Psoriasis on fingernails pictures. Nail Psoriasis: Pictures, Symptoms, and Treatments
What is nail psoriasis? What are the symptoms of nail psoriasis? How is nail psoriasis treated?
Understanding Nail Psoriasis
Psoriasis is an autoimmune disease that can affect the nails, leading to a condition known as nail psoriasis. This condition can cause a range of symptoms, from pitting and discoloration to thickening and separation of the nail from the nail bed.
Symptoms of Nail Psoriasis
The most common symptoms of nail psoriasis include:
- Pitting: Small indentations or pits in the nail surface, caused by the loss of nail cells.
- Changes in nail shape or thickness: Nails can become thicker, crumbly, or distorted in shape due to the buildup of a chalky substance underneath.
- Nail bed separation: The nail can separate from the underlying nail bed, leaving an empty space that can become infected.
- Discoloration: Nails may turn yellow, red, or purple, and can develop reddish-purple lines (splinter hemorrhages).
- Rough texture: Nails may develop a sandpaper-like appearance, a condition known as trachyonychia.
Causes of Nail Psoriasis
Nail psoriasis is caused by the same underlying immune system dysfunction that leads to skin psoriasis. In people with psoriasis, the immune system mistakenly attacks healthy cells, leading to an overproduction of skin cells and the formation of thick, scaly patches. This process can also affect the nails, leading to the characteristic symptoms of nail psoriasis.

Risk Factors for Nail Psoriasis
Certain factors can increase the risk of developing nail psoriasis, including:
- Having psoriasis on other parts of the body
- Developing psoriatic arthritis, a related joint condition
- Experiencing a traumatic injury or infection to the nails
Diagnosing Nail Psoriasis
Nail psoriasis is typically diagnosed through a visual examination by a dermatologist or other healthcare provider. They may also perform a biopsy or other tests to rule out other nail conditions, such as fungal infections.
Treatment Options for Nail Psoriasis
Treating nail psoriasis can be challenging, as the nails are a difficult area to treat effectively. However, several treatment options are available, including:
- Topical medications: Prescription or over-the-counter topical treatments, such as corticosteroids, vitamin D derivatives, and retinoids, can help reduce inflammation and slow the overproduction of skin cells.
- Injections: Corticosteroid injections directly into the affected nails can help improve the appearance and symptoms of nail psoriasis.
- Oral medications: Systemic treatments, such as methotrexate, cyclosporine, or biologic drugs, may be prescribed for more severe or widespread cases of nail psoriasis.
- Laser therapy: Some healthcare providers may use laser treatments to help improve the appearance of affected nails.
It’s important to work closely with a dermatologist or other healthcare provider to develop a treatment plan that is tailored to your individual needs and the severity of your nail psoriasis.

Managing Nail Psoriasis
In addition to seeking professional treatment, there are some steps you can take at home to help manage the symptoms of nail psoriasis:
- Keep your nails trimmed and filed down to prevent further damage
- Avoid picking or biting your nails, as this can worsen the condition
- Wear gloves or protective nail coverings when performing tasks that could injure your nails
- Maintain good nail hygiene by keeping your nails clean and dry
With the right treatment and self-care measures, many people with nail psoriasis are able to manage their symptoms and maintain the health and appearance of their nails.
Frequently Asked Questions
Does nail psoriasis always occur with skin psoriasis?
No, in some rare cases, nail psoriasis can be the only manifestation of the condition, with no visible skin lesions. However, the majority of people with nail psoriasis will also have psoriasis on other parts of their body.
How long does it take for nail psoriasis to improve with treatment?

It can take 4 to 12 months to see significant improvement in the appearance of affected nails with any given treatment. Patience and consistency are key when managing nail psoriasis.
Can nail psoriasis lead to other health problems?
Yes, in some cases, nail psoriasis can increase the risk of developing a secondary fungal infection in the affected nails. It’s important to keep the nails clean and dry and to seek prompt treatment if any signs of infection develop.
Nail Psoriasis: Pictures, Symptoms, and Treatments
Psoriasis is an inflammatory autoimmune disease that usually causes your body to produce too many skin cells, which can form thick, itchy, scaly patches on the skin. It can also affect your joints and the appearance and texture of your nails — fingernails more often than toenails.
