Treating diaper rash yeast infection. Yeast Diaper Rash: Effective Treatment and Prevention Strategies
How to identify yeast diaper rash. What are the best home remedies for yeast diaper rash. How to prevent yeast diaper rash from recurring. When to seek medical attention for diaper rash.
Understanding Yeast Diaper Rash: Causes and Symptoms
Yeast diaper rash is a distinct condition from regular diaper rash, primarily caused by an overgrowth of Candida yeast on the skin. While yeast naturally exists on the skin, certain conditions can lead to its excessive growth, resulting in an infection. This type of rash is more common in warm, moist areas and can develop where a regular diaper rash already exists.
Identifying a yeast diaper rash is crucial for proper treatment. Here are the key symptoms to look out for:
- Red skin with dots or pimples
- Rash that doesn’t respond to standard diaper creams
- Persistent rash that takes longer to heal
- Rash occurring more in the folds of legs, genitals, or buttocks
- Possible satellite spots of rash outside the main affected area
- May occur alongside thrush infection in the baby’s mouth
Understanding these symptoms can help differentiate yeast diaper rash from regular diaper rash, ensuring appropriate treatment is administered promptly.

Effective Home Remedies for Treating Yeast Diaper Rash
While yeast diaper rash often requires specific antifungal treatment, several home remedies can help alleviate symptoms and promote healing. Here are some effective strategies:
1. Maintain Proper Hygiene
Keeping the diaper area clean is paramount in treating yeast diaper rash. Gently and thoroughly clean the entire diaper area during each change. This not only helps remove yeast but also reduces the risk of secondary infections. Remember to wash your hands and any surfaces the baby has been in contact with to prevent the spread of yeast.
2. Keep the Area Dry
Yeast thrives in moist environments, so keeping the diaper area dry is crucial. Change diapers frequently, especially when wet. Allow the baby’s bottom to air dry between changes, gently patting the area dry instead of rubbing. A hair dryer on a low, cool setting can be used to speed up the drying process.
3. Implement Diaper-Free Time
Providing extended periods without a diaper can significantly help in drying out the affected area. Choose easy-to-clean areas of your home for diaper-free time, or use a towel or play mat to catch any messes. For younger babies, incorporate this into tummy time, while older, sitting babies can be entertained with toys during these periods.

4. Avoid Irritants
The infected area will be sensitive, so it’s important to avoid products that may cause further irritation. Steer clear of soap, bubble bath, and even wipes during diaper changes. Instead, use a clean towel dampened with warm water to clean the diaper area gently.
Antifungal Treatments for Yeast Diaper Rash
While home remedies can help manage symptoms, most yeast diaper rashes require specific antifungal treatment. Here’s what you need to know:
- Consult your doctor about using an antifungal or yeast cream
- Many effective treatments are available over the counter
- Follow your doctor’s or pharmacist’s instructions on application frequency and duration
- Gentian violet may be an alternative treatment, but consult your doctor first
Are natural remedies safe for treating yeast diaper rash? Always consult your doctor before using natural remedies like vinegar or oils. While natural doesn’t always mean safe, some natural treatments may be beneficial when used correctly and under medical guidance.

Preventing Yeast Diaper Rash: Proactive Measures
Prevention is often the best approach when it comes to yeast diaper rash. Here are some proactive measures you can take:
- Change diapers frequently, especially after bowel movements
- Ensure the diaper area is completely dry before putting on a new diaper
- Use breathable diapers to reduce moisture
- Consider using a barrier cream to protect the skin
- Avoid tight-fitting diapers or plastic pants over diapers
- Wash cloth diapers in hot water and avoid fabric softeners
By implementing these preventive strategies, you can significantly reduce the risk of yeast diaper rash occurring or recurring.
The Controversy Surrounding Baby Powder and Yeast Diaper Rash
The use of baby powder in preventing and treating yeast diaper rash has been a subject of debate. Does baby powder help with yeast diaper rash? The answer isn’t straightforward.
Some believe that yeast can feed on cornstarch, a common ingredient in many baby powders. However, research on this topic is mixed. A study from 1984 found no significant difference in yeast growth between skin treated with cornstarch powder and untreated skin.

Given the potential risks associated with talc-based powders and the inconclusive evidence on cornstarch-based powders, it’s best to consult with your pediatrician before using any powder in the diaper area.
When to Seek Medical Attention for Yeast Diaper Rash
While many cases of yeast diaper rash can be managed at home, there are instances when professional medical attention is necessary. Here are some signs that indicate it’s time to consult a doctor:
- The rash persists for more than a week despite home treatment
- The rash appears to be spreading or worsening
- Your baby develops a fever
- The rash is accompanied by blisters or pus-filled sores
- Your baby seems to be in significant discomfort or pain
- You notice signs of the yeast infection in other areas, such as the mouth
A healthcare professional can provide a definitive diagnosis and prescribe stronger antifungal medications if necessary. They can also rule out other potential skin conditions that may require different treatments.

The Impact of Diet on Yeast Diaper Rash
Diet can play a role in the development and persistence of yeast diaper rash, both for breastfed and formula-fed babies. Here’s what you need to know:
For Breastfed Babies
The mother’s diet can influence the baby’s susceptibility to yeast infections. Foods high in sugar and refined carbohydrates can potentially increase the risk. Some experts suggest that mothers of babies with recurring yeast diaper rash consider reducing their intake of:
- Sugar and sweetened foods
- White flour and other refined grains
- Alcohol
- Fermented foods
On the other hand, probiotic-rich foods may help combat yeast overgrowth. These include yogurt, kefir, and other fermented foods.
For Formula-Fed Babies
If your formula-fed baby is prone to yeast diaper rash, consider discussing alternative formulas with your pediatrician. Some babies may benefit from formulas with reduced sugar content or those designed to be gentler on the digestive system.
It’s important to note that dietary changes should always be made under the guidance of a healthcare professional to ensure your baby’s nutritional needs are still being met.

