Kinds of colitis. Colitis: Types, Diagnosis, and Treatment – Understanding Intestinal Inflammation
What are the different types of colitis. How is colitis diagnosed. What treatments are available for colitis. Discover the causes, symptoms, and management options for various forms of intestinal inflammation.
Understanding Colitis: Inflammation of the Large Intestine
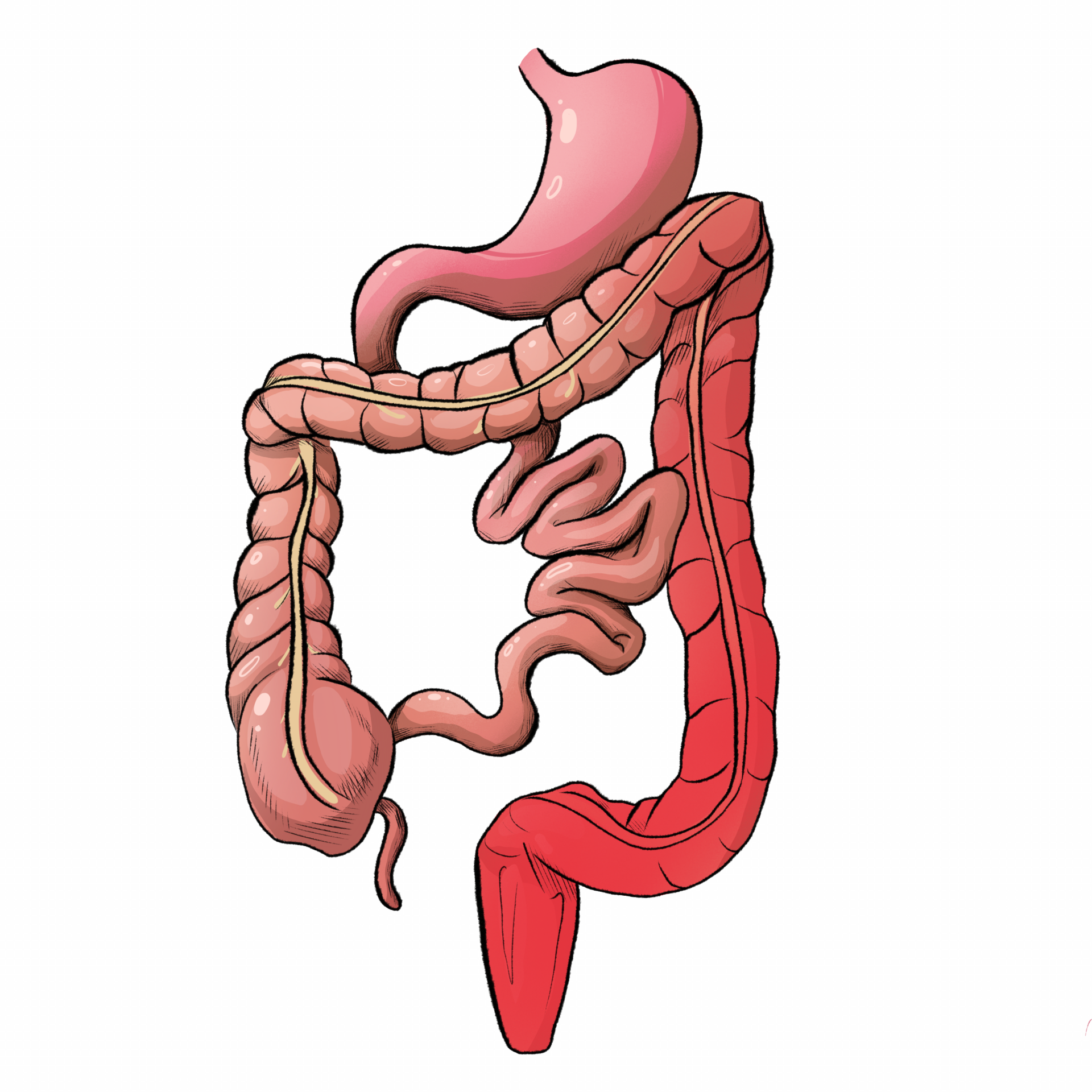
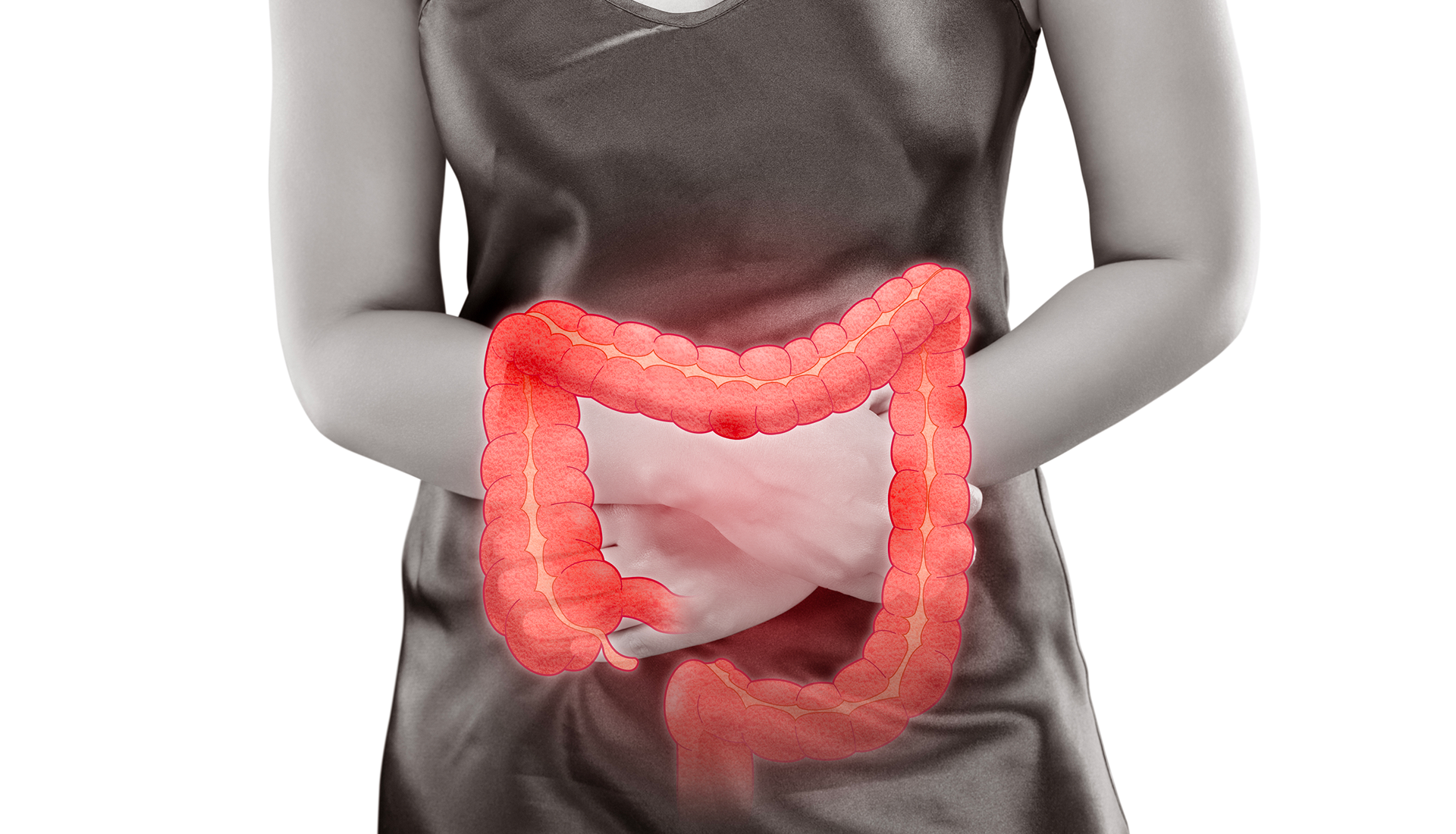
Colitis is a condition characterized by inflammation of the colon, also known as the large intestine. This inflammation can lead to a range of uncomfortable symptoms, including abdominal pain, bloating, and diarrhea. The severity of colitis can vary, with some individuals experiencing mild, recurring discomfort over extended periods, while others may face sudden and severe symptoms.
The impact of colitis on daily life can be significant, affecting everything from dietary choices to overall quality of life. Understanding the different types of colitis and their respective treatments is crucial for effective management of this condition.
What causes colitis?
The causes of colitis can vary depending on the specific type. Some forms are related to autoimmune disorders, while others may be triggered by infections, allergies, or reduced blood flow to the colon. In many cases, the exact cause remains unknown, but researchers continue to investigate potential factors that may contribute to the development of colitis.
