What is hct on lab results. Hematocrit Test: Understanding HCT in Lab Results and Its Clinical Significance
What is hematocrit (HCT) on lab results. How is HCT measured. What are normal HCT values. What factors can affect HCT levels. How is HCT used in clinical diagnosis.
What is Hematocrit (HCT) and Why is it Important?
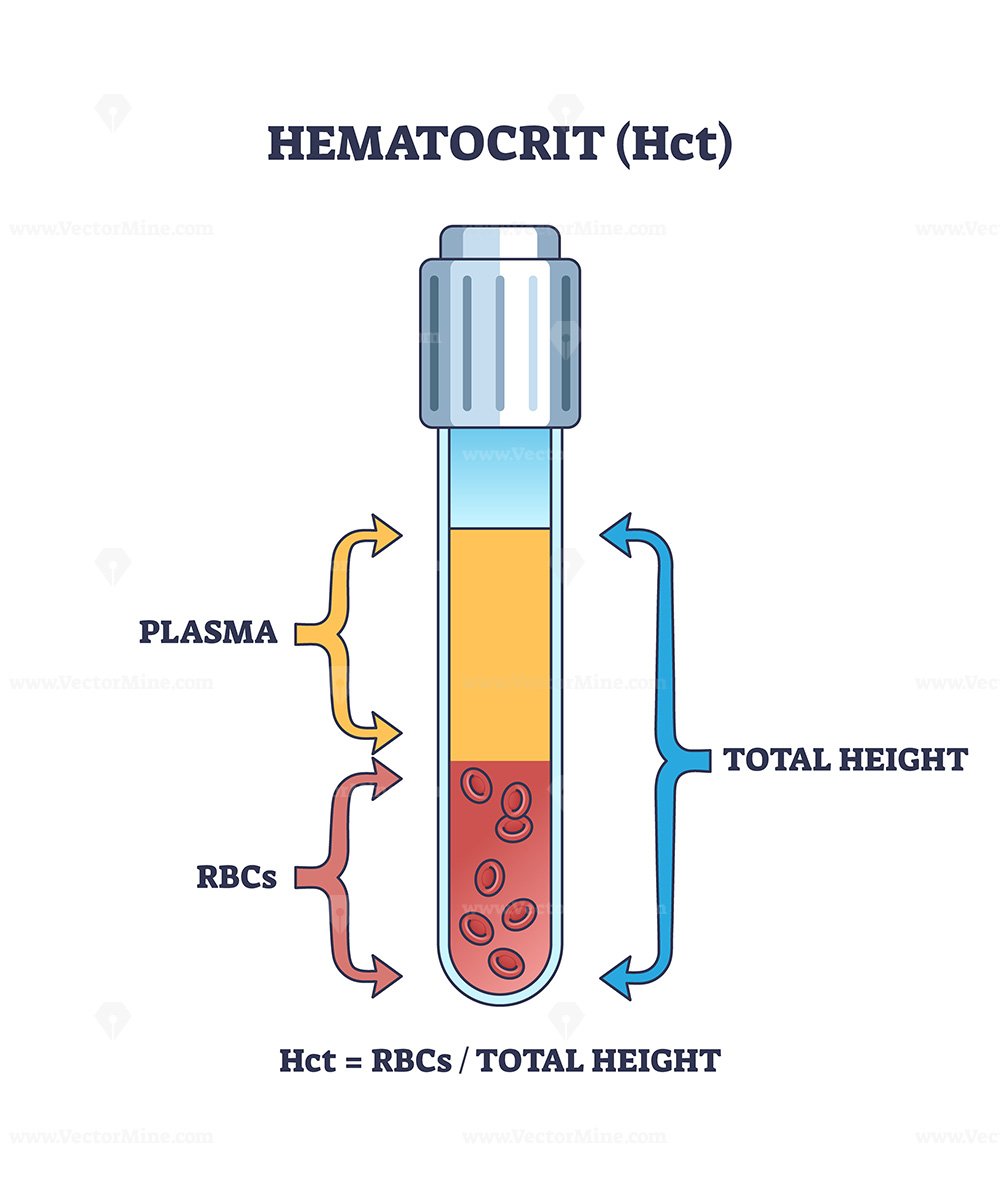
Hematocrit (HCT) is a crucial blood test that measures the volume of red blood cells (RBCs) in relation to the total blood volume. It’s also known as packed cell volume (PCV). HCT plays a vital role in diagnosing various blood-related conditions and monitoring treatment effectiveness.
The term “hematocrit” has its roots in the English prefix “hemato-” (relating to blood) and the Greek word “krites” (judge). This etymology reflects its function as a measure or “judge” of blood composition.
Clinical Significance of HCT
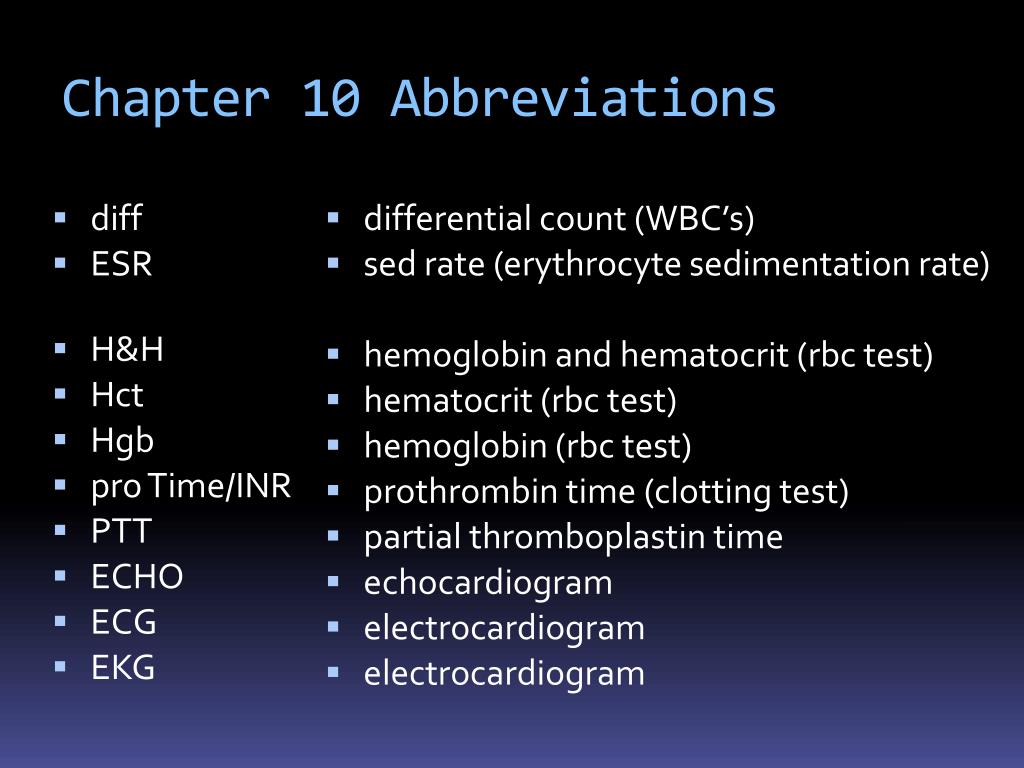
HCT is an essential component of the complete blood count (CBC) and serves several important clinical purposes:
- Diagnosing anemia and polycythemia
- Assessing overall health status
- Monitoring response to treatments for blood disorders
- Evaluating hydration status
- Screening for potential underlying health conditions
Understanding HCT values can provide valuable insights into a patient’s health, making it a fundamental tool in medical diagnostics and treatment planning.
How is Hematocrit Measured? Exploring Different Methods
There are three primary methods for measuring hematocrit: the macro-hematocrit method, the micro-hematocrit method, and automated analyzers. Each method has its own advantages and applications in different clinical settings.
Macro-Hematocrit Method
This traditional method uses a Wintrobe hematocrit tube and a centrifuge machine. Here’s how it works:
- Blood is collected in a tube containing an anticoagulant (usually EDTA).
- The blood is transferred to a Wintrobe tube using a Pasteur pipette, filling it to the 100 mm mark.
- The tube is centrifuged at 3000 rpm for 30 minutes.
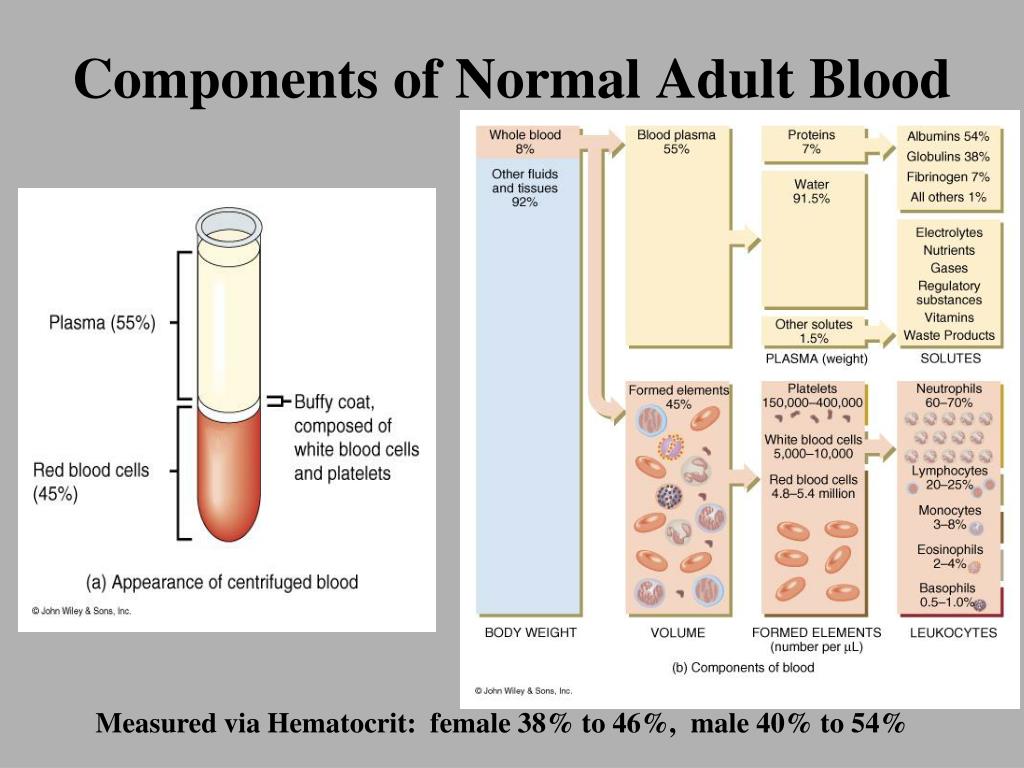
- After centrifugation, the blood separates into three distinct layers: RBCs at the bottom, a thin layer of white blood cells (WBCs) and platelets (buffy coat) in the middle, and plasma at the top.
