Causes of very watery diarrhea. Watery Diarrhea: Causes, Symptoms, and Effective Treatments
What are the main causes of watery diarrhea. How can you identify the symptoms of different types of diarrhea. What are the most effective treatments for watery diarrhea. When should you seek medical attention for persistent diarrhea. How can you prevent dehydration during a bout of watery diarrhea.
Understanding Watery Diarrhea: An Overview
Watery diarrhea is a common digestive issue that can be both uncomfortable and potentially dangerous if left untreated. It is characterized by frequent, loose, and watery stools. While most cases resolve on their own within a few days, some instances may require medical intervention. This article delves into the various causes, symptoms, and treatments for watery diarrhea, providing you with comprehensive information to better understand and manage this condition.
Acute Causes of Watery Diarrhea
Acute watery diarrhea typically lasts for a short period and is often caused by specific triggers. Here are some common acute causes:

Viral Infections
Viral infections are a frequent cause of watery diarrhea. One particularly notorious culprit is norovirus. Have you ever wondered why entire cruise ships sometimes fall ill simultaneously? Norovirus is often the answer. This highly contagious virus spreads rapidly in confined spaces, causing sudden onset of watery diarrhea, nausea, and vomiting. While unpleasant, norovirus infections usually resolve on their own within a few days.
Food Poisoning
Food poisoning, also known as foodborne illness, is another common cause of acute watery diarrhea. Despite its colloquial name “stomach flu,” it has no relation to influenza. Instead, it’s caused by consuming food contaminated with bacteria, viruses, parasites, or toxins. Symptoms typically include nausea, vomiting, diarrhea, and abdominal pain, sometimes accompanied by fever and chills.
Which foods are most susceptible to contamination? While any food can become contaminated if not handled properly, some high-risk items include:

- Meat and poultry
- Seafood
- Dairy products
- Fresh fruits and vegetables
Most cases of food poisoning resolve with supportive care, including rest, hydration, and over-the-counter pain relievers. However, severe cases can lead to dehydration, requiring medical attention and possibly intravenous fluids.
Bacterial Infections
Certain bacterial infections can cause acute watery diarrhea. One notable example is vibriosis, caused by bacteria of the Vibrio genus. Vibrio parahaemolyticus and Vibrio vulnificus are two species known to cause this illness. The primary risk factor for vibriosis is consuming raw or undercooked seafood, particularly oysters from coastal waters, especially the Gulf of Mexico.
Symptoms of vibriosis include fever, vomiting, and diarrhea, sometimes accompanied by mental confusion. For individuals with weakened immune systems or liver disease, vibriosis can be particularly dangerous. If someone experiences these symptoms after consuming raw seafood or swimming in ocean or bay water, it’s considered a medical emergency requiring immediate attention.
Chronic Causes of Watery Diarrhea
While acute diarrhea often resolves quickly, chronic watery diarrhea can persist for weeks or even months. These long-lasting cases may require more intensive treatment and sometimes hospitalization. Let’s explore some of the chronic causes of watery diarrhea:
Chronic Infections
Some infections can lead to prolonged bouts of watery diarrhea. One notable example is Clostridium difficile (C. difficile) infection. C. difficile is a bacterium that normally resides in the gut at low levels, kept in check by other gut bacteria. However, when a person takes antibiotics for another condition, these beneficial bacteria may be killed off, allowing C. difficile to proliferate unchecked.
How does C. difficile infection occur? It often follows antibiotic treatment for other conditions. The antibiotics disrupt the normal gut flora, creating an environment where C. difficile can thrive. This leads to persistent watery diarrhea that doesn’t resolve without targeted treatment.

Treatment for C. difficile infection often requires hospitalization for monitoring and proper management to prevent dangerous levels of dehydration. The initial treatment typically involves antibiotics specifically targeting C. difficile, with vancomycin being a common first-line option. In some cases, restoration of the normal gut bacteria may also be necessary.
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease is a chronic condition that can affect either the small intestine, large intestine, or both. It can manifest in various ways, producing watery diarrhea, bloody diarrhea, mucus-laden diarrhea, or a combination of these. IBD is typically treated with medications that suppress and modulate the immune response.
If you’re experiencing long-standing watery diarrhea that doesn’t respond to antibiotics, IBD could be a possibility. However, a definitive diagnosis usually requires a colonoscopy to examine the intestinal walls.
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome is a complex condition that can present with a variety of symptoms. It’s classified into three main types:
- IBS-C: Predominantly constipation
- IBS-D: Predominantly diarrhea
- IBS-M: Mixed symptoms
IBS-D, or Irritable Bowel Syndrome with diarrhea, is characterized by abdominal pain or discomfort lasting at least three days per month, with symptoms improving after a bowel movement. The onset of discomfort is typically associated with changes in stool frequency or appearance.
It’s important to note that IBS is a syndrome, meaning it’s a collection of symptoms rather than a single disease. Treatment approaches vary widely and may include dietary changes (such as avoiding food allergens and lactose), increasing fiber intake, and boosting physical activity levels. IBS is typically diagnosed only after more serious conditions like IBD or cancer have been ruled out.
Recognizing Symptoms and Seeking Medical Attention
While many cases of watery diarrhea resolve on their own, certain symptoms warrant immediate medical attention. Here are some red flags to watch out for:
- Persistent diarrhea lasting more than a few days
- Signs of severe dehydration (extreme thirst, dry mouth, little or no urination, severe weakness, dizziness, or lightheadedness)
- Fever above 102°F (39°C)
- Severe abdominal or rectal pain
- Bloody stools
- Symptoms of food poisoning in high-risk individuals (infants, older adults, pregnant women, or those with weakened immune systems)
In cases of suspected botulism (a rare but serious form of food poisoning), symptoms like blurred vision, dizziness, or paralysis require immediate emergency care. Don’t hesitate to call emergency services or go to the nearest emergency room if these symptoms occur.

Prevention and Management of Watery Diarrhea
While not all cases of watery diarrhea can be prevented, there are steps you can take to reduce your risk and manage symptoms when they occur:
Preventive Measures
- Practice good hygiene: Wash your hands thoroughly and frequently, especially before handling food and after using the bathroom.
- Ensure proper food handling: Cook foods thoroughly, store them at appropriate temperatures, and avoid cross-contamination.
- Be cautious with water and food when traveling: In areas with poor sanitation, drink bottled water and avoid raw or undercooked foods.
- Use antibiotics judiciously: Only take antibiotics when prescribed by a healthcare professional, as overuse can disrupt your gut flora.
Management Strategies
If you do experience watery diarrhea, here are some strategies to manage your symptoms:
- Stay hydrated: Drink plenty of fluids to replace what you’re losing. Water, clear broths, and electrolyte solutions are good choices.
- Eat a bland diet: Stick to easily digestible foods like bananas, rice, toast, and applesauce (the BRAT diet) until your symptoms improve.
- Avoid trigger foods: Stay away from dairy products, fatty foods, high-fiber foods, and spicy dishes until you recover.
- Consider probiotics: These may help restore balance to your gut flora, especially after antibiotic use.
- Use over-the-counter medications: Antidiarrheal medications like loperamide can provide relief, but avoid these if you have bloody stools or suspect a bacterial infection.
The Importance of Hydration in Managing Watery Diarrhea
One of the most critical aspects of managing watery diarrhea is maintaining proper hydration. Diarrhea can lead to rapid fluid loss, potentially resulting in dehydration, which can be dangerous if left unchecked. But how can you effectively stay hydrated during a bout of watery diarrhea?
Recognizing Dehydration
First, it’s crucial to recognize the signs of dehydration. These may include:
- Increased thirst
- Dry mouth and lips
- Decreased urine output or dark-colored urine
- Fatigue
- Dizziness or lightheadedness
- Dry skin that doesn’t bounce back quickly when pinched
Effective Hydration Strategies
To combat dehydration, consider the following strategies:
- Oral Rehydration Solutions (ORS): These specially formulated drinks contain the right balance of electrolytes and glucose to promote fluid absorption. You can purchase ORS at most pharmacies or make your own at home.
- Clear Fluids: Water, clear broths, and weak tea can help replenish fluids without irritating the digestive system.
- Electrolyte-Rich Foods: Once you can tolerate solid foods, incorporate items like bananas (rich in potassium) and salty crackers to help restore electrolyte balance.
- Avoid Certain Beverages: Steer clear of caffeine, alcohol, and sugary drinks, as these can worsen dehydration.
Remember, small, frequent sips are often better tolerated than large amounts of fluid at once. If you’re unable to keep fluids down or show signs of severe dehydration, seek medical attention promptly.
When to Consider Probiotics for Watery Diarrhea
Probiotics, often referred to as “good bacteria,” have gained attention for their potential role in managing various digestive issues, including watery diarrhea. But when should you consider using probiotics, and how effective are they?
Understanding Probiotics
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. They work by helping to restore balance to the gut microbiome, which can be disrupted during bouts of diarrhea or after antibiotic use.
Effectiveness of Probiotics
Research suggests that certain probiotic strains may be beneficial in specific cases of watery diarrhea:
- Antibiotic-Associated Diarrhea: Probiotics, particularly Saccharomyces boulardii and some Lactobacillus strains, have shown promise in preventing and reducing the duration of antibiotic-associated diarrhea.
- Acute Infectious Diarrhea: Some studies indicate that probiotics may shorten the duration of acute infectious diarrhea, particularly in children.
- Traveler’s Diarrhea: Certain probiotic strains may help prevent traveler’s diarrhea when taken before and during travel.
While probiotics are generally considered safe for most people, it’s always best to consult with a healthcare provider before starting any new supplement regimen, especially if you have a compromised immune system or other underlying health conditions.

Long-Term Management of Chronic Watery Diarrhea
For individuals dealing with chronic conditions that cause watery diarrhea, such as IBD or IBS, long-term management strategies are crucial. These may include:
Dietary Modifications
Identifying and avoiding trigger foods can significantly improve symptoms. Common triggers include:
- Dairy products (for those with lactose intolerance)
- High-fat foods
- Spicy foods
- Caffeine and alcohol
- Artificial sweeteners
Some individuals may benefit from following specific diets, such as the low FODMAP diet, which restricts certain types of fermentable carbohydrates.
Stress Management
Stress can exacerbate symptoms of chronic digestive conditions. Incorporating stress-reduction techniques like meditation, yoga, or regular exercise can be beneficial.
Medications
Depending on the underlying cause, various medications may be prescribed for long-term management. These could include:
- Anti-inflammatory drugs for IBD
- Antispasmodics for IBS
- Bile acid binders for bile acid malabsorption
Regular Medical Follow-ups
Chronic conditions require ongoing monitoring. Regular check-ups with a gastroenterologist can help ensure that the treatment plan remains effective and can be adjusted as needed.

