Symptoms of staph infection on lips. Understanding Staph Infections on the Lips: Causes, Symptoms, Treatment, and Prevention
What are the symptoms of a staph infection on the lips? How is it diagnosed and treated? Discover the causes, treatment options, and prevention tips for staph infections on the lips.
Understanding Staph Infections on the Lips
Staph infections on the lips can be a concerning and uncomfortable condition, but with proper diagnosis and treatment, they can be effectively managed. In this comprehensive article, we’ll delve into the causes, symptoms, diagnosis, and treatment of staph infections on the lips, as well as explore prevention strategies to help you maintain healthy skin.
Causes of Staph Infections on the Lips
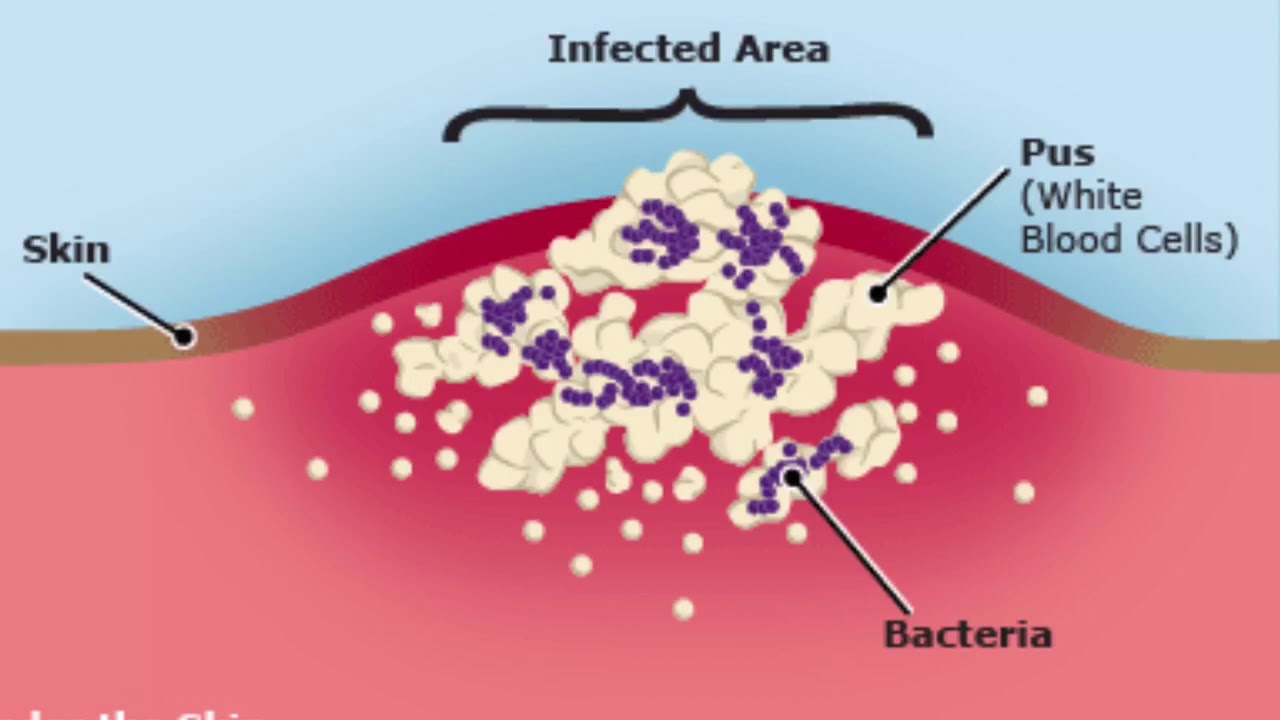
Staph infections on the lips are typically caused by the bacteria Staphylococcus aureus, also known as “staph.” This bacteria can enter the skin through a cut, scrape, or even intact skin, leading to an infection. In some cases, group A Streptococcus bacteria may also be the culprit, causing a condition known as impetigo.

What factors increase the risk of developing a staph infection on the lips? Individuals who live in tropical climates, have a pre-existing scabies infection, or engage in activities where cuts and scrapes are common may be at a higher risk. Additionally, those living in close contact or crowded situations, such as in a daycare setting, are more susceptible to contracting a staph infection.
Symptoms of Staph Infections on the Lips
The primary symptoms of a staph infection on the lips include:
- One or more pus-filled blisters that burst easily, leading to red, raw skin
- Itchy blisters containing fluid (yellow or tan) that seeps out and forms a crust
- A spreading rash
- Skin lesions (wounds) on the lips, nose, ears, arms, and legs that can spread to other parts of the body
- Swollen lymph nodes near the infected area
If the infection is caused by staph bacteria, you may also notice reddish skin surrounding the blisters, which are full of liquid or pus that eventually looks cloudy. The blisters may burst easily, leading to raw, shiny areas that scab over with a yellow or brown crust.

Diagnosing Staph Infections on the Lips
How are staph infections on the lips diagnosed? A healthcare provider can typically diagnose impetigo based on the appearance of the sores. They may also take a skin sample to send to a laboratory, where pathologists can determine the specific bacteria causing the infection. This information can help guide the appropriate antibiotic treatment.
If you or your child notice any blood or unusual color in the urine, be sure to inform your healthcare provider, as this could be a sign of a more serious condition, such as glomerulonephritis, an inflammatory kidney disease that can be a complication of certain strains of streptococcal bacteria.
Treatment for Staph Infections on the Lips
Antibiotics are the primary treatment for staph infections on the lips. Your healthcare provider may prescribe topical antibiotics, such as mupirocin (Bactroban or Centany), to be applied directly to the affected area. In cases where the infection covers a large area of skin or multiple body parts, oral antibiotics may be necessary.
It’s important to follow the treatment plan prescribed by your healthcare provider and to complete the full course of antibiotics, even if the symptoms start to improve. Stopping the medication too soon can lead to the infection returning or becoming more resistant to treatment.
Preventing Staph Infections on the Lips
To help prevent staph infections on the lips, consider the following strategies:
- Practice good hygiene, such as regularly washing your hands with soap and water, especially after touching any sores or blisters.
- Avoid sharing personal items, such as towels, clothing, or lip balm, with someone who has a staph infection.
- Keep any cuts, scrapes, or other skin injuries clean and covered to prevent bacterial infections.
- Avoid touching or scratching the sores, as this can spread the infection to other areas of the body.
- If you or your child has impetigo, follow the treatment plan prescribed by your healthcare provider and ensure the infection is fully resolved before returning to school or other close-contact environments.
By understanding the causes, symptoms, and proper treatment of staph infections on the lips, you can take proactive steps to maintain healthy skin and prevent the spread of this contagious condition.

Key Takeaways
Staph infections on the lips are typically caused by the bacteria Staphylococcus aureus or, in some cases, group A Streptococcus. Symptoms include pus-filled blisters, itchy sores, and a spreading rash. Diagnosis is usually based on the appearance of the sores, and treatment involves antibiotics, either topical or oral. To prevent staph infections on the lips, practice good hygiene, avoid sharing personal items, and keep any skin injuries clean and covered.
Causes, Symptoms, Treatment & Prevention
Overview
Impetigo on the lower lip.
What is impetigo?
Impetigo (im-pa-TIE-go) is an itchy, sometimes painful, skin infection.
Who gets impetigo?
Impetigo usually happens to children between ages 2 and 6. Older children and adults can also get it.
You may also be at higher risk if you:
- Live in a tropical climate, with hot, humid summers and mild winters.
- Have a scabies infection.
- Do activities or sports where cuts and scrapes are common.
- Live in close contact or crowded situations. Infections often happen to people living in the same house or children in day care.
How does someone get impetigo?
When you get a cut, bite or scratch that opens the skin, bacteria can enter and cause an impetigo infection. But impetigo can infect the skin even if it’s not broken or punctured.
But impetigo can infect the skin even if it’s not broken or punctured.
Impetigo happens more often in warmer months when children are outside more.
Where does impetigo occur?
Typically, the first signs of impetigo are sores and blisters on the mouth and nose. Impetigo can also appear on the legs and arms.
What is bullous impetigo?
Bullous impetigo is a rare type of impetigo. It has larger blisters that don’t break open as easily. It often appears on the neck, torso, armpits or groin.
How common is impetigo?
Impetigo is the most common skin infection in kids ages 2 to 5. It happens much less in adults. Every year, Staphylococcus aureus, the bacteria that causes impetigo, causes 11 million skin and soft tissue infections.
Symptoms and Causes
What causes impetigo?
The main cause of impetigo is a bacterial infection.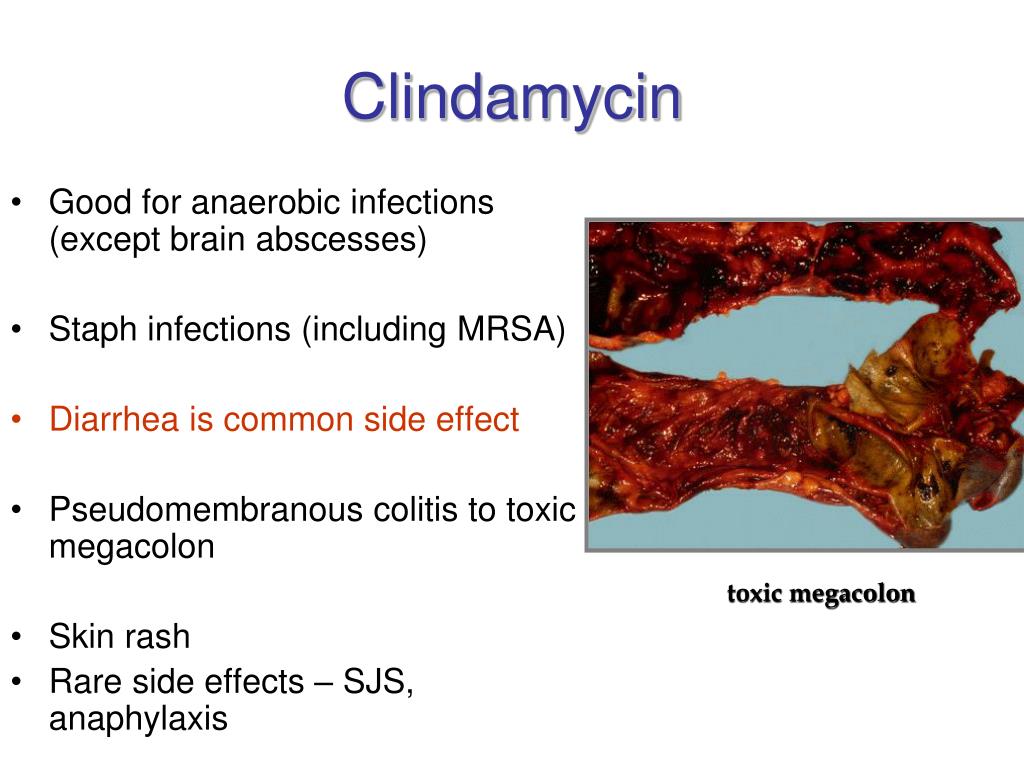 The bacteria usually enters the skin through a cut, scrape, rash or insect bite.
The bacteria usually enters the skin through a cut, scrape, rash or insect bite.
Most of the time, the cause is the Staphylococcus aureus (“staph” bacteria). Sometimes, group A Streptococcus bacteria can cause it. This type of bacteria also leads to strep throat and fever.
Certain strains of strep bacteria that cause impetigo can also cause glomerulonephritis. This inflammatory kidney disease can produce high blood pressure and blood in the urine.
Is impetigo contagious?
Impetigo is mild but highly contagious. You can spread impetigo by coming into contact with the sores or mucus or nasal discharge from someone who has it. People can also spread impetigo by sharing items such as towels, clothing or other personal items with someone who’s infected.
When do impetigo symptoms start?
Typically, once the infection happens, symptoms occur within three days. Scratching the sores can spread the infection. Symptoms first start around the mouth and nose.
What are the symptoms of impetigo?
Symptoms of impetigo include:
- One or more pus-filled blisters that burst easily, causing red, raw skin.
- Itchy blisters containing fluid (yellow or tan) that seeps out and forms a crust.
- A rash that spreads.
- Skin lesions (wounds) on the lips, nose, ears, arms and legs. The lesions can spread to other parts of the body.
- Swollen lymph nodes near the infected area.
If you or your child has impetigo caused by staph bacteria, you may notice:
- Reddish skin surrounding red blisters, full of liquid or pus that eventually looks cloudy.
- Blisters that burst easily and leak.
- Raw, shiny areas that scab over with a yellow/brown crust.
Diagnosis and Tests
How is impetigo diagnosed?
A healthcare provider can diagnose impetigo based on how the sores look. The provider may take a skin sample to send to a laboratory. Pathologists can figure out which bacteria is causing the disease, which can help determine the right antibiotic to use.
The provider may take a skin sample to send to a laboratory. Pathologists can figure out which bacteria is causing the disease, which can help determine the right antibiotic to use.
If you notice or your child notices any blood or odd color in urine, tell your healthcare provider right away.
Management and Treatment
How is impetigo treated?
Antibiotics can treat impetigo. A provider may prescribe topical antibiotics to put on the skin. Your child may need to take oral antibiotics (a liquid or pill) if the condition covers a large area of skin or multiple body parts.
Examples of antibiotic treatments include:
- Topical mupirocin (Bactroban® or Centany®) ointment.
- Oral antibiotics such as cephalosporins, clindamycin (Cleocin®) and sulfamethoxazole (Bactrim™).

Will impetigo go away on its own?
Impetigo often disappears within about three weeks, even without treatment. But it may take longer. Until it goes away, your child is contagious.
Are there complications of impetigo?
Complications are rare. They include:
- Rash that spreads to deeper skin layers.
- Kidney problems, called post-streptococcal glomerulonephritis.
Prevention
Can I prevent impetigo?
The best ways to prevent infection are to stay clean and healthy. Other tips to avoid impetigo include:
- Keep hands clean: Wash hands regularly. Use alcohol-based sanitizer if you don’t have soap and water.
- Practice good hygiene: Clip your (and your child’s) fingernails regularly to avoid scratching.
 Sneeze into a tissue and then throw the tissue away. Bathe daily (or as often as possible), especially for children with eczema or sensitive skin.
Sneeze into a tissue and then throw the tissue away. Bathe daily (or as often as possible), especially for children with eczema or sensitive skin. - Avoid scratching: Don’t scratch cuts or wounds. If your child gets a cut, scratch or wound, keep them from scratching it.
- Clean wounds: Clean cuts, scrapes and injuries with soap and water. Then put an antibiotic cream or ointment on the wound.
- Keep linens clean: Wash underwear, towels and sheets in hot water.
Outlook / Prognosis
What’s the outlook for someone who gets impetigo?
Antibiotics can cure impetigo, but the condition can return, especially in small children. Getting it once doesn’t protect someone from getting it again.
How long until the sores go away?
The sores may take some time to heal completely. The good news: The infection rarely leaves scars.
The good news: The infection rarely leaves scars.
How long is impetigo contagious?
Without treatment, impetigo can be contagious for weeks. After starting impetigo treatment, the condition is contagious until:
- The rash disappears.
- Scabs fall off.
- You have finished at least two days of antibiotics.
Can a person get re-infected?
Re-infection happens. Children are especially prone to scratching and opening their scabs, putting them at a higher risk of re-infection.
Living With
How can I take care of myself if I have impetigo?
If your healthcare provider diagnosed you or your child with impetigo, these treatment tips can help:
- Keep sores covered: Bandage sores or wear long sleeves and pants.

- Take all medication: Use your antibiotics for the full length of me your provider prescribed them to prevent re-infection.
- Stay clean: Wash the skin gently a few times a day using antibacterial soap. Doing so will remove crusts and drainage.
- Avoid touching the rash: If you do touch it, wash your hands and the exposed area with soap and water.
- Isolate children: If your child has impetigo, keep them away from other children until they finish treatment. They shouldn’t go to school or day care.
- Avoid hot tubs and swimming pools: The rash can spread if others come into contact with your child’s skin, swimsuit or towel.
A note from Cleveland Clinic Impetigo is a common skin condition that mostly affects young children. Impetigo symptoms include blisters and red sores that typically start around the mouth and nose. If you notice signs of impetigo, talk to your healthcare provider. Impetigo treatment is usually antibiotics, either oral or topical (a cream). Impetigo is very contagious, so keep children home until they’ve had at least two days of antibiotics. The medicine will clear up the rash. To prevent impetigo, practice good hygiene. Clean and cover any cuts or scratches to keep them from getting infected.
