Leg is throbbing. 15 Conditions Causing Throbbing Leg Pain: Comprehensive Guide to Nighttime Relief
What causes throbbing leg pain at night. How can you alleviate discomfort from varicose veins. Which conditions contribute to nocturnal leg pain. How does elevation impact leg pain during sleep. Why do varicose veins worsen at bedtime. What lifestyle changes can improve nighttime leg discomfort. How does hydration affect leg pain and sleep quality.
Understanding the Link Between Varicose Veins and Nocturnal Leg Pain
Throbbing leg pain can significantly disrupt your sleep, turning what should be a restorative period into a frustrating experience. While various conditions can cause nighttime leg discomfort, varicose veins are often the culprit behind these painful episodes. But why do varicose veins seem to worsen when you’re trying to rest?
Varicose veins are dilated blood vessels that struggle to pump blood efficiently. Throughout the day, the pressure of sitting or standing exacerbates this condition. When you finally lie down to sleep, the sudden change in position can cause a throbbing sensation as your circulatory system adjusts. This pain often subsides by morning, only to repeat the cycle the next night.

The Impact of Daily Activities on Varicose Veins
Your daily routine plays a significant role in the development and exacerbation of varicose veins. Prolonged periods of sitting or standing contribute to poor circulation and increased pressure in the leg veins. This pressure can cause the veins to dilate and become varicose over time.
To mitigate the impact of daily activities on your veins, consider incorporating regular movement breaks throughout your day. Simple exercises like ankle rotations, calf raises, or brief walks can help stimulate blood flow and reduce the risk of varicose vein-related discomfort at night.
Restless Leg Syndrome and Its Relationship to Varicose Veins
While varicose veins don’t directly cause Restless Leg Syndrome (RLS), they can exacerbate its symptoms, making it challenging to pinpoint the root cause of your sleep disturbances. RLS affects approximately 10% of Americans, causing an irresistible urge to move the legs, often accompanied by tingling, itching, or cramping sensations.

How can you differentiate between RLS and varicose vein-related discomfort? RLS typically involves a compelling need to move the legs, while varicose vein pain is more likely to manifest as a persistent ache or throbbing sensation. However, these conditions can coexist, complicating diagnosis and treatment.
Managing RLS Symptoms
If you suspect you have RLS in addition to varicose veins, consider these strategies to manage your symptoms:
- Establish a consistent sleep schedule
- Practice relaxation techniques before bedtime
- Avoid caffeine and alcohol in the evening
- Consider iron supplements if deficient (under medical supervision)
- Engage in regular, moderate exercise
Effective Strategies for Alleviating Nighttime Leg Pain
Addressing leg pain caused by varicose veins requires a multifaceted approach. By implementing the following strategies, you can significantly reduce discomfort and improve your sleep quality:
Elevation: A Simple Yet Powerful Solution
How does elevating your legs help reduce pain from varicose veins? By raising the foot of your bed 3-4 inches, you harness the power of gravity to assist blood flow back to your heart. This simple adjustment can alleviate pressure on your leg veins, reducing swelling and discomfort throughout the night.
To elevate your bed, place a pillow or folded blanket under the mattress at the foot end. Ensure the elevation is gradual to avoid discomfort in other areas of your body.
The Importance of a Relaxing Evening Routine
Transitioning from an active day to restful sleep can be challenging for those with varicose veins. Instead of maintaining high activity levels until bedtime, consider implementing a calming evening routine:
- Set aside time to elevate your legs before bed
- Practice gentle leg massages to improve circulation
- Engage in relaxing activities like reading or listening to soothing music
- Avoid intense exercise or stimulating activities close to bedtime
Harnessing the Benefits of Gentle Exercise
While vigorous exercise before bed can interfere with sleep, gentle stretching and yoga can promote relaxation and improve blood flow. Consider incorporating these low-impact exercises into your evening routine:
- Leg stretches (e.g., hamstring and calf stretches)
- Ankle rotations
- Gentle yoga poses like Legs-Up-the-Wall or Reclined Bound Angle
Remember to listen to your body and avoid any movements that cause pain or discomfort.

The Role of Hydration in Managing Leg Pain and Sleep Quality
Proper hydration is crucial for maintaining healthy circulation and reducing leg pain associated with varicose veins. But how exactly does hydration impact your veins and sleep quality?
When you’re well-hydrated, your blood volume increases, making it easier for your circulatory system to function efficiently. This improved blood flow can help reduce the pain and swelling associated with varicose veins. Additionally, proper hydration can help prevent muscle cramps, another common cause of nighttime leg discomfort.
Balancing Hydration and Sleep
While staying hydrated is essential, it’s important to time your fluid intake wisely to avoid disrupting your sleep with frequent trips to the bathroom. Consider these tips for optimal hydration:
- Drink water consistently throughout the day
- Reduce fluid intake 2-3 hours before bedtime
- Opt for hydrating foods like fruits and vegetables with your evening meal
- Avoid caffeinated or alcoholic beverages in the evening, as they can contribute to dehydration
Beyond Home Remedies: Medical Treatments for Varicose Veins
While lifestyle changes and home remedies can provide significant relief for many individuals with varicose veins, some may require more advanced interventions to address their symptoms effectively. What medical treatments are available for those suffering from persistent leg pain due to varicose veins?

Non-Invasive Treatments
Several non-invasive or minimally invasive treatments can effectively target varicose veins without the need for traditional surgery:
- Sclerotherapy: Injection of a solution to collapse and seal off problematic veins
- Radiofrequency ablation: Use of heat energy to close off damaged veins
- Endovenous laser treatment: Application of laser energy to seal varicose veins
- Compression therapy: Utilization of specialized stockings to improve circulation
Surgical Options
In more severe cases, surgical intervention may be necessary. These procedures are typically performed on an outpatient basis and include:
- Ambulatory phlebectomy: Removal of smaller varicose veins through tiny incisions
- Vein stripping: Surgical removal of larger varicose veins
It’s crucial to consult with a board-certified vascular surgeon to determine the most appropriate treatment for your specific condition. They can provide a comprehensive evaluation and recommend a personalized treatment plan to address your varicose veins and alleviate nighttime leg pain.

