Achilles tendon injury diagnosis. Achilles Tendon Injuries: Diagnosis, Causes, and Treatment Options
What are the common causes of Achilles tendon injuries. How are Achilles tendon injuries diagnosed. What are the most effective treatment options for Achilles tendonitis. Can Achilles tendon injuries be prevented. What are the risk factors for developing Achilles tendon problems. How long does it take to recover from an Achilles tendon injury. When should you seek medical attention for Achilles tendon pain.
Understanding the Achilles Tendon: Function and Importance
The Achilles tendon is a crucial component of the human musculoskeletal system, connecting the calf muscles to the heel bone. This fibrous band of tissue plays a vital role in everyday activities such as walking, running, and jumping. Its strength and flexibility are essential for proper movement and athletic performance.
Given its importance, injuries to the Achilles tendon can significantly impact a person’s mobility and quality of life. These injuries range from mild inflammation to complete ruptures, each requiring specific attention and treatment.

The Anatomy of the Achilles Tendon
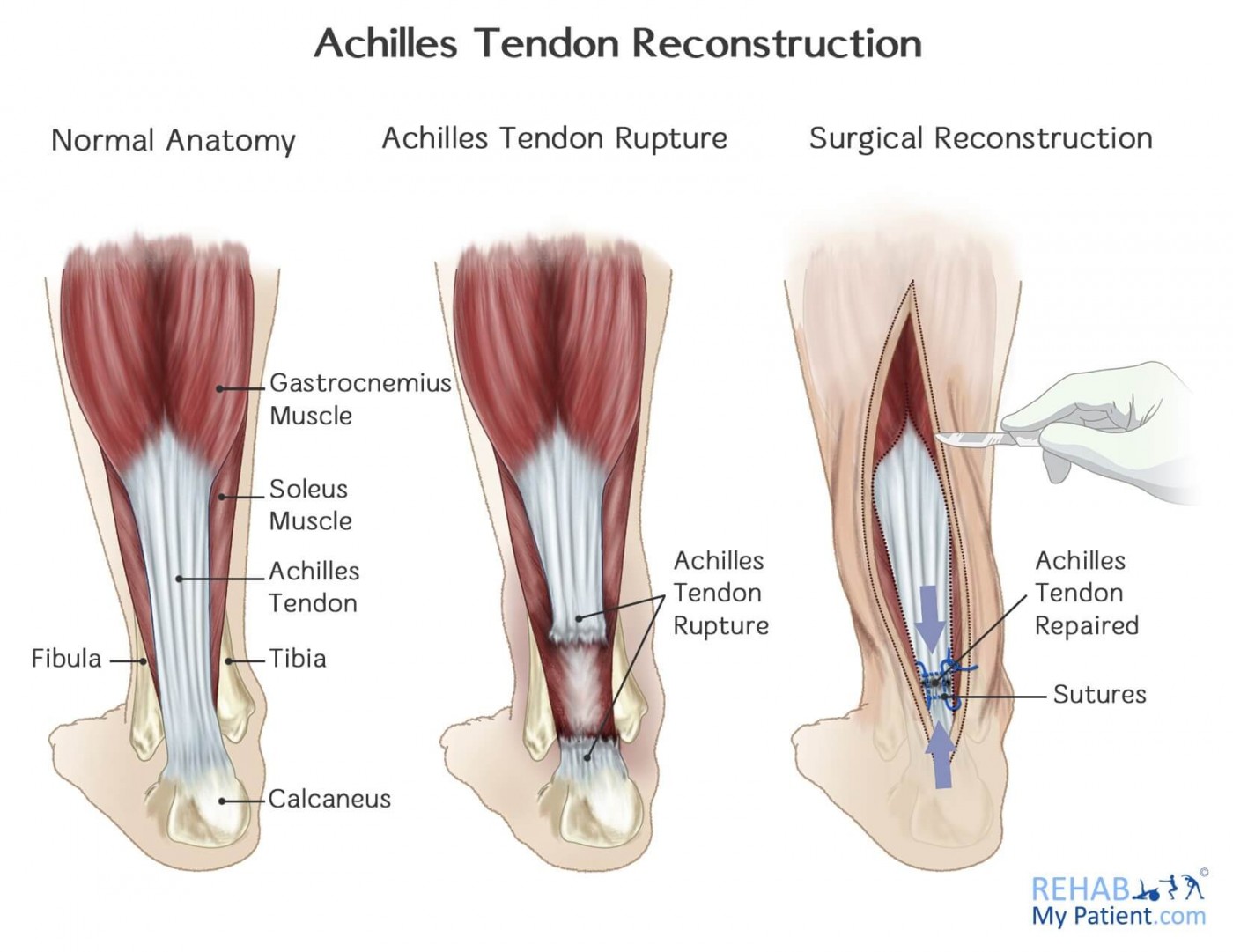
To fully comprehend Achilles tendon injuries, it’s essential to understand its anatomy. The tendon is composed of strong, fibrous tissue that extends from the gastrocnemius and soleus muscles in the calf down to the calcaneus (heel bone). This structure allows for the transfer of force from the calf muscles to the foot, enabling powerful movements like pushing off the ground when walking or running.
Types of Achilles Tendon Injuries: Tendonitis and Ruptures
Achilles tendon injuries primarily fall into two categories: tendonitis and ruptures. Each type has distinct characteristics and requires different approaches to treatment.
Achilles Tendonitis: Inflammation and Irritation
Tendonitis occurs when the Achilles tendon becomes inflamed, swollen, and irritated. This condition can be further classified into two main types:
- Non-insertional Achilles tendonitis: This type affects the middle fibers of the tendon and is more common in younger, active adults.
- Insertional Achilles tendonitis: This occurs where the tendon meets the heel bone and can affect individuals of any age, regardless of activity level.
Both types of tendonitis can lead to pain, swelling, and reduced flexibility in the affected area.