Impetigo treatment is usually antibiotics, either oral or topical (a cream). Impetigo is very contagious, so keep children home until they’ve had at least two days of antibiotics. The medicine will clear up the rash. To prevent impetigo, practice good hygiene. Clean and cover any cuts or scratches to keep them from getting infected.
A Description of Two Cases Occurred in the Same Family
Int J Med Sci. 2012; 9(1): 47–50.
Massimo Marrelli
1. Department of Oral and Maxillofacial Surgery, Calabrodental, Crotone, Italy.
3. Department of Dental Sciences and Surgery, University of Bari, Bari, Italy.
Marco Tatullo
1. Department of Oral and Maxillofacial Surgery, Calabrodental, Crotone, Italy.
2. Department of Basic Medical Sciences, University of Bari, Bari, Italy.
Gianna Dipalma
1. Department of Oral and Maxillofacial Surgery, Calabrodental, Crotone, Italy.
Francesco Inchingolo
1. Department of Oral and Maxillofacial Surgery, Calabrodental, Crotone, Italy.
Department of Oral and Maxillofacial Surgery, Calabrodental, Crotone, Italy.
3. Department of Dental Sciences and Surgery, University of Bari, Bari, Italy.
1. Department of Oral and Maxillofacial Surgery, Calabrodental, Crotone, Italy.
2. Department of Basic Medical Sciences, University of Bari, Bari, Italy.
3. Department of Dental Sciences and Surgery, University of Bari, Bari, Italy.
✉ Corresponding author: Dr. Marco Tatullo, Tecnologica Research Institute, St. E. Fermi – Passovecchio – 88900 Crotone, Dept. of “Basic Medical Sciences”, University of Bari- P.ce G.Cesare- 70124 Bari. E-mail: [email protected]; Tel.: 00393498742445
Conflict of Interest: All authors disclose any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work.
Received 2011 Sep 28; Accepted 2011 Oct 11.
Copyright © Ivyspring International Publisher. This is an open-access article distributed under the terms of the Creative Commons License (http://creativecommons.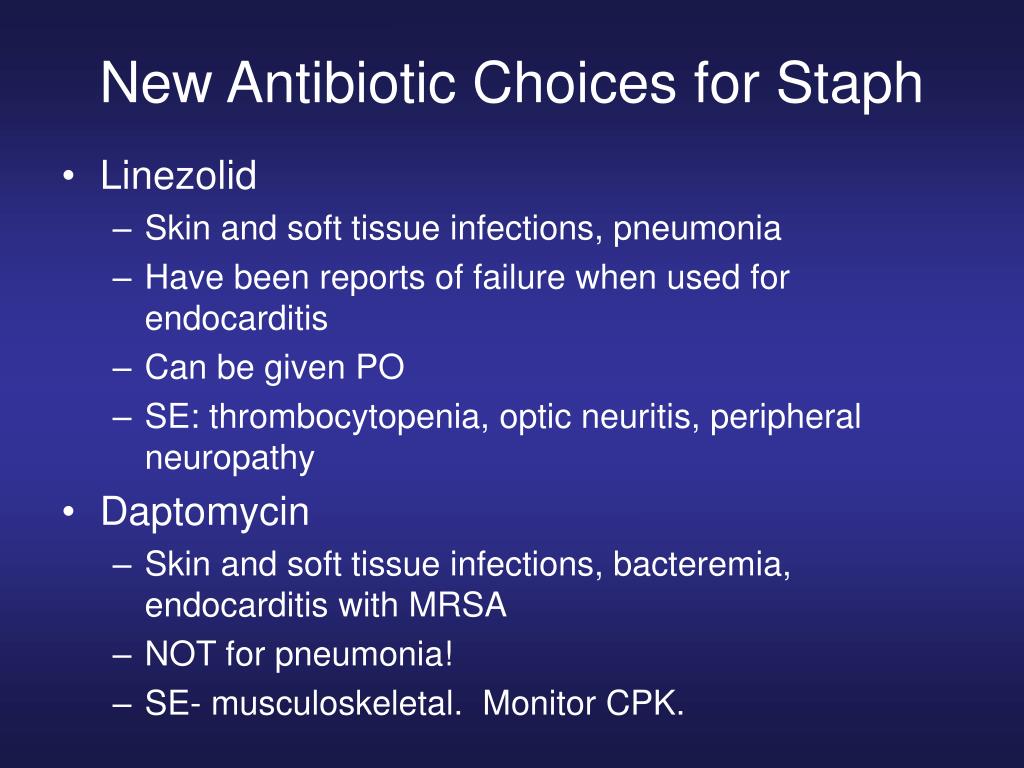 org/licenses/by-nc-nd/3.0/). Reproduction is permitted for personal, noncommercial use, provided that the article is in whole, unmodified, and properly cited.This article has been cited by other articles in PMC.
org/licenses/by-nc-nd/3.0/). Reproduction is permitted for personal, noncommercial use, provided that the article is in whole, unmodified, and properly cited.This article has been cited by other articles in PMC.
Abstract
Introduction. White Sponge Nevus (WSN) is a rare pathology with a pathogenesis on genetic basis, a benign course and a localization affecting the mucosal keratin.
WSN is usually a symptomless pathology: when pain is present, some authors reported reduction of symptoms by taking penicillin or oral tetracycline rinses, suggesting that a bacterial overinfection could be at the base of possible painful symptoms.
Case Report. We describe 2 patients affected by WSN, father and son: they presented two different oral diseases associated with an infection by Staphylococcus aureus. So, we have performed a careful oral hygiene to reduce infection in the oral cavity. In the following days we prescribed 2 rinses a day with a mouthwash containing chlorhexidine digluconate at two different percentages.
Discussion. Early diagnosis of this lesion is important, because it allows us to exclude other more serious diseases. In the most part of cases, WSN requires no treatment because of its benign and asymptomatic behaviour: up to now, no protocol of treatment for this condition was standardized. Even if WSN is a painless condition, sometime a correlated painful symptomatology was reported.
Conclusions. In our experience, we have achieved excellent results even with chlorhexidine digluconate rinses, considering that our treated cases were both infected by Staphylococcus aureus.
We hypothesize that the corrugated plaques and the altered texture of the mucosa create the right conditions for the colonization and the development of microbial species such as saprophytic bacteria or fungal species.
Keywords: White Sponge Nevus, Staphylococcus Aureus, Oral disease
Introduction
White Sponge Nevus (WSN) is a rare pathology with a pathogenesis on genetic basis, a benign course and a localization affecting the mucosal keratin.
The onset is usually during early infancy, often before 20 years, and there is no gender predilection. This mucosal alteration usually affects oral soft tissues, but it sometime involves vaginal and rectal mucosa. In literature, we can find that WSN is called also in several other ways, such as “nevus of Cannon”, “leukoderma exfoliativum mucosae oris”, “familial white folded mucosal dysplasia” and “hereditary leukokeratosis” 1.
The most recent studies indicate that a mutation in the helical domain of mucosal specific keratins, K4 and K132 could be responsible for the alteration of epithelial cells.
Lesions of WSN are easily recognized and clinically valuable: they appear as bilateral white spongy plaques, typically found on the buccal mucosa, and the patients refer no painful symptomatology. We can find these lesions in other common sites including the tongue, floor of the mouth, and alveolar mucosa 3,4.
Cytological features of this condition show that the nuclei are pyknotic.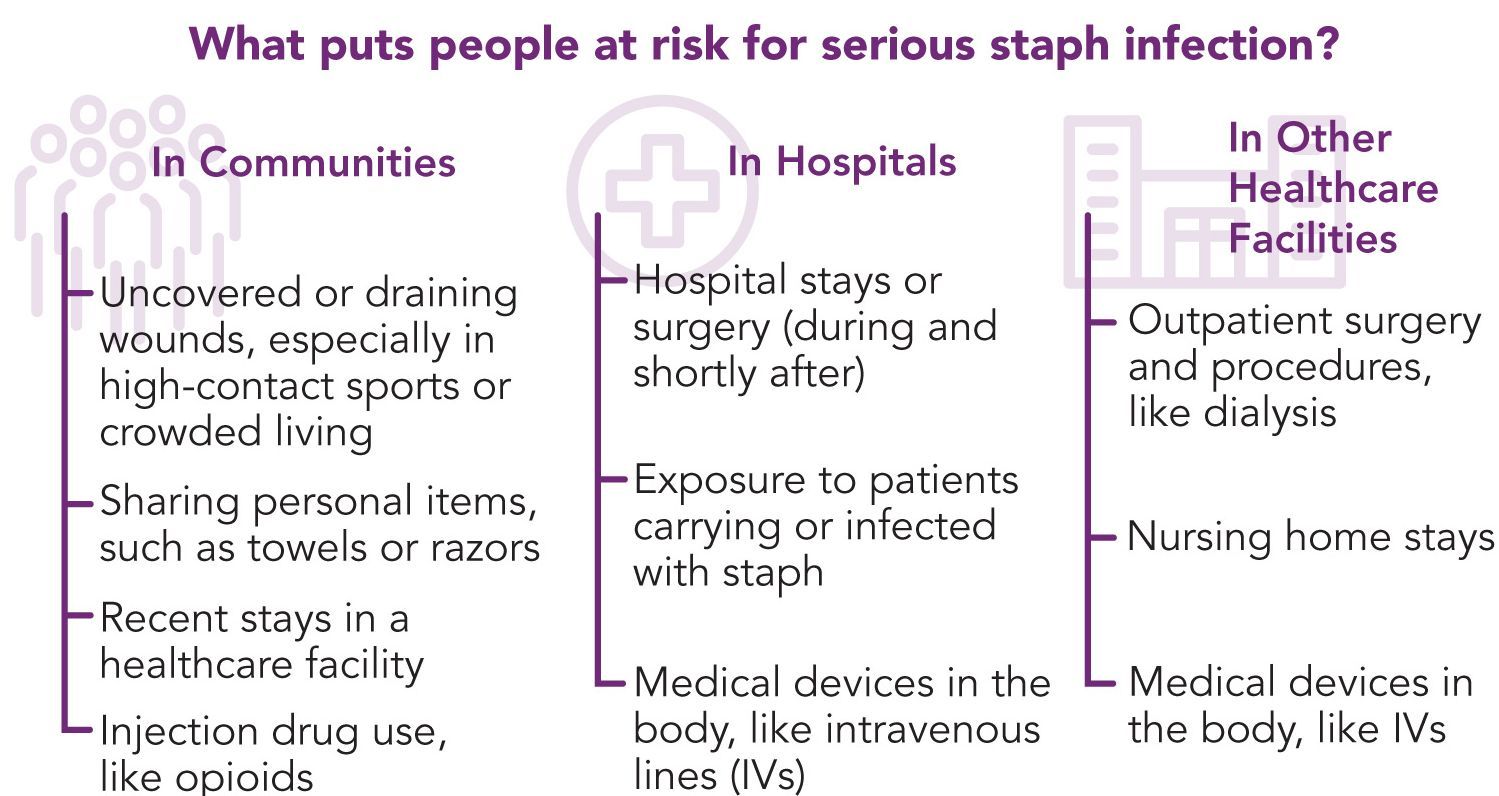 There are no aspects of malignant lesion and we have found no report of dysplasia in the literature. Other histological findings include intracellular edema of the spinous layer cells 5. However, intracellular edema is not pathognomonic for WSN; in fact, the same aspect is present in other lesions, such as the leukoedema which is quite similar to WSN, even if it shows no parakeratosis 6. When we manage a patient affected by WSN no treatment is required onto these lesions, except for a clinical condition of a plaque which extends onto the lip vermilion: in this kind of cases, we perform a surgical exeresis for aesthetic reasons 7.
There are no aspects of malignant lesion and we have found no report of dysplasia in the literature. Other histological findings include intracellular edema of the spinous layer cells 5. However, intracellular edema is not pathognomonic for WSN; in fact, the same aspect is present in other lesions, such as the leukoedema which is quite similar to WSN, even if it shows no parakeratosis 6. When we manage a patient affected by WSN no treatment is required onto these lesions, except for a clinical condition of a plaque which extends onto the lip vermilion: in this kind of cases, we perform a surgical exeresis for aesthetic reasons 7.
Concerning the differential diagnosis, WSN is often confused with a form of chronic hyperplastic candidosis resistant to treatment; moreover, the surface of mucosa affected by WSN, which presents an irregular architecture, favors secondary infection by Candida 5.
WSN typically affects several individuals in a same family, further confirming its autosomal dominant heredity 8–9.
WSN is usually a symptomless pathology: when pain is present, some authors reported reduction of symptoms by taking penicillin10 or oral tetracycline rinses11, suggesting that a bacterial overinfection could be at the base of possible painful symptoms. However, almost all cases reported in the literature describe WSN as a benign condition that does not require any treatment.
We describe 2 patients affected by WSN, father and son: because they presented two different oral diseases associated with an infection by Staphylococcus aureus (SA), we hypothesized a relationship between WSN and Staphylococcus aureus infection.
Case Report
An 38 year-old Italian man came to the Department of Oral Hygiene and Periodontology at Calabrodental clinic in April 2011 for the evaluation of white bilateral corrugated plaques developed on the buccal mucosa and on the gingiva, these plaques were been present since he was 13 years-old. (Fig. )
)
a patient showing white bilateral corrugated plaques developed on the buccal mucosa and on the gingiva.
This clinical condition was investigated by another clinician who carried out a diagnosis of White Sponge Nevus, excluding so the other similar pathologies compatible with this clinical aspect.
These plaques were always asymptomatic, however, from 2 months, the patient complained of burning symptoms that persisted throughout the day. So, he came at the clinic Calabrodental in order to alleviate these symptoms. After routine investigations, we prescribed an oral buffer to assess the possible presence of bacterial or fungal superinfection: the result was positive for Staphylococcus aureus which showed a susceptibility to methicillin. The analysis didn’t evidenced the presence of Candida albicans or other fungal infections, so the painful symptomatology could be related to a poor oral hygiene and to the presence of the methicillin-resistant Staphylococcus aureus in the oral cavity of our patient. So, we have performed a careful oral hygiene to reduce infection in the oral cavity. (Fig.)
So, we have performed a careful oral hygiene to reduce infection in the oral cavity. (Fig.)
a careful oral hygiene performed to the patient affected by white sponge nevus.
In the following days we prescribed 2 rinses a day with a mouthwash containing chlorhexidine digluconate at 0.2%. We performed the follow-up after 7 days and the patient has reported the disappearance of pain. During the check we noted that the same plaques were developed on the oral mucosa of the son of our patient, so we wanted to document the case, after obtaining the written consent of the patient.
Our little patient showed an intraoral clinical condition very similar to father’s, moreover, the patient was affected by a bilateral angular cheilitis. (Fig.,)
the little son of our patient showing white plaques developed on the gingiva.
a bilateral angular cheilitis caused by Staphylococcus aureus infection.
A buffer containing patient’s saliva was submitted to a diagnostic oral microbiology laboratory: the microbiological analysis showed in the presence of Staphylococcus aureus sensitive to methicillin (MSSA) in the oral cavity of our young patient, while, no fungal infections was found.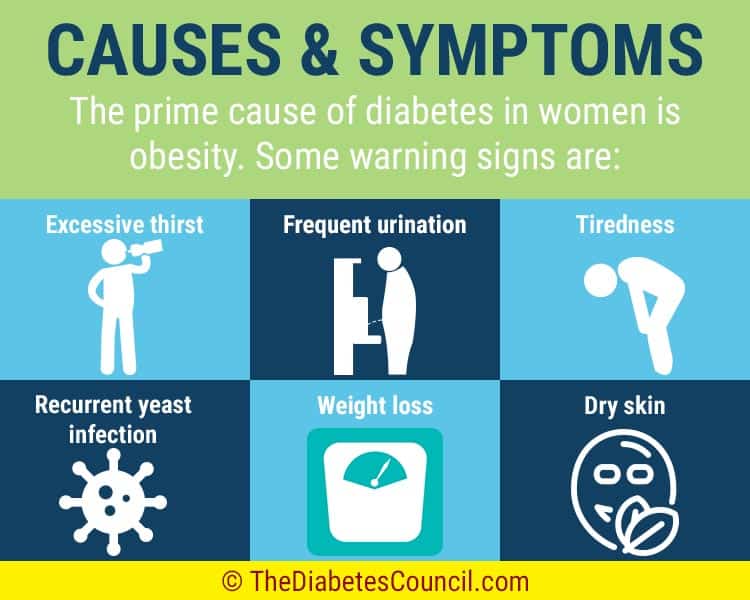
2 rinses a day with mouthwash containing chlorhexidine digluconate at 0,12% was prescribed in order to decrease the bacteria and the occurrence of relapses of angular cheilitis.
