Laryngeal bronchitis. Laryngotracheobronchitis: Causes, Symptoms, and Treatment of Croup
What are the causes of laryngotracheobronchitis. How is croup diagnosed and treated. What are the key symptoms of laryngotracheobronchitis in children. When should a child with croup be hospitalized. How can parents manage mild croup at home.
Understanding Laryngotracheobronchitis: An Overview of Croup
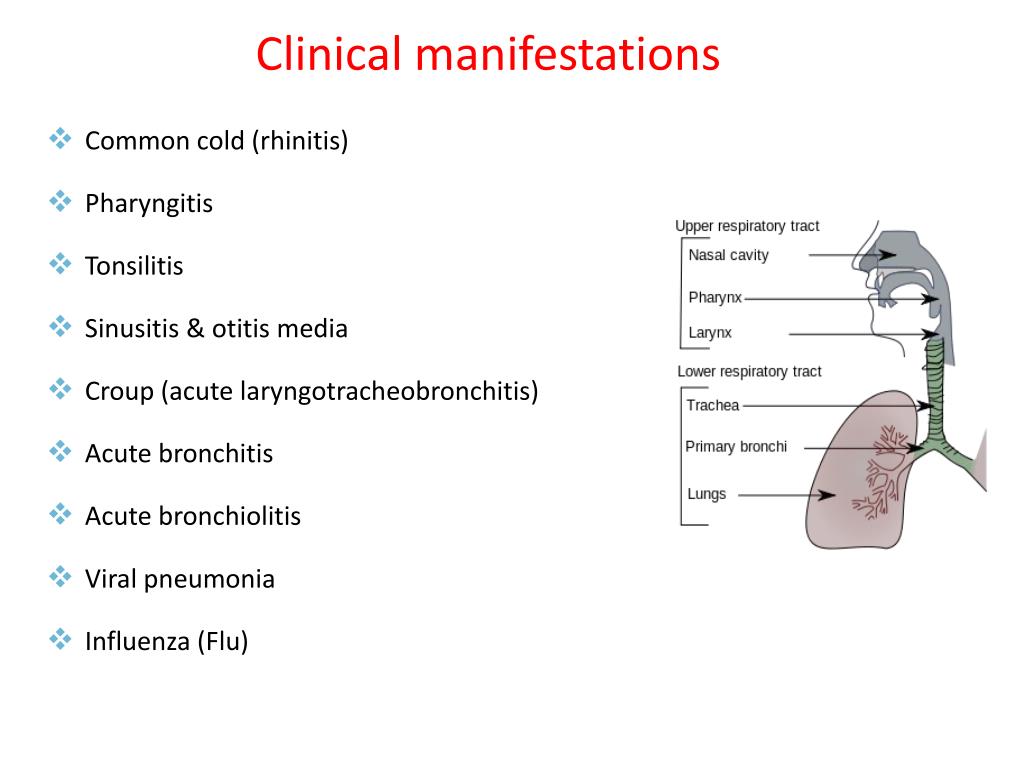
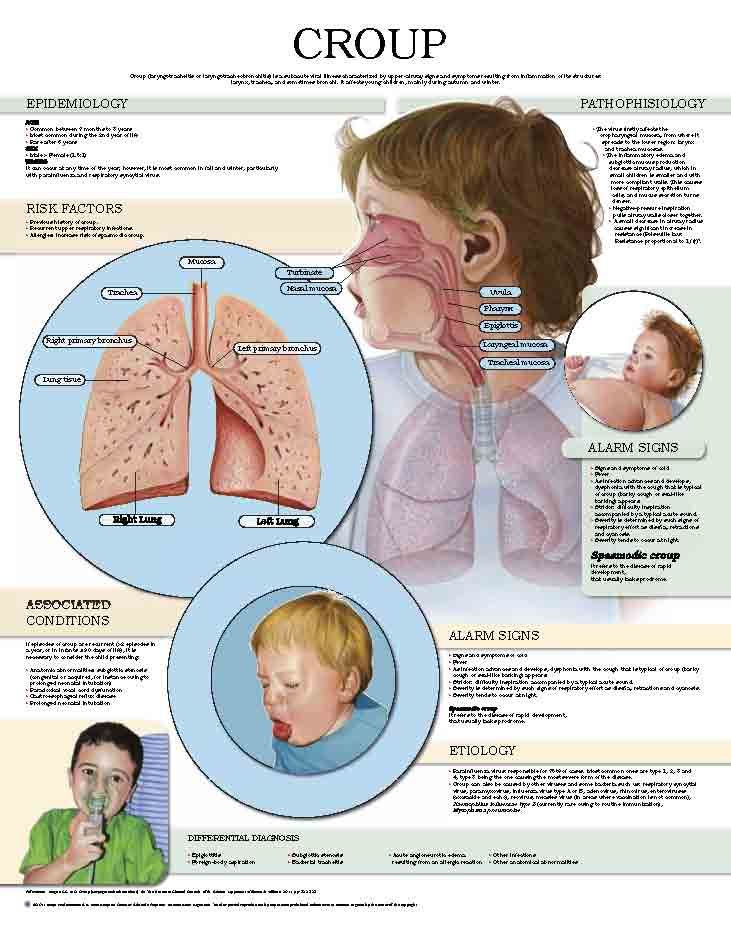
Laryngotracheobronchitis, commonly known as croup, is a respiratory condition characterized by inflammation of the larynx, trachea, and bronchi. This ailment primarily affects children and can range from mild to severe cases. Croup is a frequent cause of cough, stridor, and hoarseness in febrile children, with most recovering without complications. However, in rare instances, it can be life-threatening for infants.
Key Characteristics of Laryngotracheobronchitis
- Affects the subglottic airway
- Most common in children aged 6 months to 6 years
- Peak incidence in children 12 months to 2 years old
- More prevalent in boys than girls
- Typically occurs from late autumn to early spring
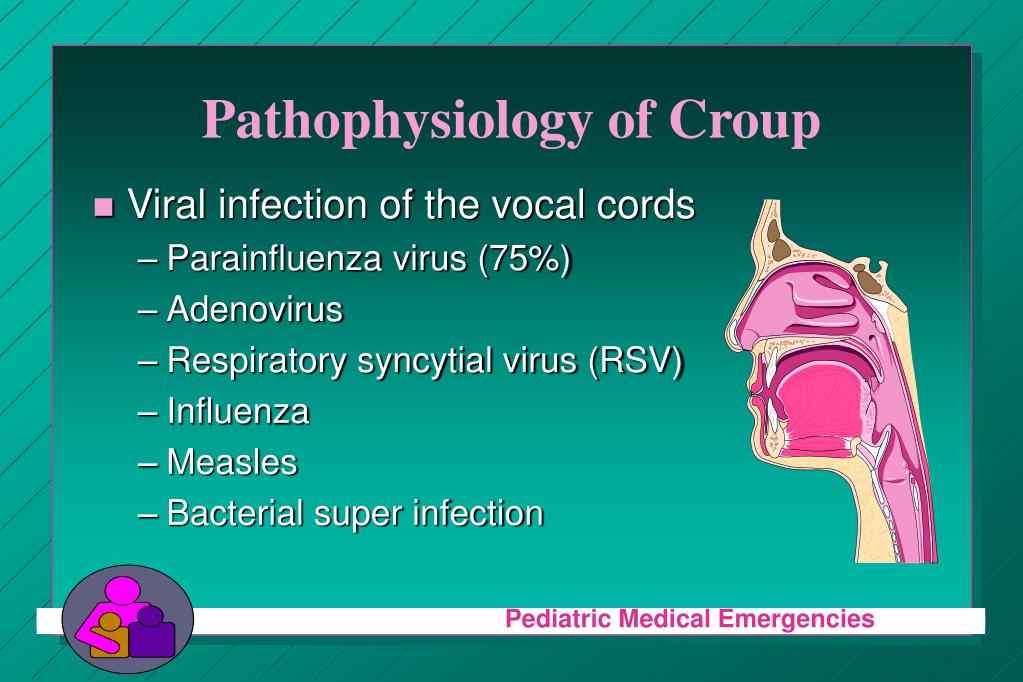
Is croup always caused by a viral infection. The vast majority of croup cases are indeed viral in nature. The most common culprit is the parainfluenza virus, but other viruses such as respiratory syncytial virus (RSV), rhinovirus, enterovirus, influenza, and adenovirus can also cause croup.
