will start with a physical exam. They’ll listen to your arteries and check for weak or absent pulses.
You might need tests, including:
- Angiogram, in which your doctor puts dye into your arteries so they’ll be visible on an X-ray
- Ankle-brachial index, a test to compare blood pressures in your lower leg and arm
- Blood tests to look for things that raise your risk of having atherosclerosis, like high cholesterol or blood sugar
- CT scan or magnetic resonance angiography (MRA) to look for hardened or narrowed arteries
- EKG, a record of your heart’s electrical activity
- Stress test, in which you exercise while health care professionals watch your heart rate, blood pressure, and breathing
You might also need to see doctors who specialize in certain parts of your body, like cardiologists or vascular specialists, depending on your condition.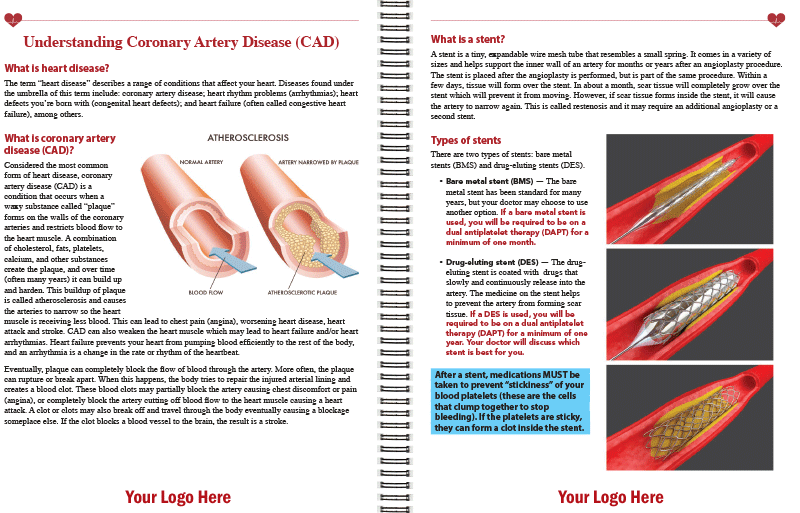
Plaques from atherosclerosis can behave in different ways.
They can stay in your artery wall. There, the plaque grows to a certain size and then stops. Since this plaque doesn’t block blood flow, it may never cause symptoms.
Plaque can grow in a slow, controlled way into the path of blood flow. Over time, it causes significant blockages. Pain in your chest or legs when you exert yourself is the usual symptom.
The worst happens when plaques suddenly rupture, allowing blood to clot inside an artery. In your brain, this causes a stroke; in your heart, a heart attack.
The plaques of atherosclerosis cause the three main kinds of cardiovascular disease:
- Coronary artery disease: Stable plaques in your heart’s arteries cause angina (chest pain). Sudden plaque rupture and clotting cause heart muscle to die. This is a heart attack.
- Cerebrovascular disease: Ruptured plaques in your brain’s arteries cause strokes with the potential for permanent brain damage.
 Temporary blockages in your artery can also cause something called transient ischemic attacks (TIAs), which are warning signs of a stroke. They don’t cause any brain injury.
Temporary blockages in your artery can also cause something called transient ischemic attacks (TIAs), which are warning signs of a stroke. They don’t cause any brain injury. - Peripheral artery disease: When the arteries in your legs narrow, it can lead to poor circulation. This makes it painful for you to walk. Wounds also won’t heal as well. If you have a severe form of the disease, you might need to have a limb removed (amputation).
Complications of atherosclerosis include:
- Aneurysms
- Angina
- Chronic kidney disease
- Coronary or carotid heart disease
- Heart attack
- Heart failure
- Peripheral artery disease
- Stroke
- Unusual heart rhythms
Once you have a blockage, it’s generally there to stay. But with medication and lifestyle changes, you can slow or stop plaques. They may even shrink slightly with aggressive treatment.
Lifestyle changes: You can slow or stop atherosclerosis by taking care of the risk factors.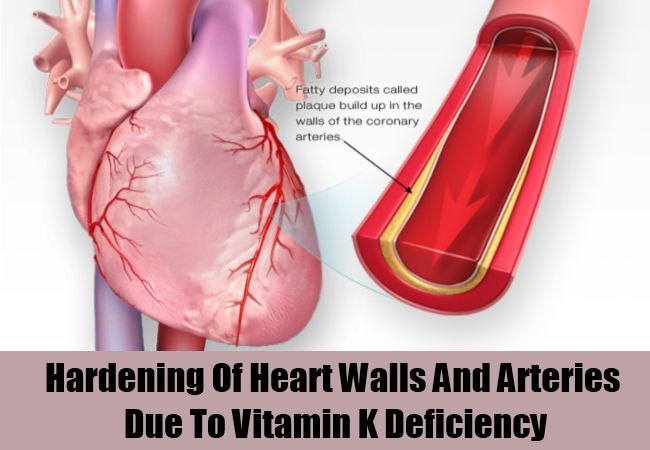 That means a healthy diet, exercise, and no smoking. These changes won’t remove blockages, but they’re proven to lower the risk of heart attacks and strokes.
