What to do in periods pain. 13 Effective Ways to Alleviate Period Pain and Stop Menstrual Cramps
What causes period pain and how can it be managed. How to relieve menstrual cramps using natural remedies and lifestyle changes. Which treatments are most effective for dysmenorrhea.
Understanding the Causes of Menstrual Pain
Period pain, also known as dysmenorrhea, affects over half of menstruating women for one to two days each month. While period discomfort can manifest as headaches or general unease, it’s most commonly associated with menstrual cramps. These cramps occur when the uterus contracts to shed its lining, potentially causing pain in the stomach, lower back, groin, or upper thighs.
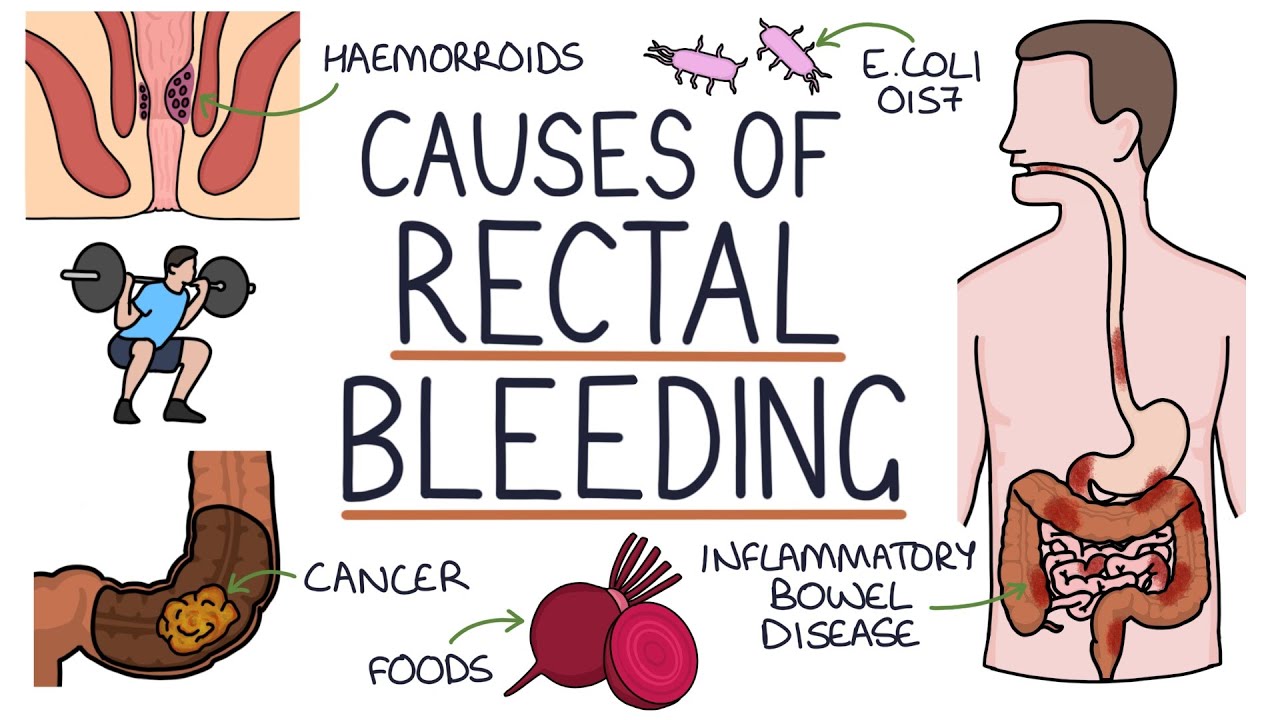
Several factors can contribute to menstrual pain:
- Premenstrual Syndrome (PMS)
- Premenstrual Dysphoric Disorder (PMDD)
- Uterine Fibroids
- Ovarian Cysts
- Pelvic Inflammatory Disease (PID)
- Endometriosis
- Adenomyosis
Premenstrual Syndrome (PMS)
PMS affects 90% of menstruating women, typically starting a few days before menstruation and continuing into the first day or two of the period. It’s believed to be caused by fluctuating estrogen and progesterone levels. Symptoms include fatigue, irritability, and menstrual cramps.

Premenstrual Dysphoric Disorder (PMDD)
PMDD is a more severe form of PMS, affecting about 5% of menstruating women. While its exact cause is unknown, women with high stress levels, depression, or a family history of depression are more susceptible. PMDD symptoms are similar to PMS but more intense, including more painful cramps.
