Isolated Breast Pain: Causes, Types, and When to Seek Medical Attention
What causes breast pain. How to differentiate between cyclical and noncyclical breast pain. When should you consult a doctor about breast pain. What diagnostic tests are used to evaluate breast pain. What are common findings in breast imaging for pain.
Understanding Breast Pain: Types and Causes
Breast pain, medically known as mastalgia, is a common concern among women, accounting for 45-70% of breast-related healthcare visits. While the experience can be uncomfortable and worrying, it’s essential to understand that most cases of breast pain are benign and often related to hormonal fluctuations or external factors like ill-fitting bras.
Breast pain can manifest in various ways, including:
- Dull aches
- Tenderness
- Burning sensations
- Sharp pains
- Uncomfortable fullness
To better understand and address breast pain, it’s crucial to recognize the two main types: cyclical and noncyclical breast pain.
Cyclical Breast Pain
Cyclical breast pain is the most common type and is closely linked to hormonal changes in the body. Key characteristics of cyclical breast pain include:

- Affects both breasts
- Involves the entire breast or upper outer portion
- May radiate to the armpit
- Varies with the menstrual cycle
- Typically worsens the week before menstruation
- Often improves or subsides after menstruation
Women experiencing cyclical breast pain may also notice increased breast lumpiness during the premenstrual period. In most cases, this type of breast pain doesn’t require medical evaluation or treatment.
Noncyclical Breast Pain
Noncyclical breast pain differs from its cyclical counterpart in several ways:
- Usually affects only one breast
- Not related to the menstrual cycle
- Can be constant or intermittent
- Often more challenging to determine the cause
While noncyclical breast pain is also typically benign, it may require more thorough evaluation to identify the underlying cause. Common reasons for noncyclical breast pain include:
- Poor-fitting bras
- Pregnancy
- Trauma
- Muscle strain
- Prior breast surgery
It’s important to note that while breast cancer is usually painless, when it does cause discomfort, it tends to be noncyclical and localized to one specific area.

When to Consult a Doctor About Breast Pain
While most cases of breast pain are benign, certain situations warrant medical attention. You should consult your doctor if:
- You discover a persistent lump in the painful area that doesn’t disappear after your period
- There’s redness, swelling, or drainage from the affected area (potential signs of infection)
- You experience nipple discharge
- The pain isn’t clearly associated with your menstrual cycle or lasts more than two weeks
- The pain is localized to one spot and doesn’t involve the entire breast
- Your breast pain is progressively worsening
- The pain is significantly impacting your daily life and activities
Even if your symptoms don’t fall into these categories, it’s always advisable to consult your doctor if you’re concerned about your breast health.
Diagnostic Approach to Breast Pain
When you consult a doctor about breast pain, they will likely follow a systematic approach to diagnose the underlying cause. This process typically involves a thorough medical history, physical examination, and possibly imaging tests.

Medical History and Physical Examination
Your doctor will ask several questions to better understand your symptoms:
- Duration of the pain
- Any associated lifestyle or body changes
- Presence of lumps or other breast changes
- Pain intensity and characteristics
- Family history of breast cancer
Following the questionnaire, your doctor will perform a physical examination of your breasts, looking for:
- Lumps
- Skin changes
- Focal tenderness
- Nipple discharge
Based on the findings from the medical history and physical examination, your doctor may recommend imaging tests for further evaluation.
Imaging Tests for Breast Pain Evaluation
Depending on your age, symptoms, and risk factors, your doctor may order one or more imaging tests to investigate the cause of your breast pain.
Mammogram
A mammogram is an X-ray of the breast tissue. Here’s what you can expect during a mammogram:
- A technologist will take at least two X-rays of your breast
- Your breast will be compressed during the imaging
- If you haven’t had a screening mammogram in over a year, both breasts may be imaged
- A breast radiologist will review the X-rays and determine if additional images or an ultrasound are necessary
Breast Ultrasound
In certain cases, such as for women under 40, pregnant, or lactating, a breast ultrasound may be recommended instead of or in addition to a mammogram. The ultrasound procedure involves:

- Application of ultrasound gel to the breast
- Scanning the painful area with a handheld ultrasound probe
- Possible recommendation for a mammogram by the breast radiologist
After the imaging tests, you’ll receive immediate feedback on the results, and a detailed report will be sent to your doctor.
Common Findings in Breast Imaging for Pain
When women undergo imaging for breast pain, the results often fall into one of three categories:
1. Normal Findings
In 75-88% of cases, mammograms and/or ultrasounds reveal completely normal breast tissue. This outcome is reassuring and often indicates that the pain is likely due to hormonal fluctuations or external factors.
2. Benign Causes
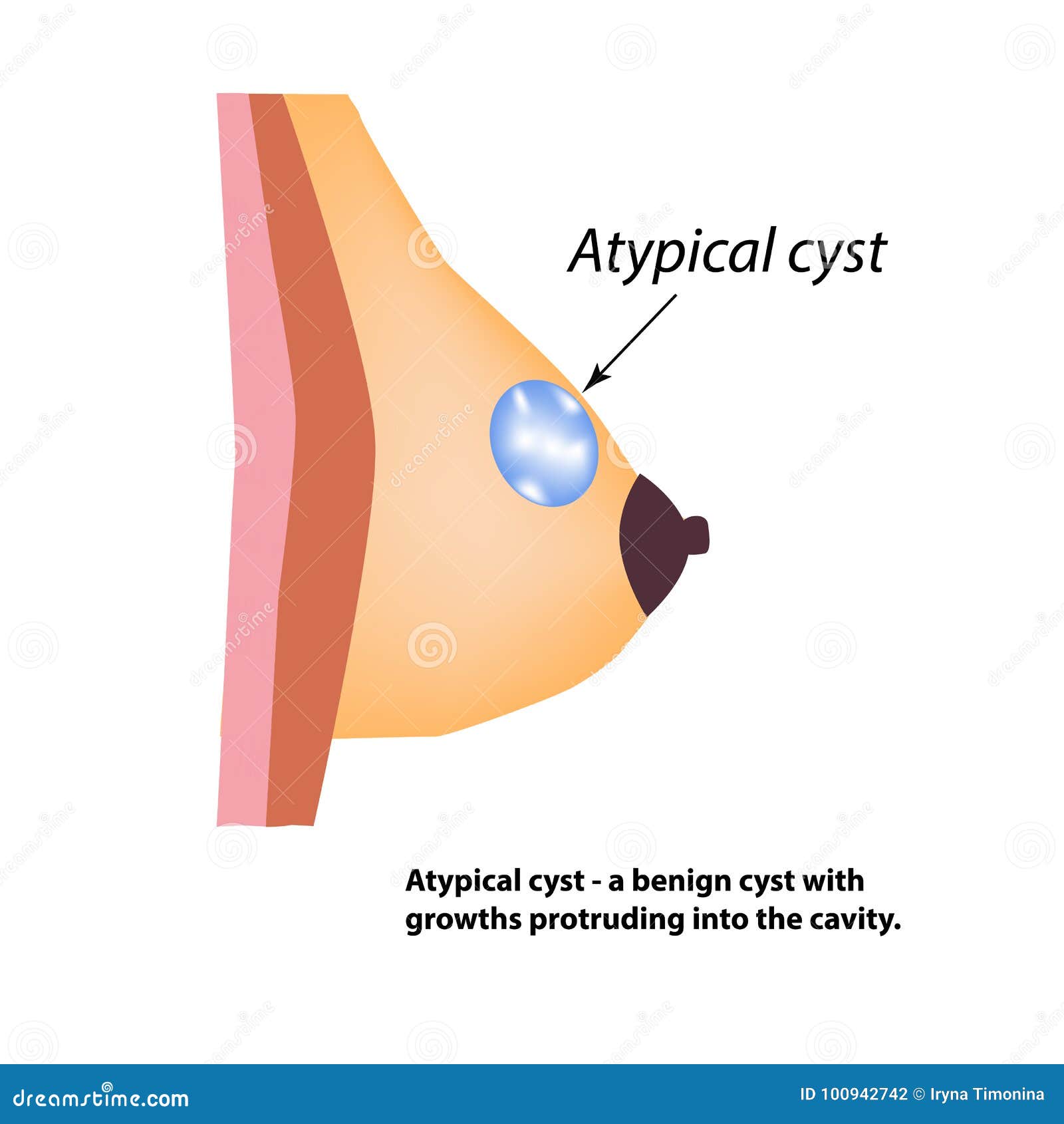
Approximately 10% of women who undergo imaging for breast pain are found to have a benign cause for their discomfort. The most common benign finding is a breast cyst.
Breast cysts are fluid-filled sacs within the breast tissue. Many women have them without ever realizing it. These cysts can become painful due to hormonal changes or increased pressure within the breast.
3. Other Findings
In a small percentage of cases, imaging may reveal other findings that require further investigation. These could include:
- Fibroadenomas (benign breast tumors)
- Lipomas (fatty lumps)
- Calcifications
- Rarely, signs of breast cancer
It’s important to remember that the vast majority of breast pain cases are not related to cancer. However, thorough evaluation is crucial for proper diagnosis and peace of mind.
Managing Breast Pain: Treatment Options and Self-Care
Once the cause of breast pain has been determined, your doctor may recommend various treatment options or self-care measures to alleviate discomfort.
For Cyclical Breast Pain
Management strategies for cyclical breast pain often focus on lifestyle modifications and over-the-counter remedies:
- Wearing a well-fitted, supportive bra
- Reducing caffeine intake
- Applying heat or ice to the breasts
- Using over-the-counter pain relievers like ibuprofen or acetaminophen
- Considering evening primrose oil supplements (consult with your doctor first)
For Noncyclical Breast Pain
Treatment for noncyclical breast pain depends on the underlying cause:

- Addressing poor bra fit with properly sized undergarments
- Physical therapy or exercises for muscle strain
- Topical anti-inflammatory medications
- In some cases, prescription medications may be recommended
Your doctor may also suggest keeping a pain diary to track patterns and potential triggers, which can help in developing a more targeted treatment plan.
Breast Pain and Cancer: Addressing the Concern
One of the most common worries associated with breast pain is its potential link to breast cancer. It’s crucial to address this concern with accurate information.
Is breast pain a sign of cancer?
In the vast majority of cases, breast pain is not a sign of cancer. Breast cancer typically develops without causing pain, especially in its early stages. However, in rare instances, breast cancer can cause discomfort. This pain is usually:
- Noncyclical (not related to menstrual cycles)
- Localized to one specific area of the breast
- Persistent and doesn’t improve with time
It’s important to remember that while these characteristics can be associated with breast cancer, they are much more commonly linked to benign conditions.

