Specialist for testicles. Scrotal Masses: Expert Guide to Diagnosis and Treatment by Urologists
When should you see a urologist for scrotal masses. How are scrotal masses diagnosed. What are the treatment options for scrotal masses. Why is early detection of testicular issues crucial. How can urologists help with various testicular conditions.
Understanding Scrotal Masses: Types and Causes
Scrotal masses are abnormal growths or swellings within the scrotum, the sac that contains the testicles. These masses can vary in size, consistency, and origin, making it crucial to understand their different types and potential causes.
Common Types of Scrotal Masses
- Testicular tumors
- Epididymal cysts
- Hydroceles
- Varicoceles
- Spermatoceles
- Testicular torsion
Are all scrotal masses cancerous? No, not all scrotal masses are cancerous. In fact, many are benign conditions that can be managed effectively with proper medical care. However, it’s essential to have any unusual growth or swelling in the scrotum evaluated by a urologist to rule out malignancy and determine the appropriate course of action.

Factors Contributing to Scrotal Masses
Several factors can contribute to the development of scrotal masses, including:
- Genetic predisposition
- Trauma or injury to the scrotum
- Infections
- Hormonal imbalances
- Age-related changes
Understanding these contributing factors can help in prevention and early detection of scrotal masses. Regular self-examinations and prompt medical attention when abnormalities are noticed are crucial steps in maintaining testicular health.
Recognizing Symptoms: When to Seek Medical Attention
Identifying the symptoms associated with scrotal masses is crucial for early detection and treatment. Men should be aware of the following signs that may indicate the presence of a scrotal mass:
- A noticeable lump or swelling in the scrotum
- Dull ache or pain in the testicles or scrotum
- Sudden, severe pain in the scrotum
- Feeling of heaviness in the scrotum
- Changes in the size or shape of the testicles
- Discomfort or pain during sexual intercourse
How long should you wait before seeing a doctor if you notice these symptoms? Dr. Jonathan Bingham, a urologic surgeon from Coordinated Health, part of Lehigh Valley Health Network, notes that the average man waits about six months after symptoms appear before seeking medical attention. However, this delay can be detrimental to proper diagnosis and treatment.

Is testicular pain always a sign of a serious condition? While testicular pain can be caused by various factors, including minor injuries or temporary conditions, persistent or severe pain should never be ignored. It’s always better to err on the side of caution and consult a urologist to rule out any serious underlying issues.
Diagnostic Procedures for Scrotal Masses
When a patient presents with symptoms of a scrotal mass, urologists employ a variety of diagnostic procedures to accurately identify the nature of the condition. These procedures are designed to provide a comprehensive assessment of the scrotal area and help determine the most appropriate treatment plan.
Physical Examination
The first step in diagnosing scrotal masses is a thorough physical examination. During this procedure, the urologist will:
- Visually inspect the scrotum for any visible abnormalities
- Palpate the testicles and surrounding structures to feel for lumps or swelling
- Assess the size, shape, and consistency of any detected masses
- Evaluate for tenderness or pain in the area
Imaging Studies
To get a more detailed view of the scrotal contents, various imaging studies may be employed:

- Ultrasound: This non-invasive procedure uses sound waves to create detailed images of the scrotum and its contents. It’s particularly useful in distinguishing between solid and fluid-filled masses.
- MRI (Magnetic Resonance Imaging): In some cases, an MRI may be recommended to provide high-resolution images of the scrotal structures and surrounding tissues.
- CT (Computed Tomography) Scan: While less commonly used for initial diagnosis, CT scans may be employed to assess the extent of certain conditions or to look for metastasis in cases of suspected testicular cancer.
Blood Tests
Blood tests play a crucial role in the diagnostic process, particularly when testicular cancer is suspected. These tests may include:
- Tumor markers (e.g., alpha-fetoprotein, beta-hCG, LDH)
- Hormonal assessments
- Complete blood count
- Liver and kidney function tests
How accurate are these diagnostic procedures in identifying scrotal masses? While no single test is 100% accurate, the combination of physical examination, imaging studies, and blood tests provides a high level of diagnostic accuracy. In cases where uncertainty remains, a biopsy may be recommended for definitive diagnosis.

Treatment Options for Scrotal Masses
The treatment of scrotal masses varies depending on the specific diagnosis, severity of symptoms, and overall health of the patient. Urologists tailor treatment plans to address each individual’s unique situation, employing a range of approaches from conservative management to surgical intervention.
Conservative Management
For some benign conditions, conservative management may be appropriate. This can include:
- Watchful waiting with regular monitoring
- Pain management techniques
- Anti-inflammatory medications
- Supportive undergarments
Minimally Invasive Procedures
Certain scrotal masses can be treated with minimally invasive procedures, such as:
- Aspiration: Used for fluid-filled cysts or hydroceles
- Sclerotherapy: Injection of a solution to shrink varicoceles
- Embolization: A technique used to block blood flow to varicoceles
Surgical Interventions
In cases where conservative measures are insufficient or when dealing with potentially malignant masses, surgical intervention may be necessary. Surgical options include:
- Orchiectomy: Removal of the affected testicle (typically for testicular cancer)
- Hydrocelectomy: Surgical repair of a hydrocele
- Varicocelectomy: Surgical correction of varicoceles
- Spermatocelectomy: Removal of a spermatocele
What factors determine the choice of treatment for scrotal masses? The selection of treatment depends on several factors, including the type and size of the mass, the patient’s age and overall health, the presence of symptoms, and the potential impact on fertility. Urologists work closely with patients to determine the most appropriate treatment approach, considering both immediate relief of symptoms and long-term outcomes.
The Importance of Early Detection and Regular Check-ups
Early detection of scrotal masses is crucial for several reasons:
- Improved treatment outcomes: Detecting masses early often leads to more effective and less invasive treatment options.
- Preservation of fertility: Timely intervention can help preserve testicular function and fertility.
- Prevention of complications: Early treatment can prevent the progression of benign conditions and reduce the risk of complications.
- Better prognosis for malignant conditions: In cases of testicular cancer, early detection significantly improves survival rates.
