Gallstones pain after eating. Gallstone Disease Treatment: Comprehensive Guide to Managing Gallbladder Pain After Eating
What are the treatment options for gallstone disease. How can you manage gallbladder pain after eating. What are the surgical and non-surgical approaches to treating gallstones. How do doctors diagnose and treat complications of gallbladder disease.
Understanding Gallstone Disease and Its Symptoms
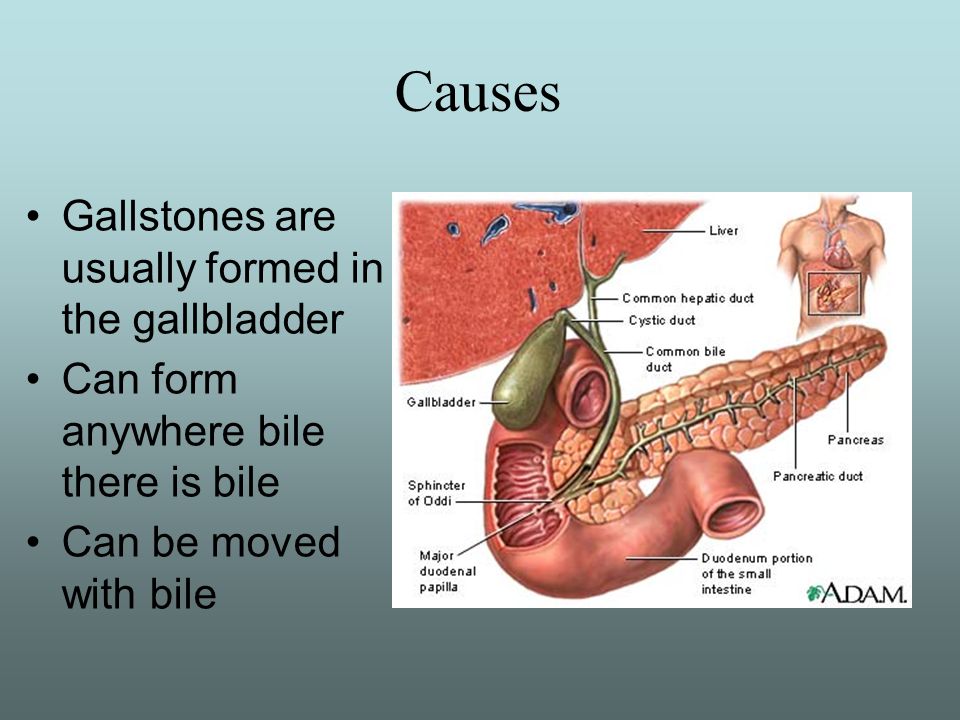
Gallstone disease is a common condition that affects millions of people worldwide. It occurs when small, hardened deposits form in the gallbladder, potentially causing pain and discomfort, especially after eating. But what exactly are gallstones, and how do they form?
Gallstones are solid, pebble-like formations that develop in the gallbladder. They can vary in size from as small as a grain of sand to as large as a golf ball. These stones are typically composed of cholesterol or bilirubin, a waste product created when red blood cells break down.
Common Symptoms of Gallstone Disease
- Sharp pain in the upper right abdomen
- Pain that radiates to the back or right shoulder
- Nausea and vomiting
- Fever and chills
- Yellowing of the skin and eyes (jaundice)
Why do gallstones cause pain after eating? When you consume food, especially fatty meals, your gallbladder contracts to release bile into the digestive system. If gallstones are present, they can block the bile ducts, causing pain and discomfort known as a gallbladder attack.
Medication as a Treatment Option for Gallstones
For some patients with symptomatic gallstones, medication can be an effective treatment option. These medications are designed to either interfere with the development of gallstones in the gallbladder or dissolve existing stones.
Types of Medications Used for Gallstone Treatment
- Ursodeoxycholic acid (Ursodiol)
- Chenodeoxycholic acid (Chenodiol)
Are medications suitable for all types of gallstones? No, these medications are most effective for patients with small, non-calcified cholesterol stones and whose gallbladder is functioning normally. The treatment typically takes at least six to twelve months to show results.
It’s important to note that while medication can be effective, there is a chance that gallstones may recur within five years after treatment. This is why many doctors recommend surgery as a more permanent solution for symptomatic gallstones.
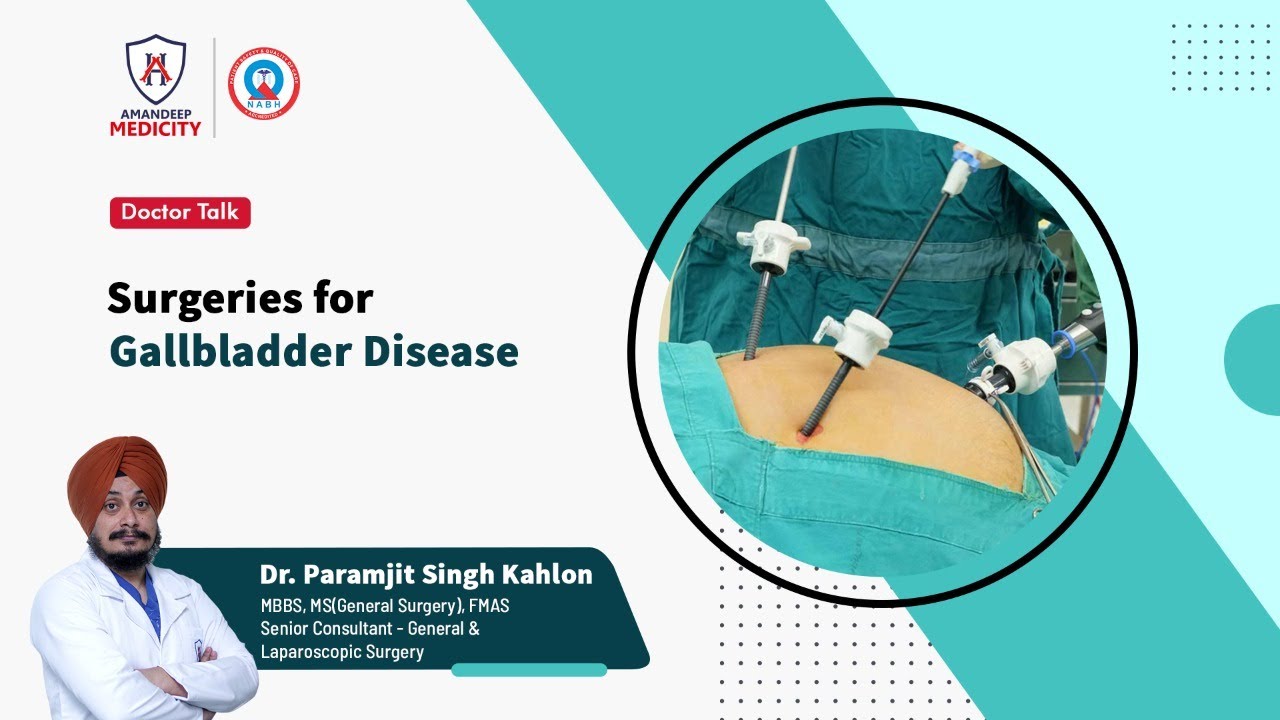
Surgical Approaches to Treating Gallstone Disease
Surgery remains the most definitive treatment for symptomatic gallstones. The procedure, known as cholecystectomy, involves the removal of the gallbladder. This approach not only eliminates existing gallstones but also prevents future stone formation.

Laparoscopic Cholecystectomy: The Gold Standard
Laparoscopic cholecystectomy has become the most common surgical procedure for gallstone removal. This minimally invasive approach offers several advantages over traditional open surgery:
- Smaller incisions
- Less post-operative pain
- Shorter hospital stay
- Faster recovery and return to normal activities
During a laparoscopic cholecystectomy, the surgeon makes a few small incisions in the abdomen. A miniature video camera and specialized instruments are inserted through these incisions, allowing the surgeon to remove the gallbladder without the need for a large open incision.
In some cases, the surgeon may need to switch from a laparoscopic approach to an open procedure. This decision is made based on factors such as scarring, infection, or other complications that may arise during the surgery.
Non-Surgical Alternatives for Gallstone Management
While surgery is often the preferred treatment for gallstones, there are several non-surgical alternatives available for patients who may not be suitable candidates for surgery or who prefer to avoid it.

Extracorporeal Shock Wave Lithotripsy (ESWL)
ESWL is a non-invasive procedure that uses high-energy sound waves to break up gallstones. This treatment is suitable for patients with small stones and a normally functioning gallbladder. The procedure doesn’t require anesthesia and can often be performed on an outpatient basis.
How does ESWL work? The shock waves produced by the machine are strong enough to fracture and disintegrate the gallstones. Once broken into smaller pieces, these fragments can pass more easily through the bile ducts.
Percutaneous Gallstone Removal
For high-risk patients who cannot undergo surgery, percutaneous (through the skin) treatment approaches may be considered. These procedures involve:
- Cholecystostomy: Opening the gallbladder and removing stones using a device called a cholecystoscope.
- Contact dissolution therapy: Injecting a solvent directly into the gallbladder to dissolve cholesterol stones.
These percutaneous methods can provide relief for patients who are not candidates for traditional surgical approaches.
Endoscopic Gallbladder Stenting: A Novel Approach
Endoscopic gallbladder stenting is another non-surgical treatment option for gallstones, particularly useful in high-risk patients who cannot undergo surgery due to other health conditions.
