Late Life Lactose Intolerance: Causes, Symptoms, and Management Strategies
Can lactose intolerance develop as you age. What are the common symptoms of lactose intolerance. How can you manage lactose intolerance in later life. What foods should you avoid if you’re lactose intolerant. Are there any treatments available for lactose intolerance.
Understanding Lactose Intolerance: A Common Digestive Issue
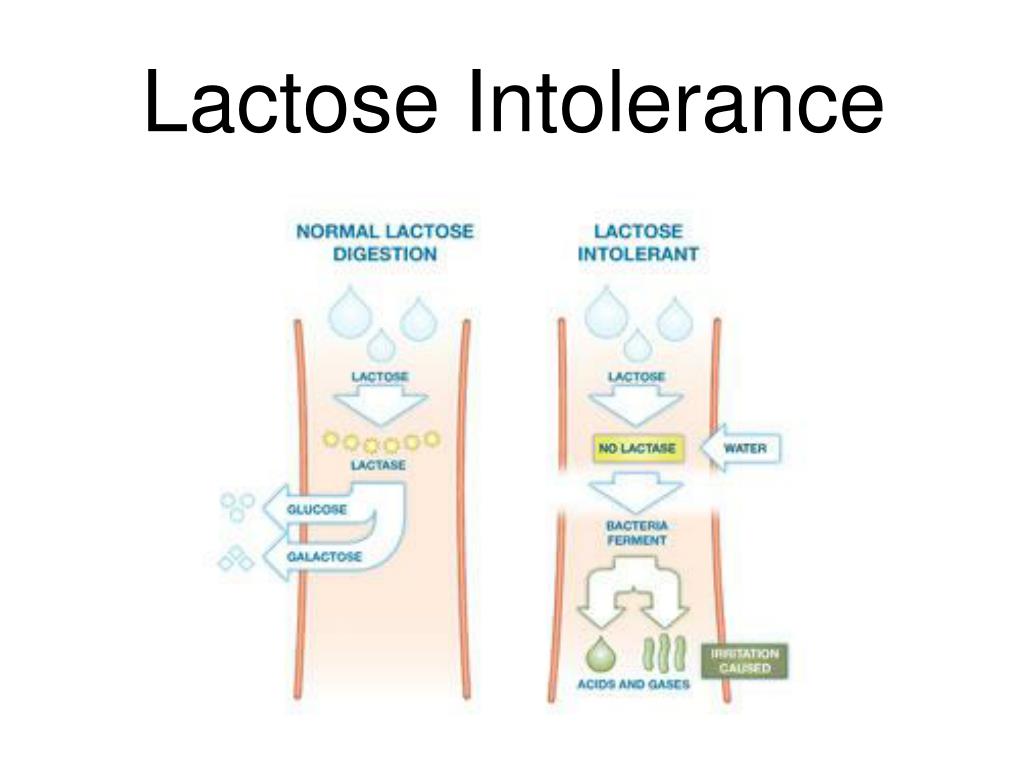
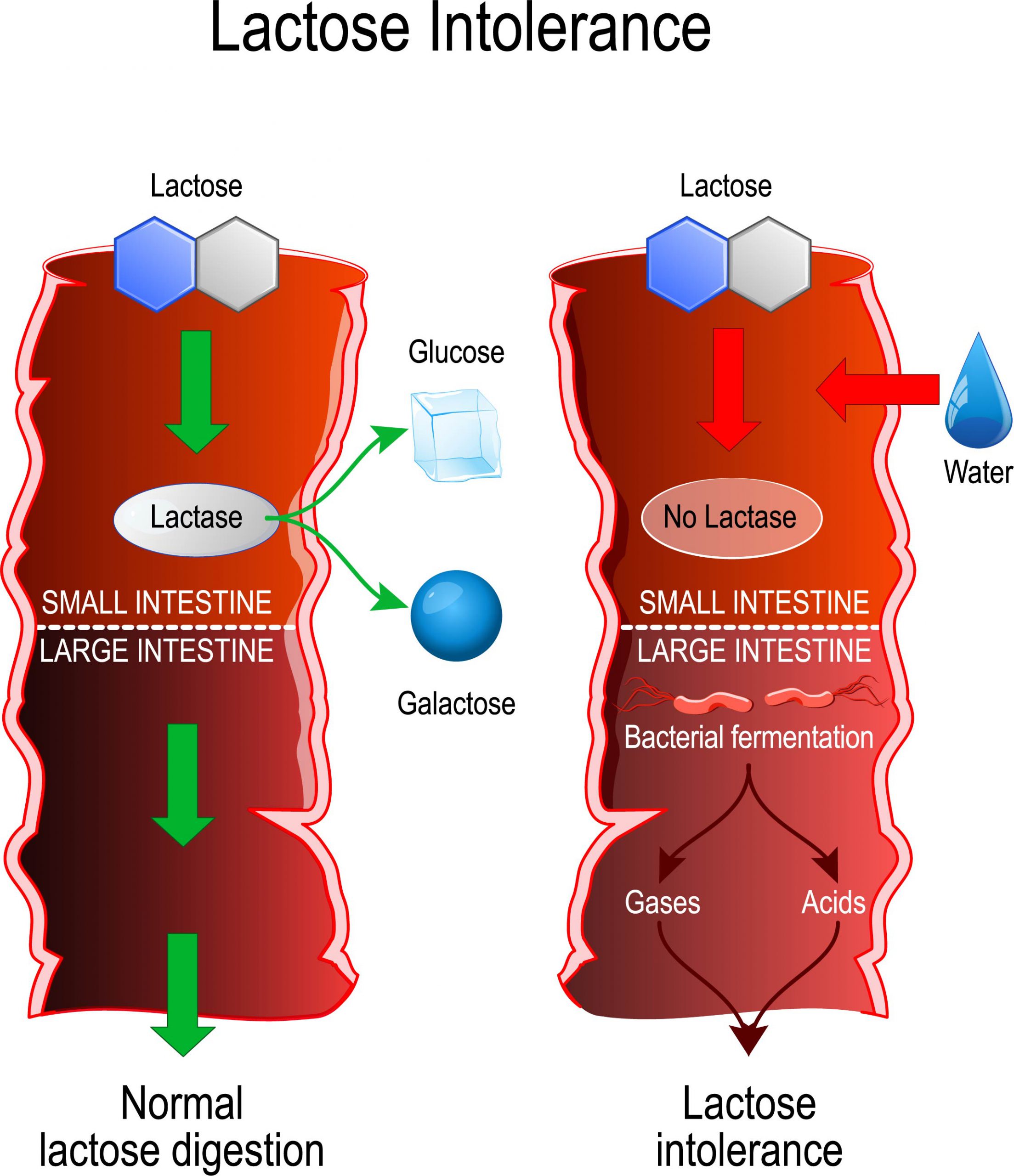
Lactose intolerance is a digestive condition that affects millions of people worldwide. It occurs when the body is unable to properly digest lactose, the primary sugar found in dairy products. This inability stems from a deficiency in lactase, an enzyme produced in the small intestine that breaks down lactose into simpler sugars for absorption.
While many associate lactose intolerance with childhood or adolescence, it’s important to note that this condition can develop at any age, including later in life. This phenomenon is known as late-onset or adult-onset lactose intolerance.
What causes lactose intolerance?
The primary cause of lactose intolerance is a decrease in lactase production. Laura Acosta, a registered dietitian at the University of Florida, explains that some individuals maintain their ability to tolerate lactose throughout their lives, while others experience a decline in lactase production as they age. This decline is often genetically determined.

The Prevalence of Lactose Intolerance in Different Populations
Lactose intolerance is not evenly distributed across all populations. Dr. Vijaya Surampudi, an assistant professor of medicine at the University of California, Los Angeles, notes that certain ethnic groups are more prone to lactose intolerance due to genetic factors.
- Southeast Asian
- East Asian
- West African
- Native American
- Hispanic
- Italian
These populations have a higher likelihood of carrying the gene mutation associated with lactose intolerance. Dr. Surampudi estimates that approximately 65% of people may experience lactose intolerance at some point in their lives.
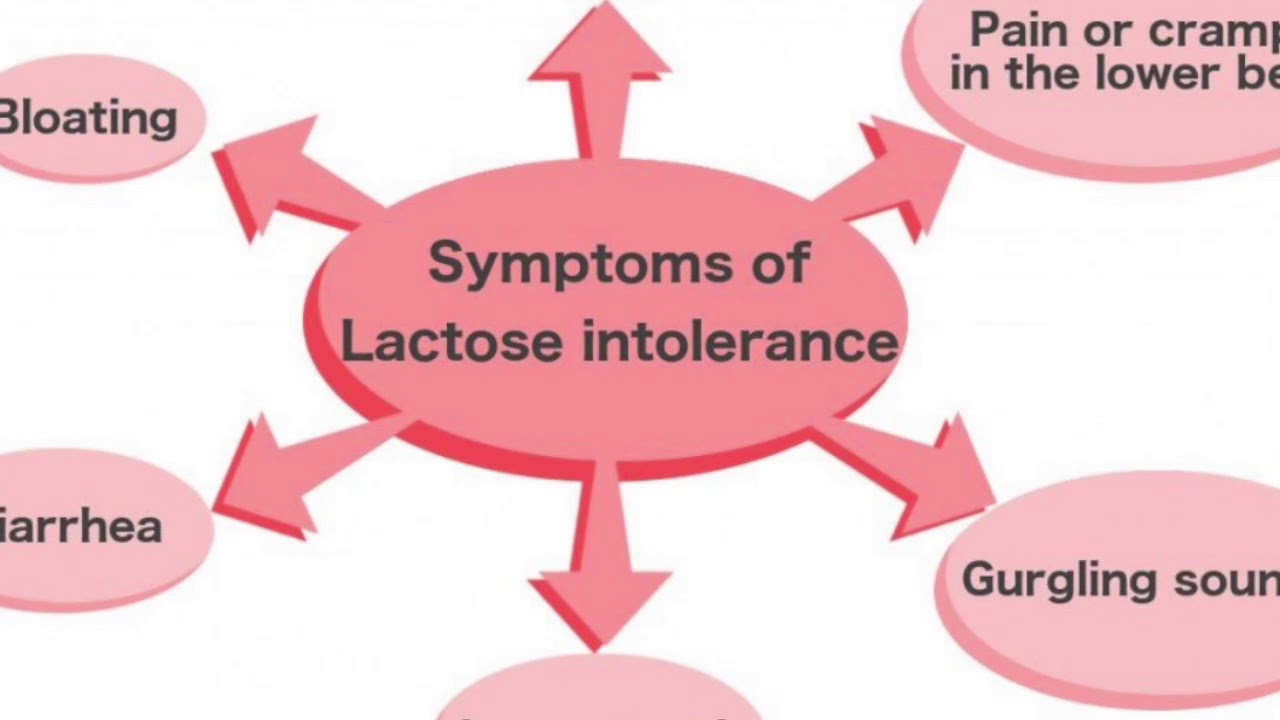
Recognizing the Symptoms of Lactose Intolerance
