Is there a lymph node on back of neck. Lymph Nodes on Back of Neck: 7 Causes Including Sebaceous Cysts
What are the common causes of bumps on the back of the neck. How can you identify a sebaceous cyst. What are the symptoms of swollen lymph nodes. When should you seek medical attention for a neck lump.
Understanding Sebaceous Cysts: A Common Neck Bump
Sebaceous cysts are a frequent cause of bumps on the back of the neck. These small, soft lumps form when sebaceous glands, which produce an oily substance called sebum, become blocked or damaged. While typically harmless, sebaceous cysts can sometimes be a cosmetic concern.
Key characteristics of sebaceous cysts include:
- Soft, movable bumps under the skin
- Common locations: face, neck, and torso
- Usually painless
- Can vary in size, but often smaller than 5 cm in diameter
Do sebaceous cysts require treatment. In most cases, sebaceous cysts don’t need medical intervention. However, if a cyst becomes infected, grows larger than 5 cm, or recurs after removal, it’s advisable to consult a healthcare professional. Some individuals opt for removal for cosmetic reasons, which can be done through a minor surgical procedure.
Ingrown Hairs: A Pesky Problem Along the Hairline
Ingrown hairs are another common cause of bumps on the back of the neck, especially along the hairline. These occur when a hair grows back into the skin or becomes trapped beneath the surface, resulting in a pimple-like bump.
Why do ingrown hairs occur. Ingrown hairs are more likely to develop in areas where hair is frequently removed through methods like shaving, waxing, or plucking. People with short hair are particularly susceptible to ingrown hairs on the back of the neck due to regular haircuts.
Identifying ingrown hairs:
- Small, red bumps resembling pimples
- May appear singularly or in clusters
- Often itchy or slightly painful
- Sometimes visible hair trapped beneath the skin
How should you treat ingrown hairs. Most ingrown hairs resolve on their own without intervention. To prevent infection, avoid squeezing or picking at the affected area. If ingrown hairs persist or become painful, consider adjusting your hair removal methods or consulting a dermatologist for advice.

Boils: When Bacteria Invade Hair Follicles
Boils, also known as furuncles, are pus-filled bumps that form under the skin due to bacterial infection in hair follicles. The back of the neck is a common site for boils due to its exposure to sweat and friction.
Recognizing a boil:
- Begins as a painful, pea-sized red lump
- Increases in size over several days
- Develops a white or yellow tip that may drain pus
- Surrounding skin may be red, swollen, and tender
How can you treat a boil at home. For small boils, applying a warm compress can help promote drainage. However, larger boils may require medical attention. A healthcare provider can safely drain the boil and prescribe antibiotics if necessary.
Lipomas: Benign Fatty Lumps
Lipomas are noncancerous, slow-growing fatty lumps that can appear anywhere on the body, including the back of the neck. These soft, doughy masses are typically harmless and more common in middle-aged individuals.
Characteristics of lipomas:
- Soft and easily movable under the skin
- Usually smaller than 5 cm in diameter
- Generally painless unless they contain blood vessels or press on nerves
- Can occur singularly or in multiples
Is treatment necessary for lipomas. In most cases, lipomas don’t require treatment unless they cause discomfort or grow large enough to be bothersome. If you suspect you have a lipoma, a healthcare provider can perform a biopsy to confirm the diagnosis and discuss removal options if desired.

Acne Keloidalis Nuchae: A Chronic Inflammatory Condition
Acne keloidalis nuchae is a condition characterized by inflammation of hair follicles on the back of the neck, resulting in bumps, scarring, and potential hair loss. This condition is more prevalent in dark-skinned males with thick, curly hair.
Factors that may contribute to acne keloidalis nuchae include:
- Close shaving practices
- Chronic irritation from clothing or sports equipment
- Certain medications
- Genetic predisposition
How is acne keloidalis nuchae managed. Treatment can be challenging and may involve a combination of approaches. Initial steps include avoiding close shaves and minimizing friction from clothing. If symptoms persist, a healthcare provider may recommend antibiotics, corticosteroids, or even laser hair removal in some cases.
Swollen Posterior Cervical Lymph Nodes: Your Body’s Defense System
Posterior cervical lymph nodes, located near the back of the neck, can become swollen in response to various factors. While often a sign that your immune system is fighting an infection, persistent swelling may warrant medical attention.

Common causes of swollen posterior cervical lymph nodes:
- Viral infections (e.g., common cold, flu)
- Bacterial infections (e.g., strep throat)
- Ear infections
- Dental abscesses
- Skin wounds or infections
When should you be concerned about swollen lymph nodes. While temporary swelling is often normal, seek medical advice if lymph nodes remain enlarged for more than two weeks, feel hard or fixed in place, or are accompanied by unexplained weight loss, fever, or night sweats.
Other Potential Causes of Neck Bumps
While the conditions mentioned above are common causes of bumps on the back of the neck, other possibilities exist. These may include:
- Skin tags
- Dermal cysts
- Benign tumors
- Allergic reactions
- Insect bites or stings
How can you determine the cause of a neck bump. If you’re unsure about the nature of a lump on your neck, it’s best to consult a healthcare professional. They can perform a physical examination and, if necessary, order additional tests to reach an accurate diagnosis.
When to Seek Medical Attention
While many neck bumps are harmless, certain symptoms warrant prompt medical evaluation:
- Rapid growth or change in appearance
- Persistent pain or tenderness
- Signs of infection (e.g., redness, warmth, pus)
- Difficulty swallowing or breathing
- Unexplained weight loss or fever
Can neck bumps be a sign of something serious. While rare, certain neck lumps can indicate more serious conditions, such as lymphoma or other cancers. Early detection and diagnosis are crucial in these cases, emphasizing the importance of professional medical assessment for any concerning symptoms.
Prevention and Self-Care
While not all neck bumps can be prevented, certain practices may help reduce their occurrence:
- Maintain good hygiene, especially when shaving or grooming
- Avoid tight clothing that may irritate the skin
- Stay hydrated and maintain a healthy diet to support immune function
- Manage stress, which can impact overall health and immune response
- Avoid picking or squeezing existing bumps to prevent infection
How can you care for a benign neck bump at home. For minor, non-infectious bumps, applying warm compresses, keeping the area clean, and avoiding irritation can often provide relief. However, always consult a healthcare provider if you’re unsure about the nature of a lump or if symptoms worsen.
Diagnostic Approaches for Neck Bumps
When evaluating a bump on the back of the neck, healthcare providers may employ various diagnostic techniques:
- Physical examination
- Medical history review
- Ultrasound imaging
- Fine-needle aspiration
- Biopsy
- Blood tests
What information should you provide to your healthcare provider. When discussing a neck bump with a medical professional, be prepared to share details about when you first noticed the lump, any changes in its size or appearance, associated symptoms, and any relevant medical history or lifestyle factors.
Treatment Options for Neck Bumps
Treatment for bumps on the back of the neck varies depending on the underlying cause. Some common approaches include:
- Watchful waiting for benign, asymptomatic lumps
- Antibiotics for bacterial infections
- Warm compresses to promote drainage
- Surgical removal for persistent or problematic cysts
- Corticosteroid injections to reduce inflammation
- Lifestyle modifications to prevent recurrence
How long does it take for neck bumps to resolve. The duration of treatment and recovery depends on the specific condition. Some bumps may resolve within days or weeks with proper care, while others may require ongoing management or surgical intervention.

Impact on Quality of Life
While many neck bumps are benign, they can still affect an individual’s quality of life. Potential impacts include:
- Cosmetic concerns
- Discomfort or pain
- Anxiety about the underlying cause
- Interference with daily activities
- Social self-consciousness
How can you cope with the emotional aspects of having a visible neck bump. If a neck lump is causing emotional distress, consider discussing your concerns with a healthcare provider or mental health professional. They can offer support and strategies to manage anxiety and improve self-image.
Emerging Research and Treatment Approaches
Medical understanding of neck bumps and their treatment continues to evolve. Some areas of ongoing research include:
- Improved diagnostic imaging techniques
- Minimally invasive treatment options
- Genetic factors influencing cyst and lipoma formation
- Novel therapies for chronic inflammatory conditions
- Enhanced understanding of the lymphatic system’s role in health and disease
What promising developments are on the horizon for neck bump treatment. While specific breakthroughs are difficult to predict, ongoing research aims to improve diagnostic accuracy, develop targeted treatments, and enhance our understanding of the underlying mechanisms behind various neck lumps.

Sebaceous Cyst and 6 Other Causes
A bump on the back of your neck can result from a cyst, ingrown hair, or another health condition. If it grows or occurs with other symptoms, you may want to have a doctor examine it.
It can be alarming to find a new bump anywhere on your body. While some lumps can be a cause for concern, a lump on the back of the neck or along your hairline usually isn’t anything serious. It could be anything from an ingrown hair to a swollen lymph node.
Keep reading to learn more about the possible causes and how to recognize them.
Sebaceous cysts are a common type of cyst that forms in blocked or damaged sebaceous glands. These glands secrete sebum, which is an oily substance that lubricates your skin and hair.
Sebaceous cysts feel like small, soft bumps. They’re usually found on your face, neck, or torso.
In most cases, your doctor can diagnose a sebaceous cyst just by looking at it. However, they may do some additional testing, such as a skin biopsy, if the bump:
- has a diameter larger than 5 centimeters (cm)
- shows signs of infection, such as redness, pain, or pus
- grows back quickly after being removed
While sebaceous cysts are harmless, some people prefer to remove them for cosmetic reasons. If you want to remove a sebaceous cyst, talk to your doctor. They can remove it with a minor surgical procedure.
If you want to remove a sebaceous cyst, talk to your doctor. They can remove it with a minor surgical procedure.
Ingrown hair
An ingrown hair is a strand of hair that either grows back into itself and reenters your skin or grows under your skin due to a clogged hair follicle. This results in a pimple-like bump around the hair. They’re more common in areas where you regularly remove hair by waxing, shaving, or other methods.
If have short hair, you might get ingrown hairs on the back of your neck, especially along the bottom of your hairline. You might have just one or a cluster of several.
Most ingrown hairs resolve on their own without any treatment. To avoid developing an infection, try not to squeeze or pick at an ingrown hair.
Boil
Boils (also called furuncles) are pus-filled bumps that form under the skin due to bacteria in your hair follicles. While you can have a boil anywhere, they’re common in hairy areas that are exposed to a lot of sweat and friction. This makes the back of your neck particularly vulnerable to boils.
This makes the back of your neck particularly vulnerable to boils.
Symptoms of a boil include:
- a painful, pea-sized red lump
- redness and swelling
- an increase in size over a few days
- a white or yellow tip that may drain pus
- tenderness and warmth
For small boils, you can apply a warm compress to help the boil drain. Larger boils, which can grow to be the size of a golf ball, usually need to be drained by a doctor. In some cases, your doctor might also prescribe antibiotics for more severe infections.
Lipoma
A lipoma is a noncancerous, fatty lump that grows slowly, usually between your skin and muscle. You might have one or several. Lipomas are more common in middle-aged people and usually don’t cause any health problems.