How is endoscopic gallbladder stenting performed? During this procedure, the doctor performs an Endoscopic Retrograde Cholangiopancreatography (ERCP) and inserts a stent from the gallbladder to the duodenum. This stent helps to relieve biliary symptoms and prevent complications by allowing bile to flow more freely.
While this approach doesn’t remove the gallstones, it can provide significant symptom relief for patients who are not candidates for more invasive treatments.
Managing Complications of Gallbladder Disease
Gallstone disease can lead to several complications, some of which can be life-threatening if left untreated. Understanding these complications and their treatments is crucial for comprehensive gallstone management.
Acute Cholecystitis
Acute cholecystitis is the most common complication of gallstone disease. It occurs when a gallstone becomes impacted in the cystic duct, trapping bile in the gallbladder and causing inflammation and damage.
How is acute cholecystitis treated? In most cases, a cholecystectomy (removal of the gallbladder) is the best treatment for acute cholecystitis. This procedure not only addresses the immediate inflammation but also prevents future gallstone formation.
Choledocholithiasis
Choledocholithiasis occurs when gallstones become displaced to the common bile duct rather than remaining in the gallbladder. This condition can lead to severe complications if left untreated.
What is the treatment for choledocholithiasis? An ERCP (Endoscopic Retrograde Cholangiopancreatography) is typically performed to both diagnose and treat gallstones in the common bile duct. During this procedure, the doctor can remove the stones and clear the duct.
Rare Complications and Their Management
While less common, several other complications can arise from gallstone disease. These require specialized treatment approaches:
Cholecystoenteric Fistulas
These fistulas form when a large gallstone erodes through the gallbladder wall into the bowel. Treatment typically involves both cholecystectomy and bowel resection to repair the damage and prevent further complications.

Mirizzi’s Syndrome
Mirizzi’s syndrome results from a gallstone blocking the cystic duct and compressing the common bile duct, leading to inflammation. ERCP is often used to diagnose and treat this condition, sometimes in combination with surgery.
Porcelain Gallbladder
Porcelain gallbladder occurs when the gallbladder wall calcifies or hardens, usually due to chronic inflammation from gallstones. This condition increases the risk of gallbladder cancer.
What is the recommended treatment for porcelain gallbladder? Due to the increased cancer risk, removal of the gallbladder (cholecystectomy) is typically recommended for patients with porcelain gallbladder.
Understanding these complications and their treatments is crucial for both patients and healthcare providers in managing gallstone disease effectively. Early recognition and appropriate intervention can prevent more serious health issues and improve overall outcomes for patients with gallbladder problems.
Lifestyle Changes to Support Gallstone Treatment
While medical and surgical interventions are often necessary for treating gallstones, certain lifestyle modifications can support treatment and potentially reduce the risk of future gallstone formation.

Dietary Adjustments
- Reduce intake of saturated fats and cholesterol
- Increase consumption of fiber-rich foods
- Maintain a healthy weight through balanced nutrition
- Stay hydrated to support proper bile flow
Can dietary changes alone treat gallstones? While dietary modifications alone are unlikely to dissolve existing gallstones, they can help manage symptoms and may reduce the risk of developing new stones after treatment.
Exercise and Weight Management
Regular physical activity and maintaining a healthy weight can contribute to overall gallbladder health. Exercise helps stimulate gallbladder contractions, promoting better bile flow and potentially reducing the risk of stone formation.
How much exercise is recommended? Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, as recommended by health authorities.
Stress Reduction Techniques
Chronic stress may contribute to gallbladder problems by affecting digestion and overall health. Incorporating stress-reduction techniques into your daily routine can support gallbladder health:
- Meditation and mindfulness practices
- Yoga or tai chi
- Deep breathing exercises
- Regular relaxation time
By adopting these lifestyle changes alongside medical treatment, patients can take an active role in managing their gallstone disease and promoting overall digestive health.
Follow-up Care and Long-term Management of Gallstone Disease
After receiving treatment for gallstones, whether through medication, surgery, or other interventions, ongoing care and management are essential to ensure long-term health and prevent recurrence.
Post-Treatment Monitoring
Regular follow-up appointments with your healthcare provider are crucial to monitor your recovery and address any potential complications. These appointments may include:
- Physical examinations
- Blood tests to check liver function
- Imaging studies such as ultrasounds or CT scans, if necessary
How often should follow-up appointments be scheduled? The frequency of follow-up visits will depend on the type of treatment you received and your individual health status. Your doctor will provide a personalized follow-up plan.

Long-term Dietary Considerations
Even after successful treatment, maintaining a gallstone-friendly diet can help prevent future problems. This may include:
- Continuing to limit high-fat foods
- Eating smaller, more frequent meals
- Gradually reintroducing foods that may have triggered symptoms before treatment
It’s important to work with a nutritionist or dietitian to develop a long-term eating plan that supports your gallbladder health while meeting your nutritional needs.
Monitoring for Recurrence
While treatments like cholecystectomy eliminate the risk of gallstone recurrence in the gallbladder, stones can still potentially form in the bile ducts. Staying vigilant about potential symptoms and maintaining regular check-ups can help catch any issues early.
What symptoms should you watch for? Be alert for signs such as abdominal pain, jaundice, or unexplained fever, and report these to your healthcare provider promptly.
Psychological Support
Dealing with gallstone disease and its treatments can be stressful. Some patients may benefit from psychological support to cope with the emotional aspects of their condition and recovery. This might include:
- Individual counseling
- Support groups for gallbladder disease patients
- Stress management techniques
By focusing on comprehensive, long-term care and management, patients can maximize the benefits of their gallstone treatment and maintain optimal digestive health for years to come.
Gallstone Disease Treatment | Johns Hopkins Medicine
If you experience symptomatic gallstones, there are a number of different treatment options available. Your exact course of treatment will depend on your symptoms and the characteristics of the gallstones you have. The goal of treatment is to relieve symptoms and prevent complications from developing. Treatment for gallstones includes:
- Medication
- Surgery
- Extracorporeal shock wave lithotripsy
- Percutaneous therapy
- Endoscopic gallbladder stenting
- Treating complications of gallstones
Gallstone Disease Treatment: Medication
There are several medications available for symptomatic gallstones, which are designed to:
- Interfere with the development of gallstones in the gallbladder
- Dissolve the stones
These medications are only useful in patients who have small, non-calcified cholesterol stones and whose gallbladder is functioning normally. Therapy takes at least six to 12 months. There is a chance that the gallstones will recur within five years.
Therapy takes at least six to 12 months. There is a chance that the gallstones will recur within five years.
Gallstone Disease Treatment: Surgery
Cholecystectomy is surgery to remove your gallbladder. It is the only treatment option to cure symptomatic gallstones. Laparoscopic cholecystectomy is the most common procedure instead of a traditional, open procedure. During a laparoscopic cholecystectomy, your surgeon:
- Makes a few small incisions in your abdomen rather than one large one
- Inserts a miniature video camera and laparoscopic instruments into the incision
- Removes the gallbladder and closes the incisions with stitches
Advantages of a laparoscopic procedure include:
- Less pain
- Shorter hospital stay
- Faster return to normal activities
Sometimes, a surgeon begins the procedure using a laparoscopic approach but then switches to an open approach because of scarring, infection or other complications.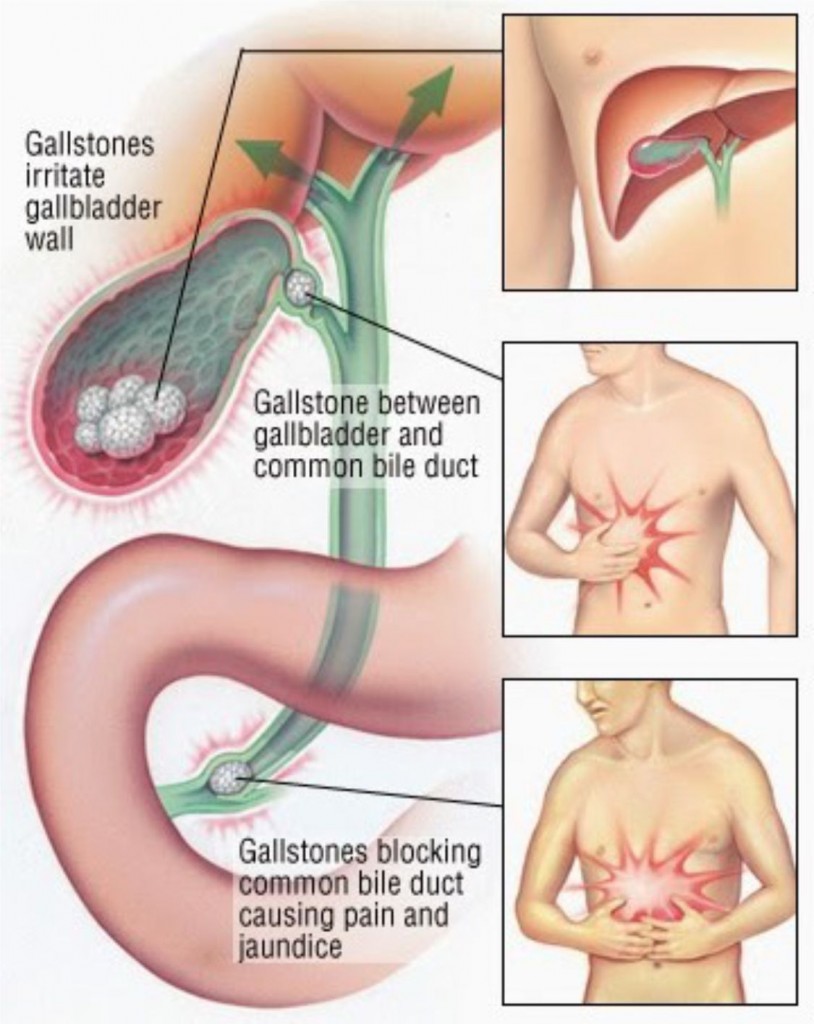 No matter which approach your doctor uses, he or she has your best possible outcome in mind.
