Foot Rash with Blisters: Causes, Symptoms, and Effective Treatments
What are the common causes of foot rashes with blisters. How can you identify different types of foot rashes. What are the most effective treatments for various foot rash conditions. When should you seek medical attention for a foot rash.
Understanding Athlete’s Foot: A Common Fungal Infection
Athlete’s foot, medically known as tinea pedis, is a widespread fungal infection that affects the feet. Caused by the Trichophyton fungus, it thrives in warm, moist environments like shower floors and the insides of shoes. This highly contagious condition can lead to uncomfortable symptoms and, if left untreated, may spread to other parts of the body.
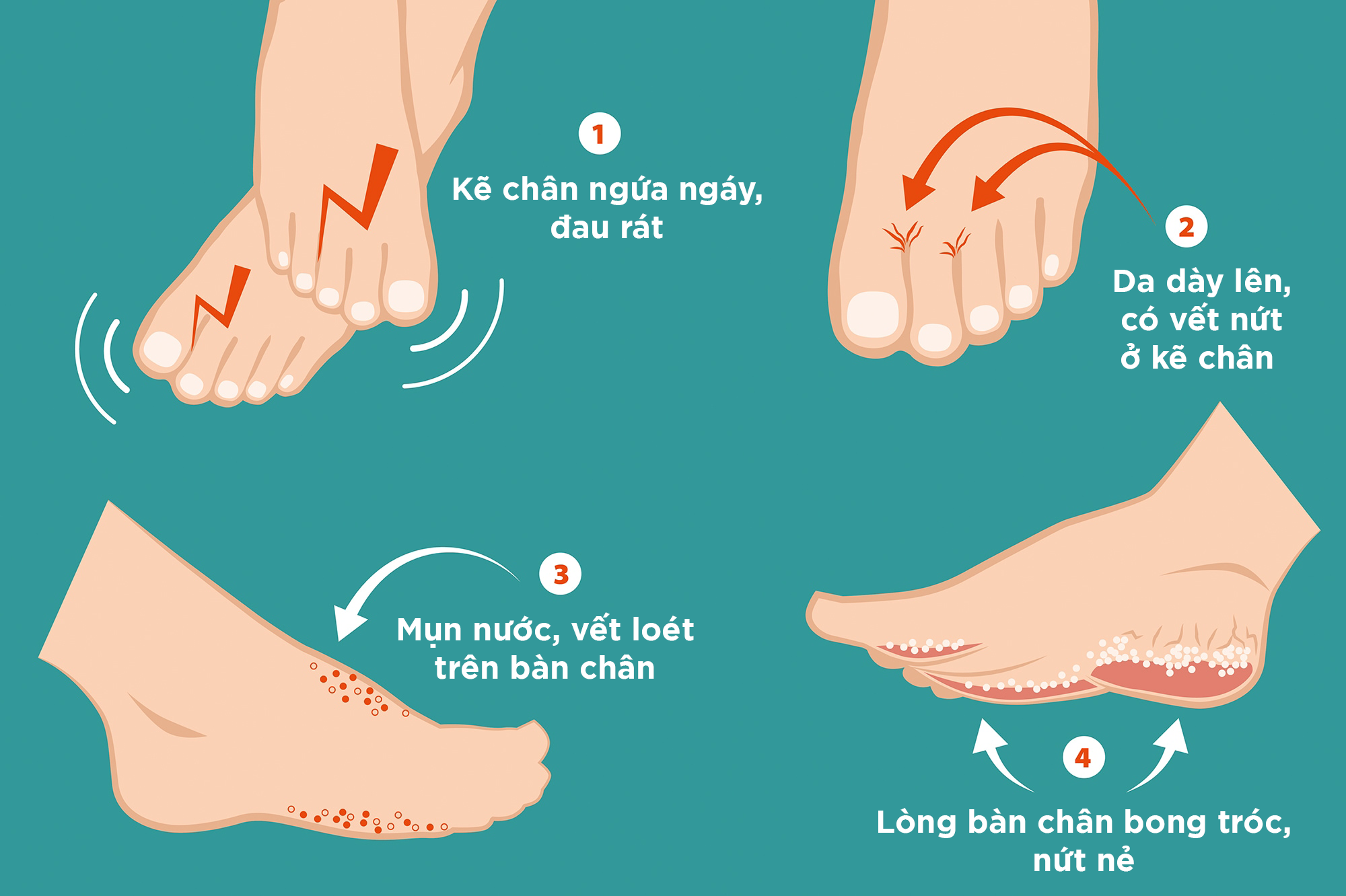
Recognizing Athlete’s Foot Symptoms
What are the telltale signs of athlete’s foot? The most common symptoms include:
- Itchy, burning sensation between the toes
- Dry, scaly, or cracked skin
- Redness and inflammation
- Weakened or discolored toenails
- Blisters on the feet that may crack or ooze
Effective Treatment Options for Athlete’s Foot
How can you treat athlete’s foot effectively? For most cases, over-the-counter antifungal treatments are sufficient. These may come in the form of:

- Oral tablets
- Topical creams or liquids
- Antifungal powders
In more severe cases, a healthcare provider may prescribe stronger antifungal medications. To alleviate inflammation and itching, topical steroids like hydrocortisone can be beneficial. It’s crucial to complete the full course of treatment to prevent recurrence.
Contact Dermatitis: When Your Skin Reacts to Irritants
Contact dermatitis is a skin condition that occurs when the skin comes into contact with irritating substances or allergens. This type of rash can affect any part of the body, including the feet. Understanding the triggers and symptoms of contact dermatitis is essential for proper management and prevention.
Common Triggers of Contact Dermatitis
What substances typically cause contact dermatitis on the feet? Some common culprits include:
- Metals, particularly nickel in shoe buckles or decorations
- Latex in shoes or socks
- Dyes or chemicals used in footwear manufacturing
