Enlarged Lymph Glands Under Arm: Comprehensive Guide to Breast Cancer
What are the key symptoms of breast cancer. How is breast cancer diagnosed and staged. What factors increase the risk of developing breast cancer. How can breast cancer be prevented and treated effectively.
Understanding Breast Cancer: A Common Yet Treatable Disease
Breast cancer is an invasive disease that develops when genetic mutations or DNA damage cause cells in the breast tissue to grow and multiply uncontrollably. While it predominantly affects females, males can also develop breast cancer in rare cases. Despite its prevalence, advancements in screening and treatment have significantly improved survival rates over the past decades.
According to the American Cancer Society (ACS), there are currently over 3.8 million breast cancer survivors in the United States. By the end of 2021, it was estimated that approximately 281,550 new cases of invasive breast cancer would be diagnosed, with around 43,600 deaths expected to occur. These statistics highlight the importance of early detection and awareness of breast cancer symptoms.
Recognizing the Signs and Symptoms of Breast Cancer
Early detection plays a crucial role in successful breast cancer treatment. Being aware of the potential signs and symptoms can help individuals seek medical attention promptly. Some common indicators include:
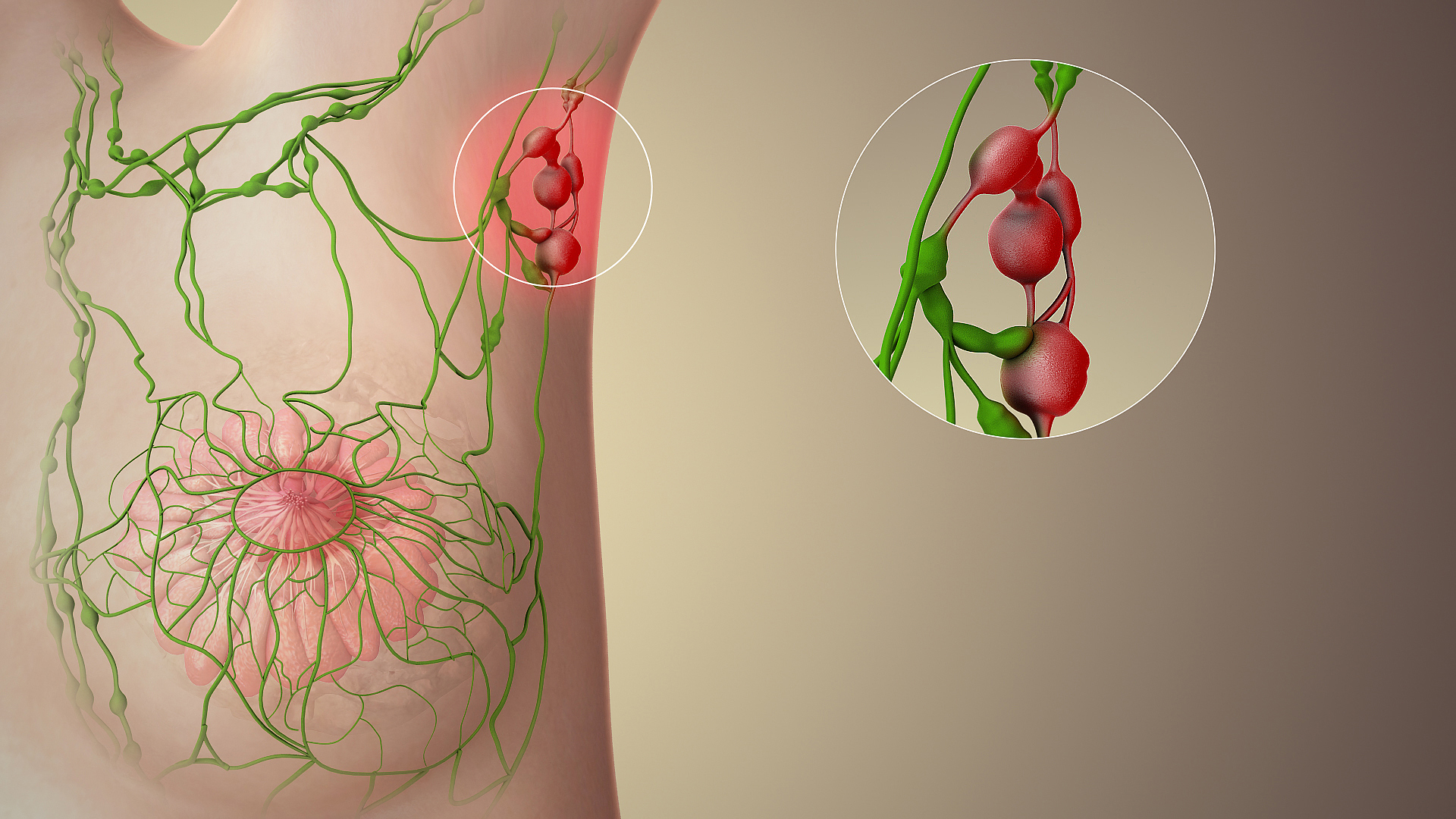
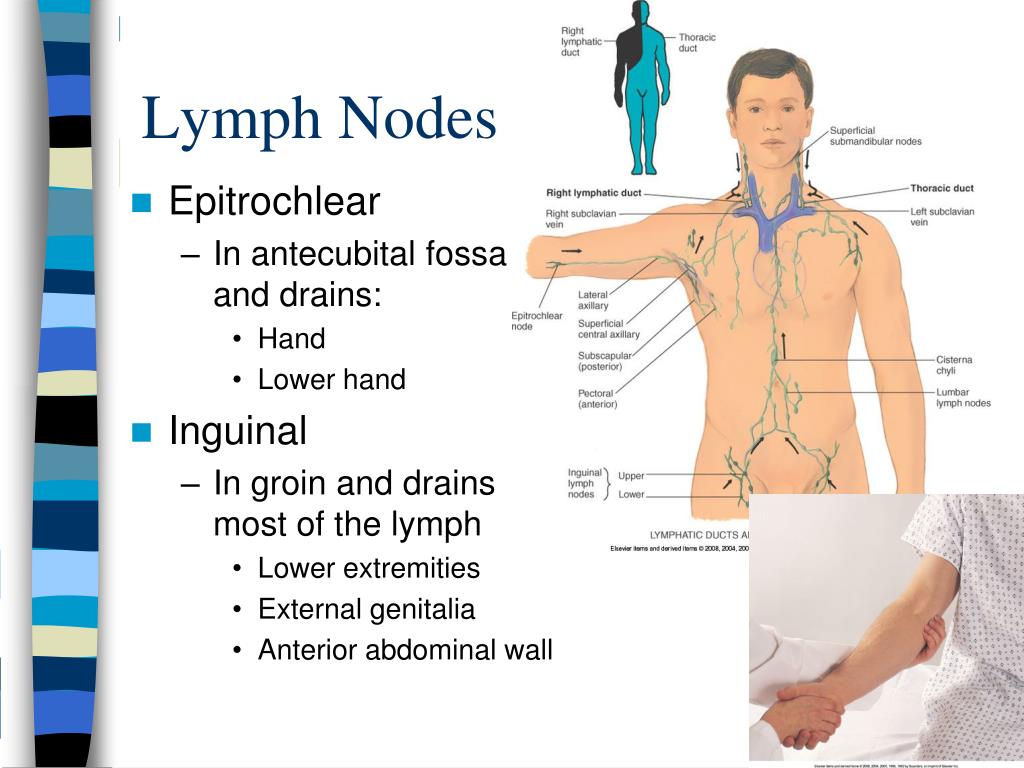
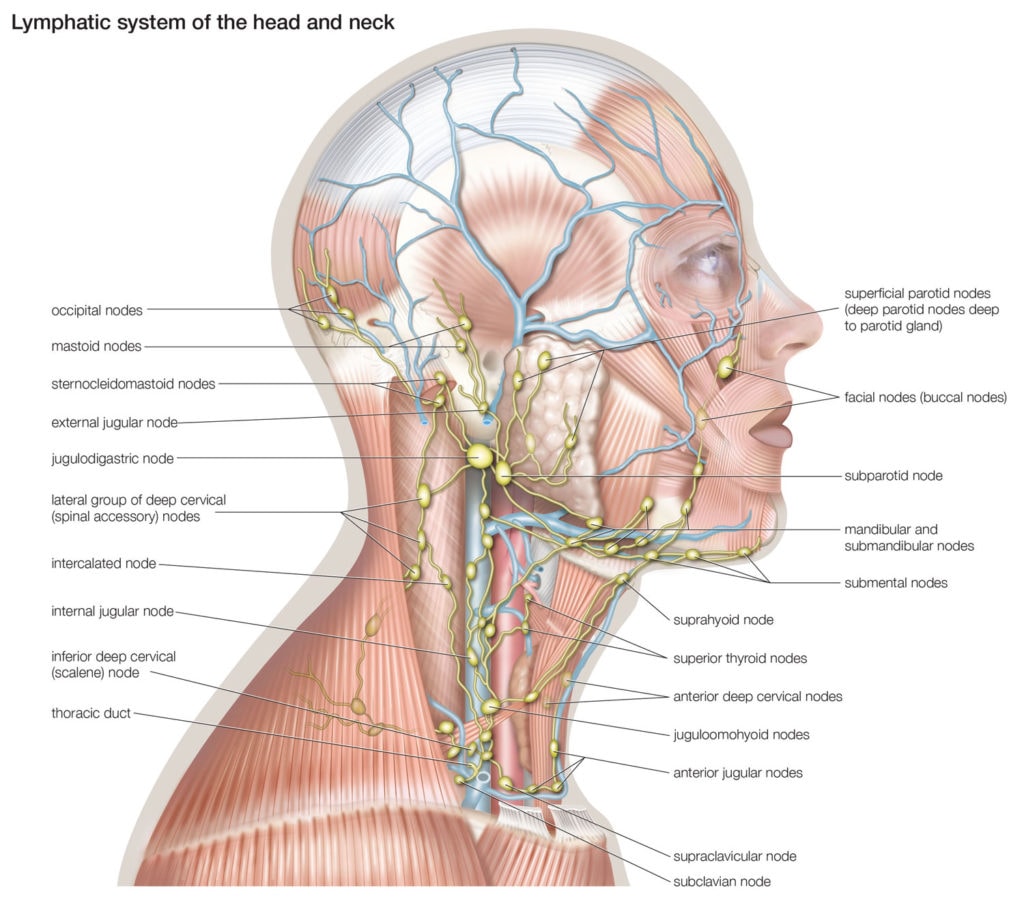
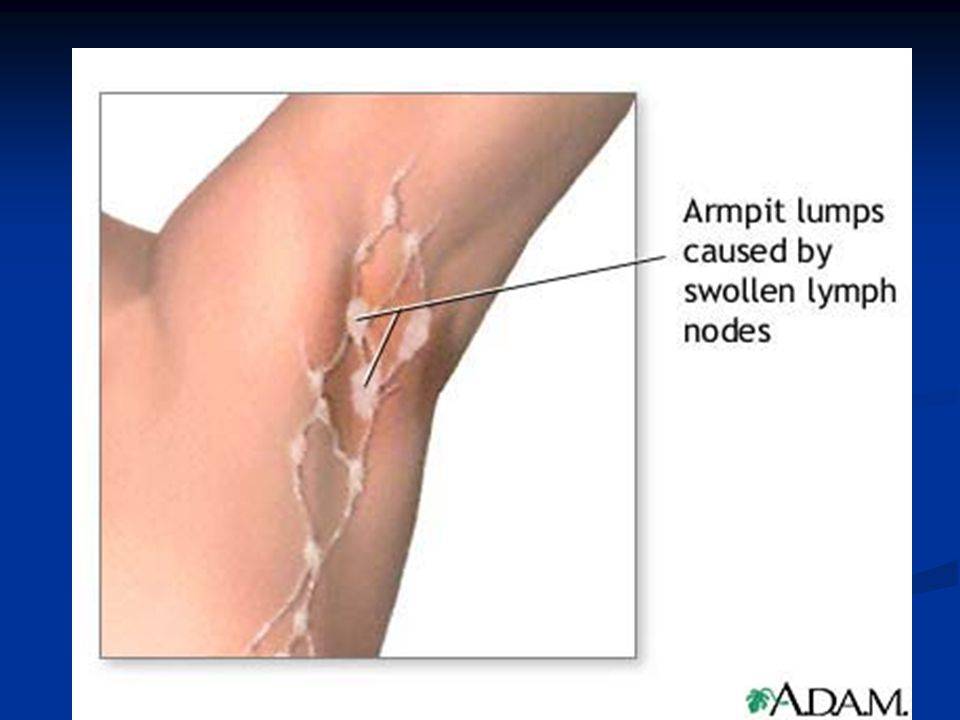
- A lump or thickened area in the breast or armpit
- Changes in breast size, shape, or appearance
- Skin changes, such as pitting, redness, or a rash
- Nipple changes, including inversion or discharge
- Persistent breast or armpit pain
While many breast lumps are non-cancerous, it’s essential to have any unusual changes examined by a healthcare professional. Breast pain associated with cancer is typically gradual and may not be related to the menstrual cycle.
