Can antibiotic be taken with milk. Antibiotics and Milk: Essential Guidelines for Safe and Effective Use
Can antibiotics be taken with milk. How do antibiotics work against bacterial infections. Why is antibiotic resistance a growing concern. What are the best practices for taking antibiotics. How can we prevent the spread of antibiotic-resistant bacteria.
The Crucial Role of Antibiotics in Modern Medicine
Antibiotics have revolutionized the field of medicine, offering a powerful weapon against life-threatening bacterial infections. These medications have saved countless lives since their discovery, particularly in treating conditions like pneumonia that were once considered untreatable. However, the effectiveness of antibiotics is now under threat due to their misuse and overuse, leading to a growing concern: antibiotic resistance.
How do antibiotics work?
Antibiotics target and eliminate harmful bacteria in the body. They can either kill bacteria directly or inhibit their growth and reproduction, allowing the body’s immune system to overcome the infection. This mechanism makes antibiotics effective against a wide range of bacterial diseases, from minor skin infections to severe systemic illnesses.

The Double-Edged Sword: Benefits and Risks of Antibiotic Use
While antibiotics offer numerous benefits, they also come with potential risks and side effects. Understanding these aspects is crucial for responsible antibiotic use.
Benefits of antibiotics
- Cure life-threatening bacterial infections
- Relieve symptoms of bacterial infections
- Accelerate recovery time
- Prevent the spread of infectious diseases
Potential risks and side effects
- Nausea and diarrhea
- Allergic reactions
- Disruption of gut microbiome
- Development of antibiotic resistance
Are antibiotics effective against all types of infections? No, antibiotics are only effective against bacterial infections. They do not work against viral infections such as the common cold, flu, or most cases of bronchitis. Using antibiotics for viral infections not only fails to treat the illness but also contributes to antibiotic resistance.
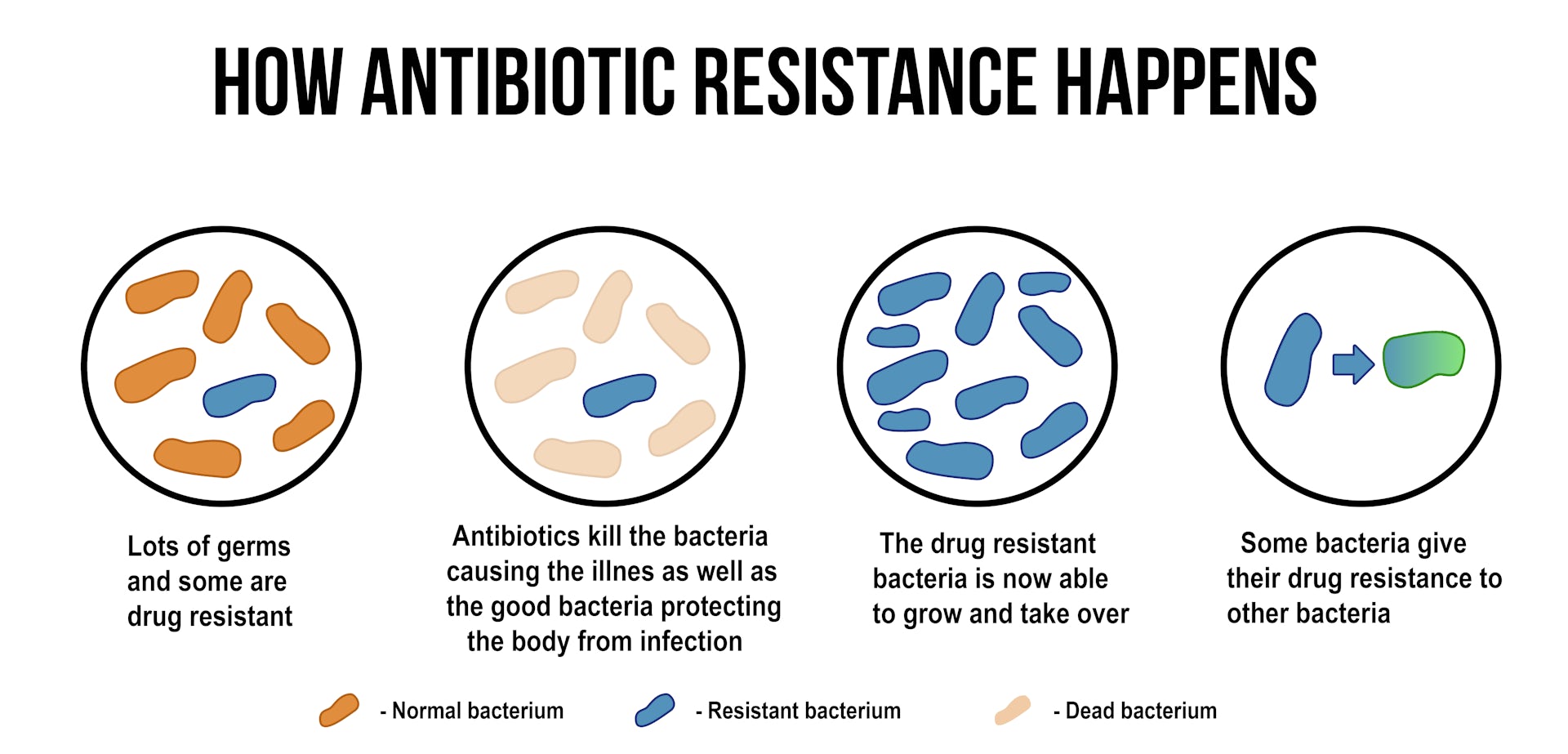
The Growing Threat of Antibiotic Resistance
Antibiotic resistance occurs when bacteria evolve to withstand the effects of antibiotics, rendering these medications ineffective. This phenomenon poses a significant threat to global public health, as it can lead to longer hospital stays, higher medical costs, and increased mortality.

What causes antibiotic resistance?
Several factors contribute to the development of antibiotic resistance:
- Overuse of antibiotics in healthcare and agriculture
- Improper use of antibiotics (e.g., not completing the full course)
- Natural genetic mutations in bacteria
- Transfer of resistance genes between different bacterial species
Which bacteria are commonly resistant to antibiotics? Some of the most concerning antibiotic-resistant bacteria include:
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Vancomycin-resistant Enterococci (VRE)
- Multidrug-resistant Escherichia coli (E. coli)
- Carbapenem-resistant Enterobacteriaceae (CRE)
Best Practices for Taking Antibiotics
To maximize the effectiveness of antibiotics and minimize the risk of resistance, it’s essential to follow these best practices:
- Only take antibiotics prescribed by a healthcare professional
- Complete the full course of antibiotics, even if you feel better
- Never share antibiotics with others or use leftover antibiotics
- Take antibiotics exactly as directed, regarding dosage and timing
- Inform your healthcare provider of any side effects or allergic reactions
Can antibiotics be taken with milk?
