Exacerbation of herpes zoster. Herpes Zoster Exacerbation: Symptoms, Complications, and Management
What are the key symptoms of herpes zoster exacerbation. How can complications of shingles be identified and managed. What are the risk factors for developing herpes zoster.
Understanding Herpes Zoster: Causes and Clinical Features
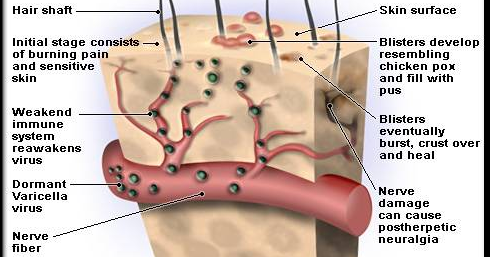
Herpes zoster, commonly known as shingles, is a viral infection caused by the reactivation of the varicella-zoster virus (VZV). This is the same virus responsible for chickenpox (varicella). After an individual experiences chickenpox, the virus remains dormant in the dorsal root ganglia, with the potential to reactivate later in life, resulting in herpes zoster.
The clinical features of herpes zoster are distinct and typically manifest as follows:
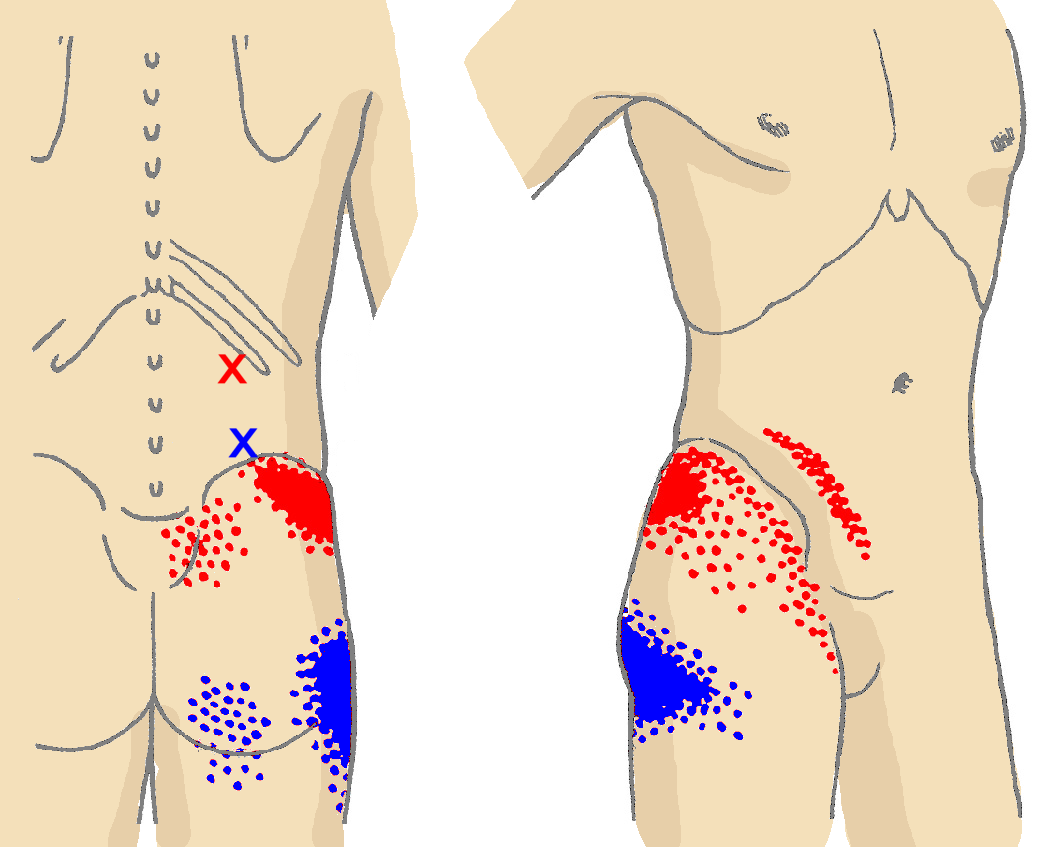
- A painful, itchy, or tingly rash appearing in one or two adjacent dermatomes
- Rash commonly located on the trunk along a thoracic dermatome or on the face
- Rash usually does not cross the body’s midline
- Development of vesicle clusters over 3 to 5 days
- Progressive drying and scabbing of the rash
- Healing typically occurs within 2 to 4 weeks
Can herpes zoster symptoms appear before the rash. Indeed, several days prior to the rash’s emergence, individuals may experience:

- Headache
- Photophobia (sensitivity to bright light)
- Malaise
Identifying and Managing Herpes Zoster Complications
While herpes zoster itself can be distressing, it’s the potential complications that often cause the most concern. Understanding these complications is crucial for proper management and prevention of long-term sequelae.
Postherpetic Neuralgia (PHN)
Postherpetic neuralgia is the most common complication of herpes zoster. It is characterized by persistent pain in the area where the rash was located, continuing for more than 90 days after the onset of the rash. PHN can significantly impact quality of life, with some patients experiencing symptoms for months or even years.
Who is at higher risk for developing PHN. The risk factors include:
- Advanced age (more common and severe in older adults)
- Experiencing intense pain during the active herpes zoster infection
- Having a large rash area
Is PHN common in younger individuals. PHN is rare in people under 40 years old, with approximately 10% to 18% of all herpes zoster patients developing this complication.

Herpes Zoster Ophthalmicus
When herpes zoster affects the ophthalmic division of the trigeminal nerve, it’s termed herpes zoster ophthalmicus. This condition can lead to severe ocular complications, including:
- Acute or chronic eye problems
- Potential vision loss
Disseminated Zoster
Disseminated zoster is a serious complication characterized by widespread skin eruptions and potential visceral involvement. This condition can be difficult to distinguish from varicella and may affect:
- The central nervous system (meningoencephalitis)
- Lungs (pneumonitis)
- Liver (hepatitis)
Who is most at risk for disseminated zoster. This complication generally occurs in individuals with compromised or suppressed immune systems, who are also more likely to experience severe and prolonged rashes.
Vaccination: A Preventive Measure Against Herpes Zoster
Prevention is often the best approach when dealing with viral infections like herpes zoster. The recombinant zoster vaccine (RZV, Shingrix) is currently the recommended vaccine to prevent shingles and its related complications.

How effective is the Shingrix vaccine. Studies have shown that Shingrix is highly effective in reducing the risk of herpes zoster and postherpetic neuralgia in adults aged 50 and older. It provides strong protection against shingles for at least the first four years after vaccination.
For detailed information about vaccination recommendations, individuals should consult the official Shingles Vaccination guidelines provided by health authorities.
Transmission and Infection Control Measures
Understanding the transmission of herpes zoster is crucial for preventing its spread and protecting vulnerable populations. People with active herpes zoster lesions can transmit VZV, potentially causing varicella in individuals who have never had chickenpox or received the varicella vaccine.
How long are herpes zoster lesions infectious. Active lesions remain infectious through direct contact with vesicular fluid or inhalation of virus particles from the blisters until they dry and scab over.
To prevent transmission, individuals with active herpes zoster should:
- Cover their lesions
- Avoid contact with susceptible people in their household and occupational settings
- Maintain these precautions until lesions are dry and scabbed
Healthcare settings require special attention to prevent VZV transmission from herpes zoster cases. Implementing proper infection control measures is essential to protect both patients and healthcare workers.
Epidemiology and Risk Factors for Herpes Zoster
Herpes zoster can affect anyone who has had varicella, but certain factors increase the risk of developing this condition. Understanding these risk factors can help in identifying high-risk individuals and implementing preventive measures.
How common is herpes zoster. Approximately 1 in 3 people in the United States will develop herpes zoster during their lifetime. While most people experience only one episode, recurrence is possible.