Remember, managing chronic watery diarrhea is often a process of trial and error. What works for one person may not work for another, so patience and open communication with your healthcare provider are key.
What Causes Watery Diarrhea & How to Get Fast Relief
Chronic causes
Chronic causes of watery diarrhea are those that are longer-lasting or more difficult to eradicate and may require hospitalization.
- Chronic infections (C. Difficile, Campylobacter): Some infections like C. difficile occur in part because of treatment for other diseases. C. difficile is a bacterium that lives peacefully in a normal bowel as it is often kept at low levels by normal gut bacteria. However, for individuals treated with antibiotics, the normal gut bacteria may have been killed along with the harmful bacteria causing an infection. This leaves C. difficile unchecked and able to reproduce in large amounts. C. difficile, unless treated with targeted antibiotics for C. difficile and / or the replacement of normal gut bacteria, will continue to produce watery diarrhea. Often treatment of C. difficile requires admission to the hospital for monitoring and proper treatment to avoid dangerous levels of dehydration.
 It is often (but not always) first treated with the antibiotic vancomycin.
It is often (but not always) first treated with the antibiotic vancomycin. - Inflammatory bowel disease: This can affect either the small intestine, large intestine, or both. It may produce watery diarrhea, bloody diarrhea, mucus-laden diarrhea or a mixture of the three. It is commonly treated with drugs that temper and lower the immune response. If you have long-standing watery diarrhea that does not respond to antibiotics, you may have inflammatory bowel disease or irritable bowel syndrome. However, a proper diagnosis will require a colonoscopy (or a scope usually inserted through the anus) to examine the walls of the intestines.
- Irritable bowel syndrome: This can have many different kinds of symptoms. It can manifest as constipation (IBS-C), diarrhea (IBS-D), or mixed (IBS-M). Irritable bowel syndrome with diarrhea is defined as abdominal pain or discomfort lasting at least three days per month with improvement on defecation and onset of discomfort associated with a change in the frequency of stool or the appearance of stool.
 It should be noted that IBS is a syndrome which means a series of symptoms, not a single disease. Treatments vary widely from avoidance of food allergens and lactose and increasing consumption of fiber and physical activity levels. Irritable bowel syndrome is only diagnosed after inflammatory bowel disease or cancer has been ruled out.
It should be noted that IBS is a syndrome which means a series of symptoms, not a single disease. Treatments vary widely from avoidance of food allergens and lactose and increasing consumption of fiber and physical activity levels. Irritable bowel syndrome is only diagnosed after inflammatory bowel disease or cancer has been ruled out.
Viral (norovirus) infection
If you ever heard of an entire cruise ship of people coming down with the same “stomach bug,” chances are that was norovirus. Fortunately, norovirus usually goes away on its own after a few days, but is pretty unpleasant and can spread extremely easily. The …
Food poisoning
Food poisoning, also called foodborne illness or “stomach flu,” is an acute infection of the digestive tract from food contaminated with bacteria, viruses, parasites, or other toxins. It actually has no relation to influenza.
Any food can become contaminated if not prepared under clean conditions, cooked thoroughly, or stored at cold temperatures.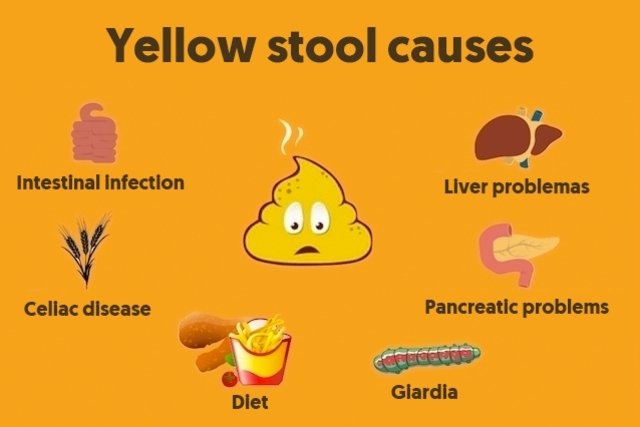 Meat, fish, dairy products, and fresh fruits and vegetables are some of the most easily contaminated foods.
Meat, fish, dairy products, and fresh fruits and vegetables are some of the most easily contaminated foods.
Symptoms include nausea, vomiting, diarrhea, and abdominal pain, and sometimes fever and chills.
Most people recover on their own with supportive care, meaning rest, fluids, and over-the-counter pain relievers and fever reducers.
However, dehydration can result if the vomiting and/or diarrhea are not controlled and IV fluids may be needed.
If there is also blurred vision, dizziness, or paralysis, the nervous system may be affected due to botulism. This is a medical emergency. Take the patient to the emergency room or call 9-1-1.
Proper food preparation and storage, along with frequent and thorough handwashing, is the best prevention.
Rarity: Common
Top Symptoms: nausea, abdominal pain (stomach ache), headache, abdominal cramps (stomach cramps), dizziness
Symptoms that never occur with food poisoning: severe fever, being severely ill, bloody diarrhea
Urgency: Self-treatment
Diarrhea caused by a bacteria called vibrio
The Vibrio genus of bacteria causes nausea, vomiting, and diarrhea that can be very serious. Vibrio parahaemolyticus and Vibrio vulnificus are two of the species that cause this illness, which is also called vibriosis.
Vibrio parahaemolyticus and Vibrio vulnificus are two of the species that cause this illness, which is also called vibriosis.
The primary risk factor is eating raw or undercooked seafood, especially oysters from any coastal waters and from the Gulf of Mexico in particular. People with weakened immune systems or liver disease are especially vulnerable to this infection.
Symptoms include fever, vomiting, and diarrhea, sometimes with mental confusion. These symptoms in a person who has recently eaten raw seafood, or has been swimming in ocean or bay water, are considered a medical emergency. Take the patient to the emergency room or call 9-1-1.
Some types of Vibrio-caused illness can worsen very quickly and lead to dehydration and septicemia, which can be life-threatening.
Diagnosis is made through patient history, physical examination, and lab tests on blood, urine, and stool samples.
Treatment will usually involve hospitalization for intravenous fluids, antibiotics, and supportive care.:max_bytes(150000):strip_icc()/GettyImages-1204278958-157f28792f424289af9c57912d3e0bf0.jpg)
Rarity: Rare
Top Symptoms: diarrhea, nausea, stomach bloating, headache, abdominal cramps (stomach cramps)
Symptoms that always occur with diarrhea caused by a bacteria called vibrio: diarrhea
Urgency: Self-treatment
Normal occurrence of diarrhea
Diarrhea can be an indication of serious illness – especially in young children – but in some cases it has a much simpler cause and can be easily cured.
If there are simply frequent loose stools – three or more times per day – without other symptoms of illness, the most common cause is food or drink.
Overuse of caffeine, beer, or wine has a laxative effect on some individuals. The artificial sweeteners sorbitol and mannitol are known laxatives, as are some herbal supplements and some over-the-counter vitamin and mineral preparations.
Lactose intolerance, or the inability to digest the natural sugar in milk, causes digestive upset and diarrhea./causes-of-diarrhea-sudden-or-chronic-1324505-5bb7c1e8c9e77c0026b0f77a.png)
Diarrhea can cause dehydration and mineral imbalance no matter what the cause, so it is still important to manage it.
The best treatment is to remove some items or supplements from the diet and watch the results. This will show which items are causing the diarrhea.
It’s always wise to use any new supplements in moderation so that if the trouble recurs, the cause will be plain.
Rarity: Common
Top Symptoms: diarrhea, mild diarrhea
Symptoms that always occur with normal occurrence of diarrhea: diarrhea
Symptoms that never occur with normal occurrence of diarrhea: bloody diarrhea, severe diarrhea, worsening diarrhea, being severely ill, ill appearance
Urgency: Self-treatment
Microscopic colitis
Microscopic colitis is caused by inflammation of the large intestine than can only be seen with a microscope. It is believed that microscopic colitis is caused by an overly aggressive immune response to a certain trigger that can be related to medication, an infection, autoimmune diseases, genetics, or a malabsorption of bile.
Symptoms primarily include watery diarrhea accompanied by abdominal pain, cramps or discomfort, and an urgency to use the restroom.
Treatment depends on the cause, such as halting offensive drugs and taking anti-diarrheal medication or steroids. It is also important to make sure you stay hydrated throughout the recovery period.
Rarity: Rare
Top Symptoms: fatigue, nausea, diarrhea, abdominal pain (stomach ache), stomach bloating
Symptoms that always occur with microscopic colitis: diarrhea
Symptoms that never occur with microscopic colitis: bloody diarrhea
Urgency: Primary care doctor
Food poisoning by the staphylococcus bacteria
Food poisoning by staphylococcus bacteria refers to the stomach and intestinal upset caused by eating foods contaminated with the staphylococcus, or “staph,” bacteria.
Most often, food is contaminated when the person preparing it did not thoroughly wash their hands first. The staph bacteria quickly multiply in food or milk, producing toxins which actually create the illness. The toxins are not destroyed by cooking and the food may look fresh.
The staph bacteria quickly multiply in food or milk, producing toxins which actually create the illness. The toxins are not destroyed by cooking and the food may look fresh.
Symptoms develop rapidly, within 30 minutes to a few hours, and include nausea, vomiting, stomach cramping, and diarrhea. The illness itself is not spread from person to person.
Diagnosis is made through patient history and physical examination. Lab tests are usually not necessary, but testing may be done if there is a large outbreak with many people affected in one place.
A food poisoning episode usually resolves on its own within 24 hours. Antibiotics are not effective against the toxins. The symptoms can be treated with rest, plenty of fluids, and electrolyte replacement with sports drinks. Severe cases may need intravenous fluids in a hospital.
Rarity: Uncommon
Top Symptoms: nausea, nausea or vomiting, diarrhea, abdominal cramps (stomach cramps), vomiting
Symptoms that always occur with food poisoning by the staphylococcus bacteria: nausea or vomiting
Urgency: Self-treatment
Traveler’s diarrhea
Traveler’s diarrhea is a digestive tract disorder that commonly causes loose stools and abdominal cramps.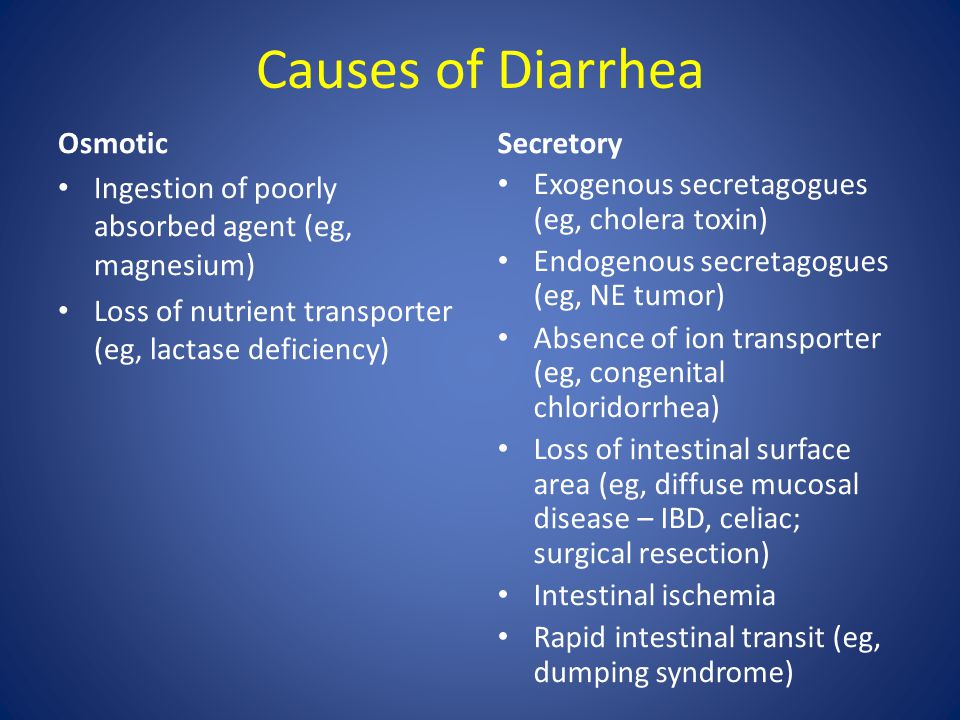 It’s caused by eating contaminated food or drinking contaminated water.
It’s caused by eating contaminated food or drinking contaminated water.
Rarity: Common
Top Symptoms: diarrhea, nausea, abdominal pain (stomach ache), fever, stomach bloating
Symptoms that always occur with traveler’s diarrhea: diarrhea
Symptoms that never occur with traveler’s diarrhea: anxiety
Urgency: Self-treatment
Shigella infection
Shigella infection, or shigellosis, is an intestinal infection caused by a strain of Shigella bacteria.
Shigellosis is highly contagious through fecal matter. Anyone coming into contact with any trace of feces in food, drink, or surfaces can get the disease. Swimming in contaminated water, even in a chlorinated pool or hot tub, is another source of infection.
Most susceptible are young children; travelers to less developed regions; and anyone with a weakened immune system.
Symptoms include fever; abdominal pain and cramps; and severe diarrhea, which may contain blood.
If not treated, there is the risk of dehydration due to the diarrhea and fever. Young children are especially susceptible.
Diagnosis is made through patient history, physical examination, and testing of a stool sample.
Treatment involves rest and fluids. Most cases clear up within a week. Sometimes antibiotics are used in more severe cases, though antibiotics are not effective against some forms of Shigella bacteria.
The best prevention is frequent and thorough handwashing, and good hygiene when preparing food.
Rarity: Rare
Top Symptoms: diarrhea, general abdominal pain, severe diarrhea, watery diarrhea, fatigue
Symptoms that always occur with shigella infection: diarrhea
Urgency: Self-treatment
Intestinal infection with ameba parasite
Visiting or living in places with poor sanitation can lead to parasite infections that can cause long-lasting diarrhea and stomach pain.:max_bytes(150000):strip_icc()/1941711-causes-of-black-stool-01-5b057bccfa6bcc0037c676bb.png)
Rarity: Rare
Top Symptoms: nausea, loss of appetite, diarrhea, constipation, general abdominal pain
Urgency: Primary care doctor
Mild, Moderate, or Severe Diarrhea
Topic Overview
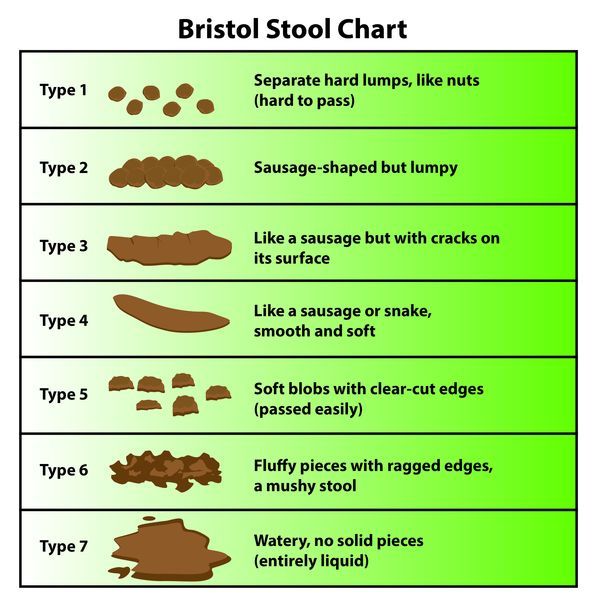
Diarrhea is described as an increase in the frequency of bowel movements or a decrease in the consistency of stools that causes the discharge of watery, loose stools. The severity of diarrhea is determined by the size and number of stools passed within a period of time.
- Severe diarrhea means having more than 10 loose, watery stools in a single day (24 hours).
- Moderate diarrhea means having more than a few but not more than 10 diarrhea stools in a day.
- Mild diarrhea means having a few diarrhea stools in a day.
Severe diarrhea has many causes. Stomach flu (gastroenteritis) or food poisoning may cause severe diarrhea.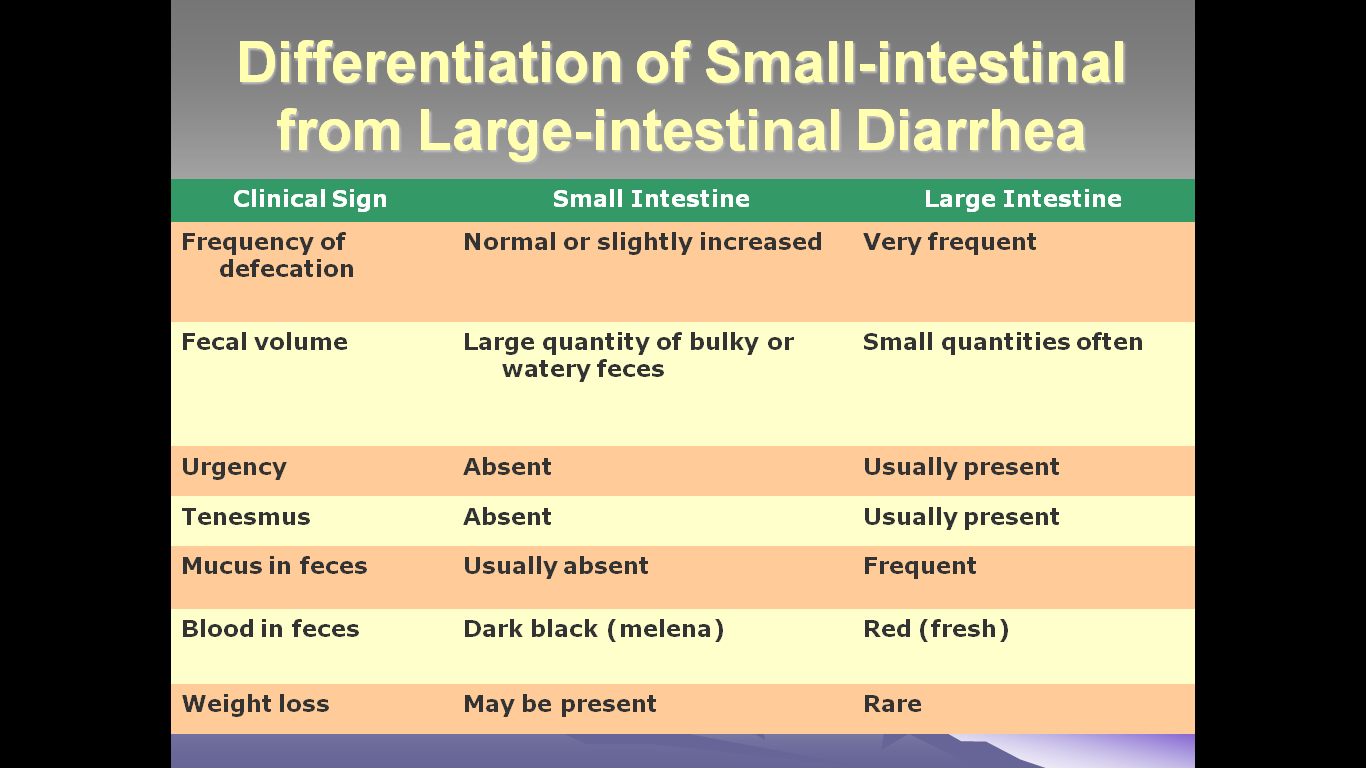 Drinking untreated water that contains the Giardia lamblia parasite can cause diarrhea that develops 1 to 4 weeks later.
Drinking untreated water that contains the Giardia lamblia parasite can cause diarrhea that develops 1 to 4 weeks later.
Severe diarrhea increases your risk of dehydration by causing your body to lose large amounts of fluid quickly. Be sure to increase your intake of fluids, such as water or a rehydration drink, and to watch for symptoms of dehydration.
Persistent diarrhea can have many causes, including dietary changes, stress, irritable bowel syndrome, and certain medicines. Occasionally, persistent diarrhea can be a symptom of a more serious condition, such as a chronic infection, inflammatory bowel disease, a malabsorption syndrome, or colorectal cancer.
Credits
Current as of:
February 26, 2020
Author: Healthwise Staff
Medical Review:
William H. Blahd Jr. MD, FACEP – Emergency Medicine
Adam Husney MD – Family Medicine
Kathleen Romito MD – Family Medicine
Current as of: February 26, 2020
Author:
Healthwise Staff
Medical Review:William H.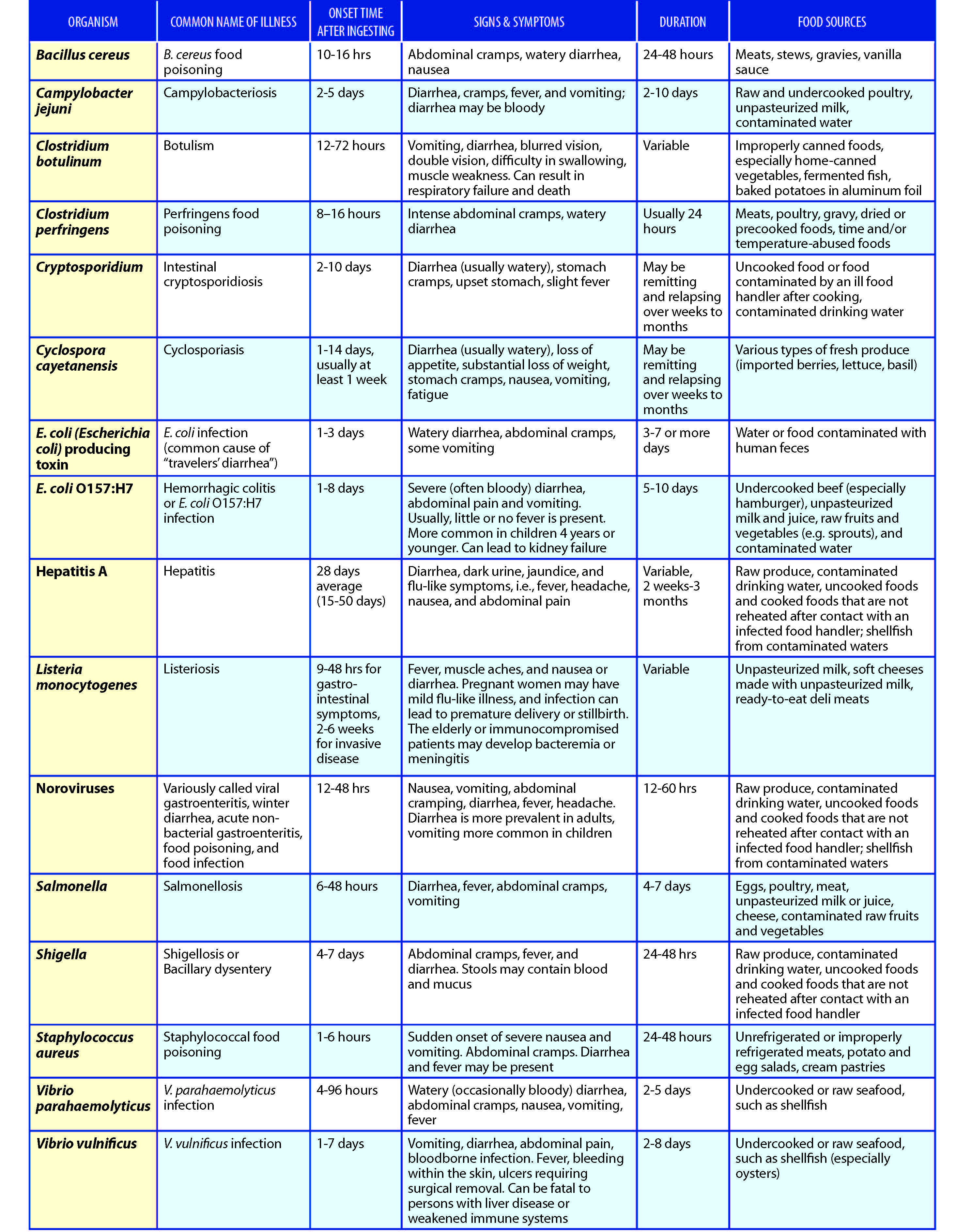 Blahd Jr. MD, FACEP – Emergency Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine
Blahd Jr. MD, FACEP – Emergency Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine
Diarrhea
Is this your child’s symptom?
- Sudden increase in the number and looseness of stools
- Diarrhea means 3 or more watery or very loose stools. Reason: 1 or 2 loose stools can be normal with changes in diet.
Causes of Acute Diarrhea
- Virus (such as Rotavirus). An infection of the intestines from a virus is the most common cause.
- Bacteria (such as Salmonella). Less common cause. Diarrhea often contains streaks of blood.
- Food Poisoning. This causes rapid vomiting and diarrhea within hours after eating the bad food. It is caused by toxins from germs growing in foods left out too long. Most often, symptoms go away in less than 24 hours. It often can be treated at home without the need for medical care.
- Giardia (a parasite).
 More likely in child care center outbreaks.
More likely in child care center outbreaks. - Traveler’s Diarrhea. Caused by germs in food or drink. Suspect this if it follows recent foreign travel.
- Antibiotic Diarrhea. Many antibiotics cause mild diarrhea. This is not an allergic reaction. Keep giving the antibiotic. Call your doctor if any serious symptoms occur.
- Serious Causes. Most bacterial diarrhea goes away on its own. A few can cause a severe large bowel infection (such as Shigella colitis). C. difficile is a serious cause that can occur after being on strong antibiotics.
- Serious Complication: Dehydration. This is the health problem where the body has lost too much fluid. (See below for more on this).
Causes of Recurrent Diarrhea
- Cow’s Milk Allergy. Can cause loose, slimy stools in babies. Can be blood-streaked. Starts within the first 2 months of life. Need to avoid cow’s milk formulas.

