Ischiorectal abscess causes. Ischiorectal Abscess: Causes, Symptoms, and Treatment of Perianal Abscesses
What are the main causes of ischiorectal abscesses. How can perianal abscesses be diagnosed and treated. What are the potential complications of untreated anal abscesses. How do risk factors contribute to the development of rectal abscesses.
Understanding Ischiorectal and Perianal Abscesses
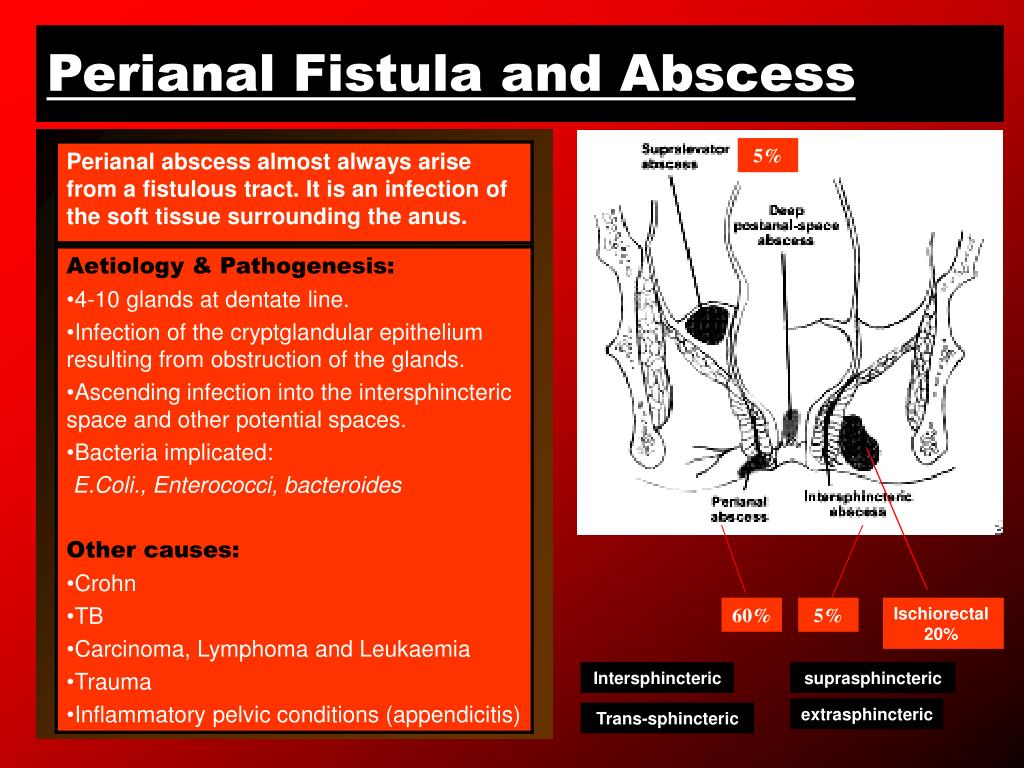
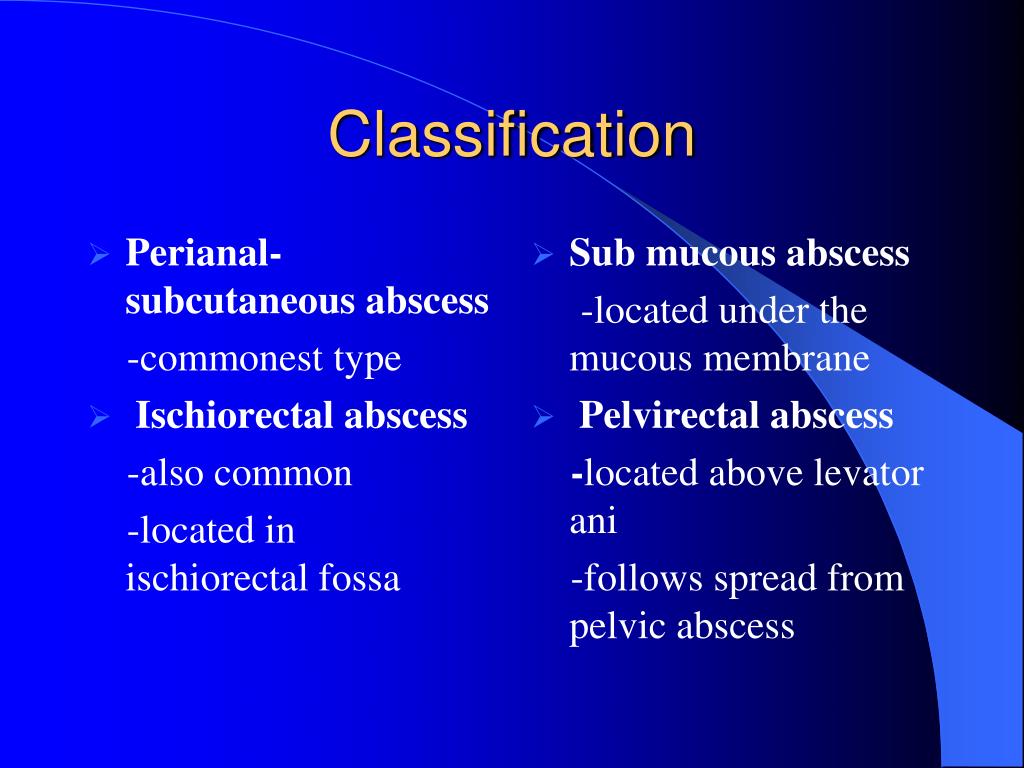
Ischiorectal and perianal abscesses are painful conditions that occur when a cavity in the anal region becomes filled with pus. These terms, along with “anal abscess” and “rectal abscess,” are often used interchangeably to describe the same condition. These abscesses can cause significant discomfort and, if left untreated, may lead to serious complications.
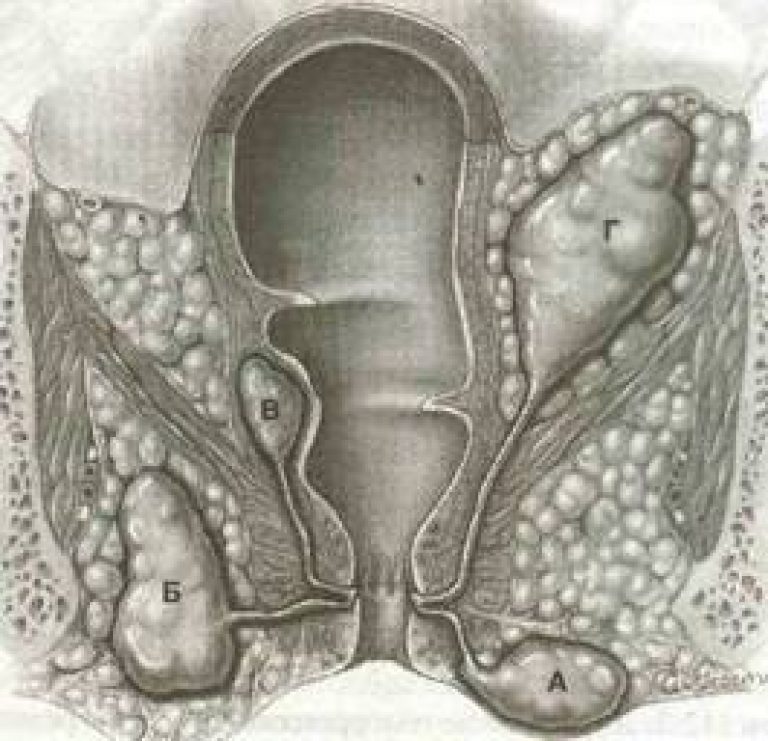
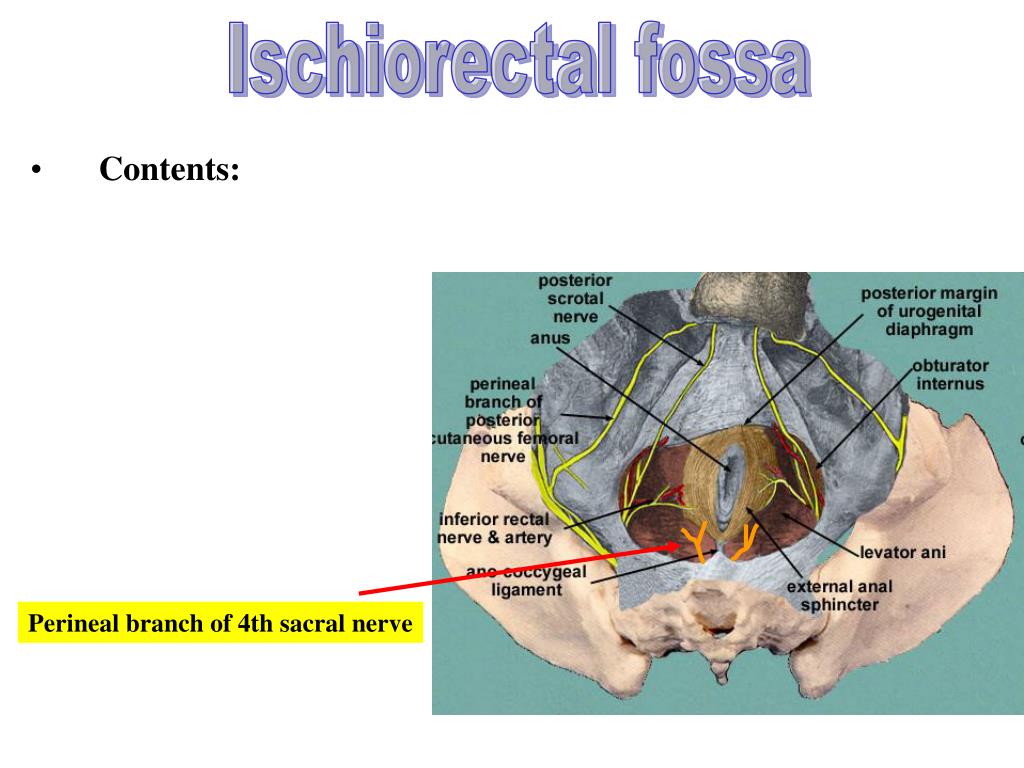
The ischiorectal fossa, a space filled with fat tissue surrounding the anal canal, is a common site for abscess formation. When an infection develops in this area, it can result in an ischiorectal abscess. Understanding the nature of these abscesses is crucial for early detection and proper treatment.

