What kinds of antibiotics are there. Understanding Antibiotics and Probiotics: Types, Benefits, and Potential Risks
What are the different types of antibiotics. Should probiotics be taken with antibiotics. How do antibiotics affect the gut microbiome. What are the potential benefits and risks of combining probiotics with antibiotic treatment.
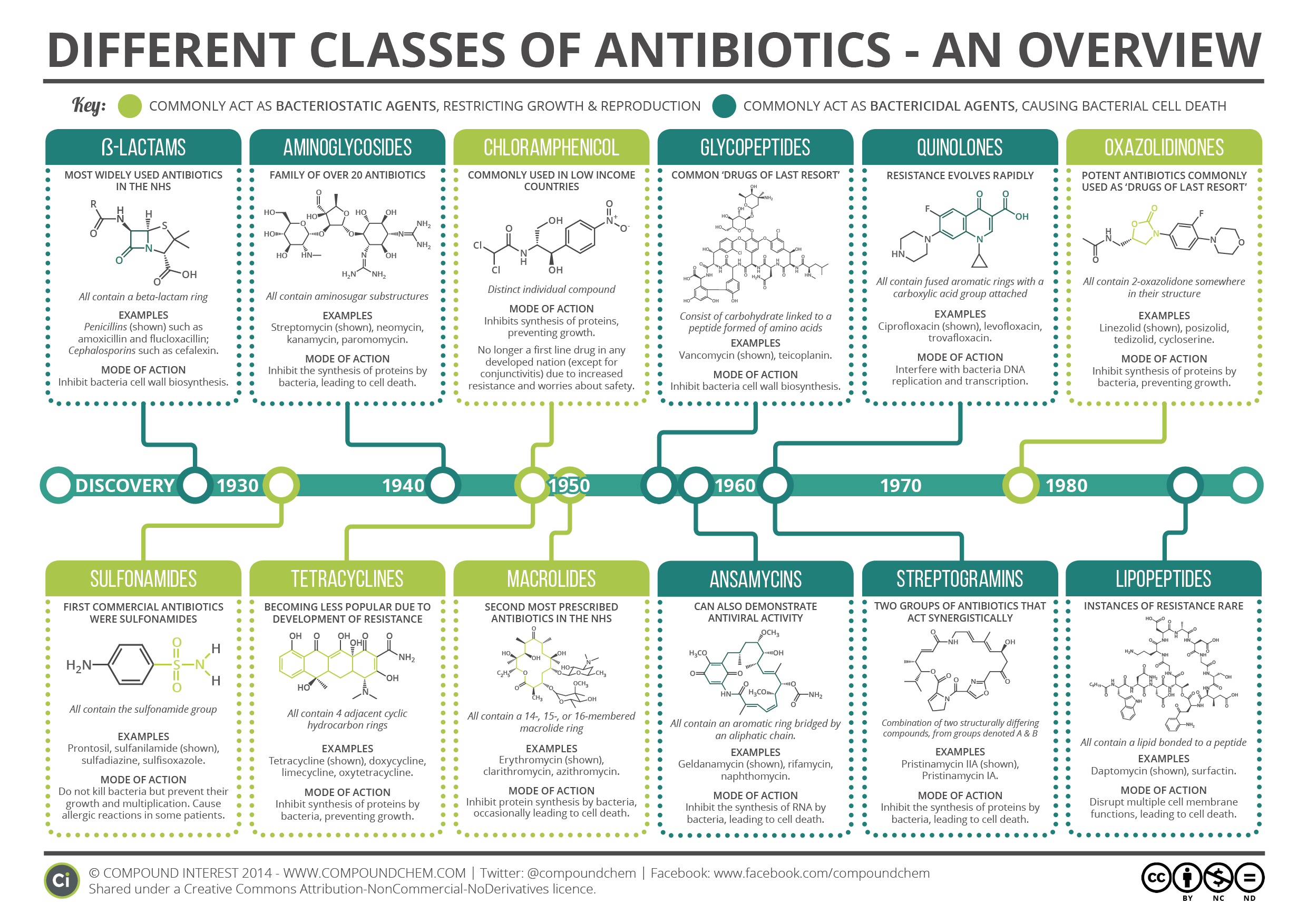
Types of Antibiotics: A Comprehensive Overview
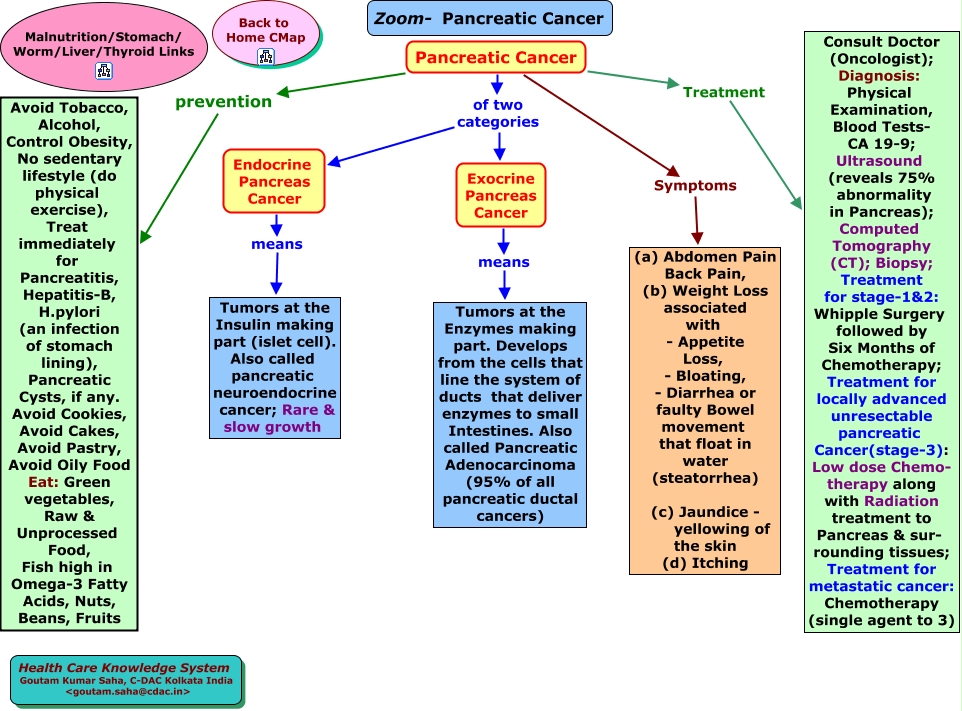
Antibiotics are powerful medications used to treat bacterial infections. They come in various types, each designed to target specific kinds of bacteria. Understanding the different classes of antibiotics can help patients and healthcare providers make informed decisions about treatment.
Major Classes of Antibiotics
- Penicillins (e.g., amoxicillin, ampicillin)
- Cephalosporins (e.g., cefaclor, cephalexin)
- Macrolides (e.g., azithromycin, erythromycin)
- Fluoroquinolones (e.g., ciprofloxacin, levofloxacin)
- Tetracyclines (e.g., doxycycline, minocycline)
- Aminoglycosides (e.g., gentamicin, tobramycin)
- Sulfonamides (e.g., sulfamethoxazole)
Each class of antibiotics works through different mechanisms to either kill bacteria or prevent their growth. The choice of antibiotic depends on factors such as the type of infection, the specific bacteria involved, and the patient’s individual health status.

The Gut Microbiome: A Delicate Ecosystem
The gut microbiome is a complex community of microorganisms residing in our digestive tract. It plays a crucial role in various aspects of our health, including digestion, immunity, and even mental well-being. The balance of this ecosystem is delicate and can be disrupted by various factors, including antibiotic use.