No matter which approach your doctor uses, he or she has your best possible outcome in mind.
Gallstone Disease Treatment: Extracorporeal Shock Wave Lithotripsy
Extracorporeal shock wave lithotripsy (ESWL) is a nonsurgical alternative to manage gallstones. You can receive this treatment as long as your gallbladder is functioning normally and your stones are small.
You do not need anesthesia for ESWL, and the procedure may be performed as an outpatient. This method uses high-energy sound waves to produce shock waves. The shock waves are strong enough to fracture and disintegrate the gallstones.
Patients who cannot undergo surgery may be good candidates for ESWL.
Gallstone Disease Treatment: Percutaneous Therapy
In certain high-risk patients, surgery may be too dangerous. A percutaneous (through the skin) treatment approach may be used. During this procedure, your doctor opens the gallbladder, dilates the tract and removes any gallstones using a device called a cholecystoscope.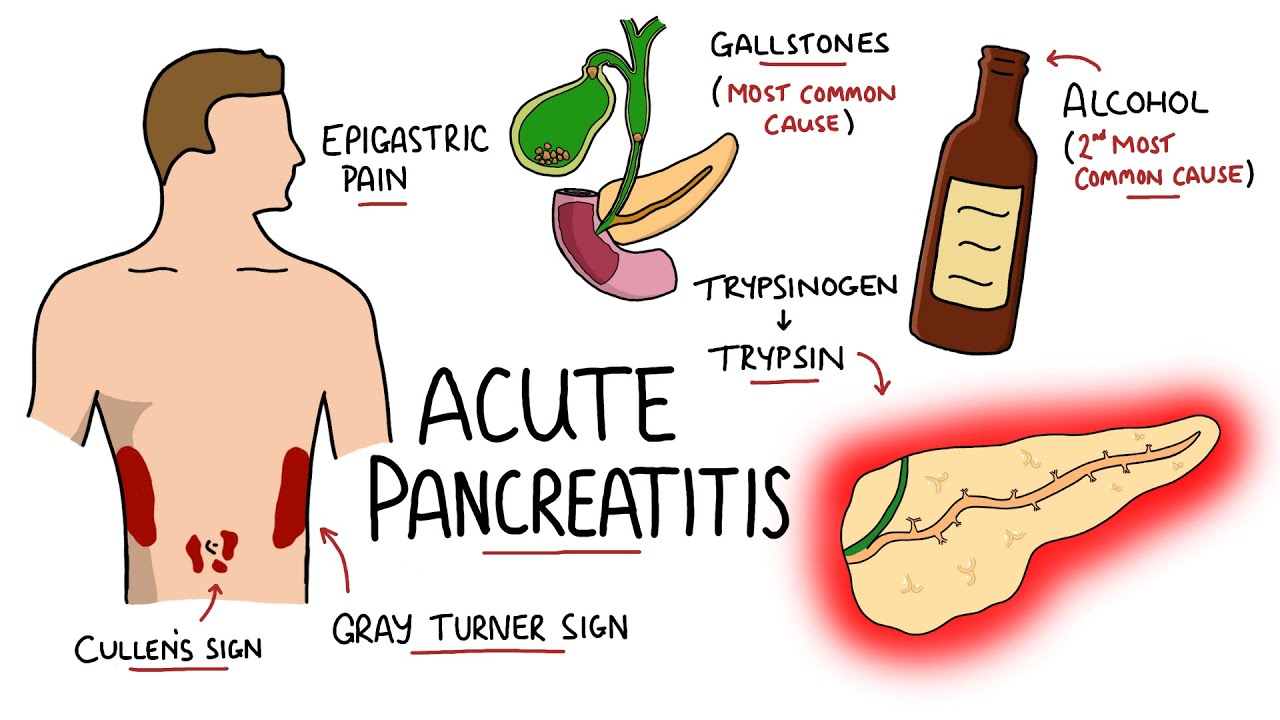
Another percutaneous method is called contact dissolution therapy. During this procedure, a catheter is inserted into your gallbladder, and a solvent is injected directly to the gallbladder. The solvent dissolves the cholesterol stones.
Gallbladder Disease Treatment: Endoscopic Gallbladder Stenting
Endoscopic gallbladder stenting is another nonsurgical approach to treat gallstones. It is useful in treating high-risk patients who cannot undergo surgery, usually due to an illness. During this procedure, your doctor performs an ERCP and inserts a stent from the gallbladder to the duodenum. The stent relieves biliary symptoms and complications.
Treating Complications of Gallbladder Disease
Certain complications may arise in patients with gallbladder disease. Your doctor will discuss with you the risks of complications.
- Acute cholecystitis: This is the most common complication, and it occurs when the gallstone becomes impacted in the cystic duct.
 The bile is then trapped in the gallbladder, causing damage and inflammation. Usually, a cholecystectomy (removal of the gallbladder) is the best treatment.
The bile is then trapped in the gallbladder, causing damage and inflammation. Usually, a cholecystectomy (removal of the gallbladder) is the best treatment. - Choledocholithiasis: This occurs when gallstones become displaced to the common bile duct rather than to the gallbladder. Choledocholithiasis can cause life-threatening conditions. An ERCP can be performed to diagnose and treat these gallstones.
Less common complications include:
- Cholecystoenteric fistulas, which form when a large stone erodes through the gallbladder into the bowel. Treatment involves cholecystectomy and bowel resection.
- Mirizzi’s syndrome is the result of a gallstone blocking the cystic duct, compressing the common bile duct and causing inflammation. ERCP is used to diagnose and treat it.
- Porcelain gallbladder occurs when the gallbladder wall calcifies (hardens), usually because of gallstones. This can lead to gallbladder cancer, so removal of the gallbladder is recommended.

Could Heartburn or Gallstones be Causing You Pain after Eating?
By James Kimbaris, MD, Gastroenterologist—Virtua Gastroenterology
There’s nothing worse than enjoying a great, delicious meal and then feeling sick soon after eating.
When the digestive system isn’t working well, issues can arise after you eat that cause pain and discomfort. The most common problems are gastroesophageal reflux disease and biliary colic (commonly known as heartburn and gallbladder attack).
Check out the symptoms and find out if it’s time to see a gastroenterologist.
Could it be heartburn?
Almost all adults experience heartburn at some point in their lives. This results from acids that churn up from the stomach and into the esophagus. When this happens, it causes a burning sensation in the middle of the chest and throat and can leave an unpleasant taste in the mouth.
Occasional reflux can be treated or prevented with over-the-counter medications—especially for younger, healthy patients. However, when heartburn persists over an extended period or is not responding to medication, your doctor may want you to have an upper endoscopy to rule out more serious issues. In this procedure, the doctor uses a thin camera (scope) to examine the esophagus and look for early changes in the lining that can lead to esophageal cancer.
However, when heartburn persists over an extended period or is not responding to medication, your doctor may want you to have an upper endoscopy to rule out more serious issues. In this procedure, the doctor uses a thin camera (scope) to examine the esophagus and look for early changes in the lining that can lead to esophageal cancer.
Tips to prevent heartburn
- Avoid high-fat foods such as burgers, ice cream and fried chicken.
- Avoid chocolate, caffeine and spicy foods.
- Avoid highly acidic foods such as oranges or tomato sauce.
- Stop smoking.
- Stop eating 2 to 3 hours before going to sleep. After-dinner snacking keeps stomach acids working at a time when you want your digestive system to settle down.
If you have heartburn that lasts a few weeks, see your doctor.
Is it a gallbladder attack?
Gallbladder attacks are another common digestive problem, and the culprit behind them is gallstones. These “stones” are mostly hardened cholesterol that create painful blockages in the gallbladder. The attacks usually occur after eating a fatty meal, and they can last for hours.
These “stones” are mostly hardened cholesterol that create painful blockages in the gallbladder. The attacks usually occur after eating a fatty meal, and they can last for hours.
Gallbladder attack symptoms include pain on the right or center of the belly area—usually under the rib cage or shoulder blade—that may be accompanied by nausea, vomiting and fever. If you experience these symptoms, call your doctor right away.
If the pain is severe and persists for several hours, go to the nearest emergency room because, in a worst-case scenario, the gallbladder could rupture.
Surgery often is required to remove the stones and gallbladder to prevent future attacks. The procedure, called a cholecystectomy, often is minimally invasive and performed through a few small incisions.
Who is at risk for gallbladder problems?