The risk of herpes zoster and related complications increases sharply after 50 years of age. This increased risk is attributed to the decline in VZV-specific cell-mediated immunity, which can result from:

- Advancing age
- Medical conditions that suppress the immune system
- Medications that compromise immune function
Who is at higher risk for developing herpes zoster. Individuals with the following conditions have an increased risk:
- Bone marrow or solid organ transplant recipients
- Cancer patients, especially those with leukemia and lymphoma
- People living with HIV
- Individuals taking immunosuppressive medications, including steroids for autoimmune diseases
Management Strategies for Herpes Zoster Exacerbation
When dealing with herpes zoster exacerbation, prompt and appropriate management is crucial to alleviate symptoms and prevent complications. The approach to management typically involves a combination of antiviral therapy, pain management, and supportive care.
Antiviral Therapy
Antiviral medications are the cornerstone of herpes zoster treatment. They help to:
- Reduce the severity and duration of the rash
- Alleviate acute pain
- Potentially decrease the risk of postherpetic neuralgia
Which antiviral medications are commonly prescribed for herpes zoster. The most frequently used antivirals include:
-Step-13.jpg)
- Acyclovir
- Valacyclovir
- Famciclovir
These medications are most effective when started within 72 hours of rash onset. However, they may still be beneficial if initiated later, especially in cases of continued new vesicle formation or in immunocompromised patients.
Pain Management
Pain associated with herpes zoster can be severe and debilitating. A multimodal approach to pain management is often necessary and may include:
- Over-the-counter analgesics (e.g., acetaminophen, ibuprofen)
- Topical treatments (e.g., lidocaine patches, capsaicin cream)
- Opioid medications for severe pain
- Anticonvulsants or antidepressants for neuropathic pain
Supportive Care
Supportive measures can help alleviate symptoms and promote healing. These may include:
- Cool compresses to soothe the affected area
- Calamine lotion to reduce itching
- Keeping the rash clean and dry to prevent bacterial infection
- Loose-fitting clothing to minimize friction on the affected area
Long-term Monitoring and Follow-up Care
The management of herpes zoster doesn’t end with the resolution of the acute rash. Long-term monitoring and follow-up care are essential, particularly for patients at risk of complications or those who have developed chronic conditions like postherpetic neuralgia.

Monitoring for Complications
Regular follow-up appointments allow healthcare providers to assess for potential complications, such as:
- Persistent pain indicative of postherpetic neuralgia
- Signs of bacterial superinfection
- Ocular complications in cases of herpes zoster ophthalmicus
Management of Chronic Pain
For patients who develop postherpetic neuralgia, ongoing pain management is crucial. This may involve:
- Adjustment of pain medications
- Referral to a pain specialist
- Consideration of interventional pain management techniques
How long should patients be monitored after herpes zoster. The duration of follow-up care varies depending on the individual case. Patients with uncomplicated herpes zoster may require only short-term follow-up, while those with persistent symptoms or complications may need long-term monitoring.
Psychological Support
The chronic pain associated with postherpetic neuralgia can have significant psychological impacts. Providing appropriate support is essential and may include:

- Referral to mental health professionals
- Support groups for chronic pain patients
- Education on coping strategies and stress management techniques
By implementing comprehensive long-term care strategies, healthcare providers can help improve outcomes and quality of life for patients who have experienced herpes zoster exacerbation.
Clinical Overview of Herpes Zoster (Shingles)
Cause
Herpes zoster, also known as shingles, is caused by reactivation of varicella-zoster virus (VZV), the same virus that causes varicella (chickenpox).
Primary infection with VZV causes varicella. After a person has varicella, the virus remains latent in the dorsal root ganglia. VZV can reactivate later in a person’s life and cause herpes zoster, a painful maculopapular and then vesicular rash.
Clinical Features
People with herpes zoster most commonly have a rash in one or two adjacent dermatomes. The rash most commonly appears on the trunk along a thoracic dermatome or on the face and it usually does not cross the body’s midline.
The rash is usually painful, itchy, or tingly. A person can experience the following symptoms several days before the rash appears:
- Headache
- Photophobia (sensitivity to bright light)
- Malaise
The rash develops into clusters of vesicles. New vesicles continue to form over 3 to 5 days, and the rash progressively dries and scabs over. The rash usually heals in 2 to 4 weeks. Permanent skin discoloration and scarring can occur.
New vesicles continue to form over 3 to 5 days, and the rash progressively dries and scabs over. The rash usually heals in 2 to 4 weeks. Permanent skin discoloration and scarring can occur.
Complications
Postherpetic neuralgia (PHN)
PHN is the most common complication of herpes zoster. PHN is pain that persists in the area where the rash once was located and continues more than 90 days after rash onset. PHN can last for months or even years.
A person’s risk of having PHN after herpes zoster increases with age. Older adults are more likely to have longer lasting, more severe pain. Approximately 10% to 18% of people with herpes zoster will have PHN. PHN is rare in people younger than 40 years old. The likelihood of PHN is also higher in people who experience more pain with the rash or have a large rash.
Herpes zoster ophthalmicus
Herpes zoster that affects the ophthalmic division of the trigeminal nerve is called herpes zoster ophthalmicus. This can result in acute or chronic ocular sequelae, including vision loss.
Disseminated zoster
Disseminated zoster can include generalized skin eruptions where the lesions occur outside of the primary or adjacent dermatomes. It can be difficult to distinguish from varicella. Visceral involvement of the central nervous system (meningoencephalitis), lungs (pneumonitis), and liver (hepatitis) can also occur. Disseminated zoster generally occurs in people with compromised or suppressed immune systems.
People with compromised or suppressed immune systems are more likely to have a severe, long-lasting rash and experience more severe complications from herpes zoster.
Vaccination
Recombinant zoster vaccine (RZV, Shingrix) is the recommended vaccine to prevent shingles and related complications. For information about vaccination recommendations see Shingles Vaccination.
Transmission
People with active herpes zoster lesions can spread VZV , which causes varicella in people who never had varicella or never received varicella vaccine.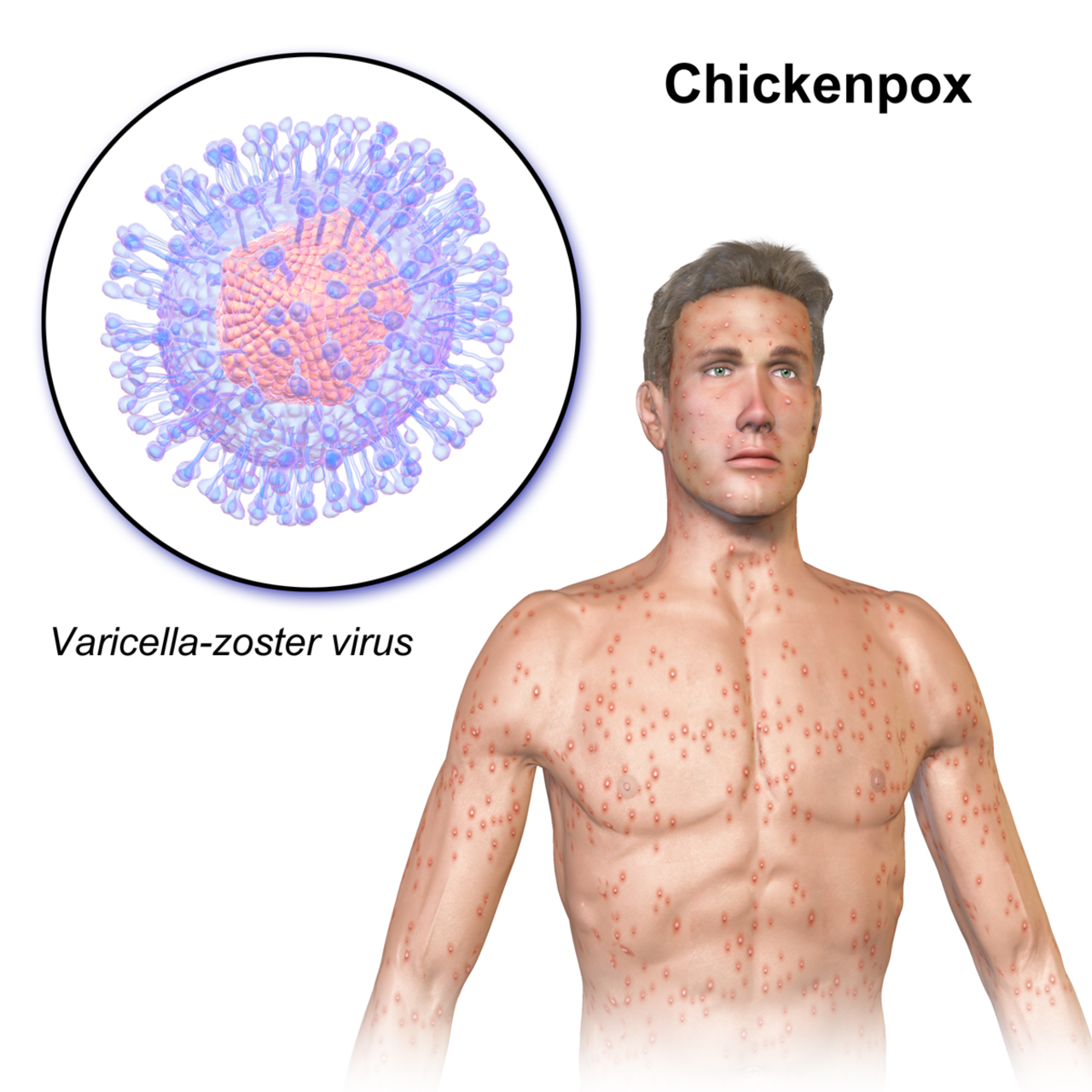 Once varicella resolves, these people would be at risk for herpes zoster.