The Pathophysiology of Laryngotracheobronchitis
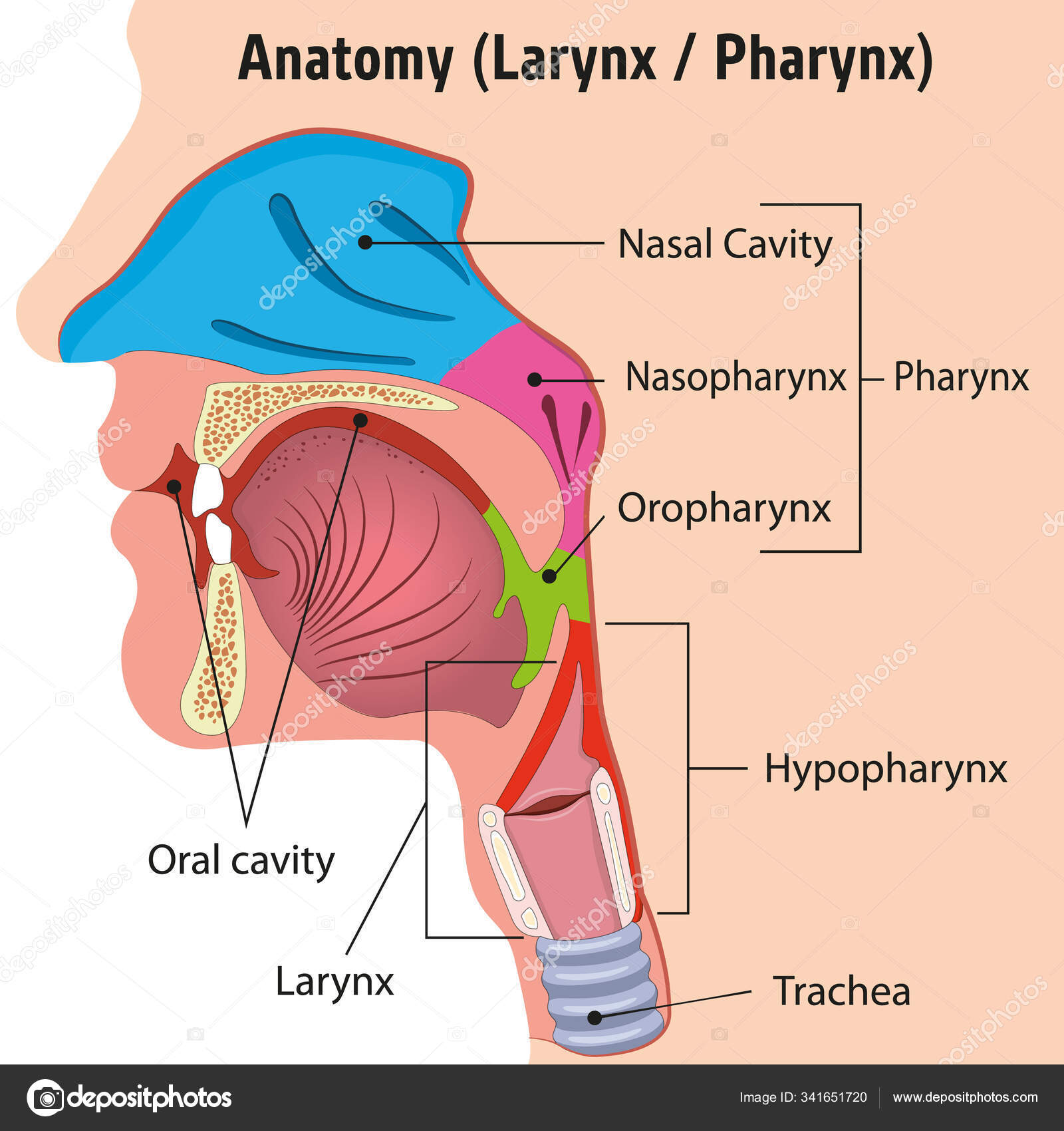
Understanding the pathophysiology of croup is crucial for effective diagnosis and treatment. The process begins with viral inhalation, which leads to infection of the nasal and pharyngeal mucosal epithelia. Subsequently, the infection spreads to the subglottic space, causing inflammation and narrowing of the airway.
Anatomical Considerations in Croup
Why is croup more severe in young children. The severity of croup in young children is primarily due to their unique anatomy. In children 8 years and younger, the subglottic space is the narrowest part of the airway. The cricoid cartilage forms a complete, non-expanding ring, which, when combined with inflamed mucosa, leads to significant airway narrowing. This anatomical feature explains the characteristic high-pitched stridor associated with croup.
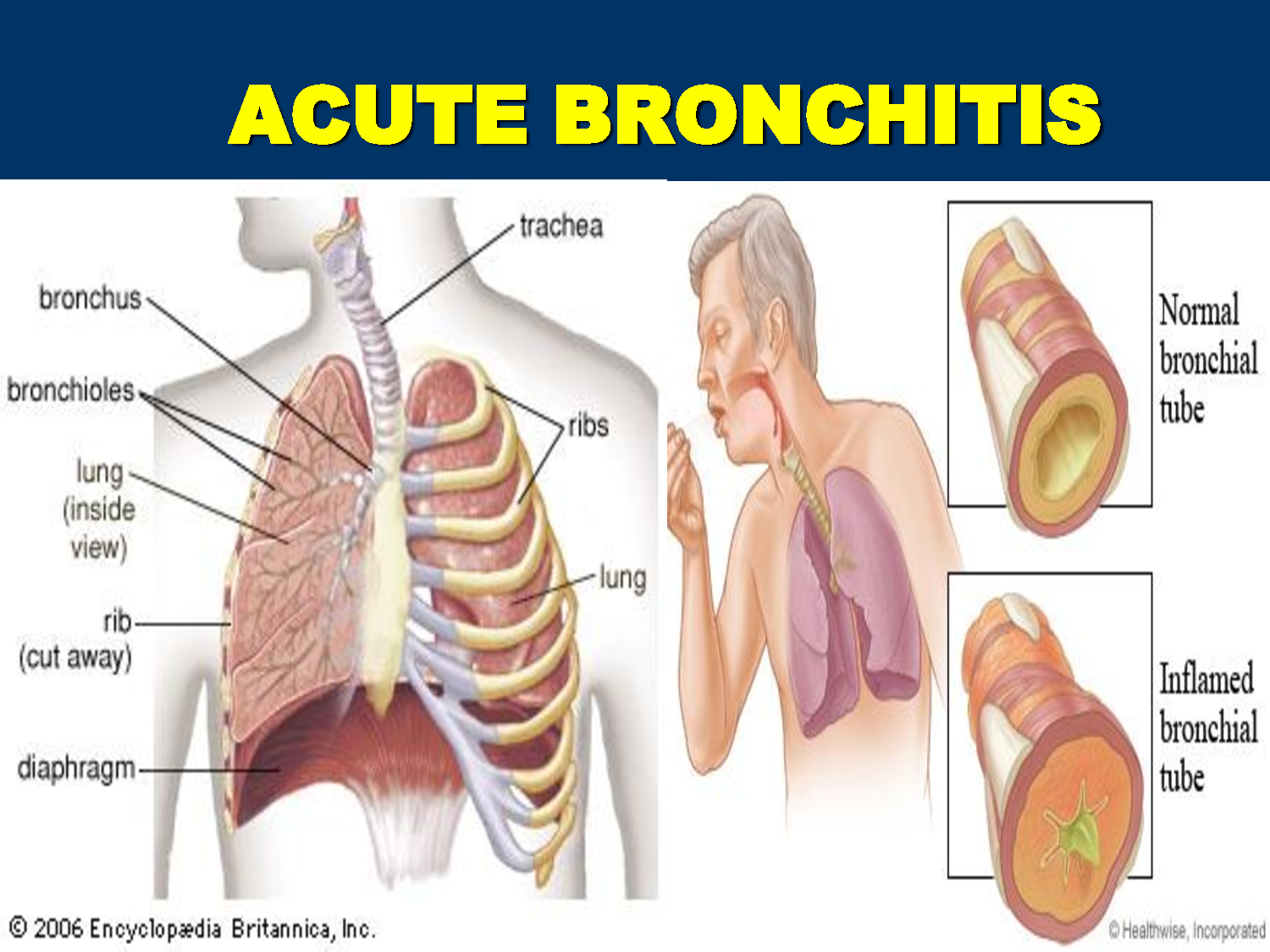
In cases of laryngotracheobronchitis, where inflammation extends into the bronchi, additional symptoms may include:
- Wheezing
- Crackles
- Air trapping
- Increased tachypnea
These symptoms can sometimes be mistaken for acute asthma, highlighting the importance of accurate diagnosis.
Recognizing the Symptoms of Laryngotracheobronchitis
The clinical presentation of croup typically follows a predictable pattern. Parents and healthcare providers should be aware of the following progression:
- Initial symptoms: 1-3 days of rhinorrhea, nasal congestion, and fever
- Characteristic croup symptoms:
- Barky or seal-like cough
- Hoarse voice
- High-pitched inspiratory stridor (often mistaken for wheezing by parents)
How can healthcare providers assess the severity of croup. Several scoring systems exist to evaluate the degree of respiratory distress in croup patients. One widely used method is the Westley score, which assesses factors such as stridor, retractions, air entry, cyanosis, and level of consciousness.
Diagnosing Laryngotracheobronchitis: Clinical Evaluation and Imaging
Diagnosing croup is primarily a clinical process based on the patient’s history and physical examination. However, in some cases, additional tests may be necessary to confirm the diagnosis or rule out other conditions.
