Homeopathic remedy urinary tract infection. Urinary Tract Infections in Women: Symptoms, Causes, and Treatment Options
What are the common signs of a urinary tract infection. How can UTIs be diagnosed and treated effectively. Which risk factors contribute to the development of UTIs in women. What dietary and lifestyle changes may help prevent recurrent urinary tract infections.
Understanding Urinary Tract Infections: A Comprehensive Guide for Women
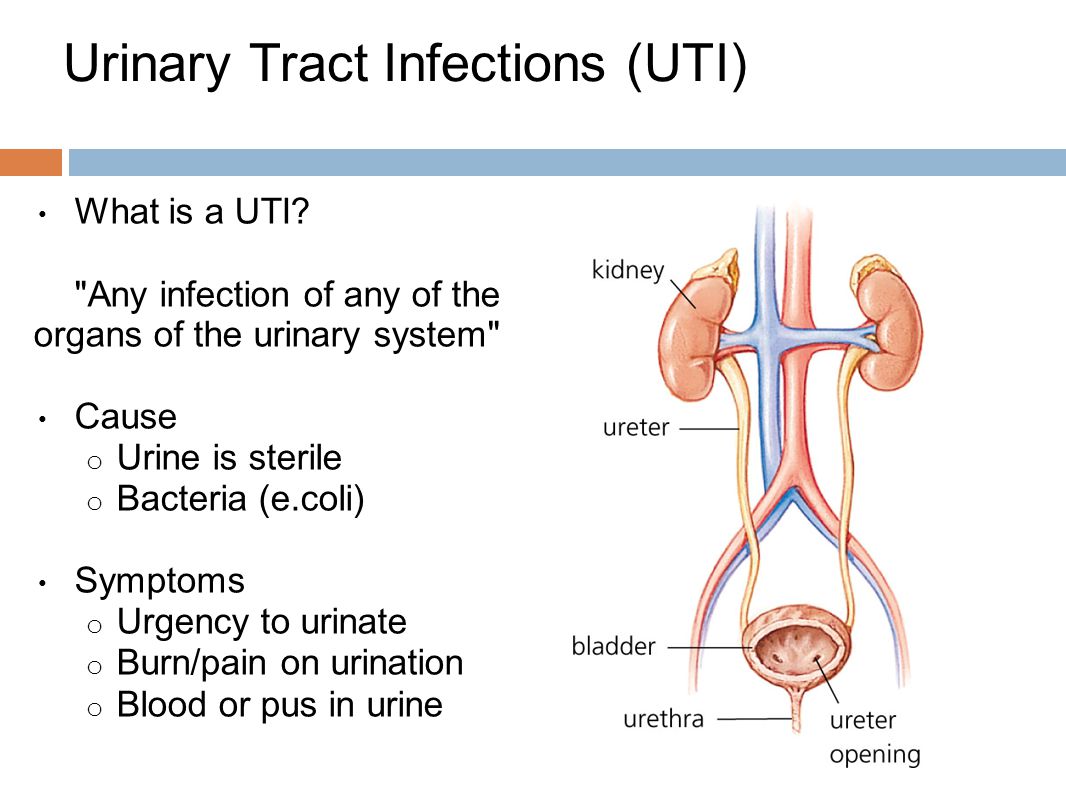
Urinary tract infections (UTIs) are a common health concern among women, affecting millions each year. These infections can cause significant discomfort and, if left untreated, may lead to more serious complications. This article delves into the various aspects of UTIs, providing essential information on symptoms, causes, diagnosis, and treatment options.
Recognizing the Signs and Symptoms of UTIs
Identifying a urinary tract infection early is crucial for prompt treatment and relief. Women experiencing UTIs often report a range of symptoms that can vary in intensity. Are you familiar with the telltale signs of a UTI? Here are the most common symptoms to watch out for:

- Pain or burning sensation during urination
- Increased frequency and urgency of urination
- Presence of blood or pus in the urine
- Lower abdominal cramps or pain
- Chills or fever (particularly in children and infants)
- Strong-smelling urine
- Discomfort during sexual intercourse
- Nausea, vomiting, and general malaise
Is it possible to have a UTI without experiencing all these symptoms? Absolutely. Some women may only exhibit a few of these signs, while others might experience additional symptoms not listed here. It’s important to consult a healthcare provider if you suspect you have a UTI, even if your symptoms seem mild.
Unraveling the Causes and Risk Factors of UTIs
Understanding the underlying causes and risk factors associated with urinary tract infections can help women take preventive measures and reduce their likelihood of developing UTIs. Do you know what puts you at higher risk for UTIs?
Common Risk Factors for UTIs in Women
- Sexual activity: New sexual partners or increased frequency of intercourse
- Hormonal changes: Pregnancy or use of birth control pills
- Medical conditions: Diabetes or urinary tract abnormalities
- Hygiene practices: Use of irritating products or improper wiping techniques
- Contraceptive methods: Diaphragms or spermicides
- Antibiotic use: Frequent or prolonged use can disrupt natural bacterial balance
- History of UTIs: Previous infections increase the risk of recurrence
- Urinary incontinence: Difficulty emptying the bladder completely
Can certain bacteria cause UTIs more frequently than others? Indeed, the most common culprit behind urinary tract infections is Escherichia coli (E. coli), followed by Staphylococcus saprophyticus. These bacteria typically reside in the digestive tract but can cause problems when they enter the urinary system.
