Hernia remedy. Hernia: Causes, Treatments, and Diagnosis – A Comprehensive Guide
What are the common types of hernias. How are hernias diagnosed and treated. What are the risk factors for developing a hernia. When should you seek immediate medical attention for a hernia. What are the surgical options for hernia repair.
Understanding Hernias: Definition and Types
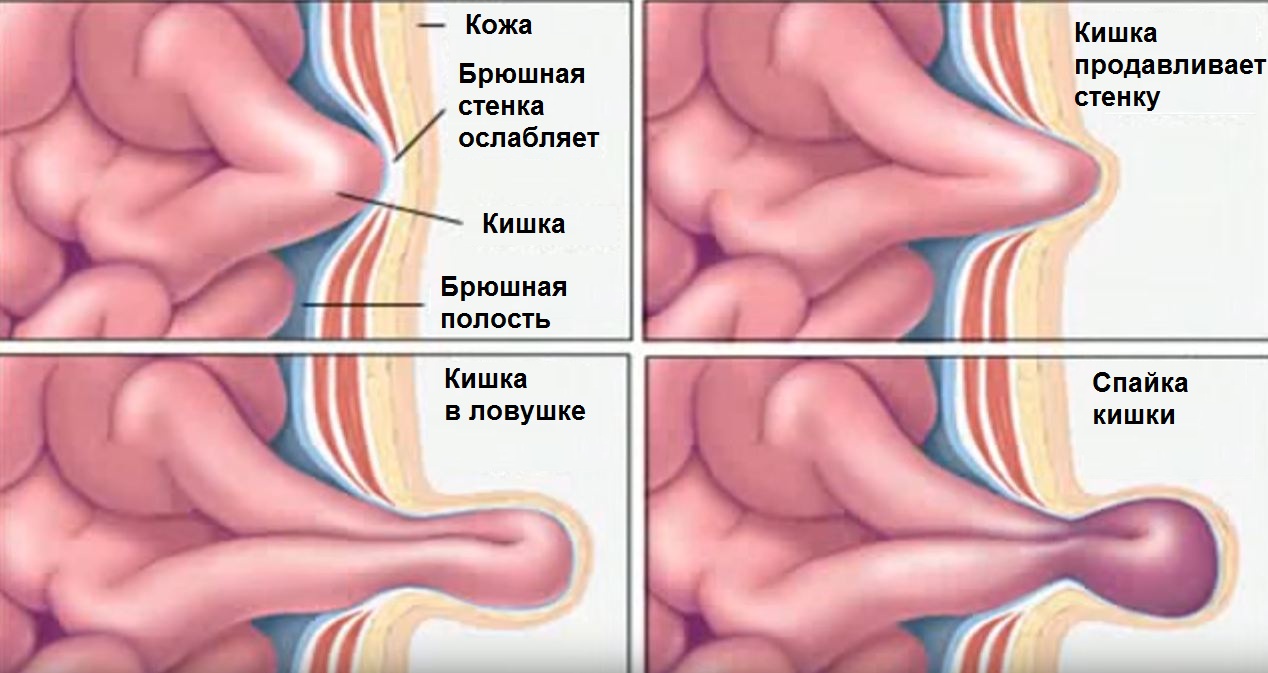
A hernia occurs when an organ or tissue pushes through a weak spot in the surrounding muscle or connective tissue. This results in a visible bulge, often in the abdomen or groin area. While hernias can sometimes be harmless, they may also cause discomfort and require medical attention.
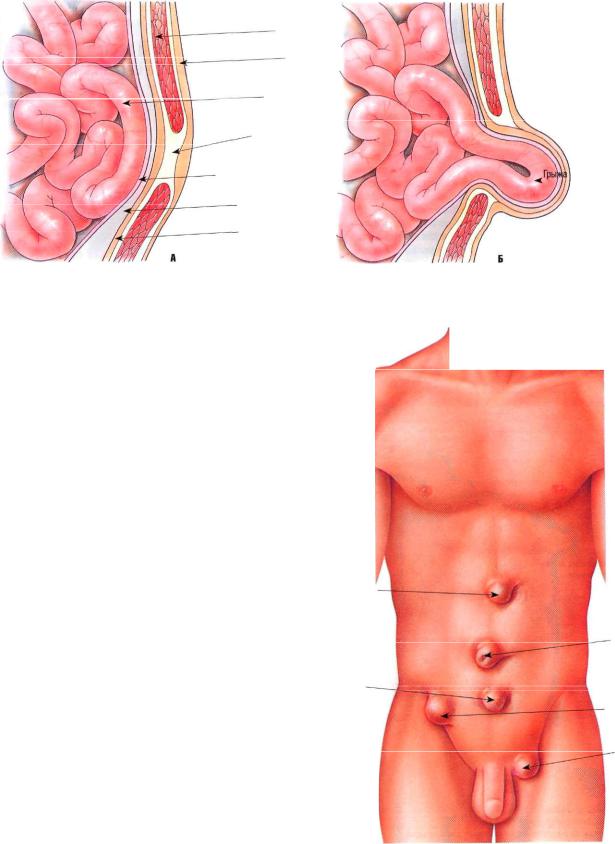
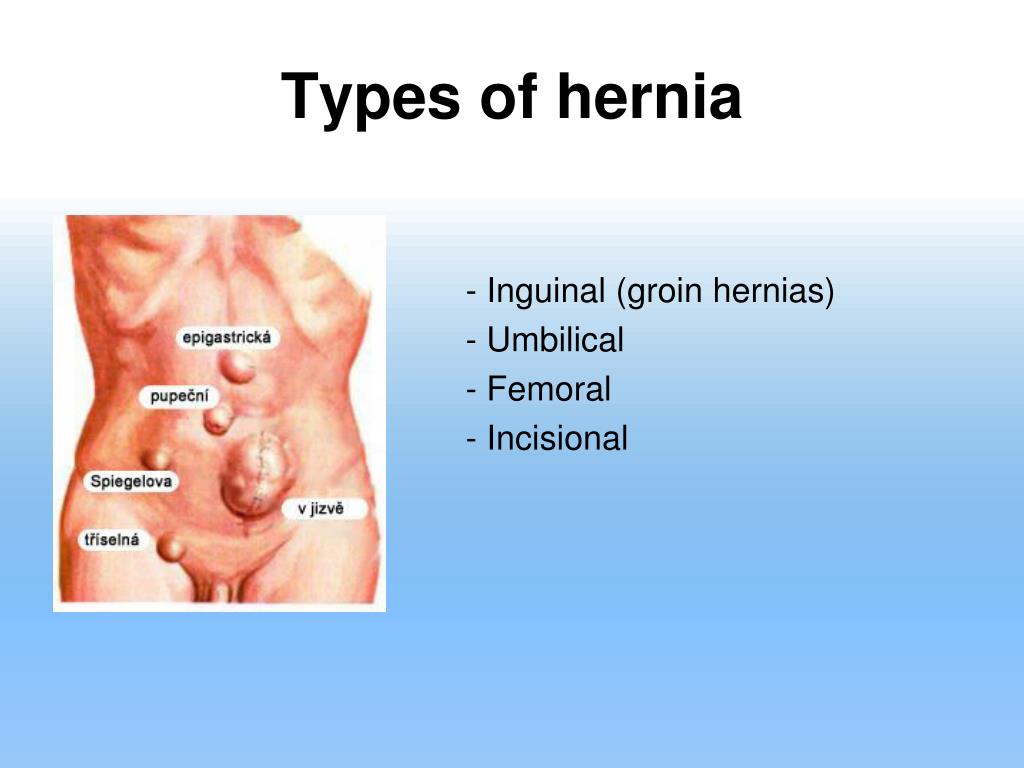
Common types of hernias include:
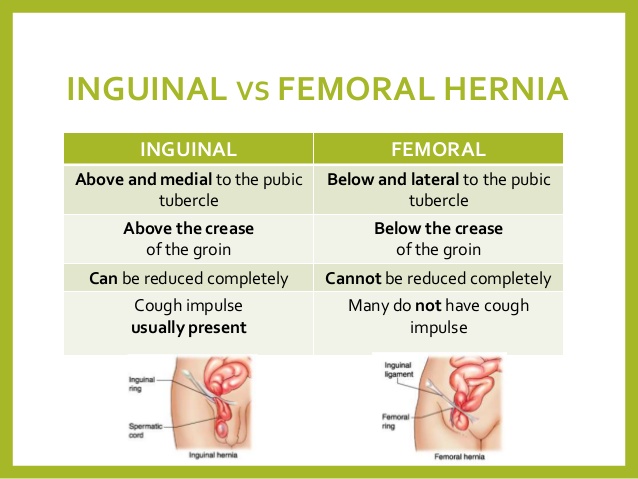
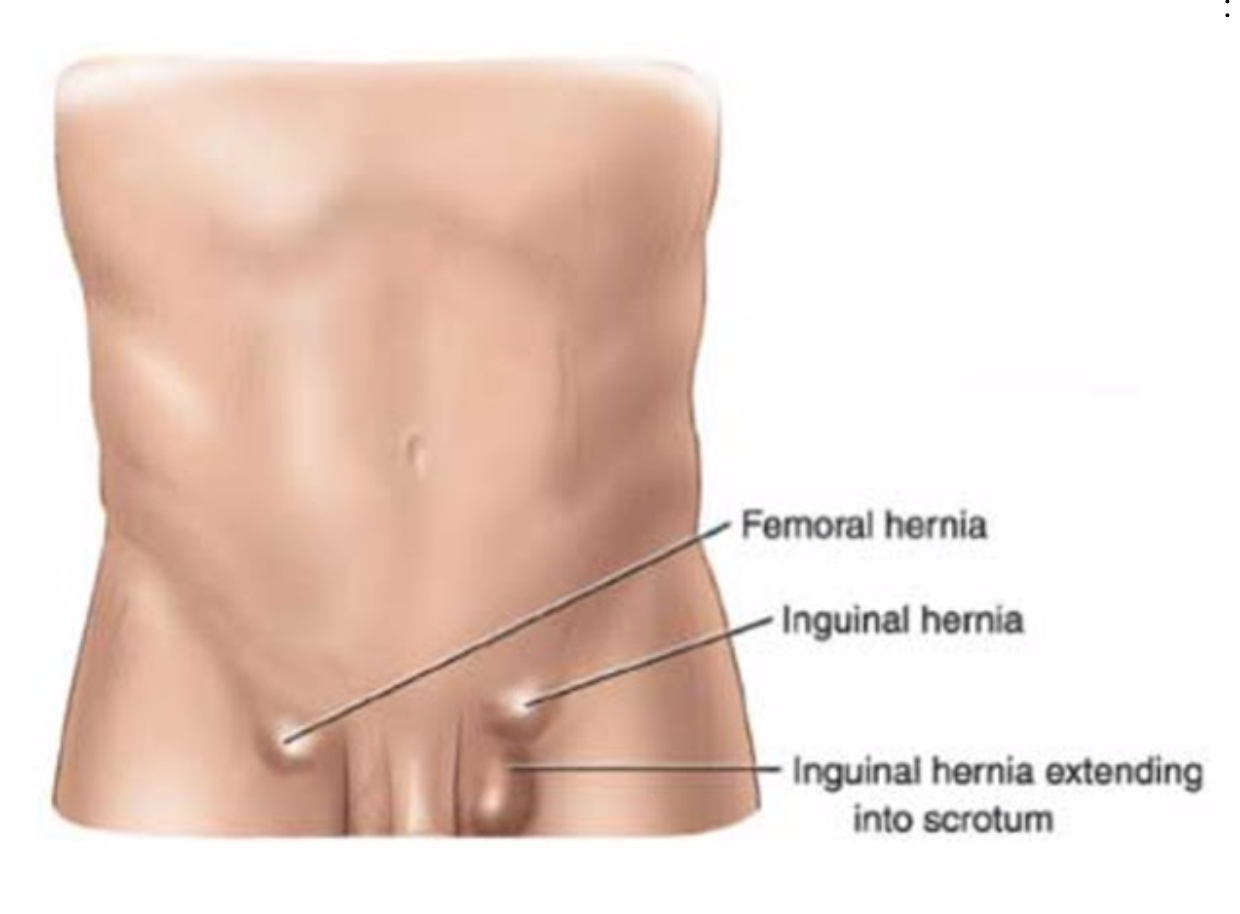
- Inguinal hernia: Located in the groin area, more common in men
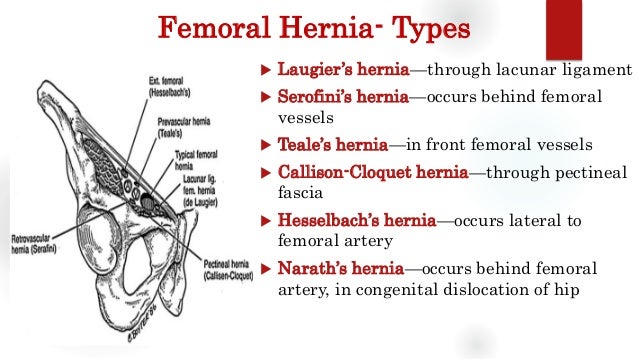
- Femoral hernia: Found just below the groin, more prevalent in women