Clinical Evaluation
When evaluating a child suspected of having croup, healthcare providers should:
- Observe the child while sitting comfortably on the caretaker’s lap to prevent agitation
- Listen for the characteristic barky cough and stridor
- Assess for signs of lower airway involvement (wheezing, crackles, decreased air movement)
- Evaluate the severity of respiratory distress
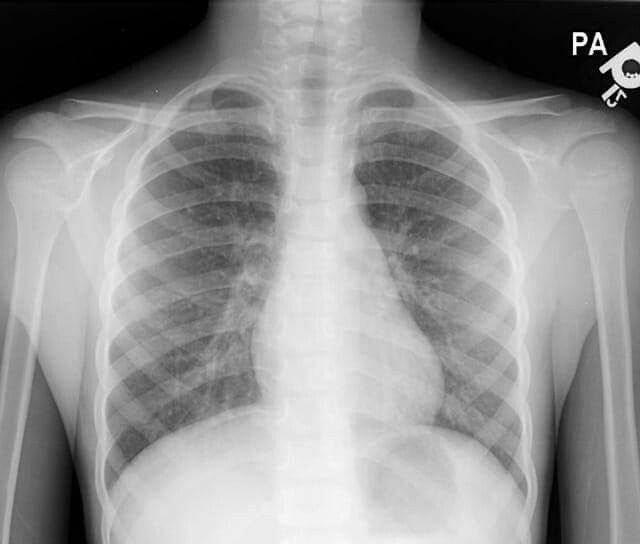
Are radiographs necessary for diagnosing croup. While not typically required, radiographs can be helpful if the diagnosis is unclear. The classic “steeple sign” on chest X-rays, indicative of subglottic narrowing, can support a diagnosis of croup.
Severity Classification
Based on the clinical presentation, croup cases can be categorized into three groups:
- Mild
- Moderate
- Severe
This classification helps guide treatment decisions and determines the need for hospitalization.
Treatment Approaches for Laryngotracheobronchitis
The management of croup varies depending on the severity of the condition. Treatment aims to reduce airway inflammation, alleviate respiratory distress, and prevent complications.

Mild Croup
For mild cases of croup, the following approaches are typically recommended:
- Humidified air or cool mist
- Oral dexamethasone (0.15-0.6 mg/kg)
- Supportive care and close monitoring at home
How effective is dexamethasone in treating croup. Dexamethasone has been shown to significantly reduce the severity and duration of croup symptoms, even in mild cases. It can be administered orally or intramuscularly, with effects typically lasting for several days.
Moderate to Severe Croup
For more severe cases, additional interventions may be necessary:
- Nebulized epinephrine (racemic epinephrine or L-epinephrine)
- Intravenous or intramuscular dexamethasone
- Oxygen therapy if hypoxemia is present
- Close monitoring in a healthcare setting
In rare, life-threatening cases, intubation or even tracheostomy may be required to secure the airway.
Home Management of Croup: Guidance for Parents
Many cases of croup can be managed effectively at home. Parents and caregivers should be educated on the following strategies:
- Keeping the child calm and comfortable
- Using a cool-mist humidifier in the child’s room
- Encouraging fluid intake to prevent dehydration
- Administering acetaminophen or ibuprofen for fever and discomfort
- Avoiding exposure to irritants like cigarette smoke
When should parents seek immediate medical attention for a child with croup. Parents should be advised to seek emergency care if their child exhibits:
- Difficulty breathing or severe retractions
- Bluish discoloration of the lips or skin
- Drooling or difficulty swallowing
- Lethargy or decreased responsiveness
Preventing Complications and Recurrence of Laryngotracheobronchitis
While croup is generally a self-limiting condition, taking steps to prevent complications and recurrence is important. Healthcare providers should counsel patients and families on the following measures:
Vaccination
Ensuring children are up-to-date on their vaccinations can help prevent some viral infections that cause croup. This includes annual influenza vaccines and other routine childhood immunizations.

Hygiene Practices
Encouraging good hygiene habits can reduce the risk of viral transmission:
- Regular handwashing
- Avoiding close contact with individuals who have respiratory infections
- Proper cleaning and disinfection of frequently touched surfaces
Environmental Factors
Minimizing exposure to environmental irritants can help prevent recurrent croup episodes:
- Maintaining a smoke-free environment
- Using air purifiers to reduce indoor air pollutants
- Controlling household allergens
Can recurrent croup be a sign of an underlying condition. While most cases of croup are isolated incidents, recurrent croup may indicate an underlying airway abnormality or other medical condition. Children with frequent episodes should be evaluated by a pediatric otolaryngologist to rule out structural issues or other predisposing factors.
The Role of the Interprofessional Team in Managing Laryngotracheobronchitis
Effective management of laryngotracheobronchitis often requires a collaborative approach involving various healthcare professionals. This interprofessional team may include:

- Emergency medicine physicians
- Pediatricians
- Otolaryngologists
- Respiratory therapists
- Nurses
- Pharmacists
How does an interprofessional approach improve outcomes for croup patients. By working together, the healthcare team can:
- Ensure accurate diagnosis and appropriate treatment
- Provide comprehensive patient and family education
- Monitor for potential complications
- Facilitate smooth transitions between different levels of care
- Improve overall patient outcomes and satisfaction
Continuing Education and Protocol Development
To maintain high-quality care for croup patients, healthcare institutions should:
- Provide regular training and updates on croup management
- Develop and implement evidence-based protocols
- Encourage participation in research and quality improvement initiatives
Laryngotracheobronchitis, or croup, remains a common childhood respiratory condition that can cause significant distress for both patients and families. By understanding its pathophysiology, recognizing its symptoms, and implementing appropriate treatment strategies, healthcare providers can effectively manage this condition and minimize complications. Ongoing research and interprofessional collaboration continue to enhance our ability to care for children with croup, ensuring the best possible outcomes for these young patients.

Laryngotracheobronchitis – StatPearls – NCBI Bookshelf
Continuing Education Activity
Laryngotracheobronchitis, as the name implies, refers to inflammation of the larynx, trachea, and bronchi. Cases of laryngotracheobronchitis can be more severe than laryngotracheitis as the former extends into the lower airway. Both may be difficult to distinguish clinically. This activity reviews the cause and presentation of laryngotracheobronchitis and highlights the role of the interprofessional team in its management.
Objectives:
Review the presentation of
laryngotracheobronchitis.Describe the evaluation of a patient with
laryngotracheobronchitis.Summarize the treatment of
laryngotracheobronchitis .Outline the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by laryngotracheobronchitis.
Access free multiple choice questions on this topic.
Introduction
Laryngotracheobronchitis, as the name implies, refers to inflammation of the larynx, trachea, and bronchi. Cases of laryngotracheobronchitis can be more severe than laryngotracheitis as the former extends into the lower airway. Both may be difficult to distinguish clinically. [1][2][3] The term “croup” colloquially describes both laryngotracheobronchitis and laryngotracheitis, and will, therefore, be used for the remainder of this article to describe this disease spectrum.
Croup is a very common cause of a cough, stridor, and hoarseness in children with a fever. Most children who have croup recover without any consequences. However, rarely, this infection can be lethal to infants.
Etiology
Croup is most often a viral infection that affects the subglottic airway, commonly caused by the parainfluenza virus. Other viruses that are known to cause croup include the respiratory syncytial virus (RSV), rhinovirus, enterovirus, influenza, and adenovirus. [4][5]
[4][5]
Epidemiology
Croup occurs more commonly in boys than in girls. It frequently occurs in children aged 6 months to 6 years old, with a peak incidence in children 12 months to 2 years of age. Most cases of croup occur from late autumn to early spring. Recurrent croup is rare unless there is a family history of the illness. Only a small percentage of patients require hospital admission. A population study conducted from 1999 to 2005 found that only 5.6% of children with croup required admission. Most patients can be safely discharged from the emergency department after appropriate management as discussed below.
