Fall precautions. Fall Prevention Strategies for Older Adults: Reducing Risks and Enhancing Safety
What are the main causes of falls in older adults. How can seniors reduce their risk of falling. What steps can be taken to fall-proof a home. How does exercise help prevent falls in the elderly. Why is medication management crucial for fall prevention. How do vision and hearing impact fall risk in seniors. What role does proper nutrition play in fall prevention for older adults.
Understanding the Prevalence and Impact of Falls in Older Adults
Falls among older adults are a significant health concern, with more than one in four individuals aged 65 years or older experiencing a fall each year. These incidents can have severe consequences, potentially leading to broken bones, long-term disability, and a cascade of more serious health problems. As the risk of falling increases with age, it’s crucial to understand the factors contributing to falls and implement effective prevention strategies.
Many older adults develop a fear of falling, even if they haven’t experienced a fall before. This fear can lead to a reduction in physical activities and social engagement, which paradoxically increases the risk of falls by contributing to muscle weakness and decreased balance. It’s essential to address this fear while taking proactive steps to reduce fall risks.
Identifying Common Causes of Falls in Seniors
Several factors contribute to the increased risk of falls among older adults:
- Age-related changes in sensory functions, such as diminished eyesight, hearing, and reflexes
- Chronic health conditions like diabetes, heart disease, and thyroid problems
- Cognitive impairment and certain types of dementia
- Sarcopenia (age-related loss of muscle mass)
- Balance and gait problems
- Postural hypotension (sudden drop in blood pressure when changing positions)
- Foot problems and unsafe footwear
- Medication side effects, particularly dizziness or confusion
- Environmental hazards in the home or community
Understanding these risk factors is the first step in developing effective fall prevention strategies.
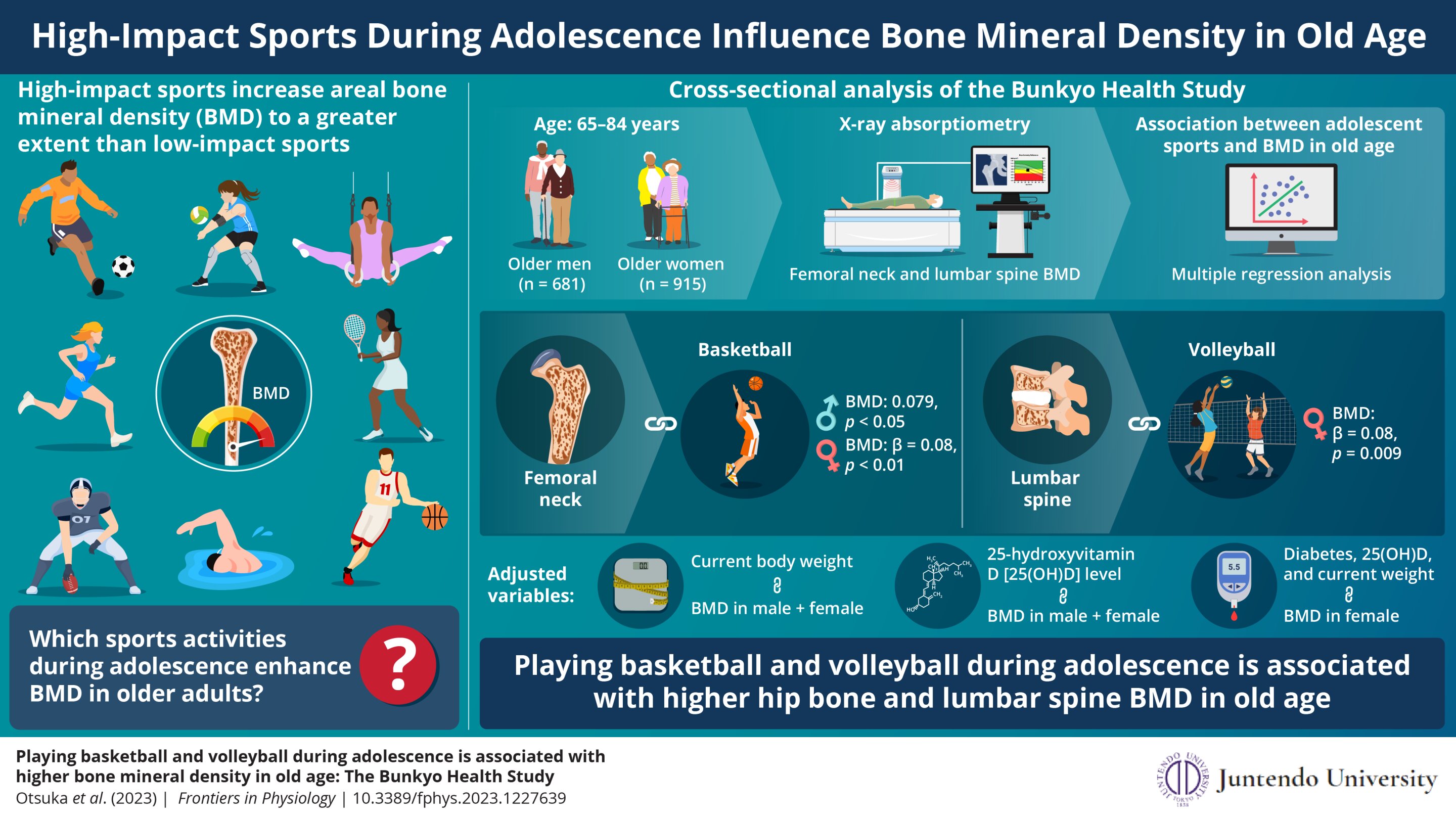
The Role of Physical Activity in Fall Prevention
Maintaining an active lifestyle is crucial for reducing the risk of falls in older adults. Regular physical activity offers numerous benefits:
- Improves muscle strength and flexibility
- Enhances balance and coordination
