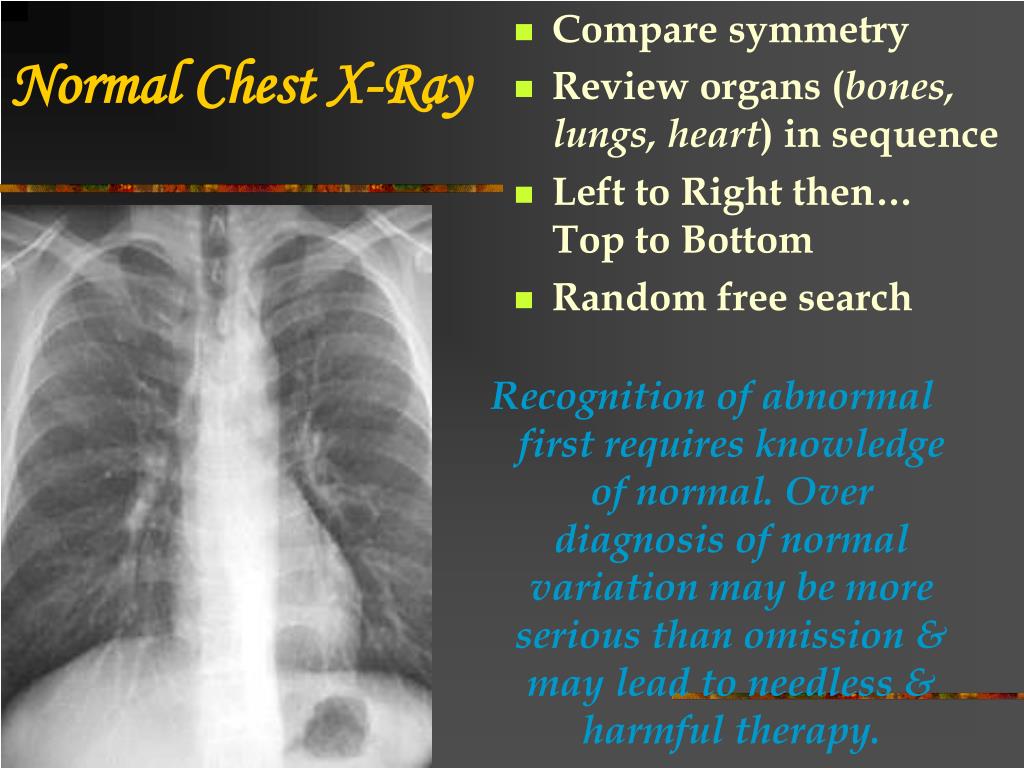
Haziness on chest x ray. Portable Chest X-ray in COVID-19: Key Findings and Imaging Patterns
How does portable chest X-ray compare to CT for detecting COVID-19 lung abnormalities. What are the most common radiographic features of COVID-19 pneumonia on chest X-ray. How can radiologists and clinicians recognize typical imaging patterns of coronavirus infection on portable chest films.
Chest X-ray vs CT for COVID-19 Detection
While much of the early radiology literature on COVID-19 focused on CT findings, portable chest X-ray (CXR) has emerged as a crucial frontline imaging tool during the pandemic. Why is this the case? There are several key reasons:
- Infection control: CXR can be performed at the bedside, avoiding patient transport and potential virus spread
- Efficiency: CT rooms require extensive decontamination after imaging COVID-19 patients
- Availability: Many parts of the world lack widespread access to CT scanners
- Triage: A positive CXR may eliminate the need for CT in high clinical suspicion cases
The American College of Radiology has endorsed the use of portable CXR to minimize cross-infection risks. However, it’s important to note that CXR is less sensitive than CT for detecting subtle COVID-19 lung abnormalities, with a reported baseline sensitivity of 69%.
Common Radiographic Manifestations of COVID-19
What are the hallmark imaging features of COVID-19 pneumonia on chest X-ray? The most frequently reported findings include:
- Ground-glass opacities
- Consolidation
- Reticular opacities
- Hazy pulmonary densities
Ground-glass opacities seen on CT may manifest as vague hazy densities on CXR that can be extremely subtle. Reticular opacities accompanying areas of ground-glass attenuation are often more readily appreciable on standard CXR compared to the ground-glass component alone.
Distribution and Patterns of Lung Involvement
How does the distribution of COVID-19 pneumonia differ from other types of pneumonia? Unlike typical community-acquired bacterial pneumonia which tends to be unilateral and confined to a single lobe, COVID-19 pneumonia frequently demonstrates the following characteristics:
- Bilateral lung involvement
- Multifocal air-space disease affecting more than one lobe
- Predominant lower lung zone distribution
- Peripheral lung involvement
The peripheral distribution is considered one of the more specific imaging features of COVID-19, often mimicking other inflammatory processes like organizing pneumonia. One study found peripheral lung involvement in 33% of COVID-19 chest CTs.

Progression of Radiographic Findings
How do COVID-19 related lung abnormalities evolve over time on chest X-ray? The typical progression includes:
- Early stage: Subtle unilateral or bilateral opacities
- Progressive stage: Increasing multifocal air-space opacities
- Peak stage: Widespread confluent bilateral opacities
- Absorption stage: Gradual resolution of opacities
It’s important to note that radiographic findings may lag behind clinical improvement. Some patients may show persistent opacities on CXR even after clinical recovery.
Challenges in Radiographic Interpretation
What are some of the difficulties in interpreting chest X-rays for COVID-19? Several factors can complicate accurate diagnosis:
- Subtle nature of early findings
- Overlap with other viral and atypical pneumonias
- Varied appearance based on disease stage
- Technical factors like patient positioning and inspiration
Radiologists and clinicians must be aware of these challenges and maintain a high index of suspicion in the appropriate clinical context.

Role of Artificial Intelligence in COVID-19 Chest X-ray Analysis
Can artificial intelligence assist in detecting COVID-19 on chest X-rays? Several AI algorithms have been developed to aid in the radiographic diagnosis of COVID-19:
- Automated detection of characteristic opacities
- Quantification of disease extent and severity
- Differentiation from other types of pneumonia
- Prediction of outcomes based on imaging features
While promising, these AI tools are still in the early stages of development and validation. They should be used as an adjunct to, not a replacement for, expert radiologist interpretation.