Exploring Other Conditions That Cause Nocturnal Leg Pain
While varicose veins are a common culprit behind nighttime leg pain, several other conditions can contribute to this discomfort. Understanding these potential causes can help you and your healthcare provider develop a more targeted treatment approach:
Peripheral Artery Disease (PAD)
PAD occurs when narrowed arteries reduce blood flow to the limbs. Symptoms often worsen at night and may include:
- Cramping pain in the legs, especially during activity
- Numbness or weakness in the legs
- Cold feet or legs
- Slow-healing sores on the feet or legs
Diabetic Neuropathy
This complication of diabetes can cause nerve damage, leading to various symptoms, including nighttime leg pain. Common signs include:
- Burning or tingling sensations
- Increased sensitivity to touch
- Numbness or loss of feeling in the legs and feet
- Muscle weakness
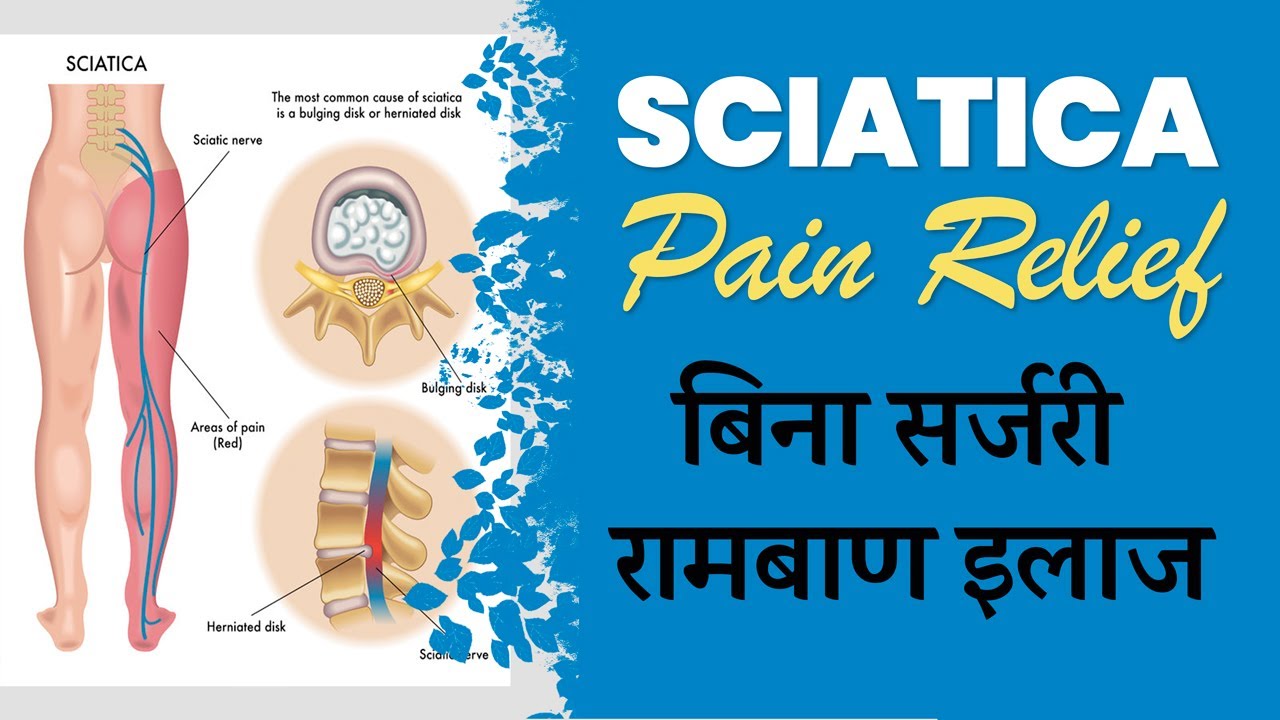
Sciatica
Compression or irritation of the sciatic nerve can cause pain that radiates from the lower back down through the legs. Sciatica symptoms may include:

- Sharp, shooting pain in the leg
- Numbness or tingling in the affected leg
- Weakness in the leg or foot
- Pain that worsens with prolonged sitting
The Importance of Professional Medical Advice for Persistent Leg Pain
While home remedies and lifestyle changes can provide relief for many individuals experiencing nighttime leg pain, persistent or severe symptoms warrant professional medical attention. Why is it crucial to seek expert advice for ongoing leg discomfort?
A healthcare professional can:
- Accurately diagnose the underlying cause of your leg pain
- Rule out potentially serious conditions
- Develop a tailored treatment plan based on your specific needs
- Recommend appropriate lifestyle modifications
- Provide access to advanced treatments when necessary
Remember, while varicose veins are a common cause of nighttime leg pain, other conditions may require different approaches to treatment. By consulting with a board-certified vascular surgeon or other relevant specialist, you can ensure that you’re addressing the root cause of your discomfort and taking the most effective steps toward relief.

When to Seek Immediate Medical Attention
While most cases of nighttime leg pain are not emergencies, certain symptoms may indicate a more serious condition requiring immediate medical care. Seek urgent medical attention if you experience:
- Sudden, severe leg pain accompanied by swelling and warmth (possible sign of deep vein thrombosis)
- Leg pain with chest pain or shortness of breath (potential pulmonary embolism)
- Severe leg pain following an injury
- Leg pain accompanied by fever or signs of infection
- Sudden loss of sensation or ability to move your leg
By staying vigilant and seeking appropriate medical care, you can effectively manage your leg pain and improve your overall quality of life, including the ability to enjoy restful, pain-free sleep.
Sleep Better Without Leg Pain at Night
You don’t want anything to disrupt your sleep — especially not leg pain. Try these tips to eliminate aching legs from varicose veins and sleep soundly all night.
Posted
by The Iowa Clinic on Tuesday, November 20, 2018
There’s nothing like a good night’s sleep. After a long or exhausting day, you can’t wait to hop in bed and get some much-needed rest.
That rest isn’t always easy to come by. Everything seems magnified once you slip under the covers. The normal noises of your house sound louder and are more distracting. Tingles and itches feel more frequent and downright annoying. Thoughts race even though you desperately want them to come to a stop. And pain crops up to keep you from fully relaxing.
Leg pain, in particular, is a common problem at night. Throbbing aches and painful cramps can last for hours as your legs wind down from being up and about all day. That makes it hard to get some shut-eye. Whether you know you have them or not, varicose veins are often the source behind your leg pain and sleepless nights.
What do varicose veins have to do with sleep?
Sitting and standing all day both lead to varicose veins and make the associated leg pain worse. One of the best ways to keep your pain down is to move often. But unless you’re a sleepwalker, that’s not an option in the night.
Your veins are basically blood pumps. Varicose veins are dilated pools of blood under pressure that ache at the end of the day. Elevating at night relieves the pressure of being upright. Legs will ache when getting into bed, but the pain and swelling are usually better by morning. Then the cycle will repeat.
Restless leg syndrome is another common sleep problem. It’s estimated that one in 10 Americans gets unwelcome urges to move their legs at night, as well as other symptoms like tingling, itching, cramping, pain and discomfort. Va–ricose veins don’t cause restless leg syndrome, but they do make the problem worse, which can make it hard to identify the true source of your sleep problems.
How can I stop leg pain at night?
Sleep is restorative, so it’s important that you get enough of it. And that starts with getting rid of disruptions. There’s little you can do to block out the lights and sounds of a Des Moines night, but leg pain is one disruption you can control. There are several things you can do to ease the nightly aches from varicose veins to catch some Zs:
- Elevate your feet. Put a pillow or folded blanket underneath your mattress. Nothing bulky, just enough to raise the foot-end of your bed three or four inches. This helps relieve the pressure on the veins in your legs and lets gravity pick up the slack in getting blood back to your heart.
- Ease into the evening. Many people are active up until the moment they jump in bed. Start winding down earlier in the evening. Put your legs up and relax so that your veins can calm down before you call it a night. A little leg massage can also help the circulation in your legs and prevent pain later on.
- Do some yoga. Exercise is not encouraged too close to bedtime because it will keep you up — even though it’s the best thing for your veins. But gentle stretching and yoga can help you relax and improve blood flow.
- Drink plenty of water. Hydration is key to healthy circulation. But don’t drink it all right before you lie down — that will lead to other sleep disruptions. Just make sure you’re properly hydrated all throughout the day.
Easing the pain may be enough to solve your sleep issues. But if your problems persist, there are many other options that can get to the root of the problem. Varicose veins are often permanent, making the leg pain when you’re sleeping permanent as well. Varicose vein removal ranges from treatments using heat energy to minimally invasive surgery.
Visit with a board-certified vascular surgeon to find the most effective treatment for your varicose veins — and eliminate the reason why your legs hurt at night.
All information offered on The Iowa Clinic website is intended to serve as general educational information only. Any content, product or service is not intended to be a substitute for professional medical advice, diagnosis or treatment. If you believe you have a medical issue, always seek the personalized advice of your physician or qualified healthcare provider.
The Iowa Clinic may provide links to outside sources for additional resources or information and is in no way responsible for the information provided by other organizations or sources. © The Iowa Clinic, 2021
Worried about aching left leg? Scared it could be serious?
Please read through.
I’ve had a sore aching in my left thigh and buttocks mainly, and in my left ankle. It doesn’t stop me walking or moving, but it has the same sensation if you had run or exercised, but I don’t as I am very inactive and only walk my dogs, that is the only exercise I get. It is mostly at night when I lay down to watch tv. It doesn’t keep me awake at night, it flares up and then goes down again. It’s not painful, just an aching, no swelling, no redness, but I have a terrible fear of blood clots and pulmonary embolisms and cancers, as I suffer with horrendous health anxiety.
I had a viral infection, that started at Christmas, and is only now starting to fade away, and I had blood tests that came back as normal. I’m 30 years old, slightly overweight, very inactive lifestyle, hypothyroid (in normal range), and I have PCOS as well (not on any pills for it). my periods are regular since starting my Eltroxin 50mg medication.
I’m a very anxious person, suffer with health anxiety, and depression, so this is starting to freak me out. Of course, I did the worst thing possible – looked on Google, only answers I got were Blood clotting, cancers and tumors. And I have major fears about all 3 of those. So now I’m worse again.