Discussion
The aspect of WSN is not strongly pathognomonic. It’s important to perform careful clinical and histological examinations to differentiate this benign condition from other potentially pre-malignant lesions as well as oral lichen planus, keratosis follicularis, candidiasis, lichenoid reactions and lupus erythematosus12.
Early diagnosis of this lesion is important, because it allows us to exclude other more serious diseases. In the most part of cases, WSN requires no treatment because of its benign and asymptomatic behaviour: up to now, no protocol of treatment for this condition was standardized 13. Even if WSN is a painless condition, sometime a correlated painful symptomatology was reported 5,10,11.
Antibiotic treatment with oral penicillin 10, ampicillin 5,11, and tetracycline has achieved a moderate success; some authors have also suggested the use of tetracycline mouthwashes. In our experience, we have achieved excellent results even with chlorhexidine digluconate rinses, considering that our treated cases were both infected by Staphylococcus aureus. WSN is not considered a bacterial disease; however, since antibiotic therapy is able to reduce the symptomatology occasionally occurred, it is possible that infections may play a role in the pathogenesis of this disease 14. Furthermore, the corrugated plaques and the altered texture of the mucosa create the right conditions for the colonization and the development of microbial species such as saprophytic bacteria or fungal species. In these 2 reported cases, the wide part of mucosa interested by the plaques of the WSN is a condition which promotes the grown of the Staphylococcus aureus 15.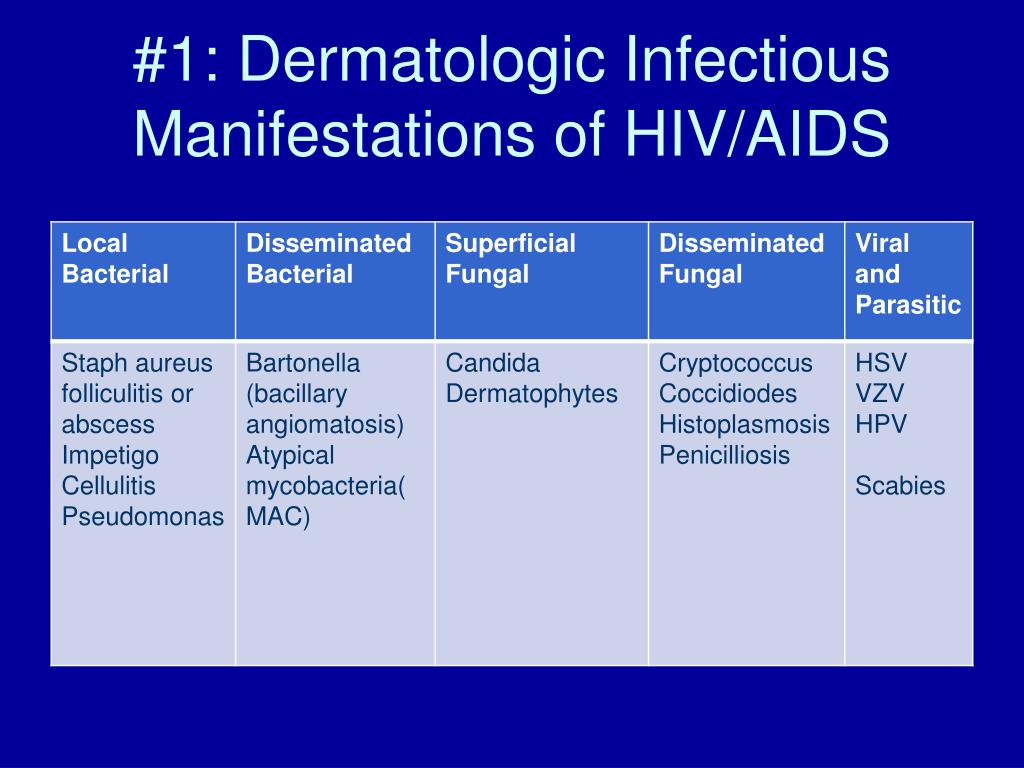
Conclusions
In all reported cases, the patients affected by WSN achieve a condition of clinical stability between 20 and 30 years, moreover, have never been described any malignant transformation of the interested mucosa16; however, if a Staphylococcus aureus infection is developing, there may be periods of exacerbation and remission of the symptoms: so we suggest to take care of the oral hygiene and to daily use a mouthwash containing chlorhexidine 0.05% in order to prevent the growth of most dangerous species of bacteria, especially the Staphylococcus aureus as we reported in our communication.
Authors’ Contributions
MM and SB participated in the clinical and pharmacological management of the treated cases.
MT drafted the manuscript and revised the literature sources.
FI participated in the follow-up examinations.
All authors read and approved the final manuscript.
Consent Statement
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
1. Cannon AB. White sponge nevus of the mucosa (naevus spongiosus albus mucosae) Arch Dermatol Syphilol. 1935;31:365. [Google Scholar]2. Woo S-B. Diseases of the oral mucosa. In: Mckee PH, et al., editors. Pathology of the Skin with Clinical Correlations. 3rd ed. Philadelphia: Elsevier Mosby; 2005. p. 387. [Google Scholar]3. Frithiof L, Banoczy J. White sponge nevus (leukoedema exfoliativum mucosae oris): ultrastructural observations. Oral Surg. 1976;41:607. [PubMed] [Google Scholar]5. Sadeghi EM, Witkop CJ. The presence of Candida albicans in hereditary benign intraepithelial dyskeratosis: an ultrastructural observation. Oral Surg Oral Med Oral Pathol. 1979;48:342–346. [PubMed] [Google Scholar]6. Jorgenson RJ, Levin LS. White sponge nevus. Arch Dermatol. 1981;117:73–76. [PubMed] [Google Scholar]7. Yavazyilmaz E. et al. Oral-dental findings in dyskeratosis congenita. J Oral Pathol Med. 1992;21:280–284. [PubMed] [Google Scholar]8. Martelli Jr H, Pereira SM, Rocha TM, Santos PLAN, Paula AMB, Bonan RF. White sponge nevus: report of a three-generation family. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:43–7. [PubMed] [Google Scholar]9. López Jornet P. White sponge nevus: presentation of a new family. Pediatr Dermatol. 2008;25(1):116–7. [PubMed] [Google Scholar]10. Alinovi A, Benoldi D, Pezzarossa E. White sponge nevus: successful treatment with penicillin. Acta Derm Venerol. 1983;63:83–5. [PubMed] [Google Scholar]11. Lim J, Ng SK. Oral tetracycline rinse improves symptoms of white sponge nevus. J Am Acad Dermatol. 1992;26:1003–5. [PubMed] [Google Scholar]12. Inchingolo F, Tatullo M, Abenavoli FM, Marrelli M, Inchingolo AD, Inchingolo AM, Dipalma G. Non-Hodgkin lymphoma affecting the tongue: unusual intra-oral location. Head Neck Oncol. 2011 Jan 4;3:1. [PMC free article] [PubMed] [Google Scholar]13. Sambucety OS, López PM, Prieto MAR, Gónzalez IR, Fernández MM. Lesiones blanquecinas en la mucosa oral. An Esp Pediatr. 2001;55:159–60. [PubMed] [Google Scholar]14. McDonagh AJG. et al. White sponge naevus successfully treated with topical tetracycline. Clin Exp Dermatol. 1990;15:152. [PubMed] [Google Scholar]15. Salgodo CO, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis. 2003;36:131–9. [PubMed] [Google Scholar]16. Lamey PJ. et al. Oral White sponge naevus: response to antibiotic therapy. Clin Exp Dermatol. 1998;23:59. [PubMed] [Google Scholar]
Staph infection in nose: Symptoms, treatment, and diagnosis
A staphylococcus, or staph, infection is an infection caused by the bacteria Staphylococcus aureus.
Many people carry Staphylococcus aureus (S.aureus) on their skin or within their nose.
Here we look at the various causes and symptoms of a staph infection in the nose. We also outline the available treatment options for a nasal staph infection, as well as some tips for prevention.
Share on PinterestExcessively blowing or rubbing the nose is a possible cause of a staph infection in the nose.
The bacteria S. aureus cause staph infection.
Between 20–80% of humans carry S. aureus within their nasal passages. Most of the time, the bacteria do not cause any harm. However, if the skin of the nose becomes damaged, the bacteria can enter the wound and cause an infection.
Damage to the surface of the skin may trigger a mild to a moderate staph infection. Damage to the deeper layers of the skin may trigger a severe or even life-threatening staph infection.
Staph bacteria are contagious and can spread to other people through:
- skin-to-skin contact
- sharing personal items, such as toothbrushes, razors, or washcloths
- coughing or sneezing, although these types of transmission are less common
A staph infection in the nose can occur as a result of a scratch, sore, or other types of damage to the skin of the nose.
Some potential causes of a nasal staph infection include:
- nose picking
- excessively blowing or rubbing the nose
- plucking or tweezing nasal hairs
A person who has a nasal staph infection may develop the following symptoms:
- redness and swelling of the nose
- crusting around the nostrils
- boils inside one or both nostrils
- facial swelling
- pain
- fever
In some cases, a staph infection may resolve by itself. In other cases, a person will require treatment to clear the infection and prevent further complications.
Some people may succeed in treating minor nasal infections at home. People can soothe sores and crusting by holding a clean, warm, damp cloth onto affected areas. It is important to wash the cloth afterward to avoid spreading the bacteria.
Some people may develop pus-filled boils inside the nostrils. A doctor will need to drain the boil in order to treat the infection and promote wound healing. This procedure typically involves the use of a local anesthetic.
If a nasal staph infection does not clear up by itself, a person may need to take oral antibiotics or apply topical antimicrobial treatments.
Without treatment, staph infections may recur. This is because S.aureus remains inside the nasal passages.
Prescription antibiotic treatments can reduce numbers of staph bacteria, thereby helping to prevent the staph infection from recurring.
Researchers have been investigating the best treatment to prevent recurrent staph infections. According to a 2015 review, topical antimicrobial medications may be more effective than oral antibiotics. This is because S. aureus may have a lower resistance to topical treatments.
Practicing good personal hygiene may also help to reduce the risk of repeat infections.
If a staph infection enters the bloodstream, it can cause serious complications. We list some potential complications below.
Facial cellulitis
Facial cellulitis is a bacterial infection affecting the deeper layers of the skin. Without treatment, the condition can be life-threatening.
Symptoms of facial cellulitis include:
Cavernous sinus thrombosis
A cavernous sinus thrombosis (CST) is a blood clot that forms in the cavernous sinuses. This is the hollow space between the brain and the eye sockets.
A CST can develop when an infection in the face or skull spreads to the cavernous sinuses. Although rare, the condition can be life-threatening.
Symptoms of a CST include:
Endocarditis
An infection can sometimes spread to the inner lining of the heart chambers and valves. The medical term for this is endocarditis.
Symptoms of endocarditis include:
Pneumonia
Pneumonia is the medical term for inflammation of one or both lungs. It typically occurs as a result of infection.
In pneumonia, the tiny air sacs, or alveoli, within the lungs fill with fluid or pus. This makes it difficult for a person to breathe.
Some common symptoms of pneumonia include:
- rapid or shallow breathing
- breathlessness, even when resting
- chest pain that worsens when breathing or coughing
- rapid heartbeat
- a fever
- chills
- feeling generally unwell
- loss of appetite
Sepsis
Sepsis is a potentially life-threatening condition in which the body’s immune system overreacts to an infection. This overreaction leads to a toxic build-up of chemicals within the blood.
Symptoms of sepsis include:
- rapid breathing
- increased heart rate
- a fever
- chills
- feeling confused or disorientated
Toxic shock syndrome
Toxic shock syndrome (TSS) is a rare condition in which staph bacteria release dangerous levels of toxins into the bloodstream. TSS can be life-threatening.
The symptoms of TSS come on suddenly and worsen rapidly. They include:
- a fever
- flu-like symptoms, such as a headache, body aches, and a sore throat
- nausea and vomiting
- diarrhea
- a widespread skin rash that appears similar to sunburn
- a bright red coloring of the lips, tongue, and eye-whites
- difficulty breathing
- fainting
- confusion
There are steps a person can take to reduce their risk of developing or spreading a staph infection of the nose or skin. These include:
- regularly washing hands with soap and clean water
- showering or bathing daily to keep skin clean
- covering any cuts or wounds with sterile bandaids or dressings
- avoiding sharing personal items, such as toothbrushes, razors, and washcloths
- covering the mouth and nose when coughing or sneezing
- disposing of tissues after blowing the nose
- avoiding picking the nose
- using only sterile equipment to pluck or tweeze nasal hair, or avoiding these practices altogether
Some staph infections may resolve by themselves, while others may require treatment.
People should see a doctor if the staph infection:
- is severe
- lasts longer than a week, or keeps coming back
- is getting worse, or spreading to other parts of the face
- causes a skin rash or redness
- causes fever or chills
- causes breathing difficulty, or a change in heart rate
Anyone who has a weakened immune system should see a doctor at the first sign of a staph infection. This includes people who:
Staph bacteria commonly live inside the nose and are usually harmless. However, if the skin of the nose becomes damaged, the bacteria can enter the wound and cause infection.
A person who has a nasal staph infection may develop redness, sores, or crusting around the nostrils. A person may need antibiotics or topical antimicrobial medications to treat the infection.
People should seek treatment if their infection is severe or persistent or accompanied by other symptoms. People who have a weakened immune system should seek treatment as soon as possible to reduce the risk of complications.
Impetigo | Cedars-Sinai
Not what you’re looking for?
What is impetigo?
Impetigo is an infection of the
outer layer of the skin. It’s most often caused by the bacteria Staphylococcus aureus
(called staph) or Streptococcus pyogenes (called group A strep). Impetigo is much
more
common in children, but adults can get it too. It’s more common in the summer months.
Normally, your skin is covered by millions of bacteria. Many of these are harmless,
and some may be good for you. But sometimes harmful bacteria can grow on your skin.
If these get through the outer layer of your skin (epidermis), they may start to grow
more. This can cause impetigo.
There are 3 kinds of impetigo:
- Nonbullous impetigo. This is the most
common form in adults. It causes thick, honey-colored crusts. - Bullous impetigo. This causes large blisters on the skin.
- Ecthyma. This is a more serious form
that often results from untreated impetigo. It causes ulcerative sores that go down
into the deeper layers of the skin.
Some impetigo is caused by a type
of bacteria called MRSA (methicillin-resistant Staphylococcus aureus). This type of
bacteria is hard to kill. This type of impetigo can be hard to treat.
What causes impetigo?
Impetigo is caused by bacteria. The
most common is Staphylococcus aureus, also called staph. Streptococci bacteria can
also
cause impetigo.
Many people have these kinds of
bacteria on their body from time to time. A smaller number of people have lifelong
(permanent) colonies of these harmful bacteria on their skin. This is known as being
colonized with the bacteria. These bacteria may grow inside your nose, armpit, throat,
genitals, hands, or some other area. When these bacteria are just on top of the skin,
they often don’t cause problems or symptoms. But a small break in the skin allows
the
bacteria to cause an infection.
Who is at risk for impetigo?
People who have these bacteria on
their skin are more likely to get impetigo. You may also get impetigo if you have
a cut
that has been in contact with someone colonized with the bacteria.
These risks are higher in people with:
- Atopic dermatitis or eczema
- Diabetes
- Liver problems
- HIV/AIDS infection
- Dialysis treatment
- IV (intravenous) drug use
- Skin sores, such as from scabies
- Immune deficiencies
You may also have an increased risk
if you live or work in a place where people are in close contact. This includes dorms,
barracks, or prisons. Having a family member with impetigo may also increase your
risk.
Not washing your hands after touching someone with impetigo greatly increases your
risk
of getting the infection.
What are the symptoms of impetigo?
Impetigo causes red bumps to form
on your skin, often on your face, arms, or legs. These bumps then become blisters.
These
blisters burst and scab over, forming a yellow-brown crust. The skin may also look
reddish or raw where the blisters have popped open. The rash often starts in a single
spot, but it may spread to other areas of the body with scratching. The rash may be
slightly painful to the touch, and it may also itch.
If you have the bullous type of impetigo, you may have larger blisters filled with
a clear fluid. If you have ecthyma, you may have deeper sores with a yellow crust
and purple borders.
How is impetigo diagnosed?
You may be diagnosed by a general
healthcare provider or a dermatologist. A dermatologist is a healthcare provider who
specializes in skin diseases.
