Soreness in hips and lower back. Treating Lower Back and Hip Pain: A Comprehensive Guide
Discover effective solutions to relieve lower back and hip pain. Learn about the common causes, signs to seek medical care, and lifestyle changes to manage and prevent recurrence of this widespread issue.
Understanding the Connection Between Lower Back and Hip Pain
The lower back and hips are closely connected through muscles, ligaments, and nerves, creating common pathways for pain. According to the 2019 National Health Interview Survey, 39% of U.S. adults reported having lower back pain, while 36.5% had pain in their hips and lower limbs. This interconnectedness means that pain in one area can often manifest in the other.
Common Causes of Lower Back and Hip Pain
There are several potential reasons for experiencing pain in the lower back and hips, including:
- Muscle Strain: Overuse, injury, or weakness in the muscles that support the back and hips can lead to strain and pain.
- Pinched Nerve: Compression of a nerve in the lower back can cause pain, tingling, numbness, and weakness that radiates to the hips and legs.
- Arthritis: Osteoarthritis in the spine’s facet joints or the hip joint can cause pain and stiffness.
- Herniated Disc: A bulging or ruptured disc in the lower back can press on sensitive nerves, leading to radiating pain.
- Sacroiliac Joint Pain: Inflammation or injury to the sacroiliac joint, which connects the lower back to the pelvis, can result in sharp or dull aching pain.
- Pelvic Floor Muscle Imbalance: Tension or weakness in the pelvic floor muscles can contribute to lower back and hip pain.
When to Seek Medical Attention
Most cases of lower back and hip pain can be effectively treated with conservative and holistic methods. However, there are some signs that may indicate the need for medical care, including:

- Persistent pain lasting more than three months
- Severe, debilitating pain
- Radiating pain down the leg or into the foot
- Numbness, tingling, or weakness in the leg or foot
- Difficulty standing or walking
- History of cancer, osteoporosis, or other underlying health conditions
Lifestyle Changes to Manage Lower Back and Hip Pain
While the specific cause of your pain may be important, the most effective approach often focuses on management and prevention rather than just addressing the underlying issue. Here are some lifestyle changes that can help treat and prevent lower back and hip pain:
- Regular Gentle Movement: Low-impact exercises, such as walking, swimming, or yoga, can help keep the back and hips mobile and strong.
- Strengthening the Core: Building up the muscles in the abdomen, back, and hips can provide better support and stability.
- Improving Posture and Ergonomics: Paying attention to your posture, especially when sitting or standing for long periods, can reduce strain on the back and hips.
- Applying Ice/Heat Therapy: Using ice packs or heat pads can help reduce inflammation and pain in the affected areas.
- Over-the-Counter Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help manage pain and reduce inflammation.
Simple Exercises to Relieve Lower Back and Hip Pain
Incorporating the following exercises into your daily routine can help alleviate lower back and hip pain:

- Cat-Cow Pose: Start on your hands and knees, then alternate between arching your back and tilting your pelvis (cat pose) and dropping your belly towards the floor while lifting your head and tailbone (cow pose).
- Pelvic Tilts: Lie on your back with your knees bent and feet flat on the floor. Slowly tilt your pelvis to flatten your lower back against the floor, then release to a neutral position.
- Glute Bridges: Lie on your back with your knees bent and feet flat on the floor. Lift your hips up, engaging your glutes, then lower back down.
- Leg Swings: Stand with one hand on a wall or chair for balance, then swing your leg back and forth, keeping your core engaged.
When to Seek Professional Help
If your lower back and hip pain persists despite trying conservative treatments, it may be time to consult a healthcare professional, such as a physical therapist or orthopedic specialist. They can provide a comprehensive evaluation, diagnose the underlying cause, and develop a personalized treatment plan to help you manage and overcome your pain.

Conclusion
Lower back and hip pain can be a debilitating and frustrating experience, but with the right approach, it can often be effectively treated and managed. By understanding the common causes, recognizing when to seek medical attention, and incorporating lifestyle changes and simple exercises, you can take steps to alleviate your pain and prevent it from recurring. Remember, the key is to listen to your body, stay active, and work closely with healthcare professionals to find the best solution for your individual needs.
How to Treat Your Lower Back and Hip Pain
If you feel like your low back and hip started aching at the same time, it’s likely not your imagination. The back and hips are often partners in pain. According to the 2019 National Health Interview Survey, some 39% of U.S. adults reported having lower back pain over the last few months, while 36.5% had pain in their hips and lower limbs.
The hips and spine are connected by muscles, ligaments, and nerves, which create common pathways to pain. Lower back and hip pain may range from a dull soreness to tingling, radiating pain. It often stops you from doing the daily activities you need to thrive. However, back and hip pain usually is not serious and can be treated and prevented with conservative and holistic practices.
Here are some common causes of back and hip pain, signs to seek medical care, and lifestyle changes to help treat pain and keep it from returning, including simple at-home exercises recommended by our physical therapists.
What Causes Lower Back and Hip Pain?
Pain in these areas may involve an injury to the soft tissues or an underlying issue with the bones or joints. Sometimes, though, there is no obvious reason for your pain, especially if it persists for more than three months. In this case, it’s much less important to focus on the why of what’s causing your pain. Rather, it’s better to think about how to get relief. Regular gentle movement is often the best thing you can do for chronic back and hip pain.
Even if your doctor finds a structural cause, the majority of people heal without surgery, using at-home remedies such as activity modifications, ice/heat therapy, physical therapy exercises, and over-the-counter medications.
Here are some of the most common reasons you may experience pain in your lower back and hips.
Muscle strain. The back and hips share a mission: to be a strong anchor for your legs. “If your back and hips are not strong and stable as your leg moves, then they are going to move, too, and that can lead to overuse issues,” says Lori Walter, PT, DPT, a physical therapist at Hinge Health. There are countless ways you might strain your back or hips, from lifting a heavy load to a traumatic fall or injury to sitting for hours at a time. Weak core muscles may also lead to strain, as your back muscles will engage to compensate for underperforming ones. Muscle strain often heals on its own in a few days.
There are countless ways you might strain your back or hips, from lifting a heavy load to a traumatic fall or injury to sitting for hours at a time. Weak core muscles may also lead to strain, as your back muscles will engage to compensate for underperforming ones. Muscle strain often heals on its own in a few days.
Pinched nerve. When muscle, bone, or tissue presses down and compresses a nerve, the result is pain, tingling, numbness, and weakness. A pinched nerve in the lower back can cause these symptoms in the back, hips, buttocks, and lower legs. There are many reasons a nerve may become pinched, including arthritis, a herniated disc, a sports injury, repetitive motion, pregnancy, or excess weight. Pinched nerves often heal over four to six weeks with rest, ice/heat therapy, and over-the-counter medications.
Arthritis. The cartilage that facilitates smooth motion of the small joints in the back of the spine can become worn over time. This can lead to osteoarthritis in the facet joints that support motion of the vertebrae.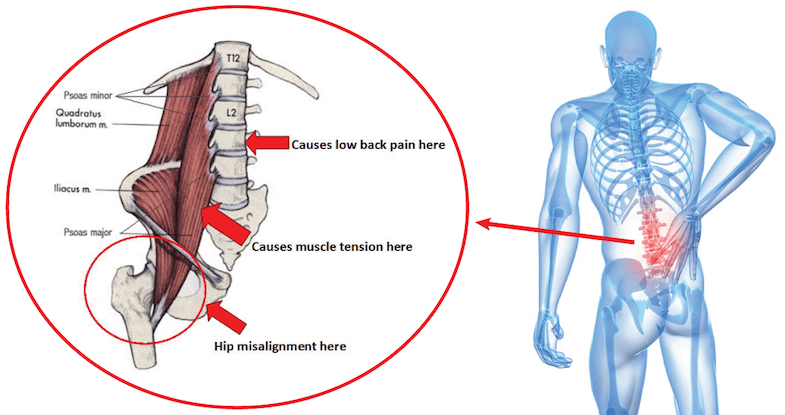 They may rub together, causing pain and stiffness. Similarly, osteoarthritis of the hip occurs when the cartilage that cushions the hip joint wears away. This can lead to pain, stiffness, and limited range of motion in the hip.
They may rub together, causing pain and stiffness. Similarly, osteoarthritis of the hip occurs when the cartilage that cushions the hip joint wears away. This can lead to pain, stiffness, and limited range of motion in the hip.
