Swelling puncture wound. Comprehensive Guide to Cuts and Puncture Wounds: Symptoms, Treatment, and Prevention
What are the main differences between cuts and puncture wounds. How can you identify the severity of a wound. When should you seek immediate medical attention for a cut or puncture wound. What are the best practices for treating minor wounds at home. How can you prevent infections in cuts and puncture wounds. What are the long-term complications of untreated wounds. How do different types of wounds affect healing time and scarring.
Understanding Cuts and Puncture Wounds: Definitions and Characteristics
Cuts and puncture wounds are common injuries that can range from minor to severe. Understanding their characteristics is crucial for proper treatment and prevention of complications.
What is a Cut?
A cut, also known as a laceration, is a break or opening in the skin. Cuts can vary in depth, appearance, and severity:
- Depth: Can be superficial or deep, potentially affecting underlying structures
- Appearance: May be smooth or jagged
- Affected areas: Can involve tendons, muscles, ligaments, nerves, blood vessels, or bone
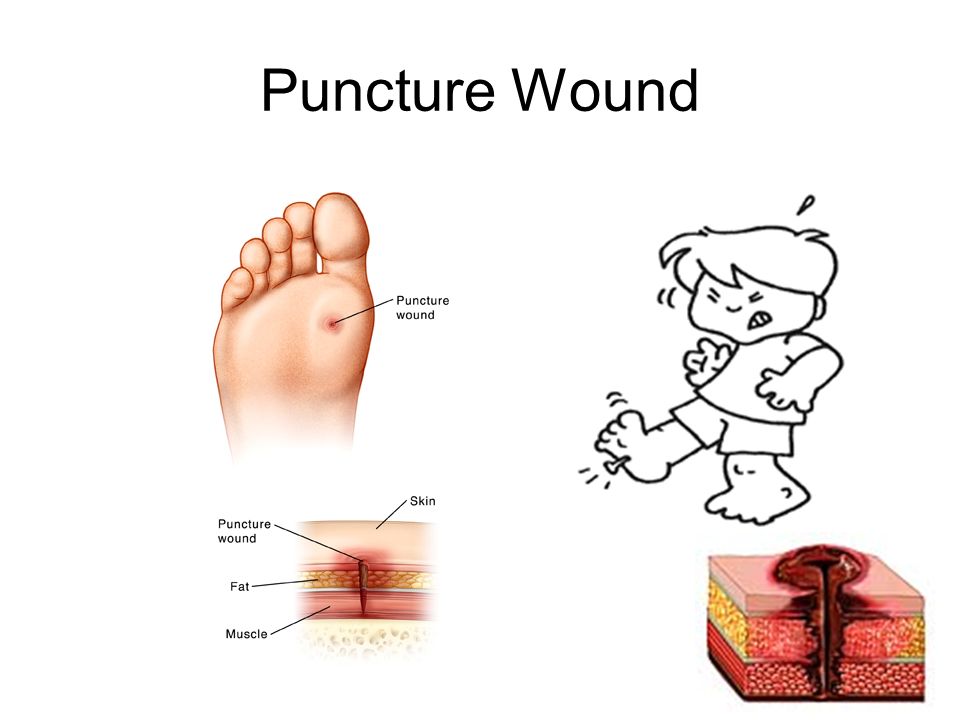
What is a Puncture Wound?
A puncture wound is caused by a pointed object penetrating the skin. Key characteristics include:

- Appearance: Often looks small on the surface
- Depth: Can extend deep into tissue layers
- Common causes: Nails, knives, sharp teeth
Identifying Symptoms and Assessing Wound Severity
Recognizing the symptoms of cuts and puncture wounds is essential for determining the appropriate course of action. Common symptoms include:
- Bleeding
- Pain
- Impaired function or movement
- Numbness or tingling below the wound site
How can you determine if a wound requires professional medical attention? Consider the following factors:
- Depth: Wounds deeper than 1/4 inch may need stitches
- Location: Facial wounds often require professional care
- Bleeding: Severe or uncontrolled bleeding necessitates immediate medical intervention
- Foreign objects: Visible debris or missing parts of the injuring object warrant medical evaluation
- Signs of infection: Redness, swelling, warmth, or pus indicate potential infection
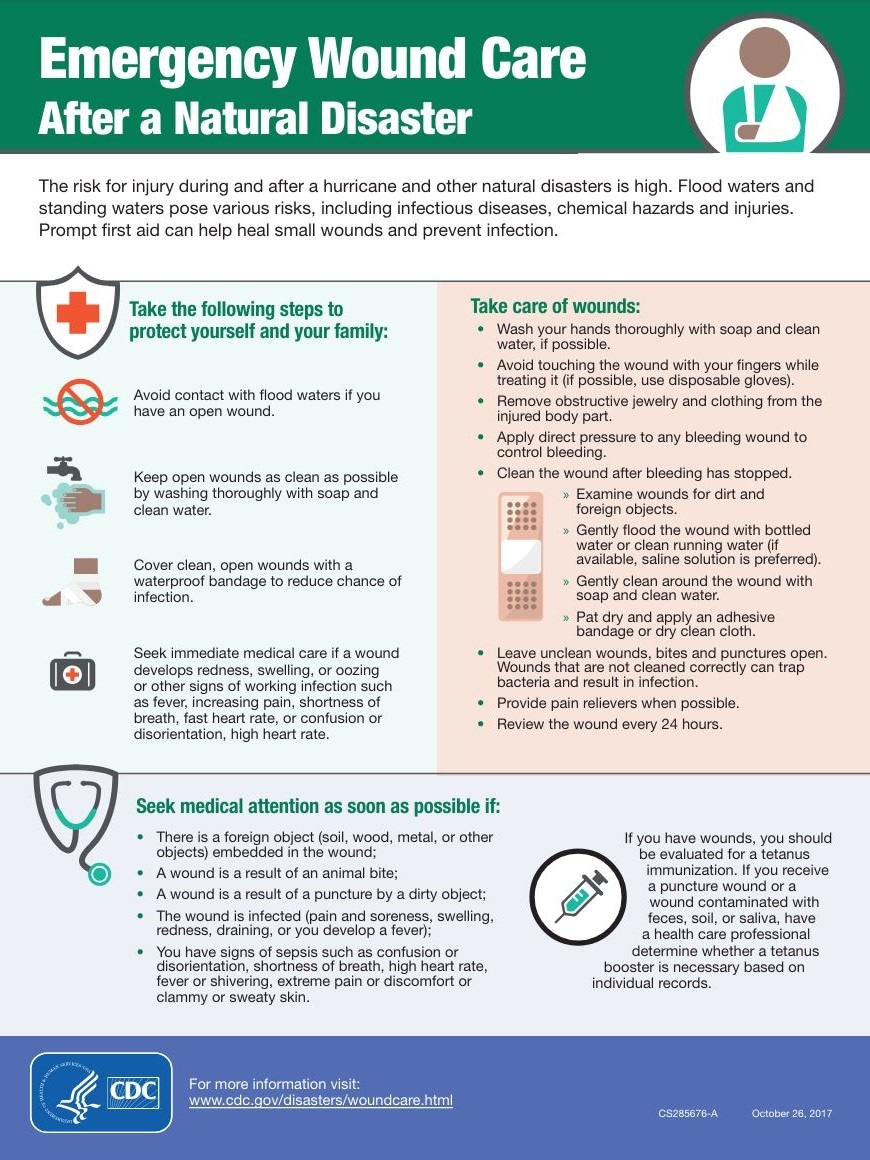
First Aid Techniques for Minor Cuts and Puncture Wounds
Proper first aid can prevent infection and promote faster healing. Follow these steps for minor injuries:
For Minor Cuts:
- Wash your hands thoroughly with soap or antibacterial cleanser
- Clean the cut with mild soap and water
