How do people get gall stones. Gallstones: Causes, Symptoms, and Treatment Options Explained
How do gallstones form in the body. What are the common symptoms of gallstones. Which treatment options are available for gallstone removal. When should you seek medical attention for gallstone-related issues. How can you prevent gallstone formation.
Understanding Gallstones: Formation and Risk Factors
Gallstones are hardened deposits that form in the gallbladder, a small organ located beneath the liver. These stones develop when substances in bile, such as cholesterol or bilirubin, crystallize and accumulate. While gallstones are common, many people remain unaware of their presence due to a lack of symptoms.
Several factors contribute to gallstone formation:
- Excess cholesterol in bile
- High levels of bilirubin
- Incomplete emptying of the gallbladder
- Genetic predisposition
- Obesity
- Rapid weight loss
- Certain medications
Understanding these risk factors can help individuals take preventive measures and recognize potential symptoms early on.

Recognizing Gallstone Symptoms: When to Seek Medical Attention
While many gallstones remain asymptomatic, some individuals experience discomfort and pain. Recognizing these symptoms is crucial for timely medical intervention.
Common gallstone symptoms include:
- Sudden, intense pain in the upper right abdomen or center of the stomach
- Pain that radiates to the back or right shoulder
- Nausea and vomiting
- Fever and chills
- Jaundice (yellowing of the skin and eyes)
- Clay-colored stools
Are gallstone symptoms always severe? Not necessarily. Some people may experience mild discomfort or intermittent pain, especially after consuming fatty foods. However, persistent or worsening symptoms warrant medical attention to prevent complications.
Silent Gallstones: The Asymptomatic Majority
Interestingly, about 80% of people with gallstones have what medical professionals call “silent gallstones.” These individuals do not experience any noticeable symptoms, and their gallstones are often discovered incidentally during imaging tests for other conditions.

Should asymptomatic gallstones be treated? In most cases, no. The American College of Gastroenterology recommends against treating silent gallstones, as the risks of surgery often outweigh the benefits for individuals without symptoms.
Diagnosis and Imaging Techniques for Gallstones
Accurate diagnosis of gallstones is essential for proper treatment. Healthcare providers employ various imaging techniques to detect and assess gallstones.
Common diagnostic methods include:
- Ultrasound: The primary tool for gallstone detection, offering a non-invasive and radiation-free option
- CT scan: Provides detailed images of the gallbladder and surrounding organs
- HIDA scan: Assesses gallbladder function and detects blockages
- MRI: Offers high-resolution images of the biliary system
- Endoscopic retrograde cholangiopancreatography (ERCP): Combines X-rays with endoscopy to diagnose and treat gallstone-related complications
How accurate are these diagnostic techniques? Ultrasound, the most commonly used method, has a sensitivity of 84% and specificity of 99% for detecting gallstones larger than 3mm. However, combining multiple imaging modalities can further improve diagnostic accuracy.

Treatment Options: From Conservative Management to Surgery
The treatment approach for gallstones depends on the severity of symptoms and the individual’s overall health. Options range from watchful waiting to surgical intervention.
Conservative Management
For individuals with mild or infrequent symptoms, conservative management may be appropriate. This approach involves:
- Dietary modifications to reduce fat intake
- Pain management with over-the-counter medications
- Regular monitoring to assess symptom progression
Is conservative management effective for all gallstone cases? No, it’s primarily suitable for those with minimal symptoms or those who are poor surgical candidates. Patients should work closely with their healthcare providers to determine the best course of action.
Surgical Intervention: Cholecystectomy
For symptomatic gallstones or complications, surgical removal of the gallbladder (cholecystectomy) is the gold standard treatment. Two main surgical approaches are available:

- Laparoscopic cholecystectomy: A minimally invasive procedure performed through small incisions
- Open cholecystectomy: A traditional surgery involving a larger incision, typically reserved for complex cases
How safe is gallbladder removal surgery? Laparoscopic cholecystectomy is considered a safe and effective procedure with a low complication rate. Most patients can return home within 24 hours of surgery and resume normal activities within a week.
Non-Surgical Alternatives
In some cases, non-surgical options may be considered, particularly for patients who are not suitable candidates for surgery:
- Oral dissolution therapy: Medications to dissolve small cholesterol stones
- Lithotripsy: Using shock waves to break up gallstones
- Percutaneous cholecystostomy: Draining the gallbladder using a catheter
Are these alternatives as effective as surgery? Generally, non-surgical options have lower success rates and higher recurrence rates compared to cholecystectomy. They are typically reserved for specific patient populations or as temporary measures.
Living Without a Gallbladder: Adjustments and Expectations
After gallbladder removal, most individuals can lead normal, healthy lives with minimal adjustments. The body adapts to the absence of the gallbladder by allowing bile to flow directly from the liver to the small intestine.
Post-cholecystectomy considerations include:
- Temporary dietary changes to ease digestion
- Gradual reintroduction of fatty foods
- Possible use of digestive enzymes or bile acid supplements
- Regular follow-ups with healthcare providers
Do all patients experience digestive changes after gallbladder removal? No, many individuals report no significant changes in digestion or bowel habits. However, a small percentage may experience diarrhea or other mild digestive issues, which typically resolve over time.
Preventing Gallstone Formation: Lifestyle and Dietary Strategies
While some risk factors for gallstones are beyond control, adopting certain lifestyle and dietary habits can help reduce the likelihood of gallstone formation.
Preventive strategies include:
- Maintaining a healthy weight through balanced nutrition and regular exercise
- Avoiding rapid weight loss or extreme dieting
- Consuming a diet rich in fiber and low in saturated fats
- Staying hydrated to support proper bile flow
- Limiting alcohol consumption
- Managing underlying health conditions, such as diabetes or high cholesterol
Can dietary changes alone prevent gallstones? While a healthy diet can significantly reduce the risk of gallstone formation, it’s important to note that some risk factors, such as genetics or certain medical conditions, cannot be modified through lifestyle changes alone.
The Role of Exercise in Gallstone Prevention
Regular physical activity plays a crucial role in reducing the risk of gallstone formation. Exercise helps maintain a healthy weight, improves insulin sensitivity, and promotes proper digestion.
Benefits of exercise for gallstone prevention:
- Reduces cholesterol production in the liver
- Enhances gallbladder motility
- Improves overall metabolic health
- Supports weight management
How much exercise is needed to reduce gallstone risk? Studies suggest that engaging in moderate-intensity exercise for at least 150 minutes per week can significantly lower the risk of gallstone formation.
Gallstones in Special Populations: Pregnancy and Older Adults
Certain populations face an increased risk of gallstone formation and may require special considerations in terms of prevention, diagnosis, and treatment.
Gallstones During Pregnancy
Pregnant women are at higher risk of developing gallstones due to hormonal changes and increased cholesterol levels. Management of gallstones during pregnancy requires careful consideration of both maternal and fetal well-being.
Key points for gallstones in pregnancy:
- Increased prevalence in the second and third trimesters
- Conservative management is preferred when possible
- Surgery may be necessary for severe cases or complications
- Close monitoring throughout pregnancy and postpartum period
Is it safe to undergo gallbladder surgery during pregnancy? While cholecystectomy can be performed safely during pregnancy, it is typically reserved for cases where conservative management fails or complications arise. The timing of surgery depends on the trimester and individual circumstances.

Gallstones in Older Adults
The prevalence of gallstones increases with age, and older adults may face unique challenges in diagnosis and treatment.
Considerations for gallstones in older adults:
- Higher likelihood of comorbidities affecting treatment options
- Increased risk of complications from untreated gallstones
- Potential for atypical presentation of symptoms
- Need for comprehensive geriatric assessment before surgery
Are there age-specific treatment guidelines for gallstones? While age alone is not a contraindication for surgery, treatment decisions for older adults should consider overall health status, life expectancy, and potential risks and benefits of intervention.
Emerging Research and Future Directions in Gallstone Management
As our understanding of gallstone formation and treatment continues to evolve, researchers are exploring new avenues for prevention, diagnosis, and management of this common condition.
Promising areas of research include:
- Genetic markers for gallstone susceptibility
- Novel pharmacological interventions for stone dissolution
- Advanced imaging techniques for early detection
- Minimally invasive alternatives to traditional surgery
- Gut microbiome’s role in gallstone formation
How might these advancements impact gallstone treatment in the future? Emerging research could lead to more personalized prevention strategies, targeted therapies, and less invasive treatment options, potentially reducing the need for surgery in some cases.

The Potential of Probiotics in Gallstone Prevention
Recent studies have highlighted the potential role of gut microbiota in gallstone formation and prevention. Probiotics, which promote a healthy balance of gut bacteria, may offer a promising approach to reducing gallstone risk.
Potential benefits of probiotics for gallstone prevention:
- Modulation of bile acid metabolism
- Reduction of cholesterol absorption
- Improvement of gallbladder motility
- Enhancement of overall digestive health
Are probiotics a proven method for preventing gallstones? While early research is promising, more large-scale clinical trials are needed to establish the efficacy of probiotics in gallstone prevention and to determine optimal strains and dosages.
As research in this field progresses, it’s essential for individuals to stay informed about the latest developments in gallstone management and to work closely with healthcare providers to develop personalized prevention and treatment strategies. By combining established medical knowledge with emerging insights, we can continue to improve outcomes for those affected by gallstones and reduce the overall burden of this common condition.