Once varicella resolves, these people would be at risk for herpes zoster.
Active herpes zoster lesions are infectious through direct contact with vesicular fluid or through breathing in virus particles from the blisters until they dry and scab over. People with active herpes zoster lesions should cover their lesions and avoid contact with susceptible people in their household and in occupational settings until their lesions are dry and scabbed.
Also see Managing People at High Risk for Severe Varicella and Preventing VZV Transmission from Herpes Zoster in Healthcare Settings
Top of Page
Epidemiology
Risk Factors
Anyone who had varicella can develop herpes zoster. Approximately 99.5% of people born before 1980 in the United States were infected with wild-type VZV. Children who receive varicella vaccine have a lower risk of herpes zoster compared with children who were infected with wild-type VZV.
Approximately 1 in 3 people in the United States will develop herpes zoster during their lifetime. Most people have only one episode; however, herpes zoster can recur.
Most people have only one episode; however, herpes zoster can recur.
A person’s risk for herpes zoster and related complications sharply increases after 50 years of age. The reasons why VZV reactivates and causes herpes zoster are not well understood. However, a person’s risk for herpes zoster increases as their VZV-specific cell-mediated immunity declines. This decline in immunity can result from increasing age and medical conditions or medications that suppress a person’s immune system. People with the following conditions that compromise or suppress their immune system have an increased risk for herpes zoster:
- Bone marrow or solid organ (renal, cardiac, liver, and lung) transplant recipients
- Cancer, especially leukemia and lymphoma
- Human immunodeficiency virus (HIV)
- Taking immunosuppressive medications, including steroids, such as for treatment of autoimmune diseases and other immune system deficiencies
Other potential risk factors for herpes zoster have been identified, but the findings are either inconsistent or unexplained. For example:
For example:
- More women than men develop herpes zoster.
- Herpes zoster is less common in Blacks than in Whites.
Disease Rates
An estimated one million cases of herpes zoster occur annually in the United States.
- The incidence of herpes zoster varies by age and is approximately 2–9 cases per 1,000 US population annually.
The precise incidence of recurrence is not known.
Complications
- Approximately 10% to 18% of people with herpes zoster will have PHN.
- Approximately 1% to 4% of people with herpes zoster are hospitalized for complications.
- Older adults and people with compromised or suppressed immune systems are more likely to be hospitalized. About 30% of people hospitalized with herpes zoster have compromised or suppressed immune systems.
Deaths
One study estimated 96 deaths occur each year where herpes zoster was the underlying cause (0.28 to 0.69 per 1 million population). Almost all the deaths occurred in older adults or those with compromised or suppressed immune systems.
Almost all the deaths occurred in older adults or those with compromised or suppressed immune systems.
Trends
Herpes zoster rates among adults in the United States gradually increased over a long period of time. We do not know the reason for this increase. However, the rates across age groups have recently plateaued or declined.
CDC studies have found that herpes zoster rates started increasing before varicella vaccine was introduced in the U.S. and did not accelerate after the routine varicella vaccination program started.
Herpes Zoster in People Who Received Varicella Vaccine
Varicella vaccines contain live attenuated VZV, which results in latent infection. Although herpes zoster has always been uncommon among children, the rate of herpes zoster in U.S. children has declined since the routine varicella vaccination program started in 1996.
- Children (healthy and immunocompromised) vaccinated against varicella have lower rates of herpes zoster compared to children who had natural infection with varicella.

- Vaccinated children are less likely to become infected with wild-type VZV.
- The risk of reactivation of vaccine-strain VZV in children is lower compared with reactivation of wild-type VZV.
- Few older adults have received the varicella vaccine since it was licensed in 1995. There is very little information on the risk of herpes zoster in people who got varicella vaccine as adults.
CDC continues to monitor the impacts of the U.S. varicella and herpes zoster vaccination programs among adults and children.
References
- CDC. Use of Recombinant Zoster Vaccine in Immunocompromised Adults Aged ≥19 Years: Recommendations of the Advisory Committee on Immunization Practices — United States, 2022. MMWR Recomm Rep. 2022;71(3):80-84.
- Leung et al. The Impact of Universal Varicella Vaccination on Herpes Zoster Incidence in the United States: Comparison of Birth Cohorts Preceding and Following Varicella Vaccination Program Launch.
 Journal of Infection Diseases. 2022.
Journal of Infection Diseases. 2022. - Harpaz and Leung. The Epidemiology of Herpes Zoster in the United States During the Era of Varicella and Herpes Zoster Vaccines: Changing Patterns Among Older Adults. Clin Infect Dis.2019;69(2):341-344.
- CDC. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP) Recommendations for use of Herpes Zoster Vaccines. MMWR Recomm Rep. 2018;67(03):103-108.
- Thomas SL, Hall AJ. What does epidemiology tell us about risk factors for herpes zoster? Lancet Infect Dis. 2004;4(1):26-33.
- Tseng HF, Smith N, Harpaz R, et al. Herpes zoster vaccine in older adults and the risk of subsequent herpes zoster disease. JAMA. 2011;305(2):160-6.
- Mahamud A, Marin M, Nickell SP, et al. Herpes zoster-related deaths in the United States: validity of death certificates and mortality rates, 1979-2007. Clin Infect Dis.2012;55(7):960-6.
- Leung J, Harpaz R, Molinari NA, et al.
 Herpes zoster incidence among insured persons in the United States, 1993-2006: evaluation of impact of varicella vaccination. Clinical Infectious Diseases. 2011;52(3):332-340.
Herpes zoster incidence among insured persons in the United States, 1993-2006: evaluation of impact of varicella vaccination. Clinical Infectious Diseases. 2011;52(3):332-340. - Yih W, Brooks D, Lett S, et al. The Incidence of varicella and herpes zoster in Massachusetts as measured by the Behavioral Risk Factor Surveillance System (BRFSS) during a period of increasing varicella vaccine coverage. BMC Public Health. 2005;5(68).
- Jumaan AO, Yu O, Jackson LA, et al. Incidence of herpes zoster, before and after varicella vaccination-associated decreases in the incidence of varicella. Journal of Infectious Diseases. 2005;191:2002-7.
- Hales CM, Harpaz R, Joesoef MR, Bialek SR. Examination of links between herpes zoster incidence and childhood varicella vaccination. Annals of Internal Medicine. 2013;159(11):739-45.
- Russell ML, Dover DC, Simmonds KA, Svenson LW. Shingles in Alberta: before and after publicly funded varicella vaccination.
 Vaccine. 2014;32(47):6319-24.
Vaccine. 2014;32(47):6319-24. - Weinmann S, Chun C, Schmid DS, et al. Incidence and clinical characteristics of herpes zoster among children in the varicella vaccine era, 2005–2009. Journal of Infection Diseases. 2013;208(11):1859-68.
- Hardy I, Gershon AA, Steinberg SP, LaRussa P. The incidence of zoster after immunization with live attenuated varicella vaccine. A study in children with leukemia. Varicella Vaccine Collaborative Study Group. N Engl J Med. 1991;325(22):1545-50.
