Tear in foot arch. Plantar Fascia Rupture: Causes, Symptoms, and Treatment Options
What is a plantar fascia rupture. How does it differ from plantar fasciitis. What are the symptoms of a torn plantar fascia. How is a plantar fascia rupture diagnosed and treated. How long does recovery from a plantar fascia tear typically take.
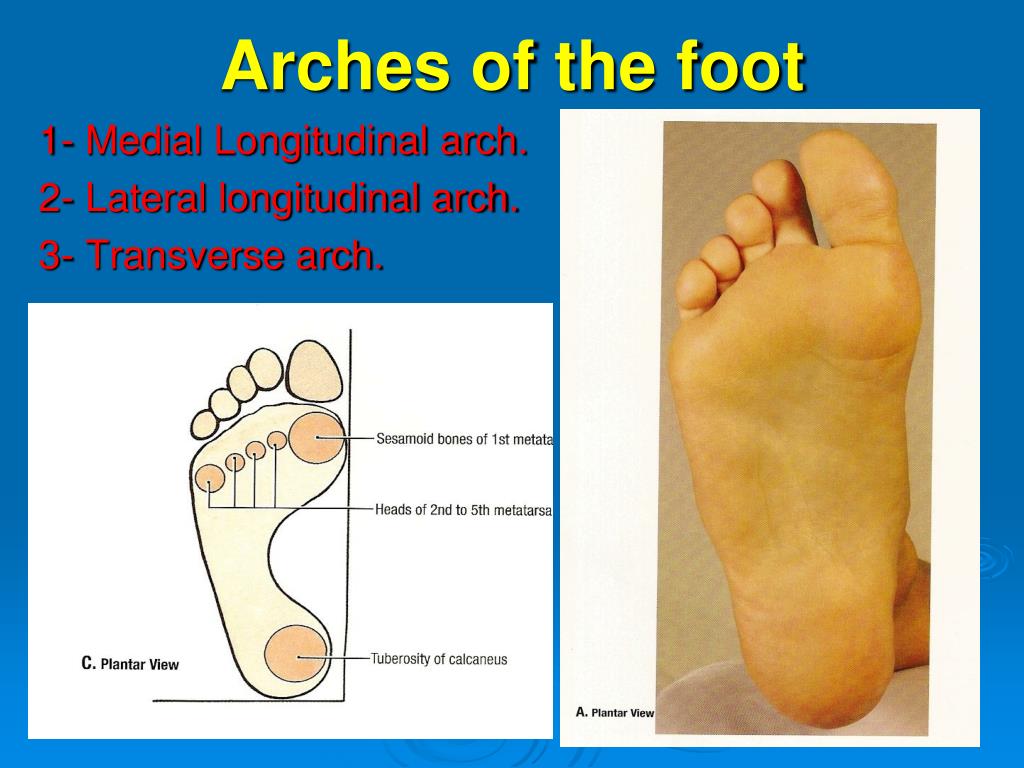
Understanding the Plantar Fascia: Structure and Function
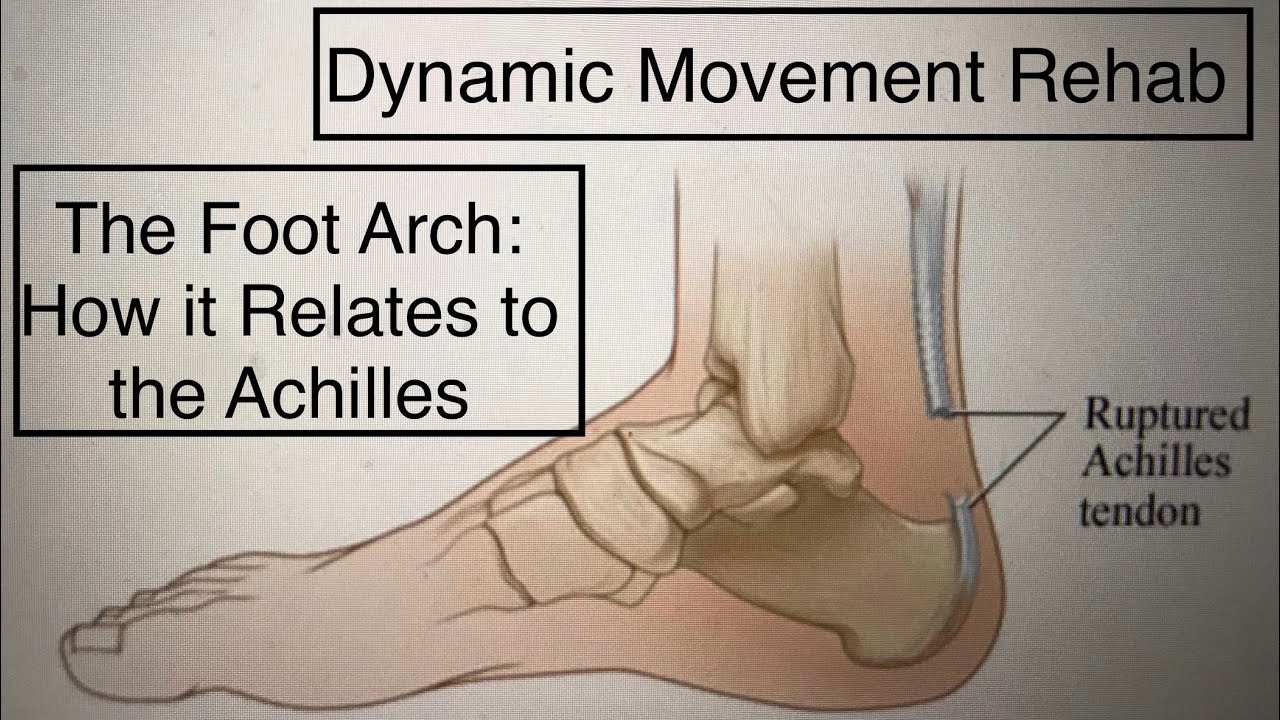
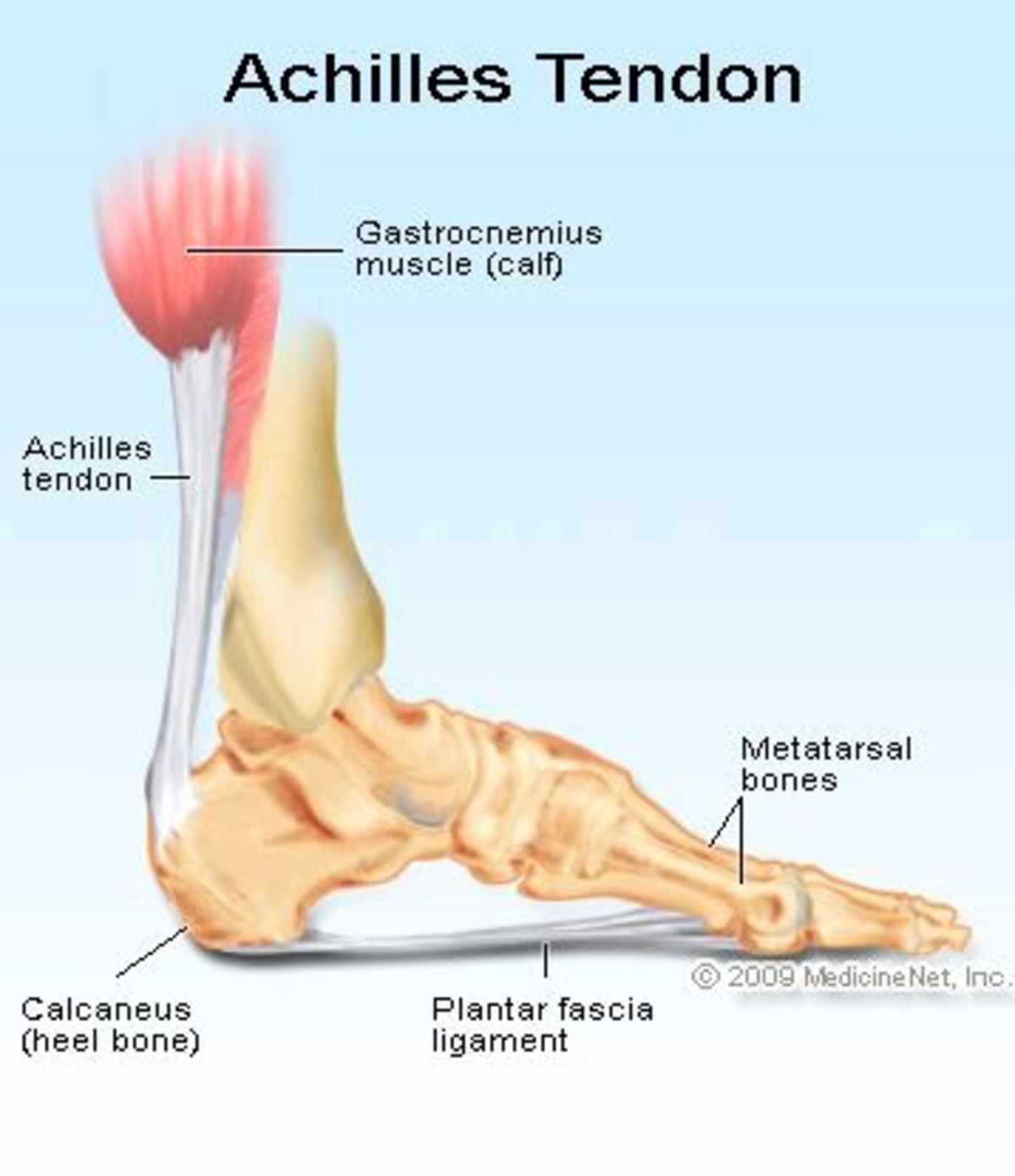
The plantar fascia is a crucial component of foot anatomy, playing a vital role in maintaining arch support and overall foot stability. This thick band of tissue extends from the heel bone (calcaneus) to the base of the toes, spanning the entire length of the foot’s underside.
Key functions of the plantar fascia include:
- Providing structural support to the foot’s arch
- Absorbing shock during walking and running
- Facilitating the transfer of weight from the heel to the toes during gait
Understanding the plantar fascia’s structure and function is essential for recognizing potential issues and seeking appropriate treatment when problems arise.
Plantar Fascia Rupture vs. Plantar Fasciitis: Identifying the Difference
While both conditions affect the plantar fascia, a rupture and fasciitis are distinct issues with different causes and symptoms. How can you differentiate between the two?
Plantar Fasciitis
Plantar fasciitis is characterized by inflammation of the plantar fascia, typically caused by repetitive stress or overuse. Symptoms include:
- Pain that is worst in the morning or after periods of rest
- Gradual onset of discomfort
- Pain that improves with activity but worsens after prolonged standing or walking
Plantar Fascia Rupture
A plantar fascia rupture, on the other hand, involves a partial or complete tear of the tissue. This condition is often characterized by:
- Sudden, sharp pain in the arch or heel
- A audible or palpable “pop” at the time of injury
- Immediate bruising and swelling
- Constant pain that doesn’t improve with rest
Recognizing these differences is crucial for proper diagnosis and treatment.