Symptoms, Causes, Treatment, and More
Gallstones are deposits of digestive fluid made of solidified substances found in bile, like cholesterol. They are common and may or may not produce symptoms. People with symptoms usually need to have their gallbladders taken out.
Read on to learn more about gallstones, the symptoms they can cause, and how to treat them.
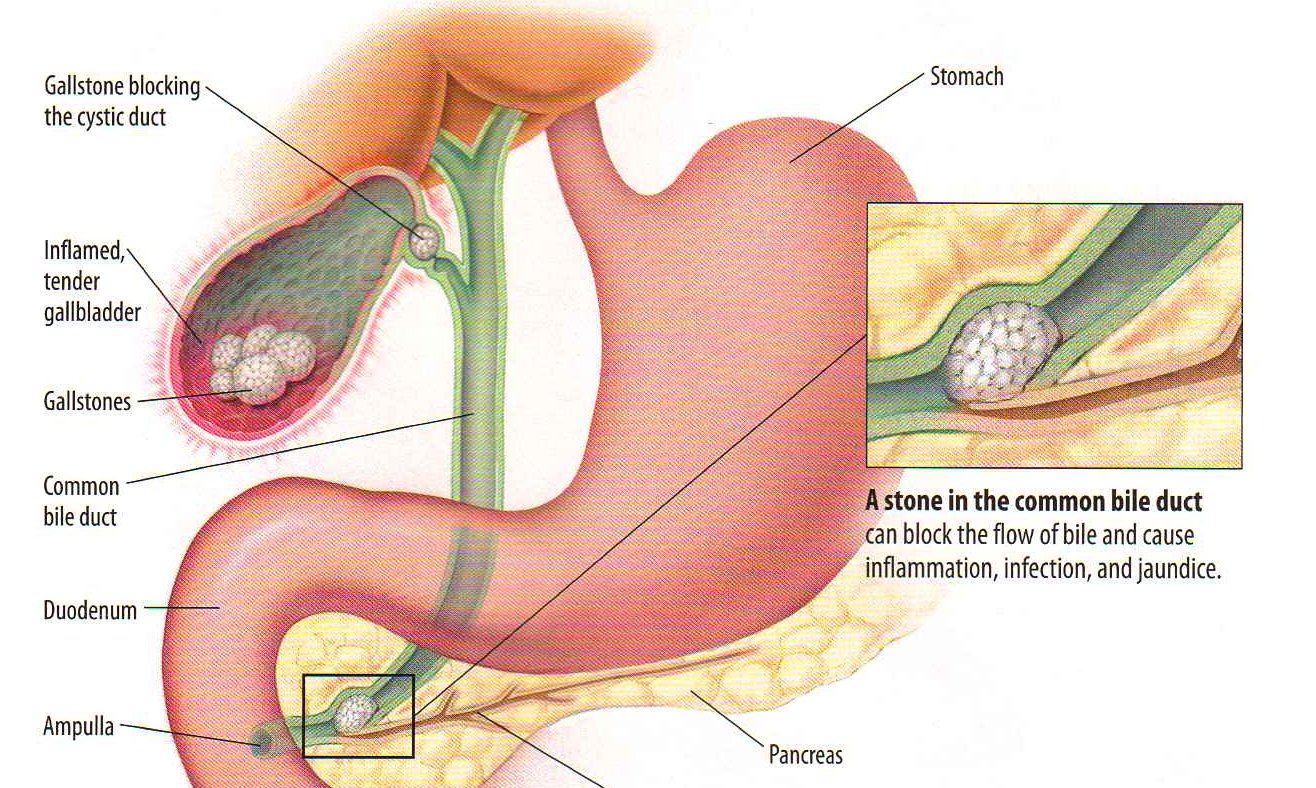
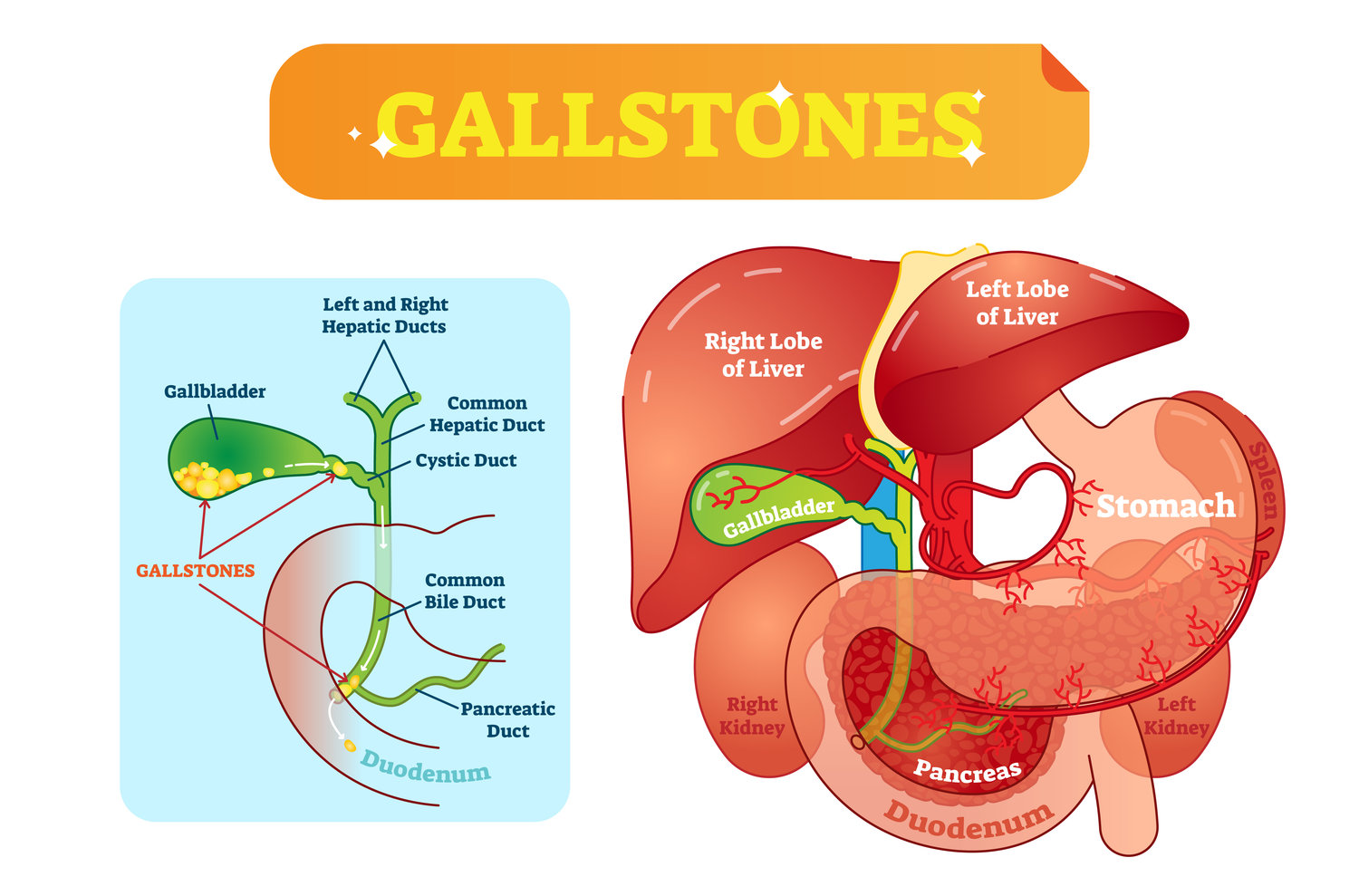
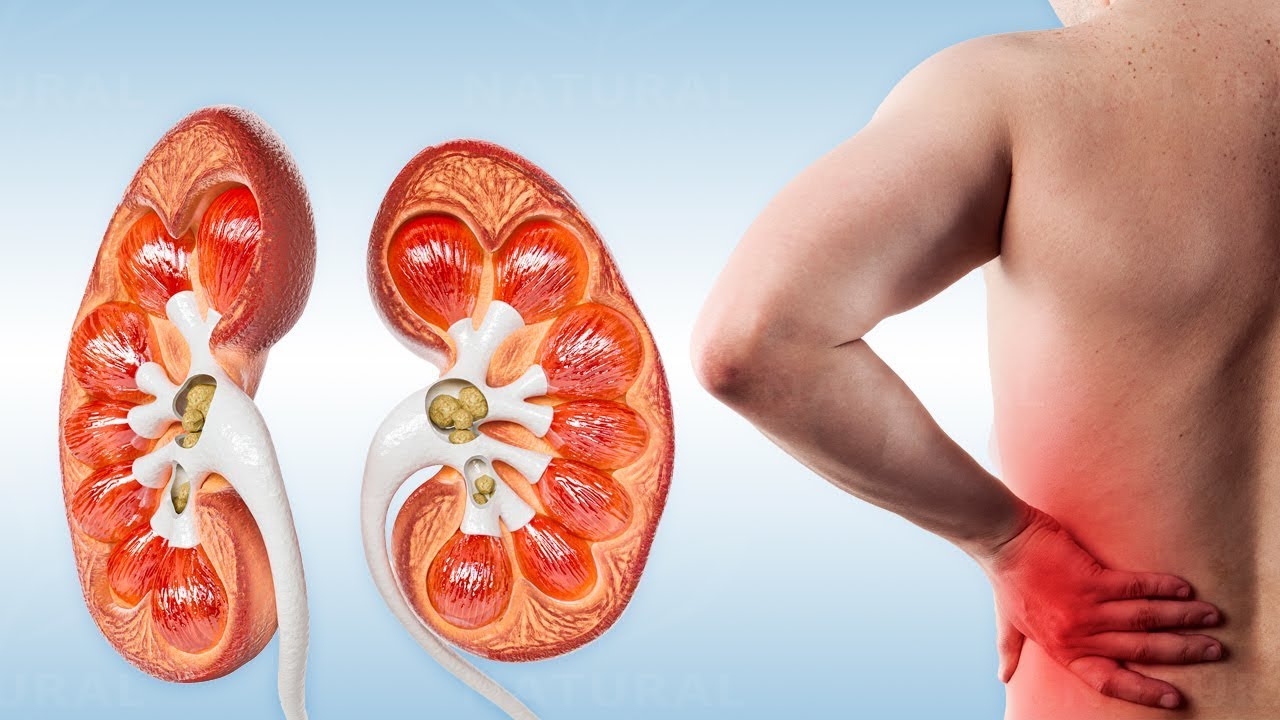
Your gallbladder is a small organ in your upper right abdomen, right below your liver. It’s a pouch that stores bile, a green-yellow liquid that helps digestion. Issues with your gallbladder typically occur when something is blocking its bile duct—like a gallstone.
Most gallstones are created when substances found in bile, like cholesterol, harden. Gallstones are very common and routinely asymptomatic.
However, about 10 percent of people who are diagnosed with gallstones will develop noticeable symptoms within 5 years.
Photo: Bruce Blaus | Wikimedia Commons | https://commons.wikimedia.org/wiki/File:Gallstones. png
png
Gallstones can lead to pain in the upper right abdomen or the center of your stomach. You may experience gallbladder pain from time to time after you eat foods that are high in fat, such as fried foods, but the pain can occur at almost any time.
Pain caused by gallstone issues usually lasts for only a few hours, but it can feel severe.
If gallstones are left untreated or unidentified, the symptoms may increase to include:
- a high temperature
- rapid heartbeat
- yellowing of the skin and whites of the eyes (jaundice)
- itchy skin
- diarrhea
- chills
- confusion
- a loss of appetite
These symptoms can be signs of a gallbladder infection, or inflammation of the gallbladder, liver, or pancreas.
Because gallstone symptoms may mimic the symptoms of other serious issues like appendicitis and pancreatitis, no matter what, if you’re dealing with one or more of these issues — it’s time to see a doctor or get yourself to the ER.
If you need help finding a urologist, then check out our FindCare tool here.
Asymptomatic gallstones
Gallstones themselves don’t cause pain. Rather, pain occurs when gallstones block the movement of bile from the gallbladder.
According to the American College of Gastroenterology, about 80 percent of people who have gallstones have “silent gallstones.” This means they don’t experience pain or have symptoms. In these cases, your doctor may discover the gallstones from X-rays or during abdominal surgery.
The actual cause of gallstones is thought to be due to a chemical imbalance of bile inside of the gallbladder. While researchers still aren’t clear about what exactly causes that imbalance to happen, there are a few possible reasons:
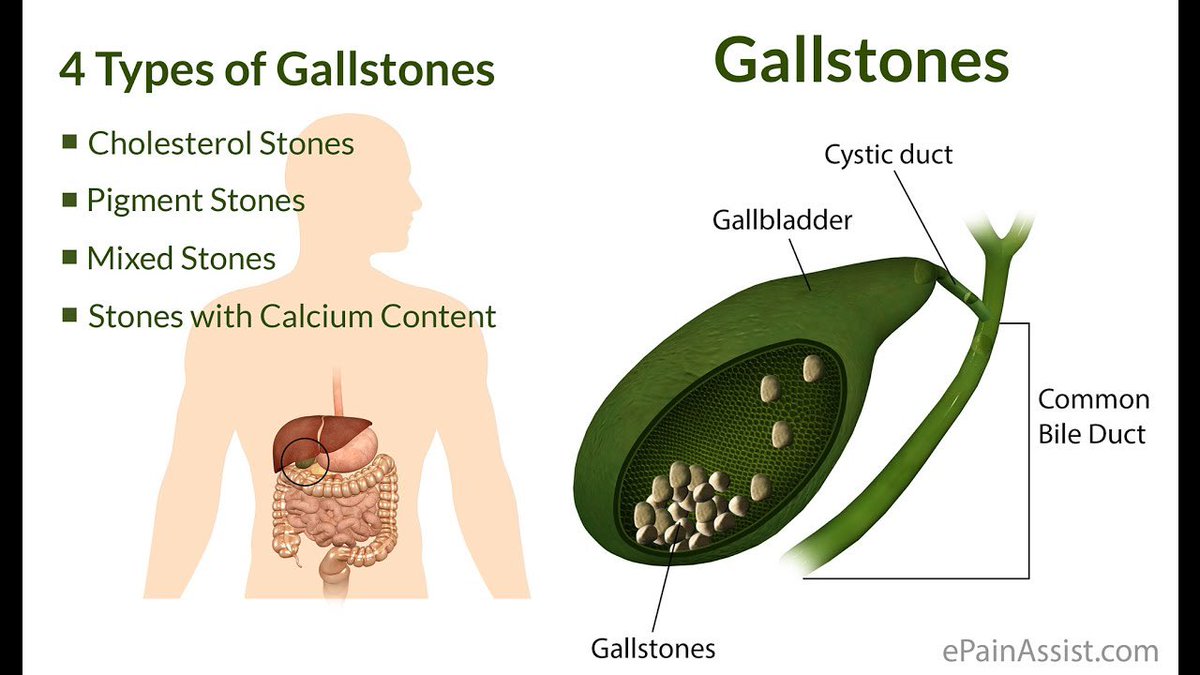
Too much cholesterol in your bile
Having too much cholesterol in your bile can lead to yellow cholesterol stones. These hard stones may develop if your liver makes more cholesterol than your bile can dissolve.
Too much bilirubin in your bile
Bilirubin is a chemical produced during the normal breakdown of red blood cells. After it’s created, it passes through the liver and is eventually excreted out of the body.
After it’s created, it passes through the liver and is eventually excreted out of the body.
Some conditions, such as liver damage and certain blood disorders, cause your liver to produce more bilirubin than it should. Pigment gallstones form when your gallbladder can’t break down the excess bilirubin. These hard stones are often dark brown or black.
Concentrated bile due to a full gallbladder
Your gallbladder needs to be able to empty its bile to function properly. If it fails to empty its bile content, the bile becomes overly concentrated, which can cause stones to form.
Most of the time, you won’t need treatment for gallstones unless they cause you pain. Sometimes you can pass gallstones without even noticing. If you’re in pain, your doctor will likely recommend surgery. In rare cases, medication may be used.
If you’re at high risk for surgery complications, there are a few nonsurgical ways to attempt to treat gallstones. However, if surgery isn’t performed, your gallstones may come back — even with additional treatment.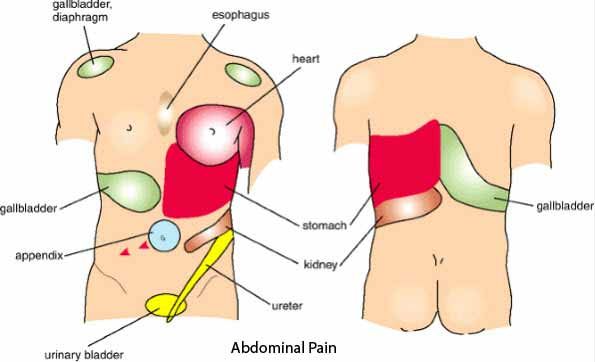 This means you may need to keep an eye on your condition for the majority of your life.
This means you may need to keep an eye on your condition for the majority of your life.
Surgery
Cholecystectomy, which is surgery to remove the gallbladder, is one of the most common operations performed on adults in the United States. Because the gallbladder isn’t an essential organ, it’s possible to live a healthy life without it.
There are two types of cholecystectomy:
- Laparoscopic cholecystectomy. This is a common surgery that requires general anesthesia. The surgeon will usually make three or four incisions in your abdomen. They’ll then insert a small, lighted device into one of the incisions, check for stones, and carefully remove your gallbladder. You can usually go home on the day of the procedure or the day after if you have no complications.
- Open cholecystectomy.This surgery is typically performed when the gallbladder is inflamed, infected, or scarred. This surgery may also happen if problems occur during a laparoscopic cholecystectomy.

