Menopause birth control pills. Menopause and Birth Control Pills: When to Stop and What to Expect
At what age should women stop taking birth control pills. How does menopause affect birth control choices. What are the safest contraceptive options during perimenopause. What happens when you stop taking birth control pills.
Understanding Perimenopause and Menopause
Perimenopause and menopause are significant milestones in a woman’s life, marking the transition from reproductive years to post-reproductive years. But what exactly are these stages, and how do they differ?
What is Perimenopause?
Perimenopause is the transitional phase leading up to menopause. During this time, hormonal changes begin to occur, causing various symptoms and changes in menstrual patterns. Here are some key points about perimenopause:
- It typically begins 4-8 years before menopause
- Most women enter perimenopause in their 40s
- Some women may experience perimenopause in their late 30s
- Periods become irregular but continue during this phase
- Symptoms like hot flashes and mood swings may begin
What is Menopause?
Menopause marks the end of a woman’s reproductive years. It is defined as the point when a woman has not had a menstrual period for 12 consecutive months. Here’s what you need to know about menopause:
- The average age for menopause is 50
- Some women may enter menopause in their late 40s
- It signifies the end of ovulation and menstruation
- Symptoms like hot flashes and night sweats may intensify
- The period after menopause is called post-menopause
Birth Control and Menopause: When to Stop?
As women approach menopause, they often wonder when it’s safe to stop using birth control. This decision isn’t always straightforward and depends on various factors. Here’s what you need to consider:
Can you get pregnant during perimenopause?
Yes, pregnancy is still possible during perimenopause. Although fertility declines with age, women can still ovulate and potentially conceive until they reach menopause. This is why continued use of birth control is recommended during this transition.
How long should you use birth control after your last period?
Healthcare professionals typically recommend using some form of birth control for at least two years after your last menstrual period. This precaution ensures that you’re protected against any unexpected pregnancies during the transition to menopause.

Safe Birth Control Options During Perimenopause
As women enter their mid to late 40s, certain birth control methods become safer than others. Let’s explore the recommended options:
What are the safest birth control methods for perimenopausal women?
- Condoms: A reliable barrier method with no hormonal side effects
- Vasectomy: A permanent option for couples who are certain they don’t want more children
- Intrauterine Device (IUD): Can help manage heavy bleeding associated with perimenopause
- Mini Pill: Contains only progestin, making it a safer option for older women
It’s important to note that high-estrogen contraceptives like the patch, combination pill, or ring are not recommended for women in their mid to late 40s due to increased risk of blood clots and other cardiovascular issues.
When to Stop Taking Birth Control Pills
Birth control pills, particularly combination pills containing estrogen and progestin, carry certain risks for older women. But when exactly should you consider stopping?

At what age should women stop taking combination birth control pills?
Most healthcare providers recommend that women stop taking combination birth control pills in their early 40s. This recommendation is based on the increased risks associated with estrogen as women age, including:
- Higher risk of blood clots
- Increased likelihood of high blood pressure
- Greater chance of developing heart conditions
Other factors that can increase these risks include:
- Being overweight
- Smoking
- Pre-existing medical conditions
- Family history of certain health issues
Should you consult a doctor before stopping birth control pills?
Absolutely. It’s crucial to discuss your birth control options with your primary care doctor or OB-GYN when you turn 40. They can assess your individual risk factors and help determine whether continuing with your current method is safe or if you should consider alternatives.
The Impact of Birth Control Pills on Menopause
Many women wonder about the relationship between birth control pills and menopause. Let’s address some common questions:

Do birth control pills delay menopause?
No, birth control pills do not delay the onset of menopause. Women will reach menopause around age 50, regardless of whether they’re taking birth control pills. However, birth control pills can mask the symptoms of perimenopause and menopause, making it difficult to determine when you’ve entered these phases.