- Toddler’s Diarrhea. Toddlers who pass 3 to 6 sloppy stools per day. Stools may run out of the diaper. Symptoms begin at age 1. Symptoms resolve at age 3 or 4, after toilet trained. Harmless and no impact on growth. Fruit juice makes it worse. The cause is rapid transit time from stomach to anus. May develop irritable bowel syndrome (IBS) in adult years.
- Lactose Intolerance. Lactose is the sugar in milk. Many people cannot absorb lactose. The gut bacteria convert the lactose to gas. The main symptoms are a lot of gas, loose stools and stomach bloating. Onset usually at age 4 or 5. This most often runs in the family (genetic).
Diarrhea Scale
- Mild: 3-5 watery stools per day
- Moderate: 6-9 watery stools per day
- Severe: 10 or more watery stools per day
- The main risk of diarrhea is dehydration.
- Loose or runny stools do not cause dehydration.

- Frequent, watery stools can cause dehydration.
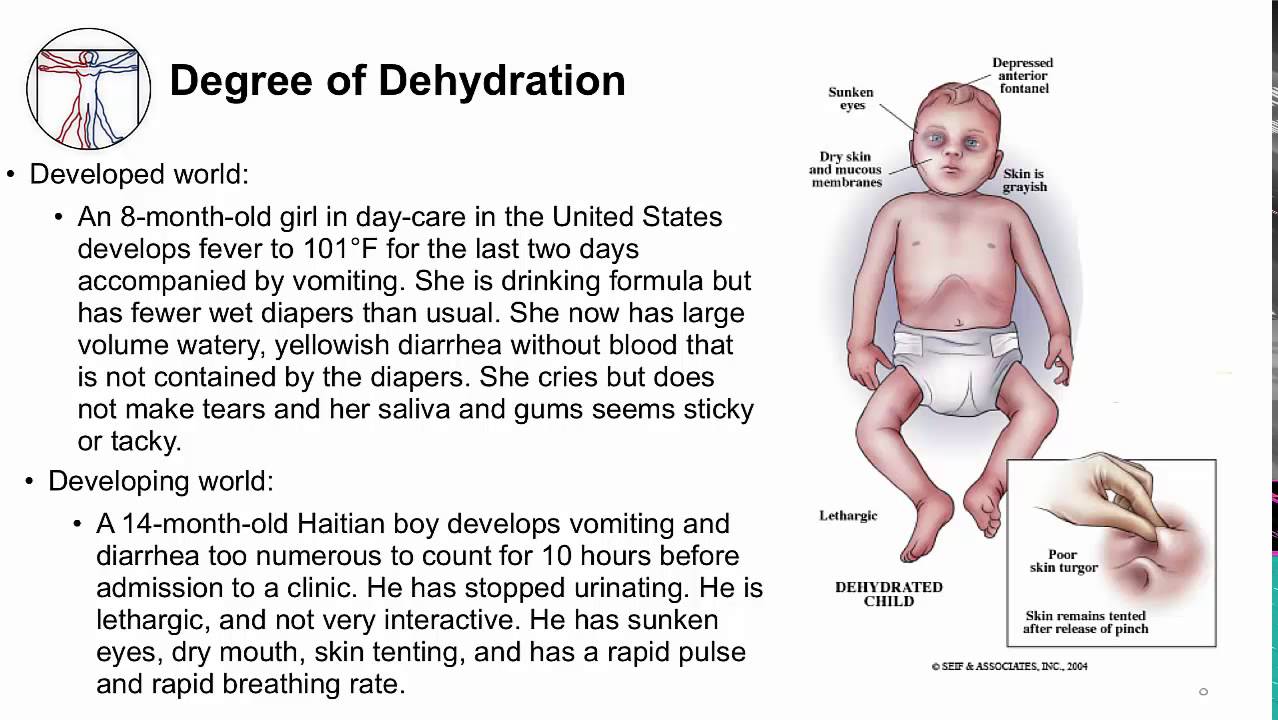
Dehydration: How to Know
- Dehydration means that the body has lost too much fluid. This can happen with vomiting and/or diarrhea. A weight loss of more than 3% is needed. Mild diarrhea or mild vomiting does not cause this. Neither does a small decrease in fluid intake.
- Dehydration is the most important problem caused by diarrhea. Dehydration is a reason to see your doctor right away.
- These are signs of dehydration:
- Decreased urine (no urine in more than 8 hours) happens early in dehydration. So does a dark yellow color. If the urine is light straw colored, your child is not dehydrated.
- Dry tongue and inside of the mouth. Dry lips are not helpful.
- Dry eyes with decreased or absent tears
- In babies, a depressed or sunken soft spot
- Slow blood refill test: longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again.
 Ask your doctor to teach you how to do this test.
Ask your doctor to teach you how to do this test. - Fussy, tired out or acting ill. If your child is alert, happy and playful, he or she is not dehydrated.
- A child with severe dehydration becomes too weak to stand. They can also be very dizzy when trying to stand.
Diarrhea in Breastfed Babies: How to Tell
- Diarrhea in a breastfed baby is sometimes hard to tell.
- Normal breastfed stools are loose (often runny and seedy). Stools are yellow, but sometimes can be green. The green color is from bile. Runny stools can even be bordered by a water ring. These are all normal stools.
- Breastfed babies often pass more than 6 stools per day. Until 2 months of age, they may pass a stool after each feeding. But, if stools suddenly increase in number and looseness, suspect diarrhea. If it lasts for 3 or more stools, the baby has diarrhea.
- If the stools contain mucus, blood or smell bad, this points to diarrhea.
- Other clues to diarrhea are poor eating, acting sick, or a fever.

Diarrhea in Formula-Fed Infants: How to Tell
- Formula-fed babies pass 1 to 8 stools per day during the first week. Then it starts to slow down to 1 to 4 per day. This lasts until 2 months of age.
- The stools are yellow in color and thick like peanut butter.
- Suspect diarrhea if the stools suddenly increase in number or looseness. If it lasts for 3 or more stools, the baby has diarrhea.
- If the stools contain mucus, blood, or smells bad, this points to diarrhea.
- Other clues to diarrhea are poor eating, acting sick or a fever.
- After 2 months of age, most babies pass 1 or 2 stools per day. They can also pass 1 every other day. They no longer appear to have mild diarrhea.
When to Call for Diarrhea
Call 911 Now
- Not moving
- Too weak or dizzy to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.

- Blood in the stool
- Constant stomach pain lasts more than 2 hours
- Vomits clear liquids 3 or more times
- Age less than 1 month with 3 or more diarrhea stools in past 24 hours
- Severe diarrhea. 10 or more watery stools in the last 24 hours.
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Moderate diarrhea. 6 or more watery stools in the last 24 hours.
- Stomach pain that do not go away after each diarrhea stool
- Loss of bowel control in a toilet trained child occurs 3 or more times
- Fever lasts more than 3 days
- Close contact with person or animal who has bacterial diarrhea
- Contact with reptile (snake, lizard, turtle) in past 14 days
- Travel to country at risk for diarrhea within past month
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Diarrhea lasts more than 2 weeks
- Loose stools are a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild diarrhea (probably caused by a virus)
- Diarrhea disease: how to prevent
Seattle Children’s Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
Care Advice for Diarrhea
Treatment for Mild Diarrhea
- What You Should Know About Diarrhea:
- Most diarrhea is caused by a virus.
- Bacterial infections as a cause of diarrhea are not common.
- Diarrhea is the body’s way of getting rid of the germs.
- The main risk of diarrhea is dehydration. Dehydration means the body has lost too much fluid.
- Most children with diarrhea don’t need to see their doctor.
- Here are some tips on how to keep ahead of the fluid losses.
- Mild Diarrhea:
- Most kids with diarrhea can eat a normal diet.
- Drink more fluids to prevent dehydration. Formula, breastmilk and/or regular milk are good choices for diarrhea.
- Do not use fruit juices or full-strength sports drinks. Reason: they can make diarrhea worse.
- Solid foods: eat more starchy foods (such as cereal, crackers, rice, pasta).
 Reason: they are easy to digest.
Reason: they are easy to digest.
- Formula-Fed Babies with Frequent, Watery Diarrhea:
- Keep giving formula but feed more often. Offer as much formula as your child will take.
- Mix formula the normal way. Reason: the formula contains plenty of water and doesn’t need more.
- Solid foods: if on baby foods, continue them. Cereals are best.
- Breastfed Babies with Frequent, Watery Diarrhea:
- Give your baby breastmilk more often.
- Also, give extra fluid if breast milk isn’t keeping up with the fluid losses. You can use formula or ORS (Pedialyte).
- Solid foods: if on baby foods, continue them. Cereals are best.
- Older Children (age more than 1 year old) with Frequent, Watery Diarrhea:
- Offer as much fluid as your child will drink. If also eating solid foods, water is fine. So is half-strength Gatorade or half-strength apple juice.
- If won’t eat solid foods, give milk or formula as the fluid.

- Caution: do not use most fruit juices, full-strength sports drinks or soft drinks. Reason: they can make diarrhea worse.
- Solid foods: starchy foods are easy to digest and best. Offer cereals, bread, crackers, rice, pasta or mashed potatoes. Pretzels or salty crackers will help add some salt to meals. Some salt is good.
- Oral Rehydration Solutions (ORS), such as Pedialyte:
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand. It can be bought in food stores or drug stores.
- When to use: start ORS for frequent, watery diarrhea if you think your child is getting dehydrated. That means passing less urine than normal. Increase fluids using ORS. Continue giving breastmilk, formula or regular milk.
- Amount: for babies, give 2-4 ounces (60-120 mL) of ORS after every large watery stool.
- For children over 1 year old, give 4-8 ounces (120-240 mL) of ORS after every large watery stool.
 Children rarely need ORS after age 3.
Children rarely need ORS after age 3. - Caution: do not give ORS as the only fluid for more than 6 hours. Reason: your child will need calories and cry in hunger.
- Probiotics:
- Probiotics are healthy bacteria (such as Lactobacilli). They can replace harmful bacteria in the gut (stomach).
- Probiotics may be helpful in reducing the number of diarrhea stools.
- Age over 12 months old: yogurt is the easiest source of probiotics. Give 2 to 6 ounces (60 to 180 mL) of yogurt. Do this twice daily. Note: today, almost all yogurts are “active culture”.
- Probiotic supplements can also be bought in health food stores.
- Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: keep your child well hydrated.
 Give lots of cold fluids.
Give lots of cold fluids.
- Diaper Rash – Prevention:
- Wash buttocks after each stool to prevent a bad diaper rash.
- To protect the skin, use an ointment (such as Vaseline or Desitin). Put it on the skin around the anus.
- Return to School:
- Your child can go back to school after the stools are formed.
- The fever should also be gone.
- The older child can go back if the diarrhea is mild.
- The toilet trained child also needs to have good control over loose stools.
- What to Expect:
- Viral diarrhea lasts 5-14 days.
- Severe diarrhea only occurs on the first 1 or 2 days. But, loose stools can last for 1 to 2 weeks.
- Call Your Doctor If:
- Blood in the diarrhea
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- Diarrhea lasts over 2 weeks
- You think your child needs to be seen
- Your child becomes worse
Preventing Diarrhea Disease
- Safety Tips in All Countries:
- Hand washing is the key to preventing the spread of infections.

- Always wash the hands before eating, feeding or handling young children or cooking.
- Always wash the hands after any contact with vomit or stools.
- Wash the hands after using the toilet or changing diapers. Help young children wash their hands after using the toilet.
- Cook all poultry fully. Never serve chicken that is still pink inside. Reason: undercooked poultry is a common cause of diarrhea in developed countries.
- Hand washing is the key to preventing the spread of infections.
- Extra Safety Tips in Developing Countries:
- Drink bottled water or boiled water. Avoid tap water, ice cubes and flavored ices.
- Eat foods that have been fully cooked and that are still hot.
- Dry foods such as bread are usually safe.
- Avoid salads and raw vegetables. Avoid fruits that cannot be peeled. Bananas, oranges and apples are safe. Wash your hands before peeling fruit.
- Avoid all undercooked meat and fish.
- Avoid buying foods and drinks from street vendors. Reason: this is a common cause of traveler’s diarrhea.

- Formula for babies: breastfeed if possible. If not, use premixed formula. If you prepare your own, mix the formula with bottled or boiled water.
- Feeding babies: wash bottles, nipples, spoons and dishes with soap and water. Then sterilize them in boiling water for 5 minutes if possible.
- Brush your teeth with bottled or boiled water.
- Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the ‘Call Your Doctor’ symptoms.
Last Reviewed: 10/06/2021
Last Revised: 09/30/2021
Copyright 2000-2021. Schmitt Pediatric Guidelines LLC.
Diarrhea (0-12 Months)
Is this your child’s symptom?
- Sudden increase in the number and looseness of stools
- Diarrhea means 3 or more watery or very loose stools. Reason: 1 or 2 loose stools can be normal with changes in diet.

Causes of Acute Diarrhea
- Virus (such as Rotavirus). An infection of the intestines from a virus is the most common cause.
- Bacteria (such as Salmonella). Less common cause. Diarrhea often contains streaks of blood.
- Giardia (a parasite). More likely in child care center outbreaks.
- Antibiotic Diarrhea. Many antibiotics cause mild diarrhea. This is not an allergic reaction. Keep giving the antibiotic. Call your doctor if any serious symptoms occur.
- Serious Causes. Most bacterial diarrhea goes away on its own. A few can cause a severe large bowel infection (such as Shigella colitis). C. difficile is a serious cause that can occur after being on strong antibiotics.
- Serious Complication: Dehydration. This is the health problem where the body has lost too much fluid. (See below for more on this).
Causes of Recurrent Diarrhea
- Cow’s Milk Allergy.
 Can cause loose, slimy stools in babies. Can be blood-streaked. Starts within the first 2 months of life. Need to avoid cow’s milk formulas.
Can cause loose, slimy stools in babies. Can be blood-streaked. Starts within the first 2 months of life. Need to avoid cow’s milk formulas. - Lactose Intolerance. Lactose is the sugar in milk. Many people cannot absorb lactose. The gut bacteria convert the lactose to gas. The main symptoms are a lot of gas, loose stools and stomach bloating. Onset usually at age 4 or 5. This most often runs in the family (genetic).
Diarrhea Scale
- Mild: 3-5 watery stools per day
- Moderate: 6-9 watery stools per day
- Severe: 10 or more watery stools per day
- The main risk of diarrhea is dehydration.
- Loose or runny stools do not cause dehydration.
- Frequent, watery stools can cause dehydration.
Dehydration: How to Know
- Dehydration means that the body has lost too much fluid. This can happen with vomiting and/or diarrhea. A weight loss of more than 3% is needed.
 Mild diarrhea or mild vomiting does not cause this. Neither does a small decrease in fluid intake.
Mild diarrhea or mild vomiting does not cause this. Neither does a small decrease in fluid intake. - Dehydration is the most important complication of diarrhea. Dehydration is a reason to see your doctor right away.
- These are signs of dehydration:
- Decreased urine (no urine in more than 8 hours) happens early in dehydration. So does a dark yellow color. If the urine is light straw colored, your child is not dehydrated.
- Dry tongue and inside of the mouth. Dry lips are not helpful.
- Dry eyes with decreased or absent tears
- In babies, a depressed or sunken soft spot
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
- Fussy, tired out or acting ill. If your child is alert, happy and playful, he or she is not dehydrated.
Diarrhea in Breastfed Babies: How to Tell
- Diarrhea in a breastfed baby is sometimes hard to tell.

- Normal breastfed stools are loose (often runny and seedy). Stools are yellow, but sometimes can be green. The green color is from bile. Runny stools can even be bordered by a water ring. These are all normal stools.
- Breastfed babies often pass more than 6 stools per day. Until 2 months of age, they may pass a stool after each feeding. But, if stools suddenly increase in number and looseness, suspect diarrhea. If it lasts for 3 or more stools, the baby has diarrhea.
- If the stools contain mucus, blood or smell bad, this points to diarrhea.
- Other clues to diarrhea are poor eating, acting sick, or a fever.
Diarrhea in Formula-Fed Infants: How to Tell
- Formula-fed babies pass 1 to 8 stools per day during the first week. Then it starts to slow down to 1 to 4 per day. This lasts until 2 months of age.
- The stools are yellow in color and thick like peanut butter.
- Suspect diarrhea if the stools suddenly increase in number or looseness.
 If it lasts for 3 or more stools, the baby has diarrhea.
If it lasts for 3 or more stools, the baby has diarrhea. - If the stools contain mucus, blood, or smells bad, this points to diarrhea.
- Other clues to diarrhea are poor eating, acting sick or a fever.
- After 2 months of age, most babies pass 1 or 2 stools per day. They can also pass 1 every other day. They no longer appear to have mild diarrhea.
When to Call for Diarrhea (0-12 Months)
Call 911 Now
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Blood in the stool
- Constant stomach pain lasts more than 2 hours
- Vomits 3 or more times
- Age less than 1 month with 3 or more diarrhea stools in past 24 hours
- Severe diarrhea. 10 or more watery stools in the last 24 hours.
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Moderate diarrhea. 6 or more watery stools in the last 24 hours.
- Stomach pains that do not go away after each diarrhea stool
- Fever lasts more than 3 days
- Close contact with person or animal who has bacterial diarrhea
- Contact with reptile (snake, lizard, turtle) in past 14 days
- Travel to country at risk for diarrhea within past month
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Diarrhea lasts more than 2 weeks
- Loose stools are a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild diarrhea (probably caused by a virus)
Seattle Children’s Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
Care Advice for Diarrhea
- What You Should Know About Diarrhea:
- Most diarrhea is caused by a virus.
- Bacterial infections as a cause of diarrhea are not common.
- Diarrhea is the body’s way of getting rid of the germs.
- The main risk of diarrhea is dehydration. Dehydration means the body has lost too much fluid.
- Most children with diarrhea don’t need to see their doctor.
- Here are some tips on how to keep ahead of the fluid losses.
- Mild Diarrhea:
- Most kids with diarrhea can eat a normal diet.
- Drink more fluids to prevent dehydration. Formula or breastmilk are good choices for diarrhea.
- Do not use fruit juices. Reason: They can make diarrhea worse.
- Solid foods: If on solid foods, eat more starchy foods (such as cereal, crackers, rice, pasta). Reason: They are easy to digest.
- Formula-Fed Babies with Frequent, Watery Diarrhea:
- Keep giving formula but feed more often.
 Offer as much formula as your child will take.
Offer as much formula as your child will take. - Mix formula the normal way. Reason: The formula contains plenty of water and doesn’t need more.
- Solid foods: If on baby foods, continue them. Cereals are best.
- Keep giving formula but feed more often.
- Breastfed Babies with Frequent, Watery Diarrhea:
- Give your baby breastmilk more often.
- Also, give extra fluid if breast milk isn’t keeping up with the fluid losses. You can use formula or ORS (Pedialyte).
- Solid foods: If on baby foods, continue them. Cereals are best.
- Oral Rehydration Solutions (ORS), such as Pedialyte:
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand. It can be bought in food stores or drug stores.
- When to use: Start ORS for frequent, watery diarrhea if you think your child is getting dehydrated. That means passing less urine than normal. Increase fluids using ORS. Continue giving breastmilk, formula or regular milk.