- Anyone over age 60
- People with a family history of gallstones
- People who have lost a significant amount of weight rapidly
- Those who are overweight or obese
- Women who are pregnant or have been pregnant, use hormone replacement therapy, or take birth control pills
If you suffer from persistent heartburn or gallbladder attacks, it’s time to have your symptoms evaluated by a doctor.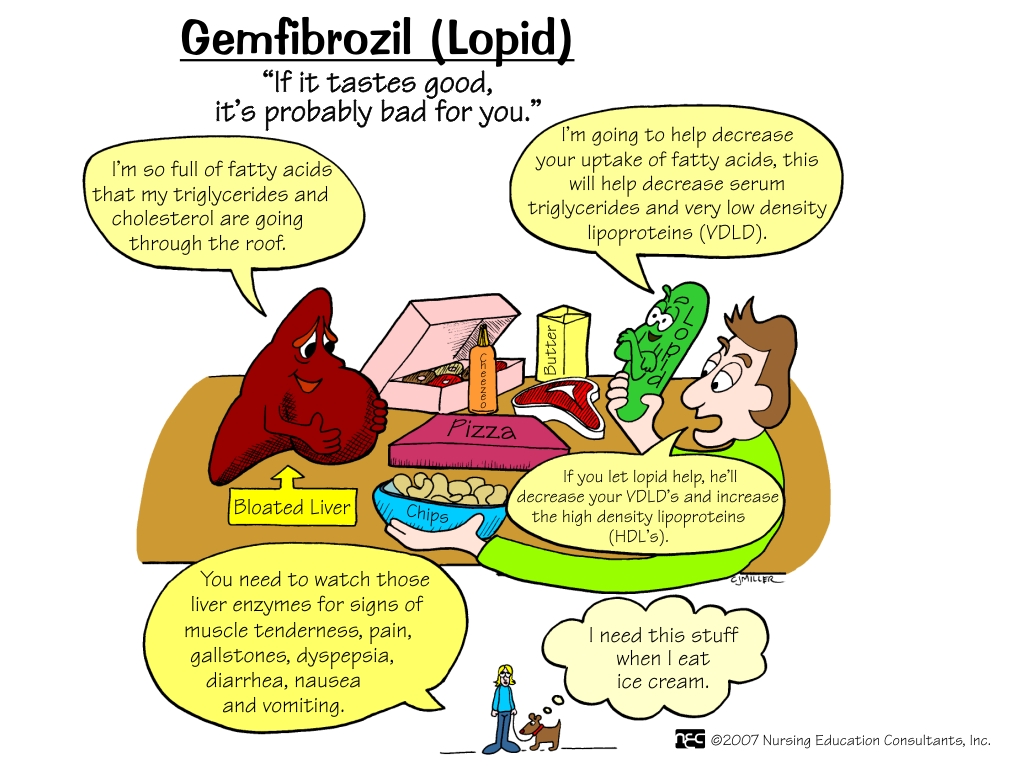
To make an appointment with a Virtua gastroenterologist, call 1-888-847-8823.
Updated January 31, 2022
Cholelithiasis: to operate or not?
Most patients who are aware of the presence of gallstones prefer to coexist peacefully with them. About what are the indications for the removal of the gallbladder, and in what cases it is possible to refrain from the operation, says the head. Department of Emergency and General Surgery EMC Vladimir Kan.
Calculous cholecystitis, cholelithiasis, or, as it is more commonly called, cholelithiasis, is a chronic inflammatory disease of the biliary tract, accompanied by the formation of gallstones.
With prolonged stagnation of bile in the gallbladder, which is facilitated by various metabolic disorders and a decrease in the contractility of the gallbladder, bile components (most often cholesterol) begin to crystallize and precipitate. Microscopic crystals – microlites – increase in size over time, merge with each other and form large stones.
What symptoms indicate the possible presence of gallstones?
The first warning signs are heaviness in the right hypochondrium, bitterness in the mouth and nausea after eating, which are common signs of diseases of the biliary tract. Often a person is unaware of the existence of gallstones until the moment when they are detected by ultrasound of the abdominal organs, and in the worst case, when biliary colic and other symptoms develop due to the ingress of stones from the gallbladder into the common bile duct and its blockage.
Gallbladder colic is pain in the right hypochondrium or “under the pit of the stomach”, in the epigastric region, due to the contraction of the walls of the gallbladder, which tends to push out the “cork” that clogged it. The intensity of the pain increases, then the pain becomes constant (up to several hours), after which it gradually decreases and disappears when the moving stone returns to the gallbladder cavity. There is no pain between attacks. But if the stone remains in the bile duct, then complications such as acute cholecystitis, obstructive jaundice, perforation of the gallbladder and the development of peritonitis can develop, which require emergency surgical care.
The intensity of the pain increases, then the pain becomes constant (up to several hours), after which it gradually decreases and disappears when the moving stone returns to the gallbladder cavity. There is no pain between attacks. But if the stone remains in the bile duct, then complications such as acute cholecystitis, obstructive jaundice, perforation of the gallbladder and the development of peritonitis can develop, which require emergency surgical care.
Is it necessary to remove the gallbladder if the stone does not bother?
Patients suffering from cholelithiasis are divided into two groups: patients with symptoms of biliary colic and a picture of acute cholecystitis, and patients in whom the presence of stones does not manifest itself in any way.
Currently, the vast majority of surgeons agree that patients with asymptomatic cholelithiasis with a first discovered small stone should not immediately undergo prophylactic cholecystectomy (gallbladder removal).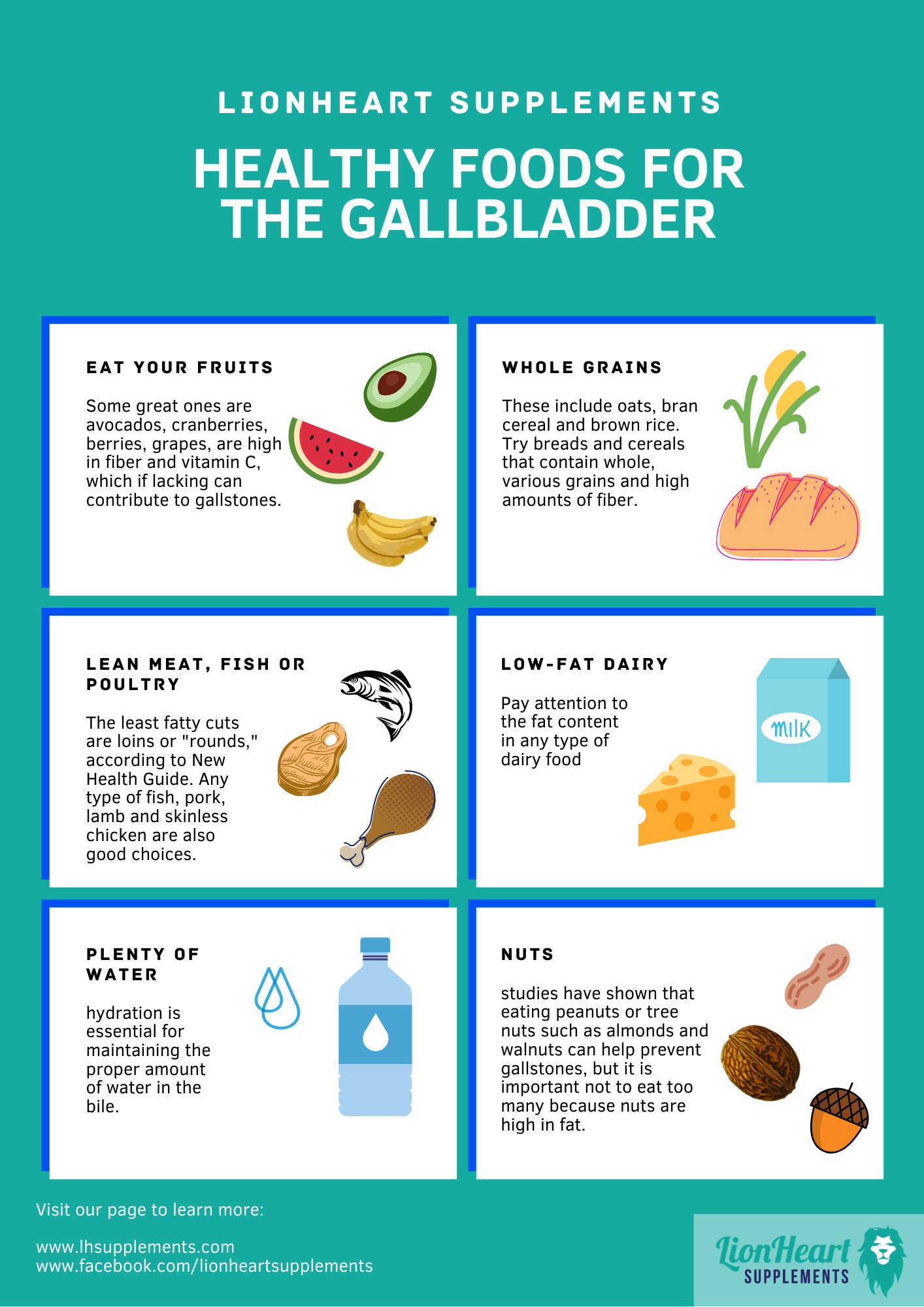 The risk of developing severe complications with small single stones is estimated to be low, therefore, such patients should undergo regular abdominal ultrasound examinations and follow lifestyle and nutrition recommendations.
The risk of developing severe complications with small single stones is estimated to be low, therefore, such patients should undergo regular abdominal ultrasound examinations and follow lifestyle and nutrition recommendations.
The presence of stones for many years is always accompanied by the addition of a secondary infection and the development of chronic cholecystitis, which entails various diseases of neighboring organs – the liver and pancreas. Long-term inflammation also increases the risk of developing gallbladder cancer. Therefore, the doctors of the EMC Surgical Clinic recommend that after observing asymptomatic stones for 2 years, nevertheless, contact the surgeon for advice. With some concomitant diseases (for example, diabetes mellitus), with large stones, with pathological changes in the gallbladder itself, the doctor may recommend removing the gallbladder in the “quiet period” of the disease after a comprehensive examination and preparation of the patient.
