Black Chalky Poop: Causes, Symptoms, and Treatment of Melena
What are the causes of black chalky poop. How to identify melena. When should you seek medical attention for black stools. What diagnostic tests are used for black tarry stools. How is gastrointestinal bleeding treated.
Understanding Black Chalky Poop: Melena Explained
Black chalky poop, medically known as melena, is a condition characterized by black or tarry stools with a foul odor. This unusual appearance of feces is often a sign of a problem in the upper digestive tract, typically indicating bleeding in the stomach, small intestine, or right side of the colon. The dark, tar-like consistency occurs when blood is exposed to digestive enzymes, resulting in a chemical reaction that alters its color.
It’s important to note that not all black stools are cause for concern. Certain foods and medications can cause similar discoloration without any underlying health issues. However, true melena is a serious condition that requires prompt medical attention.

Common Causes of Harmless Black Stools
- Consuming black licorice
- Eating blueberries or other dark-colored fruits
- Ingesting blood sausage
- Taking iron supplements
- Using activated charcoal
- Consuming medications containing bismuth (e.g., Pepto-Bismol)
In these cases, the stool’s appearance should return to normal once the causative substance is no longer consumed. If you’re unsure about the cause of your black stools, it’s always best to consult with a healthcare professional.
Identifying Melena: Signs and Symptoms
Recognizing melena is crucial for early detection and treatment of potential gastrointestinal issues. The primary characteristics of melena include:
- Black, tarry appearance of stool
- Foul, distinctive odor
- Sticky or tacky consistency
Accompanying symptoms may include:
- Abdominal pain or discomfort
- Fatigue or weakness
- Shortness of breath
- Pale skin
- Dizziness or lightheadedness
Can melena be confused with other conditions? Yes, it’s possible to mistake melena for other digestive issues. For instance, iron supplements can cause dark stools that may resemble melena. However, true melena has a distinctive tar-like appearance and strong odor that sets it apart from other causes of dark stools.

Medical Conditions Associated with Melena
Several medical conditions can lead to the development of melena. Understanding these potential causes is essential for proper diagnosis and treatment.
Peptic Ulcers: A Common Culprit
Peptic ulcers are the most frequent cause of acute upper gastrointestinal bleeding, often resulting in melena. These ulcers are open sores that develop on the lining of the stomach or small intestine, often due to bacterial infection or long-term use of certain medications.
Other Potential Causes of Melena
- Esophageal varices: Enlarged veins in the esophagus, often associated with liver cirrhosis
- Gastritis: Inflammation of the stomach lining
- Mallory-Weiss tear: A tear in the esophagus caused by severe vomiting
- Gastrointestinal cancers: Tumors in the esophagus, stomach, or small intestine
- Angiodysplasia: Abnormal blood vessels in the gastrointestinal tract
- Dieulafoy’s lesion: A rare condition where a large, abnormal blood vessel near the stomach surface bleeds
Is melena always a sign of a serious condition? While melena often indicates a significant health issue, the severity can vary. Some causes, like peptic ulcers, are treatable with medication, while others may require more intensive interventions. Regardless, any occurrence of melena warrants medical evaluation to determine the underlying cause and appropriate treatment.

Diagnostic Approaches for Black Tarry Stools
When a patient presents with black tarry stools, healthcare providers employ various diagnostic methods to identify the underlying cause and determine the appropriate course of treatment.
Initial Assessment and Medical History
The diagnostic process typically begins with a thorough medical history and physical examination. Healthcare providers may ask questions about:
- Recent medication use, including blood thinners and NSAIDs
- Dietary habits, focusing on foods that could cause dark stools
- Frequency and duration of the black stools
- Associated symptoms such as abdominal pain, vomiting, or weight loss
- Recent trauma or accidental ingestion of foreign objects
Laboratory Tests and Imaging Studies
Following the initial assessment, several diagnostic tests may be ordered:
- Stool tests: To confirm the presence of blood and rule out infections
- Complete blood count (CBC): To assess for anemia and infection
- Coagulation studies: To evaluate blood clotting function
- Serum chemistries: To check electrolyte balance and organ function
- Helicobacter pylori testing: To detect the bacteria associated with peptic ulcers
- Imaging studies: Such as CT scans or angiography to visualize the gastrointestinal tract
Endoscopic Procedures
Endoscopic examinations play a crucial role in diagnosing the cause of melena:

- Esophagogastroduodenoscopy (EGD): Examines the upper GI tract
- Colonoscopy: Investigates the large intestine
- Capsule endoscopy: Uses a swallowable camera to visualize the small intestine
- Double balloon enteroscopy: Allows examination of hard-to-reach areas of the small intestine
How accurate are these diagnostic methods? While each test has its strengths and limitations, combining multiple diagnostic approaches significantly increases the likelihood of identifying the source of bleeding. Endoscopic procedures, in particular, offer high accuracy in detecting and often treating the cause of melena.