Long-Term Management of Recurrent Yeast Diaper Rash
For some babies, yeast diaper rash can be a recurring issue. In these cases, a more comprehensive management plan may be necessary. Here are some strategies for long-term management:
- Identify and address underlying causes: Recurrent yeast infections may be a sign of an underlying health issue, such as a weakened immune system or chronic skin condition. Work with your pediatrician to identify and address any potential underlying causes.
- Consider probiotics: Some studies suggest that probiotics may help prevent recurrent yeast infections. Discuss with your doctor whether probiotic supplements might be beneficial for your baby.
- Maintain strict hygiene practices: Be vigilant about diaper changing routines, ensuring the area is always clean and dry.
- Use preventive treatments: Your doctor may recommend using an antifungal cream or powder preventively, especially after antibiotic treatment, which can disrupt the natural balance of bacteria and yeast on the skin.
- Regular check-ups: Schedule regular check-ups with your pediatrician to monitor the situation and adjust the management plan as needed.
Remember, every baby is different, and what works for one may not work for another. Patience and persistence are key in managing recurrent yeast diaper rash.
By understanding the causes, symptoms, and treatment options for yeast diaper rash, parents can effectively manage this common condition and keep their baby comfortable. Always consult with a healthcare professional for persistent or severe cases to ensure proper treatment and prevent complications.
Yeast Diaper Rash: Symptoms, Pictures, Home Remedies
Diaper rashes are a common problem for babies. But, a yeast diaper rash is different than regular diaper rash. With a regular diaper rash, an irritant causes the rash. But with a yeast diaper rash, yeast (Candida) causes the rash.
A yeast diaper rash is different than regular diaper rash. With a regular diaper rash, an irritant causes the rash. But with a yeast diaper rash, yeast (Candida) causes the rash.
Yeast is a living microorganism. It naturally lives on skin but can be hard to tame when there’s an overgrowth.
Anyone using a diaper can develop a yeast diaper rash. Read on to learn how to identify, treat, and prevent this type of diaper rash.
Yeast diaper rashes require different treatment than a standard diaper rash, so it’s important to be able to identify the type of rash.
| Yeast diaper rash symptoms | Regular diaper rash symptoms |
|---|---|
| red skin with dots or pimples | pink to reddish skin that’s smooth or chapped |
| rash doesn’t respond to standard diaper creams and takes a while to treat | rash responds to standard diaper creams and clears up in 2-3 days |
| rash may occur more in the folds of legs, genitals, or buttocks | rash may occur on smoother surfaces of the buttocks or on the vulva |
| rash may occur along with thrush infection in baby’s mouth | rash doesn’t usually occur along with oral thrush |
| may have satellite spots of rash outside the border of the rest of the rash | rash is localized to one area |
Yeast can be present on the skin and in other parts of the body with no symptoms or negative effects. However, if the yeast overgrows, it can cause an infection in the area. Overgrowth often happens in warm, moist areas or where a regular diaper rash already exists.
However, if the yeast overgrows, it can cause an infection in the area. Overgrowth often happens in warm, moist areas or where a regular diaper rash already exists.
The goal of treating a yeast infection in the diaper area is to heal the skin and reduce exposure to yeast.
The following home remedies may help treat the infection.
Keep the area clean
Gently and thoroughly clean the whole diaper area every time you change the diaper. It can help remove yeast and also reduce the risk of other infections.
It’s also important to thoroughly wash your hands and anything your baby laid on during the diaper change. This can help prevent the spread of the yeast.
Keep the area dry
Change your baby more frequently. If you notice their diaper is wet, change them right away. Yeast thrives in warm, damp areas, so keeping the area dry can help stop the spread of the yeast.
In addition to more frequent diaper changes, also allow baby’s bottom to air dry between changes. Gently pat the area dry, but avoid rubbing, which can further irritate the skin. You can use a hair dryer on the low, cool setting to help speed up the drying process.
Gently pat the area dry, but avoid rubbing, which can further irritate the skin. You can use a hair dryer on the low, cool setting to help speed up the drying process.
Have diaper-free time
Give baby extended time without any diaper on to further help dry out the diaper area. This can get messy, so consider having diaper-free time in areas of your home that are easy to clean, or put a towel or play mat under baby to help catch any messes.
To further reduce the risk of messes, have diaper-free time immediately after a diaper change. If baby has recently gone to the bathroom, they’re less likely to need to go again anytime soon.
For younger babies, you can do diaper-free time during their usual tummy time. For sitting babies, place books and engaging toys around them to try and keep them entertained on the towel.
Avoid irritants
The infected area will be tender. Irritating products can make discomfort worse, like soap and bubble bath.
You may also want to hold off on using wipes during diaper changes.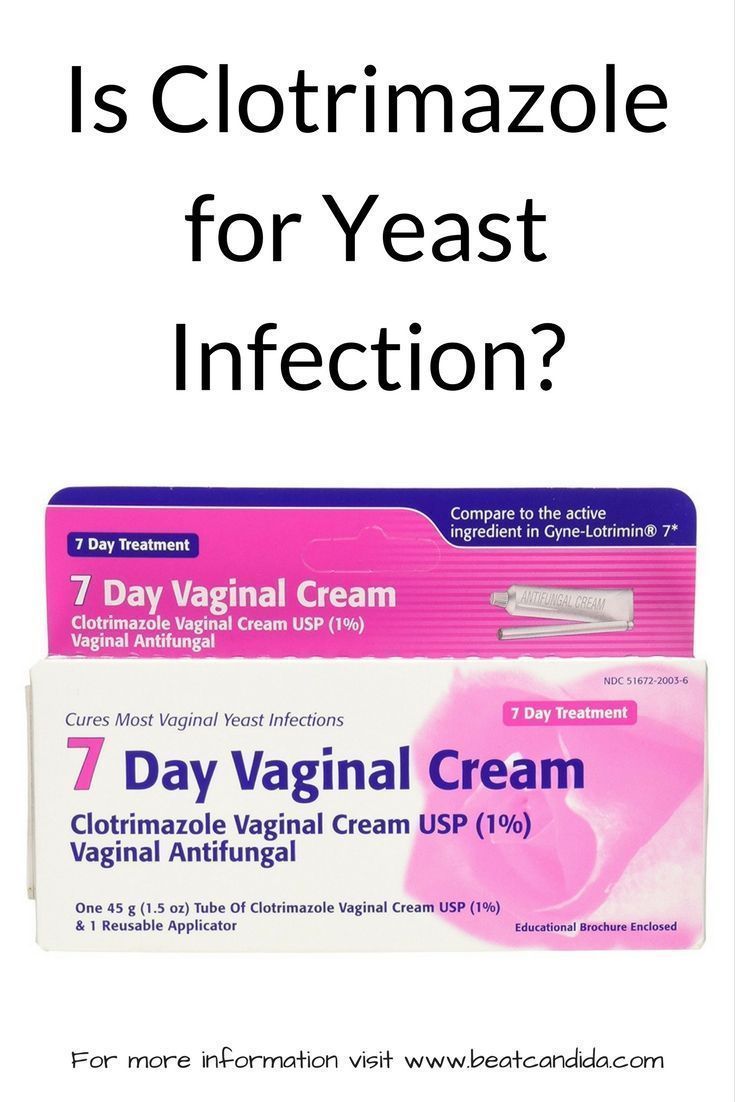 Instead, use a clean towel that’s been dampened in warm water to clean the diaper area.
Instead, use a clean towel that’s been dampened in warm water to clean the diaper area.
Use antifungal creams
The above measures can help treat the symptoms of a yeast diaper rash and may help it to go away faster, but most yeast rashes need further treatment. Ask your doctor about using an antifungal or yeast cream. Many can be purchased over the counter.
Ask your pharmacist or doctor for specific instructions, such as how often to use each day and for how long to use the treatment.
You can also ask your doctor about applying gentian violet. This is a dark purple ointment known to kill yeast, but it may not be as effective as other antifungal treatments. If you do use it, be very careful when applying, as it stains clothing.
Are natural remedies safe to use?
Ask your doctor before using natural remedies like vinegar or oils. Natural doesn’t always mean safe.
If your doctor gives you the OK, remember that a small amount goes a long way, so be sure to dilute products well.
Does baby powder help?
There’s mixed information about whether or not it’s safe to use baby powder to try to keep the diaper area dry and help prevent a yeast rash. Many believe yeast will feed on cornstarch. Cornstarch is the main ingredient in many baby powders.
As part of an older study from 1984, researchers tested for this and found no correlation between cornstarch use and increased yeast growth.
However, baby powder hasn’t been shown to treat a yeast diaper rash that’s already present. In fact, it’s not recommended to use baby powder on children, as inhaling it can damage their lungs.
Always see a doctor if your baby is very fussy, seems sick, or the rash looks infected. Doctors can help create a treatment plan to alleviate pain and help your baby heal fast.
Also see a doctor if the rash has lasted for more than a few days or isn’t responding to treatment.
In many cases, a doctor can identify a yeast infection through a physical examination of the rash. Sometimes, though, the doctor may need to scrape off a bit of skin to test for yeast or bacterial infection in the rash.
Sometimes, though, the doctor may need to scrape off a bit of skin to test for yeast or bacterial infection in the rash.
Most diaper rashes can be treated without prescriptions. Rarely, a diaper rash may be serious and affect other parts of the body. Severe yeast infections may be treated with medicated suppositories or oral antifungal medication.
Sometimes what appears as a yeast rash can actually be a bacterial infection. This is a serious issue. It may require antibiotics to treat and prevent further complications.
Possible complications from diaper rash include scabbing skin, bleeding, and irritability.
In extreme cases, a yeast diaper rash can infect other parts of the body, like skin and blood. This is more serious and needs to be urgently treated by a doctor.
Babies with a yeast diaper rash may also develop thrush. If you breastfeed, you may develop a yeast rash on your breasts.
Most diaper rashes should improve after two to three days of treatment. However, yeast infections can take several weeks to heal since the yeast is a living organism that needs to be killed.
However, yeast infections can take several weeks to heal since the yeast is a living organism that needs to be killed.
You’ll know your baby has recovered once the rash has disappeared and the skin is healed.
Call your doctor if diaper rash is persistent, doesn’t improve, gets worse with treatment, or is very painful.
The steps to prevent a yeast diaper rash are similar to many of the steps you can use to treat it at home.
Diaper rashes are very common since diapers are often warm and moist. Keeping your baby clean and as dry as possible is the best way to prevent rashes and a yeast diaper rash.
Consider these preventive tips:
- Regularly bathe baby in warm water. Clean their diaper area each time you change their diaper.
- Change diapers often. Avoid leaving baby in a wet diaper.
- Let baby’s bottom air-dry for as long as possible after every diaper change. Patting baby’s bum with a soft cloth or using a blow dryer on the cool-air setting may help speed up the process.

