Symptoms of ringworm on face. Ringworm on Face: Symptoms, Treatments, and Natural Remedies
What are the symptoms of ringworm on the face. How can you treat ringworm effectively at home. What natural remedies can help alleviate ringworm symptoms. Is ringworm contagious and how can you prevent its spread. What over-the-counter medications are effective against ringworm. When should you seek medical attention for facial ringworm. How long does it take for ringworm to clear up with proper treatment.
Understanding Facial Ringworm: Causes and Symptoms
Facial ringworm, medically known as tinea faciei, is a fungal infection that affects the skin on the face. Despite its name, ringworm is not caused by a worm but by a group of fungi called dermatophytes. These fungi thrive on the dead tissues of the skin, hair, and nails.
The primary symptoms of facial ringworm include:
- Red, scaly patches on the skin
- Circular or ring-shaped lesions
- Itching and irritation
- Slightly raised borders around the affected area
- Possible hair loss in the affected area (if present on bearded areas)
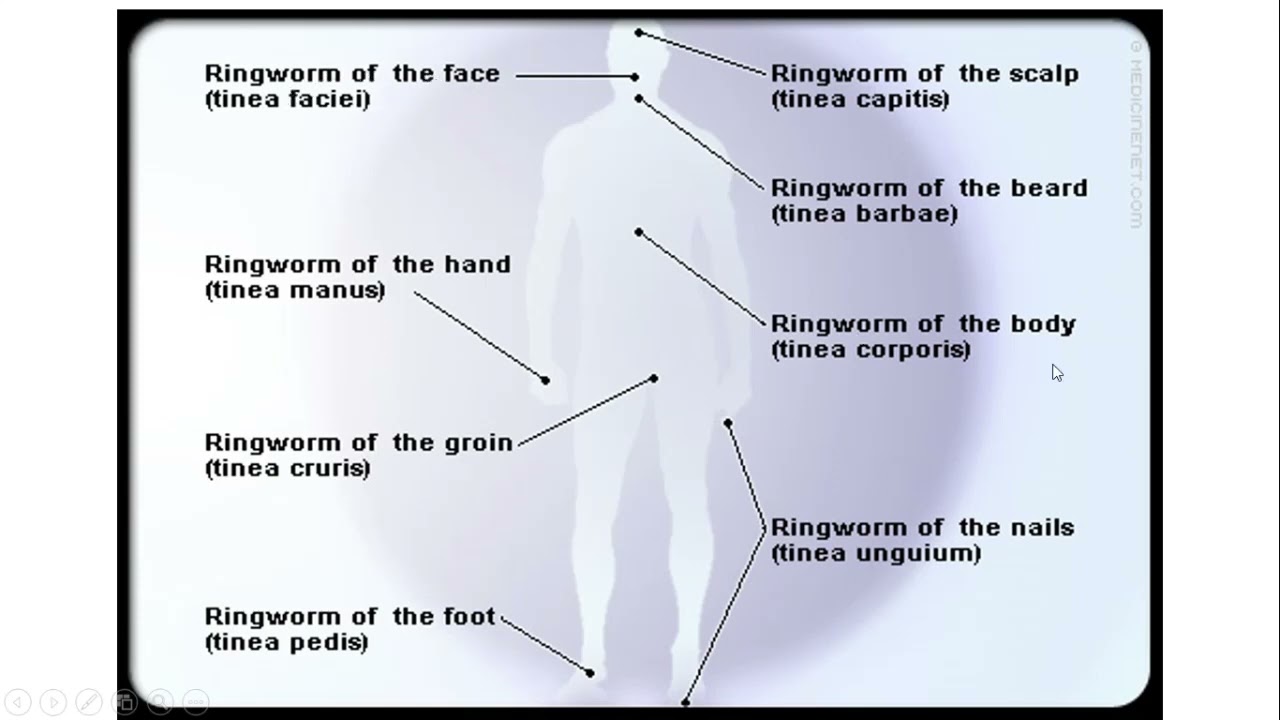
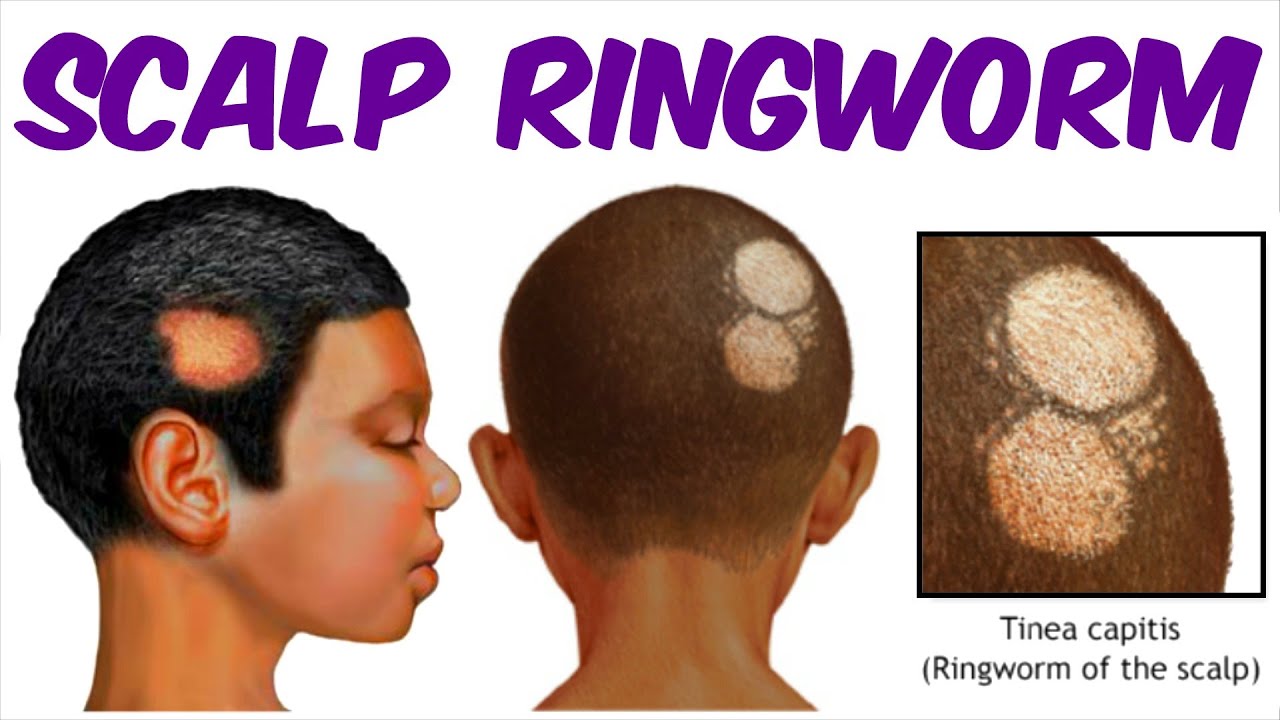
Are there different types of ringworm? Indeed, ringworm can affect various parts of the body, each with its own name. When it occurs on the face, it’s called tinea faciei. Other common types include tinea corporis (body), tinea capitis (scalp), tinea cruris (groin, also known as jock itch), and tinea pedis (feet, commonly called athlete’s foot).