- Amount: For babies, give 2-4 ounces (60-120 ml) of ORS after every large watery stool.
- Caution: Do not give ORS as the only fluid for more than 6 hours. Reason: Your child will need calories and cry in hunger.
- Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil). Caution: avoid ibuprofen until 6 months or older.
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
- Diaper Rash – Prevention:
- Wash buttocks after each stool to prevent a bad diaper rash.
- To protect the skin, use an ointment (such as Vaseline or Desitin). Put it on the skin around the anus.
- Return to Child Care:
- Your child can go back to child care after stools are back to normal.

- The fever should also be gone.
- Your child can go back to child care after stools are back to normal.
- What to Expect:
- Viral diarrhea lasts 5-14 days.
- Severe diarrhea only occurs on the first 1 or 2 days. But, loose stools can last for 1 to 2 weeks.
- Call Your Doctor If:
- Blood in the diarrhea
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- Diarrhea lasts over 2 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the ‘Call Your Doctor’ symptoms.
Last Reviewed: 10/06/2021
Last Revised: 09/30/2021
Copyright 2000-2021 Schmitt Pediatric Guidelines LLC.
Underlying causes of diarrhoea | healthdirect
beginning of content
3-minute read
Diarrhoea usually occurs when fluid cannot be absorbed from your bowel contents, or when extra fluid leaks into the bowel, causing watery stools (poo).
Conditions causing acute diarrhoea
Diarrhoea is usually a symptom of gastroenteritis, an infection of the bowel. Gastroenteritis may be caused by:
Diarrhoea caused by contaminated food or water from a foreign country is known as ‘traveller’s diarrhoea’.
Other causes of acute diarrhoea
Other short-term causes of diarrhoea include:
- food poisoning (due to eating something contaminated or ‘off’)
- emotional upset or anxiety
- drinking too much alcohol
- drinking too much coffee
- a food allergy
- appendicitis
- damage to the lining of the intestines due to radiotherapy or prescribed medications
- damage to the intestines due to reduced blood supply, for example, because of a hernia
Check your symptoms with healthdirect’s Symptom Checker to get advice on when to seek medical attention.
Conditions causing persistent (chronic) diarrhoea
Persistent or chronic diarrhoea is diarrhoea that has lasted longer than 4 weeks.
Conditions that can cause persistent diarrhoea include:
- lactose intolerance — when you have difficulty digesting dairy products
- irritable bowel syndrome — a poorly understood condition where the normal functions of the bowel are disrupted
- coeliac disease — a digestive condition where you are intolerant to the protein gluten
- Crohn’s disease — a condition that causes inflammation of the lining of the digestive system
- cystic fibrosis — an inherited condition that affects the lungs and digestive system
- diabetes — a condition where there is too much glucose in the blood
- diverticular disease — when small pouches (diverticula) form in the large intestine, causing symptoms such as diarrhoea
- gastrectomy — a surgical procedure to remove part of the stomach, for example, to treat stomach cancer
- bowel surgery — where a section of the bowel is removed and can reduce the ability of the bowel to absorb fluids
- microscopic colitis — a type of inflammatory bowel disease that causes watery diarrhoea
- chronic pancreatitis — inflammation of the pancreas, a small organ that produces hormones and digestive juices
- ulcerative colitis — a condition that causes inflammation of the colon (large intestine)
- bowel cancer — cancer in the bowel can cause diarrhoea and blood in your stools
If you have chronic or persistent diarrhoea see your doctor so it can be investigated.
Diarrhoea caused by medicines
Diarrhoea can also be a side effect of many different medicines, including:
The consumer medicines information leaflet that comes with your medicine should state whether diarrhoea is a possible side effect. Or you can contact the Medicines Line on 1300 633 424, a national information service that provides Australians with information about their medicines over the phone, Monday to Friday, 9am to 5pm EST. If you need an interpreter, you can ring the Translating and Interpreting Service (TIS National) on 131 450
Not sure what to do next?
If you are still concerned about your diarrhoea, check your symptoms with healthdirect’s online Symptom Checker to get advice on when to seek medical attention.
The Symptom Checker guides you to the next appropriate healthcare steps, whether it’s self care, talking to a health professional, going to a hospital or calling triple zero (000).
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2019
Types of Diarrhea That You Need to Know About
No matter what, diarrhea is pretty crappy. (No pun intended.) But, it also turns out that not all diarrhea is the same.
Nope. Just like there are lots of types of poop, there are lots of types of diarrhea. And each one says something very specific about your health.
That’s why, when you visit a doctor with a case of tummy troubles, they’re going to ask a few questions to try to suss out which type of diarrhea that you’re experiencing, says Rudolph Bedford, M.D., a gastroenterologist at Providence Saint John’s Health Center in Santa Monica, California. By determining the exact type of diarrhea that you have, your M.D. will be able to more quickly and easily pinpoint the cause and, most importantly, put an end to your gastro woes.
While acute diarrhea (a lose stool here or there) is incredibly common and no real biggie, if your diarrhea lasts for more than a few days, it’s important to make an appointment with your doctor.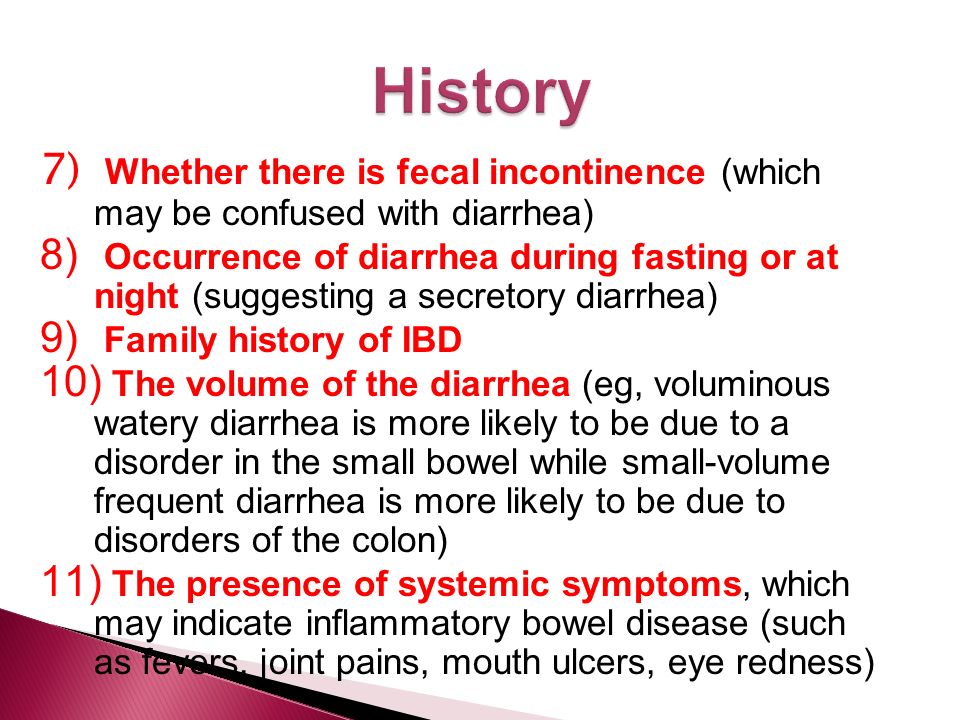 Chronic diarrhea that lasts for four weeks or more can be a sign of an underlying health issue. Meanwhile, if you also have a fever of 102 or higher, are experiencing severe pain, or think that you might be dehydrated, calling the doc is never a bad idea. (Kick-start your new, healthy routine with Women’s Health’s 12-Week Total-Body Transformation!)
Chronic diarrhea that lasts for four weeks or more can be a sign of an underlying health issue. Meanwhile, if you also have a fever of 102 or higher, are experiencing severe pain, or think that you might be dehydrated, calling the doc is never a bad idea. (Kick-start your new, healthy routine with Women’s Health’s 12-Week Total-Body Transformation!)
So, if you’re dealing with your own case of the big D, plug your nose and take a look into the toilet. What you see may be your key to getting out of the bathroom for a change.
Christine Frapech
Osmotic diarrhea happens when too much water is pulled into your bowels, creating watery No.3 (you wouldn’t call it poop either, if you saw it). “It usually indicates that something that you’ve taken in isn’t being absorbed,” Bedford says. Having a lactose intolerance is a common cause of osmotic diarrhea, as well as consumption of artificial sweeteners, he says.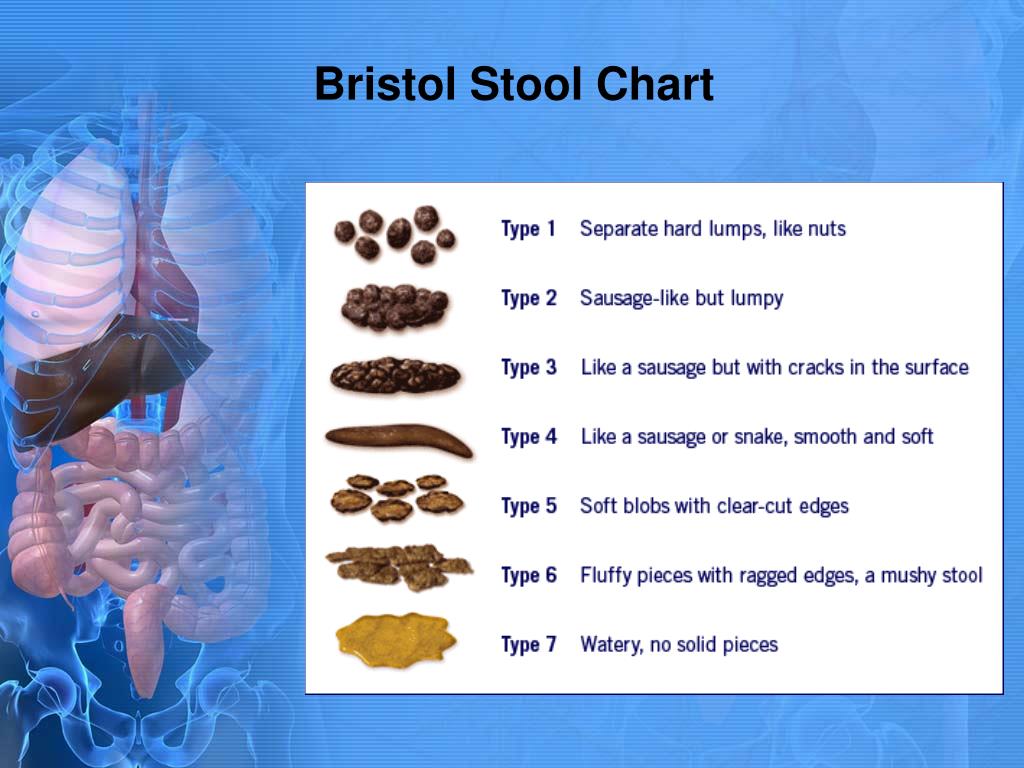 Avoiding dairy products or cutting back on sweeteners may help.
Avoiding dairy products or cutting back on sweeteners may help.
Related: 6 Signs You’ve Got A Serious Problem With Your Stomach
Christine Frapech
Secretory diarrhea looks a lot like osmotic diarrhea when you’re staring into the bowl. But if you’re avoiding the dairy and sugar that causes osmotic diarrhea, and you’re still experiencing diarrhea even when you don’t eat, it’s probably secretory.This form of diarrhea strikes when your intestines secrete electrolytes into your colon, which causes water to build up in your GI tract, says Scott Gabbard, M.D., a gastroenterologist at the Cleveland Clinic. A wide range of factors can cause this phenomenon, including an infection or, in rare cases, an endocrine problem, he says. If you’re experiencing secretory diarrhea, it’s time to call your doctor.
Find out what you MUST do the next time you go to the doctor:
Christine Frapech
If you have blood and pus in your stool, go to the doctor immediately.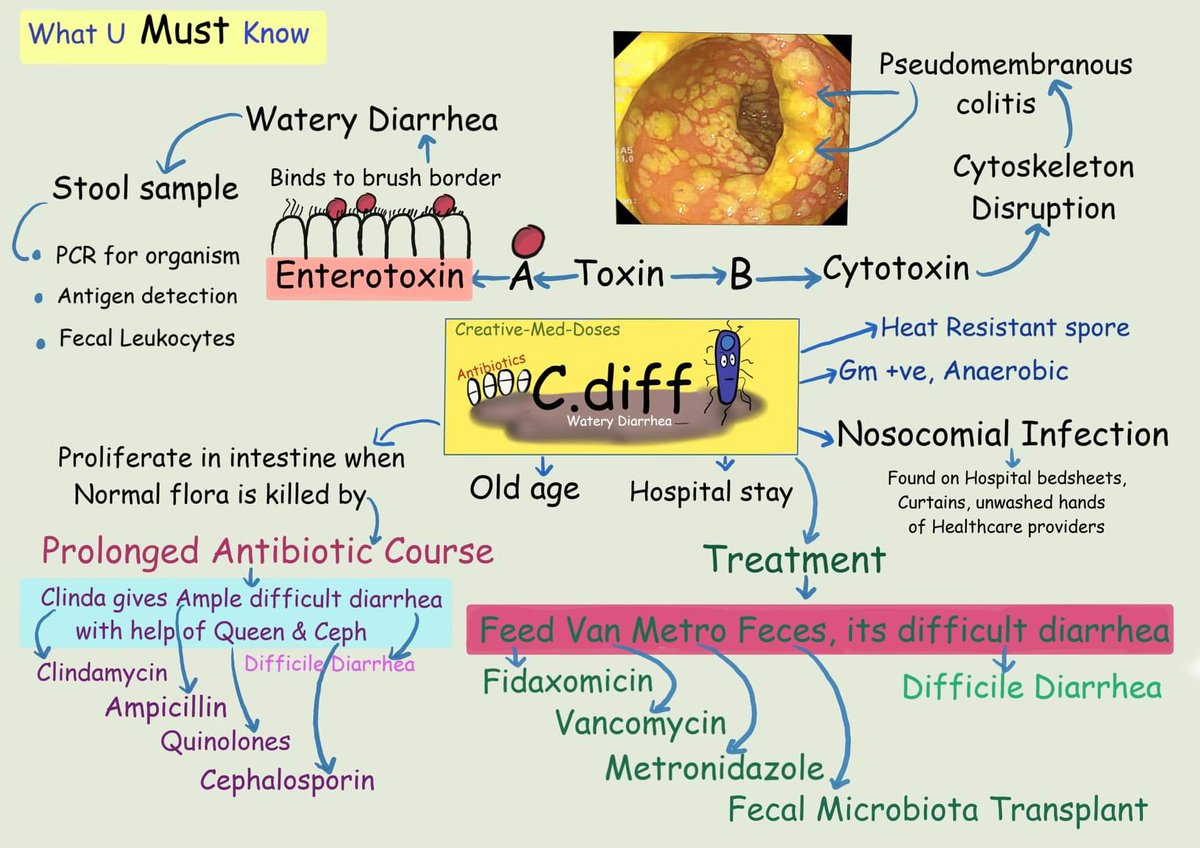 Exudative diarrhea is usually linked with inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis, Bedford says, although some infections such as E. coli can also cause it. Depending on the reason for your exudative diarrhea, steroid medications or immunosuppressants may be needed to help you feel better.
Exudative diarrhea is usually linked with inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis, Bedford says, although some infections such as E. coli can also cause it. Depending on the reason for your exudative diarrhea, steroid medications or immunosuppressants may be needed to help you feel better.
Related: 6 Warning Signs Of Stomach Cancer That Have Nothing To Do With Pain
Christine Frapech
Diarrhea is never fun, but paradoxical diarrhea is a double-whammy. This happens when people have severe constipation and liquid behind the backup gets around the poop and leaks out as diarrhea. “You literally can be constipated and put out liquid stool at the same time,” Bedford says. Relieving the constipation should help, he says—you just might need an enema to make it happen.
Related: 7 Yoga Poses to Help You Poop
Christine Frapech
If you’re having little bits of diarrhea more than three times per day, congrats! You have pseudodiarrhea. A common symptom of GI conditions such as irritable bowel syndrome, it can also occur because of constipation, just like paradoxical diarrhea, Bedford says. If adding more fiber to your diet or an enema doesn’t do anything, you’ll need to talk to your doctor about next steps.
A common symptom of GI conditions such as irritable bowel syndrome, it can also occur because of constipation, just like paradoxical diarrhea, Bedford says. If adding more fiber to your diet or an enema doesn’t do anything, you’ll need to talk to your doctor about next steps.
Korin Miller
Korin Miller is a freelance writer specializing in general wellness, sexual health and relationships, and lifestyle trends, with work appearing in Men’s Health, Women’s Health, Self, Glamour, and more.
This content is created and maintained by a third party, and imported onto this page to help users provide their email addresses. You may be able to find more information about this and similar content at piano.io
Evaluation of Chronic Diarrhea – American Family Physician
1. Fine KD,
Schiller LR.
AGA technical review on the evaluation and management of chronic diarrhea. Gastroenterology.
Gastroenterology.
1999;116(6):1464–1486….
2. Feldman M, Friedman LS, Sleisenger MH, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, and Management. 7th ed. Philadelphia, Pa.: Saunders; 2002: 137.
3. Schiller L, Sellin J. Diarrhea. In: Sleisenger MH, Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 9th ed. Philadelphia, Pa.: Saunders/Elsevier; 2010: 211–232.
4. Whitehead WE.
Diagnosing and managing fecal incontinence: if you don’t ask, they won’t tell. Gastroenterology.
2005;129(1):6.
5. Rodrigo L.
Celiac disease. World J Gastroenterol.
2006;12(41):6585–6593.
6. Nelson DA Jr.
Gluten-sensitive enteropathy (celiac disease): more common than you think. Am Fam Physician.
2002;66(12):2259–2266.
7. Phillips S,
Donaldson L,
Geisler K,
Pera A,
Kochar R.
Stool composition in factitial diarrhea: a 6-year experience with stool analysis. Ann Intern Med.
1995;123(2):97–100.
8. Bertomeu A,
Ros E,
Barragán V,
Sachje L,
Navarro S.
Chronic diarrhea with normal stool and colonic examinations: organic or functional? J Clin Gastroenterol.
1991;13(5):531–536.
9. Fernández-Bañares F,
Salas A,
Esteve M,
Espinós J,
Forné M,
Viver JM.
Collagenous and lymphocytic colitis: evaluation of clinical and histological features, response to treatment, and long-term follow-up. Am J Gastroenterol.
2003;98(2):340–347.
10. Schiller LR.
Chronic diarrhea. Gastroenterology.
2004;127(1):287–293.
11. Drossman DA, Dorn SD. Evaluation and management of chronic diarrhea: An algorithmic approach. http://www.medscape.org/viewarticle/513578_9 [login required]. Accessed July 14, 2011.
12. Manning AP,
Manning AP,
Thompson WG,
Heaton KW,
Morris AF.
Towards positive diagnosis of the irritable bowel. Br Med J.
1978;2(6138):653–654.
13. Conner BA. Persistent travelers’ diarrhea. In: Centers for Disease Control and Prevention. CDC Health Information for International Travel 2010. Atlanta, Ga.: U.S. Department of Health and Human Services, Public Health Service; 2009.
14. Longstreth GF,
Thompson WG,
Chey WD,
Houghton LA,
Mearin F,
Spiller RC.
Functional bowel disorders. Gastroenterology.
2006;130(5):1480–1491.
15. Cash BD,
Schoenfeld P,
Chey WD.
The utility of diagnostic tests in irritable bowel syndrome patients: a systematic review. Am J Gastroenterol.
2002;97(11):2812–2819.
16. Ford AC,
Chey WD,
Talley NJ,
Malhotra A,
Spiegel BM,
Moayyedi P.
Yield of diagnostic tests for celiac disease in individuals with symptoms suggestive of irritable bowel syndrome: systematic review and meta-analysis. Arch Intern Med.
Arch Intern Med.
2009;169(7):651–658.
17. Schoepfer AM,
Beglinger C,
Straumann A,
et al.
Fecal calprotectin correlates more closely with the Simple Endoscopic Score for Crohn’s disease (SES-CD) than CRP, blood leukocytes, and the CDAI. Am J Gastroenterol.
2010;105(1):162–169.
18. van Rheenen PF,
Van de Vijver E,
Fidler V.
Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis. BMJ.
2010;341:c3369.
19. Abdo AA,
Beck P.
Diagnosis and management of microscopic colitis. Can Fam Physician.
2003;49:1473–1478.
20. Levison DA,
Lazenby AJ,
Yardley JH.
Microscopic colitis cases revisited. Gastroenterology.
1993;105(5):1594–1596.
21. Riddell RH,
Tanaka M,
Mazzoleni G.
Non-steroidal anti-inflammatory drugs as a possible cause of collagenous colitis: a case-control study. Gut.
Gut.
1992;33(5):683–686.
22. Farrell R, Kelly C. Celiac disease and refractory celiac disease. In: Sleisenger MH, Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 9th ed. Philadelphia, Pa.: Saunders; 2010: 1797–1820.
23. Fasano A,
Berti I,
Gerarduzzi T,
et al.
Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med.
2003;163(3):286–292.
24. Haitha M, Pena A. Update in the diagnostic tools of celiac disease and its complications. In: Edwards MA. Celiac Disease: Etiology, Diagnosis, and Treatment. New York, NY: Nova Biomedical Books; 2009: 95–146.
25. Volta U,
Granito A,
Parisi C,
et al.
Deamidated gliadin peptide antibodies as a routine test for celiac disease: a prospective analysis. J Clin Gastroenterol.![]()
2010;44(3):186–190.
26. Osterholm MT,
MacDonald KL,
White KE,
et al.
An outbreak of a newly recognized chronic diarrhea syndrome associated with raw milk consumption. JAMA.
1986;256(4):484–490.
27. Hookman P,
Barkin JS.
Clostridium difficile associated infection, diarrhea and colitis. World J Gastroenterol.
2009;15(13):1554–1580.
28. Bartlett JG,
Perl TM.
The new Clostridium difficile—what does it mean? N Engl J Med.
2005;353(23):2503–2505.
29. Cunningham R,
Dale B,
Undy B,
Gaunt N.
Proton pump inhibitors as a risk factor for Clostridium difficile diarrhoea. J Hosp Infect.
2003;54(3):243–245.
90,000 Watery diarrhea – causes and treatment of watery diarrhea
Number of views: 269 638
Last update date: 08/26/2021
Average reading time: 5 minutes
Content: 8
9000 How is water absorption in the intestines
Causes of secretory diarrhea
What to do if diarrhea with water?
Diarrhea can have different causes, but is always accompanied by changes in intestinal absorption of water and electrolytes. And with secretory diarrhea, this process is not simply disrupted, but is replaced by active transport of electrolytes into the intestinal lumen and after them water. The osmolar pressure of intestinal contents becomes lower than the osmolar pressure of blood plasma. This supports the diffusion of water into the intestinal lumen and is fraught with rapid dehydration due to the development of water diarrhea. At the same time, the stool is liquid, abundant (more than 1 liter), defecation is painless, and fasting practically does not change the nature and quantity of bowel movements. If secretory diarrhea is accompanied by impaired absorption of bile acids or a decrease in the contractile function of the gallbladder, watery stools become bright yellow or greenish in color.This is called holographic diarrhea.
And with secretory diarrhea, this process is not simply disrupted, but is replaced by active transport of electrolytes into the intestinal lumen and after them water. The osmolar pressure of intestinal contents becomes lower than the osmolar pressure of blood plasma. This supports the diffusion of water into the intestinal lumen and is fraught with rapid dehydration due to the development of water diarrhea. At the same time, the stool is liquid, abundant (more than 1 liter), defecation is painless, and fasting practically does not change the nature and quantity of bowel movements. If secretory diarrhea is accompanied by impaired absorption of bile acids or a decrease in the contractile function of the gallbladder, watery stools become bright yellow or greenish in color.This is called holographic diarrhea.
How water is absorbed in the intestine
Every day a person consumes about 2 liters of water. It is found not only in drinks, but also in all foods eaten. In addition, liquid enters the lumen of the digestive tract as part of the digestive secretions.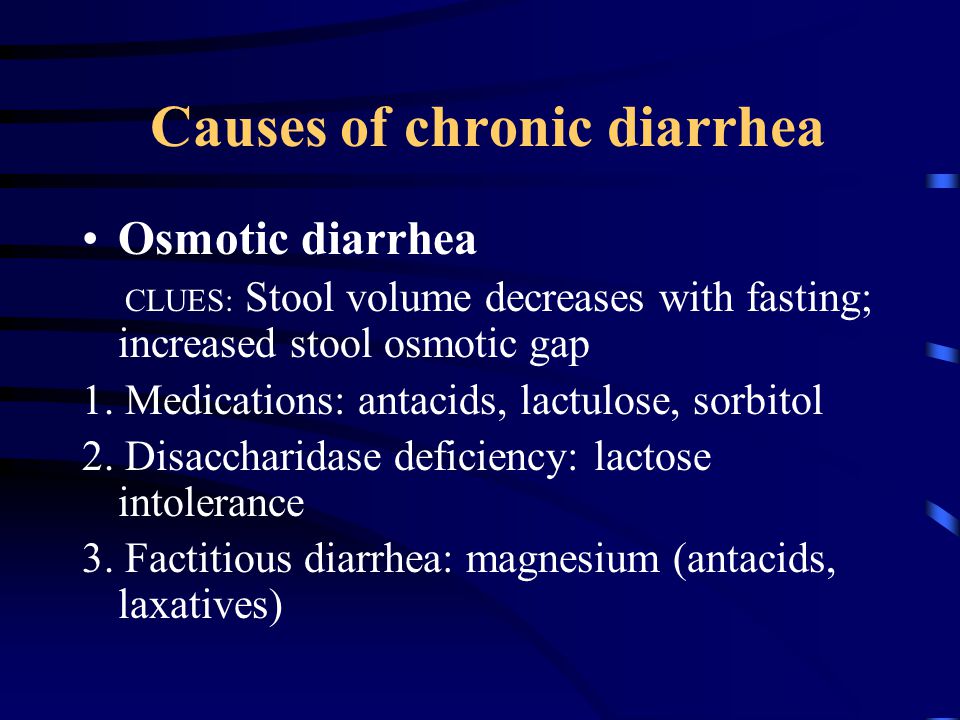 And about 7 liters of them are allocated per day! This includes 1.5 liters of saliva and pancreatic juice, 2.5 liters of gastric juice, half a liter of bile and a liter of intestinal secretions.In total, up to 9 liters of water daily enter the intestinal lumen, and only 100-200 ml (that is, about 2%) of this volume is excreted in the feces. The walls of the small intestine absorb up to 80% of all fluid, and 90% of the remaining amount is absorbed in the large intestine.
And about 7 liters of them are allocated per day! This includes 1.5 liters of saliva and pancreatic juice, 2.5 liters of gastric juice, half a liter of bile and a liter of intestinal secretions.In total, up to 9 liters of water daily enter the intestinal lumen, and only 100-200 ml (that is, about 2%) of this volume is excreted in the feces. The walls of the small intestine absorb up to 80% of all fluid, and 90% of the remaining amount is absorbed in the large intestine.
In this case, water is absorbed secondarily and passively, following the active transport of electrolytes through the walls of the digestive tract. Sodium ions play the most important role in this process, but potassium and chlorine also take an active part.All these electrolytes enter the intestines with food and digestive juices and are actively absorbed. In this case, the final absorption of water and absorption of up to 90% of sodium occurs in the large intestine. As a result, rather dense feces are normally formed here.
Causes of secretory diarrhea
Exogenous
- Medicines. Taking some medications leads to diarrhea with water. They increase the osmotic pressure inside the intestine or change the transport of ions in the intestinal wall.Watery diarrhea often occurs with laxatives, diuretics, asthma, and thyroid disorders. Drugs with cholinergic action have a great influence. These include some myasthenic, cardiotonic, and antihypertensive medications, as well as antidepressants and dementia medications.
- Toxins. Secretory diarrhea can occur against the background of poisoning with mushrooms, arsenic, organophosphorus compounds, insecticides, alcohol and a number of other drugs.
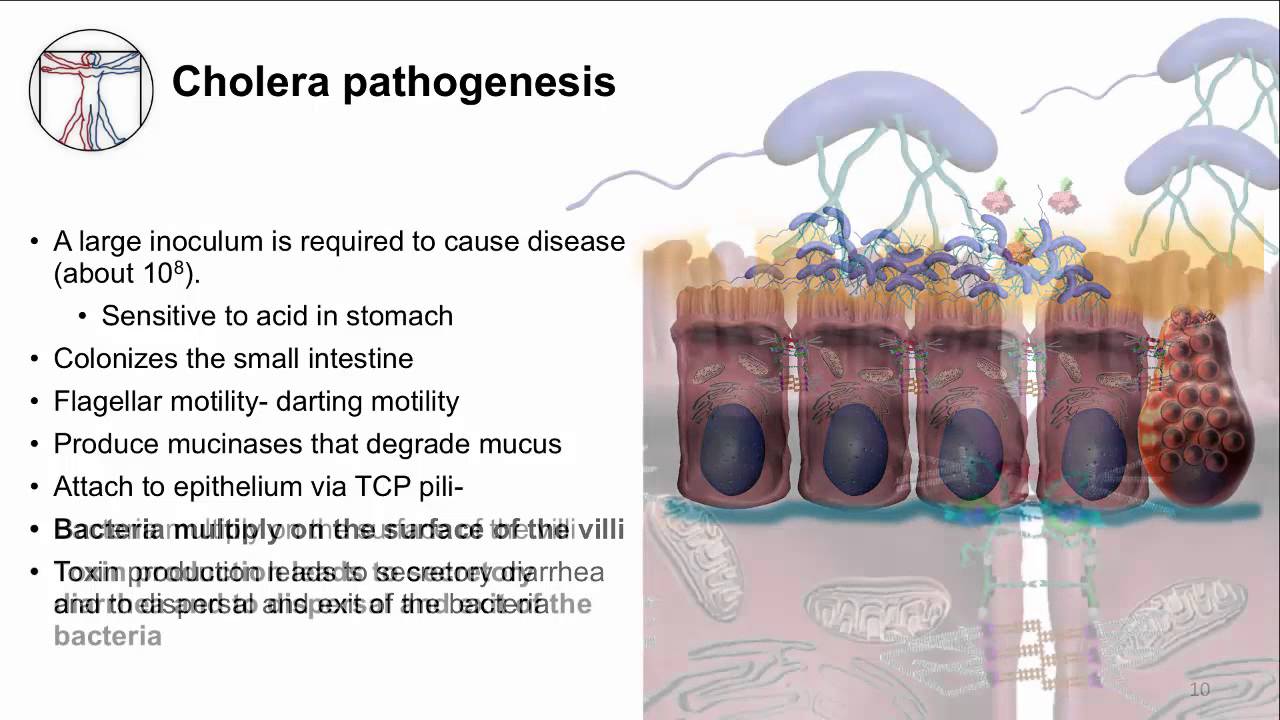
- Viral and bacterial infections . A number of infections cause liquid diarrhea with water due to exposure to the pathogens themselves and their toxins. These are cholera, yersiniosis, some strains of E. coli and staphylococci that produce enterotoxins.