You may experience loose or watery stools after gallbladder removal. Removing a gallbladder involves rerouting the bile from the liver to the small intestine. Bile no longer goes through the gallbladder and it becomes less concentrated. The immediate result is a laxative effect that can cause diarrhea, but this issue should resolve on its own for most people.
Nonsurgical treatments
If surgery can’t be performed, such as if the patient is a much older individual, there are a few other ways doctors can try to get rid of your gallstones.
- Oral dissolution therapy typically includes using the medications ursodiol (Actigall) and chenodiol (Chenix) to break up gallstones. These medications contain bile acids, which work to break up the stones. This treatment is best suited for breaking up cholesterol stones and can take many months or years to work completely.
- Shock wave lithotripsy is another option. A lithotripter is a machine that generates shock waves that pass through a person.
 These shock waves can break gallstones into smaller pieces.
These shock waves can break gallstones into smaller pieces. - Percutaneous drainage of the gallbladder involves placing a sterile needle into the gallbladder to aspirate (draw out) bile. A tube is then inserted to help with additional drainage. This procedure isn’t typically a first line of defense and tends to be an option for individuals who may not be suited for other procedures.
Some risk factors for gallstones are related to diet, while other factors are not as controllable. Uncontrollable risk factors are things like age, race, sex, and family history.
Lifestyle risk factors
- living with obesity
- a diet high in fat or cholesterol and low in fiber
- undergoing rapid weight loss
- living with type 2 diabetes
Genetic risk factors
- being born female
- being of Native American or Mexican descent
- having a family history of gallstones
- being 60 years or older
Medical risk factors
- living with cirrhosis
- being pregnant
- taking certain medications to lower cholesterol
- taking medications with a high estrogen content (like certain birth controls)
While some medications may increase your risk of gallstones, don’t stop taking them unless you have discussed it with your doctor and have their approval.
Your doctor will perform a physical examination that includes checking your eyes and skin for visible changes in color. A yellowish tint may be a sign of jaundice, the result of too much bilirubin in your body.
The exam may involve using diagnostic tests that help your doctor see inside your body. These tests include:
- Ultrasound. An ultrasound produces images of your abdomen. It’s the preferred imaging method to confirm that you have gallstone disease. It can also show abnormalities associated with acute cholecystitis.
- Abdominal CT scan. This imaging test takes pictures of your liver and abdominal region.
- Gallbladder radionuclide scan. This important scan takes about one hour to complete. A specialist injects a radioactive substance into your veins. The substance travels through your blood to the liver and gallbladder. On a scan, it can reveal evidence to suggest infection or blockage of the bile ducts from stones.