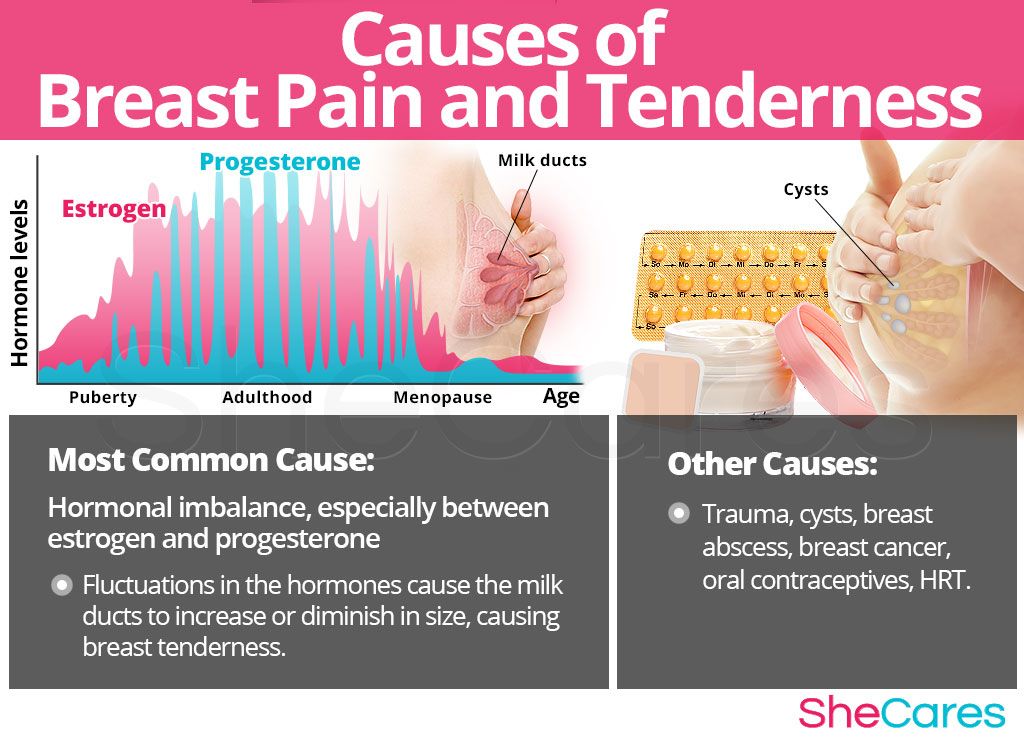
How do birth control pills affect menopause symptoms?
Birth control pills use hormones to create an artificial menstrual cycle. This means that while you’re on the pill, you’ll continue to have regular periods even if you’ve entered perimenopause or menopause. As a result, you may not experience typical menopause symptoms like irregular periods, hot flashes, or night sweats while taking birth control pills.
How can you tell if you’ve entered menopause while on birth control pills?
If you’re in your late 40s and unsure whether you’ve entered perimenopause, consider these options:
- Stop your hormonal birth control for a few months to observe any menopause symptoms
- Ask your doctor for a follicle stimulating hormone (FSH) test to check for menopause
For the FSH test, you’ll need to pause your birth control for about a month before the test.

What to Expect When Stopping Birth Control Pills
Discontinuing birth control pills can lead to various changes in your body. Here’s what you might experience:
How will your menstrual cycle change after stopping birth control pills?
After stopping birth control pills, many women experience:
- Irregular periods
- Return of PMS symptoms
- Heavier menstrual bleeding
The hormones in birth control pills regulate your menstrual cycle, creating a predictable pattern. Without these hormones, your natural cycle may be less regular, especially if you’re entering perimenopause.
Will stopping birth control pills affect your fertility?
Stopping birth control pills doesn’t directly impact your fertility. However, if you’re in your 40s, it’s important to remember that your natural fertility has likely declined due to age. If you’re hoping to conceive after stopping birth control, consult with your healthcare provider for personalized advice.
Managing the Transition from Birth Control to Menopause
Navigating the transition from using birth control to entering menopause can be challenging. Here are some tips to help manage this period:

How can you manage menopause symptoms after stopping birth control?
As you stop taking birth control pills, you may start experiencing menopause symptoms that were previously masked. Here are some strategies to manage these symptoms:
- Practice stress-reduction techniques like meditation or yoga
- Maintain a healthy diet and regular exercise routine
- Consider hormone replacement therapy after consulting with your doctor
- Use over-the-counter lubricants for vaginal dryness
- Try cooling products or breathable fabrics for hot flashes
Should you consider alternative forms of contraception?
If you’re not ready to completely stop using birth control, consider discussing these alternatives with your healthcare provider:
- Progestin-only mini pills
- Hormonal or copper IUDs
- Barrier methods like condoms or diaphragms
- Permanent options like tubal ligation or vasectomy
Remember, the best choice depends on your individual health profile, lifestyle, and preferences.

The Importance of Regular Health Check-ups During Perimenopause
As you navigate the transition from birth control to menopause, regular health check-ups become increasingly important. Here’s why:
Why are health check-ups crucial during perimenopause?