Endogenous
- Hereditary diseases. There is a congenital secretory pathology (chloridorrhea, sodium diarrhea), the cause of which lies in the mutation of genes of transport proteins of the intestinal wall.The disease manifests itself in a child from birth.
- Hormone-producing tumors. Pathological secretion of ions and water in the intestine can be promoted by some tumors – medullary carcinoma of the thyroid gland, VIPoma, gastrinoma, mastocytoma and others.
- Bile salts. Entering the large intestine of unadsorbed bile acids and free long-chain fatty acids leads to the secretion of water into the intestinal lumen. The reason for this is the impaired absorption of bile acids in diseases (for example, in Crohn’s disease) or due to a decrease in the absorption area.This happens after resection of more than 100 cm of the ileum.
What to do if you have diarrhea with water?
Loperamide (active ingredient IMODIUM ® Express) binds to opiate receptors in the intestinal wall, inhibits the local production of acetylcholine, calmodulin and prostaglandins. Also, calcium channels are blocked, the permeability of plasma membranes decreases and the activity of intestinal motility decreases. As a result, the secretion of water into the intestinal lumen is significantly reduced, and its absorption is enhanced.Therefore IMODIUM ® Express can be used in the complex treatment of secretory diarrhea (diarrhea with water).
Also, calcium channels are blocked, the permeability of plasma membranes decreases and the activity of intestinal motility decreases. As a result, the secretion of water into the intestinal lumen is significantly reduced, and its absorption is enhanced.Therefore IMODIUM ® Express can be used in the complex treatment of secretory diarrhea (diarrhea with water).
The information in this article is for guidance only and does not replace the professional advice of a physician. Consult a qualified professional for diagnosis and treatment.
“Imodium is contraindicated for use in children under 6 years of age.”
Read also:
Watery diarrhea – causes, diagnosis and treatment
Watery diarrhea is repeated (up to 15-20 times a day) defecation, which is accompanied by the release of loose loose stools.Usually the symptom is combined with other dyspeptic disorders: vomiting, cramps, abdominal pain. Diarrhea with water is most often associated with intestinal infections, but can be observed with non-infectious bowel pathologies, enzyme deficiency. To establish the causes of diarrhea, ultrasound, radiography, endoscopy, laboratory tests are used. To stop diarrhea, adsorbents, coatings and astringents are used.
Diarrhea with water is most often associated with intestinal infections, but can be observed with non-infectious bowel pathologies, enzyme deficiency. To establish the causes of diarrhea, ultrasound, radiography, endoscopy, laboratory tests are used. To stop diarrhea, adsorbents, coatings and astringents are used.
Causes of watery diarrhea
Water bowel movements often indicate infectious or non-infectious intestinal diseases.Sometimes pregnant women complain about the appearance of liquid unformed feces, which is caused by gestational changes in the digestive and endocrine systems. In children, watery stools can be a sign of a toxic form of dyspepsia or the initial stage of colitis. Diarrhea with water with dyspeptic disorders, weakness, hemorrhages is characteristic of alimentary-toxic aleukia. Profuse diarrhea occurs in 90% of patients with toxic shock.
Bacterial infections
Ingestion of pathogenic intestinal microflora is usually accompanied by secretory watery diarrhea.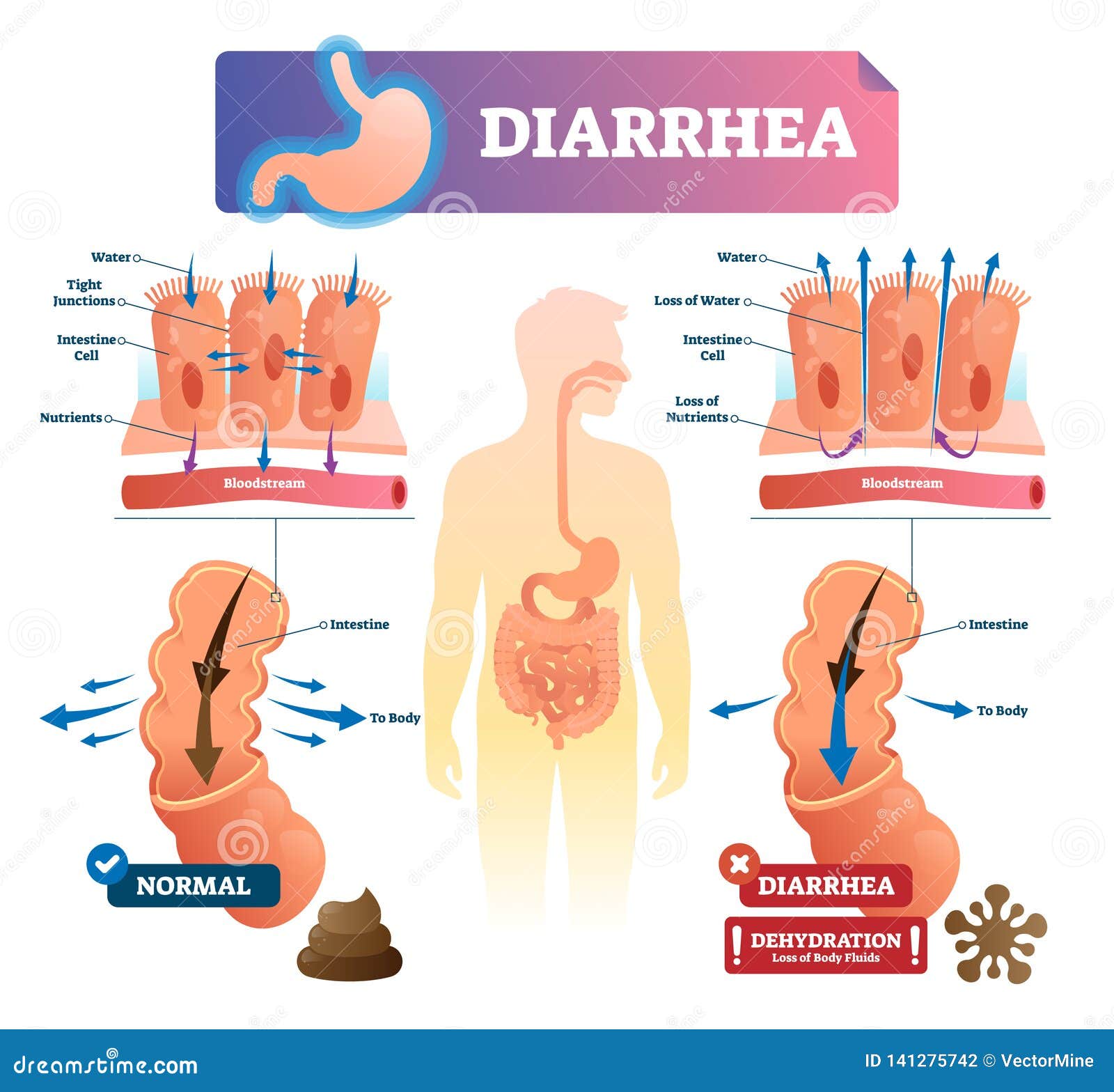 Bacteria are able to secrete a specific enterotoxin that affects the epithelial cells of the mucous membrane and causes the accumulation of adenylate cyclase, cAMP. This contributes to an increased release of ions into the intestinal lumen, followed by a large amount of fluid entering the intestine along the concentration gradient. The condition is aggravated by concomitant inflammatory lesions of the gastrointestinal tract. The following intestinal infections lead to diarrhea with water:
Bacteria are able to secrete a specific enterotoxin that affects the epithelial cells of the mucous membrane and causes the accumulation of adenylate cyclase, cAMP. This contributes to an increased release of ions into the intestinal lumen, followed by a large amount of fluid entering the intestine along the concentration gradient. The condition is aggravated by concomitant inflammatory lesions of the gastrointestinal tract. The following intestinal infections lead to diarrhea with water:
- Cholera . This infectious disease is manifested by diarrhea, which quickly loses fecal character and odor, becoming watery.Several hours later, repeated vomiting joins, which aggravates the condition, provoking severe dehydration. A distinctive feature is the complete absence of abdominal pain or moderate discomfort, detected in no more than 30% of patients.
- Escherichiosis . Watery diarrhea often develops when infected with enterotoxigenic strains of the microbe, when the disease proceeds as a mild variant of cholera.
 In young children, water-borne diarrhea is usually caused by enteropathogenic strains.Diarrhea is combined with vomiting, pain in the epigastrium, along the intestines. An increase in body temperature to subfebrile numbers is possible. General condition of patients of moderate severity.
In young children, water-borne diarrhea is usually caused by enteropathogenic strains.Diarrhea is combined with vomiting, pain in the epigastrium, along the intestines. An increase in body temperature to subfebrile numbers is possible. General condition of patients of moderate severity. - Salmonellosis . Dyspeptic disorders are the main manifestations of the gastrointestinal form of infection. The first symptoms of salmonellosis are general intoxication and headache, after a few hours there are severe cramping pains in the intestines, profuse bowel movements, first with the release of unformed feces, and then water with food particles, mucus.Greenish frothy stools (“swamp mud”) are characteristic.
- Botulism . With the gastroenterological variant of the infection, dyspeptic symptoms come to the fore: watery diarrhea, repeated vomiting, spastic abdominal pain. Patients complain of dry mouth, sensation of a lump in the throat. For botulism, eye manifestations are characteristic: double vision, flashing “flies” before the eyes, blurred vision.
 In severe cases, there are paresis, paralysis of facial muscles with facial asymmetry.
In severe cases, there are paresis, paralysis of facial muscles with facial asymmetry. - Campylobacteriosis . The disease begins acutely with a rise in temperature to 38 ° C or more, pain in muscles and joints. Multiple diarrhea immediately joins with the release of liquid fetid feces, in which streaks of mucus and blood are revealed. Patients often complain of abdominal cramps, while nausea and vomiting occur in only a quarter of campylobacteriosis patients.
Viral infections
Dyspeptic disorders, in particular watery diarrhea, are considered the main manifestations of most viral intestinal lesions.When viruses enter the gastrointestinal tract, they multiply inside the epithelial cells, causing their death and desquamation from the mucosal surface, which leads to disruption of parietal digestion, diarrhea. Pathogens also slow down the processes of reabsorption of water from the intestinal lumen, which causes profuse diarrhea. The most common viral diseases involving the intestines:
- Rotavirus gastroenteritis . Watery stools are the main manifestation of rotavirus infection.With a mild variant, the frequency of defecation is up to 10 times per day, the bowel movements are fecal in nature, with a severe course, profuse diarrhea with the discharge of a cloudy, fetid yellow-green fluid is the leading one. Diarrhea is combined with cramping pain in the umbilical region, subfebrile fever.
- Norovirus infection . Norovirus is characterized by simultaneous damage to the respiratory and digestive systems. The disease begins with a sore throat, nasal congestion, then dyspepsia joins – watery feces, vomiting, abdominal pain.Repeated bowel movements with the release of a large volume of fluid becomes a prerequisite for severe dehydration, which is manifested by dry skin, mucous membranes, decreased blood pressure, oliguria.
- Hong Kong Flu . With this type of influenza infection, symptoms from the gastrointestinal tract are combined with signs of damage to the respiratory system, general intoxication of the body. Along with headache, high fever, repeated diarrhea with water, moderate pain in the abdomen, nausea, and lack of appetite are noted.Respiratory manifestations (dry cough, sore throat, nasal congestion) occur on day 2-3 of the illness.
- Hemorrhagic fever Marburg. The disease manifests itself acutely with the onset of headache, myalgia, conjunctivitis, erosions on the oral mucosa. Dyspeptic disorders in the form of watery diarrhea, vomiting, severe pain in the abdominal cavity develop on the 3-4th day of hemorrhagic fever. Pathognomonic signs – maculopapular rash, uterine, nose and gastrointestinal bleeding, appearing on 5-6 days of illness.
- HIV infection . AIDS is characterized by abundant watery stools without pathological inclusions, caused by digestive disorders and the addition of a secondary infection against the background of severe immunodeficiency. In addition to loose stools, other nonspecific symptoms are determined – prolonged low-grade fever, increased sweating at night. Most patients lose more than 10% of their body weight.
Protozoal and helminthic invasions
Helminths and protozoa have a direct pathogenic effect on the enterocytes of the mucous membrane, causing severe disturbances in the digestion and absorption of food components.Severe malabsorption syndrome in combination with increased secretion of water and electrolytes into the intestinal cavity provokes profuse diarrhea. With insufficient replacement of fluid losses, dehydration syndrome of varying severity develops. Watery diarrhea is noted with invasions such as:
- Cryptosporidiosis . Protozoa parasitize in the lumen of the small intestine, potentiating malabsorption and inhibition of the activity of digestive enzymes, as a result of which a watery stool with a fetid odor appears.Diarrhea is accompanied by severe abdominal cramps, nausea, and vomiting. The disease more often affects people with immunodeficiencies. In such cases, there is a long course (up to 4 months) with severe dehydration.
- Strongyloidiasis . Intestinal manifestations are noted in the second phase of the disease, after 2-3 weeks from the onset of the first symptoms – urticaria, rashes and arthralgia. The development of diarrhea is associated with inflammatory lesions of the small intestinal mucosa, the formation of hemorrhages, erosions.In addition to diarrhea, the appearance of pain in the epigastric region, nausea, and vomiting is typical. Sometimes there is jaundice of the skin, pain in the right hypochondrium.
Non-communicable bowel diseases
Watery diarrhea often complicates the course of organic diseases of the digestive tract, especially in the initial stages. The increase in the volume of feces is due to both disturbances in the processes of parietal and cavity digestion, and the effect of various inflammatory mediators.Diarrhea is associated with disorders of intestinal motility in a hyperkinetic or hypokinetic type. With a change in the frequency and consistency of stools, the following non-infectious pathologies of the gastrointestinal tract occur:
- Enteritis . Watery diarrhea is a symptom of non-infectious inflammation of the small intestine that is allergic, medicinal, or autoimmune. The appearance of thin, fetid feces is mainly caused by the syndromes of malabsorption and maldigestion. The chair is observed up to 10-15 times during the day, accompanied by flatulence, rumbling in the abdomen, decreased appetite, nausea, significant loss of body weight.
- Enteropathy . Chronic watery diarrhea occurs with non-inflammatory intestinal pathologies. A change in the consistency of feces can be caused by both fermentopathies and impaired gastrointestinal motility (for example, a hypomotor variant of diabetic enteropathy). The pain syndrome is poorly expressed, digestive disorders prevail, contributing to weight loss, protein-energy malnutrition.
- Acute colitis .Colitis is characterized by spasms in the left iliac region, painful urge to defecate, the presence of pathological impurities of mucus, blood in the stool. The stool at first has a fecal character, a fetid odor, as the disease progresses, it becomes watery. The frequency of bowel movements reaches 25 times a day. Similar changes are observed in pseudomembranous colitis with exudative enteropathy.
Enzyme deficiency
In the absence of enzymes in the initial sections of the small intestine, the appearance of profuse diarrhea with water is associated with an osmotic mechanism.The presence of a large number of undigested large molecules, especially disaccharides and peptones, is a prerequisite for an increase in pressure in the intestinal lumen, the release of fluid and sodium ions. Diarrhea occurs with fibrosis of the pancreas and a decrease in its exocrine function by 80-90%, as a result of which the digestion of all types of food is impaired. The condition is aggravated by the addition of a secretory mechanism of diarrhea associated with the activation of cAMP.
Watery stools are possible with gastrinoma, Zollinger-Ellison syndrome.Increased secretion of gastrin and hydrochloric acid leads to the destruction of digestive enzymes, an increase in the osmolarity of the chyme. Diarrhea is combined with intense epigastric pain, sour belching. In children, water excretion is a consequence of galactosemia – milk intolerance due to a congenital absence of an enzyme. The symptom appears immediately after the start of breastfeeding, accompanied by malnutrition, jaundice, suppression of reflexes.
Survey
Watery diarrhea always indicates a problem with the digestive system.Examination of patients with complaints of watery diarrhea is carried out by a gastroenterologist or infectious disease specialist. To verify the clinical diagnosis, a comprehensive examination of the gastrointestinal tract is necessary using laboratory and instrumental methods to detect morphological changes, to establish the cause of diarrhea. The most valuable in terms of diagnostics are:
- Radiography . With the help of plain radiography of the abdominal cavity, the condition of the patient’s gastrointestinal tract is quickly assessed.For a detailed study of the inner surface of the digestive tract, oral contrasting with barium sulfate is used. The method is quite informative in detecting non-infectious processes that cause watery stools.
- Ultrasonic examination Investigation. A non-invasive examination method is used as a screening diagnosis to exclude severe organic diseases of the digestive system, neoplasms. Ultrasound of the abdominal cavity can reveal signs of an inflammatory process.Sonography is also done to assess the condition of the pancreas.
- Stool analysis . To study the processes of digestion, absorption of food, a microscopic examination of feces with measurement of pH is carried out. Watery diarrhea is often caused by infectious processes, therefore, all patients undergo bacteriological culture of feces, analysis for helminth eggs. To exclude ulcerative-destructive processes, the Gregersen reaction is shown.
- Serological tests .The search for antimicrobial antibodies or specific antigens in the blood is the most accurate way to identify various infectious diseases, especially of a viral nature. The study is not informative enough in the first few days after the onset of the disease, when the concentration of antibodies has not yet increased in the blood.
As an additional general clinical method, a biochemical blood test is used to help determine the degree of malabsorption and protein deficiency.If specific lesions of the gastrointestinal tract are suspected, endoscopic examination with biopsy is recommended. To assess the exocrine function of the pancreas, a blood test for amylase, lipase is sometimes prescribed.
Adsorbents are used to reduce the frequency of watery diarrhea
Symptomatic therapy
Diet correction required. In case of an acute disorder, a starvation diet is shown with the gradual introduction of rice dishes, products containing pectins, salted soups, broths, dietary protein foods (veal, turkey, chicken, hard-boiled eggs).With diarrhea, a significant amount of fluid is lost in water, therefore, if the patient is in a satisfactory condition, it is important to provide plenty of fluids to prevent severe dehydration.
Adsorbents, astringents and coating agents are used to reduce the incidence of watery diarrhea until the exact cause of stool disturbances is established. In no case should you take medications that inhibit intestinal peristalsis, as this can increase intoxication and lead to a deterioration in the patient’s condition.Antibacterial agents and antidiarrheal drugs are selected only by a doctor, taking into account the results of the examination, the sensitivity of pathogenic microorganisms.
90,000 Infections. Intestinal infections. Rotavirus. Children’s health
If an adult or a child has diarrhea, do not grab onto antibiotics right away. After all, intestinal infections are viral and bacterial, and antibiotics are needed only in the second case, and with viral diarrhea, this is just a futile blow to an already weakened body.Therefore, you first need to pass tests and figure out the origin of the infection.
As a rule, the fact that the infection is viral (it can be caused by adeno-, rota- and enteroviruses) can be indicated by a sudden and abrupt onset of the disease, when a high temperature rises quickly, vomiting and loose stools begin. Usually, such diseases do not last long (3 days) and go away on their own, without treatment. All that the patient needs is just an abundance of fluid, rest, diet and intake of enterosorbents. But bacterial infections usually develop gradually, last longer and more severely, and antibiotics are already needed to treat them.
This is not a trifle
However, do not be too lighthearted about viral intestinal infections. They are especially dangerous for the elderly with cardiovascular problems, as well as for children under 5 years of age. Their frequent diarrhea can cause rapid dehydration, which can lead to dysfunction of the heart muscle and a high risk of death. Therefore, if there are more than 10 episodes of diarrhea per day or loose stools are accompanied by a high temperature (above 38.5 degrees), it is better to immediately call an ambulance.After all, diarrhea is the second leading cause of death in children after pneumonia
The most common cause of diarrhea in babies under three years old is rotavirus infection. Despite the existence of a vaccine against this disease, according to the WHO, more than half a million babies die from it worldwide every year. Rotavirus vaccination is not included in many national calendars and only parents who are aware of the dangers of rotavirus infection vaccinate children. This contagious infectious disease mainly affects the stomach and intestines of the patient.As a rule, rotavirus infection (as with any viral diarrhea) is characterized by an acute onset. Usually, against the background of normal health, there is a sharp jump in temperature, other signs of SARS appear (runny nose and sore throat). Then there are gastrointestinal manifestations: nausea, vomiting, liquid watery abundant stools without admixture of blood.
How can you get infected?
It is easy to catch rotavirus, since this causative agent of the disease is found almost everywhere and is resistant to environmental conditions, therefore it spreads at a high speed.In addition, the immunity to this disease is not very stable (the vaccine protects against a severe form for several years), so you can get sick with it many times throughout your life. There are several ways of transmission of the virus: this is contact-household (through unwashed hands or contaminated objects), and airborne.
By the way, rotavirus infection can be contracted not only from a sick person, but also from a virus carrier. As a rule, adults with strong immunity transmit rotavirus without realizing it, since they do not have any corresponding symptoms.But for others, nevertheless, they pose a great danger. So often children become infected with this infection not from their peers in children’s groups, but from their own mothers and fathers.
Why analyzes are needed
It is almost impossible to find out without tests whether viruses or bacteria have caused diarrhea, so it is better to consult a doctor, especially if on the third day of the disease the patient does not become easier. But in the case when the child is sick, of course, one cannot wait for three days.The doctor may prescribe broad-spectrum antibiotics, and if they turn out to be ineffective, he will recommend taking a bacterial culture of feces to determine the sensitivity of microbes to the antibiotic. This will help you choose the right drug.
If you suspect a viral nature of diarrhea, blood tests should be taken to determine the RNA of rotavirus. By the way, among 7 groups of rotaviruses, the most common causative agent is group A rotavirus (occurs in 90% of cases). The genetic material of this virus can also be detected in feces (by PCR-polymerase chain reaction).Stool analysis for rotavirus can confirm the diagnosis of rotavirus infection.
For the choice of therapy, these studies are not relevant, since the treatment of viral diarrhea is symptomatic, and besides, by the time the analysis is ready (after 3 days), the disease most often resolves itself. But research will help identify the cause of diarrhea in children and adults. In addition, if you suspect rotavirus, it will not hurt to pass tests to all family members in which a small child grows up, since adults can be carriers of the disease, which is extremely dangerous for children under 3 years of age.Finally, tests for rotavirus infection are needed to examine contacts in kindergartens and schools in order to detect the virus early and start treatment on time.
If there is a suspicion of a viral or bacterial intestinal infection, but it is not clear what kind of infection causes the symptoms, an OCI test will be the optimal study. This test allows for the analysis of feces to determine the presence of rota-, noro- and adenoviruses, as well as bacteria – salmonella and shigella (causative agents of salmonellosis and dysentery).
Share article:
Still have questions?
90,000 Rotavirus in a child
Rotavirus infection is an acute infectious disease, belongs to the group of acute viral intestinal infections, is more dangerous for an early age of a child due to the risk of rapid dehydration, otherwise called “dirty hands” infection
How does the infection take place?
Rotavirus infection is highly contagious.It is transmitted by the fecal-oral route, most often it happens in kindergarten, a little less often at school, because children do not communicate as closely as in preschool institutions, there is no joint daytime sleep and common toys. The probability of the disease approaches 100% if a family member brings the infection into the house.
Rotavirus signs:
Increased body temperature
Vomit
Watery diarrhea
Abdominal pain
Lethargy
Decreased appetite
Runny nose
These symptoms appear 1-2 days after infection and usually persist for 3-5 days.
Signs of dehydration in a child:
Increased thirst
dry mucous membranes
decreased amount of urine (babies have less urine in diapers than usual)
almost complete absence of tears
weight loss
long (more than 2 seconds) straightening of the skin fold, if you squeeze the skin with two fingers on the baby’s belly
The body loses a lot of fluid and mineral salts, the child becomes moody and irritable, the heart can start beating faster, breathing becomes faster.If dehydration continues, the kidneys will stop working and the heart will not get enough fluid. Blood pressure will begin to drop and the child may develop shock.
How and how to treat rotavirus infection?
First of all, it is necessary to replenish the volume of the lost liquid (warm boiled water). But ordinary water is not very effective, since during vomiting and diarrhea, electrolytes are lost, which must be restored with the help of rehydron, glucosalan, gastrolite (available in a pharmacy without a prescription), if it is not at hand, you can make it yourself with sugar (20 g) , salt (3 g) and baking soda (3 g).It should be remembered that it is better to use this solution only for a short time, before purchasing medications, since it lacks a number of important trace elements.
At a temperature, give an antipyretic
In case of vomiting, give a drink in small portions (fractional drinking from a teaspoon)
In severe cases of dehydration, intravenous fluids may be required – in the hospital.
What to do with diarrhea?
Children should only be given antidiarrheal medication as directed by your pediatrician.
Never give your child imodium (loperamide), this can lead to increased absorption of toxic substances in the intestines and the development of toxic shock!
Should breastfeeding be discontinued?
If a child is breastfed, you do not need to deny him this, but on the contrary, you should feed him more often so that he receives the required amount of liquid, while artificially feeding, you should also not deny the child a formula.
Diet of a child with rotavirus
It is worth giving up dairy products, since the injured mucous membrane is not able to digest proteins of cow or goat origin (does not apply to breast milk and formula)
Exclude raw vegetables, fruits, dried fruits, black bread, white bread, buns from the diet.
It is worth offering the child food with an “antidiarrheal” effect (rice, pasta, fresh dryers); the dishes should be boiled or steamed.
Effective treatment of diarrhea | Clinic of Chinese medicine TAO
Diarrhea is a pathological condition characterized by the presence of abundant watery stools, increased urge to defecate.
Read completely
Diarrhea
Causes of diarrhea
Most often, diarrhea is one of the signs of food poisoning or the development of gastroenteritis.The infectious nature of the disease is accompanied by loose stools for several hours to several days. Poor food preparation hygiene, drinking contaminated water, and irregular hand washing are the most common causes of diarrhea. In addition, the symptom may occur after contact with a patient suffering from an infectious disease. A prolonged course of diarrhea may be associated with chronic intestinal inflammation – ulcerative colitis, Crohn’s disease, lactose intolerance.Chronic diarrhea is characteristic of infection with giardiasis and amebiasis.
The theoretical foundations of Chinese medicine assume that the spleen is responsible for the absorption of nutrients and their further transportation. After the food is digested, the nutrient substance extracted from it (shui-gu yin-wei) enters the spleen and rises up to the heart, blood vessels and further to the lungs, spreads throughout the body to nourish dense and hollow organs. When the spleen is working normally, Chinese medicine speaks of “healthy transportation” (jian-yun).If the qi of the spleen is normal, then the assimilation and transport of the nutrient are normal. In the opposite situation, both converting and transporting functions are violated. The patient is observed flatulence, diarrhea, fatigue, weight loss.
Clinical signs
Acute diarrhea that comes on suddenly, in most cases resolves within one to two days.In addition to loose stools, patients have general weakness, dehydration, headache, and abdominal pain. Diarrhea, lasting more than 3-4 days, requires a mandatory visit to a doctor in order to exclude the infectious nature of the disease. Chronic diarrhea lasts a month or more, and the presence of blood in the feces is the need for diagnostic procedures in order to exclude tumors, ulcerative colitis and other diseases.
Attention should also be paid to irritable bowel syndrome with a predominance of diarrhea.It is characterized by the presence of watery feces in a quarter of cases of bowel movement, in the rest, the stool remains normal, as well as pain in the lower third of the abdomen, somewhat calming down after a bowel movement.
Osmotic diarrhea occurs as a result of the accumulation of substances in the intestinal lumen that stimulate additional fluid release into the intestine. In this case, the stool is predominantly liquid, less often – mushy, occurring with a frequency of 2-4 times a day, more often after a meal.
Diarrhea treatment
For the treatment of diarrhea in most domestic clinics, patients are offered antibacterial drugs, after taking which a long period of restoration of the intestinal microflora is required, also involving the use of drugs.
In the clinic of Chinese medicine “TAO” each patient draws up an individual scheme for the complex treatment of diarrhea in adults and children. Herbal remedies based on Chinese herbs provide an anti-inflammatory effect, normalize the functions of the digestive system and metabolism, and create conditions for the restoration of normal intestinal microflora. It is important that these drugs have no side effects, they are effective and safe. Acupuncture, acupressure, moxibustion at the level of biologically active points of the patient’s body harmonize energy, restore the function of the meridians of the stomach, spleen, liver and intestines, and normalize the function of intestinal motility.Thus, the influence is, first of all, on the cause of the disease, which allows not only to relieve the patient of a specific symptom, but also to tune his body to restore the energy balance, prevent exacerbations and comprehensive recovery of the patient.
Viral diarrhea
Causes of viral diarrhea. The fact that viruses can cause diarrhea began to be discussed back in the thirties of the last century on the basis of descriptions of outbreaks of diarrhea among children, it was suggested that diarrhea is caused by viruses, and these diarrhea began to be called “intestinal flu”, “epidemic diarrhea “, viral dysentery or winter diarrhea.To date, enough data has been accumulated that viruses can provoke diarrhea and digestive disorders in children and adults. Enterovirus, rotavirus and reoviral etiology of the disease is considered today as the cause of the development of viral diarrhea. Viral diarrhea is widespread throughout the world, up to millions of children and adults are ill with them every year, they can occur both single cases and epidemic outbreaks, mainly among young children or among closed organized groups. Features of viruses One of the most characteristic features of viruses that can cause digestive damage and diarrhea is their relative stability in the external environment, as well as their good ability to preserve at low temperatures of water and air. They survive at 20 ° C water for more than 2 weeks, and at 10 ° C – up to several months. Many viruses are indifferent to the acidic environment of the stomach, they calmly pass it without collapsing., Viruses persist in open reservoirs and reservoirs, seas and rivers, and from there they can enter sources of drinking water supply.Also, viruses are excreted from the body of the infected with feces, where they persist for a long time, and can pollute the environment and water of reservoirs. How can you get infected? – sources of infection for any viral diarrhea can be people who are sick, or recovering, shedding viruses into the environment, or carriers of the virus who are not sick themselves, but shedding viruses. With some of the viral diarrhea, the transmission of infection from pets and cattle can become an actual route of infection, such viruses, depending on the method of entry into the body, can give different symptoms – with airborne infection – a clinic for a cold infection with respiratory damage, and with ingestion by the fecal-oral route – damage to the digestive system.The source of viruses in viral diarrhea can be food and water contaminated with viruses, things and toys of children that they put into their mouths, rotaviruses can be isolated from tap water that children have not boiled or drank.
The gates for diarrheal viral infections are the oral cavity and gastrointestinal tract.
The mechanism of development of viral diarrhea – viruses enter the epithelium in the upper respiratory tract, and are swallowed with saliva, penetrating the stomach and intestines.There, the cells of the epithelium of the stomach and intestines are damaged, and viruses begin to multiply on the epithelium of enterocytes, intestinal cells, they penetrate into the blood, causing manifestations of general toxicosis and fever, and can affect individual organs and systems – the nervous, pulmonary, liver. The ideal conditions for the multiplication of intestinal viruses are the duodenum and small intestine, the formation of profuse and frequent diarrhea occurs. The absorption of water by cells is impaired, a fermentation reaction occurs due to problems with the breakdown of food, this gives the complex symptoms of diarrhea (diarrhea profuse, watery, without blood and greens).
The manifestation of viral diarrhea depends on which virus and at what age causes the diarrhea. With enteroviral diarrhea, children under 2 years of age are affected, there can be both diarrhea and its combination with muscle damage, meningitis, sore throat or myocarditis. Isolated forms of enterovirus give mild, not prolonged diarrhea, pass on their own. Only enteroviruses with diarrheal syndrome in newborns and weakened children are dangerous. With diarrhea caused by the Coxsackie virus, there may be a different clinical picture, depending on the age of the child (mild diarrhea in children from 2 to 5 years old with practically no fever and toxicosis, with paroxysmal abdominal pain and loose stools up to 3-10 times a day without impurities) …After 1-2 days, the condition will return to normal.
Sometimes the disease proceeds with fever, colds, abdominal pain, loose stools and repeated vomiting, a state with fever lasts up to 3 days, and diarrhea for the first 2-3 days. Coxsackie viruses are severe in the first 2 years of life, treatment only in a hospital. Viral lesions of the ECHO-etiology occur at any age, are not severe, usually manifesting themselves in the form of gastritis and enteritis, while intestinal dysfunctions are insignificant and not long-term (nausea, vomiting, increased stool frequency within 1-2 days, impaired appetite, low temperature , stool liquefied, without impurities, 5-6 times a day).In infancy or in children during the neonatal period, viral diseases can be difficult, but they usually begin as colds, and intestinal symptoms occur later (repeated regurgitation, vomiting, bloating, loose stools). Due to the loss of fluid, toxicosis develops with exicosis, dehydration, and the severity of the condition increases.
Respiratory infections with intestinal syndrome
Intestinal disorders can be one of the symptoms of acute respiratory viral infections, initially starting as the common cold.Intestinal disorders in them arise as a result of toxic effects on the intestine, enzyme disorders, the addition of microbial flora against the background of a weakened immunity, the formation of dysbiosis. In such cases, as such, viral diarrhea can no longer exist, but they say about ARVI with intestinal manifestations.
A feature of viral diarrhea is an intestinal disorder in which the small intestine is involved in the lesion process, the course proceeds as gastroenteritis or enteritis (with or without vomiting).With viral diarrhea in the blood of children – lymphocytosis and leukopenia, there is no pronounced inflammation of the walls of the intestine (colon), diarrhea occurs without impurities (mucus, blood, greens, there are no leukocytes and erythrocytes in the coprogram). Stools with particles of undigested food, oily from pancreatic problems, copious. Viral diarrhea does not last long, does not give a severe course and microbial imbalance. Rotavirus diarrhea m. rather severe (in early childhood), therefore, today, active methods of prevention and the development of vaccines are being developed in relation to viral diarrhea.
Author: ch. m / s Striga T.V.
Diseases of dirty hands. How to keep your child safe from summer infections?
Diseases of Dirty Hands.
How to keep your child safe from summer infections?
Along with the summer, “diseases of dirty hands” are replacing “autumn-winter” diseases. Jaundice, dysentery, giardiasis or rotavirus – a child can easily catch any of these “sores” without washing his hands after a walk, eating a dirty apple or eating berries right from a bush in the country.The payback for such carelessness comes very quickly in the form of vomiting, diarrhea and abdominal pain. Why are intestinal infections dangerous, what to do with them and can they be prevented?
The symptoms of dirty hands are so similar that any such ailment can easily be mistaken for food poisoning. Common manifestations of intestinal infections are loose stools, nausea, vomiting, abdominal pain, fever, lethargy, weakness, lack of appetite, and weight loss. Diseases are caused by a variety of bacteria (dysentery bacillus, salmonella, staphylococcus, typhoid fever) and viruses.Reproducing in the intestine, both of them lead to disturbances in the digestion process and inflammation of the cells of the intestinal mucosa. That is why the typical and most characteristic consequence of these processes is diarrhea – the main symptom of any intestinal infection. The duration of the latent incubation period of diseases ranges from several hours to seven days, and full recovery can take as long as a week or several months. One of the barriers to intestinal infections is a high immune defense factor.Therefore, children with reduced immunity are in a special risk zone.
Hepatitis A
One of the most common intestinal infections. Sources of infection: dirty hands, poorly washed vegetables and fruits, and waste water. Infection with the virus always occurs when it enters the gastrointestinal tract, but the liver and biliary tract are affected. The incubation period for hepatitis A is usually 4 to 6 weeks. The disease begins with a rise in temperature to 38–39 degrees, followed by nausea and vomiting.The child complains of headache, lack of appetite. In most cases, diarrhea does not occur. The liver expands. The urine darkens and the stool becomes discolored. A week after the onset of the disease, the whites of the eyes and ears turn yellow.
Taking action
Hepatitis A is a self-destructive disease. Most often, it does not require special treatment with antiviral drugs. After the maximum manifestation of jaundice, the child begins to recover. The body produces antibodies, and immune cells gradually clear it of the virus.Treatment for hepatitis A mainly consists in relieving the unpleasant symptoms of poisoning. If necessary, your pediatrician can prescribe medications to protect your liver cells. The kid is advised to adhere to a certain diet. His menu should include: white meat, lean fish, cereals, boiled vegetables, fruits. But all kinds of sweets, smoked meats and nuts should be completely excluded from the diet. The full recovery period can take up to several months. The only sure way to protect yourself from the hepatitis A virus today is through vaccination.A child can be vaccinated after three years. The transferred illness leaves a very long, almost lifelong immunity.
Giardiasis
The disease is caused by the simplest microorganisms – lamblia. Infection occurs through unwashed hands, dirty objects and stale food. Usually bacteria die in the initial part of the intestine. But if the immune defense mechanism is weakened, it is enough for a child to lick unwashed hands, take a spoon that has fallen to the floor in his mouth, so that the body will give the disease a “green light”.The first symptoms are similar to food poisoning: frequent loose stools, less often vomiting. The child is worried about abdominal pain. He complains of weakness, does not eat well. Giardia are dangerous because they disrupt the digestion process and “steal” vitamins and nutrients intended for the growth and development of the baby. This disease can also provoke allergic reactions (rhinitis, cough, rash) or exacerbate other diseases of the gastrointestinal tract.
Taking action
The diagnosis of “giardiasis” is made solely by the results of the analysis of feces.Treatment is prescribed only in case of prolonged – more than 10 days – diarrhea. Giardiasis does not require long-term therapy. The doctor prescribes special antimicrobial drugs that destroy harmful bacteria in a very short time – 1-2 days. With giardiasis, a special diet is prescribed that limits the content in the child’s diet of food rich in carbohydrates: sweets, flour products, pasta, sweet fruits (melon, bananas, grapes, peaches). Milk is also banned – it contains a lot of lactose. Giardia do not like an acidic environment, so the baby’s diet must necessarily contain fermented milk products, sour fruits and berries.
Dysentery
An infectious disease that affects the mucous membrane of the large intestine. The disease is caused by bacteria of several types, different in strength of influence. Doctors have noticed that recently, microorganisms have become more active, provoking severe forms of dysentery. Bacteria actively multiply in a hot environment, so little patients most often suffer from this ailment in the summer. The infection is spread through dirty hands, food and drink. It is also carried by flies.Dysentery begins with general malaise. After a while, intense cramping pains appear in the left side of the lower abdomen. The child’s stool becomes frequent (up to 25 times a day), often mixed with blood and mucus. The body temperature rises sharply (up to 39 degrees), and a headache may be present.
Taking action
Recovery takes 2 to 6 weeks, depending on the severity of the illness. Antibiotics are the main drugs in the treatment of dysentery. Diet plays an important role in treatment.Foods rich in plant fiber are excluded from the diet of a sick child so as not to irritate the intestines. The baby should eat in small portions every 2-3 hours. The usual diet should be switched gradually, within 1-2 months after complete recovery.
Rotavirus infection
Rotaviruses are one of the most common causative agents of acute intestinal infections in children. They got their name not because of the way they enter our body, as it might seem, but because they have the shape of a wheel (rota means “wheel” in Latin).It is believed that at least 40% of intestinal diseases in 4-6-year-old children are caused by rotavirus infection. The main mode of transmission of the disease is food. A child can also become infected by touching the toys of an already sick toddler and even simply by taking his hand. The malaise is often accompanied by signs of a cold, which is why it is called “intestinal flu”. However, a runny nose and sore throat will only be accompanying unpleasant symptoms. The main goal of the virus is to infect the mucous membrane of the digestive tract.As a rule, the disease begins with vomiting, then the temperature rises and watery diarrhea begins. Diarrhea with rotavirus infection most often does not last more than two days.
Taking action
Rotavirus infection is easily diagnosed with a stool test. The main danger to the health of a child with this disease is dehydration. Therefore, the basis of treatment is an active fight against the loss of fluid in the body. It is important to know that during illness and during recovery, the child should not be given milk.The fact is that the infection significantly reduces the activity of some enzymes in the intestine, in particular lactase, which helps the absorption of lactose – milk sugar. Rotavirus persists for a long time on surrounding objects, therefore, after recovery, the child’s personal belongings must be thoroughly disinfected, and clothes and bedding must be boiled.
Ambulance
Dehydration.
The main danger in intestinal infections is precisely this problem: due to diarrhea and vomiting, the reserves of water and salts in the child’s body are especially small.The true severity of the disease is often determined by the degree of dehydration. This can only be done by a doctor. The primary task of parents is to try to replenish the amount of lost fluid and normalize the water-salt balance. For this purpose, medicines are ideal, which are mixtures of various salts, which must be diluted with boiled water before use (they are sold in a pharmacy). In the absence of such preparations, dried fruit compote, tea, preferably green tea, as well as mineral water, decoctions of rosehip herbs, are suitable.The temperature of the drinks should be approximately equal to the body temperature so that the absorption of liquid from the stomach into the bloodstream is as fast as possible. The liquid should enter the child’s body in small portions – use a teaspoon or tablespoon for this. Do not let your child drink from a mug: too much liquid can cause vomiting.
Diarrhea and vomiting
are ways of protecting the body, thus it gets rid of foreign, harmful substances.Therefore, in the first hours of intestinal infection, one should not try to stop diarrhea and vomiting. On the contrary, these processes need to be stimulated. Deliberately induce vomiting, thereby flushing the stomach. Cleanse the colon with an enema. For this, ordinary boiled water with a temperature of about 20 C0 is used. Be sure to make sure that all injected fluid comes out. To protect the mucous membrane of the gastrointestinal tract, use enterosorbents to help remove toxins from the body.
Get immediate medical attention if:
• the child is unable to drink because of persistent vomiting;
• no urine for more than 6 hours;
• the child has a dry tongue, sunken eyes, the skin has acquired a grayish tint;
• there is an admixture of blood in the feces;
• diarrhea has stopped, but vomiting has increased and / or body temperature has risen sharply.