When should breast pain raise a red flag?
While breast pain alone is rarely a sign of cancer, certain accompanying symptoms warrant immediate medical attention:
- A new, persistent lump in the breast or armpit
- Changes in breast size or shape
- Skin changes on the breast, such as dimpling or redness
- Nipple inversion or discharge (especially if bloody)
- Persistent pain that doesn’t respond to initial treatments
If you experience any of these symptoms along with breast pain, it’s crucial to consult your healthcare provider promptly for a thorough evaluation.
The Importance of Regular Breast Health Monitoring
While breast pain is often benign, it serves as a reminder of the importance of regular breast health monitoring. Maintaining awareness of your breast health can help detect any changes early and provide peace of mind.
Breast Self-Examinations
Performing regular breast self-examinations can help you become familiar with your normal breast tissue and detect any changes quickly. Here’s how to conduct a self-exam:

- Visually inspect your breasts in a mirror, looking for any changes in size, shape, or skin texture
- Feel your breasts while lying down, using a circular motion with varying pressure
- Check your armpits for any lumps or swelling
- Gently squeeze your nipples to check for any discharge
Perform these self-exams monthly, preferably at the same time in your menstrual cycle.
Regular Clinical Breast Exams
In addition to self-exams, regular clinical breast exams performed by a healthcare professional are crucial. These exams can detect subtle changes that you might miss and provide an opportunity to discuss any concerns with your doctor.
Mammogram Screenings
For women at average risk of breast cancer, mammogram screenings are typically recommended:
- Starting at age 40: Annual mammograms
- Ages 45-54: Annual mammograms
- Age 55 and older: Mammograms every 1-2 years, based on personal preference and risk factors
Women with higher risk factors may need to start screenings earlier or undergo additional imaging tests. Consult with your doctor to determine the best screening schedule for your individual needs.
My breasts hurt. Should I be worried?
By: Michelle Lee, MD, and Wendi Owen, MD
If you have breast pain, you are not alone. Breast pain, also known as mastalgia, is common and accounts for 45-70% of breast-related health care visits. The good news is that most causes of breast pain are benign (non-cancerous) and usually related to hormonal changes in your body or something as simple as a poor fitting bra. Breast pain varies a lot from person to person and may feel like a dull ache, tenderness, burning sensation, sharp pain or just a sense of uncomfortable fullness. To understand what causes breast pain and what to do about it, it is important to understand a little bit about the different types of breast pain.
Types of breast pain
There are two main types of breast pain. The first type is cyclical and changes with hormonal changes in your body. Cyclical breast pain typically involves both breasts, involves either the entire breast or the upper outer portion, and may radiate to the armpit. Most importantly, it varies with your menstrual cycle. Cyclical breast pain is usually worse during the week before you start your period. The pain usually subsides or improves after your period. With cyclic breast pain, it is also common to feel like your breasts are lumpier during the week before your period. Cyclical breast pain is the most common type of breast pain and usually does not require any treatment or medical evaluation.
Most importantly, it varies with your menstrual cycle. Cyclical breast pain is usually worse during the week before you start your period. The pain usually subsides or improves after your period. With cyclic breast pain, it is also common to feel like your breasts are lumpier during the week before your period. Cyclical breast pain is the most common type of breast pain and usually does not require any treatment or medical evaluation.
The second main type of breast pain is noncyclic breast pain. Noncyclic breast pain usually involves only one breast and is not related to your menstrual cycle. It can be constant or intermittent, just not associated with any particular pattern. The cause of noncyclical breast pain is often harder to determine. Just like with cyclical breast pain, most causes of noncyclical breast pain are benign. The most common cause is a poor-fitting bra. Other causes include pregnancy, trauma, muscle strain and prior surgery. Although breast cancer is usually not painful, when it does cause pain, the pain tends to be noncyclical and usually just in one focal spot. Because of this, noncyclical breast pain may require a little more evaluation to determine the cause.
Because of this, noncyclical breast pain may require a little more evaluation to determine the cause.
When should I talk to my doctor?
- You have a lump in the area of pain that does not go away after your period.
- You have redness, swelling or drainage from the area (signs of infection).
- You have nipple discharge.
- Your breast pain is not clearly associated with your menstrual cycle or lasts more than two weeks.
- Your breast pain is just in one spot and does not involve the whole breast.
- Your breast pain keeps getting worse.
- The pain is affecting your life and limiting what you can do.
Even if you do not fit into any of these categories, if you are worried, it is always a safe bet to talk to your doctor about your symptoms.
What will my doctor do?
Your doctor will probably ask you questions about your breast pain. These may include: How long has it been there? Is the pain associated with any other changes in your lifestyle or body? Have you noticed a lump or any other changes to your breast? How bad is the pain? What does the pain feels like? Do you have any family history of breast cancer?
Your doctor will likely examine your breasts for lumps, skin changes, focal tenderness or nipple discharge. Depending on the exam and your answers to the questions, your doctor may order imaging tests.
Depending on the exam and your answers to the questions, your doctor may order imaging tests.
What types of imaging tests will my doctor order?
Mammogram
Your doctor may order a mammogram, which is an x-ray of your breast. A technologist will take at least two x-rays of your breast while your breast is compressed. If you have not had a screening mammogram in over a year, they may take x-rays of your non-painful breast, too. A breast radiologist will look at your x-rays while you wait and determine if you need any additional x-rays or a breast ultrasound.
Breast Ultrasound
If you are younger than 40, lactating or pregnant, your doctor may order an ultrasound of your breast instead of a mammogram. During the breast ultrasound, a technologist or breast radiology will put ultrasound gel on your breast and scan the area of pain with a hand-held ultrasound probe. The breast radiologist may decide to perform a mammogram as well to evaluate your area of pain./iStock-865314396-5a206816845b34003674922c.jpg)
Either a technologist or a breast radiologist will discuss the results of your imaging with you before you leave and a report will be sent to your doctor.
What kinds of things might the radiologist see?
In 75-88% of women who have imaging for breast pain, the mammogram and/or ultrasound are completely normal. In around 10% of women, the radiologist will find a benign cause for the pain. The most common benign cause of pain is a breast cyst. Breasts cysts are sacs of fluid in the breast and many women have them and never know it. They can become painful with changes in your body’s hormones or when they increase in size. One-to-two percent of women may need further evaluation with a breast biopsy because the radiologist sees something on the images and cannot tell exactly what it is. A breast biopsy is an outpatient procedure where a small piece of tissue is removed from your breast to be evaluated under a microscope. Very few women with breast pain have breast cancer and some studies show that your chance of having breast cancer is the same whether you have breast pain or not.
What can I do to get rid of the pain?
- Wear a properly fitted bra without underwire.
- Wear a sports bra while exercising.
- Some changes in diet have been shown to reduce symptoms of breast pain, such as decreasing your intake of fatty foods and caffeine.
- Some over-the-counter, herbal and prescription medications have been shown to help. Ask your doctor about these options and if any are right for you.
- Some women find that ice packs or heating pads help their pain, and you can try these to see if one works for you.
- Stress reducing and relaxation techniques may also help alleviate symptoms of breast pain.
The bottom line
Breast pain is common and usually not associated with anything bad. Cyclical breast pain comes and goes with your menstrual cycle and is related to hormonal changes in your body. Non-cyclical breast pain has a wide variety of causes and the cause is harder to determine but also usually related to benign processes in the breast. Talk to your doctor about your breast pain if you are worried, particularly, if you have a lump in the area of pain that does not go away after your period, redness, swelling, drainage from the area (signs of infection), nipple discharge, or if your breast pain is not clearly associated with your menstrual cycle, lasts more than two weeks, is just in one spot, keeps getting worse or is affecting your life and limiting what you can do.
Talk to your doctor about your breast pain if you are worried, particularly, if you have a lump in the area of pain that does not go away after your period, redness, swelling, drainage from the area (signs of infection), nipple discharge, or if your breast pain is not clearly associated with your menstrual cycle, lasts more than two weeks, is just in one spot, keeps getting worse or is affecting your life and limiting what you can do.
Your doctor may order imaging tests to evaluate your breast pain. Although these are usually normal, they may help find a cause for the pain or identify something that needs to be biopsied. There are several treatments for breast pain, but there is not a single one that works for everyone, and you should talk to your doctor about any that may be right for you.
Dr. Lee is an Assistant Professor of Radiology at Washington University School of Medicine in St. Louis.
Dr. Owen is an Assistant Professor of Radiology at UK Healthcare.
This blog post was originally published March 22, 2017
If You Have Breast Pain, Should You Worry? – Cleveland Clinic
For many
women, having breast pain automatically causes concern. You don’t necessarily
expect to have pain there. So when it happens, you question what’s causing it.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Know this: Breast pain is quite common. “In fact, around 30% of women will experience breast pain in their lifetime,” says breast health specialist Holly Pederson, MD. In the majority of cases, the cause is hormonal fluctuations or — surprisingly — even how much coffee or other caffeine you drink.
Is your pain in one location?
This is an
important question.
For example,
do you have pain in both breasts? Is it worse before your menstrual period? If
the answer is “yes,” you may have cyclical pain. That’s common in
That’s common in
pre-menopausal women. The pain typically gets better when your period starts.
We also call similar pain “non-focal” pain because it’s not focused in one breast or one specific spot. Interestingly, consuming too much caffeine sometimes causes this type of pain, too. We don’t know exactly why.
In either
case, though, pain in both breasts is not likely to be a sign of breast cancer.
“If you have concerns, get a physical exam,” Dr. Pederson says. “Your doctor
will help determine if you need added screening.”
However, if
your pain is located in one breast — and especially in one specific spot on one
breast — don’t delay in getting it checked. This “focal” pain is more likely to
be a sign
of cancer than pain in both breasts, she says. If your pain is associated
with a breast lump or visible changes in your skin or nipple, those are causes
for concern, too.
These cases
apply to a small number of women, but they’re absolutely worth discussing with
a doctor, especially if you’re over age 30.
What can you do for breast pain?
Most of the
time, breast pain isn’t severe enough to require medication, Dr. Pederson says.
“If diagnostic tests such as ultrasound are normal, usually
nothing further needs to be done,” she notes. “We often recommend
conservative steps first, such as cutting out caffeine, to see if symptoms
improve.”