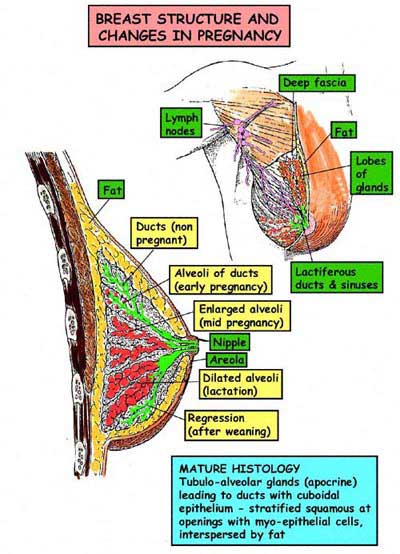
How does breast cancer develop?
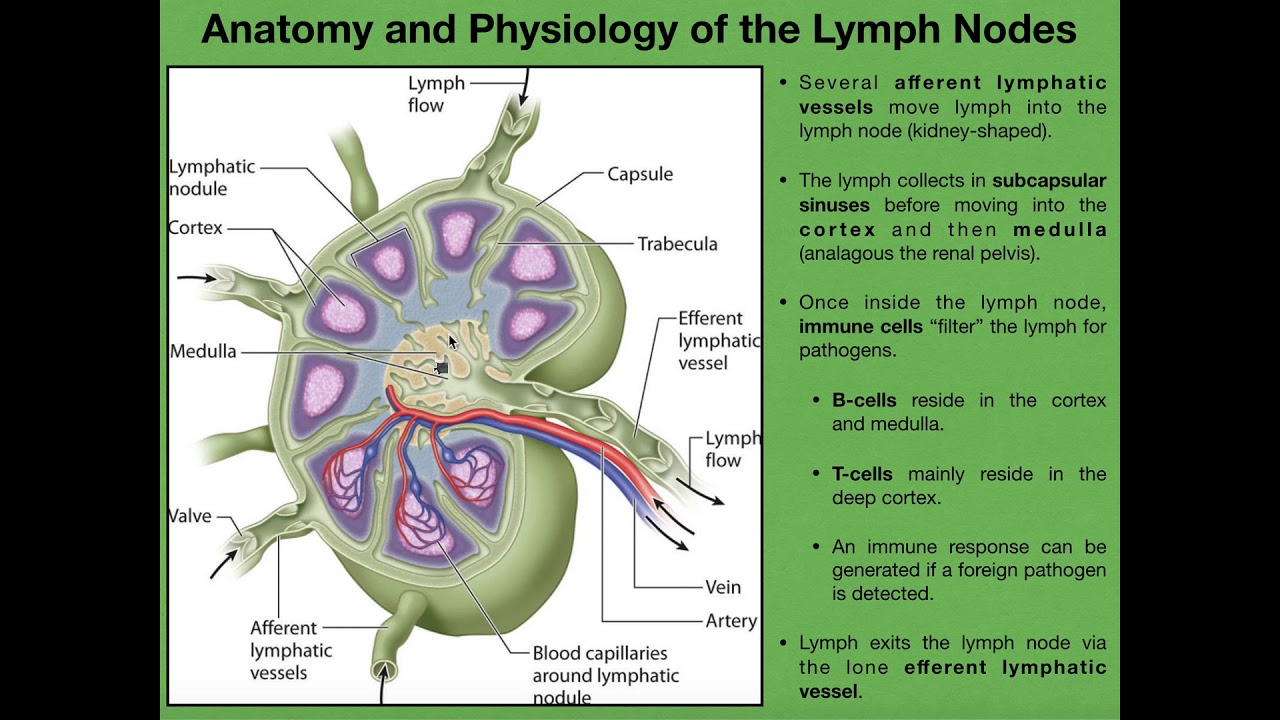
Breast cancer originates in the milk-producing glands (lobules) or the ducts that carry milk to the nipple. When genetic mutations occur, the body’s natural defense mechanisms fail to eliminate abnormal cells, leading to uncontrolled growth and tumor formation. These cancer cells can deprive surrounding healthy tissues of nutrients and eventually spread to other parts of the body.