Identifying lactose intolerance can be challenging, as symptoms may vary in severity and onset. Common signs of lactose intolerance typically appear 30 minutes to 2 hours after consuming dairy products and may include:
- Gas
- Bloating
- Stomach discomfort
- Diarrhea
Is lactose intolerance a serious health condition? While the symptoms can be uncomfortable and disruptive, lactose intolerance itself is not considered a severe health issue. However, it’s crucial to manage the condition to maintain comfort and ensure proper nutrition.

The Aging Factor: Why Lactose Intolerance Can Develop Later in Life
Dr. Christine Lee, a gastroenterologist at Cleveland Clinic, explains that it’s relatively common for lactose intolerance to manifest as we age. This is due to the natural decline in lactase enzyme production over time. However, the onset and severity of lactose intolerance can vary significantly among individuals.
Are there other factors that can trigger lactose intolerance in adults? Yes, certain conditions and circumstances can lead to the development of lactose intolerance later in life:
- Illnesses affecting the digestive system
- Intestinal infections
- Medications that impact bowel or intestinal function
- Crohn’s disease
- Ulcerative colitis
- Celiac disease
- Injury or trauma to the small intestines
Navigating Diet Choices with Lactose Intolerance
Managing lactose intolerance often involves making dietary adjustments. However, it’s important to note that not all individuals with lactose intolerance need to completely eliminate dairy from their diet.
Which foods contain lactose?
Lactose can be found in a wide range of dairy products and foods that use dairy as an ingredient. Common sources include:
- Milk and milk-based products
- Cheese
- Whey
- Butter
- Ice cream
- Heavy cream
- Cottage cheese
- Yogurt
It’s also important to be aware of hidden sources of lactose in processed foods. Always check ingredient labels for terms like “milk by-products,” “dry milk,” or “curds.”
Can lactose-intolerant individuals consume any dairy products?
Interestingly, some people with lactose intolerance may still be able to tolerate certain dairy products. Acosta explains that cheese, particularly hard varieties, contains very little lactose. Parmesan and Swiss cheese, for example, may be tolerable in small amounts for some individuals with lactose intolerance.