Key Functions of the Gut Microbiome
- Aiding in digestion and nutrient absorption
- Supporting the immune system
- Producing essential vitamins
- Protecting against harmful pathogens
- Influencing brain function and mood
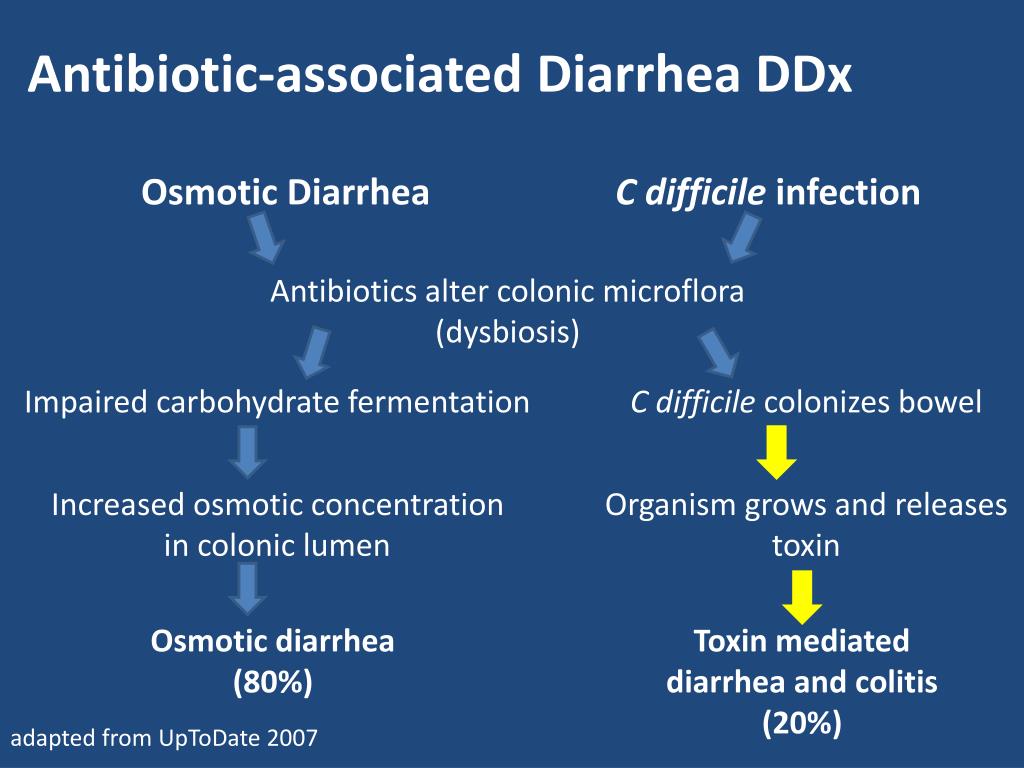
When antibiotics are introduced, they can indiscriminately kill both harmful and beneficial bacteria, potentially leading to an imbalance in the gut microbiome. This disruption can result in various side effects, including antibiotic-associated diarrhea.
Probiotics: Beneficial Bacteria for Gut Health
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. They are often suggested as a way to support gut health, particularly during and after antibiotic treatment.
Common Probiotic Strains
- Lactobacillus species
- Bifidobacterium species
- Saccharomyces boulardii
- Streptococcus thermophilus
These beneficial bacteria can help maintain a healthy balance in the gut microbiome and may alleviate some of the side effects associated with antibiotic use.
The Controversy: Probiotics with Antibiotics
The question of whether to take probiotics alongside antibiotics is a topic of ongoing debate in the medical community. While some studies suggest potential benefits, others raise concerns about long-term effects on the gut microbiome.
Evidence Supporting Probiotic Use
A Cochrane review examining 23 studies with 3,938 participants found that children given probiotics after antibiotic treatment experienced less diarrhea compared to those who didn’t receive probiotics. The review suggested that Lactobacillus rhamnosus or Saccharomyces boulardii at doses of 5 to 40 billion colony-forming units per day might be the most appropriate choice.
Concerns About Probiotic Use
A 2019 Italian study raised concerns about the long-term effects of probiotic use after antibiotic treatment. The research found that individuals given probiotics after antibiotics took six months for their gut microbiome to return to its normal state, compared to only three weeks for those not given probiotics.

Potential Benefits of Combining Probiotics with Antibiotics
Despite the controversy, there are several potential benefits to consider when discussing the use of probiotics alongside antibiotic treatment.
Reduced Risk of Antibiotic-Associated Diarrhea
One of the primary reasons for recommending probiotics during antibiotic treatment is to reduce the risk of antibiotic-associated diarrhea. The Cochrane review mentioned earlier found a significant reduction in diarrhea incidence among those taking probiotics (8%) compared to the control group (19%).
Maintenance of Gut Microbiome Balance
Probiotics may help maintain a more balanced gut microbiome during antibiotic treatment by replenishing beneficial bacteria that are often affected by antibiotics. This could potentially reduce the risk of opportunistic infections and other complications associated with microbiome imbalance.
Support for Immune Function
A healthy gut microbiome plays a crucial role in supporting immune function. By helping to maintain microbial balance, probiotics may indirectly support the immune system during and after antibiotic treatment.

Potential Risks and Side Effects of Probiotic Use
While probiotics are generally considered safe for most people, it’s important to be aware of potential risks and side effects, especially when taken alongside antibiotics.
Common Side Effects
The most frequently reported side effects of probiotic use include:
- Abdominal bloating and discomfort
- Gas and flatulence
- Nausea
- Changes in bowel habits (constipation or diarrhea)
- Headaches
These side effects are typically mild and temporary, often resolving as the body adjusts to the probiotic supplement.
Risks for Certain Populations
While probiotics are generally safe, certain groups may be at higher risk for adverse effects:
- Individuals with compromised immune systems
- Critically ill patients
- Those with central venous catheters
- Premature infants
For these populations, the potential risks of probiotic use may outweigh the benefits, and caution is advised.
Alternative Approaches to Supporting Gut Health
Given the ongoing debate about probiotic use with antibiotics, researchers are exploring alternative methods to support gut health during and after antibiotic treatment.
Fermented Foods
Incorporating fermented foods into the diet may provide natural probiotics and support gut health. Examples include:
- Yogurt
- Kefir
- Sauerkraut
- Kimchi
- Kombucha
These foods contain live beneficial bacteria that may help maintain microbial balance in the gut.
Fecal Microbiota Transplantation
Fecal microbiota transplantation (FMT) is an emerging approach for restoring gut microbiome balance. Studies have shown promising results, particularly for treating recurrent Clostridium difficile infections.
Autologous FMT, where a person’s own stool is collected before antibiotic treatment and reintroduced afterward, has shown potential in quickly restoring the gut microbiome to its pre-antibiotic state. However, this approach is currently only approved for specific medical conditions and requires further research for broader applications.
Making Informed Decisions: Probiotics and Antibiotics
The decision to use probiotics alongside antibiotics should be made on an individual basis, considering various factors:
Factors to Consider
- The specific antibiotic being used
- The patient’s overall health status
- Any pre-existing gut health issues
- The potential risk of antibiotic-associated diarrhea
- The individual’s immune system status
It’s crucial to consult with a healthcare provider before starting any probiotic regimen, especially when taking antibiotics. They can provide personalized advice based on individual circumstances and the latest medical evidence.
Timing of Probiotic Administration
If probiotics are recommended, the timing of administration can be important. Some healthcare providers suggest taking probiotics a few hours apart from antibiotics to minimize potential interactions. This approach may help ensure that the beneficial bacteria in the probiotic supplement are not immediately destroyed by the antibiotic.
Monitoring and Adjusting
When using probiotics with antibiotics, it’s important to monitor for any adverse effects or changes in symptoms. If any concerns arise, promptly communicate with a healthcare provider. They may recommend adjusting the probiotic dosage, changing the strain, or discontinuing use if necessary.
The relationship between antibiotics, probiotics, and gut health is complex and continues to be an area of active research. While some studies suggest potential benefits of combining probiotics with antibiotic treatment, others raise concerns about long-term effects on the gut microbiome. As research progresses, our understanding of how best to support gut health during antibiotic treatment will likely evolve.
For now, the decision to use probiotics alongside antibiotics should be made on a case-by-case basis, considering individual health factors and the specific antibiotic being used. Always consult with a healthcare provider for personalized advice and stay informed about the latest research in this rapidly evolving field.
As we continue to unravel the complexities of the gut microbiome and its interactions with antibiotics and probiotics, new strategies for maintaining gut health during antibiotic treatment may emerge. These could include more targeted probiotic formulations, novel approaches to microbiome restoration, or entirely new classes of gut-supportive therapies.
In the meantime, focusing on overall gut health through a balanced diet, regular exercise, and stress management can provide a strong foundation for maintaining a healthy microbiome, with or without antibiotic treatment. By staying informed and working closely with healthcare providers, individuals can make the best decisions for their gut health and overall well-being.