- The height of the RBC column is measured and reported as the HCT percentage.
While this method is still used in some primary care settings and for teaching purposes, it has largely been replaced by more efficient techniques.
Micro-Hematocrit Method
The micro-hematocrit method is an improvement over the macro-hematocrit technique, requiring less blood and time. It involves:
- Collecting blood in a small capillary tube (usually 75 mm long and 1 mm in diameter).
- Sealing both ends of the tube with clay or heat.
- Centrifuging the tube at 11,000-12,000 rpm for 4-5 minutes.
- Reading the results using a scale on a tube holder or a microhematocrit card reader.
This method is particularly useful for patients from whom blood collection is challenging, such as pediatric patients or those with hypovolemia.
Automated Analyzers
Modern clinical laboratories predominantly use automated hematology analyzers to measure HCT. These machines employ the Coulter principle, which measures the average RBC size and number by detecting changes in electrical impedance as blood cells pass through a small aperture between two electrodes.
Automated analyzers offer several advantages:
- High-throughput capability
- Increased accuracy and precision
- Simultaneous measurement of multiple blood parameters
- Reduced human error
- Faster turnaround times for results
Normal Hematocrit Values: What Do They Mean?
Understanding normal HCT values is crucial for interpreting test results accurately. However, it’s important to note that these values can vary slightly depending on factors such as age, sex, and the specific laboratory’s reference range.

Typical HCT Ranges for Adults
- Adult males: 40% to 54%
- Adult females: 36% to 48%
These ranges represent the percentage of blood volume occupied by RBCs. For example, an HCT of 45% means that 45% of the blood volume consists of red blood cells, while the remaining 55% is plasma and other components.
Interpreting HCT Results
How do healthcare providers interpret HCT results? Here’s a brief overview:
- Low HCT (below normal range): May indicate anemia, blood loss, or overhydration
- High HCT (above normal range): Could suggest polycythemia, dehydration, or living at high altitudes
- Normal HCT: Generally indicates healthy red blood cell production and overall blood volume
It’s crucial to remember that HCT values should always be interpreted in conjunction with other blood tests and the patient’s clinical presentation. A single abnormal result doesn’t necessarily indicate a health problem.
Factors Affecting Hematocrit Levels: Physiological and Pathological Influences
Numerous factors can influence HCT levels, ranging from normal physiological variations to pathological conditions. Understanding these factors is essential for accurate interpretation of HCT results.
Physiological Factors
- Age: Newborns typically have higher HCT levels, which gradually decrease during the neonatal period.
- Sex: Adult males generally have higher HCT levels than adult females due to the influence of testosterone on red blood cell production.
- Pregnancy: Pregnant women often show lower HCT due to hemodilution (increased plasma volume).
- Altitude: People living at high altitudes tend to have higher HCT levels as a compensatory mechanism for the lower oxygen levels in the air.
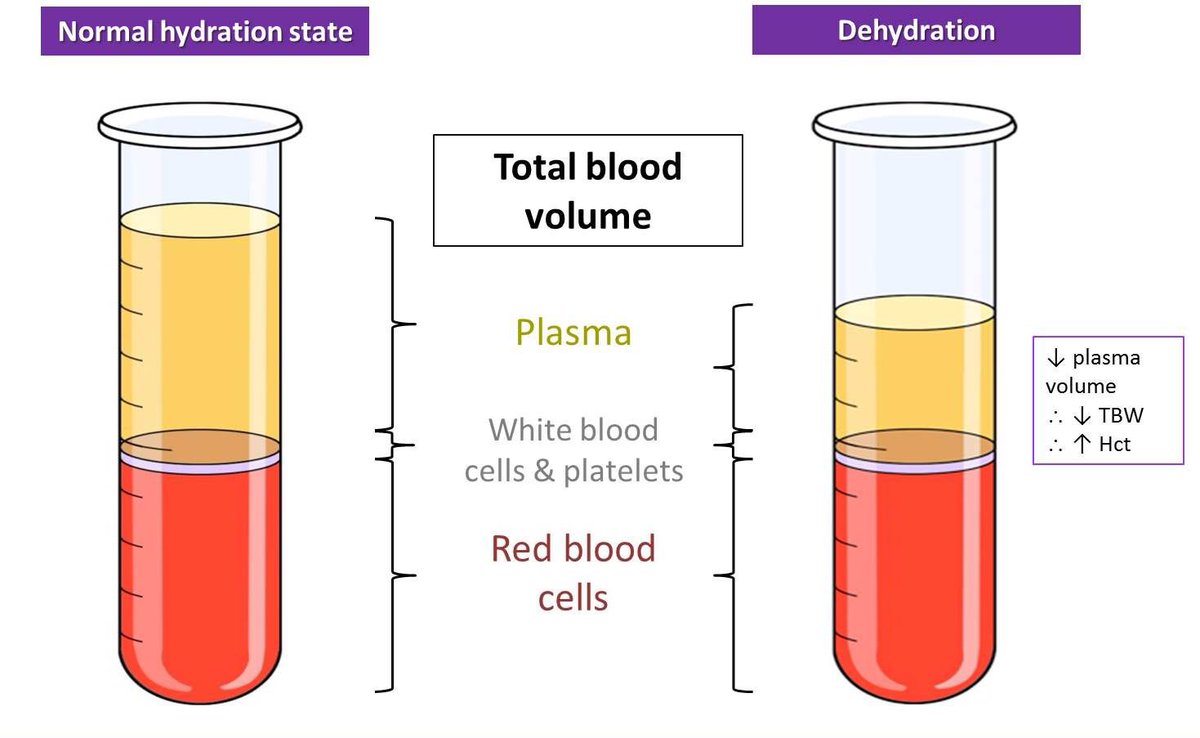
- Hydration status: Dehydration can temporarily increase HCT, while overhydration can decrease it.
Pathological Factors
- Anemia: Various types of anemia can lead to decreased HCT levels.
- Polycythemia: Conditions causing increased red blood cell production can result in elevated HCT.
- Blood loss: Acute or chronic blood loss can reduce HCT levels.
- Bone marrow disorders: Conditions affecting the bone marrow’s ability to produce blood cells can impact HCT.
- Certain medications: Some drugs can affect red blood cell production or survival, influencing HCT levels.
Recognizing these influencing factors is crucial for healthcare providers when interpreting HCT results and making clinical decisions.

Clinical Applications of Hematocrit Testing: Beyond Anemia Detection
While HCT is commonly associated with anemia diagnosis, its clinical applications extend far beyond this single condition. Let’s explore some of the key uses of HCT testing in medical practice.
Diagnosis and Monitoring of Blood Disorders
HCT plays a crucial role in:
- Anemia diagnosis and classification
- Polycythemia detection and management
- Monitoring response to treatments for various blood disorders
- Assessing the need for blood transfusions
Evaluation of Hydration Status
HCT can provide valuable information about a patient’s hydration status:
- Elevated HCT may indicate dehydration
- Decreased HCT could suggest overhydration or hemodilution
Assessment of Oxygen-Carrying Capacity
Since HCT reflects the proportion of RBCs in the blood, it indirectly indicates the blood’s oxygen-carrying capacity. This information is valuable in:
- Evaluating patients with respiratory disorders
- Assessing cardiovascular health
- Monitoring patients undergoing chemotherapy or radiation therapy
Preoperative Screening
HCT is often part of preoperative blood tests to:
- Assess a patient’s overall health status
- Identify potential risks for surgery
- Determine the need for preoperative interventions (e.g., iron supplementation)
Sports Medicine Applications
In sports medicine, HCT testing can be used to:
- Monitor athletes’ response to training
- Detect blood doping practices
- Assess adaptation to high-altitude training
These diverse applications underscore the importance of HCT as a versatile diagnostic tool in modern medicine.
Potential Limitations and Considerations in Hematocrit Testing
While HCT is a valuable diagnostic tool, it’s important to be aware of its limitations and potential sources of error. Understanding these factors can help healthcare providers interpret results more accurately and avoid misdiagnosis.
Methodological Variations
Different HCT measurement methods can yield slightly different results:
- Manual methods (macro- and micro-hematocrit) may be subject to human error in reading and interpretation.
- Automated analyzers, while generally more accurate, can be affected by abnormal red blood cell shapes or sizes.
- Variations in centrifugation speed and duration can affect results in manual methods.
Sample-Related Factors
The quality and handling of the blood sample can impact HCT results:

- Improper mixing of the blood sample can lead to inaccurate measurements.