Key Characteristics of Ischiorectal and Perianal Abscesses
- Pus-filled cavity near the anus
- Can occur in the ischiorectal fossa or surrounding anal tissue
- Often caused by bacterial infection
- May result from blocked anal glands or tissue trauma
Common Causes and Risk Factors for Anal Abscesses
Anal abscesses can develop due to various factors, ranging from local tissue damage to systemic health conditions. Understanding these causes can help in prevention and early intervention.
Primary Causes of Ischiorectal and Perianal Abscesses
- Blocked or infected anal glands
- Tears in the anal tissue (anal fissures)
- Sexually transmitted infections (STIs)
- Trauma to the anal region
Can inflammatory bowel diseases contribute to anal abscess formation? Yes, conditions like Crohn’s disease and ulcerative colitis significantly increase the risk of developing anal abscesses. These diseases cause inflammation in the digestive tract, which can lead to weakened tissue and increased susceptibility to infection.
Risk Factors Associated with Anal Abscesses
- Male gender (twice as likely as females)
- Diabetes
- Compromised immune system (e.g., HIV/AIDS)
- Anal sex
- Use of immunosuppressant medications or steroids
- Recent chemotherapy
- Chronic constipation or diarrhea
- Smoking
Does a history of anal fissures increase the risk of developing anal abscesses? Indeed, individuals with a history of anal fissures, particularly children who have experienced constipation-related tears, are at a higher risk for developing anal abscesses later in life.
Recognizing the Symptoms of Ischiorectal and Perianal Abscesses
Identifying the symptoms of anal abscesses is crucial for early diagnosis and treatment. While some symptoms may be mistaken for other conditions, such as hemorrhoids, it’s important to seek medical attention if you suspect an abscess.
Common Symptoms of Anal Abscesses
- Constant, throbbing pain in the anal area
- Swelling and tenderness around the anus
- Increased pain during bowel movements
- Constipation
- Rectal discharge or bleeding
- Fatigue
- Fever and chills
Are there any specific symptoms in toddlers with anal abscesses? In young children, the symptoms may be less pronounced. Toddlers might show signs of discomfort or irritability, and a lump or nodule may be visible or palpable around the anal area.

Deep Rectal Abscesses
Some anal abscesses may occur deeper in the rectum, particularly in individuals with inflammatory bowel diseases. These can cause:
- Pain or discomfort in the abdominal area
- Less visible external symptoms
- Potential difficulty in diagnosis without imaging
Diagnostic Approaches for Ischiorectal and Perianal Abscesses
Accurate diagnosis of anal abscesses is essential for appropriate treatment. Healthcare providers employ various methods to confirm the presence of an abscess and determine its extent.
Physical Examination
The primary diagnostic tool for anal abscesses is a physical examination. During this process:
- The doctor checks for characteristic nodules around the anus
- Pain, redness, and swelling in the anal area are assessed
- Other conditions with similar symptoms are ruled out
Internal Examination
If no visible signs are present on the skin surface, the doctor may use an anoscope to examine the anal canal and lower rectum internally.
Imaging Studies
For deeper abscesses or to get a more comprehensive view, imaging tests may be ordered:
- CT scan
- MRI
- Ultrasound
Why might additional tests be necessary in some cases? If Crohn’s disease is suspected as a contributing factor, further tests such as blood and stool analyses, additional imaging, and a colonoscopy may be required to confirm the diagnosis and guide treatment.
Treatment Options for Ischiorectal and Perianal Abscesses
Anal abscesses rarely resolve without medical intervention. Treatment typically involves draining the abscess to relieve pressure and allow proper healing.
Abscess Drainage
The most common treatment for anal abscesses is drainage of the pus-filled cavity. This procedure:
- Can often be performed in a doctor’s office
- Involves local anesthesia to numb the area
- Provides immediate relief from pressure and pain
- Allows the tissue to begin healing properly
Surgical Intervention
In cases of extremely large anal abscesses, surgery under general anesthesia may be necessary. The procedure may involve:
- Making an incision to drain the abscess
- Possible placement of a catheter for continued drainage
- Leaving the wound open to heal (typically without stitches)
Are there any special considerations for patients with certain health conditions? Patients with diabetes or weakened immune systems may require additional care, such as antibiotics, to prevent complications and ensure proper healing.
Potential Complications of Untreated Anal Abscesses
Leaving an anal abscess untreated can lead to severe complications that may require more extensive medical intervention.
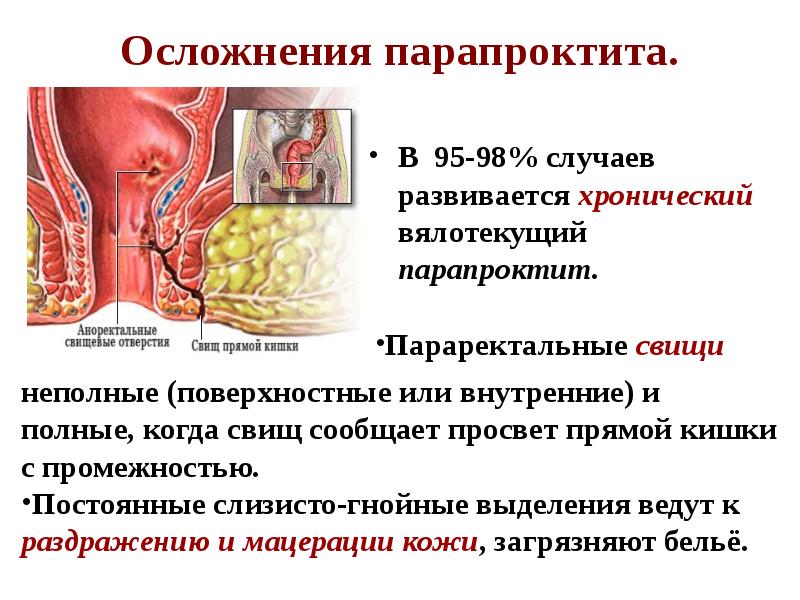
Anal Fistulas
One of the most common complications of untreated anal abscesses is the formation of an anal fistula. This occurs when the abscess breaks open on the skin surface, creating an abnormal connection between the anal canal and the skin. Fistulas can be painful and may require surgical repair.
Sepsis
In severe cases, an untreated abscess can lead to sepsis, a life-threatening condition caused by the body’s extreme response to infection. Sepsis requires immediate medical attention and can be fatal if not treated promptly.
Fournier’s Gangrene
Although rare, Fournier’s gangrene is a potentially life-threatening infection that can develop from an untreated anal abscess. This condition causes tissue death in the genital and perianal areas and requires aggressive treatment, including surgery and antibiotics.
How quickly can complications develop from an untreated anal abscess? The progression of complications can vary, but some patients may develop fistulas or more severe infections within days to weeks if the abscess is left untreated.
Prevention and Lifestyle Considerations for Anal Health
While not all anal abscesses can be prevented, certain lifestyle changes and preventive measures can reduce the risk of developing this painful condition.
Maintaining Proper Hygiene
Good anal hygiene is crucial in preventing infections that can lead to abscesses. This includes:
- Thorough cleaning of the anal area after bowel movements
- Using gentle, fragrance-free cleansers
- Avoiding excessive wiping or use of harsh toilet paper
Managing Underlying Health Conditions
For individuals with conditions that increase the risk of anal abscesses, proper management is essential:
- Adherence to treatment plans for inflammatory bowel diseases
- Good blood sugar control for diabetics
- Regular check-ups and appropriate care for immune-compromising conditions
Lifestyle Modifications
Certain lifestyle changes can help reduce the risk of developing anal abscesses:
- Maintaining a healthy diet high in fiber to prevent constipation
- Staying hydrated to promote regular bowel movements
- Avoiding prolonged sitting on hard surfaces
- Practicing safe sex and using protection during anal intercourse
- Quitting smoking to improve overall health and immune function
Can exercise help in preventing anal abscesses? Regular physical activity can promote better bowel function and overall health, potentially reducing the risk of developing anal abscesses. However, it’s important to avoid exercises that put excessive pressure on the anal area.
Long-Term Management and Follow-Up Care
After treatment for an anal abscess, proper follow-up care is crucial to ensure complete healing and prevent recurrence.
Post-Treatment Care
Following abscess drainage or surgery, patients should:
- Keep the area clean and dry
- Follow wound care instructions provided by their healthcare provider
- Take prescribed medications, including antibiotics if recommended
- Avoid strenuous activities that may irritate the area

Monitoring for Recurrence
Patients who have had an anal abscess should be vigilant for signs of recurrence or fistula formation. Regular check-ups with a healthcare provider may be necessary, especially for those with underlying risk factors.
Addressing Underlying Causes
To prevent future abscesses, it’s important to address any underlying conditions that may have contributed to the initial infection. This may involve:
- Ongoing management of inflammatory bowel diseases
- Treatment of chronic constipation or diarrhea
- Lifestyle modifications to reduce risk factors
How long does it typically take for an anal abscess to heal after treatment? Healing times can vary depending on the size and location of the abscess, as well as individual factors. Most patients experience significant improvement within a few days to weeks after drainage, but complete healing may take several weeks to months.
Perianal (Anal) Abscess: Causes, Symptoms, and More
An anal abscess, also known as a perianal or rectal abscess, occurs when a cavity in the anus becomes filled with pus. Symptoms may include pain, constipation, or fever. Treatment may include drainage of the abscess or surgery.
A perianal abscess occurs when a cavity in the anus becomes filled with pus. The terms “anal abscess” and “rectal abscess” can also be used to describe this same condition.