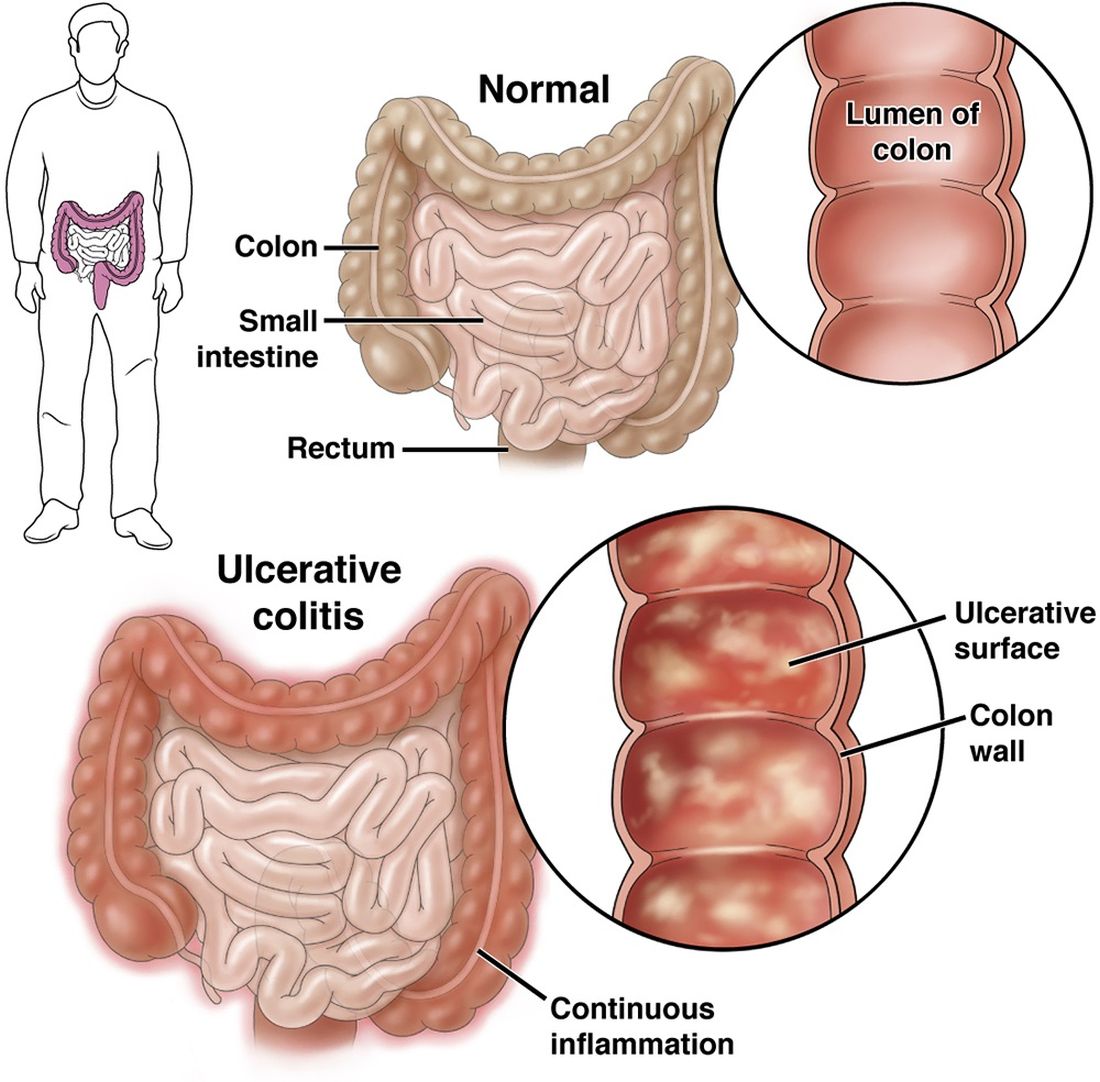
Ulcerative Colitis: A Common Form of Inflammatory Bowel Disease
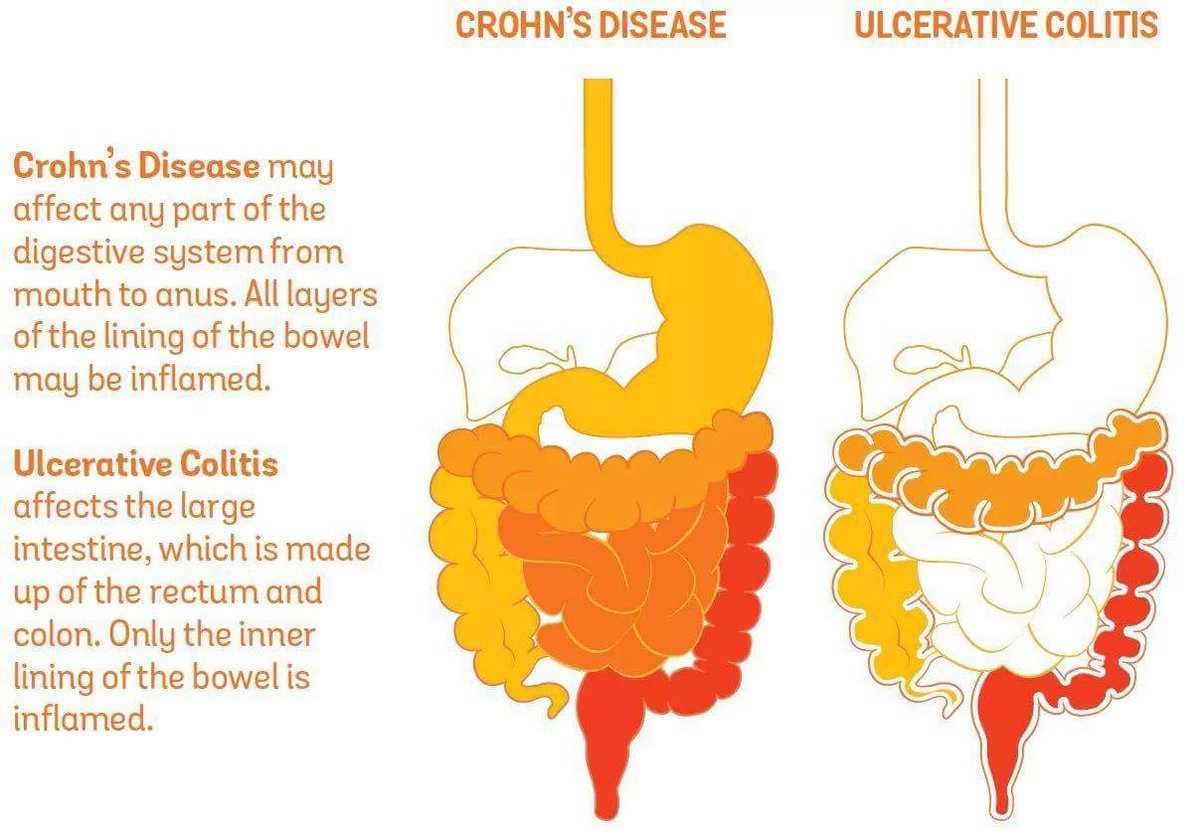
Ulcerative colitis (UC) is one of the most frequently diagnosed types of colitis. It falls under the category of inflammatory bowel disease (IBD), along with Crohn’s disease. UC is a chronic condition characterized by inflammation and ulcers in the inner lining of the large intestine.
What are the characteristics of ulcerative colitis?
Ulcerative colitis typically begins in the rectum and can spread to other parts of the colon. The inflammation is continuous, meaning it affects a single, uninterrupted area of the intestine. This distinguishes UC from Crohn’s disease, which can cause patchy inflammation throughout the digestive tract.
The exact cause of UC remains unknown, but researchers believe it results from an abnormal immune response to bacteria and other substances in the digestive tract. Genetic and environmental factors may also play a role in its development.
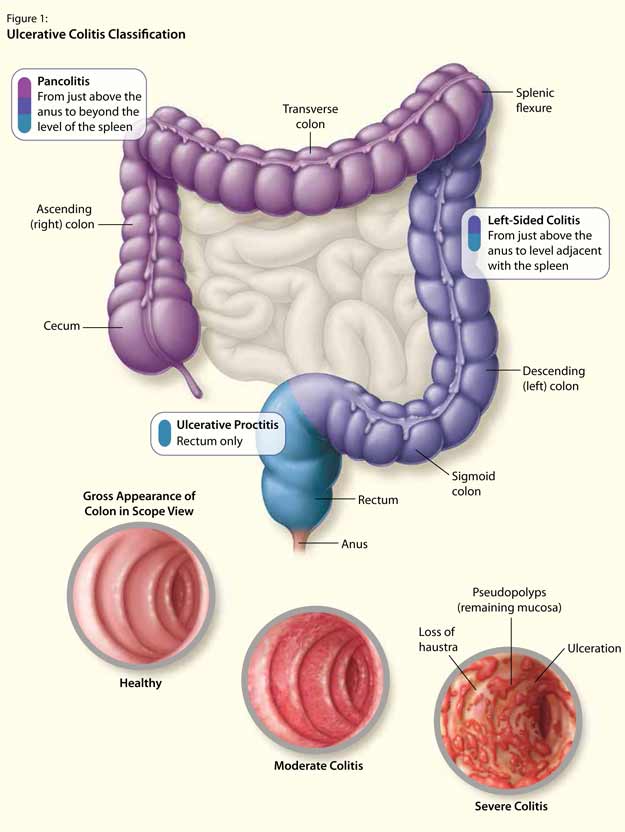
What are the different types of ulcerative colitis?
- Proctosigmoiditis: Affects the rectum and lower portion of the colon (sigmoid colon)
- Left-sided ulcerative colitis: Involves inflammation from the rectum up through the left side of the colon
- Pancolitis: Affects the entire large intestine
Each subtype of UC can present with varying symptoms and may require different treatment approaches. Understanding the extent and location of inflammation is crucial for developing an effective management plan.

Pseudomembranous Colitis: When Gut Bacteria Overgrow
Pseudomembranous colitis (PC) is a distinct form of colitis caused by an overgrowth of the bacterium Clostridium difficile (C. diff). While C. diff is naturally present in the intestines of many individuals, it usually doesn’t cause problems due to the balance maintained by beneficial bacteria.
How does pseudomembranous colitis develop?
The primary trigger for pseudomembranous colitis is the use of antibiotics. These medications can disrupt the delicate balance of gut bacteria by eliminating not only harmful bacteria but also beneficial ones. This disruption creates an opportunity for C. diff to proliferate and release toxins that cause inflammation in the colon.
Symptoms of PC can range from mild diarrhea to severe, life-threatening inflammation of the colon. The condition is particularly concerning in healthcare settings, where antibiotic use is common and the risk of spreading C. diff infections is higher.
What are the risk factors for pseudomembranous colitis?
- Recent antibiotic use, especially broad-spectrum antibiotics
- Prolonged hospital stays
- Advanced age
- Weakened immune system
- Previous C. diff infections
Preventing pseudomembranous colitis involves judicious use of antibiotics and strict adherence to infection control measures in healthcare settings. Early diagnosis and appropriate treatment are crucial for managing this potentially severe condition.
Ischemic Colitis: When Blood Flow to the Colon is Compromised
Ischemic colitis (IC) occurs when blood flow to the colon is suddenly reduced or cut off entirely. This lack of blood supply can lead to inflammation and damage to the affected area of the colon. IC can be acute (sudden onset) or chronic (recurring over time).
What causes ischemic colitis?
Several factors can contribute to the development of ischemic colitis:
- Blood clots: Sudden blockage of blood vessels supplying the colon
- Atherosclerosis: Buildup of fatty deposits in blood vessels, gradually restricting blood flow
- Underlying medical conditions: Such as vasculitis, diabetes, or heart failure
- Medications: Rarely, certain drugs like fibrates and NSAIDs may increase the risk
- Physical factors: Dehydration, blood loss, or abdominal trauma
The severity of ischemic colitis can vary widely, from mild cases that resolve on their own to severe cases requiring surgical intervention. Prompt diagnosis and treatment are essential to prevent complications and promote healing.

How is ischemic colitis diagnosed?
Diagnosing ischemic colitis typically involves a combination of clinical evaluation, imaging studies, and sometimes endoscopic procedures. Common diagnostic tools include:
- CT scans or MRI to visualize the colon and surrounding structures
- Colonoscopy to directly observe the affected area and obtain tissue samples if necessary
- Blood tests to check for signs of infection or inflammation
- Angiography in some cases to assess blood flow to the colon
Early recognition of symptoms and prompt medical attention are crucial for improving outcomes in cases of ischemic colitis.
Microscopic Colitis: Inflammation Visible Only Under a Microscope
Microscopic colitis is a unique form of colitis that can only be definitively diagnosed through microscopic examination of colon tissue samples. Unlike other forms of colitis, the inflammation in microscopic colitis is not visible to the naked eye during endoscopic procedures.
What are the subtypes of microscopic colitis?
Microscopic colitis is generally classified into two main subtypes:
- Lymphocytic colitis: Characterized by an increased number of lymphocytes (a type of white blood cell) in the colon tissue, without significant thickening of the colon lining
- Collagenous colitis: Marked by a thickening of the collagen layer beneath the colon’s lining, in addition to increased lymphocytes
While these subtypes have distinct microscopic features, they often present with similar symptoms and are treated in much the same way.
Who is at risk for developing microscopic colitis?