Correlation of Radiographic Findings with Clinical Outcomes
Do chest X-ray findings correlate with COVID-19 severity and prognosis? Several studies have investigated this relationship:
- Extent of lung involvement on CXR may predict need for hospitalization
- Rapid progression of opacities associated with worse outcomes
- Bilateral peripheral opacities more common in severe cases
- Persistent abnormalities may indicate long-term lung damage
However, it’s crucial to interpret radiographic findings in conjunction with clinical and laboratory data for comprehensive patient assessment.

Comparing Chest X-ray to RT-PCR Testing
How does the diagnostic performance of chest X-ray compare to RT-PCR testing for COVID-19? While RT-PCR remains the gold standard, CXR can play a complementary role:
- CXR may be positive in some RT-PCR negative cases
- CXR abnormalities can persist after RT-PCR turns negative
- CXR can help assess disease severity and progression
- CXR is more readily available in resource-limited settings
In areas with limited access to RT-PCR testing, CXR may serve as a valuable diagnostic tool when interpreted in the appropriate clinical context.
Portable X-ray Equipment Considerations
What are some important factors to consider when using portable X-ray equipment for COVID-19 patients?
- Infection control protocols for equipment decontamination
- Use of disposable plastic covers for the X-ray detector
- Proper personal protective equipment (PPE) for radiographers
- Optimizing exposure techniques for bedside imaging
- Strategies to minimize motion artifact in critically ill patients
Attention to these technical and safety considerations is crucial for obtaining diagnostic quality images while protecting healthcare workers.
Follow-up Imaging Recommendations
What are the current recommendations for follow-up chest imaging in COVID-19 patients? Guidelines vary, but general principles include:
- Daily CXRs not routinely recommended for stable, intubated patients
- Consider follow-up CXR for clinical deterioration or recovery assessment
- Discharge CXR may be obtained to establish a new baseline
- Long-term follow-up may be warranted for patients with persistent symptoms
The frequency and duration of follow-up imaging should be tailored to individual patient needs and clinical course.
Differentiating COVID-19 from Other Pneumonias
How can radiologists distinguish COVID-19 pneumonia from other types of pneumonia on chest X-ray? While there is significant overlap, some features that may suggest COVID-19 include:
- Bilateral, multifocal involvement
- Peripheral and lower zone predominance
- Absence of pleural effusions in early disease
- Lack of lobar consolidation typical of bacterial pneumonia
- Rapid progression of opacities over days
However, definitive diagnosis requires correlation with clinical presentation and laboratory testing.

Pediatric Considerations in COVID-19 Chest Imaging
Are there unique considerations for interpreting chest X-rays in pediatric COVID-19 patients? Several factors distinguish pediatric cases:
- Generally milder radiographic findings compared to adults
- Higher likelihood of normal initial CXR
- Peribronchial thickening more common than in adults
- Need to consider alternative diagnoses like bronchiolitis
- Importance of minimizing radiation exposure in follow-up
Pediatric radiologists must be familiar with these age-specific patterns to accurately interpret COVID-19 chest X-rays in children.
Imaging Findings in Vaccinated Individuals
Do COVID-19 chest X-ray findings differ in vaccinated versus unvaccinated individuals? Early research suggests some potential differences:
- Generally milder and less extensive abnormalities in vaccinated patients
- Possibly lower incidence of bilateral involvement
- Faster radiographic resolution in some vaccinated cases
- Need for larger studies to confirm these preliminary observations
As vaccination efforts continue worldwide, understanding these potential differences will be crucial for accurate interpretation of COVID-19 chest X-rays.

Role of Chest X-ray in Long COVID Assessment
Can chest X-ray play a role in evaluating patients with long COVID syndrome? While research is ongoing, potential applications include:
- Assessing for persistent radiographic abnormalities
- Monitoring for development of fibrotic changes
- Evaluating for alternative cardiopulmonary causes of symptoms
- Establishing a baseline for long-term follow-up
The optimal imaging strategy for long COVID patients is still being determined, but chest X-ray is likely to remain an important tool in their longitudinal care.
Future Directions in COVID-19 Chest Imaging
What developments can we expect in the field of COVID-19 chest imaging? Several exciting areas of research and innovation are emerging:
- Advanced AI algorithms for automated diagnosis and prognosis
- Novel portable X-ray technologies for improved bedside imaging
- Integration of radiomics and deep learning for outcome prediction
- Standardized reporting systems for COVID-19 chest X-rays
- Techniques to better visualize subtle ground-glass opacities on CXR
These advancements promise to enhance the diagnostic accuracy and clinical utility of chest X-ray in the ongoing management of COVID-19.

As the COVID-19 pandemic continues to evolve, portable chest X-ray remains a critical frontline imaging tool. Understanding the typical radiographic manifestations, distribution patterns, and temporal progression of COVID-19 pneumonia is essential for radiologists and clinicians alike. While chest CT offers superior sensitivity, the practical advantages of portable X-ray in terms of infection control, efficiency, and accessibility make it an indispensable modality in the fight against coronavirus. Ongoing research into AI applications, correlation with clinical outcomes, and comparison with other diagnostic methods will further refine the role of chest X-ray in COVID-19 management. As we look to the future, continued innovation in portable X-ray technology and interpretation strategies will undoubtedly enhance our ability to diagnose, monitor, and ultimately overcome this global health challenge.
Portable chest X-ray in coronavirus disease-19 (COVID-19): A pictorial review
- Journal List
- Elsevier – PMC COVID-19 Collection
- PMC7141645
As a library, NLM provides access to scientific literature. Inclusion in an NLM database does not imply endorsement of, or agreement with,
the contents by NLM or the National Institutes of Health.
Learn more about our disclaimer.
Clin Imaging. 2020 Aug; 64: 35–42.
Published online 2020 Apr 8. doi: 10.1016/j.clinimag.2020.04.001
Author information Article notes Copyright and License information Disclaimer
As the global pandemic of coronavirus disease-19 (COVID-19) progresses, many physicians in a wide variety of specialties continue to play pivotal roles in diagnosis and management. In radiology, much of the literature to date has focused on chest CT manifestations of COVID-19 (Zhou et al. [1]; Chung et al. [2]). However, due to infection control issues related to patient transport to CT suites, the inefficiencies introduced in CT room decontamination, and lack of CT availability in parts of the world, portable chest radiography (CXR) will likely be the most commonly utilized modality for identification and follow up of lung abnormalities. In fact, the American College of Radiology (ACR) notes that CT decontamination required after scanning COVID-19 patients may disrupt radiological service availability and suggests that portable chest radiography may be considered to minimize the risk of cross-infection (American College of Radiology [3]). Furthermore, in cases of high clinical suspicion for COVID-19, a positive CXR may obviate the need for CT. Additionally, CXR utilization for early disease detection may also play a vital role in areas around the world with limited access to reliable real-time reverse transcription polymerase chain reaction (RT-PCR) COVID testing.