Regular health check-ups during perimenopause serve several important purposes:
- Monitoring hormonal changes and their effects on your body
- Screening for age-related health conditions
- Adjusting your birth control method as needed
- Managing menopause symptoms effectively
- Addressing any concerns or questions you may have
What health screenings should perimenopausal women consider?
As you enter perimenopause, your healthcare provider may recommend various screenings, including:
- Mammograms for breast cancer screening
- Bone density scans to check for osteoporosis
- Pap smears and HPV tests for cervical cancer screening
- Cholesterol and blood pressure checks
- Thyroid function tests
These screenings can help detect potential health issues early, allowing for prompt treatment and better outcomes.
At what age should you stop taking birth control pills?
Menopause is a big milestone in every woman’s life. As it approaches, you may experience unpleasant symptoms like hot flashes, mood swings and trouble sleeping. And when menopause arrives, you’ll stop ovulating and getting your period.
But when is menopause “over”? When is childbearing really off the table?
“When am I safe to quit using birth control pills?”
As a certified menopause practitioner and midwife at Park Nicollet’s Women’s Center, this is a question I get often.
The answer usually isn’t black and white, as menopause symptoms can vary by woman and by age. But here are a few important things to consider when it comes to birth control and menopause.
What’s the difference between perimenopause and menopause?
Perimenopause is menopause’s opening act. It’s the time leading up to menopause when your hormones begin to change. You’ll still have periods during this time, but they become more irregular. Perimenopause usually begins about 4-8 years before menopause. For most women, perimenopause starts in their 40s, but some women experience perimenopause in their late 30s.
Perimenopause usually begins about 4-8 years before menopause. For most women, perimenopause starts in their 40s, but some women experience perimenopause in their late 30s.
Menopause is the final period you have – it’s the curtain closing, so to speak. When you haven’t had a period in 12 months, you’re in menopause. The average age women experience menopause is 50, though some women may go into menopause in their late 40s. Everything after that is post-menopause.
When can I stop using birth control after menopause?
I usually recommend that you use some form of birth control for the first two years after having your last period. But the patch, pill or ring are not recommended as you enter your mid to late 40s. This is due to the high levels of estrogen in these forms of birth control and a risk of blood clots.
The safest options for women are condoms or vasectomy. But I also suggest an intrauterine device (IUD) during menopause, which can help with the associated bleeding problems. The mini pill can be used, too. However, if you’re experiencing symptoms of menopause and being treated with the progesterone-only mini pill, it can affect how well you’re protected from pregnancy.
The mini pill can be used, too. However, if you’re experiencing symptoms of menopause and being treated with the progesterone-only mini pill, it can affect how well you’re protected from pregnancy.
Fertility declines with age. You’re far less likely to get pregnant in your 40s and early 50s, but pregnancy can still happen. That means even if you’ve gone a few months without a period, you can still get pregnant. And while it’s rare, some women can ovulate and have a random period. So if you want to prevent pregnancy, it’s better to be on the safe side when it comes to protection.
At what age should you stop taking birth control pills?
I recommend that most women stop taking birth control pills in their early 40s. Birth control pills, sometimes called combination birth control pills, contain estrogen and progestin. Estrogen increases your risk of developing blood clots, high blood pressure or other heart conditions. Other factors like your weight, pre-existing conditions, medical history and whether you smoke can also increase your risk of complications from birth control pills that contain estrogen.
If you’re on the pill, consider talking to your primary care doctor or OB-GYN when you turn 40 to make sure it’s still a safe option for you. If combination birth control pills aren’t recommended, the mini pill might work best – it only contains the hormone progestin, making it safer for women during perimenopause.
Do birth control pills delay menopause?
No, you’ll reach menopause around age 50 whether you’re taking birth control pills or not. But because birth control pills use hormones to create an artificial cycle, they can mask the symptoms of perimenopause and menopause. You’ll continue to have a period as long as you take birth control pills, making it difficult to know if you’re in menopause.
If you’re in your late 40s and aren’t sure if you’ve entered perimenopause, consider stopping your hormonal birth control for a few months. During this time, you can watch for menopause symptoms like irregular periods, hot flashes, night sweats and mood changes. Or you can ask your doctor for a follicle stimulating hormone (FSH) test to see if you’ve entered menopause. You’ll only need to pause your birth control for a month before getting this test.
Or you can ask your doctor for a follicle stimulating hormone (FSH) test to see if you’ve entered menopause. You’ll only need to pause your birth control for a month before getting this test.
What can you expect when you go off the pill?