Herniated disc. This is another problem that can be caused by common changes in the spine. As the discs compress, the jelly-like center can push out, causing the disc to press into sensitive spinal nerves. You may feel a sharp or burning pain, along with numbness, tingling, and weakness. Depending on which lumbar nerves are irritated, the pain may radiate through your hip into the front thigh or all the way down to your toes. The majority of herniated discs heal over several weeks without surgery, with physical therapy and non-steroidal anti-inflammatory drugs (NSAIDs like ibuprofen) as first-line remedies.
Sacroiliac joint pain. The sacroiliac (SI) joint connects the lower back to the pelvis. The joint can become inflamed due to arthritis or injury, leading to sharp, stabbing or dull, aching pain in the back, hip, and buttocks.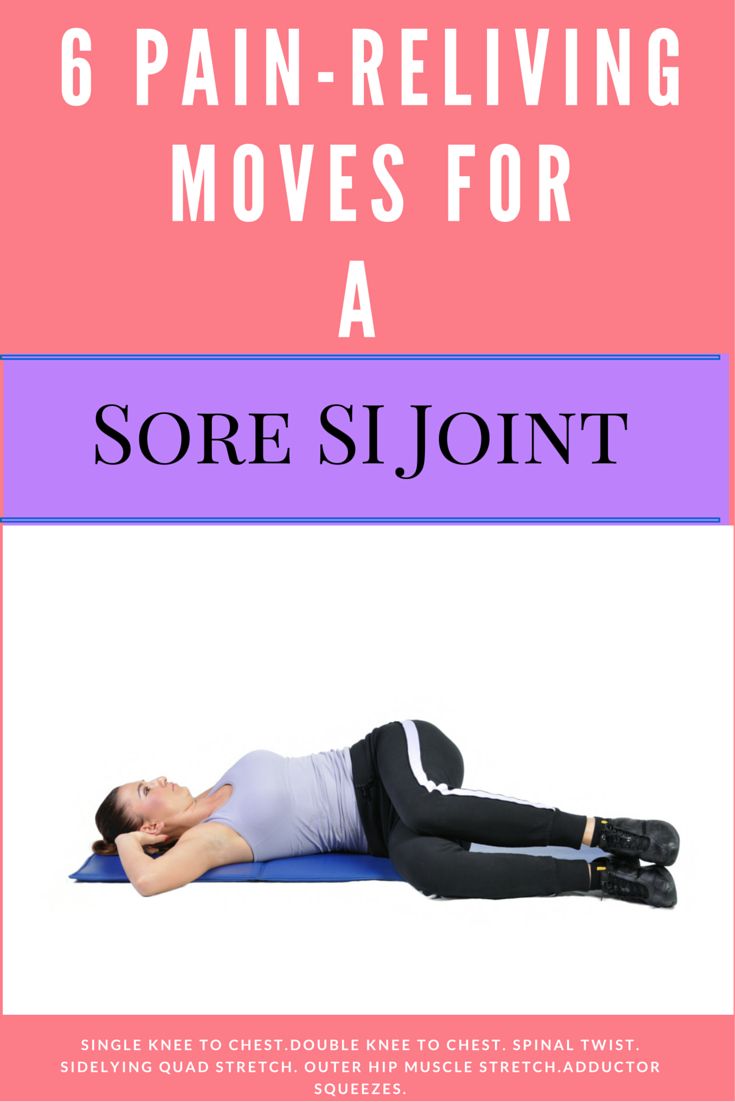 Sacroiliac joint pain may be involved in 10-25% of lower back pain cases.
Sacroiliac joint pain may be involved in 10-25% of lower back pain cases.
Pelvic floor muscle imbalance. The pelvic floor muscles line the bottom of the pelvis and connect to the back through the tailbone. If the pelvic floor muscles become tight or tense, this can lead to pain (often a dull ache). Pelvic floor pain is frequently mistaken for back pain, says Dr. Walter. As pelvic floor muscles struggle to support the internal organs of the pelvis, the back muscles work harder to compensate, leading to overuse and strain.
What About Sciatica?
You may be wondering if your low back and hip pain could be due to sciatica. This term describes pain that originates in an irritated nerve of the lower back that travels down the sciatic nerve, which runs down the buttock and lower leg. The pain can feel sharp, burning, cramp-like, or like a “pins and needles” tingling. Sciatica is usually caused by a condition that pinches the nerves, such as arthritis (particularly in older adults) or a herniated disc (typically in those under age 40).
When to See a Doctor
Most of the time, pain that’s affecting your low back and hip will improve within a few days to a few weeks, with conservative approaches like ice/heat, over-the-counter medication, and gentle exercise. However, it’s a good idea to see a doctor if you notice any of the following:
You experience weakness in your lower extremities.
Your pain is severe, unrelenting, does not improve with time and home remedies, or interferes with your daily activities.
You’ve had a traumatic fall or injury.
Your pain occurs with signs of more serious illness such as fever, chills, unexplained weight loss, or loss of bowel or bladder control.
Holistic Treatments for Back and Hip Pain
For long-term relief and prevention of future pain episodes, pain management experts recommend a holistic approach that treats the biological, psychological, and social/spiritual roots of chronic pain. Studies have shown that people’s reported pain levels often do not correspond to structural causes (like herniated discs) seen on imaging studies.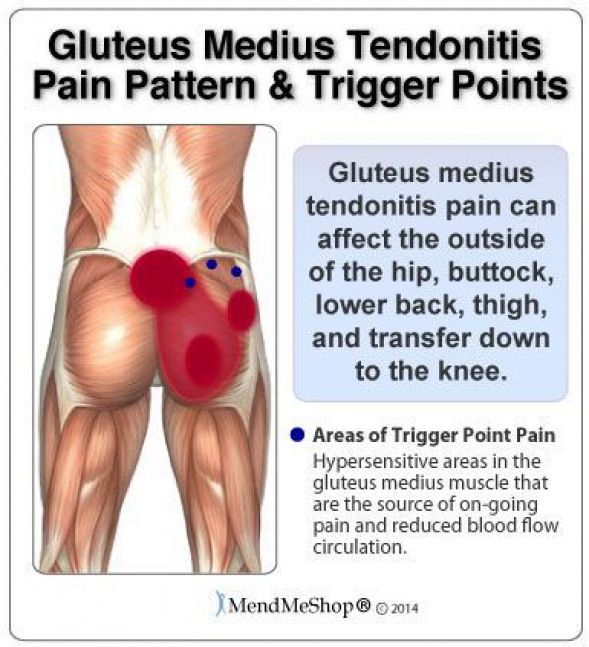 Experts now believe this is because ongoing pain actually changes how our nervous system interprets pain. Chronic pain can make people more sensitive to pain. People with chronic pain often develop emotional distress that makes pain worse.
Experts now believe this is because ongoing pain actually changes how our nervous system interprets pain. Chronic pain can make people more sensitive to pain. People with chronic pain often develop emotional distress that makes pain worse.
Holistic practices — exercise, stress management, healthy eating, and other lifestyle changes — can bring relief by addressing physical causes as well as psychological and emotional ones. Truly holistic pain management may involve different approaches and providers, including doctors, physical therapists, nutritionists, and mental health professionals. Consider these:
Physical therapy. Physical therapists can help diagnose and treat musculoskeletal imbalances that cause pain. They can design a customized exercise plan to strengthen, stretch, and stabilize muscles and joints to relieve and prevent pain. “Physical therapy also helps desensitize the nervous system to pain,” says Dr. Walter. “By guiding people to move up to the point of pain, and then come out of it, and then moving a little further next time, the brain starts to learn, ‘okay, that movement is safe. ’”
’”
You can see a physical therapist in person or use a program like Hinge Health to access a PT via telehealth/video visit.
Personal training. “After people complete physical therapy, I sometimes recommend personal training to help them stay motivated to exercise or to continue to build strength,” says Dr. Walter.
Clean diet. European researchers analyzed 10 years of studies on eating patterns and chronic pain. They found that certain diets helped improve pain and quality of life by reducing inflammation or providing important nutrients, including antioxidants and prebiotics. Experts recommend that you reduce your intake of pro-inflammatory foods, such as added sugar, processed meat, and refined grains. Fill up on anti-inflammatory choices such as fruits and vegetables, whole grains, fish, and olive oil.
Stop smoking. Smoking accelerates disc degeneration of the spine, according to the American Academy of Orthopaedic Surgeons.
Massage. An analysis of 60 studies showed that massage therapy helped people manage their pain better than people who received only sham or placebo treatments. Experts believe that massage helps people lower stress and deal with the emotional distress of pain better, and also soothe the physical discomfort of tight muscles.