Top of Page
What Causes Shingles to Activate and What to Do About It
People over 50 are most susceptible to developing shingles as the primary risk factor for shingles is a weakened immune system.
If you contract the chickenpox virus, also known as varicella-zoster, your illness will typically clear up in a week or two. However, this virus remains in your body even after you’ve recovered.
The virus lies dormant when your immune system is strong.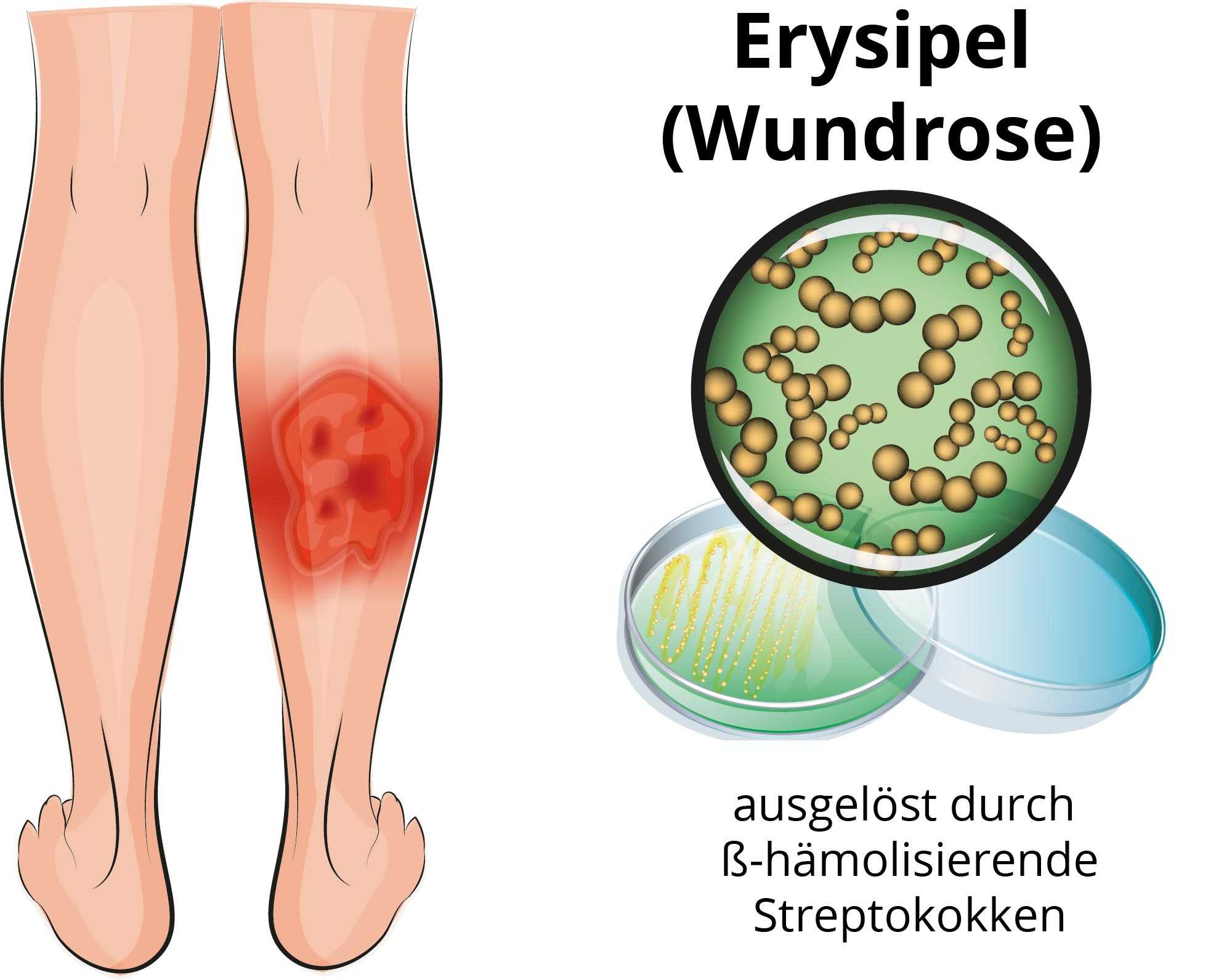 But if something causes you to become immunocompromised, the virus can reactivate. This triggers shingles.
But if something causes you to become immunocompromised, the virus can reactivate. This triggers shingles.
Shingles, known by its medical name herpes zoster, presents as a painful rash. It typically shows up on only one side of your body.
According to the Centers for Disease Control and Prevention (CDC), the chance of getting shingles at some point in your life is 1 in 3.
When you first contract the varicella-zoster virus (VZV), you’ll get chickenpox. When you fight off this virus, your body creates immunity to it, so it’s very rare to get chickenpox a second time.
However, that doesn’t mean that your body rids itself of the virus entirely. Though a strong immune system will keep the virus inactive, it’s still there for the rest of your life.
If your immune system becomes weakened or compromised, it’s possible for this virus to reactivate. A painful shingles rash may result.
Prior to the development of the varicella vaccine, chickenpox was a common childhood illness. Most people were exposed to VZV in childhood and developed chickenpox in their younger years.
Most people were exposed to VZV in childhood and developed chickenpox in their younger years.
In fact, doctors once encouraged families to expose their kids to chickenpox at an early age — after age 10 or so, the disease can be much more severe. (You may remember “chickenpox parties,” where parents actively tried to get their children to contract the virus.)
Adults who come down with chickenpox can experience serious and even life threatening complications like lung or brain infections.
These days, children and adults can receive the varicella vaccine. This weaker version of the live virus causes the body to launch an immune response so that it recognizes — and fights off — VZV in the future.
Getting a varicella vaccine appears to reduce the risk of shingles, but it isn’t a guarantee against them. Though weakened, the virus does continue to stay in your body, so it’s possible for it to reactivate and cause shingles. However, this is uncommon.
One study found that the rate of shingles infection was 78 percent lower in vaccinated children than unvaccinated children.
The varicella vaccine became available in 1995, so only time will tell its effects on the rates of shingles in older adults.
If you’ve had chickenpox or gotten the varicella vaccine, you can develop shingles.
According to the CDC, over 99 percent of people in the United States born before 1980 have had chickenpox or been exposed to VZV.
The primary risk factor associated with getting shingles is a weakened immune system. When your immune system isn’t functioning properly, VZV can reactivate.
As you age, your immune system doesn’t fight off invaders as well. Older age is associated with greater likelihood of health problems, including:
- a natural decline in immunity
- the use of immunosuppressant medications like chemotherapy, long-term corticosteroids, and anti-inflammatory medications
- certain diseases and conditions that damage your immune system, such as HIV and hypogammaglobulinemia
- autoimmune diseases that are treated with immune-suppressing drugs, such as rheumatoid arthritis, Crohn’s disease, and lupus
- procedures like bone marrow transplants and kidney transplants, which may require treatment with immunosuppressants afterward
Starting around age 50, your chance of getting shingles goes up. The severity of the disease and the risk of complications also increase with age.
The severity of the disease and the risk of complications also increase with age.
It’s important to remember, too, that stress can negatively affect your immune system. There’s been some interest in whether stressful life circumstances could weaken the immune system, leading to a shingles infection. However, research is contradictory and doesn’t yet offer firm conclusions.
Shingles isn’t a disease you “catch” in the traditional sense. It’s usually a case of VZV reactivating in your system. But people who’ve never had chickenpox can develop shingles after coming into contact with the fluid from shingles blisters. Shingles are no longer contagious after these blisters have crusted over.
Typically, shingles shows up as a painful rash on an area of skin that is supplied by a single nerve. This area, regardless of its location on the body, is known as a dermatome. Look for these hallmarks of a shingles rash:
- A band of blistering lesions may cover red, inflamed skin, often on one side of the torso or face.

- Pain starts out feeling tingly or burning. Other common sensations include itching and numbness.
- The pain progresses in severity over several days.
- It feels like the pain is coming from the organs in your abdomen, like your heart, gallbladder, appendix, or kidneys.
- Sometimes (though rarely) people experience severe pain without a rash, known as zoster sine herpete.