Just as you experienced changes when you started taking the pill, you’ll notice some changes after you stop using it. Many women have irregular periods, the return of PMS symptoms and heavier mestrual bleeding after they stop using birth control pills.
The hormones in birth control pills regulate your period. While on the pill, most women will have their period on a regular schedule. Going off the pill can feel like throwing out the calendar. You may notice missed or late periods, and possibly longer-lasting periods. Eventually, your periods will stop altogether.
Birth control pills can also help lessen PMS symptoms like period cramps, bloating, headaches, fatigue and mood swings.
Are there any benefits to taking birth control pills during perimenopause or menopause?
Oral hormonal contraceptives like the pill are often the best birth control option for perimenopause symptoms.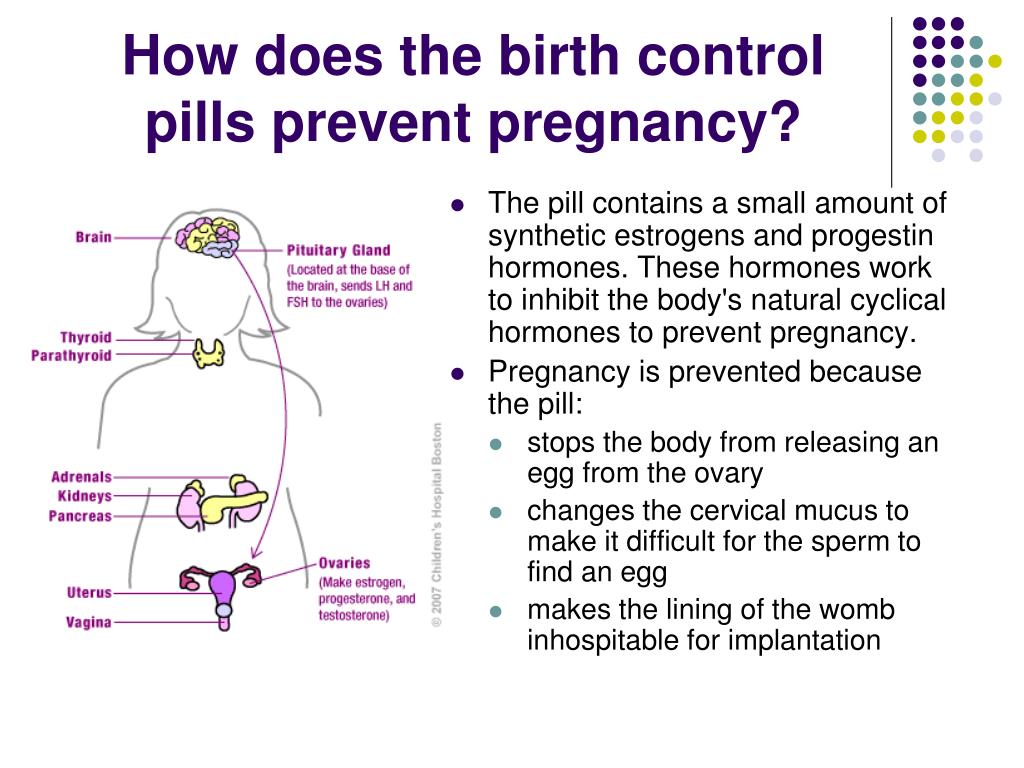
The biggest benefit of taking birth control pills during perimenopause or menopause is that it keeps you from getting pregnant. You have a chance of getting pregnant as long as you’re still getting your period. Birth control pills are 99% effective at preventing pregnancy when taken as directed.
Birth control pills can help regulate periods, reduce bleeding and pain, and help with acne, as well as keep your hormones at consistent levels. So, during perimenopause, this can mean fewer hot flashes. Oral contraceptives can also help maintain bone health and strength, which is important because estrogen deficiency can be linked to postmenopausal osteoporosis.
But I suggest my patients stop taking the pill once they reach menopause. While every woman’s situation is different, there are sometimes risks with staying on the pill. It’s best to talk with your primary care doctor or OB-GYN to help decide what’s best for you.
Are there any risks with taking birth control pills during menopause or perimenopause?
Hormonal contraceptives can sometimes mask symptoms of perimenopause. This can make it difficult to know when you’ve reached perimenopause. And even after menopause, some women can continue to cycle if they stay on hormonal contraceptives.
This can make it difficult to know when you’ve reached perimenopause. And even after menopause, some women can continue to cycle if they stay on hormonal contraceptives.