Meditation. Research shows that women with lower back pain who practiced mindfulness meditation reported lower pain and better quality of life and mental health after eight sessions, compared to those who received standard care. The women learned mindfulness techniques such as body scans and walking and sitting meditations.
Lifting and sitting mechanics. Asking your body to lift or carry more than you’re used to, or to sit in one position for too long are common causes of muscle strain, says Dr. Walter. Avoid lifting when you are tired, and don’t lift much more than what you practice lifting regularly. Bring the object as close to your body as possible and exhale as you lift, using a wide stance for stability.
When sitting, try to keep your sit bones (the bottom of your pelvis) higher than your knees. Use pillows or rolled-up towels for support if needed. Your computer screen should be at eye level and you want your feet flat on the floor with elbows bent and supported at 90 degrees. Feel free to adjust how you sit, and take regular posture breaks to stretch every 30 minutes.
Counseling. In a study of adults who participated in an eight-session telehealth counseling program that emphasized that pain is a non-dangerous brain activity rather than physical tissue injury, 66% reported being pain-free or nearly pain free after one month. This suggests that helping patients understand and conceptualize their pain could bring significant relief. Psychological counseling can also help people learn coping skills (such as cognitive behavioral therapy) to combat the depression, anxiety, and emotional distress that develops when chronic pain limits your life and continues without relief.
While all of the above steps can help lower back and hip pain, one of the most effective is regular exercise therapy. Hinge Health recommends these moves to reduce and prevent back and hip pain as part of a holistic health routine. Those moves are safe to do daily. Start slowly, aiming to do them once or twice a week, and build from there. If you’re wondering if these moves are right for you, check with your healthcare provider.
The information contained in these videos is intended to be used for educational purposes only and does not constitute medical advice or treatment for any specific condition. Hinge Health is not your healthcare provider and is not responsible for any injury sustained or exacerbated by your use of or participation in these exercises. Please consult with your healthcare provider with any questions you may have about your medical condition or treatment.
PT Tip: Use a Stool During Standing Chores
When you’re standing at a counter for a long time, such as while cooking or cleaning, put one foot up on a stool, as if you are about to step up. “This puts the back in a more neutral position and rotates the pelvis,” says Dr. Walter. “This increases comfort and allows you to tolerate standing longer.” If you don’t have a stool, open a low cabinet and put your foot on the floor of the cabinet.
“This puts the back in a more neutral position and rotates the pelvis,” says Dr. Walter. “This increases comfort and allows you to tolerate standing longer.” If you don’t have a stool, open a low cabinet and put your foot on the floor of the cabinet.
Learn More About Hinge Health for Back and Hip Relief
Our digital programs for back and joint pain are offered for free through benefit providers. Click here to see if you’re eligible.
This article and its contents are provided for educational and informational purposes only and do not constitute medical advice or professional services specific to you or your medical condition.
References
As-Sanie, S., Harris, R., Napadow, V., Kim, J., Neshewat, G., Kairys, A., Williams, D., Clauw, D., & Schmidt-Wilcke, T. (2012). Changes in regional gray matter volume in women with chronic pelvic pain—A voxel based morphometry study. Pain, 153(5), 1006–1014. doi:10.1016/j.pain.2012.
 01.032
01.032Bedson, J., & Croft, P. R. (2008). The discordance between clinical and radiographic knee osteoarthritis: A systematic search and summary of the literature. BMC Musculoskeletal Disorders, 9(1), 116. doi:10.1186/1471-2474-9-116
Buchanan, B. K., & Varacallo, M. (2022). Sacroiliitis. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK448141/
Chronic Pelvic Pain: ACOG Practice Bulletin, Number 218. (2020). Obstetrics and Gynecology, 135(3), e98–e109. doi:10.1097/AOG.0000000000003716
Crawford, C., Boyd, C., Paat, C. F., Price, A., Xenakis, L., Yang, E., & Zhang, W. (2016). The Impact of Massage Therapy on Function in Pain Populations—A Systematic Review and Meta-Analysis of Randomized Controlled Trials: Part I, Patients Experiencing Pain in the General Population. Pain Medicine: The Official Journal of the American Academy of Pain Medicine, 17(7), 1353–1375.
 doi:10.1093/pm/pnw099
doi:10.1093/pm/pnw099Dragan, S., Șerban, M.-C., Damian, G., Buleu, F., Valcovici, M., & Christodorescu, R. (2020). Dietary Patterns and Interventions to Alleviate Chronic Pain. Nutrients, 12(9), 2510. doi:10.3390/nu12092510
Dydyk, A. M., Ngnitewe Massa, R., & Mesfin, F. B. (2022). Disc Herniation. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK441822/
Foran, J. R.H. (2021, February). Hip Osteoarthritis. OrthoInfo— American Academy of Orthopaedic Surgeons. https://www.orthoinfo.org/en/diseases–conditions/osteoarthritis-of-the-hip/
Kress, H.-G., Aldington, D., Alon, E., Coaccioli, S., Collett, B., Coluzzi, F., Huygen, F., Jaksch, W., Kalso, E., Kocot-Kępska, M., Mangas, A. C., Ferri, C. M., Mavrocordatos, P., Morlion, B., Müller-Schwefe, G., Nicolaou, A., Hernández, C. P., & Sichère, P. (2015). A holistic approach to chronic pain management that involves all stakeholders: Change is needed.
 Current Medical Research and Opinion, 31(9), 1743–1754. doi:10.1185/03007995.2015.1072088
Current Medical Research and Opinion, 31(9), 1743–1754. doi:10.1185/03007995.2015.1072088Park, D. K. (2021, August). Low Back Pain. OrthoInfo— American Academy of Orthopaedic Surgeons. https://www.orthoinfo.org/en/diseases–conditions/low-back-pain/
Lucas, J. W., connor, E. M., & Bose, J. (2021, July). Products—Data Briefs—Number 415—July 2021. doi:10.15620/cdc:107894
Mostofi, K., & Karimi Khouzani, R. (2015). Reliability of the Path of the Sciatic Nerve, Congruence between Patients’ History and Medical Imaging Evidence of Disc Herniation and Its Role in Surgical Decision Making. Asian Spine Journal, 9(2), 200–204. doi:10.4184/asj.2015.9.2.200
Pinched Nerves: Causes, Symptoms & Treatment. (2021, April 7). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/6481-pinched-nerves
Abbasi, D. (2021, June 1). Piriformis Muscles Syndrome. Orthobullets.
 https://www.orthobullets.com/knee-and-sports/3095/piriformis-muscles-syndrome
https://www.orthobullets.com/knee-and-sports/3095/piriformis-muscles-syndromePArk, D. K. (2022, April). Preventing Back Pain at Work and at Home. OrthoInfo— American Academy of Orthopaedic Surgeons. https://www.orthoinfo.org/en/staying-healthy/preventing-back-pain-at-work-and-at-home/
Park, D. K. (2021, August). Sciatica. OrthoInfo— American Academy of Orthopaedic Surgeons. https://www.orthoinfo.org/en/diseases–conditions/sciatica/
Ashar, Y. K., Gordon, A., Schubiner, H., Uipi, C., Knight, K., Anderson, Z., Carlisle, J., Polisky, L., Geuter, S., Flood, T. F., Kragel, P. A., Dimidjian, S., Lumley, M. A., & Wager, T. D. (2021). Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain. JAMA Psychiatry, 79(1),13-23. doi:10.1001/jamapsychiatry.2021.2669
Why does my lower back and hip hurt?
Sometimes lower back occurs alongside hip pain. This may happen on one side or both. Certain health conditions or injuries can affect the nerves in both the hips and the lower back.
Certain health conditions or injuries can affect the nerves in both the hips and the lower back.
These pains usually occur as a result of overuse or injury, but they can also be a symptom of an underlying medical condition. People may notice the pain on the left or right side of the body or both.
In this article, we look at possible causes of lower back and hip pain. We also discuss the various treatment options and how to relieve pain.
Share on PinterestPossible causes of lower back and hip pain include sprains, strains, and a herniated disk.
It is easy to overwork the lower back and hips because they are responsible for lifting, twisting, and moving the legs and trunk. Pains due to overuse and minor injury are common in these areas of the body.
Although these pains are common, people should not ignore them. Rest and early treatment can significantly improve a person’s outlook.
The causes are similar in males and females. The following are some of the most common causes of lower back and hip pain.
Sprains and strains are a common cause of pain around the back and hips. A sprain is a torn or overstretched ligament, while a strain is a torn or overstretched tendon or muscle.
People with sprains and strains are likely to experience discomfort that worsens with activity and gets better with rest.
