Headache diarrhea nausea chills. Headache, Diarrhea, Nausea, and Chills: Decoding Food Poisoning vs. Stomach Virus Symptoms
What are the key differences between food poisoning and stomach virus. How can you identify the cause of your gastrointestinal symptoms. What are the most effective treatments for food poisoning and stomach bugs. How can you prevent these common illnesses.
Understanding the Difference: Food Poisoning vs. Stomach Virus
Many people use the terms food poisoning, stomach bug, stomach flu, and stomach virus interchangeably. However, these conditions are distinct in their causes and characteristics. Food poisoning results from consuming contaminated or spoiled food, while a stomach virus (medically known as viral gastroenteritis) is caused by a viral infection that inflames the gastrointestinal tract.
The Centers for Disease Control and Prevention (CDC) reports that food poisoning affects approximately 48 million Americans annually, making it more prevalent than viral illnesses. Understanding the differences between these conditions can help you identify the cause of your symptoms and seek appropriate treatment.
Key Distinctions Between Food Poisoning and Stomach Virus
- Cause: Food poisoning is caused by foodborne germs, including bacteria, viruses, and parasites. Stomach viruses are caused by viruses such as norovirus and rotavirus.
- Onset: Food poisoning symptoms typically appear within 2-6 hours of consuming contaminated food. Stomach virus symptoms develop 24-48 hours after exposure.
- Transmission: Food poisoning occurs through ingestion of contaminated food or beverages. Stomach viruses spread through person-to-person contact or contaminated surfaces.
- Prevention: Food poisoning can be prevented by proper food handling and storage. Stomach viruses are prevented through good hygiene practices and vaccination (for rotavirus).
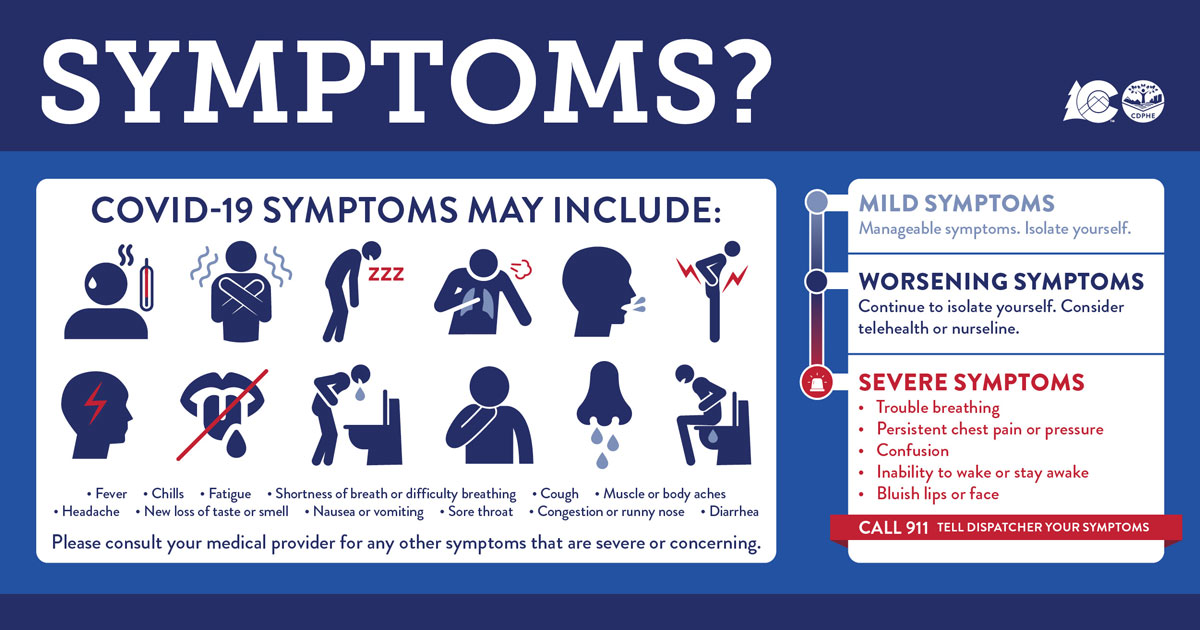
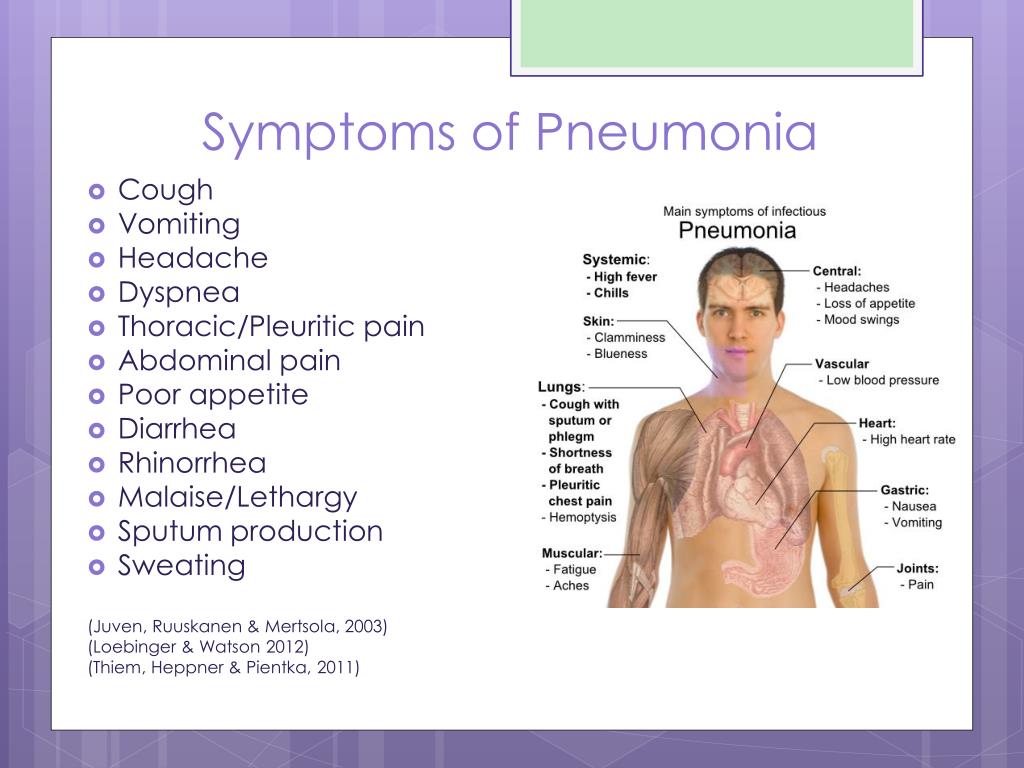
Recognizing the Symptoms: Food Poisoning vs. Stomach Virus
Both food poisoning and stomach viruses can cause similar symptoms, making it challenging to distinguish between the two. However, certain characteristics can help you identify the likely cause of your discomfort.