Diagnosis and Medical Evaluation of UTIs
When you visit your healthcare provider with suspected UTI symptoms, what can you expect during the examination? The diagnostic process typically involves several steps to confirm the presence of an infection and determine its severity.
Steps in UTI Diagnosis
- Physical examination: Your provider will palpate your abdomen and kidneys for any unusual changes or tenderness.
- Urine analysis: A sample of your urine will be tested for the presence of bacteria, white blood cells, and other indicators of infection.
- Urine culture: This test identifies the specific type of bacteria causing the infection and helps determine the most effective antibiotic treatment.
- Additional tests: In some cases, your provider may recommend further testing to rule out other conditions that may mimic UTI symptoms, such as sexually transmitted infections.
Is it possible for other conditions to be mistaken for a UTI? Yes, which is why a thorough evaluation is crucial. Conditions like sexually transmitted diseases can present similar symptoms, making accurate diagnosis essential for proper treatment.

Exploring Treatment Options for Urinary Tract Infections
Once a UTI is confirmed, what are the available treatment options? The primary approach to treating urinary tract infections typically involves antibiotics, but there are also complementary therapies that may provide relief and support recovery.
Conventional Medical Treatments
Antibiotics are the mainstay of UTI treatment. The choice of antibiotic and duration of treatment depend on the severity of the infection and the patient’s medical history. Are all antibiotic courses the same length? Not necessarily. While many treatments last 7 to 10 days, shorter courses are sometimes prescribed for uncomplicated UTIs.
Complementary and Alternative Therapies
In addition to conventional treatments, some women find relief through complementary approaches. These may include:
- Herbal remedies
- Probiotics
- Dietary modifications
- Stress reduction techniques
Can these alternative therapies replace antibiotics? It’s important to note that while complementary therapies may offer supportive benefits, they should not be used as a substitute for prescribed medical treatments without consulting your healthcare provider.

Nutritional Strategies for UTI Prevention and Management
Diet plays a crucial role in maintaining urinary tract health and may help prevent recurrent UTIs. What dietary changes can women make to reduce their risk of developing UTIs?
Beneficial Dietary Practices
- Increase fluid intake, especially water and herbal teas
- Consume cranberries and blueberries regularly
- Incorporate antioxidant-rich foods into your diet
- Boost fiber intake through whole grains, beans, and vegetables
- Reduce consumption of refined sugars and processed foods
- Opt for lean proteins and plant-based protein sources
- Use healthy cooking oils like olive oil and coconut oil
Is there a specific “UTI diet” that guarantees prevention? While no diet can completely eliminate the risk of UTIs, these nutritional strategies can support overall urinary tract health and may reduce the frequency of infections in susceptible individuals.
Lifestyle Modifications to Support Urinary Tract Health
Beyond dietary changes, what lifestyle modifications can women implement to maintain a healthy urinary tract and reduce their risk of UTIs?

Practical Tips for UTI Prevention
- Practice good hygiene: Wipe from front to back after using the toilet
- Urinate before and after sexual activity
- Avoid holding urine for extended periods
- Wear breathable, cotton underwear
- Stay hydrated throughout the day
- Avoid irritating feminine products
- Consider alternative birth control methods if prone to UTIs
- Engage in regular physical activity
Can these lifestyle changes completely prevent UTIs? While they significantly reduce the risk, some women may still experience infections despite following these guidelines. It’s important to work closely with your healthcare provider to develop a personalized prevention strategy.
The Role of Supplements in UTI Prevention and Treatment
Nutritional supplements may offer additional support for urinary tract health. Which supplements are most commonly recommended for UTI prevention and management?
Key Supplements for Urinary Tract Health
- Cranberry extract: May help prevent bacteria from adhering to the bladder wall
- D-mannose: A natural sugar that can interfere with bacterial attachment
- Probiotics: Support healthy bacterial balance in the urogenital area
- Vitamin C: Helps acidify urine, creating a less hospitable environment for bacteria
- Omega-3 fatty acids: May help reduce inflammation
Are these supplements safe for everyone? While generally well-tolerated, it’s crucial to consult with a healthcare provider before starting any new supplement regimen, especially if you have existing health conditions or are taking medications.

By understanding the various aspects of urinary tract infections, from symptoms and causes to treatment options and preventive strategies, women can take proactive steps to maintain their urinary health. Remember, while UTIs are common, they are also highly treatable when addressed promptly. If you suspect you have a UTI, don’t hesitate to seek medical attention for proper diagnosis and treatment.
