Floating bowel movement. Floating Stools: Causes, Symptoms, and When to Seek Medical Attention
What causes floating stools. How to identify if floating stools are a sign of a health problem. When should you see a doctor for floating stools. What tests may be performed to diagnose the cause of floating stools. How are floating stools treated.
Understanding Floating Stools: Common Causes and Concerns
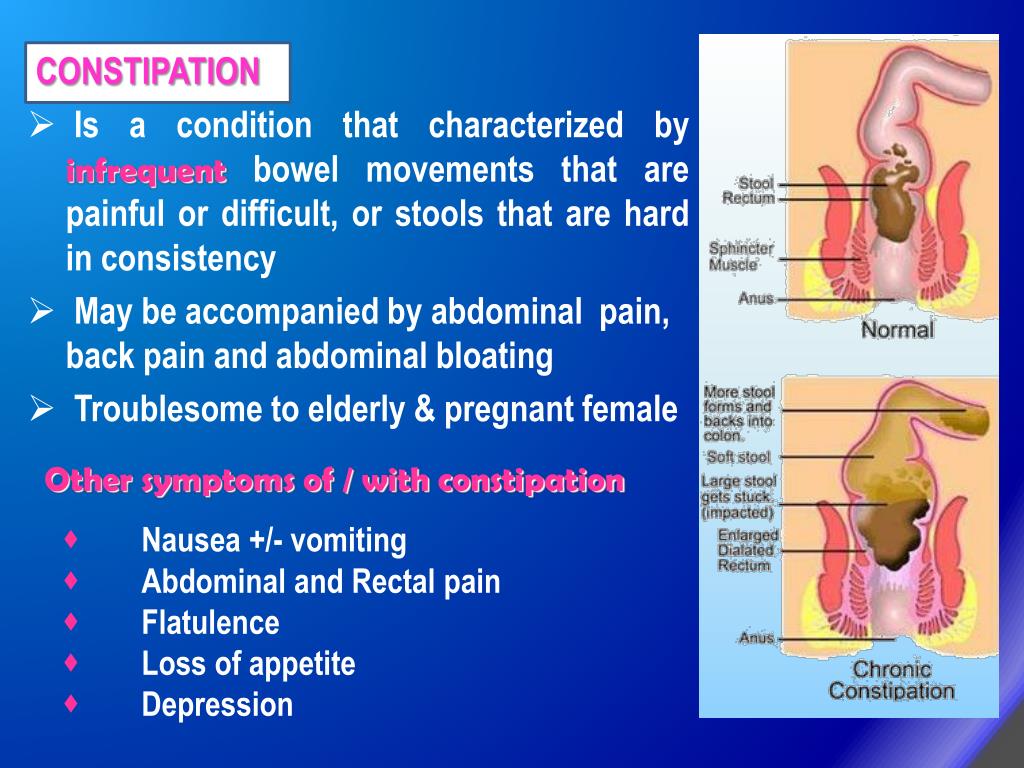
Floating stools are a common occurrence that can be attributed to various factors. While often harmless, they can sometimes indicate underlying health issues. The primary reasons for stools that float are poor nutrient absorption (malabsorption) and excessive gas (flatulence) in the digestive system.
To understand why stools float, it’s essential to grasp the basics of the digestive process:
- Food moves from the stomach to the small intestine.
- Nutrients are absorbed in the small intestine.
- Unabsorbed material passes into the colon.
- The colon absorbs water from the remaining food residue.
- The residue is eliminated as feces.
Dietary Factors Contributing to Floating Stools
In many cases, floating stools are directly related to dietary choices. Changes in your eating habits can lead to increased gas production in the intestines, causing stools to float. Some common dietary factors include:
- High-fiber foods
- Lactose intolerance
- Artificial sweeteners
- Carbonated beverages
- Certain fruits and vegetables
Are floating stools always a sign of poor nutrient absorption? Not necessarily. While malabsorption can cause floating stools, it’s not the only reason. In fact, most cases of floating stools are not due to increased fat content in the stool, which is often associated with malabsorption.