Common Symptoms of Food Poisoning
- Abdominal pain or cramping
- Diarrhea
- Vomiting
- Thirst
- Headache
- Low-grade fever
- Chills
- Sweating
- Fatigue
- Muscle aches
In severe cases of food poisoning, individuals may experience bloody stools, severe abdominal cramps, and even fainting or loss of consciousness.
Common Symptoms of Stomach Virus
- Nausea
- Vomiting (often projectile)
- Watery diarrhea
- Stomach cramps
- Fever
- Headache
- Body aches
- Fatigue
- Dry mouth
- Lightheadedness
- Decreased urination
Diagnosing Food Poisoning and Stomach Viruses
Determining whether you have food poisoning or a stomach virus can be challenging due to the overlap in symptoms. However, healthcare professionals use various methods to diagnose these conditions.
Diagnosing Food Poisoning
Food poisoning is typically diagnosed based on a patient’s medical history and symptoms. In some cases, a stool test may be performed to identify specific bacterial or parasitic infections. When considering a diagnosis of food poisoning, healthcare providers may ask about recently consumed foods and whether others who ate the same food are experiencing similar symptoms.
Diagnosing Stomach Viruses
Stomach viruses are usually diagnosed based on symptoms alone. While rapid stool tests can detect norovirus and rotavirus, these are not widely available in most health clinics. Doctors may also consider factors such as recent contact with infected individuals or outbreaks in the community.
Treatment Approaches for Food Poisoning and Stomach Viruses
While the treatment approaches for food poisoning and stomach viruses share some similarities, there are important differences to consider.
Treating Food Poisoning
- Fluid replacement: Drink plenty of clear fluids to prevent dehydration.
- Electrolyte balance: Consume oral rehydration solutions to restore electrolyte balance.
- Dietary changes: Eat bland, easily digestible foods (BRAT diet: bananas, rice, applesauce, toast).
- Rest: Allow your body time to recover and fight off the infection.
- Medication: In severe cases, antibiotics may be prescribed for certain types of bacterial food poisoning.
Treating Stomach Viruses
- Hydration: Replace lost fluids and electrolytes through oral rehydration solutions.
- Diet: Gradually introduce bland, easy-to-digest foods as tolerated.
- Rest: Allow your body to recover and boost immune function.
- Symptom management: Over-the-counter medications may help relieve nausea, diarrhea, and fever.
- Time: Most stomach viruses resolve on their own within a few days.
Prevention Strategies: Safeguarding Against Food Poisoning and Stomach Viruses
Preventing food poisoning and stomach viruses involves different strategies due to their distinct causes and transmission methods.

Preventing Food Poisoning
- Practice proper food handling and storage techniques
- Cook meats and eggs thoroughly
- Wash fruits and vegetables before consumption
- Refrigerate perishable foods promptly
- Avoid cross-contamination between raw and cooked foods
- Discard food that appears or smells spoiled
Preventing Stomach Viruses
- Wash hands frequently with soap and water
- Avoid close contact with infected individuals
- Disinfect contaminated surfaces
- Practice good hygiene when preparing food
- Consider vaccination against rotavirus for infants
When to Seek Medical Attention: Red Flags for Food Poisoning and Stomach Viruses
While many cases of food poisoning and stomach viruses can be managed at home, certain symptoms warrant immediate medical attention.
Warning Signs for Food Poisoning
- Frequent vomiting preventing fluid retention
- Bloody stools or severe abdominal pain
- Signs of dehydration (extreme thirst, dry mouth, little or no urination)
- Fever above 101.5째F (38.6째C)
- Neurological symptoms (blurry vision, muscle weakness, tingling in arms)
Warning Signs for Stomach Viruses
- Inability to keep liquids down for 24 hours
- Vomiting or diarrhea lasting more than 3 days
- Severe abdominal pain or bloating
- Signs of severe dehydration (confusion, rapid heartbeat, sunken eyes)
- Fever above 104째F (40째C)
Long-term Implications: Understanding the Potential Complications
While most cases of food poisoning and stomach viruses resolve without long-term effects, some individuals may experience complications or prolonged symptoms.

Potential Complications of Food Poisoning
- Chronic arthritis
- Brain and nerve damage
- Kidney failure (in severe cases of E. coli infection)
- Irritable bowel syndrome (IBS)
- Reactive arthritis
Potential Complications of Stomach Viruses
- Severe dehydration
- Malnutrition (especially in children)
- Lactose intolerance (temporary)
- Exacerbation of existing gastrointestinal conditions
Understanding these potential complications emphasizes the importance of proper treatment and prevention strategies for both food poisoning and stomach viruses.
Debunking Myths: Common Misconceptions About Food Poisoning and Stomach Viruses
There are several myths and misconceptions surrounding food poisoning and stomach viruses that can lead to confusion and improper management of these conditions.
Myth: Alcohol Kills Stomach Viruses
Contrary to popular belief, consuming alcohol does not kill stomach viruses or cure food poisoning. In fact, alcohol can irritate the stomach lining and worsen symptoms.