- Give baby regular diaper-free time.
- Don’t use rubber pants or diapers that prevent air flow. These can trap moisture near skin.
- Consider using a diaper cream to help protect your baby’s skin. Creams provide a barrier from urine and stool, which can irritate skin and make it prone to developing a rash.
- Avoid baby products that contain fragrances and dyes, such as lotions or soaps. These additives can irritate the skin.
- Don’t give baby unnecessary antibiotics, as they can cause an imbalance of healthy bacteria and yeasts in the body.
A yeast diaper rash is different than a regular diaper rash because it involves a microorganism (yeast) and not just irritated skin.
Treating a yeast diaper rash can be more difficult than treating a regular diaper rash. Most yeast diaper rashes can be treated at home, but see a doctor if your baby is very uncomfortable, the rash isn’t improving or keeps recurring, or if you think your baby has thrush.
Yeast Diaper Rash: Symptoms, Pictures, Home Remedies
Diaper rashes are a common problem for babies. But, a yeast diaper rash is different than regular diaper rash. With a regular diaper rash, an irritant causes the rash. But with a yeast diaper rash, yeast (Candida) causes the rash.
A yeast diaper rash is different than regular diaper rash. With a regular diaper rash, an irritant causes the rash. But with a yeast diaper rash, yeast (Candida) causes the rash.
Yeast is a living microorganism. It naturally lives on skin but can be hard to tame when there’s an overgrowth.
Anyone using a diaper can develop a yeast diaper rash. Read on to learn how to identify, treat, and prevent this type of diaper rash.
Yeast diaper rashes require different treatment than a standard diaper rash, so it’s important to be able to identify the type of rash.
| Yeast diaper rash symptoms | Regular diaper rash symptoms |
|---|---|
| red skin with dots or pimples | pink to reddish skin that’s smooth or chapped |
| rash doesn’t respond to standard diaper creams and takes a while to treat | rash responds to standard diaper creams and clears up in 2-3 days |
| rash may occur more in the folds of legs, genitals, or buttocks | rash may occur on smoother surfaces of the buttocks or on the vulva |
| rash may occur along with thrush infection in baby’s mouth | rash doesn’t usually occur along with oral thrush |
| may have satellite spots of rash outside the border of the rest of the rash | rash is localized to one area |
Yeast can be present on the skin and in other parts of the body with no symptoms or negative effects. However, if the yeast overgrows, it can cause an infection in the area. Overgrowth often happens in warm, moist areas or where a regular diaper rash already exists.
However, if the yeast overgrows, it can cause an infection in the area. Overgrowth often happens in warm, moist areas or where a regular diaper rash already exists.
The goal of treating a yeast infection in the diaper area is to heal the skin and reduce exposure to yeast.
The following home remedies may help treat the infection.
Keep the area clean
Gently and thoroughly clean the whole diaper area every time you change the diaper. It can help remove yeast and also reduce the risk of other infections.
It’s also important to thoroughly wash your hands and anything your baby laid on during the diaper change. This can help prevent the spread of the yeast.
Keep the area dry
Change your baby more frequently. If you notice their diaper is wet, change them right away. Yeast thrives in warm, damp areas, so keeping the area dry can help stop the spread of the yeast.
In addition to more frequent diaper changes, also allow baby’s bottom to air dry between changes. Gently pat the area dry, but avoid rubbing, which can further irritate the skin. You can use a hair dryer on the low, cool setting to help speed up the drying process.
Gently pat the area dry, but avoid rubbing, which can further irritate the skin. You can use a hair dryer on the low, cool setting to help speed up the drying process.
Have diaper-free time
Give baby extended time without any diaper on to further help dry out the diaper area. This can get messy, so consider having diaper-free time in areas of your home that are easy to clean, or put a towel or play mat under baby to help catch any messes.
To further reduce the risk of messes, have diaper-free time immediately after a diaper change. If baby has recently gone to the bathroom, they’re less likely to need to go again anytime soon.
For younger babies, you can do diaper-free time during their usual tummy time. For sitting babies, place books and engaging toys around them to try and keep them entertained on the towel.
Avoid irritants
The infected area will be tender. Irritating products can make discomfort worse, like soap and bubble bath.
You may also want to hold off on using wipes during diaper changes.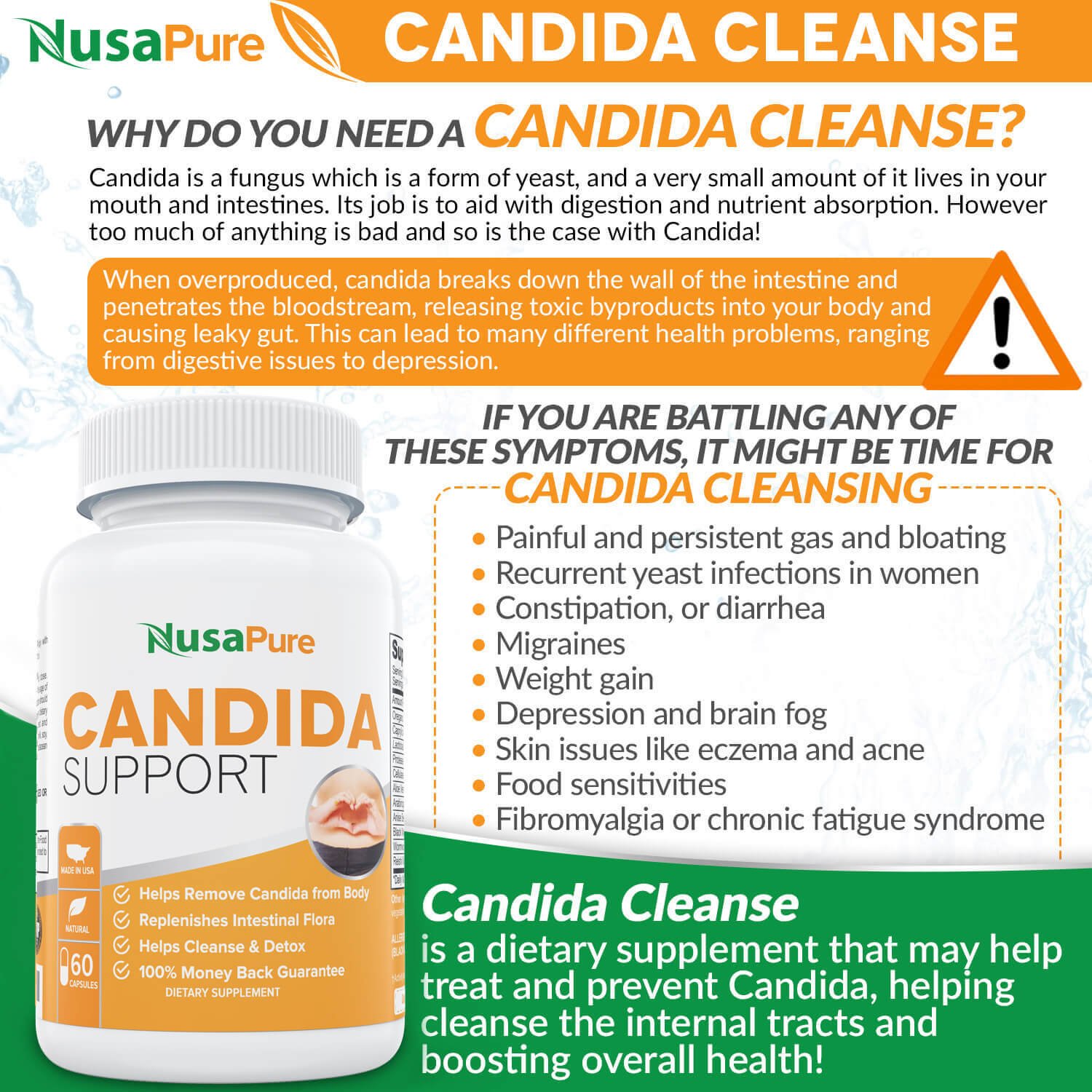 Instead, use a clean towel that’s been dampened in warm water to clean the diaper area.
Instead, use a clean towel that’s been dampened in warm water to clean the diaper area.
Use antifungal creams
The above measures can help treat the symptoms of a yeast diaper rash and may help it to go away faster, but most yeast rashes need further treatment. Ask your doctor about using an antifungal or yeast cream. Many can be purchased over the counter.
Ask your pharmacist or doctor for specific instructions, such as how often to use each day and for how long to use the treatment.
You can also ask your doctor about applying gentian violet. This is a dark purple ointment known to kill yeast, but it may not be as effective as other antifungal treatments. If you do use it, be very careful when applying, as it stains clothing.
Are natural remedies safe to use?
Ask your doctor before using natural remedies like vinegar or oils. Natural doesn’t always mean safe.
If your doctor gives you the OK, remember that a small amount goes a long way, so be sure to dilute products well.
Does baby powder help?
There’s mixed information about whether or not it’s safe to use baby powder to try to keep the diaper area dry and help prevent a yeast rash. Many believe yeast will feed on cornstarch. Cornstarch is the main ingredient in many baby powders.
As part of an older study from 1984, researchers tested for this and found no correlation between cornstarch use and increased yeast growth.
However, baby powder hasn’t been shown to treat a yeast diaper rash that’s already present. In fact, it’s not recommended to use baby powder on children, as inhaling it can damage their lungs.
Always see a doctor if your baby is very fussy, seems sick, or the rash looks infected. Doctors can help create a treatment plan to alleviate pain and help your baby heal fast.
Also see a doctor if the rash has lasted for more than a few days or isn’t responding to treatment.
In many cases, a doctor can identify a yeast infection through a physical examination of the rash. Sometimes, though, the doctor may need to scrape off a bit of skin to test for yeast or bacterial infection in the rash.
Sometimes, though, the doctor may need to scrape off a bit of skin to test for yeast or bacterial infection in the rash.
Most diaper rashes can be treated without prescriptions. Rarely, a diaper rash may be serious and affect other parts of the body. Severe yeast infections may be treated with medicated suppositories or oral antifungal medication.
Sometimes what appears as a yeast rash can actually be a bacterial infection. This is a serious issue. It may require antibiotics to treat and prevent further complications.
Possible complications from diaper rash include scabbing skin, bleeding, and irritability.
In extreme cases, a yeast diaper rash can infect other parts of the body, like skin and blood. This is more serious and needs to be urgently treated by a doctor.
Babies with a yeast diaper rash may also develop thrush. If you breastfeed, you may develop a yeast rash on your breasts.
Most diaper rashes should improve after two to three days of treatment. However, yeast infections can take several weeks to heal since the yeast is a living organism that needs to be killed.
However, yeast infections can take several weeks to heal since the yeast is a living organism that needs to be killed.
You’ll know your baby has recovered once the rash has disappeared and the skin is healed.
Call your doctor if diaper rash is persistent, doesn’t improve, gets worse with treatment, or is very painful.
The steps to prevent a yeast diaper rash are similar to many of the steps you can use to treat it at home.
Diaper rashes are very common since diapers are often warm and moist. Keeping your baby clean and as dry as possible is the best way to prevent rashes and a yeast diaper rash.
Consider these preventive tips:
- Regularly bathe baby in warm water. Clean their diaper area each time you change their diaper.
- Change diapers often. Avoid leaving baby in a wet diaper.
- Let baby’s bottom air-dry for as long as possible after every diaper change. Patting baby’s bum with a soft cloth or using a blow dryer on the cool-air setting may help speed up the process.