- Frequent exposure to water or harsh soaps
- Cleaning products like bleach
Managing Contact Dermatitis Symptoms
How can you effectively manage contact dermatitis on your feet? The primary approach involves:

- Identifying and avoiding the triggering substance
- Using antihistamines to reduce itching and inflammation
- Applying topical corticosteroids to alleviate symptoms
- Keeping the affected area clean and moisturized
In most cases, the rash should clear within 1-3 weeks once the irritant is removed. If symptoms persist or worsen, consult a dermatologist for further evaluation and treatment.
Poison Ivy, Oak, and Sumac: Nature’s Itchy Trio
While often associated with hiking or camping, poison ivy, oak, and sumac can also affect the feet, especially for those walking barefoot in affected areas. These plants contain urushiol, an oil that triggers an allergic reaction in 50-75% of adults in the United States.
Identifying a Poison Plant Rash
How can you tell if your foot rash is caused by poison ivy, oak, or sumac? Look for these symptoms:
- Red, itchy skin
- Swelling and tenderness
- Bumps or blisters, often in a linear pattern
- In severe cases, fever or difficulty breathing
Treatment and Prevention of Poison Plant Rashes
What steps should you take if exposed to poison ivy, oak, or sumac? Immediate action is crucial:
- Wash the affected area thoroughly with soap and water
- Clean any contaminated clothing or shoes
- Apply calamine lotion or hydrocortisone cream to relieve itching
- Take oral antihistamines to reduce the allergic reaction
- Seek medical attention if symptoms are severe or widespread
Prevention is key when it comes to poison plant rashes. Wear protective clothing and closed-toe shoes when in wooded or marshy areas, and learn to identify these plants to avoid contact.
Dyshidrotic Eczema: Tiny Blisters, Big Discomfort
Dyshidrotic eczema, also known as dyshidrosis or pompholyx, is a form of eczema characterized by small, itchy blisters on the palms of the hands and soles of the feet. This condition affects women twice as often as men and can be triggered by various factors, including stress, allergies, and exposure to certain metals.