I seen my doctor yesterday about it, and she gave me a physical examination on my leg, and asked me about numbness, pain, bowel problems. Non of which I have, she said it might be it band syndrome, but I looked online and that says about the knee and swelling – both of which I don’t have, and my knee isn’t the problem.
The problem is the aching in my thigh, and my buttocks, sometimes a little up from my buttocks, but around that left side. I’m really frightened at the moment, I can’t sleep and I’m crying, I’m frightened about blood clots, pulmonary embolisms, spinal tumors, ovarian cancer and cancers. I googled and these are some of the things that came up and now my brain is spinning with fear and has debilitated me with panic that its something like these things.
What is it? I’ve had it a few days, is it something serious like those things? I’m so scared!!
Symptoms, Causes, Treatment & Complications
Most calf pain is due to overuse, injury, and age-related wear and tear on the muscles, tendons and ligaments of the calf. There are two calf muscles—gastrocnemius and the soleus—that meet at the Achilles tendon, which is attached to the heel bone. Overstretching (either from overuse or injury) or tearing one of these muscles is a calf strain or tear, respectively. Usually, calf muscle injuries are not serious. You can prevent and treat overuse and minor injuries with self-care and lifestyle changes. For example, proper rest between periods of exertion and conditioning before extreme sports are two practical methods of avoiding trauma and pulled muscles.
However, infectious diseases, blood circulation problems, and other abnormal processes can also affect the calf. In some cases, calf pain may be a symptom of a serious or life-threatening condition. In particular, upper calf pain or pain behind the knee is one sign of a deep vein thrombosis, which is a blood clot deep in the leg that can lead to a pulmonary embolism, heart attack, or stroke. Calf pain can also be a sign of peripheral artery disease, which leads to intermittent pain in the legs, particularly upon mild exertion or walking.
Injury-related causes of calf pain
Calf pain may arise from injuries including:
- Muscle cramp (charley horse) commonly caused by dehydration or overuse
- Pulled or torn muscle (muscle strain) or tendon; you may feel or hear a snap or pop if the muscle or tendon tear is severe
- Pulled or torn ligament (sprain), such as the Achilles tendon
Infection-related causes of calf pain
Calf pain may arise from various infections including:
- Infected wound or other sore
Degenerative, inflammatory, and neurological causes of calf pain
Calf pain can be caused by degenerative, inflammatory, and neurological conditions including:
- Nerve entrapment or compression
- Peripheral neuropathy, such as diabetic neuropathy
Other causes of calf pain
Calf pain can be due to serious, life-threatening conditions including:
- Deep vein thrombosis (blood clot in the leg that can break loose from the leg, causing a pulmonary embolism in the lung, a heart attack, or stroke)
- Peripheral artery disease (PAD, also called peripheral vascular disease, or PVD; a narrowing of arteries due to a buildup of fat and cholesterol on the walls of arteries, which limits blood flow to the extremities). Intermittent claudication is the medical term for calf or leg pain, numbness, or cramping due to PAD.
Questions for diagnosing the cause of calf pain
To diagnose the underlying cause of calf pain, your doctor or licensed healthcare practitioner will ask you several questions related to your symptoms. You can best help your healthcare practitioner in diagnosing the underlying cause of calf pain by providing complete answers to these questions:
- What is the exact location of your pain?
- Describe the pain. When did it start? Did it develop slowly or suddenly? Is it constant or intermittent?
- Are you experiencing any other symptoms?
Provide your full medical history, including all medical conditions, surgeries and treatments, family history, and a complete list of the medications and dietary supplements that you take.
Dull, Aching Thigh Pain | 7 Possible Causes, Treatment & More
Circulatory causes
A blood clot that develops or travels to the femoral vein (also referred to as a deep vein thrombosis (DVT)) can result in dull, achy thigh pain in addition to associated symptoms. Blood clots form when blood components called platelets thicken to form a gel-like mass. The primary function of this process is to plug an injured blood vessel (for example after a cut) in order to stop bleeding. However, sometimes blood clots form inside the arteries and veins without good reason and do not properly dissolve. These can be dangerous and cause serious harm as they can cut off blood flow to the body part the muscle or vein supplies or travel to other parts of the body such as the lungs (pulmonary embolism or PE).
Cancer-related causes
In general, any cancer is the result of cells dividing and growing uncontrollably. Sometimes there is a genetic mutation in DNA or a specific protein or failure in an important checkpoint that results in this unchecked growth. These abnormal cells can accumulate to form a lump that can grow and invade throughout the body. A cancerous process in the thigh can present as a dull, achy pain that interferes with daily activity.
This list does not constitute medical advice and may not accurately represent what you have.
Patellofemoral pain syndrome
Patellofemoral pain syndrome (PFPS) is also called runner’s knee, jumper’s knee, anterior knee pain, chondromalacia patella, and patellofemoral joint syndrome.
Overuse through training for sports is a common cause, especially if there is a misalignment in the knee joint or a previous knee injury. This wears away the cartilage beneath the kneecap and causes pain on exercising.
It is most common in females and in young adults who are active in sports, but can affect anyone.
Symptoms include dull pain at the front of the knee and around the kneecap (patella) while running, squatting, or climbing stairs, or after prolonged sitting with knees bent.
Diagnosis is made through physical examination and through x-rays, CT scan, and/or MRI.
Treatment most often involves rest; over-the-counter pain relievers; low-impact exercise such as swimming or bicycling; physical therapy to strengthen and stabilize the knee; and orthotics (shoe inserts) to help correct a misaligned stride.
Surgery is needed only for severe cases, and is done through arthroscopy to remove any fragments of damaged cartilage.
Rarity: Common
Top Symptoms: knee pain, pain in one knee, knee pain that gets worse when going up stairs, dull, achy knee pain, knee pain that gets worse when squatting
Symptoms that always occur with patellofemoral pain syndrome: knee pain
Urgency: Primary care doctor
Femoral stress fracture
Femoral stress fracture means there is a break in the femur, or thighbone. The femur is the largest and strongest bone in the body and is important for bearing weight. A femoral stress fracture usually occurs in the top of the bone where it connects to the pelvis.
Stress fractures happen from overuse and/or from weakness in the bone from disease, rather than from trauma. Those in heavy physical training, such as athletes and military trainees, are vulnerable to femoral stress fracture. But anyone suffering from malnutrition or osteoporosis is vulnerable to a stress fracture, even with ordinary activities of daily living.
Symptoms include pain deep in the thigh or groin, especially during exercise. The pain may have started gradually instead of being sudden, as with a traumatic injury. The condition might be thought to be a simple strain.
Diagnosis is made through physical examination, with simple tests such as hopping on the painful leg, and imaging.
Treatment involves rest; improved nutrition; study of proper training and striding techniques; and sometimes surgery.
Rarity: Common
Top Symptoms: dull, achy hip pain, pain in one thigh, thigh pain, spontaneous hip pain
Urgency: Primary care doctor
Thigh bruise
A bruise is the damage of the blood vessels that return blood to the heart (the capillaries and veins), which causes pooling of the blood. This explains the blue/purple color of most bruises.
Rarity: Rare
Top Symptoms: pain in one thigh, thigh pain from an injury, upper leg injury, thigh bruise, swelling of one thigh
Symptoms that always occur with thigh bruise: upper leg injury, thigh pain from an injury
Urgency: Self-treatment
Compartment syndrome
Acute compartment syndrome describes the damage done to certain muscle groups of the arms or legs after a traumatic injury.
All of the long muscles are bundled into sections – “compartments” – by the white sheets of strong, tough connective tissue called fascia. If something interferes with circulation so that blood flow is trapped within the compartment, pressure rises because the fascia cannot stretch. This causes serious damage to the muscles and other tissues within the compartment.
Acute compartment syndrome is caused by a broken bone; a crush injury; burns, due to scarred and tightened skin; and bandages or casts applied before an injury has stopped swelling.
Symptoms can rapidly intensify. They include severe pain and tightness in the muscle; tingling or burning sensation; and sometimes numbness and weakness.
Acute compartment syndrome is a medical emergency which can result in loss of the limb. Take the patient to the emergency room or call 9-1-1.