Anal abscesses can cause:
- extreme pain
- fatigue
- rectal discharge
- fever
In some cases, they can result in painful anal fistulas. This occurs when the abscess breaks open on the surface of the skin. If an anal abscess isn’t drained, it can cause a lot of pain and may require surgery.
A rectal abscess can happen when a tear in that area becomes infected or an anal gland becomes blocked. A sexually transmitted infection (STI) can also cause anal abscesses.
Toddlers or children that have a history of anal fissures (tears in the anal sphincter) are also at a higher risk for developing anal abscesses later on. Such anal fissures might occur in children who have a history of constipation.
Such anal fissures might occur in children who have a history of constipation.
Anal abscesses are twice as likely in males compared with females.
Some other risk factors include:
- Crohn’s disease or ulcerative colitis, which are inflammatory bowel diseases that cause the body to attack healthy tissue
- diabetes
- a compromised immune system due to conditions like HIV or AIDS
- anal sex, which can increase the risk of anal abscesses
- use of the medication prednisone or other steroids
- current or recent chemotherapy or use of immunosuppressant medications
- constipation
- diarrhea
- smoking
This condition is likely underdiagnosed, as many people may not seek medical attention because they believe they may be experiencing hemorrhoids. It’s important to make an appointment with a doctor if you believe you have a perianal abscess.
If left untreated, anal abscesses can lead to severe complications, such as:
- an anal fistula, an atypical opening in the skin near the anus
- sepsis, a life threatening condition due to your body’s response to an infection
- Fournier’s gangrene, a rare but potentially life threatening infection
Throbbing and constant pain in the anal area can be one of the most common and immediately noticeable symptoms of an anal abscess. The pain is usually accompanied by swelling in the anal area and greater pain during bowel movements.
The pain is usually accompanied by swelling in the anal area and greater pain during bowel movements.
Common signs of an anal abscess include:
- constant pain that can be dull, sharp, throbbing, or aching
- constipation
- rectal discharge or bleeding
- swelling or tenderness of the skin surrounding the anus
- fatigue
- fever
- chills
Some people may be able to feel a nodule or lump that’s red, swollen, and tender at the rim of the anus. Fever and chills can result from the infection. You may also have rectal bleeding or urinary symptoms, such as difficulty urinating.
Anal abscesses may also occur deeper in the rectum, most often in those who have inflammatory bowel diseases. This can result in some pain or discomfort in the abdominal area.
In toddlers, there typically aren’t many symptoms other than signs of discomfort or pain, which may cause a child to become irritable. A lump or nodule may also be visible or felt around the anal area.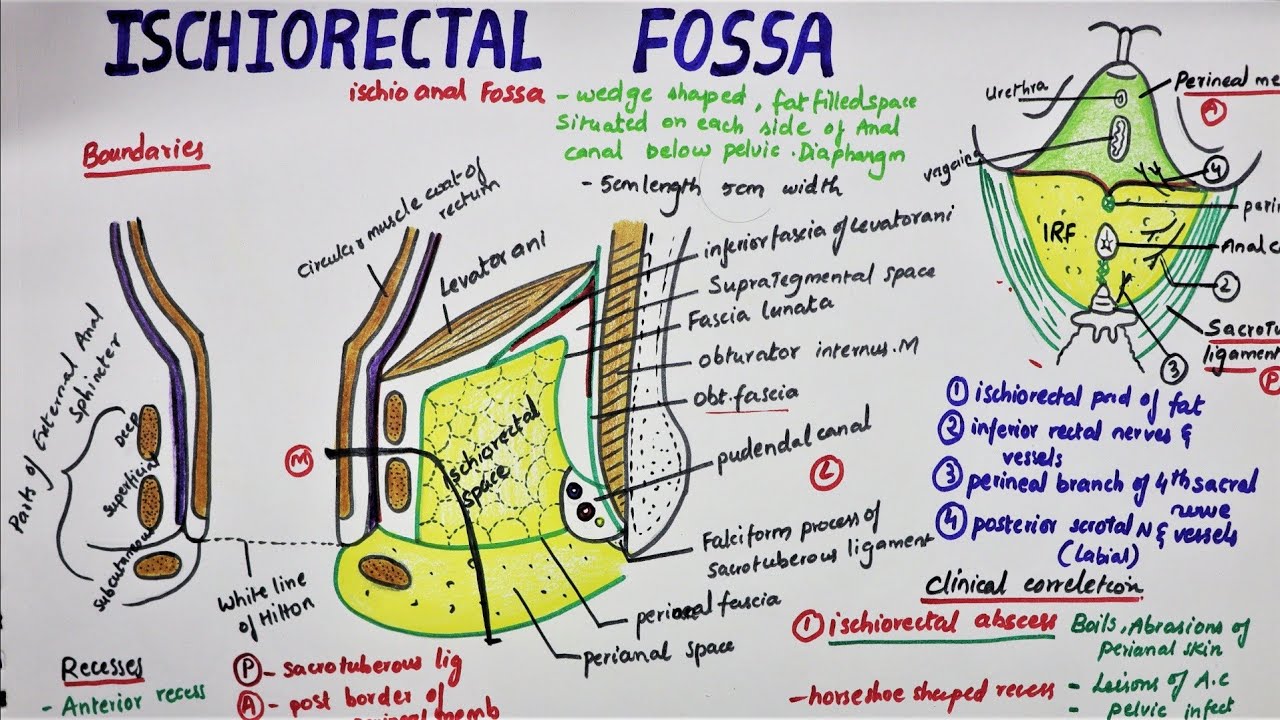
Anal abscesses are most often diagnosed through a physical exam where a doctor checks the area for characteristic nodules. The doctor may also check for pain, redness, and swelling in the anal area and rule out other conditions.
In some people, there may not be any visible signs of the abscess on the surface of the skin around their anus. The doctor will instead use an instrument called an anoscope to look inside the anal canal and lower rectum.
Sometimes, the abscess may be deeper than a physical exam can find. The doctor may order imaging tests, such as a CT scan, MRI, or ultrasound, to get a better look.
Further tests may be necessary to make sure Crohn’s disease isn’t a contributing factor.
In these cases, blood and stool tests, imaging, and a colonoscopy may be needed. A colonoscopy is an outpatient procedure in which a doctor uses a flexible scope with a light to examine the colon and large intestine.
Anal abscesses rarely go away without treatment from a doctor. Treatment may include drainage or surgery.
Treatment may include drainage or surgery.
The most common and simple treatment is for a doctor to drain the pus from the infected area.
This can usually be done in the doctor’s office. The doctor will use medication to numb the area. Any uncomfortable pressure should be relieved, allowing the tissue to begin healing properly.
If there’s an extremely large anal abscess, surgery with anesthesia may be required. In some cases, a catheter may be used to make sure the abscess drains completely. Abscesses that have been drained are typically left open and don’t require stitches.
If you have diabetes or a weakened immune system, your doctor may ask you to stay in the hospital for a few days to watch for any infection.
Treatment following drainage may include:
- Medication. The doctor may prescribe antibiotics if you have a weakened immune system or if the infection has spread. Antibiotics are not considered sufficient to treat the infection on their own but may be prescribed after draining the abscess.

- Laxatives or fiber supplements. As you heal after draining the abscess, your doctor may recommend laxatives or fiber supplements to avoid constipation.
- Warm baths. After this procedure, the doctor may provide guidance on how to keep the area clean and may recommend a sitz bath. It’s recommended you take warm (not hot) baths. Sitting in warm water may help reduce swelling.
- Follow-up appointments. Because there is a chance for anal abscesses to recur or fistulas to develop, it’s important to attend all follow-up appointments. A 2019 study found that having a higher body mass index (BMI) may be correlated with abscesses recurring.
The recovery period for a drained rectal abscess is about 3 to 4 weeks.
If anal abscesses are left untreated, they can turn into painful anal fistulas that may require more surgical treatment.
According to the American Society of Colon and Rectal Surgeons, about 50 percent of people who have an anal abscess will eventually develop an anal fistula. A fistula generally requires surgery.
A fistula generally requires surgery.
There isn’t much known about how to prevent an anal abscess. But there are some steps you can take, including:
- taking measures to protect yourself from STIs and seeking prompt treatment
- using condoms or other barrier methods, especially during anal sex, to help prevent STIs that may cause anal abscesses
- practicing good hygiene and cleanliness in the anal area
- treating conditions like Crohn’s disease that may cause anal abscesses
Anal abscesses can cause complications, but they’re treatable. It’s important to understand the risk factors and closely monitor and manage any health conditions that may increase risk.
If you notice anal problems, contact a doctor to get treatment and to prevent them from becoming worse.
Perianal (Anal) Abscess: Causes, Symptoms, and More
An anal abscess, also known as a perianal or rectal abscess, occurs when a cavity in the anus becomes filled with pus. Symptoms may include pain, constipation, or fever. Treatment may include drainage of the abscess or surgery.
Symptoms may include pain, constipation, or fever. Treatment may include drainage of the abscess or surgery.
A perianal abscess occurs when a cavity in the anus becomes filled with pus. The terms “anal abscess” and “rectal abscess” can also be used to describe this same condition.
Anal abscesses can cause:
- extreme pain
- fatigue
- rectal discharge
- fever
In some cases, they can result in painful anal fistulas. This occurs when the abscess breaks open on the surface of the skin. If an anal abscess isn’t drained, it can cause a lot of pain and may require surgery.
A rectal abscess can happen when a tear in that area becomes infected or an anal gland becomes blocked. A sexually transmitted infection (STI) can also cause anal abscesses.
