What is atenolol side effects. Atenolol: Uses, Side Effects, and Important Information
What are the main uses of atenolol. How does atenolol work to lower blood pressure. What are the most common side effects of taking atenolol. When should you contact your doctor while taking atenolol. How should atenolol be taken properly.
Understanding Atenolol: A Comprehensive Overview
Atenolol, also known by its brand name Tenormin®, is a widely prescribed medication belonging to the beta-blocker class of drugs. It plays a crucial role in managing various cardiovascular conditions, primarily hypertension (high blood pressure). To fully grasp the importance and impact of this medication, it’s essential to delve into its mechanisms, uses, and potential side effects.
What is Atenolol and How Does it Work?
Atenolol is an antihypertensive medication that functions by reducing the workload on the heart and promoting more regular heartbeats. Its primary mechanism of action involves blocking the effects of epinephrine, also known as adrenaline, on the heart and blood vessels. This results in several beneficial effects:

- Slowing down the heart rate
- Reducing the force of heart contractions
- Decreasing blood pressure
- Improving blood flow through the blood vessels
By achieving these effects, atenolol helps manage high blood pressure and alleviates symptoms associated with certain heart conditions.
Available Forms and Dosages
Atenolol is typically available in tablet form, with common dosages including:
- 25 mg tablets
- 50 mg tablets
- 100 mg tablets
In some cases, pharmacies may prepare an oral liquid suspension of atenolol for patients who have difficulty swallowing tablets. The appropriate dosage is determined by a healthcare professional based on individual patient needs and medical conditions.
Primary Uses of Atenolol in Medical Treatment
Atenolol is prescribed for various cardiovascular conditions, with its primary uses including:
Hypertension Management
As a beta-blocker, atenolol is highly effective in lowering blood pressure. High blood pressure, if left untreated, can lead to serious complications such as kidney damage, stroke, or heart failure. Atenolol helps mitigate these risks by maintaining blood pressure within a healthy range.

Angina Pectoris Relief
Atenolol is also used to alleviate certain types of chest pain, known as angina pectoris. By reducing the heart’s workload and oxygen demand, it can help prevent or reduce the frequency and severity of angina attacks.
Migraine Prevention
Some patients find atenolol effective in preventing migraine headaches. While the exact mechanism for this is not fully understood, it’s believed that the drug’s effects on blood vessels and stress hormones contribute to its migraine-preventive properties.
Arrhythmia Management
In certain cases, atenolol may be prescribed to help manage irregular heartbeats or arrhythmias. Its ability to slow and regulate heart rate can be beneficial in treating some types of heart rhythm disorders.
Common Side Effects of Atenolol
While atenolol is generally well-tolerated, it can cause various side effects. It’s important for patients to be aware of these potential effects and report any concerns to their healthcare provider.
Cardiovascular Side Effects
Some of the most common cardiovascular side effects include:
- Dizziness or lightheadedness
- Low blood pressure
- Slow heart rate (bradycardia)
- Swelling in the legs or ankles
- Irregular heartbeat or palpitations
Respiratory Effects
Atenolol can sometimes affect the respiratory system, leading to:
- Difficulty breathing
- Wheezing
These effects are more likely to occur in patients with pre-existing respiratory conditions such as asthma or chronic obstructive pulmonary disease (COPD).
Neurological and Psychological Effects
Some patients may experience neurological or psychological side effects, including:
- Headaches
- Unusual weakness or fatigue
- Anxiety
- Depression
- Nightmares or sleep disturbances
Gastrointestinal Effects
Atenolol can sometimes cause gastrointestinal discomfort, such as:
- Nausea
- Vomiting
- Diarrhea
Other Potential Side Effects
Additional side effects that some patients may experience include:
- Cold, tingling, or numb hands or feet
- Dry, itching skin
- Dry or burning eyes
- Sexual difficulties or impotence
While these side effects are generally mild and often improve as the body adjusts to the medication, it’s crucial to report any persistent or severe symptoms to a healthcare provider.

Important Precautions and Warnings for Atenolol Use
To ensure safe and effective use of atenolol, patients should be aware of several important precautions and warnings:
Gradual Discontinuation
Sudden discontinuation of atenolol can lead to serious heart-related problems. Patients should never stop taking atenolol abruptly without consulting their doctor. A gradual reduction in dosage is typically recommended when discontinuing the medication.
Regular Monitoring
Patients taking atenolol should have their blood pressure and heart rate monitored regularly. Healthcare providers will often provide specific guidelines on when to seek medical attention based on blood pressure or heart rate readings.
Interaction with Other Medications
Atenolol can interact with various other medications, including:
- Other blood pressure medications
- Cold and cough medicines
- Medications for breathing problems
- Diuretics
- Alcohol
It’s crucial to inform healthcare providers about all medications, supplements, and herbal products being taken to avoid potential interactions.

Effects on Blood Sugar Levels
Atenolol can affect blood sugar levels, which is particularly important for patients with diabetes. Regular blood sugar monitoring may be necessary while taking this medication.
Pregnancy and Breastfeeding
Women who are pregnant, planning to become pregnant, or breastfeeding should discuss the risks and benefits of atenolol use with their healthcare provider. The medication can potentially affect fetal development and may be present in breast milk.
Proper Administration and Storage of Atenolol
To maximize the effectiveness of atenolol and minimize potential side effects, proper administration and storage are essential:
Dosing Schedule
Atenolol is typically taken once daily, with or without food. It’s important to take the medication at the same time each day to maintain consistent blood levels.
Missed Doses
If a dose is missed, it should be taken as soon as remembered. However, if it’s almost time for the next scheduled dose, the missed dose should be skipped. Doubling up on doses can lead to adverse effects.