Your healthcare provider will ask
about your health history, symptoms, and if you’ve been in contact with anyone that
has
impetigo.
You will also have a physical exam,
including a close exam of your skin. Your healthcare provider will need to make sure
your symptoms aren’t caused by other skin problems that have similar symptoms. They
may
take a sample of pus from one of your blisters to check for bacteria.
How is impetigo treated?
Antibiotics are the main treatment
for impetigo. If you have only a few affected spots that don’t go deeply into your
skin,
you may be given an antibiotic cream or ointment. You apply this antibiotic to the
affected areas of your skin.
If you have a more severe
infection, you will likely need to take an antibiotic by mouth. Your healthcare provider
may choose an antibiotic based on the type of bacteria that caused your impetigo.
It’s
very important to take your antibiotics for as long as your provider prescribes, even
if
your infection goes away before then. Otherwise there’s a risk your infection will
return.
Your healthcare provider may also
give you instructions about cleaning the affected areas with soap and water several
times day. You’ll also need to wash your hands often. This is to help prevent spreading
the infection to others. You may also need to cover the affected areas of your body.
This can help prevent you from spreading the infection to other areas of your body
and
to other people.
Often the infection will go away in
a week or so with the correct treatment. Only rarely does the infection leave scars.
Getting treatment quickly also reduces the chances of serious complications.
If you get repeated bouts of
impetigo, your healthcare provider may need to check you for a skin problem that makes
it hard for you to fully fight the infection.
What are possible complications of impetigo?
Untreated impetigo can lead to deeper infection, especially if it’s caused by staph.
Possible complications include:
- Deeper infection of your skin
(cellulitis) - Infection of the lymphatic system
(lymphangitis) - Bacteria in the blood
(bacteremia)
These may need more antibiotic treatment and other types of medical support.
Rare complications include:
- Glomerulonephritis. This is inflammation in the filtering
part of your kidney. This may happen after some kinds of Streptococcal infections.
This may cause only minor problems. But it can cause sudden temporary kidney
failure. - Rheumatic fever. This can also be caused by a
Streptococcal impetigo infection. This disease may affect the heart, joints, skin,
and brain.
What can I do to prevent impetigo?
Often impetigo spreads through
direct skin-to-skin contact. You may be able to prevent impetigo by taking certain
steps. For example:
- Always wash with soap and water right after you touch someone with the infection.
- Don’t share personal items such as
towels or hair combs. - Wash towels and bed linens in hot water.
- Wash your hands after handling tissues that could contain germs.
- Sneeze into the crook of your arm, not into your hands, to help prevent spreading
germs.
When should I call my healthcare provider?
Call your healthcare provider if your infection is not clearing up
within a week of starting your treatment, or if your condition seems to be getting
worse.
Key points about impetigo
- Impetigo is an infection of the outer
layer of your skin. It’s often caused by the bacteria staph or strep that invades
injured skin. The rash may blister and appear red or yellow and crusty. - You may have a greater risk of
impetigo if you are colonized by certain bacteria, or if you have certain health
conditions. - Antibiotics are the main treatment for impetigo. You may need to apply a cream to
your skin. Or you may need to take an antibiotic by mouth. - Untreated impetigo can cause serious
complications, such as deeper infection. Getting treatment quickly can help reduce
the risk of complications. - Handwashing and other steps may help
prevent getting or spreading impetigo.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells
you. - At the visit, write down the name of a new diagnosis, and any new medicines, treatments,
or tests. Also write down any new instructions your provider gives you. - Know why a new medicine or treatment is prescribed, and how it will help you. Also
know what the side effects are. - Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that
visit. - Know how you can contact your provider if you have questions.
Medical Reviewer: Michael Lehrer MD
Medical Reviewer: Marianne Fraser MSN RN
Medical Reviewer: Raymond Kent Turley BSN MSN RN
© 2000-2021 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional’s instructions.
Not what you’re looking for?
What Does MRSA Look Like?
You get a small cut, and after two or three days, you notice it’s not healing. The area is swollen, oozing and hot to the touch. You may wonder why it’s not getting better.
What is MRSA?
MRSA (pronounced “mur-sa”) stands for methicillin-resistant staphylococcus aureus. It refers to a group of staph bacteria that are resistant to common antibiotics. MRSA germs can get into a skin injury, such as a cut, bite, burn or scrape.
Scott Hultman, M.D., M.B.A., a plastic and reconstructive surgeon and director of the Johns Hopkins Burn Center, says that MRSA is becoming more common. “If you spend time in locker rooms, schools, gyms or even prisons, be very careful to avoid cuts and scrapes, and if you get a skin injury in any of these environments, wash it thoroughly.”
Hultman notes that you’re more likely to get a MRSA infection if you have a weakened immune system caused by transplant drugs, HIV, hepatitis C or immune-modulator drugs for psoriasis or rheumatoid arthritis.
Do I have MRSA?
If you’re concerned about a skin injury that’s not getting better, be on the lookout for MRSA signs and symptoms:
Other Skin Problems That Can Be Confused with MRSA
MRSA Versus Spider Bites
A MRSA infection can look like a
spider bite
, but if you didn’t see a bug or spider on you or your child, it’s best to
check with a doctor to be sure, since the treatment is different for bites
than for MRSA.
Cellulitis Versus MRSA
Cellulitis
is a deep skin infection caused by staph or streptococcus (strep) bacteria,
including MRSA. Cellulitis leads to redness, swelling, pain and heat in the
skin, sometimes in a large, diffuse area.
MRSA Versus Impetigo
Impetigo, a skin infection most commonly seen in children, is usually
confined to the upper levels of skin. It can looks very similar to MRSA in
some cases, with sores and redness. Impetigo is highly contagious, so you
should see a doctor if you suspect either of these conditions.
What to Do If It’s MRSA
If a doctor confirms you have MRSA, don’t panic. When treated in time, the
outlook in most cases is good.
Hultman explains: “Many MRSA infections can be treated with oral
antibiotics, but some require intra-venous medications, so make sure you
and your doctor check the sensitivities found on laboratory testing.”
“Most over-the-counter ointments do not cover MRSA,” he adds, “so we
prescribe mupirocin topically, which is very effective.
Once the infection is resolved, Hultman says it is a good idea to be tested
to see if you are a carrier. If you are, he says don’t worry — nasal
ointment prescribed by your doctor can “decolonize” you so you no longer
pose a risk to yourself and others.
Keep MRSA from spreading
You can spread MRSA to other people if their skin touches the infected
area, so keep the sore bandaged and protected. Be careful to wash all of
your clothing, bed linens, towels, etc. in hot water and bleach if
possible.
It’s super important to take all of your antibiotic medicine, even if you
feel better, since MRSA can be stubborn. Follow all of your doctor’s
instructions carefully for the best chance of avoiding a return of the
infection.
Streptococcal infection – group A
Group A streptococcal (GAS) infection is caused by bacteria known as Group A (beta-haemolytic) Streptococcus, the most common type of which is Streptococcus pyogenes.
GAS is a common infection that can cause sore throats (pharyngitis), scarlet fever or impetigo (school sores).
In rare cases it can cause a toxic shock syndrome similar to that caused by the bacteria Staphylococcus aureus, also known as ‘golden staph’. GAS is one of the possible causes of the very rare illness necrotising fasciitis (flesh-eating bacteria).
Occasionally GAS can lead to serious complications such as rheumatic fever, which can affect the heart, and kidney disease (glomerulonephritis).
Symptoms of group A streptococcal infection
Streptococcal sore throat (pharyngitis)
Typical symptoms include of streptococcal sore throat include:
- a sore, red throat with thick pus-like fluid around the tonsils
- fever and chills
- enlarged and tender lymph nodes in and around the neck
- vomiting and abdominal complaints, particularly in children.
Scarlet fever
The symptoms of scarlet fever include:
- inflammation of the throat
- a pink-red rash spreading across the abdomen, side of the chest and in the skin folds. The rash may feel like sandpaper when touched
- a bright red tongue (known as ‘strawberry tongue’)
- paleness around the mouth.
Impetigo
Streptococcal bacteria can cause impetigo, or ‘school sores’. However impetigo can also be caused by the Staphylococcus aureus (‘golden staph’) bacteria.
Symptoms of impetigo include:
- blisters, typically around the nose and mouth and the legs
- fever and swollen lymph nodes in severe cases.
Diagnosis of group A streptococcal infection
For cases of pharyngitis and scarlet fever, the routine method of diagnosis is identification of the organism from a throat swab. Blood tests may also be ordered.
Impetigo is diagnosed by taking a swab of the blisters or crust of sores and checking for the presence of bacteria.
Toxic shock syndrome is diagnosed by examining symptoms and in some cases, by taking blood tests.
You can contract group A streptococcal infection after contact with infected persons. The bacteria are present in saliva and nasal discharge so sneezing, coughing and shaking hands can spread the bacteria.
In rare cases the infection can also be contracted from contaminated foods including:
- milk and milk products
- eggs.
Impetigo is highly contagious. People with skin lesions or blisters should not handle food until the infection has cleared.
Treatment for group A streptococcal infection
A course of antibiotics is the standard treatment for group A streptococcal infection; the duration will depend on the site of infection. Antibiotics which may be prescribed include:
- penicillin
- a cephalosporin or macrolide antibiotic if you are allergic to penicillin
- antibiotic ointments for impetigo.
Children with group A streptococcal infection
If your child develops group A streptococcal infection, including scarlet fever or impetigo:
- keep them away from children’s settings such childcare centres or school until your child has received at least 24 hours of antibiotic treatment and they feel well
- ensure your child completes the entire course of antibiotics
- if your child has impetigo, the child can return to school after commencing antibiotic treatment. Make sure all exposed sores are covered with a watertight dressing.
The infectious period for group A streptococcal infection
If your streptococcal infection is not treated, you could remain infectious for between 10 and 21 days. An untreated infection with a pus-filled discharge can remain infectious for months.
It is important to complete any course of antibiotics you are prescribed.
Where to get help
Here’s the Skinny On Skin Infections
It’s easy to get the care you need.
See a Premier Physician Network provider near you.
Your skin is like a protective coating that prevents infection from entering your body. But sometimes a break in the skin lets infections in. Here’s a review of the most common skin infections.
Bacterial Infections
Cellulitis and other staph infections, including MRSA are common yet should not be ignored. Bacteria gets into the deep layers of your skin through cracks or wounds, and into the tissue below the skin. It makes your skin look swollen and red and become warm and painful. You might also get a fever. These infections are usually found on your lower legs, face and/or arms. With proper treatment of an oral antibiotic, cellulitis and other staph infections will improve significantly in a few days. But without antibiotics they can spread quickly and become life-threatening.
Impetigo is a contagious skin infection common in children around ages 2 to 6. The bacteria usually get into the skin through a cut, scratch, or insect bite. Impetigo looks like small red bumps or pimples surrounded by red skin. It appears on your face, arms, and legs. When the sores break open they cause a crust that itches. Scratching the sores causes them to spread across your body. The infection can spread to others who come in contact with the sores, or who touch discharge from the infected person’s nose. Impetigo is treated with antibiotics and goes away within weeks or sooner.
Having good hygiene is the number one step in prevention.
Viral Infections
Shingles is caused by the same virus that causes chickenpox. Once you get chickenpox the virus stays in your body. Many years later, usually when you’re in your 50s or older, the virus can cause shingles. The first symptoms of shingles are burning or shooting pain and tingling or itching, usually on one side of the face or body. The pain can be mild to severe. Up to two weeks later (sometimes within just a day) a rash or blisters appear, usually as a stripe. You might also get a fever, headache, chills, and/or upset stomach. It’s important to see a doctor for advice and treatment.
The worst cases of shingles cause severe pain, vision loss, and hearing or balance problems. Such issues can be temporary or permanent. Typical cases of shingles go away in two to four weeks.
Shingles isn’t contagious, but if you’ve never had chickenpox you can catch it from someone who has shingles. Prompt treatment of shingles within the first couple of days of the rash can significantly lessen the severity of symptoms and potential long-term complications. There are also vaccines to help prevent shingles.
Herpes simplex is a virus that causes pustules on the skin, which get crusty once they open. Once you get herpes you will have the virus for life. There currently is no cure. Cold sores (also called fever blisters) and genital herpes are two forms of the virus. Over-the-counter medication for cold sores can speed the healing. Oral prescription medication is available for genital herpes to help manage outbreaks. Herpes simplex is contagious. It spreads easily through skin-to-skin contact including saliva, handshakes, kissing, and unprotected sex.
Warts are a viral infection that frequently appear on your hands, feet, elbows, and near the knees. A tiny cut or scratch on the skin can provide the opening needed to get a wart. The HPV virus that causes warts can be passed from person to person by close physical contact or from touching something that a person with a wart touches, like a towel, bathmat, or a shower floor. When warts are transmitted sexually they appear in the genital area. Over-the-counter medications are available to treat warts, but they should not be used on the face or genital area. Some warts require treatment by your physician and could take from several months to years to go away.
Fungal Infections
Fungi are usually found in moist areas of your body where skin meets skin: between the toes, in the genital area, under the breasts, and in excessive skin folds. Common fungal infections are:
Athlete’s foot usually occurs in the space between your toes. It causes itching, burning, scaly skin. Over-the-counter antifungal creams usually are all that is needed to treat athlete’s foot. For more serious cases, see your doctor for a prescription medication. It can be spread through contaminated floors, towels, or clothing.
Ringworm has nothing to do with a worm. This skin infection gets its name because of the way it looks, like a red ring on the skin (the skin is clear inside the ring). The rash is red and itchy and is spread by skin-to-skin contact with a person or animal who has the infection. An over-the-counter antifungal cream will effectively treat mild cases of ringworm. More severe cases require oral prescription medication and may take several weeks to clear up.
Jock itch gets its name because it is common in athletes and people who sweat a lot. This skin infection is an itchy, red rash on your genitals, inner thighs, and buttocks. Like other fungal infections, it occurs in warm, moist areas of your body, and it is spread by skin-to-skin contact or by sharing contaminated towels or clothing. An over-the-counter ointment, lotion, powder or spray often clears it up quickly. If not, or if it keeps coming back, your doctor may prescribe a stronger medication.
Yeast infections (Candidiasis). Candida yeast lives in your mouth, digestive tract, and vagina, and typically causes no harm. But under certain conditions (hot, humid weather; tight clothing; poor hygiene; infrequent diaper or underwear changes) the yeast can become a rash with a thick, white, pasty residue. It causes itching and burning in the vaginal area. These infections are more common in women who are taking antibiotics, have a weakened immune system, high levels of estrogen, or uncontrolled diabetes.
Treating a yeast infection requires an antifungal medication for up to a week. Some are available over-the-counter, but some doctors prefer a prescription medication. An oral medication also is available by prescription.
Risk Factors For Skin Infections
Everyone is at risk of getting skin infections, but your risk is higher if you:
- Have a suppressed immune system
- Have diabetes
- Have HIV, AIDS, or hepatitis
- Are elderly
Preventing Skin Infections
Having good hygiene is the number one step in prevention. Follow these guidelines to stop the spread and to prevent getting an infection:
- Wash hands thoroughly and often
- Shower before and after being active
- Keep your skin dry
- Don’t share clothing or towels
- Avoid tight-fitting clothes
- Wear shoes in public places
- Wipe down equipment before and after use at the gym
It’s easy to get the care you need.
See a Premier Physician Network provider near you.
Sources: Merck Manuals; American Family Physicians; Centers for Disease Control and Prevention
Staphylococcal infection
Staphylococcus aureus is an abbreviation for a common bacterium called Staphylococcus aureus. Staphylococcus bacteria are often present on the skin without causing infection. The infection develops if they penetrate the skin. This causes redness, tenderness, swelling, and sometimes runny discharge.
MRSA stands for Methicillin-Resistant Staph Aureus Unlike common staphylococcal infections, MRSA bacteria are resistant to common antibiotics and are more difficult to treat.In addition, MRSA bacteria are more toxic than regular staphylococcus bacteria. They can spread quickly in the body and cause life-threatening illness.
MRSA is transmitted by direct physical contact with bacteria. MRSA is also transmitted through items contaminated by a person carrying the bacteria, such as bandages, towels, bedding, or sports equipment. Usually bacteria are not transmitted through the air. However, they can be spread by direct contact with fluids from coughing or sneezing.If you have a skin MRSA infection, there is a risk of recurrence in the future.
If an MRSA infection is suspected, the doctor may do a wound culture to confirm the diagnosis. If an abscess is present, it can be drained. You will likely be prescribed one or more antibiotics that work on your MRSA.