Psoriasis can occur anywhere on the skin, but is typically found on the:
- elbows
- knees
- lower back
- scalp
Around 7.4 million people in the United States have psoriasis. Up to 82 percent of people with psoriasis may experience nail changes. And around 80 percent of people with psoriatic arthritis, a related joint condition, develop nail changes as well. Doctors aren’t sure why this happens to some people and not others.
In rare cases, the nails are the only parts of the body that show signs of psoriasis. But usually, people with psoriasis have a rash on other parts of their body as well.
Nail psoriasis can look different in each person. Symptoms may range from mild to severe.
Symptoms may range from mild to severe.
Pitting
The nail plate is the hard surface that sits over the nail bed. It’s made of keratin, which is a hardened protein found in skin and hair cells.
Nail psoriasis causes your nail plate to lose cells. This results in small pits forming on your fingernails or toenails, which may look like your nails were hit with the tip of a pen. The number of pits varies from person to person.
Some people may have only a single pit on each nail, while others have dozens of pits. The pits can be shallow or deep.
Changes in nail shape or thickness
In addition to pitting, weakness of the structures that support nails can cause your nails to crumble. Nails can also become thicker due to a fungal infection called onychomycosis, which is common in people with psoriasis.
Additionally, your nail may get thicker because it develops a chalky substance underneath. When this happens, it’s called subungual hyperkeratosis and may be painful or uncomfortable.
Nail bed separation
Sometimes your nail can separate from the nail bed, which is the skin underneath the nail plate. This separation is called onycholysis. It leaves an empty space under your nail.
If you have nail psoriasis, you may first notice a yellow discoloration at the tip of a nail. The color and lifting of the nail may eventually go all the way down to the cuticle.
Bacteria can get into the space under the nail and cause infection, which can turn the whole nail a dark color.
Discolored nails
The color of your nail may also change. You might see a yellow-red patch in the nail bed. It looks like a drop of oil under your nail plate, which is where it gets its name: oil-drop spot.
A more severe case of psoriasis may also cause the lunula — the small, half-moon shape that appears at the bottom of your nail — to look red. This is caused by dilated blood vessels.
You may also notice very narrow, reddish-purple lines on your nails. These are called splinter hemorrhages.
These are called splinter hemorrhages.
Additionally, your toenails or fingernails can turn a yellow-brown color. Crumbling nails often turn white.
Blood spots
You also might develop blood spots under your nail, which are called splinter hemorrhages. These deposits are narrow and several millimeters long.
Rough nails
One or all your nails may look like sandpaper, notes Morgan McCarty, DO, a dermatologist at Austin Regional Clinic in Round Rock, Texas. This rare condition is called trachyonychia.
Dermatologists typically treat nail psoriasis with the same treatments that are used for psoriasis. The treatment that’s best for you depends on several factors.
For example, McCarty considers each person’s age and the number of nails that are affected. She also works with a rheumatologist to check for psoriatic arthritis.
Nail psoriasis can be tough to treat and treatments take time to work. As McCarty points out, it can take 4 to 12 months to see improvement in your nails for any treatment.
Many helpful treatments are available, including:
Topical medications
Dermatologists may suggest an over-the-counter or prescription topical medication. You apply topical medications directly to your nail once or twice per day.
Topical medications for nail psoriasis come in various forms, such as:
- ointments
- creams
- emulsions
- nail polishes
Topical corticosteroids, including clobetasol propionate and betamethasone dipropionate, can provide mild improvement of some psoriasis symptoms.
Topical treatments with vitamin D help reduce inflammation and slow excess skin cell production. They can relieve nail thickness by reducing cell buildup under the nails.
Vitamin D topical treatments include:
- calcipotriol (Calcitreme)
- calcipotriene (Dovonex)
- calcitriol
Tazarotene (Tazorac) is a topical retinoid, a medication made from vitamin A. It can help with:
- nail discoloration
- pitting
- separation
Anthralin is an anti-inflammatory ointment that slows excess skin cell production. When applied to the nail bed once daily, it improves symptoms like thickening and onycholysis — although it may temporarily discolor nails.
When applied to the nail bed once daily, it improves symptoms like thickening and onycholysis — although it may temporarily discolor nails.