Common causes of sprains and strains in this area include:
- sports injuries
- a fall or trauma
- twisting the body in an awkward way
- lifting something heavy
Playing a sport or engaging in other physical activity without warming up properly can contribute to muscle strain.
Damage to the ligaments, tendons, or muscles in the hip or lower back can cause:
- muscle pain
- muscle weakness
- tenderness
- swelling
- reduced range of motion
Treatment
People will usually find that their symptoms improve with a few days of rest.
Gentle stretching can speed up recovery. Applying a cloth-covered ice pack to the affected area for 10 to 15 minutes at a time can also help.
Applying a cloth-covered ice pack to the affected area for 10 to 15 minutes at a time can also help.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can reduce the pain and swelling that these muscle injuries cause.
If these treatments do not reduce symptoms, the injury may be more serious, for example, a muscle tear. In this case, a person should see their doctor.
The hip flexors are muscles that extend from the hips to the knees. They are responsible for the range of motion in the legs and hips. If these muscles are stiff and tight, often due to remaining in a seated position for too long, a person may experience back and hip pain.
Hip flexor strains, which are strains in the hip flexor muscles, can also cause sharp pain in the back and hips.
Symptoms of tight hip flexor muscles include:
- tenderness in the upper leg
- muscle spasms in the hips or thighs
- soreness in the hips and thighs
Some people may also experience a sense of weakness when trying to kick the leg or lift the knee toward the chest.
Read about 10 stretches for tight hips here.
Treatment
Physical therapy exercises and stretching can help relieve tight hip flexors and reduce discomfort. Examples include pulling the knee toward the chest or lunging one leg forward from a kneeling position to create a stretch in the hips.
Avoiding activities that can increase hip flexor tightness, such as sitting too long at a desk or wearing high heels for extended periods, can also help.
Share on PinterestA herniated disk may cause pain in the lower back, legs, and hips.
A herniated disk occurs when one of the cushioning disks between the vertebrae slips out of place. The disk can put pressure on a nearby nerve, which may cause tingling and burning pain in the lower back that extends to the hips and legs.
Older adults are prone to herniated disks because of the natural wear and tear of the spine that occurs over time. The disks also become less flexible with age.
Common causes of a herniated disk include:
- improper lifting or twisting while lifting
- a fall or trauma
- being overweight
- repetitive strain on the back
- driving for long periods
- smoking
Symptoms of a herniated disk include:
- sciatica, or a sharp, shooting pain from the buttocks down the back of one leg
- numbness in the leg or foot
- muscle weakness in the leg or foot
In severe cases, people may experience a loss of bowel and bladder function. If this occurs, they should go to the hospital or call 911 right away.
If this occurs, they should go to the hospital or call 911 right away.
Treatment
The treatment for a herniated disk involves relieving pain and discomfort while it heals. Bed rest will usually help relieve the pain too.
Other treatment options include:
- physical therapy exercises
- taking NSAIDs to relieve pain and inflammation
- epidural steroid injections, which involve injecting corticosteroids into the epidural space containing the inflamed nerves
In severe cases, a doctor may recommend surgery to correct a herniated disk.
The sacroiliac (SI) joints connect the lower portion of the spine to the pelvis. If these joints move too much or too little, people may feel pain in the back and hips.
The symptoms of SI joint dysfunction include an aching lower back that makes it difficult for a person to find a comfortable position. The pain will usually worsen with physical activity, such as running or climbing stairs.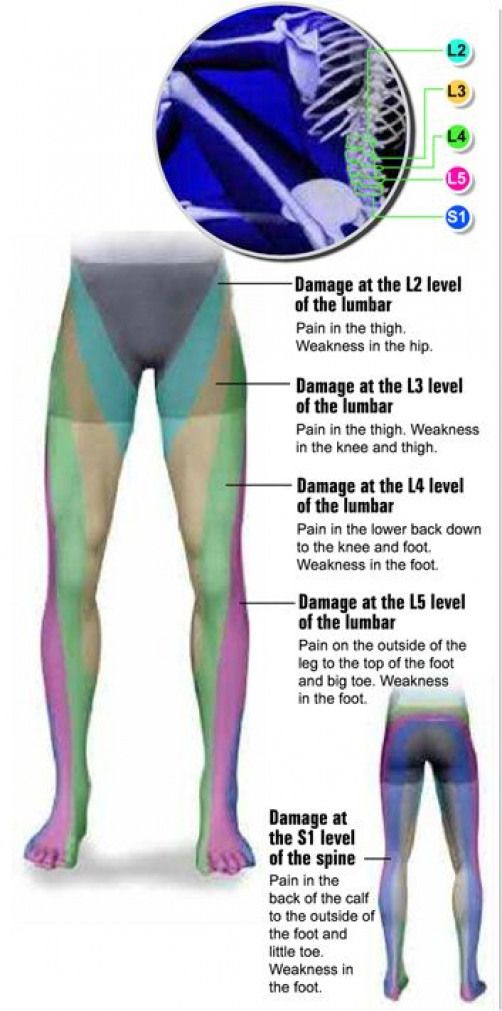
A herniated disk and arthritis can cause symptoms similar to those of SI joint dysfunction.
Treatment
Treatment options for SI joint dysfunction include:
- NSAIDs to relieve pain and inflammation
- physical therapy exercises to strengthen the core and pelvic muscles
- stretching and applying ice to the affected areas
- the injection of a steroid into the SI joint
A doctor may suggest that a person has corticosteroid injections to reduce spinal inflammation. In rare instances, they may recommend surgery to fuse the joints.
Osteoarthritis of the back can result in the breakdown of the protective and cushioning cartilage of the spine. This loss of cushioning can cause the spinal bones to rub together and place greater pressure on the nerves, including the nerves that go to the lower back and hips.
Arthritis in the back and hips causes joint stiffness and pain. A person may also experience weakness in the legs and hips, which can interfere with their everyday activities.
Treatment
Doctors do not have a cure for arthritis, but people can manage their symptoms using medication and lifestyle methods. These include:
- exercises that strengthen the back and hips muscles to improve flexibility and range of motion
- trying home remedies for arthritis
- alternative therapies, such as massage, acupuncture, and nutritional supplementation
- surgery, if arthritis causes significant spinal canal narrowing
- NSAIDs
Ankylosing spondylitis is a form of arthritis that primarily affects the spine, causing chronic inflammation in the spinal joints. Lower back and hip pain are often some of the first symptoms that a person with ankylosing spondylitis experiences.
Symptoms include muscle pain and stiffness that is usually worse in the morning. Other symptoms may include:
- low-grade fever
- appetite loss
- malaise, which is a general feeling of discomfort
Treatment
Doctors do not have a cure for ankylosing spondylitis, but, as with other forms of arthritis, people can manage the condition with a range of medical and at-home treatments.
Prescription medications, such as tumor necrosis factor (TNF) blockers and NSAIDs, can help. Certain lifestyle measures, including doing regular physical activity, icing affected areas, and not smoking, can also be beneficial.
Share on PinterestHeadaches may be a symptom of Paget’s disease.
Paget’s disease of bone is a rare disorder that affects an estimated 1% of people in the United States, according to the American College of Rheumatology.
This condition causes a person’s bones to remodel abnormally, leading to bone softening, which can affect the pelvis, lower back, hips, and arms. A person with Paget’s disease has a higher risk of bone pain and fractures.
The symptoms of Paget’s disease include:
- hip pain
- hearing loss
- bowed legs, where the knees are wider apart than usual
- headaches
- tingling and numbness down the legs
Treatment
The treatment for Paget’s disease involves medications to reduce the likelihood of the bones breaking. Doctors usually prescribe these medicines to treat osteoporosis. In rare cases, a doctor may recommend surgery to repair bones and restore alignment.
Doctors usually prescribe these medicines to treat osteoporosis. In rare cases, a doctor may recommend surgery to repair bones and restore alignment.
People should seek emergency attention if they experience any of the following symptoms alongside lower back and hip pain:
- loss of bowel and bladder function
- inability to move one or both legs
- loss of sensation in one or both legs
- visible deformity in the legs or back, such as the inability to stand up straight
If a person experiences less severe symptoms that do not improve with rest and over-the-counter treatments, they should make an appointment with their doctor. A doctor can evaluate their symptoms, make a diagnosis, and recommend the most effective treatments.
When a person experiences lower back and hip pain simultaneously, there may be an underlying injury or medical condition causing both of these symptoms. In other cases, the causes may be distinct.
