Period mental symptoms. Premenstrual Syndrome (PMS): Symptoms, Causes, and Treatment Options
What are the common symptoms of PMS. How is PMS diagnosed and treated. What is the difference between PMS and PMDD. Can lifestyle changes help manage PMS symptoms. Are there effective medical treatments for severe PMS.
Understanding Premenstrual Syndrome (PMS)
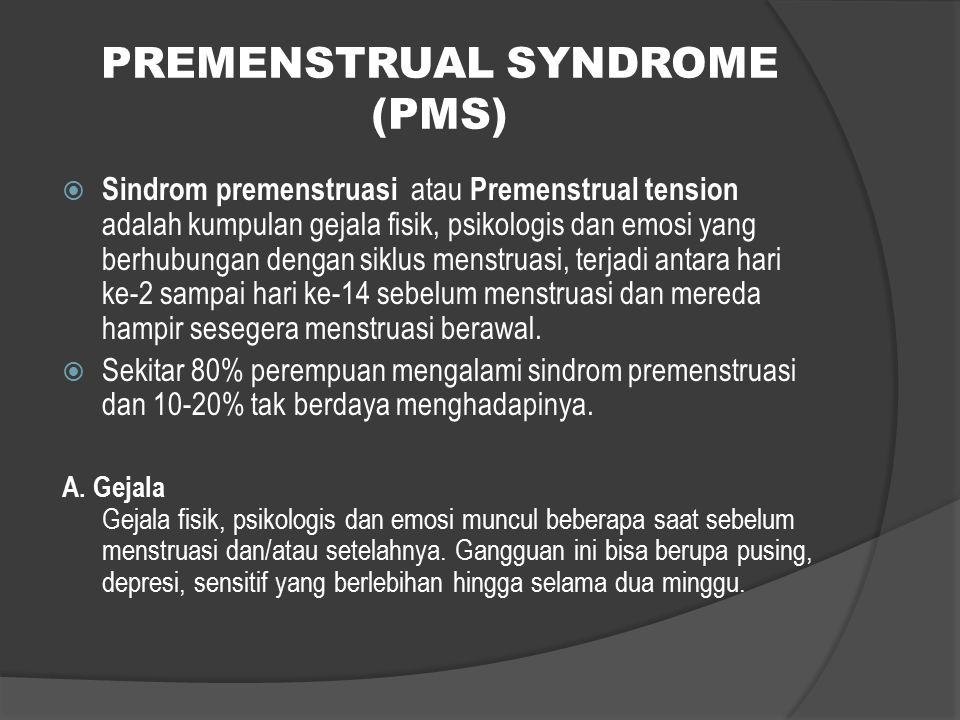
Premenstrual syndrome, commonly known as PMS, is a collection of physical and emotional symptoms that affect many women in the days or weeks leading up to their menstrual period. While the severity and specific symptoms can vary widely between individuals, PMS is a common experience for women of reproductive age.
PMS typically begins 1-2 weeks before menstruation and resolves shortly after the period starts. The cyclical nature of symptoms that correlate with the menstrual cycle is a key feature in diagnosing PMS.
How common is PMS?
PMS is extremely common, with up to 90% of women reporting at least some premenstrual symptoms. However, only about 20-40% of women experience symptoms severe enough to impact their daily lives and meet the clinical criteria for PMS diagnosis.

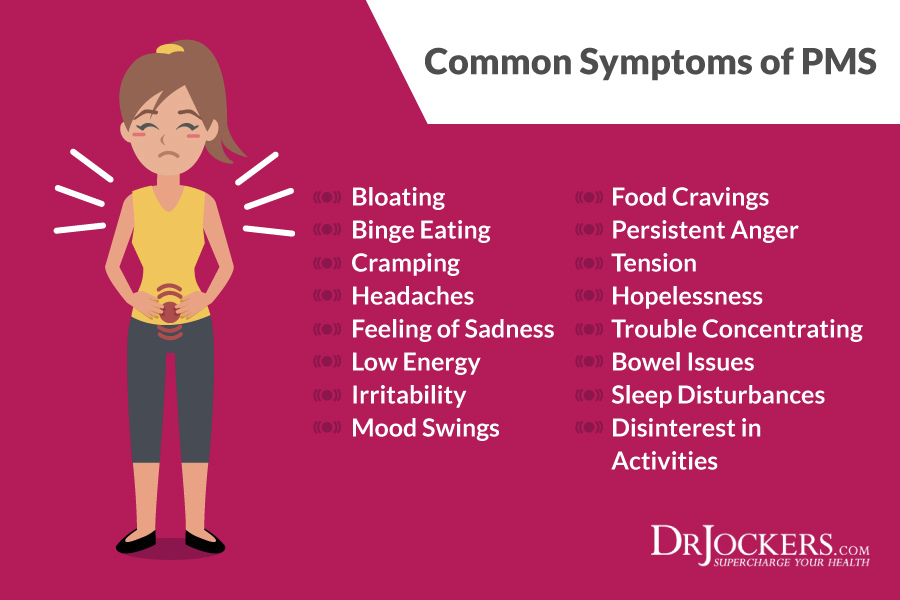
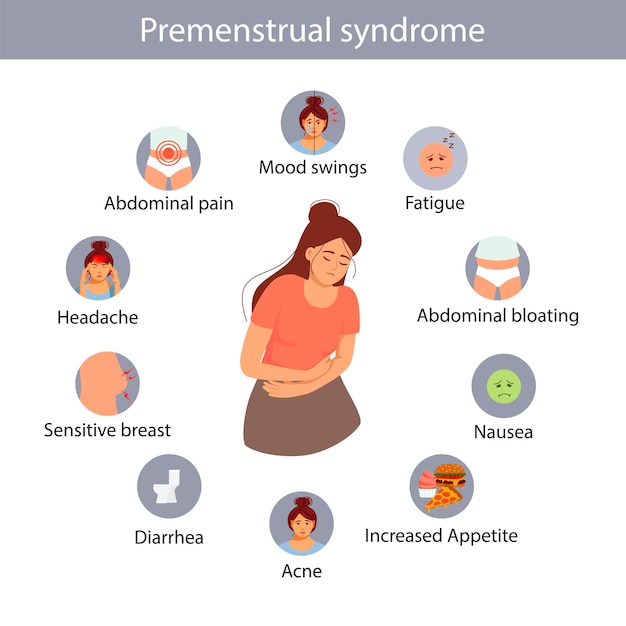
Common Physical Symptoms of PMS
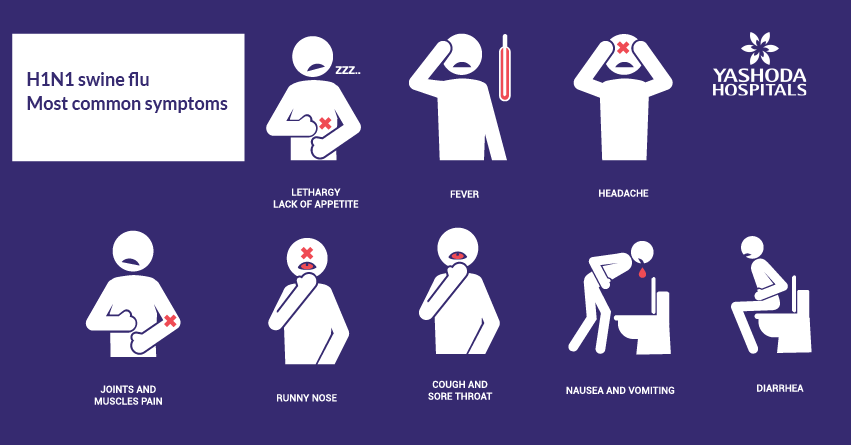
The physical symptoms of PMS can range from mildly uncomfortable to severely disruptive. Some of the most frequently reported physical symptoms include:
- Breast tenderness and swelling
- Bloating and water retention
- Headaches or migraines
- Fatigue and low energy
- Acne flare-ups
- Joint or muscle pain
- Changes in appetite and food cravings
- Gastrointestinal issues like constipation or diarrhea
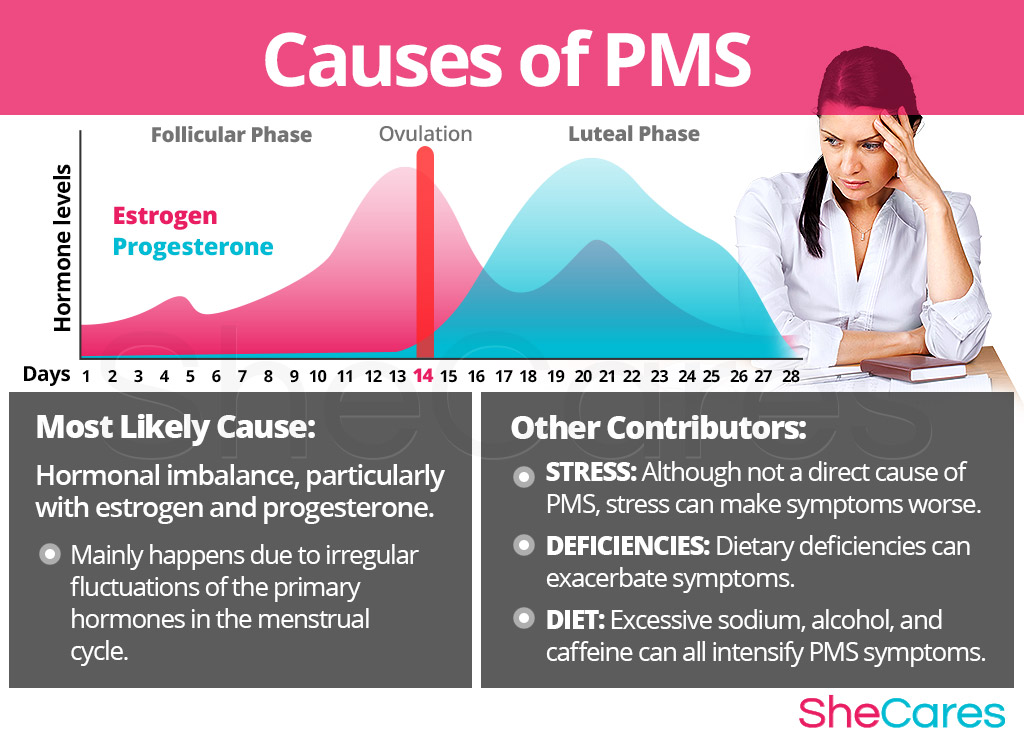
Why do physical symptoms occur during PMS?