- Increases bone density, potentially slowing bone loss from osteoporosis
- Boosts overall health and well-being
What types of exercises are most effective for fall prevention? A combination of activities targeting strength, balance, and flexibility yields the best results. Consider incorporating the following into your routine:

- Walking or climbing stairs (mild weight-bearing activities)
- Yoga or tai chi for improved balance and core strength
- Resistance training with weights or bands to build muscle
- Pilates for core stability and overall body awareness
Always consult with a healthcare provider before starting a new exercise program to ensure it’s appropriate for your individual needs and health status.
Creating a Safer Home Environment
Fall-proofing your living space is an essential step in reducing the risk of accidents. Here are some key areas to focus on:
Lighting
Ensure all areas of your home are well-lit, especially staircases and hallways. Consider installing motion-sensor lights for nighttime use.
Flooring
Remove or secure loose rugs, repair uneven flooring, and keep walkways clear of clutter.
Bathroom Safety
Install grab bars near the toilet and in the shower or bathtub. Use non-slip mats in wet areas.
Stairways
Ensure handrails are secure on both sides of staircases. Mark the edges of steps with contrasting colors for better visibility.

Furniture Arrangement
Arrange furniture to create clear pathways and remove potential tripping hazards.
By addressing these areas, you can significantly reduce the risk of falls within your home environment.
The Importance of Regular Health Check-ups
Regular health assessments play a crucial role in fall prevention. Here’s why they’re important and what they should include:
Vision and Hearing Tests
Even minor changes in sight and hearing can increase fall risk. Schedule regular check-ups with your optometrist and audiologist. If you wear glasses or hearing aids, ensure they fit properly and are worn as prescribed.
Medication Review
Some medications can increase fall risk due to side effects like dizziness or drowsiness. Review all your medications with your healthcare provider or pharmacist regularly. This includes over-the-counter drugs and supplements.
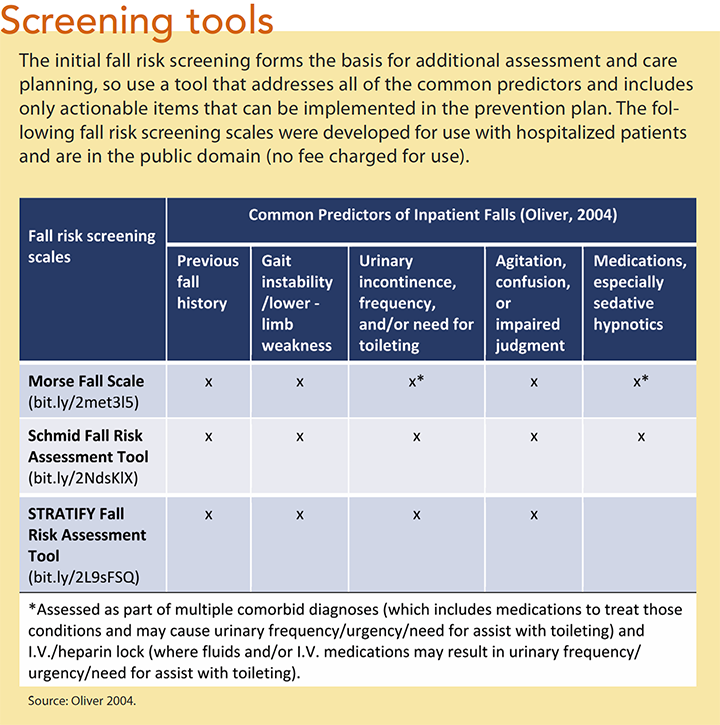
Balance and Gait Assessment
Your doctor can evaluate your walking pattern and balance to identify any issues that may increase your fall risk. They may recommend exercises or assistive devices to improve stability.