Medical Conditions Associated with Floating Stools
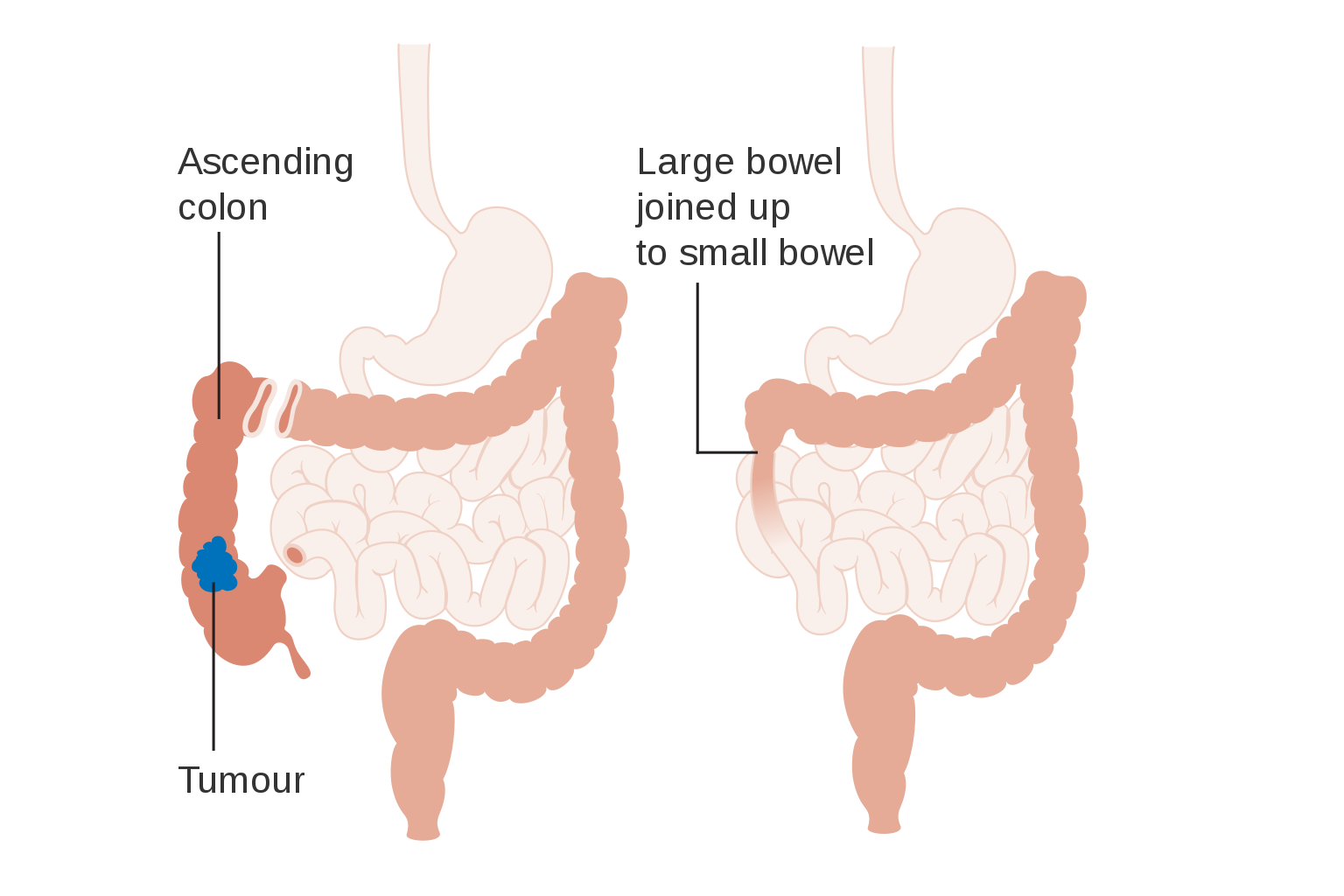
Although floating stools are often benign, they can sometimes be a symptom of underlying health issues. Some medical conditions that may cause floating stools include:
- Gastrointestinal infections
- Celiac disease
- Inflammatory bowel disease (IBD)
- Chronic pancreatitis
- Cystic fibrosis
Can floating stools indicate a serious health problem? While most cases of floating stools are harmless, persistent floating stools accompanied by other symptoms such as weight loss, abdominal pain, or changes in bowel habits may warrant medical attention.
Identifying Problematic Floating Stools
While occasional floating stools are generally not a cause for concern, certain characteristics may indicate a need for medical evaluation. Pay attention to the following:

- Persistent floating stools
- Greasy or oily appearance
- Foul odor
- Pale or clay-colored stools
- Accompanying symptoms like weight loss or abdominal pain
How can you differentiate between harmless and problematic floating stools? Monitor the frequency and duration of floating stools, along with any additional symptoms. If floating stools persist for several weeks or are accompanied by other concerning symptoms, consult a healthcare professional.
Home Remedies and Lifestyle Changes for Floating Stools
In many cases, floating stools can be addressed through simple lifestyle modifications and home remedies. Consider the following approaches:
- Identify and avoid trigger foods
- Increase water intake
- Reduce consumption of gas-producing foods
- Eat smaller, more frequent meals
- Incorporate probiotics into your diet
Can dietary changes alone resolve floating stools? In many cases, yes. If floating stools are caused by dietary factors, making appropriate changes to your eating habits can often resolve the issue.