The Impact of Reproductive Health Conditions on Period Pain
Uterine Fibroids
Uterine fibroids are benign growths that develop in the uterine lining. They can range from microscopic to large enough to alter the uterus’s shape. Fibroids typically appear during childbearing years and often shrink or disappear after menopause. Risk factors include age, African American ancestry, family history, and being overweight. As fibroids grow in the uterine lining, they can lead to heavy periods and painful menstrual cramps.
Ovarian Cysts
Ovarian cysts are fluid-filled sacs that form in or on the ovaries, often during ovulation. While most cysts are small and harmless, some women develop multiple or large cysts that can cause pain or complications. Polycystic Ovary Syndrome (PCOS) is a condition where hormone imbalances cause multiple small cysts to grow in the ovaries, potentially leading to painful periods, fertility issues, and other health concerns.

Pelvic Inflammatory Disease (PID)
PID is an infection of the uterus and ovaries, typically caused by bacteria from sexually transmitted infections or following surgical procedures. While many women experience no symptoms, PID can cause painful cramps in some cases.
Endometriosis
Endometriosis occurs when the uterine lining (endometrium) grows outside the uterus, usually on other reproductive organs. During menstruation, this misplaced tissue has nowhere to go, leading to painful cramps, heavy bleeding, irritation, and inflammation. Most cases of endometriosis can be managed effectively with modern medical treatments.
Adenomyosis
Adenomyosis is a condition where the endometrium grows into the muscle wall of the uterus. While it can affect the entire uterus, it usually impacts one specific area. Women who have had children or undergone uterine surgery have a higher risk of developing adenomyosis, which can cause severe menstrual cramps.
Natural Remedies for Alleviating Period Pain
For those seeking relief from menstrual cramps, several natural remedies and lifestyle changes can be effective:

- Apply heat to the lower abdomen
- Exercise regularly
- Practice relaxation techniques
- Maintain a healthy diet
- Stay hydrated
- Try herbal supplements
- Use essential oils
The Power of Heat Therapy
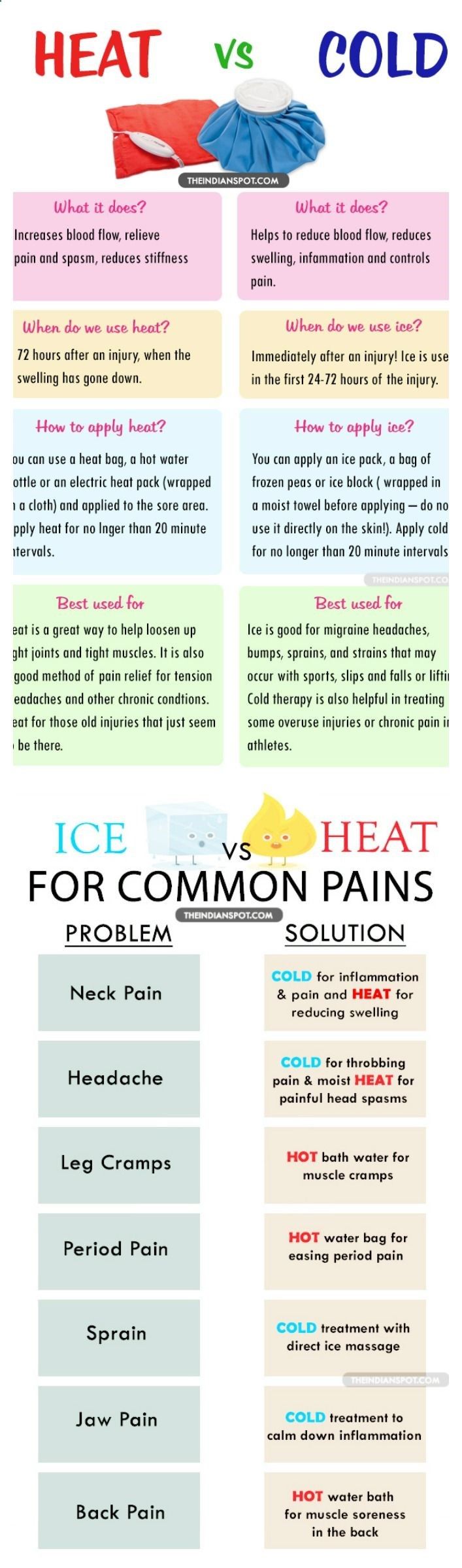
Applying heat to the lower abdomen can help relax the uterine muscles and alleviate cramping. How does heat therapy work for menstrual pain? The warmth increases blood flow to the area, reducing muscle tension and easing discomfort. You can use a heating pad, hot water bottle, or even take a warm bath to experience relief.