An herbal supplement called evening primrose oil offers relief for some women, too. Since it’s an herbal supplement, she says, there’s not a lot of clinical research behind it. But small-scale studies have supported it as being clinically effective. Over-the-counter topical pain relief cream may help too.
For more severe cases, medications are available. For example, a topical non-steroidal anti-inflammatory drug (NSAID) gel called diclofenac offers pain relief without the same long-term concerns of oral NSAIDs.
Very rarely,
doctors will prescribe tamoxifen for breast pain. Tamoxifen is an anti-estrogen
medication used to prevent and treat breast cancer, and studies have shown it
to be effective
for reducing breast pain. But it does come with potential side effects,
But it does come with potential side effects,
including hot flashes and a small risk of blood clots. “That’s why we always
weigh the benefits against the potential side effects,” Dr. Pederson says.
For many
women, simply knowing that breast pain is common — and that most of the time
it’s not associated with cancer — is enough to bring peace of mind. But when
you have pain, don’t hesitate to get an exam and find answers.
An Error Occurred Setting Your User Cookie
An Error Occurred Setting Your User Cookie
This site uses cookies to improve performance. If your browser does not accept cookies, you cannot view this site.
Setting Your Browser to Accept Cookies
There are many reasons why a cookie could not be set correctly. Below are the most common reasons:
- You have cookies disabled in your browser. You need to reset your browser to accept cookies or to ask you if you want to accept cookies.

- Your browser asks you whether you want to accept cookies and you declined.
To accept cookies from this site, use the Back button and accept the cookie. - Your browser does not support cookies. Try a different browser if you suspect this.
- The date on your computer is in the past. If your computer’s clock shows a date before 1 Jan 1970,
the browser will automatically forget the cookie. To fix this, set the correct time and date on your computer. - You have installed an application that monitors or blocks cookies from being set.
You must disable the application while logging in or check with your system administrator.
Why Does this Site Require Cookies?
This site uses cookies to improve performance by remembering that you are logged in when you go from page to page. To provide access without cookies
would require the site to create a new session for every page you visit, which slows the system down to an unacceptable level.
What Gets Stored in a Cookie?
This site stores nothing other than an automatically generated session ID in the cookie; no other information is captured.
In general, only the information that you provide, or the choices you make while visiting a web site, can be stored in a cookie. For example, the site
cannot determine your email name unless you choose to type it. Allowing a website to create a cookie does not give that or any other site access to the
rest of your computer, and only the site that created the cookie can read it.
Breast pain and cancer: should we continue to work-up isolated breast pain?
Purpose:
To assess the cancer detection rate (CDR) in patients presenting with isolated breast pain.
Methods:
A retrospective review was performed of consecutive patients presenting to a large tertiary care academic center or an affiliated hospital with isolated breast pain from October 1, 2013 to September 30, 2015./breast-test--woman-examining-her-breasts-for-cancer--heart-attack--pain-in-human-body-1066203380-02389e8f283b4395989d60cf8775510a.jpg) Medical records were reviewed for patient demographics, pain characteristics, imaging findings, and outcome.
Medical records were reviewed for patient demographics, pain characteristics, imaging findings, and outcome.
Results:
The study cohort was comprised of 971 exams in 953 patients, with a median age of 50 years. A total of 62.5% (607/971) of the cases were assessed by mammography and ultrasound, 24.4% (237/971) by ultrasound only, and 13.1% (127/971) by mammography only. Including the abnormalities detected in the asymptomatic breast, 88.7% (861/971) of the cases were negative or had benign findings (BI-RADS 1 and 2), 6.8% (66/971) were probably benign (BI-RADS 3), 3.9% (38/971) were suspicious (BI-RADS 4), and 0.6% (6/971) were highly suggestive of malignancy (BI-RADS 5). CDR on initial work-up was 0.8% (8/953), of which 0.6% (4/690) was in average-risk patients while 1.5% (4/263) was in higher-than-average risk patients.
Conclusions:
CDR in patients presenting with isolated breast pain overall was low, comparable to the expected incidence of breast cancer in asymptomatic women. Work-up for isolated breast pain may therefore be unnecessary and lead to overutilization of healthcare resources. Routine screening mammography should be encouraged and higher-than-average risk patients may benefit from additional tests.
Work-up for isolated breast pain may therefore be unnecessary and lead to overutilization of healthcare resources. Routine screening mammography should be encouraged and higher-than-average risk patients may benefit from additional tests.
Keywords:
Breast; Cancer; Mastalgia; Pain.
Breast Pain | Doctor | Patient
Synonyms: mastalgia, mastodynia
Pain is one of the most common breast symptoms experienced by women and management requires careful assessment and diagnosis. There is often understandable anxiety associated with the symptom, particularly about breast cancer. This worry is often the reason women seek medical evaluation. The risk of cancer in a woman presenting with breast pain as an isolated symptom is extremely low and suitable reassurance can usually be given.
Breast pain is uncommon in men. Pain and tenderness may occur in men who develop gynaecomastia secondary to medication, hormonal factors, cirrhosis and other conditions. Cyclical breast pain is confined to women but both non-cyclical breast pain and extramammary pain can occur in men. The assessment of these types of pain is similar for men and women.
Cyclical breast pain is confined to women but both non-cyclical breast pain and extramammary pain can occur in men. The assessment of these types of pain is similar for men and women.
Classification
[1]
Breast pain is typically approached according to its classification as:
- Cyclical breast pain – breast pain that has a clear relationship to the menstrual cycle, and the most common type of breast pain.
- Non-cyclical breast pain – may be constant or intermittent but is not associated with the menstrual cycle.
- Extramammary (non-breast) pain – is interpreted as having a cause within the breast but arises from elsewhere (the chest wall or other sources).
The classification is important because the assessment, management and response to treatment are different for the different types of breast pain. This is particularly the case in true breast pain vs extramammary pain, as the management is very different.
Epidemiology
[1, 2]
- Up to 70% of women will experience breast pain in their lifetime.

- This is a common presentation in general practice, usually in women aged 30-50 years.
- In patients attending for breast problems in specialist clinics and general practice, breast pain is the most common symptom. It is the presenting symptom in about half of new patients in breast clinics.
History
The history should be directed toward identifying and characterising breast-related symptoms. Establish:
- Nature and duration of pain.
- Severity of pain (ranges from mild discomfort to severe tenderness and pain).
- Site of pain.
- Any relationship to activity.
- Presence of other breast symptoms (lumps, discharge).
- Relationship to menstrual cycle and periodicity. Establish whether the pain is cyclical, or whether it has no relationship to menstrual cycle.
- If there is recent or current breast-feeding.
- Medication history, particularly hormonal medication.
- Reproductive, medical and family history.

Ask about any associated problems. Such problems are common and disruptive. Likely findings include:[4]
- Sleep problems.
- Symptoms affecting sex life.
- Work, school and social disruption.
- Quality of life adversely affected.
Cyclical breast pain
Features which suggest cyclical breast pain include:[5]
- Severity of pain is variable in different menstrual cycles.
- Pain is usually present in the same part of each menstrual cycle (most commonly starting 1-3 days before menses start).
- Pain has usually settled by the time menstruation ends.
- Pain tends to be in the upper outer quadrant(s) and may extend to the axillae.
- Pain is usually diffuse and bilateral (may be more severe in one breast).
- There may be generalised swelling and lumpiness but no specific lump found.
Non-cyclical breast pain[5, 6]
Pain is not related to the menstrual cycle and is more likely to be unilateral or focal. Some causes are listed in the ‘Differential diagnosis’ section below. Medication history is particularly important in this type of breast pain; establish whether the person has been on medication which may cause mastalgia – for example:
Some causes are listed in the ‘Differential diagnosis’ section below. Medication history is particularly important in this type of breast pain; establish whether the person has been on medication which may cause mastalgia – for example:
- Hormonal medication, especially hormone replacement therapy (HRT). Also oral contraceptive pills.
- Antidepressants (including sertraline, venlafaxine and mirtazapine).
- Antipsychotics (including haloperidol).
- Cardiovascular drugs (including digoxin and spironolactone).
- Antibiotics (including metronidazole) and antifungals (including ketoconazole).
Extramammary pain
Extramammary pain due to various conditions may present as breast pain. There are many such conditions (listed below in ‘Differential diagnosis’ section) but most common are costochondritis and other chest wall syndromes. Features such as location and radiation of pain, history of recent trauma or aggravating activities may lead the clinician to suspect the cause of the pain to be extramammary.
Examination
[1]
- Clinical breast examination requires careful inspection and palpation of each breast. This should include all four quadrants of each breast from the under surface of each breast right up to the upper end of the breast tail, the nipple and areola, together with examination of the regional lymph nodes.
- Palpation may demonstrate an abnormality. Commonly it reveals coarse nodular areas resembling bundles of string in the breast but check carefully for any discrete lump. Look for skin changes and nipple distortion or discharge.
- Look for signs of infection (localised redness, swelling, warmth and tenderness).
- If there is tenderness on examination, establish whether this is within the breast or in the underlying chest wall. Try lifting the breast with one hand while palpating the chest wall underneath, or ask the woman to lie on each side in turn, allowing the breast to fall away from the chest wall. It may be very reassuring for the woman if this demonstrates the area of tenderness is not within the breast tissue.
- Large pendulous breasts may be a clue that the pain is musculoskeletal in nature, especially if a well-fitting, supportive bra is not worn.[6]
- It may be appropriate to examine other potential causes of the pain. Examination of the cervical and thoracic spine, chest wall, shoulders, upper extremities, heart, lungs and abdomen may help further diagnostic evaluation.
Investigations
Exclude pregnancy where indicated. Refer urgently if there is a discrete lump, any sinister feature, or a past history of breast cancer.
Breast pain alone with no associated findings is not an indication for imaging.Consider referral, however, if there are risk factors or if pain is persistent, atypical or unexplained.
Differential diagnosis
The most important conditions to exclude are breast cancer, pregnancy and infection. There are, however, numerous potential causes of breast pain, including:
- Breast-related:
- Cyclical breast pain.
- Non-cyclical breast pain.
- Mastitis.
- Breast trauma.
- Thrombophlebitis/Mondor’s syndrome.
- Breast cysts.
- Benign breast tumours.
- Breast cancer.
- Lactation-associated – may have an infectious aetiology.[7]
- Postoperative breast pain.
- Musculoskeletal:
- Medication – as listed above.
- Miscellaneous causes:
Management
Management will depend on the cause but a variety of measures which have been routinely advised by some in the past should no longer be recommended. Measures no longer routinely recommended include:[5]
- Diets low in fat and high in carbohydrate, or low in caffeine.