Treatment Strategies for Gastrointestinal Bleeding
The treatment of melena depends on its underlying cause and the severity of bleeding. Management strategies range from conservative approaches to emergency interventions.
Conservative Management
For mild cases or when bleeding has stopped:
- Medication adjustments: Discontinuing or modifying drugs that may contribute to bleeding
- Dietary changes: Avoiding irritants and incorporating gut-friendly foods
- Proton pump inhibitors: To reduce stomach acid and promote healing of ulcers
- Antibiotics: If H. pylori infection is detected
Endoscopic Interventions
Endoscopy serves both diagnostic and therapeutic purposes:

- Cauterization: Using heat to seal bleeding vessels
- Clip application: Placing small clips to close bleeding sites
- Injection therapy: Introducing substances to stop bleeding
- Band ligation: For treating esophageal varices
Surgical Approaches
In severe cases or when endoscopic treatments fail, surgical intervention may be necessary:
- Partial gastrectomy: Removal of a portion of the stomach
- Bowel resection: Removing a segment of the intestine
- Vascular repair: Addressing abnormal blood vessels
Emergency Management
For acute, severe bleeding:
- Fluid resuscitation: To maintain blood pressure and organ perfusion
- Blood transfusions: To replace lost blood and correct anemia
- Intensive care monitoring: For close observation and rapid intervention if needed
What factors determine the choice of treatment? The selection of treatment depends on several factors, including the location and severity of bleeding, the patient’s overall health status, and the availability of specific interventions. A multidisciplinary approach, involving gastroenterologists, surgeons, and critical care specialists, often yields the best outcomes.

Preventing Recurrence of Melena
After successful treatment of melena, preventing its recurrence becomes a priority. Strategies for prevention often target the underlying cause and may include:
Lifestyle Modifications
- Dietary changes: Avoiding trigger foods and alcohol
- Stress reduction techniques: Such as meditation or yoga
- Regular exercise: To promote overall digestive health
- Smoking cessation: As smoking can increase the risk of ulcers and GI bleeding
Medication Management
Working closely with healthcare providers to:
- Adjust or discontinue medications that may increase bleeding risk
- Properly manage conditions like GERD or peptic ulcer disease
- Consider protective medications if long-term use of NSAIDs is necessary
Regular Check-ups and Monitoring
Maintaining ongoing medical care through:
- Scheduled follow-up appointments
- Periodic endoscopic examinations if recommended
- Prompt reporting of any recurrent symptoms
How effective are these preventive measures? When followed diligently, these strategies can significantly reduce the risk of recurrent melena. However, the effectiveness may vary depending on the underlying cause and individual patient factors. Regular communication with healthcare providers is key to tailoring prevention strategies to each patient’s specific needs.

Long-term Outlook and Quality of Life Considerations
The long-term prognosis for individuals who have experienced melena varies depending on the underlying cause and the effectiveness of treatment. Understanding the potential impacts on quality of life and strategies for adaptation is crucial for patients and their caregivers.
Prognosis Factors
Several factors influence the long-term outlook:
- Cause of the bleeding: Some conditions, like peptic ulcers, have a better prognosis than others, such as advanced cancers
- Severity of the initial episode: More severe bleeding may lead to complications that affect long-term health
- Timeliness of treatment: Early intervention often leads to better outcomes
- Overall health status: Pre-existing conditions can impact recovery and future risk
- Adherence to follow-up care: Regular monitoring and preventive measures reduce recurrence risk
Quality of Life Considerations
Melena and its underlying causes can affect various aspects of life:
- Physical well-being: Fatigue, weakness, or ongoing digestive issues may persist
- Dietary restrictions: Some patients may need to modify their diet long-term
- Medication management: Regular use of preventive medications may be necessary
- Emotional impact: Anxiety about recurrence or complications can affect mental health
- Social implications: Dietary restrictions or fear of symptoms may impact social activities
Coping Strategies and Support
To enhance quality of life post-melena, consider:
![]()
- Patient education: Understanding the condition and its management empowers patients
- Support groups: Connecting with others who have similar experiences can provide emotional support
- Psychological counseling: To address anxiety or depression related to the condition
- Nutritional counseling: To develop a healthy, satisfying diet within necessary restrictions
- Regular exercise: To improve overall health and well-being, as approved by healthcare providers
Can patients expect to return to normal life after experiencing melena? Many patients can return to a normal or near-normal life after successful treatment and implementation of preventive measures. However, some may need to make long-term lifestyle adjustments. The key is working closely with healthcare providers to develop a personalized plan that balances medical needs with quality of life considerations.
In conclusion, while melena can be a frightening experience, understanding its causes, recognizing its symptoms, and knowing when to seek medical attention are crucial steps in managing this condition. With proper diagnosis, treatment, and ongoing care, many individuals can overcome melena and maintain a good quality of life. Always consult with healthcare professionals for personalized advice and treatment options.