Exercise and Its Impact on Menstrual Cramps
Regular physical activity can significantly reduce the severity of menstrual cramps. Why does exercise help with period pain? Exercise releases endorphins, which are natural pain relievers. Additionally, it improves blood circulation throughout the body, including the uterus, which can help reduce cramping. Low-impact activities like walking, swimming, or yoga can be particularly beneficial during menstruation.
Dietary Approaches to Managing Period Pain
Your diet can play a crucial role in managing menstrual discomfort. Consider incorporating the following dietary changes:

- Increase intake of omega-3 fatty acids
- Consume more magnesium-rich foods
- Reduce caffeine and alcohol consumption
- Eat anti-inflammatory foods
The Role of Omega-3 Fatty Acids
Omega-3 fatty acids have anti-inflammatory properties that can help reduce menstrual pain. How do omega-3s alleviate period cramps? They help to balance prostaglandins, hormone-like substances that can cause uterine contractions and pain. Good sources of omega-3s include fatty fish, flaxseeds, and walnuts.
Magnesium: A Natural Muscle Relaxant
Magnesium is a mineral that acts as a natural muscle relaxant, potentially easing menstrual cramps. Which foods are high in magnesium? Dark leafy greens, nuts, seeds, and whole grains are excellent sources of this beneficial mineral. Some studies suggest that magnesium supplementation may help reduce the severity of menstrual pain.
Herbal Remedies and Supplements for Period Pain Relief
Several herbal remedies and supplements have shown promise in alleviating menstrual discomfort:

- Ginger
- Cinnamon
- Fennel
- Chamomile
- Dong Quai
The Anti-inflammatory Properties of Ginger
Ginger has been used for centuries to alleviate various types of pain, including menstrual cramps. How does ginger help with period pain? Its active compounds, including gingerols and shogaols, have anti-inflammatory and pain-relieving properties. You can consume ginger as a tea, in supplement form, or add it to your meals for potential relief.
Cinnamon: A Spice with Pain-Relieving Potential
Cinnamon is another spice that may help reduce menstrual pain. What makes cinnamon effective against period cramps? It contains compounds that can help regulate menstrual cycles and reduce inflammation. Some studies suggest that cinnamon supplementation may lead to less severe menstrual pain and shorter duration of bleeding.
Lifestyle Changes to Reduce Menstrual Discomfort
In addition to dietary changes and natural remedies, certain lifestyle modifications can help manage period pain:
- Get adequate sleep
- Manage stress levels
- Quit smoking
- Maintain a healthy weight
- Practice good posture
The Importance of Quality Sleep
Getting enough quality sleep is crucial for managing menstrual pain. How does sleep affect period cramps? Lack of sleep can increase sensitivity to pain and exacerbate inflammation. Aim for 7-9 hours of sleep per night, especially during your menstrual cycle, to help your body better cope with discomfort.
Stress Management Techniques
Chronic stress can worsen menstrual pain and other PMS symptoms. Which stress-reduction techniques are effective for period pain? Practices such as meditation, deep breathing exercises, and mindfulness can help reduce stress levels and potentially alleviate menstrual discomfort. Regular engagement in these activities may lead to long-term improvements in period pain management.
Medical Interventions for Severe Menstrual Pain
When natural remedies and lifestyle changes aren’t sufficient, medical interventions may be necessary:
- Over-the-counter pain relievers
- Hormonal birth control
- Prescription pain medications
- Surgical options for underlying conditions
Over-the-Counter Pain Relievers
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can effectively reduce menstrual pain. How do NSAIDs work to relieve period cramps? They inhibit the production of prostaglandins, which are responsible for uterine contractions and pain. Taking these medications at the first sign of pain or even before your period starts can maximize their effectiveness.

Hormonal Birth Control Options
Hormonal contraceptives, such as birth control pills, patches, or hormonal IUDs, can help regulate menstrual cycles and reduce pain. How do hormonal contraceptives alleviate period pain? They work by thinning the uterine lining, leading to lighter periods and less cramping. Additionally, some forms of hormonal birth control can reduce the frequency of periods or eliminate them altogether.