The interaction between antibiotics and milk is a common concern. Some antibiotics, such as tetracyclines and ciprofloxacin, can bind to calcium in milk, reducing their absorption and effectiveness. However, other antibiotics are not affected by milk. Always consult your healthcare provider or pharmacist for specific instructions on taking your prescribed antibiotic with or without milk or other dairy products.

Combating Antibiotic Resistance: A Global Effort
Addressing the challenge of antibiotic resistance requires a coordinated effort from healthcare providers, patients, and policymakers. Several initiatives are underway to combat this growing threat:
- Stricter regulations on antibiotic prescriptions
- Improved hygiene measures in healthcare settings
- Development of new antibiotics and alternative treatments
- Public education campaigns on responsible antibiotic use
- Reduction of antibiotic use in agriculture
How can individuals contribute to preventing antibiotic resistance?
Everyone has a role to play in preserving the effectiveness of antibiotics:
- Practice good hygiene to prevent the spread of infections
- Get vaccinated to reduce the need for antibiotics
- Only use antibiotics when prescribed by a healthcare professional
- Never pressure healthcare providers to prescribe antibiotics for viral infections
- Properly dispose of unused antibiotics
The Future of Antibiotic Treatment: Innovations and Challenges
As antibiotic resistance continues to evolve, researchers and healthcare professionals are exploring new approaches to combat bacterial infections:

Emerging technologies in antibiotic development
- CRISPR-Cas9 gene editing to target resistant bacteria
- Artificial intelligence for drug discovery
- Bacteriophage therapy as an alternative to antibiotics
- Nanoparticle-based antibiotic delivery systems
Will these innovations solve the antibiotic resistance crisis? While these technologies show promise, addressing antibiotic resistance will likely require a multifaceted approach combining new treatments, improved stewardship, and global cooperation.
Antibiotic Stewardship in Healthcare Settings
Healthcare facilities play a crucial role in promoting responsible antibiotic use and preventing the spread of resistant bacteria. Antibiotic stewardship programs are being implemented in hospitals and clinics worldwide to optimize antibiotic prescribing and improve patient outcomes.
Key components of antibiotic stewardship programs
- Regular antibiotic prescription audits
- Education for healthcare providers on appropriate antibiotic use
- Implementation of rapid diagnostic tests to guide antibiotic prescribing
- Development of facility-specific antibiotic guidelines
- Monitoring and reporting of antibiotic resistance patterns
How effective are antibiotic stewardship programs? Studies have shown that well-implemented stewardship programs can significantly reduce inappropriate antibiotic use, decrease healthcare costs, and improve patient outcomes.

The Global Impact of Antibiotic Resistance
Antibiotic resistance is not confined to any single country or region; it is a global health crisis that affects people worldwide. The World Health Organization (WHO) has declared antibiotic resistance one of the top 10 global public health threats facing humanity.
Economic and social consequences of antibiotic resistance
- Increased healthcare costs due to longer hospital stays and more expensive treatments
- Loss of productivity due to prolonged illnesses
- Setbacks in medical procedures that rely on effective antibiotics
- Potential food security issues due to antibiotic resistance in livestock
How can international cooperation address antibiotic resistance? Global initiatives, such as the WHO’s Global Action Plan on Antimicrobial Resistance, aim to promote collaboration between countries to implement policies, share research, and develop new strategies to combat antibiotic resistance.
Educating the Public on Antibiotic Use
Public awareness and education are crucial in the fight against antibiotic resistance. Many people still lack understanding about the appropriate use of antibiotics and the risks of misuse.

Key messages for public education campaigns
- Antibiotics are not effective against viral infections
- Never use antibiotics without a prescription
- Complete the full course of prescribed antibiotics
- Proper hand hygiene can prevent many infections
- Vaccinations can reduce the need for antibiotics
How can healthcare providers effectively communicate about antibiotic use? Clear, patient-friendly explanations, visual aids, and follow-up discussions can help patients better understand the importance of responsible antibiotic use.
The Role of Diet and Nutrition in Supporting Antibiotic Treatment
While antibiotics are essential for fighting bacterial infections, a healthy diet can support the body’s immune system and potentially enhance the effectiveness of antibiotic treatment.
Nutritional strategies during antibiotic treatment
- Consuming probiotic-rich foods to support gut health
- Staying hydrated to help flush out toxins
- Eating a balanced diet rich in fruits and vegetables
- Avoiding alcohol, which can interact with some antibiotics
Can certain foods enhance the effectiveness of antibiotics? While no food can replace or enhance antibiotics directly, a nutrient-rich diet can support overall health and potentially help the body recover faster from infections.

Antibiotic Alternatives: Exploring Natural Remedies
As concerns about antibiotic resistance grow, there is increasing interest in natural alternatives for treating minor infections and boosting the immune system. While these should never replace prescribed antibiotics for serious infections, they may offer complementary support or help prevent minor infections from worsening.
Potential natural immune boosters
- Garlic: Contains allicin, a compound with antimicrobial properties
- Honey: Particularly Manuka honey, known for its antibacterial effects
- Echinacea: May help stimulate the immune system
- Oregano oil: Contains carvacrol, which has shown antimicrobial activity
- Probiotics: Support gut health and may help prevent certain infections
Are natural remedies as effective as antibiotics? Natural remedies should not be considered equivalent to antibiotics for treating serious bacterial infections. Always consult a healthcare professional before using any alternative treatments, especially if you have a severe or persistent infection.

The Intersection of Antibiotic Use and Environmental Health
The widespread use of antibiotics not only affects human health but also has significant environmental implications. Antibiotics can enter the environment through various routes, including human and animal waste, pharmaceutical manufacturing runoff, and improper disposal of unused medications.
Environmental impacts of antibiotic contamination
- Disruption of natural microbial communities in soil and water
- Development of antibiotic-resistant bacteria in the environment
- Potential effects on aquatic life and ecosystems
- Contamination of water sources used for drinking and irrigation
How can we reduce the environmental impact of antibiotics? Proper disposal of unused medications, improved wastewater treatment technologies, and reduced use of antibiotics in agriculture are some strategies to mitigate environmental contamination.
The Promise of Personalized Medicine in Antibiotic Treatment
Advances in genomics and personalized medicine offer new possibilities for tailoring antibiotic treatments to individual patients. This approach could potentially improve treatment efficacy and reduce the risk of antibiotic resistance.