Storage Guidelines
Atenolol tablets should be stored at room temperature, away from moisture and direct light. If using a liquid suspension, it should be refrigerated and discarded after the expiration date on the label.
Shaking Liquid Suspensions
If using an oral liquid suspension of atenolol, it’s important to shake the bottle well before each use to ensure proper distribution of the medication.
Recognizing and Responding to Serious Side Effects
While most side effects of atenolol are mild, some can be serious and require immediate medical attention. Patients should be aware of the following symptoms that warrant contacting a healthcare provider:
- Severe dizziness or fainting spells
- Chest pain or severe heart palpitations
- Sudden weight gain
- Shortness of breath or wheezing
- Swelling of the hands, feet, ankles, or lower legs
- Unusual bleeding or bruising
- Fever, chills, or persistent sore throat
- Severe skin reactions or rash
In case of severe side effects or reactions, immediate medical attention should be sought. For patients receiving care at St. Jude Children’s Research Hospital, specific contact numbers are provided for reporting severe side effects.
![]()
Lifestyle Considerations While Taking Atenolol
Patients taking atenolol should be aware of certain lifestyle considerations to ensure safe and effective use of the medication:
Physical Activity and Dizziness
Atenolol can cause dizziness or lightheadedness, especially when first starting the medication. Patients should exercise caution when operating heavy machinery or driving until they know how the medication affects them. To avoid dizziness or fainting spells, it’s advisable to rise slowly from a sitting or lying position.
Alcohol Consumption
Alcohol can enhance the blood pressure-lowering effects of atenolol and increase the risk of side effects. Patients should consult their healthcare provider about safe alcohol consumption while taking this medication.
Sun Protection
Some patients may experience increased sensitivity to sunlight while taking atenolol. Using appropriate sun protection, such as sunscreen and protective clothing, is advisable.
Diet and Hydration
Maintaining a balanced diet and proper hydration is important while taking atenolol. Sudden changes in diet, especially those that affect sodium intake, can impact blood pressure and the effectiveness of the medication.

Exercise and Physical Exertion
Atenolol can affect the body’s response to physical exertion. Patients should discuss appropriate exercise regimens with their healthcare provider and be aware of potential changes in their exercise tolerance.
Understanding these various aspects of atenolol use can help patients maximize the benefits of the medication while minimizing potential risks. As with any medication, open communication with healthcare providers is crucial for safe and effective treatment.
St. Jude Children’s Research Hospital
What is atenolol?
Atenolol (also called Tenormin®) is an antihypertensive (drug for lowering blood pressure) known as a beta-blocker. It reduces the workload of the heart and helps it to beat more regularly. It lowers blood pressure in many different ways. High blood pressure levels can damage kidneys, and may lead to a stroke or heart failure. It is also used to relieve some types of chest pain and to prevent migraine headaches. Atenolol is available as 25-mg, 50-mg, and 100-mg tablets, all of which are taken by mouth.
Possible side effects of atenolol
- Feeling dizzy, light-headed or having fainting spells
- Low blood pressure
- Slow heart rate
- Swelling of legs or ankles
- Irregular heartbeat, chest pain, palpitations
- Cold, tingling, or numb hands or feet
- Difficulty breathing, wheezing
- Unusual weakness or tiredness
- Headache
- Nausea, vomiting
- Diarrhea
- Anxiety
- Depression
- Nightmares
- Dry itching skin
- Dry or burning eyes
- Difficulty sleeping
- Sexual difficulties, impotence
These are the most common side effects, but there may be others. Please report all side effects to the doctor or nurse.
Please report all side effects to the doctor or nurse.
In case of a severe side effect or reaction, call 595-3300. If you are outside the Memphis area, dial toll-free 1-866-2STJUDE (1-866-278-5833), and press 0 once the call is connected.
Special instructions for atenolol
- This medicine may cause dizziness and lightheadedness. Do not operate heavy equipment or drive a motor vehicle until you see how this medicine will affect you. To avoid feeling dizzy or having fainting spells do not sit up or stand up too quickly.
- You or your nurse should check your blood pressure and heart rate regularly while you are taking atenolol. Your doctor will tell you what to do if your blood pressure level is low or high. Your dose of atenolol may change based on your blood pressure level. If your blood pressure is above _____________ or below__________ call your doctor right away. If your heart rate is _____________ call your doctor right away.
- Do not suddenly stop taking atenolol.
 This can lead to serious heart-related problems. Ask your doctor how you should gradually reduce the dose before you stop taking this medicine.
This can lead to serious heart-related problems. Ask your doctor how you should gradually reduce the dose before you stop taking this medicine. - If you experience any of the following symptoms or side effects, call your doctor right away:
- Difficulty breathing, wheezing
- Dizziness or fainting spells
- Irregular heartbeat
- Changes in vision
- Tremor, shakes
- Vomiting
- Slow heart rate
- Swollen legs or ankles
- Increased thirst
- Increase in the amount of urine passed
- Skin rash
- Cold, tingling, or numb hands or feet
- Confusion
- Atenolol may affect the way some medicines work. Some medicines may also affect the way atenolol works. These medicines include other blood pressure medicines, medicines for colds and coughs, medicines for breathing problems, diuretics, alcohol, and others. Always tell your doctor if you are taking any of these medicines, or if you start taking any new medicine while you are taking atenolol.

- If you experience a sudden onset of severe diarrhea or vomiting or if you sweat a lot, tell your doctor right away. This loss of body fluid may decrease your blood pressure.
- Atenolol may affect your blood sugar levels, especially if you have diabetes. Your blood sugar level should be checked while you are taking atenolol.