Diagnosis is made through patient history and physical examination.
Treatment involves hospitalization for emergency surgery and, in some cases, skin graft.
Rarity: Rare
Top Symptoms: arm numbness, hand numbness, foot numbness, pain in one leg, thigh numbness
Urgency: Hospital emergency room
Repetitive strain injury of the quadriceps
Repetitive strain injury of the upper leg is caused by consistent repetitive use.
Rarity: Uncommon
Top Symptoms: upper leg numbness, thigh weakness, thigh pain from overuse
Symptoms that always occur with repetitive strain injury of the quadriceps: thigh pain from overuse
Symptoms that never occur with repetitive strain injury of the quadriceps: upper leg injury, severe upper leg pain
Urgency: Self-treatment
Thigh bone infection (osteomyelitis)
Osteomyelitis of the thigh is a bacterial or fungal infection of the thigh bone, typically caused by Staph Aureus (40-50% of the time). It is difficult to diagnose as the infection can come from a break in the skin at the area or anywhere else in the body that spreads by blood.
Rarity: Rare
Top Symptoms: moderate fever, constant upper leg pain, spontaneous thigh pain, painful surgical site, warm red upper leg swelling
Symptoms that always occur with thigh bone infection (osteomyelitis): spontaneous thigh pain, constant upper leg pain
Urgency: Hospital emergency room
Dangerous blood clots form in leg arteries of COVID-19 patients — ScienceDaily
COVID-19 is associated with life-threatening blood clots in the arteries of the legs, according to a study published in Radiology. Researchers said COVID-19 patients with symptoms of inadequate blood supply to the lower extremities tend to have larger clots and a significantly higher rate of amputation and death than uninfected people with the same condition.
COVID-19’s association with blood clots in the pulmonary arteries is well-established. Less is known about the virus’ connection to lower extremity arterial thrombosis, a condition characterized by blood clots in the arteries that impede the flow of oxygenated blood to the lower extremities.
During the peak of the COVID-19 pandemic in New York City, radiologists at the city’s Montefiore Medical Center observed an increase in patients testing positive for lower extremity arterial thrombosis on CT angiography exams. The patients had arrived at hospitals with coldness, pain or discoloration of their legs. Frequently these symptoms of leg ischemia, a condition in which blood flow to the lower extremities is restricted, were accompanied by respiratory distress, cough, fever and altered mental status.
The alarming trend prompted the researchers to look more closely at a possible connection between COVID-19 and lower extremity arterial thrombosis and whether people with the virus had a worse prognosis.
In March and April 2020, they identified 16 COVID-19-positive patients, average age 70, who underwent CT angiography of the lower extremities for symptoms of leg ischemia. These patients were compared with 32 COVID-19-negative patients, average age 71, who underwent CT angiography with similar symptoms in previous years and who were well matched with COVID-19 cohort for demographic and clinical characteristics.
All patients with COVID-19 infection undergoing lower extremity CT angiography had at least one clot in the leg, compared with only 69% of controls. The clots in the COVID-19 patients were significantly larger and affected arteries higher up in the leg with greater frequency than those in controls. Death or limb amputation was more common in the COVID-19 patients.
“We found that arterial thrombosis associated with COVID-19 infection was characterized by dire outcomes, namely strikingly increased rates of amputation and death, which in our series were 25% and 38%, respectively,” said study lead author Inessa A. Goldman, M.D., a radiologist at Montefiore and assistant professor at Albert Einstein College of Medicine in New York City. “For comparison, the rate of both amputation and death was only 3% among controls. It is unclear whether the patients’ concurrent COVID-19-related pneumonia, the virulence of the COVID-19-related clotting disorder or delayed initial arrival to the hospital contributed to these outcomes.”
COVID-19 patients presenting with symptoms of leg ischemia only were more likely to avoid amputation or death than patients who had symptoms of ischemia and systemic symptoms including cough, respiratory distress or failure, hypoxia, fever, or altered mental status.
“In our cohort none of the five patients presenting with complaints pertaining to leg symptoms only, such as pain or discoloration, without systemic symptoms sustained amputation or died,” Dr. Goldman said.
Dr. Goldman noted that with infection rates rising in many parts of the country, it is important that physicians be mindful of the connection between COVID-19 and lower extremity arterial thrombosis.
“Awareness of lower extremity arterial thrombosis as a possible complication of COVID-19 infection is important for all providers who take care of these patients, because early diagnosis is usually crucial for limb preservation in lower extremity ischemia,” she said.
COVID-19’s association with lower extremity arterial thrombosis is likely related to a combination of factors, Dr. Goldman said, including an increased tendency of the blood to clot, damage to the lining of the arteries, and immune reactions tied to the SARS-CoV-2 virus and COVID-19 infection.
“This continues to be an area of intense study around the world,” she said.
Restless Legs Syndrome (RLS) – HelpGuide.org
sleep
Bothered by unpleasant feelings in your legs at night? Learn about the symptoms, self-help, and treatment of restless legs syndrome.
What is restless legs syndrome (RLS)?
Do strange and unpleasant sensations in your legs keep you up at night? Are you bothered by an almost irresistible urge to move your legs when you lie down or relax? If so, you may have restless legs syndrome (RLS), a neurological disorder. The tingling, aching, and itching of RLS can last for hours and prevent you from getting the sleep you need.
Anyone can have restless legs syndrome, but it’s more common in older adults and women. Mild symptoms of RLS may start in early adulthood and then increase with age. After age 50, RLS symptoms often increase in severity and significantly disrupt sleep. Restless legs syndrome is also common during pregnancy (approximately 40% of pregnant women experience it).
Experts believe that low levels of iron in the brain may be responsible for RLS. An imbalance of dopamine is also believed to contribute. About 60% of people with restless legs have a family member with the condition, indicating a strong genetic component. Whatever the cause of your restless legs syndrome, though, it’s important to know that help is available. In recent years, experts have discovered better ways to manage and relieve symptoms—including simple lifestyle changes and self-help remedies you can practice at home to quiet your restless legs and enjoy a peaceful, refreshing sleep.
Restless legs syndrome: Seeking help
Studies estimate that one out of 10 people suffer from restless legs, yet it’s not always easy to find help and support. Many people with RLS never receive proper treatment. Part of the problem is that it’s hard to explain and sufferers are often dismissed as being “nervous.” Those who haven’t experienced the distressing symptoms may not understand how severely they can impact the quality of your life. Even doctors may not take restless legs seriously, recognize the symptoms, or realize that they point to a real medical condition.
The good news is that recent research has increased our understanding of restless legs syndrome, leading to more effective treatments. At the same time, RLS is becoming more widely recognized. If you or your partner suffers from restless legs, there’s never been a better time to find relief.
A night in the life of RLS
If you have restless legs syndrome, a typical night might go like this: You lie down in bed, ready to go to sleep, and just as your body begins to relax, the crawling, tingling, or itching in your legs begin. You try to ignore the uncomfortable sensations, hoping they will go away, but eventually the urge to move is too much. You get out of bed to stretch and pace the floor and, for a moment, you find relief. But when you lie down again, the restless sensations in your legs start all over again.
Signs and symptoms of restless legs syndrome
Not only do the signs and symptoms of restless legs syndrome differ from person to person, but they can be tricky to describe. Common descriptions include: a “creepy-crawly” feeling, tingling, itching, prickling, burning, pulling, tugging, and aching. Some people have said it feels like bugs are crawling up their legs, a fizzy soda is bubbling through their veins, or they have a “deep bone itch.” Sometimes the symptoms are painful, but usually they are simply uncomfortable and disturbing.
Common signs and symptoms of RLS
Leg discomfort combined with strong urge to move. Uncomfortable sensations deep within the legs, accompanied by a strong, often irresistible urge to move them.
Rest triggers the symptoms. The uncomfortable leg sensations start or become worse when you’re sitting, lying down, or trying to relax.
Symptoms get worse at night. RLS typically flares up at night. In more severe cases, the symptoms may begin earlier in the day, but they become much more intense at bedtime.
Symptoms improve when you walk or move your legs. The relief continues as long as you keep moving.