The exact mechanisms behind PMS symptoms are not fully understood, but hormonal fluctuations throughout the menstrual cycle play a significant role. The rise and fall of estrogen and progesterone levels can affect various bodily systems, leading to the diverse array of physical symptoms experienced during PMS.
Emotional and Psychological Symptoms of PMS
In addition to physical discomfort, many women experience notable changes in mood and behavior during the premenstrual phase. Common emotional and psychological symptoms include:

- Irritability and mood swings
- Anxiety or tension
- Depression or feelings of sadness
- Difficulty concentrating
- Changes in sleep patterns (insomnia or excessive sleepiness)
- Decreased interest in usual activities
- Feelings of being overwhelmed or out of control
Can PMS affect mental health?
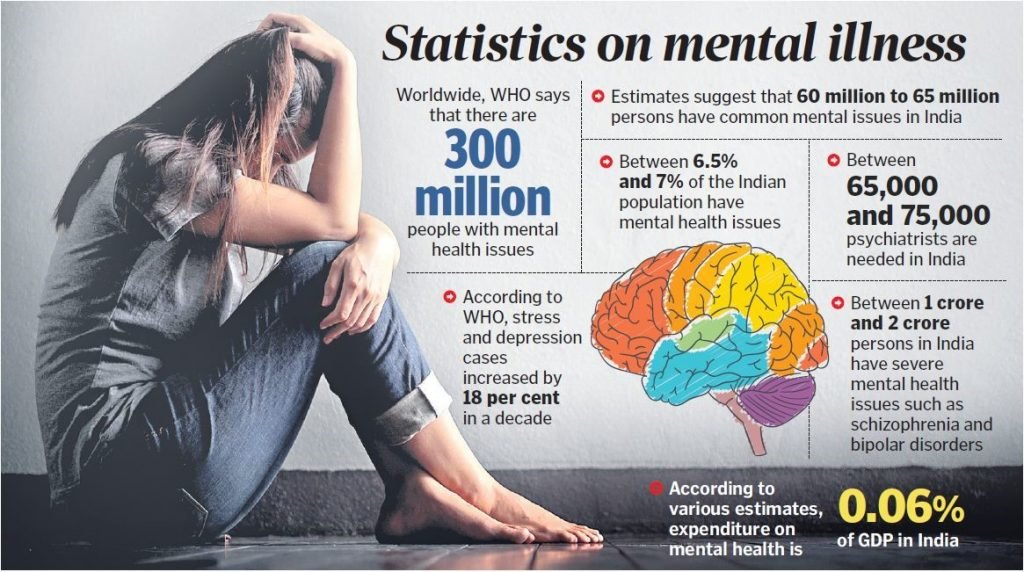
Yes, PMS can have a significant impact on mental health. For some women, the emotional symptoms of PMS can be more distressing than the physical ones. In severe cases, these symptoms may exacerbate existing mental health conditions or contribute to the development of mood disorders.
Premenstrual Dysphoric Disorder (PMDD): A Severe Form of PMS
While PMS is common, a small percentage of women experience a more severe form known as Premenstrual Dysphoric Disorder (PMDD). PMDD is characterized by intense emotional and physical symptoms that significantly interfere with daily life and relationships.
How does PMDD differ from PMS?
PMDD shares many symptoms with PMS but is distinguished by the severity and impact of these symptoms. Women with PMDD often experience:

- Severe mood swings and irritability
- Intense feelings of depression or hopelessness
- Extreme anxiety or tension
- Difficulty functioning in work, school, or social situations
- Physical symptoms that are particularly debilitating
PMDD affects approximately 3-8% of women and is recognized as a distinct disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Diagnosing PMS and PMDD
Diagnosing PMS or PMDD can be challenging, as symptoms often overlap with other conditions. Healthcare providers typically use the following criteria for diagnosis:
- Symptoms occur consistently in the luteal phase of the menstrual cycle (1-2 weeks before menstruation)
- Symptoms resolve within a few days of the onset of menstruation
- Symptoms are present for at least two consecutive menstrual cycles
- Symptoms significantly impact daily functioning or quality of life
What tools are used to diagnose PMS?
To aid in diagnosis, healthcare providers may use:
- Symptom tracking calendars or apps
- Standardized questionnaires
- Physical examinations
- Blood tests to rule out other conditions
Accurate diagnosis often requires tracking symptoms over several menstrual cycles to establish a clear pattern.
Treatment Options for PMS and PMDD
Management of PMS and PMDD typically involves a combination of lifestyle changes, over-the-counter remedies, and in some cases, prescription medications. The approach is often tailored to the individual based on the severity of symptoms and personal preferences.
What lifestyle changes can help manage PMS symptoms?
Many women find relief from PMS symptoms through lifestyle modifications such as:
- Regular exercise
- Stress reduction techniques like meditation or yoga
- Dietary changes, including reducing caffeine and salt intake
- Improving sleep habits
- Limiting alcohol consumption
Are there effective over-the-counter treatments for PMS?
Several over-the-counter options can help alleviate PMS symptoms:
- Pain relievers like ibuprofen or naproxen for cramps and headaches
- Calcium and magnesium supplements
- Vitamin B6 supplements
- Herbal remedies such as chasteberry (Vitex agnus-castus)
It’s important to consult with a healthcare provider before starting any new supplement regimen, as some may interact with medications or have side effects.
What prescription medications are used for severe PMS or PMDD?
For women with severe symptoms or PMDD, prescription medications may be necessary. Common options include:
- Selective serotonin reuptake inhibitors (SSRIs)
- Hormonal birth control pills
- Gonadotropin-releasing hormone (GnRH) agonists
- Diuretics for severe bloating
The choice of medication depends on the individual’s symptoms, medical history, and preferences.
The Role of Hormones in PMS
While the exact cause of PMS is not fully understood, hormonal fluctuations throughout the menstrual cycle play a significant role. The interplay between estrogen, progesterone, and neurotransmitters like serotonin is thought to contribute to both physical and emotional symptoms.