In the case of calculous cholecystitis, when the patient has intermittent attacks of biliary colic, surgeons recommend cholecystectomy, which should be performed in a planned manner. Each subsequent attack can cause the development of acute cholecystitis, which, as already noted, can be accompanied by severe complications from the liver and pancreas. If a picture of acute cholecystitis develops – biliary colic lasts more than 3 hours, pain is localized in the right upper quadrant of the abdomen, is not relieved by antispasmodic drugs, the temperature rises, nausea and vomiting occur – an ambulance should be called.
Each subsequent attack can cause the development of acute cholecystitis, which, as already noted, can be accompanied by severe complications from the liver and pancreas. If a picture of acute cholecystitis develops – biliary colic lasts more than 3 hours, pain is localized in the right upper quadrant of the abdomen, is not relieved by antispasmodic drugs, the temperature rises, nausea and vomiting occur – an ambulance should be called.
Doctors of the EMC Surgical Clinic are ready around the clock to perform surgery for calculous cholecystitis using the least traumatic and safest method – using laparoscopic access. Regardless of how many stones are found in the gallbladder – one large or many small – the gallbladder is removed completely. There are contraindications to laparoscopic cholecystectomy – in this case, the surgeon may decide to perform an open, laparotomy operation.
Is it possible to live without a gallbladder?
A pathologically altered gallbladder cannot fully perform its functions, and is the cause of constant pain and a source of chronic infection. Therefore, cholecystectomy, performed in accordance with the indications of a qualified physician, improves the patient’s condition and does not affect the function of digestion.
Therefore, cholecystectomy, performed in accordance with the indications of a qualified physician, improves the patient’s condition and does not affect the function of digestion.
When to run to a gastroenterologist?! – Euromed clinic
– Elena Evgenievna, what complaints do patients most often make?
The most common are abdominal pain and heartburn.
There are many causes of abdominal pain: from functional disorders due to stress to serious diseases.
Often worried about pain in the right hypochondrium due to dysfunction of the biliary tract, a feeling of discomfort in the epigastric region due to gastritis. In spring and autumn, peptic ulcer often worsens.
The situation can worsen against the background of stress and errors in nutrition. Moreover, as a rule, these two factors are interrelated: for many, stress is a trigger for eating disorders: someone has an increase in appetite or, conversely, disappears, and a person eats irregularly or overeats, reduces control over food quality, etc. All this inevitably leads to problems with the gastrointestinal tract.
All this inevitably leads to problems with the gastrointestinal tract.
Heartburn is not a separate disease, but a symptom: a burning sensation behind the sternum. In fact, this is a chemical burn by the acidic contents of the stomach when it is thrown into the esophagus, where the environment is often alkaline. This leads to damage to the esophageal mucosa by hydrochloric acid and the protein-cleaving enzyme pepsin. Sometimes with reflux disease, there is no heartburn, but there is a sensation of a lump in the throat, difficulty in swallowing, chest pain, which are confused with angina pectoris. All this significantly reduces the quality of life of the patient. This disease can and should be treated. Frequent reflux of acid from the stomach into the esophagus, especially with an admixture of bile from the duodenum, can even lead to oncological diseases of the esophagus.
Treatment is usually long-term, since the situation has developed over the years, and it will not be possible to change it instantly. In addition to medication, a change in lifestyle and eating habits is required. With the help of drugs, we can reduce the amount of acid products produced, which will lead to the fact that less of it will be thrown into the esophagus, respectively, heartburn is less manifested. There are also a number of drugs that absorb acid and remove it. These are fast acting tools. They help get rid of heartburn for 30-40 minutes. Usually, it is these drugs that are actively promoted in advertising and they will also be offered by a pharmacist in a pharmacy. The patient must, of course, be guided by the recommendations of the doctor.
In addition to medication, a change in lifestyle and eating habits is required. With the help of drugs, we can reduce the amount of acid products produced, which will lead to the fact that less of it will be thrown into the esophagus, respectively, heartburn is less manifested. There are also a number of drugs that absorb acid and remove it. These are fast acting tools. They help get rid of heartburn for 30-40 minutes. Usually, it is these drugs that are actively promoted in advertising and they will also be offered by a pharmacist in a pharmacy. The patient must, of course, be guided by the recommendations of the doctor.
Food for reflux disease should be in small portions so that the volume of food eaten does not exceed the volume of the stomach, and for better control of appetite – frequent: 4-5 times a day. Food should be chewed thoroughly for maximum grinding and release of more saliva, which, having an alkaline reaction, neutralizes the acid.
With reflux disease, boiled, baked, stewed vegetables, liquid cereals, pasta, lean meats, poultry, seafood, eggs, cottage cheese, stale bread and crackers, jelly, mousses, jelly, mashed soups, dairy products are recommended.
They increase acid formation in the stomach and therefore are not recommended: smoked meats, fatty, spicy, salty, mushrooms, raw vegetables, sour fruits and juices, carbonated drinks, black bread, muffins, fast food, strong tea and coffee
– Does a nutritional error lead to heartburn, or is its appearance still genetically determined?
– Both.
The peculiarity of the sphincters between the esophagus and the stomach is genetically determined. A fairly common problem is connective tissue dysplasia, that is, its increased elasticity, resulting in flat feet, varicose veins, “unstable vertebrae”, weakness of many sphincters, including the esophagogastric and esophageal openings of the diaphragm. That is, they do not close tightly enough, and food easily enters the stomach from the esophagus.
The number of parietal cells in the stomach is also genetically determined, which determines the quantity and quality of hydrochloric acid produced by them.
Heartburn in pregnancy
Pregnant women often complain of heartburn. This is due to two main points. Firstly, as the baby grows and the uterus grows, intra-abdominal pressure increases, the load on the stomach and intestines increases, which can provoke the reflux of acid and bile into the esophagus. By the way, this often leads to constipation in pregnant women. Secondly, pregnant women have a special hormonal background, aimed at reducing the tone of the uterus and, at the same time, the sphincters of the esophagus also relax, as a result of which acid reflux can occur.
If you have such problems, you don’t have to endure and wait that “it will go away by itself after childbirth” … Immediately contact a gastroenterologist. The doctor will select the treatment: there are drugs approved for use during pregnancy. Also, together with a gastroenterologist, you will discuss how you need to change your diet and lifestyle in order to get rid of this problem.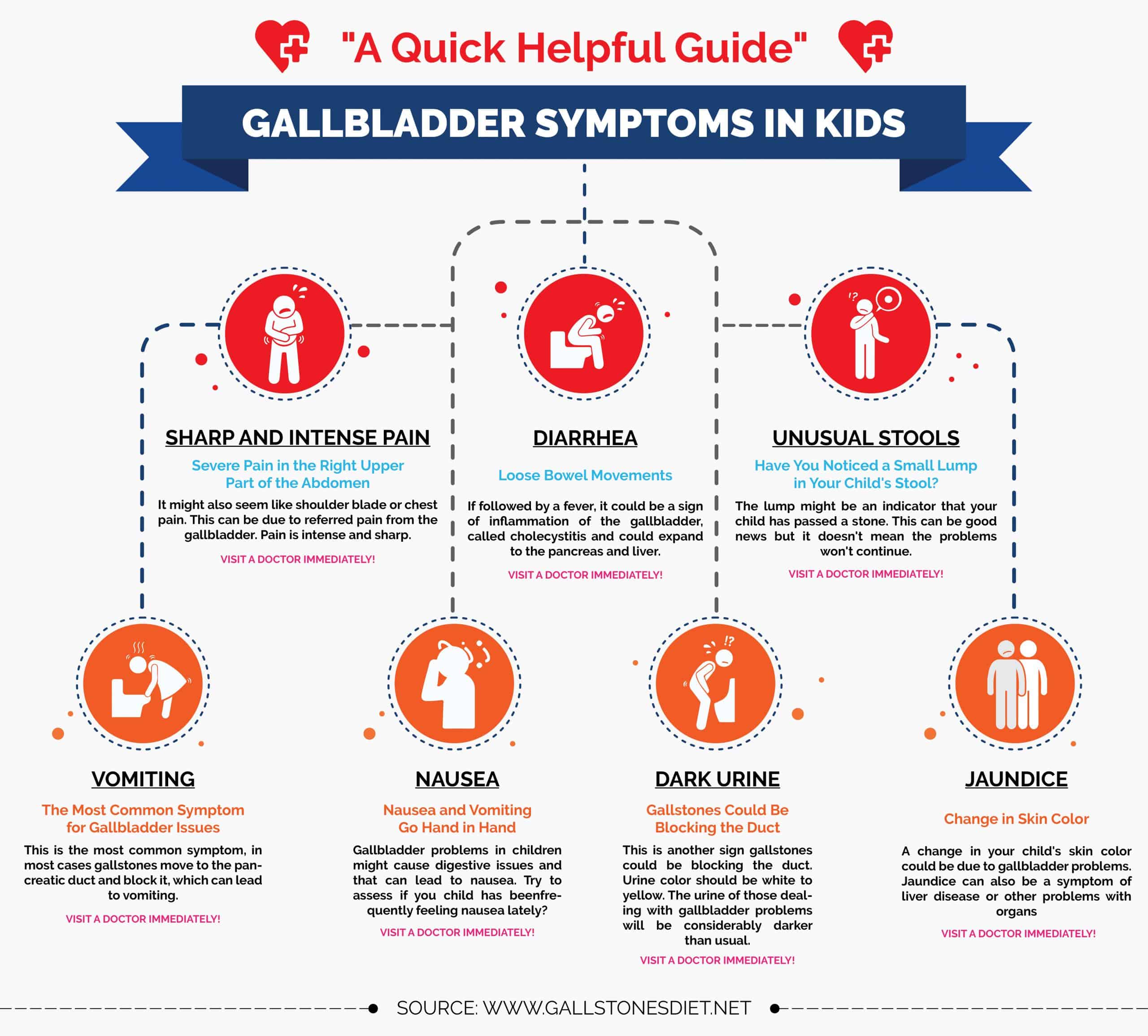
Ideally, you should contact a gastroenterologist at the stage of pregnancy planning – this way you can avoid many problems with the gastrointestinal tract that occur during this period in a woman’s life.