Toddlers or children that have a history of anal fissures (tears in the anal sphincter) are also at a higher risk for developing anal abscesses later on. Such anal fissures might occur in children who have a history of constipation.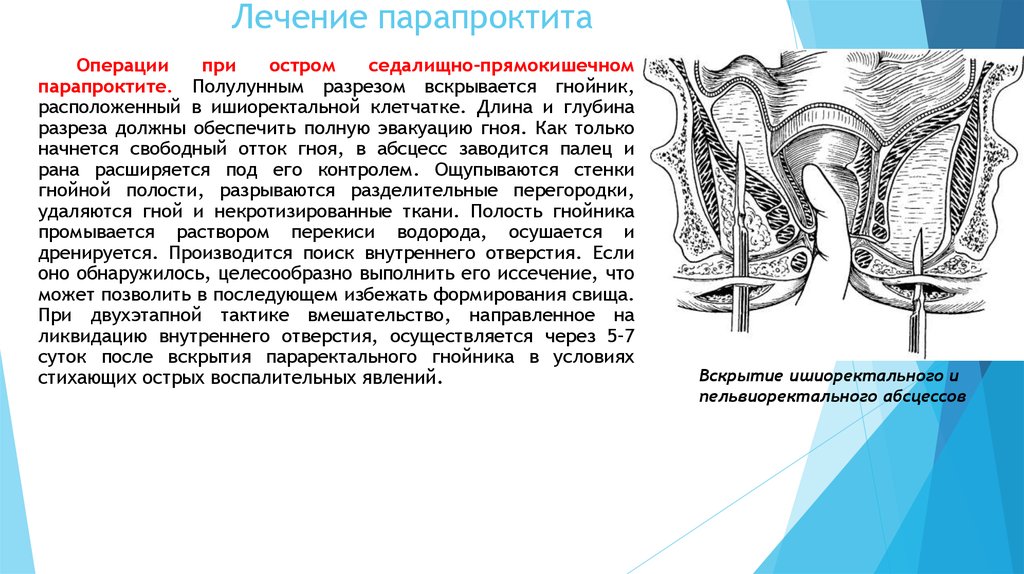
Anal abscesses are twice as likely in males compared with females.
Some other risk factors include:
- Crohn’s disease or ulcerative colitis, which are inflammatory bowel diseases that cause the body to attack healthy tissue
- diabetes
- a compromised immune system due to conditions like HIV or AIDS
- anal sex, which can increase the risk of anal abscesses
- use of the medication prednisone or other steroids
- current or recent chemotherapy or use of immunosuppressant medications
- constipation
- diarrhea
- smoking
This condition is likely underdiagnosed, as many people may not seek medical attention because they believe they may be experiencing hemorrhoids. It’s important to make an appointment with a doctor if you believe you have a perianal abscess.
If left untreated, anal abscesses can lead to severe complications, such as:
- an anal fistula, an atypical opening in the skin near the anus
- sepsis, a life threatening condition due to your body’s response to an infection
- Fournier’s gangrene, a rare but potentially life threatening infection
Throbbing and constant pain in the anal area can be one of the most common and immediately noticeable symptoms of an anal abscess. The pain is usually accompanied by swelling in the anal area and greater pain during bowel movements.
The pain is usually accompanied by swelling in the anal area and greater pain during bowel movements.
Common signs of an anal abscess include:
- constant pain that can be dull, sharp, throbbing, or aching
- constipation
- rectal discharge or bleeding
- swelling or tenderness of the skin surrounding the anus
- fatigue
- fever
- chills
Some people may be able to feel a nodule or lump that’s red, swollen, and tender at the rim of the anus. Fever and chills can result from the infection. You may also have rectal bleeding or urinary symptoms, such as difficulty urinating.
Anal abscesses may also occur deeper in the rectum, most often in those who have inflammatory bowel diseases. This can result in some pain or discomfort in the abdominal area.
In toddlers, there typically aren’t many symptoms other than signs of discomfort or pain, which may cause a child to become irritable. A lump or nodule may also be visible or felt around the anal area.
Anal abscesses are most often diagnosed through a physical exam where a doctor checks the area for characteristic nodules. The doctor may also check for pain, redness, and swelling in the anal area and rule out other conditions.
In some people, there may not be any visible signs of the abscess on the surface of the skin around their anus. The doctor will instead use an instrument called an anoscope to look inside the anal canal and lower rectum.
Sometimes, the abscess may be deeper than a physical exam can find. The doctor may order imaging tests, such as a CT scan, MRI, or ultrasound, to get a better look.
Further tests may be necessary to make sure Crohn’s disease isn’t a contributing factor.
In these cases, blood and stool tests, imaging, and a colonoscopy may be needed. A colonoscopy is an outpatient procedure in which a doctor uses a flexible scope with a light to examine the colon and large intestine.
Anal abscesses rarely go away without treatment from a doctor.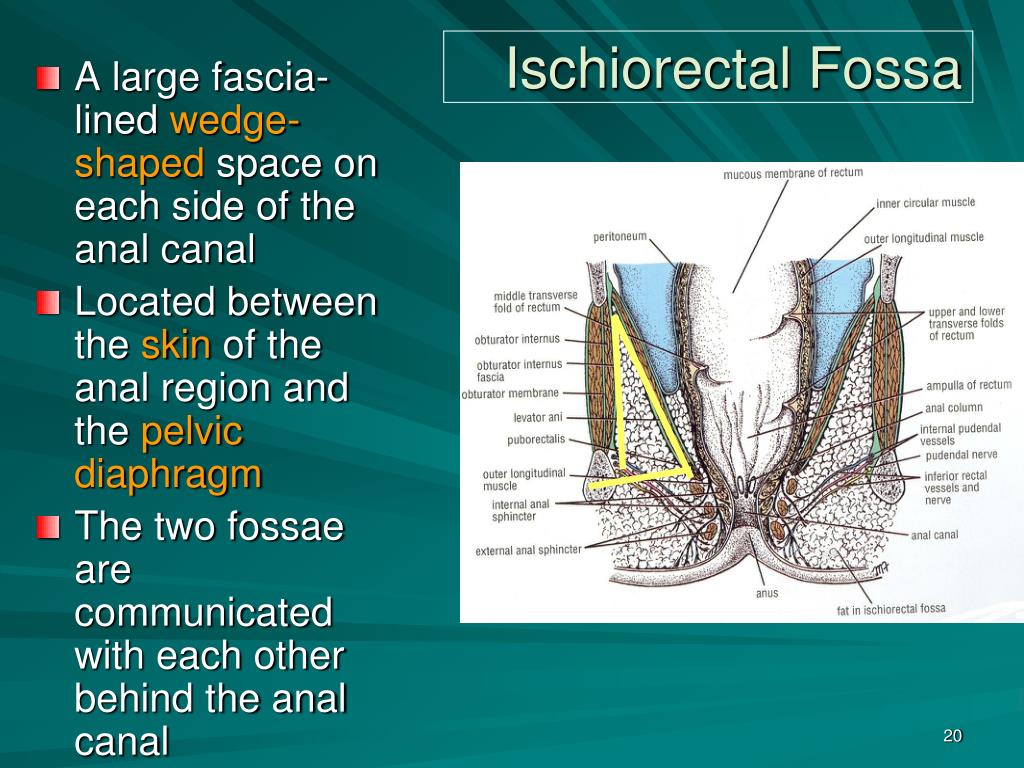 Treatment may include drainage or surgery.
Treatment may include drainage or surgery.
The most common and simple treatment is for a doctor to drain the pus from the infected area.
This can usually be done in the doctor’s office. The doctor will use medication to numb the area. Any uncomfortable pressure should be relieved, allowing the tissue to begin healing properly.
If there’s an extremely large anal abscess, surgery with anesthesia may be required. In some cases, a catheter may be used to make sure the abscess drains completely. Abscesses that have been drained are typically left open and don’t require stitches.
If you have diabetes or a weakened immune system, your doctor may ask you to stay in the hospital for a few days to watch for any infection.
Treatment following drainage may include:
- Medication. The doctor may prescribe antibiotics if you have a weakened immune system or if the infection has spread. Antibiotics are not considered sufficient to treat the infection on their own but may be prescribed after draining the abscess.

- Laxatives or fiber supplements. As you heal after draining the abscess, your doctor may recommend laxatives or fiber supplements to avoid constipation.
- Warm baths. After this procedure, the doctor may provide guidance on how to keep the area clean and may recommend a sitz bath. It’s recommended you take warm (not hot) baths. Sitting in warm water may help reduce swelling.
- Follow-up appointments. Because there is a chance for anal abscesses to recur or fistulas to develop, it’s important to attend all follow-up appointments. A 2019 study found that having a higher body mass index (BMI) may be correlated with abscesses recurring.
The recovery period for a drained rectal abscess is about 3 to 4 weeks.
If anal abscesses are left untreated, they can turn into painful anal fistulas that may require more surgical treatment.
According to the American Society of Colon and Rectal Surgeons, about 50 percent of people who have an anal abscess will eventually develop an anal fistula.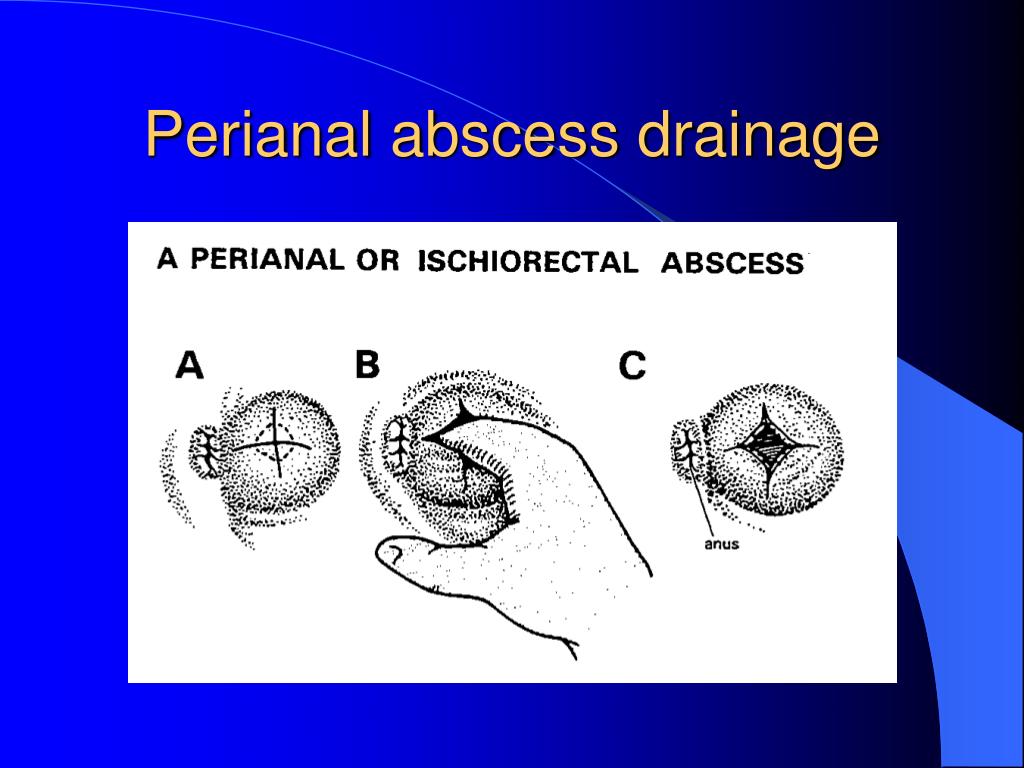 A fistula generally requires surgery.