While they can grow anywhere, they tend to appear on your neck, shoulders, arms, back, abdomen, or thighs. Lipomas are usually:
- soft and doughy
- easily movable under the skin
- smaller than 5 cm in diameter, though they can grow bigger
- painful if they contain blood vessels or are large enough to put pressure on a nearby nerve
Lipomas don’t require treatment unless they start to cause pain.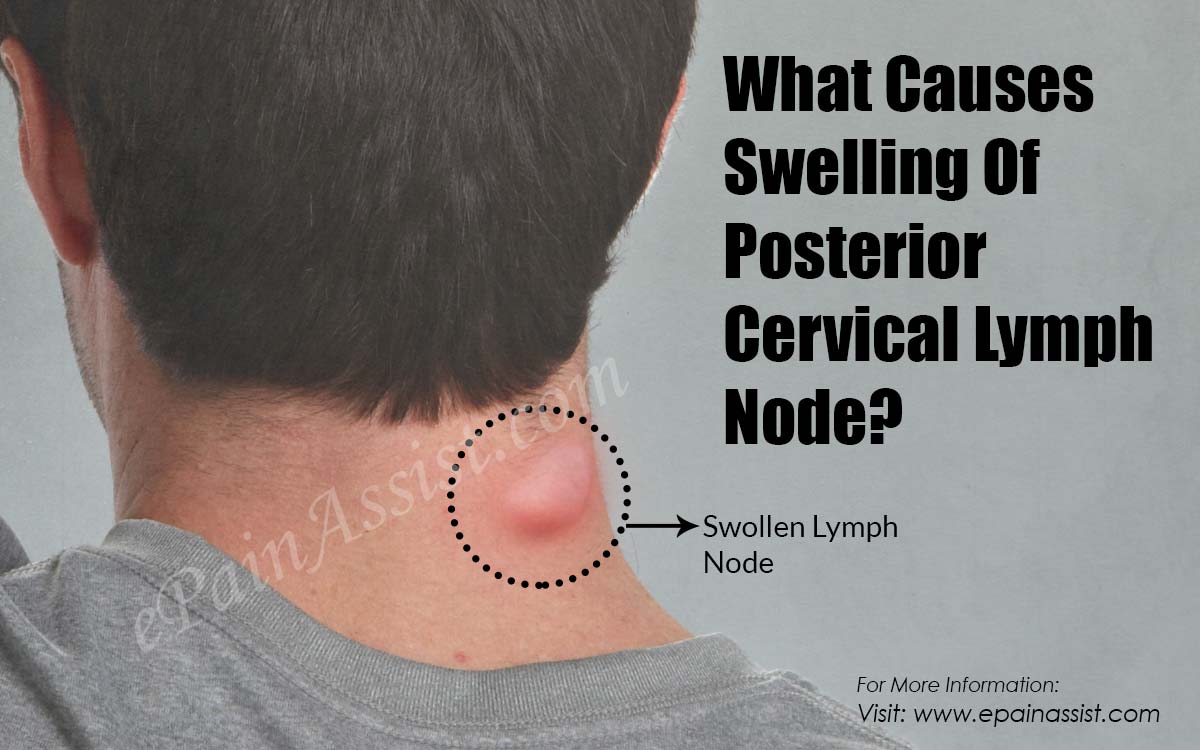 If you think you might have a lipoma, your doctor may want to do a quick biopsy to make sure it isn’t something else. They can also help you remove a lipoma, usually either with surgery or liposuction.
If you think you might have a lipoma, your doctor may want to do a quick biopsy to make sure it isn’t something else. They can also help you remove a lipoma, usually either with surgery or liposuction.
Acne keloidalis nuchae
Acne keloidalis nuchae is an inflammation of the hair follicle that causes bumps on the back of the neck, along the hairline. It begins with small, itchy bumps that eventually lead to scarring and hair loss. Over time, they turn into keloids, which are large, raised bands of scarring.
The condition is more common in dark-skinned males, particularly those with thick, curly hair. Experts aren’t sure what causes it, but it may be related to:
- close shaving
- constant irritation from sports equipment or shirt collars
- certain medications
- chronic infections
- genetic mutations
Acne keloidalis nuchae is hard to treat. Start by avoiding close shaves and making sure your shirt collar doesn’t run against the back your neck.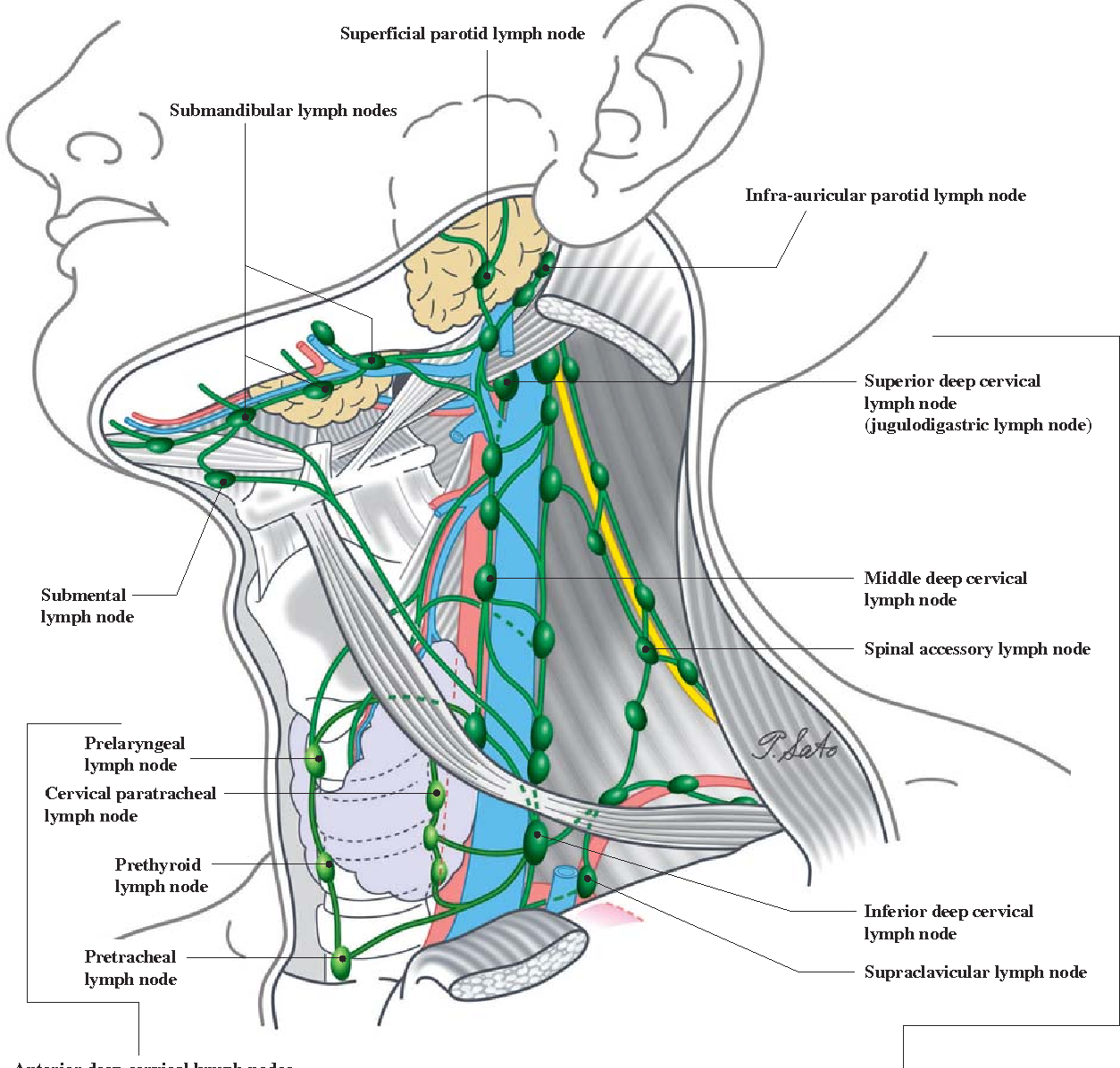 You can also try washing the area with tar soap.
You can also try washing the area with tar soap.
If keeping the area clean and free of friction doesn’t help, talk to your doctor. They might prescribe antibiotics or corticosteroids. In addition, laser hair removal or surgery can sometimes help.
Swollen posterior cervical lymph node
Your posterior cervical lymph nodes are located near the back of your neck. Several things can cause a swollen posterior cervical lymph node, but the most common cause is a viral infection, such as a cold or the flu.
Some other common causes of swollen lymph nodes include:
- strep throat
- ear infections
- abscessed tooth
- skin wounds or infections
Less common causes of swollen lymph nodes include:
- HIV
- lupus
- cancer
Depending on the underlying cause, you might also notice additional symptoms, such as:
- pain and tenderness in the lymph node
- runny nose, sore throat, and other symptoms of an upper respiratory infection
- fever
- chills
- night sweats
- multiple swollen lymph nodes throughout your body
If your swollen lymph nodes are due to an underlying infection, they should return to their usual size once the infection clears up.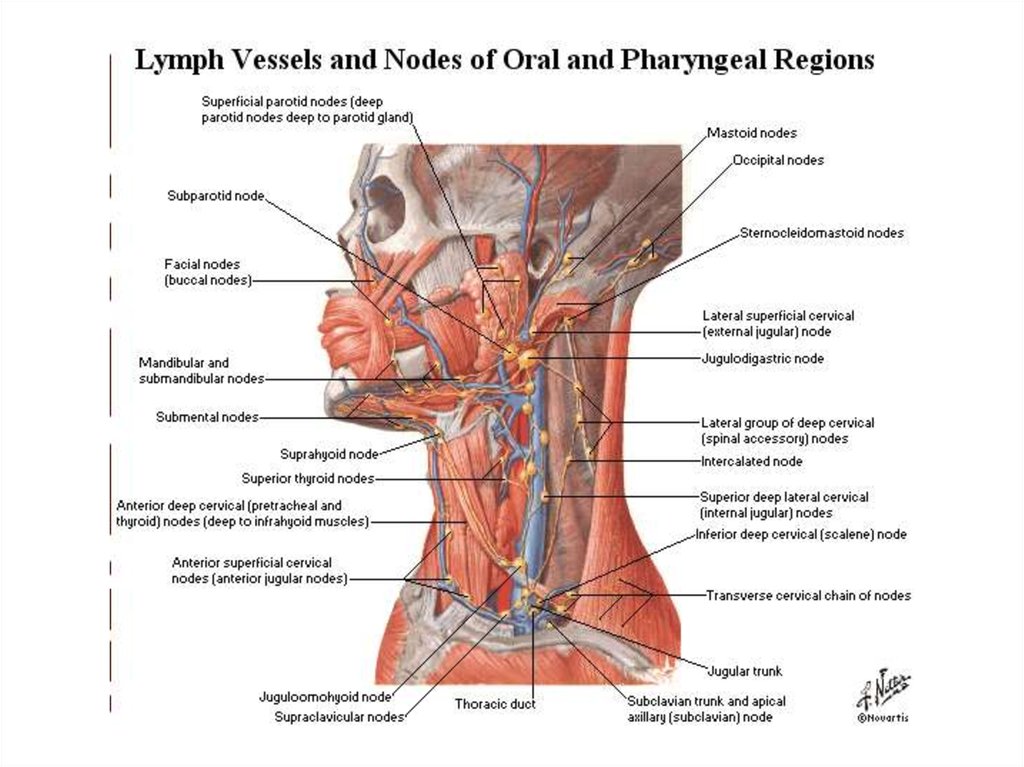 Follow up with your doctor if you can’t determine the cause or notice that the swollen node:
Follow up with your doctor if you can’t determine the cause or notice that the swollen node:
- doesn’t go away after a few weeks
- continues to grow
- is hard and not movable
- is accompanied by a fever, night sweats, and unexplained weight loss
Lymphoma
Lymphoma is a type of cancer that starts in the lymphocytes, which are your white blood cells. Swollen lymph nodes are often the first sign of lymphoma. However, according to the American Cancer Society, swollen lymph nodes are much more likely to be a sign of infection than of lymphoma.