In radiology, much of the literature to date has focused on chest CT manifestations of COVID-19 (Zhou et al. [1]; Chung et al. [2]). However, due to infection control issues related to patient transport to CT suites, the inefficiencies introduced in CT room decontamination, and lack of CT availability in parts of the world, portable chest radiography (CXR) will likely be the most commonly utilized modality for identification and follow up of lung abnormalities. In fact, the American College of Radiology (ACR) notes that CT decontamination required after scanning COVID-19 patients may disrupt radiological service availability and suggests that portable chest radiography may be considered to minimize the risk of cross-infection (American College of Radiology [3]). Furthermore, in cases of high clinical suspicion for COVID-19, a positive CXR may obviate the need for CT. Additionally, CXR utilization for early disease detection may also play a vital role in areas around the world with limited access to reliable real-time reverse transcription polymerase chain reaction (RT-PCR) COVID testing.
The purpose of this pictorial review article is to describe the most common manifestations and patterns of lung abnormality on CXR in COVID-19 in order to equip the medical community in its efforts to combat this pandemic.
Keywords: COVID-19, Coronavirus, Chest X-ray, Chest CT
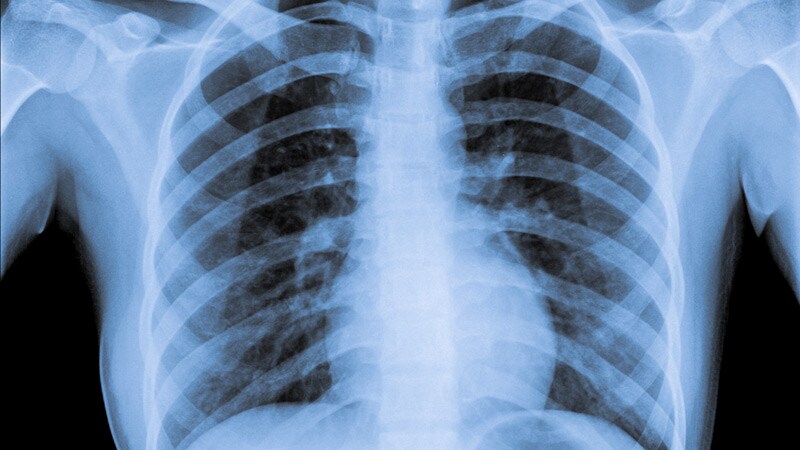
CXR is a less sensitive modality in the detection of COVID-19 lung disease compared to CT, with a reported baseline CXR sensitivity of 69% [4]. The most common reported CXR and CT findings of COVID-19 include lung consolidation and ground glass opacities2.
Ground glass densities observed on CT may often have a correlate that is extremely difficult to detect on CXR (,
).
Open in a separate window
Portable CXR (left) with vague hazy densities in the right upper lobe (white arrow) which correspond to ground glass opacities (black arrow) on coronal image from contrast enhanced CT (right) performed the same day.
Open in a separate window
CXR (left) with patchy peripheral left mid to lower lung opacities (black arrow) corresponding to ground glass opacities (white arrow) on coronal image from contrast-enhanced the contemporaneous chest CT (right).
Often, reticular opacities accompanying regions of ground glass attenuation are more easily appreciable on standard CXR (
).
Open in a separate window
CXR (left) with reticular and hazy left lower lobe opacities (black arrow) in a patient with COVID-19. Similar findings are present on the coronal CT from the same day (right).
The hazy pulmonary opacities on CXR can sometimes be diffuse making identification challenging in some instances (
).
Open in a separate window
CXR (left) with subtle ill-defined hazy opacities in the right (black arrows) greater than left lungs in a patient with COVID-19. Findings are easier to appreciate on subsequent CT the same day (right).
As opposed to community acquired bacterial pneumonia which tends to be unilateral and involving a single lobe [5], COVID-19 and other viral pneumonias typically produce lung opacities in more than one lobe. Identifying multifocal air-space disease on CXR can be a significant clue to COVID-19 pneumonia.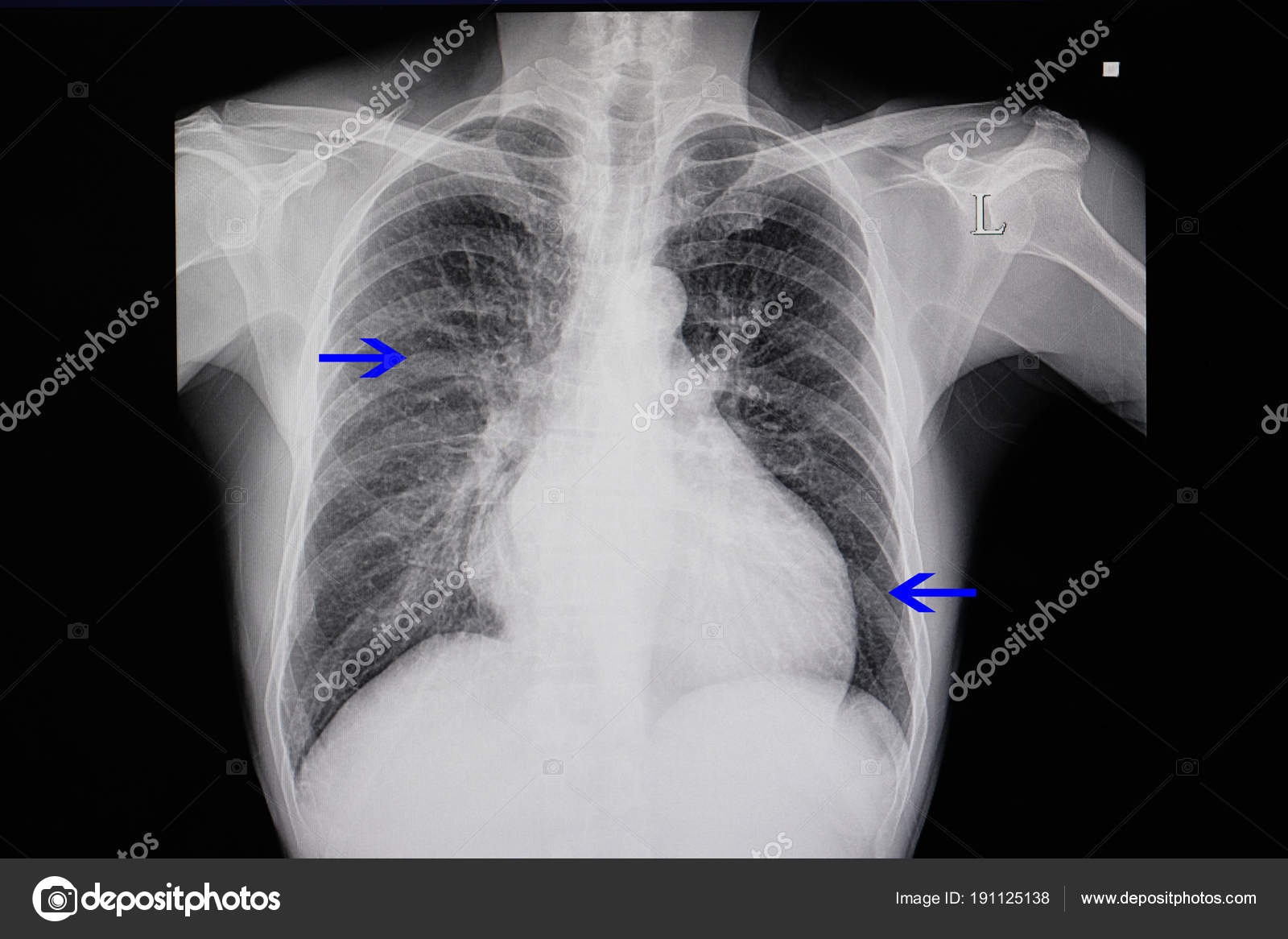 Early COVID-19 investigators have noted that the air-space disease tends to have a lower lung distribution and is most frequently bilateral [4] (
Early COVID-19 investigators have noted that the air-space disease tends to have a lower lung distribution and is most frequently bilateral [4] (
).
Open in a separate window
Six different patients with varying degrees of COVID-19 pneumonia predominantly involving the lower lung zones (black arrows) bilaterally on CXR.
One of the most unique and somewhat specific features of COVID-19 pneumonia is the high frequency of peripheral lung involvement, often mirroring other inflammatory processes such as organizing pneumonia. Chung et al. reported that 33% of COVID-19 chest CTs had peripheral lung distribution [2] and Ng et al. reported an even greater incidence of up to 86% on chest CT [6]. Such peripheral lung opacities also tend to be multifocal, either patchy or confluent, and can be readily identified on CXR (
