Yeast infections after novasure procedure. NovaSure Endometrial Ablation: A Comprehensive Guide to the Procedure and Recovery
What is NovaSure endometrial ablation. How does the NovaSure procedure work. What are the benefits of NovaSure for heavy menstrual bleeding. Who is a good candidate for NovaSure ablation. What can patients expect during and after the procedure. Are there any risks or side effects associated with NovaSure. How effective is NovaSure at reducing menstrual bleeding.
Understanding NovaSure Endometrial Ablation
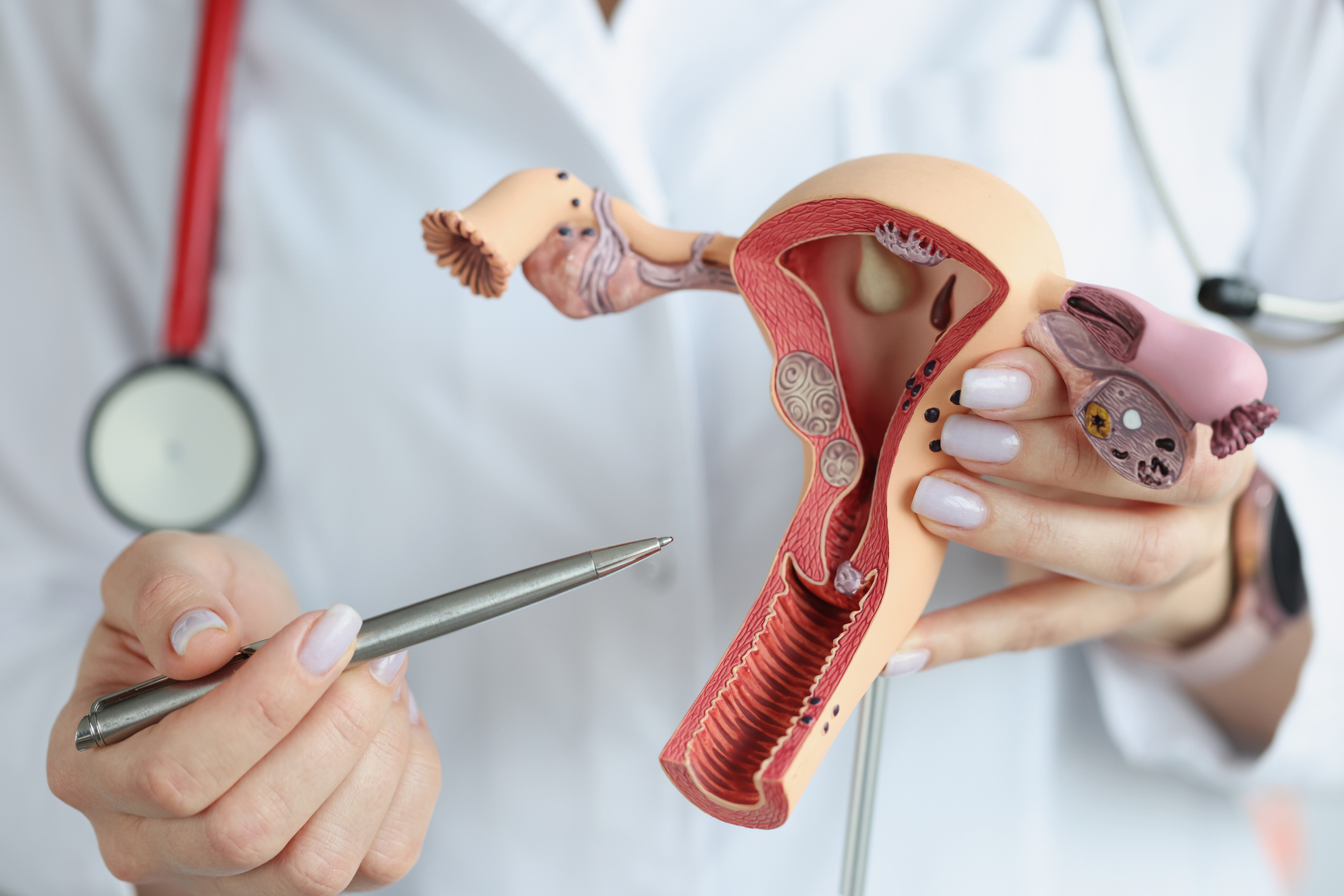
NovaSure endometrial ablation is an innovative gynecological procedure designed to treat heavy menstrual bleeding in women. This minimally invasive technique offers a safe and effective alternative to hysterectomy for many patients struggling with menorrhagia. But what exactly does the NovaSure procedure entail?
NovaSure works by removing the endometrial lining of the uterus using controlled radiofrequency energy. The procedure typically takes less than 5 minutes and can be performed in an outpatient setting. By ablating the uterine lining, NovaSure aims to significantly reduce or eliminate heavy menstrual flow in women who have completed childbearing.

How Does NovaSure Work?
During the NovaSure procedure, a slender wand is inserted through the cervix into the uterus. This wand contains a triangular mesh device that expands to fit the unique shape of each patient’s uterine cavity. Once in place, precisely measured radiofrequency energy is delivered through the mesh for about 90 seconds. This energy gently removes the endometrial lining responsible for monthly menstrual bleeding.
Benefits of NovaSure for Heavy Menstrual Bleeding
NovaSure offers several advantages for women seeking relief from heavy periods:
- Quick procedure time (average of 5 minutes or less)
- No incisions required
- Can be performed in-office without general anesthesia
- Rapid recovery with most women returning to normal activities within a day
- High success rates in reducing or eliminating menstrual bleeding
- Avoids the need for hysterectomy in many cases
- No hormones required
Is NovaSure effective at reducing menstrual bleeding? Clinical studies have shown that over 90% of women treated with NovaSure experienced a significant reduction in menstrual blood loss. Many patients report much lighter periods or even complete cessation of menstrual bleeding following the procedure.

Ideal Candidates for NovaSure Ablation
While NovaSure can be an excellent option for many women, it’s not suitable for everyone. Good candidates for the procedure typically include:
- Women who have completed childbearing
- Those experiencing heavy menstrual bleeding not caused by cancer, pregnancy, or infection
- Women who want to avoid hysterectomy
- Patients who have not responded well to other treatments like hormone therapy or IUDs
Are there any contraindications for NovaSure? The procedure is not recommended for women who are pregnant, wish to become pregnant in the future, have active genital or urinary tract infections, or have been diagnosed with endometrial cancer. A thorough evaluation by a gynecologist is essential to determine if NovaSure is the right choice for each individual patient.
The NovaSure Procedure: What to Expect
Understanding the NovaSure process can help patients feel more comfortable and prepared. Here’s a general overview of what to expect:
- Pre-procedure preparation: Your doctor may perform an endometrial biopsy and check for any anatomical issues.
- The procedure: You’ll be positioned on an exam table with your feet in stirrups. A speculum is inserted to open the vaginal canal.
- Cervical dilation: The cervix is gently opened to allow insertion of the NovaSure device.
- Device placement: The wand is carefully inserted through the cervix into the uterus.
- Energy delivery: Radiofrequency energy is applied for about 90 seconds to remove the endometrial lining.
- Completion: The device is removed, and the procedure is complete.
How long does the NovaSure procedure take? From start to finish, most NovaSure treatments are completed in less than 5 minutes. However, the total time in the office may be longer due to preparation and recovery.

Recovery and Post-Procedure Care
One of the significant advantages of NovaSure is its quick recovery time. Most women can return to normal activities within a day or two after the procedure. However, it’s essential to follow your doctor’s post-operative instructions carefully.
Common Post-Procedure Experiences:
- Cramping: Mild to moderate cramping for a few days is normal and can be managed with over-the-counter pain relievers.
- Discharge: A watery or bloody discharge may occur for several weeks. This is part of the healing process.
- Fatigue: Some women may feel tired for a day or two following the procedure.
When can patients resume normal activities after NovaSure? While individual experiences may vary, many women feel well enough to return to work and light activities within 24-48 hours. Strenuous exercise and sexual intercourse should typically be avoided for about two weeks or as advised by your healthcare provider.
Potential Risks and Side Effects of NovaSure
While NovaSure is generally considered safe, as with any medical procedure, there are potential risks and side effects to be aware of:
- Infection: Although rare, there is a small risk of uterine infection.
- Thermal injury: In very rare cases, the heat used during the procedure could damage nearby organs.
- Continued bleeding: Some women may still experience some level of menstrual bleeding after the procedure.
- Regrowth of endometrial tissue: In some cases, the endometrial lining may partially grow back over time.
Can NovaSure cause serious complications? Serious complications from NovaSure are extremely rare. However, it’s crucial to discuss all potential risks with your healthcare provider before deciding to undergo the procedure.
Long-Term Outcomes and Effectiveness
NovaSure has demonstrated impressive long-term success rates in clinical studies. Many women report significant improvements in their quality of life following the procedure.
Key Effectiveness Statistics:
- Over 90% of women experience a substantial reduction in menstrual bleeding
- Approximately 40-50% of patients report complete cessation of menstrual periods
- 97% of women say they would recommend NovaSure to a friend
- Patient satisfaction rates exceed 90% in most studies
How long do the effects of NovaSure last? The results of NovaSure are intended to be permanent. However, in a small percentage of cases, some women may experience a return of heavy bleeding over time and may require additional treatment.

NovaSure vs. Other Treatment Options
When considering treatment for heavy menstrual bleeding, it’s important to understand how NovaSure compares to other available options:
NovaSure vs. Hormonal Treatments:
Unlike birth control pills or hormonal IUDs, NovaSure doesn’t rely on hormones to control bleeding. This can be advantageous for women who experience side effects from hormonal treatments or prefer to avoid them.