Achilles Tendon Ruptures: Partial and Complete Tears
A more severe injury is an Achilles tendon rupture, which can be either partial or complete. Ruptures often occur suddenly and may be accompanied by a distinctive “popping” sound. These injuries require immediate medical attention and often necessitate surgical intervention.
Causes and Risk Factors for Achilles Tendon Injuries
Understanding the causes and risk factors associated with Achilles tendon injuries is crucial for both prevention and effective treatment. While these injuries can affect anyone, certain factors increase the likelihood of their occurrence.
Common Causes of Achilles Tendon Injuries
Achilles tendon injuries often result from a combination of factors, including:
- Overuse or repetitive stress on the tendon
- Sudden increases in exercise intensity or duration
- Improper footwear or training techniques
- Inadequate warm-up before physical activity
- Direct trauma to the tendon
Risk Factors Contributing to Achilles Tendon Problems
Several risk factors can predispose individuals to Achilles tendon injuries:

- Age: The risk of tendon injuries increases with age
- Gender: Men are more likely to experience Achilles tendon ruptures
- Obesity: Excess weight puts additional stress on the tendon
- Certain medical conditions: Diabetes and high blood pressure can increase risk
- Medications: Some antibiotics, particularly fluoroquinolones, have been associated with tendon problems
- Previous injuries: A history of tendon injuries increases the likelihood of future problems
Recognizing the Symptoms of Achilles Tendon Injuries
Identifying the symptoms of Achilles tendon injuries is crucial for early intervention and proper treatment. The manifestation of symptoms can vary depending on the type and severity of the injury.
Common Symptoms of Achilles Tendonitis
Individuals with Achilles tendonitis may experience:
- Pain and stiffness along the tendon, especially in the morning
- Increased discomfort during or after physical activity
- Swelling that worsens throughout the day
- Thickening of the tendon
- Bone spurs (in cases of insertional tendonitis)
Signs of an Achilles Tendon Rupture
A ruptured Achilles tendon often presents with more severe and sudden symptoms, including:

- A sudden “pop” or snapping sensation in the back of the leg
- Severe pain, as if being kicked or shot in the back of the ankle
- Difficulty walking or bearing weight on the affected leg
- Inability to stand on tiptoes or push off the ground with the injured leg
- Swelling and bruising around the heel and lower leg
Diagnosing Achilles Tendon Injuries: Medical Approaches
Accurate diagnosis of Achilles tendon injuries is essential for appropriate treatment and recovery. Healthcare providers employ various methods to assess the nature and extent of these injuries.
Physical Examination Techniques
The diagnostic process typically begins with a thorough physical examination. During this assessment, the healthcare provider may:
- Inspect the affected area for swelling, discoloration, or deformity
- Palpate the tendon to check for tenderness, thickening, or gaps in the tissue
- Evaluate the range of motion and strength of the ankle and foot
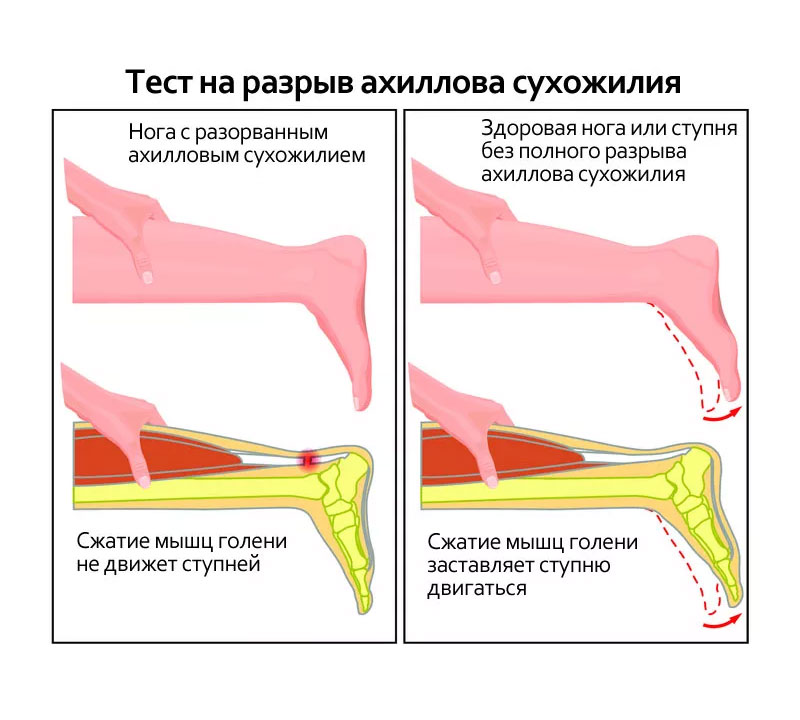
- Perform specific tests, such as the Thompson test, to assess tendon function
Imaging Studies for Achilles Tendon Injuries
To confirm the diagnosis and determine the extent of the injury, imaging studies may be necessary. Common imaging techniques include:

- X-rays: While not typically used to diagnose soft tissue injuries, X-rays can help rule out other conditions or identify bone spurs
- Ultrasound: This non-invasive technique provides real-time images of the tendon and can help assess its structure and any tears
- Magnetic Resonance Imaging (MRI): MRI scans offer detailed images of the tendon and surrounding tissues, helping to identify partial tears or other subtle injuries
Treatment Options for Achilles Tendon Injuries
The treatment of Achilles tendon injuries varies depending on the type and severity of the condition. A comprehensive approach often involves a combination of conservative measures and, in some cases, surgical intervention.
Conservative Treatment Approaches
For many Achilles tendon injuries, especially in the early stages, conservative treatments can be effective. These may include:
- Rest and activity modification to reduce stress on the tendon
- Ice therapy to manage pain and swelling
- Compression and elevation to minimize inflammation
- Non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief
- Physical therapy exercises to improve flexibility and strength
- Orthotic devices or heel lifts to reduce tendon strain
Surgical Interventions for Severe Cases
In cases of severe tendonitis or complete ruptures, surgery may be necessary. Surgical options include:
- Tendon repair: For complete ruptures, the torn ends of the tendon are sutured together
- Tendon transfer: In cases where the tendon has degraded significantly, a tendon from another part of the foot may be used to reinforce or replace the damaged Achilles tendon
- Gastrocnemius recession: This procedure involves lengthening the calf muscles to reduce tension on the Achilles tendon
Rehabilitation and Recovery from Achilles Tendon Injuries
Proper rehabilitation is crucial for successful recovery from Achilles tendon injuries. The rehabilitation process aims to restore strength, flexibility, and function while preventing re-injury.