Corticosteroid injections
In some cases, a dermatologist may inject a corticosteroid into or near your nail. Corticosteroid injections can treat symptoms such as:
- nail thickening
- ridges
- separation
Oral drugs
If a topical medicine doesn’t work or symptoms are more severe, “an oral prescription medicine is usually the next line of defense,” says McCarty.
Dermatologists also advise oral therapies when:
- Psoriasis affects more than three nails.
- The condition greatly impacts a person’s quality of life.
- More than 10 percent of an individual’s body surface is covered in psoriasis or affected by psoriatic arthritis.
Because many oral medications can have some side effects, it’s important to talk with your doctor about what you should expect if you start taking one.
Systemic (body-wide) drugs work throughout your body to clear both the skin and nails in moderate-to-severe psoriasis. These drugs are available as a liquid, pill, or injection.
Systemic drugs include:
- cyclosporine
- methotrexate
- apremilast (Otezla)
- retinoids (Soriatane)
When psoriasis hasn’t responded to other treatments, biologic drugs may be a good option. Biologics are a class of newer medications that target the specific part of the immune system that is overactive due to psoriasis.
Biologics include:
- adalimumab (Humira)
- etanercept (Enbrel)
- infliximab (Remicade)
- ustekinumab (Stelara)
- secukinumab (Cosentryx)
- risankizumab (Skyrizi)
You receive biologic drugs by infusion or injection. Many times, the injection can be performed at home.
Because biologics suppress the immune system, taking one may make you more susceptible to infection. Talk with your doctor about what you can expect if you decide to take a biologic.
Oral antifungal drugs treat fungal infections caused by nail psoriasis.
Phototherapy
Phototherapy improves nail separation and discoloration by slowing the growth of skin cells. For nail psoriasis, the treatment is called PUVA.
PUVA exposes areas of skin affected by psoriasis to:
- ultraviolet (UV) rays from the sun
- a phototherapy unit at a clinic or at home
- a laser
First, you soak your hands in a medication called psoralen or take it by mouth. Psoralen makes your skin sensitive to UVA light. After the medicine, you’re exposed to UVA light.
Laser treatment
Laser therapy for nail psoriasis uses the pulsed dye laser. It works by targeting blood vessels under the skin with a beam of light.
Laser therapy is most helpful for nail splitting and subungual hyperkeratosis, says McCarty.
Home treatments
A few natural remedies that are said to relieve psoriasis symptoms include:
- turmeric
- Dead Sea salt
- aloe vera
However, there isn’t enough scientific evidence to prove any of these alternative treatments actually work.
When it comes to nail psoriasis specifically, alternative treatment options are very limited.
One herbal remedy that may help nail psoriasis is indigo naturalis, a Chinese herbal medicine that comes from the same plant used to make blue dye.
In one small study from 2015, an indigo naturalis extract in oil (Lindioil) improved nail thickening and onycholysis better than topical calcipotriol.
Because of the lack of research around this herbal medicine and most other home remedies for nail psoriasis, it’s best to discuss treatment options with your doctor before deciding on a course of action.
To prevent nail psoriasis flares, consider trying these tips:
- Keep your nails short to avoid injury or lifting of the nail from its bed. Trimming your nails regularly will also help prevent buildup from collecting underneath them.
- Avoid biting or picking at your nails and pushing back your cuticles. Injuries to the skin can set off psoriasis flares. This is called the Koebner phenomenon.

- Wear gloves when gardening, washing dishes, or doing any kind of work in water. For the best protection, wear cotton gloves under vinyl or nitrile gloves.
- Keep your nails clean and dry to prevent infection.
- Use a moisturizing cream on your nails and cuticles. This can help prevent cracked or brittle nails.
- Avoid cleaning your nails with a nail brush or sharp object. This will help prevent nail separation.
- If you smoke, try to quit. Smoking can increase the risk of psoriasis
- If you drink, try to do so in moderation, as alcohol is also associated with a higher risk of psoriasis.
If you feel self-conscious about your nails, you can alter their appearance by gently filing and buffing them and by applying polish.
Avoid fake nails, which increase the risk of your nail separating from its bed.
The National Psoriasis Foundation recommends that everyone with psoriasis connect with a dermatologist for diagnosis and treatment. If you’ve already received a diagnosis, make an appointment with your doctor if:
If you’ve already received a diagnosis, make an appointment with your doctor if:
- Your symptoms are getting worse or are bothering you.