Myth: You Can Always Tell If Food Is Contaminated
While spoiled food often has an unpleasant odor or appearance, many foodborne pathogens do not alter the taste, smell, or appearance of food. Always follow proper food safety guidelines, regardless of how food looks or smells.
Myth: Stomach Flu Is Related to Influenza
The term “stomach flu” is a misnomer. Viral gastroenteritis is not caused by the influenza virus and is unrelated to the respiratory illness we commonly call the flu.
Myth: Antibiotics Are Always Necessary for Food Poisoning
Most cases of food poisoning do not require antibiotics and resolve on their own. Antibiotics are only prescribed in specific cases of bacterial food poisoning and can be harmful if used unnecessarily.
By understanding these myths and the true nature of food poisoning and stomach viruses, individuals can make informed decisions about their health and seek appropriate care when needed.
Food Poisoning or Stomach Virus? The Telltale Symptoms to Look For
The terms food poisoning, stomach bug, stomach flu, and stomach virus are often used interchangeably, but they’re not the same. A stomach bug or stomach flu is a sickness caused by a virus (the medical term for this condition is viral gastroenteritis). The virus causes an inflammation of the gastrointestinal tract (stomach and intestines). On the other hand, food poisoning occurs after eating contaminated food or spoiled food, caused by foodborne germs. According to the Centers for Disease Control and Prevention (CDC), food poisoning affects some 48 million Americans each year, and it is more common than viral illnesses.
Please continue reading to learn more about the telltale signs that can help you determine whether you’re dealing with a viral infection or food poisoning.
You should suspect food poisoning if the food looks, tastes, or smells bad. Germs that cause food spoilage often cause food to become slimy or mushy in appearance, develop unpleasant odors, and taste sour or “off. ”
”
How do you tell if you have a stomach bug or something else?
Food poisoning and viral gastroenteritis cause many of the same symptoms. Common food poisoning symptoms such as nausea, vomiting, stomach pain, and diarrhea are also symptoms of stomach flu. So, the truth is that you may never know if you have a stomach virus or food poisoning. However, some clues can help you figure it out (more about this later).
What are the obvious symptoms of having food poisoning?
The most common food poisoning symptoms include abdominal pain or cramping, diarrhea, and vomiting. Other symptoms of food poisoning can include thirst, headache, low-grade fever, chills, sweating, tiredness, and muscle aches. People with severe symptoms may notice bloody stools or vomit, severe abdominal cramps, and even fainting or loss of consciousness.
What are the symptoms of a stomach bug?
Viral gastroenteritis or stomach bug symptoms are similar symptoms to food poisoning.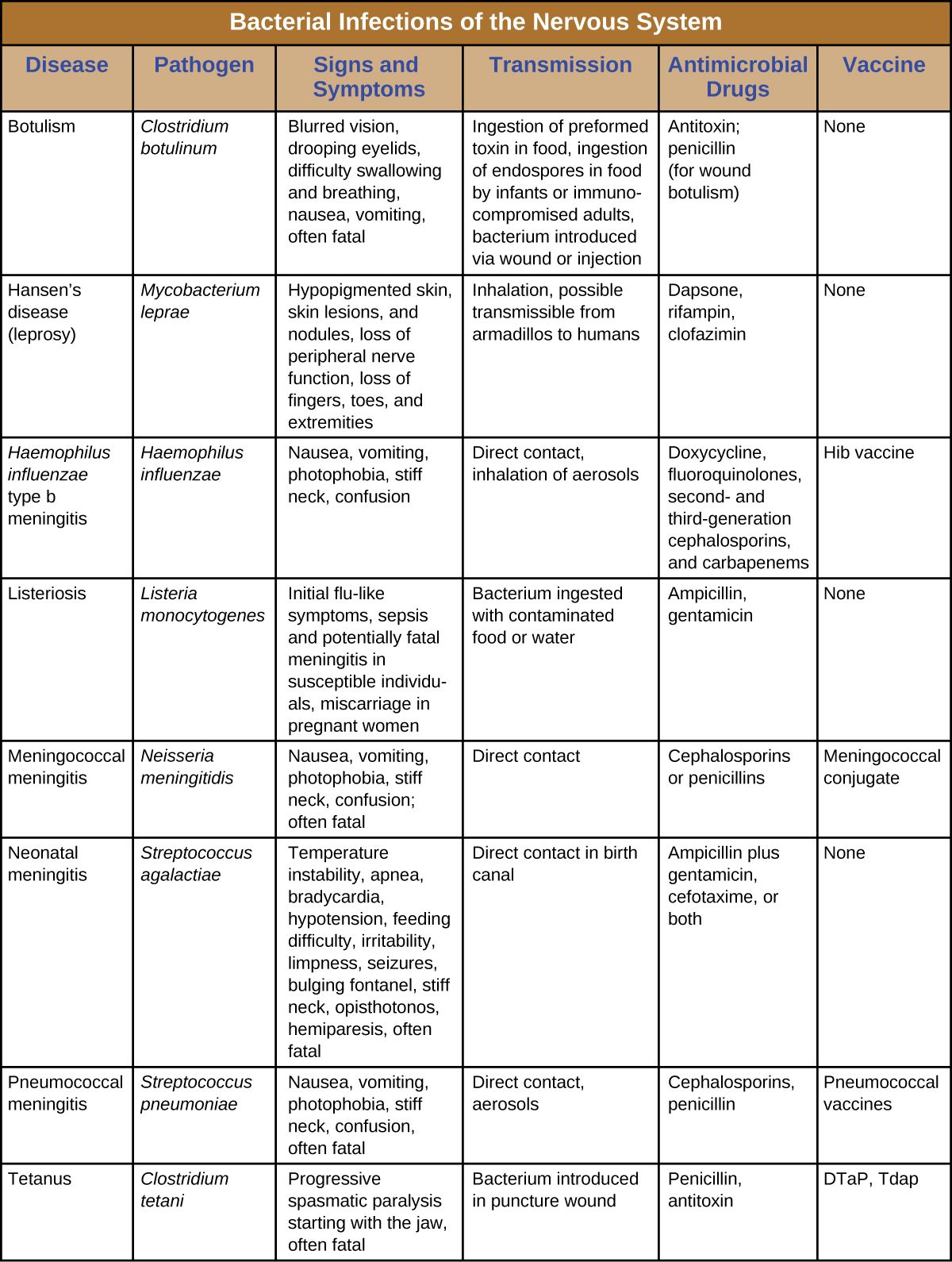 The symptoms typically include nausea, vomiting, watery diarrhea, and stomach cramps. You can also develop symptoms such as thirst, dry mouth, lightheadedness, tiredness, fever, muscle aches, joint pain, and urinating less than usual.