Phases of Rehabilitation
Rehabilitation typically progresses through several phases:
- Protection phase: Involving rest, immobilization, and pain management
- Early mobilization: Gentle range of motion exercises and gradual weight-bearing
- Strengthening: Progressive exercises to rebuild tendon and muscle strength
- Functional training: Sport-specific or activity-specific exercises to prepare for return to normal activities
Timeline for Recovery
The recovery timeline varies depending on the severity of the injury and the treatment approach. Generally:
- Mild tendonitis may improve within a few weeks with proper care
- More severe cases of tendonitis can take several months to heal completely
- Recovery from surgical repair of a ruptured tendon typically takes 4-6 months, with a full return to sports often possible after 6-12 months
Preventing Achilles Tendon Injuries: Strategies for Long-term Health
While not all Achilles tendon injuries can be prevented, adopting certain strategies can significantly reduce the risk of developing these problems.
Effective Prevention Techniques
To minimize the risk of Achilles tendon injuries, consider the following preventive measures:
- Gradually increase exercise intensity and duration to avoid sudden stress on the tendon
- Incorporate proper warm-up and cool-down routines into your exercise regimen
- Wear appropriate footwear that provides adequate support and cushioning
- Maintain a healthy body weight to reduce excess stress on the tendons
- Cross-train with low-impact activities to vary the stress on your tendons
- Stretch and strengthen the calf muscles regularly
- Listen to your body and avoid pushing through pain
By understanding the causes, symptoms, and treatment options for Achilles tendon injuries, individuals can take proactive steps to maintain the health of this crucial tendon. Whether you’re an athlete or someone who enjoys casual physical activity, proper care and attention to your Achilles tendon can help ensure long-term mobility and comfort. Remember, early intervention is key in managing these injuries effectively, so don’t hesitate to seek medical attention if you experience persistent pain or discomfort in your Achilles tendon area.
Achilles Tendon Injuries | Johns Hopkins Medicine
What are Achilles tendon injuries?
The Achilles tendon is a fibrous band of tissue that links the muscles in your calf to your heel. The strength and flexibility of this tendon are important for jumping, running, and walking. Your Achilles tendon withstands a lot of stress and pressure during everyday activities, as well as during athletic and recreational play. If it becomes inflamed, swollen, and irritated, it is called tendonitis.
What causes Achilles tendon injuries?
Tendonitis
Tendonitis might be due to overuse or damage to the area. It can cause pain down the back of your leg and around your heel. You might notice that parts of your tendon are getting thicker, and hardening, because of tendonitis. This will get worse if you don’t treat it. There are 2 main types of tendonitis:
Non-insertional Achilles tendonitis. Small tears in the middle fibers of your tendon start to break it down.
 This causes pain and swelling. This type of tendonitis usually affects active, younger adults
This causes pain and swelling. This type of tendonitis usually affects active, younger adultsInsertional Achilles tendonitis. This damage occurs in the spot where your tendon meets your heel bone. Bone spurs (extra bone growth) often form with this type. This type of tendonitis can happen at any age, even in people who are not active.
Rupture
The tears in your tendon fibers can cause a complete or partial break (or tear) in your tendon. You might hear a “pop” that seems to come from the back of your heel or calf. This may be a tendon rupture, which needs immediate medical attention.
Achilles Tendinosis: Q&A with Dr. Nigel Hsu
Dr. Nigel Hsu answers common questions about diagnosis and treatment of Achilles tendinosis.
Key points about Achilles tendon injuries
Your Achilles tendon can develop tendonitis. This is when it becomes inflamed, swollen, and irritated.
The Achilles tendon can also tear or rupture, which might sound like a “pop” that seems to come from the back of your heel or calf. This needs immediate medical attention.
Anyone can develop an Achilles tendon injury and it’s often linked to repetitive stress on the tendon.
Achilles tendon injuries often cause pain, stiffness, and swelling in the back of your leg near your heel.
Achilles tendon injuries can be treated with rest and medicines to help with the inflammation. Exercises often help too. If needed, surgery can be done to repair the tendon.
You can help prevent these injuries by doing things like increasing activity slowly, wearing the correct shoes for your activities, and not exercising on uneven surfaces.

Seminar
Common Sports and Activity Related Injuries: What to Consider from Pain to Breaks
Learn more about common sports injuries and treatments to consider from our sports medicine expert Alex Johnson, M.D., and our foot and ankle expert John Thompson, M.D., in this webinar-based video.
Watch the webinar
What are the risk factors for Achilles tendon injuries?
Anyone can develop an Achilles tendon injury. They’re often linked to repetitive stress. The most common risk factors are:
Increased amount or intensity of an activity or sport
Starting a new sport
Tight calf muscles when starting an exercise or sport, this can place more stress on your tendon
Bone spurs on your heel, which can rub against the tendon
Wearing the wrong shoes when you exercise
Exercising on an uneven surface
Treatment with fluoroquinolone, an antibiotic
What are the symptoms of an Achilles tendon injury?
Common symptoms of tendon injuries include:
Pain down the back of your leg or near your heel
Pain that gets worse when you’re active
A stiff, sore Achilles tendon when you first get up
Pain in the tendon the day after exercising
Swelling with pain that gets worse as you’re active during the day
Thickening of your tendon
Bone spurs on the heel bone
Difficulty flexing the affected foot
A “pop” sound and sudden sharp pain, which suggests a ruptured tendon
How is an Achilles tendon injury diagnosed?