Should you take probiotics with antibiotics?
Medically reviewed by Carmen Pope, BPharm. Last updated on Nov 7, 2022.
There is controversy about whether you should routinely take probiotics with antibiotics and the question cannot be answered with a straight yes or no.
Evidence for taking probiotics with antibiotics includes a Cochrane review which reported that children who were given a course of probiotics after antibiotics had less diarrhea. Evidence against taking probiotics with antibiotics includes a 2019 Italian study that reported that the gut microbiome of people given probiotics after antibiotics took six months to return to its normal state compared to only three weeks for those not given any probiotics.
More studies are needed before a definite statement can be made.
What studies support giving probiotics with antibiotics?
A Cochrane review of 23 studies (3938 participants) investigated giving probiotics containing either one or a combination of the following: Bacillus spp. , Bifidobacterium spp., Clostridium butyricum, Lactobacilli spp., Lactococcus spp., Leuconostoc cremoris, Saccharomyces spp., or Streptococcus sp.
, Bifidobacterium spp., Clostridium butyricum, Lactobacilli spp., Lactococcus spp., Leuconostoc cremoris, Saccharomyces spp., or Streptococcus sp.
Results from 22/23 trials that reported on the incidence of antibiotic-associated diarrhea show a significant benefit from probiotics compared to active, placebo, or no treatment control (8% in the probiotic group compared to 19% in the control group). None of the 16 trials (n = 2455) that reported on side events documented any serious side events attributable to probiotics with the most common ones being rash, nausea, gas, flatulence, abdominal bloating, abdominal pain, vomiting, increased phlegm, chest pain, constipation, taste disturbance, and low appetite. The author’s concluded that there was a protective effect of probiotics for preventing antibiotic-associated diarrhea. The relative risk was 0.46 (95% CI 0.35 to 0.61) and the NNT was 10.
The authors considered Lactobacillus rhamnosus or Saccharomyces boulardii at 5 to 40 billion colony forming units/day to be the most appropriate choice. They also commented that although no serious adverse events were observed among the otherwise healthy children in these trials, serious adverse events have been observed in severely debilitated or immuno-compromised children with underlying risk factors (eg, central venous catheter use), and advised that probiotics should be avoided in pediatric populations at risk for adverse events until further research has been conducted.
They also commented that although no serious adverse events were observed among the otherwise healthy children in these trials, serious adverse events have been observed in severely debilitated or immuno-compromised children with underlying risk factors (eg, central venous catheter use), and advised that probiotics should be avoided in pediatric populations at risk for adverse events until further research has been conducted.
What studies do not recommend giving probiotics with antibiotics?
Researchers from the Weizmann Institute of Science in Israel and other institutions reported that the gut microbiome took longer to return to normal in those people given an 11-strain probiotic treatment for four weeks following a course of antibiotics. This was despite the probiotics effectively colonizing the gut with healthy bacteria. The trouble was the presence of the new bacteria and yeasts strains prevented the gut microbiome from returning to normal for the full six month study period.
Conversely, the gut microbiome in those given no probiotics returned to normal within three weeks of going off the antibiotics. “ The authors did conclude that this study just examined one type of probiotic, and a different probiotic may be helpful in patients taking different antibiotics. However, they did point out the findings of the study imply that the traditional practice of taking a probiotic after antibiotic may not be beneficial.
More research is needed to determine if other options to strengthen the gut microbiome, such as fermented food products (eg, sauerkraut and kimchi) or fecal transplantation, is beneficial. Studies have shown that autologous fecal transplantation, which involves collecting stool samples before going on antibiotics and freezing them, brought the gut microbiome back to normal within eight days once the stool was returned to the gut following antibiotic treatment. It took 21 days for the gut microbiota in the group that didn’t undergo fecal transplantation to return to perfect health.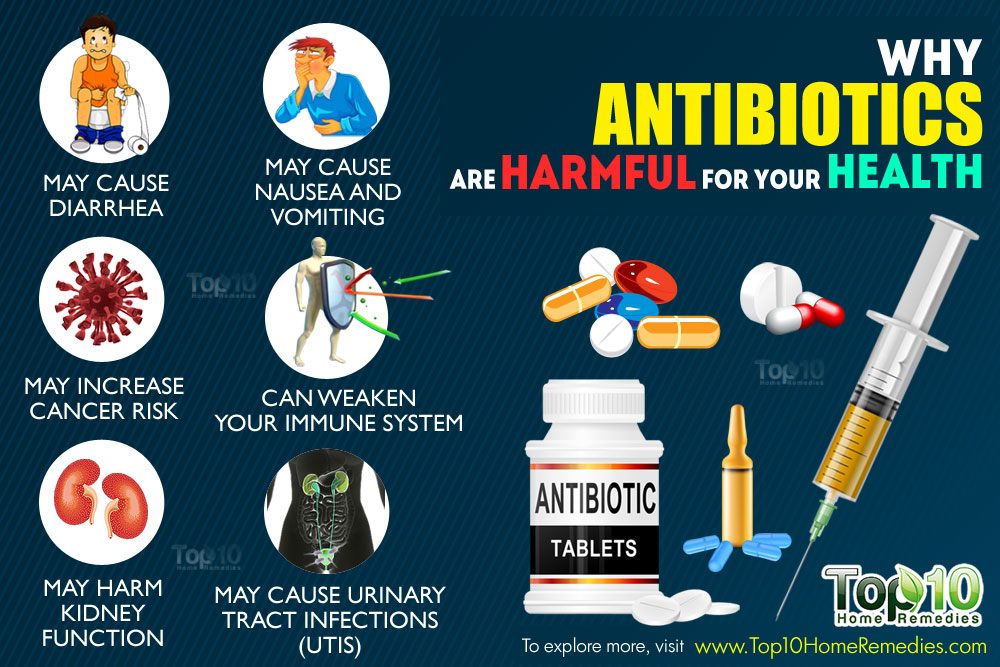 Currently, however, the only approved indication for autologous fecal transplantation is for people with C. difficile colitis, which is an inflammation of the colon caused by the bacteria Clostridium difficile.
Currently, however, the only approved indication for autologous fecal transplantation is for people with C. difficile colitis, which is an inflammation of the colon caused by the bacteria Clostridium difficile.
What are the most common side effects of probiotics?
The most common side effects reported with probiotics in clinical trials included:
- abdominal bloating
- abdominal pain
- chest pain
- constipation
- flatulence
- gas
- increased phlegm
- low appetite
- nausea
- rash
- taste disturbance
- vomiting.
What is the gut microbiome?
Our digestive tract is home to trillions of bacteria as well as fungi and viruses – these are known as the gut microbiome.
The makeup of this biome is largely genetically determined; however, it is heavily influenced by several factors such as whether we are born naturally (vaginally) or by cesarean section, if we were breastfed, our use of antibiotics, and our exposure to chemicals, pesticides, and other toxins.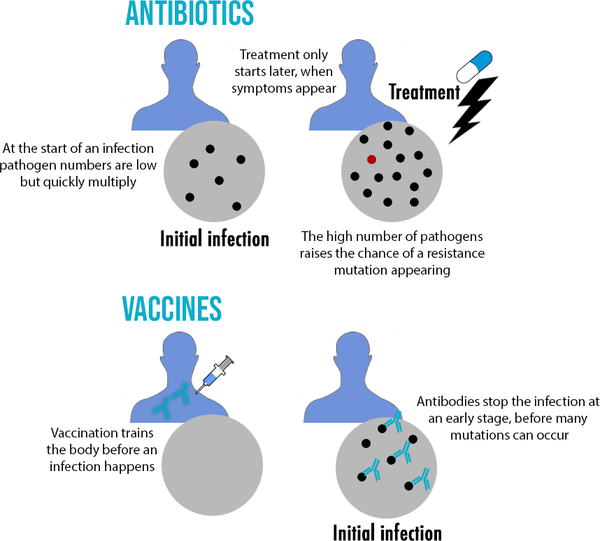
Scientists now know that this microbiome is critical to our overall well-being. Some call it our second brain. Small imbalances can cause significant changes to our mental health and in the appearance of our skin and has been linked to almost every known condition such as Alzheimer’s disease, multiple sclerosis, rheumatoid arthritis, and Type 2 diabetes.