– One of the most common diagnoses is “gastritis”. What is it connected with and how is it treated?
Gastritis is an inflammation of the lining of the stomach. This diagnosis, indeed, is very often made, and often without proper reason. This diagnosis is made morphologically, that is, after the morphologist describes the existing inflammatory changes as a result of a biopsy of the gastric mucosa. Then it’s gastritis. Only on the basis of complaints, a competent doctor can only write “functional dyspepsia syndrome” in the diagnosis.
Complaints with gastritis are quite diverse: it can be pain, a feeling of a full stomach even with a small amount eaten, belching, vomiting, etc. individually.
Myth
Probably everyone has heard the opinion: “if you eat dry food, you will get gastritis.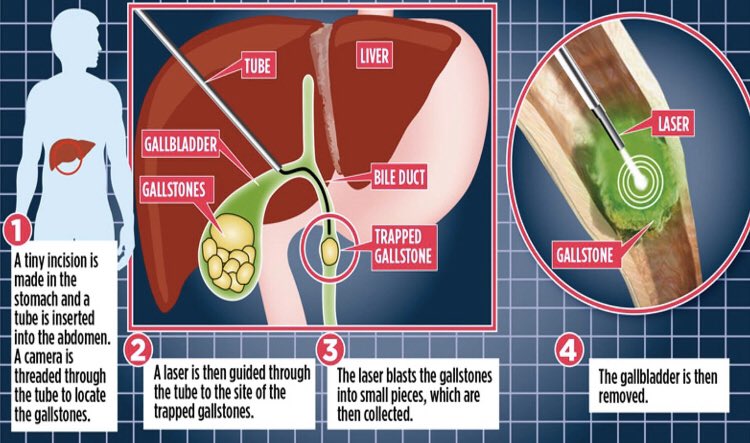 ” In fact, it is not! Food should just be without additional liquid, it should not be washed down with water, tea, coffee, etc. The liquid dilutes the acidic contents in the stomach and impairs the quality of food digestion. But eating “on the run” is really not worth it – the most important thing for a good digestion process is thorough chewing of food! A large amount of saliva released during chewing is necessary for the assimilation of food.
” In fact, it is not! Food should just be without additional liquid, it should not be washed down with water, tea, coffee, etc. The liquid dilutes the acidic contents in the stomach and impairs the quality of food digestion. But eating “on the run” is really not worth it – the most important thing for a good digestion process is thorough chewing of food! A large amount of saliva released during chewing is necessary for the assimilation of food.
What provokes gastritis? Stress, systematic violation of the diet, violation of the frequency of nutrition, abuse of semi-finished products, concentrates, spices, sour, spicy, peppery, salty, smoked, fried, too hot, too cold or otherwise thermally, chemically or mechanically irritating food, carbonated drinks, coffee, alcohol, smoking; lack of thorough chewing of food.
In addition, gastritis is often caused by the bacterium Helicobacter pylori. This bacterium needs acid-free conditions to exist, for this it “envelops” itself with a cloud of urease, an enzyme that creates an alkaline environment. All this damages the mucous membrane up to its atrophy, and can also lead to the development of stomach and duodenal ulcers, significantly increasing the risk of developing stomach cancer. 95% of gastric ulcers and 85% of duodenal ulcers worldwide are associated with Helicobacter pylori infection. Other causes of damage to the mucous membrane of the stomach and duodenum is the frequent use of non-steroidal anti-inflammatory drugs.
All this damages the mucous membrane up to its atrophy, and can also lead to the development of stomach and duodenal ulcers, significantly increasing the risk of developing stomach cancer. 95% of gastric ulcers and 85% of duodenal ulcers worldwide are associated with Helicobacter pylori infection. Other causes of damage to the mucous membrane of the stomach and duodenum is the frequent use of non-steroidal anti-inflammatory drugs.
In the treatment of gastritis and peptic ulcer, drugs are used that reduce the acid production of the gastric mucosa, improve its healing, and if Helicobacter pylori is detected, a course of antibiotic therapy is used. The patient must be prescribed a sparing diet.
All these activities are prescribed only by a doctor. Self-medication can be not only ineffective, but also harmful to the patient.
– Is stress also one of the reasons for the development of irritable bowel syndrome (IBS)?
– Yes, the classic triad for making this diagnosis: stress, pain, stool disorders (diarrhea, constipation or their alternation).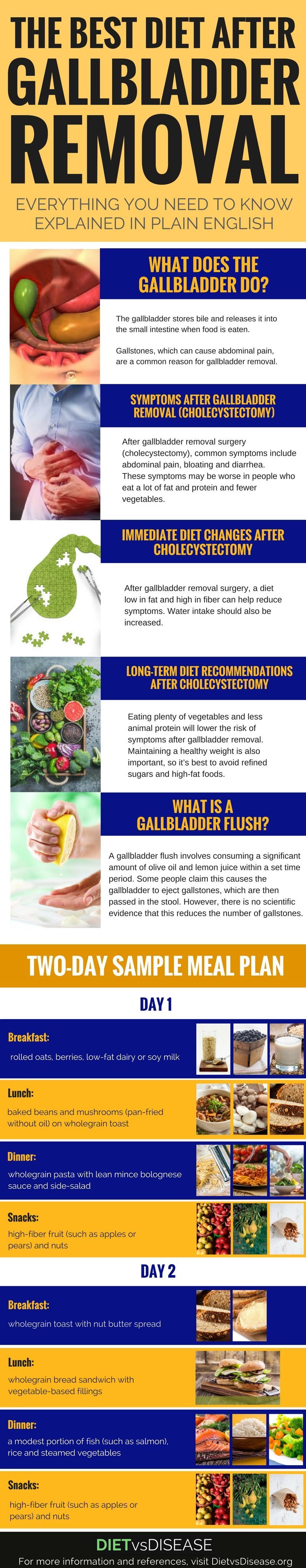 The very name of the disease contains its essence: the intestine is irritated, the sensitivity is increased.
The very name of the disease contains its essence: the intestine is irritated, the sensitivity is increased.
The peculiarity of this disease is that the patient does not have a visible lesion of the intestinal mucosa. No examinations can establish what is actually happening with the human body, and the disease is clearly manifested.
The mechanism of occurrence of symptoms is associated with the characteristics of the intestines. The intestine has its own nervous system, which is part of the autonomic nervous system. In stressful situations, failures in the work of the entire nervous system of the body begin, the brain gives the wrong signals to the intestines, and the latter incorrectly informs the brain about the processes taking place in it. As a result, intestinal motility is disturbed, the threshold of pain sensitivity decreases, and even slight discomfort causes severe attacks of pain.
In addition to stress and a low pain threshold, the risk of developing IBS is increased by eating disorders, a sedentary lifestyle, hormonal disruptions (for example, in pregnant women), and genetic predisposition.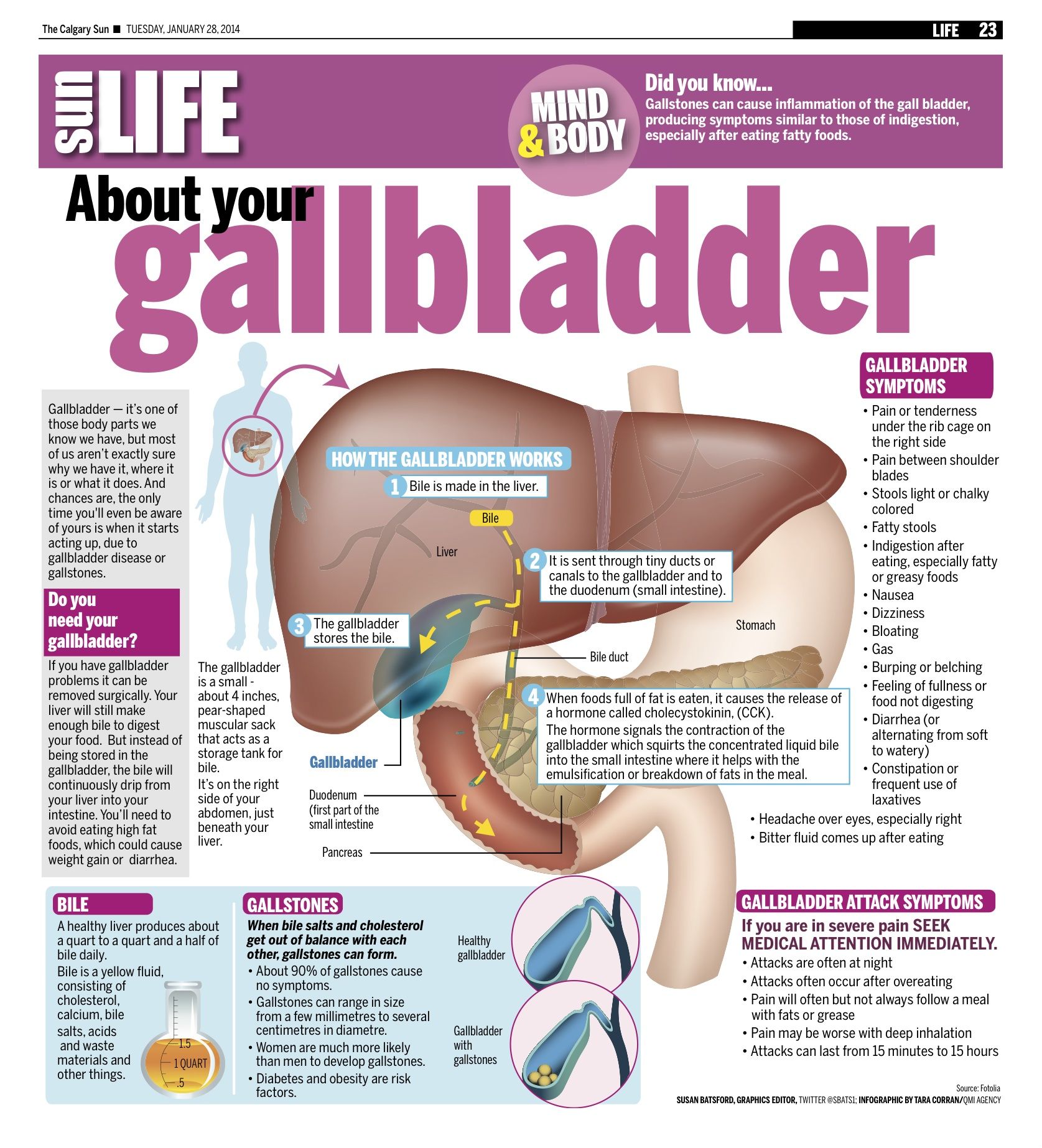 IBS can also develop after certain infectious bowel diseases.