Some people also have other, more general symptoms, like:
- fever
- chills
- headache
Shingles symptoms can last up to 4 weeks or longer.
To diagnose shingles, your doctor will ask you some questions about your symptoms. These may include:
- When did your symptoms start?
- Which symptom did you notice first?
- Are you experiencing pain?
- Where are you having pain?
- Have you had chickenpox?
- Have you had the chickenpox vaccine?
- Have you had the shingles vaccine?
They’ll also evaluate your rash, looking at its pattern, appearance, and location. Doctors can usually diagnose shingles by its distinctive rash and unique symptoms.
Doctors can usually diagnose shingles by its distinctive rash and unique symptoms.
In rare cases, though, if your doctor is uncertain whether you have shingles, you may undergo a diagnostic test. Testing is more common for people with greater risk factors for complications, including:
- people with a weakened immune system
- pregnant people
- newborns
To test for shingles, your doctor will use a swab to take a sample from a skin lesion. This will then be tested for VZV. A positive test indicates that you have shingles.
How to feel better if you have shingles
When you have shingles, you can feel better by trying the following:
- Eat a balanced diet, get lots of rest, and try some gentle exercise.
- Relieve pain and itching by soaking in a bathtub of lukewarm water and ground-up oatmeal.
- Reduce pain and promote healing of lesions by applying a cool, wet washcloth or compress to the rash.
- Do what you can to limit stress. A stressful lifestyle can weaken your immune system, worsening your symptoms.
- Wear loose-fitting clothes that won’t irritate the rash.
- Keep the lesions covered with a bandage. Prior to putting on the bandage, apply a thin layer of petroleum jelly to prevent irritation.
Although there’s no cure for shingles, the good news is that it resolves on its own. Your doctor may recommend certain medications to alleviate pain or treat infection.
Antiviral medication
Three antiviral medications are used to treat shingles:
- valacyclovir
- famciclovir
- acyclovir
Valacyclovir and famciclovir are taken three times per day. They’re usually preferred over acyclovir, which must be taken five times a day.
All three have a 7-day course if you have an uncomplicated case of shingles. If the shingles is complicated — if it’s affecting your eyes, for example — your doctor will prescribe the medication for longer than 7 days.
Antiviral medication can help:
- you recover faster
- limit the severity of your symptoms
- reduce your risk for complications
Antiviral medications offer the most benefit for people over 50 and those who are immunocompromised, since these risk factors are associated with more persistent, severe shingles symptoms.
It’s best to start an antiviral while you’re still developing new skin lesions, usually within 72 hours of noticing your first symptom. Antivirals won’t be effective after your lesions have begun to crust over.
Some people may need to take a longer course of antiviral medications or even be treated in the hospital with antivirals. This is more likely if you have the following:
- a weakened immune system
- a severe case of shingles
- a high risk of complications
Some people experience shingles on the face. This can lead to serious complications, such as:
- blindness
- hearing impairment
- brain swelling
Seek immediate medical attention if you think you have shingles on your face.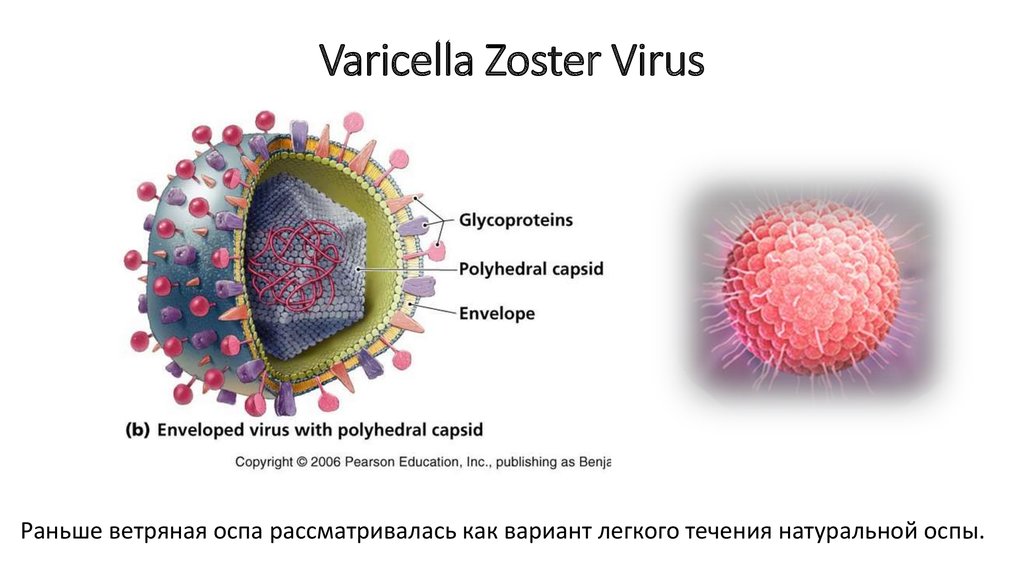
Pain medication
Mild shingles pain may improve with over-the-counter anti-inflammatory medications. Your doctor may recommend ibuprofen or acetaminophen or weak opioids, such as codeine or tramadol.
Stronger prescription opioid pain medication, such as hydrocodone, may be prescribed to treat moderate to severe shingles pain.
Another option is topical pain relievers, such as lidocaine. These are applied directly to your skin for relief. You can find topical pain relievers as ointments, creams, gels, sprays, or patches. Capsaicin, which comes in a cream or a patch, may also be helpful.
Other medications that may be used for relief include:
- diphenhydramine
- hydroxyzine
- calamine lotion to soothe itching
- antibiotics, if a bacterial infection develops around the rash
Shingix (recombinant zoster vaccine) is currently the only shingles vaccine available in the United States. It’s given to people over age 50.
Previously, an additional vaccine, Zostavax, was used, but it was phased out in the United States as of November 2020.
According to the CDC, two doses of Shingrix are over 90 percent effective at preventing shingles. You’ll retain at least 85 percent protection for 4 years after being vaccinated.
If you get shingles after being vaccinated, your symptoms will likely be less severe. You’ll also have a lower chance of developing postherpetic neuralgia — a complication where pain remains even after a shingles rash goes away.
Shingles usually follows a pattern of development. It typically progresses with the following symptoms:
- First, you may notice a tingling or burning sensation in your skin.
- One to 5 days later (or concurrent with the initial pain) a rash appears as small red spots.
- Fluid-filled blisters develop a few days later.
- After 7 to 10 days, the lesions crust over.
- The rash disappears over the next 2 to 4 weeks.
In some cases, pain may persist for several months or even years after the rash has disappeared. This complication, known as postherpetic neuralgia (PHN), can be severe enough to affect your quality of life.
Certain antiseizure medications can help manage the pain. Gabapentin and pregabalin are two that are commonly used.
It’s unlikely to get shingles more than once — but it’s possible. That’s why it’s recommended to get the shingles vaccine at age 50 and older, even if you’ve already had the disease. Getting shingles three times is extremely rare.
Shingles occurs when the varicella-zoster virus is reactivated due to a weakened immune system. This can create a painful, blistering rash. The risk of getting shingles goes up with age, with increased likelihood after age 50.
Shingles often doesn’t require treatment to make it go away, but some antiviral medications can help you recover faster and reduce your risk for complications.
Shingles (Herpes zoster) – treatment in adults and children, symptoms, is it contagious, prevention, which doctor treats
I confirm
More
Herpes
Rash
Intoxication
604
August, 26th
Shingles (Herpes zoster): causes, symptoms, diagnosis and treatment.
Herpes zoster is an infectious disease whose causative agent (herpesvirus type 3) also causes chicken pox.
Since the virus, penetrating into sensitive nerve endings, is integrated into the genetic apparatus of nerve cells, it is impossible to remove it from the body. In those who have had chickenpox, the virus goes into a latent (inactive) state.
When the immune system is weakened, the virus is activated, affecting the skin. The disease often develops in the elderly and in immunocompromised individuals.