Several factors may increase an individual’s risk of developing microscopic colitis:
- Age: More common in people over 50
- Gender: More frequently diagnosed in females
- Smoking: Current smokers have a higher risk
- Autoimmune disorders: Having other autoimmune conditions may increase susceptibility
- Medications: Certain drugs, including some PPIs, SSRIs, and NSAIDs, may contribute to the development of microscopic colitis
Understanding these risk factors can help healthcare providers identify individuals who may be more likely to develop microscopic colitis and guide appropriate screening and diagnostic measures.
Allergic Colitis in Infants: A Unique Pediatric Condition
Allergic colitis is a form of colitis that specifically affects infants, typically within the first few months of life. This condition can cause significant discomfort for babies and concern for parents, as its symptoms can be distressing and sometimes alarming.
What are the symptoms of allergic colitis in infants?
The symptoms of allergic colitis in infants can include:
- Excessive spitting up or reflux
- Fussiness and irritability
- Bloody stools (often appearing as small flecks or streaks)
- Changes in bowel habits, such as increased frequency or looser stools
- Poor weight gain or failure to thrive in some cases
These symptoms can vary in severity and may not all be present in every case. It’s important for parents to consult with a pediatrician if they notice any of these signs in their infant.
What causes allergic colitis in infants?
The exact cause of allergic colitis in infants is not fully understood, but researchers believe it is related to an allergic or hypersensitive reaction to certain proteins. These proteins may be present in:
- Breast milk: Proteins from the mother’s diet passing through breast milk
- Cow’s milk-based formula: For formula-fed infants
- Other food proteins: Introduced through solid foods or supplements
A subset of allergic colitis, known as eosinophilic colitis, is characterized by an increased number of eosinophils (a type of white blood cell) in the colon tissue. This condition is also believed to be related to food protein allergies.
How is allergic colitis in infants managed?
Management of allergic colitis in infants typically involves dietary modifications:
- For breastfed infants: Mothers may be advised to follow an elimination diet, removing potential allergens such as dairy, eggs, and wheat from their own diet
- For formula-fed infants: Switching to a hypoallergenic or elemental formula may be recommended
- For infants starting solid foods: Careful introduction of new foods and monitoring for reactions
In most cases, allergic colitis in infants is a temporary condition that resolves as the child’s immune system matures. However, close monitoring and follow-up with a pediatrician or pediatric gastroenterologist are essential to ensure proper growth and development.
Diagnosis and Treatment: Navigating the Management of Colitis
Accurate diagnosis and appropriate treatment are crucial for effectively managing colitis, regardless of its specific type. The diagnostic and treatment approaches may vary depending on the underlying cause and severity of the condition.
How is colitis diagnosed?
Diagnosing colitis typically involves a combination of the following:
- Medical history and physical examination
- Blood tests to check for inflammation markers and rule out other conditions
- Stool samples to look for infections or parasites
- Imaging studies such as CT scans or MRI
- Endoscopic procedures like colonoscopy or flexible sigmoidoscopy
- Biopsy of colon tissue for microscopic examination
The specific diagnostic tests used will depend on the suspected type of colitis and the individual patient’s presentation.
What treatment options are available for colitis?
Treatment for colitis varies based on the type and severity of the condition. Common treatment approaches include:

- Medications:
- Anti-inflammatory drugs (e.g., mesalamine, corticosteroids)
- Immunosuppressants (e.g., azathioprine, biologics)
- Antibiotics for bacterial infections
- Antidiarrheal agents for symptom relief
- Dietary modifications:
- Elimination diets to identify trigger foods
- Increased fluid intake to prevent dehydration
- Probiotics to support gut health
- Lifestyle changes:
- Stress management techniques
- Regular exercise as tolerated
- Smoking cessation
- Surgery:
- Reserved for severe cases or complications
- May involve removal of damaged portions of the colon
The goal of treatment is to reduce inflammation, alleviate symptoms, and prevent complications. Long-term management often involves a combination of medical treatment and lifestyle modifications tailored to the individual patient’s needs.
Can colitis be prevented?
While not all types of colitis can be prevented, certain measures may help reduce the risk or severity of some forms:
- Maintaining good hygiene to prevent infections
- Using antibiotics only when necessary and as prescribed
- Managing underlying health conditions effectively
- Adopting a healthy lifestyle with a balanced diet and regular exercise
- Avoiding known triggers, such as certain foods or medications
- Seeking prompt medical attention for persistent digestive symptoms
By understanding the various types of colitis, their causes, and available treatment options, individuals can work with their healthcare providers to develop effective management strategies. This comprehensive approach can help improve quality of life and reduce the impact of colitis on daily activities.
Colitis: Types, Diagnosis, and Treatment
Colitis occurs when your large intestine is inflamed. It can cause pain and other symptoms, including ulcers, bloating, and diarrhea. Different types of colitis require different treatments.
Colitis is inflammation of your colon, also known as your large intestine. If you have colitis, you’ll feel discomfort and pain in your abdomen. This discomfort may be mild and reoccurring over a long period of time, or severe and appearing suddenly.
There are different types of colitis, and treatment varies depending on what type you have.
The types of colitis are categorized by what causes them.
1. Ulcerative colitis
Ulcerative colitis (UC) is one of two conditions classified as inflammatory bowel disease. The other is Crohn’s disease.
UC is a lifelong disease that causes inflammation and bleeding ulcers within the inner lining of your large intestine. It generally begins in the rectum and spreads to the colon.
UC is the most commonly diagnosed type of colitis. It occurs when the immune system overreacts to bacteria and other substances in the digestive tract, but experts don’t know why this happens.
Common types of UC include:
- proctosigmoiditis, which affects the rectum and lower portion of the colon
- left-sided ulcerative colitis, which affects the left side of the colon beginning at the rectum
- pancolitis, which affects the entire large intestine
2. Pseudomembranous colitis
Pseudomembranous colitis (PC) occurs from overgrowth of the bacterium Clostridium difficile (C. diff). This kind of bacteria normally lives in the intestine, but it doesn’t cause problems because it’s balanced by the presence of “good” bacteria.
Certain medications, especially antibiotics, may destroy healthy bacteria. This allows C. diff to take over, releasing toxins that cause inflammation.
3. Ischemic colitis
Ischemic colitis (IC) occurs when blood flow to the colon is suddenly cut off or restricted. Blood clots can be a reason for sudden blockage. Atherosclerosis, or buildup of fatty deposits in the blood vessels that supply the colon, is usually the reason for returning IC.
Blood clots can be a reason for sudden blockage. Atherosclerosis, or buildup of fatty deposits in the blood vessels that supply the colon, is usually the reason for returning IC.
This type of colitis is often the result of underlying conditions. These may include:
- vasculitis, an inflammatory disease of the blood vessels
- diabetes
- colon cancer
- dehydration
- blood loss
- heart failure
- obstruction or blockage
- trauma or injury
Although it’s rare, IC may occur as a side effect of taking certain medications such as fibrates and nonsteroidal anti-inflammatory drugs (NSAIDs). More research is needed to fully understand all medications that could be a contributing factor.
4. Microscopic colitis
Microscopic colitis is a medical condition that a doctor can only identify by looking at a tissue sample of the colon under a microscope. A doctor will look for signs of inflammation, such as lymphocytes, which are a kind of white blood cell.
Doctors sometimes classify microscopic colitis into two categories: lymphocytic and collagenous colitis.
Lymphocytic colitis is when a doctor identifies a significant number of lymphocytes. However, the colon tissues and lining are not abnormally thickened.
Collagenous colitis occurs when the colon’s lining becomes thicker than usual due to a buildup of collagen under the outermost layer of tissue.
Doctors do not know exactly what causes microscopic colitis. However, they do know some people are more at risk for the condition. People at a higher risk include:
- current smokers
- those assigned female at birth
- those with a history of an autoimmune disorder
- people older than age 50
- people taking certain medications, such as some types of:
- proton pump inhibitors (PPIs)
- selective serotonin reuptake inhibitors (SSRIs)
- nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin
The most common symptoms of microscopic colitis are:
- chronic watery diarrhea
- abdominal bloating
- abdominal pain
5.
 Allergic colitis in infants
Allergic colitis in infants
Allergic colitis is a condition that can occur in infants, usually within the first months after birth. The condition can cause symptoms in infants including:
- reflux
- excessive spitting up
- fussiness
- possible flecks of blood in a baby’s stool
Doctors don’t know exactly what causes allergic colitis. One of the most popular theories is that infants with allergic colitis have an allergic or hypersensitive reaction to certain components in breast milk. A 2020 review of studies indicated that a protein allergy, either through breast milk, cow’s milk, or formula, could contribute.
Eosinophilic colitis is a type of allergic colitis that can also show up in infants with these symptoms. Its causes are similarly unknown, but it’s likely also related to a protein allergy.
Doctors will often recommend an elimination diet for the birthing parent, which involves slowly cutting out certain foods known to contribute to allergic colitis. Examples include cow’s milk, eggs, and wheat. If the baby stops having symptoms of allergic colitis, these foods were likely causing the problem.
Examples include cow’s milk, eggs, and wheat. If the baby stops having symptoms of allergic colitis, these foods were likely causing the problem.
In severe cases, monoclonal antibodies, such as those used to help treat inflammatory bowel disease (IBD), may also be another treatment option.
Additional causes
Other causes of colitis include infection from parasites, viruses, and food poisoning from bacteria. You may also develop the condition if your large intestine has been treated with radiation.
Different risk factors are associated with each type of colitis.
You’re more at risk for UC if you:
- are between the ages of 15 and 30 (most common) or 60 and 80
- are white or of Ashkenazi Jewish descent
- have a family member with UC
You’re more at risk for PC if you:
- are taking long-term antibiotics
- are hospitalized
- are receiving chemotherapy
- are taking immunosuppressant drugs
- are older
- have had PC before
You’re more at risk for IC if you:
- are over age 50
- have or are at risk of heart disease
- have heart failure
- have low blood pressure
- have had an abdominal operation
Depending on your condition, you may experience one or more of the following symptoms:
- abdominal pain or cramping
- bloating in your abdomen
- unexpected weight loss
- diarrhea with or without blood
- blood in your stool
- urgent need to move your bowels
- chills or fever
- vomiting
A doctor may ask about the frequency of your symptoms and when they first started. The doctor will perform a thorough physical exam and use diagnostic tests such as:
The doctor will perform a thorough physical exam and use diagnostic tests such as:
- colonoscopy, which involves threading a camera on a flexible tube through the anus to view the rectum and colon
- sigmoidoscopy, which is similar to a colonoscopy but shows only the rectum and lower colon
- stool samples
- abdominal imaging such as MRI or CT scans
- ultrasound, which can be useful depending on the area being scanned
- barium enema, an X-ray of the colon after it’s injected with barium, which helps make images more visible
Treatments aim to reduce symptoms and can vary by factors such as:
- type of colitis
- age
- overall physical condition
Bowel rest
Limiting what you consume by mouth can be useful, especially if you have IC. Taking fluids and other nutrition intravenously may be necessary during this time.