As mentioned above, I often recommend quitting the pill and similar methods of birth control for women over 40. This is because hormonal contraceptives can increase the risk of blood clots – especially as you age. They also increase your risk of high blood pressure, stroke, heart attack, heart disease and breast cancer. This is especially true of patients who have diabetes, smoke, are overweight or have a history of estrogen-dependent cancers.
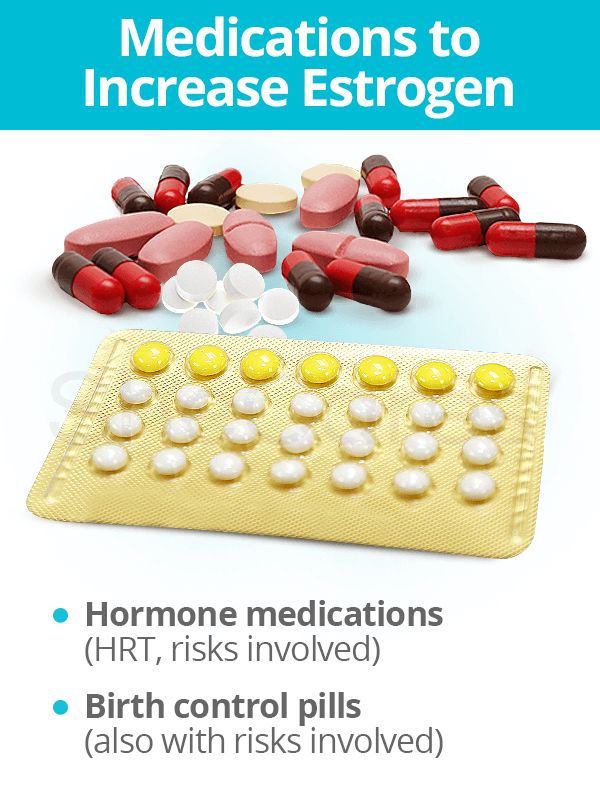
I suggest patients around their late 40s try hormone therapy instead. The lower dose of estrogen decreases risks, but still provides similar benefits as the pill.
Are birth control pills considered hormone therapy?
No, birth control pills aren’t used as hormone therapy (HT). The hormones in birth control pills are used to stop ovulation, so they’re at a much higher dose than the amount of hormones you find in HT.
The goal of HT is to get your postmenopausal hormone levels close to what they were before menopause. Typically, lower doses of hormones are used during HT. And the dose of hormones given during each HT session often varies depending on your individual needs.
When should I start talking to my doctor about birth control and menopause?
Some women choose not to see their doctor when they begin experiencing symptoms. Instead, they wait until their annual wellness visit to talk with their doctor about these changes. This is a common, safe approach to managing menopause symptoms.
However, if you experience symptoms that are concerning like heavy, irregular periods, make sure to talk with your primary care doctor or OB-GYN. Same thing goes if you feel the symptoms are affecting your quality of life. Menopause is a common, and important, phase of life. And your doctor can help determine what the best options are for you.
How to Tell if You’ve Reached Menopause on Birth Control
Written by Alexandra Benisek
Medically Reviewed by Nivin Todd, MD on August 29, 2022
- Birth Control Choices for Women in Perimenopause
- Pros and Cons of Birth Control Around Menopause
- Menopause When You’re on Birth Control
- When to Stop Your Birth Control
When you’re in perimenopause, or the time before your body shifts into menopause, you may be unsure if you still need to use birth control to avoid pregnancy. If you’re worried about pregnancy, you shouldn’t stop birth control until your doctor has told you it’s safe to do so.
If you’re worried about pregnancy, you shouldn’t stop birth control until your doctor has told you it’s safe to do so.
There are many birth control choices to choose from if you’re near menopause. You can use hormonal or nonhormonal options:
- Birth control pills
- Hormonal injection
- Skin patch
- Vaginal ring
- IUDs
- Sterilization for either men or women, which isn’t reversible
- Barrier methods such as condoms, diaphragms, or sponges
The rhythm method, also called natural family planning, is not as effective as other birth control methods if you’re in perimenopause. This is when you track your menstrual pattern to know when you’re most likely to get pregnant. When you’re in perimenopause, you’ll have irregular periods that make it hard to track your menstrual cycle. If you can’t tell when your next period will come, the rhythm method won’t help you avoid pregnancy.