Black or tarry stools: MedlinePlus Medical Encyclopedia
Black or tarry stools with a foul smell are a sign of a problem in the upper digestive tract. It most often indicates that there is bleeding in the stomach, small intestine, or right side of the colon.
The term melena is used to describe this finding.
Eating black licorice, blueberries, blood sausage or taking iron pills, activated charcoal, or medicines that contain bismuth (such as Pepto-Bismol), can also cause black stools. Beets and foods with red coloring can sometimes make stools appear reddish. In all these cases, your doctor can test the stool with a chemical to rule out the presence of blood.
Bleeding in the esophagus or stomach (such as with peptic ulcer disease) can also cause you to vomit blood.
The color of the blood in the stools can indicate the source of bleeding.
- Black or tarry stools may be due to bleeding in the upper part of the GI (gastrointestinal) tract, such as the esophagus, stomach, or the first part of the small intestine.
 In this case, blood is darker because it gets digested on its way through the GI tract.
In this case, blood is darker because it gets digested on its way through the GI tract. - Red or fresh blood in the stools (rectal bleeding), is a sign of bleeding from the lower GI tract (rectum and anus).
Peptic ulcers are the most common cause of acute upper GI bleeding. Black and tarry stools may also occur due to:
- Abnormal blood vessels in the esophagus, stomach, or duodenum
- A tear in the esophagus from violent vomiting (Mallory-Weiss tear)
- Blood supply being cut off to part of the intestines
- Inflammation of the stomach lining (gastritis)
- Trauma or foreign body
- Widened, overgrown veins (called varices) in the esophagus and stomach, commonly caused by liver cirrhosis
- Cancer of the esophagus, stomach, duodenum, or ampulla of Vater
Contact your health care provider right away if:
- You notice blood or changes in the color of your stool
- You vomit blood
- You feel dizzy or lightheaded
In children, a small amount of blood in the stool is most often not serious. The most common cause is constipation. You should still tell your child’s provider if you notice this problem.
The most common cause is constipation. You should still tell your child’s provider if you notice this problem.
Your provider will take a medical history and perform a physical exam. The exam will focus on your abdomen.
You may be asked the following questions:
- Are you taking blood thinners, such as aspirin, warfarin, Eliquis, Pradaxa, Xarelto, or clopidogrel, or similar medicines? Are you taking an NSAID, such as ibuprofen or naproxen?
- Have you had any trauma or swallowed a foreign object accidentally?
- Have you eaten black licorice, lead, Pepto-Bismol, or blueberries?
- Have you had more than one episode of blood in your stool? Is every stool this way?
- Have you lost any weight recently?
- Is there blood on the toilet paper only?
- What color is the stool?
- When did the problem develop?
- What other symptoms are present (abdominal pain, vomiting blood, bloating, excessive gas, diarrhea, or fever)?
You may need to have one or more tests to look for the cause:
- Angiography
- Bleeding scan (nuclear medicine)
- Blood studies, including a complete blood count (CBC) and differential, serum chemistries, clotting studies
- Colonoscopy
- Esophagogastroduodenoscopy or EGD
- Stool culture
- Tests for the presence of Helicobacter pylori infection
- Capsule endoscopy (a pill with a built in camera that takes a video of the small intestine)
- Double balloon enteroscopy (a scope that can reach the parts of the small intestine that are not able to be reached with EGD or colonoscopy)
Severe cases of bleeding that cause excessive blood loss and a drop in blood pressure may require surgery or hospitalization.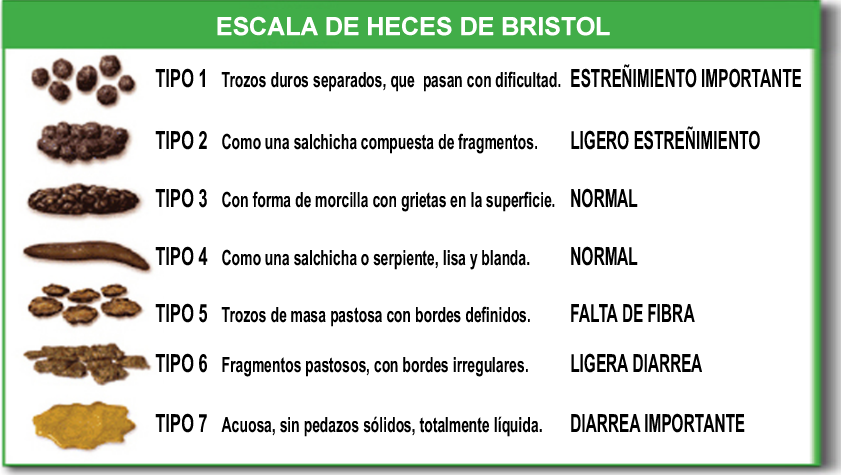
Stools – bloody; Melena; Stools – black or tarry; Upper gastrointestinal bleeding; Melenic stools
- Diverticulitis and diverticulosis – discharge
- Diverticulitis – what to ask your doctor
- Ulcerative colitis – discharge
- Abdominal organs
- Ulcer emergencies
- Mallory-Weiss tear
- Capsule endoscopy
Chaptini L, Peikin S. Gastrointestinal bleeding. In: Parrillo JE, Dellinger RP, eds. Critical Care Medicine: Principles of Diagnosis and Management in the Adult. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 72.