Breast Cancer Staging: Understanding the Progression
Staging breast cancer helps determine the extent of the disease and guides treatment decisions. The staging system typically ranges from 0 to 4, with subcategories at each stage. Here’s a brief overview of the main stages:
- Stage 0: Also known as ductal carcinoma in situ (DCIS), cancer cells are confined to the milk ducts.
- Stage 1: The tumor is up to 2 cm across and has not spread to lymph nodes or has minimal lymph node involvement.
- Stage 2: The tumor is 2-5 cm across with varying degrees of lymph node involvement.
- Stage 3: The tumor is larger than 5 cm and has spread to several lymph nodes.
- Stage 4: Cancer has metastasized to distant organs, such as bones, liver, brain, or lungs.
It’s important to note that staging can be complex and may include additional factors such as hormone receptor status and HER2 status.
Risk Factors for Breast Cancer: What Increases Your Chances?
Several factors can influence an individual’s likelihood of developing breast cancer. While some risk factors are unavoidable, others can be modified through lifestyle changes. Key risk factors include:

- Age: The risk increases with age, particularly after 50.
- Genetics: Mutations in genes like BRCA1 and BRCA2 significantly elevate risk.
- Family history: Having close relatives with breast cancer increases risk.
- Personal history: Previous breast cancer or certain non-cancerous breast conditions.
- Hormonal factors: Early menstruation, late menopause, or long-term hormone replacement therapy.
- Lifestyle factors: Obesity, lack of physical activity, alcohol consumption, and smoking.
- Radiation exposure: Previous radiation therapy to the chest area.
Can breast cancer risk be reduced?
While some risk factors cannot be changed, adopting a healthy lifestyle can help reduce breast cancer risk. This includes maintaining a healthy weight, exercising regularly, limiting alcohol intake, and avoiding smoking. Regular breast cancer screenings and self-examinations are also crucial for early detection.
Breast Cancer Diagnosis: From Screening to Confirmation
Diagnosing breast cancer involves a combination of screening methods and diagnostic tests. The process typically includes:
- Breast examination: A physical exam to check for lumps or abnormalities.
- Mammography: X-ray imaging of the breast to detect suspicious areas.
- Ultrasound: Sound waves used to create images of breast tissue.
- Magnetic Resonance Imaging (MRI): Detailed imaging for high-risk individuals or to further investigate suspicious findings.
- Biopsy: Removal of tissue samples for microscopic examination to confirm cancer diagnosis.
Additional tests may be performed to determine the cancer’s characteristics, such as hormone receptor status and HER2 status, which help guide treatment decisions.
Treatment Options for Breast Cancer: A Multifaceted Approach
Breast cancer treatment is tailored to each individual based on various factors, including cancer stage, type, and personal preferences. Common treatment modalities include:
- Surgery: Lumpectomy (removal of the tumor and surrounding tissue) or mastectomy (removal of the entire breast).
- Radiation therapy: High-energy rays to destroy cancer cells and shrink tumors.
- Chemotherapy: Drugs that kill cancer cells throughout the body.
- Hormone therapy: Blocks hormone-sensitive cancer cells from growing.
- Targeted therapy: Drugs that target specific characteristics of cancer cells.
- Immunotherapy: Boosts the body’s natural defenses to fight cancer.
Treatment plans often combine multiple approaches to maximize effectiveness and minimize side effects.

How effective are current breast cancer treatments?
Advancements in breast cancer treatment have significantly improved outcomes. The 5-year relative survival rate for localized breast cancer (confined to the breast) is 99%. Even for regional breast cancer (spread to nearby tissues or lymph nodes), the 5-year survival rate is 86%. These statistics underscore the importance of early detection and prompt treatment.