How often should men perform self-examinations? Urologists recommend monthly self-examinations of the testicles. This simple practice can help men become familiar with their normal anatomy and quickly notice any changes or abnormalities.

Steps for Testicular Self-Examination
- Perform the exam during or after a warm shower when the scrotum is relaxed
- Gently roll each testicle between your fingers, feeling for any lumps or irregularities
- Check for any changes in size, shape, or consistency
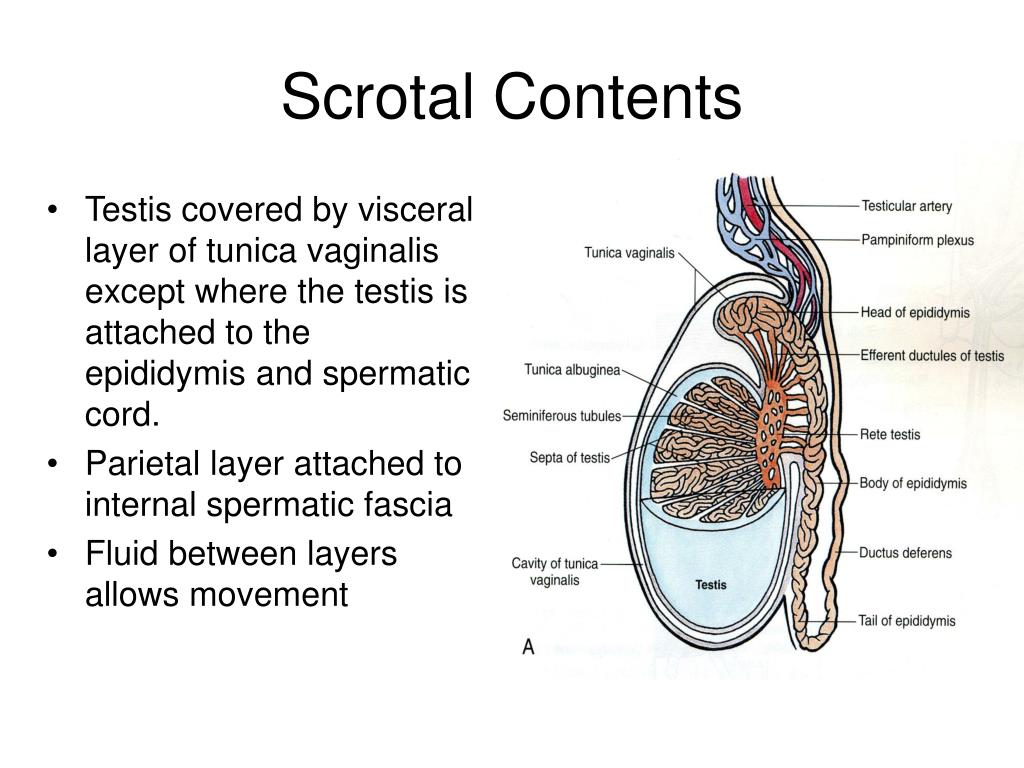
- Be aware of the normal presence of the epididymis, a tube-like structure on the back of each testicle
- Report any unusual findings to your healthcare provider promptly
Regular check-ups with a urologist are also important, especially for men with risk factors or a history of testicular issues. These visits allow for professional assessment and early intervention if necessary.
Psychological Impact and Support for Patients with Scrotal Masses
Dealing with scrotal masses can have significant psychological effects on patients. The uncertainty, fear of cancer, concerns about fertility, and potential impact on sexual function can cause anxiety and stress. It’s important to address these psychological aspects alongside the physical treatment of scrotal masses.

Common Psychological Challenges
- Anxiety about the diagnosis and treatment process
- Depression related to potential fertility issues
- Body image concerns, especially in cases requiring surgery
- Fear of recurrence or long-term health implications
- Stress about discussing the condition with partners or family members
How can patients cope with the emotional impact of scrotal masses? Coping strategies may include:
- Seeking information and understanding the condition thoroughly
- Communicating openly with healthcare providers about concerns
- Joining support groups or connecting with others who have experienced similar issues
- Engaging in stress-reduction techniques such as meditation or yoga
- Considering professional counseling or therapy if needed
Urologists and healthcare teams play a crucial role in providing not just medical care but also emotional support and resources for patients dealing with scrotal masses. This holistic approach to care can significantly improve patient outcomes and quality of life.

Advances in Urology: Improving Diagnosis and Treatment of Scrotal Masses
The field of urology has seen significant advancements in recent years, leading to improved diagnosis and treatment of scrotal masses. These innovations have resulted in more accurate diagnoses, less invasive treatments, and better outcomes for patients.
Diagnostic Advancements
- High-resolution ultrasound technology: Provides clearer images for more accurate diagnosis
- Contrast-enhanced ultrasound: Improves visualization of blood flow in scrotal masses
- Molecular imaging techniques: Helps in early detection and staging of testicular cancer
- Artificial intelligence in image analysis: Assists in identifying and classifying scrotal masses
Treatment Innovations
Recent advancements in treatment options include:
- Robotic-assisted surgery: Offers precise and minimally invasive surgical options
- Targeted therapies for testicular cancer: Improves treatment efficacy while reducing side effects
- Cryoablation techniques: Provides non-surgical treatment options for certain types of masses
- Fertility preservation techniques: Helps maintain reproductive potential in cancer patients
How have these advancements improved patient outcomes? These innovations have led to earlier detection of scrotal masses, more accurate diagnoses, and tailored treatment plans. This has resulted in improved survival rates for testicular cancer, reduced surgical complications, and better preservation of testicular function and fertility.

As research continues, we can expect further improvements in the management of scrotal masses, offering hope for even better outcomes and quality of life for patients affected by these conditions.
When Should You See a Urologist? – What to Know
UUANJ earned the “Center of Excellence” destinction for BPH and Incontinence Care!
UUANJ earned the “Center of Excellence” destinction for BPH and Incontinence Care!
UUANJ earned the “Center of Excellence” destinction for BPH and Incontinence Care!