:max_bytes(150000):strip_icc()/148536109-56a5080f3df78cf7728605b6.jpg)
When to Seek Medical Attention for Floating Stools
While floating stools are often harmless, certain situations warrant medical evaluation. Contact your healthcare provider if you experience:
- Persistent floating stools lasting several weeks
- Bloody stools
- Unexplained weight loss
- Dizziness or fever accompanied by floating stools
- Chronic diarrhea
- Abdominal pain or discomfort
How quickly should you seek medical attention for concerning symptoms? If you experience bloody stools accompanied by weight loss, dizziness, and fever, contact your healthcare provider immediately.
Diagnostic Procedures for Floating Stools
When you consult a healthcare professional about floating stools, they may perform various diagnostic procedures to determine the underlying cause. These may include:
- Physical examination
- Detailed medical history
- Stool sample analysis
- Blood tests
- Imaging studies (in some cases)
What questions might a healthcare provider ask during the evaluation? Your doctor may inquire about the onset and frequency of floating stools, your diet, any recent dietary changes, and the presence of other symptoms such as abdominal pain or weight loss.

Specific Diagnostic Questions
Healthcare providers often ask targeted questions to gather relevant information. Some common questions include:
- When did you first notice the floating stools?
- Do they occur consistently or intermittently?
- Have you made any recent changes to your diet?
- Do you experience any other digestive symptoms?
- Have you noticed any changes in stool color or odor?
Treatment Options for Floating Stools
The treatment for floating stools depends on the underlying cause. In many cases, simple dietary modifications may be sufficient. However, if a medical condition is identified, specific treatments may be necessary. Some potential treatment approaches include:
- Dietary adjustments
- Probiotics or digestive enzyme supplements
- Medications to address underlying conditions
- Treatment of infections (if present)
- Management of chronic conditions like celiac disease or IBD
Is medical treatment always necessary for floating stools? No, in many cases, floating stools resolve on their own or with simple dietary changes. However, if an underlying medical condition is identified, appropriate treatment may be required.

Dietary Recommendations for Managing Floating Stools
If dietary factors are contributing to floating stools, your healthcare provider may recommend the following adjustments:
- Reducing intake of gas-producing foods
- Limiting consumption of artificial sweeteners
- Increasing fiber intake gradually
- Staying hydrated
- Avoiding foods that trigger digestive issues
Prevention and Long-term Management of Floating Stools
While not all cases of floating stools can be prevented, certain strategies can help reduce their occurrence and promote overall digestive health:
- Maintain a balanced diet
- Stay hydrated
- Exercise regularly
- Manage stress
- Avoid trigger foods
- Practice mindful eating
Can lifestyle changes prevent all instances of floating stools? While a healthy lifestyle can significantly reduce the occurrence of floating stools, some cases may be due to underlying medical conditions that require specific treatment.
Monitoring Digestive Health
To maintain optimal digestive health and catch potential issues early, consider the following practices:

- Pay attention to changes in bowel habits
- Keep a food diary to identify potential triggers
- Schedule regular check-ups with your healthcare provider
- Discuss any persistent digestive symptoms with a medical professional
- Stay informed about digestive health and potential warning signs
Floating stools, while often harmless, can sometimes indicate underlying health issues. By understanding the potential causes, recognizing warning signs, and knowing when to seek medical attention, you can effectively manage this common digestive occurrence. Remember that maintaining a healthy lifestyle and open communication with your healthcare provider are key to optimal digestive health.
Stools – floating Information | Mount Sinai
Floating stools
Stools that float are most often due to poor absorption of nutrients (malabsorption) or too much gas (flatulence).
Food passes from the stomach into the small intestine. In the small intestine all nutrient absorption occurs. Whatever has not been absorbed by the small intestine passes into the colon. In the colon most of the water is absorbed from the food residue. The residue is then eliminated from the body as feces.
Considerations
Most causes of floating stools are harmless. In most cases, floating stools will go away without treatment.
Floating stools alone are not a sign of an illness or other health problem.
Causes
Many things can cause floating stools. Most of the time, floating stools are due to what you eat. A change in your diet may cause an increase in gas. Increased gas in the stool allows it to float.
Floating stools may also happen if you have a gastrointestinal infection.
Floating, greasy stools that are foul smelling may be due to severe malabsorption, particularly if you are losing weight. Malabsorption means your body is not properly absorbing nutrients.
Malabsorption means your body is not properly absorbing nutrients.
Most floating stools are not caused by an increase in the fat content of the stool. However, in some conditions, such as long-term (chronic) pancreatitis, the fat content is increased.
Home Care
If a change in diet has caused floating stools or other health problems, try to find which food is to blame. Avoiding this food may be helpful.
When to Contact a Medical Professional
Tell your health care provider if you have changes in your stools or bowel movements. Contact your provider right away if you have bloody stools with weight loss, dizziness, and fever.
Contact your provider right away if you have bloody stools with weight loss, dizziness, and fever.
