Chest pain middle of rib cage. Costochondritis: Causes, Symptoms, and Treatment of Rib Cage Chest Pain
What is costochondritis. How does it cause chest pain. What are the symptoms of costochondritis. What causes this condition. How is costochondritis diagnosed. What treatments are available for costochondritis. When should you seek medical attention for chest pain.
Understanding Costochondritis: A Common Cause of Chest Pain
Costochondritis is a condition characterized by inflammation of the cartilage connecting the ribs to the breastbone (sternum). This inflammation can lead to sharp, often debilitating chest pain that may mimic more serious conditions like heart attacks. While the exact cause of costochondritis is not always clear, it’s essential to understand its symptoms, potential causes, and available treatments to manage this condition effectively.
Recognizing the Symptoms of Costochondritis
The primary symptom of costochondritis is chest pain, which can vary in intensity and presentation. Here are some key characteristics of costochondritis-related pain:

- Sharp or aching pain in the front or side of the chest
- Pain that worsens with movement, deep breathing, or lying down
- Tenderness when pressing on the affected area
- Pain that may radiate to the back or abdomen
- Discomfort that can last for weeks or even months
Can costochondritis pain be mistaken for a heart attack? Yes, the chest pain associated with costochondritis can sometimes be confused with that of a heart attack. However, costochondritis pain typically worsens with movement or pressure on the chest wall, while heart attack pain is often accompanied by additional symptoms like shortness of breath, nausea, and radiating pain to the arms or jaw.
Potential Causes and Risk Factors for Costochondritis
While the exact cause of costochondritis is often unknown, several factors may contribute to its development:
- Physical trauma to the chest area
- Repetitive strain from activities like heavy lifting or intense exercise
- Respiratory infections or conditions that cause frequent coughing
- Certain viral or bacterial infections
- Inflammatory conditions like fibromyalgia or rheumatoid arthritis
Are certain individuals more prone to developing costochondritis? Research suggests that women, particularly those who are physically active, may be at a higher risk for costochondritis. Additionally, individuals who engage in high-impact activities, have recently experienced chest trauma, or have allergies with frequent exposure to irritants may also be more susceptible to this condition.

Diagnosing Costochondritis: What to Expect
Diagnosing costochondritis can be challenging, as there is no specific test to confirm the condition. Healthcare providers typically use a combination of methods to reach a diagnosis:
- Medical history review
- Physical examination, including palpation of the chest wall
- Ruling out other potential causes of chest pain
What diagnostic tests might a doctor order to rule out other conditions? While not always necessary, a healthcare provider may recommend the following tests to exclude other potential causes of chest pain:
- Electrocardiogram (ECG) to assess heart function
- Chest X-ray to examine the lungs and rib cage
- Blood tests to check for signs of infection or inflammation
- In some cases, more advanced imaging like CT scans or MRIs
Treatment Options for Managing Costochondritis
The good news is that costochondritis often resolves on its own over time. However, there are several treatment options available to help manage symptoms and promote healing:
1. Pain Management
Over-the-counter pain relievers and anti-inflammatory medications are often the first line of treatment for costochondritis. These may include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen
- Acetaminophen for pain relief
2. Rest and Activity Modification
Resting the affected area and avoiding activities that exacerbate pain can help reduce inflammation and promote healing. This may involve:
- Temporarily avoiding high-impact exercises
- Using proper posture and body mechanics
- Applying heat or ice to the affected area
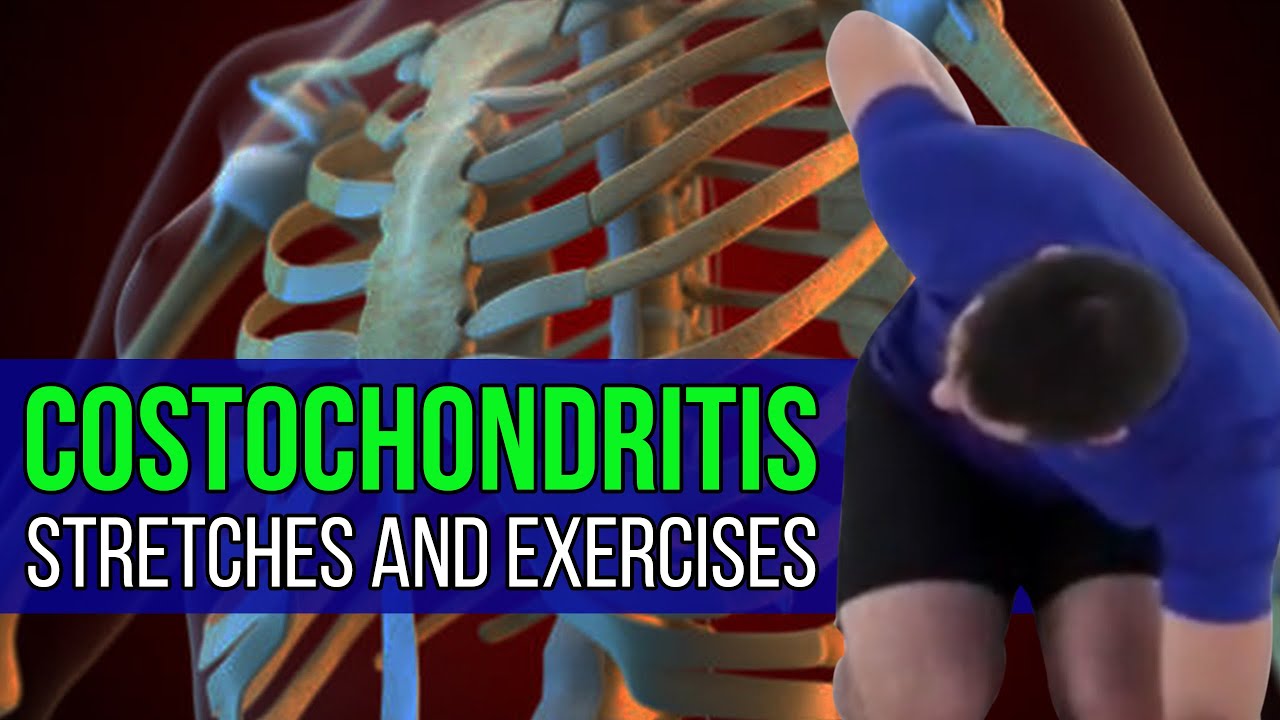
3. Physical Therapy
In some cases, a physical therapist may recommend exercises and stretches to improve posture, strengthen chest muscles, and reduce pain. These may include:
- Gentle stretching exercises
- Postural correction techniques
- Breathing exercises to improve chest expansion
4. Medical Interventions
For severe or persistent cases of costochondritis, a healthcare provider may recommend more advanced treatments such as:

- Corticosteroid injections to reduce inflammation
- Transcutaneous electrical nerve stimulation (TENS) for pain relief
- In rare cases, surgery to remove damaged cartilage
How long does it typically take for costochondritis to resolve? The duration of costochondritis can vary significantly from person to person. Some individuals may experience relief within a few weeks, while others may have symptoms that persist for several months. Consistent management and following medical advice can help speed up recovery.