A fistula generally requires surgery.
There isn’t much known about how to prevent an anal abscess. But there are some steps you can take, including:
- taking measures to protect yourself from STIs and seeking prompt treatment
- using condoms or other barrier methods, especially during anal sex, to help prevent STIs that may cause anal abscesses
- practicing good hygiene and cleanliness in the anal area
- treating conditions like Crohn’s disease that may cause anal abscesses
Anal abscesses can cause complications, but they’re treatable. It’s important to understand the risk factors and closely monitor and manage any health conditions that may increase risk.
If you notice anal problems, contact a doctor to get treatment and to prevent them from becoming worse.
Share Contents:
What are rectal abscesses (paraproctitis)? Paraproctitis – purulent inflammation of the tissues surrounding the rectum. There are acute (first-time) and chronic paraproctitis (develops as a result of spontaneous or incorrect opening (treatment) of acute paraproctitis). Rectal abscesses are common in patients with pre-existing anorectal disease, diabetes, alcoholism, and neurological disease; infections in this area also most often develop in patients with acute leukemia, especially in the presence of neutropenia. Since the clinical picture may be regarded as a fever of unknown origin for a long period, it is important that in patients with unexplained fever, a thorough digital and endoscopic examination of the rectum is mandatory. Causes of rectal abscess (paraproctitis)There are many reasons for paraproctitis:
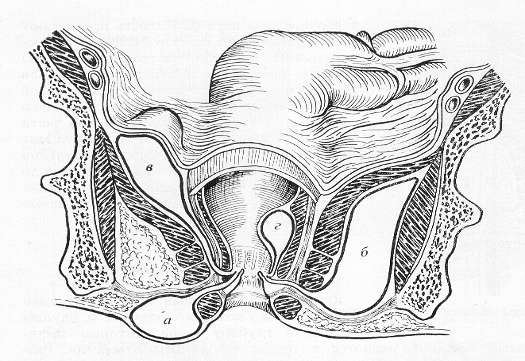
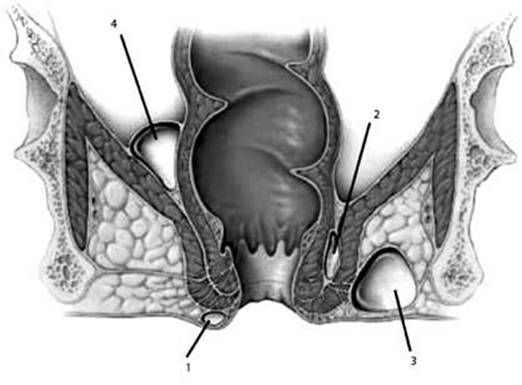
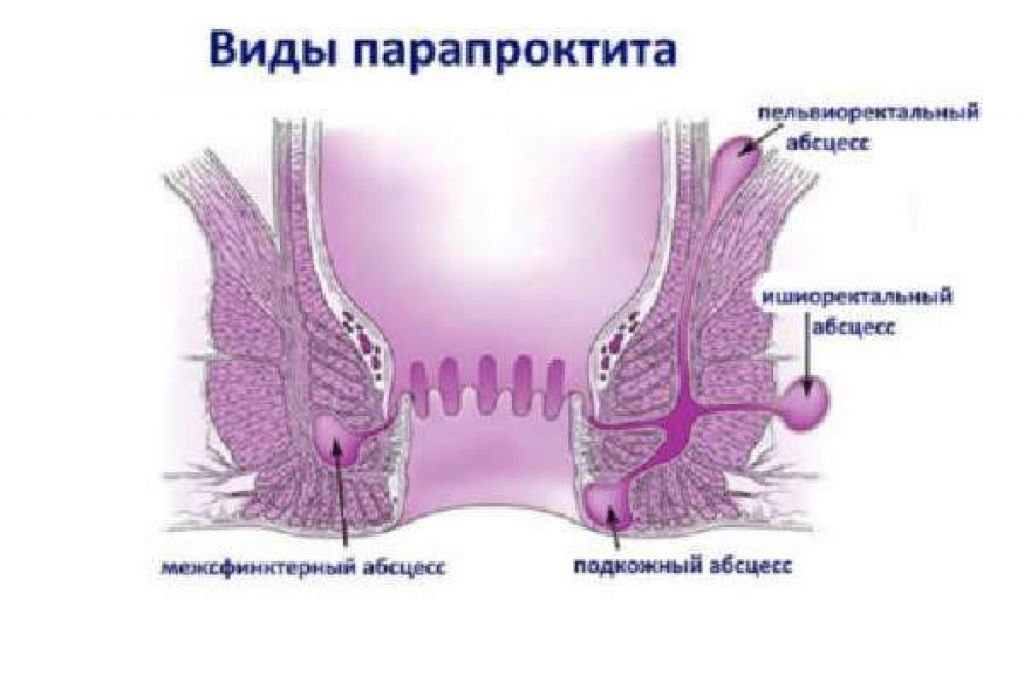
Through special glands located in the anus, the infection from the lumen of the rectum penetrates into the surrounding tissues. Acute paraproctitis occurs when the infection quickly penetrates into the pararectal (perrectal) cellular space. Depending on the immunity of a person, the size and location of the abscess can be different. An abscess can be located both directly under the skin of the perineum (subcutaneous – most often), and deep between the muscles of the perineum and buttocks (ischiorectal – sciatic-rectal, pelviorectal – pelvic-rectal, and as one of the types of pelvic-rectal – retrorectal (retrorectal)). Chronic paraproctitis often occurs with spontaneous or improper opening (treatment) of acute paraproctitis. Acute paraproctitis Acute paraproctitis occurs when the infection quickly penetrates into the pararectal cellular space – subcutaneous (most often), ischiorectal, pelviorectal, retrorectal (very rare). Symptoms of acute paraproctitis are primarily sharp pains that increase when walking, coughing, etc. The general condition worsens, especially with deep (ischiorectal, pelvic-rectal) abscesses, while there are practically no external signs – skin redness, fluctuations. With deep (high) ischiorectal and other acute paraproctitis, the patient’s condition may be severe – high fever, signs of intoxication, pain in the depths of the pelvis. Symptoms of acute paraproctitis The disease usually has an acute onset. Following a short prodromal period with malaise, weakness, headache, there is increasing pain in the rectum, perineum, or pelvis, accompanied by fever and chills. Ischiorectal abscess in the first days of the disease is manifested by general symptoms: chilling, feeling unwell, dull pain in the pelvis and rectum, aggravated by defecation; local changes – asymmetry of the buttocks, infiltration, skin hyperemia – appear at a late stage (5-6th day). The most severe is pelviorectal paraproctitis, in which the abscess is located deep in the pelvis. In the first days of the disease, general symptoms of inflammation predominate: fever, chills, headache, pain in the joints, in the pelvis, in the lower abdomen. Chronic paraproctitisChronic paraproctitis often occurs with spontaneous or improper opening (treatment) of acute paraproctitis. The internal opening of the abscess in the anal canal does not heal and a fistula remains. Healing can occur with a fragile scar, which, with minor trauma – cycling, constipation, etc. – abscess reappears, inflammation is not in the same place of the anal canal, while the localization of the abscess may be in another place in the perineum. After improper opening and treatment, the wound on the perineum does not heal – the rectal fistula remains, while re-infection with the intestinal flora occurs through the internal opening of the fistula. In most patients, the cause of the infection cannot be identified. Rectal abscesses are usually very painful, easily palpable, and often visible on examination. Treatment consists of an incision and drainage. DiagnosisThe first and main task of diagnosing acute paraproctitis is to recognize the presence and localization of an abscess in the cellular space surrounding the rectum based on the patient’s complaints, clinic and examination. The disease is detected during examination and digital examination of the rectum. To exclude complications of acute paraproctitis, women also need to consult a gynecologist, and men – a urologist. Treatment of acute paraproctitis is only surgical. Surgery should be performed immediately after diagnosis. The operation is performed under anesthesia. The purpose of the operation is to open the abscess (abscess) and remove the pus. After the operation, dressings are performed, antibiotics, vitamins, and immunity boosters are prescribed. However, opening an abscess is not a radical operation: after it, as a rule, repeated suppurations occur (chronic paraproctitis is formed). The reason for this phenomenon is the preservation of the inflammatory channel (fistula) between the rectum and surrounding tissues. For a complete cure, a second operation is required, performed in a specialized proctology hospital. As a result of such an operation, the connection between the intestinal cavity and the abscess is eliminated. It is called radical, because leads to a complete cure. ComplicationsUntimely surgical treatment of acute paraproctitis may lead to the development of complications: purulent destruction of the rectal wall and/or urethral wall in men, breakthrough of pus into the vagina in women. The most formidable complication is the breakthrough of pus into the pelvic cavity, which, if diagnosed late, can lead to death. After opening the abscess spontaneously or surgically without eliminating the purulent tract and the affected crypt, a fistula of the rectum is usually formed in the future. K61 – Abscess of the anus and rectum
Consult a healthcare professional before using any drug References
← Previous article Next article → Read more You may be interested in
|
Share Contents:
What are rectal abscesses (paraproctitis)? Paraproctitis – purulent inflammation of the tissues surrounding the rectum. There are acute (first-time) and chronic paraproctitis (develops as a result of spontaneous or incorrect opening (treatment) of acute paraproctitis). Rectal abscesses are not uncommon in patients with pre-existing anorectal disease, diabetes, alcoholism, and neurological disease; infections in this area also most often develop in patients with acute leukemia, especially in the presence of neutropenia. Since the clinical picture may be regarded as a fever of unknown origin for a long period, it is important that in patients with unexplained fever, a thorough digital and endoscopic examination of the rectum is mandatory. Causes of rectal abscess (paraproctitis)There are many reasons for paraproctitis:
Through special glands located in the anus, the infection from the lumen of the rectum penetrates into the surrounding tissues. Acute paraproctitis occurs when the infection quickly penetrates into the pararectal (perrectal) cellular space. Depending on the immunity of a person, the size and location of the abscess can be different. An abscess can be located both directly under the skin of the perineum (subcutaneous – most often), and deep between the muscles of the perineum and buttocks (ischiorectal – sciatic-rectal, pelviorectal – pelvic-rectal, and as one of the types of pelvic-rectal – retrorectal (retrorectal)). Chronic paraproctitis often occurs with spontaneous or improper opening (treatment) of acute paraproctitis. Acute paraproctitis Acute paraproctitis occurs when the infection quickly penetrates into the pararectal cellular space – subcutaneous (most often), ischiorectal, pelviorectal, retrorectal (very rare). Symptoms of acute paraproctitis are primarily sharp pains that increase when walking, coughing, etc. The general condition worsens, especially with deep (ischiorectal, pelvic-rectal) abscesses, while there are practically no external signs – skin redness, fluctuations. With deep (high) ischiorectal and other acute paraproctitis, the patient’s condition may be severe – high fever, signs of intoxication, pain in the depths of the pelvis. Symptoms of acute paraproctitis The disease usually has an acute onset. Following a short prodromal period with malaise, weakness, headache, there is increasing pain in the rectum, perineum, or pelvis, accompanied by fever and chills. Ischiorectal abscess in the first days of the disease is manifested by general symptoms: chilling, feeling unwell, dull pain in the pelvis and rectum, aggravated by defecation; local changes – asymmetry of the buttocks, infiltration, skin hyperemia – appear at a late stage (5-6th day). The most severe is pelviorectal paraproctitis, in which the abscess is located deep in the pelvis. In the first days of the disease, general symptoms of inflammation predominate: fever, chills, headache, pain in the joints, in the pelvis, in the lower abdomen. Chronic paraproctitisChronic paraproctitis often occurs with spontaneous or improper opening (treatment) of acute paraproctitis. The internal opening of the abscess in the anal canal does not heal and a fistula remains. Healing can occur with a fragile scar, which, with minor trauma – cycling, constipation, etc. – abscess reappears, inflammation is not in the same place of the anal canal, while the localization of the abscess may be in another place in the perineum. After improper opening and treatment, the wound on the perineum does not heal – the rectal fistula remains, while re-infection with the intestinal flora occurs through the internal opening of the fistula. In most patients, the cause of the infection cannot be identified. Rectal abscesses are usually very painful, easily palpable, and often visible on examination. Treatment consists of an incision and drainage. DiagnosisThe first and main task of diagnosing acute paraproctitis is to recognize the presence and localization of an abscess in the cellular space surrounding the rectum based on the patient’s complaints, clinic and examination. The disease is detected during examination and digital examination of the rectum. To exclude complications of acute paraproctitis, women also need to consult a gynecologist, and men – a urologist. Treatment of acute paraproctitis is only surgical. Surgery should be performed immediately after diagnosis. The operation is performed under anesthesia. The purpose of the operation is to open the abscess (abscess) and remove the pus. After the operation, dressings are performed, antibiotics, vitamins, and immunity boosters are prescribed. However, opening an abscess is not a radical operation: after it, as a rule, repeated suppurations occur (chronic paraproctitis is formed). The reason for this phenomenon is the preservation of the inflammatory channel (fistula) between the rectum and surrounding tissues. For a complete cure, a second operation is required, performed in a specialized proctology hospital. As a result of such an operation, the connection between the intestinal cavity and the abscess is eliminated. It is called radical, because leads to a complete cure. ComplicationsUntimely surgical treatment of acute paraproctitis may lead to the development of complications: purulent destruction of the rectal wall and/or urethral wall in men, breakthrough of pus into the vagina in women. The most formidable complication is the breakthrough of pus into the pelvic cavity, which, if diagnosed late, can lead to death. After opening the abscess spontaneously or surgically without eliminating the purulent tract and the affected crypt, a fistula of the rectum is usually formed in the future. K61 – Abscess of the anus and rectum
Consult a healthcare professional before using any drug References
|



 Inflammation develops, an abscess forms. Therefore, a simple opening of abscesses from the outside, without sanitation of the internal inflamed area, does not lead to a lasting recovery.
Inflammation develops, an abscess forms. Therefore, a simple opening of abscesses from the outside, without sanitation of the internal inflamed area, does not lead to a lasting recovery. Depending on the affected space, paraproctitis is distinguished by localization – subcutaneous, etc. The internal opening of the abscess is almost always one, there may be two or more external abscesses. In more than half of patients, the abscess is located on the border of the mucous membrane and skin.
Depending on the affected space, paraproctitis is distinguished by localization – subcutaneous, etc. The internal opening of the abscess is almost always one, there may be two or more external abscesses. In more than half of patients, the abscess is located on the border of the mucous membrane and skin.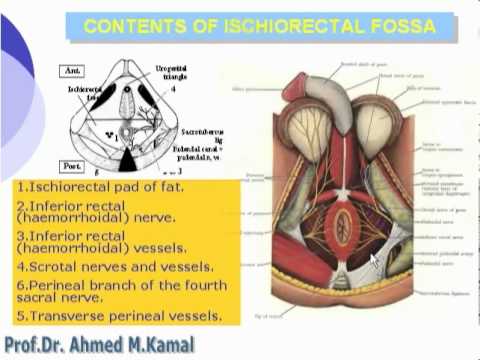 The severity of the symptoms of acute paraproctitis depends on the location of the inflammatory process, its prevalence, the nature of the pathogen, and the reactivity of the body. With the localization of the abscess in the subcutaneous tissue, the clinical manifestations are more pronounced and definite: painful infiltrate in the anus, skin hyperemia, fever, usually force you to see a doctor in the first days after the onset of the disease.
The severity of the symptoms of acute paraproctitis depends on the location of the inflammatory process, its prevalence, the nature of the pathogen, and the reactivity of the body. With the localization of the abscess in the subcutaneous tissue, the clinical manifestations are more pronounced and definite: painful infiltrate in the anus, skin hyperemia, fever, usually force you to see a doctor in the first days after the onset of the disease.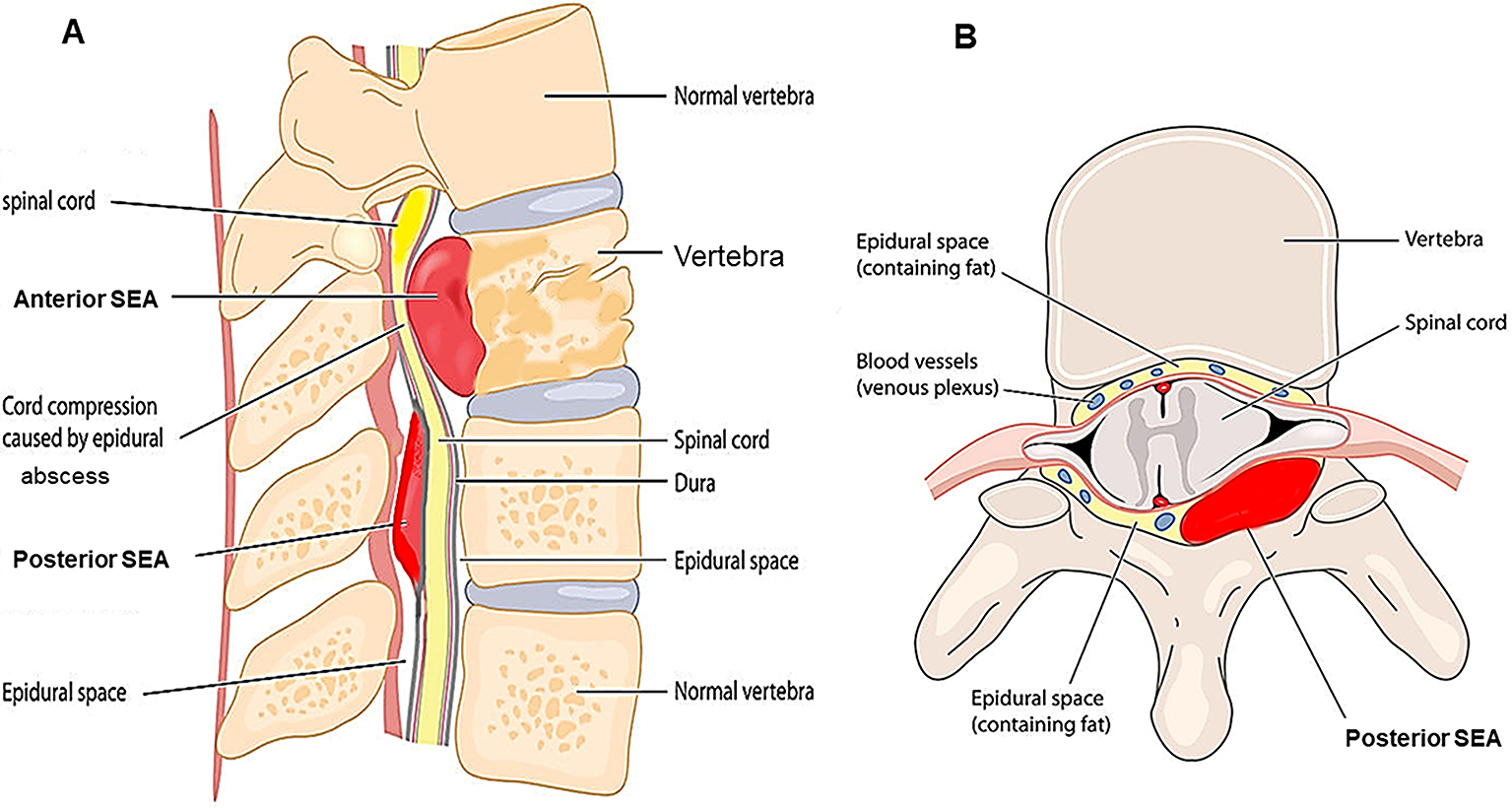 Often the patient turns to a surgeon, urologist, women – to a gynecologist. Often they are treated for acute respiratory illness, influenza. The duration of this period sometimes reaches 10-12 days. In the future, there is an increase in pain in the pelvis and rectum, retention of stool, urine, and severe intoxication.