Yogurt is another dairy product that some lactose-intolerant people can consume. The live bacteria cultures in yogurt can help produce the lactase enzyme, aiding in lactose digestion.

Strategies for Managing Lactose Intolerance
If you suspect you’ve developed lactose intolerance, it’s essential to consult with your healthcare provider for proper diagnosis and management strategies. Here are some approaches that can help:
- Gradual reduction: Some individuals may be able to tolerate small amounts of dairy or switch to skim milk with fewer symptoms.
- Lactase supplements: Over-the-counter lactase tablets or drops can be taken before consuming dairy to aid in lactose digestion.
- Lactose-free alternatives: Many dairy products now come in lactose-free versions, allowing you to enjoy the taste and nutritional benefits without the digestive discomfort.
- Treating underlying conditions: If lactose intolerance is secondary to another health issue, addressing the primary condition may help alleviate symptoms.
Ensuring Adequate Nutrition with Lactose Intolerance
One of the primary concerns for individuals with lactose intolerance is maintaining adequate calcium intake. Calcium is crucial for bone health, muscle function, and nerve signaling. Allie Wergin, a registered dietitian/nutritionist with Mayo Clinic Health System, emphasizes that there are many calcium-rich foods that don’t contain lactose:

- Lactose-free dairy products (e.g., Lactaid or Dairy Ease milks)
- Leafy green vegetables (e.g., kale, collard greens, spinach)
- Fortified plant-based milk alternatives (e.g., soy milk, almond milk)
- Canned fish with soft bones (e.g., sardines, salmon)
- Calcium-fortified juices and cereals
- Nuts and seeds (e.g., almonds, sesame seeds)
When to Seek Medical Advice
While lactose intolerance is generally not a serious condition, it’s important to be aware of symptoms that may indicate a more severe underlying issue. Dr. Lee advises seeking medical attention if you experience:
- Unexplained weight loss
- Bleeding
- Anemia
- Persistent nausea or vomiting
These symptoms may be indicative of other gastrointestinal conditions that require medical intervention.