).
Open in a separate window
Four different patients with varying degrees of COVID-19 pneumonia on CXR predominantly involving the peripheral lungs bilaterally (black arrows).
Diffuse lung opacities in patients with COVID-19 have a similar CXR pattern (
) as other widespread infectious or inflammatory processes including acute respiratory distress syndrome (ARDS).
Open in a separate window
CXR (left) and subsequent coronal image from chest CT (right) performed in a patient with COVID-19 and diffuse ground glass and consolidative opacities throughout both lungs.
When lung disease involves the majority of the pulmonary parenchyma, patients are typically hypoxic and require intubation with mechanical intubation (
).
Open in a separate window
Two different intubated patients with COVID-19 infection and diffuse lung opacities.
Lung opacities may rapidly evolve into a diffuse coalescent or consolidative pattern within 1–3 weeks of symptom onset [1,7], often peaking at around 6–12 days after initial clinical presentation (,
).
Open in a separate window
Serial radiographs over 7 days in a patient with COVID-19 infection depicting progression of diffuse lung disease that ultimately required intubation./iStock_22401848_MEDIUM-58262cb63df78c6f6adebb27.jpg)
Open in a separate window
Serial chest radiographs of a different patient with COVID-19 infection separated by 6 days depicting progression of diffuse lung disease requiring intubation.
Pleural effusions have been reported as exceedingly rare on CXR and CT in COVID-19 infected patients, and when present are most often identified late in the disease course [8].
Lung cavitation and pneumothorax are also rare findings in COVID-19 patients [8] but can occur (
).
Open in a separate window
Serial chest radiographs of a COVID-19 patient with diffuse lung opacities (left image) with interval cavitation (left image white arrows) and tension pneumothorax (right image black arrow). Successful chest tube placement was subsequently performed (not shown).
Localized large nodules have yet to be reported in the literature to this date (
).
Open in a separate window
A unique case of a rapidly enlarging right lung nodule (left image, white arrow) over the course of 5 days. Subsequent bronchoscopy with tissue sampling revealed COVID-19 infection.
Subsequent bronchoscopy with tissue sampling revealed COVID-19 infection.
Diffuse chest wall subcutaneous emphysema and pneumomediastinum after intubation in the setting of COVID-19 infection has been described in one case report [9], as of the time of this writing. This phenomenon has also been reported previously in the setting of h2N1 viral infection [10].
Since the influx of cases began at our institution, we have noticed this to occur in several patients (
). Potential mechanisms include alveolar rupture leading to interstitial emphysema from the currently recommended high positive end-expiratory pressure (PEEP) settings on COVID-19 ventilated patients according to the Macklin effect [11]. The diffuse alveolar damage in severe cases may also contribute to alveolar rupture. The exact mechanism requires additional investigation.
Open in a separate window
Two different intubated patients with COVID-19 and diffuse subcutaneous emphysema and pneumomediastinum identified on CXR. No pneumothorax was identified.
No pneumothorax was identified.
Patterns of COVID-19 lung disease can be identified on conventional chest radiography as well as chest CT. Typical verbiage when reporting patients with, or suspected COVID-19 on CXR include terms such as irregular, patchy, hazy, reticular, and widespread ground glass opacities. Grading disease severity based on total lung involvement is also important to relay to the clinicians. As the pandemic progresses, the medical community will frequently rely on portable CXR due to its widespread availability and reduced infection control issues that currently limit CT utilization.
Adam Jacobi:Conceptualization, Writing – original draft, Supervision.Michael Chung:Conceptualization, Writing – review & editing.Adam Bernheim:Writing – review & editing, Resources.Corey Eber:Writing – review & editing, Resources.