- Hiatal hernia: Occurs when part of the stomach pushes into the chest cavity
- Umbilical hernia: Appears around the belly button
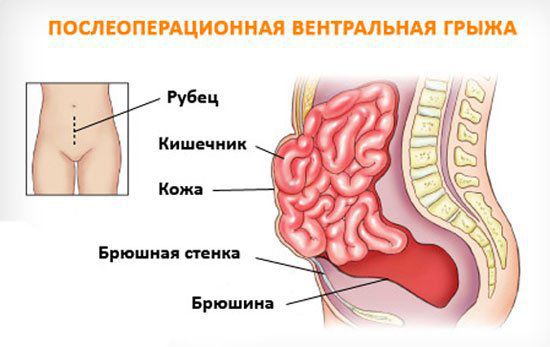
- Incisional hernia: Develops at the site of a previous abdominal surgery
Causes and Risk Factors for Hernia Development
Hernias can develop due to various factors, including congenital weaknesses in the abdominal wall and activities that increase pressure on this area. Some common causes and risk factors include:
- Chronic constipation or straining during bowel movements
- Persistent coughing
- Heavy lifting
- Obesity
- Pregnancy
- Smoking
- Family history of hernias
- Previous abdominal surgeries
Are certain age groups more susceptible to hernias? Indeed, the risk of developing a hernia increases with age, and hernias are generally more common in men than in women. However, specific types of hernias may be more prevalent in certain demographics. For instance, umbilical hernias are more common in infants, while hiatal hernias are more frequently seen in individuals over 50 years old.