Urinary tract infection in women Information | Mount Sinai
UTI
Signs and Symptoms
Symptoms of UTIs include:
- Pain or burning during urination
- The need to urinate more often than usual
- A feeling of urgency during urination
- Blood or pus in the urine
- Cramps or pain in the lower abdomen
- Chills or fever (fever may be the only symptom in infants and children)
- Strong smelling urine
- Pain during sexual intercourse
- Nausea, vomiting, and malaise
What Causes It?
Risk factors include:
- A new sex partner or multiple partners
- More frequent or intense intercourse
- Diabetes
- Pregnancy
- Escherichia coli (E coli)
- Staphylococcus saprophyticus
- Use of irritating products, such as harsh skin cleansers
- Use of irritating contraceptives, such as diaphragms and spermicides
- Use of birth control pills
- Heavy use of antibiotics
- A blockage in the urinary tract (benign masses or tumors)
- A history of UTIs, especially if infections are less than 6 months apart
- Incontinence
What to Expect at Your Provider’s Office
Your health care provider will feel your abdomen and kidneys for changes and use laboratory tests, such as a urine culture, to find out if you have a UTI. If the usual treatments do not work, your provider will explore the possibility that you have some other condition. Other illnesses, such as sexually transmitted diseases (STDs), can cause symptoms that mimic a UTI.
If the usual treatments do not work, your provider will explore the possibility that you have some other condition. Other illnesses, such as sexually transmitted diseases (STDs), can cause symptoms that mimic a UTI.
Treatment Options
Drug Therapies
Doctors may presecribe antibiotics or other drugs to treat UTIs. The course for most antibiotics is 7 to 10 days, though shorter courses of treatment are also available.
Complementary and Alternative Therapies
Some complementary and alternative (CAM) therapies may be helpful for UTIs, but they may not be right for every person. Natural medicines and supplements may interact with prescription medications. Work with a knowledgeable health care provider, and always tell all of your providers about the herbs and supplements you are taking.
Work with a knowledgeable health care provider, and always tell all of your providers about the herbs and supplements you are taking.
Nutrition and Supplements
Following these nutritional tips may help reduce symptoms:
- Drink a lot of fluids, such as herbal teas and water. Avoid sweetened fruit juices and other sweetened drinks.
- Cranberries and blueberries contain substances that inhibit the binding of bacteria to bladder tissue. Drinking unsweetened cranberry juice regularly helps lower the risk of UTIs. People who are allergic to aspirin should not consume large quantities of cranberry juice. Cranberry juice may interact with certain medications.
- Try to eliminate potential food allergens, including dairy, wheat (gluten), corn, preservatives, and food additives. Your provider may want to test for food sensitivities. If you are susceptible to UTIs, drinking cranberry juice or taking cranberry pills may help prevent recurrence.
- Eat antioxidant-rich foods, including fruits (such as blueberries, cherries, and tomatoes), and vegetables (such as squash and bell peppers).

- Eat more high-fiber foods, including beans, oats, root vegetables (such as potatoes and yams), and psyllium seed.
- Avoid refined foods, such as white breads, pastas, and especially sugar.
- Eat fewer red meats and more lean meats, cold-water fish, tofu (if no allergy to soy is present), or beans for protein.
- Use healthy cooking oils, such as olive oil or coconut oil.
- Reduce or eliminate trans fatty acids, found in commercially-baked goods, such as cookies, crackers, cakes, French fries, onion rings, donuts, processed foods, and margarine.
- Avoid coffee and other stimulants, alcohol, and tobacco.
- Drink 6 to 8 glasses of filtered water daily.
- Exercise at least 30 minutes daily, 5 days a week.
You may address nutritional deficiencies with the following supplements:
- A multivitamin daily. Containing the antioxidant vitamins A, C, E, the B-complex vitamins, and trace minerals, such as magnesium, calcium, zinc, and selenium.

- Vitamin C. As an antioxidant and for immune support.
- Omega-3 fatty acids, such as fish oil. To help reduce inflammation and promote general health. Cold-water fish, such as salmon or halibut, are good sources. Fish oil supplements can increase the effects of certain blood-thinning medications.
- Probiotic supplement (containing Lactobacillus acidophilus). For maintenance of gastrointestinal and immune health. There is strong scientific evidence to support the use of probiotics for urological conditions. Refrigerate probiotic supplements for best results. People with severely weakened immune systems should speak wiht their doctors before taking probiotics.
- Grapefruit seed extract (Citrus paradisi). For antibacterial, antifungal, and antiviral activity. Grapefruit may interact with a wide variety of medications. Speak with your doctor.
Natural hormone replacement therapy may help prevent UTIs. Ask your provider about this treatment.
Ask your provider about this treatment.
Herbs
Herbs may help strengthen and tone the body’s systems. As with any therapy, you should work with your provider before starting treatment. You may use herbs as dried extracts (capsules, powders, or teas), glycerites (glycerine extracts), or tinctures (alcohol extracts). Unless otherwise indicated, make teas with 1 tsp. (5 grams) herb per cup of hot water. Steep covered 5 to 10 minutes for leaf or flowers, and 10 to 20 minutes for roots. Drink 2 to 4 cups per day. You may use tinctures alone or in combination as noted. Many herbs interact with medications, and may make certain conditions worse, so tell your doctor about any herbal therapies you are using or considering using. The following herbs may be useful for short term treatment of a urinary tract infection.