Other symptoms of lymphoma include:
- night sweats
- fever
- fatigue
- skin itching
- rash
- unexplained weight loss
- pain when drinking alcohol
- bone pain
Most of the time, a lump on the back of the neck is harmless. However, it’s important to follow up with your doctor right away if you notice:
- symptoms of severe infection, such as an ongoing fever
- a bump that doesn’t go away after two to four weeks
- a lump that’s hard and not moveable
- a lump that grows or changes rapidly
- a lump that’s accompanied by night sweats or unintended weight loss
A lump on the back of the neck is usually not serious, and most go away without any treatment.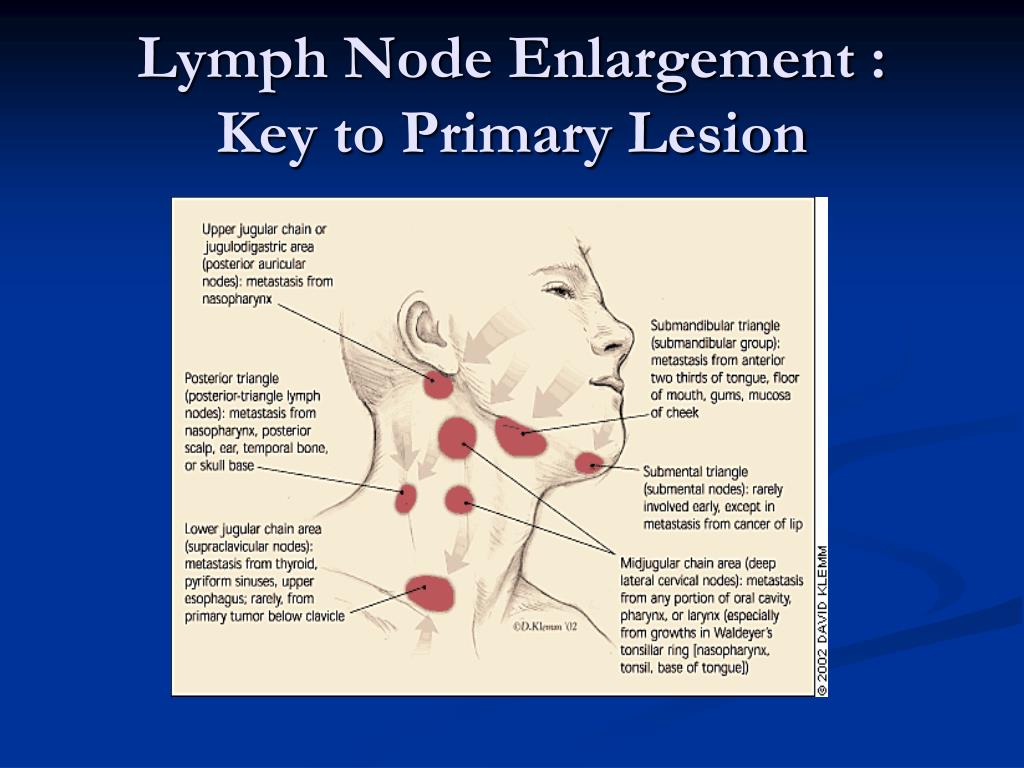 If you’re concerned or have other symptoms, talk to your doctor.
If you’re concerned or have other symptoms, talk to your doctor.
Any lump that remains longer than a couple of weeks should be examined by your doctor.
Swollen cervical lymph nodes: What does it mean?
Cervical lymph nodes are small nodes or glands in the neck. Swelling in the neck may indicate a nearby infection or other health condition.
The lymphatic system is a network of organs and tissues that helps support immunity. The lymph nodes are tiny, kidney-shaped structures that act as filters in this system. They trap and kill viruses, bacteria, and fungi before these pathogens can return to the bloodstream.
Swollen lymph nodes are usually a sign of infection but can stem from an inflammatory condition, an autoimmune disease, a reaction to a medication, or cancer. Sometimes they happen for no clear reason.
Swelling in the cervical lymph nodes may indicate a problem in the head, neck, throat, or lymphatic system.
This article outlines the potential causes of swollen cervical lymph nodes and information on treatment options and when to see a doctor.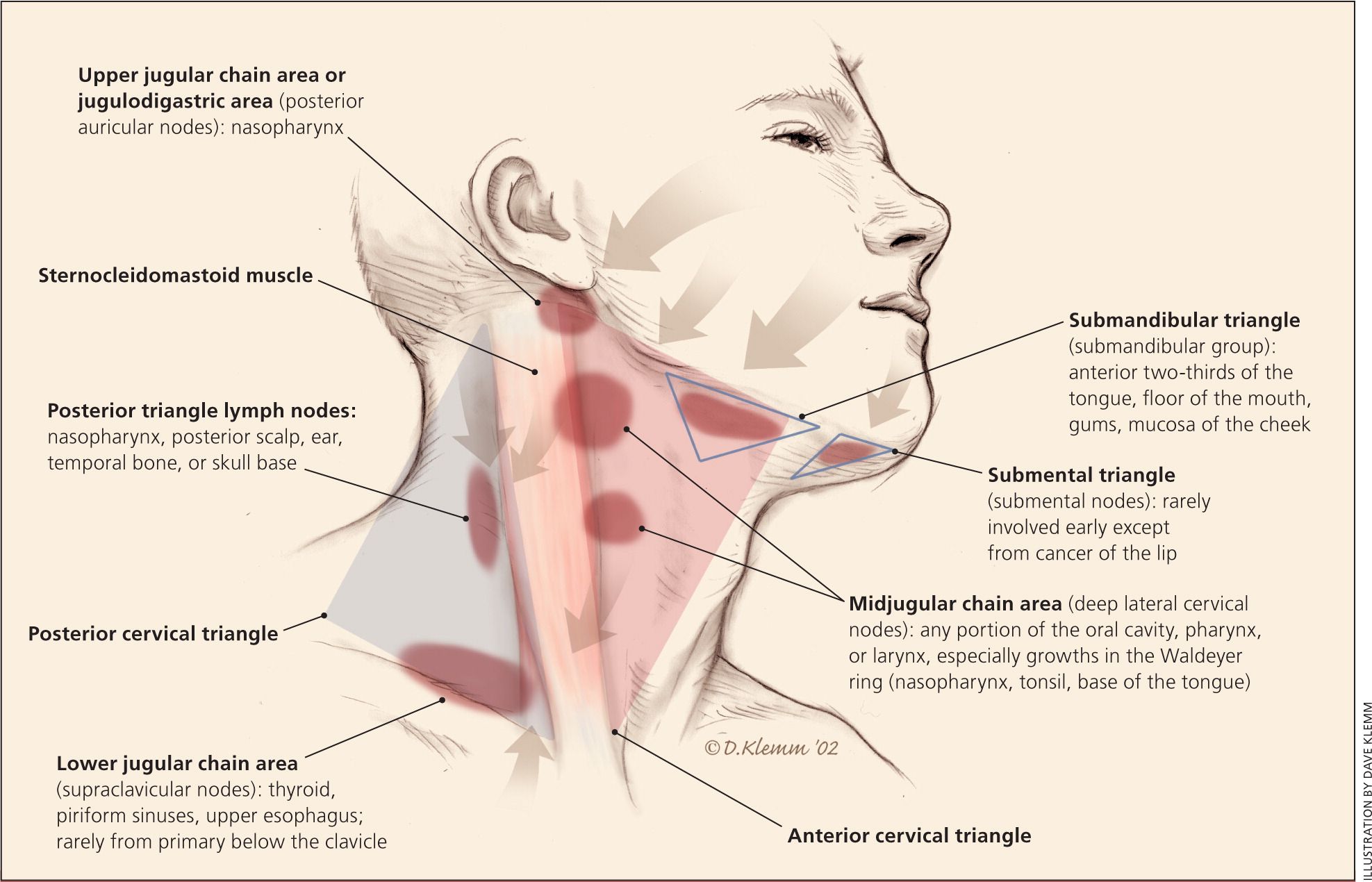
Share on PinterestCoronation Dental Specialty Group, CC BY-SA 4.0, via Wikimedia Commons
Lymph nodes are part of the immune system. They can enlarge when the system is defending the body from a nearby infection.
Cervical lymph nodes are in the front, sides, and back of the neck. They are usually smaller than 1 centimeter in diameter. If they are bigger, this could be a sign of an infection or other health problem, such as:
- an ear infection
- a dental infection
- a skin infection
- acne
- a salivary gland infection
- inflammation due to hair dye use or tight hair braids
- COVID-19
- a cold or flu
- tonsillitis
- glandular fever (mononucleosis or mono)
- some types of cancer
Lymph nodes can also become noticeable under the chin, under the arms, and around the groin, depending on where an infection occurs.
A person may or may not be able to feel if their cervical lymph nodes are swollen. However, a doctor may be able to feel one or more bumps beneath the skin when examining the neck region.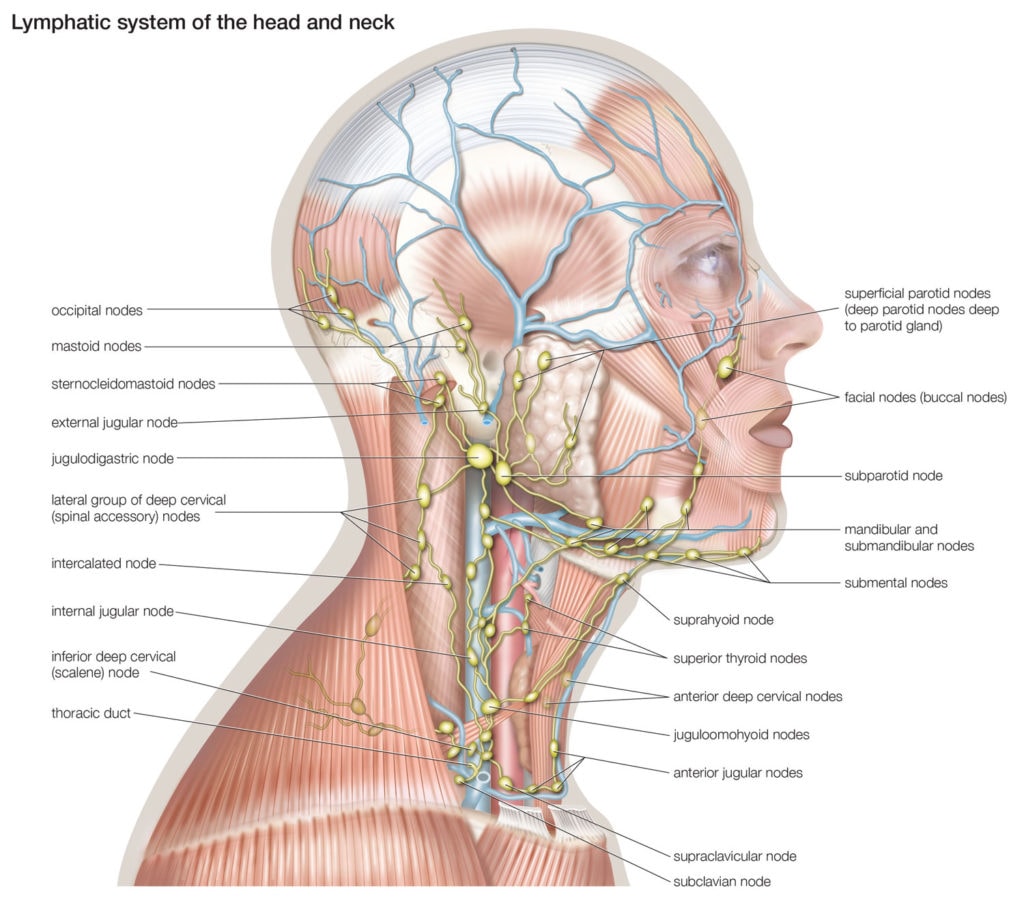
The precise symptoms that may occur with swollen lymph nodes will depend on the cause, but common symptoms of an infection include:
- fever or chills
- a general feeling of being unwell, known as malaise
- fatigue
- body aches
- pain or tenderness around the swollen nodes
Many conditions can cause swollen cervical lymph nodes, each with its own symptoms.
Here are some possible causes:
- infections
- autoimmune diseases
- inflammatory conditions
- tumors or cancer
- genetic conditions present since birth
- medication use or exposure to toxins
Here we look at some examples.
Infection
Infection is a common cause of swollen lymph nodes anywhere in the body.
When an infection occurs somewhere in the body, the lymph nodes in that area fill with white blood cells. The white blood cells then start to destroy the pathogens responsible for the infection.
The accumulation of white blood cells in the lymph nodes causes them to swell.
Some common infections that may lead to swollen cervical lymph nodes include:
- the common cold
- strep throat or tonsillitis
- ear infections
- dental infections
Additional signs of infection depend on the specific illness but may include:
- sore throat
- coughing
- earache
- fever
- fatigue
Lymph nodes that swell due to infection may be painful when a person touches them. They usually return to their usual size once the infection clears.
HIV
Swollen lymph nodes are common in the early or acute stage of HIV infection. At this stage, the body starts fighting the infection.
Research suggests the virus reaches nearby lymph nodes 3–6 days after infection. Noticeable symptoms occur in around two-thirds of people within 2–4 weeks.