- If an oral liquid suspension of atenolol is made by the pharmacy, you should shake the suspension well before you take the medicine. The oral liquid should be refrigerated. Discard the medicine after the expiration date that is on the label.
This document is not intended to take the place of the care and attention of your personal physician or other professional medical services. Our aim is to promote active participation in your care and treatment by providing information and education. Questions about individual health concerns or specific treatment options should be discussed with your physician.
St. Jude complies with health care-related federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex.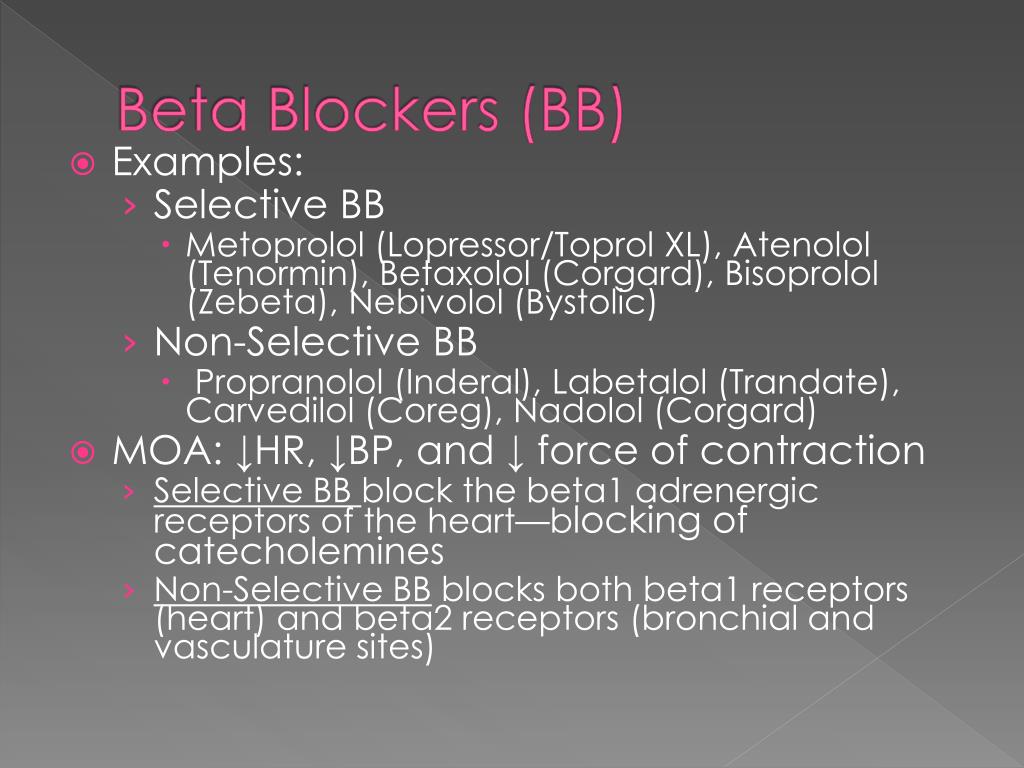
ATTENTION: If you speak another language, assistance services, free of charge, are available to you. Call 1-866-278-5833 (TTY: 1-901-595-1040).
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-866-278-5833 (TTY: 1-901-595-1040).
تنبيه: إذا كنت تتحدث باللغة العربية فيمكنك الاستعانة بخدمات المساعدة اللغوية المتوفرة لك مجانا. .يرجى الاتصال بالرقم. 5833-278-866-1 (الهاتف النصي: 1040-595-901-1).
CO Atenolol – Uses, Side Effects, Interactions
How does this medication work? What will it do for me?
Atenolol belongs to a class of medications called beta-blockers. It is used to lower high blood pressure and to prevent the symptoms of angina (chest pain). It works by reducing the demands put on the heart.
Atenolol is often used in combination with other high blood pressure medications such as diuretics (water pills) when the use of one medication by itself is not enough to control blood pressure.
This medication may be available under multiple brand names and/or in several different forms. Any specific brand name of this medication may not be available in all of the forms or approved for all of the conditions discussed here. As well, some forms of this medication may not be used for all of the conditions discussed here.
Your doctor may have suggested this medication for conditions other than those listed in these drug information articles. If you have not discussed this with your doctor or are not sure why you are taking this medication, speak to your doctor. Do not stop taking this medication without consulting your doctor.
Do not give this medication to anyone else, even if they have the same symptoms as you do. It can be harmful for people to take this medication if their doctor has not prescribed it.
What form(s) does this medication come in?
CO Atenolol is no longer being manufactured for sale in Canada. For brands that may still be available, search under atenolol. This article is being kept available for reference purposes only. If you are using this medication, speak with your doctor or pharmacist for information about your treatment options.
For brands that may still be available, search under atenolol. This article is being kept available for reference purposes only. If you are using this medication, speak with your doctor or pharmacist for information about your treatment options.
How should I use this medication?
The recommended adult dose of atenolol ranges from 50 mg to 200 mg daily depending on circumstances.
To treat high blood pressure, the usual adult starting dose is 50 mg taken by mouth, once a day. The full effect of the medication is usually reached within 1 to 2 weeks. If blood pressure is not low enough after this time, your doctor may increase the dose of the medication to 100 mg once daily or add another blood pressure-lowering medication.
The usual starting dose to treat angina pain is 50 mg taken once a day. If, after 1 to 2 weeks symptoms are not reduced enough, your doctor may increase the dose to 100 mg once daily or 50 mg taken twice a day. The maximum dose for treating angina is 200 mg daily.
The maximum dose for treating angina is 200 mg daily.
If you have reduced kidney function you may need much lower doses.