Causes and Risk Factors for Plantar Fascia Rupture
Plantar fascia ruptures can occur due to various factors. Understanding these causes can help in prevention and early intervention.
Acute Trauma
Sudden, high-impact activities can lead to an acute plantar fascia rupture. Common scenarios include:
- Jumping or falling from a height
- Rapid changes in direction during sports like basketball or football
- Sudden acceleration in running
Chronic Degeneration
In some cases, a plantar fascia rupture may occur gradually due to long-term stress on the tissue. This can happen when:
- Chronic plantar fasciitis is left untreated
- The fascia becomes weakened over time due to repetitive strain
- There’s a history of multiple corticosteroid injections in the area
Risk Factors
Certain factors may increase the likelihood of experiencing a plantar fascia rupture:
- Age (more common in middle-aged and older adults)
- Obesity
- High-impact sports participation
- Improper footwear
- Tight calf muscles
- Flat feet or high arches
Being aware of these risk factors can help individuals take preventive measures and seek timely medical attention when necessary.
Diagnosing a Plantar Fascia Rupture: Signs, Symptoms, and Medical Evaluation
Accurate diagnosis of a plantar fascia rupture is crucial for appropriate treatment. How do medical professionals identify this condition?

Clinical Presentation
Patients with a plantar fascia rupture typically report:
- A sudden, sharp pain in the arch or heel
- Difficulty walking or bearing weight on the affected foot
- Visible bruising and swelling on the bottom of the foot
- A feeling of instability in the arch
Physical Examination
During a physical exam, a healthcare provider may:
- Palpate the plantar fascia to check for tenderness and gaps in the tissue
- Assess the foot’s range of motion and stability
- Evaluate gait and weight-bearing capacity
- Perform specific tests to rule out other conditions
Diagnostic Imaging
To confirm the diagnosis and assess the extent of the injury, imaging studies may be ordered:
- X-rays: To rule out fractures or other bone-related issues
- Ultrasound: Provides real-time visualization of soft tissue structures
- MRI: Offers detailed images of the plantar fascia and surrounding tissues
A comprehensive approach to diagnosis ensures that the most appropriate treatment plan can be developed for each patient.

Treatment Approaches for Plantar Fascia Rupture
Managing a plantar fascia rupture requires a tailored approach based on the severity of the injury and individual patient factors. What are the primary treatment options available?
Conservative Management
For most cases of plantar fascia rupture, non-surgical treatment is the preferred initial approach. This may include:
- Rest and activity modification
- Ice therapy to reduce swelling
- Compression bandages
- Immobilization with a walking boot or cast
- Gradual weight-bearing as tolerated
- Physical therapy exercises
- Custom orthotics to support the arch
Advanced Therapies
In some cases, particularly for chronic or severe ruptures, additional treatments may be considered:
- Platelet-rich plasma (PRP) injections
- Amniotic tissue injections to promote healing
- Extracorporeal shock wave therapy (ESWT)
Surgical Intervention
While rare, surgery may be necessary in cases where conservative treatments fail. Surgical options may include:
- Plantar fascia release
- Repair of the torn tissue
- Addressing any associated conditions, such as heel spurs
The choice of treatment depends on various factors, including the extent of the rupture, the patient’s activity level, and overall health status. A personalized treatment plan developed in consultation with a podiatrist or orthopedic specialist is essential for optimal outcomes.

Recovery and Rehabilitation Following a Plantar Fascia Rupture
The journey to full recovery after a plantar fascia rupture can be lengthy, requiring patience and dedication. What does the rehabilitation process typically involve?
Initial Recovery Phase
During the first few weeks following the injury, the focus is on protecting the healing tissue:
- Strict adherence to weight-bearing restrictions
- Use of assistive devices like crutches or a knee scooter
- Regular icing and elevation of the affected foot
- Gentle range of motion exercises as directed by a healthcare provider
Progressive Rehabilitation
As healing progresses, rehabilitation efforts intensify:
- Gradual increase in weight-bearing activities
- Strengthening exercises for the intrinsic foot muscles
- Stretching routines for the calf muscles and plantar fascia
- Balance and proprioception training
- Gait retraining to ensure proper foot mechanics
Return to Activity
The final phase of recovery focuses on safely returning to pre-injury activities:

- Sport-specific training for athletes
- Gradual increase in activity intensity and duration
- Continued use of supportive devices like orthotics
- Regular follow-up with healthcare providers to monitor progress
The timeline for full recovery can vary significantly between individuals, ranging from 9 to 12 weeks or longer in some cases. Adherence to the rehabilitation program and patience during the recovery process are key factors in achieving optimal outcomes.
Preventing Plantar Fascia Ruptures: Strategies for Foot Health
While not all plantar fascia ruptures can be prevented, there are several strategies individuals can employ to reduce their risk. How can you protect your plantar fascia from injury?