Recognizing Hernia Symptoms and When to Seek Medical Attention
While some hernias may be asymptomatic, others can cause noticeable symptoms. Common signs of a hernia include:
- A visible bulge in the affected area
- Pain or discomfort, especially when lifting heavy objects or straining
- A feeling of heaviness or pressure in the abdomen
- Acid reflux or heartburn (in cases of hiatal hernia)
When should you seek immediate medical attention for a hernia? If you experience any of the following symptoms, it’s crucial to consult a healthcare professional without delay:
- Severe pain or tenderness in the hernia area
- Nausea or vomiting
- Inability to push the hernia back in
- Redness or discoloration of the skin over the hernia
- Fever
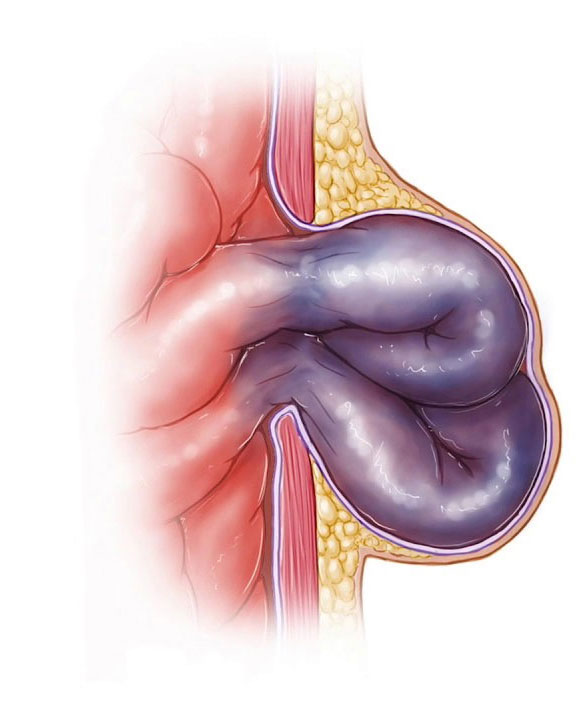
These symptoms may indicate a strangulated hernia, which is a medical emergency requiring immediate surgical intervention.
Diagnostic Approaches for Hernias
How are hernias typically diagnosed? In most cases, a physical examination is sufficient for a healthcare provider to diagnose a hernia. The doctor will visually inspect the affected area and may ask you to stand, cough, or strain to make the hernia more prominent. They may also gently palpate the area to assess the size and characteristics of the hernia.
In some cases, additional diagnostic tests may be necessary, such as:
- Ultrasound: To visualize soft tissues and confirm the presence of a hernia
- CT scan: To obtain detailed images of the abdominal area and assess the extent of the hernia
- MRI: To provide high-resolution images of soft tissues and detect small hernias
- Barium X-ray: Particularly useful for diagnosing hiatal hernias
Treatment Options: From Watchful Waiting to Surgical Intervention
The treatment approach for hernias depends on various factors, including the type, size, location, and symptoms of the hernia. What are the main treatment options available?

Watchful Waiting
For small, asymptomatic hernias, a “watch and wait” approach may be recommended. This involves monitoring the hernia for any changes or development of symptoms. However, it’s important to note that some types of hernias, such as femoral hernias, may require more immediate attention due to a higher risk of complications.
Lifestyle Modifications
In some cases, making certain lifestyle changes can help manage hernia symptoms and prevent further complications. These may include:
- Maintaining a healthy weight
- Avoiding heavy lifting
- Quitting smoking
- Treating chronic cough or constipation
- Using proper lifting techniques
Hernia Trusses
For some inguinal hernias, a hernia truss (a supportive undergarment) may be recommended to help keep the hernia in place and alleviate discomfort. However, this is typically a temporary solution and not a substitute for proper medical treatment.
Surgical Repair
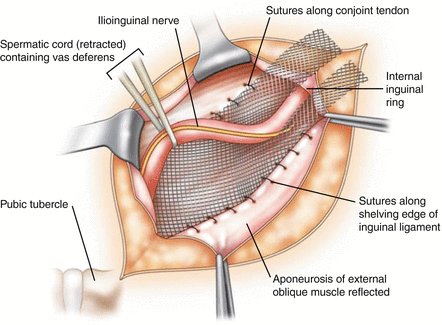
Surgery is often the most effective long-term treatment for hernias. There are two main surgical approaches:

- Open hernia repair: The surgeon makes an incision near the hernia site to push the protruding tissue back into place and reinforce the weakened area with stitches or synthetic mesh.
- Laparoscopic hernia repair: This minimally invasive procedure involves making several small incisions and using a laparoscope (a thin tube with a camera) to guide the repair. This technique often results in faster recovery times and less postoperative pain.
Which surgical approach is best for hernia repair? The choice between open and laparoscopic surgery depends on various factors, including the type and size of the hernia, the patient’s overall health, and the surgeon’s expertise. Your healthcare provider will discuss the most appropriate option for your specific case.
Recovery and Postoperative Care After Hernia Surgery
What can patients expect during the recovery period following hernia surgery? The recovery process varies depending on the type of surgery performed and individual factors. Generally, patients can expect:
- Some pain and discomfort in the days following surgery, which can be managed with prescribed pain medications
- Gradual return to normal activities, typically within 1-2 weeks for laparoscopic surgery and 3-6 weeks for open surgery
- Restrictions on heavy lifting and strenuous activities for several weeks
- Follow-up appointments to monitor healing and remove any stitches or staples
To promote optimal recovery, patients should follow their surgeon’s postoperative instructions carefully, which may include:
- Keeping the incision site clean and dry
- Wearing loose, comfortable clothing
- Gradually increasing physical activity as advised
- Eating a healthy, fiber-rich diet to prevent constipation
- Avoiding smoking, which can impair healing
Preventing Hernias: Lifestyle Strategies for Reducing Risk
While not all hernias can be prevented, certain lifestyle choices can help reduce the risk of developing a hernia or experiencing complications from an existing one. What are some effective strategies for hernia prevention?
- Maintain a healthy weight through proper diet and regular exercise
- Practice good posture and use proper lifting techniques when handling heavy objects
- Quit smoking to improve overall tissue health and reduce chronic coughing
- Eat a high-fiber diet and stay hydrated to prevent constipation
- Manage chronic conditions that may increase abdominal pressure, such as COPD or enlarged prostate
- Avoid straining during bowel movements or urination
- Strengthen core muscles through targeted exercises
By incorporating these strategies into your daily routine, you can help minimize your risk of developing a hernia and maintain overall abdominal health.
Complications and Long-term Outlook for Hernia Patients
What potential complications can arise from untreated hernias? While many hernias can remain asymptomatic for years, there are risks associated with leaving them untreated:
- Incarceration: The hernia becomes trapped in the abdominal wall, potentially leading to obstruction
- Strangulation: Blood supply to the herniated tissue is cut off, causing tissue death and requiring emergency surgery
- Bowel obstruction: Particularly in cases of intestinal hernias
- Chronic pain and discomfort
- Enlargement of the hernia over time
What is the long-term outlook for patients who undergo hernia repair? The prognosis for most hernia patients is generally good, especially when the condition is diagnosed and treated promptly. After successful surgical repair, many patients experience complete resolution of symptoms and can return to their normal activities without restrictions.
However, it’s important to note that there is a risk of hernia recurrence, even after surgical repair. The recurrence rate varies depending on factors such as the type of hernia, surgical technique used, and individual patient characteristics. To minimize the risk of recurrence, patients should:
- Follow postoperative instructions carefully
- Maintain a healthy weight
- Avoid activities that strain the abdominal muscles excessively
- Address underlying risk factors, such as chronic cough or constipation
- Attend regular follow-up appointments with their healthcare provider
By staying vigilant and adopting a proactive approach to their health, patients can significantly improve their long-term outlook following hernia treatment.
Emerging Trends and Future Directions in Hernia Management
What advancements are shaping the future of hernia treatment? The field of hernia management is continuously evolving, with several promising developments on the horizon:
Improved Surgical Techniques
Researchers are exploring new minimally invasive surgical approaches, such as robotic-assisted hernia repair, which may offer increased precision and potentially faster recovery times. Additionally, advancements in 3D imaging technology are helping surgeons plan and execute more accurate repairs.