UUANJ earned the “Center of Excellence” destinction for BPH and Incontinence Care!
UUANJ earned the “Center of Excellence” destinction for BPH and Incontinence Care!
UUANJ earned the “Center of Excellence” destinction for BPH and Incontinence Care!
Patient FormsTelehealthPatient PortalBill Pay
When it comes to health problems, men are most likely to endure their symptoms longer before going to the doctor than women. Sometimes, it may be because they don’t feel like their condition is serious enough, and other times, they may find it embarrassing to have certain parts of their body checked.
The latter is the case when it comes to testicular issues. According to Urologic surgeon, Dr. Jonatahan Bingham, it takes the average man around six months to see a doctor after symptoms of testicular mass or tumor appear. Dr. Bingham is from Coordinated Health, which is part of Lehigh Valley Health Network.
According to Urologic surgeon, Dr. Jonatahan Bingham, it takes the average man around six months to see a doctor after symptoms of testicular mass or tumor appear. Dr. Bingham is from Coordinated Health, which is part of Lehigh Valley Health Network.
Here’s when it’s time to visit your urologist:
Signs of prostate cancer
Your symptoms could mean you have prostate cancer, which is one of the most common cancers among men. Prostate cancer does not show noticeable symptoms at an early stage and can only be identified by having prostate cancer screenings. Having said that, you should highly consider going to the urologist if you feel worried about this condition.
Spotting early symptoms of prostate cancer makes it easier to cure. However, this means that you shouldn’t skip your appointments with your urologist to see symptoms and prevent them from becoming more serious.
Testicular pain
When you start to feel constant mild pains in your testicular area, it’s time to consult a urologist. If something doesn’t feel right, you need to have it checked right away to prevent any serious conditions. The urologist can also give you remedies and treatments to alleviate the pain.
If something doesn’t feel right, you need to have it checked right away to prevent any serious conditions. The urologist can also give you remedies and treatments to alleviate the pain.
Erectile dysfunction
Erectile dysfunction is common, particularly among older men. However, it is also typically tied to other medical issues that can be medical or psychological. When you observe that you have erectile dysfunction, consult the urologist right away to have any possible conditions treated.
Urinary issues
Issues like slowing of the urinary stream, painful urination, frequent urination, and sudden start and stop of the urinary stream are common among men as they grow older. That said, such issues could also be tied to the growth of the prostate gland.
It’s important to address these issues because they can lead to serious problems in the kidney or the bladder in the long run.
Blood in the urine
When you start to see blood in your urine, don’t delay testing and visit your urologist right away.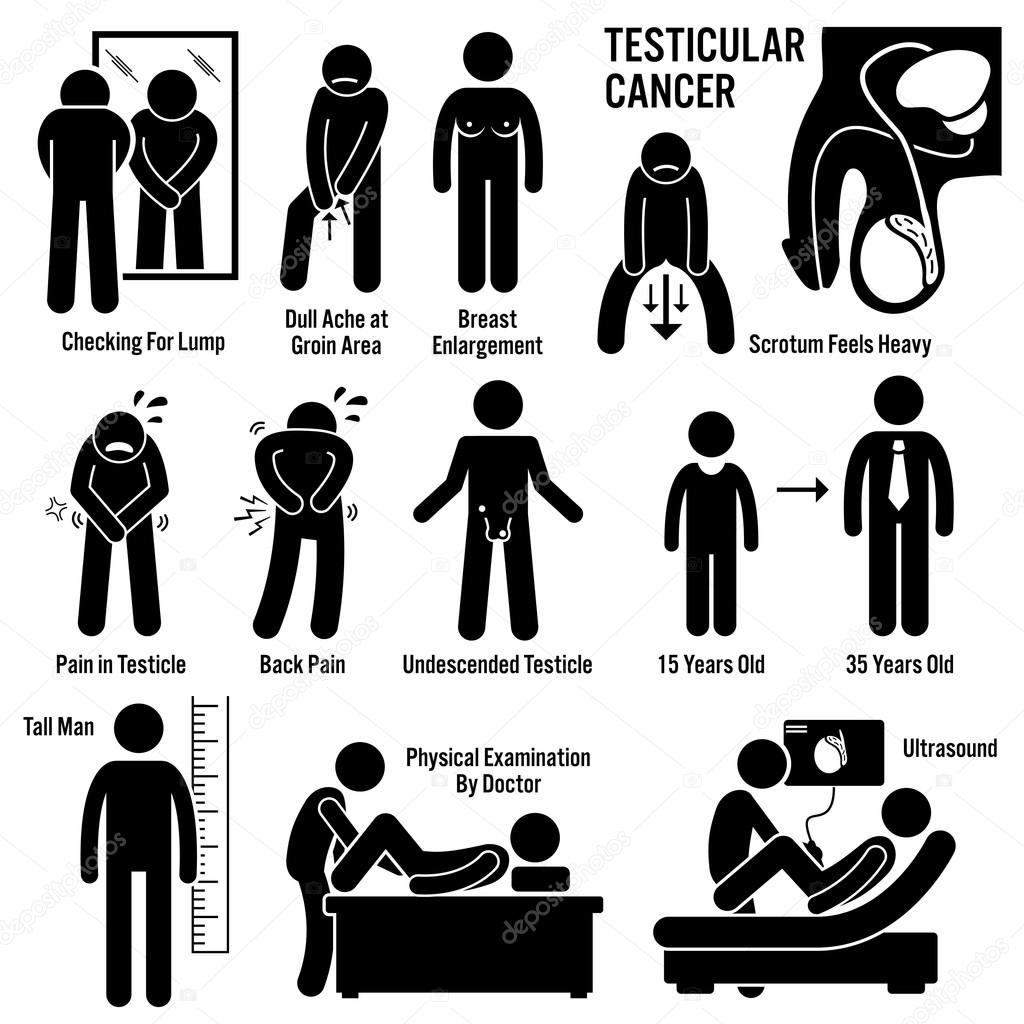 Blood in the urine can signify prostate enlargement, kidney stones, or tumors in the kidney or bladder.