Chronic Condition Management
Proper management of chronic conditions like diabetes, heart disease, or arthritis can help reduce fall risk. Work closely with your healthcare team to keep these conditions under control.
By staying proactive with your health check-ups, you can address potential risk factors before they lead to falls.
Nutrition and Hydration: Key Factors in Fall Prevention
Proper nutrition and hydration play a significant role in fall prevention for older adults. Here’s how:
Bone Health
A diet rich in calcium and vitamin D supports bone strength, reducing the risk of fractures if a fall occurs. Good sources include dairy products, leafy greens, and fortified foods.
Muscle Strength
Adequate protein intake is crucial for maintaining muscle mass and strength. Include lean meats, fish, eggs, and plant-based proteins in your diet.
Hydration
Dehydration can lead to dizziness and weakness, increasing fall risk. Aim to drink plenty of water throughout the day, even if you don’t feel thirsty.

Blood Sugar Management
For those with diabetes, maintaining stable blood sugar levels can prevent dizziness and falls. Follow your doctor’s recommendations for diet and medication management.
Consulting with a registered dietitian can help ensure you’re meeting your nutritional needs for fall prevention and overall health.
The Benefits of Assistive Devices in Fall Prevention
Assistive devices can significantly enhance stability and reduce fall risk for older adults. Here’s what you need to know:
Canes and Walkers
These devices provide additional support when walking. It’s crucial to use the correct size and type for your needs. Consult with a physical therapist or occupational therapist for proper fitting and usage instructions.
Grab Bars
Installing grab bars in bathrooms and other areas of the home can provide crucial support during transfers and when navigating potentially slippery surfaces.
Raised Toilet Seats
These can make it easier to sit down and stand up, reducing the risk of falls in the bathroom.
Shower Chairs
Using a shower chair can provide stability and reduce fatigue while bathing, decreasing the risk of slips and falls.
When considering assistive devices, it’s important to balance their benefits with maintaining independence. Work with your healthcare provider to determine which devices are most appropriate for your situation.
Sleep Quality and Fall Prevention
The relationship between sleep and fall risk is often overlooked, but it’s an important factor to consider. Here’s why sleep matters:
Cognitive Function
Adequate sleep is crucial for maintaining cognitive function, including reaction time and decision-making skills. These abilities are essential for navigating daily activities safely.
Physical Recovery
During sleep, the body repairs and rejuvenates tissues, including muscles and bones. This process is vital for maintaining the physical strength needed to prevent falls.
Balance and Coordination
Lack of sleep can impair balance and coordination, increasing the risk of trips and falls.
Medication Interactions
Some sleep medications can increase fall risk due to side effects like dizziness or drowsiness. If you’re having trouble sleeping, consult your doctor for safe solutions.
To improve sleep quality, establish a regular sleep schedule, create a relaxing bedtime routine, and ensure your sleeping environment is comfortable and conducive to rest.
By addressing these various aspects of fall prevention, older adults can significantly reduce their risk of falls and maintain their independence and quality of life. Remember, it’s never too late to start implementing these strategies. Even small changes can make a big difference in enhancing safety and well-being.
Falls and Fractures in Older Adults: Causes and Prevention
Español
A simple accident like tripping on a rug or slipping on a wet floor can change your life. If you fall, you could break a bone, which thousands of older adults experience each year. For older people, a broken bone can also be the start of more serious health problems and can lead to long-term disability.
On this page:
If you or an older adult in your life has fallen, you’re not alone. More than one in four people age 65 years or older fall each year. The risk of falling — and fall-related problems — rises with age. However, many falls can be prevented. For example, exercising, managing your medications, having your vision checked, and making your home safer are all steps you can take to prevent a fall.
Many older adults fear falling, even if they haven’t fallen before. This fear may lead them to avoid activities such as walking, shopping, or taking part in social activities. But staying active is important to keeping your body healthy and actually helps to prevent falls. So don’t let a fear of falling keep you from being active! Learn about what causes falls and how to lower your risk of falling so you can feel more comfortable with staying active.
But staying active is important to keeping your body healthy and actually helps to prevent falls. So don’t let a fear of falling keep you from being active! Learn about what causes falls and how to lower your risk of falling so you can feel more comfortable with staying active.
What causes falls in older adults?
Many things can cause a fall.
- Your eyesight, hearing, and reflexes might not be as sharp as they were when you were younger.
- Certain conditions, such as diabetes, heart disease, or problems with your thyroid, nerves, feet, or blood vessels can affect your balance and lead to a fall.
- Conditions that cause rushed movement to the bathroom, such as incontinence, may also increase the chance of falling.
- Older adults with mild cognitive impairment or certain types of dementia are at higher risk of falling.
- Age-related loss of muscle mass (known as sarcopenia), problems with balance and gait, and blood pressure that drops too much when you get up from lying down or sitting (called postural hypotension) are all risk factors for falling.