What to Expect at Your Office Visit
Your provider will perform a physical exam and ask questions about your medical history and symptoms, such as:
- When did you first notice the floating stools?
- Does it happen all the time or from time to time?
- What is your usual diet?
- Does a change in your diet change your stools?
- Do you have other symptoms?
- Are the stools foul smelling?
- Are the stools an abnormal color (such as pale or clay-colored stools)?
A stool sample may be needed. Blood tests may be done.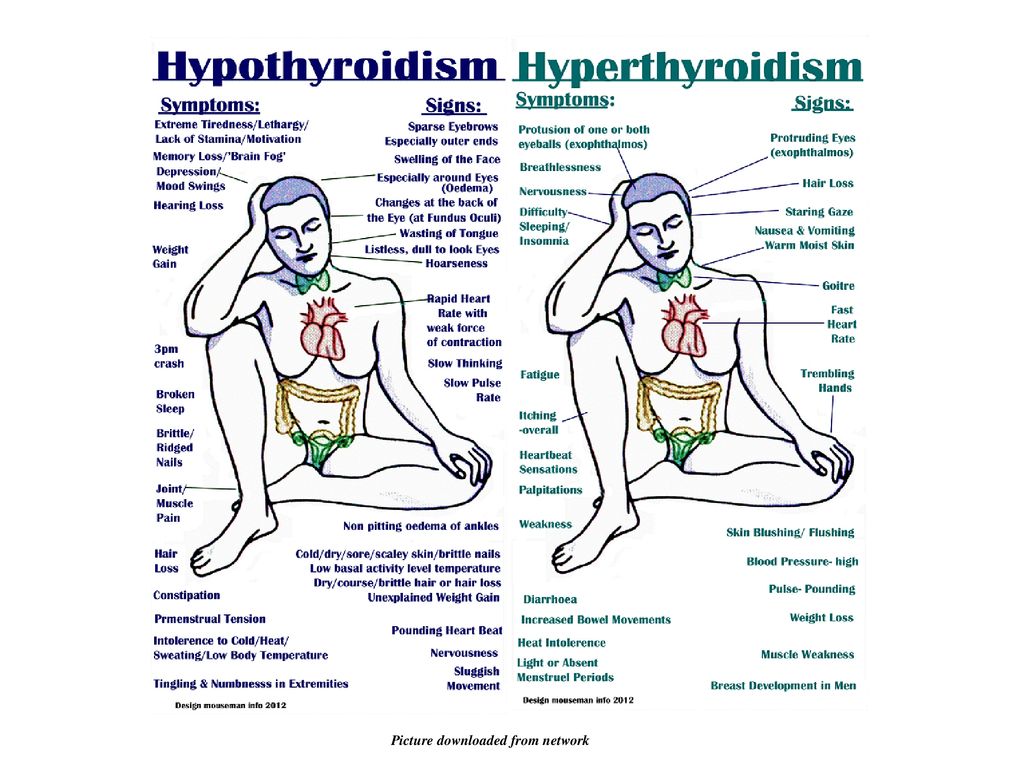 In most cases, however, these tests will not be needed.
In most cases, however, these tests will not be needed.
Treatment depends on the specific diagnosis.
Höegenauer C, Hammer HF. Maldigestion and malabsorption. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 104.
Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 16.
Semrad CE. Approach to the patient with diarrhea and malabsorption. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 131.
Last reviewed on: 5/4/2022
Reviewed by: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Acute vs. chronic pancreatitis: Differences and similarities
Pancreatitis is inflammation of the pancreas. It can be either acute, producing temporary symptoms, or chronic, leading to long-term damage.
Acute pancreatitis may lead to chronic pancreatitis in some cases, but there are some important differences between the conditions.
Diagnosing the underlying cause of the inflammation is crucial in both types of pancreatitis, as unchecked inflammation may lead to long-term damage or other complications.
Pancreatitis is inflammation of the pancreas. The pancreas has important functions in the body, including making digestive enzymes and insulin. Pancreatitis occurs when the pancreatic enzymes damage the pancreatic tissue itself, causing inflammation.
This inflammation may be either temporary or long lasting.
While acute and chronic pancreatitis share a name, they are actually two different conditions.
Acute pancreatitis is the active form of pancreatitis, in which the symptoms come on suddenly. A person may experience severe stomach pain, alongside nausea and vomiting.
A blood test will reveal high levels of pancreatic enzymes.
Chronic pancreatitis is a lasting condition that may stem from repeated damage to the pancreas rather than from an acute inflammatory process. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) note that damage to the pancreas can be permanent and may worsen over time, potentially causing long-term symptoms.
The course of the condition is also different. The NIDDK state that with treatment, most people with acute pancreatitis get better in a few days.