- Green tea (Camellia sinensis). For antioxidant, anticancer and immune effects. Use caffeine-free products. You may also prepare teas from the leaf of this herb.

- Cat’s claw (Uncaria tomentosa). For anticancer, immune and antibacterial or antifungal activity. Cat’s claw can interact with many different medications. Speak to your provider. DO NOT take cat’s claw if you have leukemia or autoimmune disease.
- Reishi mushroom (Ganoderma lucidum). For anticancer and immune effects. High doses of reishi may have a blood-thinning effect. Speak to your doctor if you are on blood-thinning medications or medications for high blood pressure.
- Milk thistle (Silybum marianum). For detoxification support. People who have a history of hormone-related cancer should use caution before taking milk thistle as it may have estrogen-like properties. Milk thistle may interact with a wide variety of medications. Speak with your doctor.
- Uva-ursi (Arctostaphylos uva-ursi) standardized extract. You may also prepare teas from the leaf of this herb.
 Uva-ursi may interact with lithium. There is a possibility that a compound in uva-ursi can have a thinning effect on the retina. DO NOT use daily as long-term therapy.
Uva-ursi may interact with lithium. There is a possibility that a compound in uva-ursi can have a thinning effect on the retina. DO NOT use daily as long-term therapy. - Buchu (Barosma betulina). For antibacterial effects. Buchu can interact with lithium and with blood thinning medications. Some health experts advise against using buchu when there is inflammation of the urinary tract or kidney infection. Others disagree. Speak with your doctor.
Homeopathy
Few studies have examined the effectiveness of specific homeopathic remedies. Professional homeopaths, however, may recommend one or more of the following treatments for UTI based on their knowledge and clinical experience. Before prescribing a remedy, homeopaths take into account a person’s constitutional type, includes your physical, emotional, and intellectual makeup. An experienced homeopath assesses all of these factors when determining the most appropriate remedy for a particular individual.
- Apis mellifica. For stinging or burning pains that tend to worsen at night and from warmth. This remedy is appropriate for people who feel an intense urge to urinate, yet can only do so in drops.
- Aconitum. For early symptoms of UTI, particularly with extremely painful urination that is often described as a hot sensation.
- Berberis. For UTIs with burning or shooting pain during urination that may radiate to the pelvis or back. When not urinating, an aching sensation is present in the bladder that worsens with movement. Pain may also extend to legs and abdomen.
- Cantharis. This is the most common and considered the most effective homeopathic remedy for UTI. This remedy is most appropriate for people who are restless, experience a burning sensation and decreased urine flow (despite a strong desire to urinate), and have increased sexual desire despite symptoms.
- Mercurius. For burning urination and a strong urge to urinate.
 Symptoms worsen at night and tend to be accompanied by chills and sweating. Urine is dark and only small amounts pass. Burning sensation is often worse when the individual is not urinating.
Symptoms worsen at night and tend to be accompanied by chills and sweating. Urine is dark and only small amounts pass. Burning sensation is often worse when the individual is not urinating. - Nux vomica. For people who have a constant urge to urinate. Pain is described as needle like. The urge to have a bowel movement may accompany urinary urgency. Some people experience mild, temporary relief from urination and warm baths. Symptoms may begin following ingestion of alcohol, coffee, drugs, or overeating.
- Pulsatilla. For bladder inflammation that begins after an individual develops a sudden chill in hot weather. This remedy is most appropriate for people with an urgent desire to urinate who may be emotional, crave attention, and dribble urine after laughing, coughing, sneezing, or being surprised.
- Sarsaparilla. For women who experience severe pain at the end of urination and who, occasionally, feel compelled to stand to urinate.
- Staphysagria.
 For UTIs usually associated with sexual intercourse or following extreme embarrassment or humiliation, particularly from sexual abuse. This remedy is most appropriate for those who have an urgent desire to urinate and have the sensation that a single drop of urine is still present even following urination.
For UTIs usually associated with sexual intercourse or following extreme embarrassment or humiliation, particularly from sexual abuse. This remedy is most appropriate for those who have an urgent desire to urinate and have the sensation that a single drop of urine is still present even following urination.
Following Up
Preventive measures you can follow:
- Urinate both before and after intercourse.
- Have your health care provider recheck the fit of your diaphragm if you use one.
- Avoid sex while you are being treated for a UTI.
Special Considerations
If you are pregnant, you are at higher risk of developing a UTI.
Supporting Research
Appleton J. Arginine: Clinical potential of a semi-essential amino. Altern Med Rev. 2002;7(6):512-22.
Arya LA, Northington GM, Asfaw T, Harvie H, Malykhina A. Evidence of bladder oversensitivity in the absence of an infection in premenopausal women with a history of recurrent urinary tract infections. BJU Int. 2012;110(2):247-251.
Cabrera C, Artacho R, Gimenez R. Beneficial effects of green tea — a review. J Am Coll Nutr. 2006;25(2):79-99.