Home Care
Take antibiotics exactly as prescribed. Even if you feel better, do not stop taking them until they run out or until you are instructed to stop taking them from your healthcare provider.
If you have been prescribed an antibiotic ointment, use it as directed.
Wash your entire body (from scalp to toes) with special soap daily for 5 days. Brush your fingernails twice a day for 1 minute with a special soap and brush.
Wounds should be covered with clean, dry dressings. If the dressings become dirty, they must be replaced. Wash your hands thoroughly every time you change dressings or touch a wound.
If you have extended nails or nail polish, they must be removed.
Treating family members
If you have been diagnosed with a possible infection with an MMR, your loved ones living with you are at a higher risk of having bacteria on your skin or nose, even if there are no signs of infection. Bacteria must be removed from the skin of all family members at the same time so that they do not pass from one to another. Instruct them on how to remove the bacteria:
Family members should use a special soap as described above.
If a family member has a skin infection, a doctor must treat it. Washing is not enough to cure an MRSA infection.
Clean countertops and children’s toys.
Each family member should only use their own personal items, such as toothbrushes or shaving razors. In this case, the use of shared glasses, plates and cutlery is allowed.
Prevent the spread of infection.
Wash your hands often with plain soap and warm water. Be sure to clean under your nails, between your fingers and your wrists. Dry your hands with disposable towels (such as paper). If soap and water are not available, you can use an alcohol-based hand sanitizer. Rub the antiseptic all over your hands, fingers, and wrists until it dries completely.
Do not use other people’s personal items such as towels, shaving razors, clothing or uniforms.Wash bed linen, towels and clothing in hot water and detergent. Set the dryer to a high temperature to kill any remaining bacteria.
If you go to the gym, wipe your equipment with an alcohol-based antiseptic before and after each use. Also, wipe down any handles and areas you grasp with your hands.
If you exercise, shower with regular soap after each workout. Use a clean towel every time you shower.
Follow-up
Come to your doctor’s appointments or as directed by our staff. If culture of wound secretions was taken, obtain results at the specified time. If any changes are made to your course of treatment, you will be informed of them.
If you have been diagnosed with MRSA, in the future you will need to tell healthcare staff that you have been treated for this infection.
When to seek medical attention
Contact your healthcare provider for any of the following:
Increasing redness, swelling, or pain
Red streaks in the skin around the wound
Weakness or dizziness
Pus or discharge from the wound
Fever higher than 100.4 ºF (38.0 ºC) or as directed by your healthcare professional
Scientists have found a way to deal with Staphylococcus aureus
22.08.2019
Serious infections with S. aureus bacteria are often difficult to treat because the pathogens are resistant to antimicrobial drugs. But scientists at the University of North Carolina School of Medicine have found a way to improve the situation: they figured out how to make these dangerous bacteria more susceptible to the effects of common antibiotics.
Give me prices
In an article published in the scientific journal Cell Chemical Biology , American researchers talked about their recent discovery.They found that molecules from the polysaccharide family – rhamnolipids – can potentiate the action of aminoglycoside antibiotics such as tobramycin against S. aureus by a factor of hundreds, including hardy strains that cannot be overcome otherwise. According to scientists, rhamnolipids modify the cell membranes of Staphylococcus aureus, making them more flexible and malleable, which makes it easier for the antibiotic to penetrate them.
“There is a great need for new – more effective – methods of fighting bacteria that will tolerate or develop resistance to standard antibiotics,” said lead author Brian Conlon, assistant professor of microbiology and immunology at the University of North Carolina School of Medicine.“In pursuit of such methods, we found that altering the permeability of bacterial cell membranes to better absorb aminoglycoside by them is an extremely effective strategy in the fight against Staphylococcus aureus.”
S. aureus is considered the most dangerous of all common staphylococci. It can cause a wide range of diseases, from mild skin infections to life-threatening conditions such as pneumonia, meningitis, and sepsis. This type of bacteria is one of the five most common causes of nosocomial infections, often causing postoperative wound infections.About 30% of the world’s population are permanent carriers of Staphylococcus aureus, which can live on the skin and mucous membranes of the upper respiratory tract.
According to the US Centers for Disease Control and Prevention, S. aureus caused nearly 120,000 cases of serious bloodstream infections in the United States in 2017, of which 20,000 were fatal.
Standard control methods for most strains of Staphylococcus aureus are ineffective, either because bacteria are genetically resistant to certain antibiotics, or because they grow in the body in a special way that makes them less vulnerable in the first place.For example, S. aureus is able to adapt its metabolism to survive in areas of low oxygen – in tissues with purulent inflammation or mucus-filled lungs in people with cystic fibrosis. In such environments, the bacterial membrane becomes relatively impermeable to aminoglycoside antibiotics such as tobramycin.
Brian Colnon and colleagues, including first study author Lauren Radlinsky, discovered two years ago that rhamnolipids significantly potentiate the action of tobramycin against standard test strains of Staphylococcus aureus.These polysaccharides are small molecules produced by Pseudomonas aeruginosa bacteria, known as Pseudomonas aeruginosa, and serve as their natural weapons against other microorganisms in the wild. In high doses, they perforate the cell membranes of the enemy bacteria.
Then scientists found out that rhamnolipids significantly increase the absorption of tobramycin molecules, even in low doses, in which they do not have their own antibacterial effect.In a new study, they tested a combination of rhamnolipid and tobramycin against populations of S. aureus that cannot be dealt with in routine clinical practice. Scientists have found that polysaccharides enhance the action of tobramycin against:
- bacteria S. aureus growing in areas with low oxygen content;
- methicillin-resistant S. aureus , which is a family of dangerous species of Staphylococcus aureus with genetically acquired drug resistance;
- tobramycin-resistant strains S.aureus, isolated from patients with cystic fibrosis;
- resistant forms S. aureus , which usually have a reduced susceptibility to antibiotics because they grow very slowly.
“Dobramycin doses that usually have little or no effect on these populations S. aureus kill them quickly when combined with rhamnolipids,” says Dr. Radlinsky.
Scientists have found that even at low doses, rhamnolipids are able to alter the membrane of Staphylococcus aureus bacteria, making it much more permeable to aminoglycoside antibiotics.Each of the drugs in this family that they tested, including tobramycin, gentamicin, amikacin, neomycin, and kanamycin, showed increased efficacy. Moreover, experiments have shown that this strategy of enhancing their action works not only with S. aureus, but also with several other species of bacteria, including Clostridium difficile , which is the main cause of serious, often fatal diarrheal diseases among the elderly and patients in hospitals.
Rhamnolipids are of different types, and now scientists hope to find out if there is an optimal type among them that will most effectively fight other bacteria, being little or completely non-toxic to human cells. The team also plans to study other types of molecules that are natural weapons of some bacteria against others, in order to find new ways to increase the effectiveness of existing antibiotics.
Get a quote at the clinic
“There are many types of bacterial interspecies interactions that can potentially affect the action of our antibiotics,” says Dr. Radlinski.“We are looking for them with the sole purpose of increasing the effectiveness of modern drugs and slowing the growth of antibiotic resistance.”
- 5
- 4
- 3
- 2
- 1
(43 votes, average: 3.6 out of 5)
Features of the course of urethritis, depending on the causative agent
Bacterial urethritis. The causative agents are: staphylococci, streptococci, Escherichia coli, gardnerella, etc. Infection in the urethra can get during sexual intercourse, as well as due to its spread from the genitourinary tract with pyelonephritis, prostatitis, vesiculitis, urethral trauma.More than 230 strains of bacteria have been isolated, which, in a certain situation, are capable of causing inflammation of the urethral mucosa.
The average duration of the incubation period for bacterial urethritis is 12-14 days (from 2 to 20 days). More often, their clinical course is asymptomatic, sluggish. Less commonly, bacterial urethritis acquire an acute course.
Urethritis caused by diplococci, similar to gonococci (pseudogonococci), usually proceed as acute urethritis.
Gardnerellas, as a rule, cause low-symptom urethritis, often resulting in self-healing.
Bacterial urethritis often (in 30% or more) end with complications (balanoposthitis, epididymitis, prostatitis, cystitis, etc.).
Chlamydial urethritis.
Caused by obligate intracellular bacteria, which are the most common cause of urethritis in men. According to various researchers, 1.5 million people fall ill with urogenital chlamydia in Russia every year.
Chlamydiae undergo extracellular and intracellular stages of development. A mature extracellular infectious form is an elementary body that can penetrate intracellularly. Intracellularly, elementary bodies are transformed into reticular bodies capable of growth and division. Elementary bodies are resistant, and reticular bodies are susceptible to antibiotic therapy.
The average incubation period is 3-4 weeks. The source of infection is a patient with an asymptomatic form of an acute or chronic disease.
Transmission occurs by contact (sexual) during genital-genital, genital-anal and oral-genital contacts, as well as asexual – through the placenta, during childbirth, in a household way, due to contamination (from the genitals to the eyes with hands, in violation of hygiene rules) …
In men, chlamydial urethritis in 70% of cases proceeds as asymptomatic or asymptomatic inflammation (with scanty mucopurulent discharge), which can last for several months.Much less often (in 5%) urethritis can be acute, while inflammation is not much different from gonococcal lesions. In 25% of cases, chlamydial urethritis can have a subacute course, not much different from a chronic one, except perhaps more abundant discharge from the urethra, especially in the morning. In the initial stages of the disease, the anterior urethra is affected; in the chronic course, the inflammation passes to the posterior part of the urethra and becomes total. In 30-40% of cases, symptoms of prostatitis, vesiculitis, epididymitis, funiculitis are added.
Chlamydial infection does not cause persistent immunity, therefore, reinfection is possible due to the exchange of infection with partners. Reiter’s disease develops in 2-4% of cases against the background of chlamydial urethritis.
Reiter’s disease. It is characterized by systemic lesions of the genitourinary organs, eyes, joints (by the type of asymmetric reactive arthritis), as well as lesions of the skin, mucous membranes and internal organs. It develops as a complication of untreated chlamydia.
Trichomonas urethritis.
Caused by Trichomonas vaginalis, which is a protozoan, flagellate; it is a unicellular parasite that multiplies by longitudinal division, grows well under anaerobic conditions, and dies quickly outside the human body. Trichomonas, entering the urethra, is fixed on the cells of the squamous epithelium of the mucous membrane and enters the body through the intercellular spaces due to the presence of proteolytic enzymes on its surface (hyaluronidase, amylase, etc.), then moves subepithelially into the connective tissue, from where it enters the urogenital organs lymphogenically …
Trichomonas is sexually transmitted. Household transmission is rare. It can persist in urine for up to 24 hours, in semen for several hours, and survive in wet laundry. The incubation period for Trichomonas urethritis is on average 5-15 days. There are the following forms of trichomoniasis: acute, subacute, chronic, trichomoniasis-denunciation.
In the acute form, the inflammatory process proceeds violently with abundant mucous-foamy in the first day and with mucopurulent discharge from the second day from the urethra with frequent and painful urination.
With subacute urethritis, the symptoms are less pronounced, discharge from the urethra occurs in small quantities, purulent. The first portion of urine contains purulent flakes.
In chronic Trichomonas urethritis, itching, burning, creeping sensation in the urethra, and frequent urination come to the fore. Urethral discharge is scanty. Since in chronic urethritis, the inflammatory process passes to the posterior urethra, complications develop in the form of prostatitis, vesiculitis, epididymitis, with a prolonged course, the formation of urethral strictures is possible.
Mycoplasma urethritis.
Caused by bacteria that have a plastic membrane and contain DNA and RNA. The ability of mycoplasmas to take any form allows them to penetrate through bacterial filters.
Infection with mycoplasma infection occurs mainly through sexual contact. Established intrauterine infection of the fetus and during its passage through the infected birth canal. Mycoplasma attaches to the epithelium of the urethra, can be carried by sperm; in addition, she colonizes the foreskin.The incubation period lasts from 3 to 5 weeks.
There are no specific signs of mycoplasma urethritis. As a rule, urethritis of mycoplasma origin is chronic. In this case, there are often lesions of the prostate gland, seminal vesicle, epididymis, which leads to infertility. By attaching to the head of the sperm, mycoplasma can reduce its fertilizing ability. Under certain conditions, mycoplasma infection can cause inflammation of the genitourinary organs (cystitis, pyelonephritis).Urogenital mycoplasmosis is often combined with intestinal damage (enterocolitis).
Herpetic urethritis.
Causes two DNA serotypes containing herpes simplex viruses HSV-1 and HSV-2. Herpes is one of the most common human infections.
The disease is transmitted mainly sexually from a patient with genital herpes. Often, the genital virus is transmitted from a herpes carrier who does not have symptoms of the disease. The method of infection with the virus can be genito-genital, oral-genital, genital-anal.There is a risk of neonatal infection in newborns, which can occur during the passage of the birth canal, and in the postpartum period with active herpetic manifestations in mothers or medical personnel.
During the initial infection with the herpes simplex virus, the virus enters the cells of the susceptible surfaces of the mucous membrane or skin. Then it is captured by sensory nerve endings and transferred to the nerve cells of the dorsal roots of the ganglia, where it is stored.Infection can be latent when the virus is present in the body without causing disease; and virulent when herpes is activated and causes local lesions. The disease in this case proceeds as chronic, recurrent, cyclic with localized, less often generalized manifestations.
The initial symptoms of herpetic urethritis may be general complaints: fever, weakness, myalgia, headache. At the same time, there is a burning sensation in the urethra, which intensifies during urination, soreness of the lymph nodes.On the head, the skin of the penis, on the visible part (possibly on the invisible) of the mucous membrane of the urethra, there is a typical development of herpetic elements, accompanied by a burning sensation, itching, pain in the genital area. Initially, bubbles appear, which erode, become wet, then dry out, forming crusts, which disappear as epithelialization proceeds. Temporary hyperemia and pigmentation remain at the site of the lesion. A light yellow discharge may appear from the urethra.
Clinical manifestations of primary infection last about 3 weeks, local symptoms appear on days 2-14.Recurrent infection in the presence of antibodies to the virus is less pronounced. The clinical picture develops within 8-15 days. Relapse is facilitated by stressful situations, overheating, hypothermia, decreased body defenses, etc. Herpes, destroying the human immune system, can cause secondary immunodeficiency.
Some researchers note the connection of genital herpes with cervical cancer and prostate cancer.
Candidal urethritis.
Caused by conditionally pathogenic yeast-like candida fungi, of which there are more than 150 species.7 species are pathogenic for humans.
Genital candidiasis is more common in women, less often in men. An important role in the pathogenesis of the disease belongs to a decrease in immunity, dysbiosis, vitamin deficiency, hormonal disorders, diabetes, the state of the mucous membranes of the skin! Candidomatous lesions are often combined with other pathogens of genital infections (chlamydia, ureaplasma, viruses, etc.).
The incubation period for candidal urethritis lasts from 2 weeks to 1 month, almost always proceeds torpidly, less often subacute begins.The onset of the disease is accompanied by parasthesia, itching, burning, scanty discharge (thick, mucous). In this case, diffuse and limited whitish-gray plaques appear on the mucous membrane of the urethra, under which a sharp hyperemia is determined. Candidal urethritis often occurs against the background of treated prostatitis, epididymitis vesiculitis, cystitis caused by other pathogens.
Often with candidal urethritis, there is a lesion of the glans and foreskin of the penis.In this case, there is swelling, hyperemia of the foreskin and glans penis, with areas of a whitish-gray plaque, when removed, surface erosion and cracks are formed. Scarring of erosions and cracks in chronic course can lead to the formation of cicatricial phimosis.
The presence of various types of causative agents of urethritis requires timely access to qualified medical care, for a comprehensive examination and the appointment of competent etiotropic treatment.On the basis of our medical clinics, a comprehensive diagnosis of infections transmitted through sexual contact is carried out. The equipment of our centers allows us to treat urethritis of any etiology in a short time and with high quality
Our specialists will be happy to help you!
90,000 Staphylococcus aureus and White Staphylococcus Attack / Health / Nezavisimaya Gazeta
According to statistics, 20% of people on Earth are carriers of these types of viruses
Furuncle is a serious ailment in which you cannot do without medical help.Photo Depositphotos / PhotoXPress.ru
Furuncle (in everyday life – boil) is a fairly common ailment among adults and children. This is an acute purulent-necrotic inflammation of the hair follicle and surrounding tissue caused by the introduction of Staphylococcus aureus. In some cases, the causative agent of the infection is the so-called white staphylococcus aureus. These two types of bacteria are widespread in the environment: street dust, rooms with insufficient ventilation, homes, clothing.Staphylococci can inhabit the skin and mucous membranes of a person, without causing disease. According to statistics, 20% of people on Earth are carriers of these microorganisms.