Many things can affect the dose of medication that a person needs, such as body weight, other medical conditions, and other medications. If your doctor has recommended a dose different from the ones listed here, do not change the way that you are taking the medication without consulting your doctor.
It is important to take this medication exactly as prescribed by your doctor. If you miss a dose, take it as soon as possible and continue with your regular schedule. If it is almost time for your next dose, skip the missed dose and continue with your regular dosing schedule. Do not take a double dose to make up for a missed one. If you are not sure what to do after missing a dose, contact your doctor or pharmacist for advice.
Store this medication at room temperature, protect it from light and moisture, and keep it out of the reach of children.
Do not dispose of medications in wastewater (e.g. down the sink or in the toilet) or in household garbage. Ask your pharmacist how to dispose of medications that are no longer needed or have expired.
Who should NOT take this medication?
Do not take this medication if you:
- are allergic to atenolol or any ingredients of the medication
- are scheduled to have anesthesia with an agent that causes myocardial depression (e.g., ether)
- have a condition known as pheochromocytoma (in the absence of alpha-blockade)
- have a condition known as right ventricular failure caused by pulmonary hypertension
- have a condition known as “sick sinus syndrome”
- have a very slow heart rate caused by heart rhythm problems
- have congestive heart failure
- have metabolic acidosis
- have cardiogenic shock
- have serious heart block (second- or third-degree AV block)
- have severe peripheral arterial disorders (blockage of blood flow to limbs of body)
- have very low blood pressure
What side effects are possible with this medication?
Many medications can cause side effects. A side effect is an unwanted response to a medication when it is taken in normal doses. Side effects can be mild or severe, temporary or permanent.
A side effect is an unwanted response to a medication when it is taken in normal doses. Side effects can be mild or severe, temporary or permanent.
The side effects listed below are not experienced by everyone who takes this medication. If you are concerned about side effects, discuss the risks and benefits of this medication with your doctor.
The following side effects have been reported by at least 1% of people taking this medication. Many of these side effects can be managed, and some may go away on their own over time.
Contact your doctor if you experience these side effects and they are severe or bothersome. Your pharmacist may be able to advise you on managing side effects.
- back or joint pain
- cough
- diarrhea
- dizziness or lightheadedness
- dry mouth
- headache
- nausea
- slow heart rate
- spinning sensation
- trouble sleeping
- unusual tiredness or weakness
Although most of the side effects listed below don’t happen very often, they could lead to serious problems if you do not seek medical attention.
Check with your doctor as soon as possible if any of the following side effects occur:
- breathing difficulty or wheezing
- cold hands and feet
- confusion (especially for seniors) or memory problems
- dizziness or lightheadedness when getting up from a lying or sitting position
- fainting
- irregular heartbeat or palpitations
- skin rash
- vision problems
- worsening heart failure (e.g., swelling of ankles, feet, or lower legs; difficulty breathing)
Stop taking the medication and seek immediate medical attention if any of the following occur:
- chest pain
- severe shortness of breath
- severely slow heartbeat (especially less than 50 beats per minute)
- symptoms of a serious allergic reaction (such as swelling of the face or throat, hives, or difficulty breathing)
Some people may experience side effects other than those listed. Check with your doctor if you notice any symptom that worries you while you are taking this medication.
Check with your doctor if you notice any symptom that worries you while you are taking this medication.
Are there any other precautions or warnings for this medication?
Before you begin using a medication, be sure to inform your doctor of any medical conditions or allergies you may have, any medications you are taking, whether you are pregnant or breast-feeding, and any other significant facts about your health. These factors may affect how you should use this medication.
Breathing conditions: In general, people who have asthma and certain other breathing problems or chronic lung disease should avoid taking a beta-blocker such as atenolol, as it can cause breathing difficulty. Low doses of atenolol may be taken with caution by people with asthma who do not respond to or cannot tolerate alternative treatment. If you have breathing problems, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Drowsiness/reduced alertness: The use of atenolol is unlikely to impair your ability to drive or operate machinery. However, it should be taken into account that dizziness, fatigue, or a slower reaction time may occur.
History of heart failure: Beta-blockers, such as atenolol, can worsen existing heart failure. It is important to take atenolol exactly as prescribed by your doctor to decrease the chance of this happening. If you have a history of heart disease, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Hyperthyroidism: If you have hyperthyroidism (high levels of thyroid hormones) you should use caution while taking atenolol, as it may reduce the symptoms of this condition, giving a false impression of improvement. Stopping the medication suddenly could worsen this condition.
Kidney disease: The kidneys are partially responsible for removing this medication from your body. Kidney disease or reduced kidney function may cause this medication to build up in the body, causing side effects. If you have reduced kidney function or kidney disease, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Low blood sugar: The signs of low blood sugar may not be as noticeable when taking atenolol. If you have diabetes and take insulin or other medications that affect insulin levels in the blood, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed. Your doctor will monitor you while you are taking this medication and may need to adjust the doses of diabetes medications.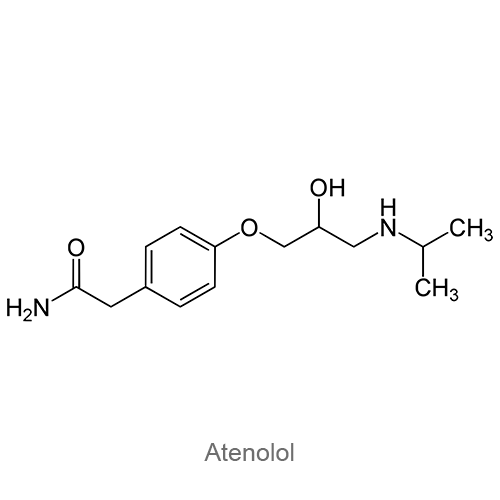
Prinzmetal’s angina: Atenolol may increase the number and duration of angina attacks for patients with Prinzmetal’s angina. If you have this condition, be cautious while taking atenolol. Report unusual chest pain to your doctor as soon as possible.