How do hormonal changes affect PMS symptoms?
Hormonal fluctuations can impact various bodily systems:
- Estrogen and progesterone affect fluid retention, leading to bloating and breast tenderness
- Changes in these hormones can influence neurotransmitter function, potentially causing mood swings and irritability
- Fluctuations may alter pain perception, contributing to headaches and muscle aches
Understanding these hormonal influences helps inform treatment strategies and explains why some interventions, like hormonal birth control, can be effective in managing PMS symptoms.
Coping Strategies and Self-Care for PMS
In addition to medical treatments, developing effective coping strategies and prioritizing self-care can significantly improve the management of PMS symptoms. Many women find that a holistic approach to PMS management yields the best results.
What self-care practices can help alleviate PMS symptoms?
Effective self-care strategies for PMS may include:
- Maintaining a regular sleep schedule
- Practicing relaxation techniques such as deep breathing or progressive muscle relaxation
- Engaging in enjoyable activities or hobbies
- Staying socially connected and seeking support from friends and family
- Using heat therapy (such as warm baths or heating pads) for physical discomfort
- Keeping a symptom diary to identify patterns and triggers
Can dietary changes impact PMS symptoms?
Nutrition can play a role in managing PMS symptoms. Some dietary strategies that may help include:
- Eating small, frequent meals to maintain stable blood sugar levels
- Increasing intake of complex carbohydrates
- Reducing consumption of refined sugars and processed foods
- Staying hydrated to help with bloating and water retention
- Limiting caffeine and alcohol, especially in the week before menstruation
While individual responses to dietary changes vary, many women report improvement in symptoms with these modifications.

The Impact of PMS on Daily Life and Relationships
PMS can have far-reaching effects on various aspects of a woman’s life, including work performance, social interactions, and intimate relationships. Understanding and addressing these impacts is crucial for comprehensive PMS management.
How can PMS affect work and productivity?
PMS symptoms can impact work life in several ways:
- Decreased concentration and focus
- Increased absenteeism or presenteeism (being present but less productive)
- Difficulty in interpersonal work relationships due to mood changes
- Physical discomfort affecting job performance
Employers and colleagues who are aware of PMS can create more supportive work environments, potentially reducing its impact on productivity.
What strategies can help manage PMS in relationships?
Open communication and understanding are key in managing the impact of PMS on relationships:
- Educating partners about PMS and its effects
- Planning important discussions or events around the menstrual cycle when possible
- Developing a support system that includes understanding friends and family
- Considering couples therapy if PMS significantly strains the relationship
By addressing PMS openly and collaboratively, many couples find ways to minimize its impact on their relationship.
Research and Future Directions in PMS Management
As our understanding of PMS and PMDD continues to evolve, ongoing research is exploring new treatment options and management strategies. These advancements offer hope for improved quality of life for women affected by severe premenstrual symptoms.
What are some promising areas of PMS research?
Current research in PMS and PMDD is focusing on several areas:
- Genetic factors that may predispose individuals to severe PMS or PMDD
- The role of inflammation in PMS symptoms
- Novel pharmaceutical treatments targeting specific neurotransmitter systems
- The potential of personalized medicine approaches in PMS management
- Exploration of alternative therapies such as acupuncture and mindfulness-based interventions
These research directions may lead to more targeted and effective treatments in the future, potentially improving outcomes for women with PMS and PMDD.
How might future treatments for PMS differ from current approaches?
Future PMS treatments may be more personalized and precise:
- Tailored hormone therapies based on individual hormone profiles
- Targeted interventions for specific symptom clusters
- Integration of wearable technology for real-time symptom tracking and management
- Development of non-hormonal medications with fewer side effects
As research progresses, the hope is that PMS management will become more effective and individualized, leading to better outcomes and improved quality of life for affected women.
Premenstrual Syndrome | PMS | PMS Symptoms
On this page
Basics
- Summary
- Start Here
- Treatments and Therapies
Learn More
- Related Issues
See, Play and Learn
- No links available
Research
- Clinical Trials
- Journal Articles
Resources
- Reference Desk
- Find an Expert
For You
- Teenagers
- Patient Handouts
What is premenstrual syndrome (PMS)?
Premenstrual syndrome, or PMS, is a group of physical and emotional symptoms that start one to two weeks before your period. Most women have at least some symptoms of PMS, and the symptoms go away after their periods start. The symptoms may range from mild to severe.
Most women have at least some symptoms of PMS, and the symptoms go away after their periods start. The symptoms may range from mild to severe.
What is premenstrual dysphoric disorder (PMDD)?
Premenstrual dysphoric disorder (PMDD) is a severe type of PMS. With PMDD, the symptoms are severe enough to interfere with your life. PMDD much less common than PMS.
What causes premenstrual syndrome (PMS)?
Researchers don’t know exactly what causes PMS. Changes in hormone levels during the menstrual cycle may play a role. These changing hormone levels may affect some women more than others.
What are the symptoms of premenstrual syndrome (PMS)?
PMS symptoms are different for everyone. You may get physical symptoms, emotional symptoms, or both. Your symptoms may also change throughout your life.
Physical symptoms may include:
- Breast swelling and tenderness
- Acne
- Bloating and weight gain
- Headache
- Joint pain
- Backache
- Constipation or diarrhea
- Food cravings
Emotional symptoms may include:
- Irritability
- Mood swings
- Crying spells
- Depression
- Anxiety
- Sleeping too much or too little
- Trouble with concentration and memory
- Less interest in sex
How is premenstrual syndrome (PMS) diagnosed?
You may wish to see your health care provider if your symptoms bother you or affect your daily life.
There is no single test for PMS. Your provider will talk with you about your symptoms, including when they happen and how much they affect your life. To be diagnosed with PMS, your symptoms must:
- Happen in the five days before your period for at least three menstrual cycles in a row
- End within four days after your period starts
- Keep you from enjoying or doing some of your normal activities
Your provider may wish to do tests to rule out other conditions which may cause similar symptoms.
What are the treatments for premenstrual syndrome (PMS)?
No single PMS treatment works for everyone. If your symptoms are not severe, you may be able to manage them with:
- Over-the-counter pain relievers such as ibuprofen, aspirin, or naproxen, to help ease cramps, headaches, backaches, and breast tenderness
- Getting regular exercise
- Getting enough sleep
- Eating healthy foods
- Avoiding salt, caffeine, sugar, and alcohol in the two weeks before your period
Some studies have shown that certain vitamins may help with some symptoms of PMS. They include calcium and vitamin B6.
They include calcium and vitamin B6.
Some women take certain herbal supplements for PMS symptoms. But there is not enough evidence to prove that supplements are effective for PMS. Check with your provider before taking any vitamins or supplements.
If you are not able to manage your PMS symptoms, your provider may suggest prescription medicines. These medicines may also be used to treat PMDD. They include:
- Hormonal birth control, which may help with the physical symptoms of PMS. But sometimes they may make the emotional symptoms worse. You may need to try several different types of birth control before you find the right one.
- Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), which may help with emotional symptoms.
- Diuretics (“water pills”) to reduce symptoms of bloating and breast tenderness.
- Anti-anxiety medicine to ease symptoms of anxiety.
Dept. of Health and Human Services Office on Women’s Health
Premenstrual Syndrome (PMS)
(Mayo Foundation for Medical Education and Research)
Premenstrual Syndrome (PMS)
(Department of Health and Human Services, Office on Women’s Health)
Also in Spanish
Premenstrual Syndrome (PMS) FAQ
(American College of Obstetricians and Gynecologists)
Black Cohosh
(National Center for Complementary and Integrative Health)
Chasteberry
(National Center for Complementary and Integrative Health)
Evening Primrose Oil
(National Center for Complementary and Integrative Health)
Mittelschmerz
(Mayo Foundation for Medical Education and Research)
Also in Spanish
Premenstrual Dysphoric Disorder (PMDD)
(American Academy of Family Physicians)
Premenstrual Dysphoric Disorder (PMDD): Different from PMS?
(Mayo Foundation for Medical Education and Research)
Also in Spanish
Water Retention: Relieve This Premenstrual Symptom
(Mayo Foundation for Medical Education and Research)
Also in Spanish
ClinicalTrials.
 gov: Premenstrual Syndrome
gov: Premenstrual Syndrome(National Institutes of Health)
Article: The role of purity and frequency in the classification of perimenstrual.