How is lactose intolerance diagnosed?
Diagnosing lactose intolerance typically involves a combination of methods:
- Hydrogen breath test: This non-invasive test measures the amount of hydrogen in your breath after consuming lactose.
- Lactose tolerance test: Blood samples are taken to measure glucose levels after consuming a lactose-containing liquid.
- Stool acidity test: This test is often used for infants and young children to measure the amount of acid in the stool.
- Genetic testing: In some cases, genetic testing may be used to identify lactase persistence.
The Future of Lactose Intolerance Management
As our understanding of lactose intolerance grows, so do the management options available to those affected. Researchers are exploring various avenues to improve the quality of life for individuals with lactose intolerance:

- Development of more effective lactase supplements
- Genetically modified dairy products with reduced lactose content
- Probiotic therapies to enhance lactose digestion
- Personalized nutrition plans based on genetic testing
These advancements hold promise for more tailored and effective management strategies in the future.
Can lactose intolerance be reversed?
While lactose intolerance is generally considered a permanent condition, some research suggests that it may be possible to improve lactose tolerance through gradual exposure. This approach, known as lactose adaptation, involves slowly increasing lactose consumption over time to help the body adjust. However, this method should only be attempted under medical supervision.
Living Well with Lactose Intolerance
Developing lactose intolerance later in life can be challenging, but it doesn’t have to significantly impact your quality of life. With proper management and dietary adjustments, most people can find a balance that works for them. Here are some tips for living well with lactose intolerance:

- Experiment with different dairy products to find your personal tolerance level
- Keep a food diary to track symptoms and identify trigger foods
- Explore lactose-free alternatives to your favorite dairy products
- Consider taking a calcium supplement if you’re unable to meet your needs through diet alone
- Stay informed about hidden sources of lactose in processed foods and medications
- Communicate with friends and family about your dietary needs to make social situations easier
Remember, lactose intolerance is a common condition that affects millions of people worldwide. With the right approach and support, you can continue to enjoy a varied and nutritious diet while managing your symptoms effectively.
Are there any benefits to being lactose intolerant?
While lactose intolerance is generally viewed as a limitation, some researchers suggest that it may have evolutionary advantages. For example, individuals who are lactose intolerant may have a lower risk of certain types of cancer associated with high dairy consumption. However, more research is needed to fully understand these potential benefits.

Lactose Intolerance in a Global Context
Lactose intolerance varies significantly across different regions and cultures. In some parts of the world, particularly in Northern Europe, lactose tolerance is the norm due to a long history of dairy consumption. In contrast, in many Asian and African countries, lactose intolerance is highly prevalent.
This global variation has led to diverse culinary traditions and dairy alternatives. For example:
- East Asian cuisines often use soy-based products as dairy alternatives
- African cuisines frequently incorporate fermented dairy products that are lower in lactose
- Mediterranean diets often feature aged cheeses and yogurt, which are more tolerable for many lactose-sensitive individuals
Understanding these cultural differences can provide valuable insights into managing lactose intolerance and expanding dietary options.
How does lactose intolerance impact the dairy industry?
The increasing prevalence of lactose intolerance has prompted the dairy industry to innovate and adapt. This has led to:

- Development of lactose-free dairy products
- Increased production of plant-based milk alternatives
- Research into cow breeds that produce milk with naturally lower lactose content
- Exploration of new processing techniques to reduce lactose in dairy products
These industry changes not only benefit those with lactose intolerance but also provide more options for consumers in general.
Dispelling Myths About Lactose Intolerance
Despite its prevalence, lactose intolerance is often misunderstood. Let’s address some common misconceptions:
Is lactose intolerance the same as a milk allergy?
No, lactose intolerance and milk allergies are distinct conditions. Lactose intolerance is a digestive issue caused by the inability to break down lactose. A milk allergy, on the other hand, is an immune system response to proteins in milk. Milk allergies can be more severe and potentially life-threatening, while lactose intolerance, though uncomfortable, is not dangerous.
Does lactose intolerance mean you can’t consume any dairy at all?
Not necessarily. Many people with lactose intolerance can tolerate small amounts of dairy or certain types of dairy products. It’s often a matter of finding your personal tolerance level and choosing dairy products wisely.

Can you become lactose intolerant overnight?
While it may seem like lactose intolerance develops suddenly, it’s usually a gradual process. The decline in lactase production typically occurs over time, but you might only notice symptoms when they reach a certain threshold.