DeGeorge LM, Nable JV. Gastrointestinal bleeding. In: Walls RM, ed. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 26.
Kovacs TO, Jensen DM. Gastrointestinal hemorrhage. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 126.
Savides TJ, Jensen DM. Gastrointestinal bleeding. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 20.
Updated by: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Causes and when to see a doctor
Black stool can result when a person eats certain foods, such as licorice or takes iron supplements. Black, tarry stools are usually a sign of gastrointestinal bleeding, due, for instance, to a stomach ulcer.
A variety of foods and medications can make a person’s stool black. These can include:
- blueberries
- black licorice
- blood sausage
- iron tablets
- the indigestion medication bismuth subsalicylate (Pepto-Bismol)
If a person has recently consumed any of these and their stool is black, there is likely no cause for concern.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) state that bleeding in a person’s gastrointestinal tract can also cause black, tarry stools. The gastrointestinal tract is the route that food takes through a person’s body.
According to NIDDK, the gastrointestinal tract can bleed for many reasons. Some are listed below.
Authors of an article in the journal Alimentary Pharmacology & Therapeutics describe angiodysplasia as abnormal groups of vessels in the mucous membrane of a person’s gastrointestinal tract.
It is not clear why angiodysplasia happens, but it can cause bleeding and blood in a person’s stool, which can make it black and tarry.
A common treatment is argon plasma coagulation, which doctors use to seal the bleeding vessels.
According to NIDDK, benign tumors or cancerous formations in the esophagus, stomach, colon, or rectum can cause blood in a person’s stool, which may make it black and tarry.
A benign tumor is a tumor that is not cancerous. Whether they are benign or cancerous, tumors can weaken the gastrointestinal wall and result in bleeding.
Whether they are benign or cancerous, tumors can weaken the gastrointestinal wall and result in bleeding.
Genetics Home Reference define ulcerative colitis as a gastrointestinal disorder that causes ulcers to form within the large intestine. This can result in blood in a person’s stool, which may make the stool appear black and tarry.
NIDDK note that the cause of ulcerative colitis is unclear. Doctors can treat the condition with medications and surgery.
Colon polyps can cause blood in the stool, giving it a black, tarry appearance.
These polyps are small growths that form in the large intestine. They are not necessarily cancerous, but they can become cancerous over time.
A doctor may suggest surgery to remove the colon polyps.
Share on PinterestSmoking can increase the risk of esophageal issues.
If a person has problems with their esophagus, this may cause bleeding, which can turn a person’s stool black and tarry.
NIDDK report that these problems can include esophageal varices and gastroesophageal reflux.
Liver issues can cause esophageal varices, which are enlarged veins in the esophagus. Treatment will focus on stopping the bleeding and resolving the underlying condition that is causing the esophageal varices.
If a person experiences gastroesophageal reflux frequently, they may have gastroesophageal reflux disease (GERD).
The key causes are complications from certain medications, smoking, or increased pressure in the abdomen. This pressure can result, for example, from being overweight or pregnant.
A person can often manage GERD by avoiding certain foods and not overeating. A doctor may also prescribe medications.
If an ulcer forms in a person’s stomach, this can cause bleeding which may make the stool black and tarry.
NIDDK note that the long-term use of some drugs, such as ibuprofen and aspirin, can cause stomach ulcers. A bacterial infection can also be a cause.
As well as blood in a person’s stool, symptoms include:
- dull, burning pain in the stomach
- bloating
- burping
- vomiting
- having a low appetite
- losing weight
If a doctor thinks that drugs such as ibuprofen or aspirin are causing stomach ulcers, treatment usually involves no longer using these pain relievers.
Or, the doctor may prescribe medications to help fight a bacterial infection.
If a person’s stool is black because of what they have eaten, the color will eventually change with the diet. However, there is no reason for people to avoid foods that have this effect if they are not experiencing any other symptoms.
If bleeding in the gastrointestinal tract is responsible for black, tarry stools, a doctor will need to diagnose the exact cause of this. Many gastrointestinal issues are treatable.
Share on PinterestA doctor can offer advice on lifestyle changes to prevent black stool.
A doctor will have to determine the underlying cause of bleeding in the gastrointestinal tract in order to treat it, if this is the reason that a person’s stool appears black and tarry.
They may recommend that the person avoids certain foods. Also, the doctor may advise against taking specific medications and propose alternatives.
Some causes of bleeding require minor surgery to correct.
The doctor will be able to advise on the best way to prevent further bleeding in the gastrointestinal tract, based on the diagnosis, as well as any lifestyle changes that they think the person should adopt.
If a person’s stool is black, the likeliest reasons are that they have eaten certain foods or that there is bleeding in their gastrointestinal tract.