Medication
Your doctor may prescribe various medications to help manage colitis symptoms.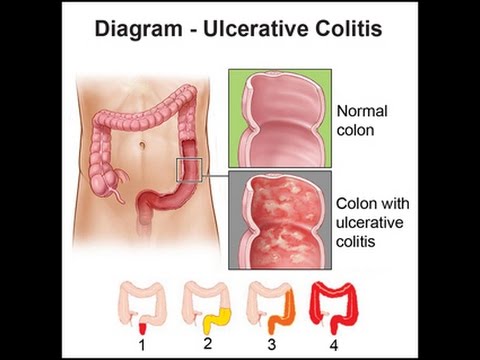 These may medications include:
These may medications include:
- anti-inflammatory medication such as 5-aminosalicylates or corticosteroids to treat swelling and pain
- immune system suppressors such as tofacitinib (Xeljanz), azathioprine (Azasan, Imuran), or cyclosporine (Gengraf, Neoral, Sandimmune)
- biologics such as infliximab (Remicade), adalimumab (Humira), and ustekinumab (Stelara)
- antibiotics to treat infection
- pain medications
- antidiarrheal medications
- antispasmodic drugs
- supplements for nutritional deficiencies
Surgery
Surgery for colitis could include removing part or all of your colon or rectum. This may be necessary if other treatments don’t work. These surgeries could include:
- ileal pouch-anal anastomosis (IPAA), in which the ileum (the end of the small intestine) is turned into a pouch that then connects to the anal canal
- proctocolectomy, in which the colon (and sometimes the rectum) are removed
- ileostomy, in which the ileum is connected to the abdominal wall, and a stoma (an opening in the abdomen) is created to allow waste to leave the body
- continent ileostomy, in which the end of the ileum is secured inside the interior of the abdomen.
 This is a possible but uncommon surgical procedure for colitis.
This is a possible but uncommon surgical procedure for colitis.
The only definitive way to prevent a colitis flare-up is to have surgery. If you’re looking to prevent flare-ups without surgery, there are ways to decrease their likelihood:
- Keep a food log to track which foods may cause an increase in symptoms.
- Ask your doctor if you should change your fiber intake and how much to eat.
- Ask your doctor if eating smaller meals more frequently will help you.
- Increase your activity levels if you can.
- Learn ways to help manage stress such as meditation, yoga, and mindfulness exercises.
- Always take medications as prescribed and tell your doctor if you have not.
- Make sure your doctor knows about all of your other medications and supplements, including vitamins.
Always check with your doctor before changing your diet or adding any new supplements.
While every person may experience diarrhea and abdominal cramps from time to time, speak with a doctor if you have diarrhea that does not seem to be related to an infection, fever, or any known contaminated foods.
Other symptoms that indicate it’s time to see a doctor include:
- joint pain
- rashes that have no known cause
- small amount of blood in your stool, such as slightly red-streaked stool
- stomach pain that keeps coming back
- unexplained weight loss
Seek immediate medical attention if you see a significant amount of blood in your stool.
In all cases, early detection is critical to recovery. Early detection may help prevent other serious complications.
If you feel that something is not right with your stomach, it’s best to talk with a doctor. Listening to your body is important to staying well.
Read this article in Spanish.
Symptoms, Triggers, Treatment, and More
Colitis occurs when your colon, or large intestine, is inflamed.
Microscopic colitis is a type of colitis that’s best identified by looking at colon cells under a microscope. The main subtypes of microscopic colitis are collagenous colitis and lymphocytic colitis.
In collagenous colitis, a thick layer of collagen — a type of connective protein — forms within the colon tissue. Its symptoms can disappear and reappear.
Lymphocytic colitis occurs when the colon contains a large number of lymphocytes, which are types of white blood cells. Learn more about it and other forms of colitis.
The symptoms of collagenous colitis can come and go, and vary in severity.
The most common symptoms include:
- chronic watery diarrhea, which can appear and disappear over a period of weeks, months, or years
- abdominal pain
- abdominal cramps
Less common symptoms include:
- dehydration
- weight loss
- bloating
- flatulence or gas
- nausea
- vomiting
- fatigue
- an urgent need to go to the bathroom
- fecal incontinence
Like many other gastrointestinal conditions, the exact cause of collagenous colitis is unknown. Research indicates that it likely has a genetic basis and could be related to autoimmune conditions.
Some possible causes of collagenous colitis include:
- genetic abnormalities
- autoimmune conditions such as rheumatoid arthritis, psoriasis, and Crohn’s disease
- certain bacteria or viruses
- smoking
Collagenous colitis isn’t contagious. It can’t spread to other people.
Medications as triggers
Medications that may trigger microscopic colitis and collagenous colitis include:
- nonsteroidal anti-inflammatory drugs (NSAIDs)
- selective serotonin reuptake inhibitors (SSRIs), the most commonly prescribed class of antidepressants
- angiotensin-converting enzyme (ACE) inhibitors for high blood pressure
- angiotensin II receptor blockers (ARBs) for high blood pressure, heart disease, or kidney disease
Research is mixed on the effects of the following medications:
- statins for high cholesterol
- protein pump inhibitors (PPIs) and h3 receptor blockers, which are used to treat acid reflux and GERD
- oral medications for diabetes
Some research states that they have little to no effect on microscopic colitis, or may even be associated with lower rates of the condition.
Other studies indicate that these medications also trigger microscopic colitis and collagenous colitis.
According to a 2021 study, if these medications are associated with increased rates of microscopic colitis and collagenous colitis, it may be because they make diarrhea worse. A worsening case of diarrhea then prompts a doctor to make a diagnosis of colitis.
Collagenous colitis is more common among women than men. It’s also more common among people who are over 50 years old.
In addition, people who have celiac disease are more likely to have collagenous colitis.
Collagenous colitis may also be more common among people who currently smoke and people with a family history of the condition.
Researchers have noticed that the number of collagenous colitis cases is increasing. This may be because better detection is available and there’s increased awareness of the condition.
Collagenous colitis can only be diagnosed with a biopsy of the colon. You’ll likely also have a colonoscopy or sigmoidoscopy so that the doctor can better evaluate the health of your colon.
During the biopsy, a healthcare professional removes several small pieces of tissue from your colon. Then the tissues are examined under a microscope.
The common diagnostic process includes:
- a medical history
- colonoscopy with a biopsy
- lab tests, such as blood and stool tests
- imaging tests, such as CT scans, MRIs, or X-rays
- endoscopy
Some tests and procedures are used to rule out other medical conditions that may cause similar symptoms, such as irritable bowel syndrome (IBS) and the infection Clostridium difficile (C. diff).
In some cases, collagenous colitis disappears on its own. However, some people need treatment.
Your treatment plan will depend on the severity of your symptoms.
Diet and lifestyle changes
Your doctor may recommend diet and lifestyle changes to help treat this condition. These changes are usually the first part of any treatment plan.
Common diet changes include:
- eating a reduced fat diet
- opting for a gluten-free diet
- drinking more fluids to prevent dehydration from diarrhea
- switching to a milk-free diet
- avoiding food with artificial sweeteners
- eliminating caffeine and lactose
Common lifestyle changes include:
- quitting smoking, if you smoke
- maintaining a moderate weight
- maintaining a healthy blood pressure
- exercising regularly
Medication
Your doctor will review the medications you currently take and make suggestions about either continuing or stopping them.
In 2016, the American Gastroenterological Association (AGA) released its guidelines on microscopic colitis. The AGA recommends starting with budesonide, a type of corticosteroid, before considering other medications.
Other medications your doctor may recommend to help treat the symptoms of collagenous colitis include:
- antidiarrheal medications
- intestinal anti-inflammatory medications, such as mesalamine (Apriso, Asacaol HD, Pentasa) or sulfasalazine (Azulfidine)
- antibiotics
- medications that block bile acids, such as cholestyramine (Prevalite)
The supplement psyllium may be recommended, too. Immunomodulators or anti-TNF (tumor necrosis factor) therapies may be used in extreme cases.
The Food and Drug Administration (FDA) hasn’t approved any medications for microscopic colitis or collagenous colitis. However, medications such as mesalamine and sulfasalazine are FDA approved for the treatment of ulcerative colitis.
If a doctor prescribes medications such as these for collagenous colitis, it’s considered an example of off-label drug use.
OFF-LABEL DRUG USE
Off-label drug use means a drug that’s approved by the FDA for one purpose is used for a different purpose that hasn’t yet been approved.
However, a doctor can still use the drug for that purpose. This is because the FDA regulates the testing and approval of drugs, but not how doctors use drugs to treat their patients. So your doctor can prescribe a drug however they think is best for your care.
Surgery
Your doctor may recommend surgery if diet and medication changes don’t help. Surgery is usually reserved for extreme cases. It’s not a typical treatment for collagenous colitis.
The most common types of surgery for collagenous colitis include:
- colectomy, which means removing all or part of the colon
- ileostomy, which means creating an opening in the abdomen after a colectomy
Collagenous colitis doesn’t cause blood in your stool, increase your risk of colon cancer, or have any effect on life expectancy. Symptoms may affect a person’s quality of life, but they’re not life threatening and won’t typically require emergency medical care.
Symptoms may affect a person’s quality of life, but they’re not life threatening and won’t typically require emergency medical care.
However, it’s worth seeing a doctor if you have chronic watery diarrhea in combination with any of the common risk factors for collagenous colitis.
You’ll also want to see a doctor if you’re diagnosed with collagenous colitis and your recommended treatment plan doesn’t help reduce your symptoms.
Collagenous colitis can come and go, and relapses are common. You may need to try several treatments to find relief from the symptoms.
The time it takes to recover can vary. Some people may have symptoms for weeks, months, or years.
There are no current recommendations for preventing collagenous colitis. However, following the diet and medication changes recommended by your doctor may reduce your likelihood of having a relapse.
Read this article in Spanish.