The symptoms typically include nausea, vomiting, watery diarrhea, and stomach cramps. You can also develop symptoms such as thirst, dry mouth, lightheadedness, tiredness, fever, muscle aches, joint pain, and urinating less than usual.
What is the difference between food poisoning and stomach bug?
Here are some of the critical differences between stomach flu and food poisoning.
Cause
- Viral gastroenteritis is caused by viruses such as norovirus, rotavirus, and other viruses.
- Food poisoning is caused by foodborne germs, including viruses, bacteria, and parasites. Some of the most common germs that cause foodborne illnesses in the U.S. are norovirus, salmonella, and Staphylococcus aureus (Staph).
Onset
- Symptoms of stomach flu develop 24-48 hours after exposure to the virus.
- Symptoms of food poisoning develop within a few hours (2-6 hours after eating contaminated food).

Diagnosis
- Doctors usually diagnose a stomach virus based on your symptoms. There is a rapid stool test that can detect norovirus and rotavirus, but it is not available at most health clinics.
- Food poisoning is diagnosed based on your history and symptoms. A stool test can help to identify bacterial or parasitic infections.
Treatment
- You can treat a stomach bug at home by replacing fluids and electrolytes to prevent dehydration and eating bland foods that are easy to digest (a BRAT diet is recommended – bananas, applesauce, rice, and toast). Some over-the-counter medicines can help to relieve your symptoms.
- Treatment for food poisoning also consists of replacing fluids and electrolytes to stay hydrated and eating easy-to-digest foods. In severe cases, doctors may prescribe antibiotics for certain types of food poisoning.
Transmission
- Viral gastroenteritis is highly contagious, and it spreads via the vomit or feces of an infected person through personal contact.
 For example, if someone is sick and has not washed their hands thoroughly, they might have the virus on their hands and can transmit it to you when you shake hands. It can also spread through contaminated food and drink or contaminated objects.
For example, if someone is sick and has not washed their hands thoroughly, they might have the virus on their hands and can transmit it to you when you shake hands. It can also spread through contaminated food and drink or contaminated objects.
- Food poisoning occurs when you eat contaminated food or drink contaminated water or beverages.
Prevention
- You can prevent viral gastroenteritis by washing your hands thoroughly if you’re sick or have been around someone who is sick. There is a vaccine available against rotavirus.
- You can prevent food poisoning by keeping your food preparation equipment and surfaces clean, refrigerating perishable foods, eating fully cooked meats and eggs, and discarding foods that appear to be spoiled.
How do I know if it’s stomach flu or food poisoning?
Both conditions cause gastrointestinal distress. However, if you have a fever, headache, body aches, and projectile vomiting, you may have a stomach bug or viral gastroenteritis. If you have bloody diarrhea, it could be food poisoning.
If you have bloody diarrhea, it could be food poisoning.
The circumstances surrounding your illness can offer clues. If you develop symptoms within a few hours of eating food that may have been spoiled or contaminated, you likely have food poisoning.
If a family member or friend ate the same food and became sick, that’s another clue that points to food poisoning.
If you have eaten foods that are easily contaminated or spoiled, such as salad greens, undercooked eggs or meat, seafood, raw milk, or dairy products just before your symptoms worsen, it could be food poisoning.
On the other hand, if you have been around someone who has a similar illness, it could be viral gastroenteritis. For example, if your child is sick and there’s a stomach bug going around your child’s school.
When to see a doctor?
Most people with a food-borne illness get better on their own in 2-5 days without medical treatment. You should see a doctor if:
- You have a high fever above 104F (40C).

- You’re not able to keep liquids down for more than 24 hours.
- You’ve been vomiting for more than 2 days.
- You have blood in your vomit or bowel movements.
- You have severe abdominal cramping or abdominal pain.
- Your symptoms have been going on for more than 7-10 days.
- You have signs of dehydration such as dry mouth, excessive thirst, dark yellow urine, less frequent urination, lightheadedness or dizziness, and severe weakness.
Keep in mind that while most forms of food poisoning aren’t serious, a type of food poisoning called botulism, which is caused by a bacterium called Clostridium botulinum, can be fatal. This bacterium produces toxins that affect the nervous system. Seek medical attention immediately if you have botulism symptoms such as blurred vision, double vision, drooping eyelids, slurred speech, or other neuromuscular symptoms.
References
- https://www.ucihealth.org/blog/2016/01/stomach-flu-or-food-poisoning
- https://ask.
 usda.gov/s/article/What-are-the-signs-of-food-spoilage#
usda.gov/s/article/What-are-the-signs-of-food-spoilage# - https://www.cdc.gov/foodsafety/foodborne-germs.html
- https://www.niddk.nih.gov/health-information/digestive-diseases/viral-gastroenteritis/symptoms-causes
Viral gastroenteritis (stomach flu) – Symptoms & causes
Overview
Viral gastroenteritis is an intestinal infection that includes signs and symptoms such as watery diarrhea, stomach cramps, nausea or vomiting, and sometimes fever.
The most common way to develop viral gastroenteritis — often called stomach flu — is through contact with an infected person or by consuming contaminated food or water. If you’re otherwise healthy, you’ll likely recover without complications. But for infants, older adults and people with compromised immune systems, viral gastroenteritis can be deadly.
There’s no effective treatment for viral gastroenteritis, so prevention is key. Avoid food and water that may be contaminated and wash your hands thoroughly and often.