Lower back and hip pain can make performing daily activities difficult. If these symptoms do not resolve or suddenly get worse, a person should seek medical attention.
If these symptoms do not resolve or suddenly get worse, a person should seek medical attention.
Regardless of the cause, early treatment helps improve the outlook of a person with back and hip pain. Without treatment, some causes of the pain can get worse and may ultimately affect a person’s mobility and quality of life.
Acute pain in the sacrum, buttocks and thigh: causes and effective treatment
Contents
- 1 Why does acute pain occur in the sacrum, buttocks and thigh? Symptoms, causes and treatments
- 1.1 Acute pain in the sacrum, buttocks and thigh: what is it?
- 1.1.1 Sacrum:
- 1.1.2 Buttocks:
- 1.1.3 Thigh:
- 1.2 Causes of acute pain in the sacrum, buttocks and thigh
- 1.3 How to diagnose acute pain in the sacrum, buttocks and thigh?
- 1.4 Effective treatment of acute pain in the sacrum, buttocks and thigh
- 1.5 Radical pharmacological therapy for acute pain in the sacrum, buttocks and thigh
- 1.
 5.1 Analgesics
5.1 Analgesics - 1.5.2 Muscle relaxants
- 1.5.3 Anti-inflammatory agents
- 1.
- 1.6 Treatment of acute pain in the sacrum, buttocks and thighs without medication
- 1.7 Important guidelines for the use of massage for acute pain in the sacrum, buttocks and thighs
- 1.8 Important information about the use of exercise for acute pain in the sacrum, buttocks and thighs
- 1.9 Post-injection complications in the treatment of acute pain in the sacrum, buttocks and thighs
- 1.9.1 What are post-injection complications?
- 1.9.2 What are post-injection complications?
- 1.9.3 How to avoid post-injection complications?
- 1.10 How to avoid acute pain in the sacrum, buttocks and thigh?
- 1.11 When should I see a doctor for acute pain in the sacrum, buttocks and thigh?
- 1.12 Related videos:
- 1.13 Q&A:
- 1.13.0.1 What causes acute pain in the sacrum, buttocks and thigh?
- 1.
 13.0.2 What symptoms may accompany acute pain in the sacrum, buttocks and thigh?
13.0.2 What symptoms may accompany acute pain in the sacrum, buttocks and thigh? - 1.13.0.3 What are the diagnostic methods for acute pain in the sacrum, buttocks and thigh?
- 1.13.0.4 What treatments are effective for acute pain in the sacrum, buttocks and thigh?
- 1.13.0.5 What exercises will help relieve acute pain in the sacrum, buttocks and thigh?
- 1.13.0.6 How to prevent acute pain in the sacrum, buttocks and thigh?
- 1.1 Acute pain in the sacrum, buttocks and thigh: what is it?
Acute pain in the sacrum, buttocks and thigh can be caused by various reasons. Find out what they are and how to properly treat this unpleasant condition. Expert advice only on our website!
An unpleasant symptom of pain in the lower back and buttocks can be associated with various causes. A life rhythm with increased working days, lack of physical activity, a tendency to scoliosis and an uncomfortable posture – all this can lead to a pain symptom in the sacrum.
Disorders of the nervous system, hidden diseases and infections can also be one of the main causes of acute pain in these parts of the body. It is important to understand that the disease will not disappear on its own. An immediate visit to the doctor is required to establish an accurate diagnosis and effective treatment.
It is important to understand that the disease will not disappear on its own. An immediate visit to the doctor is required to establish an accurate diagnosis and effective treatment.
In this article, we will look at the most common causes of acute pain in the sacrum, buttocks and thighs, as well as effective treatments.
In urgent cases, it is recommended to consult a specialist and start treatment with conservative methods. Surgical intervention is used only in extreme situations and when diagnosing serious pathologies. Do not put off going to the doctor if you experience pain symptoms in the sacrum, buttocks and thighs. An individual approach to treatment will be determined only on the basis of the results of the examination and consultation of doctors.
Acute pain in the sacrum, buttocks and thigh: what is it?
Sacrum:
The sacrum is the lower part of the spine that connects to the pelvic bones. Acute pain in the sacrum can occur due to damage to the bones, intervertebral discs or ligaments. Muscle tension is also a common cause of pain. This often occurs in the context of a sedentary lifestyle, low physical activity, and poor posture.
Muscle tension is also a common cause of pain. This often occurs in the context of a sedentary lifestyle, low physical activity, and poor posture.
Buttocks:
Pain in the buttocks can be caused by various causes, such as stretching of the muscles present in this area, damage to the joints, bones or nerves. However, the most common cause is osteochondrosis, a disease that is associated with pathological changes in the intervertebral discs.
Hip:
Hip pain can be caused by a variety of causes, including trauma, joint inflammation, nerve damage, and bone deformities. However, the most common cause is spinal disease such as osteochondrosis or herniated discs.
It is important to understand that acute pain in the sacrum, buttocks, and thigh can be a symptom of a serious illness, such as cancer or an infection. If the pain does not disappear within a few days or is accompanied by other symptoms, be sure to consult a specialist.
- Consider lifestyle changes to prevent pain, such as physical activity and improved posture.

- Stretching and massage can help relieve muscle tension that can lead to pain in the sacrum and buttocks.
- Anti-inflammatory drugs, physical therapy, and massage may be used to treat hip pain.
- Some cases require more serious treatment, such as surgery.
Causes of acute pain in the sacrum, buttocks and thigh
Acute pain in the sacrum, buttocks and thigh can be caused by various causes, ranging from injuries to diseases of the internal organs. One of the most common causes is a strain on the muscles or ligaments that run through that area of the body.
Also, acute pain in this area can occur with a kick in the nerve that runs along the thigh and passes through the sacrum. This can happen, for example, when sitting in the wrong position for a long time or when lifting weights.
Finally, acute pain in the sacrum, buttocks and thigh can be associated with diseases of the internal organs, for example, pathologies of the kidneys, bladder, gallbladder, etc. In this case, the pain can be reflex in nature and radiate to one or both legs.
In this case, the pain can be reflex in nature and radiate to one or both legs.
How to diagnose acute pain in the sacrum, buttocks and thigh?
Acute pain in the sacrum, buttocks, and hips can be caused by a variety of factors, including trauma, inflammation, problems with the structures of the spine, and other conditions. Diagnosis of such pain may require a series of studies.
The physician may begin the diagnosis by reviewing the patient’s medical history and performing a physical examination. This may be followed by x-rays, magnetic resonance imaging (MRI), computed tomography (CT), electromyography (EMG), and other tests to determine the exact cause of the pain.
It is important to remember that the diagnosis of acute pain in the sacrum, buttocks and hips requires a comprehensive approach and can take time. Patients should communicate with doctors and follow all appointments in order to determine the cause of the pain and find an effective treatment.
Effective treatment of acute pain in the sacrum, buttocks and thigh
Acute pain in the sacrum, buttocks and thigh can be stopped by applying complex treatment. Specialists are advised to use a combination of treatments to quickly eliminate pain.
It is also important to carry out physical exercises that contribute to the expansion of movement in the sacro-lumbar region. Stretching, massage and therapeutic exercises can improve the general condition and increase the mobility of the body. This helps reduce stress on muscles and ligaments, which helps reduce pain.
Alternative therapies such as swimming, acupuncture, yoga and meditation can also be used to relieve pain in the sacrum, buttocks and thigh. However, the use of any methods should be agreed with a specialist.
It is important to remember that pain in the sacrum, buttocks and hips can be a sign of a serious illness, so you need to see a specialist and start treatment immediately. Do not put off a visit to the doctor and take care of your health!