- Delayed processing of samples may affect results due to cell swelling or breakdown.
- The presence of cold agglutinins can cause red blood cell clumping, potentially leading to falsely elevated HCT.
Physiological Fluctuations
Normal physiological changes can affect HCT levels:
- Diurnal variations: HCT can fluctuate slightly throughout the day.
- Postural changes: Standing up can cause a temporary increase in HCT due to fluid shifts.
- Recent food intake or physical activity can influence HCT levels.
Interference from Medical Conditions
Certain medical conditions can interfere with accurate HCT measurement:
- Severe leukocytosis (high white blood cell count) can artificially elevate HCT in some automated analyzers.
- Hyperproteinemia (high protein levels in the blood) can affect plasma trapping between red blood cells, potentially leading to falsely elevated HCT.
- Conditions causing abnormal red blood cell shapes (e.g., sickle cell disease) can impact HCT measurements.
Limitations in Specific Populations
HCT interpretation may require special consideration in certain patient groups:
- Neonates: HCT levels are naturally higher and more variable in newborns.
- Pregnant women: Physiological hemodilution during pregnancy affects normal HCT ranges.
- Elderly patients: Age-related changes in blood composition may influence HCT interpretation.
Awareness of these limitations and considerations is crucial for healthcare providers to ensure accurate interpretation of HCT results and appropriate clinical decision-making.
Future Directions in Hematocrit Testing and Research
As medical technology and our understanding of hematology advance, the field of hematocrit testing continues to evolve. Let’s explore some of the exciting future directions and potential innovations in this area.
Point-of-Care Testing
The development of rapid, portable HCT testing devices is an area of active research:
- Microfluidic devices that can measure HCT from a single drop of blood
- Smartphone-based apps and attachments for HCT measurement
- Wearable devices for continuous HCT monitoring in specific patient populations
These innovations could revolutionize HCT testing in remote areas, emergency settings, and home healthcare.

Integration with Artificial Intelligence
The application of AI and machine learning to HCT analysis holds promise for:
- Improved accuracy in detecting abnormal HCT patterns
- Predictive analytics for early disease detection based on HCT trends
- Personalized reference ranges based on individual patient characteristics
Novel Biomarkers and Combined Analyses
Research is ongoing to identify new biomarkers that can complement HCT measurements:
- Exploration of red blood cell distribution width (RDW) in conjunction with HCT for more nuanced diagnosis
- Investigation of reticulocyte parameters for assessing bone marrow response
- Development of multi-parameter algorithms incorporating HCT and other hematological indices for improved diagnostic accuracy
Non-Invasive HCT Measurement Techniques
Efforts are underway to develop non-invasive methods for HCT measurement:
- Optical techniques using near-infrared spectroscopy
- Bioimpedance-based methods for estimating HCT
- Ultrasound-based approaches for real-time HCT assessment
These methods could reduce the need for blood draws, making HCT testing more comfortable and accessible for patients.
Personalized Medicine Applications
The future of HCT testing may involve more personalized approaches:
- Tailoring HCT reference ranges based on individual genetic profiles
- Incorporating HCT into comprehensive health monitoring programs
- Using HCT as part of predictive models for personalized treatment plans
Environmental and Global Health Applications
HCT testing could play a role in broader health initiatives:
- Monitoring population health in areas affected by environmental pollutants
- Assessing the impact of climate change on human physiology
- Large-scale screening programs in developing countries to address anemia and malnutrition
These future directions highlight the ongoing importance of HCT testing in clinical practice and research. As technology advances and our understanding deepens, HCT will likely continue to be a valuable tool in diagnosing, monitoring, and managing a wide range of health conditions.
Hematocrit – StatPearls – NCBI Bookshelf
Himel Mondal; Saran Lotfollahzadeh.
Author Information and Affiliations
Last Update: January 2, 2023.
Introduction
The term “hematocrit (HCT)” originated from English “hemato-“ and Greek “krites.” HCT measures the volume of packed red blood cells (RBC) relative to whole blood. Hence, it is also known and reported as a packed cell volume (PCV). It is a simple test to identify conditions like anemia or polycythemia and also to monitor response to the treatment. A glass tube and a centrifuge machine are sufficient to measure HCT. After centrifugation, the component of blood separates into three distinct parts. From below upwards, the layers are – a layer of red blood cells (RBC), a layer of white blood cells(WBC) and platelets, and a layer of plasma at the top. This method of determining HCT by Wintrobe hematocrit tube is known as the “macro-hematocrit” method.[1]
A Wintrobe tube is a narrow glass tube measuring 110-mm-long, with graduation from 0 to 100 mm in both ascending and descending order. This method has been succeeded by the “micro-hematocrit” method which uses a small capillary tube instead of a Wintrobe hematocrit tube. It requires less quantity of blood as well as less time requirement for the testing procedure. It is beneficial for patients from whom blood collection is difficult (e.g., pediatric patients/hypovolemia). However, the principle of the test remains the same as the “macro-hematocrit” method. HCT calculation is by dividing the lengths of the packed RBC layer by the length of total cells and plasma. As it is a ratio, it doesn’t have any unit. Multiplying the ratio by 100 gives the accurate value, which is the accepted reporting style for HCT. A normal adult male shows an HCT of 40% to 54% and a female shows 36% to 48%.[2] Though these two methods are still in use in some settings of primary care and medical teachings, they are widely replaced in the majority of settings by an automated analyzer, where HCT reports get generated along with the complete blood count.
This method has been succeeded by the “micro-hematocrit” method which uses a small capillary tube instead of a Wintrobe hematocrit tube. It requires less quantity of blood as well as less time requirement for the testing procedure. It is beneficial for patients from whom blood collection is difficult (e.g., pediatric patients/hypovolemia). However, the principle of the test remains the same as the “macro-hematocrit” method. HCT calculation is by dividing the lengths of the packed RBC layer by the length of total cells and plasma. As it is a ratio, it doesn’t have any unit. Multiplying the ratio by 100 gives the accurate value, which is the accepted reporting style for HCT. A normal adult male shows an HCT of 40% to 54% and a female shows 36% to 48%.[2] Though these two methods are still in use in some settings of primary care and medical teachings, they are widely replaced in the majority of settings by an automated analyzer, where HCT reports get generated along with the complete blood count.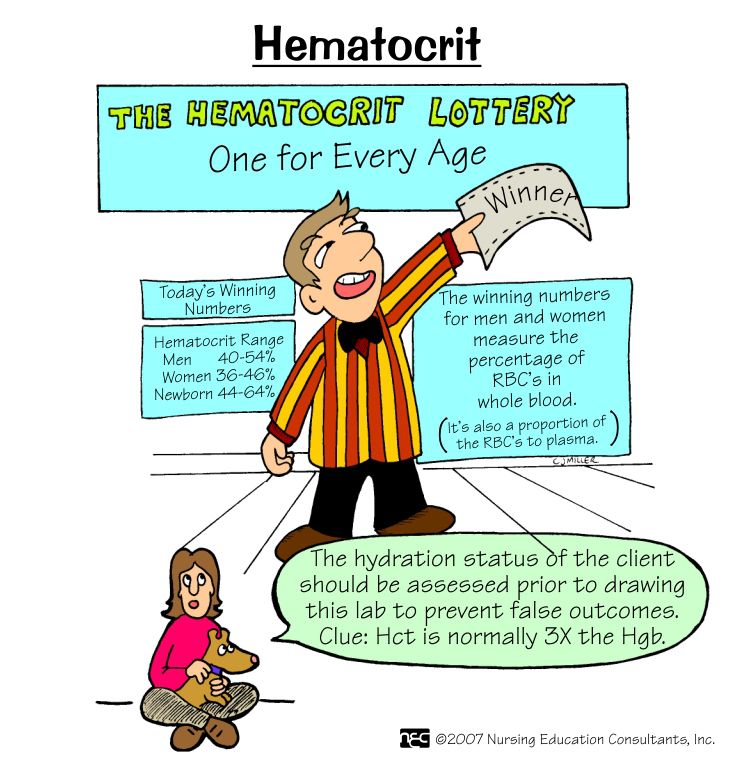
Specimen Requirements and Procedure
For the macro-hematocrit method, venous blood is taken as a random sample (i.e., no special precautions needed) maintaining proper aseptic precautions. The blood is either collected in a commercially available vacutainer containing ethylenediaminetetraacetic acid (EDTA) or in a vial/test tube with EDTA where vacutainer is not available[3]. For the microhematocrit method, the blood requirement is less, and single finger-prick blood is sufficient. Heparin filled capillary tube may is used to collect blood. However, if there is available blood with anticoagulant for other hematologic tests, a capillary tube without heparin can be used. For measurement of HCT in automated hematologic cell counter, blood with anticoagulant used for CBC is necessary.
Testing Procedures
The macro-hematocrit method uses a Wintrobe hematocrit tube, a centrifuge machine, and a Pasteur pipette. Blood is filled in Wintrobe hematocrit tube up to 100 mm mark by the help of Pasteur pipette.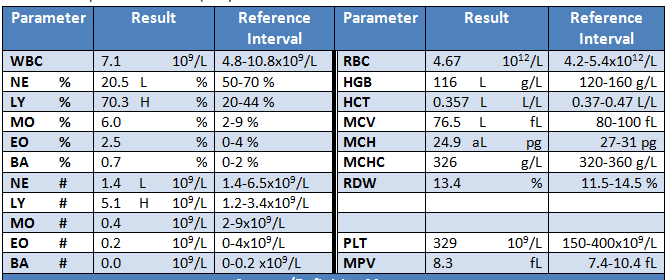 Care is taken not to leave any bubble in the blood column. For this, the tube is filled slowly with the tip of the pipette being always below the highest position of the blood column. Then, the tube gets placed in the centrifuge machine. When testing a single specimen, another blood-filled Wintrobe hematocrit tube is kept on the opposite holder to counterbalance. The spin setting is 3000 rpm for 30 min. After completion of the centrifugation, the tube is taken out, and RBC column height is reported as HCT. During the reporting, special precaution is necessary to omit the buffy coat, which is a combination of WBC and platelets. This layer should not be included in the HCT, as it may lead to false positive results.