1. Zhou S., Wang Y., Zhu T., Xia L. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China.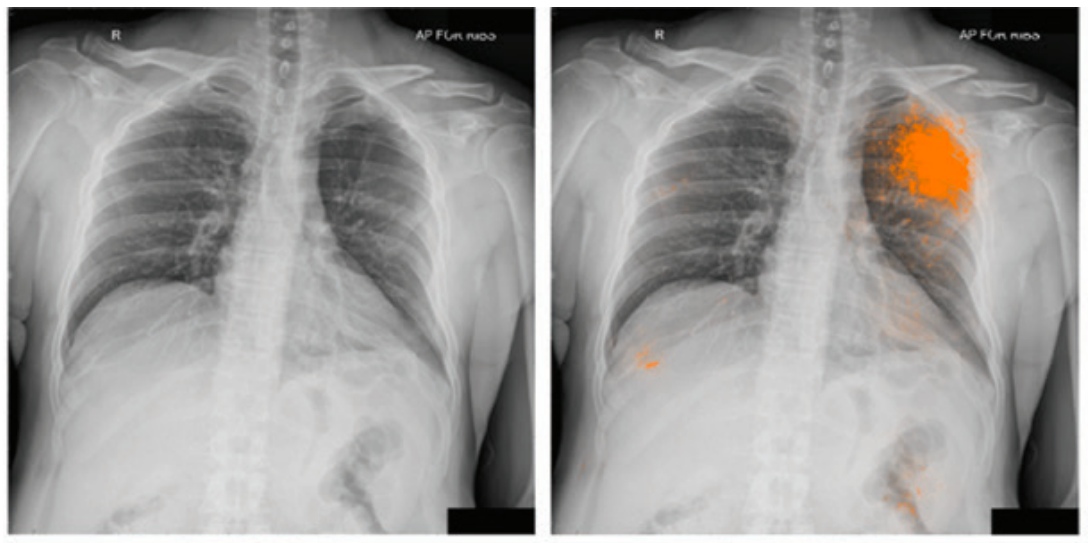 Am J Roentgenol. 2020:1–8. March. [PubMed] [Google Scholar]
Am J Roentgenol. 2020:1–8. March. [PubMed] [Google Scholar]
2. Chung M., Bernheim A., Mei X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. February 2020;200230 doi: 10.1148/radiol.2020200230. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3. ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection|American College of Radiology. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Accessed March 22, 2020. Google Scholar 2020.
4. Wong H.Y.F., Lam H.Y.S., Fong A.H. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019:201160. doi: 10.1148/radiol.2020201160. Mar 27. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Vilar J., Domingo M.L., Soto C. Radiology of bacterial pneumonia. J Eur J Radiol. 2004 Aug;51(2):102–113. [PubMed] [Google Scholar]
6. Ng M.Y., Lee E., Yang J. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2(1) [Link, Google Scholar] [Google Scholar]
Ng M.Y., Lee E., Yang J. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2(1) [Link, Google Scholar] [Google Scholar]
7. Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020:200463. Feb 20. [PMC free article] [PubMed] [Google Scholar]
8. Salehi S., Abedi A., Balakrishnan S. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020 Mar;14:1–7. doi: 10.2214/AJR.20.23034. [PubMed] [CrossRef] [Google Scholar]
9. Sun R., Liu H., Wang X. Mediastinal emphysema, Giant Bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. 2020 Mar 20 doi: 10.3348/kjr.2020.0180. [Epub ahead of print] [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Gou H.H., Sweeney R.T., Regula D. Fatal 2009 influenza a (h2N1) infection, complicated by acute respiratory distress syndrome and pulmonary interstitial emphysema.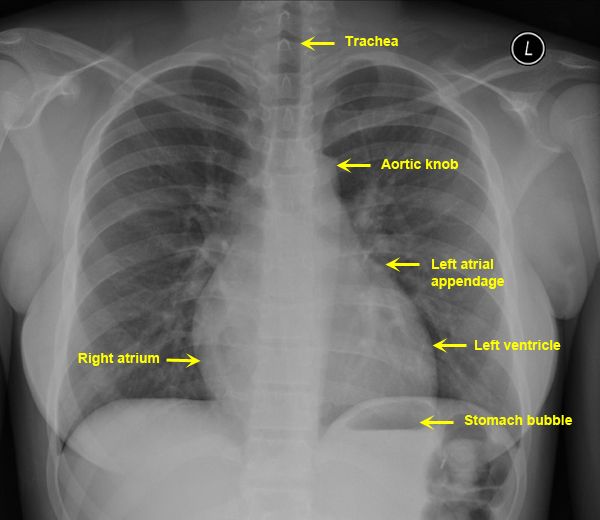 Radiographics. 2010 Mar;30(2):327–333. doi: 10.1148/rg.302095213. [PubMed] [CrossRef] [Google Scholar]
Radiographics. 2010 Mar;30(2):327–333. doi: 10.1148/rg.302095213. [PubMed] [CrossRef] [Google Scholar]
11. Poston JT, Patel BK, Davis AM. Management of critically ill Adults with COVID-19. JAMA Clinical Guideline Synopsis. https://jamanetwork.com/journals/jama/fullarticle/2763879. Accessed March 26, 2020 2020. [PubMed]
Articles from Clinical Imaging are provided here courtesy of Elsevier
Hazy on Ground-Glass Opacities? Here’s What They Are
by
Kristina Fiore, Director of Enterprise & Investigative Reporting, MedPage Today
May 29, 2020
The COVID-19 pandemic has brought radiologists’ penchant for descriptive terms front-and-center, with frequent references to one feature in particular: ground-glass opacities.
The term refers to the hazy, white-flecked pattern seen on lung CT scans, indicative of increased density. It’s not quite as dense as the “crazy-paving” pattern, which looks like a mosaic or pavers, and less confounding than the “head cheese sign,” a juxtaposition of three or more densities present in the same lung.
Essentially, a ground-glass opacity describes the “shades of grey” in between a normal lung scan and one from an extremely diseased lung that shows up nearly all white because it’s full of puss or fluid, said Henry Guo, MD, PhD, of Stanford University in Palo Alto, California.
The term has its origins in the way old movies shot their flashback scenes, through a ground-glass lens that gave the film a hazy appearance, Guo said. Chest radiologists adopted it in the 1980s, with a first appearance in the Fleischner Society Glossary of Terms for Thoracic Radiology in 1984.