Chan WK, Lam DT, Law HK, et al. Ganoderma lucidum mycelium and spore extracts as natural adjuvants for immunotherapy. J Altern Complement Med. 2005;11(6):1047-1057.
Chen SL, Wu M, Henderson JP, et al. Genomic diversity and fitness of E. coli strains recovered from the intestinal and urinary tracts of women with recurrent urinary tract infections. Sci Transl Med. 2013;5(184):184ra60.
Doron S, Gorbach SL. Probiotics: their role in the treatment and prevention of disease. Expert Rev Anti Infect Ther. 2006;4(2):261-275.
Dryden GW Jr, Deaciuc I, Arteel G, McClain CJ. Clinical implications of oxidative stress and antioxidant therapy. Curr Gastroenterol Rep. 2005;7(4):308-316.
Epp A, Larochelle A, Lovatsis D, Walter JE, Easton W, Farrell SA. Recurrent urinary tract infection. J Obstet Gynaecol Can. 2010;32(11):1082-1101.
Gagyor I, Bleidorn J, Kochen MM, Schmiemann G, Wegscheider K, Hummers-Pradier E. Ibuprofen versus fosfomycin for uncomplicated urinary tract infection in women: randomised controlled trial. BMJ. 2015;351:h6544.
Griffin C. Probiotics in obstetrics and gynaecology. Aust N Z J Obstet and gynaecol. 2015;55(3):201-209.
Aust N Z J Obstet and gynaecol. 2015;55(3):201-209.
Grover ML, Bracamonte JD, Kanodia AK, et al. Assessing adherence to evidence-based guidelines for the diagnosis and management of uncomplicated urinary tract infection. Mayo Clin Proc. 2007;82(2):181-185.
Guay DR. Cranberry and urinary tract infections. Drugs. 2009;69(7):775-807.
Heitzman ME, Neto CC, Winiarz E, Vaisberg AJ, Hammond GB. Ethnobotany, phytochemistry and pharmacology of Uncaria (Rubiaceae). Phytochemistry. 2005;66(1):5-29.
Hickerson AD, Carson CC. The treatment of urinary tract infections and use of ciprofloxacin extended release. Expert Opin Investig Drugs. 2006;15(5):519-532.
Hoesl CE, Altwein JE. The probiotic approach: an alternative treatment in urology. Eur Urol. 2005;47(3):288-296.
Horl WH. Urinary tract infections. Internist. 2011;52(9):1026, 1028-1031.
Kodner CM, Gupton EK. Recurrent urinary tract infrections in women: diagnosis and management. Am Fam Physician. 2010;82(6):638-643.
Am Fam Physician. 2010;82(6):638-643.
Litza J, Brill J. Urinary tract infections. Prim Care. 2010;37(3):491-507.
Marelli G, Papaleo E, Ferrari A. Lactobacilli for prevention of urogenital infections: a review. Eur Rev Med Pharmacol Sci. 2004;8(2):87-95.
Marschall J, Carpenter CR, Fowler S, Trautner BW. Antibiotic prophylaxis for urinary tract infections after removal of urinary catheter: meta-analyis. BMJ. 2013;346:f3147.
Marx JA, Hockberger RS, Walls RM, eds. Rosen’s Emergency Medicine. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014.
McMurdo ME, Argo I, Phillips G, Daly F, Davey P. Cranberry or trimethoprim for the prevention of recurrent urinary tract infections? A randomized controlled trial in older women. J Antimicrob Chemother. 2009;63(2):389-395.
Mishra B, Srivastava S, Singh K, Pandey A, Agarwal J. Symptom-based diagnosis of urinary tract infection in women: are we over-prescribing antibiotics? Int J Clin Pract. 2012;66(5):493-498.
2012;66(5):493-498.
Ochoa S, Malaga G. Recommendations of the consensus conference “diagnostic and therapeutic management of urinary tract infection in childhood.” An Pediatr (Barc). 2007;67(5):517-525.
Peterson J, Kaul S, Khashab M, Fisher AC, Kahn JB. A double-blind, randomized comparison of levofloxacin 750 mg once-daily for five days with ciprofloxacin 400/500 mg twice-daily for 10 days for the treatment of complicated urinary tract infections and acute pyelonephritis. Urology. 2008;71(1):17-22.
Pigrau-Serrallach C. Recurrent urinary tract infections. Enferm Infecc Microbiol Clin. 2005;23 Suppl 4:28-39.
Quintus J, Kovar KA, Link P, Hamacher H. Urinary excretion of arbutin metabolites after oral administration of bearberry leaf extracts. Planta Med. 2005;71(2):147-152.
Reid G, Bruce AW. Probiotics to prevent urinary tract infections: the rationale and evidence. World J Urol. 2006;24(1):28-32.
Rossignol L, Maugat S. Blake A, et al. Risk factors for resistance in urinary tract infections in women in general practice: a cross-sectional survey. J Infect. 2015;71(3):302-311.
Blake A, et al. Risk factors for resistance in urinary tract infections in women in general practice: a cross-sectional survey. J Infect. 2015;71(3):302-311.