Recognizing Dyshidrotic Eczema
What are the distinguishing features of dyshidrotic eczema? Look for:
- Small, deep-seated blisters on the soles of the feet or toes
- Intense itching and burning sensation
- Scaly, cracked, or flaking skin as blisters heal
- Redness and inflammation in the affected areas
- Possible pain or discomfort when walking
Managing Dyshidrotic Eczema
How can you effectively manage dyshidrotic eczema on your feet? While there’s no cure, several treatments can help:

- Apply topical corticosteroids to reduce inflammation and itching
- Use moisturizers to repair the skin barrier
- Soak feet in cool water to relieve discomfort
- Consider Botox injections to reduce excessive sweating
- Identify and avoid triggers, such as certain metals or stress
For severe cases, a dermatologist may prescribe oral corticosteroids or other immunosuppressants. Consistent management and avoiding triggers are key to controlling dyshidrotic eczema.
Hand, Foot, and Mouth Disease: Not Just for Children
Hand, foot, and mouth disease (HFMD) is a viral infection commonly associated with young children, but it can affect adults as well. Caused by coxsackievirus and enterovirus, HFMD is highly contagious and can spread through direct contact, contaminated surfaces, or respiratory droplets.
Symptoms of Hand, Foot, and Mouth Disease
What signs indicate you might have HFMD? Look for:
- Small, painful blisters on the feet, hands, and in the mouth
- Fever and general malaise
- Sore throat
- Loss of appetite
- Difficulty eating or swallowing due to mouth sores
Managing HFMD Symptoms
How can you alleviate the discomfort of HFMD? While there’s no specific treatment, you can:

- Use over-the-counter pain relievers to reduce fever and discomfort
- Drink cold liquids to soothe a sore throat and stay hydrated
- Apply topical oral anesthetics to relieve mouth sore pain
- Rest and allow your body to fight the virus
- Practice good hygiene to prevent spreading the infection
Most cases of HFMD resolve within 7-10 days. However, if symptoms worsen or persist, consult a healthcare provider for further evaluation.
Cellulitis: When Bacteria Invade the Deeper Layers of Skin
Cellulitis is a bacterial skin infection that can affect the feet and lower legs. It occurs when bacteria, typically streptococcus or staphylococcus, enter through a break in the skin. This condition can be serious if left untreated, potentially leading to systemic infection.
Identifying Cellulitis Symptoms
How can you recognize cellulitis on your feet? Look for these signs:
- Swollen, red, and warm skin
- Tenderness or pain in the affected area
- Skin dimpling or blistering
- Fever and chills
- Fatigue and general malaise
- Swollen lymph nodes near the infection site
Treating Cellulitis
What is the appropriate treatment for cellulitis? This condition requires prompt medical attention:

- Oral antibiotics are typically prescribed to fight the bacterial infection
- In severe cases, intravenous antibiotics may be necessary
- Elevate the affected foot to reduce swelling
- Apply cool compresses to alleviate discomfort
- Rest and avoid putting pressure on the infected area
It’s crucial to complete the full course of antibiotics, even if symptoms improve. If cellulitis recurs or doesn’t respond to treatment, further evaluation may be needed to rule out underlying conditions.
When to Seek Medical Attention for a Foot Rash
While many foot rashes can be managed at home, certain situations warrant professional medical care. Understanding when to seek help is crucial for preventing complications and ensuring proper treatment.
Red Flags for Foot Rashes
When should you consult a healthcare provider for a foot rash? Look out for these warning signs:
- Fever or chills accompanying the rash
- Rapid spread or worsening of the rash
- Signs of infection, such as increased redness, warmth, or pus
- Severe pain or difficulty walking
- Blisters that are large, painful, or filled with blood
- Rash that doesn’t improve with over-the-counter treatments
- Recurrent or chronic rashes
Diagnostic Approaches for Foot Rashes
How do healthcare providers diagnose foot rashes? They may use several methods:

- Visual examination of the affected area
- Review of medical history and recent activities
- Skin scrapings or swabs for laboratory analysis
- Blood tests to check for systemic infections or allergic reactions
- In some cases, a skin biopsy may be necessary
Early intervention can prevent complications and lead to faster resolution of foot rashes. Don’t hesitate to seek medical advice if you’re concerned about a persistent or severe foot rash.