NovaSure vs. Hysterectomy:
NovaSure offers a less invasive alternative to hysterectomy, with a much quicker recovery time and no need for hospitalization. However, hysterectomy may still be the best option for some patients, particularly those with certain medical conditions.
NovaSure vs. Other Endometrial Ablation Techniques:
Compared to older ablation methods, NovaSure typically offers a faster procedure time, more consistent results, and a lower risk of complications.
Which treatment option is best for heavy menstrual bleeding? The optimal treatment depends on various factors, including the underlying cause of the bleeding, the patient’s age, overall health, and future pregnancy plans. A thorough discussion with a gynecologist is crucial to determine the most appropriate approach for each individual.

Preparing for NovaSure: What Patients Should Know
If you’re considering NovaSure, proper preparation can help ensure the best possible outcome. Here are some key points to keep in mind:
Before the Procedure:
- Undergo a thorough medical evaluation, including a Pap smear and endometrial biopsy
- Discuss all medications and supplements you’re taking with your doctor
- Follow any pre-procedure instructions, such as fasting or adjusting medications
- Arrange for someone to drive you home after the procedure
Questions to Ask Your Doctor:
- Am I a good candidate for NovaSure?
- What are my other treatment options?
- What kind of results can I expect?
- What are the potential risks and complications?
- How should I prepare for the procedure?
- What will recovery be like?
How can patients best prepare for NovaSure? Open communication with your healthcare provider is key. Don’t hesitate to ask questions or express any concerns you may have about the procedure or recovery process.
Addressing Common Concerns About NovaSure
Many women have questions and concerns about NovaSure. Let’s address some of the most common ones:

Pain During the Procedure:
While some discomfort is normal, most women report only mild to moderate cramping during NovaSure. Local anesthesia or mild sedation can be used to ensure comfort.
Effect on Future Pregnancies:
NovaSure is not recommended for women who may want to become pregnant in the future. The procedure significantly reduces the likelihood of successful pregnancy and increases the risk of complications.
Impact on Hormones:
NovaSure does not affect hormone production or trigger early menopause. The ovaries continue to function normally after the procedure.
Insurance Coverage:
Many insurance plans cover NovaSure when medically necessary. However, coverage can vary, so it’s important to check with your insurance provider.
Does NovaSure affect sexual function or enjoyment? Most women report no negative impact on sexual function or satisfaction following NovaSure. In fact, many experience improved sexual quality of life due to reduced bleeding and related symptoms.
Life After NovaSure: What to Expect
Understanding what life might be like after NovaSure can help set realistic expectations:
Changes in Menstrual Bleeding:
Most women experience significantly lighter periods or no periods at all after NovaSure. It may take a few months for your bleeding pattern to stabilize.
Premenstrual Symptoms:
Some women report a reduction in premenstrual symptoms like cramping and mood swings, though this can vary.
Long-term Monitoring:
Regular gynecological check-ups remain important after NovaSure to monitor your overall reproductive health.
Potential for Additional Treatments:
While NovaSure is highly effective for most women, a small percentage may require additional treatments in the future if heavy bleeding returns.
How does NovaSure impact overall quality of life? Many women report significant improvements in their daily lives, including increased energy, better sleep, and fewer restrictions on activities due to heavy bleeding.
In conclusion, NovaSure endometrial ablation offers a promising solution for women struggling with heavy menstrual bleeding. Its minimally invasive nature, quick procedure time, and high success rates make it an attractive option for many patients. However, as with any medical procedure, it’s crucial to have a thorough discussion with a healthcare provider to determine if NovaSure is the right choice for your individual situation. By understanding the procedure, its benefits, and potential risks, women can make informed decisions about their reproductive health and take steps towards improving their quality of life.

Gynecological Conditions & Treatments Archives – Page 4 of 5 – PBGS
pbgsAdmin On July 2, 2015
/ Early Pregnancy, Gynecological Conditions & Treatments, Pregnancy / Leave a comment
Vaginal Candidiasis: Causes, Symptoms and Treatment
Vaginal candidiasis is an extremely common fungal yeast infection of the vagina. This condition is also referred to as vaginal thrush, candidal vulvovaginitis, and vaginal yeast infection. These infections are named after the Candida albicans fungus, as that’s what causes them. Normally, the Candida yeast or fungi are a part of the usual vaginal flora just like the healthy lactobacilli. However, the lactobacilli help keep the Candida in very small numbers to maintain a healthy pH and environment in the vagina. The problem arises when this balance tips towards the Candida and they grow in abnormally high numbers, thus resulting in the vaginal irritation, itching, and odorless discharge, classic signs of a vaginal yeast infection.
The problem arises when this balance tips towards the Candida and they grow in abnormally high numbers, thus resulting in the vaginal irritation, itching, and odorless discharge, classic signs of a vaginal yeast infection.
This is one of the most common and frequent vaginal infections in women. As many as 20% of the women experience a vaginal yeast infection every year and around 5% are affected by this infection at least thrice in a year, while a significant 75% are likely to experience it at least once in their lifetime. Most women experience a worsening in their symptoms or a new vaginal thrush infection around their periods.
Causes of Vagina Candidiasis
Vaginal yeast infections are a direct outcome of excessive colonization or growths of Candida albicans. However, the actual causes or factors that result in an increased growth of this fungus are yet unknown. Even so, several risk factors likely to help Candida thrive in the vagina to attain abnormal levels have been acknowledged.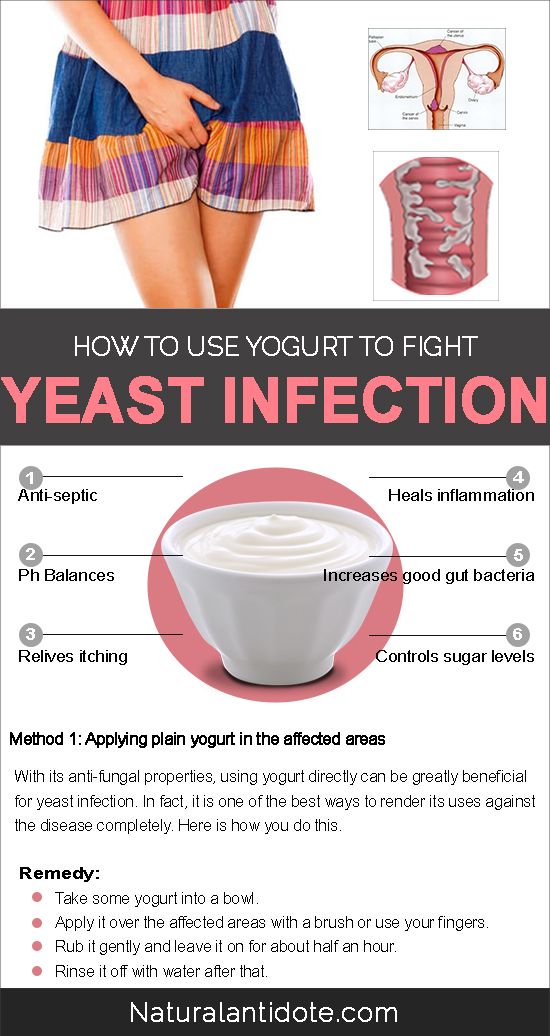 Taking note of these factors is also important in the prevention of recurrent vaginal yeast infections in women who are susceptible to them.
Taking note of these factors is also important in the prevention of recurrent vaginal yeast infections in women who are susceptible to them.
* Medications:
Antibiotics and particularly broad-spectrum antibiotics destroy the good bacteria or the lactobacilli subsequently causing the Candida to thrive. Hence, a course of antibiotics is very likely to result in a vaginal yeast infection. In fact, nearly 30% of the women, who undergo treatment with oral antibiotics, end up with this infection.
* Pregnancy:
Pregnant women are usually at an increased risk of developing vaginal candidiasis, mainly because of increased estrogen levels. This hormone allows the Candida to flourish leading to frequent vaginal yeast infections in pregnancy.
* Underlying diseases:
Diabetes Mellitus and conditions like HIV/AIDS and chemotherapy that may result in a compromised immunity often result in frequent vaginal yeast infections too. Poor sugar control among diabetics is a common risk factor for frequent candidial infections. As for the conditions that result in a compromised immunity, the frequent vaginal yeast infections mainly arise because the body isn’t capable to fight the infections thanks to a poor immune system.
As for the conditions that result in a compromised immunity, the frequent vaginal yeast infections mainly arise because the body isn’t capable to fight the infections thanks to a poor immune system.
Symptoms of Vaginal Candidiasis
The symptoms of vaginal candidiasis are characterized by itching in and around the genitals. This is the most common and most frustrating of its symptoms. However, a woman may also experience one or more of the following symptoms when affected by a vaginal yeast infection.
* Vulval and vaginal itching
* Soreness and irritation of the vulva
* Painful urination
* Pain during intercourse
* Translucent or white discharge that is generally odorless. The discharge sometimes also appears thick and lumpy like curd or cottage cheese
* Very rarely, severe vaginal thrush infections may also cause swelling or edema of the vulva with severe redness and cracked skin
How is Vaginal Candidiasis Treated?
The treatment regimen for vaginal candidiasis is quite straightforward. It mainly involves topical or local application of anti-fungal ointments sometimes coupled with oral administration of anti-fungal medications. Genreally, treatment with azoles topically is much more successful than using nystatin for this purpose. Butoconazole, miconazole, clotrimazole, tioconazole, and terconazole are some of the azoles that are frequently found in the topical suppositories, creams, and ointments used to treat vaginal candidiasis. A single dose of flucanazole taken orally along with the local applications is often used successfully to get rid of these infections too.