Schindler G, Patzak U, Brinkhaus B. et al. Urinary excretion and metabolism of arbutin after oral administration of Arctostaphylos uvae ursi extract as film-coated tablets and aqueous solution in healthy humans. J Clin Pharmacol. 2002;42(8):920-927.
Schwenger EM, Tejani AM, Lowewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev. 2015; 12.
Simopoulos AP. Omega-3 fatty acids in inflammation and autoimmune diseases. J Am Coll Nutr. 2002;21(6):495-505.
Sufka KJ, Roach JT, Chambliss WG Jr, et al. Anxiolytic properties of botanical extracts in the chick social separation-stress procedure. Psychopharmacology (Berl). 2001;153(2):219-224.
Vahlensieck W, Bauer H. Prevention and alternative methods for prophylaxis of recurrent urinary tract infections in women. Urologe A. 2006;45(4):446-450.
Urologe A. 2006;45(4):446-450.
van Pinxteren B, van Vliet SM, Wiersma TJ, Goudswaard AN. Summary of the practice guideline ‘Urinary-tract infections’ (second revision) from the Dutch College of General Practitioners. Ned Tijdschr Geneeskd. 2006;150(13):718-722.
Vincent CR, Thomas TL, Reyes L, White CL, Canales BK, Brown MB. Symptoms and risk factors associated with first urinary tract infection in college age women: a prospective cohort study. J Urol. 2013;189(3):904-910.
Urinary Tract Infection (Homeopathy) – Health Information Library
Primary Remedies
Cantharis
Strong urging to urinate—with cutting pains that are felt before the urine passes, as well as during and after—may indicate a need for this remedy. Only several drops pass at a time, with a scalding sensation. The person may feel as if the bladder has not been emptied, still feeling a constant urge to urinate.
The person may feel as if the bladder has not been emptied, still feeling a constant urge to urinate.
Nux vomica
Irritable bladder with a constant need to urinate, passing only small amounts, suggests a need for this remedy. Burning or cramping pain may be felt in the bladder area, with an itching sensation in the urethra while the urine passes. The person may feel very irritable, impatient, and chilly. Symptoms may be relieved by hot baths or other forms of warmth.
Sarsaparilla
This remedy is often useful in cystitis and often helps when symptoms are unclear, or if other remedies have not been effective. Frequent urging is felt, with burning pain at the end of urination. Urine passes when the person is standing up, but only dribbling occurs while sitting. Flakes or sediment are sometimes seen in the urine. (Sarsaparilla is sometimes helpful when stones are forming or the kidneys are involved; however, these conditions need a doctor’s care. )
)
Other Remedies
Aconitum apellus
This remedy is often useful when a person feels anxious both before and during urination, with hot, scanty urine, and a burning or spasmodic feeling in the outlet of the bladder. It can also be helpful if retention of urine occurs after a person has been very cold and chilled, or after a shaking experience.
Apis mellifica
This remedy is indicated when the person frequently needs to urinate, but only small quantities are passed. Stinging and burning sensations are felt (especially with the last few drops) and the person may also experience soreness in the abdomen. Heat and touch make the symptoms worse, and cold applications, cool bathing, and open air bring relief. A lack of thirst is another indication that Apis may be needed.
Belladonna
This remedy may be beneficial if urging to urinate is frequent and intense, and the bladder feels very sensitive. A cramping or writhing sensation may be felt in the bladder area. Small amounts of highly-colored urine pass. (This remedy is sometimes helpful if a person passes small amounts of blood and no serious cause can be found on medical examination.)
A cramping or writhing sensation may be felt in the bladder area. Small amounts of highly-colored urine pass. (This remedy is sometimes helpful if a person passes small amounts of blood and no serious cause can be found on medical examination.)
Berberis vulgaris
Cystitis with twinges of cutting pain, or a burning feeling that extends to the urethra and its opening, may indicate a need for this remedy. The passage may also burn at times when no attempt at urination is being made. After emptying the bladder, the person feels as if some urine still remains inside. Urging and discomfort are often worse from walking.
Borax
This remedy can be helpful for cystitis with smarting pain in the urinary opening and aching in the bladder, with a feeling that the urine is retained. Children may cry or shriek, afraid to urinate because they know the pain is coming. Borax is often indicated for people who are sensitive to noise and inclined toward motion sickness.
Chimaphila umbellata
If a person has a troublesome urge to urinate but has to strain (or even stand up and lean forward) to make it pass, this remedy may be useful. A scalding sensation may be felt while the urine flows, with a feeling of straining afterward.
Clematis
This remedy may be indicated if a person has to urinate frequently with only a small amount being passed. A feeling of constriction is felt in the urinary passage, and the flow may be interrupted, or there may be dribbling afterward. A tingling sensation may occur, lasting long after urination is finished.
Equisetum
If cystitis is accompanied by dull but distressing pain and a feeling of fullness in the bladder, even after urinating, this remedy may be helpful. Urging and discomfort are more intense when the bladder has recently been emptied, improving over time as the bladder become more full.