Foot rash: Causes, symptoms, and treatments
A foot rash can occur due to an allergic reaction or infection. Most foot rashes, such as athlete’s foot and contact dermatitis, are treatable with over-the-counter (OTC) medications.
However, other types of foot rashes, such as cellulitis may require medical intervention.
In this article, we list a few common causes of foot rashes along with their symptoms and treatment options.
Tinea pedis, more commonly known as athlete’s foot, is a highly contagious fungal infection that develops on the feet.
A fungus called Trichophyton causes athlete’s foot. This fungus thrives in warm, moist environments, such as shower floors and the inside of shoes.
Athlete’s foot often leads to itchy, burning skin between the toes. Other symptoms of the condition include:
- dry, scaly, or cracked skin
- flushed or raw skin
- weak, discolored toenails
- cracked or oozing blisters on the feet
Treatment
Most people can treat athlete’s foot with an OTC antifungal treatment, usually in the form of an oral tablet or a liquid or cream. More severe infections may require prescription-strength medication.
More severe infections may require prescription-strength medication.
Topical steroids, such as hydrocortisone, can help reduce inflammation and relieve itching and soreness.
Contact dermatitis is a rash that occurs when a substance irritates the skin or produces an allergic reaction.
Substances that may cause contact dermatitis can include:
- metals, such as nickel
- makeup
- latex
- frequent washing or contact with water
- bleach
Treatment
People can avoid the substance that they think is causing contact dermatitis to see whether their rash clears within 1–3 weeks. Antihistamines and topical corticosteroids may help relieve symptoms.
Poison ivy, oak, and sumac grow in both wooded and marshy areas. These plants produce sap that contains an allergen called urushiol.
Urushiol can trigger an allergic skin reaction called contact dermatitis. About 50–75% of adults in the United States are allergic to urushiol.
Symptoms of a poison ivy, oak, or sumac rash include:
- flushed, itchy skin
- bumps or blisters on the skin
- swollen, tender skin
- difficulty breathing
- fever
Treatment
Poison ivy, oak, and sumac rashes usually clear up by themselves within a few weeks.
If someone believes that they have had exposure to urushiol, they can remove the oils immediately by washing themselves and their clothes with soap and water.
OTC topical treatments, such as calamine lotion and hydrocortisone, can help relieve itching and swelling. A doctor may prescribe an oral antihistamine to lessen the allergic reaction.
Dyshidrotic eczema, or dyshidrosis, is a common form of eczema that causes itchy blisters on the palms of the hands and soles of the feet.
According to the National Eczema Association, dyshidrotic eczema is twice as common in females as males.
Symptoms can include:
- deep blisters on the toes, palms, edges of the fingers, and soles of the feet
- flushed, itchy skin
- scaly, cracked, or flaking skin
- swollen, tender skin
Treatment
There is currently no cure for dyshidrotic eczema. Treatments for this skin condition involve reducing symptoms and preventing secondary infections and other complications.
Treatments for this skin condition involve reducing symptoms and preventing secondary infections and other complications.
A doctor may prescribe a topical steroid to reduce swelling and itching. Botox injections can lessen sweating and excess moisture in the hands and feet, which can prevent infections.
At-home treatments for dyshidrotic eczema include:
- soaking the hands and feet in cool water
- applying a cold compress to the affected skin
- using moisturizer or cream that repairs the skin barrier
Hand, foot, and mouth disease (HFMD) is a skin condition that occurs due to coxsackievirus and enterovirus infections. HFMD is highly contagious, and people can contract it by:
- touching a person with the infection
- touching objects or surfaces that carry the virus
- breathing air that contains the virus particles
Although HFMD is most common among young children under the age of 5, anyone can develop the infection.
HFMD usually leads to small spots appearing on the hands and feet, as well as mouth sores. Other symptoms include:
- painful blisters
- fever
- sore throat
- loss of appetite
- pain when eating or swallowing
Treatment
There are no specific treatments for HFMD. People may be able to manage symptoms with OTC medication that reduces fever and pain.
Drinking cold liquids can help keep people hydrated while soothing a sore throat.