- The treatment you’re using isn’t helping.
- You want to try a new therapy or alternative remedy.
Psoriasis is a common skin condition that can cause nail changes in some people. If you’ve received a psoriasis diagnosis with psoriasis and notice your nails are looking brittle or pitted, talk with your doctor about treatment options.
A variety of treatments are available for nail psoriasis, and the right one for you will depend on a few factors, including the severity of your condition.
Nail Psoriasis: Pictures, Symptoms, and Treatments
Psoriasis is an inflammatory autoimmune disease that usually causes your body to produce too many skin cells, which can form thick, itchy, scaly patches on the skin. It can also affect your joints and the appearance and texture of your nails — fingernails more often than toenails.
Psoriasis can occur anywhere on the skin, but is typically found on the:
- elbows
- knees
- lower back
- scalp
Around 7.4 million people in the United States have psoriasis. Up to 82 percent of people with psoriasis may experience nail changes. And around 80 percent of people with psoriatic arthritis, a related joint condition, develop nail changes as well. Doctors aren’t sure why this happens to some people and not others.
In rare cases, the nails are the only parts of the body that show signs of psoriasis. But usually, people with psoriasis have a rash on other parts of their body as well.
Nail psoriasis can look different in each person. Symptoms may range from mild to severe.
Pitting
The nail plate is the hard surface that sits over the nail bed. It’s made of keratin, which is a hardened protein found in skin and hair cells.
Nail psoriasis causes your nail plate to lose cells. This results in small pits forming on your fingernails or toenails, which may look like your nails were hit with the tip of a pen. The number of pits varies from person to person.
The number of pits varies from person to person.
Some people may have only a single pit on each nail, while others have dozens of pits. The pits can be shallow or deep.
Changes in nail shape or thickness
In addition to pitting, weakness of the structures that support nails can cause your nails to crumble. Nails can also become thicker due to a fungal infection called onychomycosis, which is common in people with psoriasis.
Additionally, your nail may get thicker because it develops a chalky substance underneath. When this happens, it’s called subungual hyperkeratosis and may be painful or uncomfortable.
Nail bed separation
Sometimes your nail can separate from the nail bed, which is the skin underneath the nail plate. This separation is called onycholysis. It leaves an empty space under your nail.
If you have nail psoriasis, you may first notice a yellow discoloration at the tip of a nail. The color and lifting of the nail may eventually go all the way down to the cuticle.
Bacteria can get into the space under the nail and cause infection, which can turn the whole nail a dark color.
Discolored nails
The color of your nail may also change. You might see a yellow-red patch in the nail bed. It looks like a drop of oil under your nail plate, which is where it gets its name: oil-drop spot.
A more severe case of psoriasis may also cause the lunula — the small, half-moon shape that appears at the bottom of your nail — to look red. This is caused by dilated blood vessels.
You may also notice very narrow, reddish-purple lines on your nails. These are called splinter hemorrhages.
Additionally, your toenails or fingernails can turn a yellow-brown color. Crumbling nails often turn white.
Blood spots
You also might develop blood spots under your nail, which are called splinter hemorrhages. These deposits are narrow and several millimeters long.
Rough nails
One or all your nails may look like sandpaper, notes Morgan McCarty, DO, a dermatologist at Austin Regional Clinic in Round Rock, Texas. This rare condition is called trachyonychia.
This rare condition is called trachyonychia.
Dermatologists typically treat nail psoriasis with the same treatments that are used for psoriasis. The treatment that’s best for you depends on several factors.
For example, McCarty considers each person’s age and the number of nails that are affected. She also works with a rheumatologist to check for psoriatic arthritis.
Nail psoriasis can be tough to treat and treatments take time to work. As McCarty points out, it can take 4 to 12 months to see improvement in your nails for any treatment.
Many helpful treatments are available, including:
Topical medications
Dermatologists may suggest an over-the-counter or prescription topical medication. You apply topical medications directly to your nail once or twice per day.
Topical medications for nail psoriasis come in various forms, such as:
- ointments
- creams
- emulsions
- nail polishes
Topical corticosteroids, including clobetasol propionate and betamethasone dipropionate, can provide mild improvement of some psoriasis symptoms.