For a person who has no other symptoms and who suspects that foods are to blame, there should be no cause for concern.
However, if a person notices blood in their stool or experiences any other symptoms, they should speak to a doctor, who can determine the cause.
What is the name of the moment when dog poop turns white?
Contents
Doctor: OK, what exactly does that mean? Rose: Literally, this is exactly the moment when Doo becomes white. But in general, this refers to the type of people with whom you do not want to share your puzzles.
Why does dog feces sometimes turn white?
One of the most common causes of white feces is a diet high in calcium, which causes discoloration of the feces. Dogs that consume a lot of bones often have white foods. In most cases, white feces caused by too much calcium is not too dangerous for dogs, but too much calcium can cause constipation.
Dogs that consume a lot of bones often have white foods. In most cases, white feces caused by too much calcium is not too dangerous for dogs, but too much calcium can cause constipation.
Why did dog poop turn white in the 80s?
This constitution meant that the dogs were taking in too much calcium, which came out undigested at the other end. White calcium still left in the feces will be found when the water and organic matter is gone, which is why dog feces were white in the 70s, 80s and 90s.
Why does dog poop turn white when it dries?
If the dog’s diet contains too much calcium or bone, fresh stools are often white and calcareous in texture.
Why was dog litter white in the 70s?
The faeces of white dogs disappeared very quickly in the 70’s. The reason was a commercial dog food rich in beef and bone meal with a high calcium content. When calcium requirements changed, the color, texture, and smell of dog feces changed forever. This does not mean that we will never see white dog poop.
Why is my dog’s poop white-brown?
Diets high in calcium
Diet is the most common cause of white stools in dogs, especially diets high in calcium. This is common in puppies that are fed raw food, as they consume whole animal parts, including calcium-rich bones. Diets high in calcium can also lead to constipation.
Why do my dogs have white and yellow poop?
Orange, yellow or pale color is usually a liver problem. This could be a sign of a liver or biliary tract disease, or simply mean that your dog’s feces are moving too quickly through the gastrointestinal tract to collect bile, which changes color to the usual brown you see.
Why do dogs lick their owners?
If your dog likes to lick you, it is for several reasons: he is very affectionate, seeks your attention, or acts on his wild instinct. A dog licking its owner is so common that dog owners commonly refer to it as “kissing” and consider it a sign of affection.
A dog licking its owner is so common that dog owners commonly refer to it as “kissing” and consider it a sign of affection.
Why is my dog poop white and chalky?
Dogs producing chalky white feces are usually fed a diet high in calcium or too many bones. This type of feces is most common in dogs fed a raw food diet.
What does white poop mean?
White stools are not normal and should be checked by a doctor immediately. White or clay-like stools are caused by a lack of bile, which may indicate a serious problem. Bile is a digestive fluid produced by the liver and stored in the gallbladder.
Why do dogs paw at me?
Conclusion: pawing means your dog wants your attention. If your dog lays a paw on you when you’re together, it’s most likely an expression of affection or the gesture equivalent of “pet me more!”
Why is my dog’s feces GRAY?
Gray feces is a sign that your dog’s digestive system is struggling to break down fats. This can happen either as a result of eating too many fatty foods or as a result of a more serious and complex pancreatic problem.
This can happen either as a result of eating too many fatty foods or as a result of a more serious and complex pancreatic problem.
How to remove white dog poop?
White, chalky poop often indicates that you are feeding your dog a high calcium diet. This is easy to do if you feed him raw food or give him too many bones in his food.
Can dogs eat bananas?
Yes, dogs can eat bananas. In moderation, bananas are an excellent low-calorie treat for dogs. They are rich in potassium, vitamins, biotin, fiber and copper. They are low in cholesterol and sodium, but due to their high sugar content, bananas should be given as a treat and not in your dog’s main diet.
Why do dogs poop white foam?
Mucus in your dog’s stool is not always a concern. Mucus can appear naturally on dog poop due to intestinal lubrication. But if you see it on a regular basis or if a large amount is present, it could be a sign of a problem. Parasites, stress, or nutritional problems are common causes of slimy stools.
But if you see it on a regular basis or if a large amount is present, it could be a sign of a problem. Parasites, stress, or nutritional problems are common causes of slimy stools.
Can dogs eat cheese?
While cheese may be safe for your dog, there are some things to keep in mind. Cheese is high in fat, and regularly feeding your dog too much fat can cause weight gain and lead to obesity. Even more problematic, it can lead to pancreatitis, a serious and potentially fatal disease in dogs.
Why does my dog eat grass?
Dogs need roughage in their diet and grass is a good source of fiber. Lack of roughage affects a dog’s ability to digest food and pass stool, so grass can actually help their bodily functions run more smoothly.
Are dogs jealous?
But do dogs also show some of the negative side effects of deep love, such as jealousy? A study published in the journal Psychological Science says yes. Researchers have found that dogs will show jealousy even if they can only imagine their owners interacting with a potential rival.