Preventing Costochondritis: Strategies for Reducing Risk
While it’s not always possible to prevent costochondritis, there are several strategies that may help reduce the risk of developing this condition:
- Practice proper lifting techniques to avoid strain on the chest wall
- Warm up adequately before engaging in physical activities
- Maintain good posture to reduce stress on the rib cage
- Manage underlying conditions that may contribute to inflammation
- Avoid repetitive movements that strain the chest area
Can lifestyle modifications help prevent recurrent episodes of costochondritis? Yes, making certain lifestyle changes can potentially reduce the likelihood of experiencing repeated bouts of costochondritis. These modifications may include:
- Incorporating low-impact exercises into your routine
- Using ergonomic equipment at work to reduce strain
- Practicing stress-reduction techniques like meditation or yoga
- Maintaining a healthy weight to reduce pressure on the chest wall
When to Seek Medical Attention for Chest Pain
While costochondritis is generally not life-threatening, it’s crucial to seek medical attention if you experience chest pain, especially if it’s severe or accompanied by other symptoms. Here are some situations that warrant immediate medical care:
- Sudden, severe chest pain
- Chest pain accompanied by shortness of breath, sweating, or nausea
- Pain that radiates to the arms, jaw, or back
- Chest pain associated with fever or signs of infection
- Persistent pain that doesn’t improve with rest or over-the-counter medications
How can you differentiate between costochondritis and a heart attack? While it can be challenging to distinguish between costochondritis and a heart attack based on symptoms alone, there are some key differences:
- Costochondritis pain typically worsens with movement or pressure on the chest wall
- Heart attack pain is often described as a crushing or squeezing sensation
- Costochondritis doesn’t usually cause shortness of breath, while a heart attack often does
- Heart attack pain may be accompanied by nausea, sweating, and dizziness
If you’re unsure about the cause of your chest pain, it’s always best to err on the side of caution and seek immediate medical attention.
Living with Costochondritis: Coping Strategies and Long-Term Outlook
For individuals dealing with chronic or recurrent costochondritis, developing effective coping strategies is essential for maintaining quality of life. Here are some tips for managing this condition in the long term:
1. Pain Management Techniques
Exploring various pain management methods can help individuals find relief from costochondritis symptoms. These may include:
- Applying heat or cold therapy to the affected area
- Practicing relaxation techniques like deep breathing or progressive muscle relaxation
- Using over-the-counter topical pain relievers
- Exploring alternative therapies like acupuncture or massage (with medical approval)
2. Lifestyle Adaptations
Making certain lifestyle changes can help reduce the impact of costochondritis on daily activities:
- Modifying sleep positions to reduce pressure on the chest wall
- Using supportive pillows or cushions when sitting or lying down
- Wearing comfortable, non-restrictive clothing
- Pacing activities to avoid overexertion
3. Emotional Support
Dealing with chronic pain can take an emotional toll. Seeking support from the following sources can be beneficial:
- Joining support groups for individuals with chronic pain
- Consulting with a mental health professional to develop coping strategies
- Communicating openly with friends and family about the condition
What is the long-term outlook for individuals with costochondritis? For most people, costochondritis is a temporary condition that resolves with time and appropriate management. However, some individuals may experience recurrent episodes or chronic symptoms. Working closely with healthcare providers to develop an effective treatment plan can help improve long-term outcomes and quality of life.
Costochondritis in Special Populations: Considerations and Challenges
While costochondritis can affect anyone, certain populations may face unique challenges or require special considerations when managing this condition:
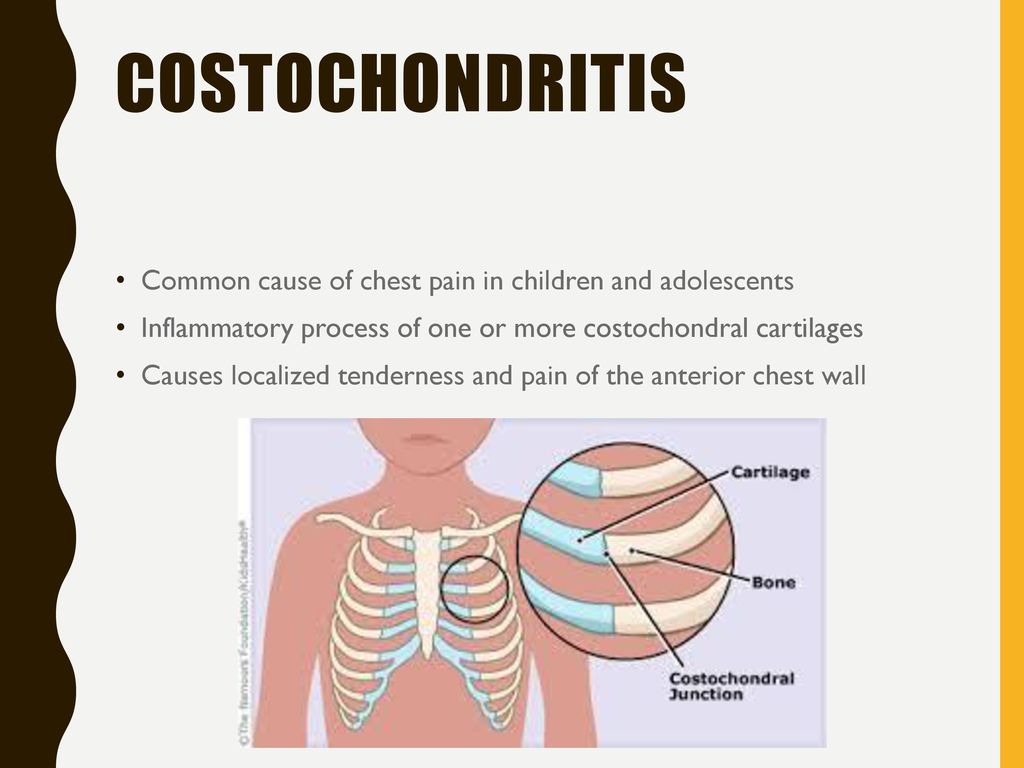
1. Costochondritis in Children and Adolescents
Costochondritis can occur in children and teenagers, often presenting challenges in diagnosis and management:
- Symptoms may be mistaken for growing pains or sports-related injuries
- Treatment approaches may need to be adjusted based on age and activity level
- Educating parents and caregivers about the condition is crucial for proper management
2. Pregnancy and Costochondritis
Pregnant women may be at increased risk for costochondritis due to changes in posture and increased strain on the chest wall:
- Treatment options may be limited due to pregnancy-related restrictions on certain medications
- Proper support and ergonomic adjustments can help alleviate symptoms
- Close monitoring is essential to distinguish between costochondritis and other pregnancy-related chest pain
3. Costochondritis in Older Adults
Older individuals may face additional challenges when dealing with costochondritis:

- Symptoms may be confused with other age-related conditions
- Existing health issues may complicate treatment options
- Careful consideration of medication interactions is crucial
How does the management of costochondritis differ across these populations? The approach to managing costochondritis may vary depending on the individual’s age, overall health, and specific circumstances. Healthcare providers must tailor treatment plans to address the unique needs and limitations of each patient, ensuring safe and effective management of symptoms.