Topical treatments with vitamin D help reduce inflammation and slow excess skin cell production. They can relieve nail thickness by reducing cell buildup under the nails.
Vitamin D topical treatments include:
- calcipotriol (Calcitreme)
- calcipotriene (Dovonex)
- calcitriol
Tazarotene (Tazorac) is a topical retinoid, a medication made from vitamin A. It can help with:
- nail discoloration
- pitting
- separation
Anthralin is an anti-inflammatory ointment that slows excess skin cell production. When applied to the nail bed once daily, it improves symptoms like thickening and onycholysis — although it may temporarily discolor nails.
Corticosteroid injections
In some cases, a dermatologist may inject a corticosteroid into or near your nail. Corticosteroid injections can treat symptoms such as:
- nail thickening
- ridges
- separation
Oral drugs
If a topical medicine doesn’t work or symptoms are more severe, “an oral prescription medicine is usually the next line of defense,” says McCarty.
Dermatologists also advise oral therapies when:
- Psoriasis affects more than three nails.
- The condition greatly impacts a person’s quality of life.
- More than 10 percent of an individual’s body surface is covered in psoriasis or affected by psoriatic arthritis.
Because many oral medications can have some side effects, it’s important to talk with your doctor about what you should expect if you start taking one.
Systemic (body-wide) drugs work throughout your body to clear both the skin and nails in moderate-to-severe psoriasis. These drugs are available as a liquid, pill, or injection.
Systemic drugs include:
- cyclosporine
- methotrexate
- apremilast (Otezla)
- retinoids (Soriatane)
When psoriasis hasn’t responded to other treatments, biologic drugs may be a good option. Biologics are a class of newer medications that target the specific part of the immune system that is overactive due to psoriasis.
Biologics include:
- adalimumab (Humira)
- etanercept (Enbrel)
- infliximab (Remicade)
- ustekinumab (Stelara)
- secukinumab (Cosentryx)
- risankizumab (Skyrizi)
You receive biologic drugs by infusion or injection. Many times, the injection can be performed at home.
Because biologics suppress the immune system, taking one may make you more susceptible to infection. Talk with your doctor about what you can expect if you decide to take a biologic.
Oral antifungal drugs treat fungal infections caused by nail psoriasis.
Phototherapy
Phototherapy improves nail separation and discoloration by slowing the growth of skin cells. For nail psoriasis, the treatment is called PUVA.
PUVA exposes areas of skin affected by psoriasis to:
- ultraviolet (UV) rays from the sun
- a phototherapy unit at a clinic or at home
- a laser
First, you soak your hands in a medication called psoralen or take it by mouth. Psoralen makes your skin sensitive to UVA light. After the medicine, you’re exposed to UVA light.
Psoralen makes your skin sensitive to UVA light. After the medicine, you’re exposed to UVA light.
Laser treatment
Laser therapy for nail psoriasis uses the pulsed dye laser. It works by targeting blood vessels under the skin with a beam of light.
Laser therapy is most helpful for nail splitting and subungual hyperkeratosis, says McCarty.
Home treatments
A few natural remedies that are said to relieve psoriasis symptoms include:
- turmeric
- Dead Sea salt
- aloe vera
However, there isn’t enough scientific evidence to prove any of these alternative treatments actually work.
When it comes to nail psoriasis specifically, alternative treatment options are very limited.
One herbal remedy that may help nail psoriasis is indigo naturalis, a Chinese herbal medicine that comes from the same plant used to make blue dye.
In one small study from 2015, an indigo naturalis extract in oil (Lindioil) improved nail thickening and onycholysis better than topical calcipotriol.
Because of the lack of research around this herbal medicine and most other home remedies for nail psoriasis, it’s best to discuss treatment options with your doctor before deciding on a course of action.
To prevent nail psoriasis flares, consider trying these tips:
- Keep your nails short to avoid injury or lifting of the nail from its bed. Trimming your nails regularly will also help prevent buildup from collecting underneath them.
- Avoid biting or picking at your nails and pushing back your cuticles. Injuries to the skin can set off psoriasis flares. This is called the Koebner phenomenon.
- Wear gloves when gardening, washing dishes, or doing any kind of work in water. For the best protection, wear cotton gloves under vinyl or nitrile gloves.