Severe allergies: If you have allergies severe enough to cause anaphylaxis (a severe allergic reaction where swelling of the face, lips, and throat make it difficult to breathe), you should talk to your doctor about what to do if you have an allergic reaction. Atenolol may make it more difficult to treat your allergic reaction with epinephrine.
Slow heart rate: In general, people with an abnormally slow pulse should not take a beta-blocker such as atenolol.
Stopping usage: Atenolol should not be stopped suddenly. There have been reports of severe worsening of angina and of heart attack or abnormal heart rhythms occurring when people with angina pectoris have done this. If this medication needs to be stopped, it should be done gradually under supervision of your doctor.
If this medication needs to be stopped, it should be done gradually under supervision of your doctor.
Surgery: If you are scheduled for surgery, inform all doctors involved in your care that you are taking atenolol.
Pregnancy: Studies have shown that atenolol does cross the placenta and there have been reports of harm to the developing baby if atenolol is taken by the mother during pregnancy. This medication should not be used during pregnancy unless the benefits outweigh the risks. If you become pregnant while taking this medication, contact your doctor immediately.
Breast-feeding: This medication passes into breast milk. If you are breast-feeding and are taking atenolol, it may affect your baby. Talk to your doctor about whether you should continue breast-feeding.
Children: The safety and effectiveness of using this medication have not been established for children.
What other drugs could interact with this medication?
There may be an interaction between atenolol and any of the following:
- aldesleukin
- aliskiren
- alpha-agonists (e.
 g., clonidine, methyldopa)
g., clonidine, methyldopa) - alpha-blockers (e.g., alfuzosin, doxazosin, tamsulosin)
- amiodarone
- amphetamines (e.g., dextroamphetamine, lisdexamfetamine)
- ampicillin
- anesthetic agents
- angiotensin converting enzyme inhibitors (ACEIs; captopril, ramipril)
- angiotensin receptor blockers (ARBs; e.g., candesartan, irbesartan, losartan)
- antipsychotics (e.g., clozapine, olanzapine, quetiapine, risperidone)
- apomorphine
- barbiturates (e.g., butalbital, pentobarbital, phenobarbital)
- beta-2 agonists (e.g., salbutamol, formoterol, terbutaline)
- beta-adrenergic blockers (e.g., metoprolol, propranolol, sotalol)
- brimonidine
- bromocriptine
- bupivacaine
- calcium channel blockers (e.g., amlodipine, diltiazem, nifedipine, verapamil)
- ceritinib
- clomipramine
- dexmethylphenidate
- diabetes medications (e.g., acarbose, canagliflozin, exenatide, glyburide, insulin, lixisenatide, metformin, rosiglitazone, sitagliptin)
- digoxin
- dipyridamole
- disopyramide
- diuretics (water pills; e.
 g., furosemide, hydrochlorothiazide, triamterene)
g., furosemide, hydrochlorothiazide, triamterene) - donepezil
- dronedarone
- duloxetine
- epinephrine
- ergot alkaloids (e.g., dihydroergotamine, ergonovine, ergotamine, methylergonovine)
- fentanyl
- fingolimod
- flecainide
- galantamine
- glycopyrrolate
- grass pollen allergen extract
- guanfacine
- ivabradine
- lacosamide
- lanreotide
- levodopa
- lidocaine
- mefloquine
- methylphenidate
- mexiletine
- minoxidil
- nabilone
- nitrates (e.g., nitroglycerin, isosorbide dinitrate, isosorbide mononitrate)
- nonsteroidal anti-inflammatory drugs (NSAIDs; e.g., ibuprofen, diclofenac, ketorolac)
- obinutuzumab
- octreotide
- ozanimod
- pasireotide
- pentoxifylline
- phosphodiesterase-5 inhibitors (e.g., sildenafil, tadalafil, vardenafil)
- pilocarpine
- procainamide
- propafenone
- quinidine
- quinine
- rasagiline
- reserpine
- riociguat
- rivastigmine
- ropinirole
- rotigotine
- sacubitril
- selegiline
- siponimod
- sulfonylureas (e.
 g., gliclazide, glyburide, tolbutamide)
g., gliclazide, glyburide, tolbutamide) - theophyllines (e.g., aminophylline, oxtriphylline, theophylline)
- tizanidine
- tofacitinib
- tranylcypromine
- yohimbine
If you are taking any of these medications, speak with your doctor or pharmacist. Depending on your specific circumstances, your doctor may want you to:
- stop taking one of the medications,
- change one of the medications to another,
- change how you are taking one or both of the medications, or
- leave everything as is.
An interaction between two medications does not always mean that you must stop taking one of them. Speak to your doctor about how any drug interactions are being managed or should be managed.
Medications other than those listed above may interact with this medication. Tell your doctor or prescriber about all prescription, over-the-counter (non-prescription), and herbal medications you are taking. Also tell them about any supplements you take. Since caffeine, alcohol, the nicotine from cigarettes, or street drugs can affect the action of many medications, you should let your prescriber know if you use them.
Also tell them about any supplements you take. Since caffeine, alcohol, the nicotine from cigarettes, or street drugs can affect the action of many medications, you should let your prescriber know if you use them.
All material copyright MediResource Inc. 1996 – 2023. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/drug/getdrug/CO-Atenolol
What they treat us with: Atenolol. How does the heart survive this loss? about that that Russia will no longer be supplied with this drug and what is the main drawback of a common group of drugs for high blood pressure, says Indicator.Ru.