When to Seek Medical Attention for Menstrual Pain
While some level of menstrual discomfort is common, severe or debilitating pain may indicate an underlying condition that requires medical attention. Consider consulting a healthcare provider if:
- Pain interferes with daily activities
- Over-the-counter medications don’t provide relief
- Pain worsens over time
- You experience heavy bleeding or irregular periods
- Pain occurs outside of your menstrual cycle
Diagnostic Procedures for Severe Menstrual Pain
If you’re experiencing severe or chronic menstrual pain, your healthcare provider may recommend various diagnostic procedures to identify the underlying cause. Which tests are commonly used to diagnose causes of severe period pain? These may include pelvic exams, ultrasounds, laparoscopy, or hormone level tests. Early diagnosis and treatment of conditions like endometriosis or fibroids can lead to more effective management of menstrual pain.

By understanding the causes of menstrual pain and exploring various treatment options, women can take control of their menstrual health and find relief from debilitating cramps. Whether through natural remedies, lifestyle changes, or medical interventions, there are numerous strategies available to manage period pain effectively. Remember that every woman’s experience is unique, and what works for one may not work for another. It’s essential to work with healthcare providers to develop a personalized approach to managing menstrual discomfort and maintaining overall reproductive health.
13 ways to stop period cramps
Over half of women who menstruate experience period pain (dysmenorrhea) for one to two days every month. And even though period pain can mean headaches or general discomfort, the pain is typically caused by menstrual cramps.
Menstrual cramps happen when your uterus contracts to shed its lining, also known as the uterine lining. This can cause pain in your stomach, lower back, groin or upper thighs. Previously, we talked about when it makes sense to see a doctor for menstrual cramps. Here, we’ll talk about what might be causing your period pain and offer 13 home remedies you can try to improve it.
What causes period pain?
There can be many reasons for period pain, and if you experience chronic painful periods, it’s only natural to wonder why. Maybe you’re the only woman in your family who gets severe cramps. Maybe your painful periods didn’t start until your 20s. Whatever your situation, a doctor can help you understand why you get painful cramps every month. Some of the most common causes of painful periods are:
Some of the most common causes of painful periods are:
PMS (premenstrual syndrome)
Also known as premenstrual syndrome, PMS affects 90% of menstruating women. PMS starts a few days before your period begins and continues into the first day or two of menstruation. Doctors think PMS is caused by estrogen and progesterone levels dipping before the beginning of each period. PMS has many symptoms, including fatigue, irritability and menstrual cramps.
PMDD (premenstrual dysphoric disorder)
Premenstrual dysphoric disorder is a more severe form of PMS that affects about 5% of menstruating women. Doctors aren’t sure what causes PMDD, but women with high levels of stress, depression or a family history of depression are more likely to experience it. Symptoms of PMDD are similar to PMS, but more intense, including more painful cramps.
Fibroids
Uterine fibroids are benign growths that may develop in the lining of the uterus. They can be so small that it’s impossible to see them with the naked eye, or big enough to change the shape of your uterus.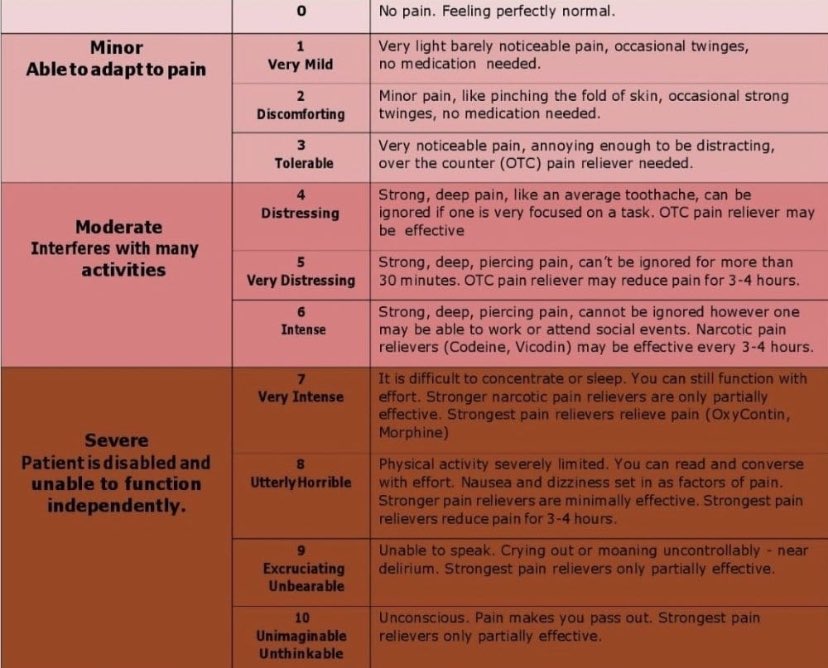 They usually appear during childbearing years and often shrink or go away completely after menopause.