Often the patient turns to a surgeon, urologist, women – to a gynecologist. Often they are treated for acute respiratory illness, influenza. The duration of this period sometimes reaches 10-12 days. In the future, there is an increase in pain in the pelvis and rectum, retention of stool, urine, and severe intoxication.
 Such an operation can be performed in any surgical hospital.
Such an operation can be performed in any surgical hospital. If the fistula was not formed, but at the same time there was a focus of inflammation in the region of the anal glands and the intersphincter space, then after some time a relapse of acute paraproctitis occurs.
If the fistula was not formed, but at the same time there was a focus of inflammation in the region of the anal glands and the intersphincter space, then after some time a relapse of acute paraproctitis occurs. 20 ml: fl. 8 pcs.
20 ml: fl. 8 pcs.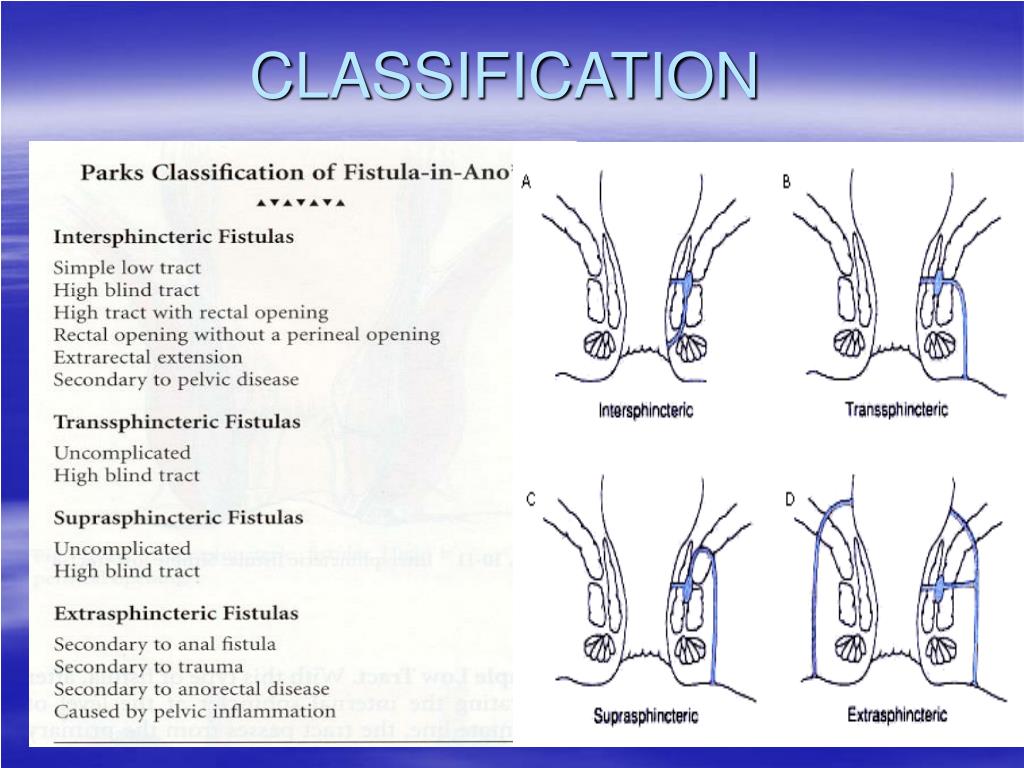 No.: P N001974/01
No.: P N001974/01 20 ml: fl. 8 pcs.
20 ml: fl. 8 pcs.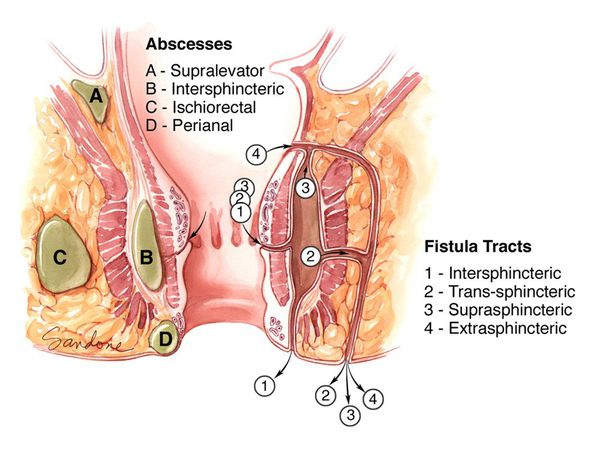 544.
544.
 Inflammation develops, an abscess forms. Therefore, a simple opening of abscesses from the outside, without sanitation of the internal inflamed area, does not lead to a lasting recovery.
Inflammation develops, an abscess forms. Therefore, a simple opening of abscesses from the outside, without sanitation of the internal inflamed area, does not lead to a lasting recovery. Depending on the affected space, paraproctitis is distinguished by localization – subcutaneous, etc. The internal opening of the abscess is almost always one, there may be two or more external abscesses. In more than half of patients, the abscess is located on the border of the mucous membrane and skin.
Depending on the affected space, paraproctitis is distinguished by localization – subcutaneous, etc. The internal opening of the abscess is almost always one, there may be two or more external abscesses. In more than half of patients, the abscess is located on the border of the mucous membrane and skin.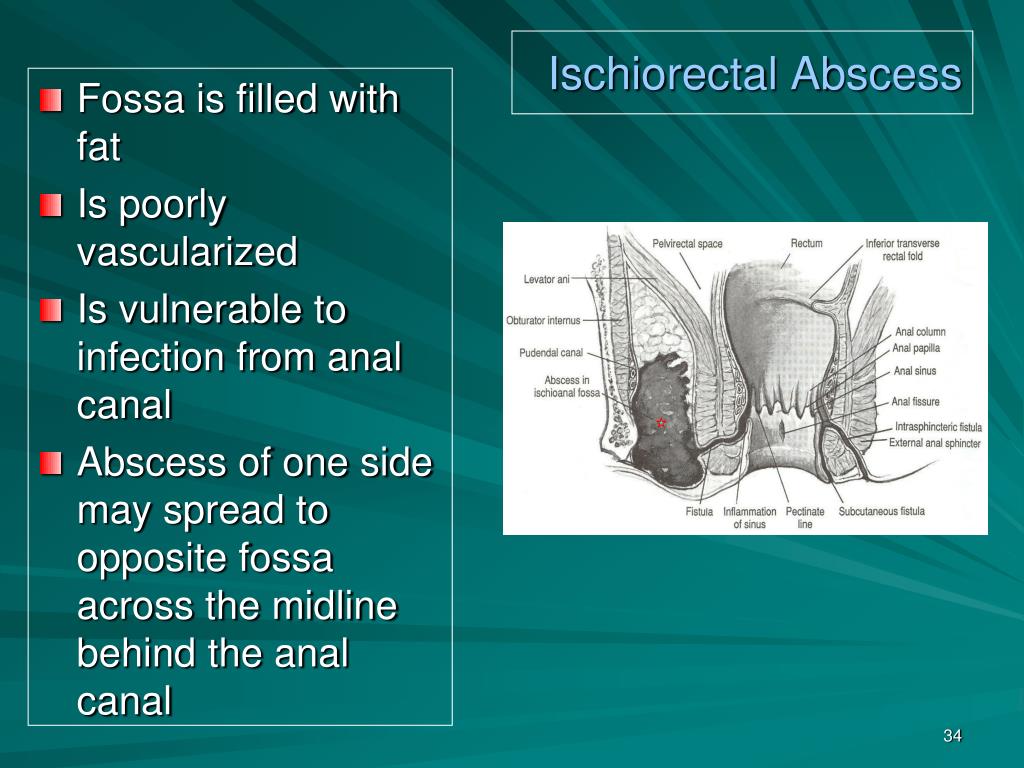 The severity of the symptoms of acute paraproctitis depends on the location of the inflammatory process, its prevalence, the nature of the pathogen, and the reactivity of the body. With the localization of the abscess in the subcutaneous tissue, the clinical manifestations are more pronounced and definite: painful infiltrate in the anus, skin hyperemia, fever, usually force you to see a doctor in the first days after the onset of the disease.
The severity of the symptoms of acute paraproctitis depends on the location of the inflammatory process, its prevalence, the nature of the pathogen, and the reactivity of the body. With the localization of the abscess in the subcutaneous tissue, the clinical manifestations are more pronounced and definite: painful infiltrate in the anus, skin hyperemia, fever, usually force you to see a doctor in the first days after the onset of the disease. Often the patient turns to a surgeon, urologist, women – to a gynecologist. Often they are treated for acute respiratory illness, influenza. The duration of this period sometimes reaches 10-12 days. In the future, there is an increase in pain in the pelvis and rectum, retention of stool, urine, and severe intoxication.