Applications of personalized medicine in antibiotic therapy
- Genetic testing to predict antibiotic response and side effects
- Rapid diagnostic tests to identify specific bacterial strains
- Customized antibiotic dosing based on individual patient factors
- Development of targeted, narrow-spectrum antibiotics
Will personalized medicine revolutionize antibiotic treatment? While personalized approaches show promise, their widespread implementation faces challenges such as cost, accessibility, and the need for further research to validate their effectiveness in diverse populations.
Antibiotics in Veterinary Medicine: Balancing Animal Health and Public Safety
The use of antibiotics in veterinary medicine and animal agriculture is a significant contributor to the development of antibiotic resistance. Striking a balance between maintaining animal health and preventing the spread of resistant bacteria to humans is a complex challenge.
Strategies for responsible antibiotic use in animals
- Implementing antibiotic stewardship programs in veterinary practices
- Promoting alternatives to antibiotics for growth promotion in livestock
- Improving animal husbandry practices to reduce the need for antibiotics
- Enhancing surveillance of antibiotic use and resistance in animal populations
How does antibiotic use in animals affect human health? Antibiotic-resistant bacteria can be transmitted from animals to humans through food products, direct contact, or environmental contamination. Responsible antibiotic use in veterinary medicine is crucial for preserving the effectiveness of these drugs for both animal and human health.

The Role of Policy and Regulation in Combating Antibiotic Resistance
Effective policies and regulations are essential for addressing the complex issue of antibiotic resistance. Governments and international organizations play a crucial role in implementing and enforcing measures to promote responsible antibiotic use and development.
Key policy areas for addressing antibiotic resistance
- Regulation of antibiotic prescribing and dispensing
- Incentives for the development of new antibiotics and alternatives
- Surveillance and reporting systems for antibiotic use and resistance
- International cooperation and data sharing
- Public awareness and education campaigns
Can policy interventions effectively combat antibiotic resistance? While policies alone cannot solve the problem, well-designed and consistently enforced regulations can significantly contribute to slowing the development and spread of antibiotic resistance.
The Future of Infection Control: Beyond Antibiotics
As the challenges of antibiotic resistance grow, researchers are exploring innovative approaches to infection control that go beyond traditional antibiotics. These emerging technologies and strategies could reshape our approach to treating and preventing bacterial infections.
Promising alternatives to traditional antibiotics
- Antimicrobial peptides: Natural or synthetic molecules that target bacteria
- Phage therapy: Using viruses that infect bacteria to treat infections
- Immune system modulators: Enhancing the body’s natural defenses
- Anti-virulence strategies: Disarming bacteria without killing them
- Microbiome manipulation: Using beneficial bacteria to fight pathogens
Will these alternatives completely replace antibiotics? While these approaches show promise, it’s likely that they will complement rather than entirely replace traditional antibiotics. A diverse toolkit of treatment options will be crucial for addressing the complex challenge of bacterial infections in the future.
Using medication: Using antibiotics correctly and avoiding resistance – InformedHealth.org
Created: November 14, 2008; Last Update: December 18, 2013; Next update: 2020.
The development of antibiotics was one of the great discoveries in modern medicine. They fight bacteria and can cure life-threatening infectious diseases such as pneumonia, for which there was previously no effective treatment. But the improper use of antibiotics means that more and more bacteria are becoming resistant to this kind of medication. So it is especially important to use them correctly.
Antibiotics can save lives, but they also relieve symptoms of bacterial infections and help us recover faster. But treatment with antibiotics also has side effects. Nausea or diarrhea are common, for example.
Antibiotics are also used far too often, and improper use is widespread. This has caused many different types of bacteria to become resistant (unresponsive) to antibiotics. Because resistance has become more common, many diseases cannot be treated as well as they could in the past.
When using antibiotics, it’s important to know the following things to prevent resistance and side effects:
Antibiotics only work against bacteria. Many infections are caused by viruses and can’t be treated using antibiotics – examples include respiratory illnesses such as a cough, stuffy nose, bronchitis or the flu.
Excessive and improper use of antibiotics causes side effects, and in the long term reduces their effectiveness.
What is antibiotic resistance?
In medicine, bacteria and other germs are said to be resistant if they are especially able to withstand exposure to external influences. For example, most germs that enter the stomach with food will be killed by stomach (gastric) acid. But some bacteria are covered with a mucous coating that protects them from the acid. They are resistant to gastric acid.
Resistance to antibiotics works on a similar principle: The bacteria have acquired a new property that protects them from the antibiotic. Some types of bacteria can produce a substance that makes certain antibiotics ineffective, for example. Bacteria that can protect themselves from several different antibiotics are referred to as “multiresistant.”
Some types of bacteria can produce a substance that makes certain antibiotics ineffective, for example. Bacteria that can protect themselves from several different antibiotics are referred to as “multiresistant.”
What causes resistance?
Many of the bacteria that are now resistant used to be sensitive to antibiotics. There are a few developments that played a role in this. To put it briefly, one kind of antibiotic could originally neutralize a certain type of bacteria and then effectively stop the infection. But the genetic material of bacteria can change by chance, sometimes creating new properties. If they protect the bacteria from an antibiotic, then the bacteria have become resistant. These kinds of properties can also transfer from one type of bacteria to another.
If antibiotics are used very often, resistant bacteria are better able to reproduce because the other non-resistant strains of bacteria are stopped. Antibiotics then no longer help against infections caused by resistant bacteria.
Which bacteria are resistant to antibiotics and why are they dangerous?
Strains of Streptococcus and Staphylococcus bacteria are often resistant to antibiotics. One example is called “methicillin-resistant Staphylococcus aureus” (MRSA). Staphylococci can be found on skin and mucous membranes and may cause infection – for example if they get into open wounds.
Resistant strains have now developed in other types of bacteria, such as Escherichia coli, Klebsiella and pseudomonads.
What is being done about antibiotic resistance?
In Germany, antibiotics are prescription-only. This means that doctors are first and foremost responsible for careful and appropriate use. They are to first see whether someone actually has a bacterial infection. If they do, then it’s important that the antibiotic is prescribed at the right dose and for long enough, and that the right antibiotic is selected that will most effectively fight the bacteria.
There are also hygiene regulations to keep resistant bacteria from spreading further and preventable infections from occurring. These measures are especially important inside of a hospital. Antibiotics are used there relatively frequently, so resistant germs can develop quite quickly. If you come into contact with someone who has an infection of resistant bacteria, it can help to wear disposable gloves, a mask and coat, and to use a hand disinfectant to stop the spread of the germs.
These measures are especially important inside of a hospital. Antibiotics are used there relatively frequently, so resistant germs can develop quite quickly. If you come into contact with someone who has an infection of resistant bacteria, it can help to wear disposable gloves, a mask and coat, and to use a hand disinfectant to stop the spread of the germs.