Care is taken not to leave any bubble in the blood column. For this, the tube is filled slowly with the tip of the pipette being always below the highest position of the blood column. Then, the tube gets placed in the centrifuge machine. When testing a single specimen, another blood-filled Wintrobe hematocrit tube is kept on the opposite holder to counterbalance. The spin setting is 3000 rpm for 30 min. After completion of the centrifugation, the tube is taken out, and RBC column height is reported as HCT. During the reporting, special precaution is necessary to omit the buffy coat, which is a combination of WBC and platelets. This layer should not be included in the HCT, as it may lead to false positive results.
For the microhematocrit method, after filling the blood in a capillary tube, the two ends of the tube (commonly 75 mm long, 1 mm diameter) are sealed with clay sealant or heat. Then, it is centrifuged at a rate of 11000 to 12000 rpm for 4 to 5 min. Reading is with the help of the scale on a tube holder or microhematocrit card reader.
The automated analyzer measures the average RBC size and number by the “Coulter principle”[4]. In this method, the size and number of the RBCs is measurable by detecting impedance while the blood passes through a passage between two electrodes.
Interfering Factors
There are several physiological and pathological conditions where the HCT may deviate from its normal range. New-born babies show a high HCT, and it gradually decreases during the neonatal period[5]. Adult male shows higher HCT than an adult female.[6] Pregnant women show lower HCT due to hemodilution. In high altitude, the number of RBC becomes high due to persistent hypoxia; hence, the inhabitant of high altitude shows higher HCT. Methodological variation may provide a minor deviation of HCT tested for the same sample. In the macro-hematocrit method, there is an increased amount of trapped plasma (approximately 2%) in the packed RBC, which may give a higher HCT. This factor becomes minimized in the microhematocrit method, where the amount of trapped plasma is less as the diameter of the capillary tube is less than that of the Wintrobe hematocrit tube.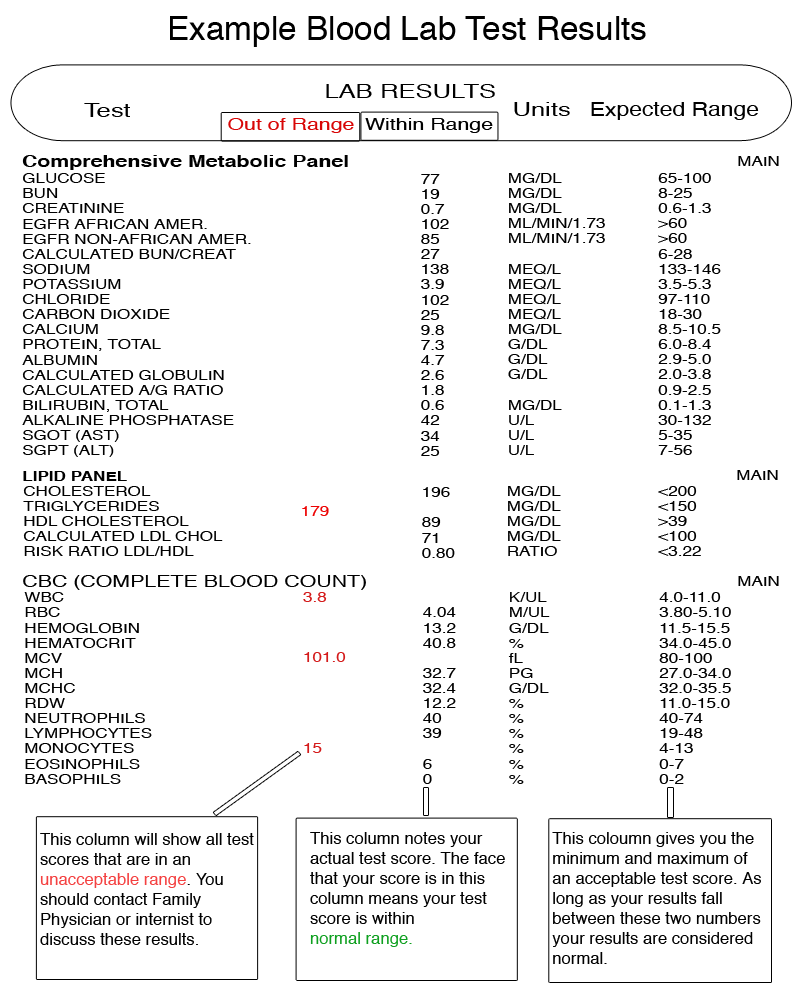 Blood collected from different sources may also show variation. Venous blood shows higher HCT than arterial blood. However, there is no difference in HCT between venous blood and finger prick blood.[7]
Blood collected from different sources may also show variation. Venous blood shows higher HCT than arterial blood. However, there is no difference in HCT between venous blood and finger prick blood.[7]
Results, Reporting, and Critical Findings
Wintrobe hematocrit tube has graduation 0 to 100 from below upwards. Hence, the highest level of packed RBC is the HCT in percentage. For the microhematocrit method, the reading is from the HCT card or scale. However, for these two methods, even without any graduation or scale, the HCT value can be calculated with a simple scale as we compare the length of the RBC column with the total length of the fluid column. The final report is a percentage. HCT, along with RBC count and hemoglobin (Hb) concentration, is used to report other blood indices manually as follows:
The mean corpuscular volume (MCV) calculation uses HCT and RBC count.
Mean corpuscular hemoglobin concentration (MCHC) is calculated with Hb concentration and HCT.
Clinical Significance
In primary health care settings, especially in resource-limited settings, macro-hematocrit and micro-hematocrit methods are two low-cost and simple tests for determining RBC in blood. Clinically, HCT is used to identify anemia and polycythemia along with other parameters (e.g., RBC count, Hb concentration). In anemia, where there are fewer RBCs in the circulating blood relative to the total volume of the blood, the HCT decreases.[8] In polycythemia, there is a higher number of RBCs in the blood; HCT increases. Smokers and chronic obstructive pulmonary disease (COPD) patients also have high HCT due to chronic hypoxia. The increase in HCT increases the viscosity of the blood, so does the peripheral resistance. Hence, patients with higher HCT may have higher blood pressure.
Quality Control and Lab Safety
Handling of blood should take place with the maintenance of proper aseptic precautions. The collected blood should be tested as soon as possible after collection.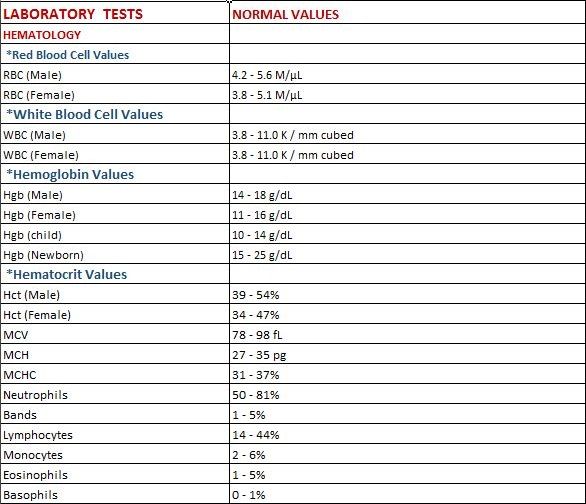 Prolonged storage at the room temperature would result in a change in the shape of the RBCs due to metabolism. After about 6 hours, the chances of hemolysis increase, which would give an erroneous result. In the macro-hematocrit method, the filing of the Wintrobe hematocrit tube requires proper care. In the microhematocrit method, the sealing of the capillary tube should be secure to prevent any leakage. The centrifuge machine should not be opened during the test to avoid erroneous results. The chances of error in the result will increase if the centrifugation is interrupted. Immediately after completion of the rotation, the operator should not open the lid should until after the complete stoppage of the rotation. For reuse of the Wintrobe hematocrit tube, proper cleaning is necessary as any foreign particle inside the tube would be counted either in the RBC column or plasma column.
Prolonged storage at the room temperature would result in a change in the shape of the RBCs due to metabolism. After about 6 hours, the chances of hemolysis increase, which would give an erroneous result. In the macro-hematocrit method, the filing of the Wintrobe hematocrit tube requires proper care. In the microhematocrit method, the sealing of the capillary tube should be secure to prevent any leakage. The centrifuge machine should not be opened during the test to avoid erroneous results. The chances of error in the result will increase if the centrifugation is interrupted. Immediately after completion of the rotation, the operator should not open the lid should until after the complete stoppage of the rotation. For reuse of the Wintrobe hematocrit tube, proper cleaning is necessary as any foreign particle inside the tube would be counted either in the RBC column or plasma column.
Enhancing Healthcare Team Outcomes
After the introduction of the automated hematology cell counters, the usage of macro-hematocrit and microhematocrit method is less used nowadays. However, in many resource-poor settings, it is still used for the diagnosis of anemia and polycythemia and monitoring response to treatment. In a rural healthcare facility, it is a more accurate method for identifying anemia than the total RBC count, as chances of error in manual RBC count is very high. The micro-hematocrit method is more acceptable as it requires less amount of blood, and the testing time is very less in comparison to the macro-hematocrit method. Due to the requirement of less amount of blood and less time for the test, it may be useful in a mass survey.