That means a healthy diet, exercise, and no smoking. These changes won’t remove blockages, but they’re proven to lower the risk of heart attacks and strokes.
Medication: Drugs for high cholesterol and high blood pressure will slow and may even halt atherosclerosis. They lower your risk of heart attack and stroke.
Your doctor can use more invasive techniques to open blockages from atherosclerosis or go around them:
- Angiography and stenting: Your doctor puts a thin tube into an artery in your leg or arm to get to diseased arteries. Blockages are visible on a live X-ray screen. Angioplasty (using a catheter with a balloon tip) and stenting can often open a blocked artery. Stenting helps ease symptoms, but it does not prevent heart attacks.
- Bypass surgery: Your doctor takes a healthy blood vessel, often from your leg or chest, and uses it to go around a blocked segment.
- Endarterectomy: Your doctor goes into the arteries in your neck to remove plaque and restore blood flow.
 They also may place a stent higher risk patients.
They also may place a stent higher risk patients. - Fibrinolytic therapy: A drug dissolves a blood clot that’s blocking your artery.
Your doctor will discuss the complications of these procedures with you.
Top Picks
Arterial stenosis – symptoms, causes, signs, diagnosis and treatment in “SM-Clinic”
This disease is treated by a Cardiologist
, Cardiovascular Surgeon
- What is it?
- Symptoms of arterial stenosis
- Causes of arterial stenosis
- Diagnosis of arterial stenosis
- Methods of treatment
- Surgical treatment
- Doctors
Symptoms of arterial stenosis
In the early stages, arterial stenosis does not manifest itself. This is the main danger of the disease: a person can live for a long time without realizing the threat hanging over him.
This is the main danger of the disease: a person can live for a long time without realizing the threat hanging over him.
The further clinical picture of the disease directly depends on the location of the artery damaged by stenosis. So, with damage to the vessels of the brain in humans, there are manifestations of insufficient blood circulation and nutrition of the brain; with blockage of the arteries of the heart, the patient feels symptoms of heart failure, etc.
Carotid narrowing symptoms
The carotid artery is responsible for supplying nutrients to the brain. If its patency is disturbed, the following manifestations occur:
- dizziness
- blackout
- tinnitus
- weakness
Arterial stenosis often precedes ischemic stroke. Pathology can be recognized by the following symptoms:
- nausea and vomiting
- coordination difficulties
- headache
- speech problems
- numbness of one of the limbs and half of the face
Symptoms of stenosis of the arteries of the legs
Narrowing of the lumen of the vessels of the lower extremities, in contrast to stenosis of the carotid artery, is not difficult to recognize at any stage.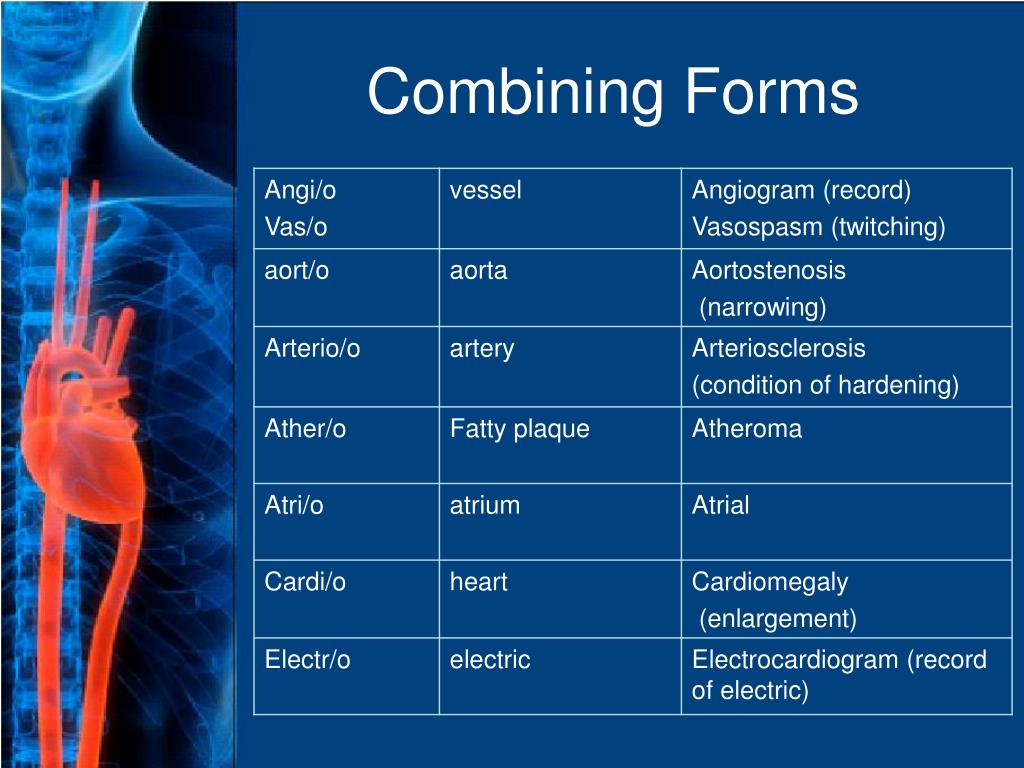 The main manifestations of the disease include:
The main manifestations of the disease include:
- pallor of the skin of the legs
- pain in legs
- lameness
- weakness in the muscles of the legs
- occurrence of ulcers on the extremities
Symptoms of stenosis of the arteries of the heart