Home Remedies for Treating Facial Ringworm
While medical treatments are available, many people find success with home remedies. Here are some effective options:
Apple Cider Vinegar
Apple cider vinegar is renowned for its antifungal properties. To use it:
- Soak a cotton ball in undiluted apple cider vinegar
- Apply it to the affected area
- Repeat this process three times daily
Does apple cider vinegar sting when applied to ringworm? It may cause a slight tingling sensation, but if you experience severe discomfort, discontinue use and consult a healthcare provider.
Tea Tree Oil
Tea tree oil is a powerful natural antifungal agent. Here’s how to use it:
- Apply a few drops of tea tree oil directly to the affected area using a cotton swab
- Repeat this application 2-3 times daily
- If you have sensitive skin, dilute the tea tree oil with a carrier oil like coconut oil
Can tea tree oil be used on all skin types? While generally safe, some individuals may experience skin irritation. Always perform a patch test before applying it to larger areas.

Coconut Oil
Coconut oil offers both antifungal and moisturizing benefits. To use:
- Warm a small amount of coconut oil until it liquefies
- Apply directly to the affected area
- Repeat at least three times daily
Is coconut oil effective against all types of ringworm? While it can be beneficial for many cases, severe or persistent infections may require additional treatment.
Over-the-Counter Treatments for Facial Ringworm
For those who prefer pharmaceutical options, several over-the-counter antifungal treatments are available:
- Clotrimazole (Lotrimin, Mycelex)
- Miconazole (Micatin, Monistat-Derm)
- Terbinafine (Lamisil)
- Ketoconazole (Nizoral)
These medications typically come in cream, ointment, or gel form and should be applied as directed on the packaging.
How long should you use over-the-counter treatments? Most treatments require application for 2-4 weeks, even if symptoms improve sooner. Always complete the full course of treatment to prevent recurrence.
Preventing the Spread of Ringworm
Ringworm is highly contagious and can spread through direct contact with infected individuals or contaminated objects. To prevent its spread:

- Wash hands thoroughly after touching the affected area
- Avoid sharing personal items like towels, combs, or clothing
- Keep the infected area clean and dry
- Wash bedding and clothing in hot water
- Avoid scratching the affected area
Can pets transmit ringworm to humans? Yes, pets can be carriers of the fungi that cause ringworm. If you suspect your pet has ringworm, consult a veterinarian promptly.
When to Seek Medical Attention
While many cases of facial ringworm can be treated at home, certain situations warrant professional medical care:
- The infection spreads or worsens despite treatment
- You develop a fever or other signs of a secondary infection
- The rash is extremely painful or causes significant discomfort
- You have a weakened immune system
- The infection persists for more than two weeks with home treatment
What treatments might a doctor prescribe? For severe or persistent cases, a doctor may prescribe oral antifungal medications such as fluconazole or itraconazole.
Natural Supplements and Dietary Changes to Support Treatment
While topical treatments are crucial, supporting your body’s immune system can aid in fighting the infection. Consider the following:
Probiotics
Probiotics can help balance the body’s microbiome, potentially making it less hospitable for fungal overgrowth. Consider incorporating probiotic-rich foods like yogurt, kefir, or sauerkraut into your diet, or taking a high-quality probiotic supplement.
Garlic
Garlic has natural antifungal properties. You can consume it raw, cooked, or in supplement form. However, consult with a healthcare provider before starting any new supplement regimen.
Dietary Adjustments
Some dietary changes that may help include:
- Reducing sugar intake, as fungi thrive on sugar
- Increasing consumption of antifungal foods like coconut oil, garlic, and oregano
- Ensuring adequate protein intake to support immune function
Can dietary changes alone cure ringworm? While a healthy diet supports overall immune function, it’s not a substitute for topical or oral antifungal treatments in most cases.
Understanding the Healing Process
Recovering from facial ringworm takes time and patience. Here’s what to expect:
- Initial improvement: You may notice reduced itching and redness within a few days of starting treatment
- Gradual healing: The rash typically begins to clear up within 2-4 weeks of consistent treatment
- Complete resolution: Full clearance of the infection may take up to 6 weeks in some cases
Why does ringworm sometimes seem to get worse before it gets better? As the fungi die off, they can release substances that temporarily increase inflammation. This is normal and usually subsides as treatment continues.
Monitoring for Recurrence
Even after the infection appears to have cleared, it’s important to continue treatment for the full recommended duration. This helps ensure all fungal spores are eliminated, reducing the risk of recurrence.
How can you prevent ringworm from coming back? Maintain good hygiene practices, avoid sharing personal items, and keep your skin clean and dry, especially in warm, humid conditions where fungi thrive.
Addressing Complications and Special Considerations
While facial ringworm is typically manageable, certain factors can complicate treatment or increase the risk of complications:

Facial Hair and Ringworm
For individuals with beards or other facial hair, ringworm can be particularly challenging to treat. The fungus can infect hair follicles, leading to a condition called tinea barbae. This may require more aggressive treatment, including oral antifungals.
Ringworm in Children
Children are particularly susceptible to ringworm due to their frequent close contact with others and their developing immune systems. When treating children:
- Use age-appropriate treatments as recommended by a pediatrician
- Teach proper hygiene habits to prevent spread and recurrence
- Monitor for any adverse reactions to treatments
Are there any special considerations for treating ringworm in infants? Infants have particularly sensitive skin, so it’s crucial to consult a pediatrician before applying any treatments, even over-the-counter options.
Ringworm and Makeup
For those who regularly wear makeup, facial ringworm presents unique challenges:
- Avoid applying makeup to the affected area until it has fully healed
- Discard and replace any makeup products that may have come into contact with the infected area
- Clean makeup brushes and applicators thoroughly
Can wearing makeup worsen ringworm? Makeup can potentially trap moisture and irritate the affected skin, potentially exacerbating the infection or slowing healing.

Long-Term Skin Care After Ringworm
After successfully treating facial ringworm, it’s important to implement a skin care routine that promotes overall skin health and prevents future infections:
Gentle Cleansing
Use a mild, non-irritating cleanser to keep your skin clean without stripping its natural oils. Avoid harsh scrubs or exfoliants until the skin has fully healed.
Moisturizing
Keep your skin well-moisturized to maintain its barrier function. Look for non-comedogenic moisturizers that won’t clog pores.
Sun Protection
The affected area may be more sensitive to sun damage after healing. Use a broad-spectrum sunscreen daily to protect your skin.
Regular Check-ups
Monitor your skin for any signs of recurrence or other skin issues. If you’re prone to fungal infections, consider regular check-ups with a dermatologist.
How long after treatment should you wait before resuming your normal skincare routine? It’s best to wait until the skin has fully healed and shows no signs of inflammation, which typically takes about 2-4 weeks after the infection has cleared.

Research and Future Treatments
The field of dermatology is continually evolving, with ongoing research into more effective treatments for fungal skin infections like ringworm. Some areas of current interest include:
Novel Antifungal Compounds
Researchers are exploring new antifungal agents that may be more effective or have fewer side effects than current treatments.
Nanotechnology
The use of nanoparticles to deliver antifungal medications more effectively is an area of active research.
Probiotics for Skin Health
Studies are investigating the potential of topical probiotics to promote a healthy skin microbiome and prevent fungal overgrowth.
What promising developments are on the horizon for ringworm treatment? While specific breakthroughs are difficult to predict, the trend is towards more targeted, personalized treatments that work in harmony with the body’s natural defenses.