Blood in the urine can signify prostate enlargement, kidney stones, or tumors in the kidney or bladder.
Kidney stones
Kidney stones may not be painful early on, but over time, it can cause excruciating pain and severe health conditions. Prolonging your treatment can lead to serious kidney issues that can be deadly. When you spot these symptoms, visit your urologist to prevent your condition from getting worse.
Conclusion
Men should not be ashamed or embarrassed to talk about testicular issues, especially if it’s for medical concerns. Visiting the urologist when symptoms first appear is essential to avoid any serious condition. More importantly, doing so will help relieve pain and stop issues that can be worrisome from appearing again.
We care about your health! Our team of expert urologists in New Jersey is more than willing to address your concerns. Request an appointment with us today!
Disclaimer: All content found on the UUANJ. COM Website, including text, images, audio, or other formats were created for informational purposes only.
COM Website, including text, images, audio, or other formats were created for informational purposes only.
The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
If you think you may have a medical emergency, call your doctor, go to the emergency department, or call 911 immediately.
What Kind of Doctor Should I See For Testicular Pain?
Ball pain. Nuts aching. Sac is hurtin’. Regardless of what you call it, testicular pain is no fun.
You’re not alone. Testicular pain is really common. Unfortunately guys don’t talk about their berries being squeezed in vice grip.
Instead they suffer in silence and walk around like John Wayne just got off of a horse.
Maybe this is something serious though. Testicular torsion (twisted testicle) or epididymitis (bacterial infection) are no joke and require immediate medical attention. I’m certain cancer might be running through your mind as well.
So what kind of doctor should you see for testicular pain? At some point you’ll need a urologist. Maybe you had no idea there was a ball pain specialist. Or maybe you’ve seen 3 of them and no one seems to help.
Let’s get you some help for those achy breaky balls. Because when they’re aching, it’s hard to feel good about anything.
What causes testicular pain?
A good doctor develops a differential diagnosis for every patient complaint. A list of possible medical conditions that could be causing the symptom. For testicular pain this list includes but is not limited to:
Testicular torsion
Testicular torsion is fancy doctor speak for a twisted testicle. No blood is going to the testicle and this is not good.
It is usually seen in kids and young adults.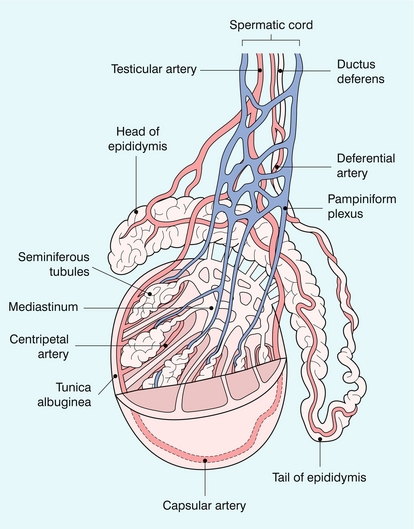 It is exceedingly rare after age 40. It will cause severe, drop you to your knees pain with nausea or vomiting. Unless you get your ball “untwisted” with surgery in 4 hours or less, the testicle unfortunately dies due to lack of blood flow.
It is exceedingly rare after age 40. It will cause severe, drop you to your knees pain with nausea or vomiting. Unless you get your ball “untwisted” with surgery in 4 hours or less, the testicle unfortunately dies due to lack of blood flow.
Although intermittent torsion can occur, this is pretty rare. If you’ve been aching for weeks to months then torsion is very unlikely.
Epididymo-orchitis
An infection of the testicle or epididymis typically presents with an acute onset (fast) of one-sided pain and swelling. An examination will clearly show swelling and tenderness. Usually this is caused by a urinary tract infection or sexually transmitted disease.
Varicocele
Swollen veins draining the testicle are seen in up to 15% of men. Sometimes visible as a “bag of worms in the sac”, varicoceles are more common on the left side. They can cause a heavy, dull ache that’s usually worse with standing throughout the day.
The veins will not “burst” but they can cause male infertility in addition to chronic pain.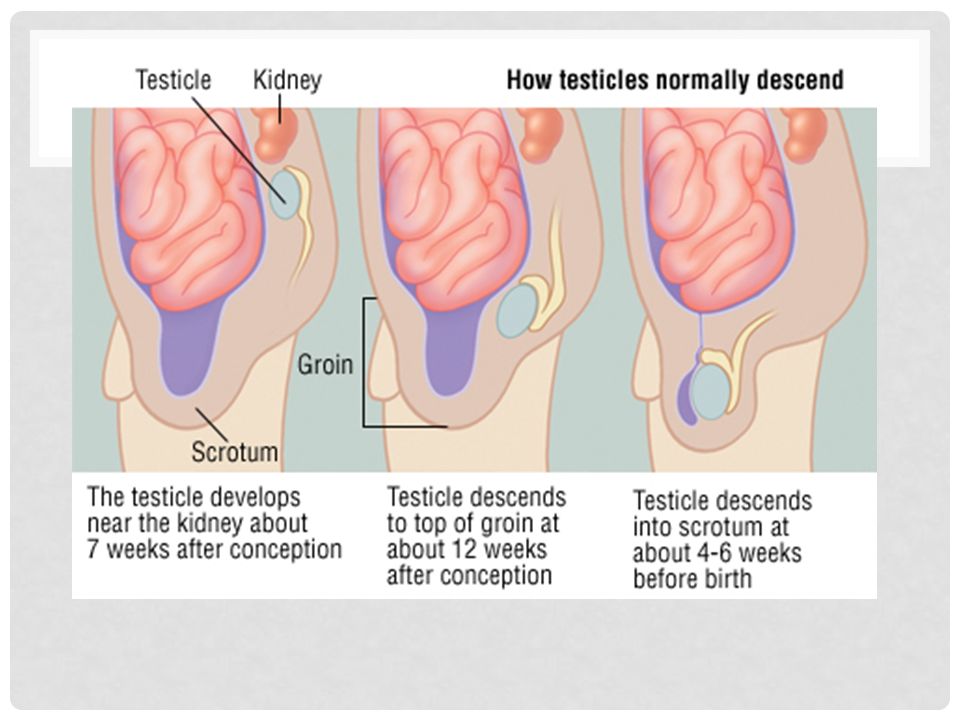 A surgical repair by a micro-surgical specialist will fix this issue for good.