- Blood tests. Your doctor may order blood tests that measure the amount of bilirubin in your blood. The tests also help determine how well your liver is functioning.
To help improve your condition and reduce your risk of gallstones, try these tips:
- Eat fewer refined carbs (like cookies and white bread) and less sugar.
- Increase your intake of healthy fats, like fish oil and olive oil, which may help your gallbladder contract and empty on a regular basis.
- Eat the proper amount of fiber per day (women need about 25 grams a day, men need about 38 grams a day).
- Get some sort of physical activity every day.
- Keep yourself properly hydrated.
If you plan to lose weight, do it slowly. Rapid weight loss may increase your risk of gallstones and other health problems.
While there is no foolproof way to completely prevent gallstones, cholesterol seems to play a major role in their formation. If you have a family history of gallstones, your doctor may advise you to limit foods with a high saturated fat content. Some of these foods include:
Some of these foods include:
- fatty meat, like sausage and bacon
- cakes and cookies
- lard and cream
- certain cheeses
Because people living with obesity are more predisposed to gallstones, keeping your weight within a moderate range is another way to limit the possibility of their formation.
If your doctor has diagnosed you with gallstones and decides you need surgery to remove them or your gallbladder, the outlook is often positive. In most cases of stone removal, stones don’t return.
If you aren’t able to have surgery and decide to take medication to dissolve the stones, the gallstones can return, so you and your doctor will need to monitor your progress.
If your gallstones aren’t causing symptoms, you will most likely not need to do anything. Still, you may want to make lifestyle changes to prevent them from getting bigger and causing problems.
Gallstones: Symptoms, diagnosis and treatment
The gallbladder is a pear-shaped pouch that sits just below the liver. It collects bile, a fluid made to help with digestion, as it flows from the liver to the intestine through the bile ducts. Gallstones are hardened bits of bile that form inside the gallbladder.
It collects bile, a fluid made to help with digestion, as it flows from the liver to the intestine through the bile ducts. Gallstones are hardened bits of bile that form inside the gallbladder.
Bile makes it easier for you to digest fat. It also contains some waste products, including cholesterol and bilirubin, a substance created when old red blood cells are destroyed.
Gallstones form when cholesterol or bilirubin particles cluster together into a solid lump. The stone grows in size as the bile fluid washes over it, much like a pearl forms inside an oyster.
Most gallstones don’t cause any symptoms or problems. Small ones can leave the gallbladder and its draining ducts, then pass out of the body through the intestines.
Gallstones can cause symptoms if they get caught in the narrow outlet of the gallbladder, or in the ducts that drain the gallbladder. After meals, especially meals high in fat, muscles in the wall of the gallbladder contract to help release bile into the intestines. It can be very painful if the gallbladder squeezes against a gallstone, or if a gallstone blocks bile from being released into the intestines.
It can be very painful if the gallbladder squeezes against a gallstone, or if a gallstone blocks bile from being released into the intestines.
More serious problems can develop if a gallstone gets into the drainage-duct system but doesn’t make it all the way through to the intestines. In this case, the stone can cause a blockage, causing a buildup of bile in the gallbladder or liver. Since the digestive tract is teeming with bacteria, blocked fluid can lead to a very serious infection. If a gallstone lodges low down in the draining ducts, it can also block drainage of digestive enzymes from the pancreas. This can lead to inflammation of the pancreas (pancreatitis).
Gallstones are very common. About 1 in 5 women and 1 in 10 men have a gallstone by age 60. They are more likely to happen to older people, those who are overweight, and those who suddenly lose weight. Women who have had multiple pregnancies, taken birth control pills, or took estrogen after menopause are also more likely to develop gallstones.
Symptoms
Eighty percent of people with gallstones do not have any symptoms and do not need treatment. When gallstones do cause symptoms, they include:
- abdominal pain, usually high in the abdomen and often on the right side (where the gallbladder is located). The pain can spread to the back. Pain from gallstones can be steady or come and go. It can last between 15 minutes and several hours each time it occurs.
- sensitivity to high fat meals. Fats trigger the gallbladder to contract and can worsen pain.
- unexplained belching, gas, nausea, or a general decrease in appetite.
Gallstones can sometimes cause more serious problems such as pancreatitis or infections in the gallbladder or bile ducts. These can cause fever, more severe abdominal pain, or jaundice (a yellow color of the skin or whites of the eyes).
Diagnosis
Most gallstones do not show up on regular X-rays, but they are seen easily with an ultrasound. Gallstones often don’t cause symptoms. If you have symptoms that may or may not be due to gallstones, it may be difficult for your doctor to know if the stones are causing your symptoms even if you they show up on an ultrasound or CT scan.
If you have symptoms that may or may not be due to gallstones, it may be difficult for your doctor to know if the stones are causing your symptoms even if you they show up on an ultrasound or CT scan.
If a stone is blocking the movement of bile, an ultrasound might show widened bile ducts. Your doctor may also order blood tests to evaluate injury to the liver and pancreas.
Prevention
You are less likely to form gallstones if you avoid becoming overweight. If you are a dieter, try to avoid diets that cause you to lose weight very quickly, such as diets restricted to fewer than 500 calories daily.
Birth control pills and estrogen can increase the likelihood of gallstones. Consider avoiding these medications if you already have other risk factors for gallstones. Groups at high risk of gallstones include American Indians, Hispanics, people with sickle cell anemia and women who have had multiple pregnancies.
Treatment
Gallstones require treatment only if they are causing symptoms. Smaller gallstones sometimes float out of the gallbladder on their own and are eliminated from the body in feces. Gallstone attacks can also calm down on their own if the bothersome stones shift position within the gallbladder. Even when gallstone symptoms go away on their own, they return within two years in about two of three people.
Smaller gallstones sometimes float out of the gallbladder on their own and are eliminated from the body in feces. Gallstone attacks can also calm down on their own if the bothersome stones shift position within the gallbladder. Even when gallstone symptoms go away on their own, they return within two years in about two of three people.
Most people whose gallstones cause symptoms will continue to have symptoms until the gallbladder is removed, although medications or procedures to break up the stones may also be used.
Surgery
Surgical treatment for gallstones is highly effective. In most people, symptoms go away completely and stay away. The gallbladder is not a necessary organ and most people do not notice any digestive changes after it is removed. Sometimes abdominal pain or diarrhea develop after the gallbladder is removed, and additional treatment or changes in the diet are needed.
Removing the gallbladder is usually done with a minimally invasive (“keyhole) operation known as laparoscopic cholecystectomy. In this procedure, a surgeon makes one or more small openings in the abdomen. A camera, called a laparoscope, is placed into the abdomen through one of these openings. It lets the surgeon see what he or she is doing during the operation.
In this procedure, a surgeon makes one or more small openings in the abdomen. A camera, called a laparoscope, is placed into the abdomen through one of these openings. It lets the surgeon see what he or she is doing during the operation.
Using small instruments inserted into the abdomen through other small openings, the surgeon removes fluid and stones from the gallbladder to deflate it. The gallbladder can then be detached from the digestive system and removed through one of the openings.
People tend to recover very quickly from laparoscopic surgery because the surgical wounds are very small.
Open cholecystectomy can be a better option for gallbladder removal among people who have significant abdominal scarring from prior surgery or those who are very obese.
About 5% of the time, a surgeon starts a laparoscopic procedure but changes to an open cholecystectomy for technical reasons.
For stones caught in the common bile duct, an additional treatment called endoscopic retrograde cholangiopancreatography (ERCP) might be needed.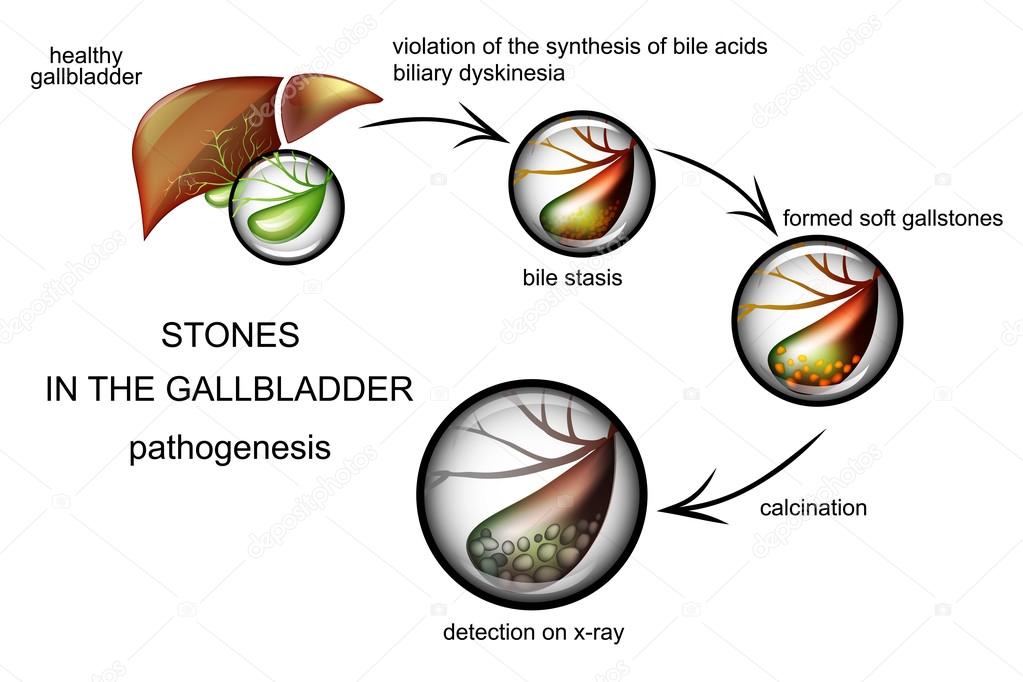 A doctor uses miniature instruments attached to a camera at the end of a flexible tube called an endoscope. The endoscope is passed maneuvered from the mouth down the esophagus and into the intestine. The doctor can tug stones out of the bile duct, or can widen the lower part of the duct so they pass into the intestine on their own.
A doctor uses miniature instruments attached to a camera at the end of a flexible tube called an endoscope. The endoscope is passed maneuvered from the mouth down the esophagus and into the intestine. The doctor can tug stones out of the bile duct, or can widen the lower part of the duct so they pass into the intestine on their own.
Medication
When surgery is not a good option, an oral medication known as ursodeoxycholic acid (Actigall) may help. It usually takes about six months to see results, and is effective only about half the time. Once the medication is stopped, gallstones are likely to return.
Other procedures
Two other ways to break up gallstones include:
- shockwaves (lithotripsy) to break apart the gallstones so they can pass out of the body on their own
- dissolving gallstones with chemicals injected directly into the gallbladder
Surgery is strongly preferred over these other treatments because stones are likely to form again if the gallbladder is not removed.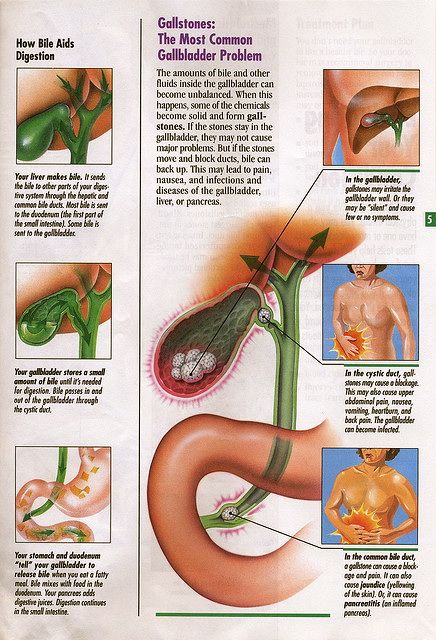
90,000 symptoms, treatment. What causes stones in the gallbladder?
The disease ranks third in prevalence after cardiovascular and endocrine pathologies. The disease is more often diagnosed in women.
Gallbladder stones: causes and mechanism of disease development
Stones in the gallbladder and bile ducts are formed due to a violation of the process of metabolism of bile components. Pathology develops with the simultaneous presence of the following factors: the production of lithogenic bile (supersaturated with cholesterol), an imbalance between the activity of pronucleating and antinucleating components, and a decrease in the contractile function of the gallbladder.
Among the main causes of gallstone disease are:
- hereditary factor;
- overweight;
- dramatic weight loss;
- eating foods high in cholesterol and low in fiber;
- inflammatory processes and biliary dyskinesia;
- taking oral contraceptives;
- malabsorption syndrome;
- disorders in the work of the endocrine system;
- Crohn’s disease;
- liver disease.