According to the Centers for Disease Control and Prevention (CDC), most people with HFMD get better within 7–10 days.
Cellulitis is a bacterial infection that develops in the deep layers of the skin and on the lower legs and feet. Symptoms include:
- skin that appears swollen
- skin that feels warm, tender, or painful to the touch
- skin dimpling
- blisters
- fatigue
- fever or chills
- cold sweats
- nausea or vomiting
- swollen, tender lymph nodes
People with light skin tones may also notice reddened skin in the affected area.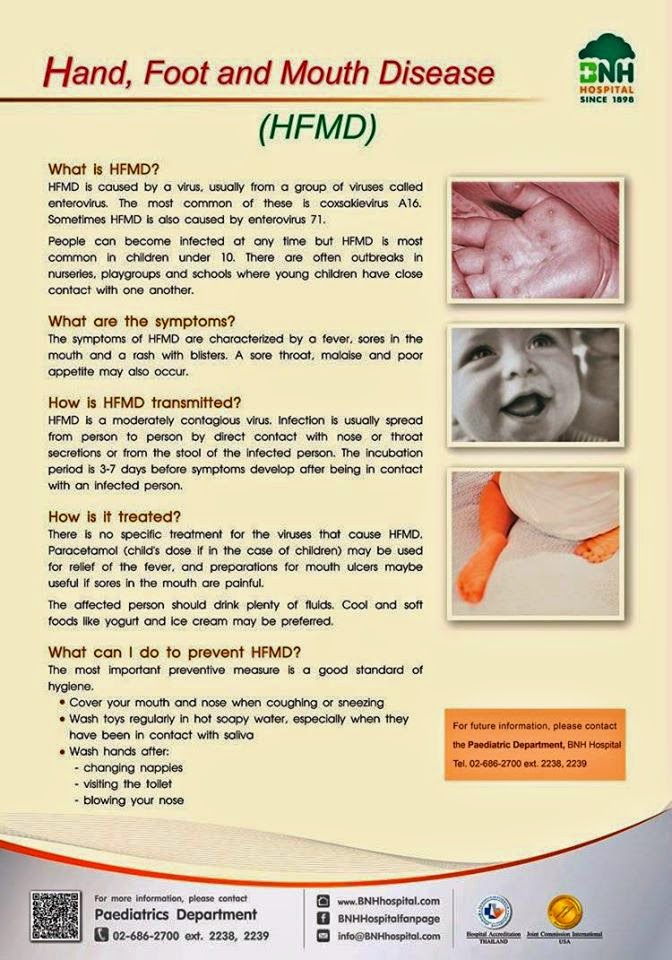
Treatment
Cellulitis can develop suddenly and can be life threatening without treatment.
Doctors usually prescribe antibiotics to treat the bacterial infection responsible for cellulitis. Other beneficial at-home treatment options include:
- keeping the affected leg or foot raised to reduce swelling
- taking OTC pain medications to relieve pain and reduce fever
- avoiding scratching or itching the affected skin
- keeping the area clean and dry
Scabies is a skin condition that occurs when microscopic scabies mites burrow into the upper layer of the skin. These mites then feed on skin cells and lay eggs. Symptoms of scabies usually develop within 4–8 weeks.
A scabies infestation can lead to a skin rash and intense itching. The affected area of skin may develop pimple-like blisters or thick, crusty scales.
Treatment
People cannot treat scabies with at-home remedies. A doctor must prescribe topical medications that kill scabies mites.
After starting treatment, people will need to disinfect their bedding, clothing, and any other fabrics that they regularly use. Doing this will help prevent recurring infestations.
People should contact their healthcare provider if their foot rash is painful or significantly interferes with their daily activities.
Parents and caregivers should see a healthcare provider if a child or infant develops a skin rash or blisters.
It is important for a person to seek medical attention straight away if their rash does not improve with treatment or they develop a fever.
There are numerous possible causes of foot rashes, ranging from allergic reactions to infections. Most cases clear up on their own, but OTC medications can help relieve swelling, itching, and pain during recovery.
A person should speak with a doctor if they have a foot rash that does not respond to treatment or they develop signs of an infection.