They include swelling in the lymph nodes. Swelling can affect any lymph nodes but commonly occurs in the cervical lymph nodes.
A 2016 study investigated lymph node abnormalities in 100 people with HIV and swollen lymph nodes. Of the participants, 60% had swelling in the cervical lymph nodes.
Of the participants, 60% had swelling in the cervical lymph nodes.
Other symptoms of the early or acute stage of HIV include:
- sore throat
- mouth ulcers
- night sweats
- muscle aches
- fever and chills
- fatigue
- a rash
Cancer
Swollen cervical lymph nodes can sometimes be a sign of cancer.
Cancers that can cause swelling in the lymph nodes are:
- Hodgkin lymphoma, which commonly appears first in the neck and usually affects young adults
- chronic lymphocytic leukemia (CLL), a type of blood cancer that may cause swollen lymph nodes in the neck, above the collarbone, and under the arms
- non-Hodgkin lymphoma, which can develop in lymph nodes anywhere in the body and is most common among people aged 64–74 years
- other cancers, especially head and neck cancers, which can spread to the cervical lymph nodes
Other symptoms that may occur with all these conditions include:
- fever
- night sweats
- fatigue
- unexplained weight loss
The outlook for most cancers is better if a person seeks early treatment.
Medication side effects
Rarely, swollen lymph nodes can occur as a side effect of a medication. When medication is the cause, swelling may develop in any of the nodes, including the cervical lymph nodes.
Medications and toxins that can cause swollen lymph nodes include:
- allopurinol (Zyloprim), used for gout
- atenolol (Tenormin), used for blood pressure and heart disease
- captopril (Capoten), an angiotensin-converting enzyme (ACE) inhibitor used for blood pressure
- carbamazepine (Tegretol), an anti-seizure and epilepsy medication
- cephalosporins, such as cephalexin (Keflex), an antibiotic
- hydralazine (Apresoline), a blood pressure medication
- penicillin
- phenytoin (Dilantin) and primidone (Mysoline), used to manage seizures
- quinidine (Quinidex), used for some irregular heartbeats
- sulfonamides, such as sulfasalazine (Azulfidine), a disease-modifying anti-rheumatic drug (DMARD) used to treat psoriatic arthritis and other chronic inflammatory conditions
In rare cases, a chemotherapy drug known as granulocyte colony stimulating factor may also cause swelling of the lymph nodes.
What autoimmune conditions are there?
A doctor can usually detect a swollen cervical lymph node by feeling a person’s neck. They may do additional tests to find out why the swelling has occurred.
A doctor will likely ask about:
- other symptoms
- personal and family medical history
- medications used and possible exposure to toxins
- lifestyle habits
- recent travel
- recent exposure to other people who may have an infectious disease
They may also order the following diagnostic tests to find out the reason for swelling:
- blood tests
- throat culture
- CT or MRI scan
- X-rays
If necessary, the doctor may also perform a biopsy of the cervical lymph nodes to check for the presence of cancer cells.
The treatment options for swollen lymph nodes depend on the underlying cause.
Infectious causes
A swollen lymph node usually occurs as a result of infection. In such cases, the lymph node should return to its usual size once the infection has cleared.
Swollen lymph nodes typically do not require treatment unless they are painful. However, the following home remedies may help relieve discomfort:
- applying a warm compress several times per day
- taking over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs)
- getting plenty of rest
A person should see their doctor if symptoms persist or worsen despite home treatment. The doctor may prescribe antibiotics if there are signs of a bacterial infection.
HIV
A person with HIV may receive antiretroviral medications to manage the virus. These drugs reduce the amount of the virus in a person’s blood and bodily fluids.
The drugs can reduce the viral load to where it is undetectable. Then, a person will no longer be able to pass on the disease. Many people can now live long and active lives with HIV, if they receive suitable treatment.
What does it mean when HIV is undetectable?
Cancer
Cancer treatments will depend on several factors, including:
- the type of cancer a person has
- the stage of the cancer
- the person’s overall health
Possible treatment options include:
- chemotherapy
- radiation therapy
- immunotherapy
In most cases, swollen cervical lymph nodes indicate the body is fighting an infection. Infections often go away without treatment, and the node should return to its usual size once the infection clears.
Infections often go away without treatment, and the node should return to its usual size once the infection clears.
A person should seek medical advice if they experience:
- severe symptoms, such as pain, a high fever, or difficulty breathing
- swelling that lasts longer than 2 weeks
- additional symptoms, such as night sweats and a persistent fever
- swelling with no other symptoms, which may be a sign of cancer or an autoimmune disease
- a hard and painless swelling in the lymph node
- a rapid change in the size of the lymph node
- swelling in more than one area of lymph nodes, such as in the neck and the groin
Swollen cervical lymph nodes are common. In most cases, swelling is a temporary response to an infection, but it can also be a sign of a more severe underlying health condition.
A person should see their doctor if the swelling persists, worsens, or if it is causing concern. A doctor will investigate the cause and recommend a suitable course of treatment.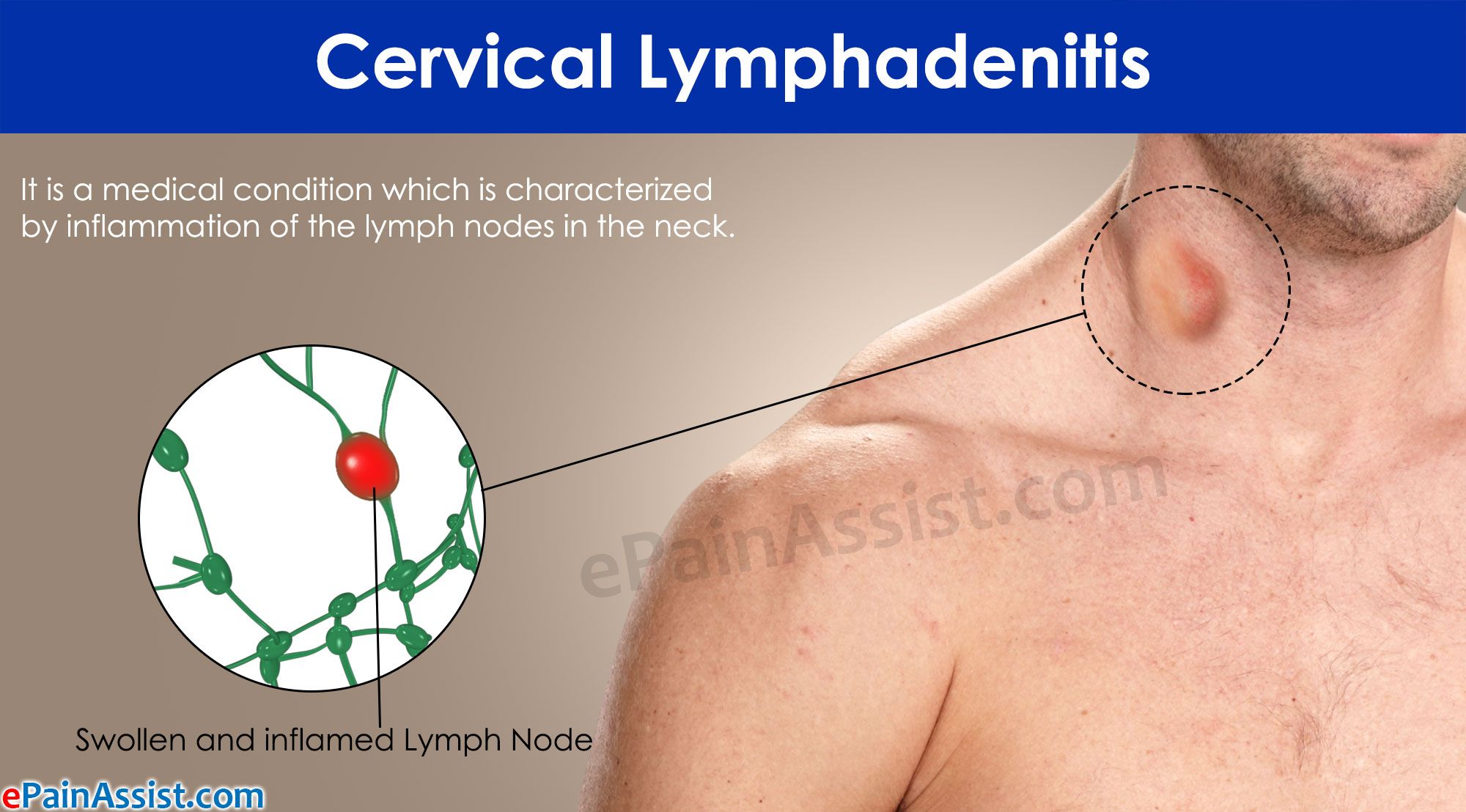
Everything you need to know about swollen lymph nodes in the neck
Introduction:
Lymph nodes are small bean-sized glands that filter the lymph that circulates through the lymphatic system. They contain white blood cells that are responsible for the immune system of the body. Therefore, the lymph nodes are an important part of the immune system. In fact, these glands trap invading microorganisms to prevent them from infecting other parts of the body. These nodes may swell as a result of infections caused by bacteria or viruses, and rarely as a result of tumors. Lymph nodes are located throughout the body, mainly on the neck, in the armpits and in the inguinal fold. They may enlarge in response to infections in the areas where they are located.
In this article, we will focus on the description of cervical lymph node enlargement or cervical lymphadenopathy, which is considered one of the most common lymphadenitis.
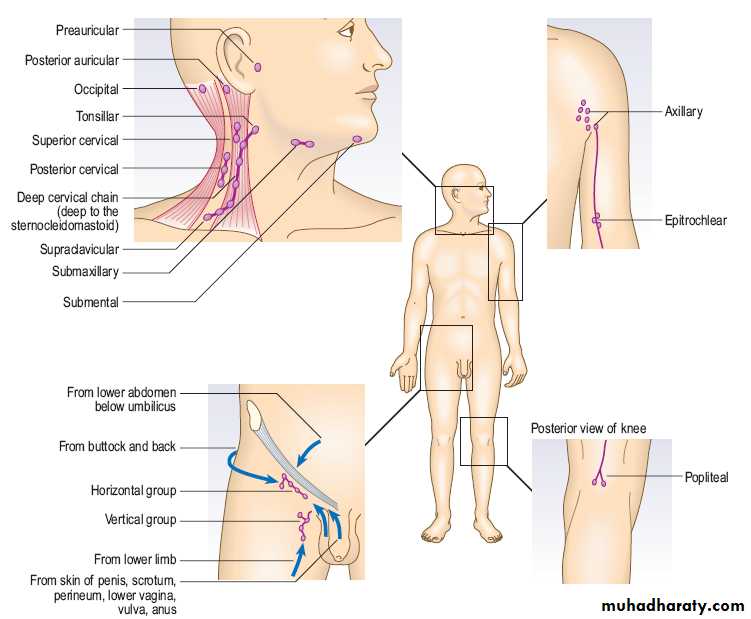
Anatomical overview
Lymph nodes collect and filter fluids, waste products, and potentially harmful pathogens. There are hundreds of lymph nodes in the human body. The following are the lymph nodes that people can see or feel:
There are hundreds of lymph nodes in the human body. The following are the lymph nodes that people can see or feel:
- Submandibular
- Neck
- Axillary
- Groin
Lymph fluid circulates throughout the body, entering and leaving the lymph nodes before returning to the chest. At the same time, the lymph nodes trap and neutralize dangerous pathogens (microbes, viruses, and waste products of the body). The lymph nodes filter the fluid and return it to the bloodstream along with essential salts and proteins.
Lymph nodes also contain immune cells that help fight disease by destroying bacteria that have accumulated in the body’s lymphatic fluid. When a person becomes ill with an acute infection, the lymph nodes may swell. The swelling is caused by the activation of immune cells in the lymph nodes.