 It is often (but not always) first treated with the antibiotic vancomycin.
It is often (but not always) first treated with the antibiotic vancomycin. It should be noted that IBS is a syndrome which means a series of symptoms, not a single disease. Treatments vary widely from avoidance of food allergens and lactose and increasing consumption of fiber and physical activity levels. Irritable bowel syndrome is only diagnosed after inflammatory bowel disease or cancer has been ruled out.
It should be noted that IBS is a syndrome which means a series of symptoms, not a single disease. Treatments vary widely from avoidance of food allergens and lactose and increasing consumption of fiber and physical activity levels. Irritable bowel syndrome is only diagnosed after inflammatory bowel disease or cancer has been ruled out.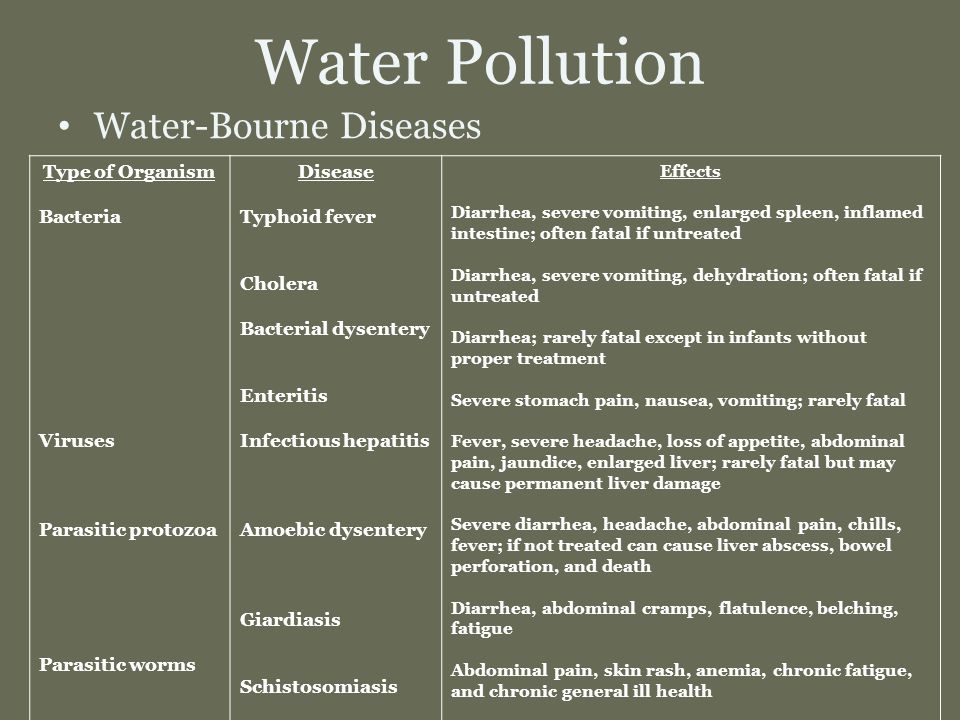 More likely in child care center outbreaks.
More likely in child care center outbreaks.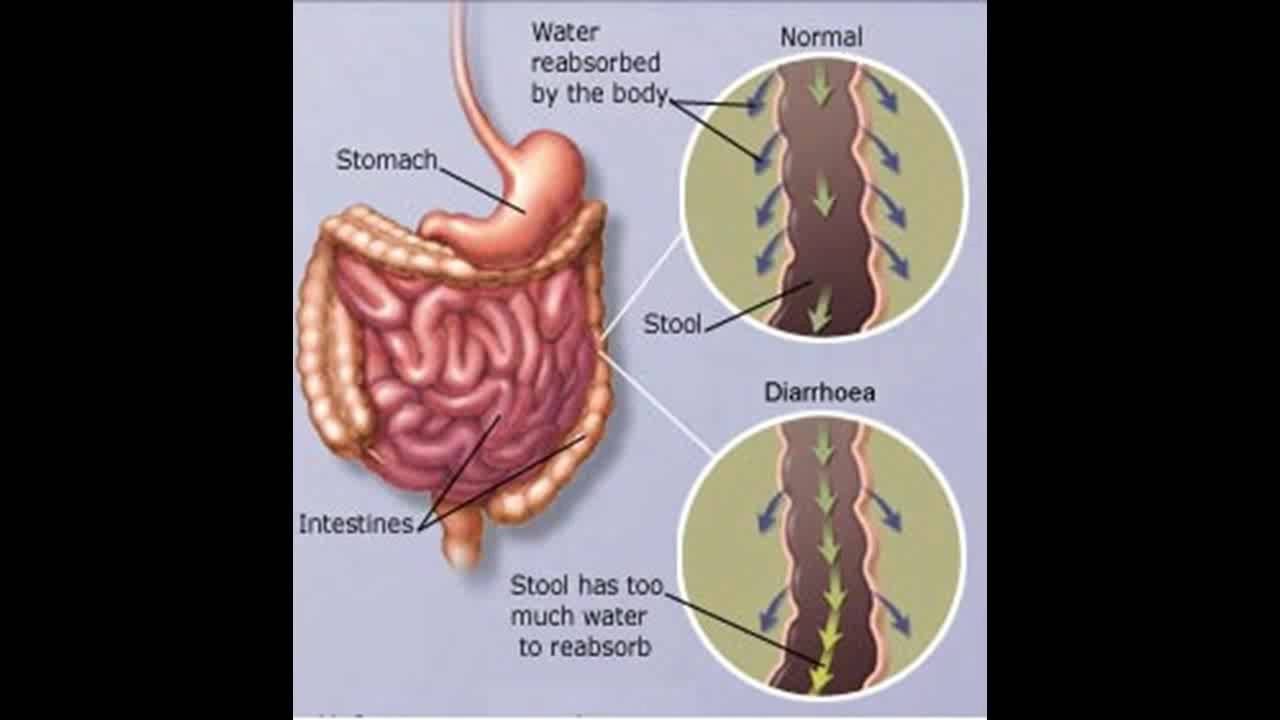
 Ask your doctor to teach you how to do this test.
Ask your doctor to teach you how to do this test.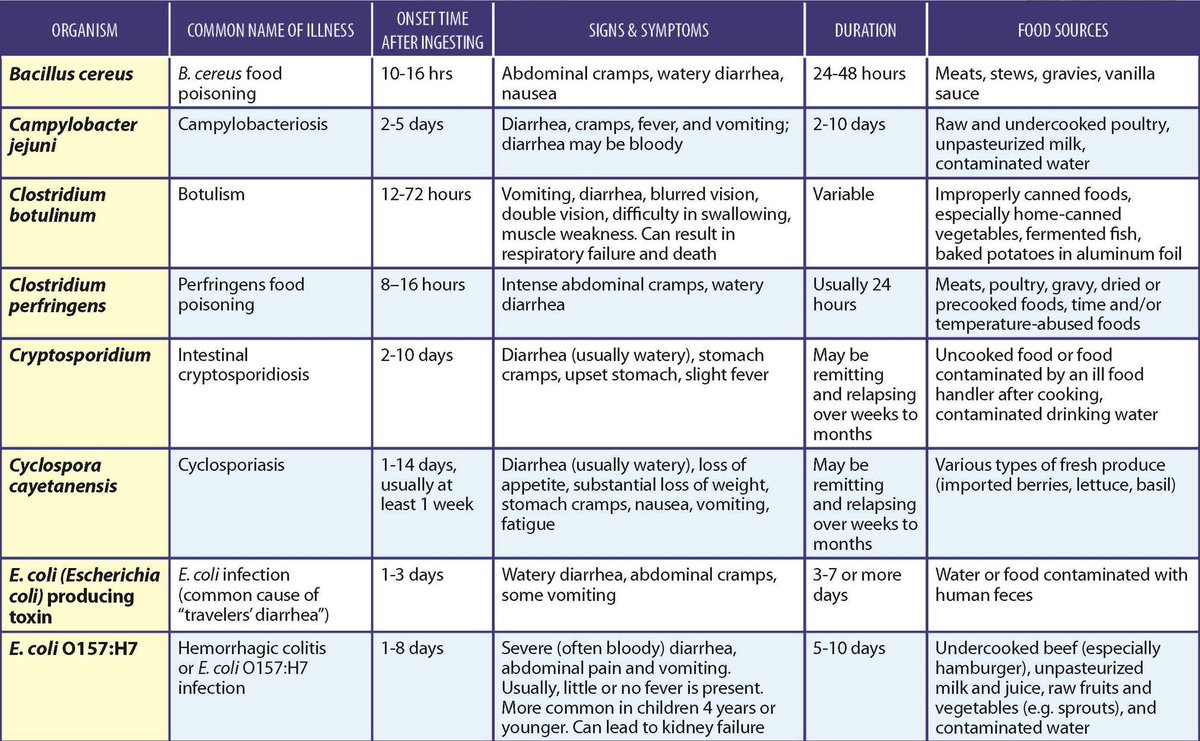
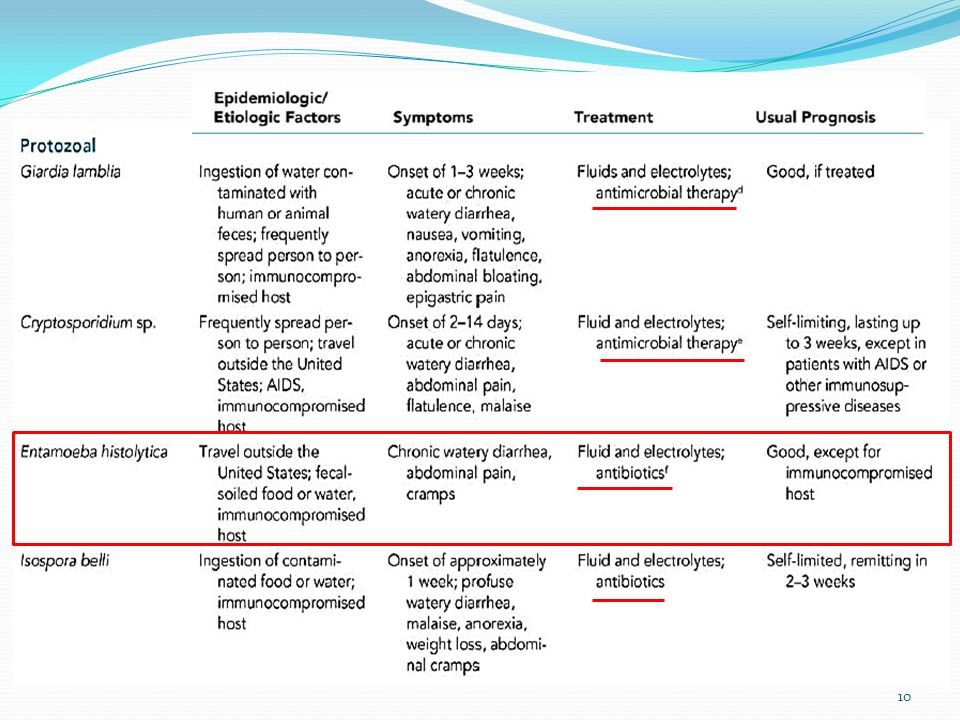
 Reason: they are easy to digest.
Reason: they are easy to digest.
 Children rarely need ORS after age 3.
Children rarely need ORS after age 3. Give lots of cold fluids.
Give lots of cold fluids.
:max_bytes(150000):strip_icc()/what-is-the-24-hour-flu-770474_color1-5b95dbc34cedfd00256c4e66.png)