Proper Footwear
Choosing appropriate shoes is crucial for foot health:
- Select shoes with adequate arch support
- Ensure proper fit, with enough room in the toe box
- Replace athletic shoes regularly, especially if you’re a runner
- Consider using orthotic inserts for additional support
Gradual Activity Progression
Avoid sudden increases in activity level or intensity:

- Follow the 10% rule when increasing running mileage
- Incorporate rest days into your exercise routine
- Cross-train with low-impact activities to reduce stress on the feet
Stretching and Strengthening
Regular foot and leg exercises can help maintain flexibility and strength:
- Perform calf stretches daily
- Practice toe curls and other intrinsic foot muscle exercises
- Use a tennis ball or foam roller for self-massage of the plantar fascia
Maintain a Healthy Weight
Excess body weight increases stress on the plantar fascia:
- Follow a balanced diet
- Engage in regular physical activity
- Consult with a healthcare provider for weight management strategies if needed
Address Early Signs of Foot Pain
Don’t ignore persistent foot discomfort:
- Seek medical attention for heel or arch pain that doesn’t improve with rest
- Address biomechanical issues like overpronation or high arches
- Consider preventive measures like night splints if you’re prone to plantar fasciitis
By implementing these preventive strategies, individuals can significantly reduce their risk of experiencing a plantar fascia rupture and maintain overall foot health.

When to Seek Professional Help: Red Flags and Complications
While many foot conditions can be managed with home care, certain symptoms warrant immediate medical attention. What are the signs that indicate a need for professional evaluation?
Severe or Persistent Pain
Seek medical help if you experience:
- Sudden, intense pain in the arch or heel
- Pain that doesn’t improve with rest and ice therapy
- Discomfort that significantly impacts your ability to walk
Visual Changes
Be alert for noticeable alterations in foot appearance:
- Significant swelling or bruising
- Visible deformity in the arch
- Changes in foot shape or alignment
Functional Impairment
Consult a healthcare provider if you experience:
- Inability to bear weight on the affected foot
- Persistent instability or a feeling that the foot is “giving way”
- Difficulty performing routine activities due to foot pain
Potential Complications
Be aware of signs that may indicate complications:
- Signs of infection, such as fever or redness extending up the leg
- Numbness or tingling in the foot
- Chronic pain that doesn’t respond to conservative treatments
Prompt medical evaluation can help prevent further injury and ensure appropriate treatment. Don’t hesitate to consult a podiatrist or orthopedic specialist if you’re experiencing concerning symptoms related to your feet or ankles.

Understanding the intricacies of plantar fascia ruptures, from their causes and symptoms to treatment options and prevention strategies, is crucial for maintaining foot health. By recognizing the signs of this condition and seeking timely medical attention, individuals can minimize the impact of a plantar fascia rupture on their daily lives and athletic pursuits. Remember, proactive care and adherence to proper foot health practices are key to preventing and managing plantar fascia injuries effectively.
What is a Plantar Fascia Rupture? — LIGHTHOUSE FOOT & ANKLE CENTER
What is the Plantar Fascia?
The plantar fascia is a thick band of tissue that extends from your heel to the base of your toes, on the bottom of your foot.
The fibrous band provides stability and supports your arch. A common cause of heel pain known as plantar fasciitis can occur when the fascia becomes inflamed where it attaches to the heel bone. If caught early, proper shoes, stretching, and inserts can alleviate the pain.
What Happens When The Plantar Fascia Tears?
Occasionally, the plantar fascia can rupture or tear. A rupture can occur after a sudden trauma when jumping or falling from a height. Runners, basketball, and football players may experience the injury with quick, sudden movements. Patients often describe a “pop” in the heel or arch followed by bruising and swelling. Typically, plantar fasciitis is worse in the morning and after sitting for long periods.
Pain from a rupture is more constant than plantar fasciitis.
A rupture can also occur slowly over time. Chronic plantar fasciitis, heel pain lasting more than 6 months, can lead to a partially torn plantar fascia. The fascia becomes frayed with overuse and loses its integrity. Pain will often be directly under the heel, with mild to moderate swelling. Patients may feel a small lump the size of a dime, in the heel area. Often patients come in with bags of orthotics and night splints that have failed to alleviate the condition.
A torn plantar fascia is very painful and requires proper treatment, whether acute or chronic. Diagnosis of a plantar fascia rupture is made by taking a complete history, an examination, and the use of diagnostic tools such as x-ray, ultrasound, and possibly MRI.
Treatment and Recovery from a Plantar Fascia Rupture
A plantar fascia tear can mimic chronic plantar fasciitis, making it frustrating to treat without a proper diagnosis. Steroid injections can make the condition worse or even cause a rupture. Treatment for an acute plantar fascial tear begins with a period of immobilization with a cam walker, or with crutches, followed by protected weight-bearing and physical therapy. An acute rupture is more obvious clinically due to swelling and bruising than a chronic plantar fascia rupture.
Steroid injections can make the condition worse or even cause a rupture. Treatment for an acute plantar fascial tear begins with a period of immobilization with a cam walker, or with crutches, followed by protected weight-bearing and physical therapy. An acute rupture is more obvious clinically due to swelling and bruising than a chronic plantar fascia rupture.
A chronic tear may require advanced therapy using amniotic tissue to repair the tear. The injection therapy can be done in the office under local anesthesia. During treatment, custom-molded orthotics are fabricated to support the fascia. Recovery may take 3 to 4 months. Because the fascia tends to heal well on its own surgery is rarely required.