Researchers have found that dogs will show jealousy even if they can only imagine their owners interacting with a potential rival.
Do dogs cry?
If by crying we mean whimpering, howling, meowing or whining, then yes, dogs certainly do.
Does the dog know their names?
Dogs also learn their names with the classic training. This means that they are learning to respond to their name when it is spoken, not that they actually know their name is Fido.
How do dogs get Giardia?
Your dog or cat can become infected: by contact with contaminated feces from another dog or cat. Skating and playing in polluted soil. Licking one’s body after contact with a contaminated surface (such as a dirty litter box, dog crate, or crate)
What is Covid feces?
New research shows that infected people start shedding coronavirus in their feces early in the course of infection and possibly days before they start shedding it from their mouth and nose. “That means we can catch them before they start spreading the infection,” she said.
“That means we can catch them before they start spreading the infection,” she said.
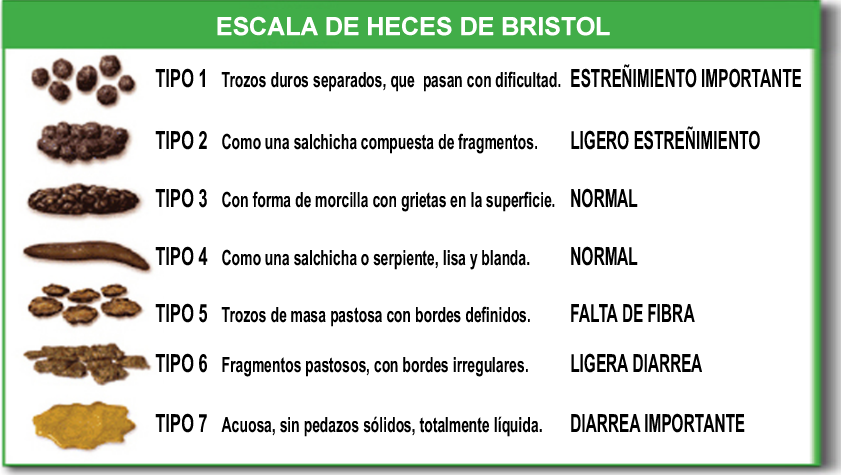
What are the 7 types of feces?
It is broken down into seven categories based on a study of 2,000 people published in another 1992, and makes poop knowledge basic and easy to understand.
- Type 1: Marble.
- Type 2: Caterpillar.
- Type 3: Hot dog.
- Type 4: Snake.
- Type 5: amoeba.
- Type 6: Soft feed.
- Type 7: Jackson Pollock.
Which animal has white poop?
Cormorants. Like most birds in our area, two-crested cormorants excrete white feces, mostly liquid. It can often be found in large numbers in and under trees where they nest, according to the National Audubon Society. Cormorants leave more streaks, like white paint.
Why do dogs put their heads between your legs?
It looks like you’ve given him a great house, and it fits him perfectly, even if “fit in” sometimes means the space between a man’s legs. The behavior you describe is not unusual and may be due to agitation or anxiety. A frightened dog may try to “hide” in a safe place.
The behavior you describe is not unusual and may be due to agitation or anxiety. A frightened dog may try to “hide” in a safe place.
How do I tell my dog that I love him?
10 ways to show love to your dog
- Ear rubbing. Your dog will naturally feel euphoric when you rub his ears.
- Have daily games.
- Teach them new tricks.
- Have warm and sincere conversations.
- Find time to cuddle.
- Surprise your dog with a treat.
- Party together.
- Treat your puppy with respect.
Why do dogs stare at you?
Just as people look into the eyes of someone they adore, dogs will look at their owners to show affection. In fact, eye contact between humans and dogs releases oxytocin, known as the love hormone. This chemical plays an important role in bonding and enhances feelings of love and trust.
Why are my dogs poop pink?
If your dog’s food looks bloody, it could be a sign of gastrointestinal bleeding or injury. Call your veterinarian to examine your dog. Pink or purple feces: Hemorrhagic gastroenteritis (HGE) kills many dogs every year, and one of its characteristic symptoms is pink or purple colored dog feces.
Call your veterinarian to examine your dog. Pink or purple feces: Hemorrhagic gastroenteritis (HGE) kills many dogs every year, and one of its characteristic symptoms is pink or purple colored dog feces.
What do the colors of dog poop mean?
Brown: A healthy puppy should have a chocolate brown stool. Green: Green stools may indicate that your dog is eating grass, possibly to soothe an upset stomach. Black or burgundy: This could be a sign of bleeding in the stomach or small intestine.
What color is parvo poop?
The exact type of poop depends on the individual dog and the severity of parvovirus in your dog. In the early stages, your puppy may not have blood in the stool, but only yellowish-brown stools. As parvovirus progresses, your puppy’s stools may be dark red or bright red.
Which dog food is rich in calcium?