The following symptoms indicate blockage of the vessels of the heart:
- shortness of breath
- increased heart rate
- chest pain
- swelling of limbs
Symptoms of renal artery stenosis
Renal artery stenosis provokes the development of ischemic nephropathy – renal failure. The pathological condition is characterized by several features:
- arterial hypertension
- scanty urination
- swelling of limbs and face
- weakness, poor performance
- gastrointestinal disorders (advanced)
Pulmonary artery stenosis
Pulmonary artery stenosis narrows the outflow tract of the right ventricle, which interferes with blood flow to the trunk of the lung. The disease is manifested by the following symptoms:
The disease is manifested by the following symptoms:
- dizziness
- weakness
- shortness of breath
- palpitations
- prone to fainting
- discoloration of the skin (pallor or blueness)
Causes of arterial stenosis
Arterial stenosis does not have a single cause. Most often, the occurrence of the disease is associated immediately with a group of external and internal factors.
First of all, it is necessary to note atherosclerosis – the accumulation of cholesterol plaques on the arterial walls. The formation of atherosclerotic plaques provokes a narrowing of the lumen of the vessels from the inside, causing vascular pathology.
Other causes of the development of the disease:
- congenital anomalies in the structure of blood vessels – tortuosity, hypoplasia
- dissection (dissection) of the walls of the artery
- compression of vessels by benign or malignant neoplasms
- increased thrombus formation
- diabetes mellitus
- metabolic disorder
- strong blow, concussion
- inflammatory vascular diseases – vasculitis, arteritis, Horton’s disease, Takayasu’s disease, etc.

Note that there are certain factors that significantly increase the risk of arterial stenosis. So, the disease is more likely to affect people who are obese, lead a sedentary lifestyle, abuse alcohol, smoke and consume large amounts of fatty foods.
Get advice
If you experience these symptoms, we recommend that you make an appointment with your doctor. Timely consultation will prevent negative consequences for your health.
To learn more about the disease, prices for treatment and sign up for a consultation with a specialist, you can call:
+7 (495) 292-39-72
Request a call back
Book online
Why SM-Clinic?
1
Treatment is carried out in accordance with clinical guidelines
2
Comprehensive assessment of the nature of the disease and treatment prognosis
3
Modern diagnostic equipment and own laboratory
4
High level of service and balanced pricing policy
Diagnosis of arterial stenosis
At the initial examination, the doctor interviews the patient, listens to complaints and conducts an examination. During the examination, the specialist measures blood pressure and pulse, listens to the heart rhythm, and conducts a visual examination of the patient’s skin. During the conversation, the doctor finds out the presence of chronic diseases in the anamnesis, learns about taking blood-clotting drugs, the presence of identified anomalies in the structure of blood vessels. Then the patient is sent for additional studies to clarify the diagnosis.