Leg twitching or kicking while sleeping. Many people with RLS also have periodic limb movement disorder (PLMD), which involves repetitive cramping or jerking of the legs during sleep.
The symptoms of RLS can range from mildly annoying to severely disabling. You may experience the symptoms only once in a while, such as times of high stress, or they may plague you every night. In severe cases of RLS, you may experience symptoms in your arms as well as your legs.
RLS self-help tip 1: Avoid triggers
Avoiding known RLS triggers is a smart first step to overcoming the problem.
Manage stress. RLS symptoms get worse when you’re anxious and overwhelmed. Anything you can do to keep stress in check will help, including relaxation techniques such as meditation and deep breathing.
Cut back or eliminate alcohol. Alcohol is known to worsen the symptoms of restless legs, so be cautious about drinking in the evening. Alcohol also disrupts sleep, so you’re more likely to wake up in the middle of the night and be bothered by RLS symptoms.
Don’t over exercise. While moderate daily exercise can significantly ease RLS symptoms, it’s important not to overdo it. Strenuous exercise can sometimes exacerbate the symptoms of RLS, especially close to bedtime, so avoid exercising to the point where your joints or muscles become painful or ache.
Stop smoking. Nicotine is a stimulant that impairs blood flow to muscles and can make restless legs worse, so it’s best to avoid cigarettes, vaporizers, and e-cigarettes.
Experiment with caffeine. For some people with RLS, caffeine is a trigger. However recent research shows that it may actually benefit others. To see which camp you fall into, try cutting out coffee, tea, and soft drinks and monitor your symptoms.
Check your medicine cabinet
There are many common medications—both prescription and over-the-counter—that can trigger the symptoms of RLS or make them worse. Medications to watch out for include:
- Over-the-counter sleeping pills.
- Cold and allergy medications containing antihistamines (such as Benadryl, NyQuil, and Dimetapp).
- Anti-nausea medications (such as Antivert, Compazine, and Dramamine).
- Calcium channel blockers (used for high blood pressure, migraines, and heart problems).
- Antidepressants (such as Prozac, Effexor, and Lexapro).
- Antipsychotics (used for bipolar disorder and schizophrenia).
Get checked for iron and vitamin deficiencies
A number of vitamin and mineral deficiencies are linked to restless legs syndrome.
Iron. Iron deficiency (anemia) is a well-known cause of RLS, so ask your doctor to test you for anemia. However, supplementing with iron can also improve RLS symptoms in those who aren’t anemic.
Magnesium. Magnesium can improve sleep and some studies have shown it to be beneficial for restless legs. Try experimenting with a magnesium supplement (250 to 500 mg) at bedtime to see if your symptoms improve.
Vitamin D. Recent studies show that RLS symptoms are more frequent and more severe in people with vitamin D deficiency. Your doctor can easily test your vitamin D levels or you can simply make it a point to get out more in the sun.
Folate (folic acid). Folate deficiency has been linked to RLS, which may explain why restless legs are so common in pregnant women (folate plays a key role in healthy fetal development). When folic acid is low, B12 is often low as well, so you may want to try supplementing with a B-complex vitamin.
Tip 2: Get daily exercise
Daily activity, including aerobic exercise and lower-body resistance training, can significantly reduce the symptoms of restless legs syndrome in most people. Choose activities you enjoy, especially those that emphasize using the legs. Try to exercise for at least 30 minutes on most days, although not too close to bed time.
The exercise doesn’t need to be intense. Simple daily activities such as walking can often deliver all the benefits you’re looking for. In fact, highly vigorous exercise—like training for a marathon—can sometimes backfire and make RLS symptoms worse.
Stretches for RLS
Simple stretching can help stop the symptoms of restless legs syndrome in their tracks. Here’s a handful to help you get started:
Calf stretch – Stretch out your arms so that your palms are flat against a wall and your elbows are nearly straight. Slightly bend your right knee and step your left leg back a foot or two, positioning its heel and foot flat on the floor. Hold for 20 to 30 seconds. Now bend your left knee while still keeping its heel and foot flat on the floor. For a deeper stretch, move your foot back a bit farther. Switch legs and repeat.
Front thigh stretch – Standing parallel to a wall for balance, grab and pull one of your ankles toward your buttock while keeping the other leg straight. Hold for 20 to 30 seconds. Switch legs and repeat.
Hip stretch – Place the back of a chair against the wall for support and stand facing the chair. Raise your left foot up and rest it flat on the chair, with your knee bent. (Or try placing your foot on a stair while holding the railing for balance.) Keeping your spine as neutral as possible, press your pelvis forward gently until you feel a stretch at the top of your right thigh. Your pelvis will move forward only a little. Hold for 20 to 30 seconds. Switch legs and repeat.
The yoga cure for restless legs
According to research published in the Journal of Alternative and Complementary Medicine, women with RLS who practiced yoga reduced their symptoms and experienced less stress, an elevated mood, and better sleep habits.
Tip 3: Improve your sleep
The symptoms of restless legs syndrome can make it hard to get to sleep. When you’re sleep deprived, you not only feel terrible, but you’re more vulnerable to stress. Stress and fatigue can worsen RLS, making it a vicious cycle, so doing what it takes to get enough sleep is crucial.
Try sleeping with a pillow between your legs. It may prevent nerves in your legs from compressing and result in fewer nighttime RLS symptoms.
Stick to a regular sleep schedule. Support your body’s natural sleep rhythms by going to bed and getting up at the same time every day (including weekends).
Optimize your bedroom for sleep. Make sure the room is dark (no lights from electronic devices), quiet, and cool.
Wind down with a relaxing bedtime routine. Try curling up in bed with a book, listening to calming music, or taking a hot bath (the heat has the added bonus of relieving restless legs).
Power down electronics 1-2 hours before bed. The blue light from screens (TVs, phones, tablets, computers) suppresses sleep-promoting hormones and stimulates your brain.
Keep a sleep diary of RLS symptoms
Logging changes in your diet, lifestyle, sleep habits, and routine might help you make helpful connections between your daily activities and the quality of your sleep at night.
Click here to download HelpGuide’s sleep diary.
Relieving restless legs in the moment
Sometimes, despite your best self-help efforts, the symptoms of restless legs flare up. The following tips will help you find quick relief:
- Get up and walk around. Fighting the urge to move can make the feelings worse.
- Distract yourself with a game or activity.
- Apply hot or cold packs to your legs.
- Try calf stretches, yoga poses, knee bends, or a simple ankle or foot rotation.
- Relax your muscles with massage or a hot bath.
- Pressure can help relieve the discomfort of restless legs syndrome. Try wearing compression socks or stockings or wrap your legs in bandages (but not so tight you’ll cut off circulation).
Avoid extended periods of inactivity
Sitting still for too long can make the symptoms of RLS worse, so try to break up periods of sitting with movement or stretches.
- Find or create a work setting where you can be active. If you work at an office, look into a desk that lets you stand and type, or walk while talking on the phone.
- Tell friends, family, and coworkers why you have to move around more than others. They’ll likely try to accommodate you and want to help you create a healthy environment.
- Schedule activities that may require long periods of sitting—such as car journeys, flights, or waiting for appointments—in the morning rather than late in the day.
- Choose an aisle seat at movies and on planes so that you can get up and move.
- Give yourself stretch breaks at work and during long car rides.
Seeking medical treatment for RLS
If you suffer from restless legs syndrome and self-help strategies simply aren’t cutting it, you may benefit from medical treatment.
Diagnosing restless legs syndrome
No laboratory test can confirm a diagnosis of restless legs syndrome. To diagnose RLS, your doctor will need:
- A complete medical history.
- A diagnostic interview, to rule out other medical conditions.
- A blood test for low iron levels.
- A list of medications and supplements you’re taking.
- A survey to see if anyone else in your family has similar symptoms.
If a medical condition, such as iron deficiency, diabetes, or nerve damage is triggering your restless legs, treating the underlying problem may relieve your symptoms. If not, you may benefit from medication or other treatments.
Health conditions linked to restless legs
- Iron deficiency (anemia).
- Pregnancy.
- Diabetes.
- Kidney disease.
- Rheumatoid arthritis.
- Parkinson’s disease.
- Thyroid problems.