Also, the disease can develop during pregnancy.
There are 2 main mechanisms for the development of the process of formation of stones in the gallbladder: vesicoinflammatory and hepatometabolic. The first variant develops against the background of an inflammatory process, leading to a violation of the acid-base balance of bile and a decrease in the protection of protein fractions, which causes crystallization of bilirubin. Further, the epithelium and mucus join it, which causes the formation of a calculus. In the second case, the disease develops against the background of a violation of the metabolic processes of the liver, which is often the result of existing liver diseases, unbalanced nutrition, endocrine disorders, hypothyroidism.
Symptoms of cholelithiasis
The disease develops gradually and may not manifest itself in the early stages. The average growth rate of stones is 3-5 mm per year, so the first symptoms often appear only after a few years.
Symptoms of gallstone disease are varied and depend on the location of the stones, their size, etc. You can suspect stones in the gallbladder by the following signs:
- pain and heaviness in the right hypochondrium;
- bitter taste in the mouth;
- nausea;
- flatulence and other bowel disorders;
- belching of air;
- yellowing of the skin and mucous membranes.
Many of these symptoms may indicate other diseases, so for an accurate diagnosis, you need to see a doctor. You can contact a general practitioner or go directly to a gastroenterologist. The main method for diagnosing cholelithiasis is ultrasound, it allows not only to confirm the diagnosis, but also to determine the exact localization of stones and their size.
Treatment of cholelithiasis
If stones are found in the gallbladder, treatment should be started immediately. Otherwise, the disease will progress and lead to complications, including: acute cholecystitis, pancreatitis, perforation of the gallbladder, stones in the intestines and the formation of intestinal obstruction.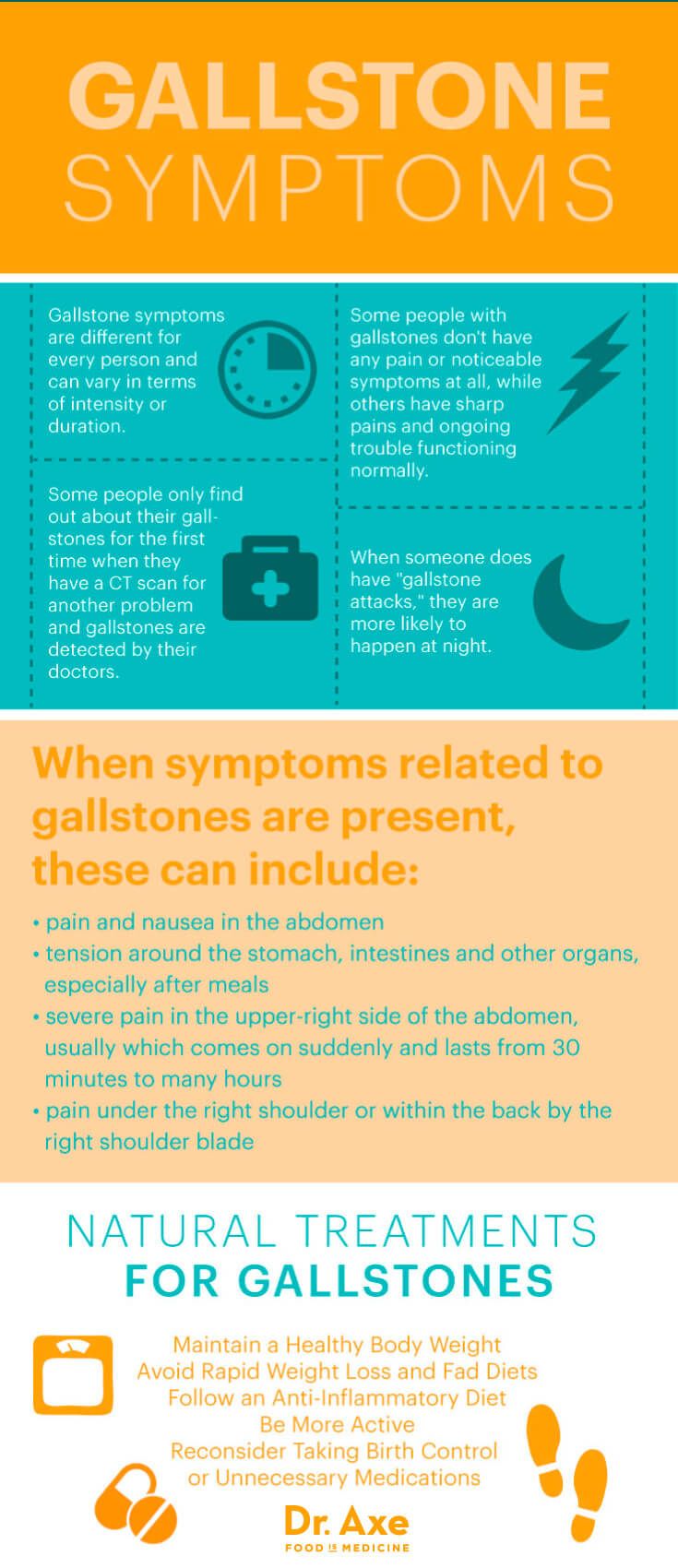 Also, over time, the disease can provoke the development of an oncological process in the gallbladder.
Also, over time, the disease can provoke the development of an oncological process in the gallbladder.
The possibilities of modern medicine make it possible to successfully treat gallstone disease. The main thing is to choose the right tactics. There are 2 main options here:
- conservative treatment;
- surgery.
Conservative treatment is aimed at dissolving stones with the help of special preparations and crushing them with the help of a laser or ultrasound. There are a number of contraindications to these methods of treatment, besides, it does not always completely solve the problem, therefore, an operation is often prescribed for stones in the gallbladder – cholecystectomy, which involves the removal of the gallbladder.
To date, most often the removal of the gallbladder is carried out by the modern laparoscopic method, since the strip operation requires a longer rehabilitation. Laparoscopy is performed under general anesthesia: the surgeon makes 2-4 punctures of the abdominal wall. A video endoscope with a light source is inserted into one puncture, and manipulators into the others. The whole process usually takes 1-2 hours. After that, the patient is sent to the hospital. In the absence of complications, in most cases, the patient is discharged after one or two days.
A video endoscope with a light source is inserted into one puncture, and manipulators into the others. The whole process usually takes 1-2 hours. After that, the patient is sent to the hospital. In the absence of complications, in most cases, the patient is discharged after one or two days.
Laparoscopic cholecystectomy can be done at the DIALINE Surgery Center. The operation is carried out using advanced high-precision equipment, which, combined with the extensive experience of our specialists, allows us to solve the problem quickly and without consequences.
You can make an appointment with a gastroenterologist either on your own in your DIALINE personal account or by ordering a call back.
Do not delay treatment, see a doctor right now:
Cholelithiasis, surgery to remove gallbladder stones price in SP
A chronic disease of the biliary tract, in which stones form in the gallbladder (more often) and bile ducts, is called cholelithiasis (GSD).
If stones are detected in the common bile duct, then this form of gallstone disease is called choledocholithiasis .
Historical information
The disease has been known since ancient times. For the first time, gallbladder stones were discovered during the autopsy and described by Galen, the great surgeon, writer and philosopher, who lived in the second half of the 2nd century AD in ancient Rome. During the Renaissance, in the writings of Gentile de Foligno in 1341, there is also a mention of CL.
A detailed description of gallbladder stones appeared in the middle of the 18th century (C. Galeati), and at the same time, the study of their chemical composition was first undertaken. All information about cholelithiasis contained in the works of various authors was summarized by Albrecht Haller (1755). In his works, he showed that gallstones are found not only in humans, but also in horses, pigs, cows, marmots, monkeys and other animals.
He divided all stones of the gallbladder and ducts into 2 groups:
- Large ovoid, often solitary, consisting of “a tasteless yellow substance which, when heated, melts like sealing wax and is liable to burn”.