Emerging Research and Future Directions in Costochondritis Management
As medical understanding of costochondritis continues to evolve, researchers are exploring new avenues for diagnosis, treatment, and prevention of this condition. Some areas of ongoing research and potential future developments include:
1. Advanced Imaging Techniques
Researchers are investigating the use of advanced imaging modalities to improve the diagnosis of costochondritis:
- High-resolution ultrasound to visualize cartilage inflammation
- Magnetic resonance imaging (MRI) to detect subtle changes in cartilage structure
- Positron emission tomography (PET) scans to identify areas of active inflammation
2. Novel Treatment Approaches
Emerging therapies and treatment modalities are being explored to enhance the management of costochondritis:
- Targeted biologic therapies to address underlying inflammation
- Regenerative medicine techniques to promote cartilage healing
- Advanced pain management technologies, such as neuromodulation
3. Genetic and Environmental Factors
Ongoing research aims to better understand the genetic and environmental factors that may contribute to the development of costochondritis:
- Identification of genetic markers associated with increased susceptibility
- Investigation of environmental triggers that may exacerbate symptoms
- Exploration of potential preventive strategies based on individual risk factors
What potential breakthroughs in costochondritis management can we anticipate in the coming years? While it’s difficult to predict specific breakthroughs, ongoing research may lead to more precise diagnostic tools, personalized treatment approaches, and improved strategies for prevention and long-term management of costochondritis. These advancements could significantly enhance the quality of life for individuals affected by this condition.
As research in the field of costochondritis continues to progress, individuals living with this condition can look forward to potentially more effective and tailored treatment options in the future. In the meantime, working closely with healthcare providers and staying informed about current management strategies remains crucial for optimal symptom control and overall well-being.
Costochondritis – NHS
Costochondritis is inflammation where your ribs join the bone in the middle of your chest (breastbone). It can cause sharp chest pain, especially when moving or breathing. It usually gets better on its own over time.
Check if you have costochondritis
Costochondritis may cause sharp pain in the front or side of your chest.
The pain may be worse when:
- moving your upper body
- lying down
- breathing deeply
- you press the middle of your chest
Urgent advice: Get help from NHS 111 if:
- you think you have costochondritis
It is important to get chest pain checked to rule out other more serious conditions.
You can call 111 or get help from 111 online.
Immediate action required: Call 999 if:
You have sudden chest pain that:
- spreads to your arms, back, neck, or jaw
- makes your chest feel tight or heavy
- started with a shortness of breath, sweating, feeling sick or being sick
- lasts more than 15 minutes
You could be having a heart attack. Call 999 immediately as you need immediate treatment in hospital.
Treatments for costochondritis
Costochondritis usually gets better on its own, over time. It can last for a few weeks to several months.
Painkillers that help with inflammation, like ibuprofen, may be recommended to help with the pain.
If you have very bad pain that does not get better over time, you may be offered a steroid injection to help reduce inflammation or local anaesthetic to ease the pain.
Causes of costochondritis
It is not always known what causes costochondritis, but it may be caused by:
- an injury to your chest
- repetitive upper body movements, like lifting
- coughing a lot
Sometimes it may be caused by a problem with the joints in the back, or another underlying condition like fibromyalgia or rheumatoid arthritis.
It can also be caused by an infection.
Page last reviewed: 26 July 2022
Next review due: 26 July 2025
Symptoms, Causes, Tests, and Treatment
Costochondritis is an inflammation of the cartilage in the rib cage. It can happen due to infection, injury, and other health conditions.
It can happen due to infection, injury, and other health conditions.
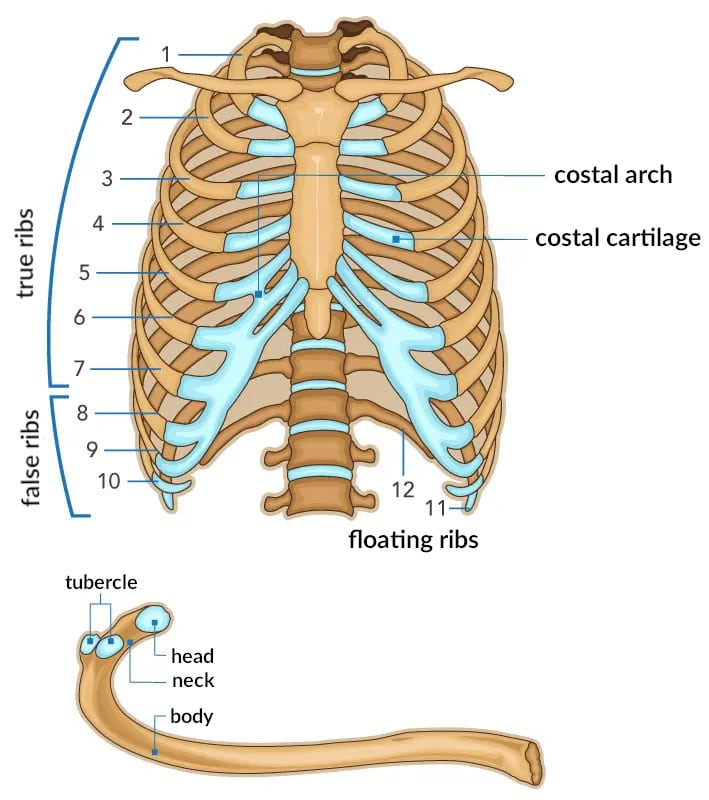
This condition usually affects the cartilage where the upper ribs attach to the breastbone, also known as the sternum, in an area known as the costosternal joint or costosternal junction.
Chest pain caused by costochondritis can range from mild to severe. Mild cases may only cause your chest to feel slightly tender or some pain when you push on the area.
More severe cases may get worse with certain movements as well as with deep breaths. The condition often goes away within a few weeks or months, but some cases may require treatment.