However, in many resource-poor settings, it is still used for the diagnosis of anemia and polycythemia and monitoring response to treatment. In a rural healthcare facility, it is a more accurate method for identifying anemia than the total RBC count, as chances of error in manual RBC count is very high. The micro-hematocrit method is more acceptable as it requires less amount of blood, and the testing time is very less in comparison to the macro-hematocrit method. Due to the requirement of less amount of blood and less time for the test, it may be useful in a mass survey.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
Wintrobe hematocrit tube containing components of blood after centrifugation. Contributed by Shaikat Mondal, MD
References
- 1.
Fred HL. Maxwell Myer Wintrobe: new history and a new appreciation. Tex Heart Inst J. 2007;34(3):328-35.
 [PMC free article: PMC1995040] [PubMed: 17948084]
[PMC free article: PMC1995040] [PubMed: 17948084]- 2.
Billett HH. Hemoglobin and Hematocrit. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Butterworths; Boston: 1990. [PubMed: 21250102]
- 3.
Bamberg R, Gwyn T, Miller J, Thompson M, Transou P. The effects of over-anticoagulated blood on hematocrit values by the microcentrifuge method. Clin Lab Sci. 2008 Summer;21(3):146-50. [PubMed: 18678135]
- 4.
Peng L, Wang W, Bai L. Performance evaluation of the Z2 coulter counter for WBC and RBC counting. Int J Lab Hematol. 2007 Oct;29(5):361-8. [PubMed: 17824917]
- 5.
Jopling J, Henry E, Wiedmeier SE, Christensen RD. Reference ranges for hematocrit and blood hemoglobin concentration during the neonatal period: data from a multihospital health care system. Pediatrics. 2009 Feb;123(2):e333-7. [PubMed: 19171584]
- 6.
Zeng SM, Yankowitz J, Widness JA, Strauss RG.
 Etiology of differences in hematocrit between males and females: sequence-based polymorphisms in erythropoietin and its receptor. J Gend Specif Med. 2001;4(1):35-40. [PubMed: 11324238]
Etiology of differences in hematocrit between males and females: sequence-based polymorphisms in erythropoietin and its receptor. J Gend Specif Med. 2001;4(1):35-40. [PubMed: 11324238]- 7.
Yang ZW, Yang SH, Chen L, Qu J, Zhu J, Tang Z. Comparison of blood counts in venous, fingertip and arterial blood and their measurement variation. Clin Lab Haematol. 2001 Jun;23(3):155-9. [PubMed: 11553055]
- 8.
Malenica M, Prnjavorac B, Bego T, Dujic T, Semiz S, Skrbo S, Gusic A, Hadzic A, Causevic A. Effect of Cigarette Smoking on Haematological Parameters in Healthy Population. Med Arch. 2017 Apr;71(2):132-136. [PMC free article: PMC5511531] [PubMed: 28790546]
Disclosure: Himel Mondal declares no relevant financial relationships with ineligible companies.
Disclosure: Saran Lotfollahzadeh declares no relevant financial relationships with ineligible companies.
Hematocrit (HCT) / Packed Cell Volume (PCV) – Lab Results explained
Hematocrit is the percentage of red cells in your blood.
Normal levels of hematocrit for men range from 41% to 50%.
Normal level for women is 36% to 48%.
What is hematocrit?
The hematocrit level is simply the percentage of red cells in your blood. For example, a level of 38% is considered the minimum needed for donating blood.
Hematocrit is the percentage by volume of red cells in your blood. Blood is made up of red blood cells, white blood cells and platelets, suspended in plasma. Together, those comprise about 45% of the volume of our blood, but the specific percentages of each can vary.
The importance of hematocrit:
Hematocrit is a significant measurement as it can identify whether you have sufficient red blood cells for oxygen transportation and delivery.
Hematocrit is important because red blood cells are essential to your survival. They contain a vital protein component called hemoglobin that binds to oxygen, which fuels all the cells in your body.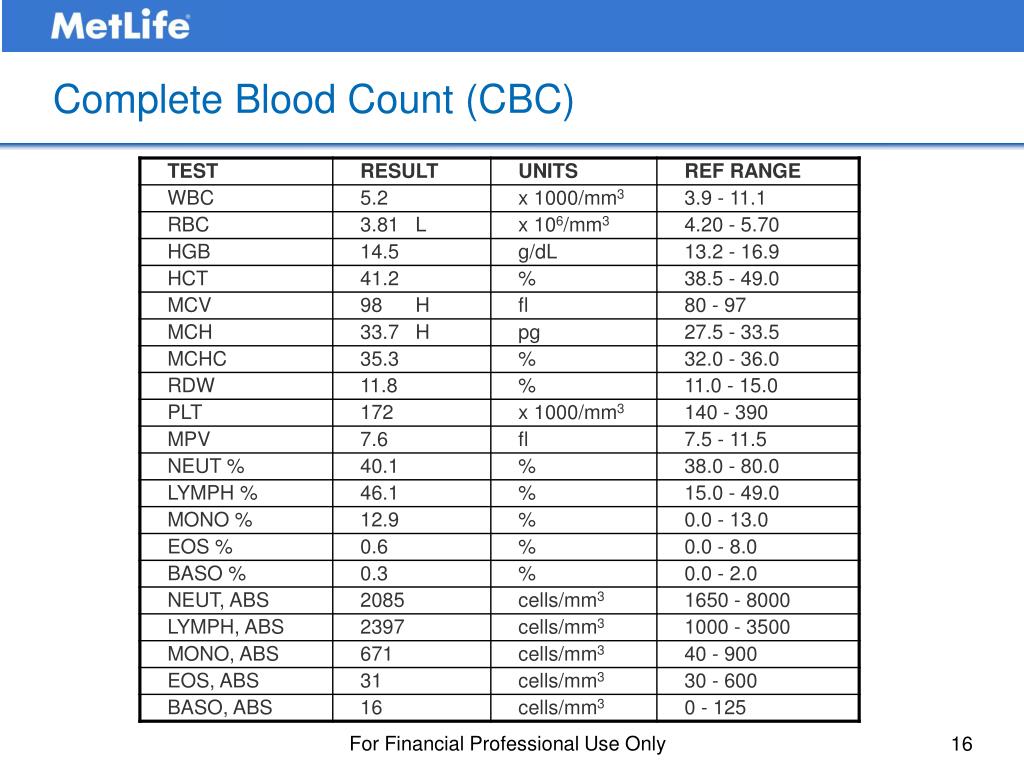 When red blood cells pass through your lungs, they bind to and transport oxygen to various cells in your body. On their way back to your lungs, they carry carbon dioxide to be exhaled.
When red blood cells pass through your lungs, they bind to and transport oxygen to various cells in your body. On their way back to your lungs, they carry carbon dioxide to be exhaled.
Why is the hematocrit test performed?
The hematocrit test checks for anemia, usually along with a hemoglobin test or as part of a complete blood count (CBC). This test can screen for, diagnose, or monitor many conditions and diseases that affect the blood’s proportion made up of red blood cells (RBCs).
What is a normal hematocrit level?
Normal hematocrit levels vary based on age and race, gender, etc.
In adults, normal levels for men range from 41%-50%. For women, the normal range is slightly lower: 36%-44%. A hematocrit level below the normal range, meaning the person has too few red blood cells, is called anemia. A hematocrit level above the normal range, meaning too many red blood cells, may indicate polycythemia or erythrocytosis.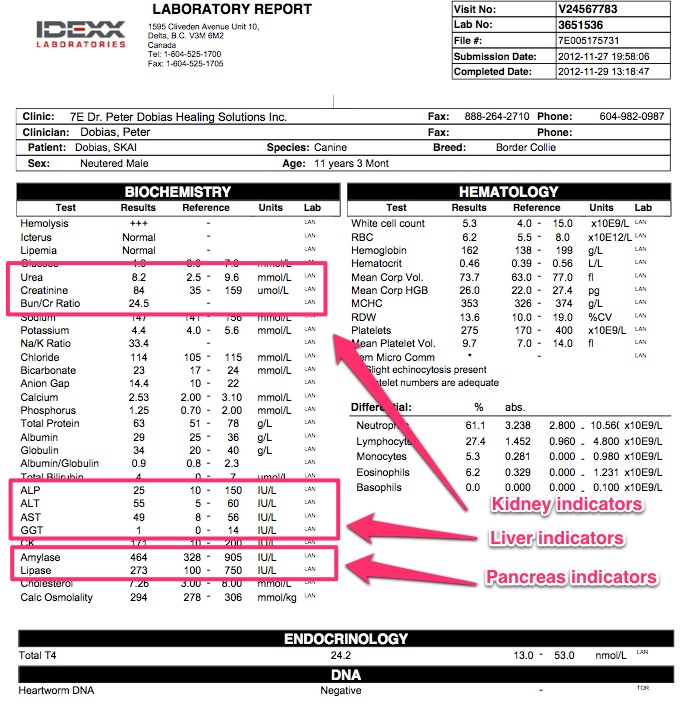
What are symptoms of anemia?
Symptoms of anemia include fatigue, shortness of breath and dizziness.
What are symptoms of polycythemia?
Symptoms of polycythemia include fatigue, itching, headaches, and sweating.
What are symptoms of erythrocytosis?
Symptoms of erythrocytosis includes headaches, dizziness, shortness of breath, and nosebleeds.
What is the difference between a hematocrit and a hemoglobin test?
Hematocrit is the percentage of red blood cells in your blood. Hemoglobin is a part of your red blood cell. Hemoglobin helps your red blood cells carry oxygen throughout your body. Hemoglobin also gives your red blood cells their color. A hemoglobin test measures the amount of hemoglobin in your red blood cells.
What is the origin of the word “hematocrit”?