Yesterday it became known that the Japanese pharmaceutical corporation Takeda stops supplying metronidazole, the antidepressant drug amitriptyline, and the blood pressure lowering drug Atenolol to Russia. The third one made all the headlines as a “heart drug”, causing a slight panic. While conspiracy theorists suspect the Japanese of sabotage, and cynics recall advice to be treated with oak bark, we figure out whether to worry.
The third one made all the headlines as a “heart drug”, causing a slight panic. While conspiracy theorists suspect the Japanese of sabotage, and cynics recall advice to be treated with oak bark, we figure out whether to worry.
The lists (not) included
Atenolol is a drug from the group of beta-blockers, for studying the principles of action of which James Black even received a third of the Nobel Prize in 1988. His discovery was then called “the greatest breakthrough in the field of drugs against heart disease since the discovery of the [medical effect] of foxglove 200 years ago.” In the ranks of the first beta-blockers was Atenolol, approved by the FDA in 1981. The drug became the standard of care, often used in comparative studies as a model to help evaluate the effectiveness of new drugs.
Even now it has not lost its former glory. In the US, atenolol (including other drugs with the same active ingredient) is in the top 20 most prescribed drugs.:max_bytes(150000):strip_icc()/inositol-what-should-i-know-about-it-89466-1a6f6de880a14d9190afa5e1b65e647c.png) In a year, American doctors write out 26 million prescriptions for it.
In a year, American doctors write out 26 million prescriptions for it.
You can learn how to understand medicines on your own in the author’s online course “How we are treated” by Ekaterina Mishchenko, editor of Indicator.Ru: https://clck.ru/Pnmtk
in the List of vital and essential drugs for medical use. However, as we know from many examples (recall the analysis of Corvalol, Anaferon, Ergoferon or Mexidol), inclusion in such lists and popularity in the market are the results of active marketing and do not at all guarantee that the drug really helps.
From what, from what
Tenormina, Estecor and others) belongs to the group of beta-blockers (together with the hero of one of our previous reviews, Concor).
Atenolol molecules block the work of beta-adrenergic receptors of the first type, pretending to be adrenaline, which is known as a substance that triggers the body’s reaction to danger in the “fight or flight” type, as well as norepinephrine. Fraudulently occupied receptors can no longer bind to these substances. Adrenaline speeds up heartbeat and breathing and increases blood pressure, while suppressing the processes associated with rest and a quiet life, while norepinephrine puts the body in a state of rest and recovery, prompting the heart to pump out more blood at a time.
Fraudulently occupied receptors can no longer bind to these substances. Adrenaline speeds up heartbeat and breathing and increases blood pressure, while suppressing the processes associated with rest and a quiet life, while norepinephrine puts the body in a state of rest and recovery, prompting the heart to pump out more blood at a time.
β1 adrenoreceptors are located on the surface of cardiac muscle cells and in kidney tissues, and the more a drug targets this type, the better it targets the cardiovascular system. Atenolol is quite finicky and, at normal doses, does not bind to β2 adrenoceptors located in the lungs, gastrointestinal tract, liver, and other organs. Of the two mirror-like varieties of the atenolol molecule, which are present as a mixture in the drug, the S-isomer is considered the most active, but, unlike levocetirizine, it is usually not used separately.
In the body, atenolol is processed and broken down by the liver, but most of it is excreted unchanged, being excreted approximately equally with feces and urine.
Toad, go away
Due to its effect on the cardiovascular system, atenolol is often called an antianginal drug – from the Latin angina pectoris so called acute tonsillitis). Both diseases cause constricting, squeezing pain (only angina pectoris in the chest – due to oxygen starvation of the tissues during spasms or blockade of the arteries supplying the heart, and tonsillitis in the throat), and this is how the word 9 is translated0009 angina is from Latin, so their names are the same. But back to the reasons for the appointment: in addition to angina, the drug can be prescribed against high blood pressure and to reduce the risk of heart attack. How effective is it in such indications?
The PubMed Medical Articles Database contains 76 double-blind, randomized clinical trials of atenolol against angina pectoris. True, in most of them the substance is used as a standard for comparing new drugs, and its effectiveness is taken as an axiom.
Double-blind, randomized, placebo-controlled method is a method of clinical drug research in which the subjects are not privy to important details of the study being conducted. “Double-blind” means that neither the subjects nor the experimenters know who is being treated with what, “randomized” means that the distribution into groups is random, and placebo is used to show that the effect of the drug is not based on autosuggestion and that this medicine helps better than a tablet without active substance. This method prevents subjective distortion of the results. Sometimes the control group is given another drug with already proven efficacy, rather than a placebo, to show that the drug not only treats better than nothing, but also outperforms analogues.
Indicator.Ru
Help
Compared to bisoprolol (which we discussed in the article about Concor), atenolol is less active and is needed in large quantities (ten times). These trials were carried out on a small group of patients (only 40 people), but lasted as much as 6 months. In both groups, the frequency of angina attacks decreased, patients also had lower blood pressure and slowed heart rate, and side effects from the respiratory system were rare. The authors of a multicenter study on 147 patients, lasting 12 weeks in 11 hospitals in the Netherlands, came to the same conclusion.
In both groups, the frequency of angina attacks decreased, patients also had lower blood pressure and slowed heart rate, and side effects from the respiratory system were rare. The authors of a multicenter study on 147 patients, lasting 12 weeks in 11 hospitals in the Netherlands, came to the same conclusion.
Atenolol may also be useful in improving the overall quality of life of patients with angina pectoris. A study in 475 patients (who were treated with atenolol and other beta-blockers) showed that the relief or disappearance of symptoms often improves the overall well-being of patients. The same is true for another population – patients with hypertension.