An imbalance may also cause constipation, diarrhea, skin rashes, yeast infections, and a suppressed immune system. Your likelihood of putting on weight also comes down to your microbiome and the influence it has on your response to insulin and thyroid gland function.
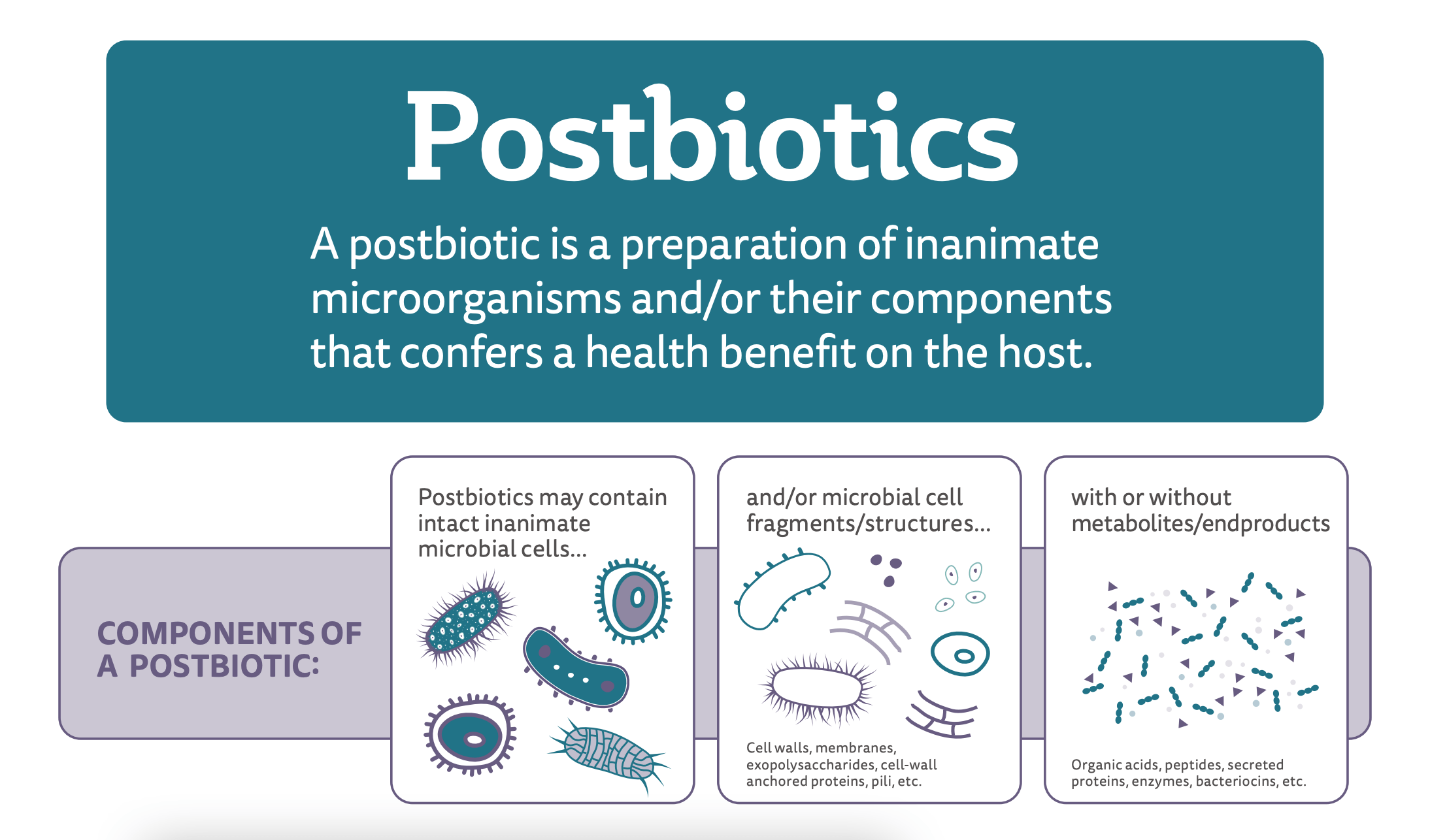
What are probiotics?
Probiotics are live bacteria and yeasts that are beneficial for health. They are often referred to as ‘good’, ‘helpful’, or ‘healthy’ bacteria.
Probiotics are available as dietary supplements and can be brought over the counter from a drug store, pharmacy, or health store. Probiotics are also found naturally or added to foods such as dark chocolate, yogurt, miso soup, pickles, sauerkraut, tempeh, or kefir.
What is the rationale behind taking probiotics with antibiotics?
Taking an antibiotic for an infection can kill beneficial bacteria that live in your gut.
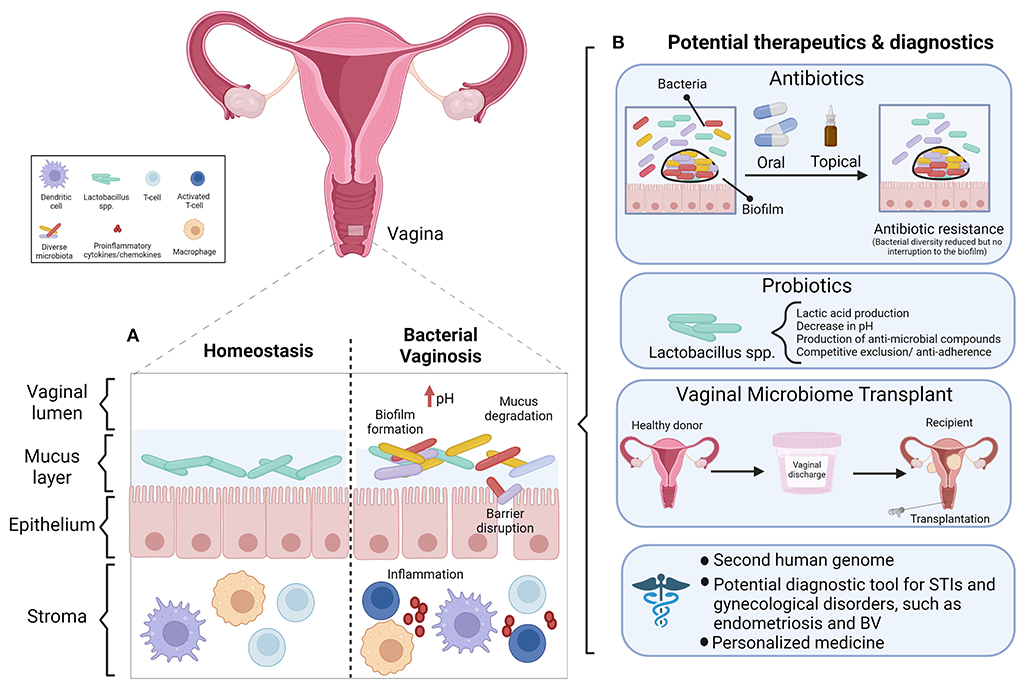
Probiotics may be taken orally to restore any imbalance in the normal intestinal or urogenital flora. This is the rationale behind taking probiotics with antibiotics. Severe antibiotic-induced diarrhea can also lead to an infection with Clostridium difficile, also known as C. difficile, a bacteria which can cause dangerous inflammation in your colon (colitis).
Experts have hypothesized that If you suffer from stomach cramping, gas or diarrhea when you take antibiotics, adding a probiotic may help to lessen, or even prevent, these symptoms. The addition of a probiotic will also reintroduce helpful bacteria into your digestive tract that have been killed or had their numbers reduced by the antibiotic.
How should I take probiotics with antibiotics?
If you do decide to take a probiotic with an antibiotic, start it the same day you start the antibiotic, but do not take it at exactly the same time as the antibiotic. Allow at least two hours to elapse after taking your antibiotic before you take your probiotic.
Allow at least two hours to elapse after taking your antibiotic before you take your probiotic.
Probiotics are usually taken twice a day on an empty stomach. They should then be continued for at least several weeks after your course of antibiotics has finished, although some people take probiotics daily to not only continue to help digestion but to boost their immune system and enhance the absorption of some nutrients.