Injury to the Achilles tendon causes pain along the back of your leg near the heel. Sometimes healthcare providers misdiagnose Achilles tendon injuries as a sprained ankle. It’s important to get the right diagnosis so you can get the right treatment. Several common injuries can make your Achilles tendon painful or prevent it from working well.
Sometimes healthcare providers misdiagnose Achilles tendon injuries as a sprained ankle. It’s important to get the right diagnosis so you can get the right treatment. Several common injuries can make your Achilles tendon painful or prevent it from working well.
To diagnose your condition, your doctor will consider:
Your overall health and medical history
A description of your symptoms
A physical exam of your Achilles tendon to check for bone spurs, pain, and swelling
A test of your ankle’s range of motion (ability to move as it should)
Imaging tests, such as X-ray or magnetic resonance imaging (MRI). An X-ray shows bones and can show if the tendon has become calcified or hardened, and can show bone spurs. Your doctor will use MRI most often to see how severe the tendon damage is and what treatment is best for you.
How are Achilles tendon injuries treated?
Treatment depends on how badly injured your tendon is.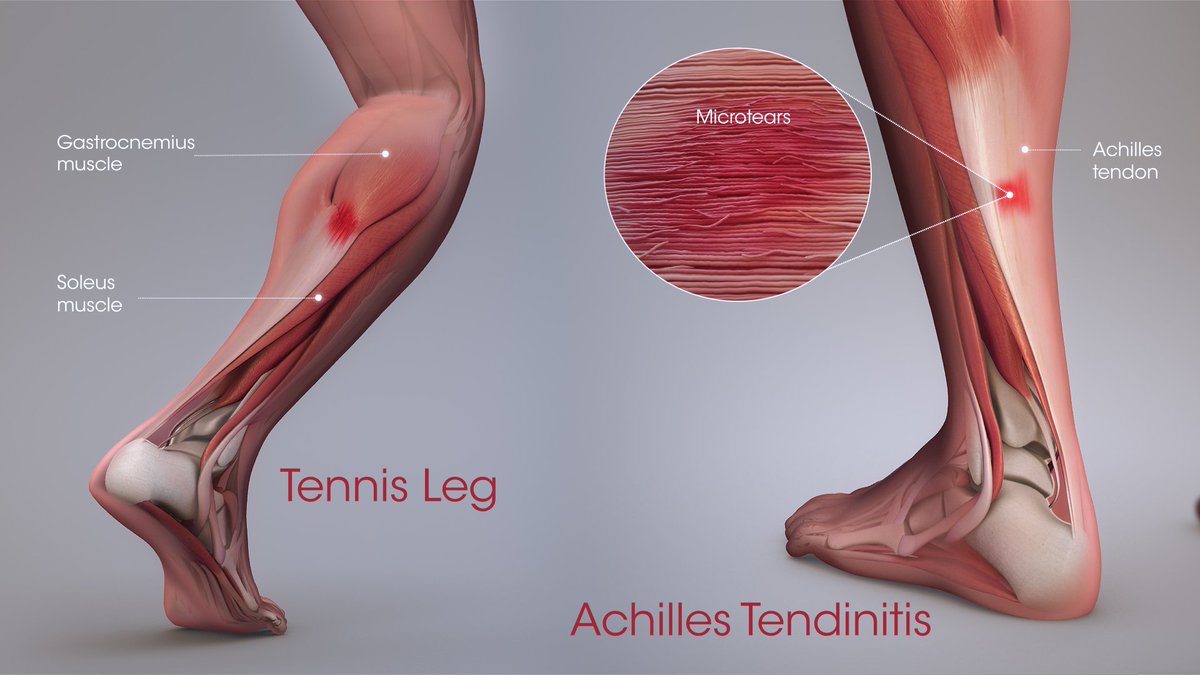 It may include:
It may include:
Rest
Ice
Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief (such as, ibuprofen or naproxen)
Specific exercises to strengthen your calf muscles
Physical therapy
A system of exercises that help strengthen your calf muscles to take the pressure off your tendon (eccentric strength training).
Low-impact exercise alternatives, such as swimming
Heel lifts in shoes, orthotic shoes, cast, splint, or a walking boot
Extracorporeal shockwave therapy: High-energy shockwave impulses help stimulate the healing process in damaged tendon tissue. This treatment isn’t often used, but your doctor may recommend it to see whether you can improve without surgery.
If these do not work, or if the injury is severe or complete, surgery may be considered. The type of surgery depends on the location and amount of damage to the tendon and other factors, such as the severity of the tendonitis. Some of the surgical procedures used include:
The type of surgery depends on the location and amount of damage to the tendon and other factors, such as the severity of the tendonitis. Some of the surgical procedures used include:
Surgery to lengthen your calf muscles (this is called gastrocnemius recession)
Debridement surgery to remove damaged tendon tissue or bone spurs and repair the tendon
Surgery to remove your damaged tendon tissue, repair the remaining tendon, and give it extra strength by moving another tendon to the heel bone (the tendon moved there is the one that helps the big toe point down)
What are the complications of Achilles tendon injuries?
Complications of an Achilles tendon injury may include:
Pain, which can be severe
Difficulty walking or being active
Deformation of your tendon area or heel bone
Tendon rupture from reinjury
Other complications can be related to the treatments used for an Achilles tendon injury. For instance,
For instance,
How can I prevent Achilles tendon injuries?
These steps can help prevent injury to your Achilles tendon:
Warm-up before exercising or before sports or other repetitive movements.
Increase activity slowly, rather than all at once.
Wear the correct shoes for your activities.
Do not exercise on uneven surfaces.
Stop activities that cause pain.
Be aware of the risks of fluoroquinolone and exercise with caution if you’re taking this drug.
How to manage an Achilles tendon injury
Follow your doctor’s recommendations to get rest and manage pain and swelling.
Choose alternative ways to be active.
Try low-impact activities that do not place a lot of stress on your tendon, such as swimming or bicycling, rather than a high-impact exercise like running.

Always let your doctor know if these strategies don’t help reduce pain, swelling, and loss of function.