The location of the swelling is often associated with the affected area. An ear infection, for example, can lead to swollen lymph nodes in the ear, and an upper respiratory infection can lead to swollen lymph nodes in the neck.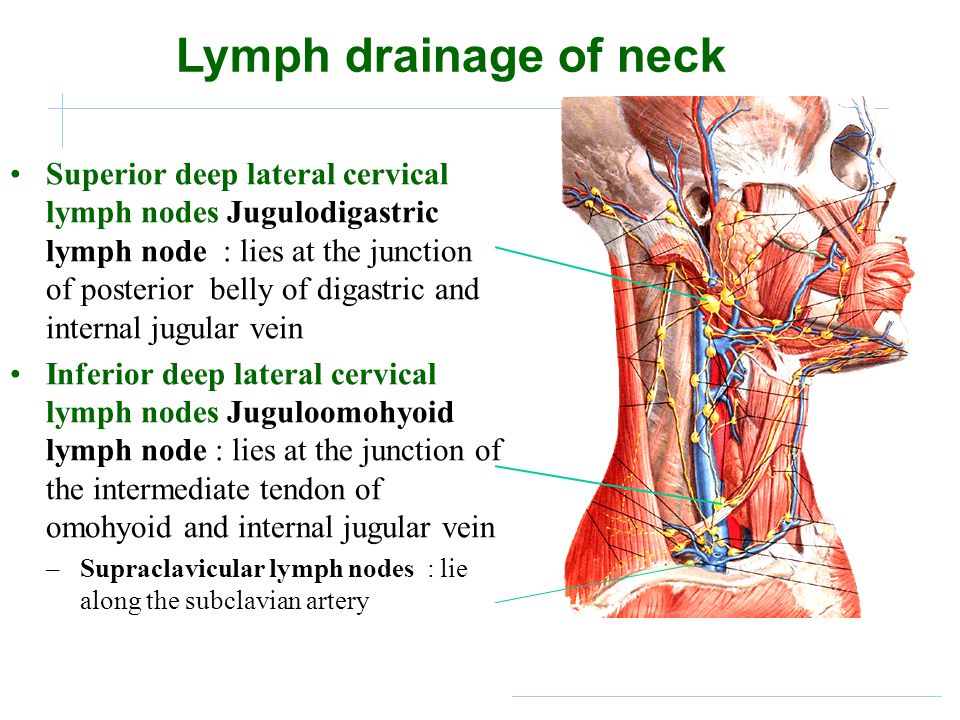
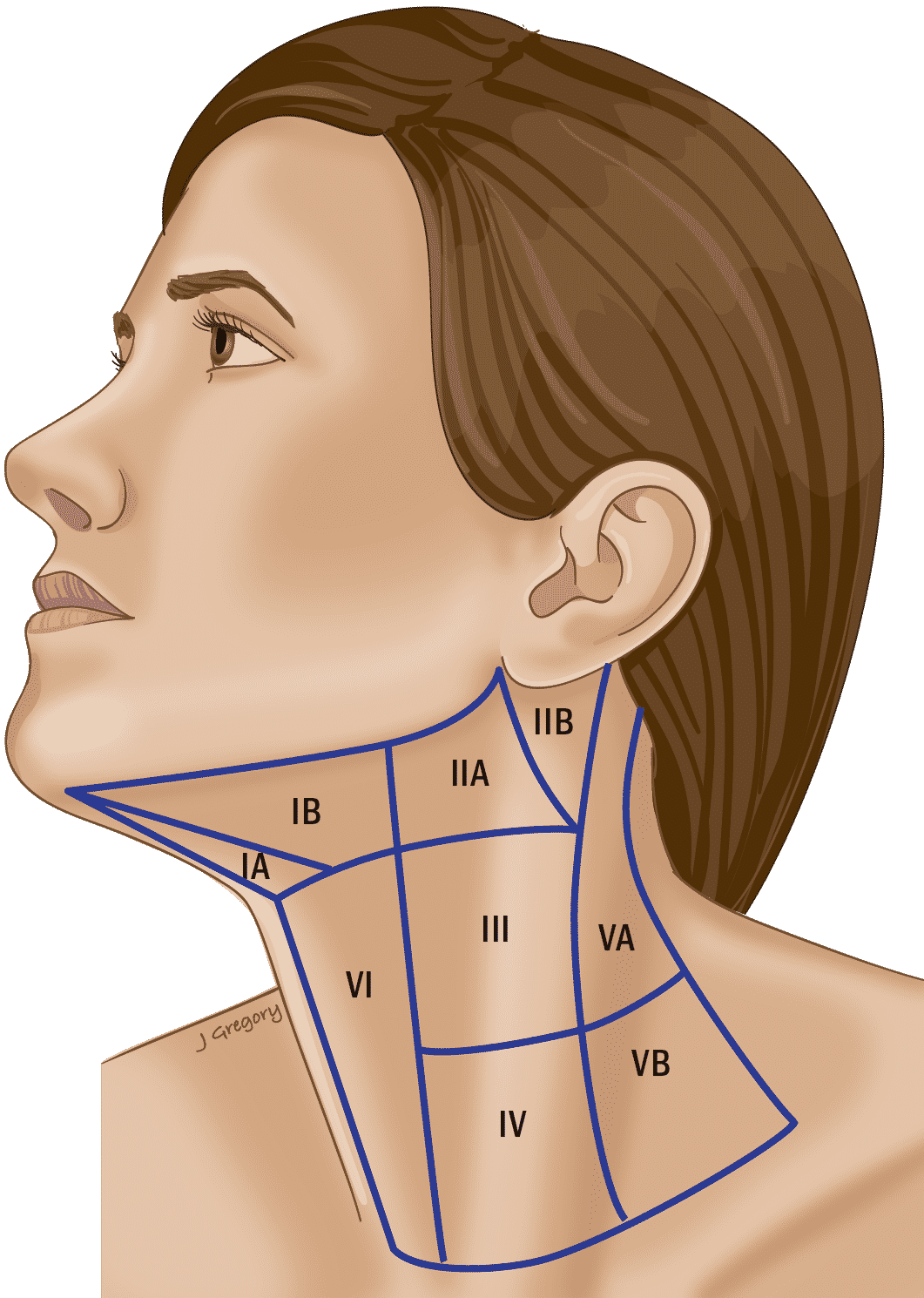
Cervical lymph node (N) classification
Level IA: Submental region
These lymph nodes are located within the triangle formed by the anterior belly of the digastric muscles (on both sides) and the hyoid bone on the underside.
Level IB: Submandibular region
These nodes are located within the triangle formed by the anterior and posterior bellies of the digastric muscle on the lower side and the mandibular body on the upper side. It should be emphasized that when the LN is excised at this level, the submandibular gland must be included in the resected material.
Level IIA and IIB: Superior jugular group
These are the lymph nodes that surround the superior part of the internal jugular vein (IJV). They expand from the base of the skull upward to the level of the lower edge of the hyoid bone downward. In front, it borders on the lateral edges of the sternohyoid and stylohyoid muscles. Behind, they are limited by the posterior edge of the sternocleidomastoid muscle.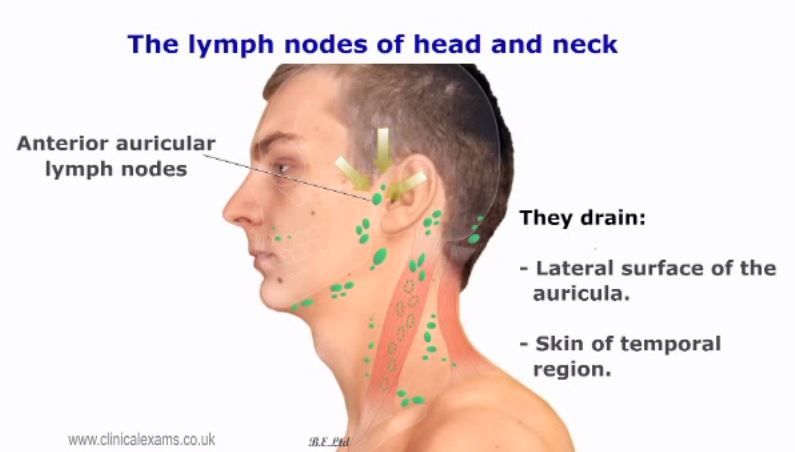
Level IIA LNs are located anterior to the vertical plane of the spinal accessory nerve, while level IIB LNs are located posterior to this plane. The vertical plane in the posterior submandibular gland radiographically separates the level IB and level IIA LNs.
Level III: Middle jugular group
These lymph nodes are located in the middle third of the VJV and extend from the lower edge of the hyoid bone above to the lower edge of the cricoid cartilage below. The anterior border is also represented by the lateral border of the sternohyoid muscle, and the posterior border is represented by the posterior border of the sternocleidomastoid muscle. This category includes the jugular-hyoid LN.
Level IV: Inferior jugular group
These LNs run from the lower edge of the cricoid cartilage to the clavicle and are located around the lower third of the VJV. This group borders anteriorly on the lateral border of the sternohyoid muscle and posteriorly on the posterior edge of the sternocleidomastoid muscle.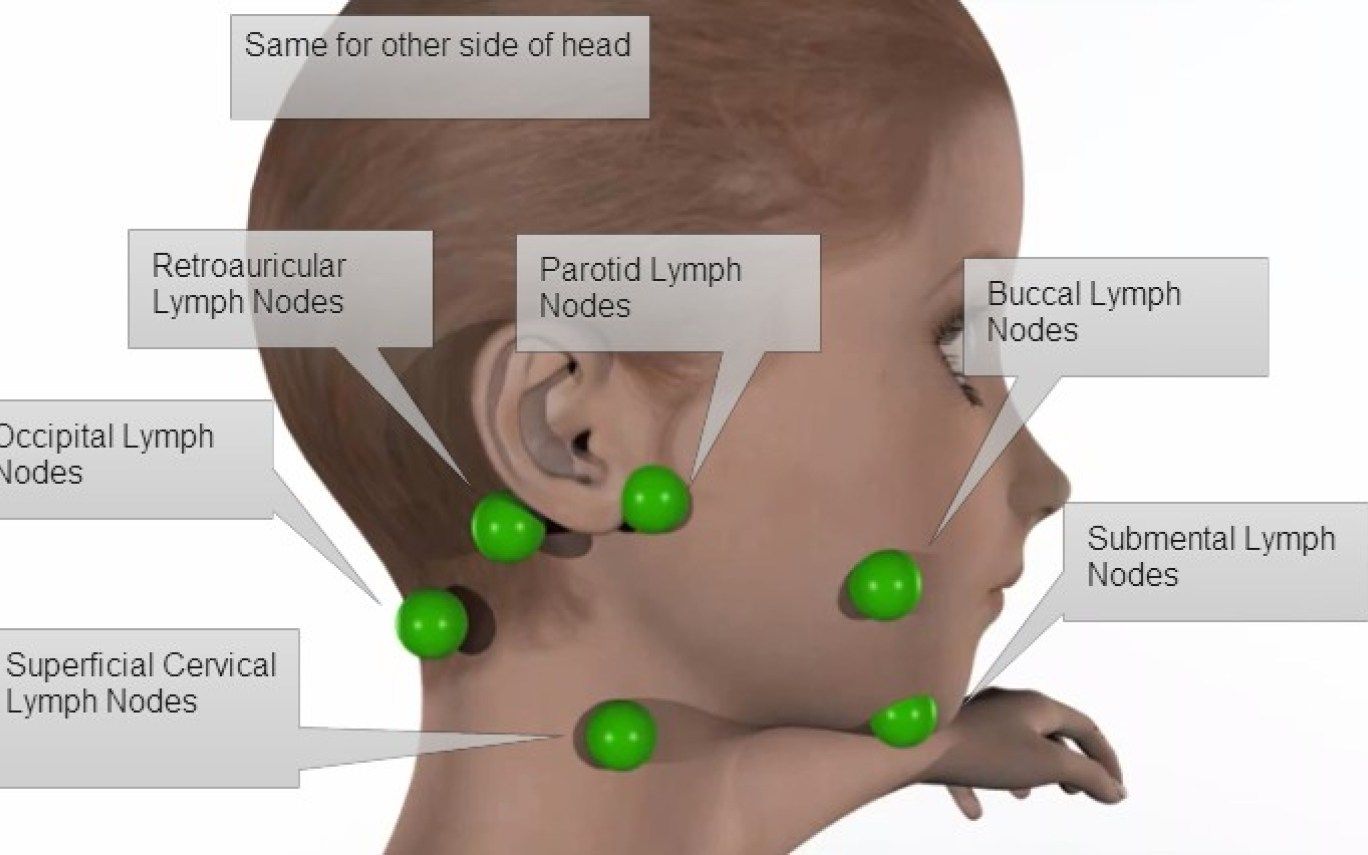 It should be noted that the Virchow lymph node falls into this category.