If you are suffering from either acute or chronic heel pain, proper diagnosis and treatment of a plantar fascia issue will ensure a quicker recovery. Dr. Michele Kurlanski is here to help. Same-day appointments are now available! Give us a call today (207) 774-0028 to schedule your next appointment at our location in Scarborough, Maine.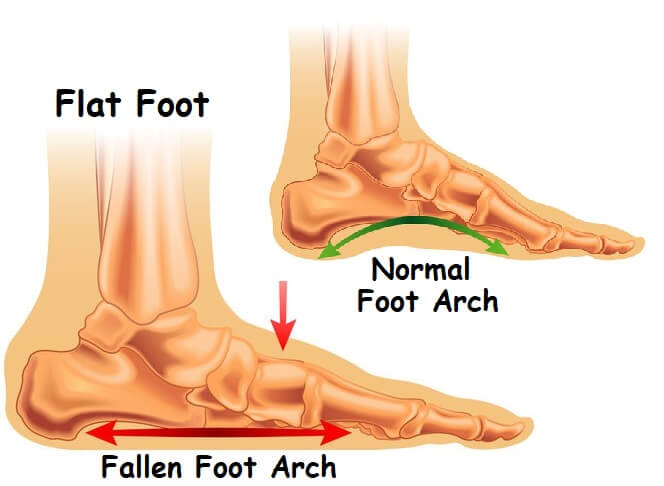
Plantar Fascia Ruptures: Hubert Lee, DPM: Podiatrist
What is a Plantar Fascia Rupture?
The plantar fascia is a thick band of tissue on the bottom of your foot that extends from your heel to your toes. It provides stability and support to your arch. A common cause of heel pain known as plantar fasciitis can occur when the fascia becomes inflamed. The plantar fascia can also traumatically tear or rupture. This can occur when jumping or falling from a height or during activities like running or basketball. If you suffer from a plantar fascia rupture, you may hear or feel a “pop” in your arch. You will also likely experience sharp pain with bruising and swelling in your arch and heel.
A torn plantar fascia is very painful and requires proper treatment. Diagnosis of a plantar fascia rupture is made by a complete history and exam. X-rays and occasionally an MRI may also be necessary.
Treatment and Recovery from a Plantar Fascia Rupture
Treatment for a torn plantar fascia begins with a period of immobilization and crutches followed by a walking boot. Physical therapy will be initiated, and a supportive, custom orthotic will be made to decrease tension on the fascia. Recovery can take 9-12 weeks. Surgery is typically not required, because the fascia tends to heal well on its own. In fact, a surgical treatment for heel pain caused by plantar fasciitis involves cutting and lengthening the tight fascia.
Physical therapy will be initiated, and a supportive, custom orthotic will be made to decrease tension on the fascia. Recovery can take 9-12 weeks. Surgery is typically not required, because the fascia tends to heal well on its own. In fact, a surgical treatment for heel pain caused by plantar fasciitis involves cutting and lengthening the tight fascia.
A ruptured plantar fascia can take several months to completely resolve. In a 2004 study involving 18 patients with a torn plantar fascia, all patients returned to activities within 4-26 weeks with an average of 9 weeks. The patients in this study were mostly runners, but this condition can occur in any activity with jumping or running. If you are suffering from either acute or chronic heel pain, proper diagnosis and treatment of a plantar fascia rupture will ensure a timely return to your activities.
Foot Conditions Associated with Obesity
Being overweight bears a connection to several different foot conditions. But, it’s possible to reduce weight through exercises, while any foot-related conditions are treated.
But, it’s possible to reduce weight through exercises, while any foot-related conditions are treated.
How to Detect Early-Stage Toenail Fungus
You can detect toenail fungus early in its development IF you know the signs. Dr. Lee offers helpful, professional insights
6 Common Summer Foot Problems
When summer arrives, it’s important to check on your feet as often as possible because some summer foot conditions can cast a shadow on your sunny days. Here are 6 Common Summer Foot Problems Dr. Lee sees in his office.
It’s Men’s Health Month: 5 Tips for Healthy Feet
June marks Men’s Health Month, today, Dr. Hubert Lee at CarePlus Foot & Ankle Specialists in Bellevue, WA, is sharing 5 tips for happy, healthy male feet.
Managing Foot Pain from Osteoporosis
It is not unusual to feel the effects of osteoporosis on your feet. Symptoms include pain, swelling, and fractures. Dr. Lee offers guidance for managing the associated foot pain.
Symptoms include pain, swelling, and fractures. Dr. Lee offers guidance for managing the associated foot pain.
Dislocations of the bones of the foot – symptoms of injury, first aid and treatment, rehabilitation – Department of Traumatology NCC No. 2 (CCH RAS)
Dislocations of the foot are rare and account for about 2% of all traumatic injuries of the lower extremities of a person. In most cases, these injuries are accompanied by ligament rupture and often in combination with fractures. The most common are incomplete dislocations of the ankle (subluxations) that are not accompanied by fractures. Much less often you can find isolated (complete) dislocations of the ankle joint, as a rule, they are accompanied by fractures and ruptures of the ligaments.
Dislocations in the joints of the foot are divided into:
- Subtalar dislocations of the foot (talocalcaneal-navicular joint)
- Dislocations of the foot in the Chopard joint (transverse tarsal joint)
- Dislocations of the metatarsal bones in the Lisfranc joint (a rather rare injury, in addition to severe pain and swelling, is accompanied by a noticeable expansion and shortening of the foot)
- Dislocations of the phalanges of the toes
Each has its own distinctive features (almost all of them occur with foot displacement).
Causes of injury.
These injuries often happen for the following reasons:
- turning the foot inward
- sharp turn of the foot
- direct blow to the metatarsus or toes
- unsuccessful fall or jump to feet from a great height
It is extremely important to seek qualified medical help in time, otherwise the consequences of a dislocation of the foot can be deplorable: there is a high probability of developing diseases such as arthritis or arthrosis; the mobility of the injured joint after its healing may be difficult; possible partial or complete atrophy of muscles, circulatory disorders in the limbs.