Radical pharmacological therapy for acute pain in the sacrum, buttocks and thigh
Acute pain in the sacrum, buttocks and thigh is a characteristic symptom of many diseases of the spine and joints.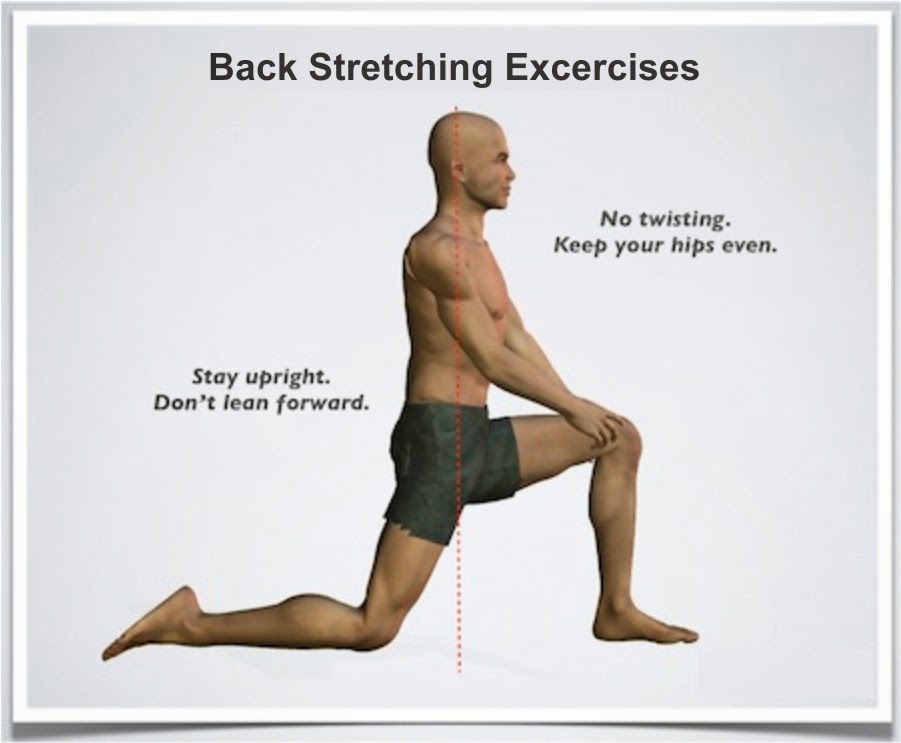 To effectively and quickly eliminate this unpleasant sensation, various methods of treatment are used. One of the most effective and reliable methods is the use of pharmacological drugs that help to quickly eliminate acute pain and reduce inflammation.
To effectively and quickly eliminate this unpleasant sensation, various methods of treatment are used. One of the most effective and reliable methods is the use of pharmacological drugs that help to quickly eliminate acute pain and reduce inflammation.
Analgesics
Analgesics are one of the most common groups of medicines used to treat acute pain in the sacrum, buttocks and thighs. Such drugs block pain impulses and reduce the sensitivity of nerve endings. This group of drugs includes drugs such as Diclofenac, Ibuprofen, Ketorolac, Nimesulide and others.
Muscle relaxants
Muscle relaxants are a group of drugs that can relax tense muscles, improve circulation and relieve pain. These drugs are prescribed for muscle spasms and other pathological conditions of the muscles and the musculoskeletal system. The most popular drugs in this group: Tizanidin, Baclofen, Mydocalm.
Anti-inflammatory drugs
Anti-inflammatory drugs are a group of drugs that can reduce inflammation and pain. These medicines are used for diseases of the joints and spine, as well as for other diseases that have caused pain. This group of drugs includes Nimesil, Meloxicam, Ketoprofen, etc.
These medicines are used for diseases of the joints and spine, as well as for other diseases that have caused pain. This group of drugs includes Nimesil, Meloxicam, Ketoprofen, etc.
All selection and use of pharmacological preparations should be made only after prescription by a doctor, since drugs cannot solve the cause, but only eliminate the symptoms.
Acute pain in the sacrum, buttocks and thighs without medication
Acute pain in the sacrum, buttocks and thighs can be caused by various causes, including sprains of muscles and ligaments, diseases of the spine, joint and nerve problems. Medications can help relieve pain, but there are other treatments.
Sit on a comfortable surface, such as the floor, with a rolled towel or pillow under your head. Then bend your knees and place a hot water bottle or heating pad on them. Alternatively, you can take a hot bath or apply a heating pad to the affected area for a while.
Another way to deal with pain is massage. No need to subject the muscles to intense pressure, gentle circular movements on the affected area are enough to help relax and relieve muscle tension.
No need to subject the muscles to intense pressure, gentle circular movements on the affected area are enough to help relax and relieve muscle tension.
- Essential oils with healing properties such as lavender, lemon balm or rosemary can be used for massage.
- Oils from cedar, juniper or aromatic mixtures can also be used to knead the muscles.
Stretching is another way to deal with pain. When performing these exercises, the muscles are stretched, blood flow improves and pain is reduced. Some stretching exercises can be done while lying on the floor, while others can be done while sitting or standing. The main thing is that the exercises lead to relaxation and reduce pain.
Exercise Name Description
| Cat and Cow | Sit on your knees and elbows. Inhale the air, bending your back up, lower your head. Exhale as you bend your back down and lower your head. |
| Glute Stretch | Lying on your back, bend your knees. Place your right foot on your left knee and pull your left knee outward towards your chest. Feel the stretch in your right buttock. Repeat on the other side. Place your right foot on your left knee and pull your left knee outward towards your chest. Feel the stretch in your right buttock. Repeat on the other side. |
| Birch | Lie on your back and lift your legs up 90 degrees. Help yourself with your arms and support your back. Hold this position for a few seconds and lower your legs to the floor. |
Another effective way to improve your well-being is to get good sleep. It is necessary for this to allocate enough time for a night’s rest, bedding should be comfortable and suitable in size. You should also avoid a sedentary lifestyle and try to relieve stress, such as meditation or yoga.
Important instructions for using massage for acute pain in the sacrum, buttocks and thighs
Massage is one of the effective methods of treating acute pain in the sacrum, buttocks and thighs. However, before using it, you need to make sure that there are no contraindications for this type of procedure.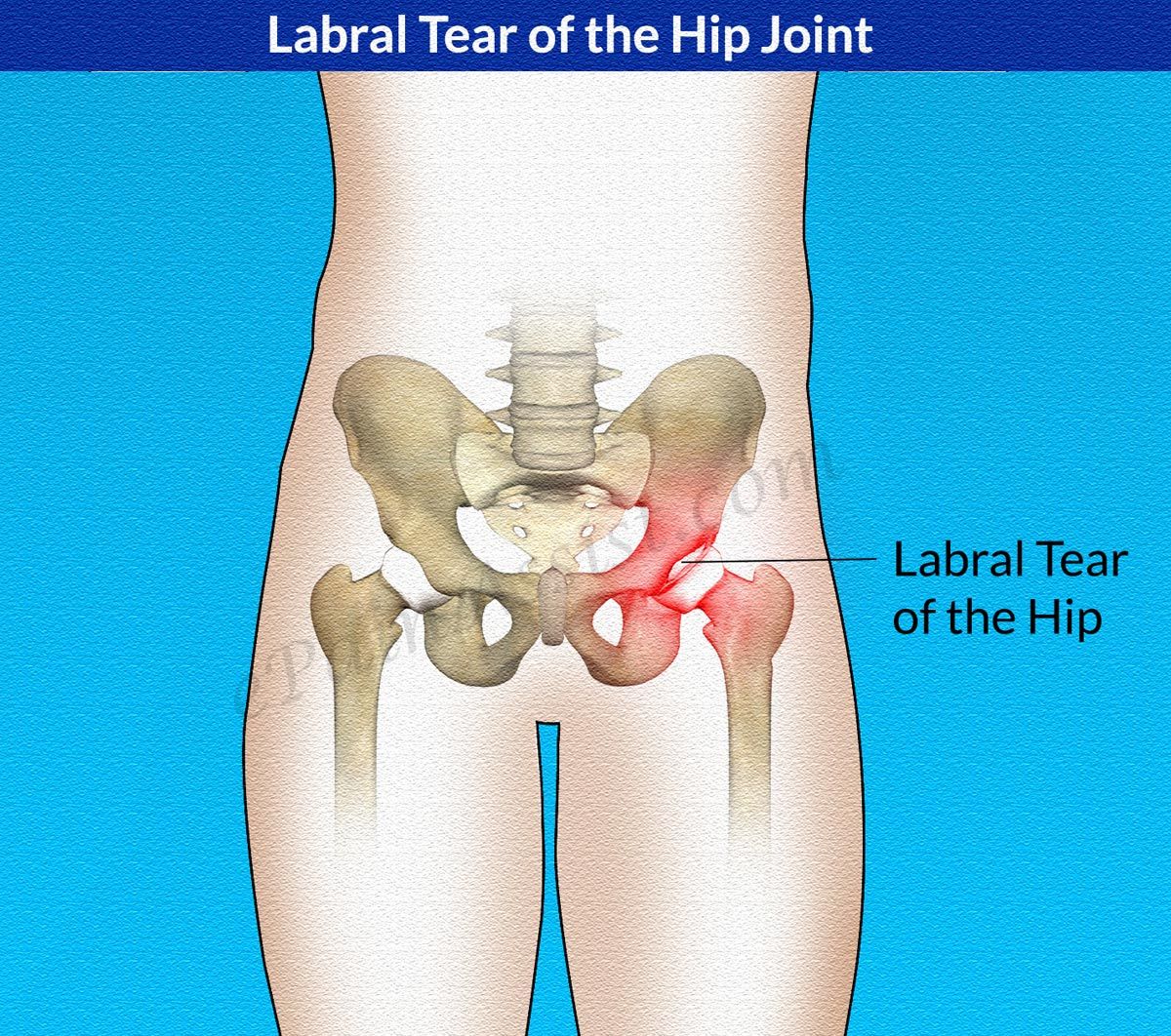
For pain in the sacrum, massage should be carried out gently and gently enough so as not to aggravate the situation. It is recommended to start the massage with gentle kneading of the muscles and gradually increase the pressure on problem areas.