- Give baby regular diaper-free time.
- Don’t use rubber pants or diapers that prevent air flow. These can trap moisture near skin.
- Consider using a diaper cream to help protect your baby’s skin. Creams provide a barrier from urine and stool, which can irritate skin and make it prone to developing a rash.
- Avoid baby products that contain fragrances and dyes, such as lotions or soaps. These additives can irritate the skin.
- Don’t give baby unnecessary antibiotics, as they can cause an imbalance of healthy bacteria and yeasts in the body.
A yeast diaper rash is different than a regular diaper rash because it involves a microorganism (yeast) and not just irritated skin.
Treating a yeast diaper rash can be more difficult than treating a regular diaper rash. Most yeast diaper rashes can be treated at home, but see a doctor if your baby is very uncomfortable, the rash isn’t improving or keeps recurring, or if you think your baby has thrush.
Yeast in baby’s stool: causes, effects and treatment
Content
- 1 Yeast in baby’s stool: causes, effects and treatments
- 1.1 What are yeast and how do they appear in stool?
- 1.2 Causes of yeast in a child’s stool
- 1.3 What signs indicate the presence of yeast in a child’s stool?
- 1.4 Effects of yeast in a child’s stool
- 1.5 When should I see a doctor if a yeast infection is found in a child’s stool?
- 1.6 How is yeast in a child’s stool diagnosed?
- 1.7 How to treat yeast in a child
- 1.8 What medications will help cure yeast in a child?
- 1.9 Folk remedies for the treatment of yeast fungi in a child
- 1.10 How to maintain a healthy microflora in the intestines and prevent the appearance of yeast fungi?
- 1.11 Diet in the treatment of yeast in a child
- 1.12 How can the use of prebiotics and probiotics help in the treatment of yeast in a child?
- 1.
 13 How can I prevent yeast infection in my child?
13 How can I prevent yeast infection in my child? - 1.14 Factors contributing to the appearance of yeast in a child
- 1.15 How to avoid the recurrence of yeast in a child after treatment?
- 1.16 The effect of yeast in the stool on the health of a child
- 1.16.1 The positive effect of yeast in the stool of a child
- 1.16.2 The negative effect of yeast in the stool of a child
- 1.16.3 How to deal with yeast oyster mushrooms in baby’s feces
- 1.17 Possible complications from yeast in the stool in a child
- 1.18 How to treat yeast in a child and what precautions should be taken?
- 1.19 Q&A:
- 1.19.0.1 What are yeast fungi?
- 1.19.0.2 How do yeasts get into the baby’s stool?
- 1.19.0.3 What symptoms indicate the presence of yeast in the stool of a child?
- 1.19.0.4 What are the consequences of having yeast in a child’s stool?
- 1.19.0.5 How is yeast in a child’s stool diagnosed?
- 1.
 19.0.6 What are the treatments for yeast in a child’s stool?
19.0.6 What are the treatments for yeast in a child’s stool? - 1.19.0.7 How to prevent the development of yeast fungi in the stool of a child?
- 1.19.0.8 How long can a yeast infection in a child’s stool last?
An article about how the detection of yeast fungi in a child’s stool affects his health, whether it is dangerous and whether treatment is required. Find out what to do if your child is the victim of a similar problem.
The presence of yeast in a child’s stool can cause concern to parents. This problem is quite common, especially in young children. However, the presence of these fungi is not always a pathology and requires a thorough medical examination.
Yeast in stool can be caused by a variety of factors, such as an unbalanced diet, antibiotics, problems with the immune system, and other illnesses. Also, excessive consumption of sweet and starchy foods can contribute to the development of this problem.
This article will tell you about the causes of yeast in the stool, the consequences and how to properly detect and treat this problem. We hope that this information will be useful for parents and will help them with a more detailed understanding of this problem and its solution.
What are yeast fungi and how do they appear in stool?
Yeasts are microscopic fungi that can be found both in the environment and inside our body. These fungi can cause various diseases, including infections of the skin, mouth, genitals, etc.
When referring to yeast in stool, it usually means the presence of Candida albicans, one of the most common types of yeast. Usually fungi appear in the intestines of the child and in some cases can be excreted in the feces.
Yeast in the stool may be due to various causes, including antibiotic therapy or malnutrition. Dietary disturbances can lead to an increase in blood sugar levels, which creates a favorable environment for yeast to thrive.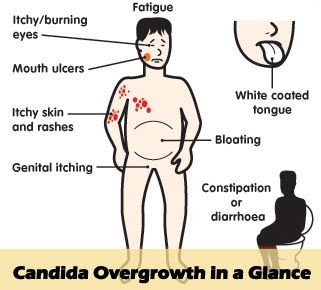 Also, the intestinal microflora can be disturbed as a result of the introduction of new foods or the introduction of complementary foods.
Also, the intestinal microflora can be disturbed as a result of the introduction of new foods or the introduction of complementary foods.
Normally, yeasts are also present in the gut and partly serve to maintain the microbiome. However, an increase in their number can lead to the development of Candidiasis, an infection caused by yeast fungi.
Causes of yeast in the stool in a child
Yeast is found in the intestines of all people, however, sometimes their number can become excessive in a child, thus causing health problems.
Some of the main reasons why yeast can multiply in a child’s gut:
- Violation of the intestinal microflora. Consuming large amounts of antibiotics can upset the balance of microbes in the baby’s gut, which will encourage yeast to thrive.
- Immunodeficiencies. A child with an immune system disorder, such as AIDS, may be more susceptible to yeast overgrowth.
- Diet. Eating a lot of sugary foods, foods with alcohol, and fried foods can also cause yeast overgrowth in a child’s intestines.

If you suspect that your child has an overgrowth of yeast in the intestines, you should contact your doctor to discuss possible treatment options and a diet that can help you avoid recurring yeast overgrowth.
What signs indicate the presence of yeast fungi in the stool of a child?
Yeast fungi can cause a number of unpleasant effects in children. Possible signs of the presence of yeast in the feces of a child are: yellowness of the skin, itching, diarrhea, constipation, an increase in the abdomen, possibly accompanied by painful sensations. If the properties of feces are violated, then it can acquire an unpleasant odor and color, which may be undesirable.
If you notice any of these signs in your child’s behavior or health, you are advised to contact your doctor immediately. The doctor will check the child’s health, if necessary, write out recommendations for restoring immunity and preventing diseases.
Effects of yeast fungus in the stool of a child
Allergic reactions: One of the possible consequences of infection with yeast fungi in the stool of a child are allergic reactions such as itching, skin rash or anaphylactic shock. With an increased skin reaction to foods or other substances, the child may be at an increased risk of developing allergic reactions when infected with yeast fungi.
With an increased skin reaction to foods or other substances, the child may be at an increased risk of developing allergic reactions when infected with yeast fungi.
Diarrhea and gastrointestinal disorders: Yeasts can cause intestinal dysbiosis in children, resulting in diarrhea, constipation, flatulence, colic and other gastrointestinal disorders. If a child has gastrointestinal health problems, then yeast infection can lead to worsening of symptoms.
Skin health problems: Yeast can be one of the causes of various skin health problems in a child. These can be eczema, dermatitis, psoriasis, various inflammations and other problems that require the intervention of a doctor.
Disturbances of normal microflora: Yeast fungi can disrupt the natural balance of the microflora in a child’s body, crowding out beneficial bacteria. This can lead to various diseases and slow down the growth and development of the child.
Development of fungal infections: If yeast fungi are found in the intestines of a child, then fungal infections may develop, which can be dangerous to the health and life of the child. If you suspect the development of fungal infections, you should immediately consult a doctor.
When should I see a doctor if I have yeast in my child’s stool?
If yeast is found in a child’s stool test, this may be a sign of infection or dysbiosis in the intestines. Therefore, at the first signs of a violation of the stool or a deterioration in the general condition of the child, it is necessary to consult a doctor.
Your doctor may order additional testing and treatment, which may include a series of tests to calibrate your gut microflora, probiotics, and recommendations for dietary and disease management.
Seek medical attention as unregulated yeast growth in the intestines can lead to serious health problems and weaken the child’s immune system.
How is yeast fungus in the stool of a child diagnosed?
Yeast fungi can cause various diseases in a child, so it is important to detect them correctly and in a timely manner. Diagnosis of yeast infections in the stool of a child is carried out using the following methods:
- Microscopy – microscopic examination of stool allows the detection of yeast fungi. However, it is not always possible to determine their appearance, and this method is not exhaustive.
- Bacteriological analysis – specialists identify fungal colonies by breeding bacteria on a special nutrient medium. This method is more accurate and allows you to determine the concentration of fungi in feces.
- PCR diagnostics is a molecular biology based method that detects fungal DNA in feces. This method is the most accurate and sensitive, but requires special equipment and highly qualified laboratory assistant.
Consult a qualified mycologist or gastroenterologist for a reliable diagnosis of yeast in a child’s stool. Only they can determine the type of fungus and prescribe an effective treatment for your child.
Only they can determine the type of fungus and prescribe an effective treatment for your child.
Treatments for yeast in children
Yeast in children can be treated in a variety of ways, depending on the type and extent of the infection. The use of antimicrobials such as fluconazole, itraconazole, or ketoconazole is often recommended.
It is also important to change the child’s diet to remove the breeding ground for fungi. It is recommended to remove sweets, starch and alcoholic beverages from the diet. You can also add probiotic-rich foods such as yogurt, kefir, and cheeses to your child’s diet.
It is important to pay attention to the child’s hygiene. It is necessary to regularly change diapers in infants and monitor the cleanliness of the oral cavity in children. It is recommended to use emollient creams to reduce irritation caused by yeast.
Applying warm compresses and applying aloe vera and calendula peel creams can help relieve itching and irritation caused by yeast infections in children.
In some cases, it may be necessary to consult a specialist, such as a neurologist or gastroenterologist, to identify and treat the underlying disease causing yeast infections.
What drugs will help cure yeast fungi in a child?
To successfully treat yeast in a child, it is important to determine the type of yeast and prescribe the appropriate treatment. The doctor may prescribe antimycotic drugs, topical or systemic antifungals.
Antimycotics such as nystatin, clotrimazole and miconazole are used to treat skin lesions such as herpes zoster or thrush. Fluconazole and itraconazole may be used for systemic treatment.
Topical antifungals such as creams and ointments may be used to treat yeast infections of the skin, ear canal, and mouth. In pediatric practice, the external preparation Pimafucin is often used in the form of suppositories and creams.
To reduce the amount of yeast in the intestines, special probiotics or a diet that excludes foods that promote fungal growth from the diet can be used. Exogenous enzymes may also be prescribed.
Exogenous enzymes may also be prescribed.
When prescribing medications, it is important to follow all the doctor’s recommendations for dosage and duration of treatment in order to avoid side effects and re-infections. Also be aware of the possibility of an allergic reaction to the drug and consult your pediatrician if any symptoms appear.
Folk remedies for the treatment of yeast fungi in a child
Diagnosis of yeast infections in children is carried out by laboratory methods, and if the diagnosis is confirmed, mandatory treatment is required. Parents can also use folk remedies as an additional treatment.
Among folk remedies, the most famous are:
- Garlic . Garlic is known for its anti-fungal properties and can help fight yeast. Garlic can be added to food or eaten raw.
- Citrus . Citrus fruits are high in vitamin C, which boosts the immune system and helps fight infections. You can also use citrus essential oils for topical application.