During the examination, the specialist measures blood pressure and pulse, listens to the heart rhythm, and conducts a visual examination of the patient’s skin. During the conversation, the doctor finds out the presence of chronic diseases in the anamnesis, learns about taking blood-clotting drugs, the presence of identified anomalies in the structure of blood vessels. Then the patient is sent for additional studies to clarify the diagnosis.
In the medical center “SM-Clinic” the diagnosis of arterial stenosis is performed by the following methods:
- arterial doppler ultrasound
- Computed angiography of vessels
- magnetic resonance angiography
- ECG of the heart
- UAC (general blood test), OAM (general urine test)
Methods of treatment
Depending on the stage of the disease, conservative or surgical treatment may be used.
Therapeutic treatment
In the early stages of the disease, conservative methods of treatment are used.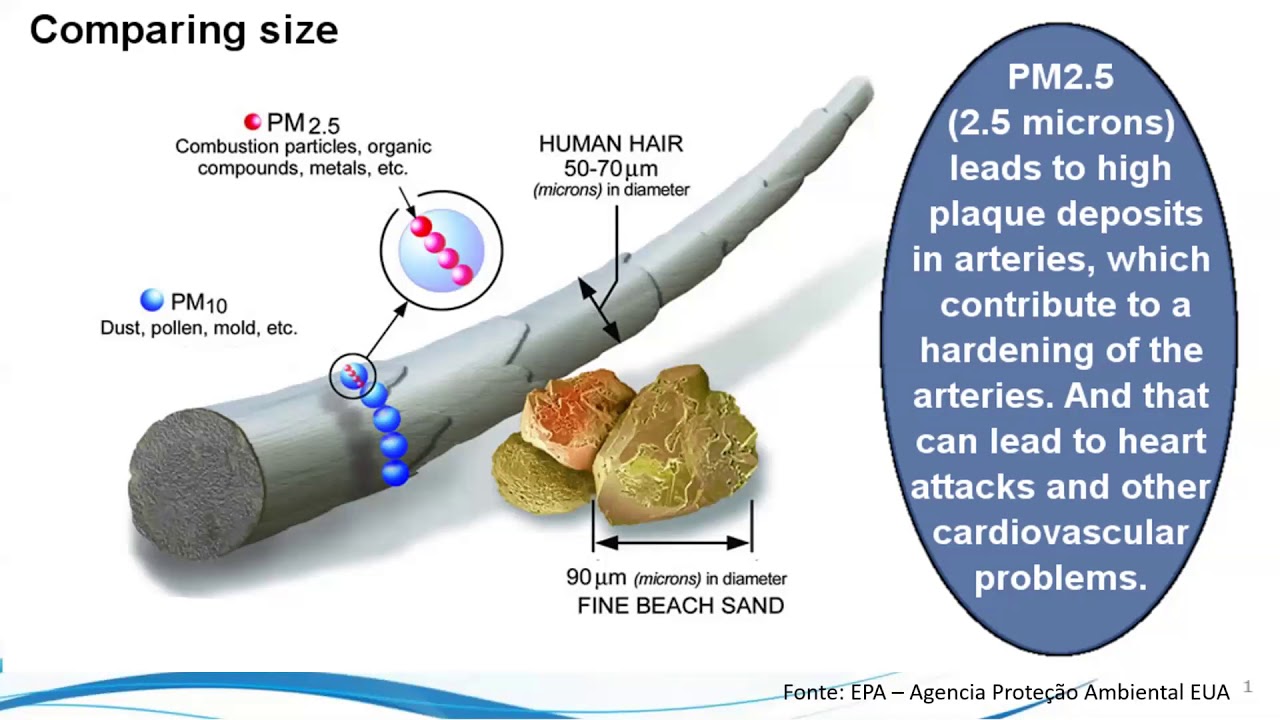 Therapy varies depending on the localization of the narrowing of the lumen of the vessels and the underlying cause of the development of pathology. So, if vascular stenosis is provoked by the formation of a blood clot in the artery, the patient is prescribed antithrombotic drugs. With atherosclerotic vascular lesions, drugs are prescribed that reduce the level of cholesterol in the blood.
Therapy varies depending on the localization of the narrowing of the lumen of the vessels and the underlying cause of the development of pathology. So, if vascular stenosis is provoked by the formation of a blood clot in the artery, the patient is prescribed antithrombotic drugs. With atherosclerotic vascular lesions, drugs are prescribed that reduce the level of cholesterol in the blood.
The patient also needs to take drugs that eliminate the symptoms of the disease – drugs that reduce blood pressure, anti-inflammatory and painkillers.