Lowering will not save you
More than 500 double-blind controlled studies in English have been devoted to the effects of atenolol against hypertension. Alas, the vast majority of them are also evaluating other drugs, taking atenolol as the standard for a well-functioning drug. But if other drugs that are taken for comparison also do not work, such studies cannot prove the effectiveness of atenolol.
However, atenolol (and beta-blockers in general) against high blood pressure has been the subject of three Cochrane reviews.
The Cochrane Library is a database of the Cochrane Collaboration, an international non-profit organization involved in the development of World Health Organization guidelines. The name of the organization comes from the name of its founder, the 20th-century Scottish medical scientist Archibald Cochrane, who championed the need for evidence-based medicine and the conduct of competent clinical trials and wrote the book Efficiency and Efficiency: Random Reflections on Public Health. Medical scientists and pharmacists consider the Cochrane Database one of the most authoritative sources of such information: the publications included in it have been selected according to the standards of evidence-based medicine and report the results of randomized, double-blind, placebo-controlled clinical trials.
Indicator.Ru
Help
A review of 2014, summarizing information from 13 studies in total on 7812 patients, shows that selective beta-blockers, which prefer to bind to type 1 receptors, lower systolic pressure (the “upper” figure on the electronic tonometer ) by 10 mm Hg. Art, and diastolic – 8 mm Hg. Art. The results are promising, but there are two “buts”, a big one and a small one. The small thing is that the data mostly relate to mild or moderate elevated blood pressure.
Art, and diastolic – 8 mm Hg. Art. The results are promising, but there are two “buts”, a big one and a small one. The small thing is that the data mostly relate to mild or moderate elevated blood pressure.
There are two separate Cochrane Reviews devoted to the Big But. One concerns the effect of beta-blockers on the risk of a second heart attack – and here no evidence of the effectiveness of this group of drugs was found for 2014. The second review talks in general about the effect of beta-blockers in hypertension on life expectancy. The authors conclude that since most clinical trials of drugs of this type (atenolol is called the most used of them) have a high risk of bias, and such treatment has either no or very little effect on mortality rates, beta-blockers should not be the first to guard humankind. life.
Two more reviews (1 and 2) are devoted to peripheral arterial disease, which affects the blood supply to the legs. This condition, like high blood pressure, increases the risk of atherosclerosis, which can lead to myocardial infarction. However, there is not enough evidence on whether beta-blockers help with peripheral artery disease to warrant their use.
However, there is not enough evidence on whether beta-blockers help with peripheral artery disease to warrant their use.
Under pressure of evidence
But how is it that atenolol lowers blood pressure, but the risk of heart attack (which usually increases with blood pressure) does not? Researchers have been asking this question for a long time. At 19In 1997, Swedish scientists found that when compared with another drug (losartan, which is part of Lozap), the pressure in both groups decreased equally, and mortality and the frequency of heart attacks in the atenolol group remained higher.
In 2004, the British Medical Journal published an analysis of eight studies with a total of 24,000 patients. He showed that atenolol does not reduce mortality and risk of heart attack at all compared to placebo: patients simply have more “healthy” blood pressure.
Therefore, although atenolol is considered one of the most commonly used beta-blocker drugs for hypertension, in 2004 the Lancet itself questioned the appropriateness of their use in clinical trials as a medical standard against which new drugs should be measured. Despite this, in 2012 the drug was prescribed 33.8 million times, and some American cardiologists and other doctors issued more than 1,000 prescriptions for it a year.
Despite this, in 2012 the drug was prescribed 33.8 million times, and some American cardiologists and other doctors issued more than 1,000 prescriptions for it a year.
Since in most cases, doctors, when they start working, do not update their knowledge and do not keep up with new research on existing drugs, it is possible to wait for a fracture only in twenty years, according to estimates given in an article in The Atlantic. Apparently, at the end of the thirties, the generation of doctors will simply change.
Indicator.Ru recommends: do not panic and think about the purpose of prescribing aspirin), how much is to prolong the patient’s life. And here Atenolol loses: by lowering blood pressure, it does not reduce the risk of a heart attack. Therefore, the drug is not needed for prophylaxis in stable patients.
In the case of angina pectoris, there are many studies of Atenolol, but they almost all use the drug as a standard for comparison, taking its own effectiveness as a given. In general, clinical trials show that the drug reduces systolic and diastolic pressure – but no worse, and sometimes even better, this is done by its analogues from the group of beta-blockers (the same Concor), as well as other drugs for hypertension, which, moreover, also reduce mortality.
In general, clinical trials show that the drug reduces systolic and diastolic pressure – but no worse, and sometimes even better, this is done by its analogues from the group of beta-blockers (the same Concor), as well as other drugs for hypertension, which, moreover, also reduce mortality.
Therefore, firstly, do not be afraid, because Atenolol is not only not unique, but sometimes patients who drink it do not need it. Secondly, when prescribing and taking this drug, you should clearly understand what goal you are striving for. If you want the patient to live longer than without drugs (in research, this end point is called secondary outcome ), Atenolol will not help. But if you are looking for a temporary solution and want to remove the discomfort from high blood pressure or angina attacks, after the supply is stopped, you can switch to a generic drug (the same atenolol, but from another manufacturer), choose another beta-blocker or a medicine from the sartans group (for example, we talked about Valsakor and Lozap) – and what suits you best will depend on the characteristics and condition of your body.
In some cases, drugs may be prescribed in combination if there are no contraindications and the pressure is too high – a number of studies (for example, this one conducted at St. Bartholomew’s Hospital in London) hint that drugs in such cases are more effective.