- Humus . Humus contains many beneficial microorganisms that help fight yeast. Mix the humus with water and use the baby bath solution.
- Thyme . Thyme is known for its anti-inflammatory properties and can help reduce irritation and itching. Use thyme as a tea or add to baby’s bath.
Home remedies can help boost immunity and reduce symptoms of yeast infections in a child. However, before using folk remedies, be sure to consult a doctor and do not forget to follow the recommendations of a specialist.
How to maintain a healthy microflora in the intestines and prevent the appearance of yeasts?
One way to maintain a healthy microflora in the gut is to eat right. The diet should contain a large amount of fruits, vegetables, herbs and fiber-rich foods. It is also worth eating foods rich in prebiotics, such as oatmeal, whole grain bread, and yogurt.
Another major factor is the reduction in the consumption of products that can disrupt the microflora, such as canned food, juices, white bread and sweets.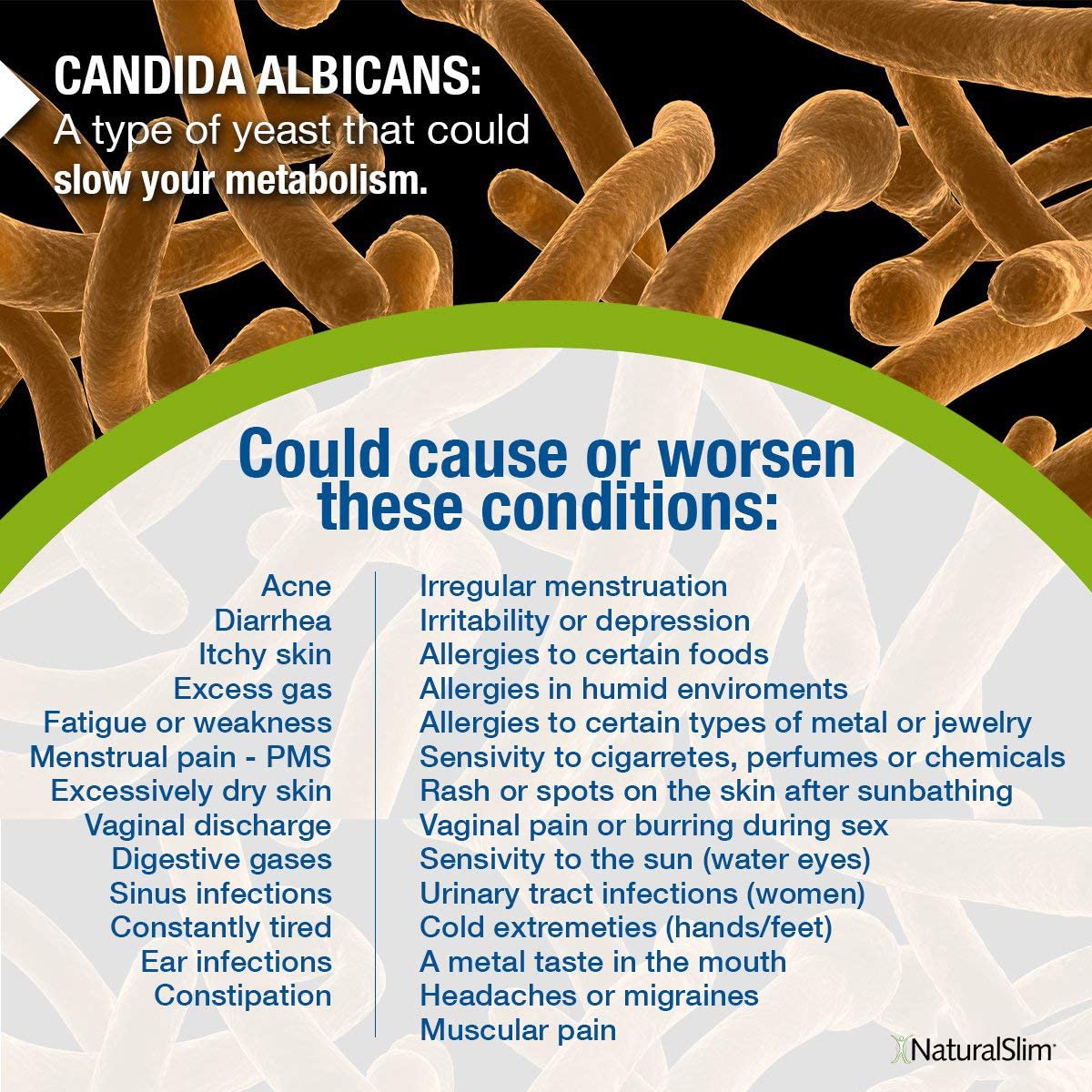 It is important to avoid excess sweet, salty, fatty and other unhealthy foods.
It is important to avoid excess sweet, salty, fatty and other unhealthy foods.
Regular intake of probiotics also contributes to a healthy microflora – they improve the condition of the digestive system and reduce the number of pathogens. But keep in mind that probiotic supplements may not be effective for all people and may cause side effects.
And, of course, it is important to keep hygiene, do not abuse antibiotics, be physically active and avoid stressful situations, which is the key to successful management of the state of your microflora.
- Summary: A healthy gut microflora plays a huge role in how our body functions. To maintain it, you need to limit the consumption of unhealthy foods, as well as add fruits, vegetables, whole grain bread and oatmeal to the diet. Regular consumption of probiotics can also improve the health of the microflora. The main thing here is hygiene and other healthy habits.
Diet when treating yeast in a child
Yeast can thrive on a carbohydrate diet, so it is recommended to monitor the child’s diet when treating a child with yeast.
Eat a diet that limits sugar and carbohydrates such as bread, processed foods, and canned foods. Meals should include more protein and fresh vegetables such as broccoli, spinach, onions, garlic, cabbage, and cauliflower.
Your child’s diet should be rich in probiotics, which inhibit yeast growth. Sources of probiotics include yogurt, kefir, tempeh, sauerkraut, and other fermented foods.
Be aware that food allergens can aggravate yeast growth. It is better to exclude dairy products from the child’s diet (if the child has allergies), processed foods, wheat flour and foods containing gluten.
It is important to note that changing your diet is not the only way to fight yeast. If your child has yeast, be sure to consult a doctor for advice on further treatment.
How can the use of prebiotics and probiotics help in the treatment of yeast fungi in a child?
Prebiotics and probiotics can be effective in treating yeast in a child. Prebiotics are substances that stimulate the growth and activity of beneficial bacteria in the gut, which helps improve the functioning of the immune system and thereby fight fungal infections. Probiotics, in turn, contain live microorganisms that help restore the balance of microflora and prevent the development of pathogenic microorganisms.
Probiotics, in turn, contain live microorganisms that help restore the balance of microflora and prevent the development of pathogenic microorganisms.
The choice of probiotics and prebiotics for the treatment of yeast in a child should be under the guidance of a physician. Some of the most effective yeast-fighting probiotics that a doctor may recommend include Lactobacillus casei, Lactobacillus acidophilus, and Bifidobacterium bifidum.
In addition, prebiotics can be found in many foods such as whole grains, vegetables, fruits and nuts. It is worth noting that the use of prebiotics and probiotics for the treatment of yeast fungi should not replace the main treatment prescribed by a doctor. However, their use in combination with other medicines may improve treatment outcomes and reduce the risk of future fungal infections.
How can I prevent yeast infections in my child?
Yeast fungi can appear in children for many reasons. To prevent their development, it is necessary to take certain preventive measures.
- Proper nutrition: Proper nutrition rich in vitamins and minerals should be provided to the child. It is not recommended to consume a large amount of sweets, carbohydrates and fatty foods, which provide fertile ground for the development of yeast.
- Hygiene: It is necessary to monitor the child’s hygiene and teach him to properly wash his hands before eating, after using the toilet, after playing outside. It is also necessary to monitor the condition of the baby’s skin for the appearance of diaper rash, cracks and other damage that can cause the development of a fungal infection.
- Immunity: It is important to strengthen the child’s immunity, for example, regularly harden, give him sports, choose the right antibacterial protection measures.
- Medical supervision: Regular medical check-ups should be carried out periodically and, if necessary, medical attention should be sought.
 An experienced doctor will be able to timely identify the manifestations of yeast in the intestines of the child and take the necessary therapeutic measures.
An experienced doctor will be able to timely identify the manifestations of yeast in the intestines of the child and take the necessary therapeutic measures.
Most importantly, parents should not panic if a yeast infection is found in their child. More importantly, keep an eye on your baby’s health and take steps to support his immunity.
Factors contributing to the appearance of yeast fungi in a child
Yeast fungi in the stool of a child can appear for various reasons. One of the factors is a violation of the microflora in the intestine. If a child has dysbacteriosis, then this creates favorable conditions for the reproduction of yeast fungi.
Another factor is the child’s diet. Overeating sweets and starchy foods can lead to an increased concentration of glucose in the intestines, which also contributes to the reproduction of yeast fungi.
Also, the child’s immune system may be weakened, which makes the body attractive to various harmful microorganisms, including yeasts.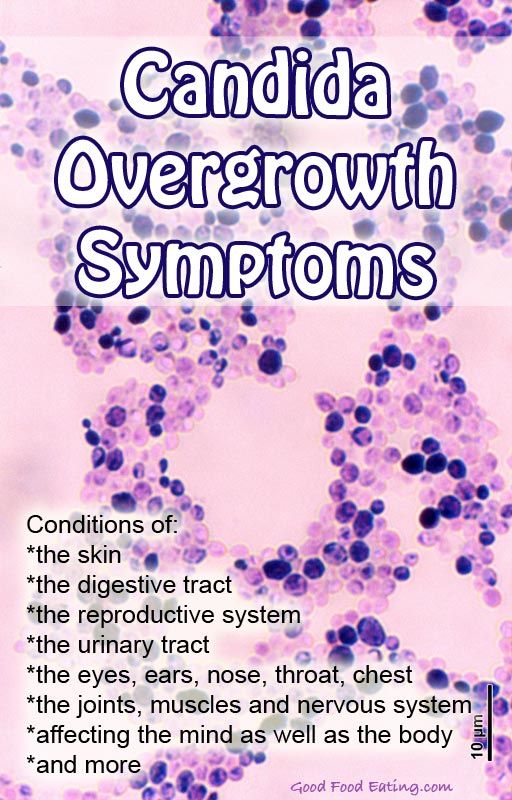
Some medicines can also cause yeast in a child. For example, antibiotics can destroy the beneficial intestinal microflora and create conditions for the reproduction of other microorganisms, including yeast fungi.
Finally, if a child’s hygiene is reduced, this can also contribute to the collection and reproduction of various microorganisms in the intestines, including yeasts.
How to avoid the recurrence of yeast fungi in a child after treatment?
After successfully treating a yeast infection in a child’s intestines, it is important to take steps to prevent re-infection of the infection. The following tips will help you avoid this problem:
- Take care of your child’s hygiene. Remember that personal hygiene is an important aspect in the prevention of yeast infections. Wash your child’s hands regularly, especially before eating, after going to the toilet, or after contact with animals. Instill good cleanliness habits from your example.