Pathophysiology
Inhalation of the virus causing croup first infects the nasal and pharyngeal mucosal epithelia, then spreads to the subglottic space. For children 8 years and younger, the subglottic space is the most narrow part of the airway. The cricoid cartilage forms a complete cartilaginous ring that is nonexpanding. This inability of the cricoid to expand leads to a significant narrowing of the subglottic region secondary to the inflamed mucosa.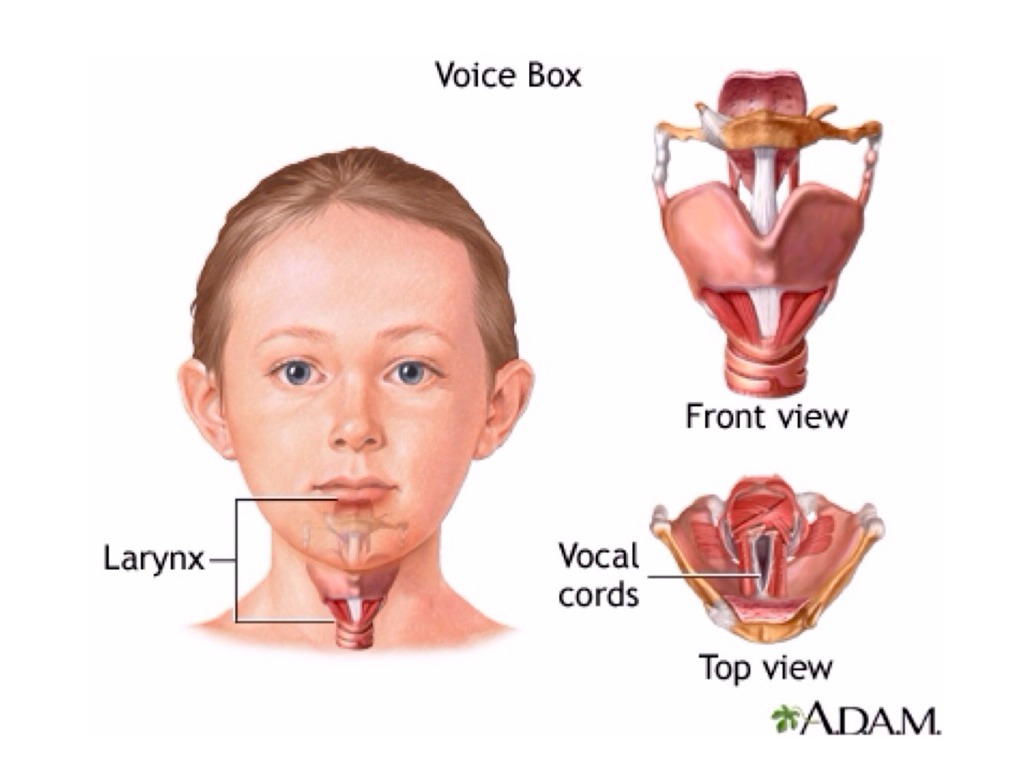 When the child cries or becomes agitated, further dynamic obstruction can occur at and below the cartilaginous ring. These factors lead to the common high-pitched stridor heard at rest and when the patient becomes agitated. Extension into the bronchi, as occurs with laryngotracheobronchitis, can lead to wheezing, crackles, air trapping, and increased tachypnea; a clinical picture that can be confused with acute asthma.
When the child cries or becomes agitated, further dynamic obstruction can occur at and below the cartilaginous ring. These factors lead to the common high-pitched stridor heard at rest and when the patient becomes agitated. Extension into the bronchi, as occurs with laryngotracheobronchitis, can lead to wheezing, crackles, air trapping, and increased tachypnea; a clinical picture that can be confused with acute asthma.
History and Physical
One to three days of rhinorrhea, nasal congestion, and fever usually precedes croup. Typical symptoms of croup include a barky or a seal-like cough, hoarse voice, and high pitched inspiratory stridor that parents may incorrectly describe as “wheezing.”
Several scoring systems can evaluate the severity of respiratory distress. The Westley score assesses the following:
Evaluation
Evaluation of the patient must include ruling out other causes of stridor (discussed in the differential diagnosis section) and prompt recognition of the rapid progression or worsening of airway obstruction. Radiographs are not necessary to diagnose croup but can be obtained if the diagnosis is unclear. The “steeple sign,” due to subglottic narrowing, can be seen on plain films of the chest in patients with croup.[6][7][8]
Radiographs are not necessary to diagnose croup but can be obtained if the diagnosis is unclear. The “steeple sign,” due to subglottic narrowing, can be seen on plain films of the chest in patients with croup.[6][7][8]
Patients should be evaluated while sitting comfortably on the caretaker’s lap to prevent agitation and further narrowing of the airway. Croup is a clinical diagnosis made when patients present with a barky cough with or without stridor. Patients with the extension of inflammation into the lower airway, or laryngotracheobronchitis, can also have wheezing, crackles, decreased air movement, and tachypnea.
Patients with croup can be placed into 3 groups: mild, moderate, or severe, as seen in Table 1 below. Careful evaluation of worsening stridor, work of breathing (chest wall/subcostal retractions, nasal flaring, sitting in a sniffing position, suprasternal retractions, grunting, accessory muscle use), vitals, mental status, hydration status, and air movement help determine the treatment and disposition. The presence of wheezing, crackles, or decreased air movement on lung auscultation suggests laryngotracheobronchitis.
The presence of wheezing, crackles, or decreased air movement on lung auscultation suggests laryngotracheobronchitis.
Treatment / Management
The goal of treatment is to decrease airway obstruction. Treatment includes nebulized epinephrine, corticosteroids, and at least 3 hours of observation after the last dose of epinephrine. Supplemental oxygen via blow by or nasal cannula can also be used for hypoxic patients with croup.[9][10][11]
Nebulized Epinephrine
Racemic epinephrine 2.25% 0.05 mL/kg nebulized with a maximum of 5 mL or L-epinephrine 0.5 mL/kg nebulized with a maximum of 5 mL is reserved for moderate and severe croup. Admit patients requiring more than 1 to 2 doses of nebulized epinephrine in the emergency department.
Corticosteroids
Regardless of severity, all patients with croup benefit from oral steroids. Dexamethasone 0.15 mg/kg to 0.6 mg/kg by mouth with a maximum of 10 mg as a one-time dose is the typical dose (the intravenous dose can be given by mouth).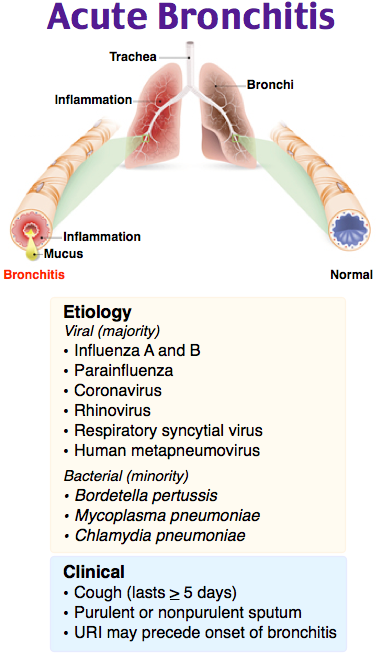
Observation
Patients with croup should be observed for a minimum of 3 hours after the completion of each dose of nebulized racemic epinephrine. Watch for worsening or recurrence of symptoms, including persistent stridor at rest, increased work of breathing, and hypoxia, during the observation period. Admit patients requiring more than one or two doses of nebulized epinephrine in the emergency department.
Heliox
Several trials have been conducted on helion in the management of croup, and the results are mixed. Overall, there is no harm from trying heliox because most anecdotal reports indicate that it helps ease breathing.
Intubation
Intubation is reserved for severe cases of croup not responding to medical treatment. The endotracheal tube size should be smaller than typical for the patient’s age and size to avoid trauma to the already edematous airway.
Differential Diagnosis
Differential diagnosis
For a patient younger than 6 months old with stridor:
laryngotracheomalacia
subglottic stenosis
vocal cord paralysis
hemangioma
vascular ring
foreign body aspiration
anaphylaxis
asthma
peritonsillar abscess
retropharyngeal abscess
For patients older than 6 months with stridor:
foreign body aspiration
bacterial tracheitis
epiglottitis
peritonsillar abscess
parapharyngeal abscess
retropharyngeal abscess
anaphylaxis.

Prognosis
The prognosis for most children with croup is excellent. Most cases can be managed with outpatient care. Fewer than 2% of patients require hospitalization. The use of nebulized epinephrine and steroids has markedly lowered the need to intubate many patients.
Complications
Complications are rare but can occur in some cases. They include:
Postoperative and Rehabilitation Care
Patients with mild croup can be safely discharged from the emergency department with strict return precautions after receiving one dose of steroids. For patients with moderate or severe croup, important criteria to meet before discharge include observation for 3 hours after epinephrine without signs of worsening or recurrence of symptoms (persistent stridor at rest, increased work of breathing, hypoxia), the non-toxic appearance of the patient, and the patient’s ability to tolerate oral liquids. Other factors to consider before discharge are that the caretaker recognizes an improvement in the child’s symptoms, the caretaker has adequate transportation to return if necessary, and there are no significant social issue concerns.
Consultations
In any child with respiratory distress, a pediatrician should be consulted on the course of management. Consultation with an otolaryngologist may be advised if visualization of the larynx is indicated.
Deterrence and Patient Education
Washing hands is highly recommended.
Pearls and Other Issues
Croup is a barky cough with or without stridor at rest.
Mild croup is a barky cough with or without stridor, with agitation. Treatment includes one dose of steroids then discharge home with strict return precautions.
Moderate croup is a barky cough and stridor at rest, with or without increased work of breathing. Treatment includes steroids and nebulized epinephrine with observation for at least 3 hours for reassessment.
Severe croup is a barky cough, stridor at rest, and prominent increased work of breathing. Treatment includes steroids and nebulized epinephrine with observation for at least 3 hours for reassessment. It will most likely include admission.
Evaluate for other dangerous diagnoses in the differential of upper airway obstruction.