Surgical treatment
In the event that the narrowing of the lumen of the vessel has reached more than 50%, as well as in the presence of external symptoms (for example, previous ischemic strokes), conservative methods of treatment will not help to achieve the desired effect. In this case, doctors resort to surgical intervention.
The specialists of the Center for Surgery “SM-Clinic” are fluent in several methods of surgical intervention at once:
- Balloon angioplasty is an intravascular operation that restores normal arterial patency.
 During the operation, a small balloon is inserted into the vessel, when it is expanded, the accumulated plaques are removed, and the lumen of the vessel expands. The operation is indispensable for the atherosclerotic nature of stenosis.
During the operation, a small balloon is inserted into the vessel, when it is expanded, the accumulated plaques are removed, and the lumen of the vessel expands. The operation is indispensable for the atherosclerotic nature of stenosis. - Vascular stenting is a modern minimally invasive technique for treating arterial stenosis, during which a stent is introduced into the lumen of the vessel – a special frame that strengthens the walls of the artery and prevents its re-narrowing. As a result of the operation, the functioning of blood vessels is restored and the blood supply to human organs is improved.
- Vascular bypass surgery is a commonly used operation that allows you to redirect blood flow around a narrowed vessel by forming a new channel. As a result of the operation, blood stops flowing through the damaged vessels, it goes around. This restores circulation.
The SM-Clinic Surgery Center is a modern world-class medical care. Our specialists help to cope with even the most difficult clinical situations.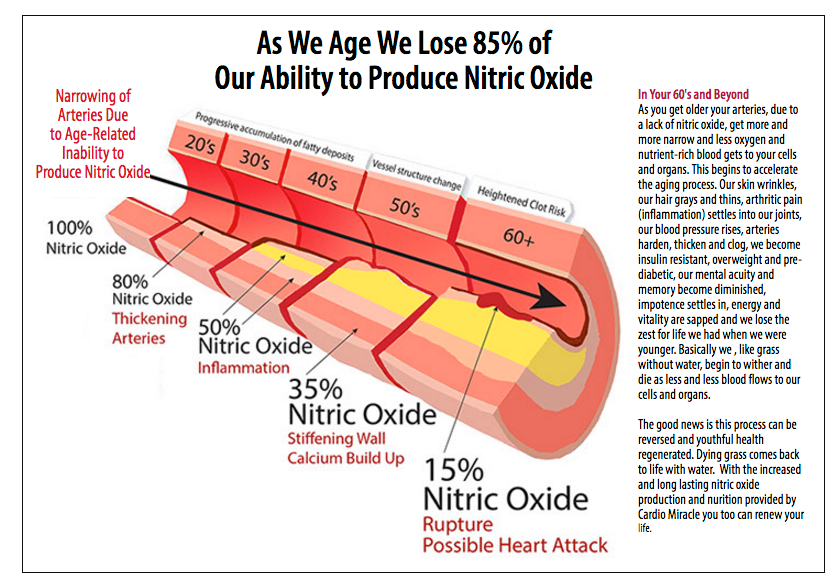
Related video
Center for Cardiovascular Surgery “SM-Clinic”. Angiograph
How is the operating room of the Center for Cardiovascular Surgery arranged?
>
Diseases referred to Cardiologist
Antiphospholipid syndrome
aortic stenosis
Heart arythmy
Atherosclerosis
Atrioventricular block
Bradycardia
Vegetovascular dystonia (VVD)
hypertension
Hypertensive crisis
Hypertension
Myocardial hypertrophy
Hypercholesterolemia
myocardial infarction
Ischemic heart disease (CHD)
Cardialgia
cardiomyopathy
Atrial fibrillation
Myocardial dystrophy
Myocarditis
Mitral insufficiency
mitral stenosis
Conduction disorders of the heart
Heart rhythm disorders
Aortic valve insufficiency
Cardiopsychoneurosis
Pericarditis
Heart disease
Postinfarction cardiosclerosis