Chicken and fish
Chicken is an excellent source of protein, which contains a sufficient amount of calcium. Salmon, trout, mackerel, and sardines are also high in calcium, ranging from 170 to 370 mg. Since both proteins contain enough calcium, this meat is often included in many types of dog food.
Since both proteins contain enough calcium, this meat is often included in many types of dog food.
Can dogs drink milk?
Milk is a safe treat in small quantities. A few tablespoons of cow’s or goat’s milk on a regular basis can be a good reward for your dog without the side effects of over-indulgence.
Is peanut butter good for dogs?
Most peanut butter is safe for dogs, and in moderation, peanut butter can be an excellent source of protein and healthy fats, vitamins B and E, and niacin.
Which fruit is poisonous to dogs?
Fruit. Stay away: Cherries are toxic to cats and dogs, while grapes and raisins can cause kidney damage. Citrus fruits such as lemons, limes, and grapefruits, as well as persimmons, can cause indigestion. All of the following fruits are safe for your dog or cat.
Can dogs eat pork?
Pork can be eaten, but there are certain conditions that must be met if you plan to feed your dog “other white meat”.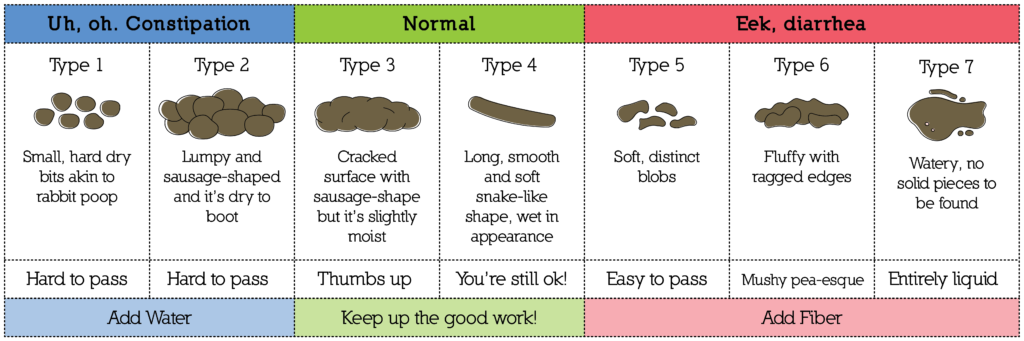 Regular pork is safe for dogs as long as you keep it simple and don’t resort to the additions people usually cook with.
Regular pork is safe for dogs as long as you keep it simple and don’t resort to the additions people usually cook with.
Is bread bad for dogs?
Is it safe for dogs to eat bread? The short answer to the question “can dogs eat bread?” Yes. Dogs can safely eat bread just like humans, but in moderation. Plain white and wheat bread is generally safe for dogs, provided they don’t have allergies, and it doesn’t usually cause stomach upset.
Can dogs eat watermelon?
The answer is yes, but with some precautions. First, the seeds can cause intestinal blockage, so be sure to remove them. It’s also a good idea to remove the peel because it can cause gastrointestinal upset.
Why do dogs bow their heads?
The dog tilts its head to show that it is busy in much the same way that a person nods during a conversation to show that he is listening. Social dogs that enjoy human interaction tend to tilt their heads more frequently to encourage further conversation and prolong human contact.
Why do dogs lick their paws?
When you think of grooming pets, dogs may not be the first animals that come to mind. However, dogs regularly lick their feet, paws, and tail to remove debris. This is a normal, healthy behavior and a sign that your furry friend wants to be clean (even if his bath time antics suggest otherwise!).
Are eggs harmful to dogs?
Eggs are completely safe for dogs, eggs are a great source of nutrition for your canine companion. They are rich in protein, fatty acids, vitamins, and fatty acids that help support your dog both inside and out. Remember that eggs are only as good as the chicken they are made from.
How do dogs laugh?
There is much debate among behaviorists about this, but most agree that dogs cannot laugh. At least not in the sense that people can laugh. However, dogs can make a sound similar to the laughter they usually make when they play. This is caused by the strong breath you exhale.
Do dogs like it when we kiss them?
Most dogs are quite good at being kissed by their owners. Some may even associate kissing with love and attention, and some even enjoy being kissed by their loved ones. They usually show their pleasure by wagging their tail, looking cheerful and happy, and licking you back.
Some may even associate kissing with love and attention, and some even enjoy being kissed by their loved ones. They usually show their pleasure by wagging their tail, looking cheerful and happy, and licking you back.
Why do dogs sleep at the end of the bed?
Because of your leadership role, your dog knows that you will have the best place for comfort there is. However, they love you and still want to be around you, so they will linger in your comfort zone. This is why your dog may sleep at the end of your bed at your feet instead of right next to you.
Do dogs smile?
Most experts agree that dogs smile in response to human smiles. Dogs smile more when they are relaxing, playing, feeling content, or greeting someone they know. Dogs don’t smile back at a joke, but they can smile back at you. Usually, when a dog smiles, it is called a submissive smile.