It should be noted that the Virchow lymph node falls into this category.
Levels VA and VB: Posterior triangle group
The upper limit of this group is defined by the convergence of the trapezius and sternocleidomastoid muscles, and the lower limit is formed by the clavicle. The anterior border is defined by the posterior border of the sternocleidomastoid muscle, and the posterior border is formed by the anterior border of the trapezius muscle.
The VA and VB lymph nodes are separated by an imaginary horizontal plane that marks the inferior border of the cricoid cartilage. VA nodes contain spinal accessory nodes, while VB nodes include nodes around the transverse cervical vessels and supraclavicular nodes.
Level VI: Central Sector Group
This level contains the pretracheal, paratracheal, precricoid (Delphic), and perithyroid nodes (including the nodes along the recurrent laryngeal nerves). This region extends from the hyoid bone above to the suprasternal notch below.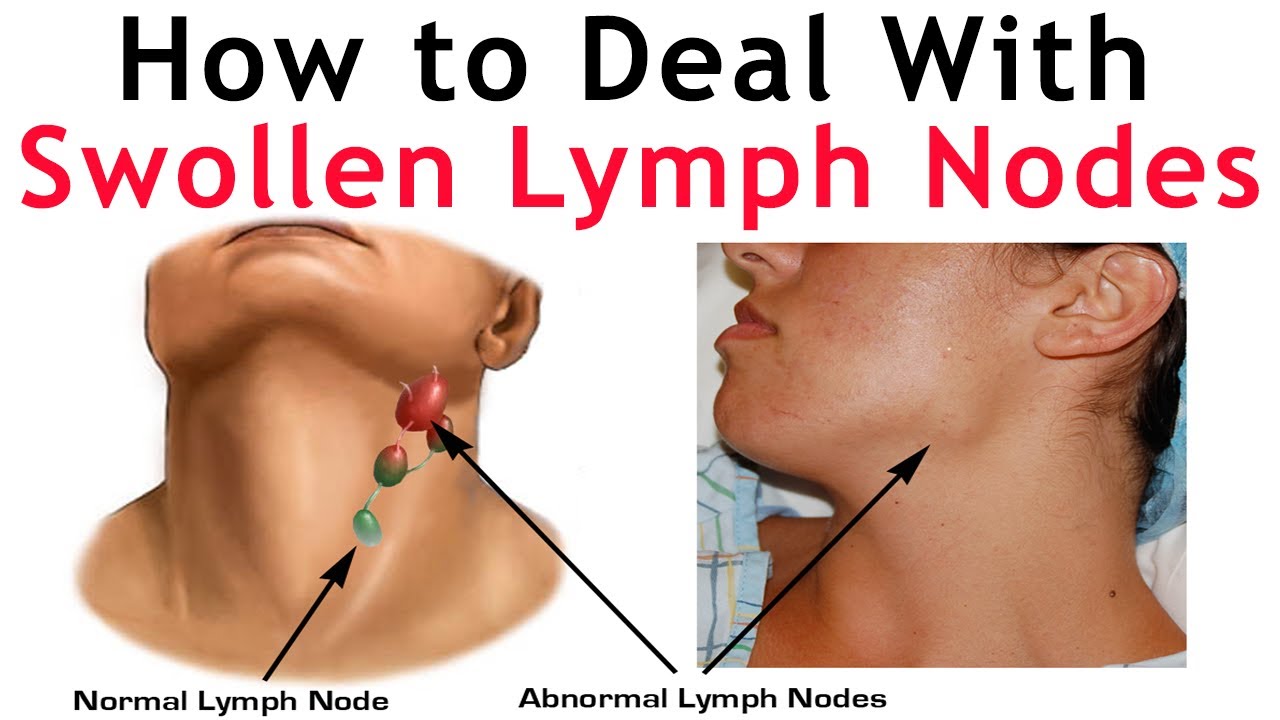 Laterally, it is bounded by the common carotid arteries (CCA).
Laterally, it is bounded by the common carotid arteries (CCA).
Pathophysiology
Lymph nodes are part of the reticuloendothelial system, which also includes blood monocytes, connective tissue macrophages, thymus, spleen, bone marrow, bones, lymphoid tissue associated with the mucous membrane of the internal organs, lymphatic veins and lymphatic fluid located in the interstitial fluid.
Lymph fluid circulates throughout the lymphatic system, passing from the organs through the lymph capillaries, lymph arteries, and eventually the lymph nodes to filter foreign agents. Foreign substances are absorbed by lymphoid cells, causing them to proliferate and expand. Cellular growth in lymphoid follicles can be seen under the microscope as multiple mitotic figures. Patients may develop local tenderness as the lymph nodes expand as a result of the increased load.
B cell development begins with bone marrow pluripotent stem cells. B cells that efficiently construct their immunoglobulin heavy chains move to germinal centers, providing antibody diversity through somatic hypermutation.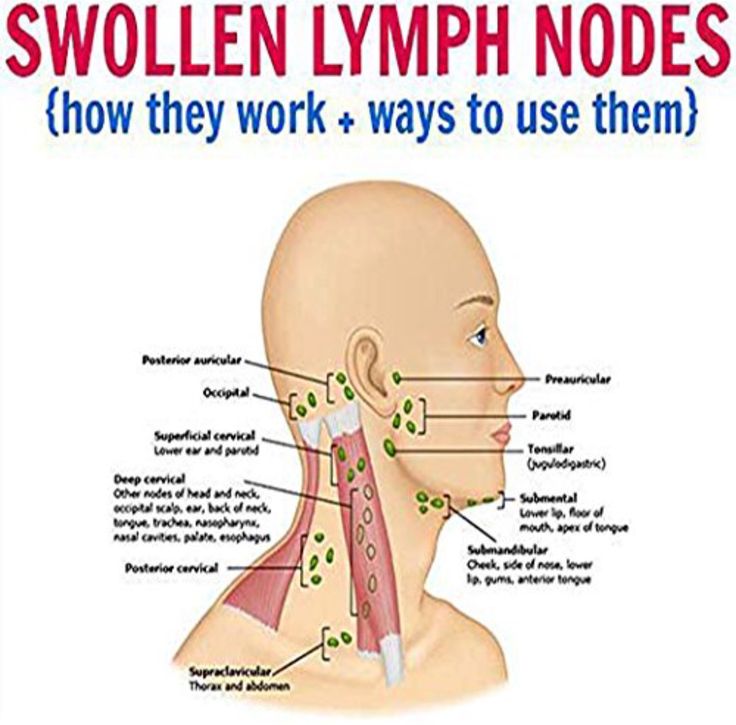 B-cell lymphomas are thought to be caused by somatic hypermutation changes and chromosomal translocations.
B-cell lymphomas are thought to be caused by somatic hypermutation changes and chromosomal translocations.
T-cell development also begins with pluripotent stem cells that mature in the thymus cortex. T cells initiate certain rearrangements in the T cell receptor while in the thymus cortex. T cell lymphogenesis is believed to be induced by chromosomal translocations at the level of T cell receptors.
Lymph node follicle necrosis can develop as a result of various diseases, including inflammatory, infectious, and malignant diseases. A predominance of neutrophilic infiltrates indicates a bacterial disease, while a predominance of lymphocytic infiltrates may indicate a viral infection. However, physicians should keep in mind that the etiology of lymph node enlargement varies; lymphomas, leukemias, tuberculosis, or even systemic lupus may be an appropriate diagnosis in certain clinical settings.
What causes swollen lymph nodes in the neck?
Swollen lymph nodes in the neck are usually a sign that your immune system is fighting to protect your body from illness caused by a foreign agent such as a virus, parasite, or bacterium. Swollen cervical lymph nodes are usually caused by conditions that affect organs near the neck, such as an infected tooth, colds, flu, tonsillitis, ear or throat infections, angina, and cellulitis.
Swollen cervical lymph nodes are usually caused by conditions that affect organs near the neck, such as an infected tooth, colds, flu, tonsillitis, ear or throat infections, angina, and cellulitis.
Various conditions can cause swollen lymph nodes in the neck:
Viral infections:
The most common cause is:
- Viral infection of the upper respiratory tract, such as a cold or flu
- Human immunodeficiency virus: HIV
- Herpes simplex virus
- Adenovirus
- Epstein Barr virus mononucleosis
- Cytomegalovirus
Bacterial infections:
- Streptococcal infection of the oropharynx due to streptococcus
- Tuberculosis
- Staphylococcus
- Syphilis (sexually transmitted infection)
- Cat scratch disease
Parasitic infections:
- Toxoplasmosis
- Leishmaniasis
More serious conditions can also lead to swollen lymph nodes throughout the body.
Autoimmune diseases:
- Systemic lupus erythematosus
- Rheumatoid arthritis
Cancers:
Swollen lymph nodes in the neck can sometimes be a sign of cancer that has spread to the lymph glands:
- Non-Hodgkin’s lymphoma
- Leukemia
- Lung cancer
- Metastatic cancer
Cancer is suspected if an enlarged cervical lymph node does not shrink for a long time or enlarges over time, is painless, and has difficulty moving. A competent doctor will help to make the correct diagnosis.
Sometimes some medications can cause swollen lymph nodes in the neck, including immunization against typhoid fever.
What are the symptoms of swollen neck lymph nodes?
Symptoms are widely varied and often associated with the underlying disease causing enlargement of the cervical lymph nodes:
- Localized pain
- High temperature
- Increased swelling
- Temperature increase in affected area
- Weakness
- Difficulty swallowing, breathing or moving
- Night sweats
- Fatigue
All aspects of a complete history and a thorough physical examination must be kept in mind at all times. The following history events should be noted:
The following history events should be noted:
- Case history: location, pain – if yes, intensity, quality, onset, precipitating factors, mitigating factors
- Medical history: It is critical to understand the patient’s past medical history as this may provide insight into the cause of the lymphadenopathy (eg, HIV/AIDS, distant history of non-Hodgkin’s lymphoma).
- Drugs: Some drugs may cause reversible lymphadenopathy (eg, cephalosporins, phenytoin)
- Social history : Important to understand living conditions, toxic exposure, alcohol, cigarette and recreational drug use, pet ownership, contact with animals, and recent travel.
- Sexual history: Need to know the number of sexual partners, whether they are sexually active with men, women, or both; use of protective equipment, history of sexually transmitted infections, and partners who knew about sexually transmitted diseases.

- Surgical history: Find out what procedures were performed and when they occurred, as well as how quickly lymphadenopathy (i.e., postoperative lymphadenopathy) developed
- Family history: It is very important to determine if there is a family history of cancer.
Physical examination includes the following:
- Vital signs: temperature, blood pressure, heart rate, respiratory rate, and oxygen saturation are important in determining whether the patient is hemodynamically stable. This can help distinguish sepsis from other illnesses.
- A complete physical examination is required , including examination of the head, ears, nose, throat, and thyroid gland. Auscultation of the lungs and heart, as well as palpation for splenomegaly and hepatomegaly. A thorough examination of the skin, including palpation where necessary, should be performed to look for rashes, lesions, and nodules.

- When palpating lymphadenopathy, be aware of location, size, stiffness, and discomfort.
Location:
- The sternocleidomastoid muscle is located above and below the anterior cervical lymph nodes. Lymph nodes in the posterior cervical region are located behind the sternocleidomastoid muscle.
- In addition, check bilaterally for supraclavicular, axillary, and inguinal lymphadenopathy.
- Local lymphadenopathy means more limited disease than extensive lymphadenopathy.
- Size:
- Cervical and axillary lymph nodes are rarely larger than 1 cm; supraclavicular nodes are rarely larger than 0.5 cm, and inguinal nodes are rarely larger than 1.5 cm.
- Hardness:
- In general, a mobile lymph node is less likely to be malignant.