- Apply direct pressure to stop bleeding
- Use antibacterial ointment and a clean, non-stick bandage
For Minor Punctures:
- Wash your hands with soap or antibacterial cleanser
- Rinse the puncture under running water for 5 minutes, then wash with soap
- Inspect for visible foreign objects (do not probe the wound)
- Apply antibacterial ointment and a clean, non-stick bandage
When to Seek Professional Medical Care
Certain situations require immediate medical attention. Seek professional care if:
- The wound is deep, gaping, or has jagged edges
- Bleeding doesn’t stop after 10-15 minutes of direct pressure
- The injury is on the face, near a joint, or could affect function
- There’s suspicion of a foreign object in the wound
- The wound resulted from an animal or human bite
- You haven’t had a tetanus shot in the last 5 years
- Signs of infection develop (redness, swelling, warmth, pus)
Preventing Infections in Cuts and Puncture Wounds
Infection is a common complication of wounds. How can you reduce the risk of infection?
- Clean the wound promptly and thoroughly
- Use antiseptic solutions or antibacterial ointments
- Keep the wound covered with a clean, dry dressing
- Change the dressing regularly
- Avoid touching or picking at the wound
- Maintain good overall hygiene
Which types of wounds are more prone to infection?
- Bites (animal or human)
- Puncture wounds
- Crush injuries
- Dirty or contaminated wounds
- Wounds on the feet
- Wounds that are not promptly treated
Special Considerations for Different Types of Wounds
Venomous Snake Bites
Venomous snake bites require immediate medical attention. They can cause severe local tissue damage and potentially life-threatening complications. Key points to remember:
- Seek emergency medical care immediately
- Do not attempt to suck out the venom
- Keep the affected limb immobilized and lower than the heart
- Remove any constricting items (e.g., jewelry, tight clothing)
- Try to remember the snake’s appearance for identification purposes
Laceration Wounds
Lacerations are often irregular and jagged, making them prone to contamination. Special care is needed:

- Clean the wound thoroughly to remove debris and bacteria
- Assess the need for stitches based on depth and location
- Monitor for signs of infection during the healing process
Understanding Wound Closure Methods: Stitches and Alternatives
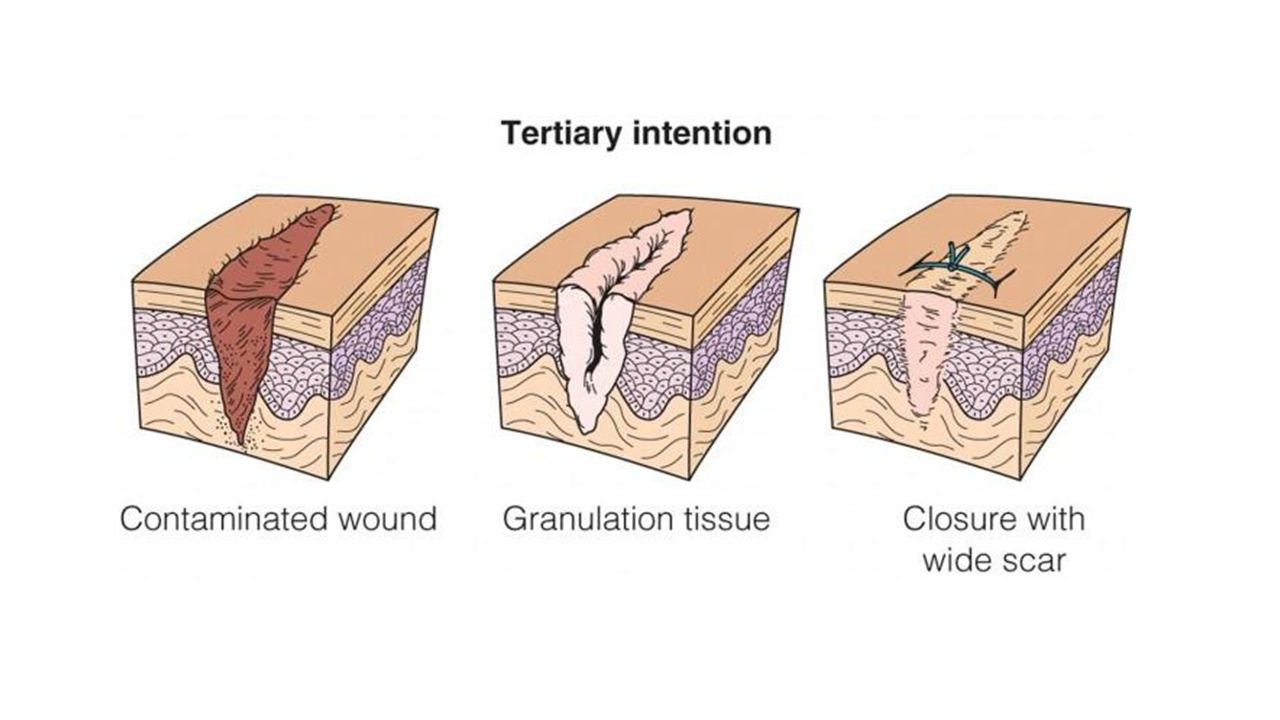
Proper wound closure is crucial for optimal healing and minimal scarring. When are stitches typically used?