- Foot problems that cause pain, and unsafe footwear such as backless shoes or high heels, can also increase your risk of falling.
- Some medications can increase a person’s risk of falling because they cause side effects such as dizziness or confusion. The more medications you take, the more likely you are to fall.
- Safety hazards in the home or community environment can also cause falls.
Steps to take to prevent falls
If you take care of your overall health, you may have a lower chance of falling. Most of the time, falls and accidents don’t just happen for no reason. Here are a few tips to help lessen your risk of falls and broken bones, also known as fractures:
Read and share this infographic and help spread the word about how to help prevent falls.
- Stay physically active. Plan an exercise program that is right for you. Regular exercise improves muscles and makes you stronger. Exercise also helps keep your joints, tendons, and ligaments flexible.
 Mild weight-bearing activities, such as walking or climbing stairs, may slow bone loss from osteoporosis, a disease that makes bones weak and more likely to break
Mild weight-bearing activities, such as walking or climbing stairs, may slow bone loss from osteoporosis, a disease that makes bones weak and more likely to break - Try balance and strength training exercises. Yoga, Pilates, and tai chi can all improve balance and muscle strength. You can also try lifting weights or using resistance bands to build strength. Learn more about different types of exercises to improve balance and strength.
- Fall-proof your home. Check out these tips for changes you can make to your home that will help you avoid falls and ensure your safety.
- Have your eyes and hearing tested. Even small changes in sight and hearing are linked to an increased risk for falls. When you get new eyeglasses or contact lenses, take time to get used to them. Wear your glasses or contacts as your eye doctor advises. If you have a hearing aid, be sure it fits well and wear it.
- Find out about the side effects of any medicines you take. If a drug makes you sleepy or dizzy, tell your doctor or pharmacist.

- Get enough sleep. If you are tired, you are more likely to fall.
- Avoid or limit alcohol. Too much alcohol can lead to balance problems and falls, which can result in hip or arm fractures and other injuries.
- Stand up slowly. Getting up too quickly can cause your blood pressure to drop. That can make you feel wobbly. Get your blood pressure checked when lying and standing.
- Use an assistive device if you need help feeling steady when you walk. Using canes and walkers correctly can help prevent falls. If your doctor tells you to use a cane or walker, make sure it’s the right size for you. Walker wheels should roll smoothly. If you borrow walking support equipment from a friend, ask your health care provider to make sure the equipment is the correct size and is safe to use. This is exceptionally important when you’re walking in areas you don’t know well or where the walkways are uneven. A physical or occupational therapist can help you decide which devices might be helpful and teach you how to use them safely.

- Take extra caution when walking on wet or icy surfaces. These can be very slippery! Use an ice melt product or sand to clear icy areas by your doors and walkways.
- Keep your hands free. Use a shoulder bag, fanny pack, or backpack to leave your hands free to hold on to railings.
- Choose the right footwear. To fully support your feet, wear nonskid, rubber-soled, low-heeled shoes. Don’t walk on stairs or floors in socks or in shoes and slippers with smooth soles.
- Consider staying inside when the weather is bad. Some community services provide 24-hour delivery of prescriptions and groceries, and many take orders over the phone.
- Always tell your doctor if you have fallen since your last check-up, even if you did not feel pain when you fell. A fall can alert your doctor to a new medical problem or issues with your medications or eyesight that can be corrected. Your doctor may suggest physical therapy, a walking aid, or other steps to help prevent future falls.

What to do if you fall
Whether you are at home or somewhere else, a sudden fall can be startling and upsetting. If you do fall, stay as calm as possible and take the following steps:
- Breathe. Take several deep breaths to try to relax. Remain still on the floor or ground for a few moments. This will help you get over the shock of falling.
- Decide if you are hurt. Getting up too quickly or in the wrong way could make an injury worse.
- Crawl to a sturdy chair. If you think you can get up safely without help, roll over onto your side. Rest again while your body and blood pressure adjust. Slowly get up on your hands and knees, and crawl to a sturdy chair.
- Slowly sit down in the chair. Put your hands on the chair seat and slide one foot forward so that it’s flat on the floor. Keep the other leg bent so the knee is on the floor. From this kneeling position, slowly rise and turn your body to sit in the chair.

- Get help. If you are hurt or cannot get up on your own, ask someone for help or call 911. If you are alone, try to get into a comfortable position and wait for help to arrive. Prepare for a fall by keeping a well-charged cordless or mobile phone with you at all times and arrange for daily contact with a family member or friend. Emergency response systems are another option: These systems enable you to push a button on a special necklace or bracelet to call for help. Some smartwatches also have this feature.