Can dogs eat ice cubes?
If your dog chews on ice cubes, he may break a tooth. However, in general, ice cubes pose very little threat to your dog. Ice cubes can be a refreshing snack, especially when paired with flavorful ingredients. Plus, ice cubes are a safe way to slowly rehydrate your dog without the risk of bloating.
Ice cubes can be a refreshing snack, especially when paired with flavorful ingredients. Plus, ice cubes are a safe way to slowly rehydrate your dog without the risk of bloating.
Do dogs fart?
While your dog’s occasional gas is normal and inevitable, excessive gas is not. There are several causes of farting in dogs, from gastrointestinal issues to food intolerances, so you need to visit your veterinarian to determine what is causing your dog’s stinky gas.
Do dogs know when you cry?
And according to new research, your pet dog may be happy to help. Previous research has shown that when people cry, their dogs get stressed too. A new study has found that not only do dogs get upset when they see their owners sad, but they also try to do something to help.
Do dogs know about their death?
Because dogs approaching death are often aware and ready, they may begin to behave differently in their final moments. However, before you read too much about these signs, know that many of them can be due to other, much more minor causes.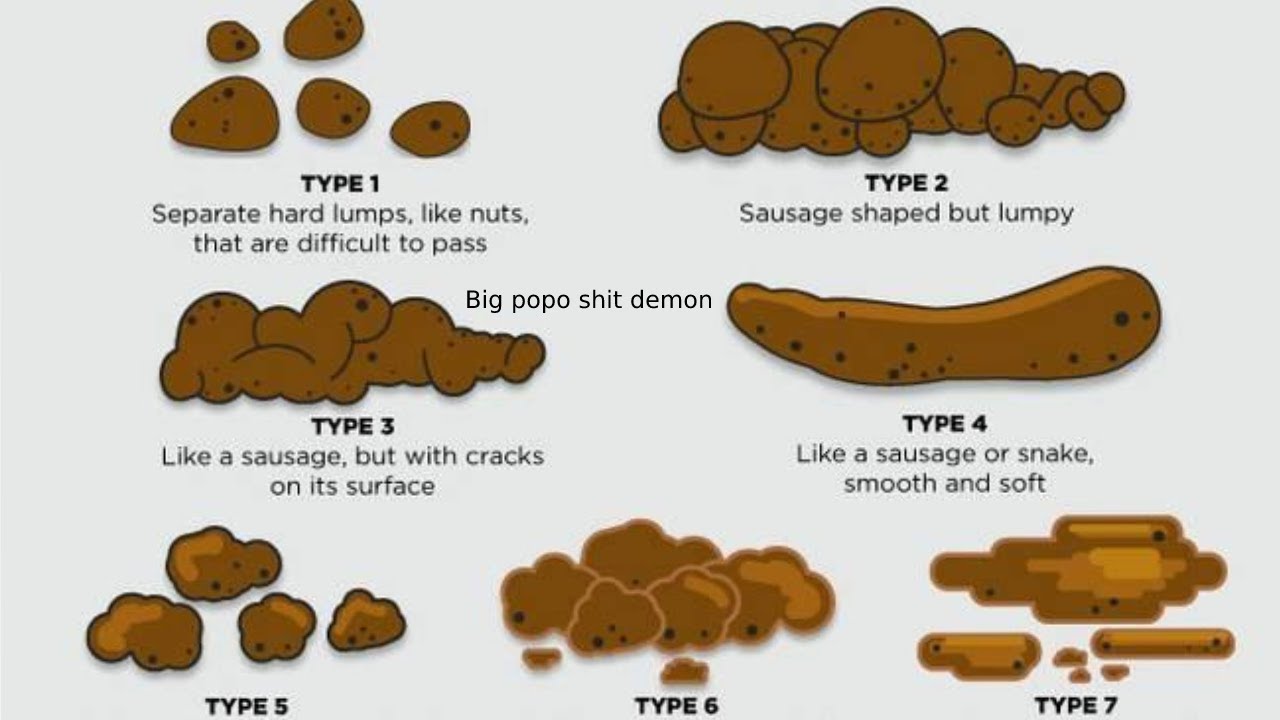
Do dogs recognize themselves in the mirror?
Although dogs cannot identify themselves in a mirror, they still have some level of self-awareness and other tests of self-knowledge. They can recognize their scent and remember certain events, according to Earth.com.
Can a dog get rid of Giardia on its own?
Although giardia outbreaks can come and go on their own, the parasite itself must be treated with medication. Metronidazole is the most common drug for the treatment of Giardia. This is an antibiotic that acts on the parasite and helps the dog’s body recover faster.
What naturally kills giardia in dogs?
There is no evidence that natural methods are effective in treating giardia. Metronidazole is a prescription drug that your veterinarian can prescribe and should work quickly and effectively. It is important to defeat the infection as soon as possible.
Will Giardia go away on its own?
Treatment for giardiasis
If symptoms are mild, treatment for giardiasis is usually not needed.