When should I call my healthcare provider?
Call your doctor immediately if you hear a “pop” sound and have sudden pain in the back of your leg or heel. Otherwise, schedule an appointment if pain or trouble moving affects your regular daily activities.
Achilles Tendon Injuries (Tear, Rupture) Causes, Symptoms, Treatments
Written by WebMD Editorial Contributors
In this Article
- What Is an Achilles Tendon Injury?
- Achilles Tendon Injury Symptoms
- Achilles Tendon Injury Causes
- Achilles Tendon Injury Risks
- Achilles Tendon Injury Diagnosis
- Achilles Tendon Injury Treatment
- Achilles Tendon Surgery
- Achilles Tendon Injury Recovery
- Achilles Tendon Injury Prevention
An Achilles tendon injury can happen to anyone, whether you’re an athlete or just going about your everyday life.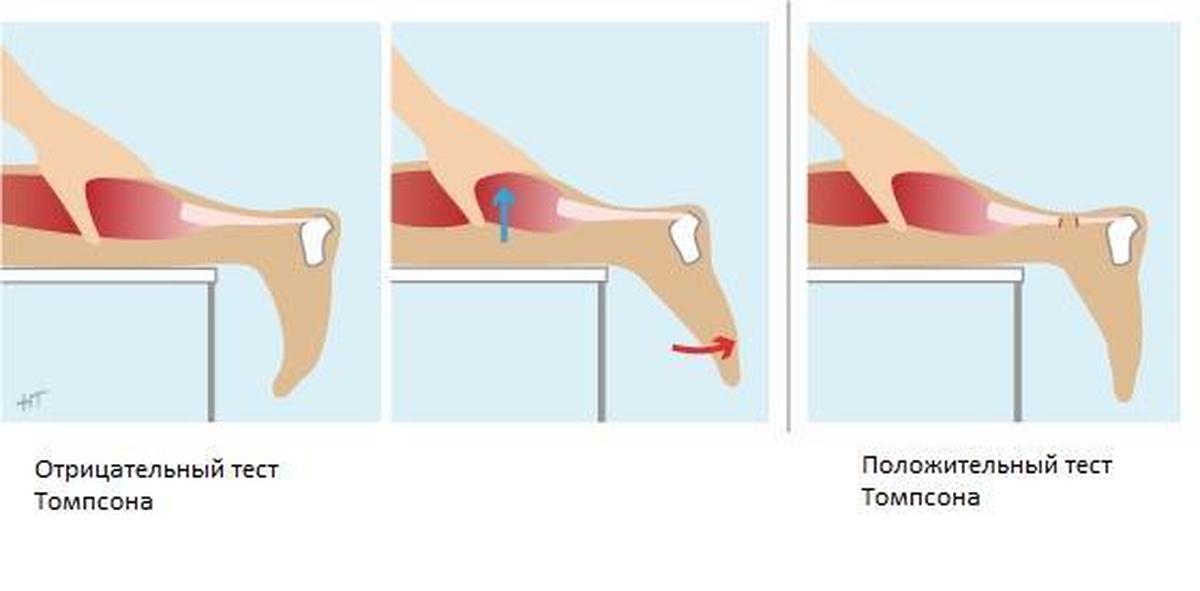
The Achilles tendon is the largest tendon in your body. It stretches from the bones of your heel to your calf muscles. You can feel it: a springy band of tissue at the back of your ankle and above your heel. It lets you point your toes toward the floor and raise up on your tiptoes.
It’s common for this tendon to get injured. It can be mild or moderate and feel like a burning pain or stiffness in that part of your leg. If the pain is severe, your Achilles tendon may be partly or completely torn.
Achilles tendinitis is another type of injury in which some part of your tendon is inflamed. There are two main types of this condition, which affect different parts of your tendon:
- Noninsertional Achilles tendinitis. Fibers in the middle of your tendon break down, swell, and get thick.
- Insertional Achilles tendinitis. This affects the lower part of your heel, where your tendon inserts, or goes into, your heel bone. It can cause bone spurs.

The most obvious sign is pain above your heel, especially when you stretch your ankle or stand on your toes. It may be mild and get better or worse over time. If the tendon ruptures, the pain is instant and severe. The area may also feel tender, swollen, and stiff.
If your Achilles tendon tears, you may hear a snapping or popping noise when it happens. You could have bruising and swelling, too. You also may have trouble pointing your toes and pushing off your toes when you take a step.
Achilles tendon injuries are common in people who do things where they quickly speed up, slow down, or pivot, such as:
- Running
- Gymnastics
- Dance
- Football
- Soccer
- Baseball
- Softball
- Basketball
- Tennis
- Volleyball
These injuries tend to happen when you start moving suddenly as you push off and lift your foot rather than when you land. For instance, a sprinter might get one at the start of a race as they surge off the starting block. The abrupt action can be too much for the tendon to handle. Men over 30 are especially prone to Achilles tendon injuries.
The abrupt action can be too much for the tendon to handle. Men over 30 are especially prone to Achilles tendon injuries.
You can also injure your Achilles tendon if you stress it over and over again with high-impact activities. These are known as repetitive stress injuries.
You don’t have to be an athlete to get this kind of injury. If you step into a hole or fall from a high place, you could rupture your Achilles.
These things may make you more likely to get an Achilles tendon injury:
- You wear high heels, which can stress the tendon.
- You have “flat feet,” also called fallen arches. This means that when you take a step, the impact causes the arch of your foot to collapse, stretching the muscles and tendons.
- Your leg muscles or tendons are too tight.
- You have bone spurs.
- You add time to your exercise routine or do more intense activity.
- You start a new type of exercise.
- You wear shoes that don’t fit well or aren’t right for the kind of physical activity you do.

- You work out on uneven surfaces.
- You take medicines called glucocorticoids or antibiotics called fluoroquinolones.
- You have a chronic condition that can weaken your Achilles, like rheumatoid arthritis, lupus, gout, or diabetes.