 ..
..Article: Evaluating the effect of educational intervention based on the health belief…
Article: Premenstrual Syndrome among Medical Students of a Medical College: A Descriptive.
 ..
..Premenstrual Syndrome — see more articles
Normal Female Reproductive Anatomy
(National Cancer Institute)
Department of Health and Human Services, Office on Women’s Health
Also in Spanish
Find an Ob-Gyn
(American College of Obstetricians and Gynecologists)
Menstrual Period: Premenstrual Syndrome (PMS) and Premenstrual Dysphoric Disorder (PMDD)
(Boston Children’s Hospital)
Also in Spanish
PMS, Cramps, and Irregular Periods
(Nemours Foundation)
Also in Spanish
Premenstrual Syndrome (PMS)
(Department of Health and Human Services, Office on Women’s Health)
Is your severe PMS actually premenstrual dysphoric disorder (PMDD)?
Premenstrual discomfort is a feeling many people assigned female at birth know well. Nearly 90% of women in the United States have uncomfortable symptoms before their period — one-third of them report symptoms that qualify as premenstrual syndrome (PMS). But if your PMS symptoms are severe and impact daily life, you may have premenstrual dysphoric disorder (PMDD).
Nearly 90% of women in the United States have uncomfortable symptoms before their period — one-third of them report symptoms that qualify as premenstrual syndrome (PMS). But if your PMS symptoms are severe and impact daily life, you may have premenstrual dysphoric disorder (PMDD).
“When you have PMDD, please know there’s no immediate life-threatening health concern. There’s nothing on your uterus, and nothing has happened to your ovaries other than perhaps an abnormal response to normal hormone changes,” says UCLA Health OBGYN Quy Nguyen, MD. “But it can greatly affect your quality of life, and you don’t have to live with it.”
What is PMDD?
PMDD is a group of physical and behavioral symptoms that show up in a recurring pattern, usually during the second half of your menstrual cycle. Experts aren’t sure what causes PMDD or why only about 5% of women develop it. But many believe it’s related to hormones and neurotransmitters (the brain’s chemical messengers).
“During your menstrual cycle, you experience rising and dropping of both estrogen and progesterone levels. Your body is sensitive to those hormonal changes,” Dr. Nguyen says. “And studies have shown that your menstrual cycle may also influence the neurotransmitters, like serotonin, in your brain.” The impact on neurotransmitters can lead to behavioral symptoms, such as anxiety, depression or trouble controlling your emotions.
Your body is sensitive to those hormonal changes,” Dr. Nguyen says. “And studies have shown that your menstrual cycle may also influence the neurotransmitters, like serotonin, in your brain.” The impact on neurotransmitters can lead to behavioral symptoms, such as anxiety, depression or trouble controlling your emotions.
There are proven risk factors that increase your likelihood of developing PMDD, including:
- Cigarette smoking
- Obesity
- Past traumatic events
- Pre-existing anxiety disorders
PMDD vs. PMS
It’s easy to mistake PMDD for PMS — many physical signs are the same. But PMDD also includes debilitating emotional and mood-related symptoms.
“The main thing that sets PMDD apart from PMS is how severely it can affect your quality of life,” Dr. Nguyen says. “If you’re wondering if you have PMS or PMDD, ask yourself how your symptoms impact your life. Are you missing work, missing school or unable to socialize?” If so, you may be living with PMDD.
PMDD symptoms
People with PMDD have severe symptoms for about six-and-a-half days during each menstrual cycle. That can amount to eight years of disabling symptoms over a lifetime.
The signs of PMDD can include:
- Common physical symptoms of PMS, such as cramps, bloating, breast tenderness and headaches
- Feelings of depression, sadness and despair (including suicidal thoughts)
- Feelings of tension and anxiety, with possible panic attacks
- Joint or muscle pain
- Low energy, exhaustion and no interest in daily activities or relationships
- Mood swings that affect other people and may include irritability, anger, crying or feeling out of control
- Trouble sleeping
“The list of possible PMDD symptoms is long, but it’s helpful to see the range,” Dr. Nguyen says. “It’s never just one symptom that someone mentions. It’s always a wide spectrum of symptoms that appear at the same time each month.”
How to know if you have PMDD
There is no test for PMDD. But the criteria for diagnosis include five or more emotional and physical symptoms — and one must be mood-related. People with PMDD also experience their symptoms in two consecutive menstrual cycles.
But the criteria for diagnosis include five or more emotional and physical symptoms — and one must be mood-related. People with PMDD also experience their symptoms in two consecutive menstrual cycles.
But it’s important to distinguish PMDD from other possible underlying conditions. Dr. Nguyen typically conducts lab work to check for issues like hypothyroidism or hyperthyroidism, which can have similar symptoms to PMDD. But the most crucial factor in diagnosis is a symptom log that notes their severity and when they come and go in relation to menstruation.
“PMDD symptoms completely resolve at the beginning of your period or shortly after,” Dr. Nguyen says. “If you have anxiety or depression or another underlying condition, and not PMDD, the symptoms can sometimes feel better during your period, but they never resolve completely.”
PMDD treatment
Since PMDD symptoms can range from moderate to severe, many treatment options are available.
Non-prescription treatment options include:
- Exercise, which can reduce stress, anxiety and depression symptoms
- Over-the-counter pain relievers (such as ibuprofen and naproxen), which can help relieve physical symptoms
- Relaxation therapy, such as meditation and hypnosis
- Vitamin and mineral supplements, such as vitamin B6 — which helps create serotonin and other neurotransmitters
Prescription medications tend to be more effective at treating PMDD and include:
- Antidepressants called SSRIs (selective serotonin reuptake inhibitors), which alter serotonin levels
- Birth control pills, which relieve typical PMS symptoms and can help you skip menstruation so you don’t undergo the cycling of hormone levels
- Ovarian suppression medications, which stop ovaries from making estrogen and progesterone to put your body into temporary menopause
“Studies show that 60% to 70% of women notice improved PMDD symptoms after taking prescription medication,” Dr. Nguyen says. “You can take an SSRI every day, or you can just take it during the second half of your menstrual cycle and that may be sufficient.”
Nguyen says. “You can take an SSRI every day, or you can just take it during the second half of your menstrual cycle and that may be sufficient.”
But the first step in treating the symptoms of PMDD is talking to your physician. They can guide you in tracking your symptoms and test you for other underlying conditions.