If you wish to take probiotic supplements, choose a high-quality probiotic made by a reputable company that contains at least one of the following: Lactobacillus rhamnosus, Saccharomyces boulardii, or Bifidobacterium sp. at 5 to 40 billion colony units/day.
Do prebiotics help return the gut microbiome to normal?
Prebiotics are foods for probiotics and include fiber-rich foods such as fruits, vegetables, cereals.
Mixing prebiotics with probiotics, such as yogurt with fruit and cereal or sauerkraut with a vegetable stir fry could be helpful for your gut, although there is no scientific evidence to support this.
Good prebiotic foods include vegetables such as artichokes, asparagus, garlic, onions, and any green vegetable; fruits such as bananas, berries, and tomatoes; herbs such as chicory or garlic; grains like barley, oat, and wheat; and other fibers such as inulin that may be available on its own or added to foods such as granola bars, cereal, and yogurt.
References
- Goldenberg JZ, Lytvyn L, Steurich J, Parkin P, Mahant S, Johnston BC. Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database Syst Rev. 2015 Dec 22;(12):CD004827. doi: 10.1002/14651858.CD004827.pub4. Update in: Cochrane Database Syst Rev. 2019 Apr 30;4:CD004827. PMID: 26695080.
- Suez J, Zmora N, Zilberman-Schapira G, et al. Post-Antibiotic Gut Mucosal Microbiome Reconstitution Is Impaired by Probiotics and Improved by Autologous FMT. Cell. 2018 Sep 6;174(6):1406-1423.e16. doi: 10.1016/j.cell.2018.08.047. PMID: 30193113.
- Goderska K, Agudo Pena S, Alarcon T.
 Helicobacter pylori treatment: antibiotics or probiotics. Appl Microbiol Biotechnol. 2018 Jan;102(1):1-7. doi: 10.1007/s00253-017-8535-7. Epub 2017 Oct 26. PMID: 29075827; PMCID: PMC5748437.
Helicobacter pylori treatment: antibiotics or probiotics. Appl Microbiol Biotechnol. 2018 Jan;102(1):1-7. doi: 10.1007/s00253-017-8535-7. Epub 2017 Oct 26. PMID: 29075827; PMCID: PMC5748437. - Neut C, Mahieux S, Dubreuil LJ. Antibiotic susceptibility of probiotic strains: Is it reasonable to combine probiotics with antibiotics? Med Mal Infect. 2017 Nov;47(7):477-483. doi: 10.1016/j.medmal.2017.07.001. Epub 2017 Aug 7. PMID: 28797834.
- Guandalini S. Probiotics for prevention and treatment of diarrhea. J Clin Gastroenterol. 2011 Nov;45 Suppl:S149-53. doi: 10.1097/MCG.0b013e3182257e98. PMID: 21992955.
- Do probiotics provide effective and safe protection against antibiotic-associated adverse effects? Best Practice Journal > 2015 > BPJ: 68 > Do probiotics provide effective and safe protection against antibiotic-associated adverse effects? https://bpac.org.nz/bpj/2015/june/probiotics.aspx
Related medical questions
- What is the best antibiotic to treat a sinus infection?
- Can you have a vaginal yeast infection if you have no uterus?
- Can antibiotics cause yeast infections?
- What are the common side effects of antibiotics?
- Can you drink alcohol with amoxicillin?
- What’s the difference between Bacteria and Viruses?
- Does azithromycin cure chlamydia: How much / how long?
- Monistat-1: white discharge and burning, is this normal?
- If I am allergic to penicillin, is it safe to use amoxicillin?
- What is the best way to reduce swelling in your face?
- Amoxicillin for ear infection: Take how many times a day?
Related support groups
- Infections
(581 questions, 968 members) - Diarrhea
(195 questions, 391 members) - Pseudomembranous Colitis
(8 questions, 8 members)
Medical Disclaimer
Antibiotics – NHS
Antibiotics are used to treat or prevent some types of bacterial infection. They work by killing bacteria or preventing them from spreading. But they do not work for everything.
They work by killing bacteria or preventing them from spreading. But they do not work for everything.
Many mild bacterial infections get better on their own without using antibiotics.
Antibiotics do not work for viral infections such as colds and flu, and most coughs.
Antibiotics are no longer routinely used to treat:
- chest infections
- ear infections in children
- sore throats
When it comes to antibiotics, take your doctor’s advice on whether you need them or not. Antibiotic resistance is a big problem – taking antibiotics when you do not need them can mean they will not work for you in the future.
When antibiotics are needed
Antibiotics may be used to treat bacterial infections that:
- are unlikely to clear up without antibiotics
- could infect others
- could take too long to clear without treatment
- carry a risk of more serious complications
People at a high risk of infection may also be given antibiotics as a precaution, known as antibiotic prophylaxis.
Read more about when antibiotics are used and why antibiotics are not routinely used to treat infections.
How to take antibiotics
Take antibiotics as directed on the packet or the patient information leaflet that comes with the medicine, or as instructed by your GP or pharmacist.
Antibiotics can come as:
- tablets, capsules or a liquid that you drink – these can be used to treat most types of mild to moderate infections in the body
- creams, lotions, sprays and drops – these are often used to treat skin infections and eye or ear infections
- injections – these can be given as an injection or through a drip directly into the blood or muscle, and are used for more serious infections
Missing a dose of antibiotics
If you forget to take a dose of your antibiotics, check the patient information leaflet that came with your medicine to find out what to do. If you’re not sure, speak to a pharmacist or a GP.
If you’re not sure, speak to a pharmacist or a GP.
In most cases, you can take the dose you missed as soon as you remember and then continue to take your course of antibiotics as normal.
But if it’s almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Accidentally taking an extra dose
There’s an increased risk of side effects if you take 2 doses closer together than recommended.
Accidentally taking 1 extra dose of your antibiotic is unlikely to cause you any serious harm.
But it will increase your chances of getting side effects, such as pain in your stomach, diarrhoea, and feeling or being sick.
If you accidentally take more than 1 extra dose of your antibiotic, are worried or you get severe side effects, speak to your GP or call NHS 111 as soon as possible.
Side effects of antibiotics
As with any medicine, antibiotics can cause side effects. Most antibiotics do not cause problems if they’re used properly and serious side effects are rare.
The common side effects include:
- being sick
- feeling sick
- bloating and indigestion
- diarrhoea
Some people may have an allergic reaction to antibiotics, especially penicillin and another type of antibiotic called cephalosporins.
In very rare cases, this can lead to a serious allergic reaction (anaphylaxis), which is a medical emergency.
Call 999 or go to A&E now if:
- you get a skin rash that may include itchy, red, swollen, blistered or peeling skin
- you’re wheezing
- you get tightness in the chest or throat
- you have trouble breathing or talking
- your mouth, face, lips, tongue or throat start swelling
You could be having a serious allergic reaction and may need immediate treatment in hospital.
Read more about the side effects of antibiotics.
Considerations and interactions
Some antibiotics are not suitable for people with certain medical problems, or women who are pregnant or breastfeeding.
Tell your healthcare professional if you’re pregnant or breastfeeding so they can prescribe the most suitable antibiotic for you.
Only ever take antibiotics prescribed for you – never “borrow” them from a friend or family member.
Some antibiotics do not mix well with other medicines, such as the contraceptive pill and alcohol.
Read the information leaflet that comes with your medicine carefully and discuss any concerns with your pharmacist or GP.
Read more about how antibiotics interact with other medicines.
Types of antibiotics
There are hundreds of different types of antibiotics, but most of them can be classified into 6 groups.
- Penicillins (such as penicillin, amoxicillin, co-amoxiclav, flucloxacillin and phenoxymethylpenicillin) – widely used to treat a variety of infections, including skin infections, chest infections and urinary tract infections
- Cephalosporins (such as cefalexin) – used to treat a wide range of infections, but some are also effective for treating more serious infections, such as sepsis and meningitis
- Aminoglycosides (such as gentamicin and tobramycin) – tend to only be used in hospital to treat very serious illnesses such as sepsis, as they can cause serious side effects, including hearing loss and kidney damage; they’re usually given by injection, but may be given as drops for some ear or eye infections
- Tetracyclines (such as tetracycline, doxycycline and lymecycline) – can be used to treat a wide range of infections, but are commonly used to treat acne and a skin condition called rosacea
- Macrolides (such as azithromycin, erythromycin and clarithromycin) – can be particularly useful for treating lung and chest infections, or as an alternative for people with a penicillin allergy, or to treat penicillin-resistant strains of bacteria
- Fluoroquinolones (such as ciprofloxacin and levofloxacin) – are broad-spectrum antibiotics that were once used to treat a wide range of infections, especially respiratory and urinary tract infections; these antibiotics are no longer used routinely because of the risk of serious side effects
Other antibiotics include chloramphenicol (used for eye and ear infections), fusidic acid (used for skin and eye infections), and nitrofurantoin and trimethoprim (used for urinary tract infections).