Antibiotics are also used in veterinary medicine and in agriculture. Veterinarians also have to comply with the rules for handling antibiotics properly.
What can I do to prevent antibiotic resistance?
Being cautious when taking antibiotics can help prevent both antibiotic resistance and side effects.
The most important thing is to not overestimate what antibiotics can do: Patients often expect antibiotics to be prescribed to treat medical conditions for which they are not suitable.
Antibiotics are needed to treat serious bacterial infections like lung infections or meningitis (inflammation of the membranes lining the brain and spinal cord).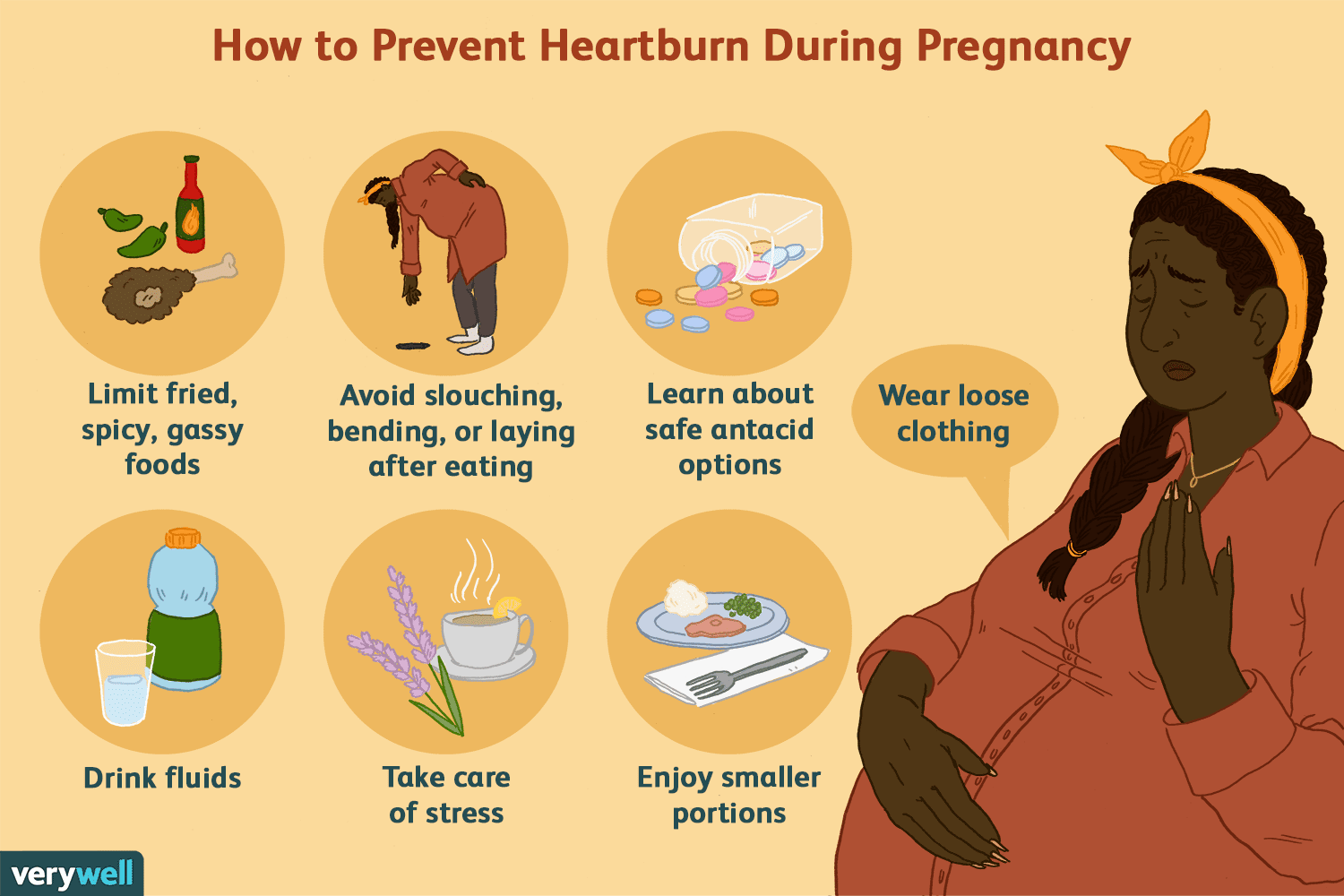 This is not the case when, for example, people who are otherwise healthy have respiratory infections caused by viruses, such as a cold or influenza (“the flu”). Antibiotics will usually be of no help because they only fight bacteria. Antibiotics also have side effects including allergic reactions, stomach and bowel problems, nausea and fungal infections. Because of these associated risks, it’s important to carefully consider the advantages and disadvantages of taking antibiotics.
This is not the case when, for example, people who are otherwise healthy have respiratory infections caused by viruses, such as a cold or influenza (“the flu”). Antibiotics will usually be of no help because they only fight bacteria. Antibiotics also have side effects including allergic reactions, stomach and bowel problems, nausea and fungal infections. Because of these associated risks, it’s important to carefully consider the advantages and disadvantages of taking antibiotics.
What’s important to consider when taking antibiotics?
Antibiotics should be taken for as long as the doctor has prescribed them. Just because the symptoms of the illness subside, it doesn’t mean that all of the germs have been killed. Remaining bacteria may cause the illness to start up again.