Schizophrenia
Schizophrenia
- Health Issues »
- A
- B
- C
- D
- E
- E
- Y
- W
- W
- I
- R
- L
- M
- H
- O
- P
- R
- S
- T
- U
- F
- X
- C
- H 900 05
- W
- W
- b
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- D
- L
- E
- Y
- W
- W
- Y
- Y
- K
- M
- H
- O
- R
- R
- S
- T
- U
- F
- X
- C
- H
- W
- W
- b
- B
- E
- S
- I
90 004 L
90 004 S
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- Case Studies
- Questions and answers
- Speeches
- Update
- Emergencies ”
- News ”
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments ”
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
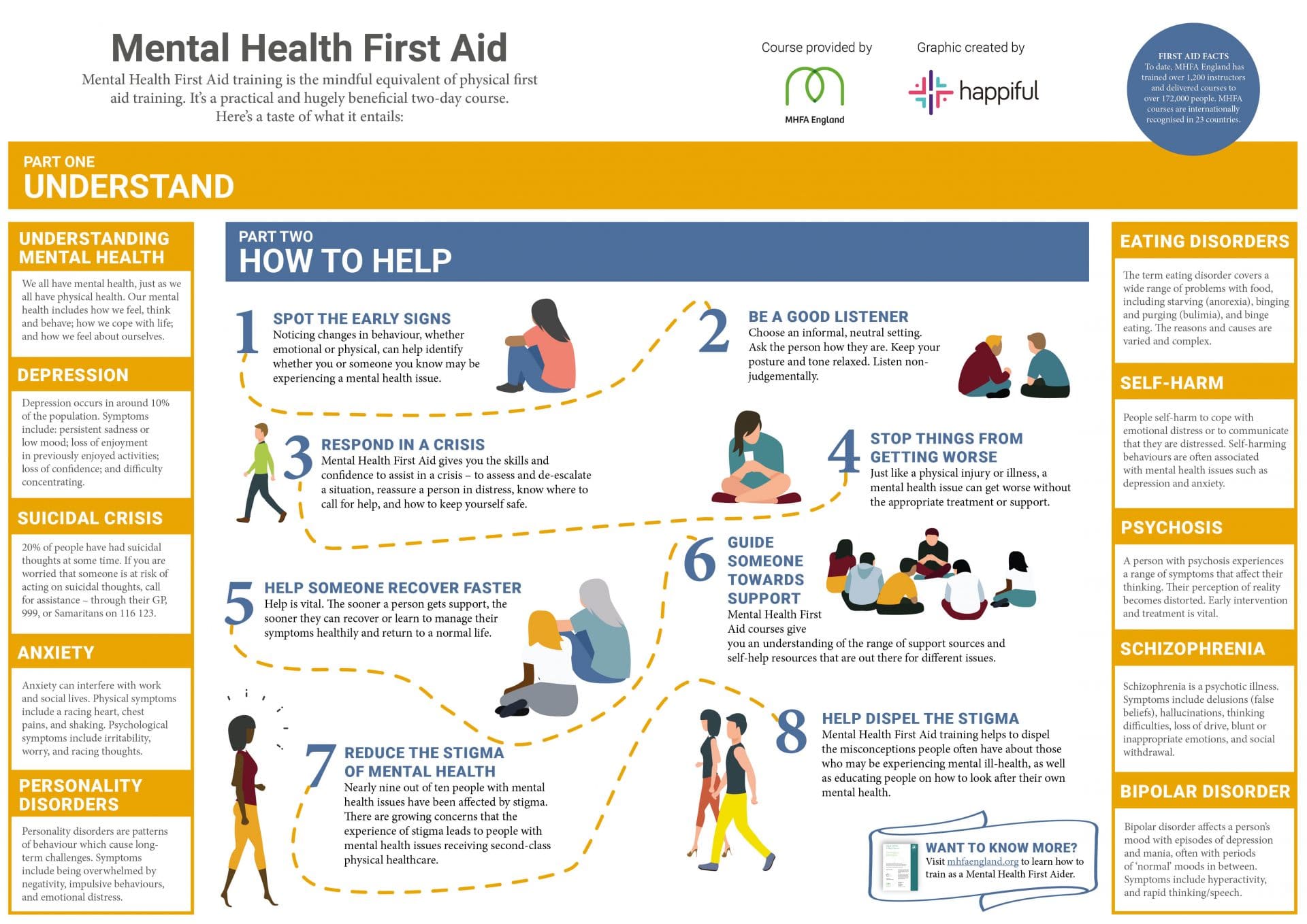
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.

- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Globally, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective options for helping patients with schizophrenia, which can lead to a complete recovery of at least one in three patients.
Symptoms
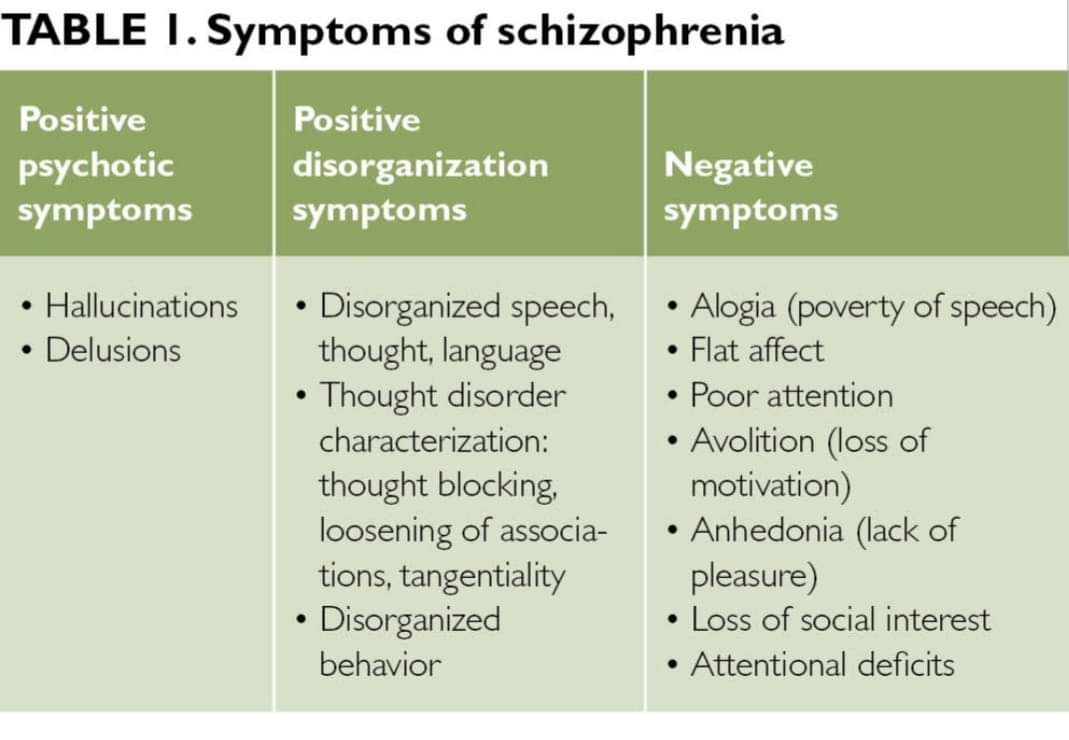
Schizophrenia is characterized by significant disturbances in the perception of reality and behavioral changes, such as:
organization of their behavior;
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia has a lower prevalence than many
other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
People with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social
isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and
supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies
to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia.
In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get
specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the fundamental rights of patients with schizophrenia.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision
a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care.
general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential
the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).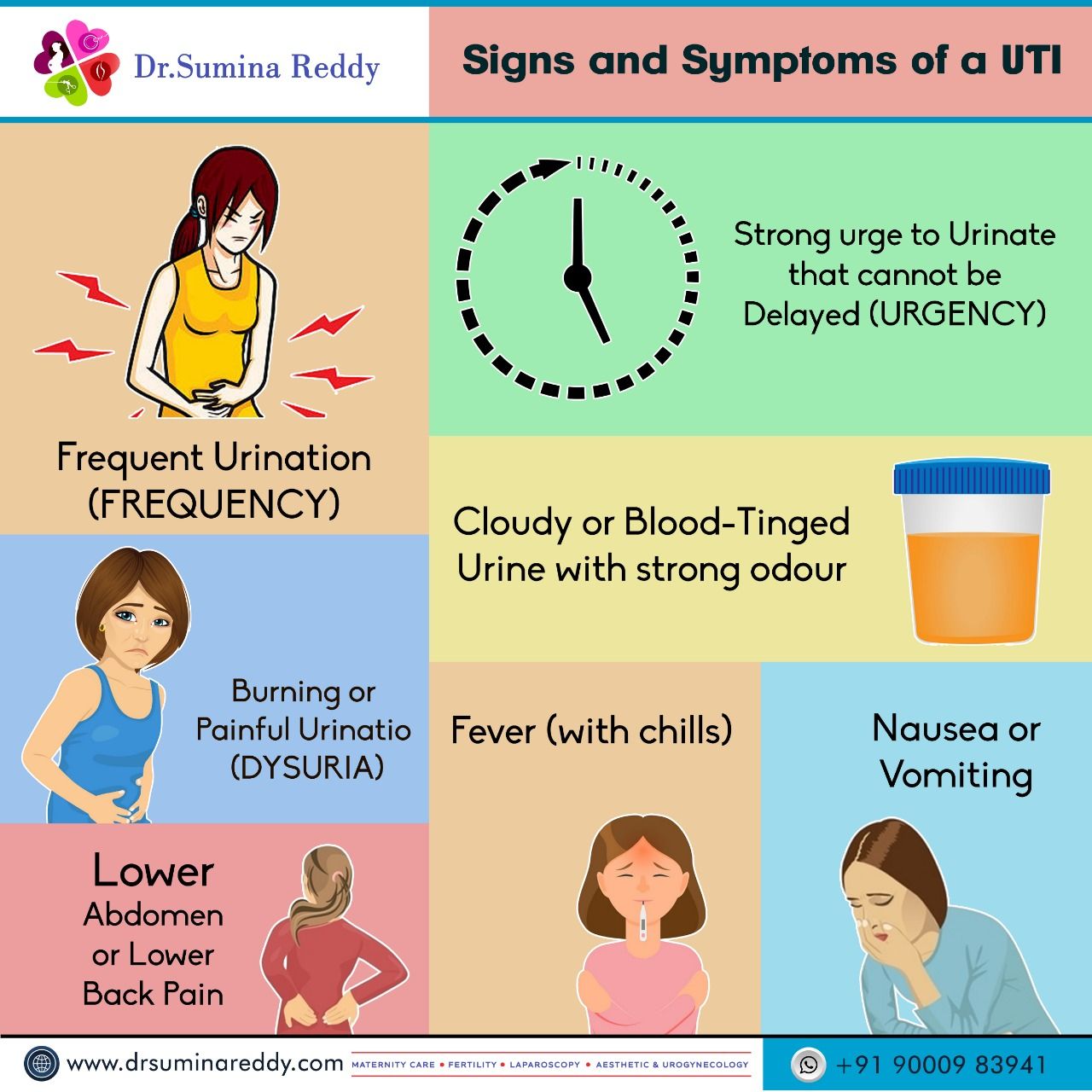
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to
a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations
The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan
mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services
in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in
as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand
opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services.