Doctors sometimes mistake an Achilles tendon injury for sprained ankle. To make the right diagnosis, your doctor will start with a physical exam. They may want to see you walk or run so they can look for problems that might have led to your injury.
They also might do something called the calf squeeze test. You’ll kneel on a chair or bench or lie on your stomach on the exam table. Your doctor will gently squeeze the calf muscle on your healthy leg. This will pull on the tendon and make your foot move. Next, they’ll do the same thing on your other leg. If your Achilles tendon is torn, your foot won’t move, because your calf muscle won’t be connected to your foot.
Your doctor may test your range of motion to see if you can move your ankle the way you should. They may also do imaging tests, such as X-ray or MRI. These tests can show what kind of tendon damage you have and help them decide on the best treatment for you.
They may also do imaging tests, such as X-ray or MRI. These tests can show what kind of tendon damage you have and help them decide on the best treatment for you.
Minor to moderate Achilles tendon injuries should heal on their own. To speed the process, you can:
• Rest your leg. Avoid putting weight on it as best you can. You may need crutches.
• Ice it. Ice your injury for up to 20 minutes at a time as needed.
• Compress your leg. Use an elastic bandage around the lower leg and ankle to keep down swelling.
• Raise (elevate) your leg. Prop it on a pillow when you’re sitting or lying down.
• Take anti-inflammatory painkillers. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can help with pain and swelling. Follow the instructions on the label to help prevent side effects, such as bleeding and ulcers. Take them with food. Check with your doctor first if you have any allergies, have medical problems, or take any other medication. If you need them for longer than 7 to 10 days, call your doctor.
If you need them for longer than 7 to 10 days, call your doctor.
• Use a heel lift. Your doctor may recommend that you wear an insert in your shoe while you recover. It will help protect your Achilles tendon from further stretching.
• Practice stretching and strengthening exercises. Your doctor or physical therapist can recommend ones for you to try.
• Take part in low-impact activities. When your doctor says it’s OK, activities like swimming can help promote healing.
If your Achilles is torn, your doctor may recommend surgery. The younger and more active you are, the more likely that surgery will be the best option.
You should have the surgery within 4 weeks of the injury. Your surgeon will make a small incision in the back of your ankle and sew the Achilles back together. Sometimes they’ll need to sew other tendons in to make things even stronger. Between 80% and 90% of these operations are successful.
Your doctor could decide not to do surgery if you’re older and less active, or if you have only a partial tear.
The nonsurgical route will involve lots of physical therapy and doing stretches and exercises on your own. You might also have ultrasound or shockwave therapy. You may have to wear a cast, a walking boot, or heel cups to take pressure off the tendon and keep it from moving.
You’ll have a longer road to full recovery, and you’ll run a bigger risk of reinjuring the tendon.
Recovery may take months, but it depends on how serious your injury is. Different conditions heal at different rates.
You can still be active while your injury heals. Ask your doctor what’s OK to do. But don’t rush things. Don’t try to return to your old level of physical activity until:
- You can move your leg as easily and freely as your uninjured leg.
- Your leg feels as strong as your uninjured leg.
- You don’t have any pain in your leg when you walk, jog, sprint, or jump.

If you push yourself too much before your Achilles tendon injury fully heals, you could get injured again, and the pain could become a long-lasting problem. You may be able to avoid some of these issues if you replace high-impact sports like running with low-impact exercise. Activities such as swimming or cycling put less stress on your tendon.
Here are some things you can try:
- Stretch and strengthen your calves.
- Cut down on uphill running.
- Wear shoes with good support that fit well.
- Stop exercising if you feel pain or tightness in the back of your calf or heel.
Top Picks
Diagnosis of Achilles tendon injury
Achilles tendon rupture is characterized by a bright clinical picture, so the diagnosis is not difficult./GettyImages-184840231-0dbb00039d6a49a8827ea381e6c0572b.jpg) In some situations (before surgery, to clarify the diagnosis and assess the severity of the process), the doctor may prescribe a number of studies. But, as a rule, the orthopedist is limited to taking an anamnesis and examining the affected leg.
In some situations (before surgery, to clarify the diagnosis and assess the severity of the process), the doctor may prescribe a number of studies. But, as a rule, the orthopedist is limited to taking an anamnesis and examining the affected leg.
- History taking
When communicating with a patient, the doctor asks about complaints and asks leading questions. He is interested, for example, what actions caused the current pain, what circumstances preceded this, what kind of pain, the time of its manifestation, the intensity, whether something was done to alleviate it. The orthopedist should receive information about concomitant diseases and medications that the patient is taking or has recently taken, about the profession and habits. The doctor will definitely ask what kind of sports the victim does, how many times a week, how and where the training takes place, how intense the training is and whether there is an excessive load on the legs. At risk are cyclists, volleyball players, athletes, football players and gymnasts. Tennis, basketball, diving involve kicking off the surface with your feet, so they are also at risk. Athletes who train less than once a week (athletes of the “weekend”) and do not pay enough attention to the warm-up are more likely to damage the Achilles tendon. The traumatologist will ask what kind of shoes the victim prefers and whether new shoes have been recently purchased? It will find out whether there were falls and injuries, whether there was a tendon rupture before, whether there were blows directly to the tendon area with a sharp or blunt object, whether relatives suffer from diseases of the musculoskeletal system.
Tennis, basketball, diving involve kicking off the surface with your feet, so they are also at risk. Athletes who train less than once a week (athletes of the “weekend”) and do not pay enough attention to the warm-up are more likely to damage the Achilles tendon. The traumatologist will ask what kind of shoes the victim prefers and whether new shoes have been recently purchased? It will find out whether there were falls and injuries, whether there was a tendon rupture before, whether there were blows directly to the tendon area with a sharp or blunt object, whether relatives suffer from diseases of the musculoskeletal system.
- Inspection
After the interview, the doctor proceeds to the examination. He asks the victim to pass, asks if his gait has changed, if he can walk on tiptoe and stand on one leg. With a tendon injury, the victim limps, sometimes moves with difficulty and cannot stand on his toes due to severe pain.