It mainly involves topical or local application of anti-fungal ointments sometimes coupled with oral administration of anti-fungal medications. Genreally, treatment with azoles topically is much more successful than using nystatin for this purpose. Butoconazole, miconazole, clotrimazole, tioconazole, and terconazole are some of the azoles that are frequently found in the topical suppositories, creams, and ointments used to treat vaginal candidiasis. A single dose of flucanazole taken orally along with the local applications is often used successfully to get rid of these infections too.
Back to Top
pbgsAdmin On June 24, 2015
/ Gynecological Conditions & Treatments / Leave a comment
NovaSure Endometrial Ablation Procedure | PBGS
NovaSure endometrial ablation is a one time, simple and very safe gynecological procedure that consists of removing the endometrium (the inner lining of the uterus).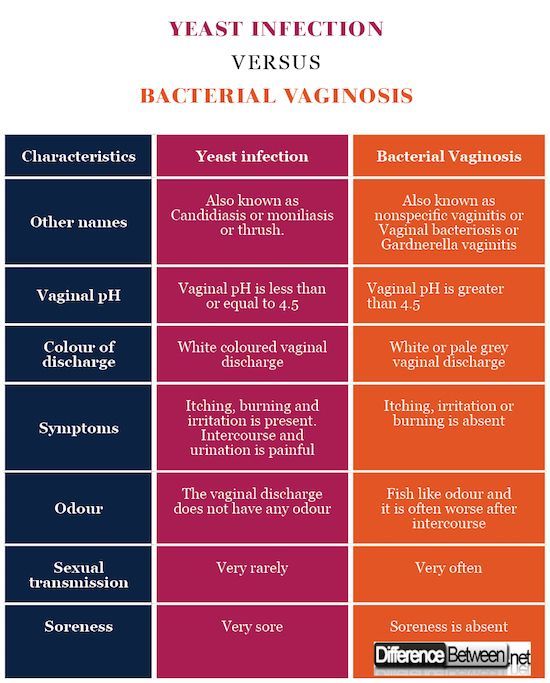 It is usually done under local or spinal anesthesia.
It is usually done under local or spinal anesthesia.
NovaSure is recommended to evaluate and treat painful periods and heavy or irregular menstrual bleeding with every menstrual cycle.
Who Is NovaSure Endometrial Ablation Recommended For?
Endometrial ablation is recommended for woman who have:
- Painful and heavy periods every month,
- Anemia due to excessive loss of blood with menstrual periods
- The need for hysterectomy but for some reason this is contraindicated
- The need to prevent the uterus.
How Is NovaSure Endometrial Ablation Performed?
NovaSure endometrial ablation has been proved to be very successful. In 90% of the cases the menstrual flow has been reduced or totally stopped. The procedure consists in destroying the inner lining of the uterus by delivering radiofrequency energy, for a couple of seconds. First your doctor will open the cervix of the uterus, insert a slender wand and extend a triangular mesh device inside of the uterus. This mesh device will gently expand and fit the size of your uterus. Through this mesh radio frequent energy is delivered into the uterus, for about 90 seconds. After the procedure is completed, the mesh device is pulled back into the wand and removed from the uterus.
This mesh device will gently expand and fit the size of your uterus. Through this mesh radio frequent energy is delivered into the uterus, for about 90 seconds. After the procedure is completed, the mesh device is pulled back into the wand and removed from the uterus.
Possible Side Effects
Even though NovaSure endometrial ablation is a safe procedure, effects and complications are possible.
Possible side effects of NovaSure endometrial ablation include:
- Abdominal cramping
- Mild to moderate pain – You may have menstrual-like cramps for a few days. Over-the-counter medications such as ibuprofen or acetaminophen can help relieve cramping after the procedure.
- Nausea
- Vomiting
- Frequent urination – You may need to pass urine more often during the first 24 hours after endometrial ablation.
- Vaginal discharge – A watery discharge, mixed with blood, may occur for a few weeks. The discharge is typically heaviest for the first few days after the procedure.

- Spotting, etc.
Complications of NovaSure Endometrial Ablation
Complications of NovaSure endometrial ablation are very rare, but when they occur they are very severe and life-threatening. Possible complications of the NovaSure endometrial ablation include:
- Accidental perforation of the uterus
- Thermal injuries of the uterus and bowel
- Cervical laceration (tearing of the cervix-opening of the uterus)
- Pulmonary embolism
- Pulmonary edema
When Is This Procedure Contraindicated?
Keep in mind that NovaSure endometrial ablation should be considered only in cases when no future pregnancies are desired. If you and your partner want to have children in the future, NovaSure endometrial ablation is not recommended. However, pregnancies are still possible, even after NovaSure endometrial ablation. In these cases, when a pregnancy occurs after endometrial ablation, there are greater risks for the baby and even for the mother. Since the uterine lining would not be able to properly support the development of the fetus, a pregnancy after NovaSure endometrial ablation will be dangerous. It will likely end in miscarriage.
Since the uterine lining would not be able to properly support the development of the fetus, a pregnancy after NovaSure endometrial ablation will be dangerous. It will likely end in miscarriage.
NovaSure endometrial ablation is also contraindicated in cases when a woman has just recently gave birth, cervical or endometrial cancer, active genital, urinary or pelvic infection or an IUD, after menopause, etc.
Keep in mind that NovaSure endometrial ablation is not a sterilization procedure. Contraception is still needed for woman who have not passed menopause.
You may also need to avoid sexual intercourse for a period of time after the procedure.
Back to Top
pbgsAdmin On June 17, 2015
/ Gynecological Conditions & Treatments / Leave a comment
Cervical Dysplasia | HPV | What You Need to Know
Cervical dysplasia is a disorder that affects the cervix, which is the lower end or opening of the uterus. A set of abnormal alterations in the cells of the cervix mark cervical dysplasia. Although, this isn’t really cancer it is considered as a precancerous stage, since the cellular abnormalities in cervical dysplasia are likely to transform into cervical cancer if left untreated. This abnormal or dysplastic appearance of the cervical cells under the microscope is what gives the disorder its name. The level of abnormalities or changes in the cervical cells observed in the cervical tissue biopsies or smears under the microscope are used as a benchmark to grade the severity and extent of this condition.
A set of abnormal alterations in the cells of the cervix mark cervical dysplasia. Although, this isn’t really cancer it is considered as a precancerous stage, since the cellular abnormalities in cervical dysplasia are likely to transform into cervical cancer if left untreated. This abnormal or dysplastic appearance of the cervical cells under the microscope is what gives the disorder its name. The level of abnormalities or changes in the cervical cells observed in the cervical tissue biopsies or smears under the microscope are used as a benchmark to grade the severity and extent of this condition.
Generally, this disorder is likely to go unnoticed due to its asymptomatic nature, unless one comes across the cellular changes on a routine examination. However, it’s equally important to detect cervical dysplasia in its initial stages to prevent it from turning into cancer. Hence, educating yourself about this precancerous condition is your best bet against it.
What Causes Cervical Dysplasia?
Women between 25 to 35 years of age are most likely to suffer from cervical dysplasia, although it may occur at any age. Certain factors like indulging in sexual intercourse before 18 years of age, giving birth before a woman turns sixteen, multiple sexual partners, smoking, and use of immunity suppressing medications may greatly increase a woman’s risk of developing cervical dysplasia. Another common cause of cervical dysplasia is the HPV or Human Papilloma Virus. This virus generally affects the female genitals and is transmitted through sexual contact. Usually, HPV infections last anywhere between 8 to 13 months and may also recur. However, these infections are silent and asymptomatic just like cervical dysplasia. Thus, avoiding risk factors like multiple sex partners and frequent unprotected or unsafe sexual practices is important to avoid these infections and subsequent cervical dysplasia. Getting yourself vaccinated with the HPV vaccination is also recommended to reduce your risk of cervical dysplasia and cervical cancer.
Certain factors like indulging in sexual intercourse before 18 years of age, giving birth before a woman turns sixteen, multiple sexual partners, smoking, and use of immunity suppressing medications may greatly increase a woman’s risk of developing cervical dysplasia. Another common cause of cervical dysplasia is the HPV or Human Papilloma Virus. This virus generally affects the female genitals and is transmitted through sexual contact. Usually, HPV infections last anywhere between 8 to 13 months and may also recur. However, these infections are silent and asymptomatic just like cervical dysplasia. Thus, avoiding risk factors like multiple sex partners and frequent unprotected or unsafe sexual practices is important to avoid these infections and subsequent cervical dysplasia. Getting yourself vaccinated with the HPV vaccination is also recommended to reduce your risk of cervical dysplasia and cervical cancer.
How Do You Know If You Have Cervical Dysplasia?
Unlike most other disorders of the female reproductive tract, cervical dysplasia rarely produces any symptoms. So, most womenaren’t even aware about this unseen tripwire within their uterus, until they come across it during a routine pap smear. Hence, regular gynecological evaluations and pap smears are important to help detect cervical dysplasia. However, a pap smear alone does not help diagnose this condition. Abnormal changes indicating cervical dysplasia on a pap smear are further verified with a cervical biopsy to confirm the diagnosis.
So, most womenaren’t even aware about this unseen tripwire within their uterus, until they come across it during a routine pap smear. Hence, regular gynecological evaluations and pap smears are important to help detect cervical dysplasia. However, a pap smear alone does not help diagnose this condition. Abnormal changes indicating cervical dysplasia on a pap smear are further verified with a cervical biopsy to confirm the diagnosis.
How Is Cervical Dysplasia Treated?