- Pay attention to baby food. Foods rich in sugar and yeast may cause the recurrence of fungi in the child’s body. Therefore, it is recommended to reduce the amount of sweets and bakery products in the child’s diet or eliminate them altogether. Include more fresh fruits and vegetables, as well as fiber-rich foods in your diet.
- Prevent your child. Certain probiotics, vitamins and minerals may help support gut health and prevent yeast infections. Talk to your pediatrician about taking these supplements.
If you notice a recurrence of symptoms of a yeast infection in your child, contact your pediatrician. He will prescribe the necessary therapeutic measures and help prevent re-infection of fungi in the future.
Health effects of yeast in baby stool
Benefits of yeast in baby stool
Some studies suggest that yeast in baby stool may have health benefits. In particular, they may reduce the risk of allergic reactions and problems with the immune system.
Also, yeast fungi are excellent producers of B vitamins, which are necessary for the normal development and functioning of the nervous system.
Negative effects of yeast fungi in the child’s feces
However, the presence of a large amount of yeast fungi in the feces may indicate a violation of the intestinal microbiocenosis. This can lead to a number of problems such as dysbiosis and digestive disorders.
In addition, yeasts can cause inflammation in the intestines, which can lead to diseases such as colitis or stomach ulcers.
How to deal with yeast in a child’s stool
If yeast is found in a child’s stool, a pediatrician should be consulted. Depending on the specific situation, the doctor may recommend additional studies and prescribe a specific course of treatment. Usually, antifungal drugs are prescribed to fight yeast, and it is also recommended to monitor the child’s nutrition and strengthen the immune system.
Possible complications from yeast fungi in the stool in a child
If a yeast infection is found in a child’s stool, treatment should be started immediately, as an unconditional delay can lead to serious complications.
One of the most common complications from yeast fungi is diarrhea. In the process of growth and reproduction, fungi release toxins that cause indigestion.
Another possible complication is malnutrition, which is due to the fact that yeast fungi suck out valuable substances from the child, which are necessary for proper development. Therefore, even if the child eats enough, he may experience signs of starvation.
In addition, yeast fungi can lead to an allergic reaction, which manifests itself in the form of skin itching, redness and swelling.
If you find yeast in your child’s stool, don’t put off seeing your doctor. The doctor will help determine the cause of the appearance of fungi and choose the right treatment that will help prevent possible complications and restore the baby to health.
How to treat yeast fungus in a child and what precautions are needed?
At the first sign of a yeast infection, you should contact your pediatrician. Antifungal drugs and dietary changes are used to treat effectively.
Antifungal drugs and dietary changes are used to treat effectively.
It is important to monitor the child’s hygiene to prevent reinfection. Change diapers and underwear regularly, provide your child with a personal towel and toys. Do not use scented soaps and bath gels as they can irritate the skin and worsen the situation.
Precautions also include maintaining the child’s immune system. Regularly monitor your child’s diet, provide him with all the necessary vitamins. Try not to overload the child, give him the opportunity to get enough sleep and be in the fresh air.
Avoid the use of harsh soap solutions and mashed powders. Use mild gel detergents instead. It is also necessary to sterilize toys that are in contact with the child.
If you suspect that your child has yeast, you should follow the doctor’s recommendations and take all precautions to prevent re-infection.
Q&A:
What are yeast fungi?
Yeast fungi are microorganisms that are part of the natural microflora of our body. They help digest food and absorb nutrients. However, with an increase in their number in the intestine, dysbacteriosis may occur, which will lead to undesirable health consequences.
They help digest food and absorb nutrients. However, with an increase in their number in the intestine, dysbacteriosis may occur, which will lead to undesirable health consequences.
How do yeasts get into a baby’s stool?
Yeast fungi can get into the feces of a child due to intestinal dysbacteriosis. The causes of dysbacteriosis can be different: unbalanced diet, antibiotics, intestinal microflora disorders after diseases, stress, etc.
What symptoms indicate the presence of yeast fungi in the child’s feces?
Symptoms of yeast in a child’s stool can include diarrhea, constipation, bloating, heartburn, bad breath, loss of appetite, etc.
What are the consequences of having yeast in a child’s stool?
The presence of yeast in a child’s stool can lead to various consequences: poor absorption of nutrients, poor immune system health, increased development of allergic reactions, and the development of antibiotic resistance in bacteria in the body.
How is yeast in a child’s stool diagnosed?
Diagnosis of yeast fungi in the feces of a child is carried out using the analysis of feces for microflora. To do this, you need to collect feces in a special container and deliver it to the laboratory for analysis.
What are the treatments for yeast in a child’s stool?
Treatment of yeast in a child’s stool may include taking probiotics, preparations that contain beneficial bacteria to restore the intestinal microflora. A special diet may also be prescribed, excluding foods that contribute to the development of a fungal infection. In case of complications, antifungal drugs may be required.
How to prevent the development of yeast fungi in the stool of a child?
Prevention of the development of yeast fungi in the feces of a child consists in proper nutrition, stress management, regular intake of probiotics and prevention of undesirable consequences when taking antibiotics.
How long can a yeast infection in a child’s stool last?
The duration of treatment for yeast in the child’s stool depends on the degree of infection and complications. On average, treatment can last several weeks to a month. However, if the infection recurs, long-term treatment may be required.
On average, treatment can last several weeks to a month. However, if the infection recurs, long-term treatment may be required.
Yeast infections: diseases, treatment and preparations
Where can I buy?
Encyclopedia
Fungus
Skin and/or mucous membrane lesions caused by yeast fungi are called yeast infections.
Author of article
Moshkova Elena Mikhailovna
Dermatovenereologist, head of the KDO for the provision of paid services, St. Petersburg State Budgetary Institution of Health “City Dermatovenerologic Dispensary”, St. Petersburg.
What yeast-like fungi cause disease in humans
Both bacteria and fungal microorganisms normally live on human skin. In small quantities, they are part of the normal microflora of the skin. Yeasts and yeast-like fungi can also live on the skin without causing any skin disease. However, if adverse factors occur (decreased immunity, impaired microflora), fungi begin to actively multiply, their number increases and leads to the development of the disease.
However, if adverse factors occur (decreased immunity, impaired microflora), fungi begin to actively multiply, their number increases and leads to the development of the disease.
How is skin fungus treated? Watch in a two-minute video with Doctor of Medical Sciences, Professor of the Russian Academy of Sciences Olga Borisovna Tamrazova
Fungi of the genus Malassezia
Yeast-like fungi of the genus Malassezia – the cause of skin dermatosis: seborrheic dermatitis and versicolor (pityriasis) lichen 90 090 . Approximately 20% of people experience occasional cases of seborrheic dermatitis. And 10% of the population suffers from versicolor (pityriasis) versicolor 3 .
Fungi of the genus Candida
Yeast fungi of the genus Candida – causative agents of candidiasis of the skin, mucous membranes and internal organs. Fungi of the genus Candida are conditionally pathogenic microorganisms, for the existence of which the presence of oxygen in the environment is an optional condition. This explains the possibility of candidiasis of internal organs.
This explains the possibility of candidiasis of internal organs.
Up to 30-50% of the population carry Candida on their skin. This type of fungus can colonize the mucous membrane of the mouth, intestines, and the genitourinary system.
How fungi of the genus Candida affect human health
Cause itching and dry skin
Provoke the appearance of a white coating on the tongue and bad breath
Contribute to vaginal candidiasis
Affect the feet
900 02 Of the 150 existing species of Candida, 20 species are the causative agents of candidiasis . Most often, Candida albicans, C.tropicalis, C.parapsilosis, C.glabrata 1 are found in patients.
Skin may show C. albicans, C. parapsilosis, C. guillermondii, C. kefyr 1 . However, skin candidiasis usually develops due to the presence of Candida albicans , other types of Candida cause skin lesions much less 1 .
The cause of candidiasis of the genitourinary system in almost 90% of people is C. albicans, in 10% – C. krusei, C. glabrata and others 1 .
albicans, in 10% – C. krusei, C. glabrata and others 1 .
Locations of yeast infections. Symptoms
Seborrheic dermatitis
Seborrheic dermatitis most often occurs on the face and scalp. But the process can be widespread and localized in other seborrheic areas of the body (skin of the back, chest). Rashes are represented by pink spots with peeling on the surface. Sometimes the inflammation is so severe that itching and excessive moisture of the skin (weeping) appear. Often the only manifestation of seborrheic dermatitis is dandruff.
Pityriasis versicolor (pityriasis)
With versicolor versicolor, there is no skin inflammation, so patients are only concerned about the aesthetic component of dermatosis. Spots up to 1 cm usually appear on parts of the body with excessive sweating. The color of the rashes can vary from beige to pink, over time the spots merge into large foci.
Candidiasis of the skin and oral mucosa
Candidiasis of the skin often occurs in the interdigital, axillary, inguinal folds, on the skin under the mammary glands, the fold of the abdomen.
Candidiasis of large folds
Candidiasis of large folds doctors also call Candida intertrigo 2 . At the bottom of the fold, small bubbles appear, which open up, exposing bright pink with a bluish tinge of skin erosion. Over time, defects in the upper layer of the skin increase in size, merge and can completely spread to the entire surface of a large fold. The erosive surface is wet with a lacquer sheen. A whitish coating may be present. On the periphery of candidal foci, screenings can be found – islands of skin with small vesicles, pustules or small erosions.
Candidiasis of the interdigital folds of the hands often occurs in housewives, catering workers. The predisposing factor is constant contact with water. Often only one interdigital fold on the “working” hand is affected. There is redness, itching, there may be cracks.
Smooth skin candidiasis
Smooth skin candidiasis is more often a complication of an underlying dermatological disease, such as atopic dermatitis or due to the spread of a fungal infection from the skin of large folds.
Candidiasis of the nail folds and nails
Redness, swelling, pain appear at the site of the fungus penetration into the skin of the periungual fold. When pressing on the periungual roller, there are no purulent compartments, in contrast to inflammation of a bacterial nature. And brownish transverse grooves appear on the nail plate, the nail thickens, loses its luster.
Urogenital candidiasis
This disease does not apply to infections that are sexually transmitted 2 .
In men, candidal balanitis, balanoposthitis and urethritis are more common.
Men report the following symptoms: 3
- Redness, whitish coating, swelling, itching, burning in the area of the glans penis
- Painful urination and sexual intercourse
See how thrush is treated in a short video by professor, doctor of medical sciences, Evgenia Valerievna Shikh
Vulvovaginal candidiasis (thrush) occurs in women – Candida fungi damage the mucous membrane of the external genitalia and vagina.
More than 70% of women have had an episode of urogenital candidiasis at least once in their lives. And 15% of them had repeated episodes of this disease 3 .
Women note: 3
- White cheesy discharge from the genital tract
- Itching, burning
- Painful urination and intercourse
Predisposing factors for yeast infections
Predisposing factors for yeast infections: 3
- Long-term antibiotic therapy
- Taking anticancer drugs (cytostatics)
- Uncompensated diabetes mellitus
- Immunodeficiency
- Hormonal disorders
Predisposing factors for skin candidiasis include: prolonged contact with water, skin abrasions, excess weight. For the development of oral candidiasis – traumatization of the mucous membrane, for example, when wearing dentures, braces.
Diagnosis of yeast infections
Diagnosis of skin candidiasis is based on the clinical picture of the disease. The doctor may additionally prescribe a skin scraping test for the presence of Candida fungi.
The doctor may additionally prescribe a skin scraping test for the presence of Candida fungi.
In the diagnosis of urogenital candidiasis, microscopic and cultural methods with the determination of the type of fungus of the genus Candida and its sensitivity to antifungal drugs are of great importance 3 . And with the help of special test systems, you can detect DNA fragments of the causative agent of urogenital candidiasis.
Diagnosis of diseases caused by fungi of the genus Malassezia is based on examination of skin manifestations, dermatoscopy, examination of skin scrapings for fungi, determination of the Besnier phenomenon (peeling of the rash when scraped with a fingernail or spatula) and Balzer’s test (5% alcohol solution of iodine is applied to the affected area with Entrapment of healthy skin.Increased staining of the rash compared to areas of healthy skin indicates the presence of fungi of the genus Malassezia).
Treatment of yeast infections
Treatment of candidiasis of the skin consists of:
1) Use of topical antifungals in the form of a cream/ointment, solution, spray
3) Elimination or correction of provoking factors
Treatment of urogenital candidiasis consists of:0003
2) Prescription of anti-allergic drugs
3) Vitamin therapy
(In some cases, immunomodulatory drugs are recommended)
, creams, ointments) and for oral administration (tablets, capsules). Most often, it is possible to solve the problem with external antifungal agents. However, with widespread rashes, severe persistent course, drugs are prescribed for oral administration
Most often, it is possible to solve the problem with external antifungal agents. However, with widespread rashes, severe persistent course, drugs are prescribed for oral administration
The use of antiseptic or antibacterial drugs when connecting a bacterial infection to the weeping areas of the skin
of the use of combined drugs containing anti -inflammatory hormone, antibiotic and antifungal components, if skin soreness occurs
for candidiasis of the skin, seborrheic dermatitis, multi -colored) external antifungal medicines: sertaconazole, clotrimazole, ketoconazole, terbinafine. For example, appointment Zalain ® cream 2% (sertaconazole) promotes recovery better than other drugs (versus clotrimazole) 5 .
Sertaconazole-based cream (Zalain®) for yeast infections
Sertaconazole-based products (Zalain ® ) are available in the form of suppositories and cream.
With local use of Zalain ® cream for two weeks, the components of the drug are not detected in the blood and urine, which indicates a high safety profile of the drug 7 .
Sertaconazole has a triple action: it prevents the growth and reproduction of fungi, promotes their death, and also prevents the transition of fungi from a passive form to a pathogenic one (only for fungi of the genus Candida) 15 .
Instruction
Zalain ® Yeast Infection Cream
How to use Zalain Cream ®
For skin candidiasis, seborrheic dermatitis, pityriasis versicolor Zalain ® cream is applied 2 times a day in a thin layer covering healthy skin for 2-4 weeks 6 .
Topical and systemic antifungal therapy may be indicated for the treatment of urogenital candidiasis.
Urogenital candidiasis in men can be treated externally:
- Zalain ® cream is applied 2 times a day in a thin layer for 14 days 6 .