A dent can be found a few centimeters above the heel if there is a tear (if not obese).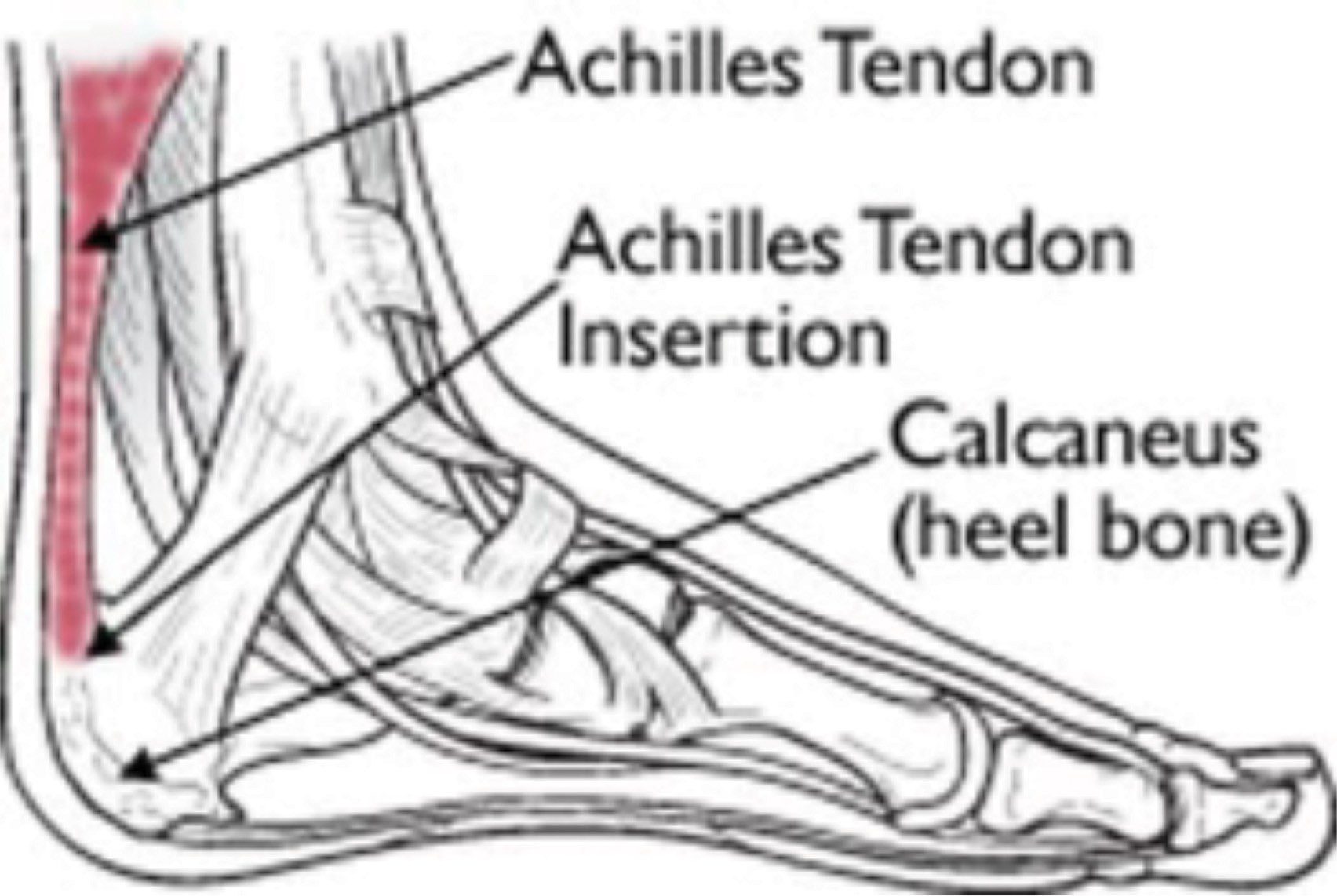 Sometimes the location or extent of the accompanying bruise indicates the nature of the injury. Decisive, however, is the altered mobility in the joint. Increased mobility in the joint can only be checked if a fracture has been ruled out by X-ray.
Sometimes the location or extent of the accompanying bruise indicates the nature of the injury. Decisive, however, is the altered mobility in the joint. Increased mobility in the joint can only be checked if a fracture has been ruled out by X-ray.
- Physical examination
Palpation examination plays an essential role in the diagnosis. The traumatologist asks the patient to lie on the couch on his stomach so that the foot hangs over the edge. He gently palpates the affected area, tracing the integrity of the fibers with his fingers. In order to exclude diagnostic errors, special tests must be carried out.
In some doubtful situations, traumatologists have to resort to additional research methods. They are also addressed in cases where several days or even weeks have passed after the injury or the developed edema and hematoma make a full diagnosis impossible.
- Ultrasound
An ultrasound is performed to confirm the diagnosis. This is the fastest and most common method. Ultrasound usually shows signs of calcification, inflammatory indurations, degenerative nodules, or fissures. Examination may reveal posterior calcaneal bursitis or tendon thickening. Ultrasound helps to assess the degree of injury, differentiate tear or rupture of the tendon fibers in the victim, but requires sufficient experience and knowledge from the expert for correct interpretation.
This is the fastest and most common method. Ultrasound usually shows signs of calcification, inflammatory indurations, degenerative nodules, or fissures. Examination may reveal posterior calcaneal bursitis or tendon thickening. Ultrasound helps to assess the degree of injury, differentiate tear or rupture of the tendon fibers in the victim, but requires sufficient experience and knowledge from the expert for correct interpretation.
- Color Doppler
Color Doppler can detect vascular grafts.
- MRI
Thanks to magnetic resonance imaging, even the smallest tendon defects can be detected. It is an ideal examination and produces high quality images, so it can be especially useful in unclear cases or for planned surgery. With the help of magnetic resonance imaging (MRI), you can accurately see all ligamentous structures and associated injuries, heel spurs; signs of Haglund’s deformity and bursitis. However, an MRI is only ordered if recovery is slow or if a more serious injury is suspected due to an accidental mechanism. Not used for standard diagnostics.