Causes of disease
The virus is transmitted from a patient with chicken pox or herpes zoster by contact or airborne droplets. The person who becomes infected primarily (most often a child) gets chickenpox. Penetrating through the mucous membranes into the blood and lymph, the virus reaches the nerve cells, where it begins to multiply. After recovery, the virus remains in the body for life, often being in an inactive state. The awakening of the infection is associated with weakened immunity caused by hypothermia, long-term use of steroid hormones, immunosuppression (after transplantation), chemotherapy and radiation therapy, as well as a general decrease in immunity in patients with blood diseases, oncological and viral diseases. Shingles is very severe in HIV-infected patients.
Classification of herpes zoster
The clinical picture of herpes zoster consists of skin manifestations and neurological disorders. There are typical and atypical forms of the disease. With an atypical form, an erased course of the disease is possible, in which papules develop in the foci of hyperemia, which do not transform into vesicles.
There are typical and atypical forms of the disease. With an atypical form, an erased course of the disease is possible, in which papules develop in the foci of hyperemia, which do not transform into vesicles.
In herpes zoster, the spread of the pathological process corresponds to a certain area of the skin and does not cross the anatomical midline of the trunk. In most patients, the rash is preceded by a burning or itching sensation in a specific area of the skin, as well as pain, which can be stabbing, throbbing, shooting, paroxysmal or constant. In a number of patients, the pain syndrome is accompanied by general systemic inflammatory manifestations: fever, malaise, myalgia, and headache.
Infection of the central nervous system and involvement of the meninges can produce meningeal, encephalic (symptoms suggest virus involvement of the brain and/or spinal cord and meninges), or mixed forms of herpes zoster. If the infection spreads along the optic nerve, ophthalmic herpes develops.
When a rash appears over the entire surface of the skin and on parenchymal organs (eg, liver, kidneys), a generalized form of herpes zoster develops. Another type of shingles is hemorrhagic. A characteristic feature is the bloody fluid inside the vesicles.
Symptoms of herpes zoster
The onset of the disease is accompanied by general intoxication, malaise and fever. Nausea and vomiting are possible. Lymph nodes are enlarged.
There are pronounced pains along the affected nerve, which can be permanent, but more often they are paroxysmal itchy in nature, intensifying at night.
As a rule, they are provoked by any irritants: touching the skin, cold, movement. Some patients complain of loss of sensation in certain areas of the skin, which may be combined with increased pain response. Sometimes the pain syndrome in the absence of skin rashes can resemble angina pectoris, myocardial infarction, renal colic, or pancreatitis. The period of neuralgia preceding the rash lasts up to 7 days. Then nodules appear on one side of the body, from which bubbles form with transparent contents, which gradually become cloudy. After 3-7 days, most of the bubbles dry up with the formation of yellow-brown crusts. When the bubbles are injured, bright red sores are exposed. After the sores heal, small scabs or scars remain on the skin.
Then nodules appear on one side of the body, from which bubbles form with transparent contents, which gradually become cloudy. After 3-7 days, most of the bubbles dry up with the formation of yellow-brown crusts. When the bubbles are injured, bright red sores are exposed. After the sores heal, small scabs or scars remain on the skin.
Most often, rash and pain are noted in the region of the ribs, lower back and sacrum, less often along the branches of the trigeminal, facial and ear nerve and on the extremities.
In rare cases, the mucous membranes are affected.
Herpes zoster diagnostics
It is possible to make a diagnosis after examining and questioning the patient. The doctor pays attention to the nature of the rash (localized and unilateral), the type of vesicles and complaints of itchy burning pain. It is more difficult to identify the atypical form of herpes zoster. With an erased form, pain and other neurological symptoms may be absent. In case of neurogenic disorders before the appearance of rashes, the diagnosis can be made on the basis of the results of laboratory tests. In this case, a histological examination is used, and the virus is isolated in cell culture. The Zanck test helps to quickly confirm the herpetic nature of the rashes: giant multinucleated cells are found in the scraping of the material taken from the base of the vesicle. However, this test does not make it possible to determine the type of herpes. The methods of enzyme immunoassay and indirect immunofluorescent reaction are also used. Recently, the diagnosis of viral infections is carried out using the polymerase chain reaction (PCR).
In this case, a histological examination is used, and the virus is isolated in cell culture. The Zanck test helps to quickly confirm the herpetic nature of the rashes: giant multinucleated cells are found in the scraping of the material taken from the base of the vesicle. However, this test does not make it possible to determine the type of herpes. The methods of enzyme immunoassay and indirect immunofluorescent reaction are also used. Recently, the diagnosis of viral infections is carried out using the polymerase chain reaction (PCR).
Antibodies of the IgG class to the Varicella-Zoster virus (Varicella-Zoster Virus IgG, anti-VZV IgG, antibodies of the IgG class to the varicella-zoster virus and shingles)
Synonyms: Blood test for antibodies to the chickenpox virus; Chicken pox; Human herpes virus type 3; HBV-3 type; varicellae-zoster virus; Herpes zoster.
chickenpox; Human h…
Up to 4 business days
Available with house call
RUB 965
Add to cart