- Pain:
- Pain may be a sign of inflammation or an acute reaction to an infection, but is rarely associated with malignancy.

However, sometimes an enlarged lymph node in the neck can also be asymptomatic with no symptoms other than swelling.
How is an enlarged cervical lymph node diagnosed?
In addition to the medical history and an accurate physical examination, the doctor will evaluate the characteristics of the node:
- Its size is
- Its consistency is
- Soreness
- Cohesion with surrounding tissues
- Form
- Softness
- Temperature
- Texture
You must disclose all the details to your doctor in order to get the best results: Have you recently been scratched by a cat or dog? Do you eat undercooked meat? Have you traveled recently? Have you had risky sexual behavior? An honest answer to all these questions is an important step in quickly determining the correct diagnosis. Also, some additional tests may be needed to help determine the cause:
- Blood tests: help assess your general health and detect some hidden diseases
- Imaging studies: e.
 g. x-ray and ultrasound scans to help detect tumors or sources of infection
g. x-ray and ultrasound scans to help detect tumors or sources of infection - Biopsy: a biopsy may be required to confirm or exclude the diagnosis. It involves making a small incision and taking a small sample from a swollen lymph node in the neck to be examined microscopically in a laboratory.
How to detect an enlarged neck lymph node?
You can find a swollen lymph node in your neck yourself.
Here are some simple and easy steps you can follow:
- Feel the lymph node by rubbing in a circular motion with your fingertips
- Gently press on the neck
- Compare lymph nodes on both sides of the neck
If you have an enlarged lymph node, you can easily find it because swollen lymph nodes in the neck feel larger than usual, soft to the touch, sometimes sore and warm, which are signs of inflammation. You may also feel pain when making sudden movements. Some common symptoms can bring out these swollen nodes.
How often should we check the lymph nodes in the neck?
It is recommended to check the lymph nodes once a month to detect asymptomatic enlarged lymph nodes in the neck at an early stage.
Treatment of enlarged lymph nodes
There is no special kit for the treatment of enlarged lymph nodes in the neck. It all depends on the underlying cause. If a swollen cervical lymph node is not a serious disease, then it will disappear on its own in a few days even without any treatment. You can take certain medications to relieve certain symptoms, such as fever and pain relievers, if necessary. Don’t forget to rest well, it can help.
If a swollen cervical lymph node is caused by a bacterial or viral infection, your doctor will prescribe antibiotics or antivirals to treat it. When the infectious agent is eliminated, the enlarged lymph node returns to its normal size.
When the cause of a swollen cervical lymph node is a tumor, your doctor will decide the best treatment for you by removing the entire node using radiation therapy, chemotherapy, or a combination of treatments.
Complications of swollen cervical lymph nodes
As already explained, a swollen cervical lymph node may be a normal response of the body to disease.
In many cases, it usually decreases on its own within a few weeks. However, the neck node can remain enlarged even after the disease has been treated, and this chronically swollen lymph node in the neck leads to a number of complications. These complications depend on the cause of the swollen cervical lymph node.
For example, if the cause is infectious and the cervical lymphadenopathy is left untreated, an abscess, which is a collection of pus under the skin, can develop, which can become a serious problem requiring surgical treatment. Otherwise, a neglected inflamed lymph node in the neck can spread the infection into the bloodstream, causing septicemia, which is a life-threatening condition.
Differential Diagnosis
Due to the variety of causes of lymphadenopathy, doctors often face diagnostic difficulties.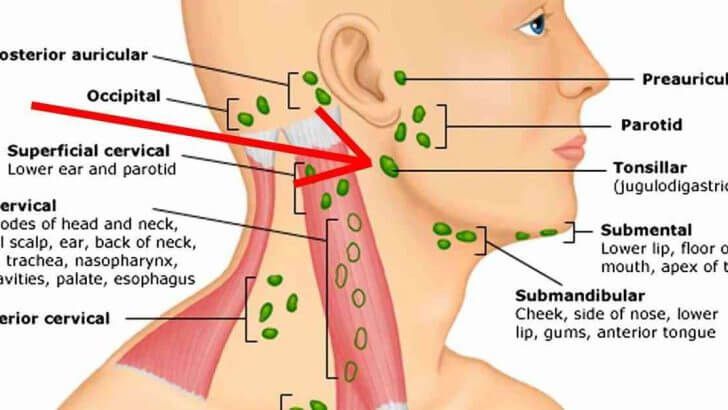 To eliminate confusion and improve diagnostic accuracy, collect a complete history and physical findings, develop a set of differential diagnoses, and categorize them based on their presentation.
To eliminate confusion and improve diagnostic accuracy, collect a complete history and physical findings, develop a set of differential diagnoses, and categorize them based on their presentation.
Causes of lymphadenopathy:
- Malignant: Lymphadenopathy may be worrisome in diagnoses such as metastatic breast cancer, Kaposi’s sarcoma, leukemia, lymphoma, metastatic disease (eg, stomach cancer), and skin malignancies if history and physical examination match.
- Autoimmune: Certain immune-mediated diseases such as dermatomyositis, Kawasaki disease, rheumatoid arthritis, sarcoidosis, Sjögren’s syndrome, Still’s disease, and systemic lupus erythematosus can cause lymph node abnormalities.
- Infectious: Various infections can cause benign changes in the lymph nodes. Many types of infections, such as bacterial, viral, and others, may be considered by healthcare professionals:
- Bacterial diseases include brucellosis, cat-scratch disease, bacterial pharyngitis, syphilis, tuberculosis, tularemia, and typhoid fever.

- Cytomegalovirus, hepatitis, herpes simplex, HIV, mononucleosis, rubella, viral pharyngitis are all viral infections.
- Drugs: Drug treatment can often cause benign lymph node enlargement. Allopurinol, atenolol, captopril, carbamazepine, cephalosporins, gold preparations, hydralazine, penicillin, phenytoin, primidone, pyrimethamine, quinidine, sulfonamides and sulindac are examples of these drugs
When should you see a doctor if you have an enlarged lymph node in your neck?
It’s time to seek medical help if:
- Nodules suddenly swollen for no apparent reason
- Nodules remain enlarged for more than two weeks
- You have difficulty breathing or swallowing
- You have a persistent high fever and night sweats
- You have unexplained weight loss or loss of appetite
- Swollen neck lymph node gets larger over time
- Swollen lymph node, painful or difficult to move
If you notice one or more of these symptoms, contact your doctor as soon as possible. You can start by visiting your primary care physician, who can diagnose your problems by discussing your symptoms, doing a physical examination and possibly some biological tests to evaluate your case and either prescribe treatment or refer you to a specialist (hematologist, infectious disease specialist, oncologist). or surgeon), depending on the cause of the enlarged cervical lymph node.
You can start by visiting your primary care physician, who can diagnose your problems by discussing your symptoms, doing a physical examination and possibly some biological tests to evaluate your case and either prescribe treatment or refer you to a specialist (hematologist, infectious disease specialist, oncologist). or surgeon), depending on the cause of the enlarged cervical lymph node.
Prognosis
- Swollen lymph nodes in young people (eg children) are often benign and associated with infection. There are a few exceptions to the norm, especially if the patient’s history and physical findings suggest persistent infection, cancer, or autoimmune disorders.
- Other risk factors that may be poor prognostic indicators include older age, duration of lymphadenopathy (> 4 weeks), widespread lymphadenopathy, male sex, no reduction in node size, and systemic features such as fever, night sweats, weight loss, and hepatosplenomegaly .
Prevention of swollen lymph nodes
The only way to avoid swollen lymph nodes is to avoid situations that can lead to them. Here are some things you can do:
Here are some things you can do:
- Maintain good oral hygiene to keep your teeth and gums healthy.
- Wash your hands frequently.
- Get immunized against diseases such as shingles, tuberculosis, and influenza.
- Avoid sharing food, drink, or personal items such as towels with someone who has an infectious virus-like illness or a cold.
- Use condoms or other barrier methods during intercourse.
- If you have an adverse or allergic reaction to medicines, talk to your doctor.
- Do not let your indoor cats play outside and do not let them come into contact with feral cats.
Summary:
Swollen cervical lymph nodes is one of the most common lymphadenitis. They usually appear as a reaction of the body to various conditions, such as an infection. It is a symptom, not a disease. Enlarged lymph nodes in the neck tend to disappear spontaneously within a short period of time and without any treatment.
However, it is important to see a doctor to diagnose the cause and decide if you need treatment, especially when you experience some specific symptoms such as persistent high fever, difficulty swallowing or breathing, and night sweats. Only identifying the exact cause of a swollen neck lymph node can help determine the right treatment.
Inflammation of the lymph nodes in the neck in children
Lymphadenitis in children is an inflammatory process that affects one or several lymph nodes at the same time, which may occur against the background of an infection. In most cases, such a disease occurs in children due to a weak immune system. Often, pathology is diagnosed at a dentist’s appointment – approximately in 5-7% of cases. Up to five years, the lymph node in the child’s neck can be inflamed due to SARS, infection in the tonsils, ear, and in older children – due to foci of purulent inflammation at the roots of the teeth.
Approximately 40% of cases of lymphadenitis in children are not diagnosed in a timely manner.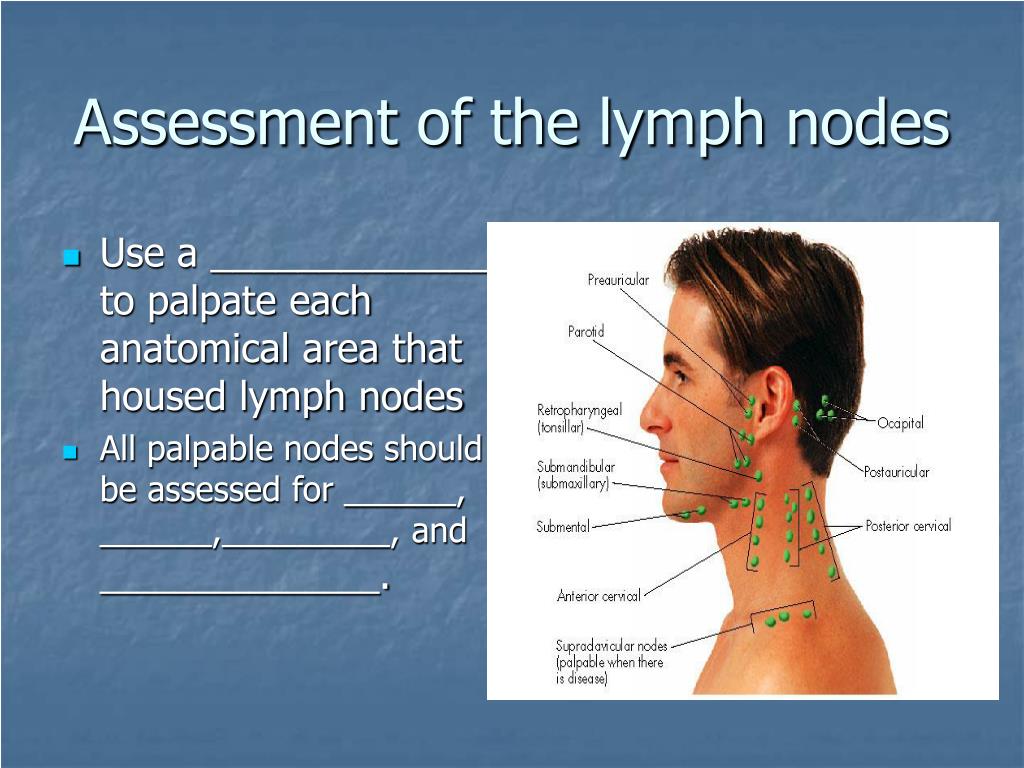 This is usually due to the lack of experience of doctors in the treatment of this pathology. In adults, the disease is less common than in children, but the causes of its occurrence are similar.
This is usually due to the lack of experience of doctors in the treatment of this pathology. In adults, the disease is less common than in children, but the causes of its occurrence are similar.
Normal lymph nodes
Lymph nodes of a healthy person have the following features:
- Diameter – no more than 5 mm.
- Lack of connection with other lymph nodes, with skin.
- Loose structure.
- No discomfort when pressed.