A surgical repair by a micro-surgical specialist will fix this issue for good.
Inguinal hernia
A hernia is a weakness of the abdominal wall. Bulging and pain can occur at this site of weakness as your “insides” are “poking out.” When this bulging occurs in the groin area we call this an inguinal hernia.
An inguinal hernia can extend into the scrotum leading to ball pain and swelling. This is usually obvious on a physical examination but at times can be subtle. This is treated with surgery to repair the weakened tissues.
Hydrocele
Another cause of a painful “big sac” is an accumulation of fluid around the testicle. A hydrocele most often occurs for no good reason. It can be a consequence of a trauma, infection or even cancer. An ultrasound of the scrotum will confirm the diagnosis.
Sometimes a hydrocele will go away on it’s own. If it doesn’t then surgery does the trick.
Epididymal cyst
Speaking of swelling of the sac you can also have lumps next to the testicle. The epididymis sits behind the testicle and carries sperm. Cysts can develop leading to a “third nut” as men have told me. These are universally benign and can be cut out if they are causing pain.
The epididymis sits behind the testicle and carries sperm. Cysts can develop leading to a “third nut” as men have told me. These are universally benign and can be cut out if they are causing pain.
Testicular cancer
Testicular cancer most often presents with a painless firm mass of the testicle itself. I’ve included it because cancer should always be considered in a differential diagnosis. The good news is that cancer rarely causes pain and is easily ruled out with an exam and ultrasound.
Kidney stone
Kidney stones are bad enough but ball pain as well? When a kidney stone is traveling down the urine tube (the ureter) it can cause a referred pain to the testicle. If you have associated back or abdominal pain, nausea/vomiting or a history of kidney stones, evaluation with CT scan should be considered.
Post-vasectomy pain syndrome
This rare condition (1/500 vasectomies) is distinguished by the start of pain shortly after a vasectomy. We are not certain why it happens but it is not fun.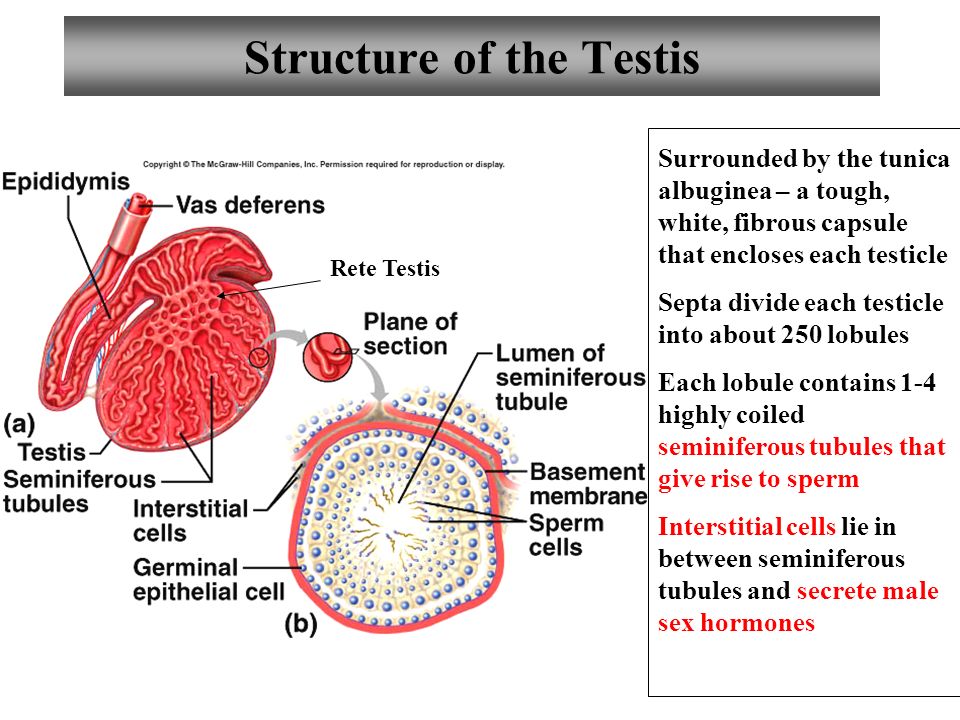 Local anesthesia blocks of the spermatic cord can temporarily relieve the pain.
Local anesthesia blocks of the spermatic cord can temporarily relieve the pain.
When necessary, microscopic denervation procedures can be performed with success rates up to 85%. Sometimes men even elect to have the vasectomy reversed (vasovasostomy) to re-hook the plumbing pipes. This releases the back pressure and solves the post-vasectomy pain as well.
Musculoskeletal cause
The testicle is connected to the spermatic cord. An anatomic structure containing blood vessels, nerves, the vas deferens and muscles running to the testicle. The muscles are known as the cremaster muscles.
The reason your balls hug tight to the body in cold water is the cremaster muscle contracting to keep your berries warm. This muscle is a continuation of the internal oblique muscle; a series of muscles fibers that make up your core abdominal wall.
When you suffer from low back pain, are hanging on to 40 extra pounds of belly fluff, or lifting heavy objects all day, you are straining your core abdominal muscles. Since these muscles are connected to the cremaster muscle, your testicle hurts.
Since these muscles are connected to the cremaster muscle, your testicle hurts.
Musculoskeletal strain is probably the cause of 95% of testicular pain seen by a urologist. If you’ve had normal exams, ultrasounds, urine tests and no one has been able to help you yet, then this is probably what’s going on. As a urologist, it’s not unusual to see 5-10 men per week for a 2nd opinion on ball pain.
Testicular pain evaluation
Regardless of the kind of doctor you see for testicular pain, every evaluation starts with a good history. Bilateral (both sides) or alternating pain eliminates almost all of the above conditions with the exceptions of post-vasectomy pain syndrome and musculoskeletal causes.