Psychological Impact of Facial Ringworm
While often viewed primarily as a physical condition, facial ringworm can have significant psychological effects, especially when it occurs on visible areas like the face. Some individuals may experience:

- Decreased self-esteem
- Social anxiety
- Depression
- Stress about potential spread or recurrence
It’s important to address these psychological aspects alongside the physical treatment. Some strategies include:
- Educating yourself about the condition to reduce anxiety
- Joining support groups or online communities for individuals dealing with skin conditions
- Practicing stress-reduction techniques like meditation or yoga
- Seeking professional counseling if the emotional impact is significant
How can you maintain a positive outlook while dealing with facial ringworm? Focus on the fact that ringworm is treatable and temporary. Engage in activities you enjoy and surround yourself with supportive people who understand your situation.
Global Perspective on Ringworm
Ringworm is a global health issue, with prevalence varying widely across different regions and populations. In some areas, particularly in tropical and subtropical climates, ringworm is significantly more common due to environmental factors that promote fungal growth.

Socioeconomic Factors
In many parts of the world, limited access to healthcare, overcrowded living conditions, and lack of education about prevention contribute to higher rates of ringworm and other fungal infections.
Cultural Practices
Certain cultural practices, such as sharing personal items or specific grooming habits, can influence the spread of ringworm in different communities.
Global Health Initiatives
Various global health organizations are working to improve education, access to treatment, and living conditions to reduce the prevalence of fungal skin infections worldwide.
How do global efforts to combat ringworm impact individual cases? While global initiatives may not directly affect your personal treatment, they contribute to overall awareness, research funding, and the development of new treatments that may benefit individuals in the future.
In conclusion, facial ringworm, while uncomfortable and potentially distressing, is a treatable condition with a variety of effective options available. By understanding the causes, symptoms, and treatment options, individuals can take proactive steps to manage the infection and prevent its spread. Whether opting for home remedies, over-the-counter treatments, or seeking professional medical care, consistent application and patience are key to successful treatment. Remember to consider not just the physical aspects of the condition, but also its potential psychological impact. With proper care and attention, most cases of facial ringworm can be effectively resolved, allowing individuals to regain clear, healthy skin.

9 Ways to Treat Symptoms
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.
Was this helpful?
A few home remedies, such as essential oils, aloe vera, and antifungal medications, may help clear a ringworm infection. It’s important to be careful, as it is highly contagious.
It’s important to be careful, as it is highly contagious.
Despite its name, ringworm isn’t actually caused by a worm or any type of living parasite. Instead, it’s a skin condition that’s caused by a type of fungus called tinea. It lives on the dead tissues of the skin, including your nails and hair.
Ringworm causes a red, scaly, itchy patch on your skin. Over time, it takes the shape of a circle or a ring (or several rings). This is where the name “ringworm” comes from.
You can get ringworm on your skin and nails. It’s most common on the arms and the scalp, but you can get it anywhere on your skin, including your face. If ringworm develops in different areas, it may be called by a different name. For example, when it affects the groin area, it’s referred to as jock itch. When it affects the area between your toes, it’s called athlete’s foot.
Fortunately, ringworm can respond well to home treatments.
A note about essential oils
Several essential oils, listed below, can help treat ringworm. When using essential oils, test that you’re not allergic to them first. Dilute the essential oil by adding three to five drops per ounce of a carrier oil such as olive or mineral oil. Then, rub it onto healthy skin in an area the size of a dime. If you have no reaction in 12 to 24 hours, it should be safe to use on your infection.
When using essential oils, test that you’re not allergic to them first. Dilute the essential oil by adding three to five drops per ounce of a carrier oil such as olive or mineral oil. Then, rub it onto healthy skin in an area the size of a dime. If you have no reaction in 12 to 24 hours, it should be safe to use on your infection.
When you have ringworm, you need to keep the area as clean as possible. This helps prevent the further spread of the rash and helps keep the affected area under control.
Wash the affected area with water and antibacterial soap daily before applying other home remedies on top of it. Dry the area thoroughly after showering, as moisture makes it easier for the fungus to spread.
Pine and coal-tar soap are older home remedies that might be an option, but they can be irritating to sensitive skin.
Apple cider vinegar has strong antifungal properties, so it may help treat ringworm when applied topically to the affected area. To use it, soak a cotton ball in undiluted apple cider vinegar and brush the cotton ball over your skin. Do this three times per day.
Do this three times per day.
Native Australians conventionally used tea tree oil as an antifungal and antibacterial, and it’s used today for the same purposes. It can be extremely effective in treating fungal skin infections.
Apply tea tree oil directly to the affected area two or three times per day with a cotton ball or swab. If you have sensitive skin, it may be helpful to dilute the tea tree oil in a carrier oil like coconut oil, which has its own antifungal benefits.
Coconut oil has both microbial and antifungal properties that can help treat ringworm infections. It’s an extremely effective topical home remedy for ringworm and infections with other fungi, like candida. Because it’s easy to apply to the scalp and an effective hair conditioner, coconut oil could be an ideal treatment for scalp ringworm.
To use it, warm the coconut oil either in the microwave or in your hand until it becomes liquid, then apply it directly to the affected area. It will absorb into the skin quickly. Apply it at least three times daily.
Apply it at least three times daily.
Turmeric has numerous health benefits, including antibacterial and anti-inflammatory properties. It’s also an effective antifungal that inhibits growth.
Combine fresh-ground turmeric, or the turmeric spice, with a small amount of water and mix until it becomes a paste. Apply it to your skin and leave it on until it dries. You can also drink turmeric water or turmeric tea daily to get the internal benefits.
Aloe vera has long been used as a natural remedy for both bacterial and fungal infections, and ringworm is no exception. Aloe vera can treat the ringworm and may soothe symptoms of itchiness, inflammation, and discomfort. You can find ointments with aloe vera or apply aloe vera gel directly to the area. Do this at least three times daily.
Oregano essential oil may be a more powerful antifungal than other commercial products that are available, and can inhibit and treat fungal skin infections, including athlete’s foot and ringworm.
Oregano oil is an extract that you can purchase online or at stores like GNC. Mix a few drops with a carrier oil like olive or coconut oil, and apply it to the affected area three times per day.
Lemongrass oil extract, and to a slightly lesser extent lemongrass tea, both have antifungal properties that can be helpful in treating fungal skin infections like ringworm.
To use lemongrass oil, mix a few drops of lemongrass oil with a carrier oil. Apply it directly to the skin twice per day. You can also apply a brewed tea bag directly to the ringworm.
Licorice has strong antimicrobial properties, and research has found that the extracts of licorice could be used as alterative treatment for fungal infections.
Mix eight teaspoons of powdered licorice with a cup of water and bring to a boil. Once boiling, reduce the heat and simmer for ten minutes. Stir until it makes a paste. When the mixture is cool enough to touch, apply the paste to the affected area twice daily. Leave it on for at least ten minutes.
Leave it on for at least ten minutes.
While all-natural ingredients are great, sometimes you need something a little stronger. OTC antifungal topical remedies are available and effective for mild cases of ringworm. Look for the active ingredients clotrimazole and terbinafine. You can apply these ointments twice per day.
You should see your doctor if your symptoms don’t clear up or don’t respond to treatment within two weeks. You should also go to the doctor if you’re in a position that could likely spread it to others, such as if you’re a teacher.