Intestinal colitis – types, causes, symptoms, signs, complications, diagnosis, treatment, prevention
Infectious
Ischemic
Ulcerative
Radiation
Toxic
Spastic
Complications
Diagnosis
Treatment
Prevention
Colitis is an inflammatory disease of the colon mucosa.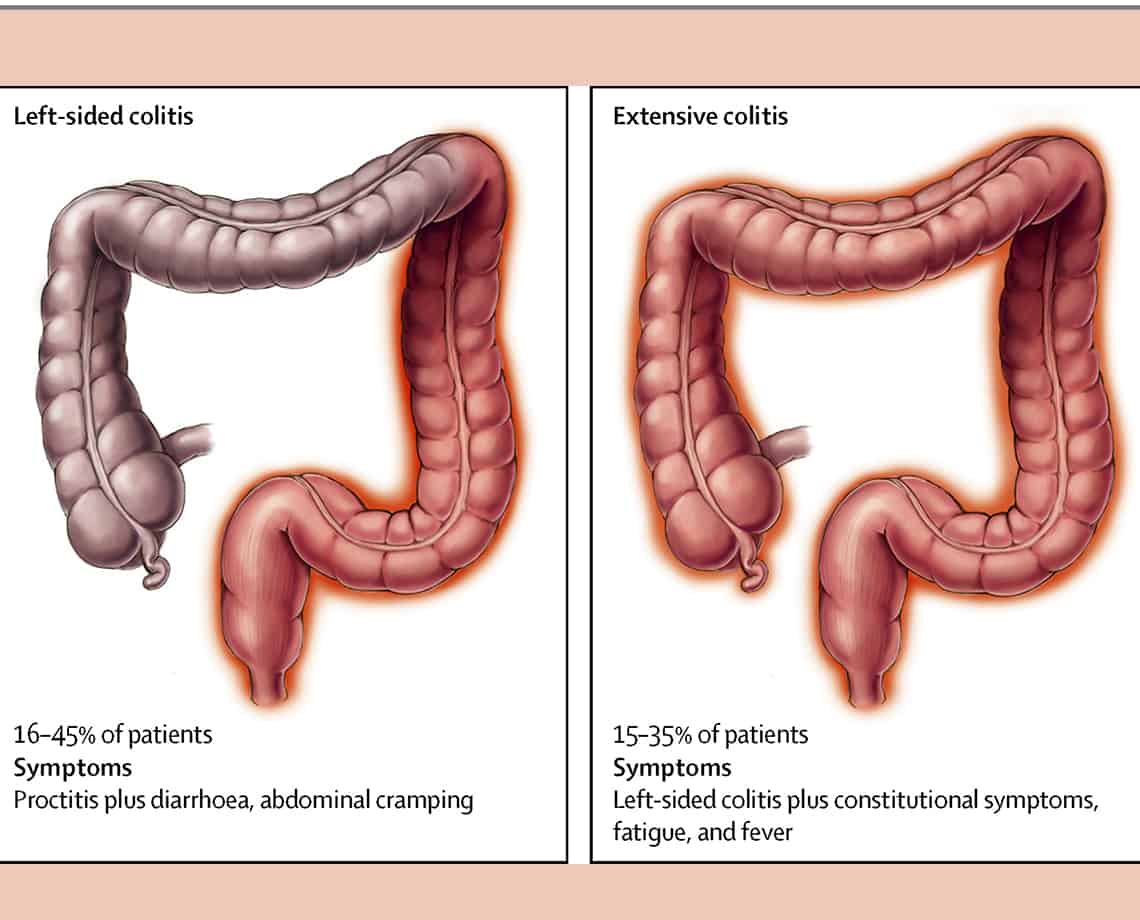 Signs of such an inflammatory process are frequent loose bloody stools, abdominal pain and fever. The causes of colitis can be very different, so this term in medicine hides several diseases that share common symptoms.
Signs of such an inflammatory process are frequent loose bloody stools, abdominal pain and fever. The causes of colitis can be very different, so this term in medicine hides several diseases that share common symptoms.
Infectious colitis
This is one of the most common variants of pathology that occurs at the time of activation of the conditionally pathogenic microflora located in the gastrointestinal tract. Most often, the disease is diagnosed in the summer, as well as while traveling to other countries.
Causes of development – bacteria, viruses, protozoa, including Koch’s bacillus, spirochete, fungus and dysbacteriosis. There are several forms of infectious inflammation of the large intestine – catarrhal, fibrinous, catarrhal-hemorrhagic, phlegmonous, phlegmonous-gangrenous and necrotic.
This type of colitis has certain symptoms, but they will depend on which microorganism has caused the inflammatory process. Common to all will be such manifestations as an acute onset, diarrhea, abdominal pain in the form of cramps, fever, deterioration of health. To identify what caused the disease, it is necessary to do a fecal analysis. This will help to prescribe specific treatment.
To identify what caused the disease, it is necessary to do a fecal analysis. This will help to prescribe specific treatment.
Ischemic colitis
Inflammation appears in the wall of the large intestine due to circulatory disorders, which can be acute or chronic. In a severe case and without timely treatment, this can cause necrosis. The main cause of circulatory disorders is blockage of the vessel by a thrombus. According to statistics, most cases of this pathology are diagnosed at the age of 50 years.
The size of the lesion will depend on the size of the occluded vessel, the duration of ischemia, and the speed at which a doctor is consulted. There is transient ischemia, in which all processes can be reversed without consequences, stenosing with the formation of a stricture, and gangrenous, when damage to the intestinal wall is irreversible and ends with tissue death.
Ulcerative colitis
Ulcerative colitis is a chronic inflammation of unknown origin. The main manifestation is the appearance on the mucous membrane of the large intestine of ulcers of various sizes and depths of the lesion. The disease proceeds in cycles with periods of exacerbation and remission.
The main manifestation is the appearance on the mucous membrane of the large intestine of ulcers of various sizes and depths of the lesion. The disease proceeds in cycles with periods of exacerbation and remission.
Long-term ulcer pathology increases the risk of developing cancer by several times. It is most often diagnosed in women and occurs with a frequency of up to 80 cases per 100,000 people. Primary detection is typical in two age groups. The first group – young people aged 15 to 25 years, the second – people over 55 years old. For what reasons this form begins to form is still unknown, but doctors suggest two provoking factors – genetic and immune.
Radiation colitis
This species occurs in people who have undergone radiation therapy for the treatment of malignant tumors of the pelvis or intestines. However, not the entire large intestine is damaged, but only the sigmoid and rectum. According to the clinical picture, such inflammation is similar to an ischemic or ulcerative form.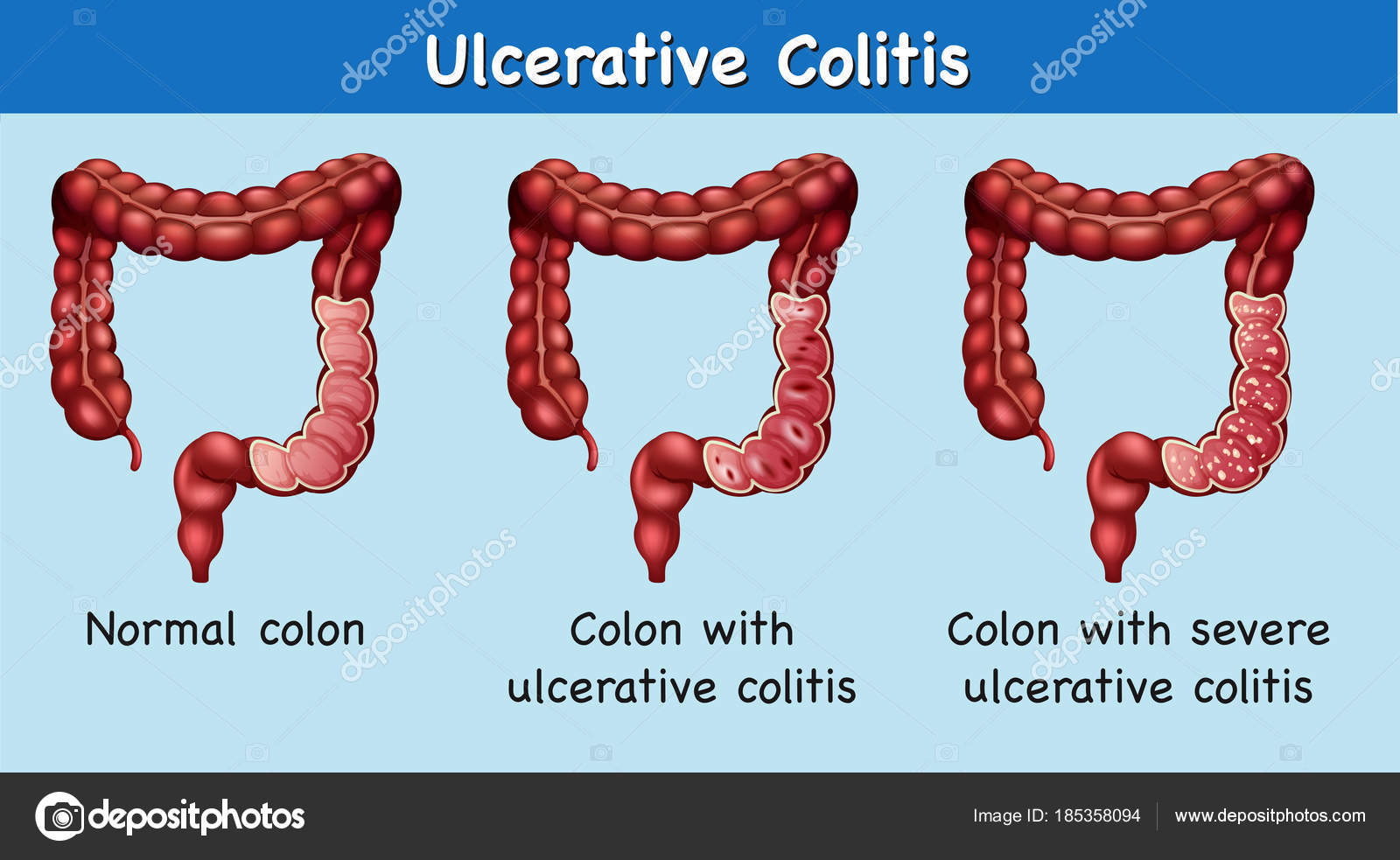
Signs of radiation colitis do not develop immediately and begin to manifest themselves by the end of radiation therapy. The patient begins to complain of copious loose stools. The absorption of nutrients in the large intestine is severely impaired, which causes anemia, weight loss, and loss of appetite.
The risk of developing inflammation depends on the dose of radiation used, as well as the duration and location of exposure. An important role is played by the individual sensitivity of the organism to the level of increased radiation.
Toxic colitis
Often in adults there is toxic colitis, which is also called medicinal. This is one of the complications when taking certain groups of drugs. There are no specific symptoms that would help to quickly make a diagnosis, the main complaints are pain in the left half of the abdomen from below, profuse diarrhea, bloating, general weakness, fatigue.
Most often, this disease occurs against the background of taking antibacterial drugs, laxatives, cytostatics, NSAIDs, drugs for high blood pressure. Pathology against the background of taking medications can develop acutely or gradually. In some cases, toxic hepatitis or pancreatitis joins.
Pathology against the background of taking medications can develop acutely or gradually. In some cases, toxic hepatitis or pancreatitis joins.
Spastic colitis
Colitis in children most often has the character of spastic. In addition to a painful attack, the patient complains of bloating, flatulence, rumbling in the abdomen. Belching may occur, diarrhea is characteristic, but in some cases, due to impaired motor skills, constipation is diagnosed. Against this background, there is no appetite, lethargy appears, body temperature may rise.
In infants, this disease develops against the background of artificial feeding. The child becomes restless, cries, tries to pull the legs to the stomach, strongly strains the muscles of the anterior abdominal wall. Other extraintestinal symptoms may also join – excessive sweating, headache, tachycardia.
Possible complications
Do not think that colitis is just an inflammatory disease. This is a serious pathology, which is dangerous for its many complications, and without treatment, they can appear at any time.
Most often, patients with colitis suffer from the following complications:
- severe intestinal bleeding;
- abrasion of the mucosa before the appearance of perforation;
- dehydration;
- osteoporosis;
- inflammation of the skin, joints and eyes;
- the likelihood of developing colon cancer;
- development of toxic megacolon;
- the risk of blood clots in the veins of the intestine.
Diagnosis
To diagnose this pathology, it is necessary not only to pass urine, blood and feces tests, but also to undergo other examinations. Most often, patients are prescribed sigmoidoscopy. This method allows you to quickly and with great accuracy assess the condition of the mucosa, detect pinpoint hemorrhages on it, change in color and vascular pattern. Also, this method helps to take a biopsy for further analysis. It is used to diagnose colitis of the rectum and sigmoid colon.