Hormonal birth control can help you in many ways when you’re in perimenopause:
- Helps maintain bone strength
- Treats acne, which may get worse when you’re in menopause
- Lowers your chances of ovarian and uterine cancer
- Lessens hot flashes
- Eases period pain and bleeding
- Makes your periods more regular
Hormonal birth control is usually safe for women in perimenopause.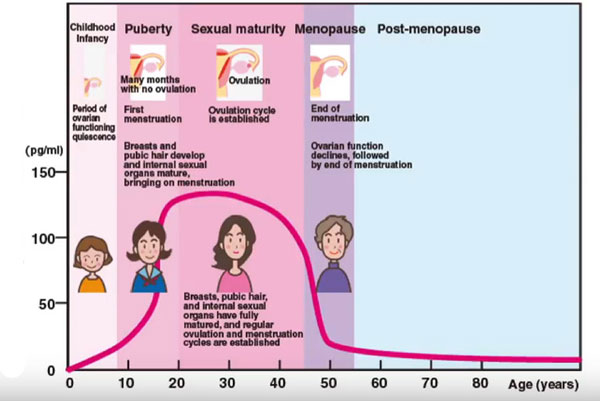 But using birth control after age 35 can raise your risk of blood clots, heart attacks, strokes, and breast cancer. Hormonal methods may not be safe options for you if you smoke or if your doctor has diagnosed you with:
But using birth control after age 35 can raise your risk of blood clots, heart attacks, strokes, and breast cancer. Hormonal methods may not be safe options for you if you smoke or if your doctor has diagnosed you with:
- Cancer
- Heart disease
- High blood pressure
- Diabetes
- Blood clots
There’s no test to tell if you’ve gone through menopause yet or not. The best way to tell is through your period.
You’ve most likely gone through menopause if you’re over 50 years old and haven’t had a period in more than 1 year, or if you’re under 50 years old and haven’t had a period in more than 2 years. But you may not be able to tell if you’ve reached menopause if you’re still on birth control.
Hormonal birth control may hide some of the symptoms of menopause, such as an abnormal period, hot flashes, or night sweats. If you take combination pills (pills that have estrogen and progestin), even after menopause, you may continue to bleed similarly to how you would on your period. This can make it hard to tell if you’ve gone through menopause and whether you’re still able to get pregnant.
This can make it hard to tell if you’ve gone through menopause and whether you’re still able to get pregnant.
In most cases, you should stop the combined pill when you’re at the age of 50. Women in this age group may have other health issues that could make it dangerous to use. Talk to your doctor to see if it’s safe for you to use it if you’re 50 or older.
If you don’t want to be on the combined pill anymore but still want protection against pregnancy, you can use a progestogen-only pill or other forms of birth control, like condoms. If you’re over the age of 55, you can probably stop hormonal methods since your chances of pregnancy are very low. But to be safe, don’t stop any type of birth control until you haven’t had a period for a full year.
Top Picks
Contraceptive pills for menopause – whether to stop taking
11/26/2020
3 min
post author
Dr. Lorraine Maitrot
Lorraine Maitrot
Gynecologist-endocrinologist. Specialist in the treatment of endocrine gynecological diseases, in particular the perimenopausal transition and menopause.
Many women stop taking birth control pills after menopause because they believe that their reproductive function is reduced and the risk of getting pregnant becomes minimal. During the premenopausal period, the menstrual cycle really becomes irregular, however, this does not mean at all that a woman can practice unprotected intercourse, since the ability to bear children does not stop immediately.
Stopping birth control pills should be recommended by your gynecologist based on a physical examination or clinical findings. Self-cancellation of drugs can not only cause unwanted pregnancy, but also hormonal disruptions. That is why women in adulthood need to consult with their doctor, especially at the first stages of manifestation of symptoms characteristic of the menopause period.