Antibodies of the IgM class to the Varicella-Zoster virus (Varicella-Zoster Virus IgM, anti-VZV IgM, antibodies of the IgM class to the varicella-zoster virus and herpes zoster)
Synonyms: Blood test for antibodies to the chickenpox virus; Chicken pox; Human herpes virus type 3; HBV-3 type; varicellae-zoster virus; Herpes zoster.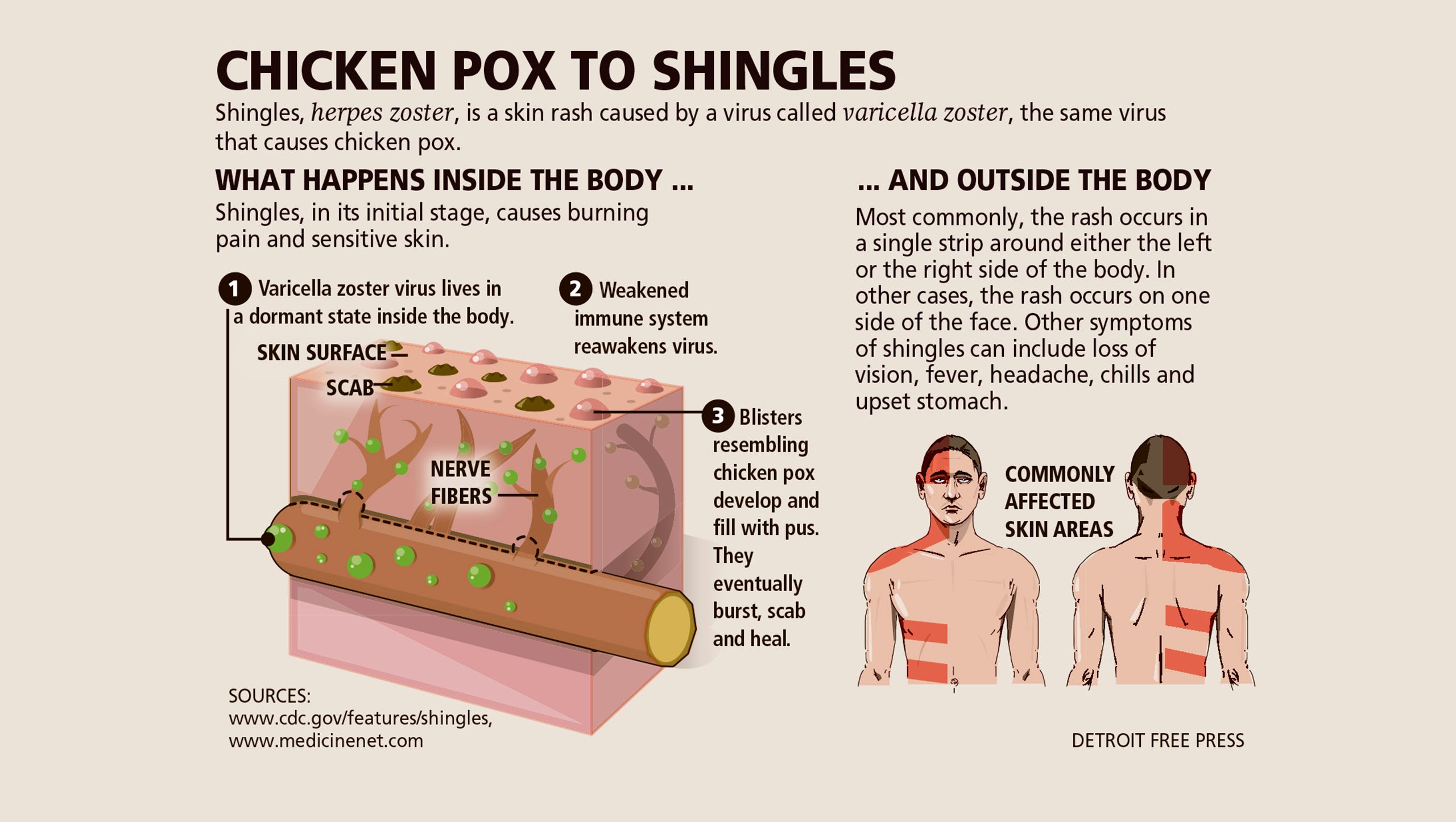
chickenpox; Human herp…
Up to 1 business day
Available with home visit
1 050 RUB
Add to cart
Which doctors to contact
Depending on the primary symptoms, patients with herpes zoster may see different specialists. However, first of all, you should go to
therapist for examination and referrals for tests. If limited, localized skin rashes appear and there are no pain symptoms, it is necessary to contact a dermatologist for differential diagnosis of erysipelas (caused by bacteria), eczema, etc. In case of severe pain syndrome, movement disorders, consultation is necessary
neurologist. In case of damage to the eyes, pain when moving the eyeballs, an ophthalmologist’s consultation is required. The generalized form of herpes often requires hospitalization and the combined efforts of an immunologist, a neurologist, and a dermatologist.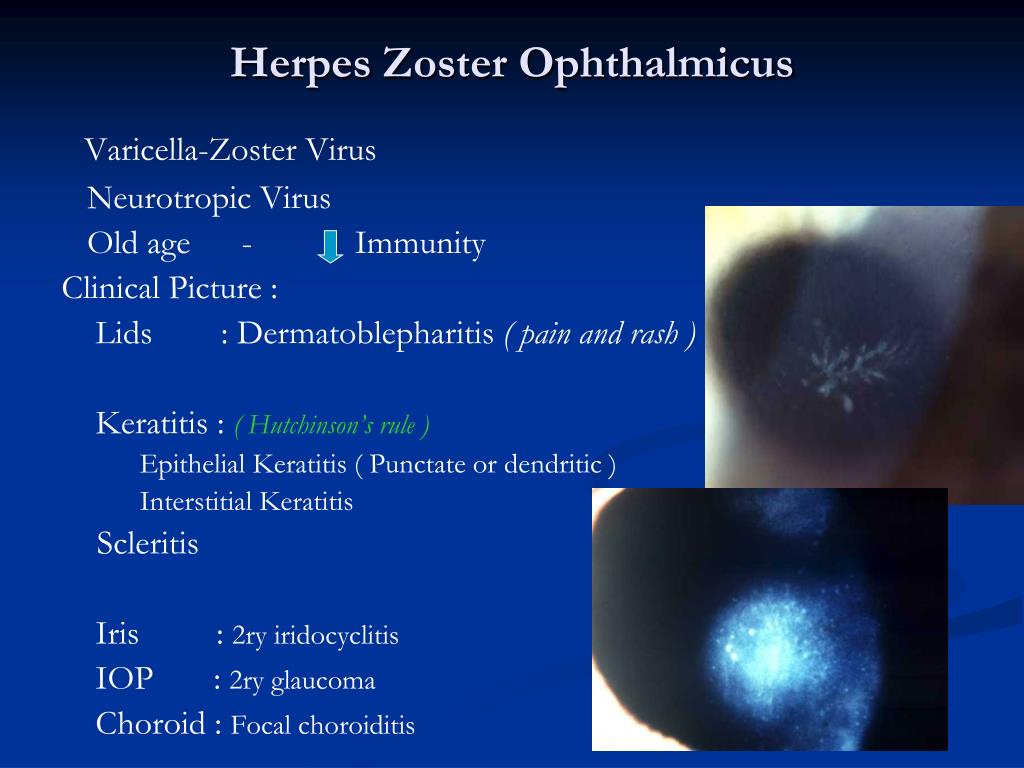
Herpes zoster treatment
With any localization of rashes, antiviral agents are first prescribed (the drug, the frequency of administration and dosage are determined by the attending physician!).
Their action is especially effective in the first 72 hours from the onset of clinical manifestations.
In the presence of a strong pain syndrome, the doctor may recommend anti-inflammatory therapy. However, contraindications must be taken into account (for example, chronic diseases such as arterial hypertension, diabetes mellitus, erosive lesions of the intestine, peptic ulcer of the stomach and duodenum). If analgesics don’t work, your doctor may prescribe central analgesics (often prescription drugs) and nerve blocks. External (topical) treatment is necessary to eliminate inflammation and prevent infection of the skin by other agents (eg, bacteria). With erosive forms of herpes zoster, creams and ointments with antibacterial action are applied to the affected areas.
Your doctor may also recommend treatments to improve immunity, such as taking vitamins (particularly B vitamins).
Complications
When the vesicles open, a secondary infection (bacterial infection of the skin) is possible, which is accompanied by fever and general intoxication.
Typical complications of herpes zoster include neuritis, paresis and paralysis of sensory and motor nerves.
Postherpetic neuralgia is difficult to treat.
The ocular form of herpes can lead to keratitis (inflammation of the cornea), less often to iritis (inflammation of the iris) or glaucoma (increased intraocular pressure). In addition, the development of optic neuritis is possible, sometimes with its subsequent atrophy and blindness. With the defeat of the branch of the oculomotor nerve, ptosis develops (drooping of the upper eyelid). Sometimes patients complain of hearing loss, damage to the vestibular apparatus, in severe cases – paralysis and paresis of the oral cavity. In addition, patients may report tinnitus or increased sensitivity to sounds. Damage to the lumbosacral nerve nodes sometimes leads to urinary retention, constipation or diarrhea. In patients with significantly weakened immunity (with HIV infection, oncological diseases), herpes zoster often occurs in a generalized form and is complicated by meningitis, encephalitis, or meningoencephalitis.
In addition, patients may report tinnitus or increased sensitivity to sounds. Damage to the lumbosacral nerve nodes sometimes leads to urinary retention, constipation or diarrhea. In patients with significantly weakened immunity (with HIV infection, oncological diseases), herpes zoster often occurs in a generalized form and is complicated by meningitis, encephalitis, or meningoencephalitis.
Shingles prevention
Since shingles is caused by the same pathogen as varicella, prevention of the disease will be based on the same measures as with chickenpox.
To prevent the spread of infection, isolation of the patient is necessary, which lasts up to 5 days from the moment the last element of the rash appears.
Persons who have been in contact with a patient with chickenpox are observed for 21 days. Active (vaccination) and passive (immunoglobulin administration) immunization are used as emergency prophylaxis. Vaccination is carried out for children older than 12 months and adults with no contraindications in the first 72-96 hours after probable contact with a person with chickenpox or shingles. Passive immunization with anti-varicella immunoglobulin is indicated for people with low immunity who have contraindications to vaccinations, pregnant women, children under 12 months of age and newborns whose mothers fell ill with chicken pox within 5 days before the birth of the child. The introduction of immunoglobulin is also carried out within 72-96 hours after contact with a patient with chicken pox or herpes zoster.
Passive immunization with anti-varicella immunoglobulin is indicated for people with low immunity who have contraindications to vaccinations, pregnant women, children under 12 months of age and newborns whose mothers fell ill with chicken pox within 5 days before the birth of the child. The introduction of immunoglobulin is also carried out within 72-96 hours after contact with a patient with chicken pox or herpes zoster.
References
- Herpes zoster: Clinical guidelines. Ministry of Health of the Russian Federation. 2016.
- Decree of the Chief State Sanitary Doctor of the Russian Federation dated February 5, 2018 No. 12 on the approval of SP 3.1.3525-18 “Chickenpox and Shingles Prevention”. 2018.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
Photodermatoses
7222
July 20
Tuberculosis of the spine
848
July 13
Chronic cerebral ischemia
877
July, 12
Show more
Cervical cancer
Uterine cancer
Human papillomavirus (HPV)
Herpes
Cervical dysplasia
Cervical dysplasia: causes, symptoms, diagnosis and treatment.