- For cuts deeper than 1/4 inch
- On facial wounds
- When the wound reaches bone
- To minimize scarring in visible areas
How long do stitches typically remain in place?
- Face: 3-5 days
- High-stress areas (hands, elbows, knees): 10-14 days
- Other body areas: 7-10 days
Are there alternatives to traditional stitches? Yes, alternative wound closure methods include:
- Surgical staples
- Skin glue (liquid stitches)
- Steri-strips (adhesive skin closures)
- Butterfly closures
Long-Term Care and Complications of Cuts and Puncture Wounds
Proper wound care doesn’t end with initial treatment. Long-term considerations include:
Scar Management
How can you minimize scarring?

- Keep the wound moist and covered during healing
- Use silicone sheets or gels once the wound has closed
- Protect the healing area from sun exposure
- Massage the scar tissue (once fully healed) to improve appearance
Potential Complications
What complications can arise from untreated or improperly treated wounds?
- Infection (local or systemic)
- Tetanus
- Impaired function or mobility
- Chronic pain
- Keloid or hypertrophic scarring
When should you consult a doctor about potential complications?
- Persistent pain or swelling
- Signs of infection (redness, warmth, pus)
- Fever or chills
- Delayed healing
- Unusual or excessive scarring
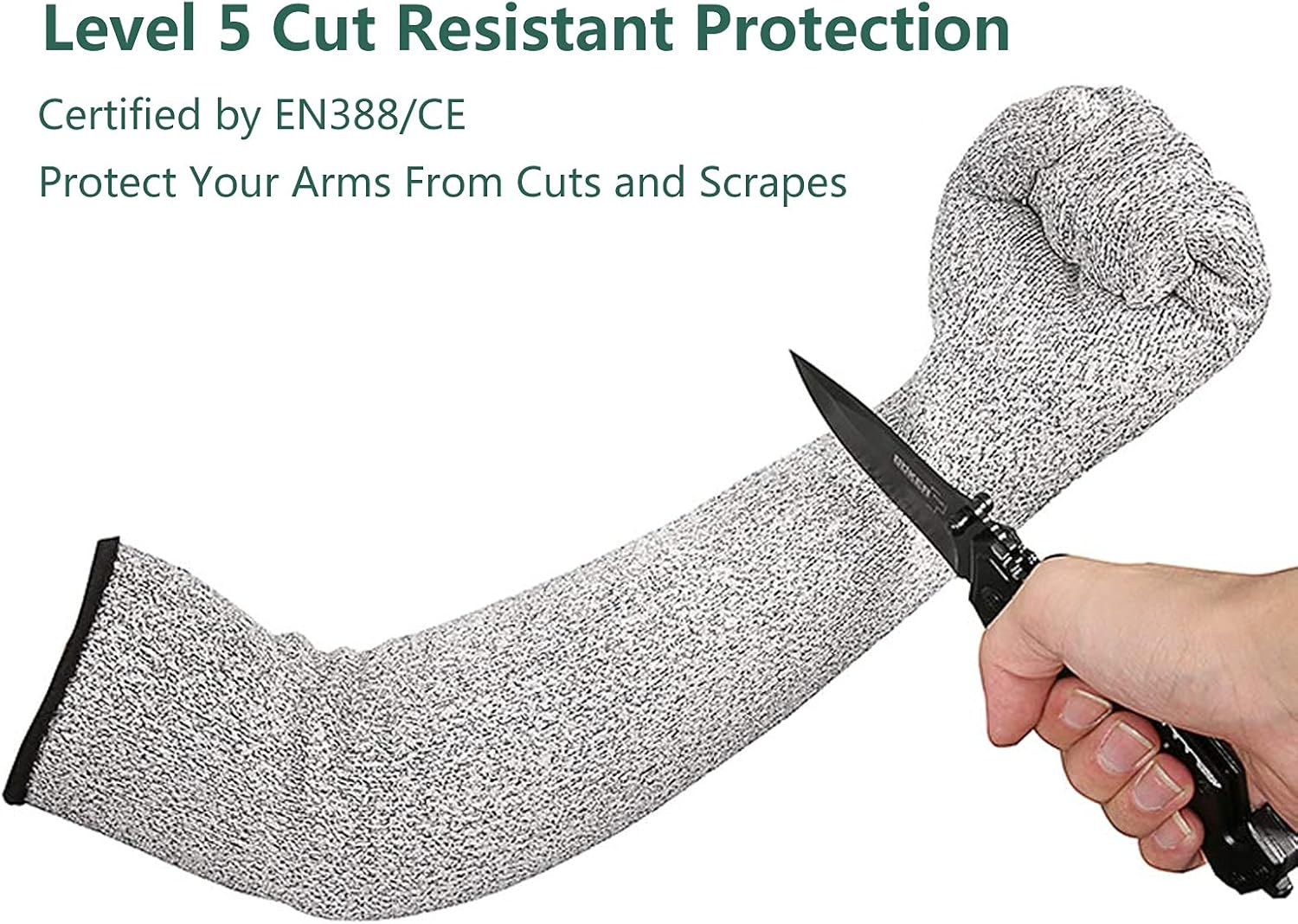
Prevention Strategies for Cuts and Puncture Wounds
While accidents happen, many cuts and puncture wounds are preventable. How can you reduce your risk?