Has a triple effect: antifungal, antipruritic, anti-inflammatory
Used 1-2 times a day
Where to buy Zalain ® Cream for the treatment of yeast infections
or
Find the nearest pharmacy
Zalain ® Suppositories
Sertaconazole-based cream (Zalain ® ) for the treatment of fungal infections al tablets or suppositories (suppositories).
Doctors also recommend vaginal suppositories based on sertaconazole (Zalain ® ). One suppository is inserted into the vagina 1 time. The use of 1 vaginal suppository is explained by the fact that sertaconazole has a high lipophilicity – it dissolves well in lipid (fat) cell structures. Due to this, the drug remains in the vaginal mucosa for a long time (7 days) at a therapeutic concentration, having a triple mechanism of action on Candida fungi. For women, this prescription of the drug is very convenient.
For women, this prescription of the drug is very convenient.
Unlike other drugs for the treatment of urogenital candidiasis, the effect of Zalain ® suppositories is observed with a single application of 7 . If necessary (maintenance of clinical symptoms), treatment can be repeated after 1 week 7 . The doctor may recommend Zalain ® suppositories to pregnant women if necessary.
The use of specially adapted intimate hygiene gels helps maintain a healthy microflora of the vulva and resist infections.
Only 1 suppository per course
Local effect of the drug
Absorption of sertaconazole into the bloodstream does not occur 13
Can be used during pregnancy and lactation*
Where to buy Zalain ® Candles
Instruction
Why is 1 candle valid for 7 days?
Zalagel ® Intim
Antiseptic properties of components Zalagel ® Intim
Zalagel ® Intim gel-soap, gently cleanses the skin of the intimate area, has a calming effect ohm and helps to reduce the feeling of discomfort.
U Zalagel ® Intim Slightly alkaline pH (8-9), creating a destructive environment for fungi of the genus Candida (causative agents of thrush). The betaine component, which is part of the gel, prevents dryness of the intimate area, maintains the physiological balance of the skin and mucous membranes.
Gently cleanses the intimate area
Creates a destructive environment for fungi of the Candida genus
Protects the female genital organs from infections
Tea tree oil in the composition of the product has an antibacterial and antiviral effect
Reduces itching and irritation 9000 3
Where to buy Zalagel ® Intimacy
or
Find the nearest pharmacy
Instruction
Answers to questions
How to understand that thrush has become chronic?
Answer: Four or more episodes of thrush per year are in favor of chronic recurrent urogenital candidiasis.
How long does versicolor treatment take?
Answer: The treatment of multicolored lichen, as a rule, consists in the appointment of external antifungal therapy. The duration of treatment is selected individually and usually lasts at least 2 weeks.
Is it possible to wet the skin with candidiasis of the folds?
Answer: In the acute period of the disease, until the skin process stabilizes, it is necessary to limit contact with water.
Popular articles
More articles
Candles for thrush
What are the candles for thrush, how do they differ, and how to choose the most effective.
Antifungal ointment/cream
What are antifungal ointments, how do they differ when applied.
Antifungal drugs, agents, antimycotics
Antifungal agents: classification and types of dosage forms. Ways to use antimycotics.
Sources
- Russian clinical guidelines.
- Textbook “Skin and venereal diseases” edited by O.L. Ivanov., 2010.
- National Guide to Dermatovenereology edited by prof. Yu.S. Butova, acad. RAMS Yu. K. Skripkina, prof. O.L. Ivanov.
- Clinical guidelines of the Russian Federation, Urogenital candidiasis 2019
- Efficacy and safety study of Zalain® 2% cream in the treatment of skin mycoses. IG Sergeeva, Yu. M. Krinitsyna Novosibirsk State University.
- Register of Medicines of Russia, official instructions for the active substance Sertaconazole.
- Register of Medicines of Russia, official instructions for Zalain® 2% cream.