Lycopodium
This remedy may be helpful if a person has to urinate frequently during the night and passes large amounts of urine. Or the person may feel a painful urge, but has to strain to make the urine flow. Pain may be felt in the back before the urine passes. (If fever is present, the urine has a reddish color, or discomfort is felt in the kidney region, the person should see a doctor.)
Sepia
This remedy may be helpful if a person has to urinate frequently, with sudden urging, a sense that urine will leak if urination is delayed, and small amounts of involuntary urine loss. The person may experience a bearing-down feeling in the bladder region, or pressure above the pubic bone. A person who needs this remedy often feels worn-out and irritable, with cold extremities, and a lax or sagging feeling in the pelvic area.
Staphysagria
This remedy is often indicated for cystitis that develops in a woman after sexual intercourse, especially if sexual activity is new to her, or if cystitis occurs after every occasion of having sex. Pressure may be felt in the bladder after urinating, as if it is still not empty. A sensation that a drop of urine is rolling through the urethra, or a constant burning feeling, are other indications. Staphysagria is also useful for cystitis that develops after illnesses with extended bed rest, or after the use of catheters.
Pressure may be felt in the bladder after urinating, as if it is still not empty. A sensation that a drop of urine is rolling through the urethra, or a constant burning feeling, are other indications. Staphysagria is also useful for cystitis that develops after illnesses with extended bed rest, or after the use of catheters.
Solidago compositum C injection 2 ml No. 100
Intramuscularly, 1 ampoule 1-3 times a week. The frequency and duration of the drug is determined by the attending physician. The course of treatment is 3 weeks.
Anti-inflammatory, immunomodulatory, reparative, diuretic, antispasmodic, antiseptic drug. The action of the drug is based on the activation of the body’s defenses and the normalization of impaired functions due to substances of plant, mineral and animal origin, which are part of the drug.
Indications for individual components:
Solidago virgaurea – Kidney weakness (diuretic effect).
Berberis vulgaris – Dry skin eruptions, diseases of the liver and gallbladder; diseases of the kidneys and bladder, for example, nephritis, nephrolithiasis, cystitis.
Vesica urinaria suis – Cystitis, bladder tenesmus, prostate adenoma.
Pyelon suis – Hydronephrosis, chronic pyelitis, nephrolithiasis.
Ureter suis – Disorders of the excretory functions of the kidneys, nephrolithiasis, hydronephrosis, nephrosis.
Urethra suis – Chronic irritation of the urethra and urinary organs, narrowing of the urethra.
Terebinthina laricina – (focal) Nephritis, cystopyelitis, nephrolithiasis, hematuria.
Mercurius sublimatus corrosivus – Acute inflammation of the mucous membrane of the kidneys and urinary tract.
Arsenicum album – Inflammation of varying severity in various organs and tissues; benign and malignant tumors.
Cuprum sulfuricum – Spasms of smooth and striated muscles, convulsions at night.
Bucco – Diseases of the urinary organs.
Hepar sulfuris – Inflammation and suppuration of mucous membranes; increased nervous sensitivity; prostate adenoma in combination with urination disorders.
Capsicum annuum – Inflammation of the mucous membrane of the bladder and ureters.
Orthosiphon aristatus – Kidney and bladder stones, uric acid diathesis.
Equisetum hyemale – Diseases of the kidneys and urinary tract.
Pareira brava – Bladder disorders, inflammation of the urethra, prostate enlargement.
Cantharis – Acute inflammation of the mucous membranes and urinary organs.
Apisinum – Inflammation and diseases accompanied by accumulation of fluid in tissues and organs; allergies.
Baptisia tinctoria – Severe febrile infections; general blood poisoning; clouding of consciousness.
Natrium pyruvicum – Influencing factor in the citric acid cycle and redox systems.
Pyrogenium-Nosode – Severe febrile infectious diseases; susceptibility to septic conditions.
Sarsaparilla – Urinary irritations.
Bacterium coli – Nosode – Urinary tract infections, eg pyelitis, cystitis, urinary tanesmus (aggravated by damp weather).
Coxsackie-Virus A9-Nosode – Diseases of the urinary tract, eg cystopyelitis, inflammation of the bladder, urethritis, prostatitis), diseases of the epididymis.
Argentum nitricum – Psychosomatic diseases of the digestive tract; migraine; chronic catarrhs of the mucous membranes, incontinence, nephritis.
Cystosan granules 20 g
Directions for use
In acute and subacute conditions, take 3-5 granules up to 6 times a day until symptoms change; further – 1 – 3 granules 2-3 times a day with breaks for 1-2 days a week.
Course application – 1-2 granules 1-2 times a day for a long time, with breaks for 1-2 days a week and 5-7 days after each month of admission.
It is well supplemented with Edemin for edema, Prostatin and Mammosan for chronic diseases of the urogenital area.
HOMEOPHYTOTHERAPY tinctures can serve as an addition to the drug: Birch, Cowberry, Budra, Heather, Gryzhnik, Spruce, St.
Description
CISTOSAN – complex homeopathic preparation
Therapeutic action: neuroregulatory, anti-inflammatory, neurovegetative.