If there are some tablets left over, they should not be kept for later use or given to other people. Leftover medication can be disposed of in the normal garbage or dropped off at some pharmacies. Pharmacies are not obligated to accept opened medicine though.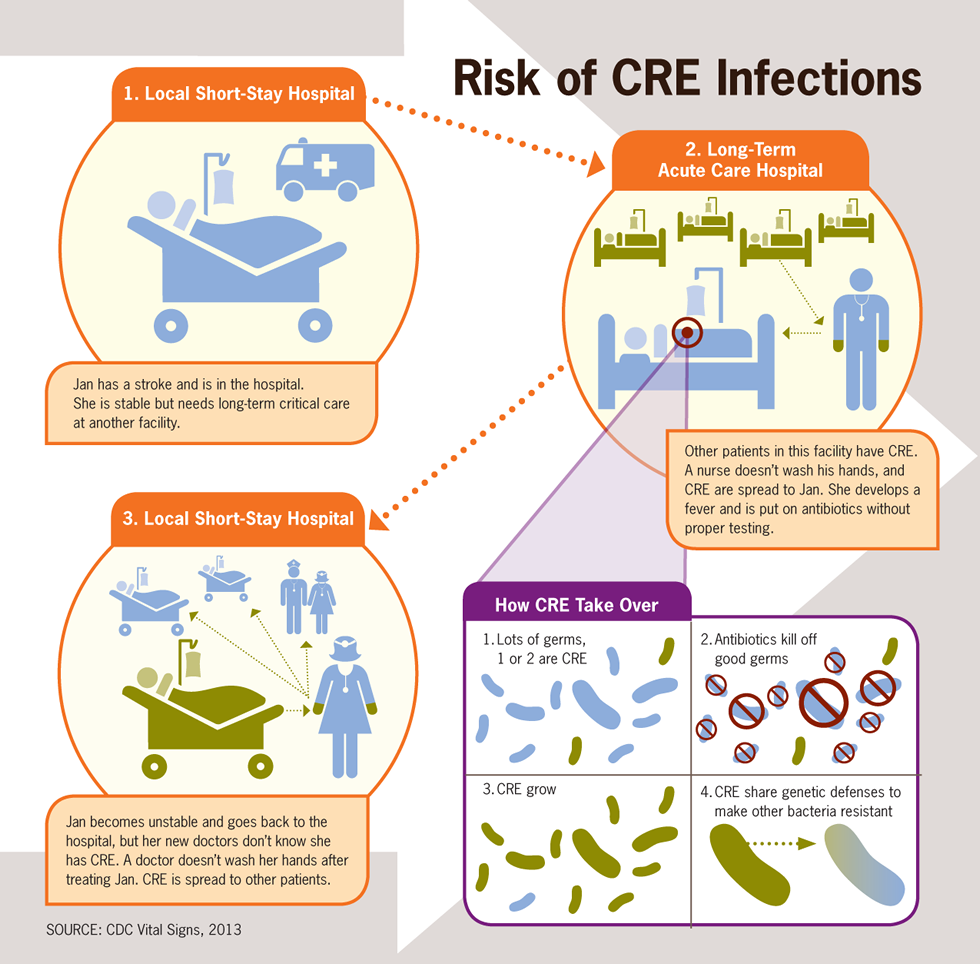 It is important not to dispose of the medication by pouring it down the drain or flushing it down the toilet. That is bad for the environment and also contributes to bacterial resistance.
It is important not to dispose of the medication by pouring it down the drain or flushing it down the toilet. That is bad for the environment and also contributes to bacterial resistance.
Medications can only work properly if they are used correctly. It’s important to know the following things when taking antibiotics:
Can the tablets be broken into smaller pieces to make them easier to swallow? Doing this can stop some medications from working properly.
What food can you take antibiotics with? Antibiotics are usually taken with water because taking them together with fruit juices, dairy products or alcohol can affect how the body absorbs some drugs. Dairy products include milk as well as butter, yogurt, and cheese. After taking an antibiotic you may need to wait for up to three hours before eating or drinking any dairy products. Grapefruit juice and dietary supplements containing minerals like calcium may also work dampen the effect of antibiotics.

When should you take antibiotics? Some antibiotics are always meant to be taken at the same time of day, others are meant to be taken before, with or after a meal. If you are supposed to take the medicine three times a day, for example, it usually needs to be taken at set times so that the effect is spread out evenly over the course of the day. You could remember the regular times of 6 a.m., 2 p.m. and 10 p.m. for an antibiotic that needs to be taken every 8 hours, for example.
Can you take antibiotics together with other medications? Because antibiotics can interact with other medications, it’s important to tell your doctor if you take other medications too. Antibiotics might interact with some blood thinners and antacids, for example. Some antibiotics can make birth control pills less effective.
You can find detailed information on the use of a specific antibiotic in the package insert. If you’re not sure about what is important to consider when taking the antibiotic, you can ask your doctor or pharmacist.
Sources
Bundesministerium für Gesundheit (BMG), Bundesministerium für Ernährung und Landwirtschaft (BMEL), Bundesministerium für Bildung und Forschung (BMBF). DART 2020. Zwischenbericht anlässlich der WHA 2016. May 2016.
Centers for Disease Control and Prevention (CDC). Antibiotic / Antimicrobial Resistance. June 12, 2017.
Deutsche Gesellschaft für Infektiologie e.V. (DGI). S3-Leitlinie: Strategien zur Sicherung rationaler Antibiotika-Anwendung im Krankenhaus. AWMF-Register-Nr.: 092-001. December 15, 2013.
Kayser FH, Böttger EC, Deplazes P, Haller O, Roers A. Taschenlehrbuch Medizinische Mikrobiologie. Stuttgart: Thieme; 2014.
Weltgesundheitsorganisation (WHO). Antimicrobial resistance. October 2016.
IQWiG health information is written with the aim of helping
people understand the advantages and disadvantages of the main treatment options and health
care services.Because IQWiG is a German institute, some of the information provided here is specific to the
German health care system. The suitability of any of the described options in an individual
The suitability of any of the described options in an individual
case can be determined by talking to a doctor. We do not offer individual consultations.Our information is based on the results of good-quality studies. It is written by a
team of
health care professionals, scientists and editors, and reviewed by external experts. You can
find a detailed description of how our health information is produced and updated in
our methods.
Using medication: Using antibiotics correctly and avoiding resistance – InformedHealth.org
Created: November 14, 2008; Last Update: December 18, 2013; Next update: 2020.
The development of antibiotics was one of the great discoveries in modern medicine. They fight bacteria and can cure life-threatening infectious diseases such as pneumonia, for which there was previously no effective treatment. But the improper use of antibiotics means that more and more bacteria are becoming resistant to this kind of medication. So it is especially important to use them correctly.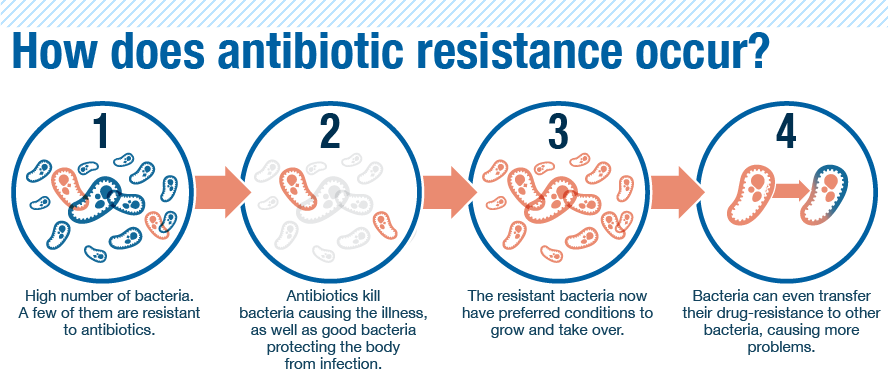
Antibiotics can save lives, but they also relieve symptoms of bacterial infections and help us recover faster. But treatment with antibiotics also has side effects. Nausea or diarrhea are common, for example.