The Psychological Impact of Late-Onset Lactose Intolerance
Developing lactose intolerance later in life can have psychological effects that are often overlooked. Some individuals may experience:
- Frustration at having to change long-established dietary habits
- Anxiety about eating out or in social situations
- Sadness over giving up favorite foods
- Worry about nutritional deficiencies
It’s important to address these emotional aspects of lactose intolerance. Support groups, nutritional counseling, and education can help individuals adapt to their new dietary needs and maintain a positive outlook.
How can you cope with the emotional aspects of lactose intolerance?
Coping with lactose intolerance involves both physical and emotional strategies:

- Educate yourself about the condition and available management options
- Focus on the foods you can eat rather than those you need to avoid
- Experiment with new recipes and lactose-free alternatives
- Connect with others who have lactose intolerance for support and tips
- Practice mindfulness and stress-reduction techniques to manage anxiety around food
Remember, developing lactose intolerance doesn’t define you. With the right approach, you can continue to enjoy a diverse and satisfying diet while maintaining your health and well-being.
Can You Get It as You Get Older?
Written by Susan Bernstein
Do you get gas, bloating, or even diarrhea after you eat dairy foods? You may be lactose intolerant. This is when you can’t digest lactose, the type of sugar found in dairy products.
Lactose intolerance isn’t a serious health condition, but symptoms can be uncomfortable. You may have stomach upset or gas about 30 minutes to 2 hours after you eat or drink any dairy food.
Lactose intolerance is caused by low levels of lactase, an enzyme that helps you digest lactose in dairy foods, says Laura Acosta, a registered dietitian at the University of Florida in Gainesville.
“Some people are able to tolerate lactose throughout their lives, but others become more lactose intolerant as they age,” usually caused by your genes, she says. “Some people stop producing lactase, or produce less of it, as they reach adulthood and beyond.”
Lactose intolerance is more common among people of Southeast Asian, East Asian, West African, Native American, Hispanic, or Italian ancestry because they’re more likely to carry the gene mutation that causes the condition, says Vijaya Surampudi, MD, assistant professor of medicine at the University of California, Los Angeles.
“We have the highest amounts of lactase when we are young because as babies, we feed on milk. But we often make less and less lactase as we age,” she says. “About 65% of people may experience lactose intolerance at some point in their lives.”
There’s a wide range of lactose intolerance, with some people having no tolerance for dairy, while others can manage to digest foods like hard cheeses or yogurt, she says.
It’s fairly common to notice the signs of lactose intolerance appear as you get older, says Christine Lee, MD, a gastroenterologist at Cleveland Clinic in Ohio.
“This enzyme production can decrease over time in some people, so most people can experience some degree of lactose intolerance as they get older,” Lee says. You can also become lactose intolerant if you have an illness, infection, or take a medication that affects the bowels or intestines.
These conditions can also cause you to develop lactose intolerance later in life:
- Crohn’s disease
- Ulcerative colitis (UC)
- Celiac disease
- Injury or trauma to your small intestines
Foods.![]() Any dairy foods or drinks can have lactose, so read food labels carefully. These foods or ingredients may trigger symptoms:
Any dairy foods or drinks can have lactose, so read food labels carefully. These foods or ingredients may trigger symptoms:
- Cheese
- Whey
- Milk by-products
- Dry milk
- Butter
- Curds
- Ice cream
- Heavy cream
- Cottage cheese
- Cheese spreads
- Yogurt
Look for milk in ingredients lists in baked goods, chocolate candies, sauces, instant mashed potatoes, pancakes, or milk-based meal replacement or protein shakes. Even non-dairy coffee creamer or whipped toppings may contain some lactose.
Medications. Some medications like birth control pills or antacid tablets also contain lactose, but these may only cause symptoms in people with severe lactose intolerance. Check the labels of your prescription or OTC medications to see if they contain lactose. Ask your doctor or pharmacist if it’s OK for you to take them.
You may not have to give up all the dairy foods you enjoy if you develop lactose intolerance.
Some people with lactose intolerance may be able to eat or drink small amounts of dairy or switch to skim milk and have fewer symptoms. Some people can eat yogurt because it contains live bacteria cultures that help you produce the lactase enzyme to break down lactose.
“Cheese actually has very little lactose. In general, the harder the cheese, the less lactose it has. So many people with lactose intolerance can still tolerate cheese like Parmesan and Swiss in small amounts. This depends on an individual’s sensitivity,” Acosta says.
Talk to your doctor to identify what’s causing your lactose intolerance so you can make the right changes to your diet, Lee says.
“If it’s due to decreased production of lactase, then you can choose to take lactase tablets or drops, enzymes sold in most grocery stores without a prescription, or buy lactose-free milk products,” she says. Supplements are taken before a meal with dairy to help you digest the lactose.
If your lactose intolerance is due to a bowel disease or other health conditions, treat that illness first, she adds. “Always play it safe and discuss your symptoms with your physician.” Unexplained weight loss, bleeding, anemia, nausea, or vomiting may be signs of a more serious medical condition, not just lactose intolerance, she says.
“Always play it safe and discuss your symptoms with your physician.” Unexplained weight loss, bleeding, anemia, nausea, or vomiting may be signs of a more serious medical condition, not just lactose intolerance, she says.