Enhanced Mesh Materials
The development of biocompatible and bioresorbable mesh materials aims to reduce the risk of complications associated with traditional synthetic meshes. These new materials may promote better tissue integration and reduce the likelihood of chronic pain or mesh-related issues.
Personalized Treatment Approaches
As our understanding of hernia pathophysiology improves, there is a growing trend towards tailoring treatment plans to individual patients based on factors such as hernia type, size, location, and patient-specific risk factors. This personalized approach may lead to better outcomes and reduced recurrence rates.
Non-Surgical Interventions
Research is ongoing into non-surgical treatments for certain types of hernias, including the use of injectable biomaterials to strengthen weakened tissue and potentially prevent hernia formation or progression.
Genetic Research
Advances in genetic research may help identify individuals at higher risk for hernia development, allowing for earlier intervention and prevention strategies.
As these innovations continue to develop, patients can look forward to potentially more effective, less invasive, and more personalized approaches to hernia management in the future.
In conclusion, hernias are a common medical condition that can affect people of all ages and backgrounds. While they can sometimes be asymptomatic, hernias have the potential to cause significant discomfort and complications if left untreated. By understanding the causes, symptoms, and treatment options available, individuals can take proactive steps to manage their health and seek appropriate medical care when needed. With ongoing advancements in surgical techniques and materials, the future of hernia treatment looks promising, offering hope for improved outcomes and quality of life for patients worldwide.
Hernia: Causes, treatments, and diagnosis
Hernia is a common problem. It causes a localized bulge in the abdomen or groin.
It can often be harmless and pain-free, but at times it can bring discomfort and pain.
In this article, we investigate what a hernia is, the common causes of hernia, and how they are treated.
Fast facts on hernias
- Hernias often produce no troublesome symptoms, but abdominal complaints may signal a serious problem.
- They are usually straightforward to diagnose, simply by feeling and looking for the bulge.
- Treatment is a choice between watchful waiting and corrective surgery, either via an open or keyhole operation.
- Inguinal hernia surgery is more common in childhood and old age, while the likelihood of femoral hernia surgery increases throughout life.
Was this helpful?
A hernia occurs when there is a weakness or hole in the peritoneum, the muscular wall that usually keeps abdominal organs in place.
This defect in the peritoneum allows organs and tissues to push through, or herniate, producing a bulge.
The lump may disappear when the person lies down, and sometimes it can be pushed back into. Coughing may make it reappear.
Hernias can commonly be found in the following areas:
Groin: a femoral hernia creates a bulge just below the groin. This is more common in women. An inguinal hernia is more common in men. It is a bulge in the groin that may reach the scrotum.
Upper part of the stomach: a hiatal or hiatus hernia is caused by the upper part of the stomach pushing out of the abdominal cavity and into the chest cavity through an opening in the diaphragm.
Belly button: a bulge in this region is produced by an umbilical or periumbilical hernia.
Surgical scar: past abdominal surgery can lead to an incisional hernia through the scar.
With the exception of an incisional hernia (a complication of abdominal surgery), in most cases, there is no obvious reason for a hernia to occur. The risk of hernia increases with age and occurs more commonly in men than in women.
The risk of hernia increases with age and occurs more commonly in men than in women.
A hernia can be congenital (present at birth) or develop in children who have a weakness in their abdominal wall.
Activities and medical problems that increase pressure on the abdominal wall can lead to a hernia. These include:
- straining on the toilet (due to long-term constipation, for example)
- persistent cough
- cystic fibrosis
- enlarged prostate
- straining to urinate
- being overweight or obese
- abdominal fluid
- lifting heavy items
- peritoneal dialysis
- poor nutrition
- smoking
- physical exertion
- undescended testicles
Risk factors for hernia
The risk factors can be broken down by hernia type:
Incisional hernia risk factors
Because an incisional hernia is the result of surgery, the clearest risk factor is a recent surgical procedure on the abdomen.
People are most susceptible 3-6 months after the procedure, especially if:
- they are involved in strenuous activity
- have gained additional weight
- become pregnant
These factors all put extra stress on tissue as it heals.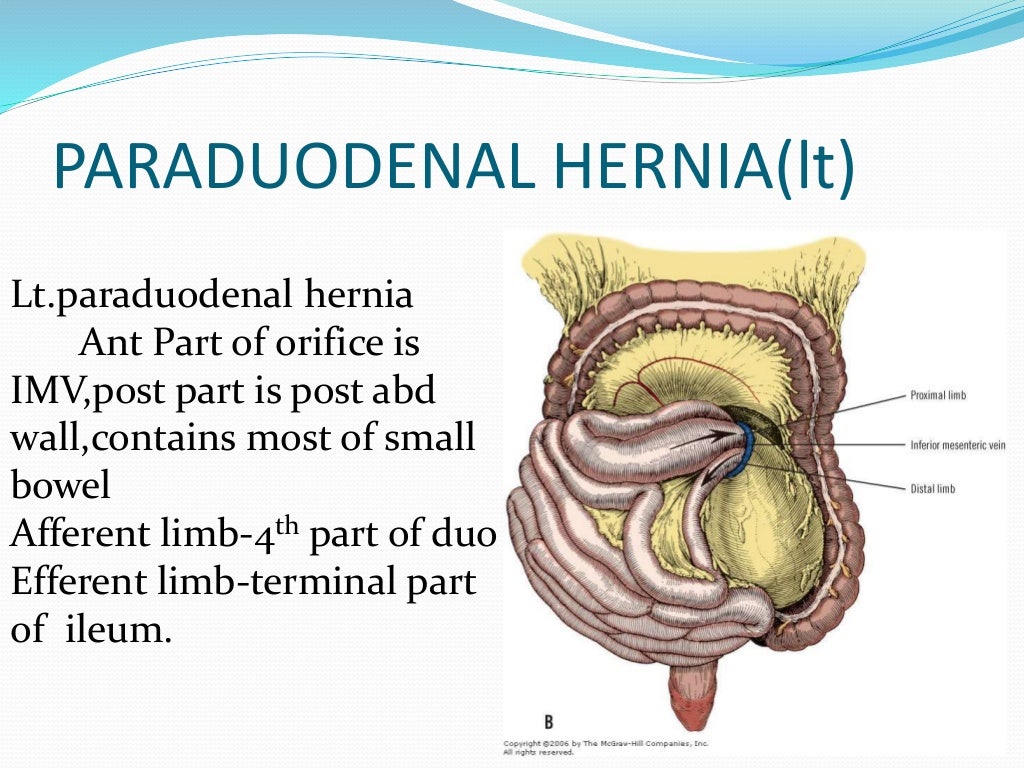
Inguinal hernia risk factors
Those with a higher risk of inguinal hernia incude:
Share on PinterestSmoking tobacco increases the risk of inguinal hernias.
- older adults
- people with close relatives who have had inguinal hernias
- people who have had inguinal hernias previously
- males
- smokers, as chemicals in tobacco weaken tissues, making a hernia more likely
- people with chronic constipation
- premature birth and low birth weight
- pregnancy
Umbilical hernia risk factors
Umbilical hernias are most common in babies with a low birth weight and premature babies.
In adults, the risk factors include:
- being overweight
- having multiple pregnancies
- being female
Hiatal hernia risk factors
The risk of hiatal hernia is higher in people who:
- are aged 50 years or over
- have obesity
In many cases, a hernia is no more than a painless swelling that presents no problems and needs no immediate medical attention.