Keep your bones strong to prevent fall-related fractures
Having healthy bones won’t necessarily prevent a fall, but if you do fall, healthy bones may help prevent serious injury, such as breaking a hip or other bone. Bone breaks and fracture can lead to a hospital or nursing home stay, long-term disability, or even death. Getting enough calcium and vitamin D can help keep your bones strong. So can staying active. Try to get at least 150 minutes per week of physical activity.
Other ways to maintain bone health include quitting smoking and avoiding or limiting alcohol use. Tobacco and alcohol use may decrease your bone mass and increase your chance of fractures. Additionally, try to maintain a healthy weight. Being underweight increases the risk of bone loss and broken bones.
Osteoporosis is a disease that weakens bones, making them thin and brittle. For people with osteoporosis, even a minor fall may be dangerous. Talk to your doctor about osteoporosis.
Falls are a common reason for trips to the emergency room and for hospital stays among older adults. Many of these hospital visits are for fall-related fractures. You can help lower your risk of fractures by keeping your bones strong and following the tips above to avoid falls.
For more information
Centers for Disease Control and Prevention (CDC)
800-232-4636
888-232-6348 (TTY)
[email protected]
www.cdc.gov
National Resource Center on Supportive Housing and Home Modifications
213-740-1364
homemods@usc.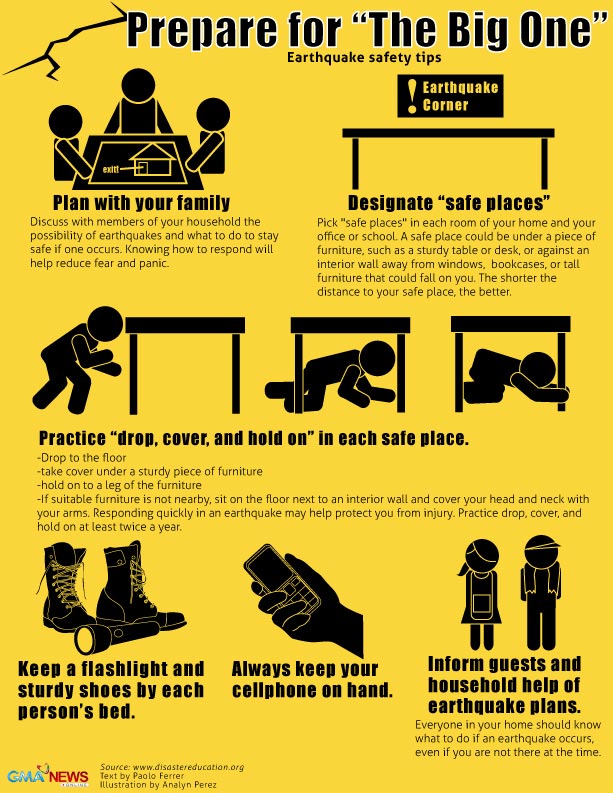 edu
edu
www.homemods.org
Rebuilding Together
800-473-4229
[email protected]
www.rebuildingtogether.org
National Falls Prevention Resource Center
571-527-3900
www.ncoa.org/center-for-healthy-aging/falls-resource-center/
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
Content reviewed:
September 12, 2022
Related Articles
How to Prevent Falls at Home
One out of four older adults will fall this year, but fewer than half of them will talk with their doctors about it, according to the Centers for Disease Control and Prevention (CDC). Per the CDC, falls are the No. 1 cause of injuries in adults over 65, resulting in hip fractures, cuts, and even serious head and brain injuries that can be fatal.
Even when there’s no serious injury, a fall can be so frightening that people may avoid certain activities out of fear they’ll fall again. And that’s not unreasonable, because if you fall once, your chance of falling again doubles, according to the CDC.
And that’s not unreasonable, because if you fall once, your chance of falling again doubles, according to the CDC.
Whether it’s slippery floors, rickety stairs, or electrical cords, some of the most common causes of falls are in the home, where you might have a false sense of security. That’s why fall prevention starts with creating a safe living space.
It doesn’t have to involve a complete house remodel. You can make your home safe from falls with just a few basic changes. Elder care experts offer the following advice for preventing falls at home.
- Clean up clutter. The easiest way to prevent falls is to keep your home neat and tidy. Remove all clutter, such as stacks of old newspapers and magazines, especially from hallways and staircases.
- Repair or remove tripping hazards. Sometimes home fixtures can contribute to falls, which can then lead to back pain and other injuries. Examine every room and hallway, looking for items such as loose carpet, slippery throw rugs, or wood floorboards that stick up.
 Then repair, remove, or replace those items for more effective fall prevention.
Then repair, remove, or replace those items for more effective fall prevention. - Install grab bars and handrails. If your mobility is limited, these safety devices can be crucial for going up and down stairs, getting on and off the toilet, and stepping in and out of the bathtub without injuring yourself. Gary Kaplan, DO, the founder and medical director of the Kaplan Center for Integrative Medicine in McLean, Virginia, suggests installing grab bars by toilets and bathtubs and handrails in stairways and hallways. Have a handyman or family member help with this if necessary.