In some cases, ringworm won’t respond to home remedies or OTC treatments. Your doctor will write you a prescription for an antifungal topical ointment or an oral medication.
Ringworm is highly contagious. While it’s most commonly spread from skin-to-skin contact, you can also catch it from touching something that someone with ringworm touched.
To prevent ringworm, you should keep your skin clean and dry. Immediately after the gym or shower, put on clean, dry clothes.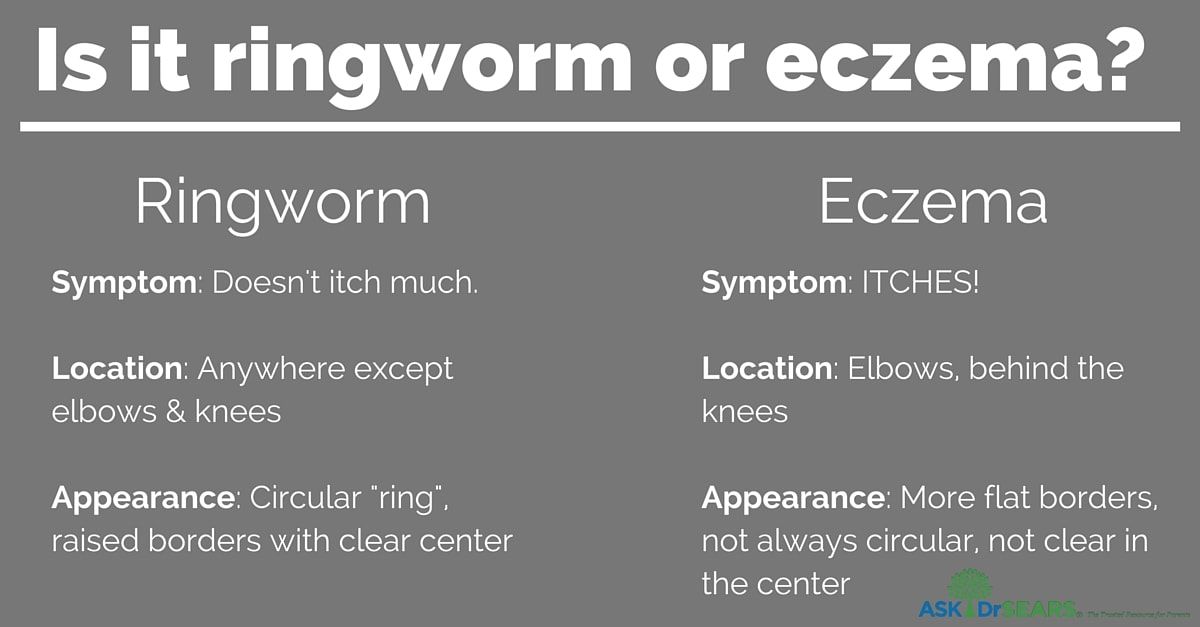 Avoid physical contact with someone who has ringworm. You should always wear shoes, like flip-flops, in public showers.
Avoid physical contact with someone who has ringworm. You should always wear shoes, like flip-flops, in public showers.
Most cases of ringworm clear up within two weeks.
Tinea faciei | DermNet
Created 2003.
toc-icon
What is tinea faciei?
Tinea faciei is the name used for infection of the face with a dermatophyte fungus. It does not include infection of the beard and moustache area, which is called tinea barbae. Tinea faciei is uncommon and often misdiagnosed at first.
Tinea faciei can be due to an anthropophilic (human) fungus such as Trichophyton rubrum (T rubrum). Infection often comes from the feet (tinea pedis) or nails (tinea unguium) originally. Zoophilic (animal) fungi such as Microsporum canis (M canis), from cats and dogs, and T verrucosum, from farm cattle, are also common.
Tinea faciei
Tinea faciei
tinea faciei
tinea faciei
tinea faciei
Kerion
tinea faciei
Clinical features of tinea faciei
Tinea faciei resembles tinea corporis (ringworm). It may be acute (sudden onset and rapid spread) or chronic (slow extension of a mild, barely inflamed, rash). There are round or oval red scaly patches, often less red and scaly in the middle or healed in the middle. It is frequently aggravated by sun exposure. It may also present as a kerion (fungal abscess).
It may be acute (sudden onset and rapid spread) or chronic (slow extension of a mild, barely inflamed, rash). There are round or oval red scaly patches, often less red and scaly in the middle or healed in the middle. It is frequently aggravated by sun exposure. It may also present as a kerion (fungal abscess).
Tinea faciei is often misdiagnosed as a non-fungal condition such as:
- Atopic dermatitis
- Seborrhoeic dermatitis
- Psoriasis
- Rosacea
- Actinic keratoses
- Contact allergic dermatitis
- Perioral dermatitis
- Cutaneous lupus erythematosus
- Polymorphous light eruption
Misdiagnosis is particularly common in those treated with topical steroids or oral steroids (tinea incognita).
Diagnosis of tinea faciei
The diagnosis of tinea faciei is confirmed by microscopy and culture of skin scrapings.
Treatment of tinea faciei
Tinea faciei is usually treated with topical antifungal agents, but if the treatment is unsuccessful, oral antifungal medicines may be considered, including terbinafine and itraconazole.
On DermNet NZ
- Tinea
- Introduction to fungal infections
- Laboratory tests for fungal infections
- Treatment of fungal infections
Other websites
- Tinea faciei — Medscape Reference
Books about skin diseases
- Books about the skin
- Dermatology Made Easy book
Pink lichen in a child. What is pink lichen in a child?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Pink lichen in a child is a skin disease of an infectious-allergic nature, which belongs to the group of papular-squamous dermatoses. Pathology is manifested by itchy red rashes on the trunk, face and scalp, which are covered with thin scales and resemble tissue paper. To diagnose the disease, a thorough examination of the skin is carried out, laboratory tests are prescribed (hemogram and biochemical blood test, microscopy of scales, serological studies). Treatment includes rational care of damaged skin, local remedies with hormones and antihistamines to relieve itching and discomfort.
Pathology is manifested by itchy red rashes on the trunk, face and scalp, which are covered with thin scales and resemble tissue paper. To diagnose the disease, a thorough examination of the skin is carried out, laboratory tests are prescribed (hemogram and biochemical blood test, microscopy of scales, serological studies). Treatment includes rational care of damaged skin, local remedies with hormones and antihistamines to relieve itching and discomfort.
ICD-10
L42 Pityriasis rosea [Gibera]
- Causes
- Pathogenesis
- Symptoms
- Complications
- Diagnostics
- Treatment of rosacea in a child
- Prognosis and prevention
- Prices for treatment
General
Pityriasis rosea (Giber’s disease, pityriasis rosea, roseola scaly) is clinically classified in dermatology as papulosquamous dermatoses, in the same group as psoriasis. Pathology accounts for up to 3.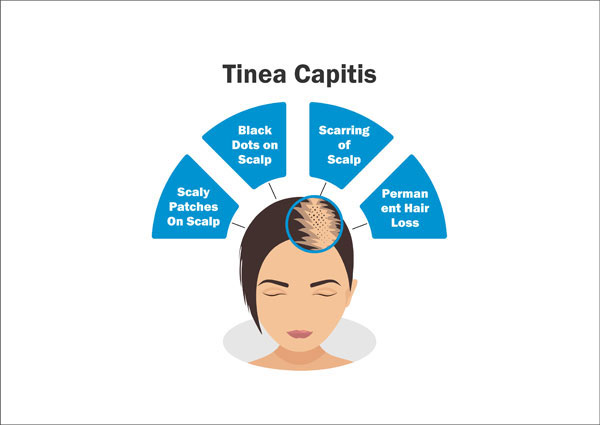 5% of all cases of childhood dermatoses. It occurs with the same frequency in boys and girls, the peak incidence occurs at the age of 10-18 years. Pink lichen rarely affects younger schoolchildren and preschoolers, and cases of the disease in children under 2 years of age have not been recorded.