Foot rash: Causes, symptoms, and treatments
A foot rash can occur due to an allergic reaction or infection. Most foot rashes, such as athlete’s foot and contact dermatitis, are treatable with over-the-counter (OTC) medications.
Most foot rashes, such as athlete’s foot and contact dermatitis, are treatable with over-the-counter (OTC) medications.
However, other types of foot rashes, such as cellulitis may require medical intervention.
In this article, we list a few common causes of foot rashes along with their symptoms and treatment options.
Tinea pedis, more commonly known as athlete’s foot, is a highly contagious fungal infection that develops on the feet.
A fungus called Trichophyton causes athlete’s foot. This fungus thrives in warm, moist environments, such as shower floors and the inside of shoes.
Athlete’s foot often leads to itchy, burning skin between the toes. Other symptoms of the condition include:
- dry, scaly, or cracked skin
- flushed or raw skin
- weak, discolored toenails
- cracked or oozing blisters on the feet
Treatment
Most people can treat athlete’s foot with an OTC antifungal treatment, usually in the form of an oral tablet or a liquid or cream. More severe infections may require prescription-strength medication.
More severe infections may require prescription-strength medication.
Topical steroids, such as hydrocortisone, can help reduce inflammation and relieve itching and soreness.
Contact dermatitis is a rash that occurs when a substance irritates the skin or produces an allergic reaction.
Substances that may cause contact dermatitis can include:
- metals, such as nickel
- makeup
- latex
- frequent washing or contact with water
- bleach
Treatment
People can avoid the substance that they think is causing contact dermatitis to see whether their rash clears within 1–3 weeks. Antihistamines and topical corticosteroids may help relieve symptoms.
Poison ivy, oak, and sumac grow in both wooded and marshy areas. These plants produce sap that contains an allergen called urushiol.
Urushiol can trigger an allergic skin reaction called contact dermatitis. About 50–75% of adults in the United States are allergic to urushiol.
Symptoms of a poison ivy, oak, or sumac rash include:
- flushed, itchy skin
- bumps or blisters on the skin
- swollen, tender skin
- difficulty breathing
- fever
Treatment
Poison ivy, oak, and sumac rashes usually clear up by themselves within a few weeks.
If someone believes that they have had exposure to urushiol, they can remove the oils immediately by washing themselves and their clothes with soap and water.
OTC topical treatments, such as calamine lotion and hydrocortisone, can help relieve itching and swelling. A doctor may prescribe an oral antihistamine to lessen the allergic reaction.
Dyshidrotic eczema, or dyshidrosis, is a common form of eczema that causes itchy blisters on the palms of the hands and soles of the feet.
According to the National Eczema Association, dyshidrotic eczema is twice as common in females as males.
Symptoms can include:
- deep blisters on the toes, palms, edges of the fingers, and soles of the feet
- flushed, itchy skin
- scaly, cracked, or flaking skin
- swollen, tender skin
Treatment
There is currently no cure for dyshidrotic eczema. Treatments for this skin condition involve reducing symptoms and preventing secondary infections and other complications.
Treatments for this skin condition involve reducing symptoms and preventing secondary infections and other complications.
A doctor may prescribe a topical steroid to reduce swelling and itching. Botox injections can lessen sweating and excess moisture in the hands and feet, which can prevent infections.
At-home treatments for dyshidrotic eczema include:
- soaking the hands and feet in cool water
- applying a cold compress to the affected skin
- using moisturizer or cream that repairs the skin barrier
Hand, foot, and mouth disease (HFMD) is a skin condition that occurs due to coxsackievirus and enterovirus infections. HFMD is highly contagious, and people can contract it by:
- touching a person with the infection
- touching objects or surfaces that carry the virus
- breathing air that contains the virus particles
Although HFMD is most common among young children under the age of 5, anyone can develop the infection.
HFMD usually leads to small spots appearing on the hands and feet, as well as mouth sores. Other symptoms include:
- painful blisters
- fever
- sore throat
- loss of appetite
- pain when eating or swallowing
Treatment
There are no specific treatments for HFMD. People may be able to manage symptoms with OTC medication that reduces fever and pain.