- The treatment of cervical dysplasia is largely dependent on the severity of the cellular abnormalities or the grade of dysplasia. Mild cervical dysplasia sometimes disappears without any treatment and with careful 6 monthly pap smears alone. The pap smears essentially monitor the changes to make sure the condition isn’t worsening, in which case treatment is mandatory. Cervical dysplasia is treated surgically with cryosurgery to freeze the dysplastic cells, or Loop electrosurgical excision procedure (LEEP) to remove the abnormal cells with electrical stimuli, or cone biopsy to surgically excise the abnormal tissue area, or laser therapy to burn the dysplastic cells.
 Some extreme or severe cases of cervical dysplasia may also require hysterectomy, wherein the entire uterus is removed surgically. Your doctor is likely to decide the best course of treatment depending on the grade and severity of your cervical dysplasia.
Some extreme or severe cases of cervical dysplasia may also require hysterectomy, wherein the entire uterus is removed surgically. Your doctor is likely to decide the best course of treatment depending on the grade and severity of your cervical dysplasia.
Back to Top
Page 4 of 5«12345»
What to Expect After an Endometrial Ablation
Women with extremely heavy periods (who soak through a pad every two hours) have been turning to endometrial ablation to combat their most intense symptoms. During your period, your body sheds endometrium, or the lining of the uterus, and this procedure … Read More
By CMG-Atlanta — September 22, 2020
Share This Article
Women with extremely heavy periods (who soak through a pad every two hours) have been turning to endometrial ablation to combat their most intense symptoms. During your period, your body sheds endometrium, or the lining of the uterus, and this procedure destroys (or ablates) that endometrium. While this surgery is not for everyone, such as people who have been recently pregnant or hope to get pregnant, the women who get this procedure experience relief from their severe period symptoms.
While this surgery is not for everyone, such as people who have been recently pregnant or hope to get pregnant, the women who get this procedure experience relief from their severe period symptoms.
If you have usually heavy periods across many days and are looking into this as a possible solution, you may be asking yourself, “What can I expect after an endometrial ablation?” This FAQ can help point out the different symptoms and experiences of women who have this common procedure.
Is bleeding after endometrial ablation normal?
Yes, vaginal bleeding for a few days is a normal part of endometrial ablation recovery. You will likely want to wear pads; do not use tampons, douche or have sex in the first few days to the first week. Persistent bleeding, though, may be a concern and may require a pelvic exam as well as a conversation with your doctor about next steps, which may lead to a future hysterectomy.
Will periods go away forever after the surgery?
Most women (9 out of 10) will either have no periods or lighter periods after endometrial ablation. It is possible that your period will come back heavier after a few years.
It is possible that your period will come back heavier after a few years.
Is it normal to experience discharge after ablation?
It’s normal to experience a thin, watery discharge after ablation. The discharge may also be bloody or mixed with blood. It will likely be heavy for the first few days after your surgery. Any endometrial ablation discharge should stop after, at the latest, a few months. If your discharge changes in color or smell, call your doctor right away.
Can you have kids after endometrial ablation?
Pregnancy after an endometrial ablation is unlikely, but possible, which is potentially dangerous. If pregnancy does happen after ablation, serious and sometimes deadly complications can occur. This type of surgery is not an alternative to a hysterectomy or sterilization surgery, so talk to your doctor if that is one of your needs. Women should still use forms of birth control after uterine ablation, as pregnancy remains possible until after menopause.
Is back pain after endometrial ablation normal?
Largely, back pain is not normal, though some abdominal cramping immediately following the surgery is to be expected. In rare cases, some women develop cyclic pelvic pain (CPP) after the procedure, which can last for months or even years. This may be a potential indication of late-onset endometrial ablation failure. If you experience back pain after the surgery, call your doctor.
Which symptoms are a cause for concern?
These are warning signs of infections or complications after your endometrial ablation:
- A fever
- Increased pain and swelling after a few days
- Trouble passing gas and/or stool
- Being sick to your stomach
- Trouble drinking fluids
- Trouble urinating
- A change in the vaginal discharge in color or smell
- An increase in bleeding for longer than two days after the procedure
- Large clots in the vaginal discharge
- Signs of a blood clot in your leg (such as pain or swelling in the leg)
- Persistent abdominal pain after the normal cramping
If you are experiencing any other unusual symptoms, please contact your doctor.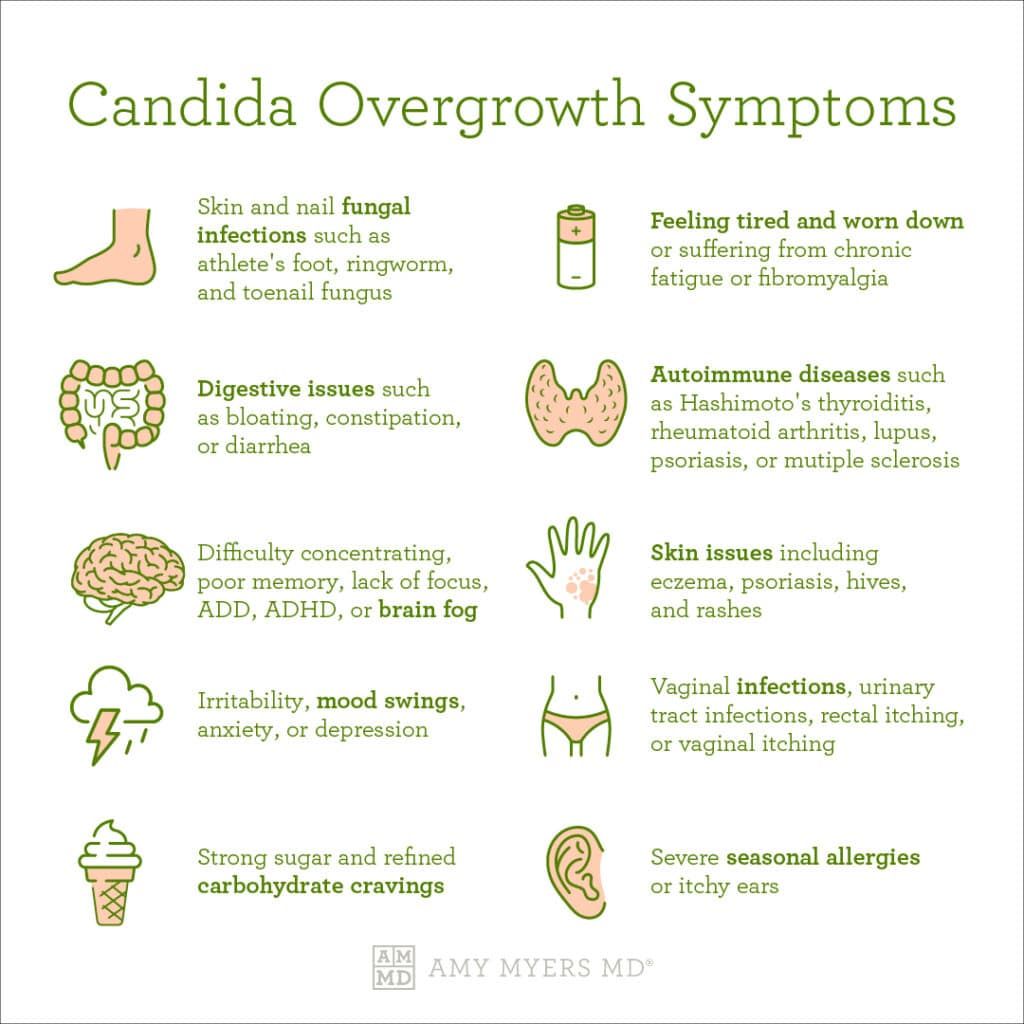
What are some other long-term side effects of having an endometrial ablation?
Immediately after surgery, women should expect cramps, some vaginal discharge and frequent urination. In the follow-up after endometrial ablation, excessive bleeding, holes in the uterus, impacts on other organs and discharge should be watched carefully. Long-term risk factors often depend on the type of surgery you’re having (whether it’s electrosurgery, microwaves, a heated balloon or other method removing the lining), but some of the less common risk factors include hematometra, which is the retention of blood in the uterine cavity caused by obstructed menstrual flow, post-ablation tubal sterilization syndrome and delays in finding and diagnosing endometrial cancer. Talk to your doctor about the details of your specific procedure for endometrial ablation. Sexually active individuals should keep in mind that pregnancy is possible but unsafe after an ablation.
If you want to know if you’re right for this surgery or more about the potential long-term symptoms, call us at (678) 253-2179 or schedule with us online.
Chemotherapy Thrush – Biovestin
A vaginal yeast infection called Candida Albicans or colloquially called thrush can cause discomfort. Vaginal yeast infections are very common. Symptoms include:
- Itching and burning in the vagina. The mucous membranes and skin are red and inflamed.
- Thick white curdled discharge. However, in some women, thrush can occur without such symptoms.
- Pain or discomfort during intercourse.
What causes a vaginal yeast infection?
Yeast fungi like to live in warm, humid environments. Yeast cannot reproduce due to the acidic environment in the vagina. As soon as the acid balance of the vagina changes (the acid balance becomes too low), the yeast begins to grow and flourish. Too low acid balance can cause:
- pregnancy;
- often thrush occurs after the menstrual cycle;
- diabetes mellitus;
- steroid preparations;
- preparations used during chemotherapy;
- Vaginal irritation can also lead to yeast growth.

Chemotherapy takes a heavy toll on the entire body. Thrush is far from the only side effect that occurs in the treatment of cancer
Side effects of chemotherapy
Side effects from chemotherapy vary. Among the most common side effects are feeling tired, nausea, diarrhea or constipation, and body hair loss (due to the effect of the drugs on the DNA of the hair follicles). Every cancer patient reacts differently to a combination of chemotherapy drugs. It is very important to remember that these side effects are temporary and gradually disappear after the end of the course of chemotherapy.