Products & Services
Symptoms
Although it’s commonly called stomach flu, gastroenteritis isn’t the same as influenza. The flu (influenza) affects only your respiratory system — your nose, throat and lungs. Gastroenteritis, on the other hand, attacks your intestines, causing signs and symptoms such as:
- Watery, usually nonbloody diarrhea — bloody diarrhea usually means you have a different, more severe infection
- Nausea, vomiting or both
- Stomach cramps and pain
- Occasional muscle aches or headache
- Low-grade fever
Depending on the cause, viral gastroenteritis symptoms may appear within 1-3 days after you’re infected and can range from mild to severe. Symptoms usually last just a day or two, but occasionally they may last up to 14 days.
Because the symptoms are similar, it’s easy to confuse viral diarrhea with diarrhea caused by bacteria, such as Clostridioides difficile, salmonella and Escherichia coli, or parasites, such as giardia.
Viral gastroenteritis
The stomach, small intestine and large intestine (colon) are part of your digestive tract, which processes the foods you eat. Viral gastroenteritis is an inflammation of these organs caused by a virus.
When to see a doctor
If you’re an adult, call your health care provider if:
- You’re not able to keep liquids down for 24 hours
- You’ve been vomiting or having diarrhea for more than two days
- You’re vomiting blood
- You’re dehydrated — signs of dehydration include excessive thirst, dry mouth, deep yellow urine or little or no urine, and severe weakness, dizziness or lightheadedness
- You notice blood in your bowel movements
- You have severe stomach pain
- You have a fever above 104 F (40 C)
For infants and children
See your child’s health care provider right away if your child:
- Has a fever of 102 F (38.
 9 C) or higher
9 C) or higher - Seems tired or very irritable
- Is in a lot of discomfort or pain
- Has bloody diarrhea
- Seems dehydrated — watch for signs of dehydration in sick infants and children by comparing how much they drink and urinate with how much is normal for them, and watching for signs such as a dry mouth, thirst and crying without tears
If you have an infant, remember that while spitting up may be an everyday occurrence for your baby, vomiting is not. Babies vomit for a variety of reasons, many of which may require medical attention.
Call your baby’s doctor right away if your baby:
- Has vomiting that is frequent
- Hasn’t had a wet diaper in six hours
- Has bloody stools or severe diarrhea
- Has a sunken soft spot (fontanel) on the top of his or her head
- Has a dry mouth or cries without tears
- Is unusually sleepy, drowsy or unresponsive
Causes
You’re most likely to get viral gastroenteritis when you eat or drink contaminated food or water. You may also be likely to get gastroenteritis if you share utensils, towels or food with someone who has one of the viruses that cause the condition.
You may also be likely to get gastroenteritis if you share utensils, towels or food with someone who has one of the viruses that cause the condition.
Many viruses can cause gastroenteritis, including:
Noroviruses. Both children and adults are affected by noroviruses, the most common cause of foodborne illness worldwide. Norovirus infection can sweep through families and communities. It’s especially likely to spread among people in confined spaces.
In most cases, you pick up the virus from contaminated food or water. But it can also spread between people who are in close contact or who share food. You can also get the virus by touching a surface that’s been contaminated with norovirus and then touching your mouth.
Rotavirus. Worldwide, this is the most common cause of viral gastroenteritis in children, who are usually infected when they put their fingers or other objects contaminated with the virus into their mouths. It can also spread through contaminated food.
 The infection is most severe in infants and young children.
The infection is most severe in infants and young children.Adults infected with rotavirus may not have symptoms, but can still spread the illness. This is of particular concern in institutional settings such as nursing homes because adults with the virus unknowingly can pass the virus to others. A vaccine against viral gastroenteritis is available in some countries, including the United States, and appears to be effective in preventing the infection.
Some shellfish, especially raw or undercooked oysters, also can make you sick. Contaminated drinking water is a cause of viral diarrhea. But in many cases the virus is passed when someone with a virus handles food you eat without washing his or her hands after using the toilet.
Risk factors
Gastroenteritis occurs all over the world and can affect people of all ages.
People who may be more susceptible to gastroenteritis include:
- Young children. Children in child care centers or elementary schools may be especially vulnerable because it takes time for a child’s immune system to mature.

- Older adults. Adult immune systems tend to become less efficient later in life. Older adults in nursing homes are vulnerable because their immune systems weaken. They also live in close contact with others who may pass along germs.
- Schoolchildren or dormitory residents. Anywhere that groups of people come together in close quarters can be an environment for an intestinal infection to get passed.
- Anyone with a weakened immune system. If your resistance to infection is low — for instance, if your immune system is compromised by HIV/AIDS, chemotherapy or another medical condition — you may be especially at risk.
Each gastrointestinal virus has a season when it’s most active. If you live in the Northern Hemisphere, for instance, you’re more likely to have rotavirus or norovirus infections in the winter and spring.
Complications
The main complication of viral gastroenteritis is dehydration — a severe loss of water and essential salts and minerals. If you’re healthy and drink enough to replace fluids you lose from vomiting and diarrhea, dehydration shouldn’t be a problem.
If you’re healthy and drink enough to replace fluids you lose from vomiting and diarrhea, dehydration shouldn’t be a problem.
Infants, older adults and people with weakened immune systems may become severely dehydrated when they lose more fluids than they can replace. Hospitalization might be needed so that lost fluids can be replaced through an IV in their arms. Dehydration can rarely lead to death.
Prevention
The best way to prevent the spread of intestinal infections is to follow these precautions:
- Get your child vaccinated. A vaccine against gastroenteritis caused by the rotavirus is available in some countries, including the United States. Given to children in the first year of life, the vaccine appears to be effective in preventing severe symptoms of this illness.
Wash your hands thoroughly. And make sure your children do, too. If your children are older, teach them to wash their hands, especially after using the toilet.