Drinking cold liquids can help keep people hydrated while soothing a sore throat.
According to the Centers for Disease Control and Prevention (CDC), most people with HFMD get better within 7–10 days.
Cellulitis is a bacterial infection that develops in the deep layers of the skin and on the lower legs and feet. Symptoms include:
- skin that appears swollen
- skin that feels warm, tender, or painful to the touch
- skin dimpling
- blisters
- fatigue
- fever or chills
- cold sweats
- nausea or vomiting
- swollen, tender lymph nodes
People with light skin tones may also notice reddened skin in the affected area.
Treatment
Cellulitis can develop suddenly and can be life threatening without treatment.
Doctors usually prescribe antibiotics to treat the bacterial infection responsible for cellulitis. Other beneficial at-home treatment options include:
- keeping the affected leg or foot raised to reduce swelling
- taking OTC pain medications to relieve pain and reduce fever
- avoiding scratching or itching the affected skin
- keeping the area clean and dry
Scabies is a skin condition that occurs when microscopic scabies mites burrow into the upper layer of the skin. These mites then feed on skin cells and lay eggs. Symptoms of scabies usually develop within 4–8 weeks.
A scabies infestation can lead to a skin rash and intense itching. The affected area of skin may develop pimple-like blisters or thick, crusty scales.
Treatment
People cannot treat scabies with at-home remedies. A doctor must prescribe topical medications that kill scabies mites.
After starting treatment, people will need to disinfect their bedding, clothing, and any other fabrics that they regularly use. Doing this will help prevent recurring infestations.
People should contact their healthcare provider if their foot rash is painful or significantly interferes with their daily activities.
Parents and caregivers should see a healthcare provider if a child or infant develops a skin rash or blisters.
It is important for a person to seek medical attention straight away if their rash does not improve with treatment or they develop a fever.
There are numerous possible causes of foot rashes, ranging from allergic reactions to infections. Most cases clear up on their own, but OTC medications can help relieve swelling, itching, and pain during recovery.
A person should speak with a doctor if they have a foot rash that does not respond to treatment or they develop signs of an infection.
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices
Doctors
The first children’s clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy – highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling
or by filling out the form on the website
Other services of the Pediatrics section
Pediatrician’s consultation
Child Health Management Program
Frequent calls
Acute bronchiolitis in children: diagnosis and treatment
SARS
Angina streptococcal tonsillitis
Frequently ill child
Intestinal infections
Colic
Feeding problems
Prolonged cough in a child: diagnosis and treatment
Acute bronchitis in children: diagnosis and treatment
Pneumonia (pneumonia) in children: diagnosis and treatment
False croup in a child
Coxsackie virus in a child
The child was bitten by a tick! What to do?
Breastfeeding advice
Online payment
Documents online
Online services
Blisters
responsible medical portal
Eruptions in the form of bubbles
Vesicle (synonym – vesicle) is the primary element of skin rashes that appears on intact skin due to various reasons. It is a cavity bounded by a lid and bottom, and rises above the skin surface. It is located in the epidermis – the surface layer of the skin. The vesicle is filled with transparent, sometimes turbid (serous) or mixed with blood (serous-hemorrhagic) contents. Size – more often up to 0.5 cm in diameter. There are single and multi-chamber bubbles. Sometimes they open, the contents expire, erosions form at this place, which, after healing (epithelialization), leave no traces. Large, more than 0.5 cm in diameter, elements similar in structure are called bubbles (or bullae).
It is a cavity bounded by a lid and bottom, and rises above the skin surface. It is located in the epidermis – the surface layer of the skin. The vesicle is filled with transparent, sometimes turbid (serous) or mixed with blood (serous-hemorrhagic) contents. Size – more often up to 0.5 cm in diameter. There are single and multi-chamber bubbles. Sometimes they open, the contents expire, erosions form at this place, which, after healing (epithelialization), leave no traces. Large, more than 0.5 cm in diameter, elements similar in structure are called bubbles (or bullae).