People with costochondritis often experience chest pain in the upper and middle rib area on either side of the breastbone. This pain can gradually increase over time, or come on suddenly.
Additional symptoms can include:
- pain that becomes worse when lying down
- pain that becomes worse when there’s pressure on your chest, like when you wear a seatbelt
- pain that intensifies with coughing or deep breaths
- pain that increases with physical activity
It’s important to note that symptoms like chest tightness and radiating pain can indicate other conditions, including a heart attack.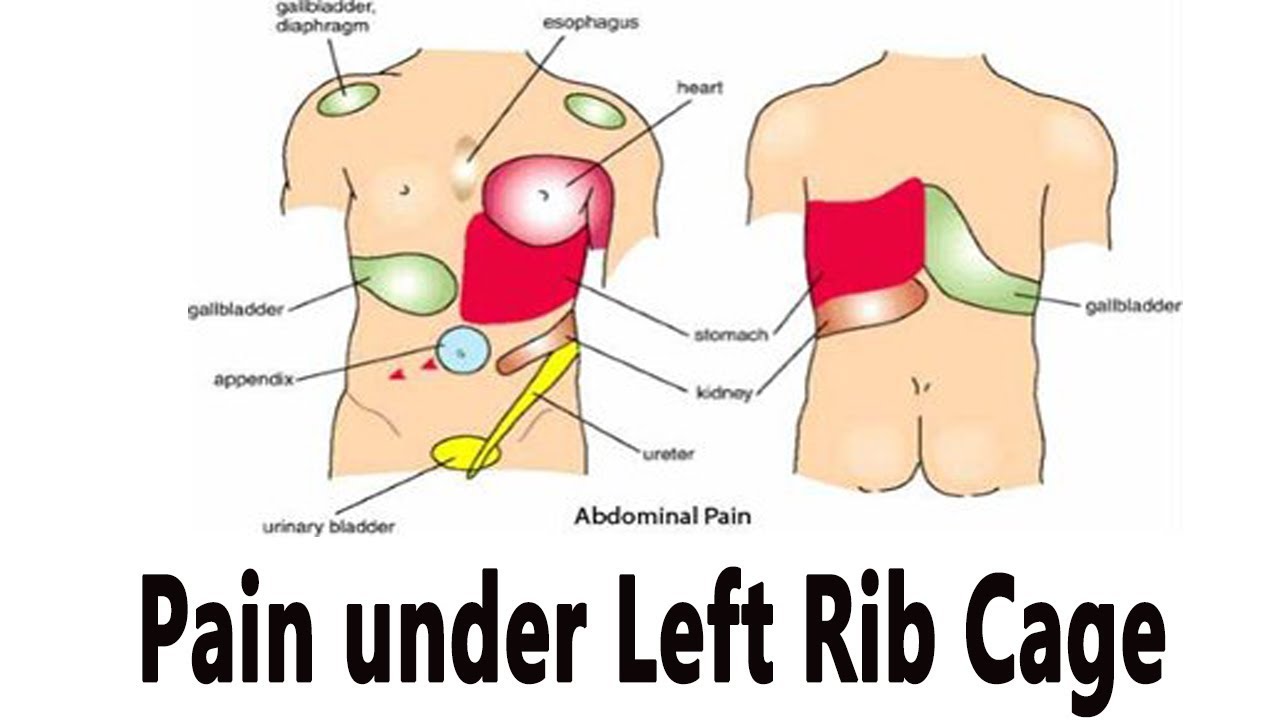 Seek immediate medical care if you’re experiencing persistent, intense chest pain.
Seek immediate medical care if you’re experiencing persistent, intense chest pain.
The exact cause of costochondritis in most people is unknown. But conditions that may cause it include:
- trauma to the chest, such as blunt impact from a car accident or fall
- physical strain from activities, such as heavy lifting and strenuous exercise
- certain viruses or respiratory conditions, such as tuberculosis, that can cause joint inflammation
- severe coughing
There’s some research that suggests costochondritis occurs more often in women, especially those who are athletes. You may also be at a higher risk for this condition if you:
- participate in high-impact activities
- recently had a physical trauma or fall that affected the chest area
- have allergies and are frequently exposed to irritants
While there’s no test to diagnose costochondritis, your doctor will most likely ask a series of questions and do a series of tests to determine the source of your chest pain.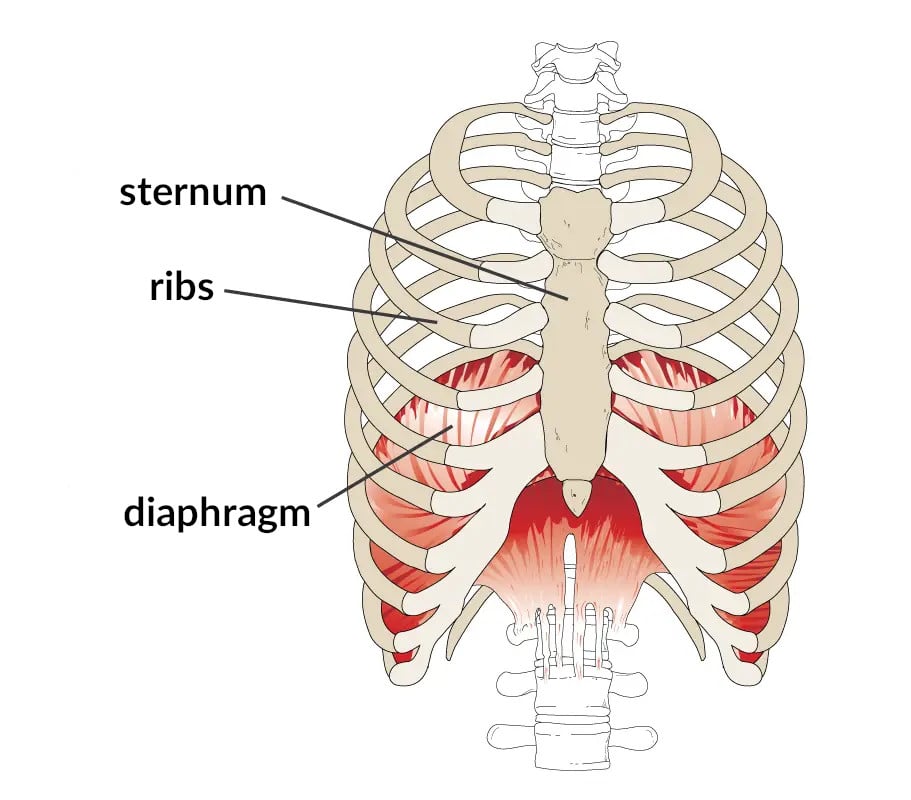
Lab tests
Typically, lab tests aren’t needed to diagnose costochondritis, but depending on your personal health history, your doctor may do some tests to see if your chest pain could be due to other issues like pneumonia or coronary heart disease.