- Keep your nails clean and dry to prevent infection.
- Use a moisturizing cream on your nails and cuticles. This can help prevent cracked or brittle nails.
- Avoid cleaning your nails with a nail brush or sharp object.
 This will help prevent nail separation.
This will help prevent nail separation. - If you smoke, try to quit. Smoking can increase the risk of psoriasis
- If you drink, try to do so in moderation, as alcohol is also associated with a higher risk of psoriasis.
If you feel self-conscious about your nails, you can alter their appearance by gently filing and buffing them and by applying polish.
Avoid fake nails, which increase the risk of your nail separating from its bed.
The National Psoriasis Foundation recommends that everyone with psoriasis connect with a dermatologist for diagnosis and treatment. If you’ve already received a diagnosis, make an appointment with your doctor if:
- Your symptoms are getting worse or are bothering you.
- The treatment you’re using isn’t helping.
- You want to try a new therapy or alternative remedy.
Psoriasis is a common skin condition that can cause nail changes in some people. If you’ve received a psoriasis diagnosis with psoriasis and notice your nails are looking brittle or pitted, talk with your doctor about treatment options.
A variety of treatments are available for nail psoriasis, and the right one for you will depend on a few factors, including the severity of your condition.
common causes, important symptoms, effective treatment and photos of the disease
Almost 7% of patients who suffer from psoriasis and have experienced inflammatory skin rashes have damage to the nail plate. This disease is called nail psoriasis and is accompanied by a darkening of the surface. Often longitudinal or transverse grooves are formed on the plate.
- Symptoms of nail psoriasis
- Thimble Syndrome
- Onycholysis
- Subungual hemorrhage
- Trachionichium
- Causes of nail psoriasis
- How to properly treat nail psoriasis?
- Treatment of nail psoriasis at home
Symptoms of nail psoriasis
This disease has been known since ancient times and the first descriptions about it appeared at the beginning of the 19th century. Then the doctors had certain difficulties with the treatment and diagnosis. But scientists put forward their assumption that the disease has an isolated form.
Then the doctors had certain difficulties with the treatment and diagnosis. But scientists put forward their assumption that the disease has an isolated form.
In the world of modern technology, experts were able to confirm this hypothesis. Damage to the nail plate in nail psoriasis manifests itself as a concomitant form of the disease. In this case, we are talking about psoriasis vulgaris , which can develop independently.
There are several common clinical manifestations of this disease. Most often, patients can find a symptom of a thimble, subungual hemorrhage, onycholysis, and trachyonychia.
Nail psoriasis
Thimble syndrome
This is a common form of nail psoriasis. This problem manifests itself in the form of tiny dimples on the surface. Their diameter reaches two millimeters. The main reason for the development of this form of the disease is a violation of the formation of the plate. Recesses can have a different size, shape and depth. Also they are characterized by a chaotic order , which in its appearance is more like the surface of a thimble. That is why this disease received this name.
Recesses can have a different size, shape and depth. Also they are characterized by a chaotic order , which in its appearance is more like the surface of a thimble. That is why this disease received this name.
If a person has one or two dimples, then this phenomenon is considered normal and the problem is not attributed to nail psoriasis. A similar form of the disease may appear during chronic dermatosis.
Onycholysis
This is a fairly common problem that occurs in many patients. This pathology is characterized by damage to the nail plate and its gradual rejection from the bed. In this case, the patient does not feel any inflammatory reactions or manifestations. The separation of the nail begins at the distal edge. The degree of expression is full and partial.