Enhancing Healthcare Team Outcomes
Croup is managed by an interprofessional team that includes a pediatrician, emergency department physician, nurse practitioner, and radiologist. The diagnosis can be difficult because there is no specific test for the disorder. The goal of treatment is to decrease airway obstruction. Treatment includes nebulized epinephrine, corticosteroids, and at least 3 hours of observation after the last dose of epinephrine. Supplemental oxygen via blow-by or nasal cannula can also be used for hypoxic patients with croup. The majority of patients can be safely discharged home from the emergency department but the caretaker must be informed about the importance of avoiding smoking in the home. Other factors to consider before discharge are that the caretaker recognizes an improvement in the child’s symptoms, the caretaker has adequate transportation to return if necessary, and there are no significant social issue concerns. [2]
[2]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Lee JH, Jung JY, Lee HJ, Kim DK, Kwak YH, Chang I, Kwon H, Choi YJ, Park JW, Paek SH, Cho JH. Efficacy of low-dose nebulized epinephrine as treatment for croup: A randomized, placebo-controlled, double-blind trial. Am J Emerg Med. 2019 Dec;37(12):2171-2176. [PubMed: 30878411]
- 2.
Elder AE, Rao A. Management and outcomes of patients presenting to the emergency department with croup: Can we identify which patients can safely be discharged from the emergency department? J Paediatr Child Health. 2019 Nov;55(11):1323-1328. [PubMed: 30779245]
- 3.
Lodeserto FJ, Lettich TM, Rezaie SR. High-flow Nasal Cannula: Mechanisms of Action and Adult and Pediatric Indications. Cureus. 2018 Nov 26;10(11):e3639. [PMC free article: PMC6358040] [PubMed: 30740281]
- 4.
Moraa I, Sturman N, McGuire TM, van Driel ML.
 Heliox for croup in children. Cochrane Database Syst Rev. 2018 Oct 29;10(10):CD006822. [PMC free article: PMC6516979] [PubMed: 30371952]
Heliox for croup in children. Cochrane Database Syst Rev. 2018 Oct 29;10(10):CD006822. [PMC free article: PMC6516979] [PubMed: 30371952]- 5.
Baillie VL, Olwagen CP, Madhi SA. Review on Clinical and Molecular Epidemiology of Human Rhinovirus-Associated Lower Respiratory Tract Infections in African and Southeast Asian Children. Pediatr Infect Dis J. 2018 Jul;37(7):e185-e194. [PubMed: 29893746]
- 6.
Gates A, Gates M, Vandermeer B, Johnson C, Hartling L, Johnson DW, Klassen TP. Glucocorticoids for croup in children. Cochrane Database Syst Rev. 2018 Aug 22;8(8):CD001955. [PMC free article: PMC6513469] [PubMed: 30133690]
- 7.
Dalal R, Grujic D. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 8, 2022. Epinephrine. [PubMed: 29489283]
- 8.
Hilmes MA, Daniel Dunnavant F, Singh SP, Ellis WD, Payne DC, Zhu Y, Griffin MR, Edwards KM, Williams JV. Chest radiographic features of human metapneumovirus infection in pediatric patients.
 Pediatr Radiol. 2017 Dec;47(13):1745-1750. [PMC free article: PMC5901753] [PubMed: 28831577]
Pediatr Radiol. 2017 Dec;47(13):1745-1750. [PMC free article: PMC5901753] [PubMed: 28831577]- 9.
Anderson-James S, Marchant JM, Chang AB, Acworth JP, Phillips NT, Drescher BJ, Goyal V, O’Grady KF. Burden and emergency department management of acute cough in children. J Paediatr Child Health. 2019 Feb;55(2):181-187. [PubMed: 30066972]
- 10.
Ortiz-Alvarez O. Acute management of croup in the emergency department. Paediatr Child Health. 2017 Jun;22(3):166-173. [PMC free article: PMC5804741] [PubMed: 29532807]
- 11.
Cutrera R, Baraldi E, Indinnimeo L, Miraglia Del Giudice M, Piacentini G, Scaglione F, Ullmann N, Moschino L, Galdo F, Duse M. Management of acute respiratory diseases in the pediatric population: the role of oral corticosteroids. Ital J Pediatr. 2017 Mar 23;43(1):31. [PMC free article: PMC5364577] [PubMed: 28335827]
Disclosure: Stacey Ernest declares no relevant financial relationships with ineligible companies.

Disclosure: Paras Khandhar declares no relevant financial relationships with ineligible companies.
Croup – Acute Laryngotracheobronchitis
- Download PDF Copy
By Dr. Liji Thomas, MDReviewed by Dr. Tomislav Meštrović, MD, Ph.D.
Croup, or acute laryngotracheobronchitis, is an acute infectious respiratory disease of infants and children caused by infection of the larynx or the trachea – alone or together. It can cause partial or severe obstruction of the airway, which results in breathing difficulties and coughing. In some children it can be life-threatening.
Croup – Image Copyright: joshya / Shutterstock
Cause
Croup is most often caused by the parainfluenza virus, but may also be the result of infection with respiratory syncytial virus (RSV), adenoviruses, or the measles virus. Bacterial croup is also known to occur, as is croup due to allergic reactions, acid reflux or irritation of the airway by a foreign body. Croup usually affects children simply because their airways are narrower than in adults, making any swelling more dangerous and likely to block the air flow.
Croup usually affects children simply because their airways are narrower than in adults, making any swelling more dangerous and likely to block the air flow.
Symptoms
The affected child is most often between 3 months and 5 years of age, with the incidence peaking at around 24 months. Croup starts usually as an ordinary cold, but worsens after a few days. It is characterized by noisy breathing and a hoarse voice, although the most impressive feature is the barking cough, often likened to a seal barking. In addition, there may be difficulty with breathing, especially at night. The symptoms start mildly in most cases. They may last for up to a week, and are especially severe on the first and second nights.
Diagnosis and management
Croup is diagnosed on the basis of the symptoms and the cough. Physical examination will show various signs related to laryngeal inflammation and respiratory difficulty.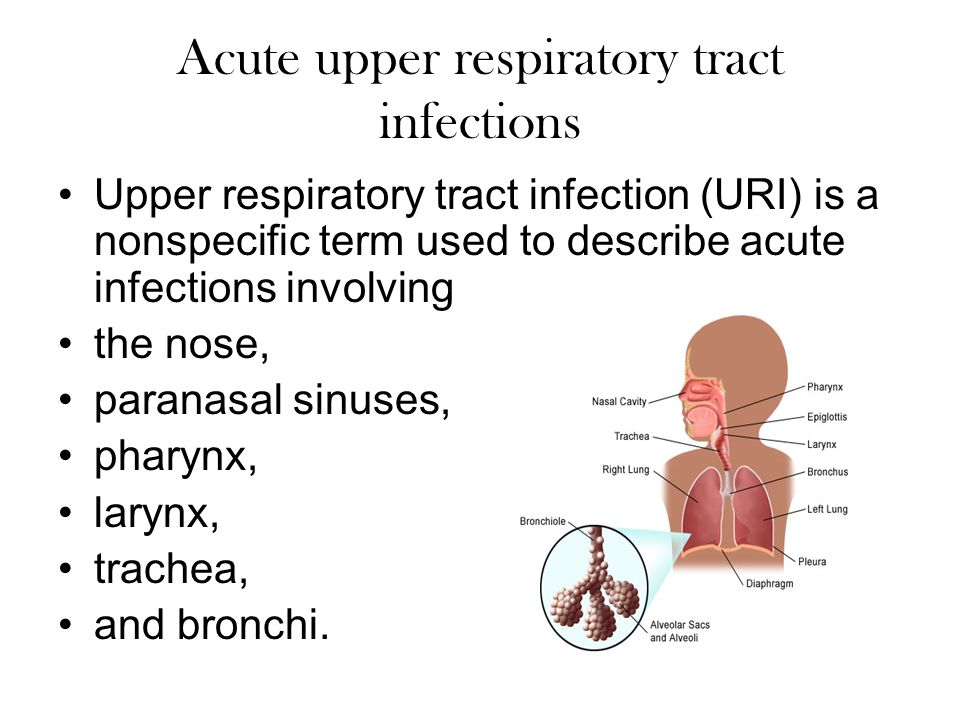
Croup in most cases responds to home care, under the advice of a medical professional. The child should be comforted because anxiety and fear exaggerate the obstruction and increase the breathing rate.
Related Stories
- Study finds hospitalizations for COVID-19–related croup increased after the onset of the Omicron variant
- Do the symptom profiles among children with SARS-CoV-2 infection differ by variant type?
In many cases, moist air in the form of steam is used to relieve the obstruction. Cool air vaporizers may be helpful. This time-hallowed form of treatment has, however, no scientific backing.
Fever is treated with acetaminophen titrated according to the child’s body weight and age. In certain instances, antibiotics or steroid inhalers may be required, on the prescription of a doctor. Steroids help to relieve the airway obstruction, but require some time to act when taken systemically. Inhaled steroids act much faster.
Medical treatment is essential when the child is seriously distressed, tired out from the effort of breathing, or cyanosed because adequate oxygen is not reaching the body. Admission is required for approximately 5% of croupy children.