Wash your hands after changing diapers and before preparing or eating food, too. It’s best to use warm water and soap and to rub hands well for at least 20 seconds. Wash around cuticles, beneath fingernails and in the creases of the hands. Then rinse thoroughly. Carry sanitizing wipes and hand sanitizer for times when soap and water aren’t available.
- Use separate personal items around your home. Avoid sharing eating utensils, drinking glasses and plates. Use separate towels in the bathroom.
- Prepare food safely. Wash all your fruits and vegetables before eating them. Clean kitchen surfaces before preparing food on them. Avoid preparing food if you’re sick.
- Keep your distance. Avoid close contact with anyone who has the virus, if possible.
- Disinfect hard surfaces. If someone in your home has viral gastroenteritis, disinfect hard surfaces, such as counters, faucets and doorknobs, with a mixture of 5-25 tablespoons (73 to 369 milliliters) of household bleach to 1 gallon (3.
 8 liters) of water.
8 liters) of water. - Avoid touching laundry that may have been exposed to a virus. If someone in your home has viral gastroenteritis, wear gloves while touching laundry. Wash clothing and bedding in hot water and dry them on the hottest setting. Wash your hands well after touching laundry.
- Check out your child care center. Make sure the center has separate rooms for changing diapers and preparing or serving food. The room with the diaper-changing table should have a sink as well as a sanitary way to dispose of diapers.
Take precautions when traveling
When you’re traveling in other countries, you can become sick from contaminated food or water. You may be able to reduce your risk by following these tips:
- Drink only well-sealed bottled or carbonated water.
- Avoid ice cubes because they may be made from contaminated water.
- Use bottled water to brush your teeth.
- Avoid raw food — including peeled fruits, raw vegetables and salads — that has been touched by human hands.

- Avoid undercooked meat and fish.
More Information
symptoms and treatment (reminder for parents)
Enteroviral infections – is a group of diseases caused by several types of viruses. The disease is caused by Coxsackieviruses, polioviruses and ECHO (ECHO).
After an enterovirus infection, persistent lifelong immunity is formed, however, it is serospecific. This means that immunity is formed only to the serological type of virus that the child has had and does not protect him from other varieties of these viruses. Therefore, a child can get sick with an enterovirus infection several times in his life. Also, this feature does not allow the development of a vaccine to protect our children from this disease. The disease has a seasonality: outbreaks of the disease are most often observed in the summer-autumn period.
Causes of infection with enterovirus infection.
Infection occurs in several ways. Viruses can enter the environment from a sick child or from a child who is a carrier of the virus. Virus carriers do not have any manifestations of the disease, but the viruses are in the intestines and are excreted into the environment with feces. This condition can be observed in children who have been ill after a clinical recovery, or in children in whom the virus has entered the body, but could not cause the disease due to the strong immunity of the child. The virus carrier can persist for 5 months.
Once in the environment, viruses can persist for quite a long time, as they tolerate adverse effects well. Viruses are well preserved in water and soil, when frozen, they can survive for several years, are resistant to disinfectants (when exposed to solutions of high concentrations of phenol, chlorine, formalin, viruses begin to die only after three hours), but are susceptible to high temperatures (when heated to 45ºС, they die in 45-60 seconds).
How enterovirus infection is transmitted.
The transmission mechanism can be airborne (when sneezing and coughing with droplets of saliva from a sick child to a healthy one) and fecal-oral if personal hygiene is not observed. Most often, infection occurs through water, when drinking raw (not boiled) water. It is also possible to infect children through toys if children take them in their mouths. Most often, children aged 3 to 10 years are ill. In children who are breastfed, there is immunity in the body received from the mother through breast milk, however, this immunity is not stable and quickly disappears after the cessation of breastfeeding.
Symptoms of enterovirus infection.
Viruses enter the body through the mouth or upper respiratory tract. Once in the child’s body, the viruses migrate to the lymph nodes, where they settle and begin to multiply. The further development of the disease is associated with many factors, such as virulence (the ability of the virus to resist the protective properties of the body), tropism (the tendency to infect individual tissues and organs) of the virus, and the state of the child’s immunity.
Enteroviral infections have both similar manifestations and different ones, depending on the species and serotype. The incubation period (the period from the virus entering the child’s body until the first clinical signs appear) is the same for all enterovirus infections – from 1 to 10 days (usually 2-5 days).
The disease begins acutely – with an increase in body temperature to 38-39º C. The temperature most often lasts 3-5 days, after which it drops to normal numbers. Very often, the temperature has a wave-like course: the temperature stays for 2-3 days, after which it decreases and stays at normal levels for 2-3 days, then rises again for 1-2 days and finally returns to normal. When the temperature rises, the child feels weakness, drowsiness, headache, nausea, and vomiting may occur. With a decrease in body temperature, all these symptoms disappear, but with a repeated increase, they may return. The cervical and submandibular lymph nodes also increase, as viruses multiply in them.
Depending on which organs are most affected, there are several forms of enterovirus infection. Enteroviruses can affect: the central and peripheral nervous systems, oropharyngeal mucosa, eye mucosa, skin, muscles, heart, intestinal mucosa, liver, testicles may be affected in boys.
When the mucous membrane of the oropharynx is affected, enterovirus angina develops. It is manifested by an increase in body temperature, general intoxication (weakness, headache, drowsiness) and the presence of a vesicular rash in the form of fluid-filled vesicles on the mucous membrane of the oropharynx and tonsils. These bubbles burst, in their place ulcers are formed, filled with white bloom. After recovery, no traces remain at the site of the sores.
When the eyes are affected, conjunctivitis develops. It can be one- or two-sided. It manifests itself in the form of photophobia, lacrimation, redness and swelling of the eyes. There may be hemorrhages in the conjunctiva of the eye.
With muscle damage, myositis develops – muscle pain. Pain appears on the background of an increase in temperature. Soreness is observed in the chest, arms and legs. The appearance of pain in the muscles, as well as temperature, can be undulating. When the body temperature decreases, the pain decreases or disappears completely.