The term “hematocrit” (british english: haematocrit) originated from the ancient greek word haimas (= blood) and krites (= judge) and hematocrit means “to separate blood”.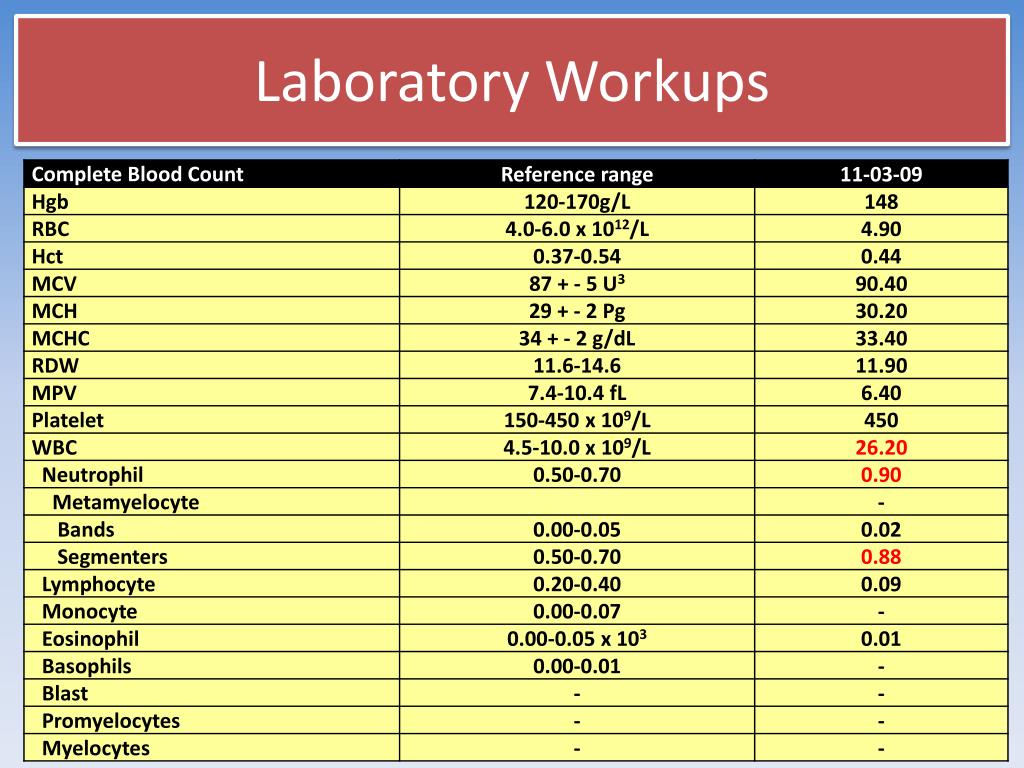
What does it mean if your Hematocrit (HCT) / Packed Cell Volume (PCV) result is too low?
Look for Possible Connected Biomarkers: Low hematocrit + low RBC count + low hemoglobin indicates anemia.
Anemia is usually defined as a decrease in red blood cells (RBCs) or hemoglobin in the blood. It can also be defined as a lowered ability of the blood to carry oxygen.
Some causes of low hematocrit include:
– Nutritional deficiencies such as iron, folate, or B12 deficiency.
– Chronic inflammatory diseases or conditions.
– Excessive loss of blood from, for example, severe trauma, or chronic bleeding from sites such as the digestive tract (e.g., ulcers, polyps, colon cancer), the bladder or uterus (in women, heavy menstrual bleeding, for example).
– Damage to the bone marrow from, for example, a toxin, radiation or chemotherapy, infection, or drugs.
– Bone marrow disorders such as aplastic anemia, myelodysplastic syndrome, or cancers such as leukemia, lymphoma, multiple myeloma, or other cancers spread to the marrow.
-Kidney failure—severe and chronic kidney diseases lead to decreased erythropoietin production, a hormone produced by the kidneys that stimulate RBC production by the bone marrow.
– Decreased production of hemoglobin (e.g., thalassemia)
– Excessive destruction of red blood cells. That is caused by autoimmunity or defects in the red blood cell itself. For example, hemolytic anemia.
What does it mean if your Hematocrit (HCT) / Packed Cell Volume (PCV) result is too high?
Look for Possible Connected Biomarkers: A high hematocrit alongside with a high RBC count and high hemoglobin indicates polycythemia.
Polycythemia (also known as polycythaemia or polyglobulia) is a disease state in which the proportion of blood volume occupied by red blood cells increases.
Some causes of a high hematocrit include:
– Dehydration—this is the most common cause of a high hematocrit. As the volume of fluid in the blood drops, the RBCs per volume of fluid artificially rises; with adequate fluid intake, the hematocrit returns to normal.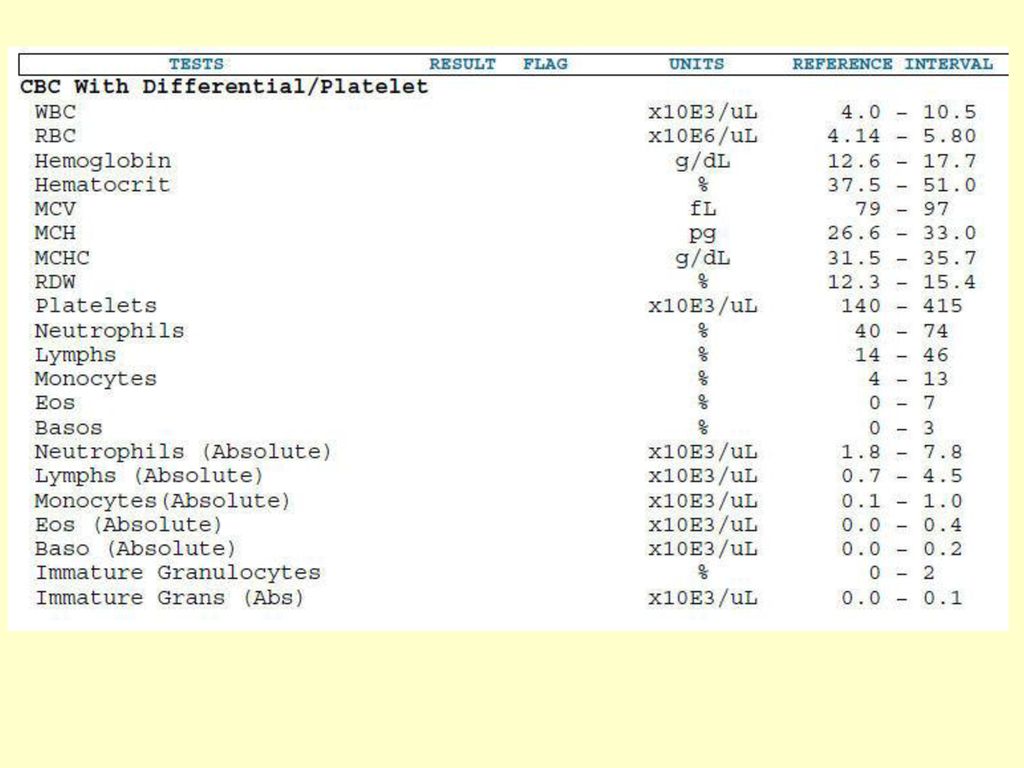
– Living at high altitudes (a compensation for decreased oxygen in the air)
– Smoking
– Lung (pulmonary) disease—if someone cannot breathe in and absorb sufficient oxygen, the body tries to compensate by producing more red blood cells.
– Congenital heart disease—in some forms, there is an abnormal connection between the two sides of the heart, leading to reduced oxygen levels in the blood. The body tries to compensate by producing more red blood cells.
– Genetic causes (altered oxygen sensing, abnormality in hemoglobin oxygen release)
– Kidney tumor that produces excess erythropoietin
– Polycythemia vera—a rare disease in which the body produces excess RBCs inappropriately.
10 000+
happy customers
100%
satisfaction
★ ★ ★ ★ ★
customer support
We implement proven measures to keep your data safe.
At HealthMatters, we’re committed to maintaining the security and confidentiality of your personal information. We’ve put industry-leading security standards in place to help protect against the loss, misuse, or alteration of the information under our control. We use procedural, physical, and electronic security methods designed to prevent unauthorized people from getting access to this information. Our internal code of conduct adds additional privacy protection. All data is backed up multiple times a day and encrypted using SSL certificates. See our Privacy Policy for more details.
We’ve put industry-leading security standards in place to help protect against the loss, misuse, or alteration of the information under our control. We use procedural, physical, and electronic security methods designed to prevent unauthorized people from getting access to this information. Our internal code of conduct adds additional privacy protection. All data is backed up multiple times a day and encrypted using SSL certificates. See our Privacy Policy for more details.
Good to know
What genetic tests should be performed in patients diagnosed with lung cancer
Views: 78
More
Anxiety, resistance, exhaustion. Medical psychologist NMIC Kristina Kondratieva talks about burnout of medical workers
Views: 94
especially in such a traumatic system for the human psyche as oncology. permanent
interaction with other people in an emergency situation
cancer, inevitably affects doctors and nurses themselves.
More
What is an immune status test and what treatment can be prescribed based on its results?
Viewings: 682
Almost all cancer patients have some kind of immunity disorders, oncoimmunologists of the N.N. N.N. Petrov based on the results of research they have been doing since 1997.
More
Why are mutations in the BRCA1 and BRCA2 genes determined? What is the best diagnostic method?
Viewings: 4126
The BRCA1 and BRCA2 genes carry information about proteins that are able to repair DNA double-strand breaks. If one of the genes is damaged by a mutation (the DNA sequence changes), then a non-functioning protein is synthesized in the cells.