Antibiotics are also used far too often, and improper use is widespread. This has caused many different types of bacteria to become resistant (unresponsive) to antibiotics. Because resistance has become more common, many diseases cannot be treated as well as they could in the past.
When using antibiotics, it’s important to know the following things to prevent resistance and side effects:
Antibiotics only work against bacteria. Many infections are caused by viruses and can’t be treated using antibiotics – examples include respiratory illnesses such as a cough, stuffy nose, bronchitis or the flu.
Excessive and improper use of antibiotics causes side effects, and in the long term reduces their effectiveness.
What is antibiotic resistance?
In medicine, bacteria and other germs are said to be resistant if they are especially able to withstand exposure to external influences. For example, most germs that enter the stomach with food will be killed by stomach (gastric) acid. But some bacteria are covered with a mucous coating that protects them from the acid. They are resistant to gastric acid.
For example, most germs that enter the stomach with food will be killed by stomach (gastric) acid. But some bacteria are covered with a mucous coating that protects them from the acid. They are resistant to gastric acid.
Resistance to antibiotics works on a similar principle: The bacteria have acquired a new property that protects them from the antibiotic. Some types of bacteria can produce a substance that makes certain antibiotics ineffective, for example. Bacteria that can protect themselves from several different antibiotics are referred to as “multiresistant.”
What causes resistance?
Many of the bacteria that are now resistant used to be sensitive to antibiotics. There are a few developments that played a role in this. To put it briefly, one kind of antibiotic could originally neutralize a certain type of bacteria and then effectively stop the infection. But the genetic material of bacteria can change by chance, sometimes creating new properties. If they protect the bacteria from an antibiotic, then the bacteria have become resistant. These kinds of properties can also transfer from one type of bacteria to another.
These kinds of properties can also transfer from one type of bacteria to another.
If antibiotics are used very often, resistant bacteria are better able to reproduce because the other non-resistant strains of bacteria are stopped. Antibiotics then no longer help against infections caused by resistant bacteria.
Which bacteria are resistant to antibiotics and why are they dangerous?
Strains of Streptococcus and Staphylococcus bacteria are often resistant to antibiotics. One example is called “methicillin-resistant Staphylococcus aureus” (MRSA). Staphylococci can be found on skin and mucous membranes and may cause infection – for example if they get into open wounds.
Resistant strains have now developed in other types of bacteria, such as Escherichia coli, Klebsiella and pseudomonads.
What is being done about antibiotic resistance?
In Germany, antibiotics are prescription-only. This means that doctors are first and foremost responsible for careful and appropriate use. They are to first see whether someone actually has a bacterial infection. If they do, then it’s important that the antibiotic is prescribed at the right dose and for long enough, and that the right antibiotic is selected that will most effectively fight the bacteria.
They are to first see whether someone actually has a bacterial infection. If they do, then it’s important that the antibiotic is prescribed at the right dose and for long enough, and that the right antibiotic is selected that will most effectively fight the bacteria.
There are also hygiene regulations to keep resistant bacteria from spreading further and preventable infections from occurring. These measures are especially important inside of a hospital. Antibiotics are used there relatively frequently, so resistant germs can develop quite quickly. If you come into contact with someone who has an infection of resistant bacteria, it can help to wear disposable gloves, a mask and coat, and to use a hand disinfectant to stop the spread of the germs.
Antibiotics are also used in veterinary medicine and in agriculture. Veterinarians also have to comply with the rules for handling antibiotics properly.
What can I do to prevent antibiotic resistance?
Being cautious when taking antibiotics can help prevent both antibiotic resistance and side effects.
The most important thing is to not overestimate what antibiotics can do: Patients often expect antibiotics to be prescribed to treat medical conditions for which they are not suitable.
Antibiotics are needed to treat serious bacterial infections like lung infections or meningitis (inflammation of the membranes lining the brain and spinal cord). This is not the case when, for example, people who are otherwise healthy have respiratory infections caused by viruses, such as a cold or influenza (“the flu”). Antibiotics will usually be of no help because they only fight bacteria. Antibiotics also have side effects including allergic reactions, stomach and bowel problems, nausea and fungal infections. Because of these associated risks, it’s important to carefully consider the advantages and disadvantages of taking antibiotics.
What’s important to consider when taking antibiotics?
Antibiotics should be taken for as long as the doctor has prescribed them. Just because the symptoms of the illness subside, it doesn’t mean that all of the germs have been killed. Remaining bacteria may cause the illness to start up again.
Remaining bacteria may cause the illness to start up again.
If there are some tablets left over, they should not be kept for later use or given to other people. Leftover medication can be disposed of in the normal garbage or dropped off at some pharmacies. Pharmacies are not obligated to accept opened medicine though. It is important not to dispose of the medication by pouring it down the drain or flushing it down the toilet. That is bad for the environment and also contributes to bacterial resistance.
Medications can only work properly if they are used correctly. It’s important to know the following things when taking antibiotics:
Can the tablets be broken into smaller pieces to make them easier to swallow? Doing this can stop some medications from working properly.
What food can you take antibiotics with? Antibiotics are usually taken with water because taking them together with fruit juices, dairy products or alcohol can affect how the body absorbs some drugs.
 Dairy products include milk as well as butter, yogurt, and cheese. After taking an antibiotic you may need to wait for up to three hours before eating or drinking any dairy products. Grapefruit juice and dietary supplements containing minerals like calcium may also work dampen the effect of antibiotics.
Dairy products include milk as well as butter, yogurt, and cheese. After taking an antibiotic you may need to wait for up to three hours before eating or drinking any dairy products. Grapefruit juice and dietary supplements containing minerals like calcium may also work dampen the effect of antibiotics.When should you take antibiotics? Some antibiotics are always meant to be taken at the same time of day, others are meant to be taken before, with or after a meal. If you are supposed to take the medicine three times a day, for example, it usually needs to be taken at set times so that the effect is spread out evenly over the course of the day. You could remember the regular times of 6 a.m., 2 p.m. and 10 p.m. for an antibiotic that needs to be taken every 8 hours, for example.
Can you take antibiotics together with other medications? Because antibiotics can interact with other medications, it’s important to tell your doctor if you take other medications too.
 Antibiotics might interact with some blood thinners and antacids, for example. Some antibiotics can make birth control pills less effective.
Antibiotics might interact with some blood thinners and antacids, for example. Some antibiotics can make birth control pills less effective.
You can find detailed information on the use of a specific antibiotic in the package insert. If you’re not sure about what is important to consider when taking the antibiotic, you can ask your doctor or pharmacist.
Sources
Bundesministerium für Gesundheit (BMG), Bundesministerium für Ernährung und Landwirtschaft (BMEL), Bundesministerium für Bildung und Forschung (BMBF). DART 2020. Zwischenbericht anlässlich der WHA 2016. May 2016.