“We see [ground-glass opacities] so often in chest imaging,” Guo told MedPage Today. They come in different shapes, sizes, quantities, and locations, and they can indicate many different underlying pathologies — including other viral infections, chronic lung disease, fibrosis, other inflammatory conditions, and cancers.
“Clinical context matters for interpreting these findings,” said Javad Azadi, MD, of Johns Hopkins University in Baltimore.
Ground-glass opacities aren’t likely to be found in healthy lungs, though, and wouldn’t result from exposures like air pollution or smoking, radiologists said.
“It’s safe to say that if you are a healthy person, you shouldn’t have ground-glass opacities,” said Paras Lakhani, MD, of Thomas Jefferson University in Philadelphia, speaking on behalf of the Radiological Society of North America (RSNA).
Lakhani noted that a study of more than 200,000 patients found ground-glass opacities were present in 15% — but these are patients “who have or are more likely to have cancer so this data isn’t reflective of the prevalence in the general population.”
Given how common ground-glass opacities can be in various diseases, researchers have taken a hard look at their clinical features in COVID-19.
Adam Bernheim, MD, of the Mount Sinai system in New York City, authored one of the early papers on chest CT findings in COVID-19. He and his colleagues studied images captured from 121 patients at four centers in China mostly in late January.
“There are a lot of diseases that can cause ground-glass opacities, but in COVID-19, there’s a distinct distribution, a preference for certain parts of the lung,” chiefly in the lower lobes and periphery, and it appears multifocally and bilaterally, Bernheim said.
COVID-related ground-glass opacities also have a very round shape that’s “really unusual compared with other ground-glass opacities,” he said.
“Influenza or other pneumonias don’t often have that pattern,” he said. “Patients with flu can have ground-glass opacities, but they won’t be in that distribution. It would be more in the middle parts of the lungs. And flu doesn’t have these round, circular shapes.”
Soon after their study published, New York’s coronavirus case count started to rise, and Bernheim’s team saw those features borne out in their own practice.
“Before long, we had cases here in our hospital in New York, and it turned out to be the same pattern,” he said. “It substantiated and confirmed what we were seeing in the Chinese patients. “
“
They also had many cases where COVID-19 wasn’t initially suspected but was detected incidentally. For instance, patients who had gastrointestinal issues but no respiratory symptoms were sent for abdominal CT, which catches the bottom of the lungs. “In many cases we saw ground-glass opacities” and those patients were subsequently diagnosed with COVID-19, he said.
Yet chest CT has not panned out as an official diagnostic tool for COVID-19.
Matthew Cham, MD, of the University of Washington in Seattle, said there was initial hope as one study determined that CT can show ground-glass opacities during the first few days of COVID infection, when PCR testing may be especially susceptible to false negatives.
“This initial observation led to substantial excitement around the potential usefulness of chest CTs for the early detection of COVID-19,” Cham told MedPage Today.
Subsequent studies, however, showed some COVID patients have normal chest CTs with no ground-glass opacities during the first few days of the infection, Cham said.
No radiological society has recommended diagnostic chest CT for COVID-19. Instead, RSNA, the American College of Radiology, and the Society of Thoracic Radiology issued a consensus statement to help radiologists recognize COVID-19 pneumonia and communicate their findings to others.
Chest CT is still useful in detecting additional bacterial infections that appear on top of COVID-19, and will probably play a more important role in managing patients who have residual scarring after recovering from COVID-19, Bernheim said.
“The role of chest CT in COVID-19 is evolving,” he said, “and it can be useful in providing a lot of helpful information for diagnosing and managing patients.”
Please enable JavaScript to view the comments powered by Disqus.
Chest x-ray in Moscow from 1500 rubles.
X-rays of the chest and lungs are performed in the X-ray department of the clinic. As prescribed by the doctor, x-rays can be performed in two projections. Image transcription is included in the price.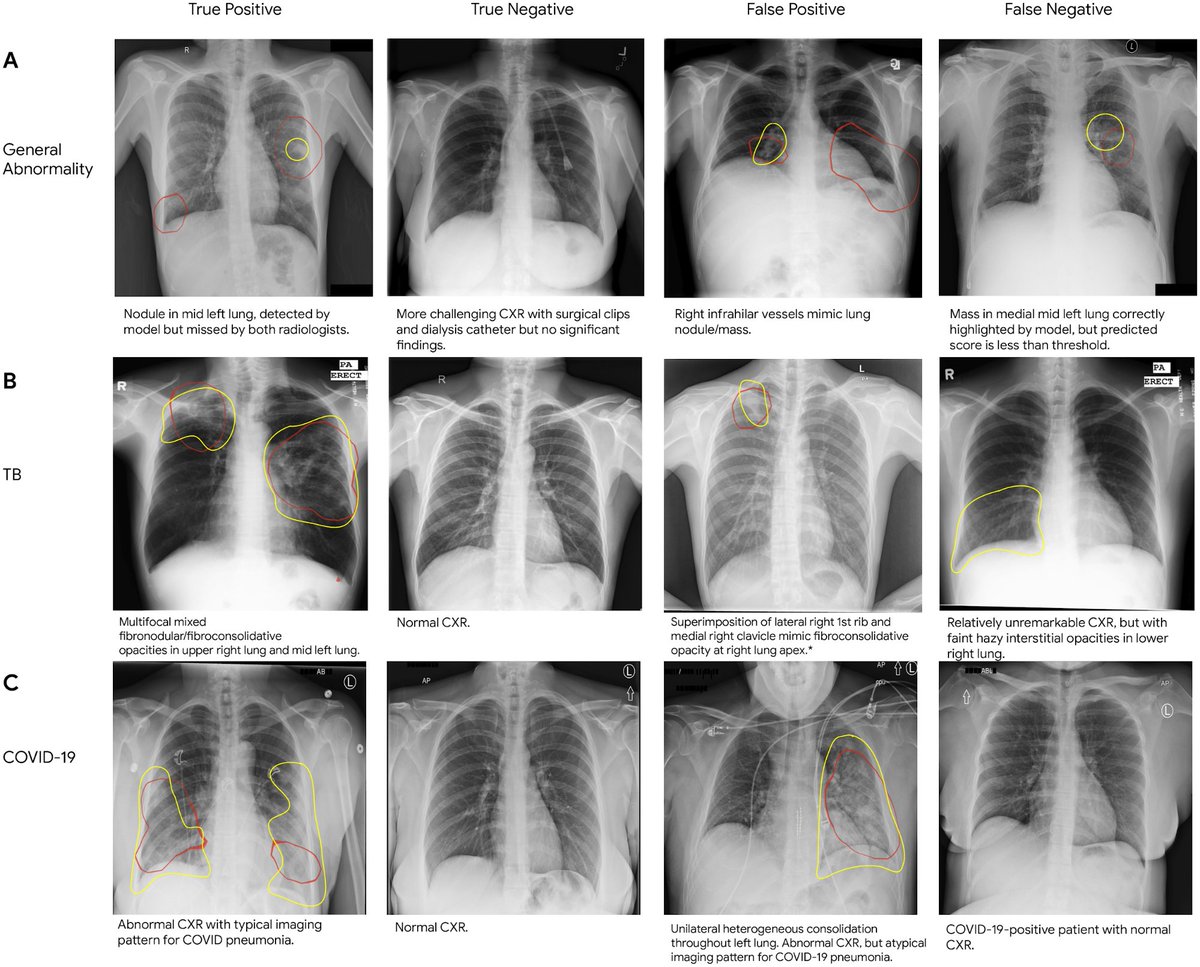
You can make an appointment and undergo an examination at a convenient time for you.