- Avoid loose clothing. You want to feel comfortable at home, but very baggy clothes can sometimes make you more likely to fall. Opt for better-fitting and properly hemmed clothing that doesn’t bunch up or drag on the ground.
- Light it right. Inadequate lighting is another major hazard. To create a home that’s easier to navigate, install brighter light bulbs where needed, particularly in stairways and narrow hallways.
 Robert Bunning, MD, the associate medical director of inpatient services at MedStar National Rehabilitation Hospital in Washington, DC, recommends adding night-lights in bedrooms and bathrooms for better guidance at night.
Robert Bunning, MD, the associate medical director of inpatient services at MedStar National Rehabilitation Hospital in Washington, DC, recommends adding night-lights in bedrooms and bathrooms for better guidance at night. - Wear shoes. Socks may be comfortable, but they present a slipping risk. Preventing falls at home can be as simple as wearing shoes. You can also purchase nonslip socks that have grips on the soles of the feet if shoes are too uncomfortable.
- Make it nonslip. Bathtubs and showers, as well as floors in kitchens, bathrooms, and porches, can become extremely dangerous when wet. To prevent falls on slick surfaces, Dr. Kaplan recommends nonslip mats.
- Live on one level. Even with precautions like guardrails, stairs can present a significant falling hazard. “If possible, live on one level,” says Kaplan. “Otherwise, be extra careful when you negotiate stairs.” If it’s not possible to live on one level, try to limit the trips you take up and down the stairs.

- Move more carefully. Dr. Bunning explains that many people fall at home by moving too quickly from a sitting to a standing position and vice versa. Preventing falls can be as easy as taking your time. “All you have to do is pause after going from lying down to sitting and from sitting to standing,” he says. “Also take a pause before using the railing on stairs, whether you’re going up or down.”
- Join a preventive exercise program. Many community centers, gyms, and health systems offer exercise programs for older adults aimed at preventing falls. These exercise regimens focus on improving balance and strengthening muscles. A physical therapist can also recommend exercise programs and assistive devices, if necessary, to keep you safe.
For older adults, fall prevention means injury prevention. Ask your loved ones to help you ensure that your rooms and stairways are clutter-free and well-equipped with lighting, handrails, grab bars, and nonslip mats — all of which can go a long way toward keeping you safe in your home.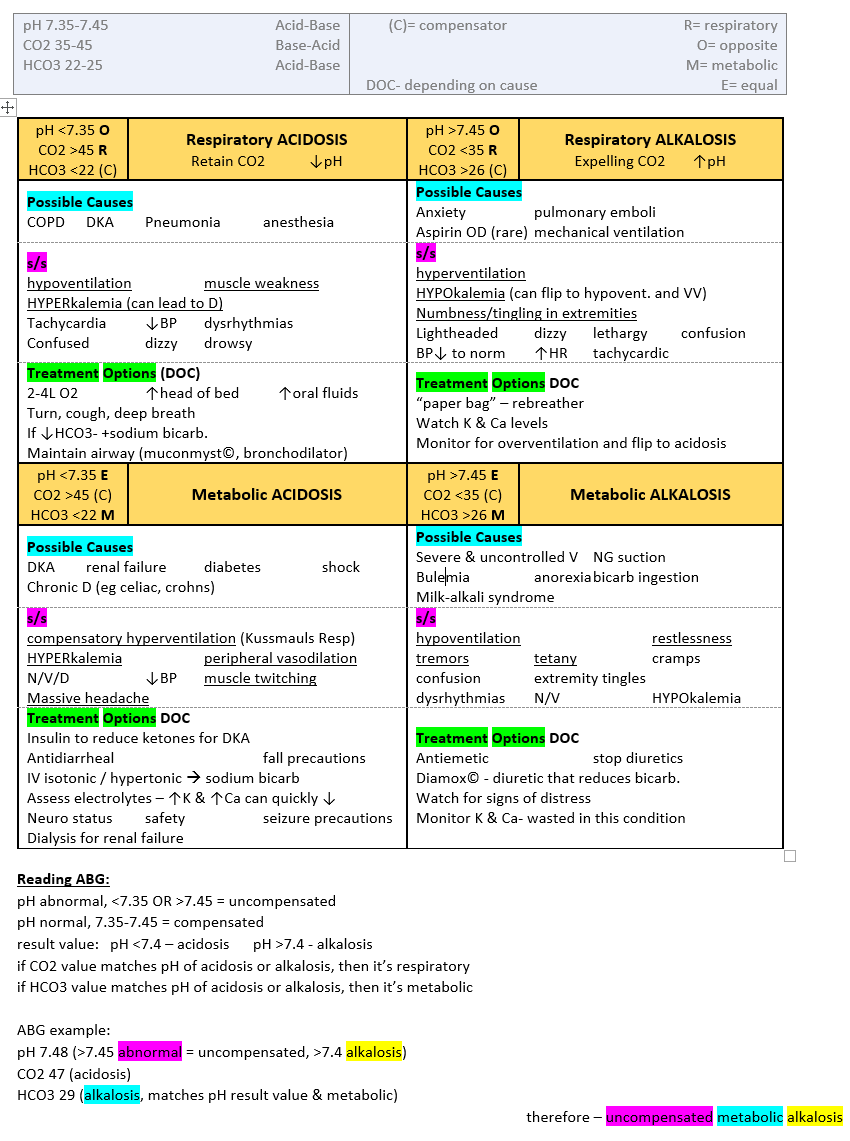 In the event a fall does occur, having a proper Medicare plan can help alleviate surprise medical costs.