5% of all cases of childhood dermatoses. It occurs with the same frequency in boys and girls, the peak incidence occurs at the age of 10-18 years. Pink lichen rarely affects younger schoolchildren and preschoolers, and cases of the disease in children under 2 years of age have not been recorded.
Pink lichen in a child
Causes
The etiology of the disease has not yet been established. Most scientists agree that pitiriasis is provoked in a child by herpes viruses types 6 and 7, but there is no convincing scientific evidence of this fact. Another theory calls the cause of the disease the allergization of the body caused by chronic infectious foci. Among the predisposing factors for lichen in children are viral intestinal and respiratory infections, a tendency to allergic reactions.
The main provoking factor in the development of the disease is a decrease in immunity, which leads to a high incidence of pink lichen in spring and autumn, during periods of seasonal beriberi./ativan-withdrawal-symptoms-4588394_final-6bb2e0e1202b4092ba7297c475a8509f.png) The risk of dermatosis increases with acute skin injuries (cuts, abrasions, bruises), with improper body care (non-compliance with hygiene, using too coarse washcloths and towels, cosmetics with allergens and harmful synthetic components).
The risk of dermatosis increases with acute skin injuries (cuts, abrasions, bruises), with improper body care (non-compliance with hygiene, using too coarse washcloths and towels, cosmetics with allergens and harmful synthetic components).
Pathogenesis
The mechanism of development of Gibert’s disease is not fully understood. Presumably, pink lichen has an infectious-allergic nature. Typical skin changes are caused by inflammatory changes in the thickness of the epidermis and dermis, the formation of cytokines, immune complexes and immunoglobulins. These reactions lead to disruption of keratinization processes, excessive formation of keratinized cells.
Symptoms
Pityriasis rosea predominantly debuts with prodromal disorders that include headaches, body aches, malaise, and weakness. They occur 1-3 days before specific skin lesions. Most children do not notice these signs or do not focus on them, considering them to be ordinary fatigue, so the symptoms are revealed only during a detailed survey of the child and parents at the doctor’s appointment.
In 80% of cases, dermatosis is manifested by a maternal plaque – a large red spot of a round or oval shape, the edges of which slightly rise above the surface of the skin. The epidermis in the affected area is covered with small whitish scales that look like papyrus paper. The plaque has a typical localization: the back, abdomen or chest, sometimes the child’s face and scalp are affected. On the legs, pink lichen does not occur.
Gradually, the spread of skin lesions from the primary focus in different directions. Around a large plaque, small red spots and blisters appear, outwardly resembling urticaria, which have clear boundaries and rounded outlines. In shape, they are similar to “medallions”, located along the lines of Langer. The rashes are covered with the same scales as the maternal plaque. Sometimes large bubbles are formed, filled with transparent contents.
In childhood, pink lichen Zhibera is characterized by a more active inflammatory process and infiltration, compared with adults, so the elements of the rash are accompanied by intense itching and discomfort. Unpleasant skin and subjective symptoms persist in the child for 4-8 weeks. In most cases, pitiriasis occurs once in a lifetime, but there are cases of recurrence of dermatosis.
Unpleasant skin and subjective symptoms persist in the child for 4-8 weeks. In most cases, pitiriasis occurs once in a lifetime, but there are cases of recurrence of dermatosis.
Complications
If left untreated, the child may scratch the skin until it bleeds, which is the gateway for a bacterial infection. At the same time, pyoderma develops – multiple pustular rashes on the skin, accompanied by soreness, itching, burning. Another possible complication of dermatosis is eczematization, which is characterized by the appearance of skin lesions typical of eczema in areas where pink lichen has arisen.
Diagnostics
To make a preliminary diagnosis, a clinical examination by a pediatric dermatologist is sufficient, which reveals a maternal plaque, “medallions” and other characteristic manifestations of pink lichen. Establishing a connection between the onset of a rash and a previous viral infection, hypothermia, and a decrease in immunity is of diagnostic value.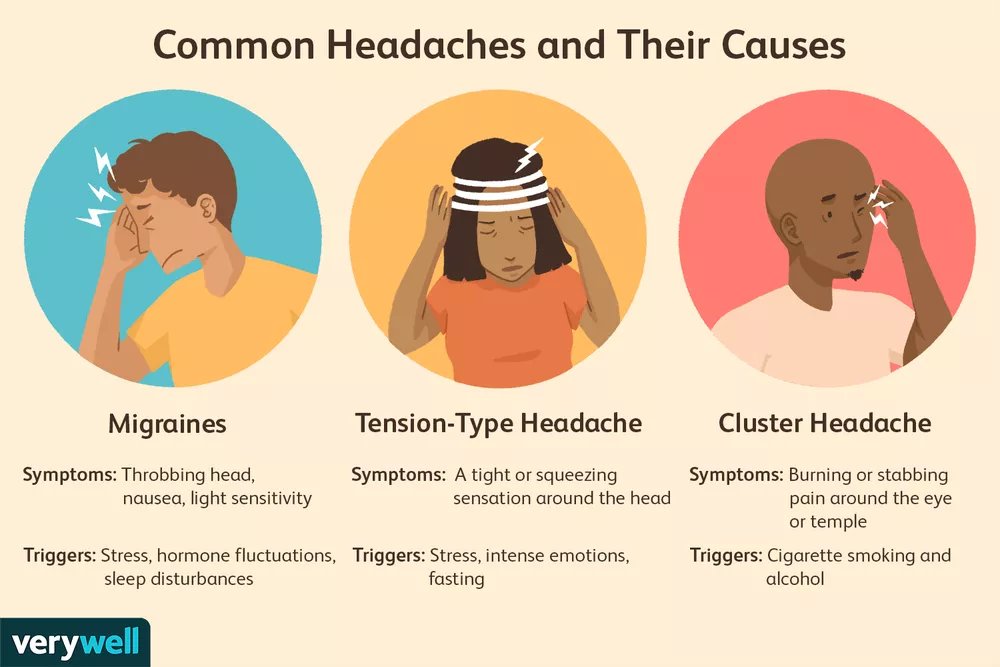 To verify the diagnosis and justify the treatment, laboratory methods are prescribed:
To verify the diagnosis and justify the treatment, laboratory methods are prescribed:
- Blood tests. In terms of hemogram, the doctor pays attention to the level of leukocytes and the ratio of different forms, which may indicate an existing viral or immune inflammatory process in the child’s body. According to the indications, a biochemical blood test, an assessment of acute phase proteins and an extended immunogram are recommended.
- Microscopy of skin scrapings. Some elements of pink lichen resemble a mycotic infection. To choose the right treatment, the doctor examines a sample of scales under a microscope: if the mycelium of fungi is not detected during the diagnosis, the diagnosis of Gibert’s disease is confirmed.