- Smaller, dark-colored, multifaceted, which are often found not only in the gallbladder, but also in the bile ducts.
Since the middle of the 19th century, there have been various theories of the origin of gallstones. Of these, two main directions can be distinguished.
Supporters of one of them saw the cause of cholelithiasis in an abnormal state of the liver. Such a liver produces bile of a changed composition, as a result of which its dense parts precipitate, forming stones. Other researchers considered bile stasis and inflammation of the biliary tract and gallbladder as the main cause of the disease.
More thorough work on GSD appeared already in the 20th century. In addition to a detailed study of the structure of gallstones, a theory of the occurrence of cholelithiasis was developed. It was based on the concept of “stagnant gallbladder” and metabolic disorders.
The incidence of gallstone disease
The incidence of gallstone disease has increased dramatically in the last decade and continues to increase. According to the National Institutes of Health (1992), 10-15% of the adult population of the world suffers from gallstone disease. Seeking doctors for bile duct and gallbladder stones in the Russian Federation is approximately 1 million people a year.
According to the National Institutes of Health (1992), 10-15% of the adult population of the world suffers from gallstone disease. Seeking doctors for bile duct and gallbladder stones in the Russian Federation is approximately 1 million people a year.
Women get sick 3-5 times more often than men, and cholelithiasis was also more common in them (5-6 times) than in men.
Modern understanding of the causes leading to gallstones
- First, it is a metabolic disorder that affects the chemical composition of bile. The composition of bile, which is a complex chemical solution, includes poorly soluble substances. In order for them not to precipitate, it is necessary to preserve them in strict proportions. If their percentage is violated in one direction or another, then a precipitate forms, which can then turn into stones.
- Secondly, this is a violation of the correct movement of bile along the bile ducts . The occurrence of obstacles to the outflow of bile into the duodenum, long periods of starvation lead to stagnation of bile in the gallbladder, its thickening and precipitation.

In turn, the formation of stones contributes to the disruption of the normal process of digestion: there are failures in the formation, storage and secretion of bile, which is one of the most important components for proper digestion of food. There are groups of people who are at high risk of gallstone disease and chronic calculous cholecystitis.
The following risk factors are distinguished:
- Heredity . The likelihood of developing gallbladder and duct stones increases in the presence of direct relatives suffering from this pathology.
- Diseases associated with metabolic disorders: diabetes mellitus, gout, obesity, atherosclerosis, decreased thyroid function.
- Liver diseases : cirrhosis, fatty liver, chronic hepatitis.
- Diseases of the digestive system eg pancreatitis, duodenitis, colitis, dysbacteriosis and others. Sometimes there is the so-called “Saint’s triad” – a combination of cholelithiasis with diaphragmatic hernia and diverticulosis of the colon.