More
Hormone dependent breast cancer: diagnosis and treatment
Views: 14138
The most common cancer diagnosis in women worldwide is breast cancer. Every year in Russia this disease is diagnosed in 50 thousand people.
Every year in Russia this disease is diagnosed in 50 thousand people.
More
What is cancer and how not to miss it? What is cancer and how not to miss it? N. N. Petrova.
More
Triple-negative breast cancer: features of the disease and treatment options two million people.
More
What is cytokine therapy, in what cases is it used?
Viewings: 18844
Aleksey Viktorovich Novik, oncologist, oncoimmunologist, chemotherapist, N.N. N.N. Petrova, candidate of medical sciences
More
Bacteriological examination of urine
Viewings: 4847
Microorganisms that enter the urine multiply rapidly, and an inflammatory process occurs.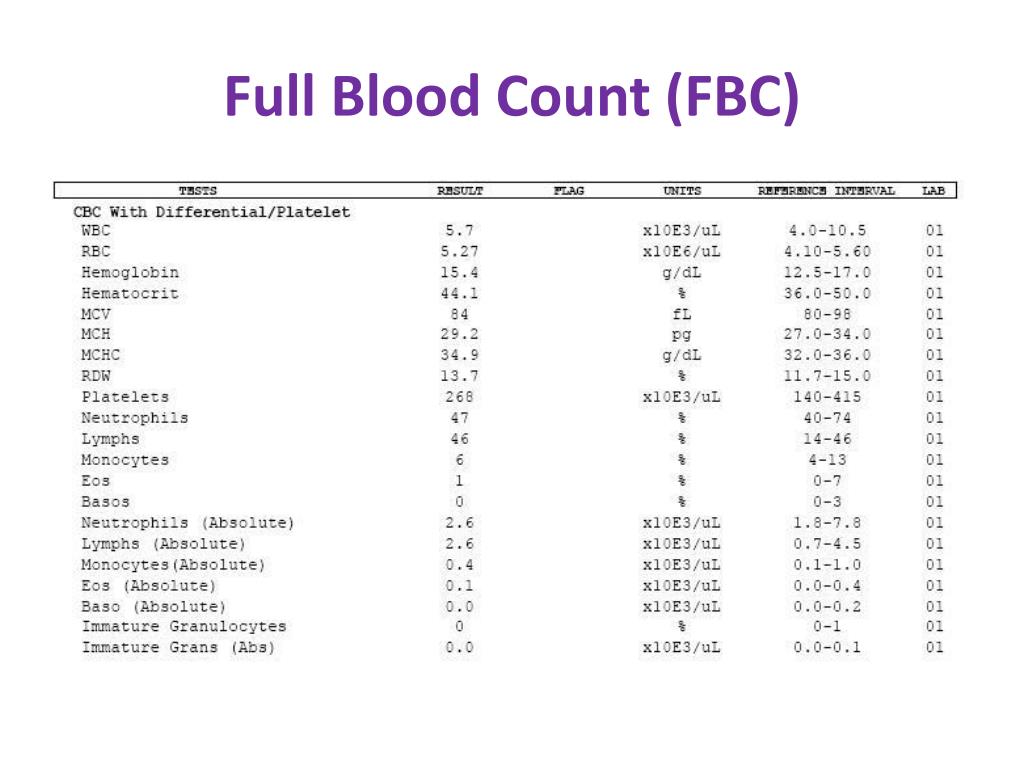 If a urinary tract infection (UTI) is suspected, to diagnose and monitor its course, as well as to evaluate the effectiveness of treatment, the patient is offered to conduct a bacteriological study of urine.
If a urinary tract infection (UTI) is suspected, to diagnose and monitor its course, as well as to evaluate the effectiveness of treatment, the patient is offered to conduct a bacteriological study of urine.
More
What does a urinalysis say?
Viewings: 59100
Urinalysis is used not only to detect pathology in the urinary system, but also to assess the state of the body as a whole, using immunological, bacteriological, molecular biological, immunochromatographic and many other research methods. Among the variety of methods, perhaps the most popular is the general analysis of urine.
More
Complications of anticancer drug treatment: skin toxicity
Views: 38734
Skin toxicity is the result of the toxic effects of drugs on rapidly dividing cells, which, in addition to tumor cells, also include cells of the skin and its appendages.
More
Skin Cancer: Prevention, Diagnosis, Treatment
Views: 256971
Skin cancer rarely occurs out of nowhere. Precancerous conditions (precursors of cancer) due to a combination of adverse factors can pathologically change, become malignant: actinic keratosis, skin horn, trophic ulcers, keratoacanthoma.
More
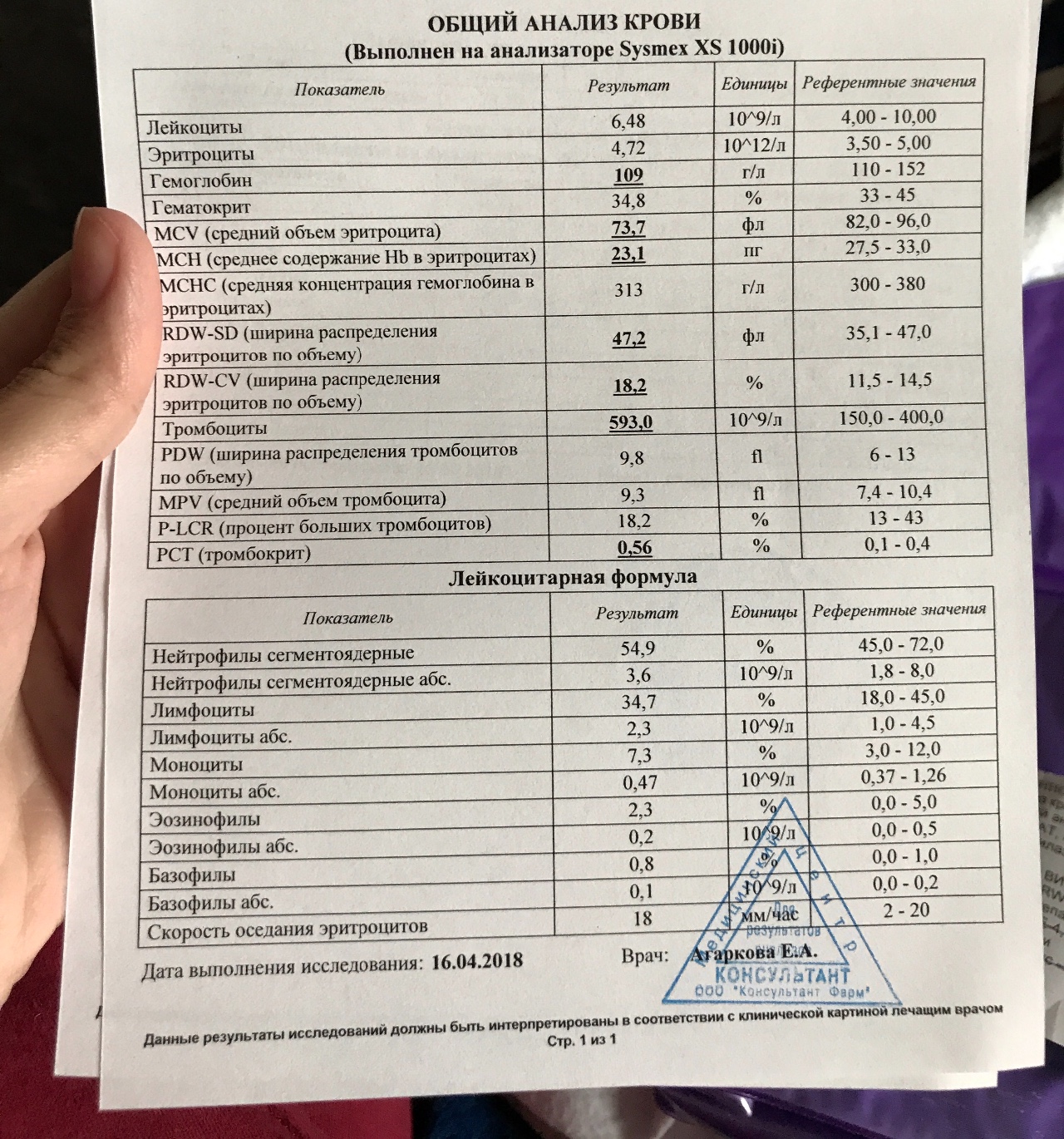
What does a general (clinical) blood test say?
Viewings: 73730
Blood tests are perhaps the most frequently performed tests. It is an integral element of any examination, both at the stage of diagnosis and during treatment. What do the indicators of the general blood test mean?
More
What does a coagulogram say?
Viewings: 19053
This test with a hard-to-pronounce name is mandatory for admission to an oncology hospital. What does the coagulogram show, what do the numerous abbreviations mean?
What does the coagulogram show, what do the numerous abbreviations mean?
More
Peculiarities of vaccination of cancer patients: recommendations for children and adults
Views: 18792
Is it possible to get vaccinated for oncology? Natalya Alexandrovna Efremova, oncologist, researcher at the Scientific Department of Oncoimmunology, N.N. N.N. Petrova, answered a number of important questions about the vaccination of cancer patients.
More
What is a tracheostomy and how can I take care of it at home? Olga Sergeevna Korneeva N.N. Petrova, spoke about the important rules for self-care for a tracheostomy and the tools and devices necessary for this.
More
Cancer at a young age: has the incidence increased?
Views: 18831
Let’s find out why this is not so, together with Anna Nikolaevna Malkova, Head of the Information Service and Department of Telemedicine Technologies of the N. N. N.N. Petrova
N. N.N. Petrova
More
Can cancer be cured?