Centers for Disease Control and Prevention (CDC). Antibiotic / Antimicrobial Resistance. June 12, 2017.
Deutsche Gesellschaft für Infektiologie e.V. (DGI). S3-Leitlinie: Strategien zur Sicherung rationaler Antibiotika-Anwendung im Krankenhaus. AWMF-Register-Nr.: 092-001. December 15, 2013.
Kayser FH, Böttger EC, Deplazes P, Haller O, Roers A.
 Taschenlehrbuch Medizinische Mikrobiologie. Stuttgart: Thieme; 2014.
Taschenlehrbuch Medizinische Mikrobiologie. Stuttgart: Thieme; 2014.Weltgesundheitsorganisation (WHO). Antimicrobial resistance. October 2016.
IQWiG health information is written with the aim of helping
people understand the advantages and disadvantages of the main treatment options and health
care services.Because IQWiG is a German institute, some of the information provided here is specific to the
German health care system. The suitability of any of the described options in an individual
case can be determined by talking to a doctor. We do not offer individual consultations.Our information is based on the results of good-quality studies. It is written by a
team of
health care professionals, scientists and editors, and reviewed by external experts. You can
find a detailed description of how our health information is produced and updated in
our methods.
Why can’t you drink milk with antibiotics? – Save24.me
Milk with antibiotics?
The discovery of antibiotics has led to a great medical breakthrough, but many people do not forget about the benefits of familiar foods and try to combine drug therapy with traditional methods of health promotion. In the case of antibiotics, this is strictly prohibited, as this is one of the most “harmful” methods of treatment, and simultaneous use with other drugs and certain products can be harmful to health.
In the case of antibiotics, this is strictly prohibited, as this is one of the most “harmful” methods of treatment, and simultaneous use with other drugs and certain products can be harmful to health.
The question of whether milk is allowed while taking antibiotics is relevant enough, so let’s explore it!
About dairy products, that is, about the combination of milk and drugs, experts doubt. There is no doubt that dairy products themselves are good for the human body. However, most people have a skewed idea of the usefulness that they think will increase the effect. Some believe that if they drink milk along with medicines, the effect will increase by 2 times. In this case, the doctor will say: “Milk with conventional medicines may be useful, but milk with antibiotics is no good.”
However, any dairy product can be taken 1-2 hours after taking the drug or 1:00 before taking it. Only those drugs that stimulate the gastric mucosa and do not bind to blood proteins and calcium contained in milk are washed down with milk.
Antibiotics are a very capricious drug. Once in the body, it affects everything that is in the stomach. Experts note the importance of following the instructions for using the drug, as well as the doctor’s recommendations on the correct use of antibiotics.
According to experts, antibiotics should only be taken with water. Eating should be postponed for several hours, unless this item is indicated in the instructions. Each drug has its own nuances and features and this must be borne in mind!
What if a person drank both milk and antibiotics? What results are expected?
Experts will tell you in which nuances you can use dairy products. You should always pay attention to the instructions, as well as:
1. When the time of eating coincides with the intake of medicines, that is, antibiotics, the intake of dairy products is possible. In this case, the benefits for the body will be greater, because you take the necessary substances and strengthen your health.
2. On the other hand, if the package leaflet says “do not take with food”, then it should not be taken with milk. Since food and dairy products can inhibit the effect of the drug in question. The entire treatment process is disrupted, antibiotics do not have the necessary effect on the disease. Treatment may require additional time.
3. For example, kefir may contain medicinal enzymes that should not be used in combination with other drugs. Absorption of the main drug is impaired and may affect the entire treatment.
4. Specialists do not recommend the combined use of therapeutic agents. Because the calcium contained in milk is combined with the drug, it can lead to unexpected results during treatment.
In most cases, taking a milk drink while taking antibiotics is not the best solution for the patient. This list can include not only milk, but all dairy products. Antibiotics and dairy products are best taken separately. Thus, the drug has a full effect on the problem, and dairy products help restore the intestinal flora.
Antibiotics aggressively act on bifidobacteria in the intestines, but thanks to milk drinks, you can recover.
Antibiotics and milk — Viola magazine
A meaningful search for such substances was initiated by the British microbiologist A. Flemming in 1928, and already in 1943 mass production of penicillin was launched in America. The Nobel Prize received by Flemming, Flory and Chain confirms the importance of this discovery.
Meanwhile, in 1942 in the USSR, microbiologist Zinaida Ermolyeva developed a method for obtaining domestic penicillin. For this, she was awarded the Stalin Prize, and thousands of Soviet soldiers survived thanks to her discovery.
Now penicillin is practically not used in its pure form. Stronger modern drugs have been synthesized. It became possible to control the course of infectious diseases. At first, this led to false conclusions about the victory over pathogens. But gradually, with the advent of information about the resistance of bacteria to antibiotics, the enthusiasm of the researchers was replaced by concern. And when outbreaks of intestinal infections in hot countries began to claim thousands of lives and antibiotics were powerless, scientists began to sound the alarm. The result was the development by the World Health Organization (WHO) of a global strategy to contain antimicrobial resistance.
And when outbreaks of intestinal infections in hot countries began to claim thousands of lives and antibiotics were powerless, scientists began to sound the alarm. The result was the development by the World Health Organization (WHO) of a global strategy to contain antimicrobial resistance.
Surprisingly, it is with food that we, without noticing it, take antibiotics. Or rather, we can accept if we buy and use products of unknown origin.
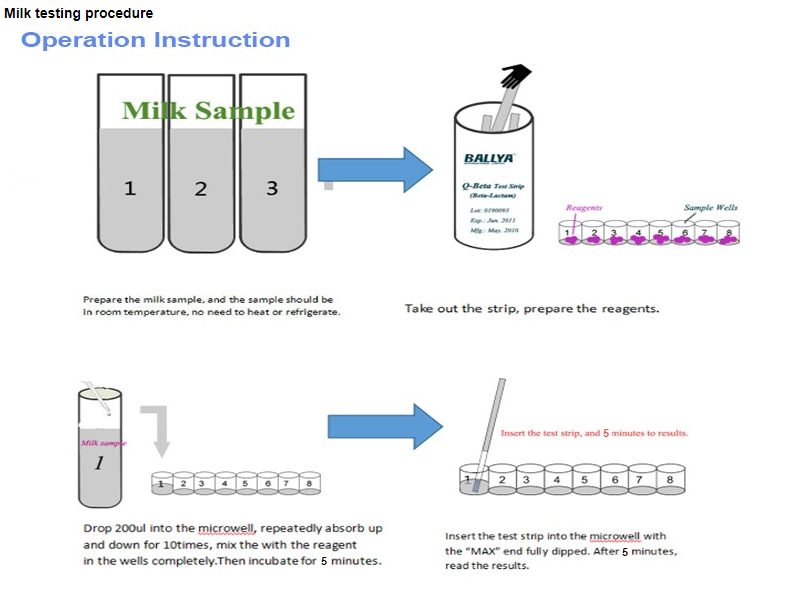
Let’s see how things are with milk. Cows that produce milk sometimes get sick. Veterinarians treat these cows successfully. At the same time, modern antibiotics are used, which are similar in composition to those that people are treated with. Some time after recovery, the animals excrete the remnants of drugs with milk. Farm employees are required to milk such animals separately, and destroy the milk from them. Finally, the waiting period expires and the milk is checked with a rapid test. Restrictions are lifted if no antibiotic residues are found. The cow begins to be milked together with the rest of the herd in one common container.