Did you like the material? Add Indicator.Ru to “My Sources” of Yandex.News and read us more often.
Subscribe to Indicator.Ru on social networks: Facebook, VKontakte, Twitter, Telegram, Odnoklassniki.
Author: Ekaterina Mishchenko
Tags #How we are treated
Blood test for drug monitoring of the drug Atenolol in the Optimum laboratory in Sochi (Adler)
Get test results
- Home
- Analyzes and prices
- Atenolol
More about the doctor
Deadline for
(working days):
up to 10 days.
Price:
1650 ₽ *
* Taking biomaterial is paid separately
Atenolol drug monitoring is a laboratory diagnostic test from the spectral analysis group, designed to determine the level of the test drug atenolol in the blood.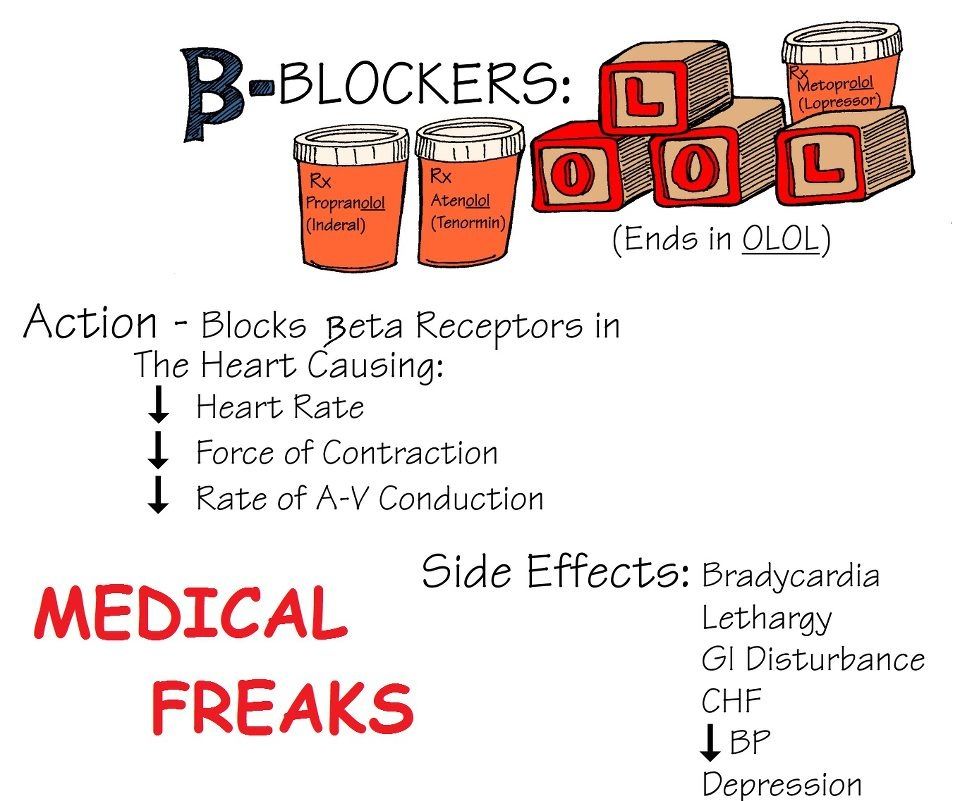 The method is relatively new and allows the most effective assessment of the correctness and effectiveness of treatment with this drug. The study is carried out on special electronic digital equipment – a spectrometer using mass spectrometry technology.
The method is relatively new and allows the most effective assessment of the correctness and effectiveness of treatment with this drug. The study is carried out on special electronic digital equipment – a spectrometer using mass spectrometry technology.
When is Atenolol monitoring indicated?
Atenolol belongs to a group of drugs that block the type 1 beta receptors of the adrenal system. Thanks to this, a powerful therapeutic effect on the cardiovascular system is achieved in the form of expansion of the coronary vessels, lowering blood pressure, and normalizing the heart rhythm. Most patients with chronic forms of such diseases require systematic and long-term use of atenolol. Against this background, the likelihood of side effects and overdose . In order to monitor the effectiveness of the treatment process, drug monitoring of this drug is intended.
Important to remember! The World Health Organization’s recommended treatment monitoring for Atenolol is best achieved through laboratory testing. Evaluation of the adequacy of treatment is based on a comparison of clinical data and data from a control blood test!
Evaluation of the adequacy of treatment is based on a comparison of clinical data and data from a control blood test!
Preparation for drug monitoring Atenolol
The reliability of the obtained results of drug monitoring of the drug atenolol depends on compliance with the general rules for all blood tests. Additional preparation is not required. It is not necessary to change the dosage regimen and taking the drug on the eve of the study. 1-3 days before blood sampling from a vein, it is desirable to minimize the amount of drugs taken with atenolol.
Ideally, blood sampling is performed before taking the next recommended dose of the drug, as well as 2-3 hours after it (the time of maximum plasma concentration).
How to evaluate the result of the analysis?
Uniform generally accepted reference values relative to the norm concentration of atenolol in the blood serum have not been developed. Laboratories conducting drug monitoring for this drug indicate their standards in the results of the study.

 This can lead to serious heart-related problems. Ask your doctor how you should gradually reduce the dose before you stop taking this medicine.
This can lead to serious heart-related problems. Ask your doctor how you should gradually reduce the dose before you stop taking this medicine.
 g., clonidine, methyldopa)
g., clonidine, methyldopa) g., furosemide, hydrochlorothiazide, triamterene)
g., furosemide, hydrochlorothiazide, triamterene) g., gliclazide, glyburide, tolbutamide)
g., gliclazide, glyburide, tolbutamide)