Signs of foot dislocations.
With various dislocations of the ankle, the patient has the following symptoms (they appear quite quickly):
- acute pain occurs
- instant swelling
- bruising
- cyanosis
- obvious deformity in the ankle joint
Diagnostics.
After an accident, the victim must be immediately taken to the traumatology department, while he must not make any movements of the leg (active and passive). Upon admission of the patient, the doctor performs a detailed examination of the injured limb, draws up a complete anamnesis. The main method for diagnosing dislocations of the foot is radiography. Only with the help of x-rays can a traumatologist make an accurate diagnosis (determine the type of dislocation) and begin appropriate treatment. In the case of complicated dislocations with fractures, surgical intervention may be required.
Treatment.
Treatment should be carried out only by a qualified traumatologist.
- Reduction of dislocation of the foot bones using local or general anesthesia
- Fixation of the reduced joint with a plaster splint
- The period of immobilization is from 8 to 12 weeks (depending on the type of dislocation and the severity of associated injuries)
- Prescribing painkillers (if necessary)
- In the first days, it is necessary to provide the patient with an elevated position of the leg and cold
- For the duration of treatment, it is strictly forbidden to lean or step on the injured limb
Rehabilitation.

During the recovery period after the removal of the plaster, the patient is prescribed a set of procedures.
- Physiotherapy
- Physiotherapy course (strictly according to doctor’s prescription)
- Therapeutic massage
- Vitamin therapy
- Swimming
Preventive measures.
- A full load on the leg is allowed to be given no earlier than a month later (for uncomplicated dislocations) or three months later (for severe injuries). Crutches
- After an ankle injury, the patient must wear orthopedic shoes with arch support for a year
- Regular exercise to strengthen the muscles of the lower extremities
- Safety at work, when playing sports, when driving on slippery surfaces
- Daily diet should include foods rich in vitamins and calcium
can be used during this time if necessary.
Longitudinal and transverse flat feet – treatment, symptoms, causes, diagnosis
Nature always expediently gives organisms one or another form of an organ as the most optimal for performing the complex of movements that is performed by a living organism. This also applies to the shape of the human foot. The human foot is a highly specialized structure, made up of 26 different bones, 33 joints, over 100 muscles, tendons and ligaments. And all these structures somehow participate in the formation of the arch of the foot. The task of the arch of the foot is to perform a supporting function and distribute the weight of the body over the surface of the foot. The structure of the foot is elastic enough to allow a person to move smoothly, but at the same time strong enough to withstand heavy loads. Most people have a gap under the arch of the foot when a person is in a standing position. The arch of the foot, or the inside of the foot, is slightly raised off the ground. People with flat feet either have no arch at all or have very low arches.
This also applies to the shape of the human foot. The human foot is a highly specialized structure, made up of 26 different bones, 33 joints, over 100 muscles, tendons and ligaments. And all these structures somehow participate in the formation of the arch of the foot. The task of the arch of the foot is to perform a supporting function and distribute the weight of the body over the surface of the foot. The structure of the foot is elastic enough to allow a person to move smoothly, but at the same time strong enough to withstand heavy loads. Most people have a gap under the arch of the foot when a person is in a standing position. The arch of the foot, or the inside of the foot, is slightly raised off the ground. People with flat feet either have no arch at all or have very low arches.
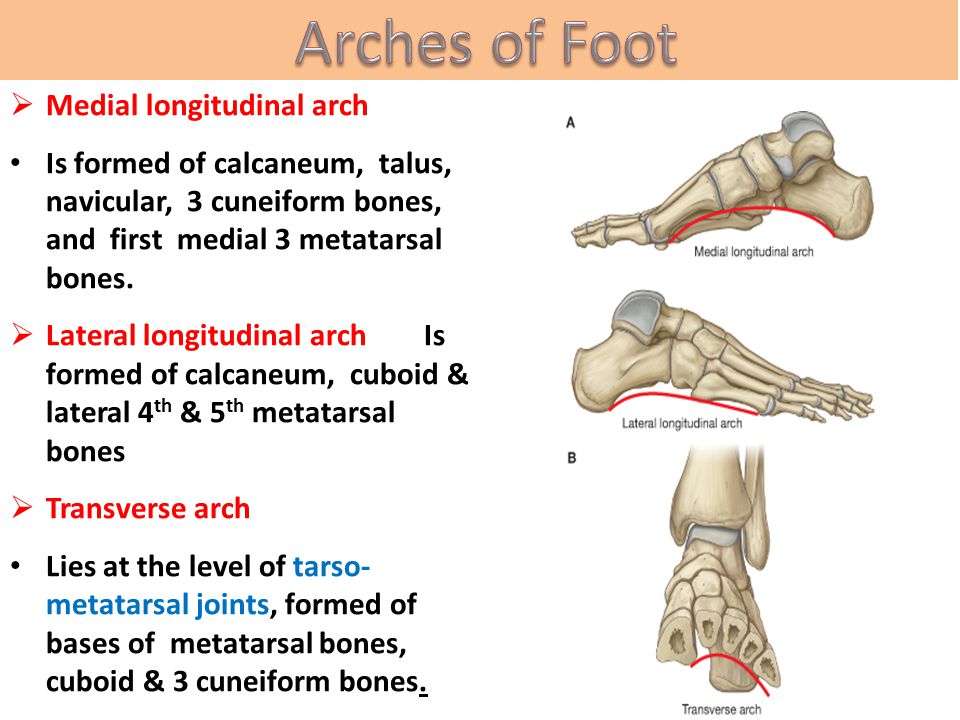
The foot normally has two arches – longitudinal (along the foot along the medial edge) and transverse (located under the bases of the fingers). All types of flat feet are divided into longitudinal flat feet (reduction of the longitudinal arch of the foot) and transverse flat feet (flattening of the transverse arch). The foot, therefore, can increase both in width and in length. With combined flatfoot there is a decrease in both the transverse and longitudinal arch of the foot. The most common is transverse flatfoot. Flatfoot is a condition in which the longitudinal arch descends and the entire sole touches the ground.