More
Herpes
Lymphadenitis
Chickenpox
Chickenpox: causes, symptoms, diagnosis and treatment.
More
Chickenpox
Herpes
Fungus
Lichen
Lichen: causes, symptoms, diagnosis and treatment.
More
Diarrhea
Intoxication
Paralysis
Paresis of the facial nerve
Botulism
Botulism: causes, symptoms, diagnosis and treatment.
More
Sore throat
Enterovirus
Conjunctivitis
Stomatitis
Hand-foot-mouth syndrome
Myocarditis
Pericarditis 9 0003 Coxsackie virus
Coxsackie virus: causes, symptoms, diagnosis and treatment.
More
Subscribe to our newsletters
Enter e-mail
I consent to
processing of personal data
Subscribe
Herpes zoster (shingles) | Memorial Sloan Kettering Cancer Center
This information tells you about herpes zoster (shingles), including how it spreads and how it is treated.
back to top of page
What is herpes zoster?
Herpes zoster, also called herpes zoster, is an infectious disease caused by the varicella-zoster virus. This is the same virus that causes chickenpox. Herpes zoster occurs only in those individuals who have previously had chickenpox. When chickenpox passes, the varicella-zoster virus remains in the body as inactive. This means that you may not feel symptoms, but the virus is still present in the body. When the varicella-zoster virus becomes active again, it causes herpes zoster.
back to top of page
What are the symptoms of herpes zoster?
Persons with herpes zoster develop a rash similar to chicken pox. It can cause itching, burning and pain.
In localized herpes zoster, the rash usually appears as a wide streak on one side of the body. In disseminated (more widespread) herpes zoster, the rash covers a larger area of the body.
back to top of page
How is herpes zoster spread?
Herpes zoster can be spread by touching the blisters of an infected person.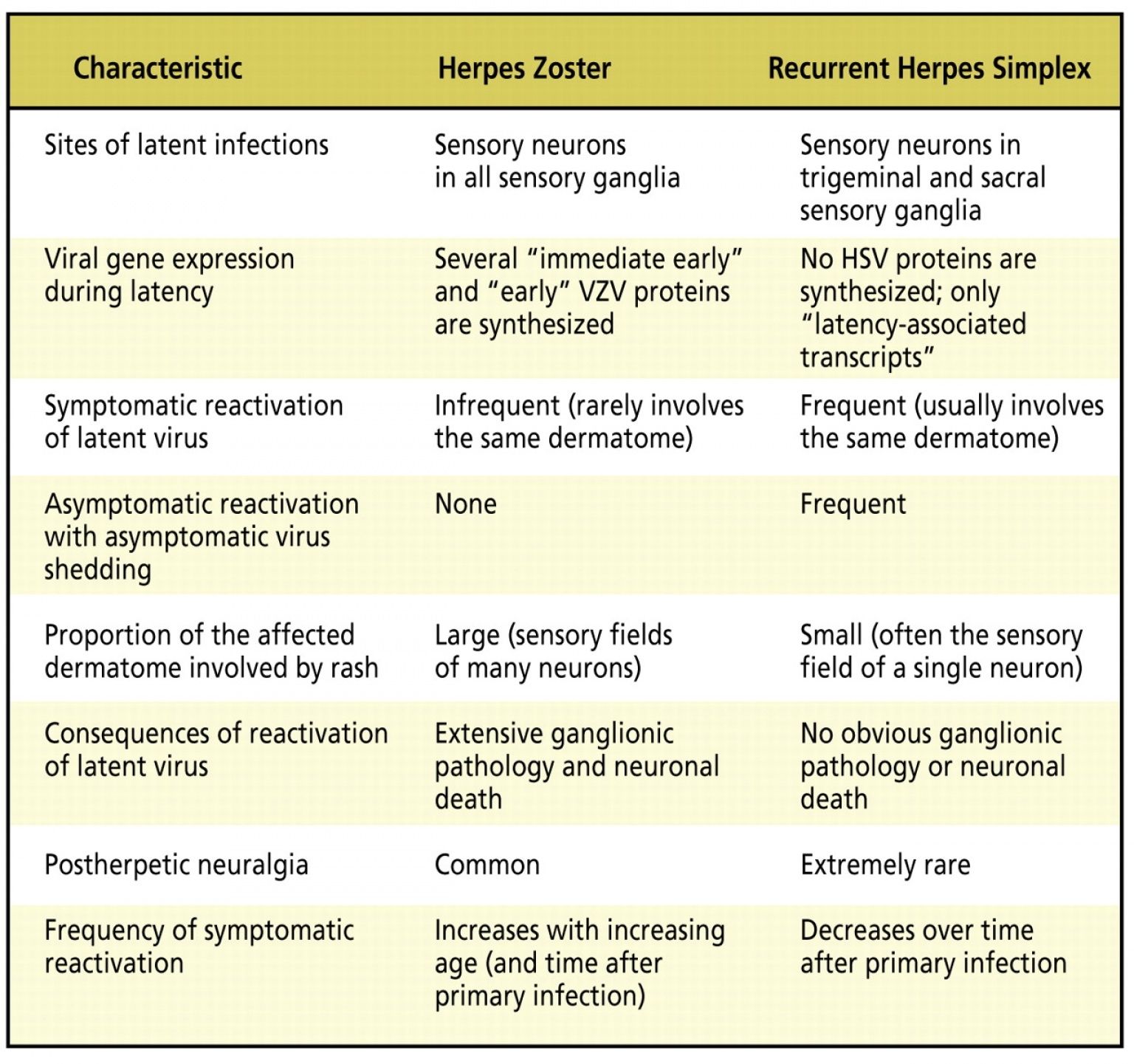 Disseminated herpes zoster can be spread through contact with liquid droplets from the nose and throat of an infected person. Droplets containing the virus are released into the air when an infected person coughs or sneezes. They are easy to inhale and become infected.
Disseminated herpes zoster can be spread through contact with liquid droplets from the nose and throat of an infected person. Droplets containing the virus are released into the air when an infected person coughs or sneezes. They are easy to inhale and become infected.
If you have had chickenpox before, your virus will not become active through contact with a person who has herpes zoster. However, if you haven’t had chickenpox, you can get it after being in contact with someone who has herpes zoster.
back to top of page
Who is at risk of getting herpes zoster?
Herpes zoster usually develops in people with serious illnesses or weak immune systems.
back to top of page
How to treat herpes zoster?
Herpes zoster is treated with antiviral medicines, skin creams and, if necessary, pain medicines.
back to top of page
What precautions are taken in the hospital if I have herpes zoster?
Isolation measures are measures we take to prevent the spread of infection among patients.
If you were diagnosed with chickenpox during your hospital stay or were at risk of contracting the disease:
- You will be placed in a separate room.
- The door to your room should always be closed.
- There will be a sign on your door telling all staff and visitors to wash their hands with soap or alcohol-based hand rub before entering and after leaving your room.
- Isolation measures taken in the case of localized and disseminated herpes zoster are different.
- For localized herpes zoster, all visitors and staff must wear a yellow gown and gloves while in your room. They are issued outside your room and can be disposed of in your room.
- For disseminated herpes zoster, visitors and staff should wear a yellow gown, gloves, and a respiratory mask while in your room.
- If you follow these isolation measures, you are not allowed to walk around the ward.
- With any type of herpes zoster, you are prohibited from walking around the department and access to the following areas of the hospital:
- food pantry in your department;
- recreation center at M15;
- children’s recreation areas in M9;
- cafeteria;
- main lobby;
- any other common areas within the hospital.



 Journal of Infection Diseases. 2022.
Journal of Infection Diseases. 2022. Herpes zoster incidence among insured persons in the United States, 1993-2006: evaluation of impact of varicella vaccination. Clinical Infectious Diseases. 2011;52(3):332-340.
Herpes zoster incidence among insured persons in the United States, 1993-2006: evaluation of impact of varicella vaccination. Clinical Infectious Diseases. 2011;52(3):332-340. Vaccine. 2014;32(47):6319-24.
Vaccine. 2014;32(47):6319-24.