Causes of blisters:
- prickly heat – a pathological condition of the skin, accompanied by the appearance of many blisters with transparent contents on closed areas of the body and in natural skin folds. The disease develops due to excessive overheating and sweating. Vesicles are scattered or grouped (more often in the folds of the skin – inguinal, intergluteal; in the armpits, under the mammary glands).
 Sometimes the contents of the bubbles become cloudy and suppurate, the elements are surrounded by a zone of redness; in severe cases, they can merge and form weeping foci.
Sometimes the contents of the bubbles become cloudy and suppurate, the elements are surrounded by a zone of redness; in severe cases, they can merge and form weeping foci. - herpes simplex – viral disease affects the area of the lips, nasolabial folds, another part of the face, can be located in the oral cavity. Vesicles have cloudy contents and are surrounded by a reddish corolla (a zone of hyperemia). Swelling and redness visits the patient even before they appear. Rashes bring pain and discomfort in the affected area, may be subject to fusion. After some time, they dry up, crusts form on the surface, sometimes small ulcers. The disease may be accompanied by a rise in temperature.
- chickenpox (or shingles) – a disease of a viral nature (causative agent – herpes zoster virus). The rash is staged: first papules appear (raised reddish-pink skin densities), and then they are converted into vesicles, first with a transparent, and then cloudy content.
 These elements subsequently dry out with the formation of brown crusts. It is localized throughout the body, occurs on the scalp, mucous membranes of the mouth, eyes and genitals. Rashes have a wave-like character, which corresponds to a surge in temperature reaction. The rash passes without a trace if it is not injured by scratching, otherwise scars may remain.
These elements subsequently dry out with the formation of brown crusts. It is localized throughout the body, occurs on the scalp, mucous membranes of the mouth, eyes and genitals. Rashes have a wave-like character, which corresponds to a surge in temperature reaction. The rash passes without a trace if it is not injured by scratching, otherwise scars may remain. - felinosis or cat-scratch disease – parasitic disease, vector – domestic cats. At the site of a scratch inflicted by a pet, or its bite, after two weeks (incubation period), a small papule (a seal that rises above the skin surface) is formed with a zone of redness, which then transforms into a vesicle or pustule (abscess), followed by the formation of a crust. A characteristic feature of the clinic is regional lymphadenitis (damage to the lymph nodes) two weeks after the rash; axillary and ulnar are more often involved in the process, less often – cervical and inguinal. The temperature reaction is expressed.

- scabies – a contagious disease caused by the scabies mite. The way of transmission is contact. Clinic – more often in the skin between the fingers, on the wrist, genitals, the tick makes moves; at the affected sites, a rash appears in the form of papules with a reddish corolla, which can transform into vesicles and be accompanied by itching. Scratching the affected areas can lead to infection of the rash.
- allergic reaction (contact and food allergy) – manifests itself in the form of contact dermatitis. Rashes may look like bubbles with transparent contents, redness and swelling around; accompanied by severe itching, while, as a rule, the general condition of the patient is not disturbed. When an allergen is identified, eliminated, or antihistamines are taken, the rash is neutralized.
- autoimmune diseases (pemphigus, bullous pemphigoid, dermatitis herpetiformis) is a pathology in which the body’s immune system fights its own healthy cells, as well as body tissues.


 Sometimes the contents of the bubbles become cloudy and suppurate, the elements are surrounded by a zone of redness; in severe cases, they can merge and form weeping foci.
Sometimes the contents of the bubbles become cloudy and suppurate, the elements are surrounded by a zone of redness; in severe cases, they can merge and form weeping foci. These elements subsequently dry out with the formation of brown crusts. It is localized throughout the body, occurs on the scalp, mucous membranes of the mouth, eyes and genitals. Rashes have a wave-like character, which corresponds to a surge in temperature reaction. The rash passes without a trace if it is not injured by scratching, otherwise scars may remain.
These elements subsequently dry out with the formation of brown crusts. It is localized throughout the body, occurs on the scalp, mucous membranes of the mouth, eyes and genitals. Rashes have a wave-like character, which corresponds to a surge in temperature reaction. The rash passes without a trace if it is not injured by scratching, otherwise scars may remain.