Women can still be fertile after menopause.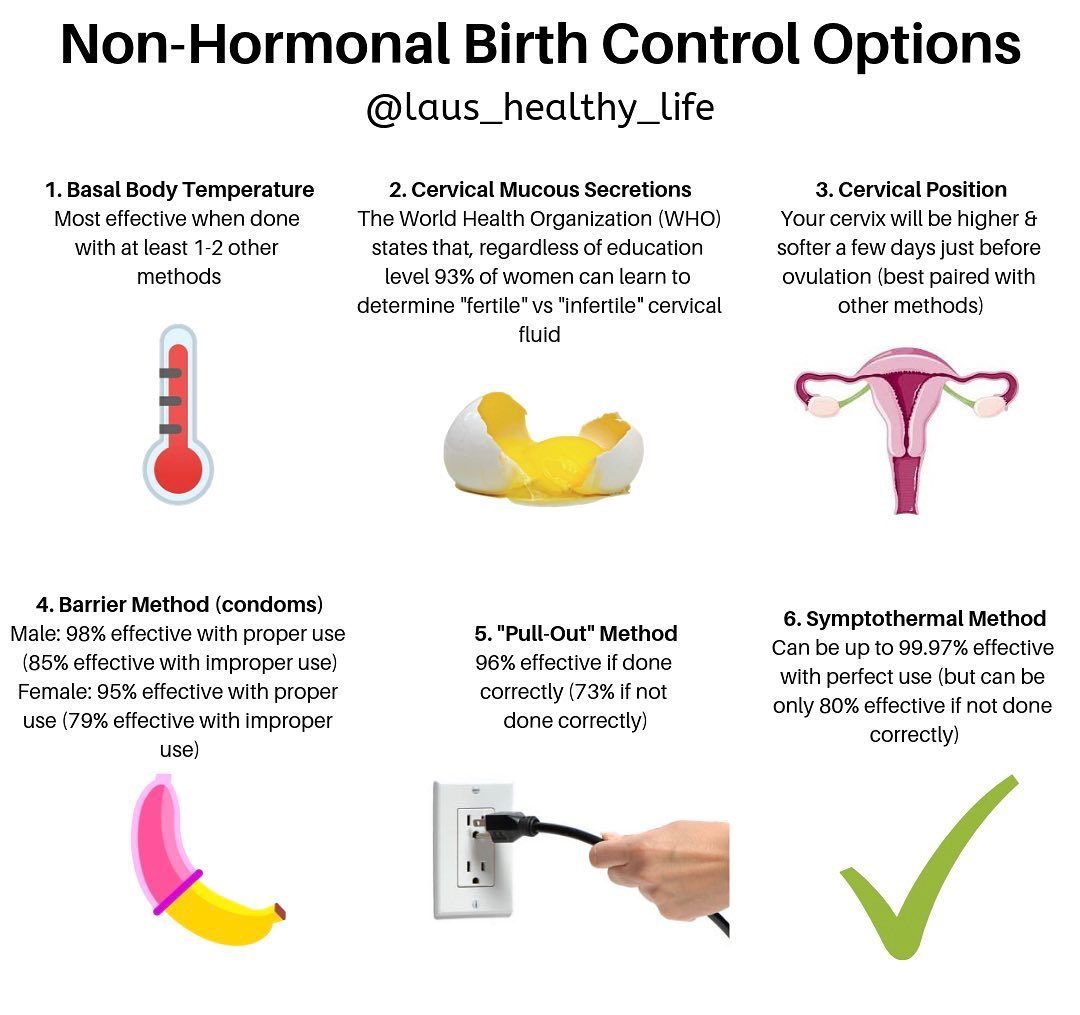
Since fertility does not stop immediately, it is recommended to consult a gynecologist first.
If there is no immediate opportunity to visit a doctor, then it is better to postpone the discontinuation of contraceptives until it appears. Self-cancellation of hormonal drugs is strictly not recommended.
Reasons why you should not stop taking oral contraceptives on your own with the onset of menostasis
Premenopause refers to the transitional period preceding menopause, which can last from several months to several years. This is due to hormonal disorders of the body, which cause irregular menstruation. Therefore, against the background of premenopause, it is not recommended to conduct clinical studies or prescribe hormonal treatment, since the level of hormones in the blood is constantly changing and it becomes impossible to correctly interpret the obtained indicators. This is the main reason why at the stage of premenopause, doctors do not advise giving up effective methods of contraception – as long as the hormonal background of a woman is unstable, she continues to be fertile.
Starting from the age of 35, most women experience a decrease in the function of the reproductive system, which accelerates with the onset of menopause, which subsequently leads to the loss of the ability to bear children. This is affected by the cessation of the production of follicles and female sex hormones by the ovaries, which are responsible for the reproductive function of the female body.
Despite this, according to statistics, the probability of an unexpected pregnancy due to unprotected intercourse in women aged 45+ is about 15%. For this reason, premenopausal women who are sexually active should definitely use contraceptive methods (1).
After the age of 50, the risk of becoming pregnant is significantly reduced, however, without the consent of a gynecologist, it is also not recommended to cancel any method of contraception on your own. If you no longer want to take birth control pills, then do not rule out local contraception.