rheumatic heart disease
cardiac asthma
Heart failure
Wolff-Parkinson-White Syndrome (WPW)
Marfan syndrome
Obstructive sleep apnea syndrome (OSAS)
Angina pectoris (angina pectoris)
Tachycardia
Extrasystole of the heart
Endocarditis
Diseases referred by Cardiovascular Surgeon
Cardiac Arrhythmia
Atherosclerosis
Atherosclerosis of the vessels of the lower extremities
Atrioventricular block
Bradycardia
myocardial infarction
Ischemic heart disease (CHD)
Ischemia of the lower extremities
Conduction disorders of the heart
Heart rhythm disorders
Heart disease
Tachycardia
vein thrombosis
Thrombophlebitis
Phlebitis
Endocarditis
All doctors
VDNKh metro station
Belorusskaya metro station
Lesnaya, d. 57, bld. 2 m. Sevastopolskaya
57, bld. 2 m. Sevastopolskaya
m. Chertanovskaya
Krylatskoye metro station
Voykovskaya metro station
Staropetrovsky proezd, 7A, building 22
Clara Zetkin, 33 bldg. 28
Baltiyskaya metro station
Staropetrovsky proezd, 7A, building 22
st. Clara Zetkin, 33 bldg. 28
Maryina Roshcha
Novye Cheryomushki
Vodny Stadion
Ulitsa 1905 Goda
Yugo-Zapadnaya
Sukha revskaya
All doctors
Loading
Licenses
Go to the license sectionGo to the legal information section
Thoracic aortic atherosclerosis – causes, symptoms, who treats
What should be done to diagnose and treat atherosclerosis of the thoracic aorta ? To solve this problem, the first step for the patient is to make an appointment with a therapist.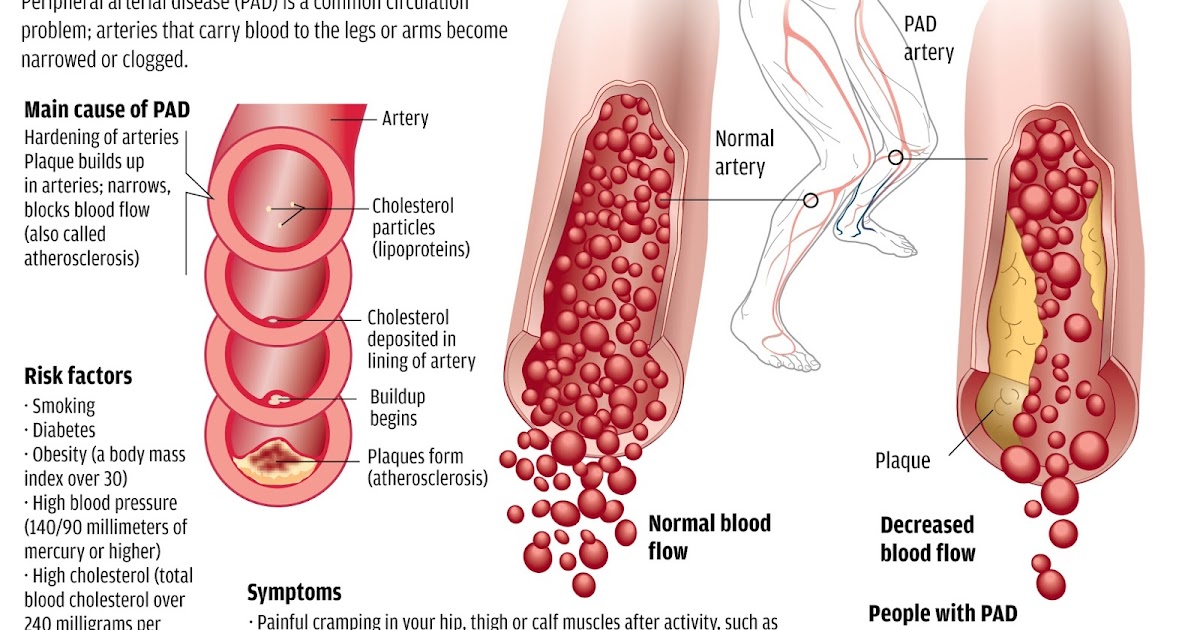 After the initial examination, the doctor may prescribe additional examinations:
After the initial examination, the doctor may prescribe additional examinations:
- Consultation with a pulmonologist
- Laboratory tests
- CT thoracic aorta
- Ultrasound of the thoracic aorta and its branches
- Lung CT with contrast
- Aortography
- exercise tolerance test
- ECG.
Thoracic aortic atherosclerosis is a narrowing of the aorta (the main arteries) caused by plaque buildup. The aorta is the main blood vessel that carries oxygen and nutrients from the heart to the rest of the body. As the body ages, fats, cholesterol, and calcium can accumulate in the aorta and its branches and form plaque. The accumulation of plaque makes it difficult for blood to flow through the arteries a. The condition can lead to a lack of blood and oxygen. The plaque can also collapse, causing the formation of a blood clot. Left untreated, atherosclerosis can lead to stroke or bleeding. Atherosclerosis is a fairly common problem associated with aging. This condition is preventable and there are many successful treatment options.