With damage to the intestinal mucosa (enteritis), there is a liquid stool. Stools of normal color (yellow or brown), liquid, without pathological (mucus, blood) impurities. The appearance of loose stools can be both against the background of an increase in temperature, and isolated (without an increase in body temperature).
Enteroviral infections can affect various parts of the heart. So, if the muscle layer is damaged, myocarditis develops, if the inner layer is damaged with capture of the heart valves, endocarditis develops, if the outer shell of the heart is damaged, pericarditis develops. The child may experience: increased fatigue, weakness, palpitations, drop in blood pressure, rhythm disturbances (blockade, extrasystoles), pain behind the sternum.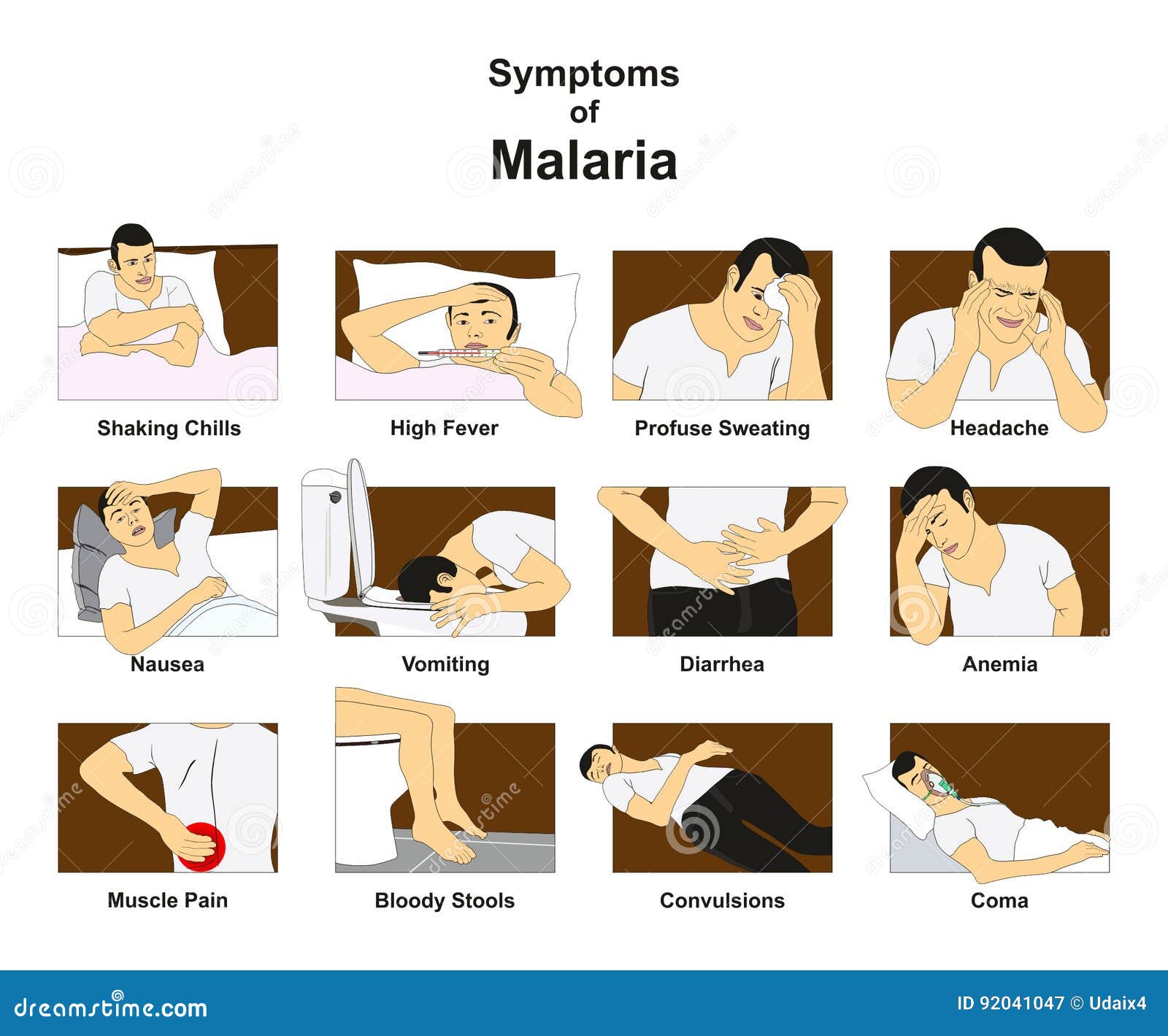
With damage to the nervous system, encephalitis, meningitis can develop. The child has: severe headache, nausea, vomiting, fever, convulsions, paresis and paralysis, loss of consciousness.
With liver damage, acute hepatitis develops. It is characterized by an increase in the liver, a feeling of heaviness in the right hypochondrium, pain in this place. Perhaps the appearance of nausea, heartburn, weakness, fever.
When the skin is damaged, exanthema may appear – hyperemia (red coloration) of the skin, most often on the upper half of the body (head, chest, arms), does not rise above the level of the skin, appears simultaneously.
Boys may have inflammation in the testicles with the development of morchitis. Most often, this condition develops 2-3 weeks after the onset of the disease with other manifestations (tonsillitis, loose stools, and others). The disease passes quite quickly and does not bear any consequences, however, in rare cases, the development of aspermia (lack of sperm) in adulthood is possible.
There are also congenital forms of enterovirus infection, when viruses enter the child’s body through the placenta from the mother. Usually, this condition has a benign course and is cured on its own, however, in some cases, an enterovirus infection can cause an abortion (miscarriage) and the development of a sudden death syndrome in a child (the death of a child occurs against the background of complete health).
Very rarely, damage to the kidneys, pancreas, lungs is possible. The defeat of various organs and systems can be observed both isolated and combined.
Treatment of enterovirus infection
There is no specific treatment for enterovirus infection. Treatment is carried out at home, hospitalization is indicated in the presence of damage to the nervous system, heart, high temperature, which cannot be reduced for a long time when using antipyretics. The child is shown bed rest for the entire period of fever.