Fill out the form to enroll now
Contents:
Cost of a lung x-ray
Chest x-ray
What x-ray shows
Indications for prescribing a chest x-ray
Contraindications for x-rays
Preparing for a chest x-ray
Explanation of images
Cost of a lung x-ray
X-ray examinations
Price
900 02 Radiography (plain) of the chest 1 projection
1,500, 00
Chest x-ray in 2 projections
1,700.00
Chest x-ray
Chest x-ray is considered the simplest, most informative and affordable diagnostic method. It is used to examine patients with signs indicating pathological changes in the lungs and adjacent structures. Radiography in two projections – these are two pictures, one lateral and one direct, is prescribed if it is necessary to clarify the diagnosis and the expected benefit of the procedure exceeds the possible harm from radiation.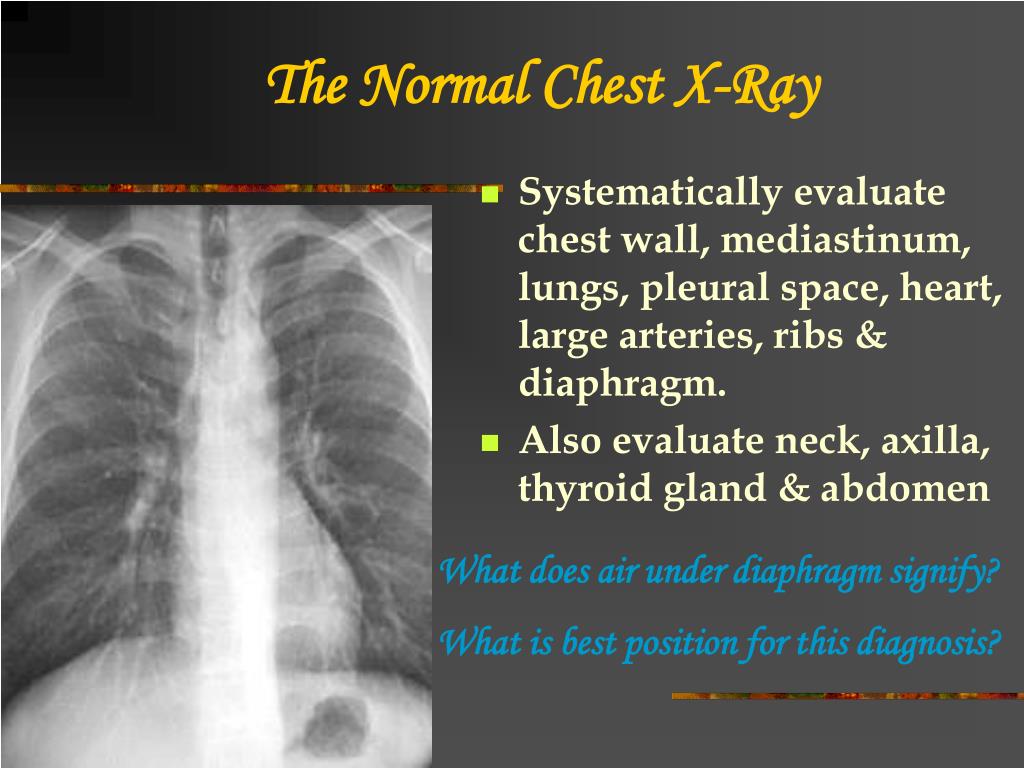
What the x-ray shows
Chest x-ray in 2 projections (lateral and anteroposterior) determines the exact localization of foci of inflammation and infiltration. On direct images, the lung segments are not clearly visible. The image on the lateral images is more accurate, the interlobar boundaries with their anatomical features are well visualized on them. At the same time, the doctor receives a lot of information about the mediastinal organs – their size, pathological foci, neoplasms. The pictures also show the heart – its position and size.
Obligatory when deciphering the radiograph, secondary signs are also evaluated:
- The volume of lung tissues;
- Soft tissue condition;
- Features of lung fields;
- Airiness of large and small bronchi;
- The position of the roots of the lungs and their structure;
- Diaphragm dome status.
All changes are evaluated in aggregate. After a plain chest x-ray, the attending physician may refer you to other diagnostic procedures to clarify or exclude the diagnosis.
Indications for prescribing a chest x-ray
Plain chest x-ray in 1 projection is the standard of investigation. It is prescribed for suspected bronchitis and acutely developing pneumonia, after injuries and to exclude tuberculosis.
X-ray in 2 projections as a diagnostic method is required if the doctor needs to know exactly the morphological changes in the lungs, the functionality of the organs, and the features of the diaphragm displacement. According to two pictures, you can find hidden foci of inflammation, dystrophic processes, tumor-like formations. The examination also shows anomalies in the structure of the broncho-pulmonary system and the heart.
Doctors prescribe radiography for:
- Acute and chronic pneumonia;
- Bronchitis;
- Pulmonary emphysema;
- Pleurisy;
- Malignant tumors in the chest;
- Pneumothorax;
- Cysts;
- Tuberculosis.
A chest x-ray is used to check the placement and position of the cardiac catheter and pacemaker leads. Diagnosis is necessary if the patient complains of severe weakness, loss of appetite, persistent cough, rapid weight loss, pain in the projection of the lungs.
Diagnosis is necessary if the patient complains of severe weakness, loss of appetite, persistent cough, rapid weight loss, pain in the projection of the lungs.