Page last reviewed: 11 November 2022
Next review due: 11 November 2025
What are antibiotics? – article on the website Aptechestvo, Nizhny Novgorod
Antibiotics are a group of drugs that are used in the treatment of bacterial infections. Bacteria are living microorganisms that, having penetrated into the human body, begin active life and reproduction. The effect of antibiotic therapy is the direct destruction of the pathogen, as well as slowing down the reproduction of pathogens. In connection with these antibacterial drugs are divided into 2 large groups: bactericidal – destroying the bacterium itself, as well as bacteriostatic, inhibiting their growth. In addition, antibiotics have a narrow and broad spectrum of action. Narrow-spectrum drugs destroy the infection selectively, while broad-spectrum drugs destroy most of the microorganisms, including those that benefit humans. What antibiotics to take for the treatment of various diseases should be decided by the doctor after the diagnosis.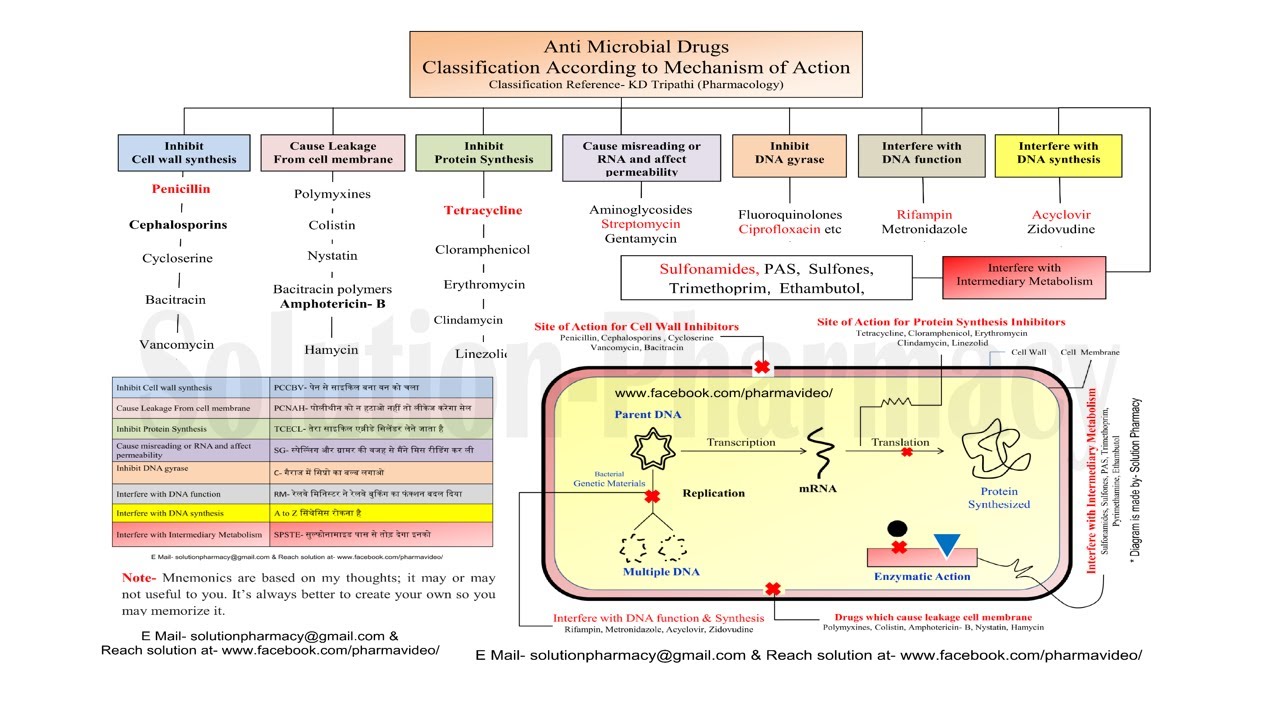 Taking such drugs at your own discretion is fraught with complications.
Taking such drugs at your own discretion is fraught with complications.
Fluoroquinolones
They suppress the activity of enzymes involved in the formation of bacterial DNA, as a result of which the infection dies. The drugs are available in the form of tablets, injections, ophthalmic drops. Indications for appointment:
This group of drugs:
Ciprofloxacin;
Ofloxacin;
Pefloxacin;
Norfloxacin.
Aminoglycosides
Broad-spectrum agents that kill most types of Gram-negative aerobic and facultative bacteria. The active substance disrupts the process of protein synthesis, as a result of which the pathogen is destroyed and dies.
Aminoglycosides are poorly absorbed when taken orally, so, as a rule, they are prescribed as intravenous or intramuscular injections. Members of this group:
Amikacin;
Gentamicin;
Kanamycin;
Neomycin;
Plazomycin;
Streptomycin.

As a rule, these drugs are used in combination with other antibiotics to treat such infectious diseases:
Tetracyclines
Bacteriostatic antibiotics that retard the growth of pathogenic microorganisms, but do not completely destroy them. As a result, the reproduction of the infection stops, and it gradually dies.
Tetracyclines have a wide spectrum of activity, with pronounced activity against aerobic gram-positive and gram-negative bacteria. Tetracyclines are not prescribed for children under 8 years of age, since long-term use causes a number of serious complications.
The drugs of this group can be prescribed in tablet forms and in the form of injections. For the treatment of ophthalmic infections, ointments are produced, the active substance of which is tetracycline.
Medicines:
doxycycline;
minocycline;
Tetracycline;
Oxytetracycline.

Diseases for which tetracyclines are prescribed:
Macrolides
They suppress vital activity and prevent the reproduction of anaerobic and aerobic gram-positive bacteria. Preparations of this group are used in the treatment of bronchopulmonary infections, tonsillitis, otitis, scarlet fever, intestinal infections. Medicines that are included in this group:
Erythromycin;
Azithromycin;
Clarithromycin;
Spiramycin.
Penicilli
A group of antibiotics produced by the fungus Penicillium. Penicilli are active against most Gram-positive and some Gram-negative bacteria. This group of drugs:
Amoxicillin;
Augumetin;
Amoxiclav;
Flemoxin Slutab.
Cephalosporins
These are bactericidal beta-beta-lactam antibiotics that interfere with cell protein synthesis. There are 5 generations of cephalosporins. The active substance penetrates well into most body fluids, having a pronounced bactericidal effect. Cephalosporins are used for uncomplicated skin and soft tissue infections caused by staphylococcal and streptococcal bacteria. This group of drugs:
There are 5 generations of cephalosporins. The active substance penetrates well into most body fluids, having a pronounced bactericidal effect. Cephalosporins are used for uncomplicated skin and soft tissue infections caused by staphylococcal and streptococcal bacteria. This group of drugs:
Ceftriaxone;
Cefodox;
Cefix;
Tsepefim.