In the event a fall does occur, having a proper Medicare plan can help alleviate surprise medical costs.
Additional reporting by Rachael Robertson.
The Nutrient Taurine Shown to Slow Aging in Animal Studies
The nutrient, found in meat and fish and added to energy drinks, had anti-aging properties in animal studies, but the impact on humans isn’t clear.
By Lisa Rapaport
Reducing Calories Could Slow the Aging Process
For the first time, a study in humans has shown that calorie restriction can slow biological aging and improve heart health and metabolism.
By Becky Upham
8 Everyday Health and Wellness Habits Linked With a Longer Life
The average life expectancy in the United States is on a historic decline. Here are research-backed habits you can do every day to help improve your likelihood. ..
..
By Stephanie Thurrott
6 Fun Apps That May Help Improve Brain Health
You may improve your memory, boost brain speed, and more by downloading these apps to your phone. Get background info on how to play them and what they…
By Lauren Bedosky
Autumn safety measures
9
Nov
11/09/2020
The Central Inspectorate and the Patrol Group of the GIMS EMERCOM of Russia inform about security measures in the autumn period.
The most dangerous thing when you are near the water in autumn is the possibility of unexpectedly falling into the water, especially in rainy weather, when the banks of water bodies are slippery. Here are the main criteria for accidents at water bodies in the autumn.
- Takes your breath away.

- The head is as if squeezed by an iron hoop.
- Rapid heart rate.
- Blood pressure rises to alarming limits.
- The muscles of the chest and abdomen reflexively contract, causing first exhalation and then inhalation. An involuntary respiratory act is especially dangerous if at this moment the head is under water, because a person can choke.
- Trying to protect itself from the deadly effects of cold, the body turns on the reserve system of heat production – the mechanism of cold shivering.
- Heat production sharply increases due to the rapid involuntary contraction of muscle fibers, sometimes three to four times. However, after a certain period of time, even this heat is not enough to compensate for heat loss, and the body begins to cool. When the skin temperature drops to 30°C, the shivering stops, and from that moment on, hypothermia begins to develop at an increasing rate. Breathing becomes less frequent, the pulse slows down, blood pressure drops to critical numbers.

The main causes of human death in cold water : · Hypothermia, since the heat produced by the body is not enough to compensate for heat loss. Death can occur in cold water, sometimes much earlier than hypothermia sets in, the reason for this may be a kind of “cold shock”, sometimes developing in the first 5-15 minutes after immersion in water. Respiratory dysfunction caused by massive irritation of cold receptors in the skin. Rapid loss of tactile sensation. Being close to a lifeboat, a person in distress sometimes cannot climb into it on their own, as the temperature of the skin of the fingers drops to the temperature of the surrounding water.
First aid:
Even before the victim is taken to the doctor, he must immediately receive first aid, if necessary, give artificial respiration, encourage and calm.
With a safe stay in it is about 20 minutes. If an unprepared person gets into cold water, especially a child who is not yet physically very strong, then after about 15-20 minutes he loses consciousness and may die if help does not come in time or he does not get out of the water on his own. do not forget about the possibility of hypothermia (hypothermia) of the victim. The temperature of the water in the reservoir is always lower than the temperature of the human body (36 – 37C), so being in the water for any time leads to cooling of the body. And if the stay in the water is very long or the water is very cold, hypothermia of the body can be deadly. So at a water temperature of +5
do not forget about the possibility of hypothermia (hypothermia) of the victim. The temperature of the water in the reservoir is always lower than the temperature of the human body (36 – 37C), so being in the water for any time leads to cooling of the body. And if the stay in the water is very long or the water is very cold, hypothermia of the body can be deadly. So at a water temperature of +5
There are two forms of hypothermia: mild and severe.
- Rescued conscious in mild form. He needs to change wet clothes to dry ones and give him hot and sweet drinks (alcohol is contraindicated).