Most often, a boil appears on such areas of the body as the armpits, chest, groin, buttocks, but it can also be on the face, in the nose, in the ear. Boils are single and multiple. In the latter case, when a rash of boils occurs, they speak of furunculosis, or staphyloderma.
Among the causes of this skin disease, we should first of all note weakened immunity and metabolic disorders, especially carbohydrate metabolism.In addition, pollution and microtrauma of the skin, non-observance of hygiene rules, hypovitaminosis, poor nutrition, chronic ailments, such as diabetes mellitus, contribute to its appearance.
The initial signs of the onset of this disease include itching and tingling in a limited area of the skin. Then, at the site of inflammation, a small, painful red nodule forms when touched. It gradually increases in size and soon an abscess appears in its center.If you experience these symptoms, you should see a doctor. It should be emphasized that in no case should you squeeze out and pierce the boil! Such self-medication can lead to such serious complications as sepsis (blood poisoning) or acute thrombophlebitis (inflammation of a vein, accompanied by the formation of a blood clot).
The greatest threat is a boil located on the face, especially in the area of the lips and nose. Here is an extensive network of blood and lymphatic vessels, contributing to the rapid spread of infection.So, it can enter the brain and cause purulent meningitis (inflammation of the lining of the brain). Other possible complications include lymphangitis (inflammation of the lymphatic vessels) and regional lymphadenitis (inflammation of the lymph node).
In a word, a boil is a serious ailment in which you cannot do without medical help. It is all the more necessary if the patient has a fever and signs of intoxication (poisoning) appear – weakness, headache, nausea.
First of all, the patient needs good rest and good nutrition. As for drugs, vitamins and drugs are prescribed to strengthen the immune system. If necessary, antibacterial drugs are used, the action of which is aimed at preventing complications. A medical procedure such as a patient’s own blood transfusion also has a good effect. Diet plays an important role in treatment. So, in the diet, you should limit the use of carbohydrate and fatty foods, hot spices.The menu can include boiled meat and fish, black bread, buckwheat and oatmeal, rich in B vitamins, as well as dairy products.
As for local treatment, at the initial stage it consists in treating the area of inflammation with an antiseptic solution. This procedure is repeated when the boil ripens and opens. To accelerate the maturation process, physiotherapeutic procedures are shown to the patient in the absence of temperature. After opening and removing the pus, a bandage with antimicrobial ointment is applied to the area.With recurrent boils, a course of immunotherapy is carried out using a special vaccine. In cases where the boil threatens to turn into an abscess (abscess), they resort to surgical intervention.
The best preventive measure is a healthy lifestyle that has a positive effect on the immune system. And this, in turn, helps to strengthen the body’s defenses against the introduction of the pathogen. It is necessary to eat regularly and fully, to prevent violations of the work and rest regime, to observe the rules of personal hygiene.In addition, it is important to temper the body, exercise and exercise.
Why does the child have seizures?
Almost every wound in the area of the outer and inner surfaces of the lips, as well as the corner of the mouth, can be called a bite. The exception is traumatic injuries to the skin and mucous membranes, which are quite common in children. Such wounds, although they resemble seizures, have a completely different origin.
In short, a child’s seizure can occur due to infection, allergic reactions, vitamin deficiency.In most cases, seizures in children are caused by streptococci.
Although, according to pediatricians, the most common cause of a child’s seizure is a deficiency in riboflavin, which is essential for healthy skin and normal hair and nail growth. Also, seizures often occur due to a decrease in immunity and certain diseases. Many children with seizures also have a history of chronic tonsillitis, caries, frequent colds and viral diseases. Among the reasons for a child’s seizure, there may also be staphylococci, streptococci, fungal diseases, helminthic invasions.Timely treatment of such skin lesions helps to get rid of such unpleasant consequences.
Several factors play a role in the etiology of true seizure in children. The most important of these are:
- Microbes;
- Allergic reactions;
- Various diseases and pathological abnormalities in the body;
Regardless of the root cause of the seizure in children, all the same, its central link is the microbial factor.In this case, the pathogens are ordinary microorganisms that normally live on the surface of the skin. But, when the child’s body is healthy, then such microbes do not cause any manifestations. As soon as there is a decrease in protective forces, they immediately begin to actively multiply, causing inflammation of the skin with the formation of wounds on the lips or in the corners of the mouth (seizures).
With regard to specific types of pathogens that provoke the formation of seizures, the main role belongs to streptococcal and fungal infections.It is these two classes of microbes that live on the surface of the skin in children and are capable of causing inflammatory damage to the surface layers of the skin, which ends in the formation of a small ulcerative surface, which is called a seizure.
Important! For the occurrence of seizures, a decrease in the immune function of the child’s body must occur, against which the conditionally pathogenic microflora (fungi and steptococci) is activated. Sometimes this condition occurs as a result of infection by these microbes from the environment.
The following factors can lead to this very decrease in immune surveillance:
- Colds;
- Increased body temperature;
- Allergic reactions;
- Foodstuffs, toys and objects infected with pathogenic microbes, which the child pulls into the mouth;
- Anemia of various types and origins;
- Hypovitaminosis;
- Diseases of the immune system;
- Diseases of the blood system;
- History of chemotherapy.
The most important thing is that biting in children is not a frequent phenomenon. But, if they arise, then, as a rule, they are worn for a long time. Most of all, children are prone to their appearance in transitional age periods (6-8 years old and 13-17 years old).
Symptoms of a child’s seizure
Among the first symptoms of a seizure in a child, small bubbles appear in the corners of the mouth, which eventually burst, and erosion forms in their place. The skin of the corners of the lips becomes wet and bleeds, microcracks appear.Erosion heals, then becomes inflamed again. Children may experience painful sensations that prevent them from eating and talking.
Treatment for a child’s snack
Treatment of a jam should be comprehensive. Before starting treatment, laboratory diagnostics are performed to identify the pathogen and implement more effective treatment. They also do a general blood test, sowing feces for enterobiasis and dysbiosis, and examine the thyroid gland. In addition to antibacterial ointments and antiseptic lotions, multivitamins, immunostimulants are prescribed, and dysbiosis is treated.Correction of the diet is carried out: the consumption of dairy products, vegetables and fruits is increased.
If the child does not bite
Sometimes it happens that seizures do not respond to local treatment for a long time. This is possible, even despite the use of different combinations of funds, the action of which is aimed at different causes and mechanisms of the development of this problem. This situation clearly indicates a serious weakening of the body’s immune and protective resources.Therefore, every mother is obliged to take this fact into account. After all, children with such problems are subject to careful examination:
- Pediatrician examination;
- Consultation with a dermatologist;
- General analysis of blood and urine;
- Biochemical blood tests;
- Sowing of seizures on microflora and its sensitivity to the action of specific drugs;
This will help to establish the true cause of the formation of seizures in the child and their resistance to local treatment.
Serious health problems are always hidden behind a long-term non-healing seizure. The main thing is to identify them in time. This will not only get rid of the seizure, but also prevent the progression of the causative disease.
Additional measures
For treatment-resistant wounds in combination with local preparations, the following may be prescribed:
- Antibiotics for systemic use: azithromycin, flemoxin, augmentin in small doses;
- Antifungal agents: fucis, fluconazole, nystatin;
- Means for strengthening the immune system;
- Vitamins: vitamins A, E, C, B, multi-tabs, kinder biovital.
Do not self-medicate, consultation with a dentist is required.
90,000 Inflammatory diseases of female genital organs
The problem of inflammatory gynecological diseases occupies an important place in the activities of an obstetrician-gynecologist.
These diseases in gynecological patients occur much more often than other diseases of the genital organs.
The importance of inflammatory diseases is especially great, since it is known that they are often exacerbated, leading patients to disability and even disability.In addition, inflammatory processes of the genital organs often lead to violations of menstrual function, cause infertility, general intoxication of the body with the involvement of the nervous system, liver, kidneys and other vital organs and systems in the pathological process.
The cause of the development of inflammatory diseases of the female genital organs is usually microbial or viral pathogens.
Routes of entry of microbes into the genitals:
- Sexual – active transport of microbes from the vagina to the overlying organs is realized by spermatozoa and Trichomonas.Sperm cells have a negative charge, which is a kind of receptor for microbes.
- Passive transport (independent spread of microbes and viruses through the genitals).
- Hematogenous transport (from other organs with blood flow).
- Lymphogenic (through the lymphatic system), for example, from the intestines with purulent appendicitis.
Factors contributing to the spread of infection (provoking factors):
- Hypothermia, weakening of the general defenses of the body as a result of diseases of other organs and systems.
- Physiological (menstruation, childbirth) or artificial (abortion, intrauterine devices, intrauterine diagnostic and therapeutic interventions, operations on the abdominal organs, IVF, etc.) weakening or damage to the protective (barrier) mechanisms of the cervix.
- Social factors: chronic stressful situations, low standard of living (inadequate and inappropriate nutrition, unfavorable living conditions), chronic alcoholism and drug addiction.
- Behavioral factors: early onset of sexual activity, high frequency of sexual intercourse, a large number and frequent change of sexual partners, while using hormonal rather than barrier contraception, unconventional forms of sexual intercourse (orogenital, anal), sexual intercourse during menstruation, frequent douching and self-medication, improper use of intravaginal tampons, etc.
The onset of the disease is often associated with a change in sexual partner.
Experts classify inflammatory diseases of the female genital organs by the causative agents that caused them, by the place of localization, by the duration and severity of symptoms.
By the type of pathogen diseases in gynecology can be specific and non-specific:
- Specific inflammations are caused by sexually transmitted infections. These include HIV, gonorrhea, herpes, trichomoniasis, gonococcus, Trichomonas, chlamydia and others.Sometimes several infections can act as pathogens at once.
- Nonspecific inflammations are caused by a woman’s own flora, which is activated if the body malfunctions: E. coli, streptococcus, staphylococcus, etc. In the past few years, viruses and protozoan fungi, which are normally part of the normal microflora of the vagina, have become more and more problematic for women.
As such, there is no difference between specific and non-specific diseases, but there is a general rule – to begin treatment immediately after the first symptoms appear.
By the nature of inflammation can be acute, subacute, chronic and exacerbated:
- The acute course of the process occurs for the first time and is accompanied by vivid clinical manifestations.
- The subacute also worries the woman for the first time, but it is not so pronounced.
- Chronic course lasts more than four weeks. Complaints from the patient during this time, as a rule, are absent and appear only with an exacerbation of the chronic process.Complaints may also be associated with complications of the chronic process that have already occurred (menstrual dysfunction, infertility, dysfunction of other organs and systems).
The course of the inflammatory process depends on the nature of the pathogen and the characteristics of the defenses of the body of women. If the body’s defenses are disrupted, the process may spread (sepsis).
At the site of the lesion female diseases are divided into two types – lesions of the upper and lower genitals.
Lesions of the upper section combine the following diseases: salpingo-oophoritis (inflammation of the ovaries and fallopian tubes), endometritis (inflammation of the mucous membrane of the uterine body), pelvioperitonitis (inflammation of the peritoneum), parametritis (inflammation of the peritoneal tissue), tubo-ovarian abscess (purulent inflammation of the uterine appendages).
The most common inflammatory disease in women is salpingo-oophoritis .
Symptoms:
Most often, acute, purulent salpingo-oophoritis begins acutely:
- Fever, sometimes accompanied by chills.The range of temperatures can be different, characterized by an evening rise in temperature with normal or subfebrile readings in the morning.
- Pain in the lower abdomen. They arise sharply. At the onset of the disease, they are usually local in nature, and the patient can clearly indicate the area of the lesion; in the presence of concomitant inflammation of the uterus and surrounding tissues, pain can be widespread and radiate to the lower back, rectum and thigh).
- Abundant purulent (less often serous-purulent) leucorrhoea and cuts during urination.As a rule, they are accompanied by purulent discharge from the urethra, which also leads to the appearance in patients of frequent, small portions, painful urination or severe cuts during urination.
- Subsequently, symptoms of purulent intoxication (weakness, tachycardia, muscle pain, dry mouth), dyspeptic and emotional-neurotic and functional disorders join.
Complete cure, as a rule, does not occur, more often the disease acquires a chronic course with periodic exacerbations.Exacerbation of chronic salpingo-oophoritis can begin under the influence of many external factors: hypothermia, overheating, fatigue, less often associated with reinfection. During the period of exacerbation, the temperature rises, pains in the lower abdomen appear or intensify, and the amount of discharge increases. Usually, the pain intensifies before and during menstruation, sometimes the cycle is disrupted. Up to half of patients note sexual dysfunctions: libido disappears, coitus becomes painful. With a prolonged course and frequent relapses, the urinary, nervous, endocrine, vascular systems are involved in the pathological process, and the disease takes on the character of a polysystemic process.
Endometritis
Symptoms:
The acute form of the disease usually develops after undergoing medical and diagnostic interventions on the uterus, operations. Predisposing factors are the leaving of the membranes in the uterus during abortion, blood clots, a large number of pathogenic and opportunistic (Escherichia, Proteus, etc.) microorganisms in the vaginal biocenosis.
The acute form begins with an increase in body temperature, pains appear in the lower abdomen, discharge from the genital tract of a different nature (purulent, bloody-purulent), women complain of weakness, headache.
Without treatment, inflammation can spread to all layers of the uterus and parametrium – the fiber located between the leaves of the wide ligaments of the uterus. The parameter develops. The acute form of parametritis can lead to a parametric abscess, which sometimes spontaneously opens into the rectum, uterus, abdominal cavity or bladder.
With inadequate treatment, development becomes chronic.
Chronic endometritis is characterized by light serous discharge from the genital tract, periodic uterine bleeding outside of menstruation.Sometimes the chronic process proceeds without any external symptoms, but at the same time leads to menstrual irregularities, miscarriage, infertility.
Pelvioperitonitis – inflammation of the pelvic peritoneum. More often it is a complication of the above diseases.
Symptoms: the disease is characterized by acute abdominal pain, nausea, vomiting, bloating, stool and gas retention, fever, increased heart rate. Tongue dry, coated with white bloom.With a modern (erased) course, a small severity of symptoms or the absence of some of them is possible.
Patients need special supervision in connection with the possibility of the transition of pelvioperitonitis to diffuse peritonitis, which requires an emergency operation.
Lesions of the lower section include vulvitis, colpitis (vaginitis), urethritis, bartholinitis and cervicitis (exocervicitis, endocervicitis).
Vulvitis – inflammation of the mucous membrane of the vestibule.Develops mainly in girls. Infection is facilitated by diaper rash, scratching, abrasions, endocrine pathology (IDDM), helminthic infestations, and childhood viral infections. In adults, as a rule, vulvitis is combined with inflammation of the vaginal mucosa.
Clinic: pain, vulvar edema, purulent discharge.
Bartholinitis is an inflammation of the large glands of the vestibule of the vagina. Very often, if the rules of hygiene of the genitals are not followed, various bacteria and STIs enter it.Its excretory duct is clogged and an inflammatory process occurs in the gland. One-sided lesion of the Bartholin gland is more common.
It manifests itself first by redness around the external opening of the excretory duct, then inflammatory edema can clog the duct of the gland, preventing the release of purulent secretions, which, lingering in the duct, stretches it, forming a false abscess (abscess), which protrudes the inner surface of the labia majora and closes the entrance to vagina.The body temperature may rise, soreness in the perineal region. In rare cases, the inflammatory process can directly capture the tissue of the gland, while a true abscess occurs with strong suppuration and enlargement of the gland. The large and small labia are swollen. The inguinal lymph nodes are enlarged. The body temperature rises. A true abscess differs from a false abscess in constant pain, sharp swelling of the labia, immobility of the skin over the abscess, high temperature.
The abscess can spontaneously open with the outflow of thick yellow-green contents, after which the condition improves.The inflammatory process can subside on its own (without suppuration). In this case, there is a compaction and a slight increase in the gland. However, quite often, after a while, the inflammatory process resumes and becomes more complicated.
Colpitis – inflammation of the vagina (vaginitis).
In the clinical picture there is a triad of symptoms: pain, leucorrhoea, itching.