A hernia may, however, be the cause of discomfort and pain, with symptoms often becoming worse when standing, straining, or lifting heavy items. Most people who notice increasing swelling or soreness eventually see a doctor.
In some cases, a hernia needs immediate surgery, for instance, when part of the gut becomes obstructed or strangulated by an inguinal hernia.
Immediate medical attention should be sought if an inguinal hernia produces acute abdominal complaints such as:
- pain
- nausea
- vomiting
- the bulge cannot be pushed back into the abdomen
The swelling, in these cases, is typically firm and tender and cannot be pushed back up into the abdomen.
A hiatal hernia can produce symptoms of acid reflux, such as heartburn, which is caused by stomach acid getting into the esophagus.
For a hernia without symptoms, the usual course of action is to watch and wait, but this can be risky for certain types of hernia, such as femoral hernias.
Within 2 years of a femoral hernia being diagnosed, 40 percent result in bowel strangulation.
It remains unclear whether non-emergency surgery is worthwhile for hernia repair in cases of an inguinal hernia without symptoms that can be pushed back into the abdomen.
The American College of Surgeons and some other medical bodies consider elective surgery unnecessary in such cases, recommending instead a course of watchful waiting.
Others recommend surgical repair to remove the risk of later strangulation of the gut, a complication where blood supply is cut off to an area of tissue, which requires an emergency procedure.
These health authorities consider an earlier, routine operation preferable to a more risky emergency procedure.
Types of surgery
Share on PinterestBelly button following hernia surgery.
Although surgical options depend on individual circumstances, including the location of the hernia, there are two main types of surgical intervention for hernia:
- open surgery
- laparoscopic operation (keyhole surgery)
Open surgical repair closes the hernia using sutures, mesh, or both, and the surgical wound in the skin is closed with sutures, staples, or surgical glue.
Laparoscopic repair is used for repeat operations to avoid previous scars, and while usually more expensive, is less likely to cause complications such as infection.
Surgical repair of a hernia guided by a laparoscope allows for the use of smaller incisions, enabling a faster recovery from the operation.
The hernia is repaired in the same way as in open surgery, but it is guided by a small camera and a light introduced through a tube. Surgical instruments are inserted through another small incision. The abdomen is inflated with gas to help the surgeon see better and give them space to work; the whole operation is performed under general anesthetic.
Hernia in children
Inguinal hernia is one of the most common surgical conditions in infants and children.
A 2014 systematic review of 20 years of data on conventional open hernia repair (herniorrhaphy) and laparoscopic hernia repair (herniorrhaphy) in infants and children found that laparoscopic surgery is faster than open surgery for bilateral hernias, but that there is no significant difference in operating time for unilateral inguinal hernia repair.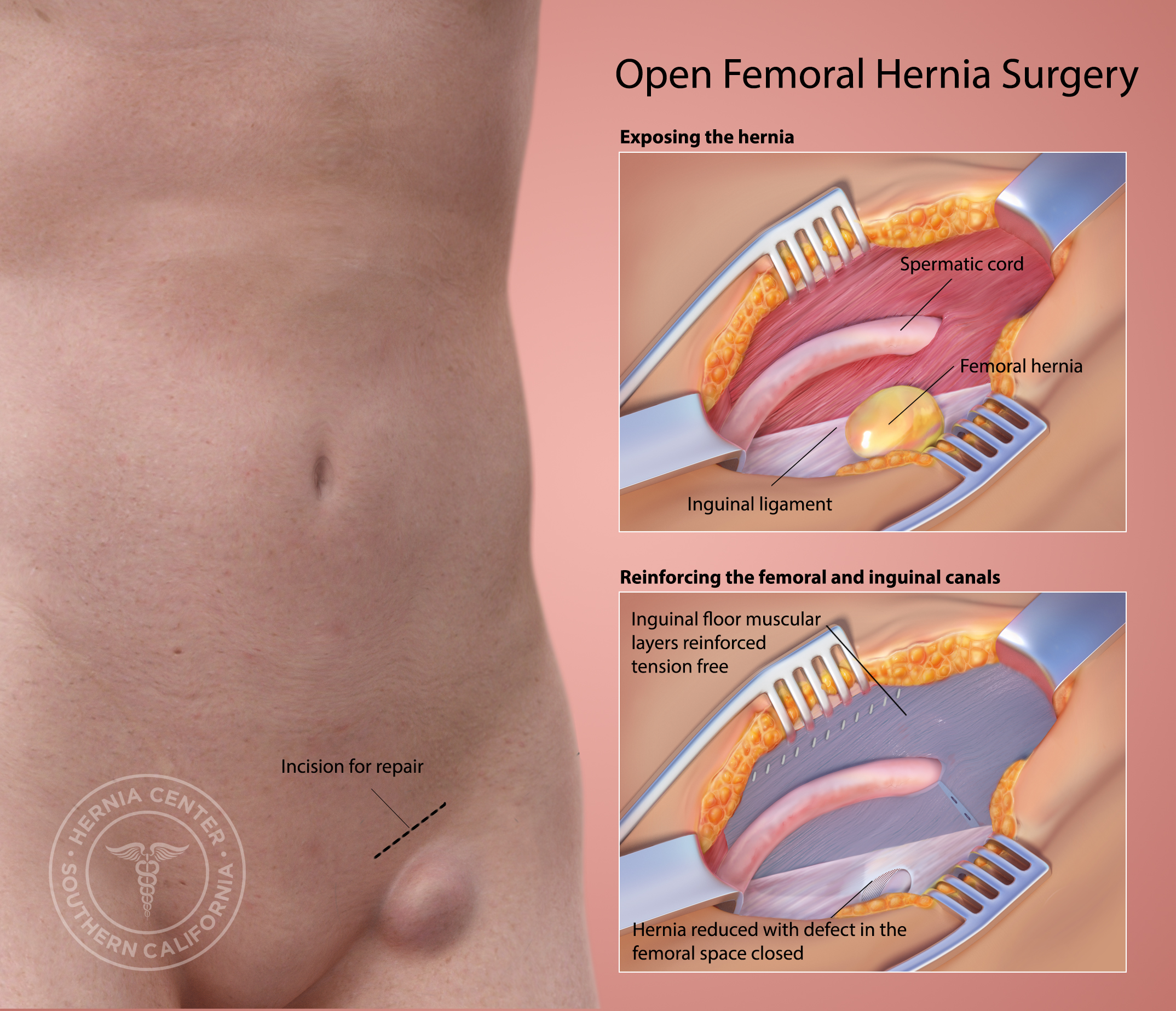
The rate of recurrence is similar for both types of procedure, but complications, such as wound infection, are more likely with open surgery, especially in infants.
Read the article in Spanish
Hernia: Causes, treatments, and diagnosis
Hernia is a common problem. It causes a localized bulge in the abdomen or groin.
It can often be harmless and pain-free, but at times it can bring discomfort and pain.
In this article, we investigate what a hernia is, the common causes of hernia, and how they are treated.
Fast facts on hernias
- Hernias often produce no troublesome symptoms, but abdominal complaints may signal a serious problem.
- They are usually straightforward to diagnose, simply by feeling and looking for the bulge.
- Treatment is a choice between watchful waiting and corrective surgery, either via an open or keyhole operation.
- Inguinal hernia surgery is more common in childhood and old age, while the likelihood of femoral hernia surgery increases throughout life.

Was this helpful?
A hernia occurs when there is a weakness or hole in the peritoneum, the muscular wall that usually keeps abdominal organs in place.
This defect in the peritoneum allows organs and tissues to push through, or herniate, producing a bulge.
The lump may disappear when the person lies down, and sometimes it can be pushed back into. Coughing may make it reappear.