The most common side effects are vomiting and nausea, fatigue (anemia and neutropenia), diarrhea and constipation, weight changes and hair loss. Less common side effects are described here (recall, they are usually associated with chemotherapy that affects fast-growing cells):
- General skin changes. They include:
- itching;
- redness;
- dryness and peeling;
- pimples and acne;
- sun sensitivity;
- brittle or discolored nails;
- herpes zoster.

- Headaches.
The doctor may ask the patient to use over-the-counter headache pills other than aspirin, or suggest another medication option. Aspirin is not recommended due to blood-thinning reactions and its effect on the gastric mucosa, which is likely to be more sensitive due to chemotherapy.
- Muscle pain.
Your doctor may recommend over-the-counter anti-inflammatory drugs or give you a prescription for stronger pain relievers. Sometimes light massage is recommended for these pains.
- Burning or painful sensation during urination.
It is important to report these symptoms to your doctor so that you can be checked for a bladder infection. If this is the cause, they will give you medicine to protect and treat the infection.
- Discolored urine.
Sometimes this discoloration is due to a bladder infection and the doctor will check the tests and then prescribe medicine to fight the infection
Sometimes discoloration is caused by the type of chemo you are using and you have nothing to worry about. The color can be red, orange, bright yellow or blue-green. There may be a medicinal smell. Your urine color will return to normal after you are done with chemotherapy.
The color can be red, orange, bright yellow or blue-green. There may be a medicinal smell. Your urine color will return to normal after you are done with chemotherapy.
- Vaginal infections (itching, burning, redness, odorous white or grayish discharge from the vagina; if you have these symptoms, contact your doctor for the correct type of ointment to control the infection).
Soft tissue changes after chemotherapy may increase the chance of vaginal infections. What can be done to avoid these problems?
- Wear cotton underwear.
- Avoid wearing nylon tights.
- Avoid wearing jeans or tight trousers.
- Avoid using petroleum jelly in or around the vagina (this may increase the chance of infection because it is not water based)
- Mouth and throat changes
Chemotherapy can cause sores or ulcers in the mouth and on the oral mucosa. These injuries can be very painful.
- While you’re on chemotherapy, your white blood cell count, which helps fight infection, goes down.
 The most common infection is called thrush or candidiasis.
The most common infection is called thrush or candidiasis.- This is a fungal infection in the mouth.
- White patches or white coating on the tongue and oral mucosa.
- Thrush most often occurs in the vagina.
- Treat with antifungals.
- It may take several days before you notice relief.
- Dry mouth, meaning that there is very little saliva in the mouth. Swallowing problems may occur. Drink plenty of water and soft juices such as apple or carrot juice.
- Inflamed or bleeding gums. The patient may notice this only when brushing his teeth or when eating. Avoid hard, sugary, or acidic foods or drinks (such as vinegary salad dressing)
- Changes in your tastes and smells. A side effect of some chemotherapy drugs is a change in how you feel. Sometimes there is a metallic taste that causes the food and drinks you often like to suddenly taste bad. Rinse your mouth with small sips of water before eating.
- Prickling, burning sensation in hands or feet.
 You must tell your doctor about this. This may mean that chemotherapy is damaging your nerves and the provider may change the medications.
You must tell your doctor about this. This may mean that chemotherapy is damaging your nerves and the provider may change the medications. - Fever. If body temperature exceeds 38°, call your doctor. The high fever is probably caused by some kind of infection.
- Chill. If you feel like you’re shivering or shivering and can’t get warm, call your doctor. It’s probably due to some kind of infection.
- Fluid retention. Some of the chemotherapy drugs cause fluid retention. Doctors don’t usually want patients to take a diuretic to get rid of excess fluid while you’re on chemotherapy. They may recommend avoiding foods or drinks with a lot of sodium (like tomato juice) in them.
- Problems with blood clotting.
- General problems with sexuality: gynecomastia, loss of libido, vaginal dryness, vaginal infection and pain in the genitals.
How to treat thrush during chemotherapy?
Chemotherapy thrush is treated in the same way as normal thrush, but should be discussed with the gynecologist’s oncologist to avoid medications that are incompatible with your type of cancer and the drugs used.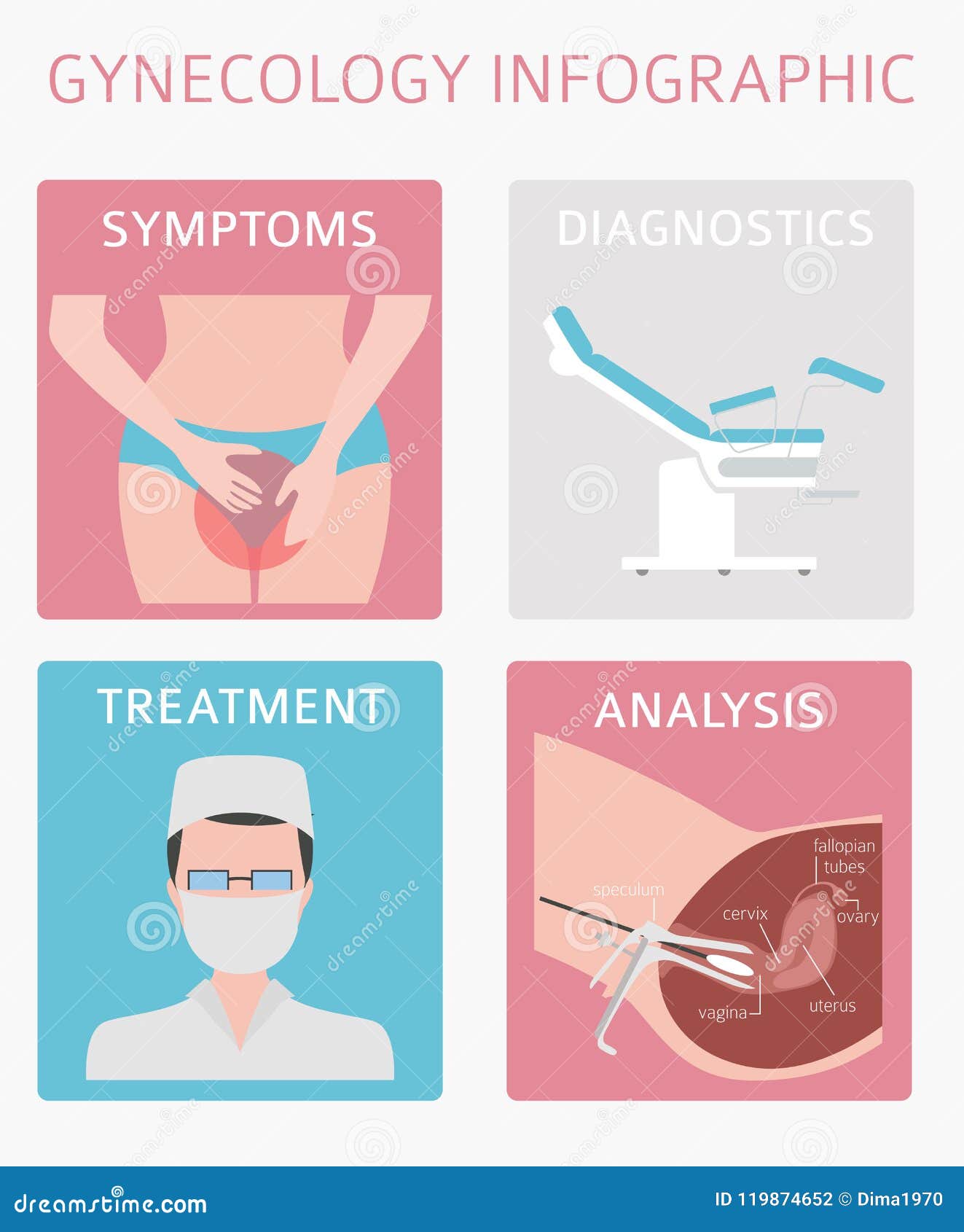
Vaginal infections can be difficult to treat during chemotherapy due to the body’s reduced ability to fight infection. Prevention of vaginal yeast infections is very important.
Tell your doctor right away if you have any signs of a vaginal yeast infection (severe itching, burning, or unusual thick discharge). Mild thrush is usually treated with a short course of antifungal medications. Symptoms usually resolve within a week or two.
Treatment may need to be continued longer if you have recurring thrush attacks.
Several thrush medications are available over the counter at pharmacies, while others are only available with a prescription from your GP.
To be highly effective in reducing the chances of developing a vaginal yeast infection:
- Avoid wearing tights, swimwear, nylon panties or tight pants. Do not wear synthetic fiber clothing.
- Cotton panties and loose clothing recommended.
- Avoid scented oils, bubble baths, powders, feminine hygiene sprays, or showers.
 Sanitary pads and tampons can also affect the acid balance of the vagina.
Sanitary pads and tampons can also affect the acid balance of the vagina. - Avoid using petroleum jelly as a vaginal lubricant as it may increase the chance and severity of vaginal yeast infections.
- Wipe from the front of your body to the back after using the bathroom. This can prevent any abnormal bacteria from entering the vagina.
- Do not wear wet swimwear or clothing for extended periods of time.
- Make sure your genital area is dry after bathing or showering.
Talk to your healthcare provider about your specific health condition and treatments. The recommendations in this article, as well as on information sites on cancer and chemotherapy, are nothing more than information that you need to know, but in no case can serve as guidelines for treatment, choice of drugs, etc. Only the attending physician and doctors of related specializations: oncologist, gynecologist, nutritionist – can draw up a competent scheme of drugs and procedures.:max_bytes(150000):strip_icc()/yeastgard-14a6a91bf7084203ae4b02f68e2d8f00.jpg) Which will lead to getting rid of problems.