- Use appropriate protective equipment when working with sharp tools or machinery
- Keep sharp objects stored safely and out of reach of children
- Be cautious when handling knives, scissors, and other sharp implements
- Wear shoes to protect feet from puncture wounds
- Use caution when walking on uneven or potentially hazardous surfaces
- Keep tetanus vaccinations up to date
By understanding the nature of cuts and puncture wounds, recognizing when to seek professional care, and following proper first aid and prevention techniques, you can minimize the risk of complications and promote optimal healing. Remember, when in doubt about the severity of a wound, it’s always best to consult a healthcare professional for guidance.
Cuts and puncture wounds Information | Mount Sinai
Wound – cut or puncture; Open wound; Laceration; Puncture wound
A cut is a break or opening in the skin. It is also called a laceration. A cut may be deep, smooth, or jagged. It may be near the surface of the skin, or deeper. A deep cut can affect tendons, muscles, ligaments, nerves, blood vessels, or bone.
A puncture is a wound made by a pointed object such as a nail, knife, or sharp tooth. Puncture wounds often appear to be on the surface, but may extend into the deeper tissue layers.
The essentials of a good first aid kit include a variety of bandages, medications, and equipment to stabilize injuries until proper medical attention can be administered.
A laceration is a wound that is produced by the tearing of soft body tissue. This type of wound is often irregular and jagged. A laceration wound is often contaminated with bacteria and debris from whatever object caused the cut. A puncture wound is usually caused by a sharp pointy object such as a nail, animal teeth, or a tack. This type of wound usually does not bleed excessively and can appear to close up. Puncture wounds are also prone to infection and should be treated appropriately.
Stitches are primarily used if the cut is more that a quarter inch deep, is on the face, or reaches bone. Stitches help hold the wound together so it can heal properly. Stitches are removed between 3 to 14 days after they are put depending upon which area of the body was injured. Stitches on the face can be removed within 3 to 5 days but areas of high stress such as hands, elbows, and knees must stay in 10 to 14 days.
Venomous snake bites are medical emergencies and require immediate attention. A venomous snake bite can cause severe local tissue damage and often requires follow-up care. The right anti-venom can save a person’s life. Even though most snakes are not venomous, avoid picking up or playing with any snake unless you have been properly trained.
A venomous snake bite can cause severe local tissue damage and often requires follow-up care. The right anti-venom can save a person’s life. Even though most snakes are not venomous, avoid picking up or playing with any snake unless you have been properly trained.
To treat a minor cut at home first wash your hands thoroughly with soap to avoid infection. Next wash the cut with mild soap and water.
Symptoms
Symptoms include:
- Bleeding
- Problems with function (movement) or feeling (numbness, tingling) below the wound site
- Pain
Infection may occur with some cuts and puncture wounds. The following are more likely to become infected:
- Bites
- Punctures
- Crush injuries
- Dirty wounds
- Wounds on the feet
- Wounds that are not promptly treated
First Aid
If the wound is bleeding severely, call your local emergency number, such as 911.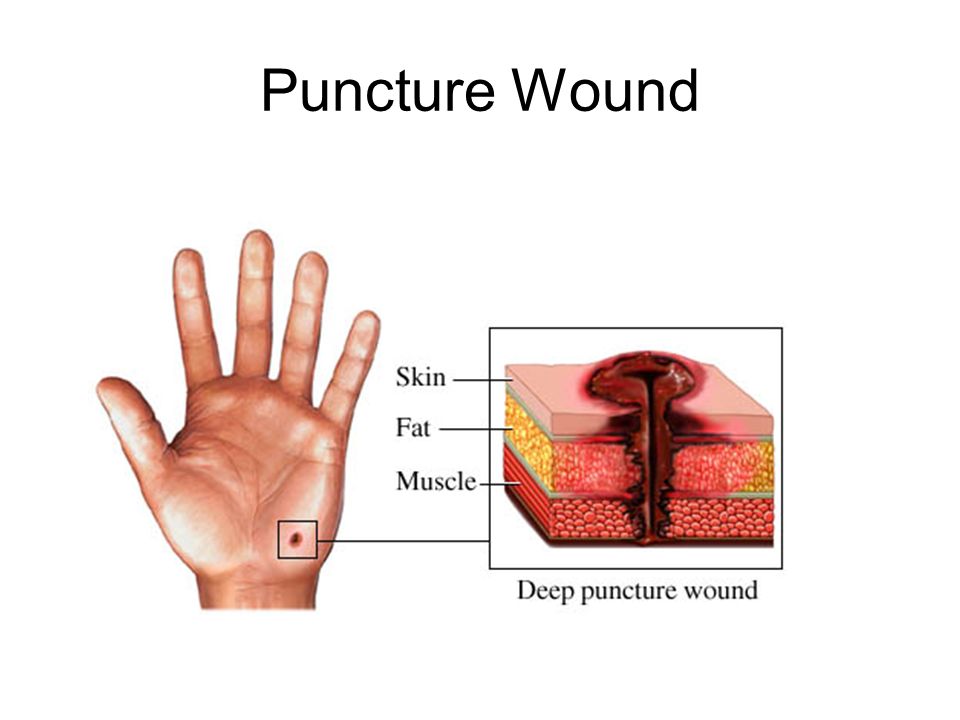
Minor cuts and puncture wounds can be treated at home. Prompt first aid can help prevent infection and thereby speed healing and reduce the amount of scarring.