Irrigoscopy is an x-ray technique that allows you to assess the location and size of the colon, its functional features and existing disorders.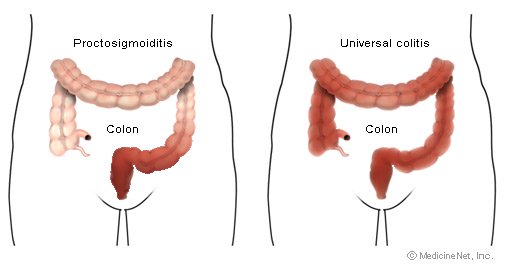 It is carried out using a contrast agent, and the result can be seen on a conventional x-ray.
It is carried out using a contrast agent, and the result can be seen on a conventional x-ray.
Colonoscopy is a diagnostic method during which the doctor examines and evaluates the condition of the mucous surface of the large intestine. In addition to diagnosis, this method also allows you to take a biopsy and remove small polyps on the walls of the intestine.
Treatment
Unfortunately, today there is no single treatment regimen for colitis of various origins. Therefore, all therapy is carried out depending on what provoked the disease.
For the infectious form, it will be taking antibiotics or antifungal drugs, depending on the sensitivity of the microflora. Replenishment of fluid is carried out using special solutions for drinking. Probiotics and prebiotics help to normalize the microflora, and sorbents remove toxins. Symptomatic therapy is prescribed depending on the symptoms present. Colitis pain is relieved with painkillers.
Ischemic colitis may require surgical treatment, and ulcerative colitis requires long-term therapy, diet and removal of the inflammatory process.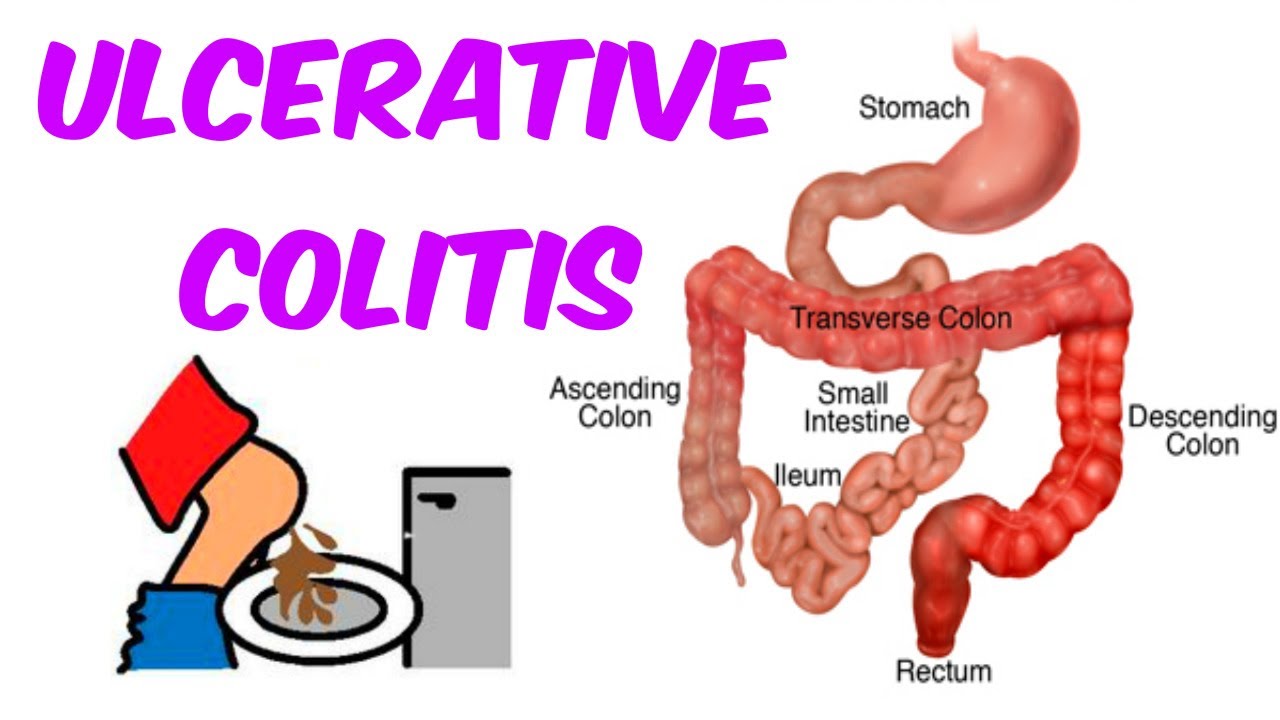 Medicines for colitis in this case are prescribed only by a gastroenterologist, because the disease progresses rapidly, and surgery may be required in the later stages.
Medicines for colitis in this case are prescribed only by a gastroenterologist, because the disease progresses rapidly, and surgery may be required in the later stages.
The toxic form requires a review of the dose of the drug taken, drug withdrawal or replacement with another. Spastic – treated with antispasmodics, enzyme preparations, enterosorbents and drugs that help relieve inflammation.
Prevention
Inflammation of the colon is a very preventable disease. Prevention of colitis includes maintaining an active lifestyle, proper nutrition, avoiding fast food snacks and the mandatory inclusion of soups in the diet. It is recommended to always monitor the state of the psyche, try not to worry, treat stress and depression in a timely manner. It is necessary to observe hygiene measures, wash your hands more often and take tests for helminths once a year.
When the first unpleasant symptoms appear in the area of the stomach or intestines, you should immediately contact a general practitioner or gastroenterologist.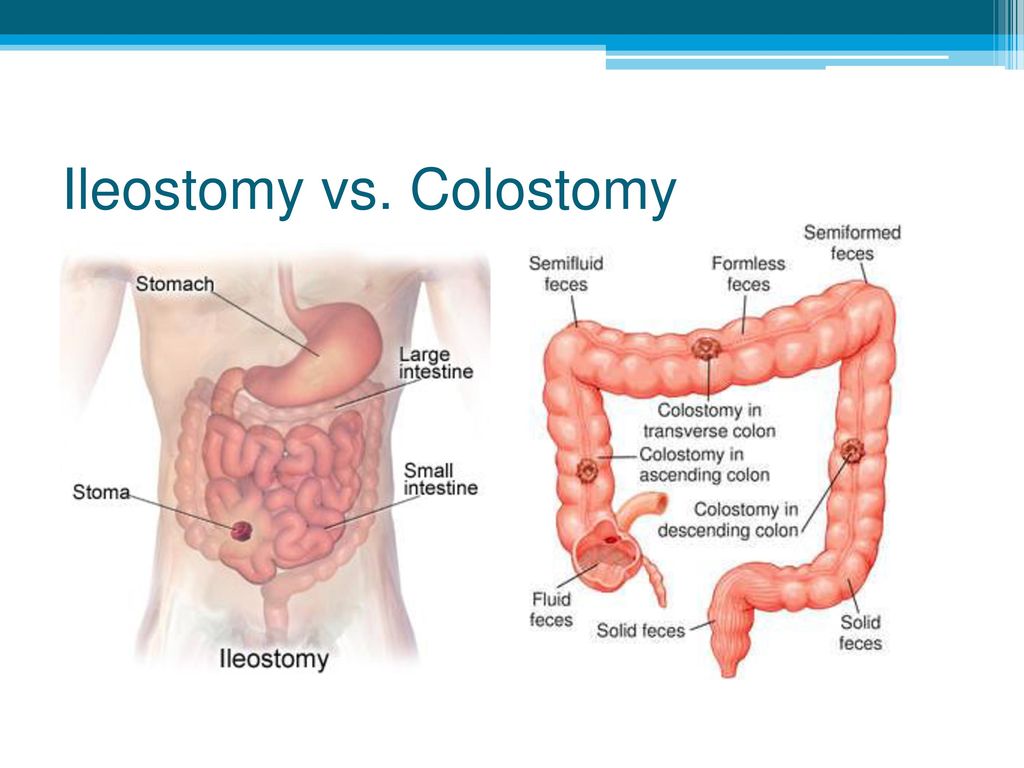
The author of the article:
Nikitina Olga Ivanovna
therapist, gastroenterologist, Ph.D.
work experience 5 years
reviews leave a review
Clinic
m. Street 1905 Goda
Reviews
Services
- Title
- Primary appointment (examination, consultation) with a gastroenterologist2300
- Repeated appointment (examination, consultation) with a gastroenterologist1900
Health articles
All articlesAllergistGastroenterologistHematologistGynecologistDermatologistImmunologistInfectionistCardiologistCosmetologistENT doctor (otolaryngologist)MammologistNeurologistNephrologistOncologistOphthalmologistProctologistPsychotherapistPulmonologistRheumatologistTraumatologist-orthopedistTrichologistUrologistPhlebologistSurgeonEndocrinologist
Our doctors
Specialization of the doctorAllergistAndrologistAnesthetistPediatrician house callPaediatrician house callGastroenterologistHematologistGynecologistBreastfeedingDermatologistPediatric allergologistPediatric gastroenterologistPediatric gynecologistPediatric dermatologistPediatric infectious disease specialistPediatric cardiologistPediatric ENT specialistPediatric chiropractorPediatric massagePediatric neurologistPediatric neurologist phrologistPediatric oncologistPediatric osteopathPediatric ophthalmologistPediatric psychiatristPediatric traumatologistPediatric urologistPediatric surgeonPediatric endocrinologistPediatric departmentDietologistImmunologistInfectionistHeadache roomCardiologistCosmetologistENT doctor (otolaryngologist)MammologistManual therapistMassageNarcologistNeurologistNeurologistNephrologistOncologistOperational unitOsteopathOt department of pediatrics m.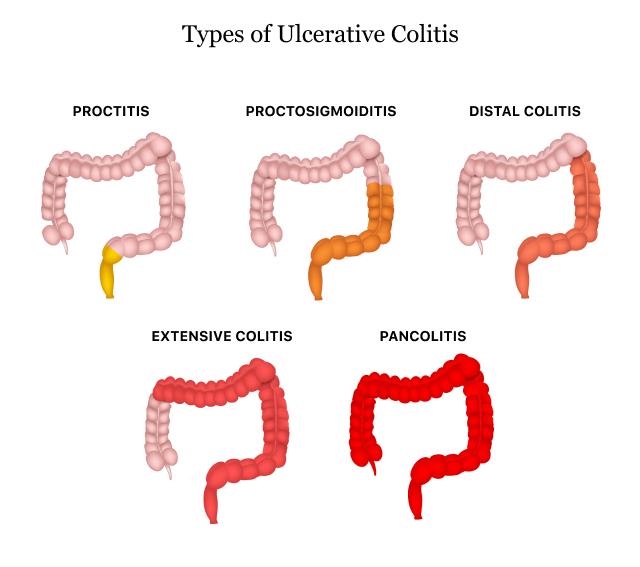 TherapistTraumatologist-orthopedistTrichologistUltrasound (ultrasound examination)UrologistPhysiotherapistPhlebologistSurgeonEndocrinologistAesthetic gynecologyClinics. Smolensk. Taganskaya. Street 1905 years. Red Gates. AvtozavodskayaPharmacy. Glades. Sukharevskaya. st. Academician Yangelam. Frunzenskaya Zelenograd
TherapistTraumatologist-orthopedistTrichologistUltrasound (ultrasound examination)UrologistPhysiotherapistPhlebologistSurgeonEndocrinologistAesthetic gynecologyClinics. Smolensk. Taganskaya. Street 1905 years. Red Gates. AvtozavodskayaPharmacy. Glades. Sukharevskaya. st. Academician Yangelam. Frunzenskaya Zelenograd
Kushnir Maria Vadimovna
gastroenterologist
reviews
Make an appointment
Clinic
Zelenograd
Tsurgan Anastasia Vasilievna
gastroenterologist
reviews
Make an appointment
Clinic
m. Street 1905 Goda
Marzoeva Diana Mairbekovna
gastroenterologist
reviews
Make an appointment
Clinic
m. Red Gate
Bonadyseva Tatyana Mikhailovna
gastroenterologist
reviews
Make an appointment
Clinic
m.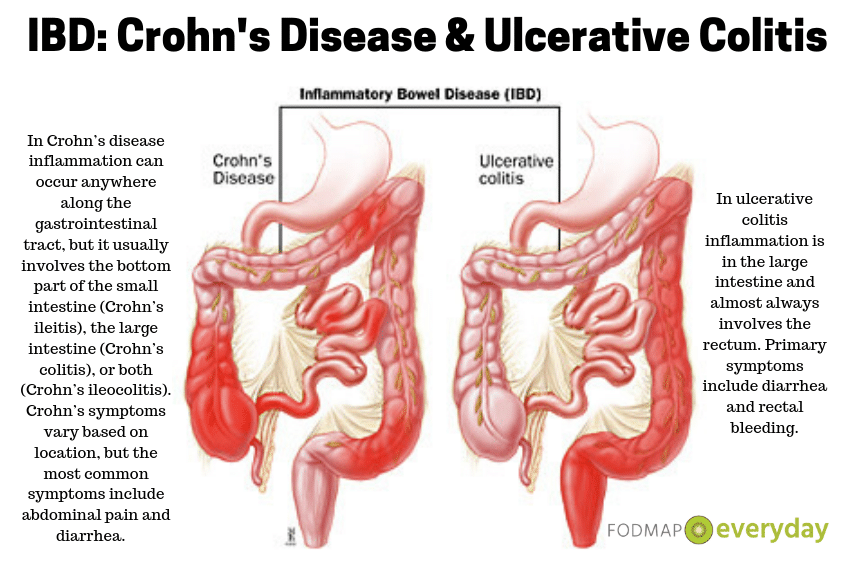 Smolenskaya
Smolenskaya
Stolbova Tatyana Sergeevna 1905, therapist, gastroenterologist
reviews
Clinic
m. Street 1905 Goda
Pogosyan Victoria Eduardovna
gastroenterologist
reviews
Make an appointment
Clinic
m. Red Gate
Matveeva Yulia Evgenievna
gastroenterologist, endoscopist
reviews
Make an appointment
Clinic
m. Sukharevskaya
Grishchenko Ekaterina Borisovna
gastroenterologist, Ph.D.