- Serological reactions. In children at risk, it is necessary to exclude syphilitic roseola, for which a number of laboratory methods are used. For screening diagnostics, RIF is used, and in case of doubtful results, the study is supplemented with the Wasserman reaction (RSK) and the immobilization reaction of pale treponema.

Treatment of rosacea in a child
Treatment begins with adequate hygiene measures, dietary and lifestyle modifications. In order not to provoke new rashes, it is necessary to limit the traumatization of the skin as much as possible. Therefore, doctors allow a short hygienic shower once a day using a hypoallergenic soap or gel. After bathing, do not rub the child’s body with a towel. Clothing should be made from natural fabrics that do not cause sweating and irritation.
Since pink lichen can be associated with an allergization of the body, treatment is supplemented with a hypoallergenic diet. Honey, citrus fruits, nuts and other foods that most often lead to sensitization of the child are excluded from the diet. Children are forbidden to sunbathe and stay in the sun for a long time. Since SPF creams can cause additional skin irritation, they are not used; if lichen arose in the summer, then they refrain from long walks in the open sun.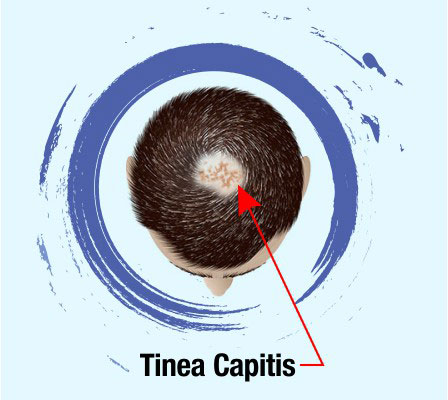
Often, the disease does not require medication, it resolves on its own after 1-1.5 months. Drug treatment is required for intense subjective symptoms of lichen or in case of extensive damage to the skin. For the treatment of Zhiber’s disease, children are prescribed drugs from several pharmacological groups:
- Corticosteroids. The discomfort and itching associated with dermatosis is treated with topical anti-inflammatory hormone creams and ointments. Children are treated with non-absorbable formulations with a minimal concentration of glucocorticoids.
- Antihistamines. Tableted medicines are recommended for severe swelling of the skin and excruciating itching, which is not stopped by local remedies. Usually they use modern medicines of 2-3 generations, which are well tolerated by the child and do not cause drowsiness.
- Hyposensitizing drugs. In pediatric dermatology, sodium thiosulfate is administered as an oral solution or intravenous injection.
 It has a high ability to detoxify, it is effective for stopping the active immune inflammatory process.
It has a high ability to detoxify, it is effective for stopping the active immune inflammatory process. - Antibiotics. Antimicrobial treatment is prescribed according to strict indications if the child is diagnosed with chronic foci of infection (tonsillitis, rhinosinusitis, cholecystitis). The selection of therapy is carried out empirically, mainly macrolides and penicillins are used.
Prognosis and prevention
For most children, recovery takes 1-2 months, and timely treatment accelerates this process. Complications with pink lichen are rare, they are not life-threatening, so the prognosis for all variants of the course of pink lichen is favorable. Given the unclear etiopathogenetic features of pitiriasis, specific prevention measures have not been developed. Prevention of viral diseases and rehabilitation of chronic foci of infection are recommended.
You can share your medical history, what helped you in the treatment of pink lichen in a child.
Sources
- A method for the differential diagnosis of smooth skin microsporia and Zhibera pink lichen in children / M.A. Ufimtseva // RMJ. — 2018.
- Deprive pink Zhibera. Clinical recommendations of the Russian Society of Dermatovenerologists and Cosmetologists. – 2016.
- Differential diagnosis of infectious exanthems in children / D.Yu. Ovsyannikov // Children’s infections. — 2015.
- Pityriasis rosea / V.P. Adaskevich // Dermatology. Supplement to Consilium Medicum. — 2013.
- This article was prepared based on the site materials: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
how to treat at home, what happens, symptoms
Today, among diseases in children under 14 years old, such skin pathology as lichen is quite common. It is characterized by the formation of various types of spots on the skin. Unusual rashes are highly contagious, making sick children a potential threat to people they come into contact with. Therefore, parents need to be more attentive to all strange rashes, and when the first symptoms of the disease appear, refer the child to a doctor.
It is characterized by the formation of various types of spots on the skin. Unusual rashes are highly contagious, making sick children a potential threat to people they come into contact with. Therefore, parents need to be more attentive to all strange rashes, and when the first symptoms of the disease appear, refer the child to a doctor.
What is lichen
According to the frequency of diagnosis, lichen is among the top ten most common skin pathologies in children. The peak of the disease is usually recorded in the spring and summer, in warm and humid weather. Lichen is caused by viruses and fungi, in connection with which scientists attribute to it an infectious origin. Most often, the disease occurs on the skin with a large number of sweat glands, such as the back, face and chest of a child. Varieties of pathology are classified according to causes, course and manifestations that occur outside. With various forms of lichen, different types of rashes are formed, for example, dry or wet, pale pink or deep red.
What is ringworm in children
Ringworm
The most common form of the disease. First of all, the disease manifests itself on the nails, skin and hair. At the same time, ringworm in children has an incubation period of one to six weeks, which slows down the healing process due to delayed diagnosis. You can notice the disease by reddish oval and round spots, which are covered with scales and a crust. Hair at the site of the formation of the focus may break off or even fall out. The patient develops severe peeling, itching and burning in the affected area. An increase in basal body temperature, a decrease in appetite, and an increase in lymph nodes are also common. Treatment methods for ringworm are determined by the doctor, after clarifying the type of fungus that provoked the disease. Treatment is usually carried out at home. (1
Pityriasis rosea or Gibert’s disease
Pityriasis rosea usually occurs on the body: on the abdomen, chest, shoulders, flanks or back.:max_bytes(150000):strip_icc()/hormone-allergy-82663-ca91df10002742eeab0c0618d95fbaaf.jpg) As the first manifestation of the disease, you can notice a spot of bright pink color up to five centimeters in size. After one or two weeks, small oval-shaped rashes begin to spread from the spot in different directions. In the middle of the rash, the skin is prone to peeling, and a red outline appears along the edges. Most often, the lesion is localized in natural skin folds. There is a feeling of light and unpleasant itching. The rashes stay on the skin for about a month and a half, after which they disappear without a trace. It is important to prevent their injury, due to which an infection can enter the wound, causing complications.
As the first manifestation of the disease, you can notice a spot of bright pink color up to five centimeters in size. After one or two weeks, small oval-shaped rashes begin to spread from the spot in different directions. In the middle of the rash, the skin is prone to peeling, and a red outline appears along the edges. Most often, the lesion is localized in natural skin folds. There is a feeling of light and unpleasant itching. The rashes stay on the skin for about a month and a half, after which they disappear without a trace. It is important to prevent their injury, due to which an infection can enter the wound, causing complications.