- Stopping or changing other medication, including combined oral contraceptives.
- Evening primrose oil.
- Progestogen-only contraceptives.
- Antibiotics.
- Diuretics.
- Pyridoxine.
- Tibolone.
- Vitamin E
Cyclical breast pain
[5]
First-line management
- Reassurance that the pain is not due to breast cancer and an explanation as to its hormonal nature may be all the management that some women require. Studies have shown that reassurance alone is effective management in 70% of women.[1]
- A better-fitting bra and simple analgesia is the first line of treatment. Simple non-opioid analgesia can be helpful for mild discomfort.
- Topical diclofenac may be helpful. There is some consensus that topical non-steroidal anti-inflammatory drugs (NSAIDs) are effective and well tolerated but the evidence is inconclusive.[2]
- Although there is little evidence to support its use, some women find a soft support sleep bra helpful at night.
- Continue first-line measures for six months before considering second-line treatment.
- Pain will resolve spontaneously in 20-30% but has a high recurrence rate (~60%).[2]
Second-line management
Consider referring to a specialist for other treatment options if pain is severe or persistent. A diary of pain and symptoms for two months may help in assessment. Further treatment may include:
- Danazol (an anti-gonadotrophin) is licensed for severe pain and tenderness in benign fibrocystic breast disease which has not responded to other treatment. Adverse effects (commonly nausea, dizziness, rash, backache, weight gain, menorrhagia) may be minimised by reducing the dose of danazol to 100 mg from the initial starting dose of 300 mg daily, and restricting treatment to two weeks preceding menstruation. Non-hormonal contraception is essential, as danazol has androgenic effects in the fetus.
- Tamoxifen (an oestrogen-receptor antagonist) has also been shown to be effective. However, it is not licensed for mastalgia in the UK, and side-effects include hot flushes, vaginal bleeding, vaginal discharge, increased risk of thromboembolism and increased risk of endometrial cancer. Non-hormonal contraception is required during use because of potential teratogenicity. There is a risk of thromboembolism but this may be less when given for this indication, usually at a lower dose than the dose used for breast cancer, and for only the luteal phase of the cycle. Tamoxifen gel applied topically may also be effective, but is not in common use or generally available.[1]
- Goserelin injections (a gonadorelin analogue which inhibits gonadotrophin release) are occasionally used for severe refractory mastalgia. The incidence of side-effects (mainly vaginal dryness, hot flushes, decreased libido, oily skin or hair, decreased breast size, irritability) can be reduced by using in conjunction with HRT.
- Bromocriptine is now rarely used because of frequent and intolerable adverse effects (mainly nausea, dizziness, postural hypotension, constipation).
- Gestrinone (inhibits pituitary gonadotrophin).
- Toremifene (a selective oestrogen-receptor modulator).
Non-cyclical and extramammary breast pain
[1]
- Non-cyclical breast pain responds poorly to treatment but resolves spontaneously in 50% of women.[2]
- Chest wall pain often responds to NSAIDs. Referred pain should be appropriately treated.
- Trigger spots sometimes respond to infiltration with local anaesthetic and steroid injection.
- For true diffuse breast pain a support bra, soft sleep bra and oral or topical NSAIDs may be helpful.
- For chest wall pain, gentle exercise and stretching of the muscles (for example, by swimming) are often advised but there is no evidence base for this. Lifestyle changes such as increased exercise and activity and reducing long periods of time sitting in front of a computer are also usually advised and there is some early evidence to support this.[8]
- Gabapentin, pregabalin or amitriptyline are used for neuropathic pain such as scar pain or neuralgia. External neuromodulation for postoperative neuropathic pain has also been used.
- Acupuncture has been reported as beneficial in a pilot study.[9]
Evaluating breast pain following negative mammogram: Is US needed?
By Staff News Brief
Should a patient with breast pain and a normal mammogram also have a breast ultrasound examination? Unless the patient presents with multiple symptoms, such as nipple discharge or palpable concerns, research conducted at Columbia University Medical Center in Manhattan suggests not. In a study published online in Current Problems in Diagnostic Radiology in January, radiologists reported that mammography alone effectively excluded malignancy in over 500 women with isolated complaints of breast pain.
Mastalgia — cyclic and noncyclic breast pain — generates concern that it may be a symptom of malignancy, especially if it is persistent, localized, and unilateral. While rates of malignancy in patients presenting with mastalgia have been reported in multiple studies as less than 4%, a mammogram is usually performed, followed by targeted ultrasound examination in the area of indicated pain.
The authors conducted a study to evaluate the diagnostic value of breast ultrasound following a normal mammogram ordered for all patients with breast pain during a calendar year. The study included 559 women who ranged in age from 27 to 97 (median 46 years). The majority (70%) had no other symptoms, but one-fourth also reported skin changes, nipple discharge, and/or had concerns about palpable masses.
Patients’ breast pain was categorized into five types: focal, diffuse, cyclical, unilateral or bilateral. Mammographic breast density scores and Breast Imaging-Reporting and Data System (BI-RADS) final assessments were recorded and analyzed. Nearly half of the patients had heterogeneously dense breasts (46%) and 8.6% had dense breasts. The overwhelming majority (79%) had BI-RADS 1 or 2 scores, with 12.9% having BI-RADS 3, and 8.1% having BI-RADS 4.
Twenty-six patients underwent tissue biopsy. This included only one patient in the group of 374 women who did not have additional symptoms (0.0003%). Lead author Eralda Mema, MD, reported that malignancy was identified in 2 patients, one who also had nipple discharge (1 out of 22 patients, or 4.5%) and the other with palpable concern (1 out of 134 patients, or 0.7%).
“Our results suggest that ultrasound evaluation in the setting of a negative mammogram is not indicated. No malignancies were identified with the addition of ultrasound examination in mammographically normal patients presenting with mastalgia. Furthermore, malignancy was not impacted by bone density,” wrote the authors. “We believe that obtaining an ultrasound examination in these patients may increase the number of follow-ups of probably benign (BI-RADS 3) lesions and subsequently increase the rate of benign biopsies. Mammography alone was effective in excluding malignancy in our cohort of patients with isolated complaints of breast pain.”
The authors recommend that similar, larger studies be performed to validate their findings. They also recommend that long-term multi-year studies of women who present with breast pain be initiated, noting that none have yet been performed.
REFERENCE
- Mema E, Cho E, Ryu Y-K, et al. In the setting of negative mammogram, is additional breast ultrasound necessary for evaluation of breast pain? Curr Probl Diagn Radiol. Published online January 9, 2018. doi: 10.1067/j.cpradiol.2017.12.007.
Back To Top
Evaluating breast pain following negative mammogram: Is US needed?.
Appl Radiol.
By Staff News Brief|
April 26, 2018
About the Author
%PDF-1.6
%
148 0 obj
>
endobj
xref
148 110
0000000016 00000 n
0000003353 00000 n
0000003574 00000 n
0000003703 00000 n
0000003739 00000 n
0000003975 00000 n
0000004074 00000 n
0000004233 00000 n
0000004377 00000 n
0000004569 00000 n
0000004711 00000 n
0000004903 00000 n
0000005095 00000 n
0000005238 00000 n
0000005431 00000 n
0000005576 00000 n
0000005768 00000 n
0000005913 00000 n
0000006106 00000 n
0000006250 00000 n
0000006442 00000 n
0000006585 00000 n
0000006777 00000 n
0000006920 00000 n
0000007080 00000 n
0000007225 00000 n
0000007490 00000 n
0000008050 00000 n
0000009760 00000 n
0000010952 00000 n
0000012150 00000 n
0000013338 00000 n
0000014008 00000 n
0000014116 00000 n
0000014226 00000 n
0000014496 00000 n
0000015051 00000 n
0000015140 00000 n
0000015393 00000 n
0000015893 00000 n
0000016009 00000 n
0000016680 00000 n
0000017249 00000 n
0000017534 00000 n
0000019313 00000 n
0000021002 00000 n
0000022521 00000 n
0000024047 00000 n
0000025536 00000 n
0000026950 00000 n
0000028208 00000 n
0000029634 00000 n
0000031170 00000 n
0000086874 00000 n
0000095347 00000 n
0000098761 00000 n
0000099016 00000 n
0000099427 00000 n
0000153261 00000 n
0000200649 00000 n
0000256242 00000 n
0000256505 00000 n
0000257089 00000 n
0000257561 00000 n
0000257820 00000 n
0000258232 00000 n
0000265607 00000 n
0000265646 00000 n
0000301570 00000 n
0000301609 00000 n
0000301945 00000 n
0000302034 00000 n
0000302170 00000 n
0000303368 00000 n
0000303587 00000 n
0000303701 00000 n
0000304010 00000 n
0000304058 00000 n
0000304301 00000 n
0000304383 00000 n
0000304508 00000 n
0000304580 00000 n
0000304836 00000 n
0000304909 00000 n
0000305043 00000 n
0000305154 00000 n
0000305228 00000 n
0000305352 00000 n
0000305426 00000 n
0000305544 00000 n
0000305618 00000 n
0000305791 00000 n
0000305864 00000 n
0000305983 00000 n
0000306154 00000 n
0000306282 00000 n
0000306355 00000 n
0000306429 00000 n
0000306605 00000 n
0000306679 00000 n
0000306752 00000 n
0000306825 00000 n
0000306932 00000 n
0000307047 00000 n
0000307120 00000 n
0000307240 00000 n
0000307313 00000 n
0000307433 00000 n
0000307506 00000 n
0000002496 00000 n
trailer
]/Prev 979720>>
startxref
0
%%EOF
257 0 obj
>stream
hb“`f` ̀
Ankylosing spondylitis
Bechterew’s disease or ankylosing spondylitis refers to systemic inflammatory diseases of the connective tissue. Typical is the defeat of the articular-ligamentous apparatus of the spine, as well as peripheral joints and internal organs (heart, aorta, kidneys). The disease has a tendency to a chronic, progressive course with the development of ankylosis (joint stiffness) and affects mainly men aged 20 to 40 years.Any anatomical areas of the spine and adjacent tissues can potentially be involved in the pathological process, which usually begins with the sacroiliac joints, slowly and unevenly spreading to the overlying parts of the spine. In response to inflammatory changes, a reflex spasm of the muscles adjacent to the spine occurs. This muscle tension, in turn, increases pain and causes coordination disorders. With the further course of the inflammatory process gradually leads to the development of immobility in the intervertebral joints, ossification (calcium deposition) in the ligaments and degenerative-dystrophic changes in the hyaline plates and vertebral bodies.In some cases, the pathological process can begin with the hip and knee joints, followed by damage to the spine. In this case, the lesion of the peripheral joints proceeds according to the type of inflammatory, as in rheumatoid arthritis.