health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
Acute psychotic disorder: causes, symptoms, signs, stages, consequences, treatment
One of the most common mental illnesses known since the time of Hippocrates is an acute psychotic disorder.:max_bytes(150000):strip_icc()/lamictal-withdrawal-symptoms-380259_v2-8c92ee1d1cf7493199fad1ba24c0da45.png) This is a painful condition in which a perceptual disorder occurs: a person is haunted by false ideas that cannot be corrected, and phenomena (auditory, visual, tactile) that do not exist in reality. These symptoms significantly limit the life of the patient and his loved ones. If left untreated, it can be dangerous to those around you.
This is a painful condition in which a perceptual disorder occurs: a person is haunted by false ideas that cannot be corrected, and phenomena (auditory, visual, tactile) that do not exist in reality. These symptoms significantly limit the life of the patient and his loved ones. If left untreated, it can be dangerous to those around you.
Disease definition
Acute psychotic disorder (acute psychosis) is a mental illness characterized by a disturbance in the perception of the surrounding reality, including a misconception of one’s personality. A person has delusional thoughts and hallucinations. He loses touch with reality, his behavior becomes inadequate.
If left untreated, serious complications may develop, which can significantly limit the life of the patient and his loved ones, and even lead to death.
It is especially important to diagnose acute psychotic disorder on time in adolescents. Some symptoms of the disease can be explained by the peculiarities of adolescence.:max_bytes(150000):strip_icc()/itching-as-a-symptom-of-multiple-sclerosis-2440786-312145dee4c6483ead62da0547d8bea1.png) As a result, if untreated, the symptoms worsen, leading to the development of more severe forms of acute psychosis.
As a result, if untreated, the symptoms worsen, leading to the development of more severe forms of acute psychosis.
The ICD-10 treats acute psychotic disorder under Acute and transient psychotic disorders (F23). At the same time, Acute polymorphic psychotic disorder without symptoms of schizophrenia (F23.0) and with symptoms of schizophrenia (F23.1), as well as other types of psychosis, not otherwise specified.
Symptoms
Acute psychotic disorder is characterized by a diverse clinical picture. In the course of diagnostics during the conversation, the doctor draws attention to such symptoms of acute psychosis , as changes in speech, mood instability, movement disorders.
The patient may be emotionally aroused, which is reflected in fast, jerky, often useless movements. At the same time, he speaks so loudly and quickly that it is difficult to understand his words. Speech is devoid of meaning and logic. In some cases, the opposite picture is observed: the patient is inhibited, ignores the questions addressed to him, refuses to perform simple household activities.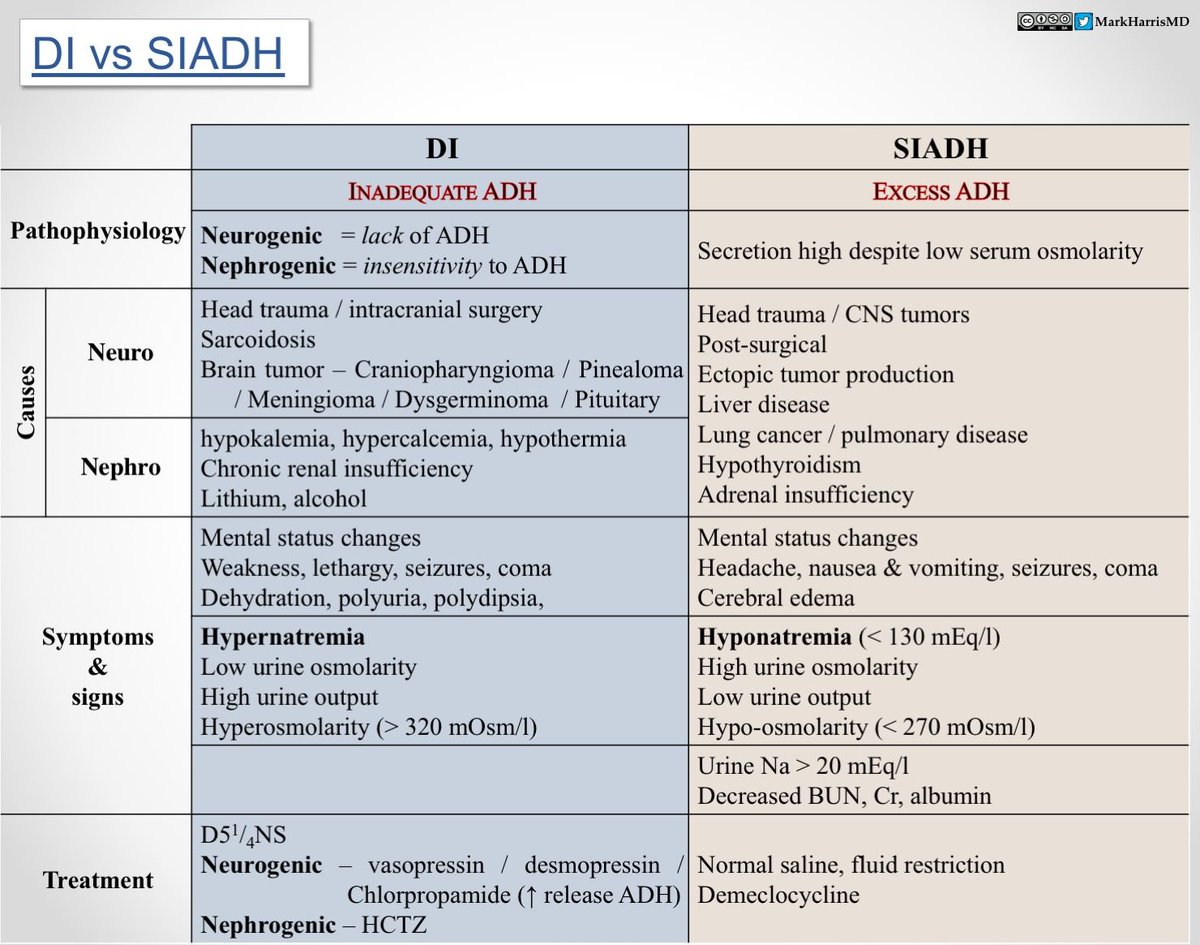
There is polarity in mood. It can be sublime, with delusions of grandeur and grandiose plans, when a person thinks that he is able to achieve any goals. In another case, the patient is in a state of depression: he is tormented by fears, anxiety, anxiety, suicidal thoughts arise.
The characteristic features of a psychotic disorder include the presence of senestopathies, delusions, delusions, and hallucinations.
- Senestopathy.
- Illusions.
- Delusional thoughts and ideas
In acute psychosis, the patient develops symptoms of a somatic nature (insomnia, problems with appetite, weight loss, etc.). They can disturb a person and be the result of diseases of the internal organs, or a disease that exists only in the imagination of the patient, but affect his state of health.