Take the following steps:
FOR MINOR CUTS
- Wash your hands with soap or antibacterial cleanser to prevent infection.
- Then, wash the cut thoroughly with mild soap and water.
- Use direct pressure to stop the bleeding.
- Apply antibacterial ointment and a clean bandage that will not stick to the wound.
FOR MINOR PUNCTURES
- Wash your hands with soap or antibacterial cleanser to prevent infection.
- Rinse the puncture for 5 minutes under running water. Then wash with soap.
- Look (but do not poke around) for objects inside the wound. If found, don’t remove them. Go to your emergency or urgent care center.
- If you can’t see anything inside the wound, but a piece of the object that caused the injury is missing, also seek medical attention.
- Apply antibacterial ointment and a clean bandage that will not stick to the wound.

Do Not
- DO NOT assume that a minor wound is clean because you can’t see dirt or debris inside. Always wash it.
- DO NOT breathe on an open wound.
- DO NOT try to clean a major wound, especially after the bleeding is under control.
- DO NOT remove a long or deeply stuck object. Seek medical attention.
- DO NOT push or pick debris from a wound. Seek medical attention.
- DO NOT push body parts back in. Cover them with clean material until medical help arrives.
When to Contact a Medical Professional
Call 911 or your local emergency number if:
- The bleeding is severe or cannot be stopped (for example, after 10 minutes of pressure).

- The person cannot feel the injured area, or it doesn’t work right.
- The person is otherwise seriously injured.
Call your health care provider right away if:
- The wound is large or deep, even if the bleeding is not severe.
- The wound is more than a quarter inch (.64 centimeter) deep, on the face, or reaching the bone. Stitches may be needed.
- The person has been bitten by a human or animal.
- A cut or puncture is caused by a fishhook or rusty object.
- You step on a nail or other similar object.
- An object or debris is stuck. Do not remove it yourself.
- The wound shows signs of infection such as warmth and redness in the area, a painful or throbbing sensation, fever, swelling, a red streak extending from the wound, or pus-like drainage.
- You have not had a tetanus shot within the last 10 years.
Prevention
Keep knives, scissors, sharp objects, firearms, and fragile items out of the reach of children. When children are old enough, teach them to how to use knives, scissors, and other tools safely.
When children are old enough, teach them to how to use knives, scissors, and other tools safely.
Make sure you and your child are up to date on vaccinations. A tetanus vaccine is generally recommended every 10 years.
Ball JW, Dains JE, Flynn JA, Solomom BS, Stewart RW. Skin, hair, and nails. In: Ball JW, Dains JE, Flynn JA, Solomom BS, Stewart RW, eds. Seidel’s Guide to Physical Examination. 9th ed. . St Louis, MO: Elsevier; 2019:chap 9.
Lammers RL, Aldy KN. Principles of wound management. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges’ Clinical Procedures in Emergency Medicine and Acute Care. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 34.
Simon BC, Hern HG. Wound management principles. In: Walls RM, Hockberger RS, Gausche-Hill M, eds, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice.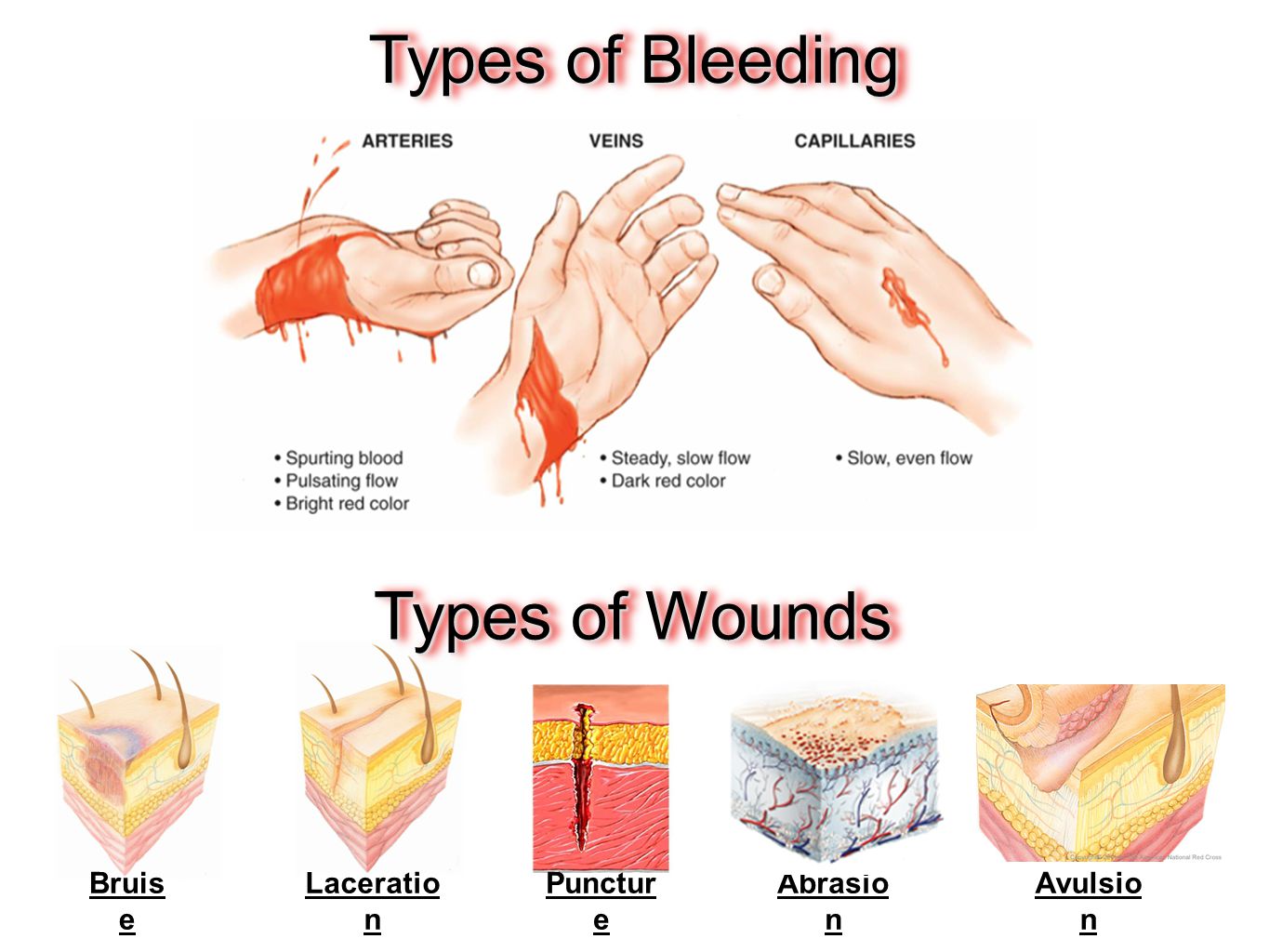 9th ed. Philadelphia, PA: Elsevier; 2018:chap 52.
9th ed. Philadelphia, PA: Elsevier; 2018:chap 52.
Last reviewed on: 11/13/2021
Reviewed by: Jesse Borke, MD, CPE, FAAEM, FACEP, Attending Physician at Kaiser Permanente, Orange County, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Puncture Wounds: Care Instructions | Kaiser Permanente
Skip Navigation
Overview
A puncture wound can happen anywhere on your body. These wounds tend to be narrower and deeper than cuts.