reviews
Make an appointment
Clinic
m. Avtozavodskaya
Gabulova Natalya Nikolaevna
gastroenterologist
reviews
Make an appointment
Clinic
m. Taganskaya
Taganskaya
Kataev Sergey Semenovich
Doctor-gastroenterologist, therapist Professor, DMN
reviews
Make an appointment
Clinic
m. Frunzenskaya
types, symptoms, complications, diagnosis and treatment methods
- Causes
- Varieties
- Infectious colitis
- Ischemic colitis
- Toxic colitis
- Spastic colitis
- UC (nonspecific ulcerative colitis)
- Symptoms
- Complications
- Diagnostics
- Treatment
- Surgical treatment
- Nutrition for colitis
- What not to eat with colitis
Image by graystudiopro1 on Freepik
Colitis is a disease that affects the large intestine, causing inflammation of the mucous membrane. The disease can occur in acute and chronic form.
The entire intestine or its individual sections may be involved in the pathological process.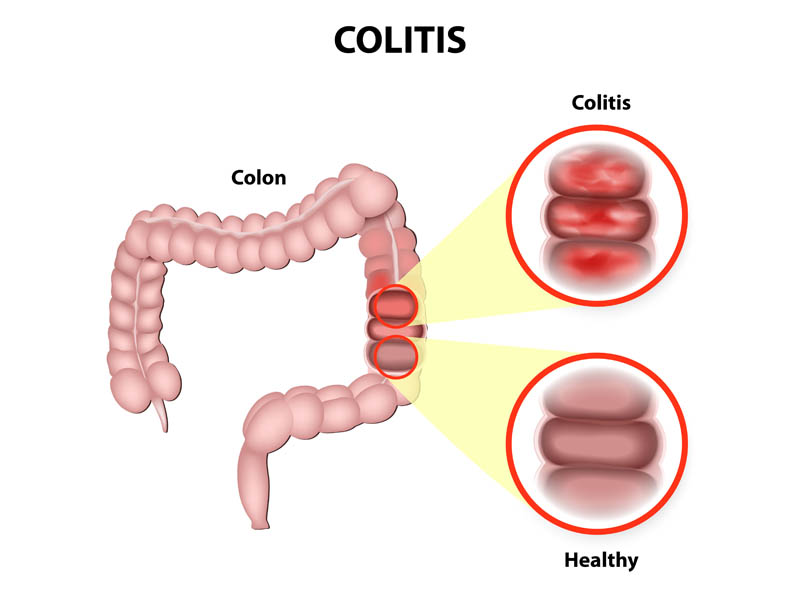 Thus, colitis is a common name for a whole group of diseases:
Thus, colitis is a common name for a whole group of diseases:
- pancolitis – affection of the entire large intestine;
- sigmoiditis – inflammation of the sigmoid colon;
- typhlitis – inflammation of the caecum;
- transverse – damage to the colon;
- proctitis – inflammation of the rectum;
- enterocolitis – inflammation of the small and large intestines.
Causes
Colitis is a multifactorial disease. It occurs for one reason or a combination of them. The disease is provoked by:
- intestinal infections;
- malnutrition;
- allergens;
- drug abuse;
- toxins;
- helminths;
- unfavorable ecology;
- psycho-emotional overload;
- violation of the blood supply to the intestines.
Recently, doctors have noted an increase in the number of patients diagnosed with colitis.
Experts attribute this to the peculiarities of the lifestyle of the inhabitants of the metropolis.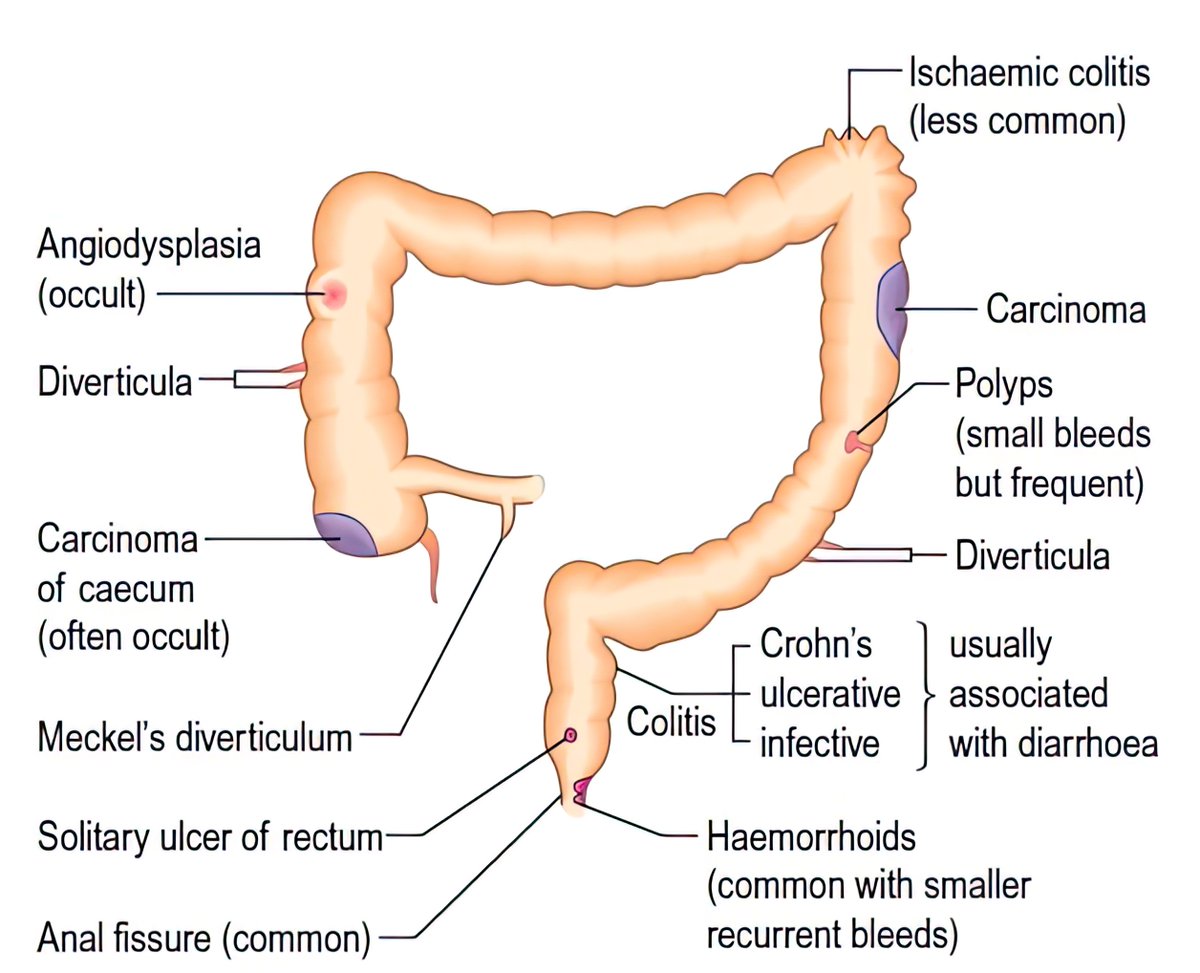 Many people who have a sedentary job experience a regular lack of movement. This negatively affects the blood circulation of organs and systems.
Many people who have a sedentary job experience a regular lack of movement. This negatively affects the blood circulation of organs and systems.
The situation is aggravated by nutrition with an abundance of canned, fatty and spicy foods, and alcoholic beverages.
However, in some cases, the disease occurs for unknown reasons without apparent reason. Experts are sure that the cause of this phenomenon is unfavorable heredity, improper functioning of the immune system, which attacks its own cells.
Varieties
Depending on the cause of the pathology, there are several types of colitis: infectious, ischemic, toxic, spastic and NUC (ulcerative colitis).
Infectious colitis
This is the most common type of the disease. It is provoked by pathogenic bacteria, helminths or fungi. Infection occurs through the use of poor-quality food and drinking water.
The danger is poorly washed vegetables and fruits, uncooked meat and fish, raw eggs, confectionery. They can serve as a source of salmonella and shigella – bacteria that affect the intestinal tract and cause acute infectious diseases (salmonellosis).
They can serve as a source of salmonella and shigella – bacteria that affect the intestinal tract and cause acute infectious diseases (salmonellosis).