- Physical inactivity.
- Improper diet: abuse of high-fat, high-calorie foods, sweets.
- Prolonged fasting, diets . A break in eating for more than 8 hours, as well as a long diet that does not contain animal fats, leads to stagnation in the gallbladder.
- Taking certain medications, such as steroid hormones and oral contraceptives.
- Changes in hormonal balance during pregnancy.
- Smoking and alcohol abuse .
Symptoms of gallstone disease
The manifestations of the disease are extremely varied. Most often, the following forms of GSD are distinguished:
- latent,
- chronic dyspeptic,
- chronic pain,
- chronic relapsing,
- other forms.
In a certain sense, these forms can be considered as stages in the development of cholelithiasis. In the same patient, after a period of latent course, dyspeptic disorders may appear, after a while – a moderately severe pain syndrome and, finally, typical attacks of hepatic colic. However, such a development of the disease is far from necessary. Often, its first manifestation may be an attack of acute cholecystitis and hepatic colic.
However, such a development of the disease is far from necessary. Often, its first manifestation may be an attack of acute cholecystitis and hepatic colic.
Dyspeptic form of cholelithiasis
It is characterized by complaints associated with a violation of the digestive process. There is a feeling of heaviness in the stomach, heartburn, flatulence, unstable stool. Usually these sensations occur periodically, but can be permanent. They usually occur after meals. Moreover, patients often associate their appearance with the use of certain foods: fatty, fried, spicy dishes. The appearance of complaints can also be associated with taking too large portions of food.
Painful chronic form of cholelithiasis
It proceeds without bouts of acute pain. The pains are aching in nature, localized under the pit of the stomach and in the region of the right hypochondrium, aggravated after eating, especially fatty foods. Their irradiation to the region of the right scapula is characteristic.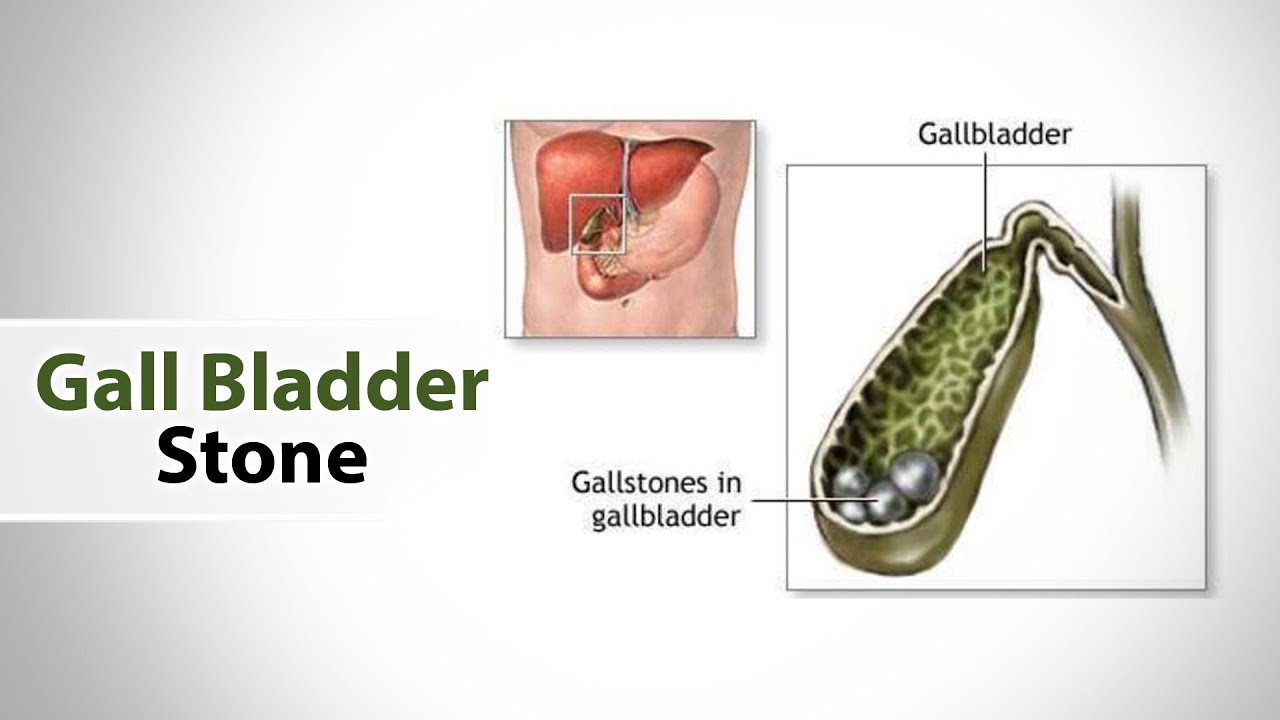 The long existence of stones in the gallbladder can last indefinitely, but, ultimately, leads to the occurrence of an inflammatory process in it.
The long existence of stones in the gallbladder can last indefinitely, but, ultimately, leads to the occurrence of an inflammatory process in it.
Chronic calculous cholecystitis
One of the frequent manifestations of chronic calculous cholecystitis is constant heaviness and pain in the right hypochondrium, nausea, which is aggravated by fatty and spicy foods. Small stones can be manifested by hepatic colic: an attack of acute pain in the right side of the abdomen, sometimes in the epigastric region. An attack can be triggered by the intake of fatty spicy foods or alcohol, as well as shaking while driving or stress. Vomiting and nausea are frequent companions of pain. Characterized by irradiation of pain in the right shoulder blade, right shoulder or right arm. The cause of a painful attack may be wedging a stone into the neck of the gallbladder. This leads to severe spasm. The gallbladder itself at this time is significantly reduced, trying to push out the bile, but a stuck stone prevents it from leaving. The duration of the pain attack is different – from several minutes to many hours and even days. If the obstruction has been removed and the stone has ceased to block the exit from the gallbladder, the symptoms quickly subside. Vomiting stops, temperature normalizes; general well-being improves. For some time, weakness and a feeling of weakness persist, and dyspeptic phenomena are occasionally noted. The patient’s condition may remain quite satisfactory until the next attack, which may develop in a few days, weeks, months or years.
The duration of the pain attack is different – from several minutes to many hours and even days. If the obstruction has been removed and the stone has ceased to block the exit from the gallbladder, the symptoms quickly subside. Vomiting stops, temperature normalizes; general well-being improves. For some time, weakness and a feeling of weakness persist, and dyspeptic phenomena are occasionally noted. The patient’s condition may remain quite satisfactory until the next attack, which may develop in a few days, weeks, months or years.
Consequences of chronic cholecystitis
People who suffer from chronic cholecystitis for a long time end up risking their health and even their lives. The inflammatory process from the gallbladder spreads to neighboring organs, primarily the pancreas and liver. Almost all such patients have a chronic form of pancreatitis and changes in the liver. At the same time, irreversible changes occur in the gallbladder, which leads to three options for the development of the disease.
- 1. The process of gallstone formation does not stop. The addition of infection and inflammation creates favorable conditions for the growth and formation of new stones. The bubble is filled with stones and ceases to be a reservoir for the accumulation of bile. It cannot perform its main functions in the digestive process. Food is poorly digested.
- 2. Frequent inflammation of the gallbladder due to attacks of hepatic colic leads to a change in the wall of the gallbladder: it becomes overgrown with adhesions, and the muscles are replaced by dense scar tissue. The bladder cavity sharply decreases in size, a “scar-wrinkled bladder” is formed, which also does not participate in the digestion process.
- 3. When the cystic duct is blocked by a stone, the bladder becomes large and overdistended. Overflowing with bile, which does not find a way out, the bladder loses its ability to contract, and even after the stone leaves the duct, it remains stretched, while it is no longer able to push out the bile.
 Gradually, the contents become colorless – “white bile”. Hydrocele of the gallbladder develops. Sometimes it is asymptomatic (apparently, the patient simply forgets about the attack). However, if dropsy appeared after an attack of hepatic colic, the enlarged gallbladder remains painful for a long time. Such a gallbladder is also turned off from the digestion process. In addition, bile, which remains in the gallbladder and is not renewed, easily suppurates when an infection joins, gallbladder empyema develops.
Gradually, the contents become colorless – “white bile”. Hydrocele of the gallbladder develops. Sometimes it is asymptomatic (apparently, the patient simply forgets about the attack). However, if dropsy appeared after an attack of hepatic colic, the enlarged gallbladder remains painful for a long time. Such a gallbladder is also turned off from the digestion process. In addition, bile, which remains in the gallbladder and is not renewed, easily suppurates when an infection joins, gallbladder empyema develops.
It is necessary to carry out a differential diagnosis of biliary (hepatic) colic from an attack of acute calculous cholecystitis. This is inflammation of the gallbladder, provoked by the presence of stones in it, which is manifested not only by severe pain, but also by the presence of fever, signs of intoxication, sometimes positive peritoneal symptoms and requires emergency inpatient treatment. The appearance of a fever, jaundice, and a decrease in blood pressure in a patient with cholelithiasis requires the exclusion of such possible complications as acute cholecystitis, pancreatitis, cholangitis, etc.
Basic methods for diagnosing gallbladder stones
Laboratory studies
- With exacerbation of gallstone disease, changes in the clinical blood test are observed: the number of leukocytes increases with the appearance of their young forms, the ESR rises, which indicates the presence of an inflammatory process. There may be changes in the biochemical parameters of the blood: an increase in the level of hepatic transaminases, amylase, lipase, total bilirubin. In most cases of asymptomatic stone carrying, the blood test may not be changed. Also, without changes in laboratory parameters, short attacks of biliary colic can pass.
Instrumental diagnostics
- 1. The most affordable and effective method for screening diagnostics of all stages of cholelithiasis is ultrasound examination of the abdominal organs (ultrasound). Ultrasound of the liver and gallbladder allows you to see stones in the bladder cavity, determine their size, mobility, evaluate the size of the residual cavity of the gallbladder, identify signs of inflammation or deformation of its wall.
 Also, with ultrasound, the intra- and extrahepatic bile ducts are clearly visible, it is possible to assess their deformation, expansion and the presence of additional inclusions (calculi) in them.
Also, with ultrasound, the intra- and extrahepatic bile ducts are clearly visible, it is possible to assess their deformation, expansion and the presence of additional inclusions (calculi) in them. - 2. A more accurate diagnosis of the condition of the biliary tract is shown by magnetic resonance imaging – MR cholangiography.
When performing MR – cholangiography, an image of the gallbladder, cystic duct, segmental, lobar ducts, common hepatic duct, choledochus and main pancreatic duct is obtained. You can evaluate their deformation, identify the expansion or narrowing of their lumen in certain areas. It becomes possible to accurately visualize stones not only in the gallbladder, but also in the lumen of the bile ducts. Additional examination methods for cholelithiasis include computed tomography (CT) and videoduodenoscopy. - 3. Computed tomography (CT) of the abdominal cavity is performed in case of suspected pathology of neighboring organs (liver, pancreas), in case of suspected oncological pathology in the biliary system.