Meals should be light, rich in proteins. A sufficient amount of liquid is needed: boiled water, mineral water without gases, compotes, juices, fruit drinks.
A sufficient amount of liquid is needed: boiled water, mineral water without gases, compotes, juices, fruit drinks.
Treatment is carried out symptomatically, depending on the manifestations of the infection – tonsillitis, conjunctivitis, myositis, loose stools, heart damage, encephalitis, meningitis, hepatitis, exanthema, orchitis. In some cases (tonsillitis, diarrhea, conjunctivitis …) bacterial complications are prevented.
Children are isolated for the entire period of the disease. In the children’s team may be after the disappearance of all symptoms of the disease.
Prevention of enterovirus infection.
For prevention, it is necessary to observe the rules of personal hygiene: wash hands after going to the toilet, walking on the street, drinking only boiled water or water from a factory bottle, it is unacceptable to use water from an open source (river, lake) to drink a child.
There is no specific vaccine against enterovirus infection, since a large number of serotypes of these viruses are present in the environment.
Severe dizziness: causes and treatment
- 8 (812) 318-53-53
- Make an appointment
In the standard vertigo syndrome, the condition is characterized by a sensation of moving the body in space, imaginary rotation, lack of soil under the feet, “helicopters”, etc. For the treatment of dizziness of the head when standing up (at normal pressure), the causes of this condition are of paramount importance, since this condition in itself is not a disease, but a symptom indicating the presence of one or both disease. At the moment, about 80 pathologies are known, the signs of which may be dizziness, weakness, headache, nausea and vomiting, and the causes of these conditions are very diverse and require immediate treatment.
The most common causes of persistent dizziness, tinnitus, weakness in the legs and other symptoms:
- Abnormalities of the inner ear;
- Basilar migraine;
- Meniere’s disease;
- Psychogenic dizziness – in the treatment of psychogenic vestibular dizziness with nausea, vomiting, weakness and pain in the eyes, the help of not only a general practitioner, but also a psychologist or even a psychotherapist is required;
- Vestibular neuritis;
- Widespread benign paroxysmal positional vertigo with weakness, drowsiness, apathy;
- Tumor of the brain;
- Multiple sclerosis;
- A cerebrovascular accident characterized by vasoconstriction, drowsiness, dizzy spells, numbness and other symptoms;
- Pathologies of the cervical spine, vertebrobasilar insufficiency;
- History of head or spinal injury;
- Anemia;
- Low blood pressure;
- Diabetes mellitus.

- PMS – in some cases, assistance to a woman with dizziness, abdominal pain and low temperature before menstruation should be provided at a professional medical level; menopause can also cause dizziness in women, and only a specialist can tell how to get rid of it;
- Noise, ringing and pain in the ears, nausea, diarrhea and dizziness may be symptoms of a number of infectious diseases;
- Severe stress leads to darkening of the eyes and prolonged dizziness, causing a lot of inconvenience.
Many patients want to understand why dizziness, pressure when walking, sweating and fatigue in men accompany them for many years. Others are troubled by severe dizziness and nausea with normal pressure in a lying or sitting position. Mild benign positional vertigo may also occur in adolescents and young adults. In all these cases, careful diagnosis is required.
Trembling in the extremities, severe weakness, unsteadiness, neck pain with dizziness and chills may indicate an injury, subclavian artery stenosis or circulatory disorders in the brain (hypoxia, neurocirculatory dystonia, encephalopathy). One of the causes of dizziness in the back of the head in the morning can be Meniere’s disease. The main disease sometimes turns out to be a brain tumor, perlymphatic fistula, BPPV and a number of other diseases.
One of the causes of dizziness in the back of the head in the morning can be Meniere’s disease. The main disease sometimes turns out to be a brain tumor, perlymphatic fistula, BPPV and a number of other diseases.
Vertigo attacks in cervical osteochondrosis
The spine and its diseases have the most direct influence on chronic dizziness. Degenerative disorders of the cervical spine are accompanied by impaired functioning of internal receptors and impaired blood circulation in the vertebral arteries, which leads to nausea, fainting, dizziness when turning the head, and other not very pleasant phenomena. When diagnosed with cervical osteochondrosis, dizziness may be accompanied by various symptoms. With osteochondrosis, the treatment of vomiting after eating, weakness and dizziness is impossible without referring to the main source of trouble. Effective treatment of persistent dizziness in cervical osteochondrosis involves the use of a complex of medical techniques and a number of procedures.
Treatment of persistent headaches and fainting
When answering the question of what to do with severe dizziness and nausea, especially if you feel sick when bending over, you need to understand that this is not a momentary phenomenon, but a symptom. Dizziness does not appear and does not disappear on its own – this is evidence of a disease, sometimes very serious and life-threatening. Self-treatment and neglect of these disorders entails serious consequences for human health and life. Treatment with drugs and tablets for severe dizziness should be prescribed only by a specialist.
For the diagnosis and treatment of the causes of severe dizziness, headaches and sudden weakness, it is necessary to undergo an examination by a neurologist, otolaryngologist, ophthalmologist, endocrinologist. In addition, a number of other laboratory and instrumental studies should be completed.
- general blood test;
- blood glucose test;
- electrocardiogram;
- audiographic study;
- tomography – computer or magnetic resonance;
- duplex scanning (otherwise ultrasonic dopplerography) of head vessels;
- radiography.



 For example, if someone is sick and has not washed their hands thoroughly, they might have the virus on their hands and can transmit it to you when you shake hands. It can also spread through contaminated food and drink or contaminated objects.
For example, if someone is sick and has not washed their hands thoroughly, they might have the virus on their hands and can transmit it to you when you shake hands. It can also spread through contaminated food and drink or contaminated objects.
 usda.gov/s/article/What-are-the-signs-of-food-spoilage#
usda.gov/s/article/What-are-the-signs-of-food-spoilage# 9 C) or higher
9 C) or higher The infection is most severe in infants and young children.
The infection is most severe in infants and young children.

 8 liters) of water.
8 liters) of water.