A physical exam can detect masses, lumps and swellings. Tenderness with an otherwise normal exam is seen with many of these conditions. Some doctors you see for testicular pain may be experienced (urologist) or inexperienced (pretty much everyone else) with performed a thorough and accurate exam for testicular pain.
When necessary imaging can be performed. A CT scan should be considered for suspected kidney stones. A scrotal ultrasound will confirm findings on a physical exam.
Sometimes a scrotal ultrasound will show incidental findings that are not felt on an exam (small hydrocele or cyst). If a doctor can’t feel it then it’s not the source of the pain.
Treatment for Testicular Pain
I’m going to assume that you’ve had a normal exam, imaging tests and have never had a vasectomy. This leads us to our diagnosis of chronic testicular pain (also known as orchialgia).
First and foremost, we recommend viewing this condition like headaches and backaches. Most headaches aren’t due to brain cancer. Most backaches don’t require a visit to the spine surgeon. They are musculoskeletal in nature.
When muscles and nerves are irritated, most exams are normal. Unfortunately quick fixes are not always possible.
Here are some options for treating chronic testicular pain:
Improved diet and exercise
It’s amazing how often clean eating and moving our body is the answer to chronic medical conditions. Eating chalupas on the couch never served anybody except the business owners of Taco Bell. The crap we eat causes inflammation. Inflammation causes chronic pain.
Eating chalupas on the couch never served anybody except the business owners of Taco Bell. The crap we eat causes inflammation. Inflammation causes chronic pain.
When we exercise we release our body’s natural pain killers called endorphins. Strengthening your core and lower back can help testicular pain over time.
As a result of diet and exercise you should start shedding some pounds from your belly. All this extra weight we carry in our midsection strains our back and core muscles. Lose the weight, lose the ball pain.
I’ve had more patients tell me their testicular pain resolved after weight loss than any other thing I’m about to suggest.
Pelvic physical therapy
Muscle tension of the lower abdomen and pelvic floor is associated with chronic testicular pain. An experienced pelvic physical therapist can identify any muscle imbalances, improving chronic pain. It doesn’t work for everybody, but there’s little risk in giving a session a try.
Off-label medications
Sometimes medications designed for another purpose are helpful for seemingly unrelated medical conditions.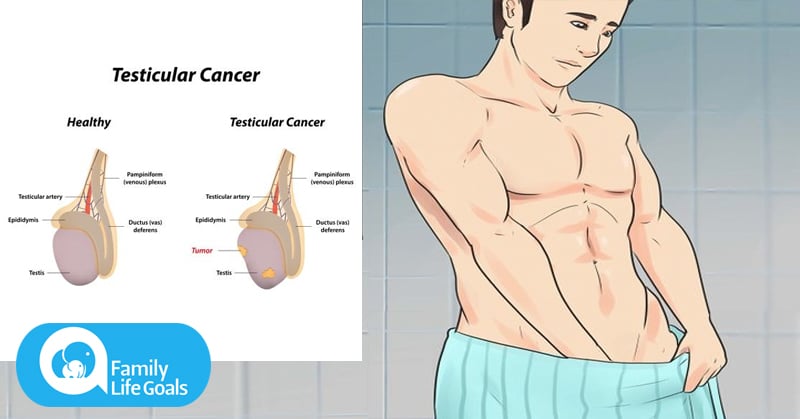 This is known as an off-label medication. For chronic testicular pain I’ve had success with Tamsulosin (prostate medication), hydroxyzine (anti-histamine) and amitriptyline (anti-depressant).
This is known as an off-label medication. For chronic testicular pain I’ve had success with Tamsulosin (prostate medication), hydroxyzine (anti-histamine) and amitriptyline (anti-depressant).
Every urologist has his or her favorite for helping men get a little relief. It’s really important to avoid narcotics at all costs. This is a chronic condition and the last thing you want is an opioid dependence.
Surgery
Some of the same microsurgical options are available for testicular pain. Referral to a urologist fellowship trained in microsurgery may be your last option for treating unresolved testicular pain. Performed under anesthesia in the office or surgery center, spermatic cord denervation or cryotherapy can have success rates of 70-85%.
Who’s The Best Doctor For Testicular Pain?
If you haven’t had an in-person visit with a doctor then you should start there. This is one of those instances where a physical examination is important. A scrotal ultrasound is not a bad idea either to dot the “I’s” and cross the “T’s. ”
”
If you’ve already been to a urologist, and are frustrated, then why not consider a second opinion with a VirtuCare specialist. We can review any medical records that you provide and do a deep dive to make certain nothing has been missed.
Our second opinion visits last on average 30 minutes so you know you won’t be rushed for time. We are hear to listen to you.
With our network of colleagues, we’d be happy to make a referral to a microsurgical expert if that’s what it takes to cure your testicular pain.
Unfortunately there are certain medical conditions that can’t be cured. But you at least deserve care from an expert who will listen and do everything they can to help.
Your family jewels deserve the best.
Ultrasound of the scrotum
Ultrasound of the scrotum organs (testicles, epididymis, scrotal parts of the spermatic cords) is attended by patients from various specialists – a surgeon, urologist, andrologist, pediatrician, internist, oncologist.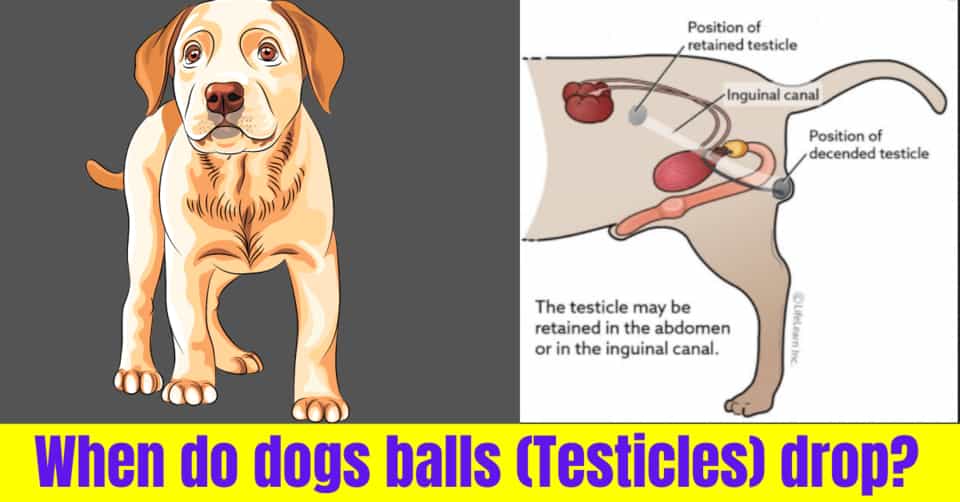 This is due to the wide range of tasks that can be solved by the method of ultrasonic scanning of this area. Primarily the following:
This is due to the wide range of tasks that can be solved by the method of ultrasonic scanning of this area. Primarily the following:
- Search for possible causes of the scrotal complaints that the patient describes or symptoms found on examination:
- pain, enlargement, skin changes, palpable mass in testis, scrotum, groin.