- Neurologic lesions (spinal cord tumors, peripheral nerve lesions, or spinal cord injury).
- Sleep apnea or narcolepsy.
- Varicose veins or trouble with the nerves in the hands or feet.
- Alcoholism.
Non-pharmaceutical treatments
There are a number of non-pharmaceutical treatments that have shown promise for treating restless legs syndrome.
Relaxis vibrating pad. The FDA-approved Relaxis pad is placed under your legs and vibrates at different intensities for 30-minute periods to provide counter-stimulation to the restless legs sensation. While it doesn’t work for everyone, the device does seem to help some RLS sufferers get better sleep without the unpleasant side effects of medication. In the U.S., the device is offered only with a prescription and can be either rented or purchased.
Transcutaneous electric nerve stimulation (TENS). Fifteen to 30 minutes of daily TENS therapy (using low-voltage electrical current) appears to help people who experience a lot of muscle spasms. You can purchase a portable, bedside TENS unit online. They are relatively inexpensive and don’t require a prescription.
Positional release manipulation. A small medical trial in the United Kingdom found that an osteopathic exercise technique known as positional release manipulation (PRM) could benefit people with restless legs syndrome. PRM involves holding different parts of the body in a position that reduces feelings of discomfort and pain.
Alternative therapies such as acupuncture, massage, hypnotherapy, and reflexology may also help relieve RLS symptoms.
Medication
If you have severe RLS symptoms that haven’t improved with lifestyle changes or other treatments, you may benefit from medication. However, no single medication works for everyone with RLS. In fact, a drug that relieves one person’s restless legs may actually make your symptoms worse. In addition, drugs used to treat RLS come with serious side effects, so it’s important to weigh the benefits against the risks.
The following types of medications are most commonly used to treat RLS:
- Parkinson’s medications that affect dopamine.
- Benzodiazepines (a type of anti-anxiety medication).
- Prescription painkillers (opiates).
- Anti-seizure medications.
Many people with restless legs syndrome find that medications that work initially become less effective over time, so experts recommend also pursuing self-help remedies to give yourself the best chance of effectively relieving symptoms over the long term.
Authors: Melinda Smith, M.A., Lawrence Robinson, and Robert Segal, M.A.
Growing Pains (for Parents) – Nemours KidsHealth
Growing pains are leg pains and soreness that happen to children at night. Growing pains usually start when kids are 3–12 years old.
What Are the Signs & Symptoms of Growing Pains?
Most kids with growing pains have pain in their thighs, calves, shins, or behind the knees. The pain usually is in both legs and does not involve the joints. Occasionally, kids may have pain in the arms along with leg pain, but they do not have pain only in the arms. Growing pains often strike in late afternoon or early evening before bed but pain can sometimes wake a sleeping child.
Most kids are pain-free and active as usual during the day. Growing pains may last for months or years, but they don’t happen every day. There might be days, weeks, or months between pain episodes.
What Causes Growing Pains?
Doctors don’t know what causes growing pains. Pain is not worse during growth spurts and the pain is not around the growth areas of bones. So “growing” pains might just be aches from the jumping, climbing, and running that kids do during the day. Often, a child’s growing pains happen after a very active day.
How Are Growing Pains Diagnosed?
There is no medical test for growing pains. Doctors diagnose them based on a child’s symptoms. It’s likely growing pains if a child:
- is healthy and has leg pain at night that gets better with massage, heat, and over-the-counter pain medicine
- is active and has no pain during the day
- has a normal physical exam
If symptoms do not fit this pattern, the doctor may order blood tests and X-rays to look for another cause.
How Are Growing Pains Treated?
To help ease growing pains, your child can:
- Massage the area.
- Stretch.
- Use a heating pad.
- Take an over-the-counter pain reliever like ibuprofen or acetaminophen. Follow the label directions for how much to give and how often.
When Should I Call the Doctor?
Call your doctor if your child has:
- pain that doesn’t get better with massage, heat, and pain medicine
- pain during the day
- swelling, redness, or joint pain
- pain due to an injury
- a fever or other signs of illness, like poor appetite or weight loss
- a limp
Pulsing vein in the leg – causes and treatment
Varicose veins are a chronic disease of the venous system of the legs. Complaints with varicose veins of the lower extremities can be completely different: from fatigue, a feeling of heaviness to severe pain and a feeling that a vein in the leg is throbbing. The slightest discomfort in the lower extremities is a serious reason to consult a doctor for advice.
Why is the vein in the leg pulsating?
Pulsation is a contraction of the heart and vascular walls.In a healthy person, only the arteries and large veins, located in the immediate vicinity of the heart, pulsate. Therefore, if there are sensations of pulsation of veins in the leg area, then this should alert you. The most common causes of this symptom are:
- Various injuries of the lower extremities. For example, with a closed fracture or injury, a vein in the leg may pulsate;
- Varicose veins . With an increase in the diameter of the vessels, the venous wall becomes thinner and blood stagnation is formed, therefore, pulsation can be felt;
- Sciatic nerve injury (sciatica). Most often, with this condition, pain appears along the back of the thigh and under the knee, as well as a feeling that a vein in the leg is pulsating. Neurologists are involved in the treatment of this pathology;
- Vascular thrombosis of the lower extremities. Thrombosis often develops as a complication of varicose veins.
Which doctor should you contact if a vein in your leg is pulsating?
Among the above reasons, varicose veins occupy a special place.According to statistics, in the majority of patients with complaints that a vein in the leg is pulsating, the examination reveals a pathology of the venous system.
In connection with this fact, the first thing we recommend is to contact a phlebologist and angiologist (they specialize in vascular diseases and their treatment). A phlebologist’s appointment consists of 3 mandatory components:
- Poll. It is important for a doctor to know how long the vein in the leg has been pulsating and what other symptoms bother the patient;
- Inspection. Varicose blood vessels are often seen on the skin of the legs and they have an important diagnostic value;
- Instrumental research. Color Doppler is the gold standard in vascular examination. The procedure is safe, painless and takes no more than 15-20 minutes.
The obtained data allow a phlebologist to determine whether varicose veins are the cause of vascular pulsation in the lower extremities.
What treatment is needed if a vein in the leg is pulsating?
In cases where a phlebologist has identified varicose veins, appropriate therapy is prescribed.Treatment of varicose veins in the early stages can be conservative. But usually the pulsation of the vessels appears already at the later stages of development.
In this regard, it is highly likely that surgical treatment will be required. The most effective and modern techniques include Endovenous Laser Vein Coagulation and Radiofrequency Ablation. With their help, without open access, without anesthesia and long-term recovery, it is possible to permanently remove varicose vessels.
How to quickly help if a vein in your leg is pulsating?
Many people, when pulsation and other unpleasant symptoms of the disease appear, seek to quickly stop them.It should be noted that ointments, gels, creams, as well as hirudotherapy (treatment with medical leeches), massage and other local effects can only temporarily relieve symptoms.
In this case, varicose veins are actively progressing and can lead to serious complications (thrombophlebitis, pulmonary embolism, rupture of a vein in the leg, etc.). Therefore, you should not use them to mask the manifestations of pathology and postpone the surgical treatment of varicose veins.
90,000 Appendix 2. First aid kit (automobile).Rules for the provision of first self- and mutual assistance
Appendix N 2
to Order
Ministry of Healthcare of Russia
dated 24.06.96 N 266
FIRST AID KIT
FIRST AID (CAR)
RULES FOR PROVIDING THE FIRST SELF- AND MUTUAL AID
1. Injury
Bruises, fractures, dislocations – pain, swelling, pathological mobility, bone crepitus, pain with axial load, shortening of the limb, protrusion of fragments into the wound with an open fracture.Anesthesia (1.1), immobilization (with splints, improvised means), or fixing the arm to the body, leg to the leg; cold at the site of injury (1.2).
Shock – the same signs, plus pallor, euphoria or confusion, the presence of fractures, bleeding. Give pain reliever (3.2.).