A puncture wound is usually left open instead of being closed. This is because a puncture wound can be easily infected, and closing it can make infection even more likely.
You will probably have a bandage over the wound.
The doctor has checked you carefully, but problems can develop later. If you notice any problems or new symptoms, get medical treatment right away.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor if you are having problems. It’s also a good idea to know your test results and keep a list of the medicines you take.
How can you care for yourself at home?
- Keep the wound dry for the first 24 to 48 hours. After this, you can shower if your doctor okays it. Pat the wound dry.
- Don’t soak the wound, such as in a bathtub. Your doctor will tell you when it’s safe to get the wound wet.
- If your doctor told you how to care for your wound, follow your doctor’s instructions.
 If you did not get instructions, follow this general advice:
If you did not get instructions, follow this general advice:- After the first 24 to 48 hours, wash the wound with clean water 2 times a day. Don’t use hydrogen peroxide or alcohol, which can slow healing.
- You may cover the wound with a thin layer of petroleum jelly, such as Vaseline, and a nonstick bandage.
- Apply more petroleum jelly and replace the bandage as needed.
- Prop up the sore area on pillows anytime you sit or lie down during the next 3 days. Try to keep it above the level of your heart. This helps reduce swelling.
- Avoid any activity that could cause your wound to get worse.
- Be safe with medicines. Read and follow all instructions on the label.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.

- If your doctor prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
When should you call for help?
Call your doctor now or seek immediate medical care if:
- You have new pain, or your pain gets worse.
- The wound starts to bleed, and blood soaks through the bandage. Oozing small amounts of blood is normal.
- The skin near the wound is cold or pale or changes color.
- You have tingling, weakness, or numbness near the wound.
- You have trouble moving the area near the wound.
- You have symptoms of infection, such as:
- Increased pain, swelling, warmth, or redness around the wound.

- Red streaks leading from the wound.
- Pus draining from the wound.
- A fever.
- Increased pain, swelling, warmth, or redness around the wound.
Watch closely for changes in your health, and be sure to contact your doctor if:
- The cut reopens.
- You do not get better as expected.
Where can you learn more?
Go to https://www.healthwise.net/patientEd
Enter S876 in the search box to learn more about “Puncture Wounds: Care Instructions”.
Soft tissue wounds – health articles
11/10/2022
What are soft tissue wounds?
Soft tissue injuries include injuries to the skin, mucous membrane, deep-lying tissues (subcutaneous tissue, muscles, etc.), as well as tendons, vessels and nerves. As a result of violation of the integrity of the skin, microbial contamination of the wound surface occurs, which can lead to the development of infection.
According to the damaging factor, wounds are divided into mechanical, thermal (burn) and chemical; on the instrument of injury – on wounds from blunt, sharp objects, tools and weapons, firearms and weapons; according to the nature of the damage, the wounds are classified into bruised, torn, combined, bitten, stab, cut, stab-cut, chopped, sawn, combined bullet, shot, fragmentation.
According to the depth of damage, superficial wounds are distinguished, located in different layers of the skin, and deep, passing in deeper tissues. Wounds of internal organs and joints that communicate with the external environment through a wound channel are called open wounds, and wounds whose wound channels pass through cavities or terminate in them are called penetrating wounds. Wounds of internal organs that do not communicate with the external environment are classified as closed.