In case of acute pain in the buttocks and thighs, massage should only be used after consulting a doctor. Some conditions may be due to the presence of hernias in the lumbar region, the presence of tumors or dislocations. In such cases, improper massage can lead to poor health.
- To get the most out of your massage, it is recommended that you consult an experienced massage therapist;
- Increased pressure on soft tissues can lead to increased pain, so it is recommended to massage with reasonable pressure on problem areas;
- During the massage it is necessary to take care of hand hygiene and use oils or creams so as not to injure the skin;
- After the massage, it is recommended to carry out a light physical load on the body in order to eliminate possible weakness and pain.

Important information about exercise for acute pain in the sacrum, buttocks and hips
Exercise is one of the most effective treatments for pain in the sacrum, buttocks and hips. However, not all exercises are suitable for every person, so it is recommended to consult a doctor before starting classes.
The main goals of exercise for acute pain in the sacrum, buttocks and thighs:
- Strengthening the muscles of the lower body, which reduces the load on the spine and reduces the likelihood of recurrence of pain.
- Improved flexibility and mobility of the hip joints and spine.
- Relieve muscle tension and reduce inflammation.
Recommended exercises for acute pain in the sacrum, buttocks and thigh:
- Glute stretch: Lie on your back, bend your knees and lift them up to your chest. Fasten your hands behind your shins and press your legs tightly to your chest.
 Gently stretch the muscles of the buttocks and linger in this position for 20-30 seconds.
Gently stretch the muscles of the buttocks and linger in this position for 20-30 seconds. - Static plank exercise: Get into a push-up position, but don’t lower yourself to the floor. Hold the body in this position for 20-30 seconds. This exercise strengthens your core and back muscles.
- Hip Stretch: Stand facing a wall and place your feet on the wall with your knees bent at a right angle. Grasp the wall with your hands and gradually move away from it, gently stretching your hips.
Sequence of classes: it is recommended to start with light exercises, gradually increasing the load and difficulty. Be sure to warm up before you start exercising to avoid even more muscle tension.
Exercises not to do for acute pain in the sacrum, buttocks and thigh:
| Exercise | Reason not to do |
| Body bend forward | Increase the load on the spine and may worsen pain. |
| Jumping and running | Puts a lot of stress on the sacrum and can make pain worse. |
| Violent body movements | May increase muscle tension and worsen soreness. |
Post-injection complications in the treatment of acute pain in the sacrum, buttocks and hips
What are post-injection complications?
Post-injection complications are unwanted effects that can occur after the introduction of any drug into the body. These complications may be related to the drug itself or the injection process. In the treatment of acute pain in the sacrum, buttocks and thigh, post-injection complications are often associated with the use of injections directly into the back.
What are the post-injection complications?
The most common post-injection complications in the treatment of acute pain in the sacrum, buttocks and thighs include the following:
- Bleeding in the tissue where the injection was given;
- Infections associated with the introduction of microbes;
- Symptoms associated with nerve roots, eg aching, numbness, decreased sensation.

How to avoid post-injection complications?
Factors that may increase the likelihood of post-injection complications in the treatment of acute pain in the sacrum, buttocks and thighs include improper dilution of the drug, use of coarse needles, infection at the injection site, and increased vascular permeability. In order to avoid these complications, it is important to choose a qualified specialist to perform the injection, to maintain the sterility of the instruments and the injection site, as well as to observe the correct dosage and dilution of the drug.
How to avoid acute pain in the sacrum, buttocks and thigh?
To prevent acute pain in the sacrum, buttocks and thighs, it is recommended to monitor your posture. Correct back position and even distribution of weight will help to avoid unnecessary tension in the muscles and joints.
It is also worth avoiding a long stay in one posture, especially if it is a sitting posture. If you need to sit for a long time, it is recommended to use chairs with a comfortable back or inserts to support the lower back.
It is equally important to monitor the level of physical activity. If you play sports, remember to warm up before your workout and stretch after. At the same time, you should not put too much stress on the muscles and joints, especially if you are just starting to play sports.
Do not forget about normal nutrition. Well-strengthened muscles and bones can only be obtained with proper nutrition and a sufficient dose of vitamins and minerals.
Also, pay attention to the items you use. For example, some mattresses and pillows can put extra pressure on muscles and joints, which can lead to pain in the sacrum, buttocks, and hips. This is especially true for those who suffer from osteochondrosis.
As you can see, the modern lifestyle often puts us at an unfavorable condition for back health, but with a few simple rules, discomfort and long-term problems with the spine, sacrum, buttocks and hips can be avoided.
When should I see a doctor for acute pain in the sacrum, buttocks and thigh?
Acute pain in the sacrum, buttocks and thigh can have many causes, and in most cases the cause can only be determined after examination by a doctor. However, there are cases when you need to see a doctor immediately.
However, there are cases when you need to see a doctor immediately.
- If the pain in the sacrum, buttocks and thigh is caused by an injury, blow or fall
- If the pain is accompanied by numbness, weakness or loss of sensation in the limbs
- If the pain does not stop after several days of treatment with analgesics
- If the pain occurs in an elderly person or an immunocompromised person
Other symptoms that may accompany acute pain in the sacrum, buttocks, and hips, such as fever, nausea, vomiting, or discoloration of the skin in the area of pain, should also be observed. If you notice these symptoms, see your doctor as soon as possible.
Related videos:
Q&A:
What causes acute pain in the sacrum, buttocks and thigh?
Acute pain in the sacrum, buttocks and thigh can be caused by many factors: scoliosis, herniated disc, spondylolisthesis, trauma, inflammation of the sciatic nerve, hypothermia, etc.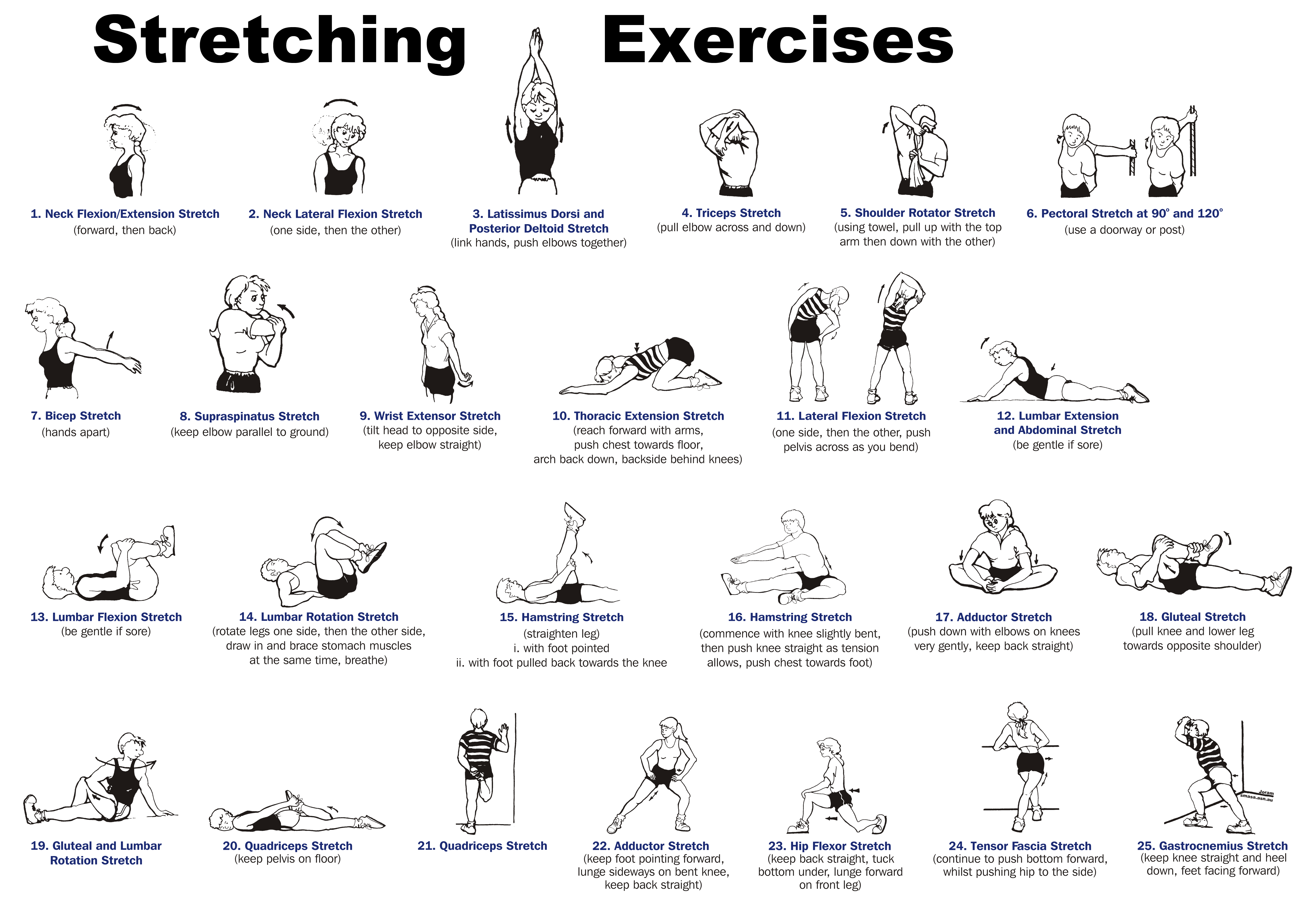
What symptoms can accompany acute pain in the sacrum, buttocks and thigh?