 Can cause loose, slimy stools in babies. Can be blood-streaked. Starts within the first 2 months of life. Need to avoid cow’s milk formulas.
Can cause loose, slimy stools in babies. Can be blood-streaked. Starts within the first 2 months of life. Need to avoid cow’s milk formulas.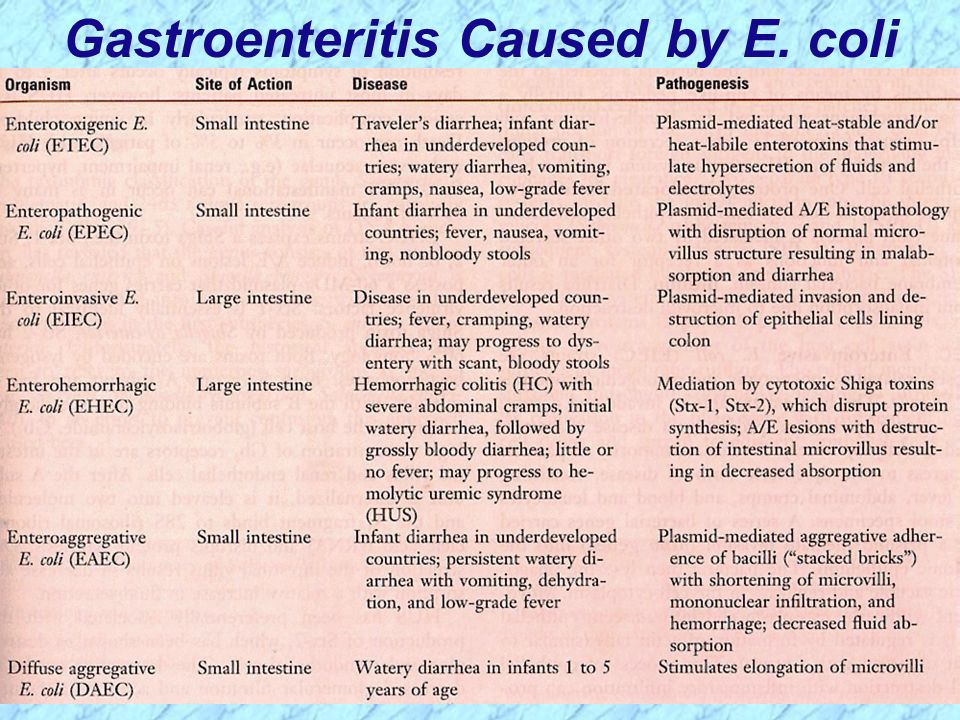 Mild diarrhea or mild vomiting does not cause this. Neither does a small decrease in fluid intake.
Mild diarrhea or mild vomiting does not cause this. Neither does a small decrease in fluid intake.
:max_bytes(150000):strip_icc()/1942943-what-causes-orange-stool-01-5b2fe57deb97de0036f361e7.png) If it lasts for 3 or more stools, the baby has diarrhea.
If it lasts for 3 or more stools, the baby has diarrhea. Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. Offer as much formula as your child will take.
Offer as much formula as your child will take.