X-rays and ECGs
Your doctor may want you to get an X-ray to make sure there’s nothing abnormal going out with your lungs.
If you’re dealing with costochondritis, your X-ray should look normal. They may also recommend an electrocardiogram (ECG) to make sure your heart isn’t the cause of your chest pain.
Many times, diagnosing costochondritis is a matter of eliminating other possible, more serious causes.
See your doctor right away if you have trouble breathing or are feeling intense chest pain.
Always seek immediate emergency care when you have abnormal and debilitating pain in your chest. It can indicate something serious, such as a heart attack.
Getting care as soon as possible limits the possibility of complications, especially if an underlying issue is causing your costochondritis.
Costochondritis can be treated in several ways.
Most cases of costochondritis are treated with over-the-counter medications. If your pain is mild to moderate, your doctor will probably recommend nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil) or naproxen (Aleve).
Your doctor may also recommend:
- prescription-strength NSAIDs
- oral steroids or injection of a steroid into the area involved
- transcutaneous electrical nerve stimulation (TENS), which is a mild electric current that is delivered to the area via a small, battery-powered device
Lifestyle changes
Your doctor may tell you to make permanent lifestyle changes if you have persistent or chronic costochondritis.
Some types of exercise can aggravate this condition, including rowing and weightlifting. Manual labor may also have a negative effect.
Your doctor may also recommend:
- rest
- physical therapy
- hot or cold therapy using a heating pad and ice
Normally, treatment of the inflammation and pain causes costochondritis to eventually go away on its own.
If you have chronic costochondritis, the pain may persist or return — even with treatment — when you exercise or engage in certain activities. In these cases, you may need to seek long-term care to make sure that costochondritis doesn’t affect your quality of life and ability to take part in daily activities.
Pains associated with costochondritis can indicate other issues. Chest pain can often mean that you’re having heart or lung issues, so see your doctor right away when you feel pain in your chest to make sure that you’re not having a heart attack or have pneumonia.
The chest pain associated with costochondritis can be a symptom of fibromyalgia. With fibromyalgia, you may experience soreness in your chest in addition to:
- pain throughout your body
- fatigue and inability to rest due to pain
- difficulty focusing or concentrating
- feelings of depression
- headaches
If you experience chest pains along with these other symptoms, talk with your doctor about getting tested for fibromyalgia.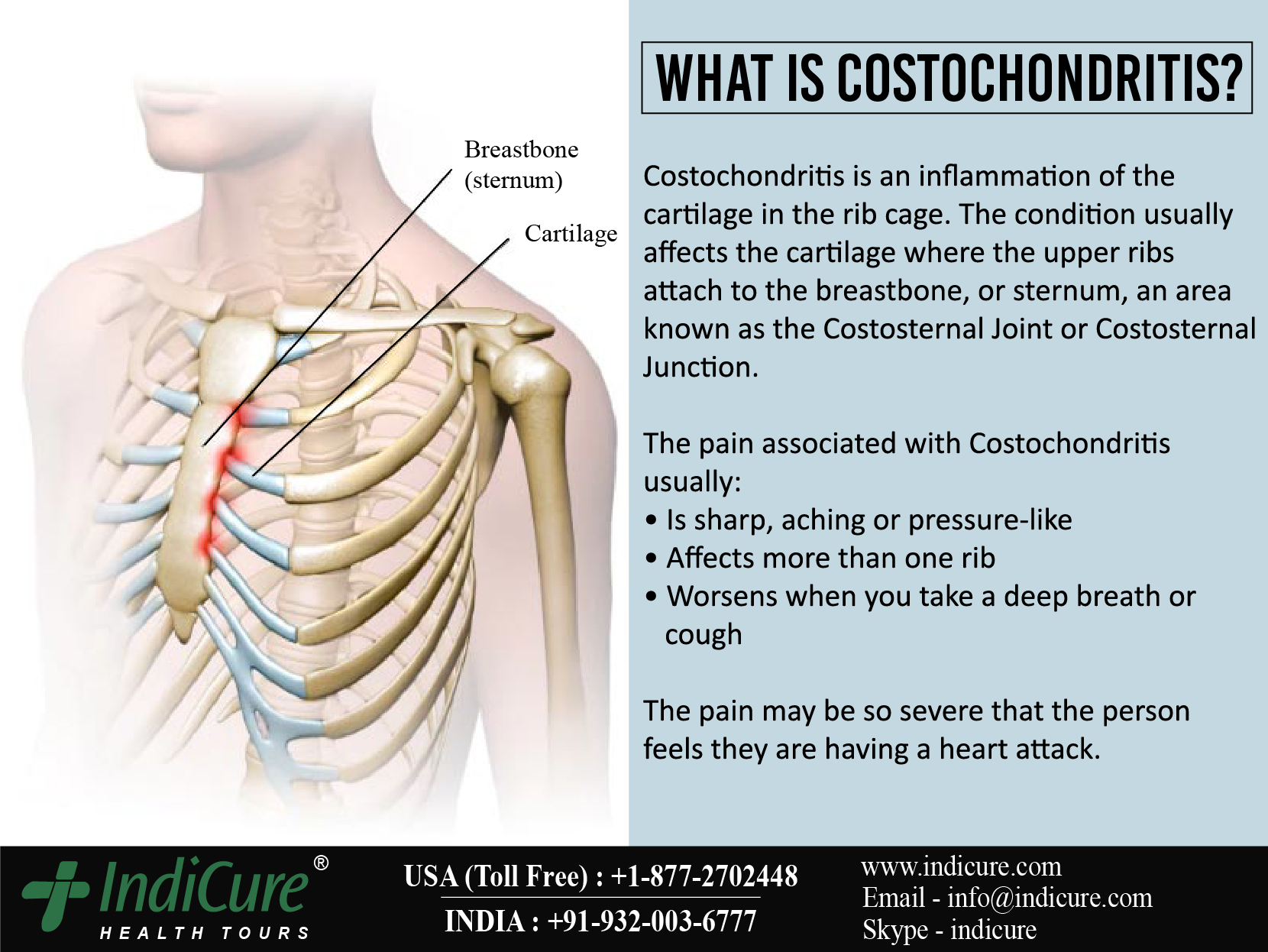 Understanding this condition can help you address the symptoms and ensure that it doesn’t interrupt your daily life.
Understanding this condition can help you address the symptoms and ensure that it doesn’t interrupt your daily life.
Costochondritis is caused by inflammation and typically presents as chest pain that gets worse with certain movements or pressure. This condition usually isn’t persistent. In many cases, costochondritis goes away on its own.