- Establishment of the volume of traumatic damage to the contents of the scrotum.
- Search for possible causes of infertility ( see Ultrasound for male infertility ).
- Establishment of developmental anomalies.
- Dynamic monitoring during treatment.
How is ultrasound of the scrotum organs performed at the Seven Doctors Clinic
Start the examination with the patient lying on the couch. The area to be examined is free from clothing. A gel is applied to the skin of the scrotum for better contact with the transducer. For a detailed examination of the anatomical structures in different modes, as well as for all the necessary measurements, an average of 15 minutes is required, during which the doctor performs sliding movements with the sensor. If the test reveals an enlarged vein in the spermatic cord (varicocele), an additional test will be recommended. Inspection in this case will be continued in a standing position. At the same time, the doctor will evaluate changes in blood flow in the veins of the scrotum in the color mapping mode and register them in the pulse Doppler mode. The images that best illustrate the changes that deserve attention are usually saved and printed.
If the test reveals an enlarged vein in the spermatic cord (varicocele), an additional test will be recommended. Inspection in this case will be continued in a standing position. At the same time, the doctor will evaluate changes in blood flow in the veins of the scrotum in the color mapping mode and register them in the pulse Doppler mode. The images that best illustrate the changes that deserve attention are usually saved and printed.
The conclusion of the doctor of ultrasound diagnostics
The doctor reflects the data obtained during the study in the description of the study. At the end of this document, the specialist formulates his conclusion, where he reports the following information:
- whether there are ultrasound signs of pathological changes in the scrotum organs;
- which pathological conditions or diseases are most likely to correspond to the seen ultrasound picture.
In addition, it can be recommended which doctor should be consulted based on the ultrasound results, if the patient came before contacting a specialist. If it turns out that a follow-up ultrasound is necessary, the desired dates will be indicated. The final diagnosis and treatment recommendations are the competence of a specialist in medical disciplines.
If it turns out that a follow-up ultrasound is necessary, the desired dates will be indicated. The final diagnosis and treatment recommendations are the competence of a specialist in medical disciplines.
900 02
Did the article help you?
Thank you for your rating. How can we improve the article?
By clicking on the button, you consent to the processing of your personal data and agree to the privacy policy.
Ultrasound of the scrotum in Moscow, prices
Ultrasound of the scrotum is a highly informative, non-invasive and safe study that allows you to obtain an objective assessment of the state of tissues and internal structures, make a diagnosis and identify pathological changes. As part of the diagnosis, the doctor can examine the inguinal region in detail, detect tumors, accumulations of fluid and other dangerous conditions that require close attention from specialists and treatment.
As part of the diagnosis, the doctor can examine the inguinal region in detail, detect tumors, accumulations of fluid and other dangerous conditions that require close attention from specialists and treatment.
In “Nearmedic” in Moscow, ultrasound of the scrotum organs is performed using expert equipment. It is possible to conduct an ultrasound of the scrotum organs with Dopplerography, that is, with an additional study of blood flow and the state of the vessels located in the scrotum. We have created comfortable conditions for men, provided high information content of the study. You can sign up for an ultrasound scan of the scrotum in the near future – contact the Nearmedic registry!
Ultrasound Benefits:
- The comfort of the examination for men. As part of the diagnosis of the inguinal zone, the doctor delicately passes the sensor along the testicles, soft tissues of the groin – there is no pain, no discomfort. Also, doctors make efforts so that the patient does not experience embarrassment during the ultrasound of the scrotum.

- Security. The emitted ultrasonic waves are not able to have a harmful effect on organs, adjacent structures and tissues. There is no radiation exposure to the organs when performing color flow and ultrasound of the scrotum.
- High information content of the ultrasound of the scrotum. Doppler ultrasound diagnostics provides a large amount of diagnostic data, which allows you to make a diagnosis, clarify the condition of the internal tissues and structures of the scrotum. It is difficult to overestimate the importance of examining the scrotum with an ultrasound method!
- Fast execution. Ultrasound of the scrotum takes no more than 20 minutes. This study can be done at lunchtime or between important tasks during the working day.
- Affordable price for ultrasound (with doppler).