Shingles. Photo: shutterstock.com
Shingles
This is a form of the disease that occurs due to exposure to a viral infection, mainly in children who do not have immunity to it. This type of illness is most common among older teenagers who have previously had chickenpox. After the onset of recovery, the virus remains in the nerve cells in a latent form, due to which, during a decrease in immunity, an exacerbation of the disease occurs, accompanied by severe pain. This is the danger of shingles. Also, the disease can lead to such serious consequences as neuralgia, inflammation of the meninges, loss of sensitivity and vision. Even before the appearance of rashes, the patient develops weakness, drowsiness, and an increase in overall body temperature. Sometimes the first symptoms are confused with the flu or SARS. Pathology can be recognized by the formation of small rashes at the locations of the nerve endings. Visually, the rash with a disease is similar to chickenpox: small swollen blisters on the body. Often recovery comes on its own. However, in severe cases, the patient is placed in a hospital and prescribed painkillers and antiviral drugs.
This is the danger of shingles. Also, the disease can lead to such serious consequences as neuralgia, inflammation of the meninges, loss of sensitivity and vision. Even before the appearance of rashes, the patient develops weakness, drowsiness, and an increase in overall body temperature. Sometimes the first symptoms are confused with the flu or SARS. Pathology can be recognized by the formation of small rashes at the locations of the nerve endings. Visually, the rash with a disease is similar to chickenpox: small swollen blisters on the body. Often recovery comes on its own. However, in severe cases, the patient is placed in a hospital and prescribed painkillers and antiviral drugs.
Lichen planus
Today, lichen planus is extremely rare in children. A characteristic feature of this form of the disease is its location in the places of folds and on the abdomen. Eruptions of lichen planus can be distinguished by watery spots of bright red or dark brown color. The affected skin of the patient is very itchy and itchy, which leads to irritability and tearfulness of the child. Over time, after recovery, persistent pigment spots may form at the site of the rash. (2)
The affected skin of the patient is very itchy and itchy, which leads to irritability and tearfulness of the child. Over time, after recovery, persistent pigment spots may form at the site of the rash. (2)
Pityriasis versicolor or pityriasis versicolor
Pityriasis versicolor is not contagious, it is caused by pathogens living in every person. This is a rare form of lichen that affects only the upper stratum corneum of the skin and is not transmitted by contact. In places of localization of the disease – on the back, abdomen and shoulders – a rash appears in the form of pink or yellow-brown spots covered with skin scales. After the spots can grow, forming foci with blurry edges. During the course of the disease, the rash may change color, becoming dark brown or dark brown, which led to the name of this form of the disease. (3)
Provoking factors
A child’s fragile body often cannot withstand the threats of the outside world. The main reason for the appearance of lichen is considered to be the penetration of a viral or fungal infection into the body of a child.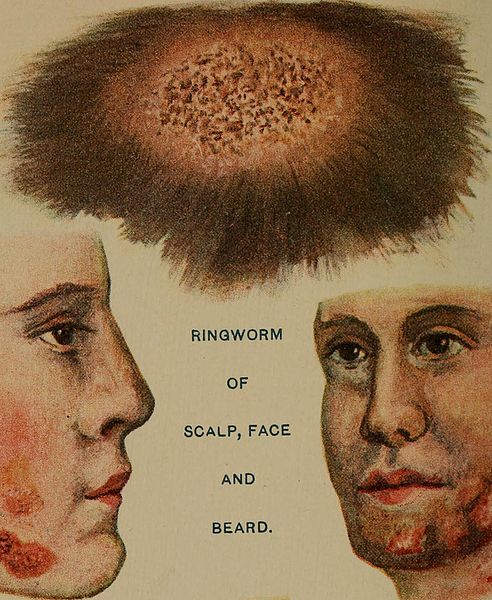 Different forms of lichen have their own causes. For example, pink lichen received an infectious-allergic nature of development, herpes zoster is formed due to the virus entering the child’s body, and ringworm and pityriasis due to fungi.
Different forms of lichen have their own causes. For example, pink lichen received an infectious-allergic nature of development, herpes zoster is formed due to the virus entering the child’s body, and ringworm and pityriasis due to fungi.
Nevertheless, to date, scientists have not exactly determined why not all children (even those who fall into the risk group list) can become infected with lichen. There are main provoking factors that increase the risk of getting sick:
- excessive emotional and physical stress;
- stress and emotional overstrain;
- reduced overall immunity;
- beriberi;
- occurrence of infectious inflammatory processes;
- allergic reactions;
- endocrine diseases – obesity, diabetes mellitus, thyroid problems;
- skin lesions;
- neglect of the rules of personal hygiene and the occurrence of favorable conditions for the formation of pathological microflora on the skin;
- abrupt change in climatic conditions or thermoregulation – heat, cold, high humidity, increased sweating;
- hereditary predisposition.

Photo: pavel-danilyuk, pexels.com
Most often, children become infected in crowded places, such as kindergarten, summer camp, school or public pool. Also often, as the main cause of infection, doctors cite contact with domestic or street animals, after which the rules of personal hygiene were not observed. (4)
Symptoms of lichen in children
The shape, color and nature of the rash may vary. Only a doctor can accurately diagnose and distinguish the disease from ordinary dermatitis, therefore, at the first signs of a pathology, it is necessary to consult a specialist. The treatment of lichen in children is carried out by such doctors as a pediatrician, a dermatologist and an infectious disease specialist. Clinical signs of diagnosis of different types of lichen in children are different. Despite this, common symptoms have been identified for all types of lichen, in the event of which an urgent need to consult a doctor.
Spotted rash
Depending on the form of lichen, the rash may look different. With herpes zoster and lichen planus, small vesicles with serous-hemorrhagic contents form on the skin. With multi-colored lichen, spots are formed of various sizes and types. And with pink lichen, a papule appears (a flat tissue growth that rises above healthy epithelium). Papules can connect with each other and become covered with scales. The color of the rash can vary from pale pink and white to purplish red and brownish yellow.
With herpes zoster and lichen planus, small vesicles with serous-hemorrhagic contents form on the skin. With multi-colored lichen, spots are formed of various sizes and types. And with pink lichen, a papule appears (a flat tissue growth that rises above healthy epithelium). Papules can connect with each other and become covered with scales. The color of the rash can vary from pale pink and white to purplish red and brownish yellow.
Itching and burning
An unpleasant sensation of burning and itching often occurs at the affected area. Different forms entail different intensity of sensations, but in any case they will cause irritation and discomfort to the child, which will affect his quality of life.
Hair loss
Quite often, a large area of baldness occurs in the affected areas, along the edges of which the hair breaks off at a length of one centimeter from the skin. Multiple small lesions may appear next to the main formation.
Sometimes during an exacerbation of the disease, the general condition of the child may worsen – the temperature rises, weakness, vomiting, headaches or joint pain occur.
Photo: pixabay.com
How to treat lichen in children at home
Regardless of the form, lichen requires a timely start of the treatment procedure. Advanced cases are amenable only to complex and lengthy therapy, so you should not self-medicate, but you should immediately consult a doctor. Lichen treatment should be prescribed by a doctor after examination and diagnosis. After the interview, the specialist should examine the site of the lesion visually and with the help of a mercury-quartz magnifying lamp, under which various forms of lichen acquire different shades of the brown-yellow spectrum. To determine the type of pathogen, the doctor may prescribe a microscopic examination of the scraping of the affected area of the skin, the Balzer iodine test, or a test for Besnier’s symptoms./ringworm-overview-2632044_FINAL-e1669cad90b347b981a4c1ae42865fcc.png) Also, if necessary, they may recommend taking a biochemical blood test and a general urine test. After diagnostic data are obtained and a complete clinical picture of the disease is formed, the specialist will be able to choose the most effective treatment tactics.