- In severe hypothermia, the victim is usually unconscious. A complex of resuscitation actions is needed:
- place the victim in a warm room;
- change clothes to dry, trying not to disturb the victim;
- lay the casualty face up on a hard, level surface;
- give artificial respiration if necessary;
- actively warm the victim using one of the following methods: towels previously dipped in hot water (70C) are applied to the head, neck, chest, stomach; or warm the victim with the warmth of your body, snuggling tightly against him (both should be wrapped in a blanket).

Do not: give the victim alcohol; try to massage or rub the rescued; place in hot water or warm the limbs (arms and legs) of the victim. After first aid, the victim must be taken to the nearest medical facility as soon as possible.
VKontakte School history School museum Electronic diary Version for the visually impaired
Useful links
- School psychologist’s page
- Independent assessment of the quality of the conditions for the implementation of educational activities by the organization
- GTO
- Results of an independent assessment of the quality of educational activities
- Commissioner for the rights of participants in the educational process
- Memorable dates of the military history of Russia
- Anti-corruption policy
- Prosecutor’s office explains
- Improving the quality of mathematics education
Helpline
8-800-450-23-22
Water safety measures in autumn
In autumn, the activity of vacationers near the water decreased. But on good sunny days and weekends, you can still meet those who want to spend their holidays near the reservoirs. However, it should be remembered that in the autumn period one must be especially careful and follow the elementary rules of behavior on the water in order to avoid accidents.
But on good sunny days and weekends, you can still meet those who want to spend their holidays near the reservoirs. However, it should be remembered that in the autumn period one must be especially careful and follow the elementary rules of behavior on the water in order to avoid accidents.
In autumn, the water temperature is only 6-10 ° C, and if a person suddenly finds himself in the water, wet clothes will immediately pull him down, and cold water will hinder his movements. Rescue in such a situation can be quite difficult.
If you are relaxing on the beach with small children, be especially vigilant, do not leave them alone by the water unattended. Try to choose places for games and entertainment away from steep banks, slippery stones and rocks, from which you can fall into cold water by negligence!
If you use a small boat for recreation, remember: – children can be on a small boat only if their number corresponds to the number of adults who can swim; – all people on the ship must wear life jackets. – if a small boat capsized, first of all, it is necessary to provide assistance to people who cannot swim. In order to ensure safety on small boats, it is prohibited: – riding a small boat while intoxicated, without life-saving equipment, in windy weather, at night.
– if a small boat capsized, first of all, it is necessary to provide assistance to people who cannot swim. In order to ensure safety on small boats, it is prohibited: – riding a small boat while intoxicated, without life-saving equipment, in windy weather, at night.
Rules for the safety of people on the water in the autumn-winter period.
Autumn ice in the period from November to December, that is, before the onset of stable frosts, is fragile. Bonded in the evening or night cold, it is still able to withstand a small load, but during the day, quickly heating up from the melt water seeping through it, it becomes porous and very weak, although it retains sufficient thickness.
Formation of Ice:
· As a rule, reservoirs freeze unevenly, in parts: first near the coast, in shallow water, in bays protected from the wind, and then in the middle.
On lakes, ponds, stakes (in all reservoirs with stagnant water, especially those where not a single stream flows, in which there is no bed of a bottom river, underwater springs), ice appears earlier than on rivers, where the current delays ice formation.
On the same body of water, one can find alternation of ice, which, with the same thickness, has different strength and carrying capacity.
The main condition for the safe stay of a person on ice is that the thickness of the ice corresponds to the applied load:
Safe ice thickness for one person is at least 7 cm;
Safe ice thickness for crossing on foot is 15 cm or more;
Safe ice thickness for the passage of cars is not less than 30 cm. Time of safe stay of a person in the water:
at a water temperature of 24°C, the safe stay is 7-9 hours,
At a water temperature of 5-15°C – from 3.5 hours to 4.5 hours;
The water temperature of 2-3°C is fatal for humans in 10-15 minutes;
At a water temperature of minus 2 ° C – death can occur in 5-8 minutes.
Thin ice criteria
The color of the ice is milky cloudy, gray ice, usually spongy and porous.


 Mild weight-bearing activities, such as walking or climbing stairs, may slow bone loss from osteoporosis, a disease that makes bones weak and more likely to break
Mild weight-bearing activities, such as walking or climbing stairs, may slow bone loss from osteoporosis, a disease that makes bones weak and more likely to break



 Then repair, remove, or replace those items for more effective fall prevention.
Then repair, remove, or replace those items for more effective fall prevention. Robert Bunning, MD, the associate medical director of inpatient services at MedStar National Rehabilitation Hospital in Washington, DC, recommends adding night-lights in bedrooms and bathrooms for better guidance at night.
Robert Bunning, MD, the associate medical director of inpatient services at MedStar National Rehabilitation Hospital in Washington, DC, recommends adding night-lights in bedrooms and bathrooms for better guidance at night.