Often the patient turns to a surgeon, urologist, women – to a gynecologist. Often they are treated for acute respiratory illness, influenza. The duration of this period sometimes reaches 10-12 days. In the future, there is an increase in pain in the pelvis and rectum, retention of stool, urine, and severe intoxication.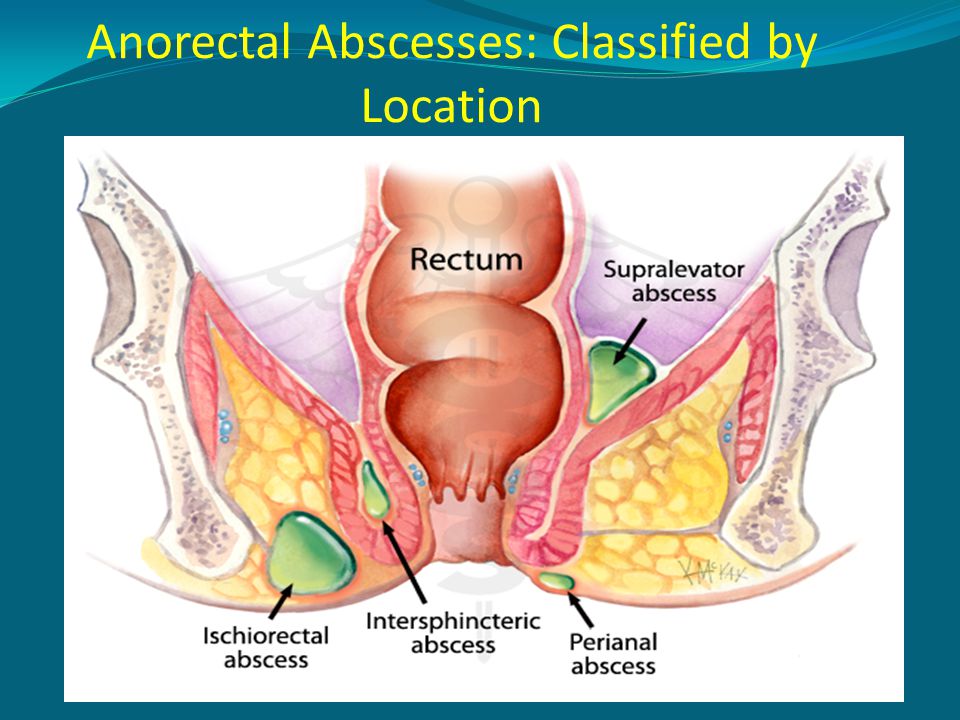
 Such an operation can be performed in any surgical hospital.
Such an operation can be performed in any surgical hospital.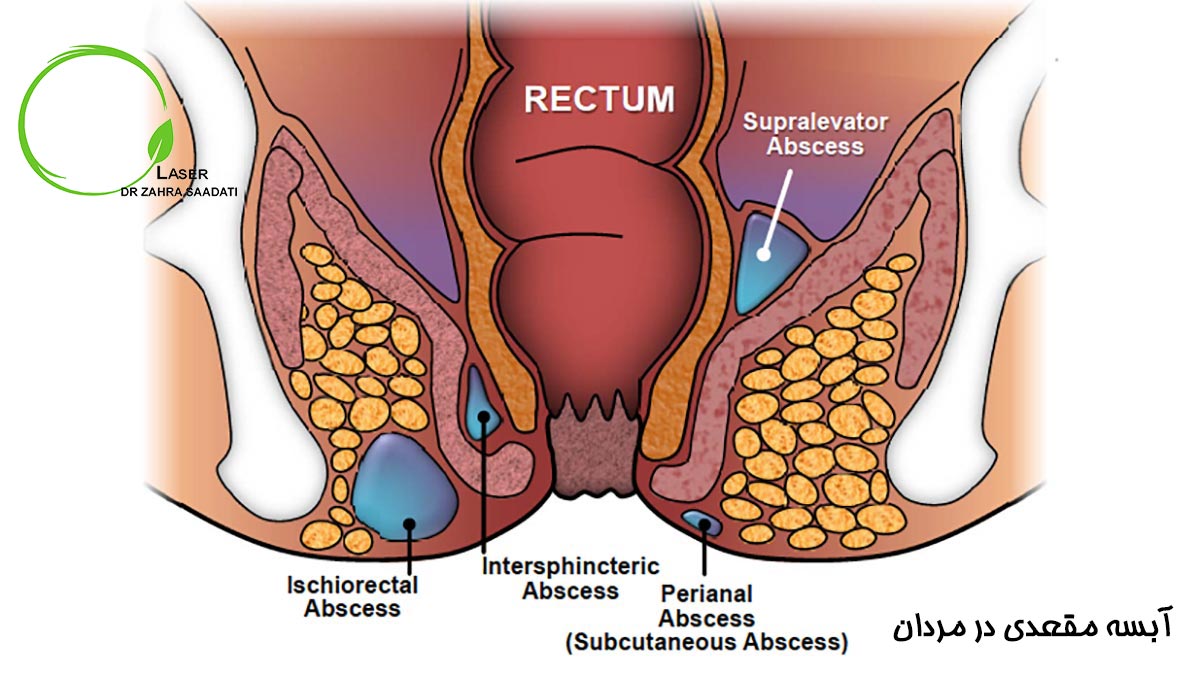 If the fistula was not formed, but at the same time there was a focus of inflammation in the region of the anal glands and the intersphincter space, then after some time a relapse of acute paraproctitis occurs.
If the fistula was not formed, but at the same time there was a focus of inflammation in the region of the anal glands and the intersphincter space, then after some time a relapse of acute paraproctitis occurs.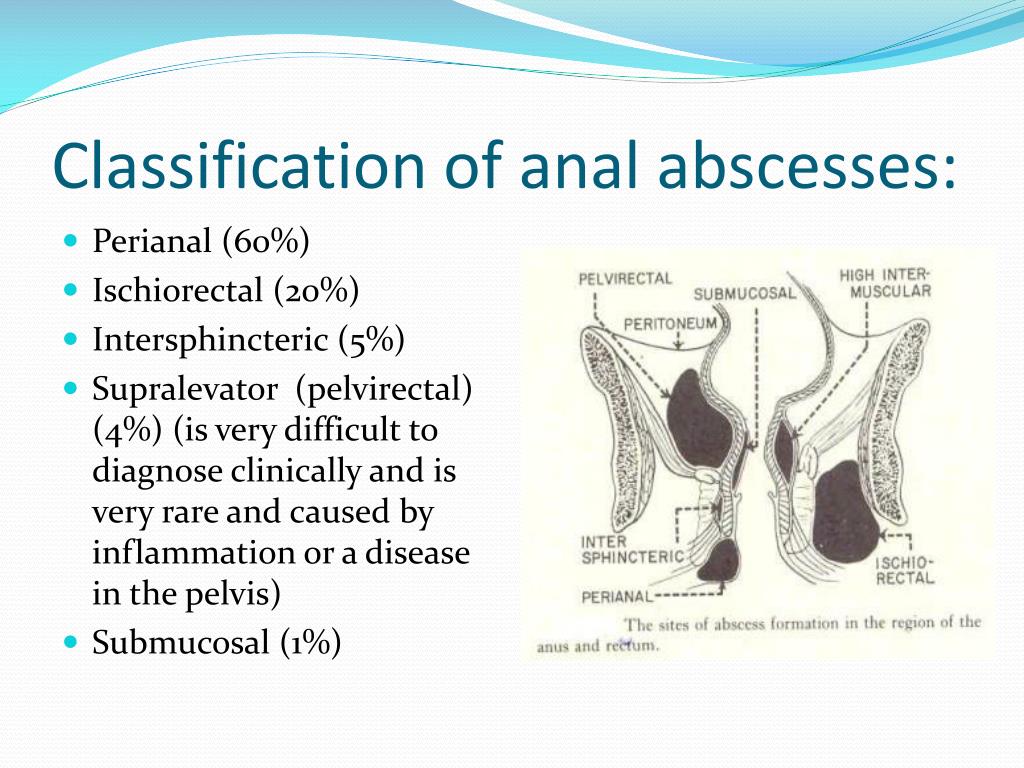 20 ml: fl. 8 pcs.
20 ml: fl. 8 pcs. No.: P N001974/01
No.: P N001974/01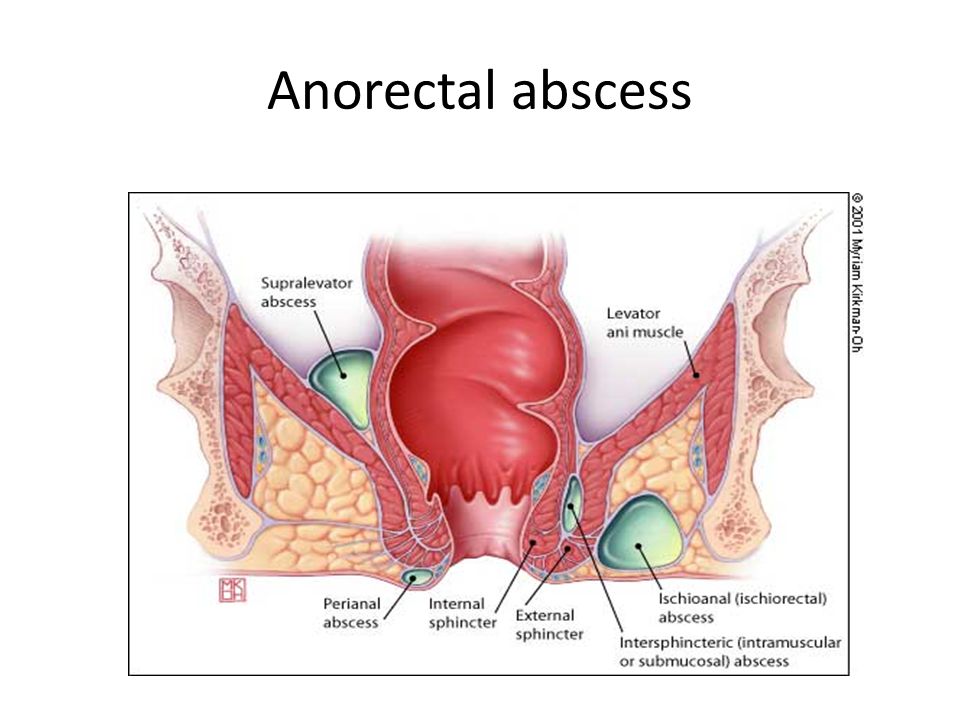 20 ml: fl. 8 pcs.
20 ml: fl. 8 pcs.