Admission is required for approximately 5% of croupy children.
Hospital treatment may include nebulization with epinephrine to urgently bring down the inflammation in severe cases. Other measures include:
- The use of an oxygen tent to improve the oxygenation and thus reduce the work of breathing, consequently relieving the child
- Glucocorticoids to further reduce and keep down inflammatory swelling have been found to be highly effective in decreasing the need for hospital admission of such children; they may be given by inhalation, orally or intravenously
- Fluids for dehydration, either orally or more often intravenously
- Antibiotic therapy if there is actual or likely secondary infection
Sources
- https://medlineplus.gov/ency/article/000959.htm
- www.betterhealth.vic.gov.au/health/conditionsandtreatments/croup
- https://www.ncbi.nlm.nih.gov/
Further Reading
- All Croup Content
- Symptoms and Causes of Croup
- Diagnosis and Treatment of Croup
- Home Care for Croup
Last Updated: Jan 24, 2023
- Download PDF Copy
Please use one of the following formats to cite this article in your essay, paper or report:
APA
Thomas, Liji.
 (2023, January 24). Croup – Acute Laryngotracheobronchitis. News-Medical. Retrieved on June 10, 2023 from https://www.news-medical.net/health/Croup-Acute-Laryngotracheobronchitis.aspx.
(2023, January 24). Croup – Acute Laryngotracheobronchitis. News-Medical. Retrieved on June 10, 2023 from https://www.news-medical.net/health/Croup-Acute-Laryngotracheobronchitis.aspx.MLA
Thomas, Liji. “Croup – Acute Laryngotracheobronchitis”. News-Medical. 10 June 2023. <https://www.news-medical.net/health/Croup-Acute-Laryngotracheobronchitis.aspx>.
Chicago
Thomas, Liji. “Croup – Acute Laryngotracheobronchitis”. News-Medical. https://www.news-medical.net/health/Croup-Acute-Laryngotracheobronchitis.aspx. (accessed June 10, 2023).
Harvard
Thomas, Liji. 2023. Croup – Acute Laryngotracheobronchitis. News-Medical, viewed 10 June 2023, https://www.news-medical.net/health/Croup-Acute-Laryngotracheobronchitis.aspx.
Barking cough – symptoms, causes, treatment and prevention in children and adults.
 — Clinic “Doctor nearby”
— Clinic “Doctor nearby”
Barking cough is a dry, paroxysmal cough that sounds like a dog barking and is characterized by spasmodic expiration. Due to the influence of pathogenic pathogens, the larynx swells, the voice becomes hoarse, rough. From a physiological point of view, a barking cough can be called useless, since it does not contribute to the removal of sputum, does not protect the throat, and is accompanied by pain. Most often, a dry barking cough occurs in a child of kindergarten age; infants suffer from it quite rarely. Coughing fits are very difficult and painful for a small organism, often accompanied by vomiting and shortness of breath. If a barking cough in a child occurs without a temperature, it is required to immediately take him to the hospital and show the doctor. In this condition, there is a very high risk of developing a serious swelling of the larynx, in which air will not enter through the respiratory tract, which will lead to suffocation of the baby. A barking cough in an adult with the inability to cough also requires a visit to a medical facility. It may indicate the progression of a viral infection in the vocal cords. A strong barking cough in adults is not as painful as in young children, but there is also a high risk of swelling of the larynx and suffocation.
A barking cough in an adult with the inability to cough also requires a visit to a medical facility. It may indicate the progression of a viral infection in the vocal cords. A strong barking cough in adults is not as painful as in young children, but there is also a high risk of swelling of the larynx and suffocation.
Barking cough is not a separate nosological unit. This is a symptom that indicates the development of various diseases, the identification and treatment of which should be given the closest attention.
Causes of barking cough in children and adults
True croup . This disease can be deadly for children of the first year of life due to the narrow lumen of the respiratory passage of the nasopharynx in infants. The characteristic symptoms of true croup are:
dry barking cough;
the occurrence of shortness of breath;
lethargy, weakness;
pain in the chest area.

True croup can lead to respiratory arrest, so you should immediately seek medical help!
Laryngitis – inflammation of the vocal cords due to the activity of pathogenic microorganisms. Symptoms of laryngitis include:
frequent paroxysmal barking cough;
the occurrence of wheezing in the upper respiratory system;
heat;
weakness, lethargy;
loss of voice
runny nose;
pain in the throat when swallowing.
Pharyngitis is an inflammatory process of the lymphoid tissue and mucous membrane of the larynx, caused by infection, viruses, bacteria, fungi. The development of pharyngitis can provoke diseases of the nasopharynx, caries, allergies, inhalation of too cold or hot air. Symptoms include:
dry barking cough;
the occurrence of perspiration and dryness in the throat;
severe pain in the throat.

Acute stenosing laryngotracheitis (ASLT) – popularly known as false croup. Often it is caused by a viral infection. It is extremely rare in adults. The characteristic symptoms of false croup are:
barking cough in a child;
hoarseness of voice or its complete disappearance;
increase in body temperature.
It is important to remember: in cases of unstoppable and intensifying coughing attacks, if the barking cough in a child becomes very rough or goes silent, it is urgent to call a doctor – every minute can be a journey!
Influenza, parainfluenza, SARS, adenoviruses, respiratory syncytial infections . Basically, their occurrence is provoked by viruses. Symptoms include:
painful barking cough;
asthma attacks that occur late in the evening or at night;
wheezing on inspiration;
hoarseness of voice;
blanching of the skin;
elevated body temperature.

Diphtheria is an acute infectious disease caused by diphtheria bacillus (Leffler’s wand). Infection can occur both by airborne droplets and by household routes. Localization of infection occurs in the respiratory tract, oropharynx, on the skin, eyes, ears. The vast majority of children suffer from oropharyngeal diphtheria. Symptoms of diphtheria include:
swollen lymph nodes;
increased body temperature;
sore throat;
the appearance of a plaque in the throat of a yellow or grayish-white color;
with the development of true croup against the background of diphtheria – a barking cough, wheezing breathing.
The development of diphtheria can be fatal! If you find any signs of it, you should immediately contact a specialist.
Whooping cough is an infectious disease affecting the mucous membranes of the respiratory tract, the causative agent of which is the bacillus bordetella pertussis. Infection can occur by airborne droplets. The characteristic symptoms of whooping cough are:
Infection can occur by airborne droplets. The characteristic symptoms of whooping cough are:
strong, hysterical paroxysmal barking cough, which often ends in vomiting;
the occurrence of hemorrhages in the mucous membranes;
increase in body temperature;
chills;
headache;
secretion of mucus from the nose.
Bronchial asthma is a chronic disease, the main cause of which is considered to be allergic reactions of the human body. With this disease, bronchial spasm occurs against the background of the inflammatory process of the respiratory tract. Asthma symptoms include:
An allergic reaction to may cause a barking cough in children and adults. It is characterized by the absence of temperature. Usually, the development of allergies can be provoked by pets, various smells, household chemicals, foods, plants, flowers. Allergy symptoms include:
Allergy symptoms include:
the appearance or intensification of a dry cough by barking near the source of an allergic reaction;
no runny nose;
disappearance and resumption, as well as the seasonality of the occurrence of cough.
Foreign body in the larynx . Most often, this situation occurs during the game in children. Symptoms depend on the size of the foreign object:
if there is a small object in the larynx – a strong barking cough, heavy breathing, sputum may be separated with pus;
foreign bodies of large size provoke hoarseness of voice, blue face – in this case, coma, respiratory and cardiac arrest can occur. The man needs immediate help!
How to treat a barking cough
The doctor will best answer the question of how to treat a dry barking cough in a child, so in no case should you postpone a visit to him for a long time.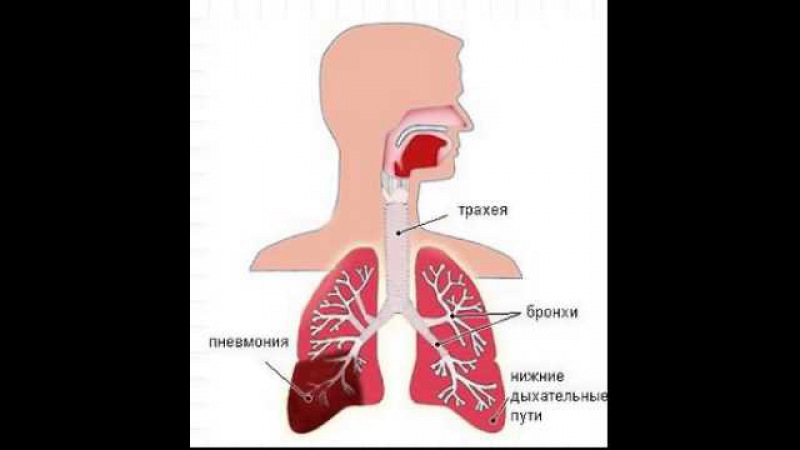
As a remedy for barking cough for children, the doctor may prescribe:
antibiotics. Antibiotic drugs are effective against viruses and bacteria and are usually given at elevated temperatures unless antipyretics help. The following medications are recommended: aminopenicillins, tetracyclines – are prescribed for children over 8 years old, macrolides – one of the most gentle among antibiotics, have a strong antimicrobial effect, Roxithromycin and Azithromycin are usually prescribed, fluoroquinolones – for children from 8 years old, pediatricians prescribe Levofloxacin or Moxifloxacin .
antitussives. It helps to relieve bouts of barking cough, especially at night. Babies at the age of 2 months are prescribed Sinekod drops, from 6 months – Panatus syrup, from a year – Hederin syrup, from 3 years – Bronchoton, Bronchocin, Bronholitin, Codelac Neo, Omnitus, Sinekod syrups, from 4 years – Alex Plus lozenges and syrup Glycodin.
antihistamines.