In those with chronic pancreatitis, the symptoms may not fully subside. The condition remains present due to damage in the pancreas that does not go away.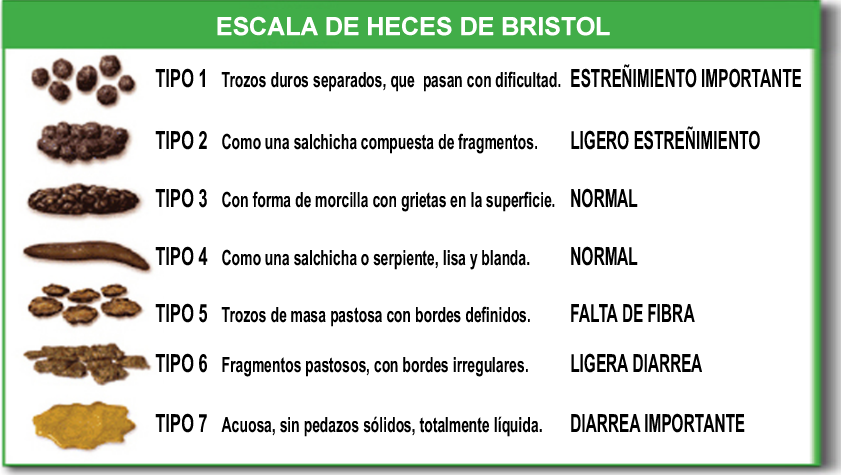
The underlying causes are also different for both types. There are many possible causes of pancreatitis.
The NIDDK note that acute pancreatitis most commonly occurs as a complication of gallstones. Gallstones may cause inflammation in the pancreas or pancreatic duct.
Common causes of chronic pancreatitis are heavy alcohol use and genetic disorders.
Other causes of both types of pancreatitis may include:
- reactions to some medicines
- complications from infections
- complications from surgery
- pancreatic cancer
- injury to the abdomen
- a condition called pancreas divisum
Both acute and chronic pancreatitis can sometimes be idiopathic, which means that doctors cannot identify an underlying cause.
Pain may be another differentiating factor for acute and chronic pancreatitis.
Acute pancreatitis is generally temporary, and the person will often fully recover within a few days. On the other hand, pain from chronic pancreatitis may come and go or be consistent for months at a time.
While they are different issues, acute pancreatitis may also be a risk factor for chronic pancreatitis.
Research from 2018 notes that about 20% of people with acute pancreatitis have a recurrence of the issue. Of these individuals, about 36% will go on to develop chronic pancreatitis.
Chronic pancreatitis has numerous other risk factors, including:
- alcohol use
- smoking
- obesity
- genetic factors
- autoimmune responses
- abnormalities within the organ itself
Acute pancreatitis causes a sudden bout of active inflammation in the pancreas. This inflammation may cause a few symptoms, such as:
- stomach pain
- pain that comes on suddenly or intensifies quickly
- pain that radiates from the abdomen to the back
- pain that gets worse after a meal
- a tender, swollen abdomen
- fever
- fast resting heart rate
The symptoms are generally uncomfortable enough for the person to seek medical attention. Doctors will perform blood tests, which will reveal high levels of pancreatic enzymes in the person’s blood.
Doctors will perform blood tests, which will reveal high levels of pancreatic enzymes in the person’s blood.
Chronic pancreatitis may produce symptoms similar to those of acute pancreatitis, but it has distinct symptoms and risks.
Chronic pancreatitis causes constant or regular bouts of stomach pain. This pain may not go away completely, or it may come and go.
Other symptoms may include:
- pain that gets worse after a meal
- nausea or vomiting
- fatigue
- excessive thirst
- changes in skin color
- unintentional weight loss
- malnutrition
- greasy or oily stools
- fibrosis or scarring on the pancreas
The condition can also make diabetes more difficult to manage.
Diagnosing acute or chronic pancreatitis involves analyzing the person’s symptoms via tests and eliminating other possible causes.
Doctors will carry out a physical exam to look for signs of trauma or other abdominal symptoms. They will ask the person about their medical history and any lifestyle choices that may affect the organs, such as drinking or smoking.
They will also order blood work to check for high levels of pancreatic enzymes. If the results of these tests are inconclusive, doctors may order imaging tests, such as a CT scan or ultrasound, to look at the pancreas itself or the organs around it.
In cases of chronic pancreatitis, doctors use various imaging tests, such as CT scans, MRIs, and ultrasounds, to check the pancreas.
Chronic pancreatitis may produce telling symptoms, such as constant or regular stomach pain, diabetes that is difficult to control, and oily or greasy stools. Doctors are likely to ask about or test for these factors before confirming a diagnosis.
Pain management is important in treating both acute and chronic pancreatitis. Doctors will give the person medications to control pain while carrying out the diagnosis and developing a proper treatment plan.