/GettyImages-476375927-56a772383df78cf772960769.jpg)
 In young children, water-borne diarrhea is usually caused by enteropathogenic strains.Diarrhea is combined with vomiting, pain in the epigastrium, along the intestines. An increase in body temperature to subfebrile numbers is possible. General condition of patients of moderate severity.
In young children, water-borne diarrhea is usually caused by enteropathogenic strains.Diarrhea is combined with vomiting, pain in the epigastrium, along the intestines. An increase in body temperature to subfebrile numbers is possible. General condition of patients of moderate severity.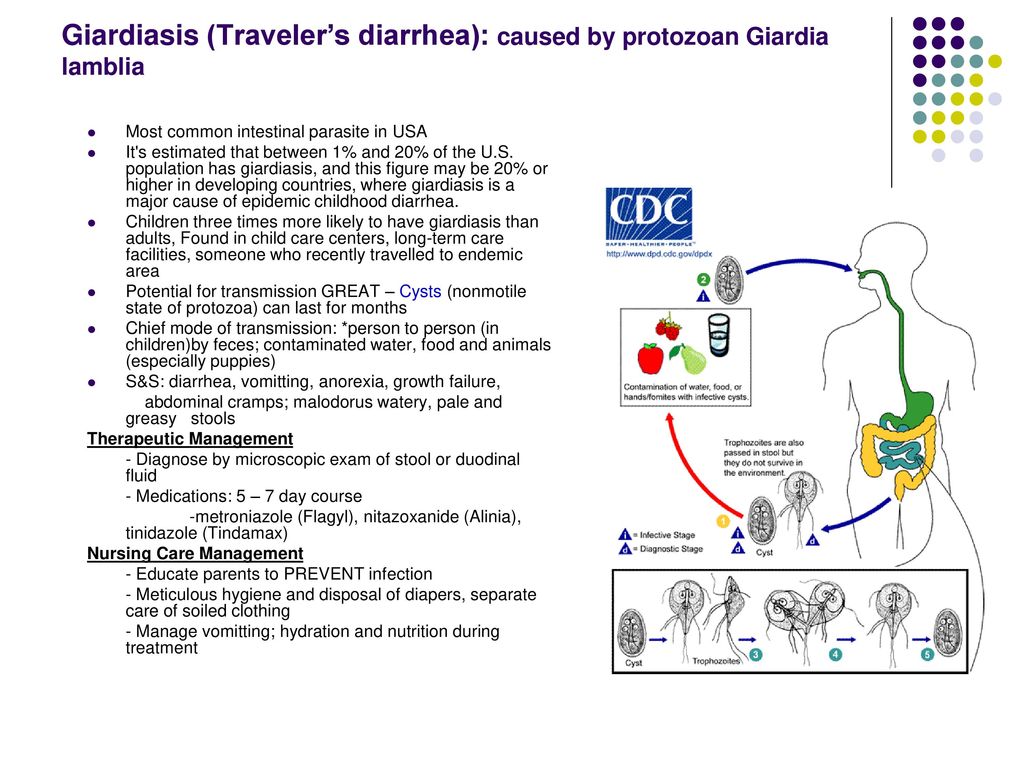 In severe cases, there are paresis, paralysis of facial muscles with facial asymmetry.
In severe cases, there are paresis, paralysis of facial muscles with facial asymmetry.