Under the peeled nail there is an empty space where particles of dust, dirt or air bubbles can get in. Immediately, dead epidermis gradually accumulates, which is able to give the nail plate a gray-white tint.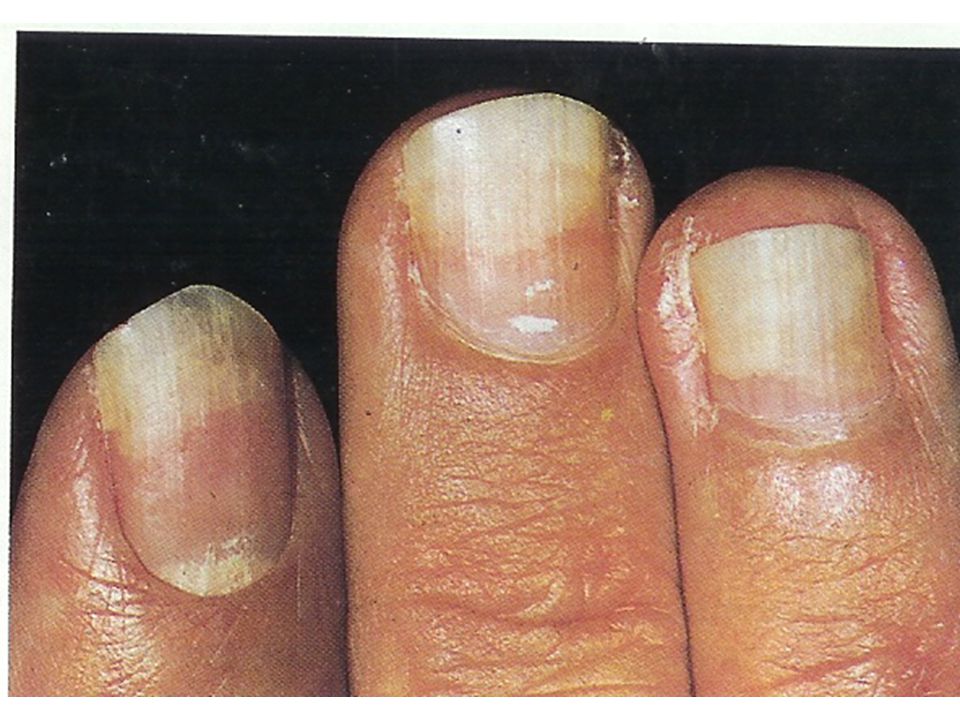
In severe and advanced forms, the disease is accompanied by an unpleasant odor. The main distinguishing feature of onycholysis is the presence of a narrow strip of pink color.
Subungual hemorrhage
There are two varieties of subungual hemorrhage, which are characterized by a variety of characteristics. In the first case, patients are faced with the appearance of spots on the nail plate, which have a different color and size. This disease is called oil spot syndrome.
In the second case, subungual hemorrhage is characterized by band-like hemorrhages of reddish, brown or black hues. This type of disease develops after the rupture of blood capillaries.
Trachyonychia
Trachyonychia develops in 10% of patients who develop nail psoriasis. It has several features – this is the roughness and dull color of the surface of the nail plate. In this case, the hole at the base of the nail is completely absent.
There are cases when the presented pathology is accompanied by coyolonychia, then a small depression appears in the center of the plate. Serious problems can be avoided if seek help from a qualified technician immediately. When the nail becomes denser, after a few weeks it may gradually acquire a concave shape. The subungual tissue is not subject to any changes and pathologies.
Causes of nail psoriasis
There are several important reasons for the development of nail psoriasis in patients:
- the presence of an infectious disease;
- disorders of the immune system;
- interruptions in the hormonal background;
- wrong metabolism;
- regular stress and overexertion;
- genetic predisposition.
How to properly treat nail psoriasis?
A large number of people do not know how to properly treat nail psoriasis. It should be noted that is a rather long and laborious process , which will require a lot of effort. At the first signs of psoriasis, the patient should seek qualified help. Only a doctor can determine the cause of the development of pathology and prescribe an effective treatment.
At the first signs of psoriasis, the patient should seek qualified help. Only a doctor can determine the cause of the development of pathology and prescribe an effective treatment.
Nail psoriasis can be chronic, relapsing and undulating. The main condition of therapy is the correct and regular care of the affected, as well as healthy nails. For patients, important rules have been drawn up that must be followed during treatment:
- cut nails short;
- try to prevent the appearance of microtraumas;
- procedures such as manicures and pedicures must be postponed;
- Gloves must be worn when doing household chores and washing dishes.
In case of any damage to the nail plate, patients are advised to take the vitamin complex selected for them by their doctor, which should contain a high amount of useful microelements. In order for the nails to have the correct shape and form in the right direction, it is necessary to pay attention to the sufficient intake of potassium, calcium, silicon and zinc in the body. It is these recommendations and useful tips that will help to avoid such a problem as nail psoriasis. A photo of the affected nail plate and the consequences of improper treatment can be viewed in the doctor’s office.