Treatment for both forms of pancreatitis may include intravenous (IV) fluids, which prevent dehydration and provide nutrition if the person cannot eat or swallow. Some people may require antibiotics or other medications.
Some people may require antibiotics or other medications.
Those with acute pancreatitis may also need other forms of treatment, depending on the underlying cause. In cases where gallstones cause symptoms, doctors may recommend surgery to remove the gallbladder.
Other procedures may be necessary, such as processes to drain fluids from abscesses or remove damaged parts of the pancreas itself.
For acute pancreatitis, the NIDDK note that symptoms may subside within a few days with treatment. Even in mild cases, it is important to see a doctor for a thorough diagnosis of the underlying cause.
Treatment for chronic pancreatitis involves controlling the symptoms and complications. The inflammation and damage from chronic pancreatitis are irreversible, and the pancreas does not heal over time.
Treatment may sometimes include surgery to remove pancreatic stones or other blockages.
Other treatments may include:
- treatment for diabetes
- nutritional supplements and vitamins
- enzyme tablets
- other procedures, such as nerve blockers
With proper treatment, many people can maintain their quality of life.
Anyone experiencing severe stomach pain should call their doctor or seek immediate medical attention. A quick diagnosis is important in each case to begin any possible treatments.
Controlling damage from acute pancreatitis is important to reduce the chance of complications. Although it is not possible to reverse the damage or inflammation that chronic pancreatitis causes, regular treatment is important to help control other complications and help the person get relief from the symptoms.
Feces buoyancy linked to intestinal microbiota
American researchers figured out why some feces sink in water while others float on the surface. According to experiments on mice, the composition of the intestinal microbiota is solely responsible for this. The report on the work was published in the journal Scientific Reports .
Feces 10-15 percent of people float on the surface of the water, and this is not associated with any pathological condition. Among people with functional bowel disorders, this proportion rises to about one in four. Historically, it was believed that the buoyancy of feces is due to the high content of fat in it, but in 19In 1972, Michael Levitt, a gastroenterologist from the University of Minnesota, and his student William Duane, in experiments with the stool of 39 people (including six patients with steatorrhea), showed that even fatty feces sink when gas is removed. The researchers did not specify the origin of the gas component, and this question, which has the potential for clinical application, has remained open until now.
Historically, it was believed that the buoyancy of feces is due to the high content of fat in it, but in 19In 1972, Michael Levitt, a gastroenterologist from the University of Minnesota, and his student William Duane, in experiments with the stool of 39 people (including six patients with steatorrhea), showed that even fatty feces sink when gas is removed. The researchers did not specify the origin of the gas component, and this question, which has the potential for clinical application, has remained open until now.
To understand it, staff at the Mayo Clinic in Rochester, Minnesota, under the direction of Nagarajan Kannan, used conventional C57BL/6 (B6) and gnotobiotic (born and reared in aseptic conditions that do not have a microbiome) mice. Some of the latter have been colonized with microbiota in their intestines by a single intragastric injection of the drug, either in the faeces of normal mice or one of two healthy women, or by allowing contact with environmental bacteria. Fecal sterility of germ-free mice and successful colonization of the intestines of the rest were confirmed by polymerase chain reaction, scanning electron microscopy, and measurement of bacterial DNA concentration (a measure of microbiota density).
Fecal sterility of germ-free mice and successful colonization of the intestines of the rest were confirmed by polymerase chain reaction, scanning electron microscopy, and measurement of bacterial DNA concentration (a measure of microbiota density).
Flow cytometry showed that the number of undigested particles of food biomass is inversely related to the density of the intestinal microbiota. In thermogravimetry, the feces of germ-free mice differed from the rest of the samples in at least three temperature ranges; pycnometry revealed its significant superiority in relative density. The shape, size and color of the stool in all groups of animals did not differ.
To assess the buoyancy of faeces, the researchers used a simple LIFT test they had previously developed – levô in fimo (literally translated from Latin as “raising in dung”) test. It consists in placing stool fragments in water and a Trump fixer solution (10 percent formaldehyde and one percent glutaraldehyde) in phosphate buffer (TFS), followed by recording their position (at the bottom or surface) after a minute, hour and day. It turned out that all samples from germ-free mice sink in water and TFS in less than a minute, while about half of the bacteria-colonized samples remain on the surface of the water and all of them continue to swim in TFS after a day.
It turned out that all samples from germ-free mice sink in water and TFS in less than a minute, while about half of the bacteria-colonized samples remain on the surface of the water and all of them continue to swim in TFS after a day.
Also, the authors of the work performed simultaneously LIFT and microbiota density determination in gnotobiotic mice before intragastric colonization (all faeces were drowned, bacterial DNA was practically not determined) and after it weekly for 12 weeks. By the third week, with all methods of microbiota formation (transplantation from mice and humans, from a non-sterile environment), the DNA concentration in the whole stool began to stabilize at a level of more than 10 thousand nanograms per milligram, from that time all biosamples floated.