Hernias can commonly be found in the following areas:
Groin: a femoral hernia creates a bulge just below the groin. This is more common in women. An inguinal hernia is more common in men. It is a bulge in the groin that may reach the scrotum.
Upper part of the stomach: a hiatal or hiatus hernia is caused by the upper part of the stomach pushing out of the abdominal cavity and into the chest cavity through an opening in the diaphragm.
Belly button: a bulge in this region is produced by an umbilical or periumbilical hernia.
Surgical scar: past abdominal surgery can lead to an incisional hernia through the scar.
With the exception of an incisional hernia (a complication of abdominal surgery), in most cases, there is no obvious reason for a hernia to occur. The risk of hernia increases with age and occurs more commonly in men than in women.
A hernia can be congenital (present at birth) or develop in children who have a weakness in their abdominal wall.
Activities and medical problems that increase pressure on the abdominal wall can lead to a hernia. These include:
- straining on the toilet (due to long-term constipation, for example)
- persistent cough
- cystic fibrosis
- enlarged prostate
- straining to urinate
- being overweight or obese
- abdominal fluid
- lifting heavy items
- peritoneal dialysis
- poor nutrition
- smoking
- physical exertion
- undescended testicles
Risk factors for hernia
The risk factors can be broken down by hernia type:
Incisional hernia risk factors
Because an incisional hernia is the result of surgery, the clearest risk factor is a recent surgical procedure on the abdomen.
People are most susceptible 3-6 months after the procedure, especially if:
- they are involved in strenuous activity
- have gained additional weight
- become pregnant
These factors all put extra stress on tissue as it heals.
Inguinal hernia risk factors
Those with a higher risk of inguinal hernia incude:
Share on PinterestSmoking tobacco increases the risk of inguinal hernias.
- older adults
- people with close relatives who have had inguinal hernias
- people who have had inguinal hernias previously
- males
- smokers, as chemicals in tobacco weaken tissues, making a hernia more likely
- people with chronic constipation
- premature birth and low birth weight
- pregnancy
Umbilical hernia risk factors
Umbilical hernias are most common in babies with a low birth weight and premature babies.
In adults, the risk factors include:
- being overweight
- having multiple pregnancies
- being female
Hiatal hernia risk factors
The risk of hiatal hernia is higher in people who:
- are aged 50 years or over
- have obesity
In many cases, a hernia is no more than a painless swelling that presents no problems and needs no immediate medical attention.
A hernia may, however, be the cause of discomfort and pain, with symptoms often becoming worse when standing, straining, or lifting heavy items. Most people who notice increasing swelling or soreness eventually see a doctor.
In some cases, a hernia needs immediate surgery, for instance, when part of the gut becomes obstructed or strangulated by an inguinal hernia.
Immediate medical attention should be sought if an inguinal hernia produces acute abdominal complaints such as:
- pain
- nausea
- vomiting
- the bulge cannot be pushed back into the abdomen
The swelling, in these cases, is typically firm and tender and cannot be pushed back up into the abdomen.
A hiatal hernia can produce symptoms of acid reflux, such as heartburn, which is caused by stomach acid getting into the esophagus.
For a hernia without symptoms, the usual course of action is to watch and wait, but this can be risky for certain types of hernia, such as femoral hernias.
Within 2 years of a femoral hernia being diagnosed, 40 percent result in bowel strangulation.
It remains unclear whether non-emergency surgery is worthwhile for hernia repair in cases of an inguinal hernia without symptoms that can be pushed back into the abdomen.
The American College of Surgeons and some other medical bodies consider elective surgery unnecessary in such cases, recommending instead a course of watchful waiting.
Others recommend surgical repair to remove the risk of later strangulation of the gut, a complication where blood supply is cut off to an area of tissue, which requires an emergency procedure.
These health authorities consider an earlier, routine operation preferable to a more risky emergency procedure.
Types of surgery
Share on PinterestBelly button following hernia surgery.
Although surgical options depend on individual circumstances, including the location of the hernia, there are two main types of surgical intervention for hernia:
- open surgery
- laparoscopic operation (keyhole surgery)
Open surgical repair closes the hernia using sutures, mesh, or both, and the surgical wound in the skin is closed with sutures, staples, or surgical glue.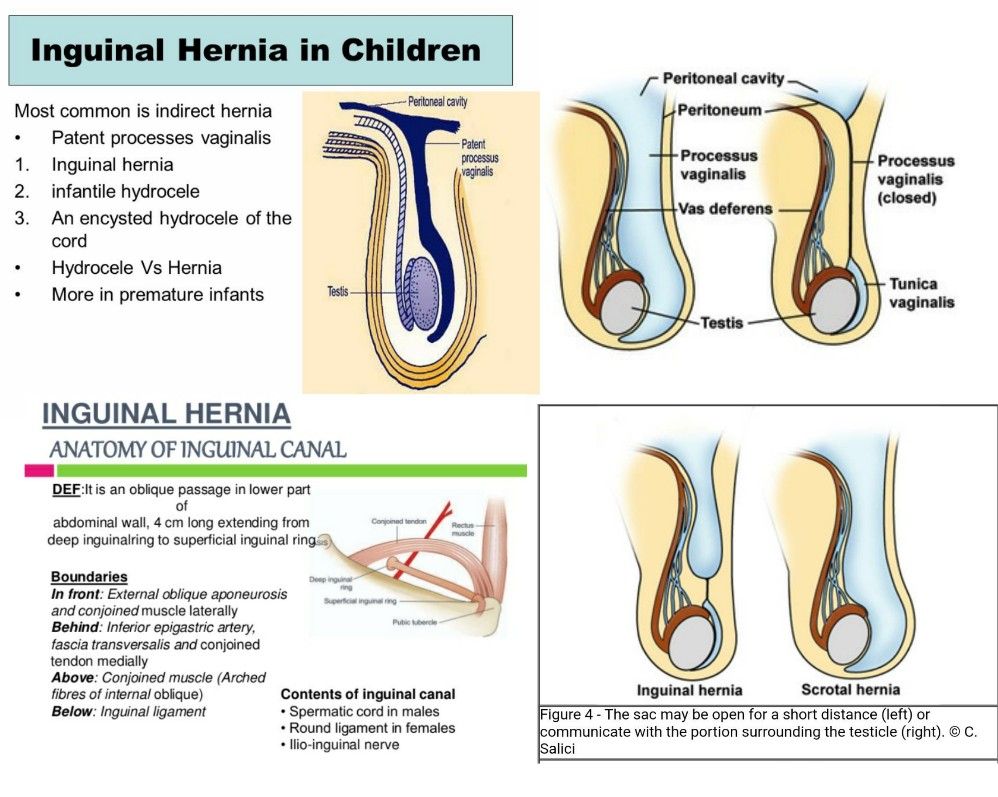
Laparoscopic repair is used for repeat operations to avoid previous scars, and while usually more expensive, is less likely to cause complications such as infection.
Surgical repair of a hernia guided by a laparoscope allows for the use of smaller incisions, enabling a faster recovery from the operation.
The hernia is repaired in the same way as in open surgery, but it is guided by a small camera and a light introduced through a tube. Surgical instruments are inserted through another small incision. The abdomen is inflated with gas to help the surgeon see better and give them space to work; the whole operation is performed under general anesthetic.
Hernia in children
Inguinal hernia is one of the most common surgical conditions in infants and children.
A 2014 systematic review of 20 years of data on conventional open hernia repair (herniorrhaphy) and laparoscopic hernia repair (herniorrhaphy) in infants and children found that laparoscopic surgery is faster than open surgery for bilateral hernias, but that there is no significant difference in operating time for unilateral inguinal hernia repair.