Colpitis can be caused by gonococci, Trichomonas, chlamydia, as well as opportunistic microorganisms such as staphylococci, streptococci, Candida fungi, Escherichia coli, etc.Allocate acute and persistent vaginitis. In an acute process, women complain of itching in the vaginal vestibule, burning, pressure, heat in the genitals and small pelvis, many note dysuric disorders. Profuse discharge is characteristic – leucorrhoea. The inflammatory process caused by various pathogens has its own characteristics. For example, profuse, frothy, yellowish-green discharge with an unpleasant odor is characteristic of Trichomonas vaginitis; allocation of a white cheesy look – for a fungal.In chronic forms of inflammation, pain is absent, mainly patients complain of discharge, itching, burning, small ulceration in the vestibule of the vagina.
Bacterial vaginosis (diagnosed since 1980) Gardner’s disease. Complaints only about increased discharge of leucorrhoea (abundant discharge, foul smelling). There are no symptoms of inflammation. Often women complain of discomfort and burning sensation in the vagina. Recently, bacterial vaginosis has been considered as a kind of vaginal dysbacteriosis, which occurs when the number of lactobacilli secreting lactic acid decreases, and the pH of vaginal secretion increases (more than 4.5).This creates conditions for massive reproduction of microorganisms such as gardnerella and obligate anaerobic bacteria. This disease is rare in prepubertal girls and in postmenopausal women, which indicates the great importance of the hormonal component in the occurrence of such an imbalance.
Cervicitis is an inflammation of the cervix, which occurs as a result of penetration into the cervical canal of gonococci, Trichomonas, chlamydia, staphylococcus, streptococcus and other bacteria, less often viruses.The occurrence is facilitated by ruptures of the cervix during childbirth, prolapse of the genitals, infectious processes in the vagina and, conversely, in the internal genital organs. In an acute process, a woman is worried about weak pain in the lower abdomen, discomfort in the vagina, sometimes itching, mucous or purulent mucous discharge from the vagina, painful sensations during sexual intercourse. In a chronic process, complaints are less pronounced.
Endocervicitis – inflammation of the mucous membrane of the cervical canal.It can occur with the penetration of various bacteria (staphylococci, streptococci, gonococci, intestinal escherichia, etc.). Endocervicitis is often combined with an inflammatory process in other parts of the reproductive apparatus – colpitis, salpingo-oophoritis, erosion of the cervix.
Symptoms: mucopurulent vaginal discharge, no pain. Clinical signs are poorly expressed. In the acute stage, hyperemia around the external pharynx and mucopurulent discharge are determined. In the chronic stage, there is almost no hyperemia, the discharge remains.With a long course of the process, hypertrophy (thickening) of the cervix develops – cervicitis
Genital warts (multiple growths on the surface of the external genital organs and the vaginal opening). Can spread to the perineum, vagina, cervix. The cause of genital warts is a filterable virus (human papillomavirus), the development of the process is facilitated by abundant discharge from the genital tract with colpitis and endocervicitis. Very quickly, genital warts grow during pregnancy.
Symptoms: condylomas are most often localized on the external genitalia, perineum, around the anus. In cases of necrosis of genital warts and the addition of a secondary infection, purulent discharge appears. Vaginal and cervical warts during pregnancy and childbirth can cause bleeding. Diagnosis is by physical examination.
Examination program for pelvic inflammatory disease (PID)
Name of survey | Information that a survey can provide |
General blood test | Leukocytosis, stab shift to the left, accelerated ESR, lymphopenia in acute and 1 m variant of exacerbation of chronic PID |
SRV, seromucoids | Increased level in acute and 1st variant of exacerbation of chronic PID |
Total protein, protein fractions | Decrease in the level of total protein, albumin, increase in the content of globulins in acute and 1st variant of exacerbation of chronic PID |
Medium molecules, medium molecular peptides for the assessment of endogenous intoxication | Increase in the level (norm: average molecules -56.8 ± 1.3 U / ml; average molecular peptides -85.4 ± 1.8 μg / ml) in acute and 1st variant of exacerbation of chronic PID |
Ultrasound of the pelvic organs | Informative in combination with anamnestic, clinical and clinical laboratory data in the diagnosis of serous and purulent TOVO, abscesses of the small pelvis, pathological changes: the structure of the ovaries, adhesions, infiltrative changes in organs and tissues of the small pelvis, when assessing the results of conservative treatment in dynamics |
Immunogram | In acute and exacerbation of a chronic process: an increase in the absolute and relative number of neutrophilic granulocytes in the peripheral blood, as well as their functional activity in the NBT test with a low functional reserve; decrease in phagocytosis indicators; increased IL-1 – producing activity of monocytes; increased serum lysozyme content; increased levels of IgM and IgG in peripheral blood; decrease in the number and functional activity of peripheral blood lymphocytes; an increase in the value of the T4L8 ratio (helpers / suppressors). |
Primary microscopy of native material from the vagina, cervical canal, uterine cavity, small pelvis (punctate), fallopian tube (laparoscopy) | Key cells, Trichomonas, fungal flora, leukocytosis. |
Gram stained smear from the vagina, cervical canal, uterine cavity, small pelvis (punctate), fallopian tube (laparoscopy) | Diagnostics of gonorrhea, trichomoniasis, bacterial vaginosis, candidiasis; leukocytosis, the degree of functional activity of leukocytes. Assessment of the degree of contamination of the material separately for gram-negative and gram-positive rods, gram-positive cocci, fungi using the following criteria: in large numbers – more than 100 microorganisms in the field of view; in moderation – 20-100 microorganisms in the field of view; in small quantities – 5-20 microorganisms in the field of view; microflora is not determined.To determine the invasiveness (aggressiveness) of the fungal microflora, the presence of budding yeast cells, elements of mycelium and pseudomycelium is noted. The result is obtained within 1 hour. |
Culture for aerobic and anaerobic microflora, determination of sensitivity to antibiotics of the contents of the vagina, cervical canal, uterine cavity, fallopian tubes and small pelvis | Determination of the nature of the vaginal biocenosis, identification of etiologically significant aerobic and anaerobic microorganisms and their antibiotic sensitivity. |
Determination of the pathogen by PCR or quantitative methods (tank culture, Femoflor) in scrapings from the cervical canal, endometrium, fallopian tubes, small pelvis (chlamydia, mycoplasma, ureaplasma, viruses) | Confirmation of the diagnosis of chlamydia, mycoplasmosis, ureaplasmosis, viral infection of the genitals. The result is obtained within 1 day. |
Aspiration biopsy of the endometrium | Assessment of the functional capabilities of the ovaries and the reception of the endometrium by histological changes in the uterine mucosa, diagnostics of the nature of the inflammatory process in the endometrium, histobacterioscopic characteristics of the pathogen, obtaining ideas about the state of local immunity (immunomorphological reactions) and protective capabilities of the mucus-forming apparatus of the uterus (lectinohistochemical studies). |
Hysteroscopy | It is carried out with chronic PID for: identifying the most altered areas of the endometrium; conducting targeted biopsy of the endometrium for histological, histochemical studies and identification of the pathogen; detection of concomitant pathology. |
Laparoscopy – the “gold” standard for diagnostics of acute PID | Establishing the nature of inflammation, the degree of changes in the fallopian tubes, the presence of complicated PID.Differential diagnosis. Biopsy of material for bacteriological and histological (immunomorphological, lectinohistochemical) studies. Therapeutic measures. |
Treatment of inflammatory diseases of female genital organs
Important to remember !!!
It is a serious mistake to choose a method of treatment on your own, based on the experience of friends, relatives or information in the media, literature. Only contacting an obstetrician-gynecologist immediately when the first symptoms appear will help to avoid serious complications and the transition of the inflammatory process to a chronic one.Since there are no two identical people, the treatment regimen is always prescribed individually, taking into account the characteristics of the body, examination indicators, the presence of diseases of other organs in a woman, etc. In this case, the doctor pays attention to possible allergic reactions, the state of immunity.
Also, do not forget that chronic diseases are very difficult to treat and you can get rid of them only with the help of a highly qualified specialist. Otherwise, relapses and complications are inevitable, which are often more dangerous than the disease itself.
Chronic gynecological diseases are often the root cause of an unstable emotional state and a decrease in the quality of sexual life. It is worth remembering about the real danger of dysfunction of the reproductive system, that is, the inability to conceive and give birth to a child. Whatever the consequences of illness, they always change a woman’s life for the worse.
The general principles of successful treatment are:
- Timely and accurate diagnostics, including control after a course of treatment
- Timely start of treatment
- Individual, comprehensive and competent approach
- Simultaneous treatment of sexual partners
- Compliance with diet during treatment
- Prevention of complications and exacerbations
!!!! Treatment of inflammatory diseases of the female genital organs should be complex, that is, affect all the mechanisms of the development of the disease !!!!
So, the following methods of treatment are in the arsenal of gynecologists:
- In acute inflammation, exacerbation of chronic, antibacterial antiviral drugs are prescribed, which are designed to fight the pathogen.
- Correction of immune disorders is carried out in parallel.
- To reduce the body’s response to the destruction of microbes, desensitizing therapy is performed.
- To remove toxic substances from the body, detoxification therapy is prescribed
- If necessary, during the course of treatment, treatment of accompanying complaints and symptoms is prescribed (for example, drugs for itching, pain, etc.)
- Enzyme preparations and probiotics are prescribed to prevent the negative effects of drugs on other organs, as well as to ensure that the prescribed drugs “work” more fully.*
* Preparations for the above methods can be prescribed both in tablet form for oral administration, and in the form of various injections. Injections of drugs must be carried out in a medical institution under the supervision of medical personnel (usually in a procedure room) - Local treatment (douching, baths, tampons with drugs, treatments, applications, irrigation, etc.) are used to enhance the effect of antibacterial and antiviral therapy, as well as as an independent type of treatment for certain diseases.It is carried out in a treatment room or at home. For local treatment, various drugs are used, the action of which is aimed at combating the pathogen, relieving the symptoms of inflammation, removing the decay products of microbes, etc.
- Phytotherapy – treatment with herbal preparations. It can be used in combination with other methods and independently. For general treatment as well as for local treatment.
- Drug-free treatment combines a large number of methods:
- Surgical (usually used when conservative treatment is ineffective or to remove pathological formations during the “cold period”, that is, after the acute inflammation subsides).It is carried out in a hospital setting.
- Acupuncture – impact on biologically active points (mesotherapy, electrical stimulation of active points, finger massage, acupuncture)
- Physiotherapy exercises
- Diet food
- Spa treatment
- Physiotherapy is one of the methods of treatment in which not chemical factors (drugs) are used, but physical ones: currents, magnetic fields, laser, ultrasound, etc.
Physiotherapy (in gynecology in particular) in medicine and, like drug therapy, is selected individually, depending on many, many characteristics of a person and his illness.The beauty of physical therapy is that it helps and complements the treatment of conditions that do not always respond well to conventional therapy.
The use of physical factors has traditionally been an important component in the prevention and treatment of obstetric and gynecological pathology. Physical factors can be the main or auxiliary method in the complex of therapeutic measures. Physiotherapy is especially relevant in the treatment of acute inflammatory processes and in the treatment of chronic ones.For example, in a number of chronic diseases of the female genital area, blood flow to the pelvic organs can be impeded due to changes in tissues and blood vessels. In this case, the drug effect is ineffective, since the active substance with the blood flow does not enter the organ or tissue in the proper volume, while exerting a general, often negative effect on the woman’s body as a whole. The combination of the same medicine with physiotherapy, an integrated approach to the treatment of the disease can improve the condition and quality of life of a woman with minimal drug load.
For some diseases physiotherapy is often the only treatment . For example, chronic pelvic pain as a result of adhesions and neuralgia of the pelvic nerves after inflammatory diseases, surgical interventions exhaust patients physically and mentally, disrupting the normal lifestyle and harmony of sexual relations. The carried out physiotherapeutic treatment helps not only to shorten the length of the recovery period, but also prevents the formation of adhesions.The latter fact is especially important for women with infertility. Thus, , when carrying out physiotherapy treatment , a number of positive effects are observed:
- reduction of treatment time
- mild painless healing effects
- prevention of complications and relapses
- no side effects typical of drug treatment
- reducing the drug load or, in some cases, eliminating them
The following hardware physical factors are most commonly used today in gynecology:
- Electric and magnetic fields. The acting factor of the electromagnetic field can be mainly its electric or magnetic component. Magnetotherapy is mainly characterized by an anti-inflammatory effect, which is associated with the anti-edema effect of the factor. This makes it possible to widely use the magnetic field in gynecology in the early postoperative period after surgical interventions.
- Electrotherapy (use of electric current). It is possible to use direct current (galvanization, drug electrophoresis), pulse currents (interference therapy, electrical stimulation, etc.)). Treatment with impulse currents relieves spasm of blood vessels and smooth muscles, which improves the blood supply to tissues, and has an analgesic effect.
- Action of mechanical factors (ultrasound therapy). Ultrasonic (US) effects carry out a kind of micromassage of cells and tissues, accompanied by the appearance of heat, and provide an analgesic effect, “softening of adhesions”, improve the blood supply to tissues and increase the hormonal activity of the ovaries.
- Phototherapy. Light therapy – the use of ultraviolet (UV), infrared and visible rays. Short-wave UV rays, for example, with direct contact with pathogenic microorganisms located directly on the skin or mucous membrane, cause a pronounced bactericidal effect and are used in the treatment of inflammation of the mucous membrane of the external genital organs and vagina. Phototherapy also includes the use of laser radiation. Low-intensity laser radiation is included in the treatment of endocervicitis (inflammation of the cervical canal), colpitis (inflammation of the vaginal mucosa) and inflammatory diseases of the pelvic organs.
In inflammatory diseases of the female genital area, the following physical effects are more often used:
- Induction therapy
- UHF
- Electrophoresis of drugs, phonophoresis
- Ultrasound
- Impulse currents of low frequency
- Paraffin therapy
- Mud therapy
- Ozokerite
- Balneotherapy
Non-traditional methods of treatment are also used, such as hirudotherapy (treatment with leeches), apitherapy (treatment with bees and bee products).
Prevention of inflammatory diseases in women
He who is forewarned is armed, therefore experts strongly recommend that girls and women follow a number of simple rules that will help avoid serious health problems.
- Eat as many citrus fruits and legumes as possible, fish and potato dishes, and fermented milk products (especially those containing bifidobacteria). This will avoid dysbacteriosis of the external genital organs.
- During menstruation, use tampons during the day and pads at night. Remember that super absorbent tampons, or tampons that remain in the vagina for six hours or more, promote the growth of microorganisms.
- Do not purchase specific intimate hygiene products: colored tampons and toilet paper, perfumed soap and sprays – this can cause irritation of the mucous membranes and the development of dysbiosis and inflammation.
- After swimming or swimming in the sea, try not to walk for a long time in a wet swimsuit, as this is fraught with the danger of hypothermia of the pelvic organs and the activation of microbial and viral flora in these organs.Plus, you unwittingly create ideal greenhouse conditions for germs.
- Give preference to underwear made from natural fabrics – synthetic fabrics hardly absorb moisture and do not provide enough good air circulation in the genital area. Cotton underwear does not allow the formation of an alkaline environment on the vaginal mucosa.
- Limit high sugar foods in your diet. According to many well-known doctors, refined sugar has properties sufficient to maintain chronic candidiasis.
- Pay attention to even minor discomfort when urinating – it can be a harbinger of serious discomfort.
- Do not eat too much bread and mushrooms, do not abuse alcohol, especially beer – all of these foods are conducive to the occurrence of chronic fungal infections.
- Practice good hygiene and use only your shaving razors and other toiletries.
- During hygienic procedures of the genital and perianal area, your movements should be directed towards the anus in order to avoid the introduction of intestinal diseases into the genitals from the anus.
- If your partner has any infection, you should also see a gynecologist – with a high degree of probability, the microbial flora will also bother you.
- Avoid casual sex. If there was unprotected contact with a casual sexual partner, you must contact the clinic as soon as possible to carry out preventive measures to prevent infection with urinary infections.
Staphylococcus on the labia
Staphylococcus in the vagina is the presence in the mucous membranes of the organ of staphylococcus, a spherical bacteria that can cause inflammation.Within the limits of acceptable values, a woman may have a transient type of staphylococcus such as epidermal staphylococcus. In a healthy woman, it will not cause disease, as a normally functioning immune system will inhibit the growth of this bacterium.
Less than 10% of women are carriers of Staphylococcus aureus in the vagina, and the bacteria also do not cause inflammation in them, due to strong local immunity. In the remaining 90%, Staphylococcus aureus in the vagina causes an infectious and inflammatory process.
Symptoms of staphylococcus in the vagina
If there are problems in the immune system and staphylococcus in the vagina began to multiply actively, this will lead to the development of the following symptoms:
Pain localized in the pelvic area.