The most vivid somatic sensations are manifested in patients with acute psychotic disorder with symptoms of schizophrenia, as well as in elderly patients, when age-related changes in the functioning of internal organs and cells are triggered./ativan-withdrawal-symptoms-4588394_final-6bb2e0e1202b4092ba7297c475a8509f.png)
The emergence of illusory ideas about the surrounding reality is one of the special signs of acute psychosis. A real-life object is perceived by the patient in a distorted form.
With psychosis, verbal (speech) illusions are triggered. In every phrase of the surrounding people, the patient hears a conspiracy. It seems to him that everyone around him is hostile towards him. During the formation of visual illusions (pareidolia), real objects acquire bizarre forms of expression. For example, in the patterns on the wallpaper, the patient sees crawling insects, and moving cars are perceived as alien robots.
Thoughts and ideas that are false, but are perceived by the patient as true and real, accompany an acute psychotic disorder. Such ridiculous and absurd ideas seem so plausible to the patient that it is impossible to convince him otherwise. At the same time, delusional states can have a subjective evidence base, i. e. a person can even explain the resulting delirium. If there is no evidence and logic, then they simply exist in his perception as a given.
e. a person can even explain the resulting delirium. If there is no evidence and logic, then they simply exist in his perception as a given.
Delusional representations manifest themselves in various variations, the most common of which are:
- thoughts of self-flagellation, when a person accuses himself of something bad;
- ideas of influence, in which it seems to the patient that something or someone influences him. For example, he hangs himself with metal objects to protect himself from the influence of higher forces;
- ideas of persecution, in which a persistent idea is formed that the patient is being followed;
- hypochondriacal thoughts, expressed in a person’s concern about his health;
- paraphrenic ideas associated with megalomania, when the patient overestimates his abilities, considering himself omnipotent, great and rich.
The symptoms of a psychotic disorder include hallucinations, in which the patient perceives objects and phenomena that do not exist in reality.
Auditory (verbal) hallucinations are more common, less often – visual and tactile. Simple auditory hallucinations occur in the form of separate sounds – a cat’s meow, a rustle in the corner, the howling of the wind outside the window, and false forms of hallucinations in the form of a voice of a non-existent person or a dialogue between people.
Complex hallucinations are one of the most dangerous symptoms of acute psychosis, since the voices in the psychotic’s head can push him to commit various actions. The patient, as a rule, does not resist and succumbs to imaginary provocations.
Causes of disease
The causes of psychotic disorder are not fully understood. It is generally accepted that acute psychosis can be the result of such phenomena as:
- Lesions and injuries of the brain, as a result of which its functionality is impaired.

- Mental disorders.
- Oncological diseases that lead to disruption of the structure of the vessels of the brain and blood circulation in general.
- Infectious diseases (AIDS, syphilis, tuberculosis, malaria, etc.).
- Intoxication with chemicals that cause disruption of the brain (mercury, lead, carbon disulfide, etc.).
- Excessive use of psychoactive substances (alcohol, drug, drug addiction), which negatively affect the psyche and cause antisocial behavioral reactions.
The pathogenesis of psychotic disorder is associated with impaired functioning of the dopamine neurotransmitter system of the brain. Hyperfunction of dopamine, a special substance that is involved in the process of transmitting impulses from cell to cell, can provoke a state of psychosis.
The occurrence of acute psychotic disorder may be due to a decrease in the functions of NMDA receptors.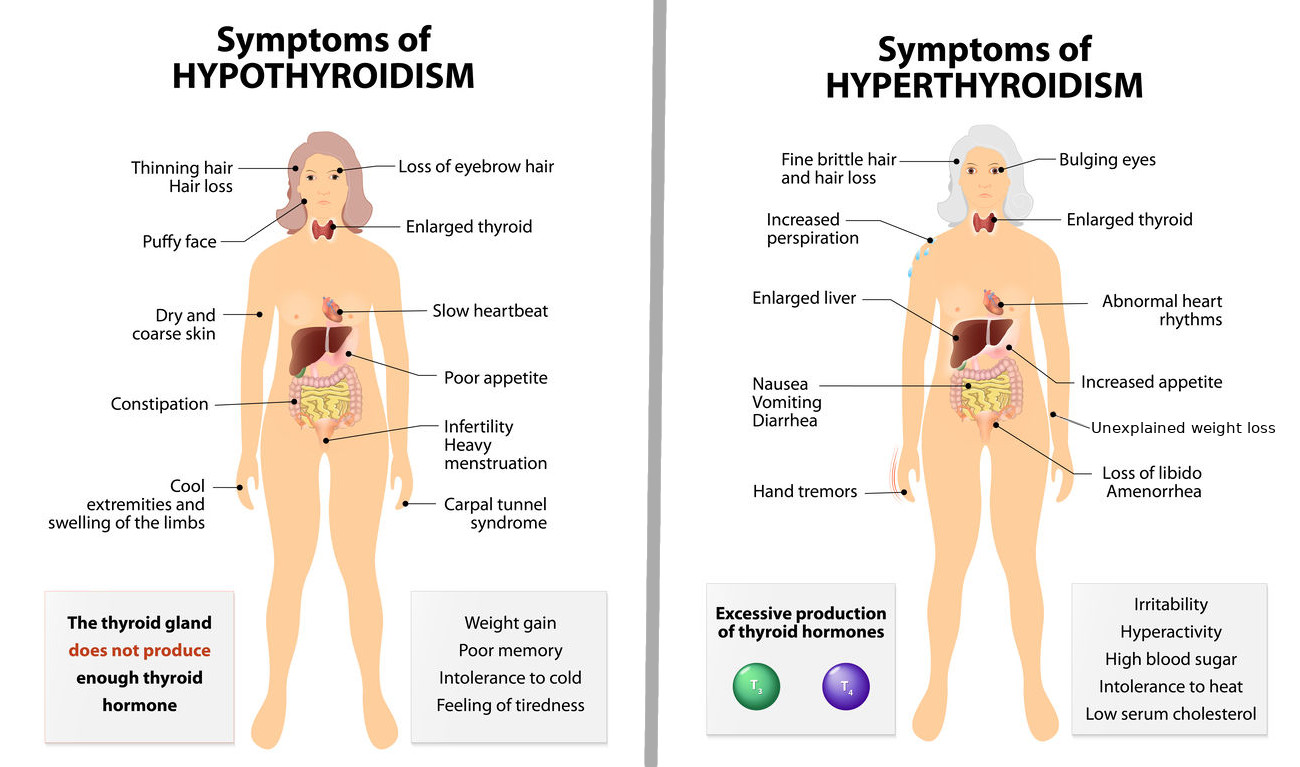 These are nerve cells that respond to glutamic acid molecules, which is one of the most important carriers of excitatory signals.
These are nerve cells that respond to glutamic acid molecules, which is one of the most important carriers of excitatory signals.
Stages and classification
If we consider the stages of a psychotic disorder, then the disease is characterized by an acute onset with a vivid clinical picture. It is rapidly unfolding, and within 10-14 days there is an anomalous perception of reality. Gradually, the symptoms of a psychotic episode fade away. Complete relief of symptoms occurs after a few weeks or months. It is possible to pass these stages in a few days.
In the ICD-10, acute psychotic disorder has a separate section “Acute and transient psychotic disorders (F23). The following types of psychotic disorder are distinguished as subsections:
- F23.0 Acute polymorphic psychotic disorder without symptoms of schizophrenia (acute delirium without symptoms of schizophrenia or unspecified, cycloid psychosis without symptoms of schizophrenia or unspecified).

- F23.1 Acute polymorphic psychotic disorder with symptoms of schizophrenia (acute delusions with symptoms of schizophrenia, cycloid psychosis with symptoms of schizophrenia).
- F23.2 Acute schizophreniform psychotic disorder (acute (undifferentiated) schizophrenia, brief schizophreniform psychosis/disorder, oneirophrenia, schizophrenic reaction).
- F23.3 Other acute, predominantly delusional psychotic disorders (paranoid reaction, psychogenic paranoid psychosis).
- F23.8 Other acute and transient psychotic disorders
- F23.9 Acute and transient psychotic disorder, unspecified
There are specific symptoms acute psychosis (hallucinations, delusions, perceptual disturbances), but they are unstable and quickly pass without recurring in the future.
Symptoms of schizophrenia join the unstable symptoms of acute psychosis.