The foot, therefore, can increase both in width and in length. With combined flatfoot there is a decrease in both the transverse and longitudinal arch of the foot. The most common is transverse flatfoot. Flatfoot is a condition in which the longitudinal arch descends and the entire sole touches the ground.
The feet of people with flat feet may twist on the inside, while standing and walking, and as a result, the feet of the feet may bulge outward.
A significant proportion of people with flat feet do not experience pain and have no problems with their feet. However, some may experience pain in the legs, especially if there is associated ligament and muscle tension. The knee joints can also be a source of pain. If the ankles turn inward due to flat feet, then the asymmetry can have a damaging effect on the feet, ankles, and knee joints. In some people, flat feet occur due to a congenital malformation of the foot, while in others, flat feet occur as they age and develop involutional changes or after pregnancy.
Every day people around the world are born with flat feet . Many of them are quite active, go in for sports (running, football), do hard work. Thus, the question arises how some people with flat feet feel great and lead an active lifestyle, while others experience discomfort and pain in their legs. First of all, it is necessary to understand the operation of normal feet and feet with flat feet . During walking, the foot usually flattens out a little so that it can absorb the load vector and distribute it over the supporting surface of the foot. A straightened or pronated foot is quite flexible. The location of the bones of the foot essentially exposes the foot. Conversely, when the foot has a higher arch or is in a supinated position, the foot is locked and inactive and poorly absorbs the load and is less firmly attached to the surface when the foot pronates.
Since flat feet are structurally weaker, this leads to chronic muscle tension as the muscles try to keep the feet in a stable position. For people who have always had flat feet, the muscles are most likely very well adapted to normal activity levels. However, when the load on the muscles or the intensity of the load increases, this can lead to the appearance of pain. A decrease in the stability of the foot naturally increases the displacement of the medial (inner) part of the foot.
For people who have always had flat feet, the muscles are most likely very well adapted to normal activity levels. However, when the load on the muscles or the intensity of the load increases, this can lead to the appearance of pain. A decrease in the stability of the foot naturally increases the displacement of the medial (inner) part of the foot.
When the leg flattens excessively, it can cause internal rotation of the tibia. Naturally, there is also a disposition of the femur and a change in movement in the hip joint. So, ultimately, excessive or increased movement towards the flattening of the foot can lead to the formation of pain from the foot to the hip and even in the lower back.
Therefore, it must be clearly defined whether the foot itself is the cause of leg rotation or whether there are other causes. Just as a flat foot can lead to rotation of the lower extremity, rotation of the hip can in turn lead to flattening of the foot. And only a thorough examination, including gait analysis, allows you to accurately diagnose and decide on treatment tactics.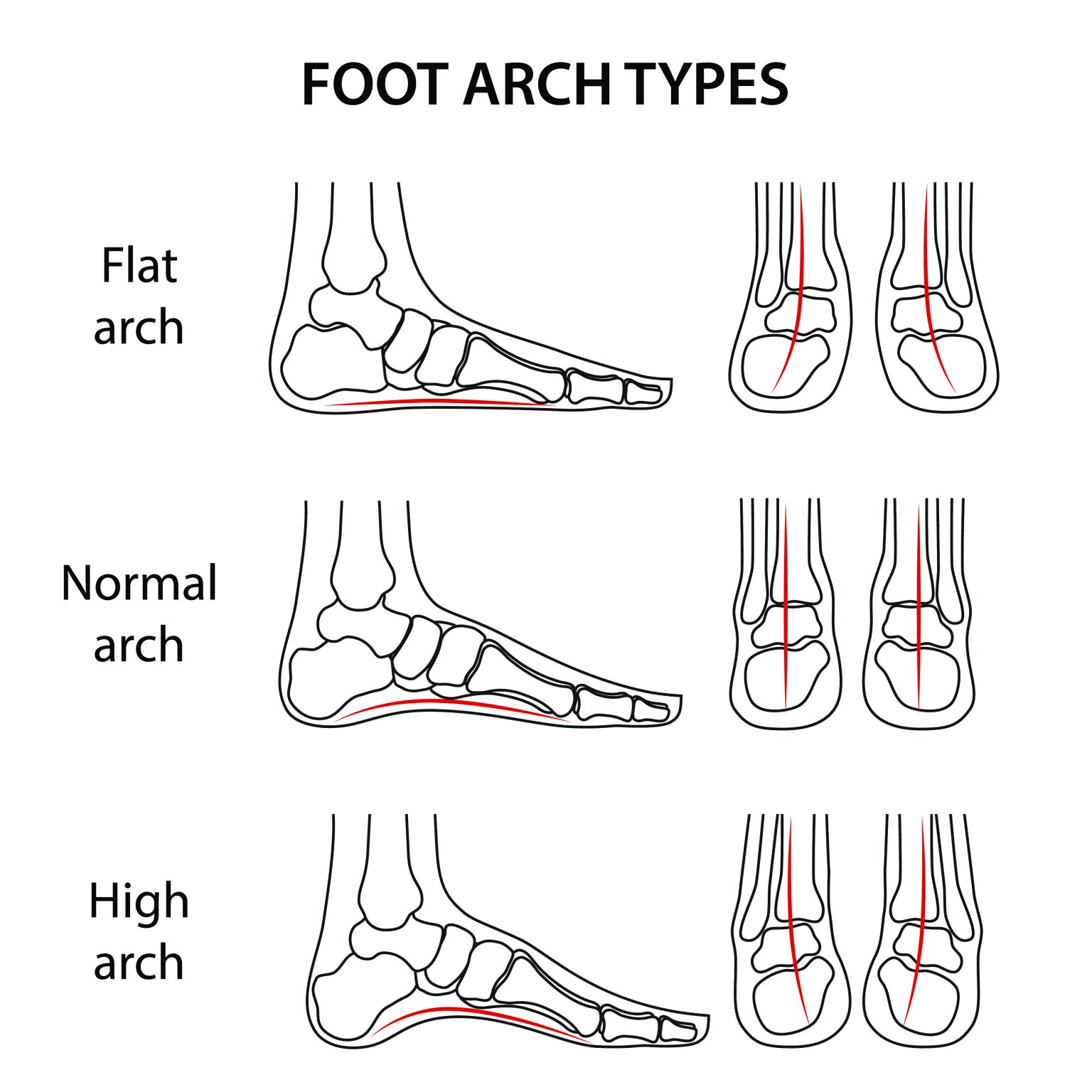
Symptoms
Most often, the patient does not experience any sensations, only a certain disturbance in gait, which may be noted by others or the doctor. The main symptom is ankle pain, which may increase after exercise. There may also be swelling in the ankle area. Symptoms can vary and usually depend on the severity of the flatfoot. Some of them have an uneven distribution of body weight and a person may notice that the heel of the shoe wears out faster on one side than on the other. Most common symptoms of flat feet are:
- Ankle pain (inner side), there may also be swelling
- Foot pain
- Pain in the arch of the foot
- Calf pain