Take the first step – make an appointment
Leave your contacts and we will contact you as soon as possible.
Your name:
Phone number or e-mail:*
Select date:
Note:
* I agree with the personal data processing rules set out in the privacy policy
9 0002 Fields marked with “*” required to fill out.
X-ray contraindications
There are no absolute contraindications for chest x-rays. However, there are a number of relative contraindications, these include:
- Pregnancy;
- Multiple rib fractures;
- Severe bleeding from chest trauma;
- General serious condition of the patient.
However, relative contraindications are neglected if the X-ray is necessary for health reasons, that is, diagnostics are needed for diagnosis and treatment.
Chest x-ray preparation
Chest x-ray does not require specific preparation. The patient will only need to undress to the waist at the time of the procedure, remove metal objects from the body and listen to the orders of the health worker. During the diagnosis, the laboratory assistant may ask you to hold your breath. The picture in the lateral projection is taken from the prone position.
Explanation of images
The images taken are interpreted by the radiologist. After evaluating all organs, the doctor writes his opinion, but only the attending doctor can make a diagnosis for the patient. Based on the results, therapy is prescribed, or the patient is sent for further examination.
You can make an appointment for a chest x-ray at our clinic by phone. We take pictures on modern devices with a small dose of radiation. There are few queues in the diagnostic department of our center, since the flow of patients is distributed by registrars quickly and correctly.
Ask a doctor
Leave your contacts and we will contact you shortly and answer all your questions.
Your name:
Phone number:*
* I agree with the rules for processing personal data set out in the privacy policy
Fields marked with “*” are required.
** Not all issues can be resolved online, face-to-face consultation may be required.
Chest x-ray in St. Petersburg – the price is 1500 rubles in the center of radiation diagnostics “Affordable Medicine”
1 projection
Price:
1 500 rubles
In 2 projections
Price:
2,000 rubles
Additional projection
Price:
500 rub
Sign up
- Prices
- Description
- Addresses
- Execution time
15 minutes
Description
X-ray diagnostics is based on its ability to pass through living and non-living objects. Including through the human body. Organs of different densities absorb different amounts of radiation, as a result, in a classic negative image, the most dense formations, bones, are displayed as the lightest, and those filled with air are almost black. Soft tissues are visualized as spots of gray shades. Areas, the color and shape of which are not typical, speak of pathology.
Including through the human body. Organs of different densities absorb different amounts of radiation, as a result, in a classic negative image, the most dense formations, bones, are displayed as the lightest, and those filled with air are almost black. Soft tissues are visualized as spots of gray shades. Areas, the color and shape of which are not typical, speak of pathology.
A chest x-ray is used to obtain an image of the organs located here: the lungs and airways, the contours of the heart with vessels, as well as the spine and bones. Usually, one image is enough for the diagnosis – in a direct projection, when the rays go from back to front. Sometimes the doctor prescribes a picture in the lateral projection, that is, on the left or right. This is necessary if you want to more accurately determine the segment of the lesion or reliably exclude the pathological process. It is extremely rare that oblique projections are required, but they also happen.
X-ray acquisition is a non-invasive and painless procedure with extremely low radiation exposure, which allows you to quickly and accurately identify obvious tissue damage.
To whom a chest x-ray is prescribed
This type of diagnosis refers to the primary methods of examination of patients presenting the following complaints:
- Cough that does not go away for a long time;
- Sputum;
- Blood in sputum;
- Shortness of breath;
- Pain in chest or back: constant, aching or on motion;
- Weakness, fatigue, fever.
Physician – internist, surgeon, traumatologist, pulmonologist, cardiologist or oncologist – will refer for X-ray examination if necessary to confirm or rule out:
- Tuberculosis;
- Pneumonia and other lung disorders;
- Pleurisy;
- Parasitic diseases, eg echinococcosis;
- Occupational lung injury;
- Oncology;
- Bone injuries, including old ones.

What a chest x-ray shows
The radiograph shows the following formations located in the chest:
- Soft tissues: pectoral muscles, skin folds;
- Skeleton: ribs, clavicles, sternum, indistinctly – vertebrae, in old age – cartilage;
- Lung fields: their transparency, symmetry, pulmonary pattern are determined;
- Lung roots: topography, shape, structure, width;
- Mediastinum: the position of the heart and the vessels that form its arches;
- Diaphragm dome: clarity, location;
- Sinuses: free or filled.
Only pathological changes are described in the protocol. In pathology, the following can be detected:
- Deviations from the normal radiograph;
- Neoplasms;
- Pathological inclusions;
- Injuries, fractures;
- Foreign bodies.

Preparing and conducting procedure
Diagnosis of chest organs by X-ray does not require special training or diet and can be performed at any time.
The patient removes clothing from the upper half of the body, removes all metal objects, such as watches or jewelry, and pins up the hair. Then the radiologist helps to put on a protective cape, shows where to stand and what position to take:
- For direct or postero-anterior projection, press your chest and shoulders firmly against the plate, rest your hands on your sides or take hold of the special handrails;
- If lateral projection is additionally required, the patient stands up and leans sideways with arms raised above head.
At the doctor’s command, it is necessary to inhale and hold the breath for 2-3 seconds, until the specialist’s permission. In this case, you need to freeze and not move. Then you can get dressed. Thus, the procedure itself takes about 5 minutes, during which you will not feel anything.
Then you can get dressed. Thus, the procedure itself takes about 5 minutes, during which you will not feel anything.
Often, the doctor will need no more than an hour to describe the image, after which the conclusion, along with a CD, is handed out or sent to you or your doctor by e-mail.
Contraindications
The X-ray machine used in the Affordable Medicine clinic emits a minimum amount of radiation in one procedure – 0.02 mSv. This is a small part of the recommended maximum allowable radiation dose per year – 100 mSv. That is, the diagnostic dose is small and allows you to conduct as many studies per year as necessary.
However, there are absolute and relative contraindications: a chest examination is not recommended for pregnant women at any time, and for children under 18 years of age, it is carried out only on the recommendation of the attending physician. If necessary, perform a study, as in all other cases, be sure to use protective lead aprons and capes that cover the vital organs.
For breastfeeding mothers, we recommend feeding the baby for 1 day after the test with pre-expressed milk or powdered formula. Express and discard your milk.
Prices
Fluorography 1 100 rub 800 |
| org/Product”> |
| org/Product”> |
| org/Product”> |