This condition is preventable and there are many successful treatment options.
Symptoms of atherosclerosis of the thoracic aorta
Most symptoms of atherosclerosis of the thoracic aorta do not appear until a blockage occurs. General symptoms of the disease:
- chest pain or angina pectoris
- irregular breathing
- fatigue.
It is also important to know the symptoms of a heart attack. This condition may be caused by atherosclerosis and require immediate medical attention:
- chest pain or discomfort
- pain in shoulders, back, neck, arms and jaw
- abdominal pain
- irregular breathing
- sweating
- nausea or vomiting
- feeling of impending doom, panic.
Causes of atherosclerosis of the thoracic aorta
When plaque builds up and the arteries of the heart become hard and inflamed, blood cannot circulate efficiently to the rest of the body. This prevents organs and tissues from receiving the oxygenated blood they need to function. The most common causes of hardening of the arteries are the following factors and conditions:
This prevents organs and tissues from receiving the oxygenated blood they need to function. The most common causes of hardening of the arteries are the following factors and conditions:
- High cholesterol
- Diet
- Aging.
Which doctor diagnoses atherosclerosis of the thoracic aorta
A vascular surgeon or cardiologist will perform a physical examination to detect symptoms of atherosclerosis, such as:
- weak pulse
- aneurysm – abnormal protrusion or expansion of an artery due to weakness of the arterial wall
- slow wound healing indicating limited blood flow
- Noise or whistling sound made by blood as it passes through a blocked artery.
The doctor examines the heart with a stethoscope to look for abnormal sounds. In addition, the patient is assigned specialized tests:
- blood test to check cholesterol levels
- Ultrasound of the thoracic aorta
- magnetic resonance angiography of the aorta
- cardiac angiogram, which is a type of chest x-ray that is done after a radioactive tracer 9 is injected into an artery0006
- electrocardiogram (ECG) measures electrical activity in the heart to identify areas of reduced blood flow
- EMT or exercise tolerance test that monitors heart rate and blood pressure during cardiac stimulation with exercise or special drugs.

Share:
The best doctors in St. Petersburg
Gavrilko Tatyana Andreevna
Rating: 4.7 / 5
Enroll
Prokopets Anna Igorevna
Rating: 4.9 / 5
Enroll
Sabelnikov Vladimir Vasilievich
Rating: 4.5 / 5
Enroll
Toshchev Alexey Andreevich
Rating: 4.8 / 5
Enroll
Scientific sources:
- Endovascular methods in the treatment of patients with multifocal atherosclerosis / A.V.Ter-Akopyan // Annals of Surgery. -2002.-№1.-S. 11-17.
- Mishalov V.G. Features of surgical treatment of atherosclerotic lesions of brachiocephalic arteries in patients with concomitant coronary heart disease / V.G. Mishalov, N.Yu. Litvinov / 2003 – No. 1. – S. 90-96.
- Belenkov Yu.N., Ternovoy S.K., Sinitsyn V.E. Magnetic resonance imaging of the heart and blood vessels. M.: Vidar, 1997. – 144 p.
- Mitkov V.V. Physics of Ultrasound// Clinical Guide to Ultrasound Diagnostics/ Ed.
 V.V. Mitkov. M.: Vidar. 1996. V.1. P.9-24.
V.V. Mitkov. M.: Vidar. 1996. V.1. P.9-24. - Bessemeltsev S.S., Abdulkadyrov K.M. Ultrasound diagnostics in hematological practice// St. Petersburg. 1997. S. 178.