The clinical picture characteristic of schizophrenia appears, but with a limited duration of up to one month.
Relatively stable hallucinations or delusions are present, but there are not enough symptoms to make a diagnosis of Schizophrenia.
This subsection deals with mental disorders that cannot be classified under other subsections.
(brief reactive psychosis NOS, reactive psychosis).
The subsection combines psychotic disorders that do not have additional clarifications on the clinical picture.
Reactive psychosis, classified in this subsection, has several forms:
- postpartum psychosis, which develops in a woman after the birth of a child;
- psychogenic psychosis that occurs as a response to stress.
By origin, the following forms of psychosis are distinguished:
- Exogenous form of psychosis. It arises under the influence of external factors – traumatic situations (loss of a loved one, identification of dangerous diseases, legal discrimination, etc.).
- Endogenous form of psychosis.
 It is provoked by other diseases, most often of a mental orientation, for example, schizophrenia, bipolar disorder, dementia.
It is provoked by other diseases, most often of a mental orientation, for example, schizophrenia, bipolar disorder, dementia.
When prescribing a course of treatment, the cause that caused the disorder is important. Therefore, in psychiatry, the following types of psychotic disorder are distinguished:
- Primary, in which acute psychosis is considered as a mental disorder in the absence of other previous mental disorders.
- Secondary, if psychosis is provoked by the presence of other pathological processes (intoxication, infection, oncological pathologies).
Antipsychotics are used in the treatment of primary psychosis. In secondary psychosis, it is necessary to stop the symptoms of the disease that caused the psychotic disorder.
Complications of the disease
If left untreated, serious complications of a psychotic disorder can occur. The patient’s symptoms worsen, which leads to social maladaptation and loss of social status. There are problems in the professional sphere up to the loss of a job. Conflicts and misunderstandings appear in family life, social contacts are lost. The patient consciously withdraws from communication, seeks solitude.
There are problems in the professional sphere up to the loss of a job. Conflicts and misunderstandings appear in family life, social contacts are lost. The patient consciously withdraws from communication, seeks solitude.
Inadequate behavior and lack of moral principles lead to problems with the law, which often end in forced placement in a psychiatric hospital.
The person does not realize the severity of the consequences of a psychotic disorder. It can develop into schizophrenia or schizotypal disorder, which require lifelong observation and medical support.
Acute psychosis is characterized by increased conflict, uncontrolled actions, lack of adequacy, excessive emotionality, which significantly increases the risk of developing pathological addictions: alcohol, drugs, drugs.
Being in a state of psychosis, the patient can harm himself and others. A high risk of self-harm and suicide, the development of severe depression, loss of adequacy and connection with reality is what leads to delayed diagnosis, lack of or delayed treatment.
At the first signs of a psychotic disorder, you should consult a doctor. If a person has ridiculous thoughts that are not related to reality, he sets himself unattainable goals, while he sincerely believes in their achievement, complains about the voices that talk to him and send secret signs, then this is a reason to immediately contact a specialized clinic. At risk are those people in whose family there have already been cases of mental disorders.
Diagnosis
In the diagnosis of acute psychotic disorder, laboratory and instrumental research methods are used.
If acute psychosis is suspected, the specialist conducts a conversation with the patient, paying attention to his behavior. Usually clinical signs of mental experiences become noticeable during the first communication. The patient expresses himself incomprehensibly, there is no logic or meaning in his speech. He inappropriately answers questions, sometimes completely ignoring them. There are indirect indicators of the presence of delusional thoughts and / or hallucinations. For example, some oddities are observed in the appearance or behavior of the patient: he can constantly wear dark glasses, thinking that he is being watched and want to harm him, talking to himself or with an imaginary interlocutor, etc.
There are indirect indicators of the presence of delusional thoughts and / or hallucinations. For example, some oddities are observed in the appearance or behavior of the patient: he can constantly wear dark glasses, thinking that he is being watched and want to harm him, talking to himself or with an imaginary interlocutor, etc.
Differential diagnosis is important. Acute psychotic disorder must be distinguished from other mental disorders. In addition, it is necessary to exclude the presence of oncological processes, vascular diseases, withdrawal symptoms caused by exposure to psychoactive substances. For this purpose, CT and MRI of the brain, a biochemical blood test, and a urine test are performed.
An accurate diagnosis can be made by a specialist clinic doctor who has experience working with patients with mental illness.
Treatment
Treatment of acute psychotic disorder is carried out under the supervision of a doctor in a specialized clinic. To minimize the dangerous consequences of acute psychosis, an integrated approach to treatment is used. It includes medication and psychotherapy.
To minimize the dangerous consequences of acute psychosis, an integrated approach to treatment is used. It includes medication and psychotherapy.
Drug treatment involves taking medications: neuroleptics, tranquilizers, antidepressants, mood stabilizers.
Atypical neuroleptics are used to relieve an attack and block the effects of excess dopamine in the brain. They reduce feelings of anxiety, apathy, tension. To eliminate severe symptoms of delusions and hallucinations, long-term use of this group of drugs during treatment and for some time after as maintenance therapy is necessary. They can be taken as tablets or injections.
In addition to neuroleptics, the following can be prescribed:
- tranquilizers that help relieve feelings of anxiety, anxiety, fear, reduce hypochondria and cases of obsessive thoughts;
- antidepressants used to get rid of depressive symptoms and increase mental activity, normalize appetite, phases and duration of sleep;
- normotimics aimed at stabilizing the patient’s mood, mitigating the manifestations of psychosis, eliminating irascibility, impulsiveness, irritability.

When choosing drugs, the following factors should be considered:
- the duration of the psychotic disorder;
- intensity of symptoms;
- drugs that the patient took before contacting a doctor;
- individual intolerance to drugs.
At the stage of recovery, when it is possible to remove the acute symptoms of the disorder, psychotherapy is used. In order to correct antisocial emotional and behavioral reactions, change thoughts and perception of reality, cognitive behavioral therapy is used. This is a short-term rehabilitation program, which is based on the restoration of interaction skills, the search for and solution of current mental problems, and the management of one’s fears.
Family therapy is important. The support of relatives, the correct organization of communication with the patient, the elimination of emotional and behavioral disorders within the family have a significant impact on the patient’s recovery process.
In modern specialized clinics for the treatment of mental disorders and addictions, there are several options for the treatment of acute psychosis, depending on the severity of the clinical picture:
- In mild cases, treatment of the patient at home with a visit to a specialist at the appointed time.
- In severe cases – hospitalization of the patient in a hospital (staying in the clinic without restriction of movement within the department, with restriction of movement, with constant accompaniment by medical workers).
By decision of the medical commission, partial hospitalization (stay in the clinic for a certain time – day or night) and medical leave (stay outside the clinic from several hours to several days) are allowed.
+7 (495)
121-48-31
Prophylaxis
There is no specific prevention of psychotic disorder. Compliance with general clinical recommendations significantly reduces the risk of developing psychosis. In primary prevention, people with an unstable psyche and excessive emotionality, who tend to exaggerate fear and anxiety, need to avoid stressful situations.
In primary prevention, people with an unstable psyche and excessive emotionality, who tend to exaggerate fear and anxiety, need to avoid stressful situations.
Compliance with the daily routine, good nutrition, rational distribution of time for sleep and wakefulness, feasible physical activity, positive emotions stabilize the mental state of a person.
If there are cases of a mental illness in the family, a person needs to be attentive to any changes in his perception of the surrounding reality, to control mood swings and his behavioral reactions.
Secondary prevention is necessary when the first episode of psychosis has already occurred. In such cases, the patient must be registered with a doctor and follow all his recommendations.
References:
- Bardenstein L.M., Aleshkina G.A. On the place of acute and transient psychotic disorders in the classifications of mental illness / Mental health. – 2013. – T. 11.


 gov: Premenstrual Syndrome
gov: Premenstrual Syndrome ..
.. ..
..
:max_bytes(150000):strip_icc()/overview-of-myoclonic-epilepsy-4175105_final-294e31312f174513a65079058ebb40fb.png)
 It is provoked by other diseases, most often of a mental orientation, for example, schizophrenia, bipolar disorder, dementia.
It is provoked by other diseases, most often of a mental orientation, for example, schizophrenia, bipolar disorder, dementia.