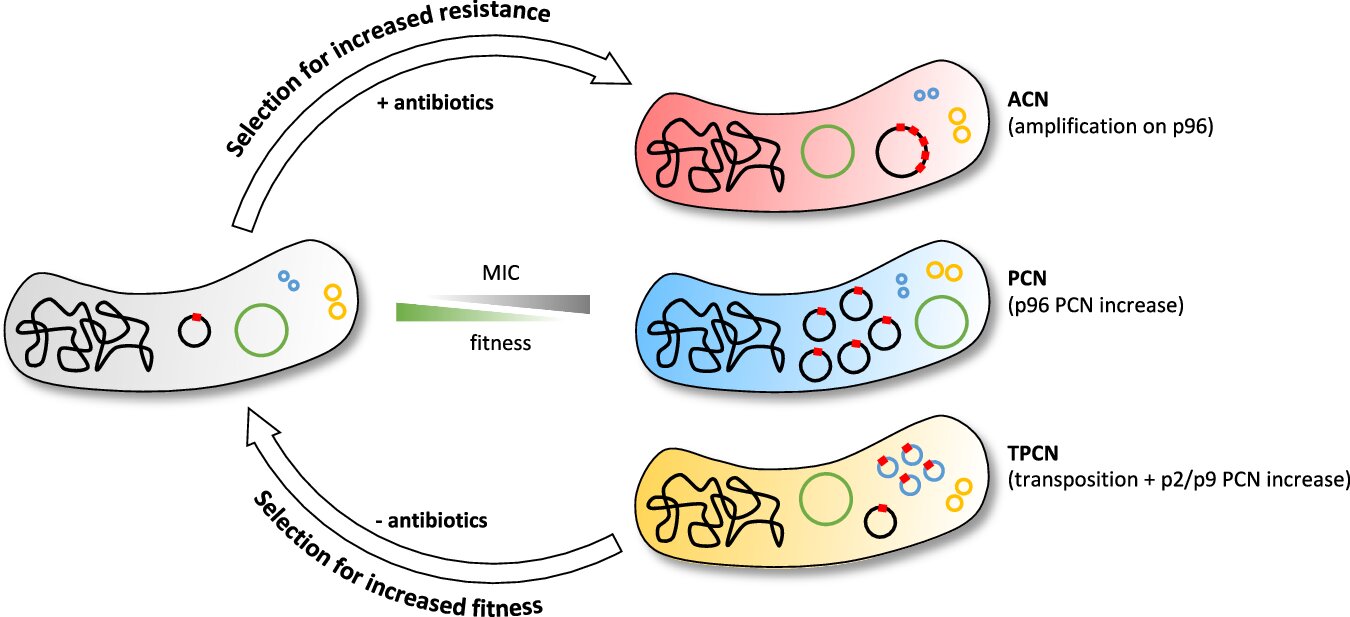
Bacteria are organisms that do not live long, but in order to restore their population, they multiply rapidly, and, accordingly, quickly mutate, adapting to new living conditions. Microorganisms that survive after taking antibiotics become resistant to them. Their offspring also become immune to a particular drug.
Antibiotic resistance is a common problem of modern man, which causes serious complications. A person who has tried many antibiotics, that is, self-medicated, is at risk for patients with antibiotic resistance.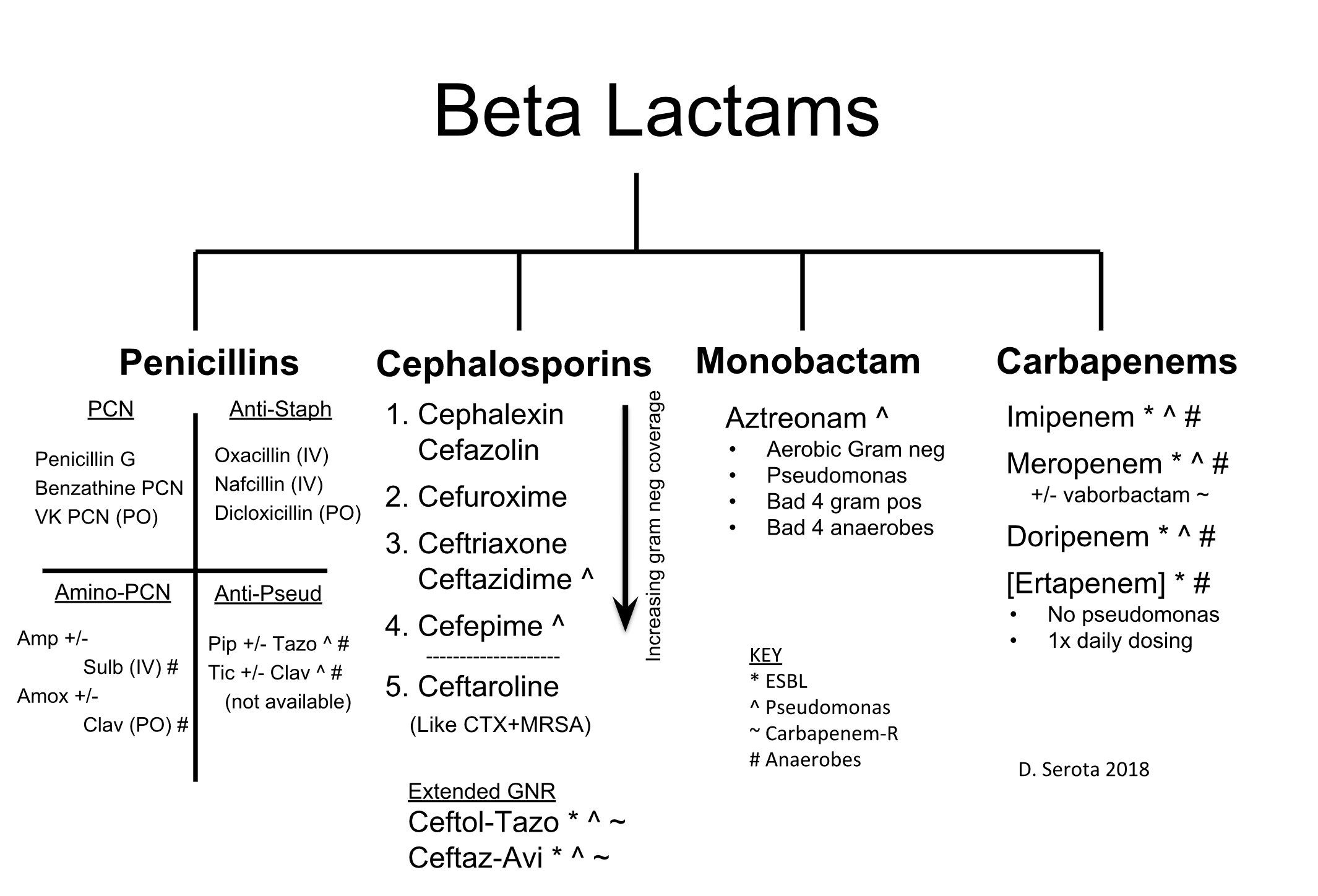 Very often they die before a specialist can pick up a drug that works against a specific pathogen. Therefore, it is important to follow the recommendations of the doctor and take antibacterial agents strictly according to an individual scheme.
Very often they die before a specialist can pick up a drug that works against a specific pathogen. Therefore, it is important to follow the recommendations of the doctor and take antibacterial agents strictly according to an individual scheme.
Broad spectrum antibiotics – buy in Ukraine
- Goods
Prices in pharmacies
Item: 494
Sorting:
RatingCheapest Expensive
Type:
Jump to box
Jump to box
Jump to box
Jump to box
Jump to box
9 0179 Go to box
Go to box
Go to box
Jump to kit
Jump to kit
Jump to kit
Jump to kit
Jump to kit
Jump to box
Jump to box
Jump to box
Jump to box
Jump to box
9 0177 Go to box
Go to box
Jump to box
Go to
Go to
Go to
Go to
Go to
Jump to box
Jump to box
Jump to box
Jump to box
Jump to box
Jump to box cat
go to cat
go to cat
go to cat
go to cat
go to cat
go to cat
go to cat
go to cat
Jump to box
Jump to box
Jump to box
Jump to box
Jump to box
9 0179 Go to box
Go to box
Go to box
Go to box
Go to box
Editorial group
Creation date: 06/04/2022
Date updated: 15. 07.2023
07.2023
Broad-spectrum antibiotics
A variety of bacteria live in the human body, many of which are necessary for normal functioning. Prote, you can also see the ailments that call different pathologies. To fight against bacterial infections, antibiotics are used – preparations of direct action, yakі reshkodzhayut їх reproduction and growth, priming the life of microorganism. More medical benefits are added only to the song type of pathogens, which makes the therapy easier and the need for the necessary medication. For the cure of the ailment caused by the culprit, a broad-spectrum antibiotic is used.
The widest pardon for the use of antibacterial drugs for the treatment of viral diseases. The stench is powerless against viruses, which have a daily clitin structure. In this case, an antibiotic may be used in combination with other drugs, since a viral infection may be aggravated and bacterial infection may be included.