- 4. Videogastroduodenoscopy is an endoscopic examination that resembles videogastroscopy, but is performed using a special endoscope with lateral optics, which allows you to clearly see the area of \u200b\u200bthe major duodenal papilla or “papilla of Vater” (the place where the bile ducts enter the duodenum).
Treatment of cholelithiasis and chronic calculous cholecystitis
Conservative treatment of gallstones
In the arsenal of doctors there are preparations of ursodeoxycholic acid, which changes the chemical composition of bile. These are drugs henofalk and ursofalk, they are prescribed for the purpose of drug lithosis (dissolution of stones). Treatment should be carried out against the background of strict adherence to diet and diet, as well as anti-inflammatory therapy. The duration of treatment is up to 2.5-3 years and does not always achieve the desired result. It should be remembered that true “stones”, consisting mainly of calcium, do not dissolve. Therefore, drug treatment can be used only in the initial stages of the disease, when the sediment in the bile is mainly represented by cholesterol stones.
Therefore, drug treatment can be used only in the initial stages of the disease, when the sediment in the bile is mainly represented by cholesterol stones.
Gallbladder removal surgery with stones
Cholecystectomy – removal of the gallbladder – the main method of surgical treatment. The operation is performed either in an open way through an incision in the abdominal wall, or laparoscopically – endovideosurgical cholecystectomy. The purpose of the operation: removal of the gallbladder with stones. The difference lies only in what instruments the surgeon works with and in what way the gallbladder with stones is removed.
In an open surgical operation, the incision through which the bladder is removed can be made from the xiphoid process to the navel, or the second access can be made in the right hypochondrium. The laparoscopic method is less traumatic – special instruments and optics are inserted through 4 small incisions on the skin. With the help of these tools, the gallbladder is removed. After such an operation, the scars are hardly noticeable. The length of stay in a hospital bed is 2-3 days. A week later, the patient is well.
After such an operation, the scars are hardly noticeable. The length of stay in a hospital bed is 2-3 days. A week later, the patient is well.
Patient essential
In the modern world, cholelithiasis is a well-studied pathology, and laparoscopic surgery is the “gold standard of treatment”. Unfortunately, many people do not pay attention to the initial manifestations of the disease, do not undergo clinical examination or preventive examination to detect stones in the gallbladder. As a result, the disease is detected at late stages, when drug treatment is not only ineffective, but also contraindicated, and the success of a minimally invasive surgical operation also becomes doubtful.
In the presence of the complaints described above, as well as the listed risk factors, it is necessary to contact a surgeon or a gastroenterologist for recommendations on examination and selection of optimal treatment or preventive measures.
Our Clinic performs a full range of diagnostics, surgical and endoscopic treatment of cholelithiasis and its complications.


 These shock waves can break gallstones into smaller pieces.
These shock waves can break gallstones into smaller pieces.



 Gradually, the contents become colorless – “white bile”. Hydrocele of the gallbladder develops. Sometimes it is asymptomatic (apparently, the patient simply forgets about the attack). However, if dropsy appeared after an attack of hepatic colic, the enlarged gallbladder remains painful for a long time. Such a gallbladder is also turned off from the digestion process. In addition, bile, which remains in the gallbladder and is not renewed, easily suppurates when an infection joins, gallbladder empyema develops.
Gradually, the contents become colorless – “white bile”. Hydrocele of the gallbladder develops. Sometimes it is asymptomatic (apparently, the patient simply forgets about the attack). However, if dropsy appeared after an attack of hepatic colic, the enlarged gallbladder remains painful for a long time. Such a gallbladder is also turned off from the digestion process. In addition, bile, which remains in the gallbladder and is not renewed, easily suppurates when an infection joins, gallbladder empyema develops.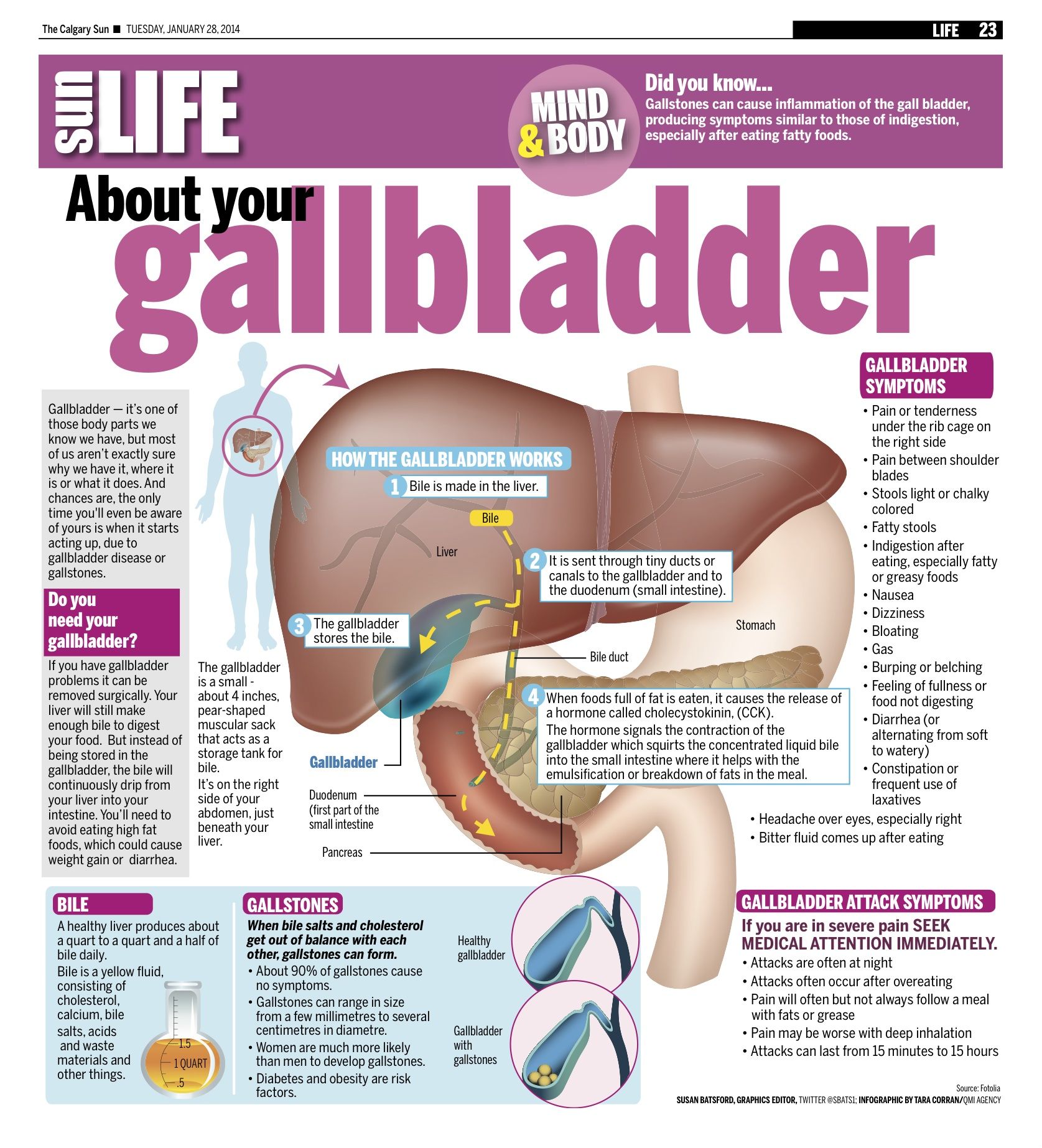 Also, with ultrasound, the intra- and extrahepatic bile ducts are clearly visible, it is possible to assess their deformation, expansion and the presence of additional inclusions (calculi) in them.
Also, with ultrasound, the intra- and extrahepatic bile ducts are clearly visible, it is possible to assess their deformation, expansion and the presence of additional inclusions (calculi) in them.