SOURCES
1. Lambert M, Begon E, Hocke C. La contraception apres 40 ans. RCP Contraception CNGOF 2018.
Lambert M, Begon E, Hocke C. La contraception apres 40 ans. RCP Contraception CNGOF 2018.
Myths about COCs (combined oral contraceptives)
1. COCs can hasten menopause by damaging the ovaries and disrupting the production of pituitary hormones.
Never before has a single synthetic steroid hormone been able to “kill” a single
egg in our body.
Violation of hormone production by the pituitary gland has nothing to do with
menopause, since menopause occurs when the supply of eggs in the
ovaries runs out. Egg laying occurs at
stage of embryonic development, each girl is born with her own
egg reserve, and it is strictly genetically determined.
Operations on the ovaries, when part of it is removed, chemotherapy, smoking
, etc. damage the eggs and can really accelerate the onset of menopause
, but COC has nothing to do with it.
2. COCs cause infertility.
A meta-analysis in 2018, which included scientific data from 1985 to 2017
(22 large studies, tens of thousands of women), showed a total of
Pregnancy rate of 83. 1% during the first 12 months
1% during the first 12 months
after COC withdrawal is the same pregnancy rate
as among women who have never taken COCs.
Meta-analysis is scientific evidence of the highest quality and can be
trusted and relied upon.
Why is the pregnancy rate not 100, but only 83–85? Yes
because there is a certain percentage of married couples on planet Earth
(15-20%) who, for various reasons, cannot have children, but
this has nothing to do with taking COCs. COCs cannot cause infertility.
3. COCs can delay the onset of menopause, the eggs are stored “for later”, ovulation is blocked.
There are many stages of follicle maturation and
it lasts about six months. COCs indirectly block only
the last, hormone-dependent stage, lasting two weeks.
COCs do not store eggs, they still die, regardless of whether
ovulation occurred this month or not.
4. COCs restore an irregular menstrual cycle, “adjust” the hormonal background and ovarian function, they can “tune” them to pregnancy, and after their cancellation, pregnancy will come faster.:max_bytes(150000):strip_icc()/can-birth-control-pills-cause-a-miscarriage-2371726-1-a8bc6e0aa90f4f3484f659b233da3ecf.png)
COCs block ovulation, doing it indirectly, by suppressing
the production of pituitary hormones – LH and FSH, that is, they do not directly affect
ovarian function.
A “false” menstrual cycle is created, which is not accompanied by
ovulation (at 99% of cases). While taking COCs, there will be
regular periods (this is called withdrawal bleeding), but they are
artificially created by hormones.
COCs have never cured the root cause of irregular menstrual cycles
, so after stopping them everything will be the same as before taking them.
Thus, if you want to get pregnant, under no circumstances,
under no circumstances, can you be prescribed
hormonal contraceptives to treat anything or increase your chances
for pregnancy, do not waste time!
5. COCs do not cure anything, and after their withdrawal, everything will be even worse.
COCs do not cure anything, but this does not mean that they cannot be used
for symptomatic treatment.
They have existed for more than 70 years, and their mechanism of action is
well understood. They can be used for acne, endometriosis, PCOS,
abnormal uterine bleeding,
congenital ovarian underdevelopment (hypogonadism) or ovarian prematurity
failure.
They can, but they shouldn’t.
For example, one of the causes of acne is increased genetic
sensitivity of
receptors to the action of male sex hormones, and
a woman with an ideal weight, nutrition, who has not coped with her
problem with a dermatologist, can be helped by reducing the content of free androgen in the blood
. COCs do this by increasing the production of a protein (sex-binding globulin) that binds these
hormones.
This is a temporary effect that lasts only for the duration of the
drug, but this does not mean that it cannot be used.
If you don’t want to take COCs, you don’t have to. No one has yet died from acne or endometriosis, in addition, a number of other drugs can be used
.
6. COCs are addictive, the ovaries “forget” how to work
, after their cancellation it will be more difficult to get pregnant.
This is a myth, see point 2.
7. Hormones contained in COCs accumulate in the body, and then these “deposits” poison it for many more years.
The half-life of the drug is 24-48 hours (depending on the type of
progestin), which is why if a woman misses pills or
cancels them, she can become pregnant even while taking COC
(missing a pill) or in the first cycle after stopping them.
8. COCs cause cancer, disease and have a lot of side effects.
COC use is associated with a risk of cancer in the same way as obesity,
smoking, red meat and alcohol. In general, this is no more than 1-3%, and
some studies do not find such a connection at all. The risk of cancer
is balanced by reducing the risk of ovarian and endometrial cancer
9.