Reasons
Not definitively installed. The role of heredity is great (in 95% of patients, HLA-B27 is determined), the pathological immune response in genitourinary and intestinal infections.
Classification
- Central (with isolated lesions of the spine and sacroiliac joints) form is subdivided into kyphosis (described by V.M. Bekhterev as a “petitioner pose”) and a rigid type (“board-like back”).
- Rhizomelic form (in addition to the spine, the sacroiliac joints, the shoulder and hip joints are affected).
- Scandinavian or rheumatoid-like form (small joints are affected, there are typical changes in the spine and sacroiliac joints).
- Peripheral (the spine, sacroiliac joints, elbow, knee and ankle joints are affected)
- The visceral form is characterized by obligatory damage to internal organs: heart (endocarditis, pericarditis, conduction disturbances), kidney (nephritis), eyes (iridocyclitis is recurrent and often precedes damage to the spine and sacroiliac joints), aorta (damage to the aortic valve).
- Youthful form (joints are affected, often hip, characteristic radiological changes develop late).
Symptoms
Early pains in the sacrum or lumbar region, radiating to the hip joints or groin. With physical exertion or prolonged stay in one position, pain occurs in the lumbosacral spine, in some cases pain occurs after carrying a heavy load in one hand. Also, pain can occur in the area of the calcaneus, heel tendons.Temporary pain can appear in the shoulder, hip, knee joints. When the thoracic spine is involved in the pathological process, intercostal neuralgia, girdle pain in the chest, aggravated by deep inhalation, coughing or descending stairs are characteristic. Pain in the places of attachment of the ribs to the sternum and spine on both sides. In the late stage of the disease, the pathological process spreads to all parts of the spine. The pain becomes less pronounced, but is permanent, intensifying with movement and physical exertion.There is a restriction of chest excursion, which is accompanied by the appearance of shortness of breath (especially after eating). The patient’s posture acquires characteristic changes, most often kyphosis and kyphoscoliosis of the thoracic spine, hyperlordosis of the cervical spine, flattening of the lumbar lordosis, hypotrophy of the long back muscles and a sharp limitation of the mobility of the spine are observed. Changes in gait occur: the patient moves with his legs wide apart, making rocking movements with his head. When the process spreads to the cervical region, pain appears during head movements, complete immobility can occur – the neck is fixed in the forward tilt position, the head is lowered down, the chin touches the chest.
Diagnostics
Limitation of mobility of the lumbar spine in three directions (flexion, extension, lateral tilt) and pain in the sacroiliac region (remaining at rest and disturbing for at least three months), limitation of chest excursion during breathing. Typical radiological signs in most cases are detected only 2 years after the onset of the disease, however, early signs of sacroiliitis can be detected after 3 to 4 months. The most valuable early sign is damage to the joints of the intervertebral arches.In the future, typical ankylosis of the sacroiliac and costal-transverse joints, osteoporosis of the spine, ossification of the ligamentous apparatus of the spine, which usually begins from the lateral parts of the anterior longitudinal ligament (in the lateral projection, the spine resembles a bamboo stick). A blood test may indicate the presence of inflammation (increased ESR) and contain a genetic marker for the disease.
Treatment
The basis of treatment is the regular implementation of special exercises that improve blood circulation and metabolism in individual segments of the limbs and trunk, restore reduced strength and speed of muscle contraction, mobility in individual joints, etc.Breathing exercises, coordination and balance exercises are required. Special exercises help to develop replacement movements when walking (with ankylosis of the hip joints, the step is carried out by turning the torso, pelvis, swinging the arms, etc.). Physiotherapy and spa treatment, non-steroidal anti-inflammatory drugs are used. Endoprosthetics of the hip and knee joints.
90,000 Stomach pain
Abdominal pain is one of the most common reasons for seeking emergency medical help and, in some cases, one of the symptoms of acute surgical diseases of the abdominal organs (acute appendicitis, perforated stomach ulcer, intestinal obstruction, etc.)), requiring an emergency referral of the patient to the surgical department.
Etiology
The main causes of pain localized by patients in the abdominal region are as follows:
- Diseases and injuries of the abdominal organs (stomach, gallbladder, intestines, uterus and its appendages, etc.).
- Diseases and injuries of the retroperitoneal organs (kidney, pancreas, retroperitoneal hematomas with fractures of the pelvic bones and kidney injuries, dissecting aneurysm of the abdominal aorta).
- Thrombosis and embolism of the vessels of the abdominal cavity.
- Irradiating pain in diseases of the chest organs (croupous pneumonia, pleurisy, basal pleuropneumonia, myocardial infarction, pericarditis).
- Diseases and injuries of the anterior abdominal wall (abdominal hernias, spontaneous and traumatic ruptures of the vessels of the anterior abdominal wall with the formation of hematomas in its thickness, phlegmon of the abdominal wall).
- Irradiating pain in diseases and injuries of the spine and spinal cord (fractures of the lower thoracic and lumbar vertebrae, tumors of the spinal cord and crises with dorsal tabes, lumbosacral radiculitis, etc.)etc.).
Localization of pain in most cases indicates a lesion of one or another organ.
So, pain in the right upper abdomen is observed mainly in diseases of the liver, gallbladder and biliary tract, head of the pancreas, duodenum, ascending colon, right kidney and right-sided phrenic pleurisy.
Pain in the upper left abdomen is characteristic of diseases of the stomach, pancreas, left half of the large intestine and left kidney.
The most common cause of pain in the right lower abdomen is acute appendicitis. It can also be caused by lesions of the blind and terminal ileum, diseases of the internal genital organs in women.
The causes of pain in the left lower abdomen are usually diseases of the sigmoid colon and internal genital organs.
However, in some cases, the localization of pain to patients does not coincide with the topography of the affected abdominal organ. So, most patients with acute appendicitis during the first hours from the onset of the disease note pain not in the right iliac region, corresponding to the location of the appendix, but in the epigastric region.Sometimes the diagnosis of acute appendicitis can be made precisely by the characteristic movement of pain from the epigastrium or umbilical region to the lower right quadrant of the abdomen. With a disturbed ectopic pregnancy and significant hemorrhage into the abdominal cavity, the main complaint of patients is often excruciating pain in the epigastrium and both hypochondria, radiating to the neck and shoulder joints. This is due to the accumulation of blood in the upper abdomen, poured out during the rupture of the pregnant fallopian tube, and irritation of the diaphragmatic peritoneum.
Irradiation of pain is characteristic of a number of diseases and lesions of certain organs. So, pain in the right hypochondrium, emanating from the gallbladder and biliary tract, as a rule, radiates upward, into the right half of the chest and the right shoulder. Pain in the epigastrium with stomach ulcers and pain in acute pancreatitis are given to the back and lower back. Pain in both iliac regions, caused by diseases of the internal genital organs in women, usually have a characteristic downward irradiation with a feeling of pressure on the bladder and rectum.
A number of acute processes in the abdominal cavity are accompanied by a characteristic isolated irradiation of pain to the area of the shoulder joint in the complete absence of any changes in the joint itself or its surrounding tissues (the so-called phrenicus symptom). This complaint sometimes comes to the fore, but even if the patient himself does not state this, one should actively ask him about such a radiation of pain. Shoulder phrenicus symptom is characteristic of those diseases in which suddenly there is an outpouring of blood or stomach contents into the abdominal cavity and irritation of the diaphragmatic peritoneum.It often accompanies hemorrhages caused by rupture of the fallopian tube, liver, spleen, and is extremely common with perforation of stomach and duodenal ulcers.
Diagnostics
Determination of the nature of abdominal pain greatly contributes to the correct diagnosis. It is necessary to find out if the pain started suddenly or increased gradually. So, a sudden acute, so-called dagger, abdominal pain is observed with perforation of stomach and duodenal ulcers.The sudden nature of abdominal pain is characteristic of some types of acute intestinal obstruction (volvulus, entrapment, nodulation). Abdominal pain suddenly begins with acute pancreatitis, intestinal thrombosis, rupture or torsion of ovarian cysts in women. The sudden onset of pain is extremely characteristic for hepatic and renal colic. Less acutely the pain syndrome increases with intestinal obstruction; a gradual increase in pain is also characteristic of acute inflammatory diseases (acute appendicitis, cholecystitis, inflammation of the uterine appendages).
A clear connection between the pain localized by the patient in the epigastric region with food intake, a gradual increase in pain soon after eating or its occurrence at night, a seasonal spring-autumn exacerbation of the process are characteristic of gastric ulcer and duodenal ulcer. Prolonged or constant pulling, pressing pain in the epigastric region with a feeling of distention of the stomach in elderly patients, combined with weight loss, makes it possible to suspect a neoplasm of the stomach.
Observation of the patient’s behavior and posture during an attack of acute abdominal pain is of great diagnostic value.Patients with exacerbation of peptic ulcer disease usually sit or lie, hunched over, with their legs brought to the stomach. Patients with perforation of gastric and duodenal ulcers usually groan or scream from intense pain, but retain the forced horizontal position of the same type, since an attempt to change it leads to a sharp increase in pain. The same situation is typical for patients with local or diffuse peritonitis of various etiologies, with the difference that independent (independent of examination) abdominal pains are usually less intense and the patients are relatively calm.
For profuse intra-abdominal hemorrhages (ectopic pregnancy, ruptures of the liver, spleen), in some cases, a persistent attempt is characteristic of patients to raise their head or sit up (the so-called “vanka-stand” symptom, caused by excruciating pain during breathing due to irritation of the diaphragmatic peritoneum with accumulated blood).
Sharp and constant anxiety of patients, groans or screams, continuous attempts to change the position of the body (the horizontal position is replaced by walking, sitting) are very often observed with hepatic and renal colic.These attacks are also characterized by sudden onset and termination.
Patients in the early stage (before the development of intestinal necrosis and peritonitis) of acute intestinal obstruction caused by compression of the intestinal loop with a plug, its volvulus, nodulation or intussusception, behave extremely anxiously. However, for these cases, in contrast to colic, pains are characterized by cramping and their replacement by periods of relative well-being, due to the termination of the peristaltic wave.