As you age, you still need to get enough calcium even if you develop lactose intolerance. Calcium helps you maintain strong bones and teeth, and healthy muscles and nerves.
“There are many calcium-rich foods people can eat if they’re avoiding lactose,” says Allie Wergin, a registered dietitian/nutritionist with Mayo Clinic Health System. “These include lactose-free dairy products like Lactaid or Dairy Ease milks, where the lactose is predigested or hydrolyzed. This means the milk protein has already been broken down and is easier to digest.”
Other foods that are good sources of calcium, according to Wergin:
- Calcium-fortified cereals and fruit juices
- Tofu prepared using calcium sulfate
- Canned salmon or sardines with bones
- Plant-based soy, almond, oat, or rice milks
- Leafy green vegetables like spinach, kale, bok choy, or collard greens
- Broccoli
- Almonds
- Beans like garbanzo, kidney, or navy
“We recommend that you get calcium through your diet. There are different calcium supplements, including calcium carbonate, which is best absorbed if you take it with food, and calcium citrate, which you can take with or without food,” Surampudi says. Only take a calcium supplement if your doctor says you need one, she says.
There are different calcium supplements, including calcium carbonate, which is best absorbed if you take it with food, and calcium citrate, which you can take with or without food,” Surampudi says. Only take a calcium supplement if your doctor says you need one, she says.
Top Picks
Mayo Clinic Q and A: Lactose Intolerance Can Develop at Any Age
By
Liza Torborg
DEAR MAYO CLINIC: What would cause someone to become lactose-intolerant later in life? I’m in my 40s and have never had an issue with dairy, but, now, I can’t seem to have it without problems.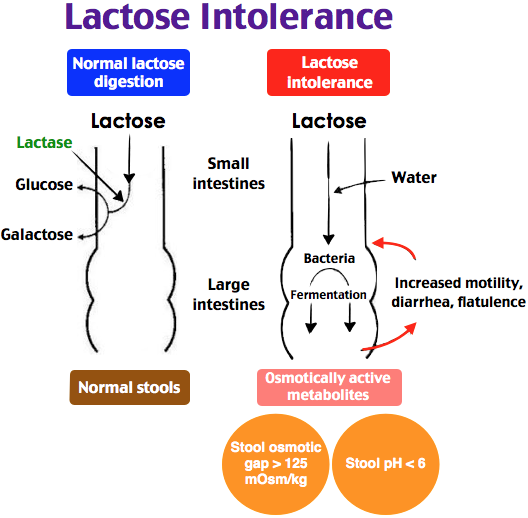 Do I need to see a doctor to be tested for allergies, or should I just avoid dairy?
Do I need to see a doctor to be tested for allergies, or should I just avoid dairy?
ANSWER: Lactose intolerance isn’t a true allergy, and it can develop at any age. In some people, lactose intolerance may be triggered by another medical condition, such as Crohn’s disease. In others, it develops without a specific underlying cause. It would be a good idea to have your condition evaluated by your doctor to confirm that what you’re dealing with truly is lactose intolerance.
Lactose intolerance results from a problem with the carbohydrate lactose, a type of sugar found in dairy products. When you eat or drink dairy products, enzymes in your small intestine digest lactose, so the body can make energy. In people with lactose intolerance, a certain enzyme, called lactase, is missing from the body. When those people eat dairy products, the body has no way to break down the lactose. This leads to fermentation of the sugar in the intestines and triggers symptoms, such as diarrhea, nausea, abdominal cramps, bloating and gas.
Sometimes, lactose intolerance develops when the small intestine’s production of lactase decreases after an illness, injury or surgery involving the small intestine. This is called secondary lactose intolerance. Among the diseases associated with this kind of lactose intolerance are celiac disease, bacterial overgrowth and Crohn’s disease. Treatment of the underlying disorder may restore lactase levels and improve symptoms.
More common than secondary lactose intolerance is primary lactose intolerance. People who develop primary lactose intolerance start life making normal levels of lactase — a necessity for infants, who get all their nutrition from milk. As children replace milk with other foods, lactase production normally decreases. It stays high enough, though, to digest the amount of dairy in a typical adult diet. In primary lactose intolerance, lactase production declines below normal at some point for reasons that are unclear. The low amount of lactase then makes milk products difficult to digest and leads to lactose intolerance symptoms.
Your doctor can confirm a diagnosis of lactose intolerance with a clinical test. One that’s often used is a lactose tolerance test. It assesses your body’s reaction to a dose of lactose. After you consume a drink containing lactose, a sample of your blood is taken to measure glucose levels. If your glucose level does not rise, it means your body isn’t properly digesting and absorbing the lactose.
Alternatively, another test called the hydrogen breath test may be used. This test also requires you to consume a drink that contains high levels of lactose. Your doctor next measures the amount of hydrogen in your breath. Normally, very little hydrogen is detectable. However, if your body doesn’t digest the lactose, the fermentation reaction in your colon releases hydrogen and other gases. Your intestines absorb those gases, and you exhale them. Larger-than-normal amounts of hydrogen measured during this test are a sign that your body isn’t fully digesting and absorbing lactose.