Causes
Cut wounds result from the direct impact of a sharp weapon on the surface of the skin.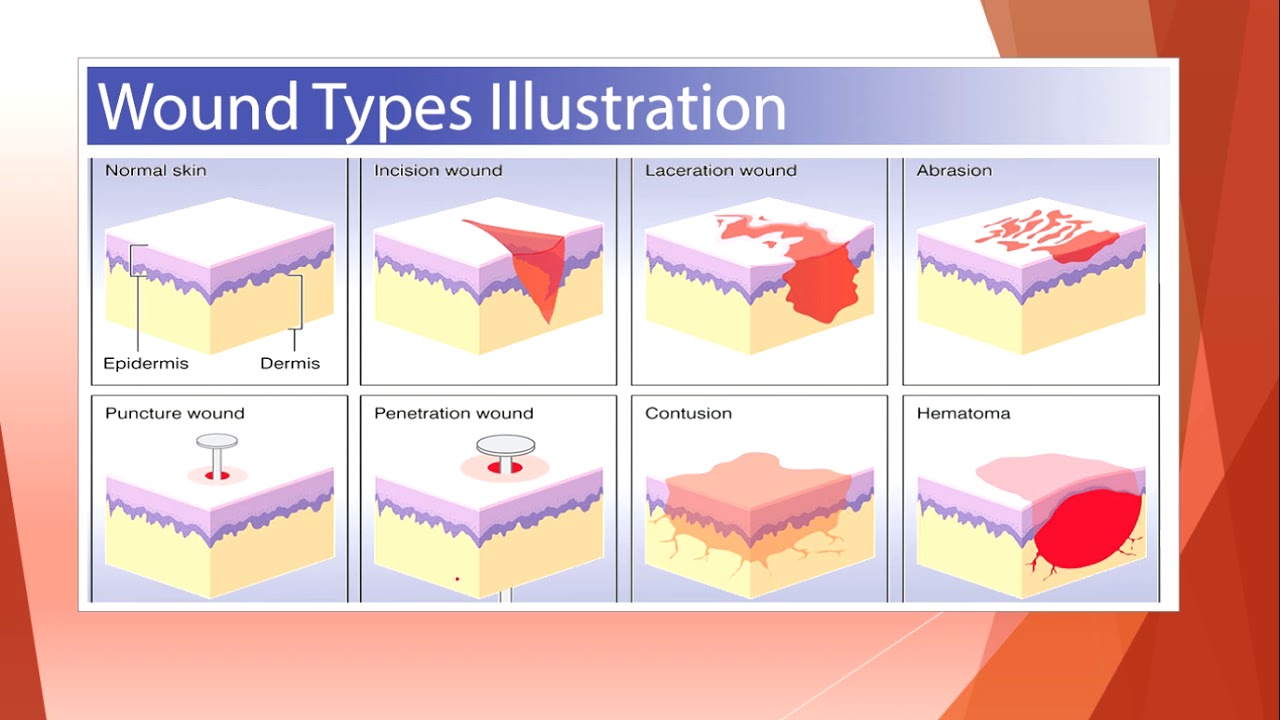
Chopping wounds are caused by lowering a sharp weapon on the skin at an angle.
Puncture wounds are the result of deep penetration of a sharp thin instrument. Possible injury to the cavities or joints.
Contusion wounds occur when some part of the body comes into contact with a hard obstacle and there is a solid support in the form of the bones of the skull or other bone.
Crushed, crushed wounds are formed due to the impact of a blunt instrument with a wide surface when opposed to a solid support.
Bite wounds. As a result of a bite by an animal or a person, highly virulent causative agents of wound infection can enter the wound.
Symptoms
A closed injury can be suspected by knowing the mechanism of injury (eg, blunt force impact) and by the presence of one or more of the following: bruising, swelling, pain.
Some signs suggest the nature of the injury. For example, swelling and deformity may indicate a closed fracture. A bruise on the head, bloody discharge from the nose, ears and mouth – an injury to the cervical spine or brain is possible. Bruises on the chest, deformation, violation of symmetry – a chest injury is possible with damage to the ribs and sternum. Respiratory failure may indicate lung injury. Large bruises on the abdomen – possible injury to the internal organ.
Bruises on the chest, deformation, violation of symmetry – a chest injury is possible with damage to the ribs and sternum. Respiratory failure may indicate lung injury. Large bruises on the abdomen – possible injury to the internal organ.
Signs of a wound vary depending on the type and depth of tissue damage. As a rule, any damage accompanies pain, possibly a violation of the integrity of the skin, as well as bleeding.
Diagnosis
For small, superficial wounds that are not accompanied by general symptoms, the diagnosis is made on the basis of the clinical picture. A detailed study is carried out during the primary treatment of the wound. With extensive and deep wounds with a violation of the general condition, additional studies are needed, the list of which is determined taking into account the location of the damage. In case of injuries in the chest area, a chest x-ray is prescribed, in case of damage to the abdomen, an x-ray of the abdominal cavity, ultrasound or laparoscopy, etc. If a violation of the integrity of blood vessels and nerves is suspected, a consultation of a neurosurgeon and a vascular surgeon is required.
If a violation of the integrity of blood vessels and nerves is suspected, a consultation of a neurosurgeon and a vascular surgeon is required.
Treatment
First medical aid consists of primary surgical treatment of the wound, during which foreign bodies are removed from the wound, bleeding stops, the wound is washed with antiseptics, and non-viable tissues are excised. The issue of prevention of tetanus and rabies (if the wound is bitten) is also being resolved. Wounds with a pronounced inflammatory process are not sutured, they are drained. An infected wound heals by secondary intention. Dressings and drains are changed daily. General treatment consists of anti-inflammatory therapy, the introduction of hemostatic agents, painkillers.
In case of profuse blood loss, the issue of compensating the volume of circulating blood (CBV) is solved, blood substitutes, blood components are introduced. Subsequently, with severe cicatricial contractures and deformities, a restorative operation can be repeated.
Most superficial wounds do not bleed much. Therefore, help consists in bandaging the wound. Before this procedure, the edges are smeared with an antiseptic, making sure that it does not get into the wound.