It is these recommendations and useful tips that will help to avoid such a problem as nail psoriasis. A photo of the affected nail plate and the consequences of improper treatment can be viewed in the doctor’s office.
But if the patient has an acute stage of the disease, then you should refrain from taking the drugs presented. Also, they are not used with possible individual intolerance. Mild psoriasis does not require medical treatment from the patient.
In this case, it would be advisable to use useful healing varnishes that will effectively hide possible defects. The process of nail damage will be slowed down and repeated relapses are prevented. If patients do not seek qualified help in time, then dermatologists prescribe additional local treatment. At the same time, patients regularly use healing solutions, creams and ointments. The duration of such therapy is at least three months.
Treatment of nail psoriasis at home
There are several important points for treating psoriasis at home:

Psoriasis is a multifactorial disease that occurs most often in young people. The photo shows that the main symptom of this disease is excessive peeling of the nail plate. Exacerbations occur during the winter months.
When the first signs of psoriasis are detected, which can be seen in detail in the photo, you should immediately seek qualified help. Only the doctor will determine the cause of the development of the pathology and prescribe the appropriate treatment that will be effective.
Foot psoriasis, what to do?
Diagnosing psoriasis is not easy even for dermatologists, as the various forms of psoriasis often resemble other diseases caused by eczema, athlete’s foot, or even cancer.
In the presence of psoriasis on the legs, treatment is carried out by a venereologist-cosmetologist and a podologist:
- The venereologist prescribes drug therapy, monitors all the results.

- It is very important to properly care for the feet – mechanical injuries, cuts provoke the development of psoriasis, which is already difficult to contain even with corticosteroid drugs. The solution is a gentle medical pedicure. With psoriasis, the classic edged pedicure is prohibited!
You can maintain the condition of the feet, remove characteristic keratinization, peeling in the podiatrist’s office.
Foot psoriasis – what is it?
Psoriasis often occurs on the foot with a transition to the nail plate. The most difficult case of foot psoriasis is its vesicular form, also known as pustular psoriasis (palmoplantare pustuloese psoriasis). Unfortunately, it is often confused with skin fungus, sweat eczema, hyperkeratosis of the epidermis due to excessive sweating, keratosis due to papillary infection, lichen planus or atopic dermatitis.
Nail psoriasis is difficult to hide. Whether we are among colleagues or among friends, affected nails are always visible. They are thickened, have a yellowish color.
They are thickened, have a yellowish color.
Why do we need podiatry?
If you notice changes in your foot, the most important thing is to consult a podiatrist as soon as possible.
If the changes progress, you will need the help of a dermatologist anyway.
In podiatric practice, the aesthetics of nails affected by psoriasis plays an important role, since its articular shape can even lead to the almost complete loss of the nail plate. The pustular form of psoriasis has the worst effect on deforming changes in the nail plate.
Along with a pedicure, pharmacotherapy is required as prescribed by a doctor.
Severe conditions of nail psoriasis are precursors of articular psoriasis. In such cases, you can not rely only on care. The sooner pharmacotherapy is carried out, the easier it is to prevent the deterioration of the condition of the nails.
Early pharmacological treatment is likely to slow down the approaching joint shape. Treatment takes a lot of time, but the result will be a cumulative result.
The biggest problem in the treatment of nail psoriasis is the lack of patience.
How to distinguish psoriasis from mycosis?
Nail psoriasis without cutaneous or articular inclusion is possible but occurs in only 5% of cases. So usually psoriasis affects the nail plate and the entire foot.
On the toenails, we most often observe changes in the form of dimples, spots similar to vitiligo and normal pigmentation.
General symptoms of nail psoriasis:
- thimble syndrome – microscopic crotch-like depressions in the nail plate;
- yellowish brown color of the nail, similar to a drop of oil;
- longitudinal and transverse grooves – splitting of the nail plate;
- leukonychia – white spots on nails;
- elevated hyponychium – masses of keratinized epidermis accumulate under the nail, which raise the hyponychium, deform the nail, make it brittle;
- swelling of the skin – painful and swollen skin on the nail folds.



 This will help prevent nail separation.
This will help prevent nail separation.