2. Wounds and bleeding
a) Arterial (scarlet blood flows out in a pulsating stream). Apply a tourniquet (2.1) above the wound, leave a note indicating the time of the tourniquet application, apply a bandage to the wound (2.2, 2.3, 2.4). Immobilize the limb, give the patient anesthetic (1.1.).
b) Venous, capillary (dark blood, does not pulsate). Apply a napkin (2.8 or 2.9) and a pressure bandage to the wound with a bandage (2.2, 2.3, 2.4). In case of large blood loss, dilute one salt powder (1.3) per liter of water and give the patient a drink, cold to the injury site (1.2).
c) Apply a sterile bandage (2.2, 2.5) to the wound, give anesthetic (1.1). Treat minor wounds and abrasions with iodine or brilliant green (2.10) and cover with a bactericidal plaster (2.6, 2.7).
3. Burns
In case of extensive burns, apply a sterile bandage (2.2), give anesthetic (1.1). Dilute the salt powder (1.3) per liter of water and give to the patient to drink.
4. Pain in the heart
Validol (3.2) one tablet or nitroglycerin or trinitralong (3.1) one tablet, 15 drops of Corvalol (7.1) in 50 ml of water.
5. Fainting
Put the patient on the floor, raise his legs, let the ammonia smell (5.1) on a fleece.
6. Stress reactions
Dilute 30 drops of Corvalol (7.1) in 50 ml of water and give to the patient to drink.
7. Cardiopulmonary resuscitation
Conducted in the absence of consciousness, breathing and pulse on the carotid artery in the patient (chest compressions and artificial respiration using the device (4.1) until the arrival of the health worker or restoration of breathing and pulse.
8. Poisoning
Rinse the stomach. Dilute 1 tbsp in 100 ml of water.spoon of enterodesis (6.1) and give the patient a drink.
9. Damage to eyes
(Ingress of foreign bodies and substances). Rinse eyes with water, add 3 – 5 drops of sodium sulfacil (1.4).
Deputy Head
Office of the organization
medical assistance to the population
V.M. DONIN
Open the full text of the document
90,000 Scientists have identified the cause of blood clots after vaccination from AstraZeneca – Society
TASS, June 30.Experiments on mice have shown that blood clots after vaccination against coronavirus with drugs from the company AstraZeneca occur only if the drug is injected directly into the blood vessels. Scientists published the results of the study on bioRxiv.
“One of the main reasons for the formation of blood clots after vaccination can be accidental ingestion of the drug in a vein. You can protect against this by injecting the vaccine intramuscularly with preliminary aspiration of fluid,” the researchers write.
The fact that after vaccination with drugs from AstraZeneca and Johnson & Johnson, blood clots may form in patients in the blood vessels, it became known this spring.Because of this, in some countries of the world, AstraZeneca vaccinations were abandoned.
The researchers then began to closely study the side effects of this vaccine. According to the results of a new study, German and Italian doctors led by Leo Nicolai of the University of Munich suggested how such blood clots occur.
Nicolai and his colleagues came up with the idea to conduct this study after a 27-year-old man who had suffered from unexplained headaches for ten days after the AstraZeneca vaccine came to a clinic at the University of Munich for help.A CT scan showed that there was a blood clot in one of the large veins in his brain.
After dissolving the blood clot, the scientists examined the patient in detail and found no evidence that he was formed as a result of an autoimmune reaction provoked by the vaccine. This led scientists to the idea that particles of adenoviruses can interact with platelets on their own and cause them to form blood clots.
Guided by this idea, biologists have traced how the body of several dozen mice reacted to the introduction of the AstraZeneca vaccine into their muscle tissue, as is usually the case with vaccination, as well as when it enters various blood vessels, where particles of adenoviruses can freely interact with blood cells.
Experiments have shown that particles of adenoviruses could indeed bind to platelets. and provoked the spontaneous formation of small blood clots in the veins and other blood vessels of mice. This reaction sharply intensified in those cases when the immune system had time to detect adenoviruses attached to the surface of platelets, and began to produce antibodies to them.
Scientists have obtained similar results in experiments on cultures of human blood cells. At the same time, mRNA vaccines, as well as inactivated particles of adenovirus, did not cause a similar reaction either in the body of mice or in cell culture.All this indicates that the disturbances in the work of platelets were directly associated with the entry of viable particles of adenovirus into the bloodstream.
Therefore, scientists suggest that a significant part of the blood clots that occur after the AstraZeneca vaccine may have appeared due to the accidental ingestion of adenovirus particles into the bloodstream of patients after unsuccessful injections. This can be fought if doctors begin to closely monitor where they inject the drug, summed up Nicolai and his colleagues.
It should be added that the scientists’ article was not reviewed by independent experts or reviewed by the editors of scientific journals, as is usually the case in such cases. Therefore, conclusions from it and similar articles should be treated with caution.
Spinal cord injury
Problem
The term “spinal cord injury” refers to injury to the spinal cord as a result of injury (eg, in a car accident) or disease or degeneration (eg, cancer).Currently, there is no reliable estimate of the prevalence of this phenomenon in the world, but the global incidence rate is estimated at 40-80 cases per million inhabitants per year. Up to 90% of these cases are due to trauma, although the proportion of atraumatic spinal cord injuries appears to be on the increase.
The symptoms of spinal cord injury depend on the severity of the injury and its location on the spinal cord. Symptoms may include partial or complete loss of sensory or motor function of the upper limbs, lower limbs, and / or body.The most serious spinal cord injuries affect the systems that regulate the gastrointestinal tract or bladder, breathing, heart rate, and blood pressure. Most people with spinal cord injuries experience chronic pain.
Demographic trends
Men are most at risk at an early stage of maturity (20-29 years old) and in old age (over 70 years old). Women are at greatest risk during adolescence (15-19 years) and old age (over 60 years).According to research, the ratio of exposure ratios for men and women in adulthood is at least 2: 1, and sometimes much higher.
Death rate
The risk of mortality is highest in the first year after injury and remains high compared to the general population. People with spinal cord injury are 2-5 times more likely to die earlier.
The risk of mortality increases with the level and severity of injury and is largely due to the availability of timely and quality medical care.Factors such as the method of transportation to the hospital after injury and the time taken before admission to hospital are also important.
Secondary preventable conditions (such as infections from untreated pressure ulcers) are no longer considered the leading causes of death in people with spinal cord injury in high-income countries, but these conditions remain the leading causes of death in people with spinal cord injury , in low-income countries.
Health, economic and social consequences
Spinal cord injury is associated with a risk of secondary conditions that can lead to general health problems and even life-threatening conditions, such as deep vein thrombosis, urinary tract infection, muscle spasms, osteoporosis, pressure sores, chronic pain, and airway complications. Prevention and treatment of these conditions requires emergency care, a system of rehabilitation services and ongoing medical care.
Spinal cord injury may result in the person in need of assistance. Orthopedic and rehabilitation techniques are often needed to facilitate mobility, communication, self-care or homework. An estimated 20-30% of people with spinal cord injury show clinically significant symptoms of depression, which in turn has a negative impact on improving vital functions and overall health.
Misperceptions, negative attitudes and physical barriers that inhibit basic mobility functions make many people unable to participate fully in society.Children with spinal cord injury are likely to be less likely than their peers to start school and, after enrollment, less likely to be successful in school. Adults with spinal cord injury face similar barriers that prevent them from participating in economic life, as evidenced by their global unemployment rate of over 60%.
Existing data do not provide a global estimate of the cost of spinal cord injury, but they do provide an opportunity to paint the big picture:
- The level and severity of injury has a significant impact on these costs – the higher the injury to the spinal cord (eg tetraplegia versus paraplegia), the higher the costs;
- direct costs are highest in the first year immediately after spinal cord injury and then decline significantly over time;
- indirect costs, in particular loss of sources of income, often exceed direct costs;
- Most of these costs are borne by the people themselves who have suffered spinal cord injury;
- The costs associated with spinal cord injury are higher than those associated with comparable conditions such as dementia, multiple sclerosis, and cerebral palsy.
Prevention
The leading causes of spinal cord injury are car accidents, falls and acts of violence (including attempted suicide). A significant proportion of traumatic spinal cord injuries are due to work-related or sports-related injuries. Effective measures are now in place to prevent some of the leading causes of spinal cord injury, including improving road conditions, vehicles and road behavior to avoid car accidents, equipping windows with anti-fall protections, and policy measures that have to prevent alcohol abuse and restrict access to firearms in order to reduce the incidence of violence.