Acute pain may be accompanied by numbness, tingling, sticky skin, sensory disturbances, muscle weakness, decreased mobility.
What are the methods of diagnosing acute pain in the sacrum, buttocks and thigh?
Diagnosis may include a general physical examination, x-ray, MRI, CT, puncture of the intervertebral disc and other methods necessary in each case.
What treatments are effective for acute pain in the sacrum, buttocks and thigh?
Therapy can be varied: pain and inflammation medications, physiotherapy, manual therapy, surgery, therapeutic exercises, massage, yoga, Pilates, etc.
What exercises can help reduce acute pain in the sacrum, buttocks and thigh?
Some exercises that can help reduce pain: plank, bridge, buttock stretching exercises, posture correction exercises, abdominal strengthening exercises, etc. But before starting any exercise, you should definitely consult your doctor.
How to prevent acute pain in the sacrum, buttocks and thigh?
To prevent acute pain in the sacrum, buttocks and thighs, it is necessary to monitor your posture, avoid hypothermia, observe the correct mode of work and rest, allocate time for physical exercises, monitor nutrition, etc.
Pain in the lumbosacral spine
Pain in the sacrum, in one of the areas of the back – most often a symptom of acute or chronic sciatica. And here the diagnosis and treatment should be taken seriously. After all, the spine is the physical basis of a “upright” human. The anatomical structure of our body suggests a natural locomotion for the representatives of the human race – walking on the lower limbs. During walking, various groups of skeletal muscles of the trunk and limbs are involved in the body, but the main load falls on the spine, especially its lower part.
Biologists ironically call the pain in the lumbosacral spine the price for freed hands and upright posture. Indeed, according to the statistics of complaints of stiffness, burning in the back is one of the most common reasons for contacting specialized specialists.
Indeed, according to the statistics of complaints of stiffness, burning in the back is one of the most common reasons for contacting specialized specialists.
As a rule, regardless of age and gender, localization of discomfort occurs in the sacral region. A wedge-shaped, fairly large bone located at the base of the spine in the lower back is the sacrum. Below it is articulated with the coccyx, above – with the last lumbar vertebra.
The sacrum, with openings through which the branches of the sacral nerves pass, as well as the lateral arteries, is located in the center between the two pelvic bones. That is why painful sensations in the sacral region are especially dangerous. Periodic or regular, sluggish or acute pain in the back or sacrum is an alarming sign and a reason to start treatment. If the sacrum hurts when sitting, the reason may be that the disease has already gone quite far, and you should hurry with a visit to a specialist.
In most cases, more or less severe pain in this area is directly caused by non-specific structural disorders in the sacrum, such as a displaced disc or malignancy. Discomfort in the lumbosacral spine is symptomatic and requires careful diagnostic measures to help determine the true causes of its occurrence.
Discomfort in the lumbosacral spine is symptomatic and requires careful diagnostic measures to help determine the true causes of its occurrence.
Pain in the lumbosacral spine may be a signal of developing sciatica. One of the obvious causes of painful sensations is physical damage to the sacrum (blow, bruise).
Injured sacro-vertebral muscles react with spasm when exerting or performing sudden movements. There are also anomalies – congenital or developmental, which remind of themselves with sharp pain in an uncomfortable position of the body or loads.
Displacement of the lumbar vertebra (spondylolisthesis), damage to the sacroiliac ligaments, pathological processes in the area of the gluteal muscles are accompanied by pulling aching pain. Osteoporosis is characterized by prolonged dull pain.
Severe aching pains in sacrum and small of back.
Lower back pain radiating to the knee or back of the thigh (along the inflamed roots emerging from the spinal cord) is characteristic of sciatica. As a rule, such pain strongly radiates to the sacrum. Soreness and functional impairment may be due to displacement of the sacroiliac joint. Pain in the sacrum on the right or left side when sitting may be a cause for concern and a visit to a doctor.
As a rule, such pain strongly radiates to the sacrum. Soreness and functional impairment may be due to displacement of the sacroiliac joint. Pain in the sacrum on the right or left side when sitting may be a cause for concern and a visit to a doctor.
Pain in the sacrum in women.
Acute pain in the sacrum in women on the left can be both the result and the cause of gynecological diseases, which, however, is directly related to the mobility of the intervertebral discs of the sacrum. It is noteworthy that the reaction to displacement on the right or left side has cardinal differences. Left-sided displacement is accompanied by constipation, possible problems with the lungs and heart, the appearance of a tendency to be overweight. Right-sided displacement affects the circulatory system of the right leg, the patient suffers from indigestion, women are prone to inflammatory processes in the genital area.
Age-related changes, metabolic disorders, trauma, strain and sprains contribute to greater mobility of the sacroiliac joint, which in turn provokes the formation of osteophytes and inflammation (sacroiliitis). In this situation, doctors most often state the presence of symptoms of rheumatic diseases, psoriatic arthritis, ankylosing spondylitis. In any case, pain in the sacrum is a reason to contact a neurologist.
In this situation, doctors most often state the presence of symptoms of rheumatic diseases, psoriatic arthritis, ankylosing spondylitis. In any case, pain in the sacrum is a reason to contact a neurologist.
Sacrodynia
Sacrodynia – symptomatic pain in the sacral region – can be caused by any pathology in the sacrum itself, the small pelvis or organs located in adjacent areas. It is not limited solely to diseases of the bones, displacement of the vertebrae, inflammation (sciatica, neuromyalgia) or pinching of the roots of the spinal cord. Very often, acute or aching pain in the sacrum occurs due to diseases of the internal organs: prostate, appendages, uterus, intestines, kidneys.
Endometriosis, abnormal position of the fetus in the womb during pregnancy, thrombophlebitis, gynecological and urological inflammations, pathologies of the prostate, rectum, tumors, metabolic diseases, infections – the causes are not only acute attacks or chronic pain of a reflex nature, but also a serious reason to see a doctor .

 01.032
01.032 doi:10.1093/pm/pnw099
doi:10.1093/pm/pnw099 Current Medical Research and Opinion, 31(9), 1743–1754. doi:10.1185/03007995.2015.1072088
Current Medical Research and Opinion, 31(9), 1743–1754. doi:10.1185/03007995.2015.1072088 https://www.orthobullets.com/knee-and-sports/3095/piriformis-muscles-syndrome
https://www.orthobullets.com/knee-and-sports/3095/piriformis-muscles-syndrome 5.1 Analgesics
5.1 Analgesics 13.0.2 What symptoms may accompany acute pain in the sacrum, buttocks and thigh?
13.0.2 What symptoms may accompany acute pain in the sacrum, buttocks and thigh?

 Gently stretch the muscles of the buttocks and linger in this position for 20-30 seconds.
Gently stretch the muscles of the buttocks and linger in this position for 20-30 seconds.