IBS can also develop after certain infectious bowel diseases.
The main difficulty in IBS is that the symptoms are very unpleasant, and the correction must be carried out, first of all, the psycho-emotional state, which is quite difficult without the help of a competent psychologist. At the same time, there is still a problem that often patients do not even admit to themselves that they need psychological help.
When making this diagnosis, it is very important to show oncological vigilance. However, in our time it is always important, even in young patients, but especially in older people. IBS is more common in young people, so if these symptoms are observed in mature patients, first of all, the doctor should rule out cancer.
– When taking antibiotics, doctors often advise taking probiotics or prebiotics. Is it really necessary?
– Antibiotics affect the intestinal flora, this is indisputable. Often, against the background of antibiotic therapy, the patient develops dysbiosis (“dysbacteriosis”), that is, a qualitative and / or quantitative change in the ratio of microorganisms that live in the intestine. Dysbiosis is manifested by a violation of the stool, flatulence (excessive gas formation), the presence of inflammation on the mucosa. As a preventive measure for the development of this unpleasant condition, it is recommended to take pro- and prebiotics.
Dysbiosis is manifested by a violation of the stool, flatulence (excessive gas formation), the presence of inflammation on the mucosa. As a preventive measure for the development of this unpleasant condition, it is recommended to take pro- and prebiotics.
Probiotics are medicinal products or biologically active food supplements that contain live microorganisms that are representatives of the normal human microflora. They are designed to restore the disturbed balance of microorganisms that inhabit various human mucosa, and therefore are used to treat and prevent immunodeficiency, dysbiosis and related diseases. Probiotics stimulate the immune system at all levels, as proven by numerous clinical studies.
Prebiotics are food ingredients that are not digested by human enzymes and are not absorbed in the upper gastrointestinal tract. They stimulate the growth and vital activity of beneficial microflora: breaking down into fatty acids, they increase the acidity in the colon, inhibiting the growth of opportunistic microflora, which also creates favorable conditions for the development of normal microflora.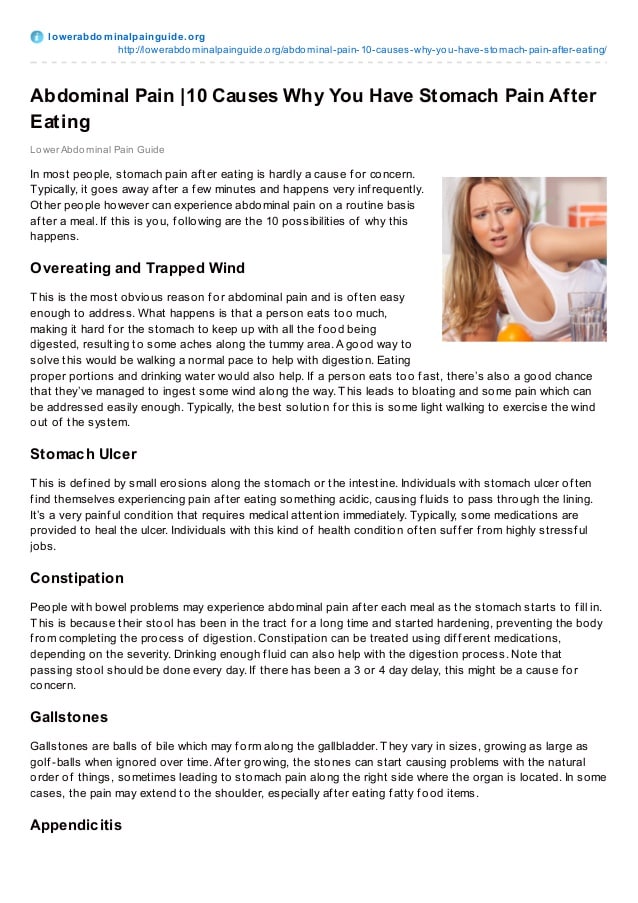
Prebiotics are found in dairy products, corn flakes, cereals, bread, onions, field chicory, garlic, beans, peas, artichokes, asparagus, bananas and many other foods. They also exist in the form of dietary supplements.
There is an opinion that probiotics in tablet and liquid forms are less effective, since they cannot always pass through the highly acidic environment of the stomach, bile aggressive to bacteria. And only capsules are designed to dissolve in the colon – where bacteria should live.
Not so long ago, synbiotics appeared on the market – combined preparations that combine pre- and probiotics. To date, they are considered to have the most advanced mechanism of action.
I recommend choosing preparations that normalize microflora together with a doctor – because it is quite difficult for a non-specialist to understand all the variety of existing remedies, and it is unlikely that you will be able to understand what is suitable in each specific case.
— Why is constipation dangerous?
– Constipation is a condition characterized not only by a decrease in the frequency of bowel movements: less than 3 times a week, but also by the appearance of dense, dry feces or the absence of a feeling of complete bowel emptying or bowel emptying with tension or the use by patients of additional techniques to empty the bowel.
Prolonged constipation causes:
chronic intoxication (poisoning), which leads to sleep disturbance, unmotivated fatigue, increased fatigue and, finally, to depression, deterioration of the skin and hair;
the formation of intestinal diverticula (protrusions of the wall), which can cause abdominal pain, and when an infection is attached, inflammation of the intestinal mucosa (diverticulitis) and the need for intensive antibiotic therapy or surgical treatment in case of intestinal obstruction;
varicose hemorrhoidal veins, chronic anal fissures;
colon cancer.

It is necessary to start solving the problem of constipation not with self-treatment, but with a visit to a gastroenterologist. There are many reasons for constipation. These can be very serious illnesses. Only a competent specialist can understand this. Solving the problem of constipation on your own, you can significantly worsen your condition.
– Is there a cure for such a delicate problem as flatulence?
– Flatulence (increased gas formation) is associated with fermentation. There can be many reasons: insufficient bile secretion, insufficiently concentrated bile, violations of the secretion of pancreatic juice – as a rule, problems with the sphincter of Oddi. All this leads to a change in the bacterial flora of the intestine. As a result, flatulence develops. This is a common problem, but it can be solved. Although I will not say that it is always simple and fast. The main thing is to find the root cause, since flatulence can be a symptom of various diseases.
– Sometimes a person suffers from bad breath or bad taste in the mouth. Is this a symptom of some disease?
– Halitosis – bad breath – can occur for various reasons. First of all, I would recommend contacting a dentist and checking the condition of the teeth and oral cavity. In second place are ENT diseases. If everything is in order in these areas, then, indeed, halitosis may be the result of digestive problems.
As for the taste in the mouth, it can be a symptom of certain diseases. But here everything is very individual: the taste can be sweet, bitter, sour, metallic, etc. It can be constant or appear only after eating or, conversely, on an empty stomach, etc. Therefore, you need to look and look for the cause.
– It is not uncommon for patients who have had an abdominal ultrasound to find out they have a kinked gallbladder – how serious is that?