Indications for ultrasound of the scrotum (groin)
Ultrasound is performed both for preventive purposes and when characteristic signs of the development of urological pathologies appear.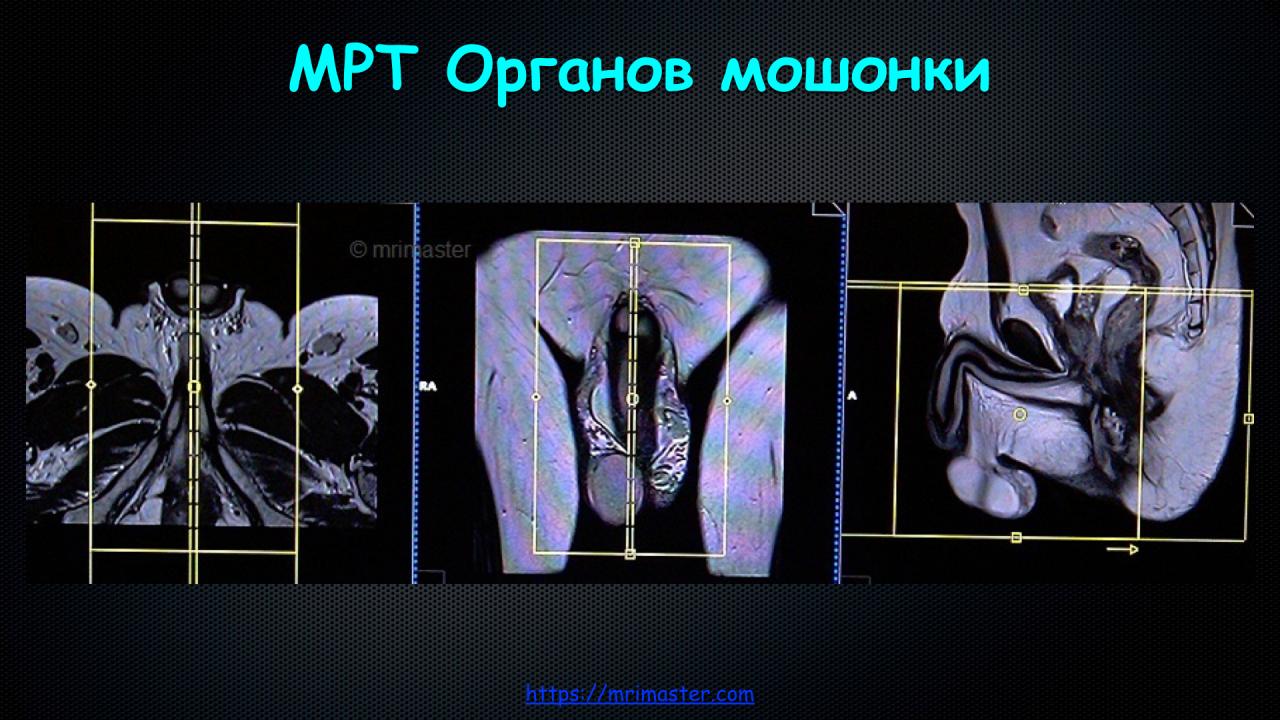
Ultrasound of the scrotum with CFD (Doppler scanning) is performed in cases where there are disorders in the vascular system that can somehow affect the condition of the testicle, prostate or other structures of the inguinal zone. “Male” diseases are often asymptomatic in the early stages,
Reasons for urgent ultrasound in men:
- blood in semen;
- enlarged inguinal lymph nodes;
- pain in the testicles or in the soft tissues of the inguinal zone;
- redness, induration of testis;
- signs of testicular hernia;
- swelling of the testis or soft tissues of the inguinal zone;
- signs of an inflammatory process in the inguinal zone;
- changes and deviations from the norm in the results of the spermogram;
- infertility;
- erectile dysfunction.
Testicular and scrotum ultrasound is due to recent trauma. For example, if there was a fall or there was a blow to the groin. Even if there are no severe symptoms and pain, it is better to conduct an ultrasound of the testicles and scrotum in order to identify hidden or delayed effects.
Even if there are no severe symptoms and pain, it is better to conduct an ultrasound of the testicles and scrotum in order to identify hidden or delayed effects.
Ultrasound of the scrotum is performed to monitor and evaluate the effectiveness of the treatment, for example, with varicocele, orchitis and other urological diseases in men.
Once a year, ultrasound is performed for those patients who are at risk for the development of severe urological diseases. For example, if a cyst grows in the testicle, it increases in size, but the doctors have not yet decided on a surgical intervention. Or there are acquired anomalies that can go on to take severe and complicated forms. Ultrasound makes it possible to monitor the course of the disease and track the dynamics.
Purpose of organ ultrasound (scrotum)
The purpose of the ultrasound of the testicles and scrotum is to obtain reliable data on the state of tissues and structures.
Ultrasound of the testicles and scrotum reveals inflammatory diseases, tumor and cystic processes. For example, ultrasound of the testicles and scrotum reveals: orchitis, epididymitis, varicocele, hydrocele.
For example, ultrasound of the testicles and scrotum reveals: orchitis, epididymitis, varicocele, hydrocele.
Testicular and scrotal ultrasonography may be used to evaluate surgery or conservative management.
Inguinal Ultrasound Preparation
No special preparation is required for testicular and scrotal ultrasound. The only recommendation is to remove the hair in the groin area. The hair itself will not interfere with the ultrasound of the scrotum, however, after the diagnosis, it will be quite difficult to completely remove the gel from the skin. For this reason alone, depilation of the inguinal zone is recommended.
Ultrasound examination of the scrotum
The Nearmedic doctor receives the patient in his office, collects an anamnesis, then helps to take a comfortable position on the couch. At the first stage, a study of internal structures and tissues is performed and diagnostics is carried out in a supine position. The doctor studies the structure of the testicles by moving the sensor along the inguinal zone. Further, for the diagnosis of blood flow, the use of Doppler and a change in body position may be required. To assess the circulatory system in the inguinal zone, a man needs to take a standing position, fixing the penis. Doppler scanning and ultrasound of the scrotum are performed in various planes: oblique, transverse, longitudinal.
Further, for the diagnosis of blood flow, the use of Doppler and a change in body position may be required. To assess the circulatory system in the inguinal zone, a man needs to take a standing position, fixing the penis. Doppler scanning and ultrasound of the scrotum are performed in various planes: oblique, transverse, longitudinal.
All diagnostic data is captured. It takes approximately 15-20 minutes to prepare the protocol and conclusion. If pathological foci are identified, images can be printed.
Data interpretation after scrotum ultrasound
Nearmedic doctor issues a detailed report. But it should not be interpreted independently. You need to contact a urologist or a doctor of another specialization for a competent explanation. The fact is that the conclusion cannot be considered a diagnosis – it is made by the doctor based on the combination of clinical symptoms and examination results. In some cases, additional diagnostic procedures are required.