Living with Breast Cancer: Coping Strategies and Support
A breast cancer diagnosis can be emotionally and physically challenging. Coping strategies and support systems play a crucial role in navigating the journey. Some helpful approaches include:
- Educating yourself about the disease and treatment options
- Seeking emotional support from family, friends, or support groups
- Maintaining open communication with your healthcare team
- Practicing stress-reduction techniques like meditation or yoga
- Focusing on overall health through nutrition and exercise
- Exploring complementary therapies to manage side effects
Many organizations offer resources and support for individuals affected by breast cancer, including counseling services, financial assistance, and educational materials.
Breast Cancer Research: Paving the Way for Better Treatments
Ongoing research continues to enhance our understanding of breast cancer and improve treatment outcomes. Some promising areas of study include:
- Personalized medicine: Tailoring treatments based on genetic profiles
- Immunotherapy: Developing more effective ways to harness the immune system
- Targeted therapies: Creating drugs that specifically attack cancer cells
- Liquid biopsies: Using blood tests to detect and monitor cancer
- Prevention strategies: Identifying new ways to reduce breast cancer risk
These advancements offer hope for more effective, less invasive treatments and improved quality of life for breast cancer patients.
How can individuals contribute to breast cancer research?
Participating in clinical trials is one way to support breast cancer research. These studies help researchers evaluate new treatments, diagnostic tools, and prevention strategies. Additionally, donating to reputable breast cancer research organizations can help fund crucial studies and accelerate progress in the field.

Global Impact of Breast Cancer: Addressing Disparities
Breast cancer affects millions of people worldwide, but its impact is not evenly distributed. Factors such as socioeconomic status, access to healthcare, and cultural beliefs can influence breast cancer outcomes. Addressing these disparities is crucial for improving global breast cancer care.
- Promoting awareness and education in underserved communities
- Improving access to screening and treatment in low-resource settings
- Developing culturally sensitive approaches to breast cancer care
- Advocating for policies that support breast cancer research and treatment
- Fostering international collaborations to share knowledge and resources
By addressing these challenges, we can work towards reducing the global burden of breast cancer and improving outcomes for all individuals affected by the disease.
What role do international organizations play in breast cancer control?
International organizations like the World Health Organization (WHO) and the Union for International Cancer Control (UICC) play crucial roles in coordinating global efforts to combat breast cancer. They develop guidelines, support research, and advocate for policies that improve breast cancer prevention, early detection, and treatment worldwide.
The Future of Breast Cancer Care: Emerging Technologies and Approaches
As we look to the future, several promising technologies and approaches are poised to revolutionize breast cancer care:
- Artificial Intelligence (AI) in mammography interpretation
- 3D-printed breast implants for more natural reconstruction
- Gene editing techniques to correct cancer-causing mutations
- Nanotechnology for targeted drug delivery
- Liquid biopsies for early detection and monitoring
- Telemedicine for improved access to specialist care
These innovations have the potential to enhance early detection, improve treatment precision, and reduce the physical and emotional burden of breast cancer.
How might AI transform breast cancer diagnosis and treatment?
Artificial Intelligence has shown promise in improving the accuracy of mammogram interpretation, potentially reducing false positives and missed diagnoses. AI algorithms can also analyze vast amounts of patient data to predict treatment outcomes and suggest personalized treatment plans, leading to more effective and targeted care.
Empowering Individuals: Taking Control of Breast Health
While medical advancements play a crucial role in breast cancer care, individuals can also take proactive steps to promote breast health and reduce their risk:
- Perform regular breast self-exams to familiarize yourself with your breast tissue
- Adhere to recommended screening guidelines based on your age and risk factors
- Maintain a healthy lifestyle through diet, exercise, and stress management
- Learn about your family history and discuss genetic testing if appropriate
- Stay informed about the latest breast cancer research and prevention strategies
- Advocate for yourself and others in healthcare settings
By taking an active role in breast health, individuals can contribute to early detection and improved outcomes.
How often should breast self-exams be performed?
While there’s no strict rule, many healthcare professionals recommend performing breast self-exams once a month, preferably a few days after menstruation when breasts are least likely to be swollen or tender. For those who no longer menstruate, choosing a consistent day each month can help establish a routine. Remember, self-exams are not a substitute for professional screenings but can help you become familiar with your breast tissue and detect changes early.