Indications for the use of the components of the complex:
1. BELLADONNA – Belladonna C9 (Belladonna – Belladonna in breeding 10 – 18).
– Anti-inflammatory, anti-spastic, anti-allergic agent that regulates vasomotor disorders. It also regulates vegetative and volitional functions, incl. urination and urination.
– Promotes the regulation of cerebral vascular tone, relieves pain, spasms and inflammation.
– Action on the nervous system (including sensory endings of the facial nerve), lymphatic system, mucous membranes, synovial membranes, muscles, blood vessels, skin, tissue.
– Angina (relieves inflammation of the mucous membranes of the throat, improves blood flow, relieves pain and spasms), bronchitis, pneumonia, boils, carbuncles, erysipelas, rheumatism, cystitis, nephritis, convulsions in children, chorea, epilepsy.
– Acute, sudden, violent course of the disease, worse from the slightest external irritation; headaches – throbbing, with flushes.




 Uva-ursi may interact with lithium. There is a possibility that a compound in uva-ursi can have a thinning effect on the retina. DO NOT use daily as long-term therapy.
Uva-ursi may interact with lithium. There is a possibility that a compound in uva-ursi can have a thinning effect on the retina. DO NOT use daily as long-term therapy.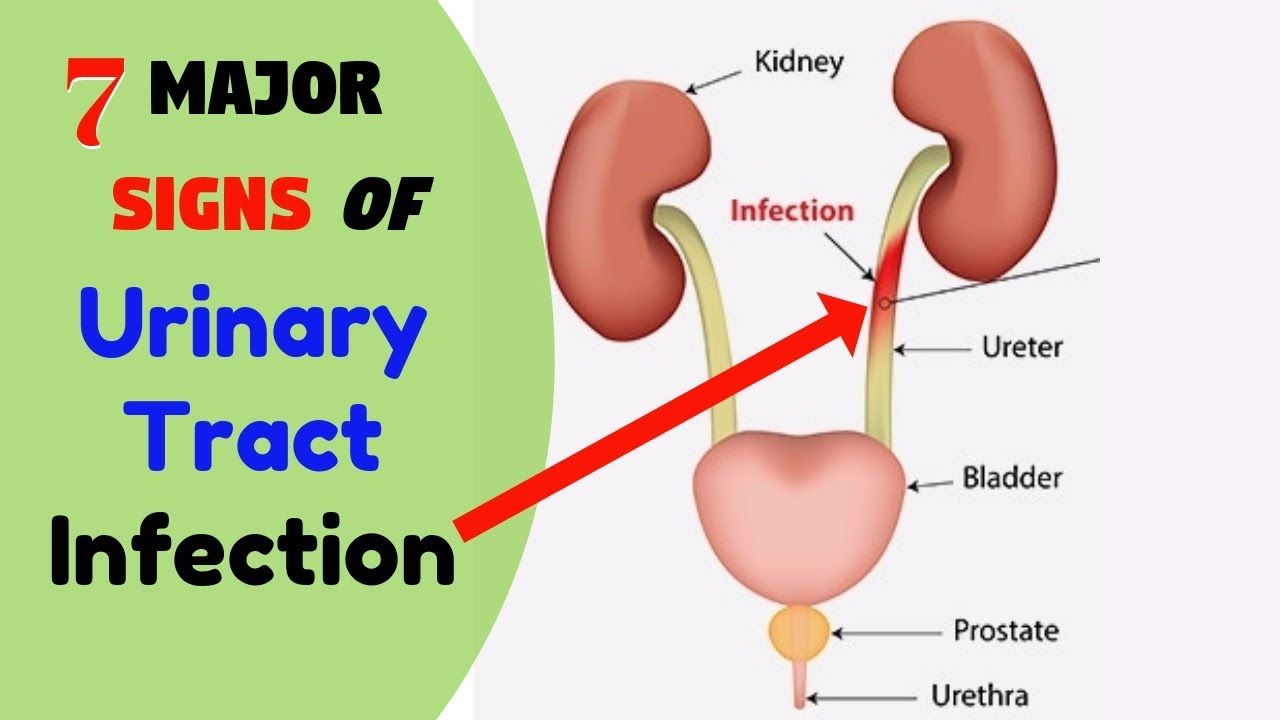 Symptoms worsen at night and tend to be accompanied by chills and sweating. Urine is dark and only small amounts pass. Burning sensation is often worse when the individual is not urinating.
Symptoms worsen at night and tend to be accompanied by chills and sweating. Urine is dark and only small amounts pass. Burning sensation is often worse when the individual is not urinating. For UTIs usually associated with sexual intercourse or following extreme embarrassment or humiliation, particularly from sexual abuse. This remedy is most appropriate for those who have an urgent desire to urinate and have the sensation that a single drop of urine is still present even following urination.
For UTIs usually associated with sexual intercourse or following extreme embarrassment or humiliation, particularly from sexual abuse. This remedy is most appropriate for those who have an urgent desire to urinate and have the sensation that a single drop of urine is still present even following urination.