Views: 85219
Can cancer be cured or is it a deadly disease, is it possible to get rid of the diagnosis forever?
More
Protecting a doctor from slander and insult Medical lawyer Natalya Kosolapova told how to punish an offender
Views: 4851
Professional medical activity is associated with constant communication with patients. Unfortunately, this communication does not always take place in a calm atmosphere. Often, patients show not only disrespect, but also real aggression towards the medical staff.
More
Surgical treatment of peritoneal carcinomatosis (peritoneal carcinomatosis)
Views: 31097
The modern strategy of surgical treatment of peritoneal carcinomatosis consists in surgical interventions, the purpose of which is the most complete removal of all visible manifestations of the tumor.
More
Complete blood count with ESR without leukocyte formula in Moscow
In the medical company “LabQuest” you can get a personal consultation from the doctor of the Doctor Q service on deciphering the results of a blood test without a leukocyte formula during an appointment or by phone.
It must be remembered that the interpretation of the results of a general blood test without a leukoformula should be carried out only by a doctor, since the results of laboratory tests are not the only criterion for making a diagnosis and prescribing appropriate treatment. They should be considered in conjunction with the history data and the results of other possible examinations, including instrumental diagnostic methods.
ESR is a non-specific indicator of the inflammatory process. The level of ESR depends on physiological and pathological factors. It increases with inflammatory processes, intoxications, tumors, infections (acute and chronic), paraproteinemia, hepatitis, amyloidosis, tuberculosis, etc. The level of ESR decreases with an increase in the number of red blood cells (erythremia, erythrocytosis).
The level of ESR decreases with an increase in the number of red blood cells (erythremia, erythrocytosis).
Red blood cells (RBCs) are red blood cells that contain the protein hemoglobin. The average lifespan of erythrocytes is 110-130 days. The main function of red blood cells is to carry oxygen from the lungs to other organs and tissues. An increase in the number of red blood cells (erythrocytosis) occurs with tissue hypoxia, polycystic kidney disease, renal artery stenosis, hydronephrosis, tumors, etc. A decrease in the number of red blood cells (erythrocytopenia) occurs after blood loss, with anemia, after radiation exposure, with increased breakdown of red blood cells, with diseases of the kidneys and liver, against the background of infectious diseases.
Hemoglobin (Hb) increases with dehydration, with an increase in the number of red blood cells. The concentration of hemoglobin decreases with anemia and with hyperhydration.
Hematocrit (HCT) is an indicator that is determined by calculating the ratio of the volume of erythrocytes to the volume of the liquid part of the blood. Hematocrit increases with an increase in the number of red blood cells, with burn disease and dehydration of the body. HCT decreases with anemia, overhydration, pregnancy.
Hematocrit increases with an increase in the number of red blood cells, with burn disease and dehydration of the body. HCT decreases with anemia, overhydration, pregnancy.
Mean cell volume (MCV) is a measure of the average volume of the entire population of red blood cells. According to this indicator, the doctor determines the type of anemia (normocytic, microcytic and macrocytic). A decrease in MCV is more common in iron deficiency anemia, and an increase in B12 deficiency anemia or folate deficiency anemia.
Mean erythrocyte hemoglobin (MCH) is an indicator of the average content of hemoglobin protein in 1 erythrocyte. Analogue of the obsolete color index (CPU). According to this indicator, the doctor divides anemia into normochromic, hypochromic and hyperchromic. MCH decreases with iron deficiency anemia, porphyria, and increases with macrocytic anemia.
Average concentration of hemoglobin in erythrocytes (MCHC) – the indicator reflects the saturation of erythrocytes with hemoglobin. MCHC increases with spherocytosis, cold agglutination of erythrocytes, after chemotherapy, decreases with hemoglobinopathies, anemia of chronic disease, iron deficiency anemia.
MCHC increases with spherocytosis, cold agglutination of erythrocytes, after chemotherapy, decreases with hemoglobinopathies, anemia of chronic disease, iron deficiency anemia.
Distribution of erythrocytes by volume (RDW CV) – the indicator reflects the degree of anisocytosis of erythrocytes (change in the size of an erythrocyte). An increase in RDW occurs with a combination of red blood cells of different sizes (for example, normocytes and microcytes).
Platelets (PLT) are nuclear-free small blood cells that are involved in the formation of blood clots in normal conditions (in case of damage to the vessel) and in pathology (when an atherosclerotic plaque is “opened”). The number of platelets increases with increased physical exertion, after surgical interventions, against the background of oncological diseases, in acute and chronic inflammatory processes in the body. A decrease in the number of platelets occurs with bacterial and viral infections, pregnancy, enlarged spleen, autoimmune diseases, etc.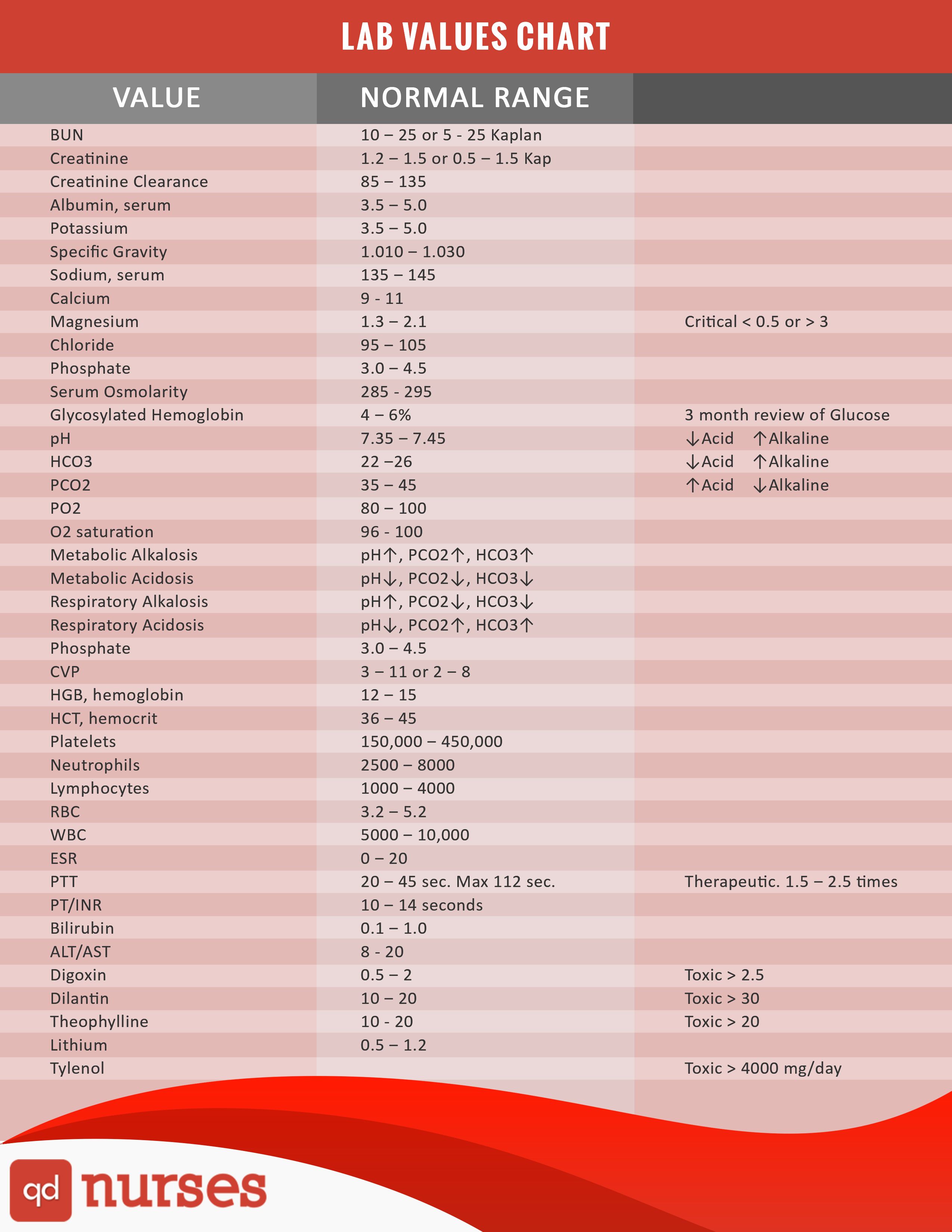
Mean platelet volume (MPV) is a measure of the average volume of the entire population of platelets. An increase in MPV is observed in patients with idiopathic thrombocytopenic purpura, hyperthyroidism, diabetes mellitus, smokers, and alcohol abuse. The indicator decreases after removal of the spleen, with ulcerative colitis and Crohn’s disease.
Leukocytes (WBC) are blood cells that are part of cellular immunity. The main function is to attack pathogenic microorganisms (bacteria, viruses, fungi) that have entered the body and remove the remains of cells after their destruction. Leukocytes include neutrophils, eosinophils, lymphocytes, monocytes, and basophils. An increase in leukocytes occurs normally after exercise, physiotherapy, against the background of pain of a different nature (for example, with a headache), after eating, emotional stress, exposure to cold and heat. The increase in leukocytes in these conditions is temporary and is called physiological (redistributive) leukocytosis.

 [PMC free article: PMC1995040] [PubMed: 17948084]
[PMC free article: PMC1995040] [PubMed: 17948084] Etiology of differences in hematocrit between males and females: sequence-based polymorphisms in erythropoietin and its receptor. J Gend Specif Med. 2001;4(1):35-40. [PubMed: 11324238]
Etiology of differences in hematocrit between males and females: sequence-based polymorphisms in erythropoietin and its receptor. J Gend Specif Med. 2001;4(1):35-40. [PubMed: 11324238]