Metagenomic analysis of the intestinal microbiota of conventional, artificially colonized gnotobiotic and their donor mice revealed 13 dominant species of gasogenic bacteria from 11 genera, and their composition in different animals was extremely heterogeneous. The most common was methane-producing Bacteroides ovatus , associated, as previously shown, with an increased risk of flatulence in humans.
The most common was methane-producing Bacteroides ovatus , associated, as previously shown, with an increased risk of flatulence in humans.
Thus, the buoyancy of feces depends solely on the gases produced by the microbiota; Swallowed air and the chemical composition of the dense matter of the stool do not play a role in this, Kannan concluded.
In 2019, Tufts University researchers reported that fecal transplants from physically fit older adults significantly increased the grip strength of mice. At the same time, a Belgian-Dutch scientific group showed that the intestinal microbiota affects the quality of life and the risk of developing depression. In turn, the species composition of bacteria in the gastrointestinal tract depends on at least 69 main factors, including such non-obvious ones as the opinion of one’s own body weight and plans to reduce it, preferences for chocolate varieties and taking antidepressants – the Dutch, Belgian, Russian and British scientists.
You can read about the various uses of excrement in wildlife in the blog “It’s the norm: about the instrumental use of feces.” Issues related to fecal transplantation are analyzed in detail by Doctor of Biological Sciences, Professor Mikhail Gelfand.
On mice
Found a typo? Select the fragment and press Ctrl+Enter.
Flakes in the urine – the causes of occurrence, in what diseases it occurs, diagnosis and methods of treatment
Fungus
Cystitis
Thrush
Colpitis
75903
27th of December
Flakes in the urine: the causes of occurrence, in which diseases they occur, diagnosis and methods of treatment.
Definition
Urine is a waste product produced by the complex process of blood filtration by the kidneys. Urine flows from the kidneys through the ureters to the bladder, then through the urethra it is excreted.
By producing urine, the kidneys remove protein breakdown products, food additives, processed drugs from the body, and also regulate the amount of water and electrolytes in the body. Normal urine is more than 90% water, it can detect urea, uric acid, ammonia, creatinine, sodium, potassium, chlorine, calcium ions. In minimal amounts, protein and blood cells (erythrocytes and leukocytes), epithelium (cells lining the urinary tract) enter the urine. Urine color is determined by the pigments urobilin and urochrome. Normally, and subject to the technique of collecting urine, glucose, hemoglobin, bilirubin pigment, ketone bodies (a product of carbohydrate and fat metabolism), lipids, salts, bacteria, fungi, and mucus are not detected in it. There are no cylinders – casts of protein, epithelium, leukocytes, erythrocytes, hemoglobin and fats.
With the proper functioning of the internal organs, a balanced diet, a normal drinking regime and the absence of coloring substances in food, urine is formed in the amount of 1–1. 5 liters per day, it is yellow or straw-yellow in color, without a strong odor, does not foam, is transparent, has no suspension and sediment.
5 liters per day, it is yellow or straw-yellow in color, without a strong odor, does not foam, is transparent, has no suspension and sediment.
In case of pathology of the urinary system or in case of incorrect collection of biomaterial, substances appear in the urine that should not be in it.
Urine flakes are visible clots, usually white, yellow, or red, floating in the collected urine.
Varieties of flakes in urine
Flakes in urine vary in composition. In the form of flakes, there may be protein, leukocytes, erythrocytes, pus, accumulation of bacteria, fungi, mucus, epithelium (the surface layer of the skin and mucous membranes), etc.
Possible causes of flakes in the urine
The most common causes of flakes in the urine include inflammatory diseases of the genitourinary system.
A precipitate in the form of flakes is detected when the rules for collecting urine are not followed, because of which vaginal discharge, the secret of the glands of the external genital organs, the epithelium of the skin and mucous membranes, etc. , get into it.
, get into it.
What diseases cause flakes in the urine
Urethritis – inflammation of the mucous membrane (inner lining) of the urethra. The disease is usually infectious, caused by bacteria, fungi, viruses, or protozoa. Less commonly, urethritis is allergic or traumatic. Symptoms of urethritis are pain, burning, cramps when urinating. With bacterial urethritis, the amount of protein in the urine increases, mucus, pus appear, the number of leukocytes increases, bacteria are present, sometimes epithelial cells of the urethra and blood. With candidal urethritis, accumulations of yeast-like fungi are found in the urine.
With cystitis – inflammation of the bladder – frequent painful urination, pain above the womb, radiating to the perineum, anus, in men – to the penis.
The disease is infectious in nature and is manifested by the same changes in the urine as urethritis.