 They are used to relieve swelling in the airways. Usually antihistamines are prescribed for asthmatic diseases caused by allergic reactions. In pharmacies in Moscow, a large selection of such tablets is presented: Tavegil, Edem, Diazolin, Fenistil, Suprastin, Clemastin, Loratadin.
They are used to relieve swelling in the airways. Usually antihistamines are prescribed for asthmatic diseases caused by allergic reactions. In pharmacies in Moscow, a large selection of such tablets is presented: Tavegil, Edem, Diazolin, Fenistil, Suprastin, Clemastin, Loratadin.
During treatment with antibiotics, it is required to take probiotics – Linex, Laktovit, Bifidumbacterin. They will help minimize the effect of drugs on the gastrointestinal tract.
When deciding how to treat a barking cough in an adult, the doctor first of all focuses on the cause that causes it. For very strong, debilitating attacks, opioid drugs are usually prescribed, which include dextromethorphan and codeine. These tablets successfully suppress the cough reflex. Antibiotics are also used. In order to get rid of the barking cough that occurs at night, the doctor may prescribe antihistamines or preparations containing glaucine – syrups Bronchitusen Vramed, Broncholitin, Broncholitin sage, Bronchosevt, Bronchoton, Bronchocin, Glauvent or Glaucin (dragees, syrup or tablets).
Also, mustard plasters, aromatherapy, baths can be used as a remedy for dry cough with barking. A good result is given by inhalation, which can be done by children and adults at home. To do this, pour a liquid containing the medicine into the container, bend over it, cover your head with a cloth (towel, diaper), and carefully inhale the steam. It is important that the liquid is not excessively hot, otherwise there is a high risk of burning the respiratory tract. In children, a nebulizer is usually used for inhalation – it is safe and convenient. In solutions for inhalation treatment, the following are used:
saline;
mucolytics in solution – ACC injection, Fluimucil, Acestine, Mukomist;
decoctions of medicinal plants – licorice, chamomile, coltsfoot, plantain, calendula, elecampane, pine;
essential oils – eucalyptus, mint, pine.
It is important to remember that it is forbidden to do inhalation in the presence of cardiovascular diseases and high temperature. After completing the procedure, you should stay at home for two hours, especially when the air temperature is cold outside.
After completing the procedure, you should stay at home for two hours, especially when the air temperature is cold outside.
Traditional medicine methods can also be used in the fight against barking cough in children and adults. These include the preparation of milk with honey, egg mixture, onion or lemon decoction, ginger drink, date tea, cabbage and carrot juices.
When to urgently call an ambulance
In no case do not try to treat or be treated on your own and immediately call an ambulance in the following cases:
when the barking cough does not stop;
when, along with coughing, attacks of suffocation appeared;
hyperthermia occurred;
breathing became wheezing;
the skin turned pale.
Prevention of barking cough in children and adults
Measures to prevent the appearance of a barking cough include maintaining a healthy lifestyle, walking in the fresh air, wearing clothes for the season, and a healthy and balanced diet.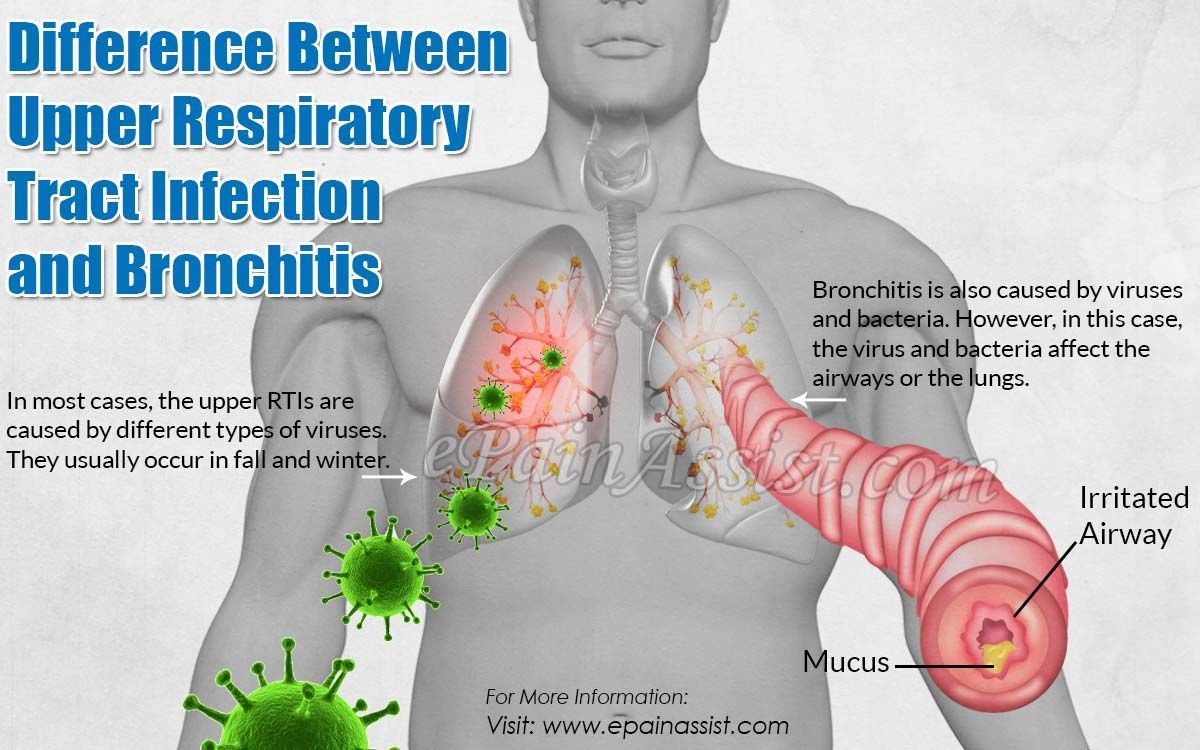 Also a very important way of prevention is a timely visit to the doctor at the first sign of malaise.
Also a very important way of prevention is a timely visit to the doctor at the first sign of malaise.
Pulmonology: Chronic cough – diagnosis and treatment in St. Petersburg, price
In the vast majority of cases, patients with pulmonary diseases often complain of cough. As a rule, the disease of the respiratory tract begins with this symptom and cough during the initial examination is revealed as the main complaint.
It is a natural protective reflex, through which the body removes excess sputum, foreign bodies, pollutants (dust, dirt, smoke). Physiologically, this process is a sharp, rapid, expiratory contraction of the respiratory muscles, aimed at cleansing the bronchial tree.
Cough is usually associated with diseases of the respiratory system, but this is not always the case, it can also be with some diseases that are not related to the pathology of the respiratory system.
Based on the classification, we conditionally divide the cough by duration:
- if the cough lasts 3 weeks or less, then it is called acute .

- cough lasting more than 3 weeks – chronic .
If we talk about the reasons, then acute cough occurs more often with colds, and the cause of chronic cough, as a rule, is a complex of diseases. In 25% of patients, chronic cough is usually associated with 2 causes, and in 3% there are three causes of its occurrence.
Cough in bronchial asthma
This is a disease that has different clinical manifestations, including the cough form. With this form of the disease, coughing may be its only manifestation and the only complaint of the patient. However, adequately selected anti-asthma therapy brings a good effect from the treatment, which confirms the correctness of the diagnosis.
In bronchial asthma, basic therapy is prescribed, which includes inhaled corticosteroids and bronchodilators. Bronchodilators, in turn, can be divided into drugs that act briefly and drugs that act for a long time. In the arsenal of doctors for the treatment of this disease, there are also combined drugs.
Cough with postnasal drip
The cause of Drip-syndrome is a secret that, during a runny nose, flows from the nasal cavity into the pharynx, its laryngeal part. Cough is reflex in nature and appears as a result of mechanical irritation of the pharyngeal receptors. In this case, it is necessary to treat rhinitis, which caused the syndrome of postnasal drip. And, of course, the treatment depends on the genesis of this rhinitis. With non-allergic rhinitis, vasoconstrictor drugs and antihistamines are prescribed. The combination of these drugs reduces swelling and mucus production. In the case of allergic rhinitis, glucocorticoids and cromoglycates in the form of a nasal spray are commonly used.