- Pain in the knee area
- Pain in the thigh.
- Back pain
- Patients with flat feet may also experience stiffness in one or both legs.
- One or both feet may be placed flat on the ground.
- Uneven shoe wear.

Causes
- Genetic determinism.
- A weak arch of the foot may not be a concern while the person is sitting, but as soon as he gets to his feet, he may fall.
- Trauma
- Arthritis of the ankle joint
- Posterior tibial tendon rupture
- Pregnancy
- Diseases of the nervous system or muscles – such as cerebral palsy, muscular dystrophy, or spina bifida.
- Tarsal fusion can cause hardening and flat feet. Most often diagnosed in childhood.
- Diabetes
- Age changes. Long-term loads (running, jumping, walking) can have negative consequences. One possible consequence could be flat feet. The tibialis posterior tendon may become weak after repeated microtearing. The tibialis posterior tendon is the main supporting structure of the arch of the foot. The tendon can become inflamed (tendonitis) after exercise or even tear. After injury to the tendon, the arch of the foot may flatten.

The presence of flat feet in childhood is not a pathology, since the formation of the foot ends with the end of the formation of the musculoskeletal system. In other words, the presence of flat feet in childhood does not mean at all that flat feet will remain in an adult. People with a low arch or no arch at all may not experience any problems until a certain time.
Diagnosis
People who have flat feet may not experience any symptoms and may not see an orthopedic doctor. However, if there are certain signs, such as a visually flat foot, pain in the foot, ankles or lower limbs, a feeling of tension in the legs, heaviness in the legs, especially after exercise, then you need to consult an orthopedist.
Diagnosis of flatfoot is not difficult for a qualified doctor, who can make such a diagnosis based on the examination of the patient. The doctor will evaluate the person’s gait, the location of the foot to the surface, and evaluate the functional state of each leg.
In some cases, the doctor may order X-ray, CT or MRI, especially if it is necessary to determine the cause of flat feet. A good result is also given by podography, which allows to assess the degree of flat feet .
Treatment
Some patients with flat feet will adapt to the change in the arch and in such cases no treatment is required.
Foot pain caused by flat feet can be greatly minimized with well-fitting footwear.
Ready-made orthopedic insoles or made-to-measure insoles can largely compensate for the lowering of the arch of the foot, and can reduce both the load on the foot and reduce the violation of the biomechanics of movement.
Patients with tibialis posterior tendonitis may benefit from orthotic inserts that reduce stress on the tendon.
Wearing ankle braces helps patients with tendinitis reduce inflammation in the tendon.
Reducing the load on the foot also reduces foot discomfort.
For tendon rupture or arthritis, a combination of NSAIDs and orthopedic insoles is possible, but if conservative treatment is not effective, then surgical treatment may be required in such cases.
In the presence of congenital anomalies in the development of the foot, surgical treatment may also be prescribed, especially if there is a fusion of the bones of the foot.
Weight loss in obesity reduces the load on the foot and significantly reduces pain.
As a rule, with flat feet caused by degenerative changes, surgical treatment is not required, but if there is a pronounced pain syndrome, then surgical operations are possible – arthrodesis, removal of bone growths, change in the shape of the bone (osteotomy), cleansing of tendons from membranes (synovectomy) , tendon plasty using autografts, reconstructive operations on bone tissue.
Prophylaxis
- Wearing shoes or insoles appropriate for the activity.
- Rest for legs after exercise.
- exercise therapy helps to strengthen the muscles of the foot and prepare the feet for physical activity.
- Treatment or management of factors that contribute to the development and increase of flat feet, such as diabetes, obesity, or vascular disease.