With pyelonephritis – bacterial inflammation of the kidney tissue – the temperature rises sharply (up to 40 ° C), chills, increased sweating, weakness, pain in the lumbar region occur. Urine becomes cloudy, a large number of bacteria, leukocytes are found in it, pus appears, the level of protein and erythrocytes increases.
Urine becomes cloudy, a large number of bacteria, leukocytes are found in it, pus appears, the level of protein and erythrocytes increases.
Pyelonephritis often occurs against the background of obstruction of urine output, for example, when the ureters are compressed by the uterus in pregnant women, prostate enlargement, with urolithiasis, and prolonged urinary retention.
Prostatitis – inflammation of the prostate gland. The disease is usually bacterial in nature. In addition to the possible appearance of epithelium, leukocytes, erythrocytes, mucus, bacteria, pus in the urine, with prostatitis, there are impaired urination with frequent urges, pain in the sacrum, perineum and anus, and fever.
Candidiasis (fungal colonization) of the vagina is accompanied by itching and discomfort in the vagina and in the vulva, as well as cheesy secretions, which, together with mucus and epithelium, can enter the urine.
Bacteria, leukocytes, mucus, epithelium may appear in the urine in the form of flakes with bacterial vaginosis – imbalance of the vaginal microflora in favor of opportunistic microorganisms (living in the vagina permanently and capable of causing disease under certain circumstances), as well as with colpitis or vaginitis (inflammation of the vagina infected with Trichomonas, gonococci, streptococci, staphylococci, etc. ).
).
Another disease that causes the appearance of flakes in the urine is bladder leukoplakia , in which the epithelium of the bladder mucosa thickens (keratinizes), becomes similar in structure to the skin, and when rejected appears in the urine in the form of flakes.
Symptoms are frequent painful urination with frequent urges, frequent nighttime urination, pain over the womb, blood and flakes in the urine. The disease can lead to the development of bladder cancer.
Which doctors to contact
If flakes appear in the urine, contact
general practitioner or
therapist. If necessary, a consultation can be scheduled
urologist,
gynecologist.
Diagnosis and examination in the presence of flakes in the urine
If flakes are found in the urine, the doctor will conduct a thorough questioning and examination of the patient, identify additional symptoms, if any.
To clarify the diagnosis, you may need:
- complete blood count;
Clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes)
Synonyms: Complete blood count, UAC. Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram.
Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram.
Brief description of the study CBC: general a…
Up to 1 business day
Available with home visit
RUB 810
Add to cart
General urinalysis (Urine analysis with sediment microscopy)
Method of determination
Determination of physical and chemical parameters is carried out on an automatic analyzer using the “dry chemistry” method.
Hardware microscope…
Up to 1 business day
Available with home visit
410 RUB
Add to cart
Nechiporenko Urine Test
Synonyms: Determination of the amount of blood cells in the urine sediment; Sample of Nechiporenko; Urinalysis by the Nechiporenko method.
Analysis of urine Nechiporenko; Urinalysis; Urine…
Up to 1 business day
Available with home visit
475 RUB
Add to cart
Urinalysis
Material for research:
smears prepared in the laboratory from the sediment of transudates, exudates, secrets, excreta and urine;
smears prepared from …
Up to 2 business days
Available with home visit
RUB 1,030
Add to cart
Detection of STI pathogens (7+KVM*), scraping of epithelial cells of the urogenital tract
Determination of the DNA of microorganisms that cause the most common sexually transmitted infections (STIs) in the vaginal, cervical and urethral nipples. ..
..
Up to 1 business day
Available with home visit
RUB 3,185
Add to cart
Ultrasound of the prostate
Ultrasound scan of the prostate, giving an idea of the condition of the prostate and the presence of pathology.
RUB 2,190
Sign up
Treatment for flakes in the urine
Treatment for flakes in the urine is to eliminate the cause of the flakes.
In case of inflammatory diseases of the urinary tract and organs of the reproductive system, the doctor may recommend antibacterial, antifungal therapy, as well as prescribe anti-inflammatory, analgesic and antispasmodic drugs. In women, after the main treatment, the normal microflora of the vagina is restored.
A sparing diet is recommended with the exception of fried, spicy, salty, floury, sweet, alcohol, drinking plenty of water, as well as sexual abstinence for the duration of treatment.
What to do if flakes are found in the urine
If you notice flakes in the urine, you need to make sure that all the rules for collecting urine have been observed: urine should be collected in a special sterile container about two hours before delivery, after having carried out hygiene procedures (with water, without use of soap and intimate hygiene products). You need to collect an average portion of urine, during urination, cover the entrance to the vagina with a sterile napkin.
If all the conditions are met, and there are still flakes in the urine, it is this urine that needs to be taken for analysis.
To confirm the detected changes, the doctor may recommend a second urine test. You should not leave this symptom unattended or self-medicate, this can lead to unpredictable consequences.