Mild cases of costochondritis may disappear after a few days. Chronic cases can last for weeks or more, but most cases don’t last any longer than a year.
To lower your chances of developing persistent costochondritis, carry and lift heavy loads properly. Try doing fewer high-impact exercises or manual labor, when possible.
Seek medical attention immediately if you experience chest pain while performing any of these activities.
Costal chondritis (Tietze’s syndrome) – treatment, symptoms, causes, diagnosis The disease is characterized by local pain in the chest, aggravated by palpation and pressure on these areas. Costal chondritis is a relatively harmless condition and usually goes away without treatment.
 The cause of occurrence is not known.
The cause of occurrence is not known.
- Costochondritis is a common cause of chest pain in childhood and adolescence and accounts for 10-30% of all chest pain in this age group. It most often occurs between the ages of 12-14 years.
- Costal chondritis is also considered a possible diagnosis in adults who have chest pain. Chest pain in adults is considered a potentially serious symptom of the disease and, first of all, it is necessary to exclude the pathology of the heart (ECG, tests, examination, etc.). Only after a thorough examination and exclusion of the cardiac genesis of pain can we assume the presence of costal chondritis. Sometimes differential diagnosis is difficult. In adults, costal chondritis is more common in women.
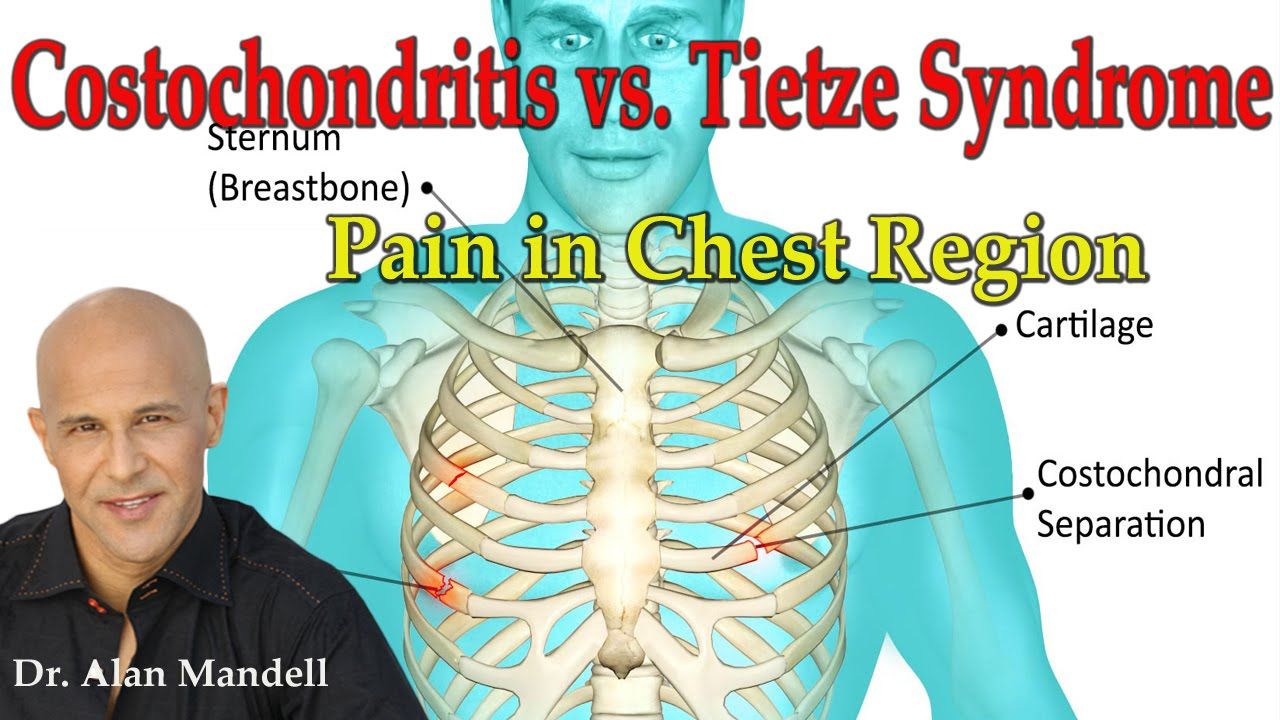
Costal chondritis is often referred to as Tietze’s syndrome. Tietze’s syndrome is a rare inflammatory disorder characterized by chest pain and cartilage swelling at the attachment of the second or third rib to the sternum.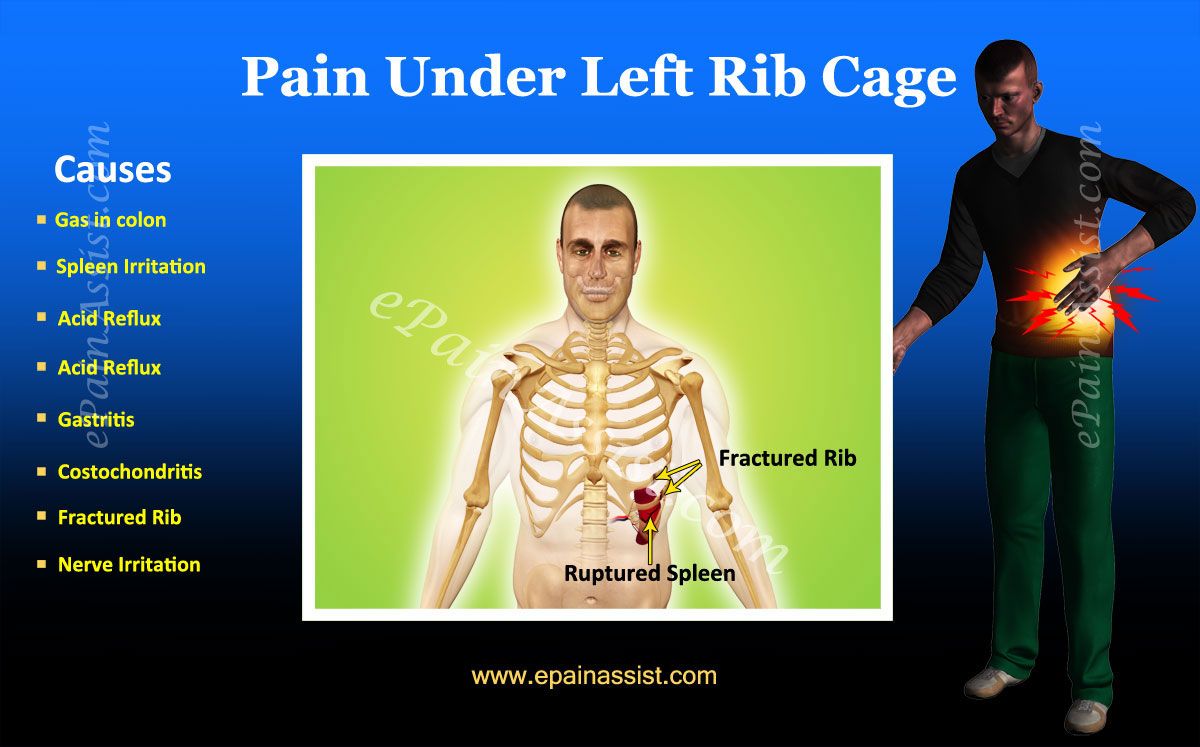 The pain occurs acutely and radiates to the arm, shoulder. Both men and women get sick more often between the ages of 20 and 40. It occurs mainly in people whose work is associated with physical activity or athletes.