Which will lead to getting rid of problems.
Main types of drugs prescribed:
- Pessaries are special tablets that are inserted directly into the vagina using a special applicator.
- Intravaginal creams or gels – these are also inserted into the vagina using the applicator
- Oral capsules are swallowed and may be more convenient to use than pessaries or intravaginal cream, but may have more unpleasant side effects such as vomiting or upset stomach.
All of these options are equally effective. You can usually choose the treatment you prefer, although pregnant or breastfeeding women should not take the capsules.
Creams are also recommended for application to the skin around the vaginal opening. They can help reduce itching and soreness, although you may find that a regular emollient (moisturizer) works just as well.
The main components of the preparations are antifungal. There are drugs with prolonged action, so they do not have to be taken for a long time.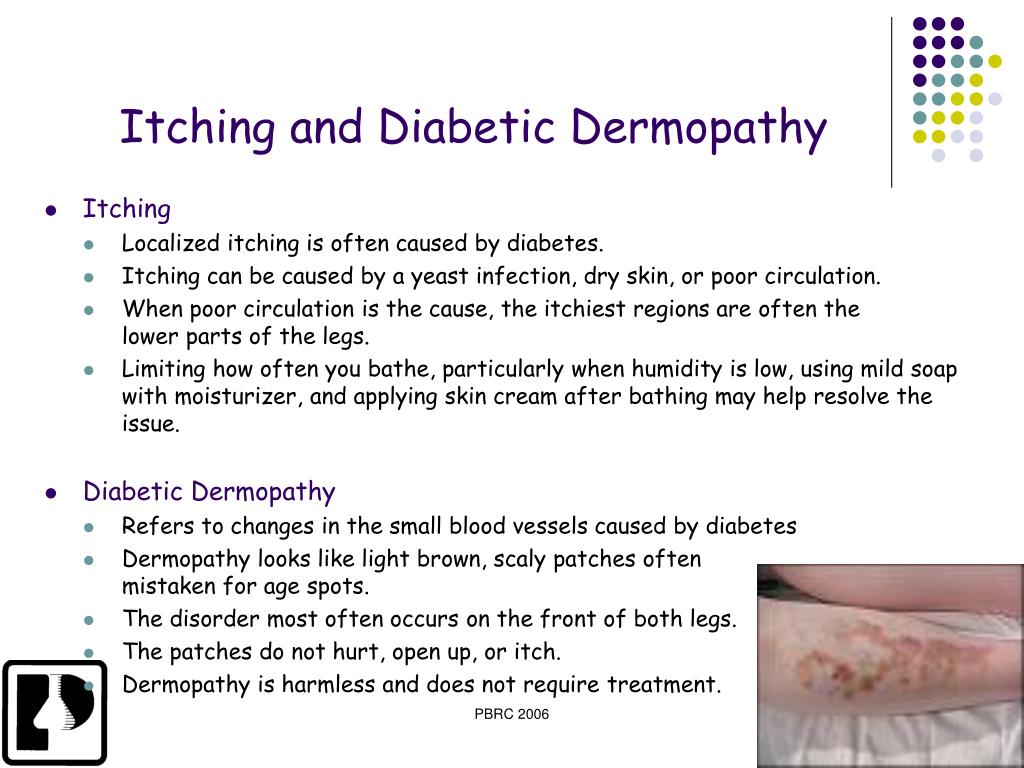
Use of probiotics
Yeast infections occur when a fungus called Candida grows. There are many different strains of Candida, but Candida albicans is the most common cause of vaginal yeast infections.
Our body is home to trillions of microorganisms, including fungi, bacteria and viruses. These tiny organisms are harmless and live in colonies. Together they are known as the human microflora or microbiota. Candida is part of the normal human microflora, but sometimes it grows too much. This disrupts your normal microflora, causing a yeast infection.
Probiotics are a set of live microorganisms that are beneficial to your body. Some of the most common probiotics are bacteria called Lactobacillus. The microflora of the vagina contains Lactobacillus. This helps prevent Candida and other bacteria from getting out of control.
Do they really work?
Women have used yogurt, which often contains Lactobacillus, to treat yeast infections for centuries. Recent research suggests that it may be more effective than experts originally thought.
Recent research suggests that it may be more effective than experts originally thought.
A 2012 study of 129 pregnant women with a yeast infection found that a mixture of antimicrobial honey and yogurt had similar effects to traditional antifungal medications. A mixture of yogurt and honey was better at reducing symptoms, while antifungals were more effective at eliminating fungi. A 2015 study showed similar results in non-pregnant women. The concentrated bacteria in liquid probiotic preparations can be more effective than when using food products containing beneficial microorganisms.
Another 2015 study found that combining prescription antifungal medications such as fluconazole (Diflucan) with probiotic vaginal suppositories made the antifungal more effective. The combination also reduced the likelihood of a yeast infection returning. This suggests that probiotics can be very beneficial for women who recur with yeast infections at least four times a year.
It should be remembered that many of the existing studies on the use of probiotics for the treatment of yeast infections are quite rare, so it is difficult to draw any firm conclusions from them. However, these studies also did not find any risks associated with using probiotics to treat a yeast infection.
However, these studies also did not find any risks associated with using probiotics to treat a yeast infection.
If a patient is regularly diagnosed with yeast infections or is experiencing side effects from conventional antifungal medications, probiotics may be especially helpful.
How to use probiotics
Probiotics come in several forms that are used in different ways. You can find them in the form of capsules or suppositories that you insert into your vagina. When choosing a capsule or suppository or a regular liquid preparation with live bacteria, pay attention to the composition. It is important that lactobacilli are present, they are essential for the vaginal microflora to fight pathogenic microflora and fungi.
For a more cost-effective option, you can also use yogurt. Just make sure you choose one with a label that mentions live cultures and Lactobacillus. Avoid yogurts with added sugar or flavorings. Yeast feeds on sugar, so plain yogurt is best for a yeast infection. But still, the best option is 0H liquid remedy.
But still, the best option is 0H liquid remedy.
To use a liquid product, simply fill the applicator or use a syringe. You need to lie down and release a portion of the drug into the vagina. Wait a few minutes before standing up to give the product time to spread. Do not forget. That liquid will flow out and take care of the gaskets. You can also apply the product to the vulva, which is the outer part of the vagina, to reduce itching and burning.
In addition, you should consume supplements and foods rich in probiotics by mouth. Be sure to check with your doctor before taking supplements.
How long do they work?
Studies involving the use of yogurt and honey in the vagina show that this mixture takes about a week to work. On the other hand, oral probiotics may work to improve the vaginal microflora in one to four weeks. If you choose to use oral probiotics, you can still apply the drug to your vulva to help manage your symptoms.
Risks of using probiotics
Bad reactions to probiotics are extremely rare. These bacteria already exist in your body, so adding them usually carries no risks. Patients sometimes experience mild side effects such as gas and bloating.
These bacteria already exist in your body, so adding them usually carries no risks. Patients sometimes experience mild side effects such as gas and bloating.
However, if you have a weakened immune system due to an underlying condition or treatment you are receiving, it is best to check with your doctor before adding any bacteria to your body. In some types of cancer, immune fluctuations cannot be tolerated, in which case the use of probiotics is prohibited.
why it occurs and what to do about it
Thrush after sex: why it occurs and what to do about it
Medical appointments
- Syphilidologist
- INFECTIONIST
- Dermatologist
- Therapist
- Cardiologist
- Oncologist
- Endocrinologist
- Neurologist
- Medical certificates
- Ultrasound diagnostics – Ultrasound
- Functional diagnostics
- Urologist
- Venereologist
- Parasitologist
- Mammologist
- All services
Diagnosis
- Gynecology
- Dermatovenereology
- Cardiology
- Neurology
- Oncology
- Therapy
- Urology
- Endocrinology
- Infectology
Treatment
- A
- B
- B
- D
- D
- E
- Yo
- F
- Z
- and
- Y
- K
- L
- M
- H
- O
- P
- P
- C
- T
- W
- F
- X
- C
- H
- W
- W
- E
- Yu
- I
COVID
Full range of medical care for viral infection COVID
CHECK-UP
Full range of comprehensive medical diagnostics
Tests
take tests at affordable prices
Drugs 9000 3
specialized pharmacy
Online
specialized consultation
DISCOUNTS
Only profitable offers for you!
St. Petersburg, Ivana Chernykh st., 25A
Petersburg, Ivana Chernykh st., 25A
Mon.-Sat. from 9:00 – 20:00, sun. from 10:00 – 18:00
- home
- •
- News
- •
- Women Health
- •
Thrush after sex: why it occurs and what to do about it
Burning and cheesy discharge 1-3 days after intimacy are symptoms familiar to many girls. But do not blame your partner ahead of time – thrush itself is not related to sex and occurs for other reasons. It can be caused by prolonged use of antibiotics, hormonal changes, improper selection of intimate hygiene products, and many other factors.