If you have lactose intolerance, there isn’t a way to cure it. The most effective way for people with lactose intolerance to get relief from symptoms is to lower the amount of dairy products they eat. You may be able to use dairy products that have reduced levels of lactose or are lactose-free. Some people who have lactose intolerance benefit from taking lactase enzyme supplements, as well.
The most effective way for people with lactose intolerance to get relief from symptoms is to lower the amount of dairy products they eat. You may be able to use dairy products that have reduced levels of lactose or are lactose-free. Some people who have lactose intolerance benefit from taking lactase enzyme supplements, as well.
If test results do not point to lactose intolerance, your doctor may recommend additional tests to check for another condition that could be causing your symptoms, such as a milk allergy, intestinal disorders or other problems within your digestive tract. — Dr. Rohit Divekar, Allergic Diseases, Mayo Clinic, Rochester, Minnesota
Related articles
Understanding effects of heat on mental health
A heat wave is affecting parts of the U.S., including much of the Southwest, through the Southeast and parts of Europe. When temperatures soar, the …
By Deb Balzer • July 13, 2023
Lactose intolerance | Symptoms, complications, diagnosis and treatment
People with lactose intolerance are unable to fully digest the lactose in milk. As a result, they develop diarrhea, gas, and bloating after eating or consuming dairy products. The condition, also called lactose malabsorption, is usually harmless, but its symptoms can be uncomfortable. Most people with lactose intolerance can manage the condition without giving up all dairy products.
As a result, they develop diarrhea, gas, and bloating after eating or consuming dairy products. The condition, also called lactose malabsorption, is usually harmless, but its symptoms can be uncomfortable. Most people with lactose intolerance can manage the condition without giving up all dairy products.
Lactase deficiency, an enzyme produced in the small intestine, is usually responsible for lactose intolerance. Many people have low lactase levels but can digest dairy products without problems. If you are actually lactose intolerant, lactase deficiency leads to symptoms after you eat dairy products.
Signs and symptoms of lactose intolerance usually begin 30 minutes to two hours after eating or drinking foods containing lactose. General signs and symptoms include:
- Diarrhea
- Nausea and sometimes vomiting
- Abdominal cramps
- Inflate
- Gases
Make an appointment with your doctor if you often experience symptoms of lactose intolerance after eating dairy products, especially if you are worried about getting enough calcium.
Reasons
Lactose intolerance occurs when the small intestine does not produce enough enzyme (lactase) to digest milk sugar (lactose).
Normally, lactase converts milk sugar into two simple sugars, glucose and galactose, which are absorbed into the bloodstream through the intestinal lining.
If you are lactase deficient, the lactose in food moves to the large intestine instead of being processed and absorbed. In the colon, normal bacteria interact with undigested lactose, causing the signs and symptoms of lactose intolerance.
There are three types of lactose intolerance. Various factors cause lactase deficiency underlying each type.
Primary lactose intolerance
This is the most common type of lactose intolerance. People with primary lactose intolerance begin their lives by producing large amounts of lactase, a must for babies who get all their nutrients from milk. As children replace milk with other foods, their lactase production usually decreases but remains high enough to digest the amount of dairy in a normal adult diet.
As children replace milk with other foods, their lactase production usually decreases but remains high enough to digest the amount of dairy in a normal adult diet.
In primary lactose intolerance, lactase production drops dramatically, making it difficult for adults to digest dairy products. Primary lactose intolerance is genetically determined, which occurs in a significant proportion of people of African, Asian, or Hispanic ancestry. This condition is also common among Mediterranean or South European ancestry.
Secondary lactose intolerance
This form of lactose intolerance occurs when the small intestine reduces its production of lactase after illness, injury, or surgery involving the small intestine. Diseases associated with secondary lactose intolerance include celiac disease, bacterial overgrowth, and Crohn’s disease. Treating the underlying disorder can restore lactase levels and improve symptoms and signs, although this may take some time.
Congenital or developing lactose intolerance
This disorder is passed from generation to generation in a form of inheritance called autosomal recessive. Premature babies may also be lactose intolerant due to insufficient lactase levels.
Factors that may make you or your child more likely to become lactose intolerant, include:
- Growing up. Lactose intolerance usually appears in adulthood. This disease is rare in children and young children.
- Ethnos. Lactose intolerance is most common in African, Asian, Hispanic, and American Indian people.
- Premature birth. Babies born prematurely may have low lactase levels because the small intestine does not develop lactase-producing cells until late in the third trimester.
- Diseases affecting the small intestine. Small intestinal problems that can cause lactose intolerance include bacterial overgrowth, celiac disease, and Crohn’s disease.

- Some treatments for cancer. If you’ve had radiation therapy for abdominal cancer or intestinal complications from chemotherapy, you’re at increased risk of lactose intolerance.