Colitis also develops when streptococcal and staphylococcal infections, Escherichia coli enter the intestine.
Non-compliance with the rules of personal hygiene, improper storage and preparation of products can lead to helminthiases – infection with worms. Children are most susceptible to this disease. Worm infestation negatively affects the health of the whole organism, but the intestines suffer first of all.
A variety of infectious colitis is hemorrhagic. It is caused by certain strains of E. coli, which can be ingested through unpasteurized milk or beef. The pathogen produces a toxin that can damage the walls of blood vessels, which leads to inflammation of the intestines, acute diarrhea with blood.
Regardless of the type of pathogen, infectious colitis proceeds rapidly, is characterized by pronounced symptoms.
Ischemic colitis
This is a very dangerous type of colitis, which is caused by narrowing of the mesenteric arteries. At risk – people of mature age, patients with atherosclerosis. With ischemic colitis, there is an immediate threat to life due to circulatory disorders and the development of necrosis of the intestinal wall.
Toxic colitis
The ingestion of toxic substances into the body, the use of potent drugs can lead to inflammation of the intestines. At risk are workers in hazardous industries, patients taking non-steroidal anti-inflammatory drugs, antibiotics. Inflammation can develop against the background of radiation sickness in people living in a zone of radioactive contamination. Intoxication inhibits the normal intestinal microflora, which provokes the development of pathogenic microbes.
Spastic colitis
The main cause of inflammation is a violation of intestinal motility, that is, motor function. This leads to spasms that cause pain. People who are prone to anxiety and fears are susceptible to such a disease, since the main factor in the development of pathology is psychosomatics.
People who are prone to anxiety and fears are susceptible to such a disease, since the main factor in the development of pathology is psychosomatics.
UC (ulcerative colitis)
The disease is characterized by inflammation and bleeding of the colon. The main reason is the autoimmune process, hereditary predisposition to the disease. Any infection can provoke an immune response.
Symptoms
Symptoms of colitis depend on the form of the disease. Acute colitis manifests itself as fever, intoxication, stool disorder, abdominal pain, flatulence. A pronounced sign of inflammation is frequent bowel movements with blood impurities.
If the disease becomes chronic, the symptoms become less pronounced. Patients note frequent stool disorders, which can be manifested by constipation and diarrhea. There are pains on the sides, which are aggravated by defecation. After eating, there is bloating, rumbling. Many patients with colitis complain of a feeling of incomplete bowel movement after a bowel movement.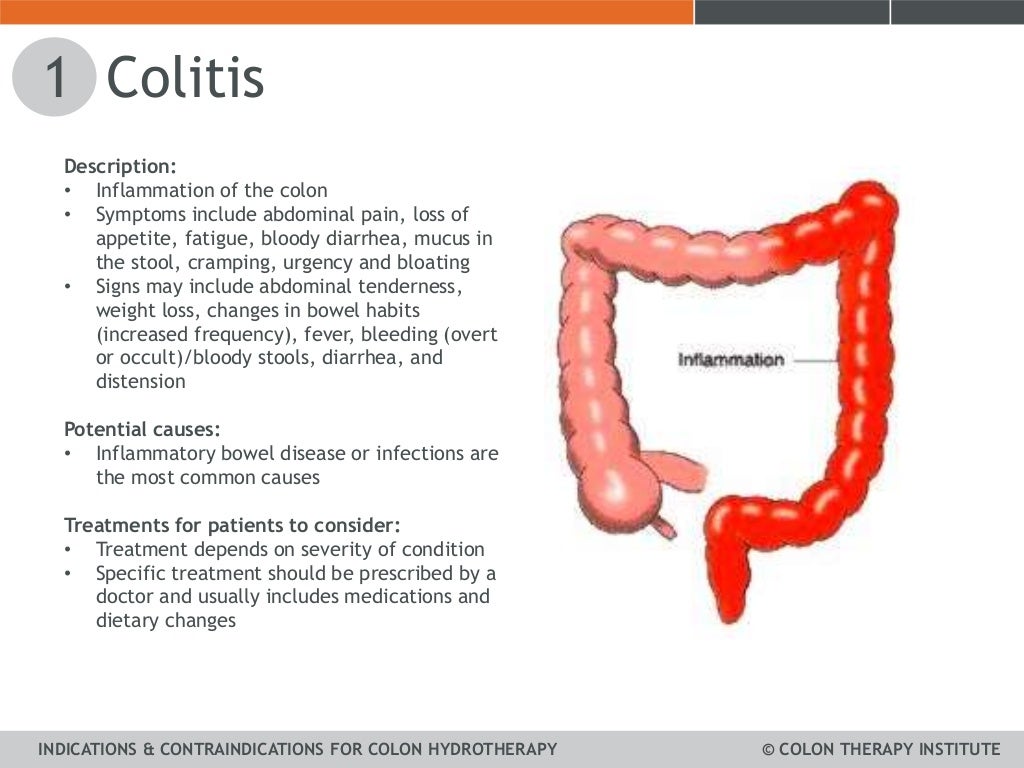 Against the background of the disease, appetite decreases, which can lead to weight loss. Due to intoxication, the patient experiences weakness, decreased performance.
Against the background of the disease, appetite decreases, which can lead to weight loss. Due to intoxication, the patient experiences weakness, decreased performance.
Complications
Colitis can cause life-threatening and health complications:
- Prolonged diarrhea deprives the body of moisture, prevents the absorption of nutrients. The patient may develop dehydration and other dangerous complications.
- Damage to the blood vessels of the colon leads to bleeding, which increases the risk of anemia.
- Prolonged inflammation leads to thinning of the intestinal wall and its perforation. Through the hole, the contents of the intestine enter the abdominal cavity, causing peritonitis.
- Toxic megacolon – an enlargement of the colon – interferes with the normal functioning of the intestine and requires urgent surgical intervention.
- Patients with chronic colitis are more likely to develop colon cancer.
Diagnosis
A gastroenterologist deals with the treatment of intestinal diseases.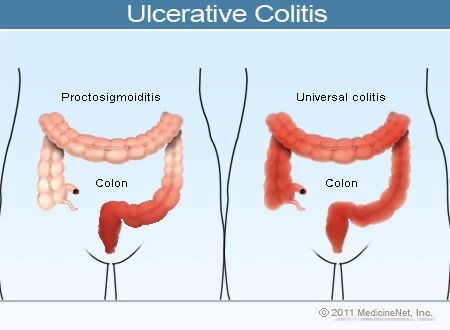 With signs of colitis, the doctor examines the patient, feels the stomach. Clinical analyzes of urine and feces, a general and biochemical blood test, and bacterial culture are prescribed. With colitis, impurities of mucus and blood are found in the feces, the level of leukocytes and ESR is increased in the blood.
With signs of colitis, the doctor examines the patient, feels the stomach. Clinical analyzes of urine and feces, a general and biochemical blood test, and bacterial culture are prescribed. With colitis, impurities of mucus and blood are found in the feces, the level of leukocytes and ESR is increased in the blood.
Of the instrumental methods, colonoscopy is used. It allows you to assess the condition of the intestinal mucosa and take material for research. Manometry is used to assess intestinal motility.
Treatment
In most cases, colitis is treated at home. The need for hospitalization arises with an infectious lesion of the intestine and complications of chronic colitis, which endanger the patient’s life.
Therapy is selected depending on the cause of the inflammation. In infectious colitis, antibacterial agents are indicated that are active against the causative agent of the disease. If the disease is caused by intoxication, adsorbents are used to remove decay products.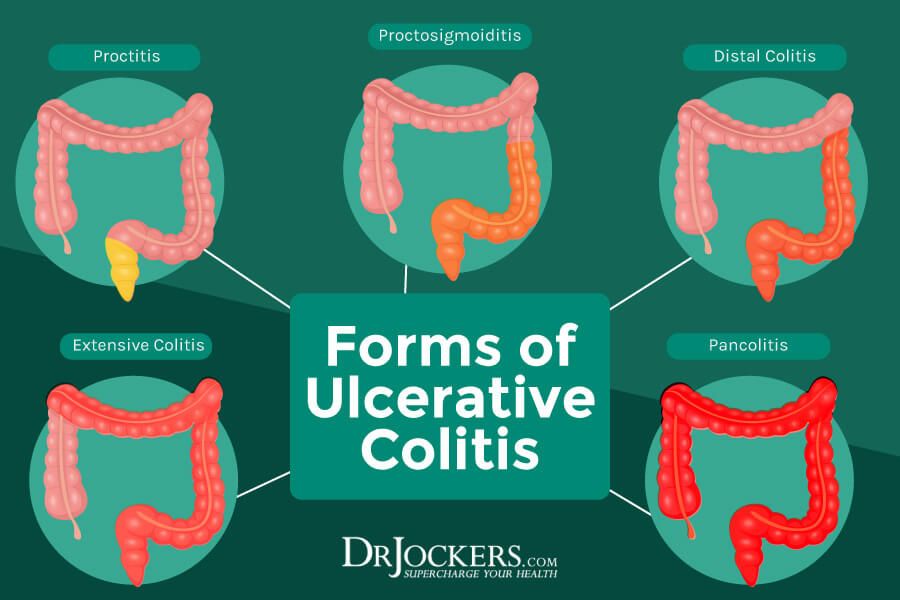 As an adjuvant therapy, the doctor may prescribe drotaverine for spasms. There are contraindications, you need to consult a doctor.
As an adjuvant therapy, the doctor may prescribe drotaverine for spasms. There are contraindications, you need to consult a doctor.
Also, the patient is prescribed antispasmodics to reduce pain. To improve digestion, enzyme-based preparations, drugs for normalizing stools are indicated. Probiotics and prebiotics are used to restore intestinal microflora.
Surgical treatment
Surgical treatment for colitis is indicated for patients with complications of the disease or in the absence of the effect of drug therapy. As a rule, surgery is performed in the case of UC, which requires constant supportive therapy.
The essence of the operation is to remove the affected colon. This procedure is called a colectomy.
There are several methods for performing the operation. The first of these is the removal of the colon and rectum with the imposition of an ileostomy. It ensures the removal of feces through the anterior wall of the abdomen. This is a radical method that is used in the most severe cases.
A more delicate way is to remove the large intestine, followed by the connection of the small intestine and a portion of the rectum. This retains the ability to naturally defecate.
Nutrition for colitis
A diet for colitis is needed to prevent exacerbations and complications. The patient is recommended to eat 5-6 times a day in small portions. It is necessary to exclude salty and spicy foods, alcohol, foods with a high acid content. With diarrhea and flatulence, fresh vegetables and fruits, carbonated drinks are prohibited. If the disease is accompanied by constipation, then you need to increase the amount of vegetable fiber, but it is better to eat mashed food. For example, you can make a vegetable casserole or baked apple puree.
The diet is based on mucous soups and cereals, lean meat and fish, boiled vegetables. The most useful will be oatmeal, rice and buckwheat, potatoes, zucchini, cauliflower. Very useful for steaming or baking food.
Chicken eggs can be eaten boiled or in the form of an omelette.

 This is a possible but uncommon surgical procedure for colitis.
This is a possible but uncommon surgical procedure for colitis.