Why does thrush get worse after sex
Most often, this situation occurs in girls who suffer from chronic thrush and do not receive proper treatment.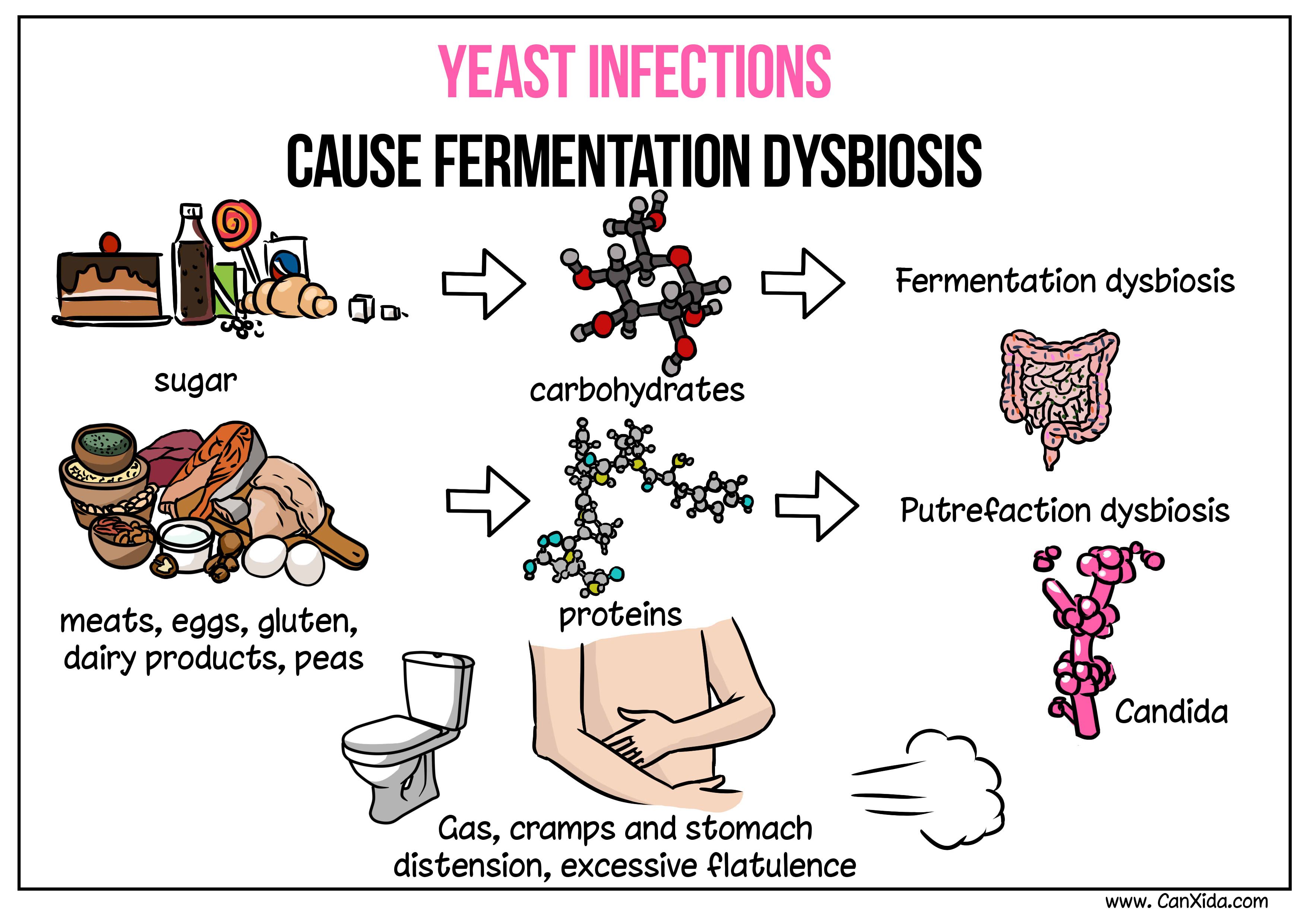 The exchange of microflora with a partner, the ingress of sperm and secretions into the vagina, the use of lubricants and other intimate products – all this aggravates existing disorders and provokes a relapse.
The exchange of microflora with a partner, the ingress of sperm and secretions into the vagina, the use of lubricants and other intimate products – all this aggravates existing disorders and provokes a relapse.
The appearance of symptoms of thrush after sex also contributes to:
● non-observance of hygiene before and after sexual intercourse;
● frequent change of sexual partners or unprotected contacts;
● microtrauma of the vaginal mucosa.
Is it possible to get thrush from a partner
In men, candidiasis mainly affects the glans penis. If the partner does not follow hygiene and does not undergo treatment, a large number of Candida fungi can enter the vagina during sex. Further development of events depends on the immune defense and the presence of risk factors in a woman.
If the composition of the microflora is normal, then beneficial microorganisms quickly suppress the reproduction of fungi, and there will be no thrush. If a woman has recently taken antibiotics, is fond of douching and antibacterial gels, has hormonal disorders, then sexual contact can become a provoking factor for vaginal candidiasis.
If a woman has recently taken antibiotics, is fond of douching and antibacterial gels, has hormonal disorders, then sexual contact can become a provoking factor for vaginal candidiasis.
Sex with thrush – possible or not
In acute vaginal candidiasis and in the period of exacerbation of chronic thrush, it is recommended to refrain from sexual intercourse. The vaginal mucosa is inflamed, so intimacy will be uncomfortable for the woman and will exacerbate existing symptoms. In addition, vaginal suppositories, which are used to treat thrush, reduce the effectiveness of condoms – there is a risk of both STI infection and unplanned pregnancy.
What to do if you have symptoms of thrush
Even if a woman is sure that she has thrush, treatment should not be started without a visit to a gynecologist. The ID-Clinic doctor will perform a gynecological examination, take a vaginal swab to confirm the diagnosis, and if necessary, prescribe an extended health examination. Then the specialist will select an effective treatment, taking into account the cause of the problem, the severity of the inflammation and other individual characteristics of the body.
Then the specialist will select an effective treatment, taking into account the cause of the problem, the severity of the inflammation and other individual characteristics of the body.
A timely visit to the gynecologist is a necessary condition for maintaining and restoring reproductive health!
Tags:
sex
symptoms
mycoses
Cost
Inspection
Reception (examination, consultation) of a gynecologist
3000 ₽
B01.001.002
Reception (examination, consultation) of an obstetrician-gynecologist repeated
3000 ₽
Online consultation with a gynecologist
3000 ₽
Online consultation with a gynecologist (30 min)
2500 ₽
Make an appointment
St.:max_bytes(150000):strip_icc()/TipstoPreventingRecurringYeastInfections_5206120_Color-ffe9c4aa2d794c37a5ac4c6853ec3147.jpg) Petersburg, Ivan Chernykh st., 25A
Petersburg, Ivan Chernykh st., 25A
Mon-Sat 09.00-20.00, Sun 10.00-18.00
By clicking the button you agree to the terms of the Privacy Policy
Krotov Kirill Yurievich
Urologist,
Oncologist,
Oncourologist,
Doctor of the highest categoryMake an appointment
SavchenkoMikhail Andreevich
Infectionist,
Hepatologist,
Doctor of the first category,
Candidate of Medical SciencesMake an appointment
Efimov Georgy Alexandrovich
Infectionist,
ParasitologistMake an appointment
Korneeva Tatyana Sergeevna
Infectionist,
Hepatologist,
Ultrasound doctor,
PhDMake an appointment
Sizova Natalia Vladimirovna
Infectionist,
Doctor of the highest category,
Doctor of Medical Sciences,
ProfessorMake an appointment
TeslyaOlga Vladimirovna
Cardiologist,
Ultrasound doctor,
Functional diagnostics doctor,
Doctor of the highest categoryMake an appointment
Mayorova
Svetlana Olegovna
Infectionist,
Doctor of the highest category,
Candidate of Medical SciencesMake an appointment
Zvontsova Svetlana Alexandrovna
Infectionist,
ParasitologistMake an appointment
Kozminsky Evgeniy Borisovich
Dermatovenereologist,
Syphilidologist,
Doctor of the highest categoryMake an appointment
Lavrenchuk Dmitry Vadimovich
Infectionist,
Hepatologist,
Therapist,
PhDMake an appointment
Fadeev Kirill Aleksandrovich
Infectionist,
Hepatologist,
Parasitologist,
Doctor of the highest category,
Candidate of Medical SciencesMake an appointment
Bortulev Sergey Alexandrovich
Head doctor of the clinic,
Therapist,
Cardiologist,
Functional diagnostics doctor,
Doctor of the highest category,
Candidate of Medical SciencesMake an appointment
Kiseleva Lyudmila Ivanovna
Therapist,
Pulmonologist,
Ultrasound doctor,
Somnologist,
InfectionistMake an appointment
Bortuleva Viktoria Valerievna
Dermatovenereologist,
Mycologist,
Podiatrist,
Doctor of the highest categoryMake an appointment
Savelyeva Karolina Anatolyevna
Endocrinologist,
Diabetologist,
Doctor of the highest category,
Candidate of Medical SciencesMake an appointment
VeliherMarina Georgievna
Therapist,
Ultrasound doctor,
Somnologist,
Psychologist,
RadiologistMake an appointment
SmirnovaUlyana Sergeevna
Gynecologist,
SexologistMake an appointment
Ulitko Tatyana Vladimirovna
Urologist
Make an appointment
Balandina Anna Borisovna
Infectionist,
Hepatologist,
Parasitologist,
RabiologistMake an appointment
Unguryan Nikolay Ivanovich
Therapist,
Clinical Psychologist,
Psychiatrist-narcologistMake an appointment
Yuzefovich Tatyana Sergeevna
Neurologist,
Epileptologist,
Functional diagnostics doctor,
Doctor of the highest categoryMake an appointment
Veronica Golovanova
Gynecologist,
Mammologist,
Oncogynecologist,
Gynecologist-Endocrinologist,
Ultrasound Doctor,
PhDMake an appointment
Shekhovtsova Anna Anatolyevna
Endocrinologist,
Diabetologist,
Nutritionist,
NutritionistMake an appointment
Selivanova Marina Andreevna
Infectionist,
Hepatologist,
Parasitologist,
RabiologistMake an appointment
Elena Vertiletskaya
Gynecologist,
Gynecologist-endocrinologist,
Doctor of the highest categoryMake an appointment
KononchukOlga Nikolaevna
Infectionist,
Hepatologist,
Therapist,
Phthisiatrician,
Functional Diagnostics Doctor,
Doctor of the highest categoryMake an appointment
All specialists
Other clinic services
Cystoscopy
Uroflowmetry
Bladder ultrasound
Urologist
Stories and testimonials from our patients
Dmitry
I have a good impression of Dr. Savchenko. He speaks professional language, and, as I understand it, Botkin’s practice also helps him become the best specialist in his field. The only question is the age of the doctor – very young, the rest is on the level. Perhaps I will contact him again. At the moment, all the doctor’s appointments have already been completed, it remains only to wait for the results of the tests. In principle, if there is any need for the next, the first thing we will have in mind is this clinic. The clinic seemed good to us, but a bit expensive.