Variety of broad-spectrum antibiotics
Antibacterial drugs in a large assortment are presented in Ukrainian pharmacies.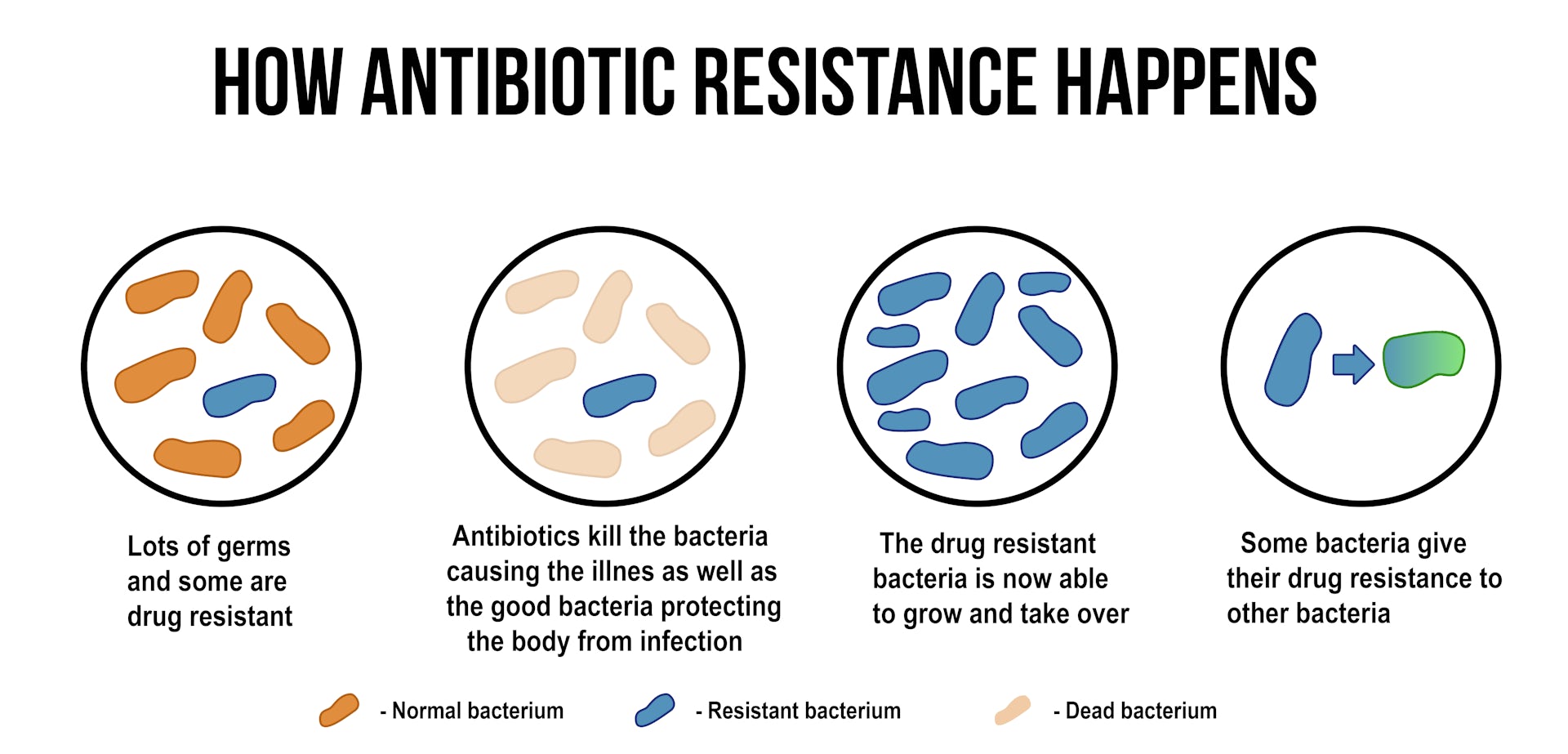 It is smarted by this building to effectively excite various infectious diseases, both in children and in adults. According to the chemical warehouse, broad-spectrum antibiotics are subdivided into 5 main groups, the skin may have its pharmacological activity:
It is smarted by this building to effectively excite various infectious diseases, both in children and in adults. According to the chemical warehouse, broad-spectrum antibiotics are subdivided into 5 main groups, the skin may have its pharmacological activity:
- Penicillin – ampicillin, bicillin, carbicillin are still available. Qi speech disrupts the synthesis of clitin membranes and pereskodzhayut proper osmosis of clitin, preventing the growth of microorganism. Antibiotics of the penicillin series are effective in the treatment of angina, sieve paths, infectious lesions of the bones, scoliosis and soft tissues, pneumonia.
- Cephalosporins of another generation (ceflaxor, cemafondol, ceflaquin) – drugs of this series are prescribed, as the patient is suspected of intolerance to antibiotics of the penicillin series. They may be similar to them for the treatment of infections of the sechostatic system, ENT organs, gynecology, postoperative infections of the cystic and soft tissue.

- Tetracyclines (doxycycline, tetracycline) – a speech agent that affects the impaired protein synthesis of bacteria of various species. Tetracyclines are good at coping with acne, infectious ENT diseases, and problems with ICT.
- Aminoglycosides (gentamicin, streptomycin) – block the production of proteins, which are necessary for the development of pathogenic bacteria. Use them with other antibacterial drugs for treatment of endocarditis, osteomyelitis, peritonitis, infections of the sacs, tuberculosis.
- Rifamycin (rifampicin) – speech is related to the DNA of pathogenic microorganisms. Rifamycins cause disruption of their synthesis and are especially effective in treating tuberculosis and other diseases that provoke mycobacteria. Also, an antibiotic should be used for the treatment of damage to the dichal system and the sec- ondary organs. To rifampicin, resistance is largely blamed for this, which is due to the presence of rifampicin in combination with other antibacterial drugs.

How to choose the right drug?
First name to buy broad spectrum antibiotics, consult your doctor. Only fahіvets zdatny signs of competently likuvannya and choose the necessary pharmacological form of the drug, yogo dosing that scheme to receive. Call the doctor and recommend a specific name for the drug, or the patient can ask for an antibiotic with a viable fluctuating speech, another trade name. You can find such an analogue in a different way, for example, on the website of MIS Pharmacy 9-1-1 on antibiotics of a wide range of prices to lie in the company-virobnik, dosing and pharmacological authorities of the people. You can replace the necessary goods online or with delivery in Ukraine. Sales zdіysnyuєtsya for the prescription of a doctor, he does not rely on the advice of those who know and engage in self-admiration. Uncontrolled intake of antibiotics can lead to the development of bacterial resistance to the drug and not to give an overbearing effect. It is very important for him to take the dosage of that scheme to the reception, and also not to interrupt the course at the first visible flushes.
Copy of vikoristan literature
- physio-pedia.com;
- Sovereign register of medical supplies of Ukraine;
- betterhealth.vic.gov.au.
FAQ
Why can broad-spectrum antibiotics be combined?
It is important to remember that antibiotics are applied to all types of bacteria, including the corysnus microflora. That is why it is necessary to supplement them with the intake of probiotics, in order to take revenge on the obviousness of the bacterium in a dried-up or shriveled look. In some cases, additional use of antihistamines is required.
How can antibiotics cover a wide spectrum of activities?
The most popular antibiotics in tablets and ampoules (vials) of a wide spectrum can be seen: Azithromycin, Cefuroxime, Amoxicillin/clavulanic acid, Levofloxacin, Cefixime.
Broad spectrum nutrition
What are inexpensive products in the category Broad spectrum antibiotics?
What are the imported goods in the category Broad spectrum antibiotics?
What are the most popular products in the category Broad Spectrum Antibiotics?
What is the list of products in the category Antibiotics of a wide spectrum?
Prices for goods in the category Broad spectrum antibiotics start at 4.

 Helicobacter pylori treatment: antibiotics or probiotics. Appl Microbiol Biotechnol. 2018 Jan;102(1):1-7. doi: 10.1007/s00253-017-8535-7. Epub 2017 Oct 26. PMID: 29075827; PMCID: PMC5748437.
Helicobacter pylori treatment: antibiotics or probiotics. Appl Microbiol Biotechnol. 2018 Jan;102(1):1-7. doi: 10.1007/s00253-017-8535-7. Epub 2017 Oct 26. PMID: 29075827; PMCID: PMC5748437.