Useful information
Aneurysm of the descending thoracic aorta
What should be done to diagnose and treat an aneurysm of the descending thoracic aorta? To solve this problem, the first step for the patient is to make an appointment with a vascular surgeon. After the initial examination, the doctor may prescribe additional studies:
Consultation with a pulmonologist
Lab tests
CT scan of the pulmonary aorta
Lung CT with contrast
Ultrasound of the heart
Ultrasound of the thoracic aorta and its branches
read more +
What is the difference between CT and MRI
Computed tomography, abbreviated as CT, is a modernized form of the well-known X-ray. CT is performed using a special machine. X-rays are used to obtain an image of the examined part of the body.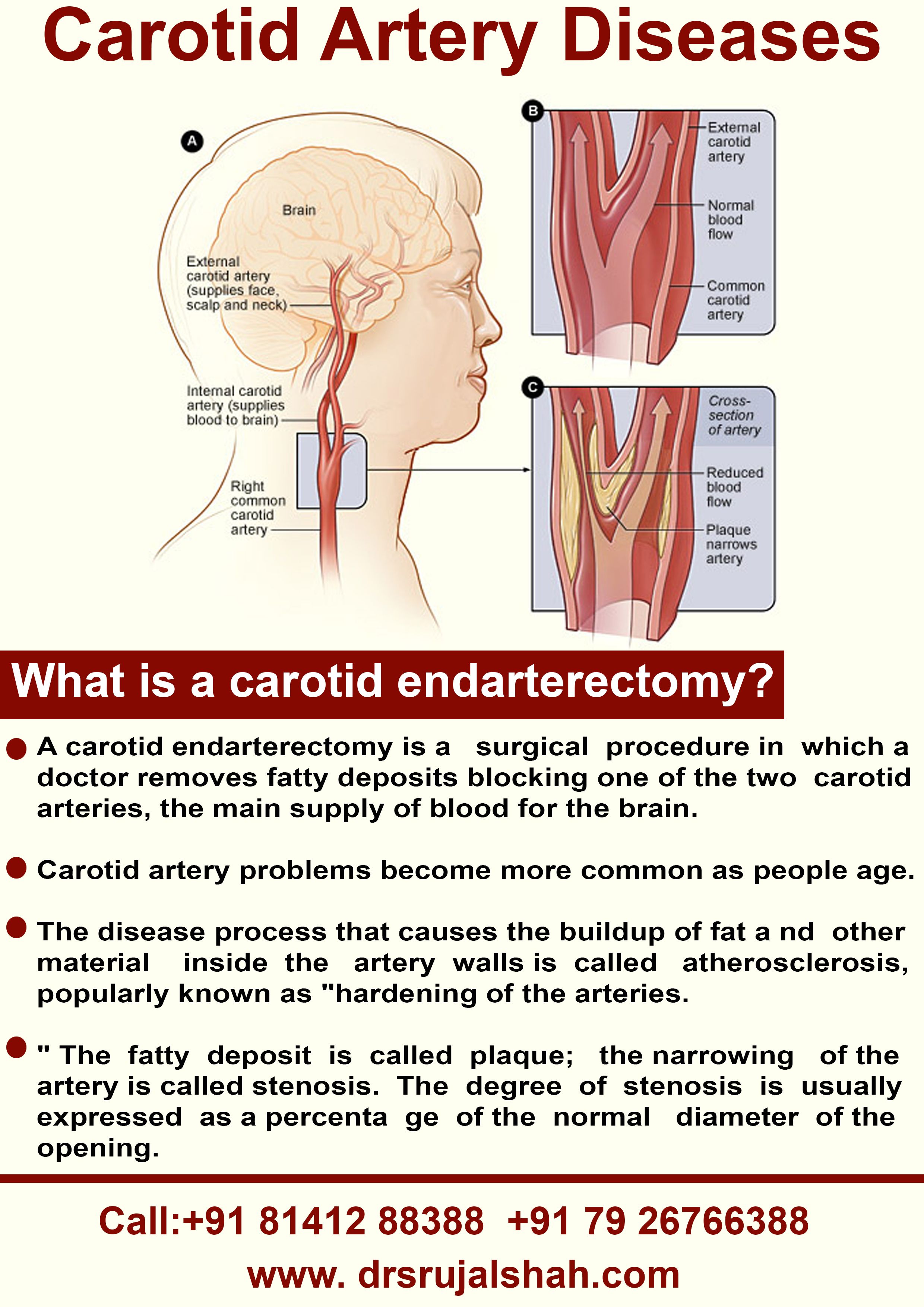

 Temporary blockages in your artery can also cause something called transient ischemic attacks (TIAs), which are warning signs of a stroke. They don’t cause any brain injury.
Temporary blockages in your artery can also cause something called transient ischemic attacks (TIAs), which are warning signs of a stroke. They don’t cause any brain injury. They also may place a stent higher risk patients.
They also may place a stent higher risk patients.
 During the operation, a small balloon is inserted into the vessel, when it is expanded, the accumulated plaques are removed, and the lumen of the vessel expands. The operation is indispensable for the atherosclerotic nature of stenosis.
During the operation, a small balloon is inserted into the vessel, when it is expanded, the accumulated plaques are removed, and the lumen of the vessel expands. The operation is indispensable for the atherosclerotic nature of stenosis.
 V.V. Mitkov. M.: Vidar. 1996. V.1. P.9-24.
V.V. Mitkov. M.: Vidar. 1996. V.1. P.9-24.