The wound is covered with a sterile dressing and bandaged. If the edges of the wound are strongly dispersed, before applying the bandages, they must be brought together (but not until they close) and fixed in this position with 2-3 strips of adhesive tape.
The wound must not be washed with water (risk of infection), nor with alcohol or tincture of iodine. The disinfectant solution, getting into the wound, causes the death of damaged cells, and also causes significant pain. No ointment should be applied to the wound, and cotton should not be placed directly into the wound.
Vitamin therapy should not be forgotten. Vitamin deficiency sharply slows down reparative (restorative) processes.
To accelerate wound healing, proper nutrition of patients is important, especially those who have undergone traumatic shock, severe infection or major surgery. They need a complete diet with an increased amount of protein and vitamins. Physiotherapy exercises are indicated primarily for purulent wounds of the upper extremities. Physiotherapeutic procedures play an important role: UV, UHF, etc.
They need a complete diet with an increased amount of protein and vitamins. Physiotherapy exercises are indicated primarily for purulent wounds of the upper extremities. Physiotherapeutic procedures play an important role: UV, UHF, etc.
Complications of wounds – Clinic 29
Wounds can be accompanied by a variety of complications both immediately after the infliction of wounds, and in the long term. These include:
- Gray — accumulation of exudate in the residual cavity of the wound. Its infection leads to suppuration of the wound. Requires timely evacuation.
- Wound hematoma – formed due to incomplete stop of bleeding. Serves as a potential source of infection. A tense hematoma compresses the surrounding tissues and leads to their ischemia. The hematoma must be removed by puncture or revision of the wound.
- Necrosis of the surrounding tissues – develop when blood supply is disturbed in the corresponding area due to tissue trauma during surgery or improper suturing.
 Moist necrosis of the skin must be excised because of the danger of deep accumulations of pus. Superficial dry skin necrosis is not removed, as they perform a protective function.
Moist necrosis of the skin must be excised because of the danger of deep accumulations of pus. Superficial dry skin necrosis is not removed, as they perform a protective function. -
Suppuration with the subsequent development of abscesses, phlegmon
– their development is facilitated by a high level of contamination (wound contamination) and high virulence (aggressiveness) of the microflora that got into the wound, the presence of foreign bodies in the wound, necrosis, accumulations of fluid or blood, chronic disturbance of local blood supply, general factors affecting the course of the wound process, as well as late surgical treatment. It is the patient’s refusal to seek timely specialized care that can lead to serious complications.
The most common development of pyogenic (pyogenic) wound infection occurs on the 3-5th day after injury, less often – at a later date – on the 13-15th day. Anaerobic infection can develop very quickly, with fulminant forms it manifests itself within a few hours after the injury. The first symptoms are swelling, redness and pain. Increasing pain in the area of the wound is an early, but, unfortunately, often ignored sign of an infection.
The first symptoms are swelling, redness and pain. Increasing pain in the area of the wound is an early, but, unfortunately, often ignored sign of an infection.
Adequate surgical treatment is required: the wound is opened, pus is removed, thoroughly washed, after which, according to indications, it is drained with tubular drainage and packed with a material with sorption properties. After cleansing the wound and the appearance of granulation tissue, secondary sutures are applied or the edges of the wound are pulled together with adhesive tape.
- Wound dehiscence may occur when the applied external forces exceed its strength. Most often, the divergence of the skin edges of the wound occurs within the first month after its suturing, precisely during the period of time when the sutures have already been removed, and the formation of cross-links of collagen fibrils has not been completed. Even with a normal metabolism, the postoperative scar acquires only 35% of its original strength in one month and never becomes stronger than the tissue it replaced.
 The divergence of the edges of the wound is eliminated by surgery.
The divergence of the edges of the wound is eliminated by surgery. - Suppuration of postoperative wounds . Among all postoperative complications, surgical infection ranks first and accounts for 32-75%. After planned surgical interventions, infectious complications occur in 6.5% of cases, after emergency – in more than 12%
Manifestations of postoperative wound infection do not have specific symptoms relative to any other wound infection. Among the local symptoms, there are edema and hyperemia (redness) or cyanosis (cyanosis) of the skin up to the development of necrosis, severe pain at rest and on palpation in the wound area, fluctuations in places of the greatest accumulation of exudate, wound discharge, divergence of the edges of the wound, slowing down of reparative processes in wound.
Patients debilitated by major surgery, comorbidities, or trauma may have mild symptoms.
In case of total suppuration of the wound, the sutures are completely removed, the edges of the wound are parted, exudate or hematoma is evacuated, non-viable tissues are excised, pockets and streaks are opened.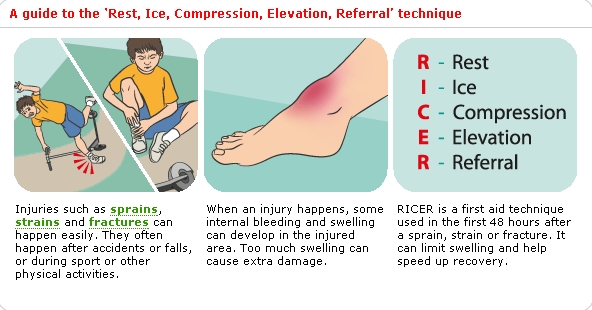


 If you did not get instructions, follow this general advice:
If you did not get instructions, follow this general advice:

 Moist necrosis of the skin must be excised because of the danger of deep accumulations of pus. Superficial dry skin necrosis is not removed, as they perform a protective function.
Moist necrosis of the skin must be excised because of the danger of deep accumulations of pus. Superficial dry skin necrosis is not removed, as they perform a protective function. The divergence of the edges of the wound is eliminated by surgery.
The divergence of the edges of the wound is eliminated by surgery.