Savchenko. He speaks professional language, and, as I understand it, Botkin’s practice also helps him become the best specialist in his field. The only question is the age of the doctor – very young, the rest is on the level. Perhaps I will contact him again. At the moment, all the doctor’s appointments have already been completed, it remains only to wait for the results of the tests. In principle, if there is any need for the next, the first thing we will have in mind is this clinic. The clinic seemed good to us, but a bit expensive.
Specialist:
Savchenko Mikhail Andreevich
User on the amendment
I did the vaccine Previnar-13 in the clinic. Everything went perfect! The doctor examined me carefully and gave the necessary recommendations. After vaccination, she sat in the clinic for 20 minutes, offered coffee, and was constantly interested in her well-being. In general, I really liked everything! Thank you very much to the staff, doctor, head nurse for your professionalism and wonderful attitude!
In general, I really liked everything! Thank you very much to the staff, doctor, head nurse for your professionalism and wonderful attitude!
Natalia Natalia
This is not the first time we have contacted the whole family, the main thing is testing, the administrators are always friendly, no queues, unnecessary questions and waste of time. We arrived, handed over, the result was received by mail. Always fast and extremely polite. Prices are not too high. Always on time and even faster. We are very satisfied and will continue to use. If necessary, you can contact narrow-profile specialists. Very pleased that there is a good pulmonologist. For me, this is extremely important.
The location is excellent, no problems with waiting, everything is simple and clear on the call. No vague stories “Go to the site”, everything is decided by phone. No questions in the spirit of “Do you definitely need this, or maybe this and this and that and that and that for reliability . ..?” Just fast and simple. Pleased with professionalism, competence, tact, level of security.
..?” Just fast and simple. Pleased with professionalism, competence, tact, level of security.
User (SberHealth)
Anna Borisovna is very polite, informatively told everything. I chose the doctor based on reviews. At the appointment, the doctor explained everything in an accessible way, prescribed an additional examination and gave recommendations. The specialist spent enough time at the reception and answered all questions.
Specialist:
Balandina Anna Borisovna
User (On Correction)
I went to a doctor with an already diagnosed diagnosis to prescribe treatment. I can say that it helped quite quickly. The doctor is very polite and friendly, he spent enough time with me. The process of issuing test results is not very clearly organized in the clinic, and the processing time has also been extended.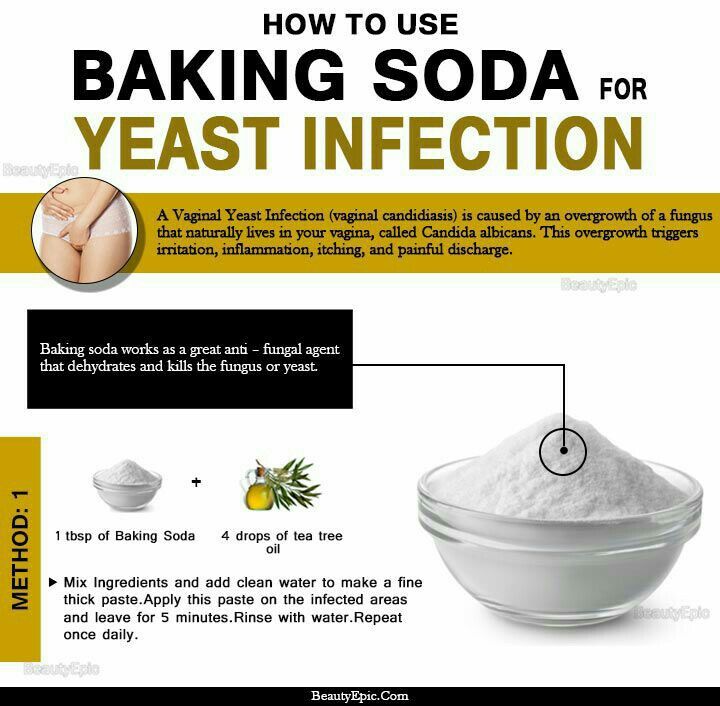 I had to call and find out myself, although I asked to send everything to the post office.
I had to call and find out myself, although I asked to send everything to the post office.
Specialist:
Balandina Anna Borisovna
Irina R
I visited this clinic with my daughter on the advice of a friend. I was incredibly impressed with the attentive attitude, professionalism, humanity of the doctors. Separately, we want to thank Bazyuk Evgenia Mikhailovna!!! She is an amazing doctor!!! We also thank Daria Mikhailovna Surzhenko!! A deep bow to Evgenia Mikhailovna and Daria Mikhailovna!!!
Specialist:
Bazyuk Evgenia Mikhailovna
Specialist:
Surzhenko Daria Mikhailovna
User (SberHealth)
Veronika Anatolyevna is a pleasant doctor. Thinking and analyzing. It was clear that she cared about the patient. The specialist listened to me carefully. She tried to figure it out and was very interested in my problem. As a result of the admission, I received the necessary document. An ultrasound was also performed.
Thinking and analyzing. It was clear that she cared about the patient. The specialist listened to me carefully. She tried to figure it out and was very interested in my problem. As a result of the admission, I received the necessary document. An ultrasound was also performed.
Specialist:
Golovanova Veronika Anatolyevna
Prodoctors
I express my gratitude to the oncourologist Krotov Kirill Yuryevich for his help in a successful operation! The doctor gave me invaluable help. Earlier, doctors said that I would need an expensive operation, I had no money for it. When I checked with Krotov and passed all the tests in his directions, he undertook to operate on me himself, he did everything in an hour, and the operation was successful. No complications or other problems. He spent three days in the hospital after her and was discharged home. Thank you very much doctor.
Thank you very much doctor.
Specialist:
Krotov Kirill Yurievich
User (On Correction)
Signed up for a coronavirus vaccination Sputnik Light. Everything went well, hosted by Efimov Georgy Aleksandrovich. I liked everything, the doctor was very attentive, measured the pressure, temperature, got vaccinated, I endured it easily. And, perhaps, I will also sign up for the next vaccination in this medical center.
Specialist:
Efimov Georgy Aleksandrovich
Irina Maslova
Passed the test for the presence of antibodies to COVID-19, after treatment in the hospital. Fast, convenient, the result will be sent by e-mail in three days.


 Some extreme or severe cases of cervical dysplasia may also require hysterectomy, wherein the entire uterus is removed surgically. Your doctor is likely to decide the best course of treatment depending on the grade and severity of your cervical dysplasia.
Some extreme or severe cases of cervical dysplasia may also require hysterectomy, wherein the entire uterus is removed surgically. Your doctor is likely to decide the best course of treatment depending on the grade and severity of your cervical dysplasia.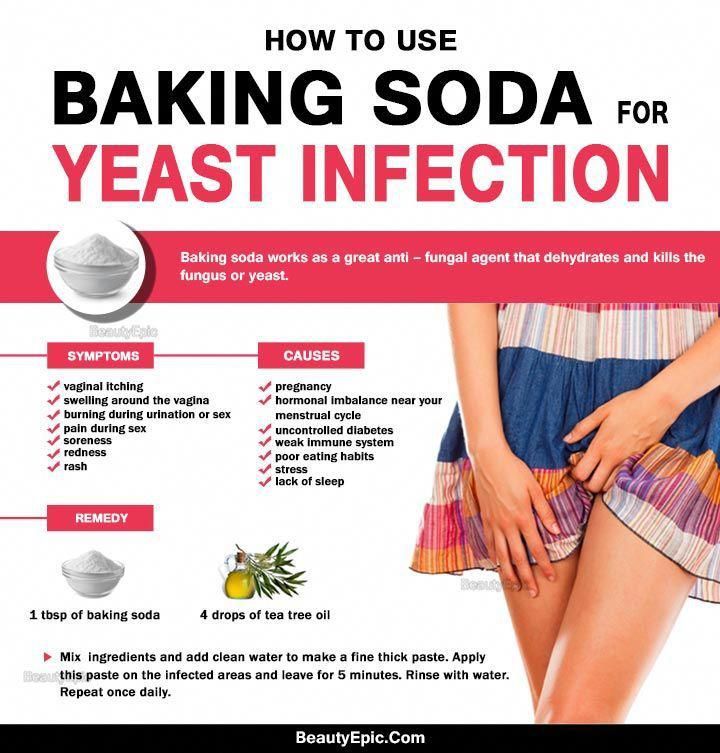

 The most common infection is called thrush or candidiasis.
The most common infection is called thrush or candidiasis. You must tell your doctor about this. This may mean that chemotherapy is damaging your nerves and the provider may change the medications.
You must tell your doctor about this. This may mean that chemotherapy is damaging your nerves and the provider may change the medications. Sanitary pads and tampons can also affect the acid balance of the vagina.
Sanitary pads and tampons can also affect the acid balance of the vagina.