- Mobility.
How to correctly estimate the size of the lymph nodes?
Parents should regularly carefully palpate the lymph nodes in the child’s neck to correctly assess size. In some cases, the increase can be so strong that it becomes noticeable even externally – a “bump” is visible on the skin. In addition, lymphadenitis in children is often accompanied by pain, so they independently indicate to their parents the area that bothers them.
Note that it is not recommended to palpate the lymph nodes too often (more than 2 times a day) – this can provoke an aggravation of the condition.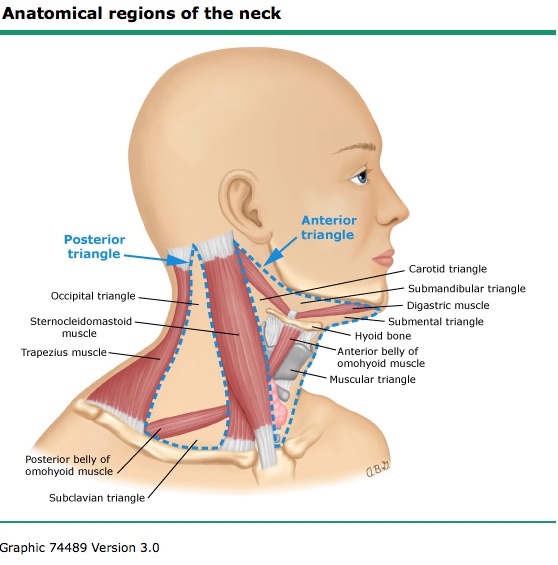
Causes of enlargement and main groups of lymph nodes
| Group of lymph nodes | Most common causes of enlargement |
|---|---|
| Parotid | Development of inflammation of the scalp associated with pus, inflammation of the middle or external ear, pediculosis, eczema, dermatitis |
| Occipital | Pathology in the scalp, rubella, fungus |
| Chin | Inflammation in the region of the lower lip, stomatitis, gingival lesions in the region of the anterior teeth, jaw abscess |
| Submandibular | Dental disease, stomatitis |
| Neck (in the area of the muscles in the back of the neck) | Angina, tonsillitis, tonsillitis, adenoids, infectious mononucleosis |
| Neck (middle) | Scarlet fever, angina, cat-scratch disease, lymphoma, toxoplasmosis |
| Neck (side) | Tumors, tuberculosis of the lymph nodes, infections in the nasopharynx |
| Elbow | Infections in the forearm, hand |
| Axillary | Shoulder or arm infections, vaccine reaction, cat-scratch disease |
| Crotch | Infections of the skin, bones and muscles of the legs, dermatitis, inflammatory process in the genital organs, reaction to the vaccine that was injected into the femoral area |
Symptoms
Inflammation of the lymph nodes in the neck in children is usually easily visible visually.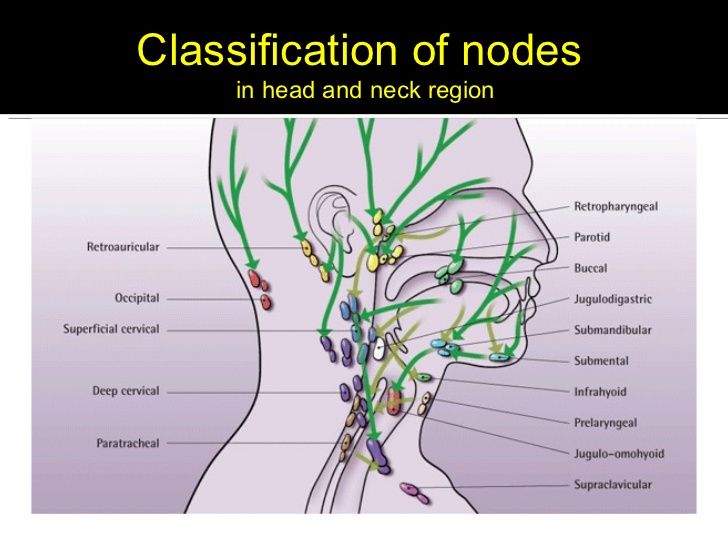 They increase significantly and are felt on palpation. In addition, the lymph node acquires an altered structure. In the case of inflammation, it becomes denser, and with suppuration, its consistency, on the contrary, becomes too soft, pain is felt on palpation.
They increase significantly and are felt on palpation. In addition, the lymph node acquires an altered structure. In the case of inflammation, it becomes denser, and with suppuration, its consistency, on the contrary, becomes too soft, pain is felt on palpation.
An enlarged lymph node in the child’s neck is accompanied by weakness, nausea and chills, fever from 37.5 degrees and above. Often there is a headache. At the same time, we note that with chronic lymphadenitis, clinical manifestations may not be at all.
Differences between odontogenic and non-odontogenic lymphadenitis
In the case of odontogenic lymphadenitis, as a rule, patients complain that the lymph nodes in the child’s neck are inflamed only on one side, and this usually corresponds to the submandibular group. When questioning the patient, it usually turns out that before the inflammation itself, he felt a toothache, he had a gumboil on the gum. Recent dental treatment is also possible. In other words, one can see a clear connection between the inflammatory process and the tooth or with the pathology of the oral mucosa.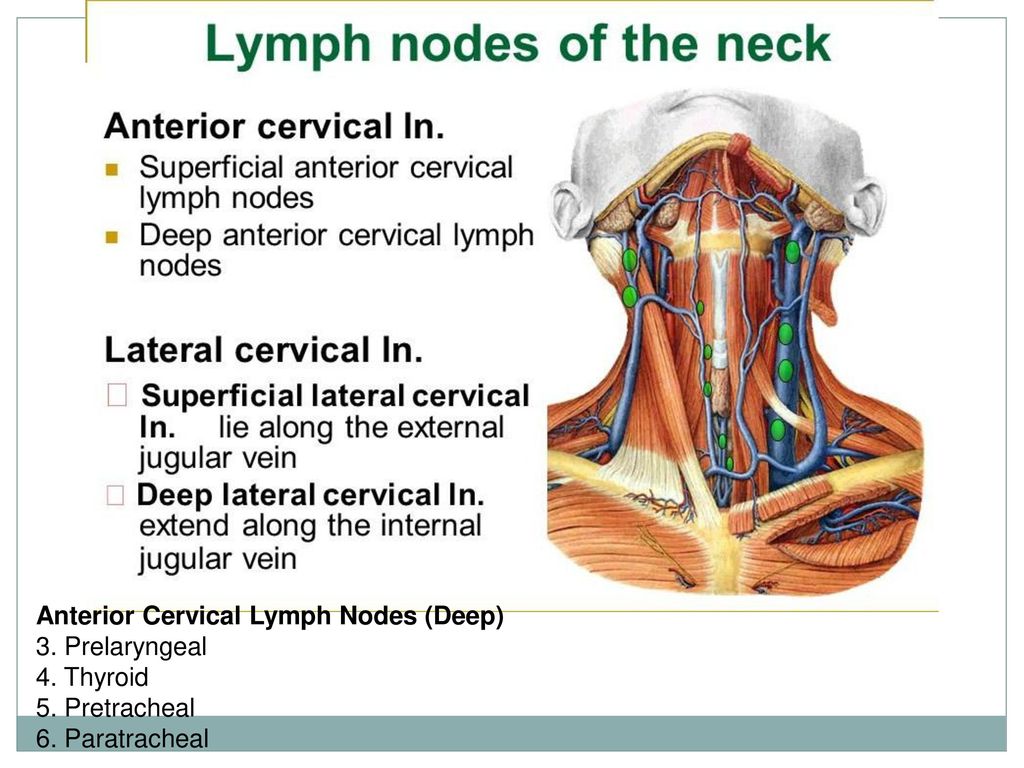
When it comes to acute non-odontogenic lymphadenitis, patients usually complain of the appearance of several “tubercles” in the upper part of the neck at the back or in the submandibular region. However, they often associate this with a sore throat that has been cured recently, a viral infection, or ear diseases. The main feature of this type of lymphadenitis is that the inflammation of the lymph nodes in the child’s neck is observed in several places at once.
Risk of oncology
In some cases, enlarged lymph nodes in the child’s neck may appear as a result of lymphogranulomatosis, as well as lymphosarcoma. These are malignant processes in the body, for which painlessness is typical, but a significant increase in lymph nodes, while there are no other reasons for their inflammation. They can change their sizes in groups and at the same time asymmetrically. At the initial stage of the development of the pathology, the lymph nodes often retain their mobility, are located separately from each other, but with the spread of the malignant process and the absence of treatment, they can become soldered.
If there is an increase in the lymph nodes in the neck in a child and an adult:
- more than 7 days;
- more than 1 group;
- in an infant under one year of age;
- in combination with an increase in temperature;
- progressive;
- with skin changes –
you need to see a doctor as soon as possible to get a referral for diagnosis and appropriate advice.
Benefits of visiting the Miracle Doctor Clinic
Miracle Doctor Medical Center offers each patient the most complete and detailed diagnostics, as well as the services of professional doctors. We use advanced examination equipment and provide comfortable conditions. If a child has inflamed lymph nodes, it is recommended to immediately contact a specialist of our clinic in order to diagnose and receive timely treatment.
Methods of diagnosis
First of all, the specialist conducts an examination and collects an anamnesis, and then sends the patient for an examination, including general urine and blood tests, x-rays. Additionally, a biopsy of the lymph node and subsequent cytological examination, ultrasound can be performed.
Additionally, a biopsy of the lymph node and subsequent cytological examination, ultrasound can be performed.
Methods of treatment
Enlarged lymph nodes in a child’s neck are not a separate pathology, but a symptom of another disease. In this regard, the treatment is carried out to eliminate the cause of such a reaction of the body, and in each case it is different. The nodes can return to normal size after a different period – it all depends on the type, severity of the underlying pathology.
If a child has inflamed lymph nodes and at the same time he often suffers from infectious diseases, SARS, the doctor may recommend immunomodulators.
Complications of lymphadenitis
Lymphadenitis can be complicated by adenophlegmon, which can subsequently lead to phlebitis and sepsis. This is due to a significant weakening of the immune system, poor-quality or untimely treatment.
Prevention
Since there are several reasons for an enlarged lymph node in a child’s neck, prevention should be versatile.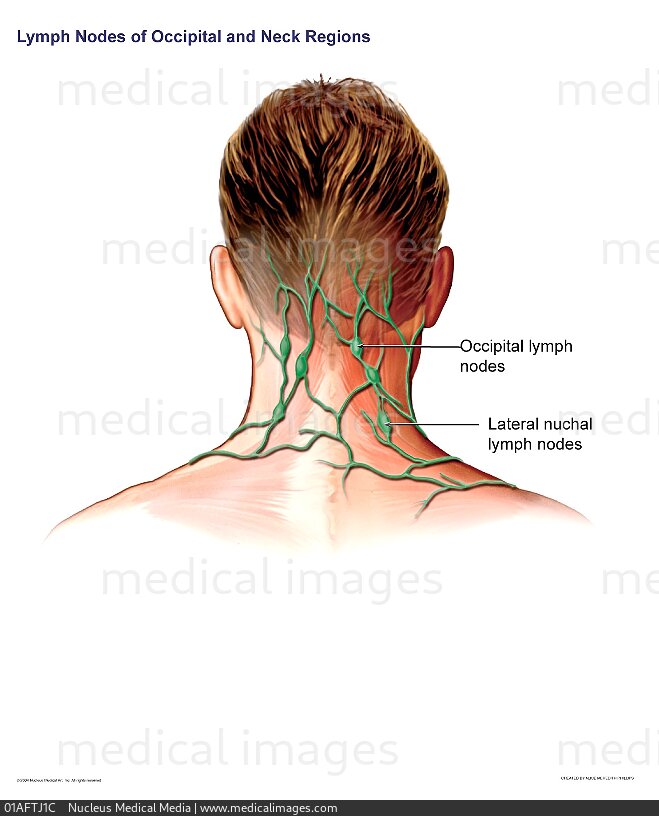




 g. x-ray and ultrasound scans to help detect tumors or sources of infection
g. x-ray and ultrasound scans to help detect tumors or sources of infection