The cow begins to be milked together with the rest of the herd in one common container.
Tests to detect antibiotic residues in milk are expensive. And in some cases, in a household or on a small farm, they can be neglected. This explains the high risk of encountering drug residues in milk of unknown or unverified origin.
What is the danger of getting small amounts of antibiotics into our body? The doses of drugs that we can get with dairy products are small. The risk that they will harm us directly is low. But we are not alone.
Changes are taking place in the bacterial world around and within us. Having “acquainted” with small doses of drugs, bacteria acquire resistance to them, and then transfer these new qualities to their close and distant relatives. Thanks to the mechanisms of genetic information exchange, harmless bacteria transfer the properties of antibiotic resistance to their pathogenic relatives . In other words, one day we may not see a positive result from the drug prescribed to you, because the bacteria living in our body have become resistant to antibiotics and transferred these properties to the causative agents of the current disease. This is what underlies the outbreaks of refractory infections in the developing southern countries.
This is what underlies the outbreaks of refractory infections in the developing southern countries.
Is there any danger in any product on the supermarket shelf? Of course not. The residual content of antibiotics in food is strictly controlled by law. Violation of the maximum allowable standards is fraught with significant financial and image losses for the manufacturer. Therefore, conscientious companies closely monitor the quality and safety of their products, both on farms and in production, for example, by carrying out incoming laboratory control of incoming raw materials.
Viola operates a very small number of dairy farms in Russia. Before approving a new supplier of raw milk, we conduct a thorough audit of the conditions of housing and feeding of animals, as well as technological processes. We know that prevention of diseases is cheaper and more profitable than their treatment. In addition, tasty milk can only be obtained from healthy cows.
If, nevertheless, the cow becomes ill, then for her treatment, drugs are used, agreed in advance with Viola specialists. This allows us to monitor milk safety with highly sensitive tests available.
This allows us to monitor milk safety with highly sensitive tests available.
Often we hear questions about the reasons for long-term storage of UHT milk. Say, in addition to heat treatment, such milk is additionally “enriched” with antibiotics or preservatives. This question needs to be answered in more detail. And we will definitely do it in a separate message. And here we note that the reason for the long shelf life of such products lies not in antibiotics and “chemistry”, but in the complete destruction of the vegetative forms of microorganisms during sharp and short-term heating of milk, which, in the absence of heat treatment, cause it to turn sour.
- Avoid buying raw milk and dairy products “on hand”, for example from barrels in gardening in summer, or from unknown producers.
- Do not self-prescribe antibiotics for yourself, your children, or even pets.
- Follow the doctor’s recommendations regarding the dosage of the drug and the duration of its administration.


 The suitability of any of the described options in an individual
The suitability of any of the described options in an individual Dairy products include milk as well as butter, yogurt, and cheese. After taking an antibiotic you may need to wait for up to three hours before eating or drinking any dairy products. Grapefruit juice and dietary supplements containing minerals like calcium may also work dampen the effect of antibiotics.
Dairy products include milk as well as butter, yogurt, and cheese. After taking an antibiotic you may need to wait for up to three hours before eating or drinking any dairy products. Grapefruit juice and dietary supplements containing minerals like calcium may also work dampen the effect of antibiotics.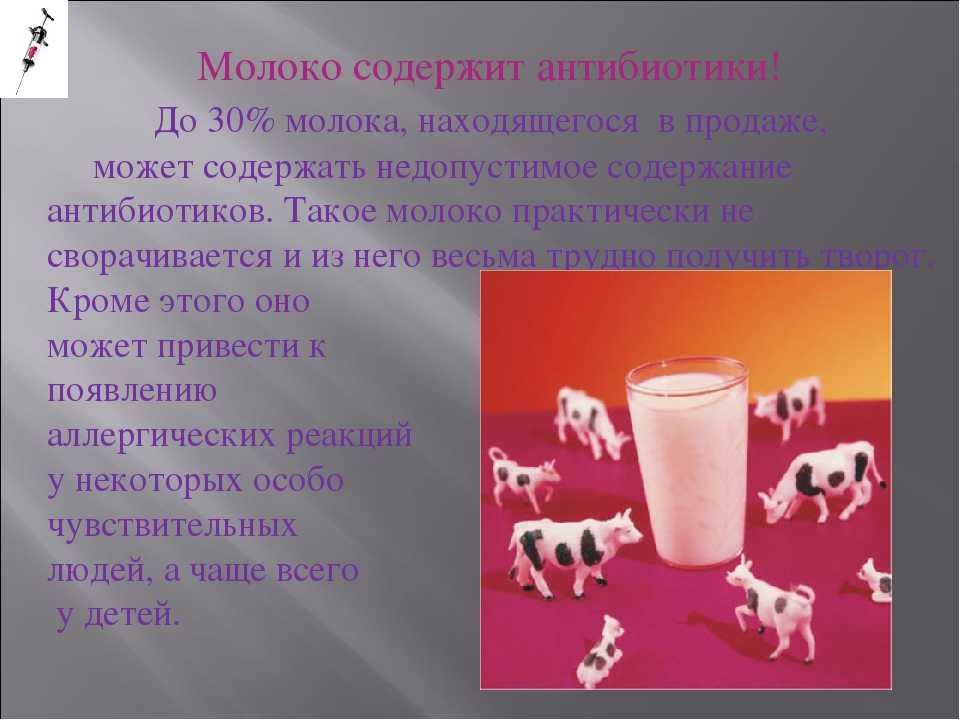 Antibiotics might interact with some blood thinners and antacids, for example. Some antibiotics can make birth control pills less effective.
Antibiotics might interact with some blood thinners and antacids, for example. Some antibiotics can make birth control pills less effective. Taschenlehrbuch Medizinische Mikrobiologie. Stuttgart: Thieme; 2014.
Taschenlehrbuch Medizinische Mikrobiologie. Stuttgart: Thieme; 2014.