The rate of recurrence is similar for both types of procedure, but complications, such as wound infection, are more likely with open surgery, especially in infants.
Read the article in Spanish
Three ways to cure spinal hernia at home –
- Post category: Articles
- Post author: Author of the article Alexander Serik
- This entry was published on: 11/22/2019
- Entry modified: 01/06/2021
- Reading time: 1 min(s) read
Home treatment
There are many stories on the net about how to heal a herniated disc on your own. Do you think this is possible? Perhaps, if you try very hard and do not stop treatment.
Where to start?
From plan. You need to adjust the diet, lead an active lifestyle, do exercises, use folk remedies.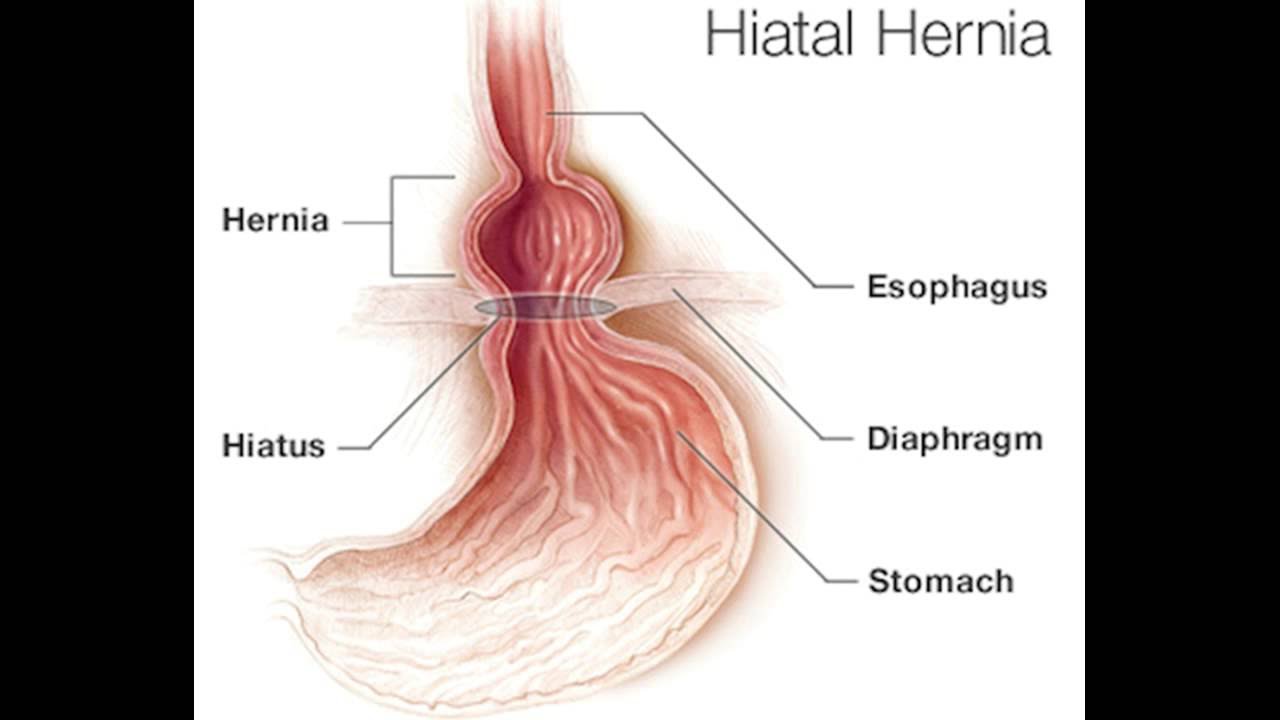 But remember that you can not do without a doctor. Those remedies that we will write about will help you enhance the effect of treatment.
But remember that you can not do without a doctor. Those remedies that we will write about will help you enhance the effect of treatment.
Let’s start with the diet.
spinal hernia diet
Watch your diet. This will help to give “nutrition” to the diseased disc, because a hernia occurs due to a lack of nutrition.
What can you eat?
- Wholemeal bread
- Fruit: pears, apples
- Vegetables: pumpkin, beets
- Aspic
- Fresh milk
- Nuts
- Cereals
- Dietary meat
What should not be consumed? We adjust our lifestyle
Hernia of the spine lifestyle
Perhaps, before the hernia appeared, you were actively involved in sports, carried store and easily rearranged at home. Now no heavy bags more than two kilograms
- Walk
- Swim
- Don’t make sudden movements
- Squat instead of bending over to pick up objects from the floor
Do back exercises every day. Here is one of the simplest, which must be performed every day, 5-10 times, and it will be possible to cure a hernia without surgery.
Here is one of the simplest, which must be performed every day, 5-10 times, and it will be possible to cure a hernia without surgery.
- Lie on your back, palms on the floor. Try to lift your pelvis up. Stay in this position for 5-10 seconds. Then drop down. Repeat 5 times, increasing the number of repetitions.
folk remedies
spinal hernia folk remedies
Below we will publish three recipes that are successfully used during treatment.
Camphor oil and milk
Rub the affected area of the spine with camphor oil. Apply a compress with warm cow’s milk on top. You can wrap this place with a warm scarf or wrap yourself up and sit warm for at least two hours.
Garlic and vodka
You will need 300 gr. garlic, 500 ml of vodka. Grind garlic, pour vodka and let it brew for 10 days. Transfer the finished mixture to gauze and apply to the spine. Cover with polyethylene and insulate.
Birch leaves and oil
You need to collect birch leaves, pour them with oil (about 200 ml). Let it brew for two weeks, and then you can rub the sore spot with this remedy.
Let it brew for two weeks, and then you can rub the sore spot with this remedy.
We have described to you the healthiest way to get rid of a hernia without surgery or medical treatment. Believe in yourself, take care of your health and you will be able to get rid of pain forever.
Call now and sign up for a free appointment
+7 (812) 922-44-24
If you have similar SYMPTOMS or a medical condition,
then you can Make an appointment for a free appointment right now to
By phone number: +7 (812) 922-44-24
Advanced Joint and Spine Treatment
Non-surgical spine rehabilitation program in St. Petersburg. A complex of procedures that not only relieves pain, but also ensures the recovery of the patient without pain and surgery.
An innovative way to restore joints at any age, with virtually no contraindications. It is possible to carry out the procedure at the first appointment, and feel the improvement after 2 weeks.
Not only pain relief, but also effective treatment of joints and spine
+7 (812) 922-44-24
+7 (911) 922-44-24
sign up for a free consultation
Tags: hernia, hernia treatment, folk remedies
Next PostMore Articles
Drug treatment of intervertebral hernia, osteochondrosis, back pain, joints joints, relieve muscle tension). For pathogenetic therapy, anti-inflammatory, decongestant drugs, chondroprotectors, enzyme, vitamin, tonic drugs and others are prescribed.
Drug treatment of degenerative-dystrophic diseases of the spine and joints (arthrosis, osteochondrosis, spondylosis, spondylarthrosis, protrusion or herniation of the intervertebral disc, etc.) is conditionally divided into three main areas:
- etiotropic therapy – treatment is aimed at identifying and eliminating the cause of the disease ;
- pathogenetic therapy – influence on the mechanisms of disease development;
- symptomatic therapy – elimination of external symptoms of the disease.

Etiotropic treatment , aimed at identifying and eliminating the cause of the disease, is considered the most effective method of treatment. The impact on the cause of the disease allows not only to reduce the external manifestations of the disease, but also to stop its development. With the appointment of etiotropic therapy in the early stages of the disease, it is possible to achieve complete recovery and restore the lost functions of the spine and joints.