In some cases, acute abdominal pain is the leading complaint of patients with acute pathology of the chest organs (basal pleuropneumonia, gastralgic form of myocardial infarction, etc.).etc.). Often, it is accompanied by the appearance of objective signs characteristic of acute surgical diseases of the abdominal organs, and, above all, limited tension of the muscles of the abdominal wall. A sharp stretching of the liver capsule with a rapid increase in right ventricular failure can cause pain that intensifies on inspiration during palpation in the right hypochondrium and simulate acute cholecystitis. However, the constant presence of subjective and objective signs of damage to the respiratory and circulatory organs (shortness of breath, cough, hemoptysis, heart rhythm disturbances, the presence of wheezing in the lungs and dullness of the percussion sound over their areas) usually allows.correctly interpret the nature of acute abdominal pain. Nevertheless, the true nature of the disease in a number of cases can be revealed only with an inpatient examination of the patient and the use of a number of special research methods (ECG, X-ray examination of the chest organs).
A careful and comprehensive assessment of abdominal pain and patient observation therefore provides significant information. Thorough questioning and full-fledged objective examination of a patient complaining of acute abdominal pain can solve the main problem facing the doctor at the prehospital stage – to identify patients with acute surgical diseases of the abdominal organs.All patients with suspected peritonitis, intestinal obstruction, mesenterlal thrombosis, acute appendicitis, cholecystitis, pancreatitis, and renal colic are subject to emergency hospitalization in a surgical hospital. Patients with cholelithiasis and urolithiasis, gastroenteritis, etc., that is, with diseases that cause abdominal pain, but without signs of acute abdomen, can be hospitalized in a planned manner.
Do not self-medicate.
Seek medical attention promptly.
Excess estrogen in the body: symptoms, causes and prevention
Lack of orgasm, psychological complexes and health problems – both an older woman and a very young girl can face these problems. They asked an expert how a girl gets an orgasm, which causes complexes and how to fix the situation.
Sexual dysfunction
This term is often attributed only to men. But only 30% of women nowadays experience orgasmic discharge.This is catastrophically small, because the remaining 70% are silent, hiding their feelings – a number of unresolved questions arise. More than half of women are unable to realize their sexual component.
6 main reasons (it is related to women’s health)
1. Atrophy of the pelvic floor muscles
It is a fact that we are static. Our work is most often connected with a computer – we constantly sit, move a little and do even less physical activity.
The journey from home to work does not count – the pelvic floor muscles are atrophic in almost all women, even young women, precisely because of physical inactivity and a sedentary lifestyle.
2. Descent of internal organs
It is the atrophy of the pelvic floor that leads to tears during childbirth – during the passage of the fetal head, the ligaments of the small pelvis break and deform. The muscles are also deformed, but it is easier with them – they can be restored due to their hyper-extensibility, which cannot be said about the ligaments.
If the ligaments are torn, then they are torn “with ends” and no longer fix the sensitive areas. As a result, organs prolapse – the bladder, the uterus, and the rectum enter here.Sensitivity to sexual intercourse decreases sharply 90 130.
3. Lack of estrogen
All over the world women began to abandon estrogens early – we began to live longer, but the aging process is often much faster. In many women, early menopause occurs after 40 years – before, a woman at this age could only wait for the perimenopausal period, which, by the way, now begins at 37.
This is precisely due to the lack of estrogens – they have less and less effect on the pelvic floor muscles (which are less supplied with blood) and the vaginal mucosa, from which hyaluronic acid leaves (it gives moisture to the vagina).During sex, a woman begins to experience terrible discomfort – natural lubrication is no longer enough for her, and she has to resort to lubricants.
4. Incontinence
Torn ligaments lead to urinary incontinence when coughing or sneezing. Previously, this problem was relevant for women well over 50 years old, when estrogens began to leave them during the extinction of ovarian function. But now this also applies to young girls against the background of traumatization during childbirth.
We recall that most of the work is sedentary, and the pelvic floor muscles are atrophied.Therefore, now young women are forced to resort to plastic surgery and surgery (for example, installing a special mesh under the urethra) in order to avoid incontinence when the pressure in the bladder rises.
5. Relaxed vaginal syndrome
During childbirth, among other things, the vagina expands – this is no secret, and due to the stretching of the muscles, we get the relaxed vaginal syndrome. During sexual intercourse, these women have significantly reduced sensations – in medicine, this is called “anorgasmia”.
The point is in the so-called “G-spot”, which is actually nothing more than the legs of the clitoris – they are the organ that gives women the desired release. If the vagina is enlarged, then during the frictions, the “G-spot” does not receive any stimulation or receives too little of it – hence the weak sensations or their complete absence.
6. Stress and depression
Does a girl get an orgasm – this ability is given by nature precisely for relaxation, because our life is full of an impossible amount of stress.Despite the fact that the level of modern medicine is now much higher than in the same XX century, our grandparents who lived through the war, for some reason, were much healthier than us. The secret is simple – as much information did not pass through them as now passes through us.
We need stress, but in a small amount – for what we call stress, adrenaline and cortisol, hormones produced by the adrenal glands, are responsible.
Thus, the body tones our blood vessels – if these hormones cease to be released, a person simply will not be able to live.Therefore, in small amounts, stress helps, but when it becomes much more than necessary, the adrenal glands simply get tired of producing these hormones.
An increased level of stress and anxiety leads to many diseases – both to depression and to various somatic disorders. Nature gave sexual release so that women could “release” all neuro-emotional stress with the help of a real orgasm. If it is not there, then the body begins to give us relief through diseases – for example, hysteria.
A person’s whole life is aimed at being happy. We enter into relationships, give birth to children and create families for this very reason.
Happiness in the body manifests itself through the production of dopamine and serotonin – these neurotransmitters, including oxytocin, also activate our orgasmic function.
Dopamine often leads to addiction, serotonin is called the hormone of happiness, and oxytocin is our tenderness. During orgasm, all these neurotransmitters are released, and if it is not there, then the state of health goes straight towards depression.
Why is this happening
We live in the 21st century and process so much information that the number of mental illnesses will only grow, and their peak is not far off. Alzheimer’s, dementia and other diseases of this spectrum are senile processes, but already now they are formed in people at the age of 50. For comparison, in the XX century, these diseases were typical for people of 70 years old.
The world is entering an epidemic of psychological disorders and mental illness, women return to partners overwhelmed and often either forget about the need for relaxation, or have no strength for it.
Obesity also contributes to the above problems – the more body weight we have, the less active the orgasmic function becomes: muscle tissue is not developed, and the muscles themselves practically do not work. In the absence of a correct lifestyle, a competent nutritional strategy and physical activity, we begin to gradually gain weight, achieve complete atrophy of the pelvic floor muscles and forget what an orgasm is.
How to avoid stress and problems with sexual function
Take magnesium, vitamin D and Omega-3
Frankly speaking, not everyone can develop resistance to stress.But everyone can fight stress with magnesium. H
Signs of magnesium deficiency
It needs to be replenished – either take magnesium (the citrate formula is better absorbed by the body), or drink Donat Mg (Donat Magnesium) pharmacy water – 2 glasses of water a day will completely fill this need.
Vitamin D
This is the “vitamin of the sun”. The Russians, for obvious reasons, have very little of it – the rays of the sun fall on us at a not very favorable angle.It’s not even a vitamin, but a hormone, and for a minute, it activates 3000 receptors in the body.
Lack of vitamin characterizes abnormal fatigue – when, for example, you have just woken up and are already tired.
Omega-3
You need energy even on the flap of your eyelashes – it is provided by the mitochondria, and this is their main function. The stronger they are, the more energy they produce, but even mitochondria age if they don’t know how to rest.
Omega-3s are healthy fats that the body needs.In theory, we should get it from fish, but in fact the fish itself does not contain Omega-3 – it contains algae, which the fish feeds on.
Of course, fish grown in an artificial reservoir is deprived of such a diet – they are given compound feed, and there is nothing to do with fish oil there. But Omega-3 contains wild fish – for example, herring.
Get enough sleep
From 23:00 to 1:00 melatonin, the hormone of youth, is released in our body. Falling asleep before midnight, you need to sleep from 8 to 10 hours – if you went to bed at 2 am and slept for ten hours, there will not be much sense.
You can retrain yourself and rebuild the body, as many are doing now – they literally make the body get used to it and sleep for 4-5 hours, but in the long run it will not bring anything good.
Eat good quality
80% of foods contain sugar. It is because of him that sarcopenia gradually occurs – a disease of the elderly, in which the muscles atrophy, and the strength in them is lost. Instead, a person accumulates adipose tissue – he consumes a lot of sugar, and often does so unconsciously.
To lose weight, you need to eat, but right. This is a problem not only in aesthetic medicine, but also in medicine in general – eating behavior is now being corrected not only by nutritionists, but also by doctors of all specialties.
Exercise
The benefits of moderate physical activity have long been confirmed – when scientists began to study centenarians, they revealed a common feature in everyone: none of them exhausted themselves with hours of exercise in the gym, but each had moderate physical activity and restriction of calories (i.e.i.e. moderation in food). It can be walking at a moderate pace – every woman can afford it, regardless of age, status, employment and opportunities.
What to do if problems already exist
All of them are solved with the help of aesthetic gynecology. This branch of medicine can fully restore orgasmic function in those 70% of women who cannot live life to the fullest.
1. Hyaluronic acid
The injection of hyaluronic acid into the “G-spot” (clitoral feet) is very similar to the procedure for injecting fillers into the lips, which young girls love so much.It is inserted into the legs of the clitoris to make them more voluminous – in this case, they will hang more in the vagina. As a result, during the frictions, the “G-spot” will finally be activated, due to which the orgasm will come.
Hyaluronic acid also helps when estrogens leave a woman. The mucous membrane immediately becomes dry, does not moisturize and does not produce natural lubrication. The procedure for intimate plastic surgery of the vagina is carried out with a preparation of not dense hyaluronic acid, which we inject into the lips, but, on the contrary, more liquid.
It literally pulls on all the water, and if we inject it into the vagina, it just pulls up all the moisture. In this case, there is no need for lubricants.
2. Kegel Exercises
Regular Kegel exercises solve most of the problems – they prevent the prolapse of the pelvic organs, strengthen the muscles, and the vagina becomes more capacious. As a result, the “G-spot” becomes easily attainable for the penis, which automatically eliminates anorgasmia.
The same exercise is shown if a woman has a relaxed vaginal syndrome – muscle turgor improves, and the woman begins to feel something that she did not feel before.
3. Plasmolifting
During plasmolifting of the vagina, we inject the woman with her own fibroblasts, which in themselves are the source of her own hyaluronic acid.