Lactase deficiency in adults
Lactase deficiency is a violation of the breakdown of lactose due to a deficiency of the lactase enzyme of the small intestine mucosa, accompanied by clinical symptoms.
Lactose is milk sugar. The enzyme that breaks down lactose is called lactase.
Adult-type lactase deficiency develops after a period of breastfeeding. This is due to a gradual decrease in lactase activity with age. After taking dairy products or whole milk, intestinal disorders (diarrhea, flatulence) usually appear. Prevention and treatment consists of following a low-lactose diet or eliminating it completely.
Russian synonyms
Congenital adult lactase deficiency (delayed onset type), primary adult lactase deficiency, hypolactasia, lactose intolerance, lactose malabsorption.
English synonyms
#OMIM 223100, Lactose intolerance, adult type, Hypolactasia, adult type, Disaccharide intolerance III.
Symptoms
Lactase deficiency is characterized by the development of intestinal symptoms after taking milk and dairy products: flatulence, pain and rumbling in the abdomen, diarrhea, bloating. Possible nausea. The stool is liquid or mushy, light yellow in color, with a sour smell.
General information about the disease
Lactase deficiency, or primary lactase deficiency, is a violation of the breakdown of lactose due to a deficiency of the lactase enzyme of the small intestine mucosa, accompanied by clinical symptoms. It is caused by a genetically determined decrease in its production, which manifests itself in the inability to absorb milk sugar (lactose).
Lactase activity manifests itself from the 12-14th week of intrauterine development and reaches its maximum values by the time of birth (at the time of 39-40 weeks). After birth, lactase is produced in large quantities, but by the end of the first year of life, its production decreases. This is the primary, or congenital, late-onset lactase deficiency, which is inherited in an autosomal recessive manner.
After birth, lactase is produced in large quantities, but by the end of the first year of life, its production decreases. This is the primary, or congenital, late-onset lactase deficiency, which is inherited in an autosomal recessive manner.
Non-specific abdominal symptoms (bloating, upset stool, nausea) develop after consumption of foods containing lactose, mainly whole milk and dairy products. But today lactose is added to other foods (for example, meat, confectionery). The pharmaceutical industry also uses it as an excipient.
The severity of hypolactasia symptoms depends on individual physiological characteristics of a person, intestinal microflora, diet, and psychological factors. Conscious avoidance of milk, which is an important source of calcium, can lead to a deficiency of this element and, as a result, to osteoporosis. This should be remembered and compensate for the daily requirement through other foods rich in calcium. This is especially important for postmenopausal women.
Primary lactase deficiency should be distinguished from secondary (acquired), which occurs when the mucous membrane of the small intestine is damaged due to any acute or chronic disease. Such damage is possible with infectious (intestinal infection), immune (intolerance to cow’s milk protein), inflammatory processes in the intestine, atrophic changes (with celiac disease, after a long period of complete parenteral nutrition, etc.).
Also, this disorder should not be confused with congenital lactase deficiency, a rare genetic disorder whose symptoms appear immediately after birth and are associated with the onset of breastfeeding.
There is a genetic diagnosis of late-onset primary lactase deficiency. The MCM6 gene region is one of the important regulatory elements of the lactase gene. The genetic marker MCM6 (C(-13910)T) is associated with lactose intolerance.
Who is at risk?
- Persons with relatives who are intolerant to milk and dairy products.

- Certain ethnic groups. Lactose intolerance is most common in North America, Africa, Southeast Asia (the incidence of lactase deficiency is 70-100%) In the Russian population, lactase deficiency is observed in approximately 16%.
- The condition rarely occurs in the first year of life, the development of lactose intolerance is associated with growing up.
Diagnosis
The diagnosis can be assumed on the basis of genealogical data, results of coprology (increase in starch, fiber, iodophilic microflora, decrease in fecal pH less than 5.5), determination of carbohydrates in feces. The diagnosis uses a hydrogen breath test. The concentration of hydrogen in the exhaled air is determined before and after lactose loading. In patients with lactase deficiency, an increase in the hydrogen content is recorded, which is associated with increased bacterial breakdown of lactose in the colon. That is, lactose, not completely absorbed in the small intestine, reaches the large intestine, where it is broken down by anaerobic microflora.
Important in the diagnosis is molecular genetic testing for predisposition to lactase deficiency. The analysis will help in the differential diagnosis of the causes of lactose malabsorption and in the selection of an appropriate diet.
With severe clinical manifestations, refusal of milk, it is also important to determine the calcium content in the blood serum and urine.
Treatment
Diet therapy: restriction of products containing lactose.
It is possible to prescribe enzyme preparations that break down lactose.
It is allowed to use fermented milk products with a reduced amount of lactose (yogurt, curdled milk), cottage cheese, butter, hard cheeses, as well as lactose-free.
It is important to take into account the possible lack of calcium intake on a dairy-free diet, which is recommended to be compensated by other foods rich in it or medications.
In young children, often lactase deficiency is combined with intolerance to cow’s milk proteins.