The main cause of degenerative-dystrophic diseases of the spine and joints is a violation of blood supply, a decrease in the trophism of the vertebrae, intervertebral discs, joints of the spine, surrounding soft tissues, which develops as a result of a sedentary lifestyle, insufficiency of targeted exercises for the spine and joints, overload of the musculoskeletal system and other factors.
- The main methods of etiotropic therapy are:
- Lifestyle changes , adequate targeted physical activity on the spine and joints, proper nutrition, proper organization of the workplace, control of posture and body weight.

- Restoration of normal function of the joints of the spine, back muscles, intervertebral discs, which is achieved with the help of such methods of treatment as: massage, manual therapy, physiotherapy, reflexology, therapeutic blockades, physiotherapy exercises.
- The following groups of drugs can be classified as etiotropic drugs:
Chondroprotectors. In the modern scheme of treatment of osteochondrosis, osteoarthrosis and other diseases of the spine and joints, an important place is given to chondroprotectors. According to the recommendations of the Association of Rheumatologists of Ukraine, they, along with non-steroidal anti-inflammatory drugs (NSAIDs), are the basis of the therapeutic approach in patients with osteoarthritis.
The main chondroprotectors are glucosamine and chondroitin sulfate. They are natural components of articular cartilage, are part of the proteoglycans and glycosaminoglycans of cartilage tissue. The most important moment in the pathogenesis of osteoarthritis is the formation of proteoglycan deficiency, which consists in the depolymerization of protein-polysaccharide complexes with the formation of smaller compounds that leave the cartilage. At the same time, the function of chondrocytes is also impaired, they synthesize less stable proteoglycans, the loss of the physiological properties of cartilage develops, which is accompanied by the formation of erosions and cracks in the cartilage.
At the same time, the function of chondrocytes is also impaired, they synthesize less stable proteoglycans, the loss of the physiological properties of cartilage develops, which is accompanied by the formation of erosions and cracks in the cartilage.
Glucosamine and chondroitin sulfate are used in the treatment of osteoarthritis and similar diseases as natural metabolites as agents capable of exerting a protective effect on cartilage.
Synovial fluid implants . Currently, high molecular weight hyaluronic acid preparations are widely used in the medical practice of osteoarthritis. They improve the elasticity and viscosity of endogenous hyaluronan. This is actually an analogue of the synovial fluid in the joints. By protecting pain receptors, hyaluronic acid preparations eliminate pain, improve joint mobility by improving depreciation (elasticity), increase lubrication of intraarticular tissues, protecting articular cartilage from inflammatory mediators.
Homeopathic medicines . They have a therapeutic effect on the principle of “similarity”, causing an exacerbation of chronic long-term diseases, as a result of which the body’s own defenses are activated, aimed at combating this disease. Homeopathic medicines do not cause side effects.
They have a therapeutic effect on the principle of “similarity”, causing an exacerbation of chronic long-term diseases, as a result of which the body’s own defenses are activated, aimed at combating this disease. Homeopathic medicines do not cause side effects.
Pathogenetic treatment – aimed at eliminating the mechanisms of disease development. These include anti-inflammatory, decongestant, hormonal and enzyme preparations, muscle relaxants, etc. These drugs can reduce the symptoms of the disease by eliminating pathological processes such as inflammation, swelling, muscle spasm.
If you stop taking these drugs and do not eliminate the underlying cause of the disease, the symptoms of the disease usually return. Therefore, these drugs are usually prescribed for a long period of time, and in some cases, patients are prescribed lifelong use of them.
The use of these drugs is also often accompanied by various side effects, for example: NSAIDs can cause toxic damage to the liver, kidneys, central nervous system, irritant effect on the gastrointestinal tract, depression of the hematopoietic system, allergic reactions; long-term use of glucocorticoids leads to the destruction of articular cartilage, the development of osteoporosis, decreased immunity, and metabolic disorders.
Non-steroidal anti-inflammatory drugs (NSAIDs) – the most commonly used drugs for the treatment of degenerative-dystrophic diseases of the spine and joints, have analgesic, antipyretic and anti-inflammatory effects, reduce pain, fever and inflammation.
Most drugs in this group are non-selective inhibitors of the cyclooxygenase enzyme, which is responsible for the production of inflammatory mediators (prostaglandins, thromboxane).
The use of NSAIDs also has many undesirable side effects, such as damage to the mucous membrane of the digestive tract, impaired liver and kidney function, leukopenia, allergic reactions, etc.
Muscle relaxants . They are prescribed to reduce muscle tone, in complex therapy – to eliminate contractures.
Glucocorticosteroids . These drugs include the natural hormones of the adrenal cortex. They are often prescribed for symptoms of reactive synovitis. Long-term use significantly worsens the course of the disease due to damage to articular cartilage – inhibition of metabolic processes in chondrocytes, resulting in a violation of the organization of the matrix, which reduces the resistance of cartilage to stress. Such drugs are prescribed in a short course.
Such drugs are prescribed in a short course.
Biogenic stimulants . Aloe liquid extract is an adaptogenic agent that stimulates regeneration processes.
Administer s.c. 1 ml daily. The course – 15-25 injections.
Fibs – a drug that stimulates tissue regeneration processes.
Administer s.c. 1 ml daily. The course – 15-25 injections.
Preparations that improve blood microcirculation in tissues .
Pentoxifylline is an angioprotector, a derivative of methylxanthine. The mechanism of action is associated with the inhibition of phosphodiesterase and the accumulation of cAMP in vascular smooth muscle cells, in blood cells, and in other tissues and organs. The drug improves microcirculation and tissue oxygen supply, to the greatest extent – in the limbs and the central nervous system.
Administered intravenously as a drip infusion (5 ml solution) to 200 ml saline once a day. The course – 15 infusions. It is also taken orally 2 tablets (200 mg) 3 times a day. Patients with a large weight are prescribed 400 mg 3 times a day. The course is a month. IV infusions can be carried out not only in a hospital, but also in a polyclinic in a specially equipped treatment room.
Patients with a large weight are prescribed 400 mg 3 times a day. The course is a month. IV infusions can be carried out not only in a hospital, but also in a polyclinic in a specially equipped treatment room.
Enzyme preparations . Systemic Enzyme Therapy (SET) is a treatment using targeted mixtures of hydrolytic enzymes, the therapeutic effectiveness of which is based on a complex effect on key processes in the body.
Acting systemically, enzymes have a variety of effects, realizing their influence through anti-inflammatory, immunomodulatory, antiplatelet, fibrinolytic, decongestant and secondary analgesic effects.
Vitamins . For the treatment of osteochondrosis, it is recommended to use vitamins A, B1, B6, B12, C, D, E.
B group vitamins reduce the severity of neurological disorders caused by osteochondrosis, restore normal tissue sensitivity, and reduce pain.
In the treatment of osteochondrosis, B vitamins can be taken in the form of tablets or injected. There are a number of complex preparations containing these vitamins in their composition.
There are a number of complex preparations containing these vitamins in their composition.
For the treatment of osteochondrosis, vitamin D is also successfully used, which is desirable to combine with the additional administration of calcium. There are complex preparations of vitamin D and calcium that help restore normal bone density and strengthen the ligamentous apparatus. The use of vitamin D preparations is especially indicated in cases where osteochondrosis develops against the background of ongoing osteoporosis. This phenomenon is often observed, especially among the elderly.
Vitamins A, C and E are powerful antioxidants that contribute to the additional oxidation of free radicals, which appear in large quantities in the pathology zone and provoke further damage to intervertebral cartilage tissues. In turn, antioxidant vitamins contribute to the enhancement of regeneration processes.
For the treatment of osteochondrosis, based on the characteristics of the disease, the doctor may prescribe the intake of certain vitamins or a vitamin complex.