Discharge with impurities of pus and having an unpleasant odor.
Excessive discharge can cause itching and burning in the genital area.
In case of damage to the bladder and urinary tract, there may be burning and pain during urination.
Unpleasant, often painful sensations during intimacy.
The presence of abscesses in the genital area, most often boils.
General malaise and weakness.
Sleep disorders and neuroses.
The appearance of orange cups on the skin of the labia.
Frequent exacerbations of candidal vaginitis, with all accompanying symptoms.
Causes of staphylococcus in the vagina
Staphylococci constantly surround a person and live on the skin, household items, in the dust, in the air.
They can get to the vaginal mucosa in several ways:
During hygiene procedures, staphylococcus can enter the vaginal mucosa, for example, from the intestines. Especially if intimate hygiene is carried out incorrectly.
During a medical examination, with insufficient compliance with sanitary and hygienic standards.
During intercourse.
In addition, in order for the bacterium to begin to multiply actively, it needs certain conditions.
Decrease in the body’s immune forces against the background of an infectious disease, with an exacerbation of a chronic disease, etc.;
Disorders of the endocrine system, diabetes mellitus;
Injury to tissues, for example, during labor or during diagnostic procedures;
Diseases of the genital area, for example, endometritis, fibroids, etc.;
Poor or improper hygienic care;
Violations of the vaginal microflora, the death of lactobacilli and the prevalence of an acidic environment.
All these factors contribute to the fact that even staphylococcus, which has not shown itself in any way before, begins to grow and multiply, causing an inflammatory process.
Treatment of staphylococcus in the vagina
In order to confirm or deny the presence of staphylococcus in the vagina, a woman will need to take a smear for bacterial culture. When the diagnosis is confirmed, the doctor prescribes treatment. It is aimed at eliminating pathogenic flora, at restoring it, as well as at correcting and maintaining the body’s immune forces.
Therefore, doctors practice the following therapeutic scheme:
Taking antibacterial agents in tablet form. The most popular are penicillin drugs, including Ampicillin, as well as combined drugs, for example, Amoxiclav, Flemoklav and others. The choice of a specific drug name will depend on the bacterial culture carried out and the sensitivity of the bacteria to a particular drug.
Local treatment using antibacterial suppositories, such as: Zalain (with the active ingredient cericonazole), Livarol (with the active ingredient – ketoconazole).Vaginal tablets are often prescribed, among which the most popular are imidil, clotrimazole, antifungol 500, etc.
Local treatment with antiseptic preparations used for douching. It can be Miramistin, potassium permanganate solution, hydrogen peroxide.
Restoration of normal vaginal microflora, for which vaginal tablets are used – Vagilak, Ginoflor, Ekofemin.
Treatment of concomitant disease, if any, with etiotropic agents.
Reception of vitamin and mineral complexes.
Use of antihistamines.
As an additional recommendation, doctors advise a woman to abstain from sexual activity during treatment. If there is a regular sexual partner, then he also needs to undergo research and, if necessary, therapy.
In addition, a woman should follow a light diet with the exception of spicy, fried and fatty foods.
Prevention of staphylococcus in the vagina
Preventive measures should be directed not only to prevent infection of the vagina with staphylococcus, but also to restrain its growth and development with possible asymptomatic carriage.
The following are considered the most effective preventive measures:
Thorough intimate and personal hygiene, with obligatory hand washing;
Refusal to take any medicines without a doctor’s prescription, especially antibacterial action;
Rejection of low-quality underwear made of synthetic materials, which can not only injure the skin, but also become a favorable environment for the development of bacteria;
Timely treatment of diseases of the genital area;
Avoiding frequent stress, genital trauma;
Use of reliable contraceptive methods such as condoms;
Refusal from bad habits, poor quality food, maintaining physical fitness;
Use of personal hygiene products.
These simple rules will help to avoid infection and maintain the microflora of the vagina, as well as the state of the immune system is normal. As for the prognosis for recovery, it is favorable with timely treatment.
The author of the article: Lapikova Valentina Vladimirovna | Gynecologist, fertility specialist
Education: Diploma in Obstetrics and Gynecology received at the Russian State Medical University of the Federal Agency for Health and Social Development (2010.). In 2013 completed postgraduate studies at N.N. N.I. Pirogova.
10 Proven Reasons to Eat Chia Seeds Every Day!
The best diets for 3 days – “minus 3 kg”
The danger of these microorganisms is that they produce toxins and enzymes that are pathogenic for cells and disrupt their vital activity. Bacteria have a devastating effect on connective tissues, skin and subcutaneous tissue. They cause a number of the most dangerous diseases, including.
Among the folk methods of treatment and prevention of Staphylococcus aureus, copper treatment or metal therapy, known since the time of Aristotle, deserves special attention. Aristotle in his works mentions the treatment of bruises, ulcers and edema by applying copper.
How can a child become infected with staphylococcus? The carriers of this dangerous bacterium are both sick and healthy people, because there are different forms of infection carrier (temporary and permanent). The course of the disease can also occur in mild and severe forms.
In fact, there is only one objective reason for using antibiotics against such a resistant and flexible pathogen as Staphylococcus aureus – the expected benefits will outweigh the inevitable harm. Only in the case when the infection covered the entire body, got into the bloodstream, caused a fever, as well.
Staphylococcus aureus in the nose is the presence of bacteria in the nasal mucosa that can cause a purulent-inflammatory disease. There are more than 20 varieties of staphylococcus, and most of them are constant companions of humans and are normally present on mucous membranes, including.
Staphylococcus in the throat is the presence of bacteria in the mucous membrane of the pharynx or larynx that can cause an infectious and inflammatory process. The microbe can exist there as a conditionally pathogenic microflora, that is, without causing a disease, but can cause an inflammatory reaction.
Staphylococcus aureus in the intestine is the colonization of its mucous membrane by a bacterium belonging to the group of staphylococci and capable of causing an infectious and inflammatory process. This bacterium does not always cause an inflammatory reaction in the intestines, but only if its concentration exceeds the permissible levels.
Among the etiology of various gynecological diseases, bacterial infections play an important role. Staphylococcus aureus in the vagina causes the development of an inflammatory process. It is important to treat this disease on time, preventing its chronicity and complications.
Methods of infection
This infection is found quite often in gynecology. Most women are carriers of staphylococcus, but with good local immunity, inflammation does not develop.
There are a number of factors contributing to inflammation:
- decrease in general and local immunity;
- hormonal balance failure;
- Violation of vaginal acidity;
- improper treatment of infections;
- dysbiosis;
- gynecological diseases.
In case of a decrease in the body’s defenses, a pathological process develops, which is facilitated by injuries of the mucous membranes and a change in the pH of the vagina towards alkaline. Violation of the acid-base balance causes the death of lactic acid bacteria and the reproduction of conditionally pathogenic microflora.
Failure of the hormonal background is displayed on the state of the mucous membranes of the vagina, due to which their protective function suffers, they become the entrance gate for infection.
Staphylococcus aureus enters the vagina from the skin of the carrier.This bacterium often lives on the lining of the throat and causes the development of sore throat. Infection occurs from another person through the sharing of hygiene items. Like other sexually transmitted infections, infection can occur during intercourse.
If Staphylococcus aureus lives on the membranes of the throat, then one of the ways of infection is oral sex. You can get infected during hygiene procedures and medical procedures.
Infection occurs when a smear is taken from the urethra, during urethroscopy and other instrumental research methods.An important role is played by insufficient intimate hygiene, when staphylococcus is introduced from the skin around the intestines.
The incubation period takes on average 5-10 days. Sometimes it can be reduced to 2 days or extended to a month, depending on the state of the body and the activity of bacteria.
Symptoms
The course of the disease in women can pass with sluggish symptoms, without pronounced clinical manifestations. In other cases, acute symptoms of inflammation develop, which forces a woman to turn to a gynecologist with obvious complaints.
In some cases, spontaneous recovery is possible, but more often the untreated process turns into a long chronic stage. The clinical picture of staphylococcal infection in women is largely similar to the manifestations of gonorrhea. Therefore, only the attending gynecologist should carry out diagnostics and therapy.
Typical symptoms of staphylococcus in the vagina are as follows:
- pain in the lower abdomen;
- burning and itching in the genitals;
- painful urination;
- yellow vaginal discharge with an unpleasant odor;
- Pain in the lower back;
- disturbed menstrual cycle;
- discomfort during sexual intercourse;
- the appearance of pustular eruptions on the genitals;
- development of candidal vaginitis.
- general malaise;
- fever;
- Sleep disturbance.
A woman comes to an appointment with a gynecologist with complaints about aching pain in the lower abdomen and lower back. Sexual contact becomes painful. When the infection spreads to the urethra and bladder, painful urination occurs.
Menses with pathological yellow discharge. This causes itching and burning in the perineum, and a pungent odor appears. Of the menstrual irregularities, menstruation is more often delayed.
The development of vaginal candidiasis is evidenced by the appearance of cheesy discharge. The general malaise is moderately pronounced, and the increase in body temperature can reach 38 degrees.
Treatment and prevention
To confirm the staphylococcal etiology of the disease, it is necessary to take a vaginal smear for bacterial culture. It is important to see a doctor on time, and self-medication is unacceptable. Improper use of drugs is fraught with complications and chronicity of the disease.
In addition to isolating staphylococcus, its sensitivity to antibiotics is determined, which determines the choice of a specific drug.General treatment is most often carried out with penicillin antibiotics and combination agents. The preference is given to protected drugs (Amoxiclav, Flemoklav).
Local therapy consists in the use of antibacterial suppositories: Livarol, Zalain. Vaginal tablets are used:
Combined local treatment is carried out by douching with antiseptic solutions. For this, a pale solution of potassium permanganate, hydrogen peroxide, Miramistin is used.
Restoration of the vaginal microflora takes an important place in the complex of therapy.For this, vaginal tablets are prescribed:
For general strengthening of the body, combined preparations with minerals and vitamin complexes are used. As symptomatic therapy to eliminate itching, swelling, with antipyretic purposes, antihistamines are prescribed.
To achieve the maximum effect, as well as to prevent re-infection, examination and treatment of the sexual partner is necessary.
During the course of therapy, a pause in sexual activity should be made.During this period, the female body needs a special diet that excludes fried, fatty and spicy foods. After a month, it is necessary to repeat the bacterial inoculation.
To prevent staphylococcal infection, you should take care of individual general and intimate hygiene. Natural underwear should be preferred. Condoms are the safest way to protect yourself during sexual intercourse.
Conclusion
Staphylococcus aureus in the vagina is a common problem in gynecology and causes severe symptoms.For a favorable prognosis, it is important to prescribe the correct and timely treatment.
During a routine examination by a gynecologist, a woman takes a smear, and laboratory technicians often find a microorganism such as staphylococcus in it. What does this analysis result mean?
Ways of getting staphylococcus into the vagina
Let’s consider where the staphylococcal infection comes from.
- Staphylococci live around us, on the skin, in the intestinal tract.Therefore, when washing, for example, with water, staphylococcus can move into the vagina on the mucous membranes and begin to develop in favorable conditions for it.
- Staphylococcus aureus can also be brought in during medical procedures.
- During sexual intercourse.
Staphylococcus aureus in the vagina
Staphylococcus aureus can be especially common and dangerous. Getting into the vagina, Staphylococcus aureus may not manifest itself in any way. Its appearance on the genitals can cause vulvovaginitis with painful sensations and a burning sensation in the vagina, as well as the appearance of abnormal discharge.A particularly advanced form of staphylococcus is the appearance of yellow, orange scales on the skin, which means that the disease is already breaking out.
All this can provoke diseases of the urinary system. Once on the urethra, staphylococcus aureus causes a burning sensation when urinating. Vaginal staphylococcus aureus can cause frequent recurrent thrush caused by dysbiosis. And itching on the labia further complicates the process of transferring the disease. Vaginal Staphylococcus aureus can begin to develop if there is a violation of vaginal acidity.
Treatment of vaginal staphylococcus
If vaginal staphylococcus is suspected, a bacterial culture test is taken, if the diagnosis is confirmed, then the treatment should be prescribed by an infectious disease doctor. Often used in the treatment of autovaccines, autohemotherapy and toxoid. Local treatment of vaginal staphylococcus is also carried out using tampons with bacteriophages.
At the same time, immunity should be increased. Probiotics are prescribed to restore normal vaginal flora.The main thing is not to abuse antibiotics during treatment, since staphylococcus quickly adapts to them, and later this can cause great difficulties with treatment.


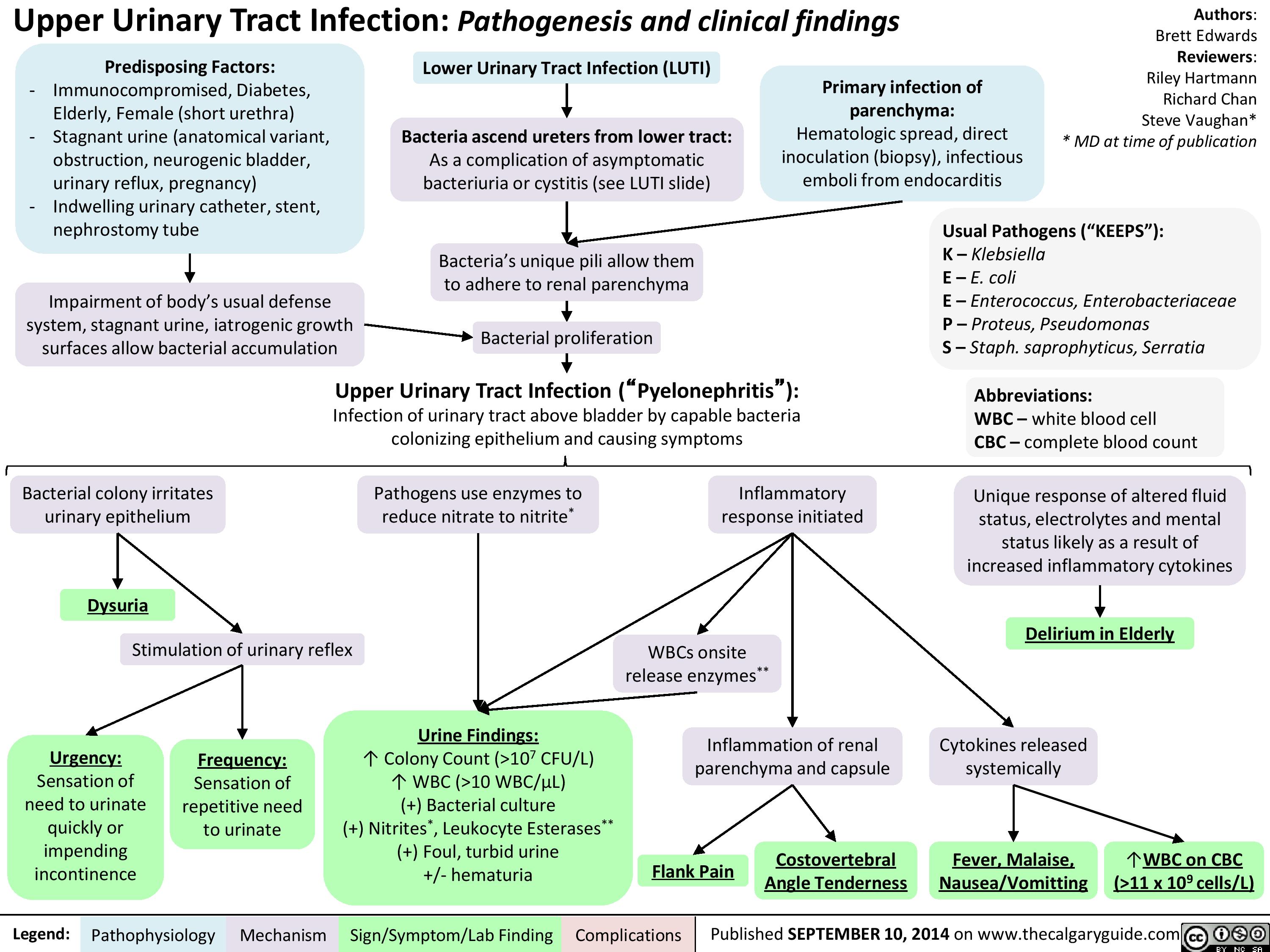 Sneeze into a tissue and then throw the tissue away. Bathe daily (or as often as possible), especially for children with eczema or sensitive skin.
Sneeze into a tissue and then throw the tissue away. Bathe daily (or as often as possible), especially for children with eczema or sensitive skin.