– Deformities of the gallbladder – inflection, membranes, etc.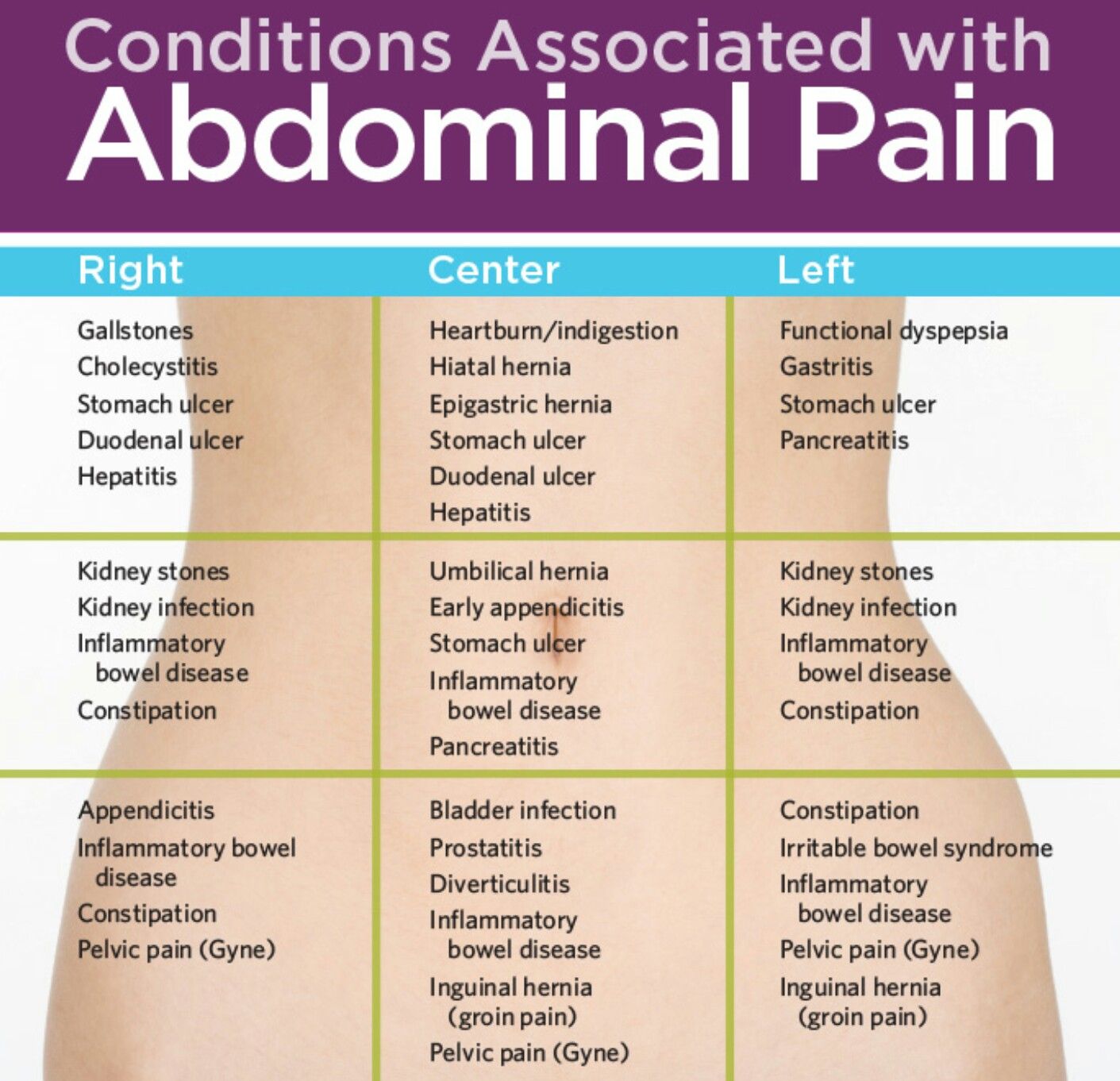 increase the risk of bile stasis. The gallbladder should normally empty almost completely after each meal. Because this gallbladder has to work harder to contract, some patients may experience pain. After its reduction, part of the bile may remain behind the inflection and “stagnate”, which can lead to the formation of stones. I recommend patients with gallbladder deformity to control their condition: to be observed by a doctor, to do an ultrasound of the abdominal organs once a year to see the state of bile and gallbladder. If the ultrasound diagnostic doctor notes that the bile is “viscous”, “heterogeneous”, “inhomogeneous”, etc., it is important to immediately contact a gastroenterologist and undergo a course of therapy to prevent the formation of stones. It is especially important to take gallstone prevention seriously if someone in your immediate family has these problems.
increase the risk of bile stasis. The gallbladder should normally empty almost completely after each meal. Because this gallbladder has to work harder to contract, some patients may experience pain. After its reduction, part of the bile may remain behind the inflection and “stagnate”, which can lead to the formation of stones. I recommend patients with gallbladder deformity to control their condition: to be observed by a doctor, to do an ultrasound of the abdominal organs once a year to see the state of bile and gallbladder. If the ultrasound diagnostic doctor notes that the bile is “viscous”, “heterogeneous”, “inhomogeneous”, etc., it is important to immediately contact a gastroenterologist and undergo a course of therapy to prevent the formation of stones. It is especially important to take gallstone prevention seriously if someone in your immediate family has these problems.
– What methods of preventing gastrointestinal diseases can be used? Maybe you need to take medications or do tubazhi?
– Do not use any prophylactic drugs without a doctor’s prescription.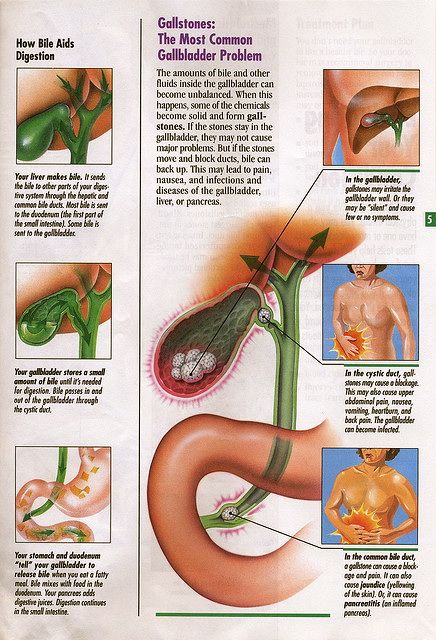 All medicines have side effects and are not recommended to be taken without indications.
All medicines have side effects and are not recommended to be taken without indications.
To carry out tubage (a procedure that is the intake of choleretic agents for the simultaneous emptying of the gallbladder), certain indications and contraindications are also necessary. More often, the doctor prescribes this procedure in combination with other therapeutic measures, selects drugs, etc.
The best prevention of gastrointestinal diseases is proper nutrition: in small portions, with thorough chewing of food to gruel. You need to eat at least 4-5 times a day, be sure to have breakfast within an hour after a night’s sleep. The volume of water drunk per day should be at least 1.5 liters.
Try to minimize the amount of food that provokes the development of diseases. We have already listed them above: fast food, pickles, smoked meats, fried, spicy, etc. Add some physical activity: a sedentary lifestyle has been proven to contribute to digestive troubles, while abdominal exercises, brisk walking, and yoga have a beneficial effect on bowel function.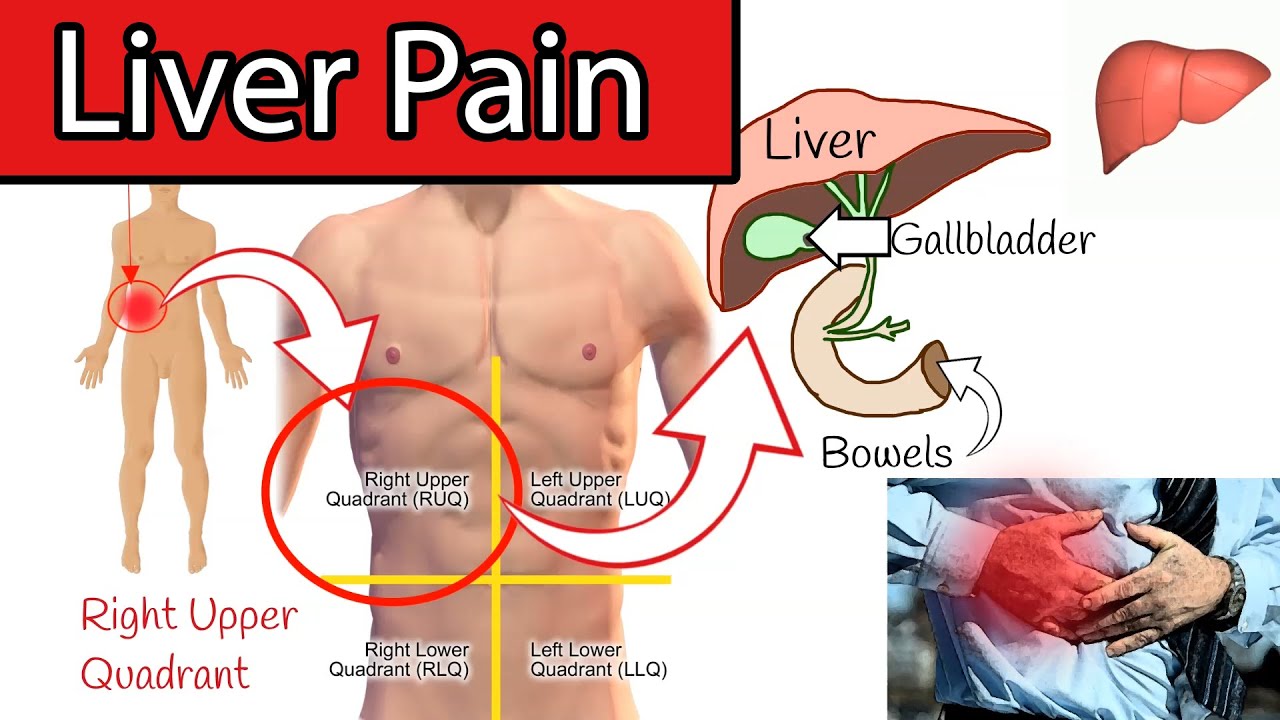

 The bile is then trapped in the gallbladder, causing damage and inflammation. Usually, a cholecystectomy (removal of the gallbladder) is the best treatment.
The bile is then trapped in the gallbladder, causing damage and inflammation. Usually, a cholecystectomy (removal of the gallbladder) is the best treatment.