Also, if necessary, they may recommend taking a biochemical blood test and a general urine test. After diagnostic data are obtained and a complete clinical picture of the disease is formed, the specialist will be able to choose the most effective treatment tactics.
However, at home, you can relieve the child’s condition before visiting the doctor. Before a visit to a specialist, the affected area should not be smeared with various ointments and creams that can modify the rash, as this will complicate the diagnostic process. To prevent germs from multiplying, the child should be bathed regularly and his underwear should be changed. When choosing clothes, it is recommended to give preference to natural lightweight and breathable fabrics. Wash your baby in the shower to reduce the possibility of the rash spreading. It is necessary to exclude sweet and fatty foods from the diet, replacing them with vegetables and sour-milk products.
Before visiting the specialist’s office, you need to limit the possibility of contact with other people. During the treatment of contagious forms of lichen, protective gloves should be worn during treatments, and the child should be provided with separate dishes and hygiene items.
During the treatment of contagious forms of lichen, protective gloves should be worn during treatments, and the child should be provided with separate dishes and hygiene items.
Still, lichen is easier to prevent than to cure, so it is important to take preventive measures, which include maintaining good hygiene and reducing contact with street animals. Lichen develops only when immunity is weakened, which will be strengthened by frequent walks, sports, a balanced diet and sleep patterns.
Popular Questions and Answers
To finally understand the peculiarities of the occurrence and course of lichen in children, dermatologist, trichologist Suzanna Matevosyan answered the most common questions about an unpleasant disease.
How to determine lichen in a child with iodine?
The easiest and cheapest way to determine pityriasis versicolor is the Balser test (iodine test). For diagnosis, a 5% alcohol iodine solution is smeared on the affected area.:max_bytes(150000):strip_icc()/ringworm_symptoms-5ae1f3c4a474be00366fef35.png) If the rash really appeared due to lichen, skin pigmentation will change: the affected area of \u200b\u200bthe skin will become brown or black. Thus, the reaction of foci of inflammation to iodine is manifested. It is important to consider that not all forms of lichen can be tested in this way. Some of them, which have a viral or allergic etymology, are highly discouraged from diagnosing with an iodine solution: for example, herpes zoster, lichen planus, or pink lichen.
If the rash really appeared due to lichen, skin pigmentation will change: the affected area of \u200b\u200bthe skin will become brown or black. Thus, the reaction of foci of inflammation to iodine is manifested. It is important to consider that not all forms of lichen can be tested in this way. Some of them, which have a viral or allergic etymology, are highly discouraged from diagnosing with an iodine solution: for example, herpes zoster, lichen planus, or pink lichen.
Why is lichen dangerous?
For children, lichen is a particular danger. A disease that causes a violation of skin pigmentation can cause not only a cosmetic defect. If you do not treat it and at the same time touch and comb the lesions, you can bring an infection into the wound. Also, the disease can begin to spread throughout the body or even to internal organs. Therefore, it is important to diagnose it in time and immediately begin treatment.
How can you get lichen?
Most often, the transmission of the disease to the child occurs due to the contact with the skin of particles of hair or skin of sick people or animals.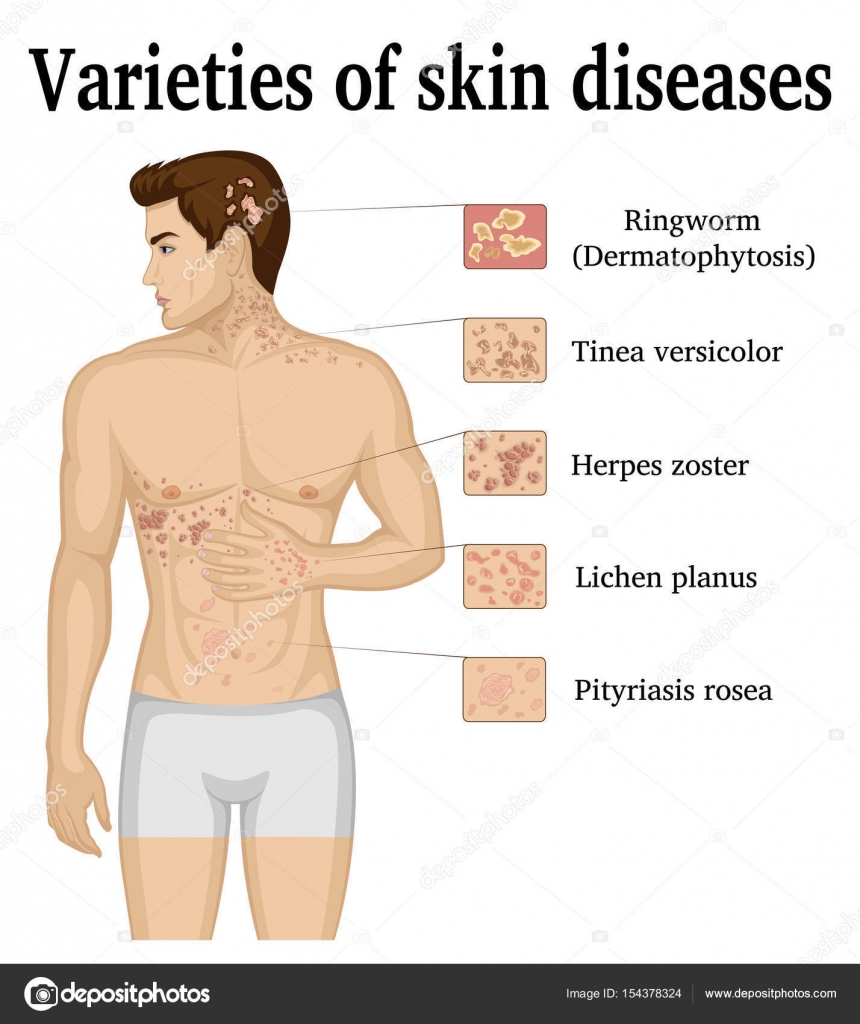 However, you can catch an unpleasant pathology through direct contact with a sick person or the use of his personal hygiene items.
However, you can catch an unpleasant pathology through direct contact with a sick person or the use of his personal hygiene items.
Sources
- Microsporia – ringworm of the 21st century / A. G. Shevchenko, M. I. Gluzmin, E. V. Egorova // Advances in medical mycology. – 2019. – T. 20. – S. 106-109. URL: https://www.elibrary.ru/item.asp?id=38171128
- Dvoryankova EV, Krasnikova VN, Korsunskaya IM Lichen planus in pediatric practice // Pediatrics. Supplement to Consilium Medicum. – 2018. – No. 3. URL: https://cyberleninka.ru/article/n/krasnyy-ploskiy-lishay-v-detskoy-praktike.
- Kukalo, SV Pityriasis versicolor, errors in diagnosis / SV Kukalo, NM Sharova // Advances in Medical Mycology. – 2018. – T. 18. – S. 327-328. URL: https://www.elibrary.ru/item.asp?id=35079977
- Kandrashkina M. S. Ringworm // In the world of scientific discoveries: materials of the V conference. – 2016 – p. 145-146. URL: http://lib.



 It has a high ability to detoxify, it is effective for stopping the active immune inflammatory process.
It has a high ability to detoxify, it is effective for stopping the active immune inflammatory process.