- Register of medicines of Russia, official instruction Zalain 300 mg, vaginal suppositories.
- RMJ No. 9, 2015. “Vulvovaginal candidiasis. The use of Zalain in clinical practice. E. S. Vanke, N. S. Vanke.
- Mondello F, De Bernardis F, Girolamo A, Cassone A, Salvatore G. In vivo activity of terpinen-4-ol, the main bioactive component of Melaleuca alternifolia Cheel (tea tree) oil against azole-susceptible and -resistant human pathogenic Candida sp. BMC Infect Dis. 2006;6:158.
- Hammer KA, Carson CF, Riley TV. In vitro susceptibilities of lactobacilli and organisms associated with bacterial vaginosis to Melaleuca alternifolia (tea tree) oil. Antimicrob Agents Chemother 1999;43:196.
- Pena EF. Melaleuca alternifolia oil. Its use for trichomonal vaginitis and other vaginal infections. Obstet Gynecol 1962;19:793-5.
- Astani A, Reichling J, Schnitzler P. Comparative study on the antiviral activity of selected monoterpenes derived from essential oils.




 13 How can I prevent yeast infection in my child?
13 How can I prevent yeast infection in my child? 19.0.6 What are the treatments for yeast in a child’s stool?
19.0.6 What are the treatments for yeast in a child’s stool?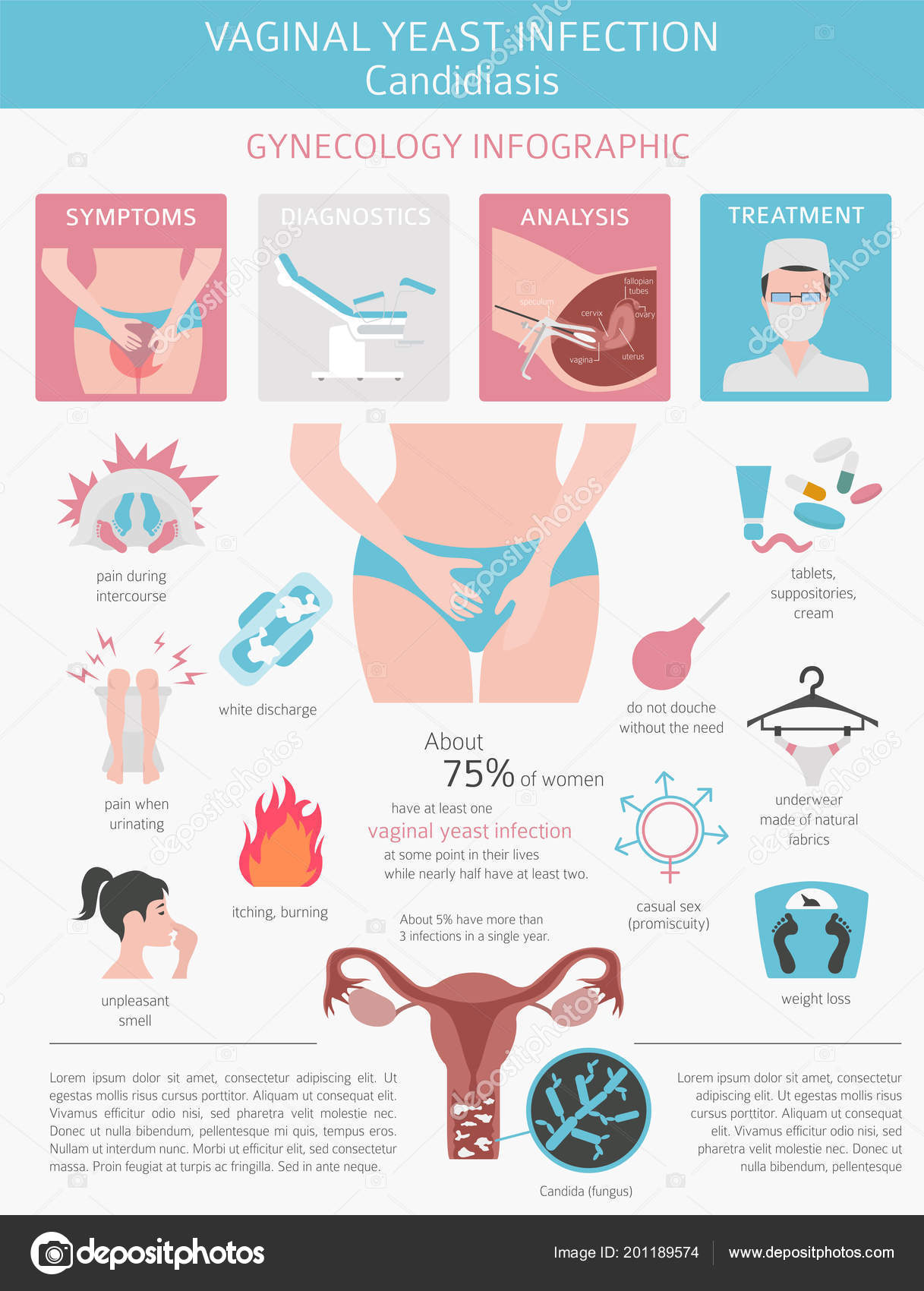

 An experienced doctor will be able to timely identify the manifestations of yeast in the intestines of the child and take the necessary therapeutic measures.
An experienced doctor will be able to timely identify the manifestations of yeast in the intestines of the child and take the necessary therapeutic measures.