The pain occurs acutely and radiates to the arm, shoulder. Both men and women get sick more often between the ages of 20 and 40. It occurs mainly in people whose work is associated with physical activity or athletes.
Causes
Costal chondritis is an inflammatory process in cartilage, usually without any specific cause. Repeated minor chest injuries and acute respiratory infections can cause soreness in the area of attachment of the ribs (both the effects of the viruses themselves and frequent coughing on the areas of attachment of the ribs). Sometimes costal chondritis occurs in people who take parenteral drugs or after surgery on the chest. After surgery, damaged cartilage tissue is more susceptible to infection due to impaired blood supply.
Symptoms
Chest pain associated with costal chondritis is usually preceded by physical exertion, minor trauma, or acute upper respiratory infections.
- The pain is usually acute and localized in the anterior region of the chest.
 The pain may radiate down or more often to the left side of the chest.
The pain may radiate down or more often to the left side of the chest. - The most common localization of pain is the region of the fourth, fifth and sixth ribs. Pain is aggravated by movement of the body or deep breathing. And, conversely, there is a decrease in pain at rest and with shallow breathing.
- Soreness, which is clearly detected on palpation (pressure in the area of attachment of the ribs to the sternum). This is a characteristic feature of chondritis and the absence of this feature suggests that the diagnosis of costal chondritis is unlikely.
When costal chondritis is caused by a postoperative infection, swelling, redness and/or pus may be seen in the area of the postoperative wound.
Considering that the symptoms of chondritis are often similar to emergencies, it is necessary to urgently seek medical help in the following cases:
- Breathing problems
- High temperature
- Signs of an infectious disease (swelling, redness in the area of attachment of the ribs)
- Persistent chest pain with nausea, sweating
- Any chest pain without clear localization
- Increased pain during treatment
Diagnosis
Diagnosis is based on the medical history and external examination. Characteristic of this syndrome is pain on palpation in the attachment area of 4-6 ribs.
Characteristic of this syndrome is pain on palpation in the attachment area of 4-6 ribs.
Radiography (CT, MRI) is usually not very informative for the diagnosis of this syndrome and is used only for differential diagnosis with other possible causes of chest pain (cancer, lung disease, etc.). ECG, laboratory tests are necessary to rule out heart disease or infections. The diagnosis of costal chondritis is made last, after all possible other causes (especially heart disease) have been ruled out.
Treatment
If the diagnosis is verified, then the treatment consists in the appointment of NSAIDs for a short time, physiotherapy, restriction of physical activity for a certain period of time, sometimes injections of an anesthetic together with a steroid into the area of pain localization.
Middle chest pain: possible causes, treatment
Doctors call the phenomenon when a person has pain in the chest in the middle, thoracalgia. There can be a lot of reasons for the appearance of pain syndrome, from the most harmless to quite serious pathologies. In order not to miss an important “alarm bell” from your body, it is best to turn to to a neurologist who will examine you and determine why your chest began to hurt.
In order not to miss an important “alarm bell” from your body, it is best to turn to to a neurologist who will examine you and determine why your chest began to hurt.
Middle chest pain: causes
There can be many reasons why pain appeared in the middle of the chest, so it is worth considering the intensity of the pain syndrome, its frequency and the specific localization of pain. By doing this, it will be possible to narrow the search for pathology leading to unpleasant sensations.
Cardiac pathologies
Pain in the chest is often associated with diseases of the cardiovascular system, the heart. If you feel thoracic all the time, this may indicate an aortic aneurysm. In this case, the pain in the left or right side of the chest is felt for a long time, and it will become stronger every time the person moves from rest to physical activity. The condition is treated exclusively surgically, so hospitalization will be required to confirm this diagnosis.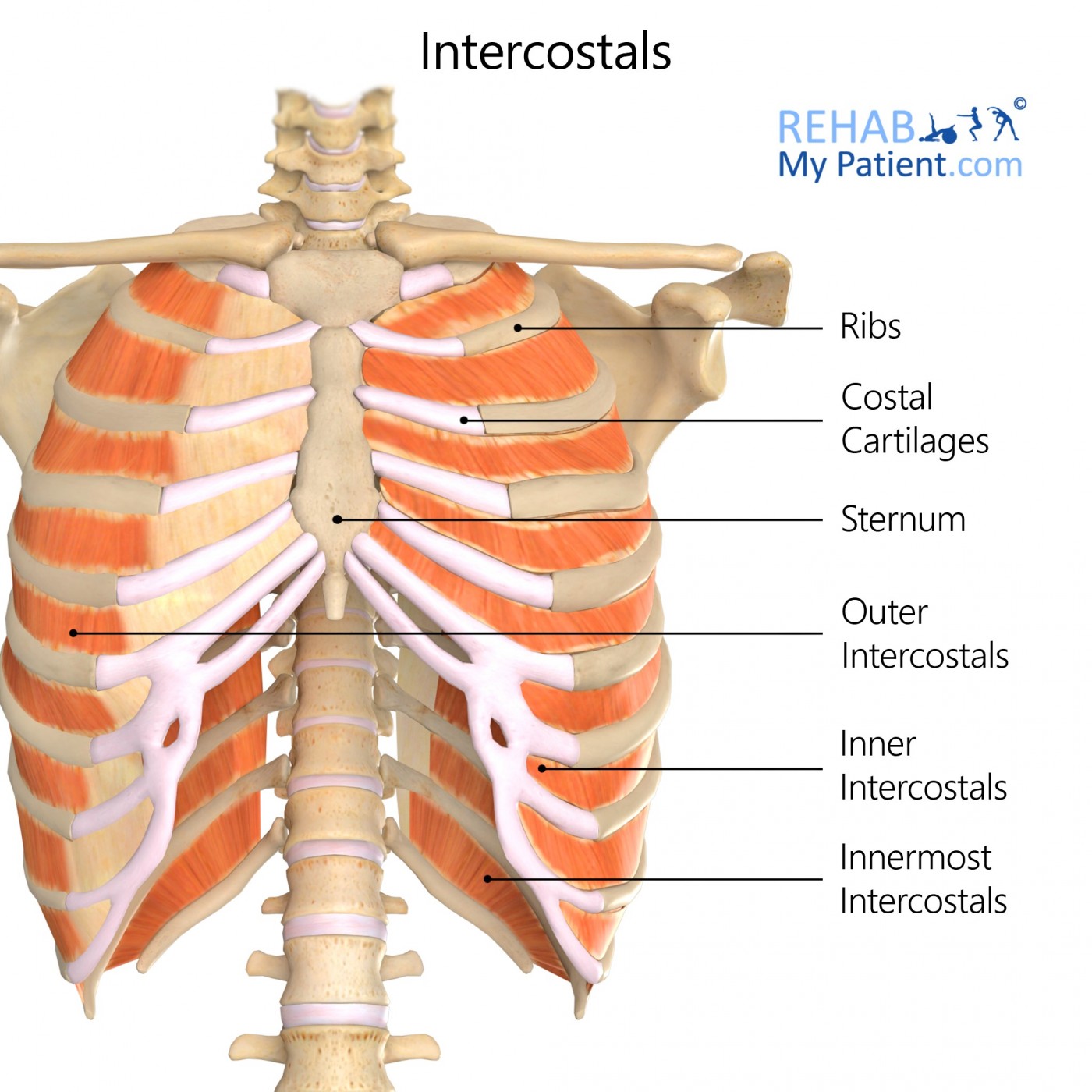 Pain in the center of the chest in front can also appear if a pulmonary embolism develops. The pain syndrome becomes stronger on inspiration, and taking analgesics allows you to suppress it. Compressive pain may indicate that a person has angina pectoris, and pain can also be a symptom of myocardial infarction.