Blood is taken from a woman, driven through a centrifuge and after a while we draw plasma into a syringe, which will remain on top of the test tube. After that, we inject plasma into the vagina, and hyaluronic acid begins to do its job, that is, to attract water to itself.
Often, after this procedure, women also no longer need artificial lubricants – it is in our power to renew the epithelium, moisturize it and “feed it with goodies.Then both the clitoris and the vagina will start to please us again.
4. Laser treatment
The laser is a unique tool that can fix almost all problems. Very often, patients who seek the help of a laser have undergone oncology. Often, due to illness, women are forced to remove the uterus along with the ovaries, so estrogens are no longer produced.
Accordingly, the vaginal mucosa is very dry, and such women simply cannot live a sexual life – when everything is removed, the vagina has nowhere to take hormones to moisturize.Due to dryness, the vagina becomes very thin – like the peel of an apple, which should be juicy. New laser technologies make a thick vagina out of a thin vagina, because the better it is estragonized, the better – the vagina again begins to moisturize and produce its own hyaluronic acid.
The laser also fights against the relaxing vaginal syndrome – it is an ideal alternative to the classic surgery. In fact, it does not affect the muscles in any way, but it can tighten the mucous membrane – it becomes elastic and contracts more strongly.Under the influence of a laser, the vagina narrows by 20%, and often for women, this is quite enough.
In the first place on the list of reasons why women end up in the gynecologist’s office is vaginal discharge. They recur – patients are given treatment, and in the best case, we take them with the same problem in six months. Therefore, when we cannot cope with the problem with the help of local treatment (candles, etc.), we turn to the laser.
The vaginal tract as a whole, like the microbes in it, also reflects the general state of the body – we do not understand what we eat, we live in cities where only one name remains from the ecology.All this is reflected in the vaginal tract. There are 10,000 germs in the vagina, and when this number grows, the woman begins to experience such problems. The laser renews the epithelium in the vagina – thanks to its effect, the vaginal walls begin to secrete glycogen, a nutrient for lactobacilli.
They live only where they can eat, and leave the place where they cannot survive – then microbes come in their place, which are manifested by secretions. The laser, on the other hand, stimulates the layer of the walls of the vagina and triggers the production of glycogen – lactobacilli begin to return, and the discharge passes.
Obstetrician-gynecologist, doctor of ultrasound diagnostics, member of the Association of Gynecologists and member of the Russian Association of Endometriosis Inna Davidovna Dzhidzhoeva.
Lungs from the back photo
Lungs are the main part of the human respiratory system, which play the main function in the process of breathing and supplying blood with oxygen.
Where are they in the human body? Which doctor should I go to if I have lung problems?
Location of the lungs in the human body
The lungs are located in the human chest, which, due to its shape, affects the appearance of the respiratory organ.They can be narrow or wide, elongated.
This organ is located, starting from the clavicle up to the nipples, at the level of the thoracic and cervical spine. They are covered with ribs, as they are vital in humans.
The lungs are separated from the rest of the internal organs that do not belong to the respiratory system (spleen, stomach, liver and others) by the diaphragm. In the chest, in the middle of the lungs, are the heart and blood vessels.
In the autumn, during stress, with a lack of vitamin, a person’s immunity weakens, so it is so important to strengthen it.The drug is completely natural and allows you to recover from colds in a short time.
Possesses expectorant and bactericidal properties. Strengthens the protective functions of the immune system, perfect as a prophylactic agent. I recommend.
Human Lung Anatomy
The right lung is one tenth larger than the left lung, however, it is shorter. The left lung is narrower, this is due to the fact that the heart, being in the middle of the chest, moves more to the left, taking away some space from the lung.
Each part of the organ has the shape of an irregular cone, its base is directed downward, and the apex is rounded, slightly protruding above the rib.
The lungs have three parts:
- Lower . Located at the diaphragm, adjacent to it.
- Rib. Convex part touching the ribs.
- Medial. Concave part touching the spine.
The lungs consist of:
Take care of your health! Strengthen your immune system!
Immunity is a natural reaction that protects our body from bacteria, viruses, etc.It is better to use natural adaptogens to increase the tone.
It is very important to maintain and strengthen the body not only by the absence of stress, good sleep, nutrition and vitamins, but also with the help of natural herbal remedies.
In such cases, our readers recommend using the newest tool – Immunity to strengthen the immune system .
It has the following properties:
- Kills viruses and eliminates secondary signs of influenza and SARS in 2 days
- 24 hours of immunity protection during the infectious period and during epidemics
- Kills putrefactive bacteria in the gastrointestinal tract
- The preparation contains 18 herbs and 6 vitamins, extracts and concentrates of plants
- Removes toxins from the body, shortening the rehabilitation period after illness
Blood supply to the lungs
One of the functions of the lungs is gas exchange in the blood.For this reason, both arterial and venous blood flows.
The latter flows to the pulmonary capillaries, emits carbon dioxide, receives oxygen in return.
Pulmonary alveoli are small vesicles with a thick network of capillaries. The exchange of oxygen and carbon dioxide directly depends on these “balls”, and they provide the blood with oxygen.
Stories from our readers!
“After pneumonia, I drink to maintain immunity.Especially during the autumn-winter periods, during epidemics of flu and colds.
Drops are completely natural and not only from herbs, but also with propolis and badger fat, which have long been known as good folk remedies. It performs its main function perfectly well, I advise. “
Lung specialist
If a person has complaints related to the lungs, he can make an appointment with the pulmonologist – a specialist who examines and treats the respiratory organ.
A treating therapist, otolaryngologist, infectious disease specialist can also refer to him if complications are observed after colds, flu, tonsillitis, bronchitis, tracheobronchitis, when harmful bacteria descend through the bronchi below – into the lungs.
In case of tuberculosis, the lungs are not dealt with by a pulmonologist, but by a phthisiatrician. A surgeon who operates on the respiratory organs is called a thoracic surgeon.
The main cause of bronchitis accompanied by sputum is a viral infection.The disease occurs due to damage by bacteria, and in some cases – when the body is exposed to allergens.
Now you can safely buy excellent natural preparations that alleviate the symptoms of the disease, and in up to several weeks allow you to completely get rid of the disease.
Types and methods of lung examination
To understand what kind of ailment struck the respiratory organ, it is necessary to conduct diagnostic studies. What are they?
- Real-time X-ray, when the image is displayed.The most common, completely painless examination method.
Gives a clear picture of the pulmonary pattern, where all foci of inflammation and fluid are visible. There are also disadvantages: only large foci of pathology are visible. - X-ray. The difference of this diagnostic method is that the image is displayed not on the monitor of the device, but on a special film.
Thus, it is easy to identify tuberculosis, pneumonia, consequences after injury, developmental anomalies, the presence of neoplasms, parasites. - Fluorography. By the principle of research, it is similar to X-ray. This procedure must be completed annually by people over 15 years of age.
Often in polyclinics, in some cases, when hiring, they require fresh results of fluorography. - MRI. Computer diagnostics gives a clear picture of the chest in cross section. With this method, you can see all the changes in the bronchi and trachea, lung tissue.
- Bronchography. Performed with local anesthesia to diagnose the condition of the bronchi.
A special substance is injected into the lumen of these organs, which does not allow X-rays to pass through, after which a regular picture is taken, in which you can see a detailed and clear image of the bronchial system.
In this way, you can see the expansion, abscesses, foreign bodies, formations. - Bronchoscopy. The procedure is performed using a special tool.So that the patient does not experience discomfort, it passes under anesthesia.
The device is inserted through the mouth, a biopsy is performed, a tissue image is taken. With this method, it is easy to remove foreign objects from the lungs from the patient, remove polyps. Revealed erosion and ulcers, neoplasms. - Thoracoscopy. It is also carried out with the help of a special object, only it is inserted not through the mouth, but a puncture in the chest.
- Ultrasound. Doctors do not often use this method of examination.After all, ultrasound does not penetrate the alveoli. This is how the puncture procedure is mainly controlled.
- Pulmonary ventilation. Determines the volume of the lungs.
- Pleural puncture. The contents of the pleural cavity are taken through the puncture, so that this biomaterial is subsequently sent for study. It is carried out to check for abnormal accumulations of fluid and air.
- Examination of sputum.
Common lung diseases
- Pneumonia. Inflammatory process in the lungs caused by microbes and viruses.
The main symptoms are severe cough, high fever, sebaceous gland dysfunction, shortness of breath (even at rest), chest pain, sputum streaked with blood. - Cancer. Cause a bad habit (smoking), a hereditary factor. The appearance of cancer cells in the respiratory organ leads to their rapid multiplication and the appearance of malignant tumors.
They make breathing difficult, spread to other internal organs.Ends with a lethal outcome if you start treating in the last stages, not treating at all. - Chronic obstructive pulmonary disease.
Restriction of air flow in the lungs.
Begins with common cough and mucus.
If you do not start treatment on time, it will be too late, the disease will become irreversible. - Tuberculosis. A highly contagious disease. Called with Koch’s wand. It affects not only the lungs, but also other internal organs, for example, the intestines, bone tissue, joints.
- Emphysema. The main symptom is shortness of breath. Pulmonary alveoli burst, merge into large air sacs, which do not cope with their function. This makes breathing difficult.
- Bronchitis. The mucous membrane of these organs becomes inflamed and swells. An abundant secretion of mucus begins, from which the human body tries to get rid of. This causes coughing fits.
- Asthma. Contraction of the fascicular and striated muscles.The airways are narrowed, seizures occur when the patient begins to lack oxygen in the body. Asthma often appears on the background of allergies.
The lungs are located in the chest above the diaphragm, but below the collarbones. They are protected as an important organ of vital activity by the ribs. Respiratory diseases are very common.
These include bronchitis, asthma, pneumonia, cancer and others. The lungs can be examined in many ways, the most popular is the procedure when an X-ray is taken.
A specialist who studies and treats the lungs is called a pulmonologist.
More than 60% of people are faced with back pain in the area of the lungs behind at the age of 20-60. And reasons for this may be a mass: osteochondrosis, pneumonia, bronchitis, tuberculosis, inflammation, hypothermia and even great physical exertion.
Many people wonder if the lungs can hurt from the back, discomfort and heaviness in the right lung, spasm in the chest and discomfort when breathing in air can be felt.And the answer is definitely yes!
Why does my back and lungs hurt?
Pain in the lungs when coughing and in the back on the left occurs for various reasons, which must be immediately identified, and only then to fight the symptoms and disease. Sometimes the reason lies in the fact that the person has a cold back and warms up enough, and sometimes the patient is diagnosed with lung cancer.