GERD is the third cause of chronic cough. In this case, the cough reflex occurs due to increased acidity in the lower esophagus, caused by the reflux of stomach contents into the esophagus. In this case, the patient is shown a consultation with a gastroenterologist, so that the doctor evaluates the duration and frequency of GERD episodes, prescribes an endoscopic examination of the esophagus and stomach, conducts a 24-hour esophageal PH-metry and suggests adequate treatment.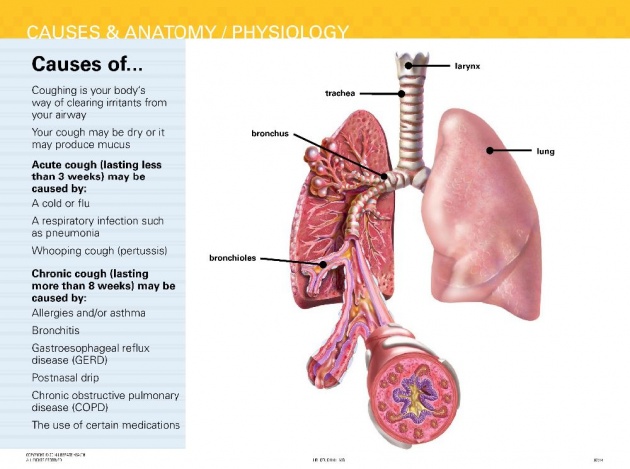
Chronic cough in chronic bronchitis
This disease is characterized by chronic inflammation of the airways and excessive sputum production. The therapy of this chronic disease is aimed at reducing the formation of sputum and its effective removal from the bronchial tree, reducing the level of inflammation of the respiratory tract, and reducing bronchospasm. It should be noted the need to stop the impact of adverse factors (smoking cessation, compliance with labor protection standards in hazardous industries).
Another disease in which cough is one of the important symptoms of the disease is bronchiectasis . The disease is characterized by a chronic suppurative process in irreversibly altered (enlarged, deformed) and functionally defective bronchi, mainly in the lower sections of the lungs. It is also accompanied by a violation of the drainage function of the bronchial tree and stagnation of sputum. The doctor establishes the diagnosis by carefully collecting an anamnesis and analyzing the data obtained as a result of the examination. Specialists perform endoscopic examination of the bronchi (video bronchoscopy), as well as examine the chest organs using computed tomography.
Specialists perform endoscopic examination of the bronchi (video bronchoscopy), as well as examine the chest organs using computed tomography.
It should be noted that chronic cough in bronchiectasis is a way to remove large volumes of sputum and does not require treatment without exacerbation. In exacerbation of bronchiectasis, antibiotic therapy is indicated based on the results of sputum culture, as well as mucolytic (thinning sputum) and expectorant therapy, the purpose of which is to improve mucociliary clearance.
Mention should also be made of chronic cough, which disturbs the patient for a long time, after suffering infectious diseases of the respiratory tract, for example: o.bronchitis, o.tracheitis and pneumonia. With a cough that continues after an infectious disease, laboratory and radiographic findings of the chest organs are usually normal. Usually, this kind of cough stops on its own over time, however, in cases of a protracted course, physiotherapy, drainage massage, and nembulizer therapy are recommended.
Cancers of the respiratory system can also cause chronic cough. To diagnose such dangerous diseases, the doctor uses anamnesis, a thorough examination of the patient, radiation methods of research, fibro- or video bronchoscopy are prescribed, if necessary, a bronchial biopsy is performed followed by a histological examination, sputum is examined by laboratory methods, etc.
ACE inhibitors may cause coughing
Specialists often prescribe ACE inhibitors to patients suffering from arterial hypertension and cardiac pathology. This group of drugs is widely used in therapy, but all drugs in this group, to one degree or another, have a class-effect cough. In this case, the cough is dry, accompanied by perspiration and occurs with any dose of the drug taken. If the drug is discontinued, then the cough disappears within 3-4 weeks on its own.
Chronic cough can also occur in patients with impaired swallowing reflex, which occurs with neurological diseases. In this case, the help of a qualified neurologist is required.
Cough diagnosis
In this article, it was not possible to list all diseases in which cough occurs as a symptom. Summing up, we can say that cough is characteristic of many diseases and arises from various reasons, in some cases it does not require treatment by itself. In order to assess this symptom in the pathogenesis of the disease and prescribe adequate therapy, a complete and comprehensive diagnosis is required, which includes a consultation with a therapist, an ENT doctor, a pulmonologist, and, if necessary, a cardiologist and neurologist, and maybe other specialists.
The gold standard for diagnosis is Rg-diagnosis of the organs of the chest cavity, and, if necessary, computed tomography. Such a research method as fibro- or video bronchoscopy (FBS) is often prescribed for coughing, it allows you to visually assess the patency and condition of the mucous membranes of the bronchial tree, as well as obtain swabs and tissue samples for laboratory and cytological studies.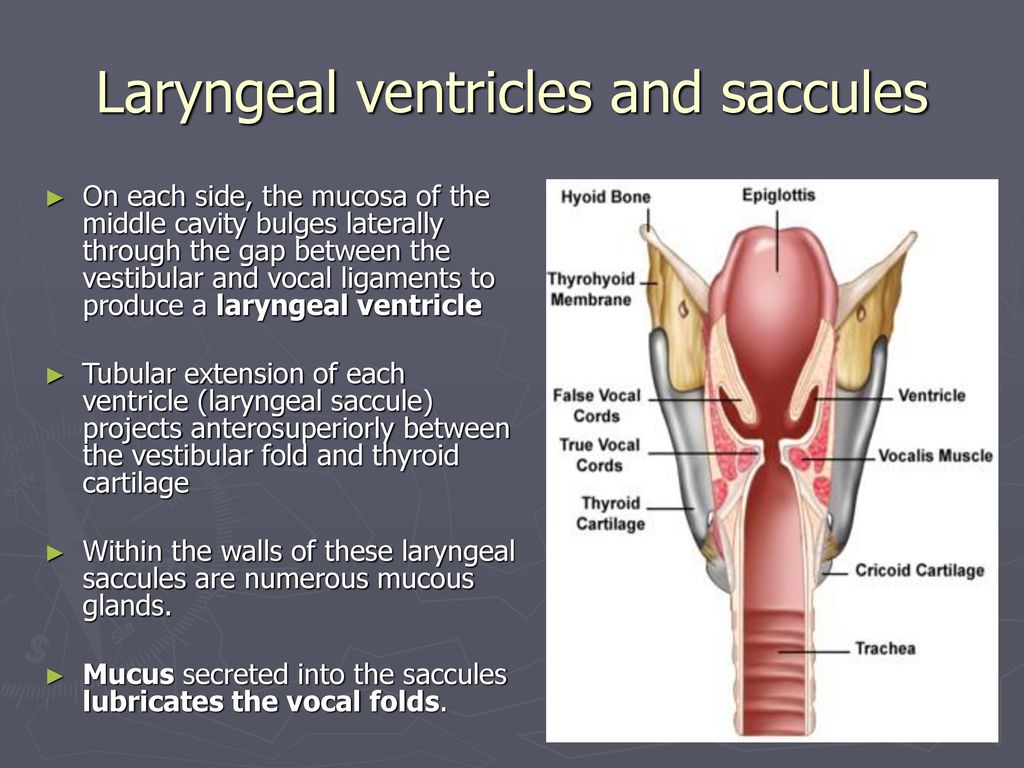


 Heliox for croup in children. Cochrane Database Syst Rev. 2018 Oct 29;10(10):CD006822. [PMC free article: PMC6516979] [PubMed: 30371952]
Heliox for croup in children. Cochrane Database Syst Rev. 2018 Oct 29;10(10):CD006822. [PMC free article: PMC6516979] [PubMed: 30371952] Pediatr Radiol. 2017 Dec;47(13):1745-1750. [PMC free article: PMC5901753] [PubMed: 28831577]
Pediatr Radiol. 2017 Dec;47(13):1745-1750. [PMC free article: PMC5901753] [PubMed: 28831577]
 (2023, January 24). Croup – Acute Laryngotracheobronchitis. News-Medical. Retrieved on June 10, 2023 from https://www.news-medical.net/health/Croup-Acute-Laryngotracheobronchitis.aspx.
(2023, January 24). Croup – Acute Laryngotracheobronchitis. News-Medical. Retrieved on June 10, 2023 from https://www.news-medical.net/health/Croup-Acute-Laryngotracheobronchitis.aspx.

 They are used to relieve swelling in the airways. Usually antihistamines are prescribed for asthmatic diseases caused by allergic reactions. In pharmacies in Moscow, a large selection of such tablets is presented: Tavegil, Edem, Diazolin, Fenistil, Suprastin, Clemastin, Loratadin.
They are used to relieve swelling in the airways. Usually antihistamines are prescribed for asthmatic diseases caused by allergic reactions. In pharmacies in Moscow, a large selection of such tablets is presented: Tavegil, Edem, Diazolin, Fenistil, Suprastin, Clemastin, Loratadin.