Pain in the center of the chest in front can also appear if a pulmonary embolism develops. The pain syndrome becomes stronger on inspiration, and taking analgesics allows you to suppress it. Compressive pain may indicate that a person has angina pectoris, and pain can also be a symptom of myocardial infarction.
Respiratory damage
If there is pain in the front in the center of the chest, and at the same time you feel interruptions in breathing, you cannot breathe deeply, cough and shortness of breath appear, the problem may be the occurrence of pulmonary diseases, which include tracheitis, pneumonia, bronchitis, pleurisy and some others. The same symptoms can occur with diseases of the diaphragm.
Injuries
Pain in front of the chest, in the middle, or between the ribs may occur in a person who has survived an accident, has been involved in a fight, or has damaged chest structures from a fall or blow. Such pains intensify when he tries to turn around, bend down, take a deep breath, and are explained by the fact that blood vessels rupture, the periosteum is damaged, cracks and fractures form. In such a situation, at rest, the pain syndrome can disappear almost completely, which gives a person a false confidence that there is no need to consult a doctor.
In such a situation, at rest, the pain syndrome can disappear almost completely, which gives a person a false confidence that there is no need to consult a doctor.
Diseases of the spine
The most common reason why the chest hurts in the middle is osteochondrosis, if we talk about the pathologies of the spinal column. Pain in osteochondrosis can be constant or manifest in the form of seizures. The pain will be the same in intensity and manifestation with radiculopathy in the thoracic spine. Also, pain syndrome can indicate an intervertebral hernia and congenital anomalies in the structure of the spinal column.
Neurological diseases
Causes of pain in the chest in the middle can be neuralgic in nature. The most common diagnosis in this case is intercostal neuralgia, in which it is very painful in the sternum, it radiates to the back under the shoulder blade, which makes it easy for a person to confuse pain with heart pain.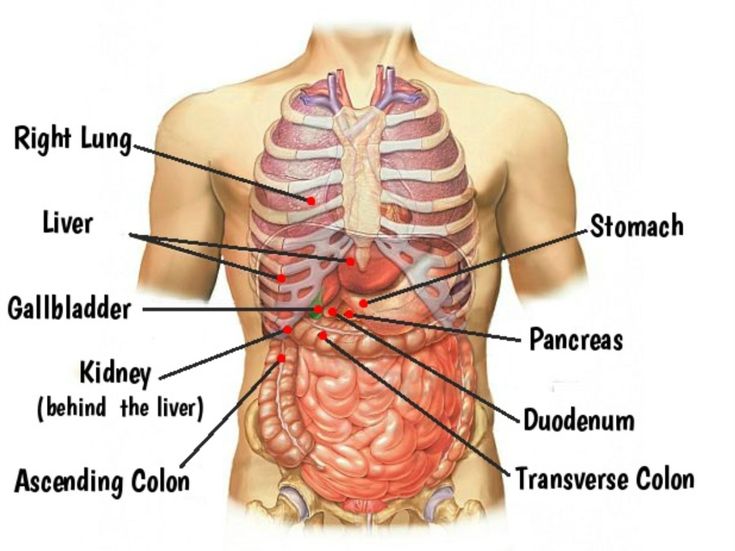
Esophageal problems
Pain in the shoulder blades and in the middle of the chest may be associated with pathologies of the esophagus. The reason in this case is, as a rule, a spasm, which manifests itself more often in the morning or after eating. Pain in the chest area is relieved by taking antispasmodic drugs. Often spasms of the esophagus are accompanied by spasm of the muscular walls of the stomach.
How to relieve pain. First Aid
Often a person who has pain in the middle of the chest does not know what to do in such a situation. Some people are in so much pain that they faint. At the same time, a strong fright is observed, the pulse rate increases, the skin turns pale. The first thing to do if suddenly a person has severe pain in the sternum, internal organs and spine:

Also, if a person has pain in the middle of the chest, it is best to ask everyone present to leave the room and ensure complete rest for the patient until the ambulance arrives.
Diagnosis
The first thing the doctor will do is to interview and examine the patient, which will narrow the search for pathology by concomitant signs. After that, various diagnostic procedures can be prescribed to determine the cause of the pain syndrome. 9 may be useful0059 magnetic resonance or computed tomography , x-ray , ultrasound , blood tests, etc. This will determine why there are pains in the middle of the chest that radiate to the back, upper limbs or ribs.
Which doctor to contact
If you are able to visit the clinic on your own, you can make an appointment with GP . He will determine the approximate cause of the pain syndrome and the direction of further search, as well as give you directions for diagnostic procedures and, if necessary, to specialized specialists./GettyImages-186449742-56a05fee3df78cafdaa14dcf.jpg)

:max_bytes(150000):strip_icc()/costochondritis-in-fibromyalgia-716178_FINAL-5c92ae8746e0fb0001ac1350.png) The pain may radiate down or more often to the left side of the chest.
The pain may radiate down or more often to the left side of the chest.