Also occurs:
- Osteochondrosis;
- Hernia;
- Pneumonia;
- Lung cancer;
- Ischemia and pathology of the heart;
- Neuralgia in the rib area.
Photo Gallery:
But at the last stage of the disease and the clinical picture will be enough.
Signs of illness
The type of problem can be determined by a number of signs that depend on the disease, the stage of damage to the body, the location of the foci of inflammation and the general condition of the patient.
Back pain can be classified into the following groups:
| Group No. | Description |
|---|---|
| 1 | Stitching, aching and pressing |
| 2 | Moderate, pronounced |
| 3 | Permanent and occasional |
| 4 | Arising during inhalation, movement of the chest |
| 5 | Releasing to the back, neck and abdomen |
Pathologies of the spinal column
To enlarge, click on the photo
If the problem lies in the pathology or diseases of the spine, then pain occurs when the body moves, has an acute or aching character.
A number of signs can indicate the development of osteochondrosis, hernia and rheumatism:
- Numbness, tingling;
- Decreased sensitivity;
- Change in skin tone;
- Decreased muscle tone, weakness.
Recommended for viewing:
Pneumonia
Pneumonia on X-ray
If you feel discomfort in the chest, heaviness in the lungs on the left, then there may be problems with the lungs, namely pneumonia or pleurisy.
Then the manifestations are expressed in:
- Cough;
- Discharge of pus or mucus;
- Temperature change.
The pain is especially aggravated during inhalation-exhalation, during coughing.
Related videos:
Headache, decreased physical activity and weakness are considered additional symptoms of the disease. Pneumonia can be detected only after radiography and cytological analysis.
Sometimes tingling in the back from the side of the lungs with cancer, and the last stage, when the disease has spread to the bone tissue and lymph nodes.
Then the main signs may be completely absent, but there are such manifestations:
- Lingering cough;
- Shortness of breath;
- Discharge of blood when coughing;
- Poor appetite;
- General weakness;
- Exhaustion.
Initially, the pain appears when inhaling, then it becomes difficult to breathe, the temperature rises to 37-37.5 degrees.
It is also important that the location of the pain can determine the localization of the tumor, which simplifies the diagnosis.
It will be useful to view:
Ischemia and heart disease
With a feeling of heaviness and pain behind the sternum, which radiates to the side or arms, it is possible to exclude a heart attack and angina pectoris, and talk about ischemia.
It also has the following manifestations:
- Pallor;
- Increased perspiration;
- Difficulty breathing;
- Rapid pulse;
- Tingling sensation in the chest.
Useful video:
Neuralgia of the rib department
If pain appears in the area of the scapula, behind the back when inhaling, then we can talk about neuralgia of the ribs. Usually, the pain intensifies and spreads along the sternum during movement.
We wrote more about pain in the sternum in this article.
Also observed:
- Numbness;
- Loss of sensitivity or increased sensitivity;
- Spread of pain in the arms and lower back.
Video about intercostal neuralgia:
Hospital examination
External examination or conclusions from the clinical picture are not enough to determine the type of disease.
Typically, patients are prescribed differential diagnosis in the hospital, which includes:
- Complete blood count;
- Bacteriological and cytological analysis of sputum from the lungs;
- X-ray of the spine and lungs;
- Bronchoscopy;
- Tomography or ultrasound.
Related photos:
Discomfort with inflammation of muscles and joints
Areas affected by myositis
Muscle disorders are often the cause of pain, spasms and discomfort. Then they swell and constantly contract, which is called “myositis”.
Causes of the problem:
- Hypothermia;
- Great physical stress;
- Damage;
- Infection and inflammation.
When the inflammation spreads, the pain is felt in the back, it intensifies with the load on the sternum.
Pain on the right side of the lungs
If pain during breathing and coughing is concentrated on the right side, under the ribs and back in the lungs, then there are several reasons, depending on the clinical picture discussed in the table:
| Disease | Manifestations |
|---|---|
| Pleurisy, pneumonia and tuberculosis | Cough, shortness of breath, bleeding, fever and sweating. |
| Pancreatitis, liver cirrhosis | Spasmolytic pain in the lungs or behind the back, abdominal discomfort, vomiting, general weakness and high fever, feeling as if colitis under the right side. |
to contents ↑
Other problems
Often, back pain occurs for a number of other reasons, and not only pathology of the spine or pneumonia.
Since the back is a vast area in the human body, malfunctioning of all internal organs can affect it, namely:
- Heart , when vasospasm with angina pectoris is sufficient for the occurrence of pain that spreads to the sternum and scapula.Even with a heart attack, only the dorsal muscles of the back are often affected without other symptoms;
- Lungs , when inflammation makes itself felt only during coughing, breathing and movement of the chest;
- Kidney , when the organ increases in size due to stone and inflammation. Then the pain appears in the back and can be given to the abdomen, ribs and lungs from behind;
- Pathology of the gastric tract , when pulling pains in the abdomen are projected onto the back, the back of the lungs and ribs.The reason for this may be a hernia, diseases of the stomach and intestines. Increased back pain in the back of the lungs after eating.
Suggest viewing:
Pain treatment
Often with the appearance of back pain, coughing, shortness of breath and discomfort, and cramps in the back of the chest, patients take painkillers or blockers such as Analgin, Novocaine or Renalgan. But they only relieve general manifestations and symptoms, but do not cure the disease.
You can use non-steroidal anti-inflammatory drugs that relieve inflammation and infections in tissues, have an analgesic effect.
They are taken only for pathology of the spine and hypothermia of the discs, because with diseases of the digestive tract, they worsen the symptoms. At the same time, chondoprotectors or warming ointments, corsets and compresses can be prescribed.
The course of treatment is developed by a doctor, but depends on the specific problem. After all, self-medication often leads to death or dysfunction of the kidneys, liver and myocardial infarction.
Results
It is important that a patient with back pain in the back immediately goes to the hospital and undergoes a full diagnosis.
It is impossible to make a diagnosis on your own based on a couple of signs, because only doctors will provide qualified assistance on the territory of the hospital. This saves not only health, but also life!
Add article to social networks:
Comments
I do not care very much about my health, but when I have pains from the back against the background of coughing, I go to the doctor.Pneumonia is a dangerous disease, you can not start it in any case.
In the structure of the human body, quite interesting is such an “anatomical structure” as the chest, where the bronchi and lungs, the heart and large vessels, as well as some other organs are located. This part of the body, formed by the ribs, sternum, spine and muscles, is designed to reliably protect the organ structures located inside it from external influences. Also, due to the respiratory muscles, the chest provides breathing, in which the lungs play one of the most important roles.
The human lungs, the anatomy of which will be discussed in this article, are very important organs, because it is thanks to them that the breathing process is carried out. They fill the entire chest cavity, with the exception of the mediastinum, and are the main ones in the entire respiratory system.
In these organs, oxygen in the air is absorbed by special blood cells (erythrocytes), and carbon dioxide is released from the blood, which then breaks down into two components – carbon dioxide and water.
Where are the lungs in humans (with photo)
Approaching the question of where the lungs are located, it is worth first paying attention to one very interesting fact concerning these organs: the location of the lungs in humans and their structure are presented in such a way that they very organically combine the airways, blood and lymphatic vessels and nerves.
Outwardly viewed anatomical structures are quite interesting. In its shape, each of them looks like a vertically dissected cone, in which one convex and two concave surfaces can be distinguished.Convex is called costal, due to its direct attachment to the ribs. One of the concave surfaces is diaphragmatic (adjacent to the diaphragm), the other is medial, in other words the median (i.e., located closer to the median longitudinal plane of the body). In addition, interlobar surfaces are also distinguished in these organs.
With the help of a diaphragm, the right part of the anatomical structure we are considering is separated from the liver, and the left part from the spleen, stomach, left kidney and transverse colon.The median surfaces of the organ are bordered by large vessels and the heart.
It is worth noting that the location of the lungs in humans also affects their shape. If a person has a narrow and long chest, then the lungs are correspondingly elongated and vice versa, these organs have a short and wide appearance with a similar shape of the chest.
Also in the structure of the described organ there is a base that lies on the dome of the diaphragm (this is the diaphragmatic surface) and the apex protruding into the neck area about 3-4 cm above the clavicle.
To form a clearer idea of what these anatomical structures look like, as well as to understand where the lungs are located, the photo below will be perhaps the best visual aid:
Anatomy of the right and left lung
Remember that the anatomy of the right lung is different from that of the left lung. These differences are, first of all, in the number of shares. There are three of them on the right (the bottom, which is the largest, the top, slightly smaller, and the smallest of the three is the middle), while in the left there are only two (top and bottom).In addition, the left lung has a tongue located on its anterior edge, and this organ, due to the lower position of the left dome of the diaphragm, is slightly longer than the right one.
Before entering the lungs, air first passes through other, equally important parts of the respiratory tract, in particular the bronchi.
The anatomy of the lungs and bronchi overlaps, and so much so that it is difficult to imagine the existence of these organs separately from each other. In particular, each lobe is divided into bronchopulmonary segments, which are parts of the organ, to one degree or another isolated from the same neighboring ones.Each of these sites has a segmental bronchus. In total, there are 18 such segments: 10 on the right and 8 on the left of the organ.
The structure of each segment is represented by several lobules – areas within which the lobular bronchus branches out. It is believed that a person has about 1600 lobules in his main respiratory organ: about 800 each on the right and left.
However, the conjugation of the location of the bronchi and lungs does not end there. The bronchi continue to branch, forming bronchioles of several orders, and they, in turn, give rise to alveolar passages, dividing from 1 to 4 times and ending, in the end, with alveolar sacs, into the lumen of which the alveoli open.
A similar branching of the bronchi forms the so-called bronchial tree, otherwise called the airways. In addition to them, there is also an alveolar tree.
Anatomy of the blood supply to the lungs in humans
Anatomy connects the blood supply to the lungs with the pulmonary and bronchial vessels. The former, entering the small circle of the bloodstream, are mainly responsible for the function of gas exchange. The latter, belonging to a large circle, provide nutrition to the lungs.
It should be noted that the provision of the body largely depends on the extent to which the various pulmonary areas are ventilated. It is also influenced by the relationship between the rate of blood flow and ventilation. A significant role is also played by the degree of saturation of the blood with hemoglobin, as well as the rate of passage of gases through the membrane located between the alveoli and capillaries, and some other factors. When even one indicator changes, the physiology of respiration is disturbed, which negatively affects the entire body.
.