Not used for standard diagnostics.
- X-ray
X-rays are not usually required for diagnosis. Anterior and lateral images are prescribed (heel, ankle joint) rather as excluding other diseases. For example, an X-ray image shows a heel spur, which can cause similar symptoms, or a crack or fracture in the calcaneus may be visible. Additional x-rays are taken only for specific problems, such as in cases of suspected chronic instability or before surgery.
- Laboratory tests
Laboratory tests aid in the diagnosis of other underlying diseases. Therefore, the doctor may prescribe a clinical and biochemical analysis of blood and urine.
***
Experts believe that in more than 90% of cases, a doctor can diagnose a fresh Achilles tendon rupture through a physical examination. In some cases, to differentiate with another pathology, it is necessary to conduct an instrumental examination. The exception is mainly for injuries that are older than 48 hours. After this time, the ligaments may rupture during the examination and lead to disrupted scarring with permanent instability. Also, very pronounced edema can limit the duration of the examination. Therefore, if a tendon rupture is suspected, it is urgent to contact the emergency room.
The exception is mainly for injuries that are older than 48 hours. After this time, the ligaments may rupture during the examination and lead to disrupted scarring with permanent instability. Also, very pronounced edema can limit the duration of the examination. Therefore, if a tendon rupture is suspected, it is urgent to contact the emergency room.
Achilles tendon treatment in Germany
The largest and strongest tendon in the human body is the Achilles tendon, formed by the fusion of the flat tendons of the gastrocnemius muscle with the soleus. It is located on the back of the lower leg and is responsible for flexing the ankle joint. Between the tendon itself and the surface of the calcaneus is a mucous bag that reduces friction between them. After various injuries, an inflammatory process begins in this bag, developing into Achilles tendon bursitis, the treatment of which should not be postponed. Any delay with treatment can lead to tendon rupture and even complete immobilization of the joint.
Achilles injuries mostly affect people 30 – 50 years of age. Tendon rupture usually occurs at a distance of 4-5 cm from the place of its attachment to the calcaneus, since it is in this area that the level of blood circulation is reduced.
Achilles tendon injuries: causes
Treatment of the Achilles tendon may be needed for a variety of reasons. According to the type of impact, injuries can be:
- direct, for example, a blow with a sharp or heavy blunt object;
- indirect, caused by a sudden muscle contraction due to an unsuccessful fall, a sharp jump and other unsuccessful movements.
Achilles tendon rupture and surgery is often caused by degeneration resulting from prolonged inflammation or treatment with corticosteroids.
Achilles injury symptoms
The first thing a person feels when the Achilles tendon is damaged is a sharp pain. The moment of injury can sometimes be accompanied by an unpleasant crunch or crackle, as a result of which the functionality of the affected leg is noticeably reduced. Edema occurs at the site of damage, which after a few days turns into a large hematoma, while capturing the entire lower part of the leg. If the Achilles tendon is not treated in a timely manner, then the risks of lameness or complete loss of leg performance are maximum.
Edema occurs at the site of damage, which after a few days turns into a large hematoma, while capturing the entire lower part of the leg. If the Achilles tendon is not treated in a timely manner, then the risks of lameness or complete loss of leg performance are maximum.
Diagnosis
To determine the type of treatment – conservative or Achilles tendon surgery, it is necessary to correctly identify the cause of the pain. Due to the fact that X-rays do not linger in the tissues of the tendon, it is impossible to determine the likelihood of a rupture using radiography. To diagnose a rupture, specialists use magnetic resonance imaging and ultrasound diagnostics.
Regardless of the established diagnosis, partial damage, rupture or bursitis of the Achilles tendon, treatment in any case should be timely.
Achilles injury: treatment by German orthopedists
Depending on the severity of the injury, the Achilles tendon is treated using two main methods:
- conservative therapy;
- Achilles tendon surgery.

The essence of the conservative is to ensure tissue fusion by immobilizing the leg using special brace, hypo splints and cuts. The duration of such treatment is from 6 to 8 weeks and it is shown mainly to people whose motor activity is reduced. And when a person leading an active lifestyle or a professional athlete is diagnosed with an Achilles rupture, surgery is the most effective way to restore the usefulness of limb functions.
Surgical treatment of Achilles injuries
The most reliable and effective way to restore Achilles after an injury is surgery. And the sooner it is carried out, the more satisfactory the result will be. Achilles tendon surgery is performed under spinal or local anesthesia and under general anesthesia.
Taking into account the duration of the injury and the nature of the injury, as well as the physiological characteristics of the patient, surgical procedures can be as follows:
- subcutaneous suture.
 This method is used in cases where no more than a week has passed from the moment of damage and it is possible to completely match the torn ends of the Achilles;
This method is used in cases where no more than a week has passed from the moment of damage and it is possible to completely match the torn ends of the Achilles; - open suture, in which the plastic of the tendon of the plantar muscle is performed. The method is used in cases where a displacement occurred during a rupture and the ends of the damaged Achilles are not matched;
- Achilles plasty by gastrocnemius fascia is effective when the ends of the tendon have undergone excessive defibration caused by an injury lasting 3 weeks or more.
Regardless of the complexity of the Achilles rupture, operations are carried out at a high professional level by specialists from German clinics using minimally invasive techniques. Surgeons perform suturing by endoscopic access or using separate skin punctures.
Postoperative rehabilitation
Achilles after surgery requires a long rehabilitation. The first few days after the operation, the patient is observed in the hospital.

 This causes pain and swelling. This type of tendonitis usually affects active, younger adults
This causes pain and swelling. This type of tendonitis usually affects active, younger adults





 This method is used in cases where no more than a week has passed from the moment of damage and it is possible to completely match the torn ends of the Achilles;
This method is used in cases where no more than a week has passed from the moment of damage and it is possible to completely match the torn ends of the Achilles;