Improving health care and solving problems
Many of the consequences associated with spinal cord injury are not due to the individual’s condition, but to inadequate levels of medical care and rehabilitation services, as well as barriers in the physical environment, the social sphere and at the policy level.
Implementation of the UN Convention on the Rights of Persons with Disabilities (CRPD) requires action to address these gaps and challenges.
Key interventions to improve the survival, health and community participation of people with spinal cord injury include the following:
- Timely and proper examination before admission to hospital: prompt recognition of an injury with suspected spinal cord injury, rapid assessment and first aid measures, including immobilization of the spine.
- Emergency care (including surgery) appropriate to the type and severity of injury, degree of instability and presence of nerve compression, and as desired by the patient and family.
- Access to available medical supplies, information materials and medical supplies (eg catheters) to reduce the risk of secondary conditions and improve quality of life.
- Access to qualified rehabilitation and mental health services to maximize functional recovery, autonomy, general well-being and inclusion in society. Maintaining the function of the bladder and gastrointestinal tract is essential.
- Access to appropriate assistive devices that can enable people to carry out daily activities that they would otherwise not be able to do, thereby reducing functional limitations and dependence. In low- and middle-income countries, only 5-15% of people have access to the assistive devices they need.
- Specialized knowledge and skills among healthcare professionals and rehabilitation services.
Necessary measures to ensure the right to education and economic participation include legislation, policies and programs that support the following areas:
- Creation of physically accessible homes, schools, jobs, hospitals and transportation;
- Creation of an education system for all;
- professional skills restoration in order to optimize the chances of finding a job;
- Microfinance and other forms of self-employment incentives to support alternative forms of self-sufficiency;
- Ensuring access to a social security benefit system that does not act as a measure to discourage re-employment;
- Correct understanding of the problem of spinal cord injury and a positive attitude towards people who live in this condition.
90 011 elimination of cases of discrimination at work and in education;
WHO Activities
WHO works across the spectrum, from primary prevention of traumatic and non-traumatic causes of spinal cord injury, improving trauma care, strengthening health and rehabilitation services, and supporting the inclusion of people with spinal cord injury in society. WHO has the following tasks:
- works in a multi-sectoral manner in partnership with national stakeholders across a wide range of sectors (e.g. health, law enforcement, transport, education) to improve prevention of spinal cord injury, including from road accidents, falls, violence and defects of the neural tubes;
- guides and supports Member States in raising awareness of disability issues and promoting the inclusion of disability as a component of national health policies and programs;
- promotes the collection and dissemination of information and data related to disability;
- Develops normative tools, including guidelines and good practice examples, to strengthen primary prevention (car crashes, falls and violence), trauma care, health care, rehabilitation and support, and other care;
- builds relevant capacity among health policymakers and service providers;
- promotes scaling up of local rehabilitation work; and
- promotes strategies to ensure that people with disabilities are well aware of their health conditions and that health care personnel support and protect the rights and dignity of people with disabilities.
Possible causes, diagnostic methods, advice from phlebologists
If a person feels short-term pain in the lower extremities, then it is believed that his veins are pulsating. But the veins themselves cannot pulsate, because only arteries are subject to pulsations. In any case, the painful sensations can cause permanent discomfort. This symptom indicates the need to seek medical help and the appointment of appropriate treatment.
Causes of leg pain
Why are the veins in the legs pulsing? Often injuries can be troubling, and both fresh and long-standing old fractures, muscle overstrain or an inflammatory process violate the integrity of tissues.This means that the problem remains forever. The cause of the pain may be varicose veins, which appear as a result of poor valve function. As a result, venous blood accumulates in the vessels, causing them to stretch. In this case, the veins become clearly visible.
If the veins in the legs are pulsating, and the sensation is accompanied by a feeling of numbness and pain, then this indicates that the problem is in the nerves. The pathology can be caused by diabetes, prolonged smoking or chronic lack of vitamins.Often, the sensations that the patient takes for the pulsation of the veins are actually caused by the pathology of the lumbar spine. Pinched nerves in the pelvis almost always affect the lower extremities.
If a vein in the leg is pulsating, what does it mean? Unpleasant sensations can be triggered by deep vein thrombosis. Blood circulation is impaired when blood vessels are clogged with bad cholesterol. In this case, bed rest is shown. Excess weight or prolonged stress can cause tension in your legs.This will not lead to a threat to life, but it also requires correction.
Sharp muscle contraction
In some cases, if a vein in the leg pulsates strongly, it can be triggered by a contraction of the motor muscles. Veins cannot pulsate, but the patient can take a sharp muscle contraction for this. Most often, such pulsations are concentrated on the face, but can be felt in the lower leg area. Muscle contractions usually go unnoticed. With such a symptom, you should consult a doctor only if muscle weakness is observed.
Varicose veins
Are the veins in your legs pulsing? A common cause is varicose veins. Today the disease is rapidly growing younger. Often, varicose veins are diagnosed by the age of 28-32, and more often the pathology occurs in women. Varicose veins are caused by a sedentary lifestyle, sedentary work, malnutrition and constant stress.
One of the many symptoms that accompanies varicose veins is the pulsation of the veins in the legs. Spider veins appear, heaviness in the legs and pain, veins become visible.These are reasons to appear to a phlebologist. It is better to start treatment at the initial stages, because as the disease progresses, the pain becomes pronounced, the symptoms worsen and can cause many inconveniences.
If your legs hurt, but these are not joints, then in eighty percent of cases, the cause is precisely varicose veins. Patients complain of a feeling of puffiness, swelling and cramps, heaviness in the legs, aching and throbbing pains in the veins, as well as a feeling of warmth on the way of the veins. With treatment, pain sensations decrease.
The phlebologist will recommend wearing compression underwear, regularly playing sports (preferably doing exercises on the legs – a bicycle, birch tree or scissors), using special ointments (the doctor will recommend the names depending on the severity of the disease and accompanying symptoms). Of course, you need to change your lifestyle. At a minimum, nutrition should be normalized.
Diseases of the arteries
Found a pulsating vein in your leg? What to do? Pulsating sensations in the thigh or lower leg area may indicate vascular disease of the lower extremities.To confirm the diagnosis, the doctor will refer the patient to an ultrasound scan. The most common cause of pain in this case is smoking, because it is nicotine that causes narrowing of the lumen of the arteries. During the examination, the doctor will definitely ask the question of how long the patient has been smoking and how many cigarettes a day. Effective treatment should begin with giving up the habit.
Arterial pathologies can lead to all possible sensations of pain. When the tissue lumen narrows, the surrounding arteries begin to experience oxygen starvation.As a result, the leg muscles gradually atrophy, and this can lead to the development of gangrene if there is no medical intervention. Atherosclerosis or thromboangiitis (Buerger’s disease) can lead to increased pulsation at the initial stages of the development of the disease.
Atherosclerosis
In this case, the disease begins with the calves, and then can be localized in several places. The artery is clogged, blood no longer moves through it, so that there is a violation of blood circulation in the limb.Often, the disease accompanies diabetes mellitus.
Thromboangiitis, or Buerger’s disease
Do veins in your legs pulsate? The cause may be thromboangiitis (Buerger’s disease). As a result of the proliferation of the middle layer of blood vessels, the lumen narrows. Then blood clots can form, which impede the movement of blood. The disease occurs mainly at a young age (up to 40 years), more often in men who smoke, and only in twenty percent of cases in women. Today, doctors believe that it is a bad habit that causes such a reaction in the body.
Diagnosis of pathology
What to do if the veins in the legs are pulsating? You need to contact a specialist who will give a referral for ultrasound, ultrasound or triplex ultrasound of the vessels and veins of the legs. These technologies are not invasive. MRI is also often used. With the help of the procedure, it is possible to identify the causes of blood flow disturbances, assess the pathology and select the appropriate therapy, and detect abnormalities.
After accurate diagnosis, adequate treatment will be prescribed. Drug therapy for thromboangiitis, for example, consists in the use of non-steroidal analgesics, angiospasmolytic drugs, training walking, sanatorium treatment and photohemotherapy are additionally prescribed.