They usually appear during childbearing years and often shrink or go away completely after menopause.
Doctors can’t be sure who will develop uterine fibroids, but certain factors can increase one’s risk. These include age, African American ancestry, having a family history of fibroids and being overweight.
Since fibroids grow in the uterine lining, they can cause heavy periods and painful menstrual cramps.
Ovarian cysts
A cyst is a usually harmless sac of fluid that forms in or on your body. Ovarian cysts develop in the ovaries, typically during ovulation. Many women develop at least one small cyst every month that naturally fades. However, some women have multiple or large ovarian cysts which can cause pain or complications. In these cases, medical treatment might be needed to manage the cysts.
Ovarian cysts can also be caused by polycystic ovary syndrome (PCOS). This is a condition where a hormone imbalance causes many small, harmless cysts to grow in the ovaries. This can cause painful periods, difficulty getting pregnant, insulin resistance and other health concerns. Symptoms of PCOS include irregular periods, excess hair on the face and body, weight gain, difficulty losing weight, acne and thinning hair. A doctor can prescribe treatments to help manage PCOS symptoms.
This can cause painful periods, difficulty getting pregnant, insulin resistance and other health concerns. Symptoms of PCOS include irregular periods, excess hair on the face and body, weight gain, difficulty losing weight, acne and thinning hair. A doctor can prescribe treatments to help manage PCOS symptoms.
PID (pelvic inflammatory disease)
When the uterus and ovaries become infected, this is called pelvic inflammatory disease (PID). The infection usually begins when bacteria from a sexually transmitted infection (STI) makes its way to the reproductive organs. PID can also happen following a surgical procedure. While many women experience no symptoms of PID, it can cause painful cramps for some people.
Endometriosis
The uterine lining, also known as the endometrium, grows inside the uterus. But if you have endometriosis, your endometrium grows outside the uterus, usually in other parts of your reproductive organs like the ovaries or fallopian tubes. When your body tries to shed uterine tissue during your period, the endometrium growing outside the uterus has nowhere to go. It can become trapped in the body. This can cause painful cramps, heavy bleeding, irritation and inflammation. With advances in medicine, most cases of endometriosis can be well managed with medications and procedures.
It can become trapped in the body. This can cause painful cramps, heavy bleeding, irritation and inflammation. With advances in medicine, most cases of endometriosis can be well managed with medications and procedures.
Adenomyosis
Adenomyosis is a treatable condition where the endometrium grows into the muscle wall of the uterus. The endometrium can affect the entire uterus muscle, but it usually affects one spot. Adenomyosis is a manageable condition, but it can cause severe cramps. Doctors aren’t sure exactly what causes adenomyosis, but women who’ve had children or undergone uterine surgery have a higher risk of developing it.
13 things that may help with period cramps
Dealing with menstrual cramps every month can be as frustrating as it is painful. The good news is there are many remedies that might help you relieve period cramps. It’s important to remember that these techniques won’t always work, especially for chronic conditions, but they can offer relief for mild to moderate period pain.
1. Drink more water to reduce bloating
Bloating can cause discomfort and make menstrual cramps worse. While it may sound counterintuitive, drinking water can reduce bloating during your period and alleviate some of the pain it causes. Also, drinking hot water can increase blood flow throughout your body and relax your muscles. This can lessen cramps caused by uterine contractions.
2. Enjoy herbal teas to relieve inflammation and muscle spasms
Certain types of herbal tea have anti-inflammatory properties and antispasmodic compounds that can reduce the muscle spasms in the uterus that cause cramping. Drinking chamomile, fennel or ginger tea is an easy, natural way to relieve menstrual cramps. Plus, these herbal teas can have other benefits, like stress relief and helping with insomnia.
3. Eat anti-inflammatory foods to relax menstrual cramps
Some foods can offer natural relief for cramps, and they taste great. Anti-inflammatory foods can help promote blood flow and relax your uterus.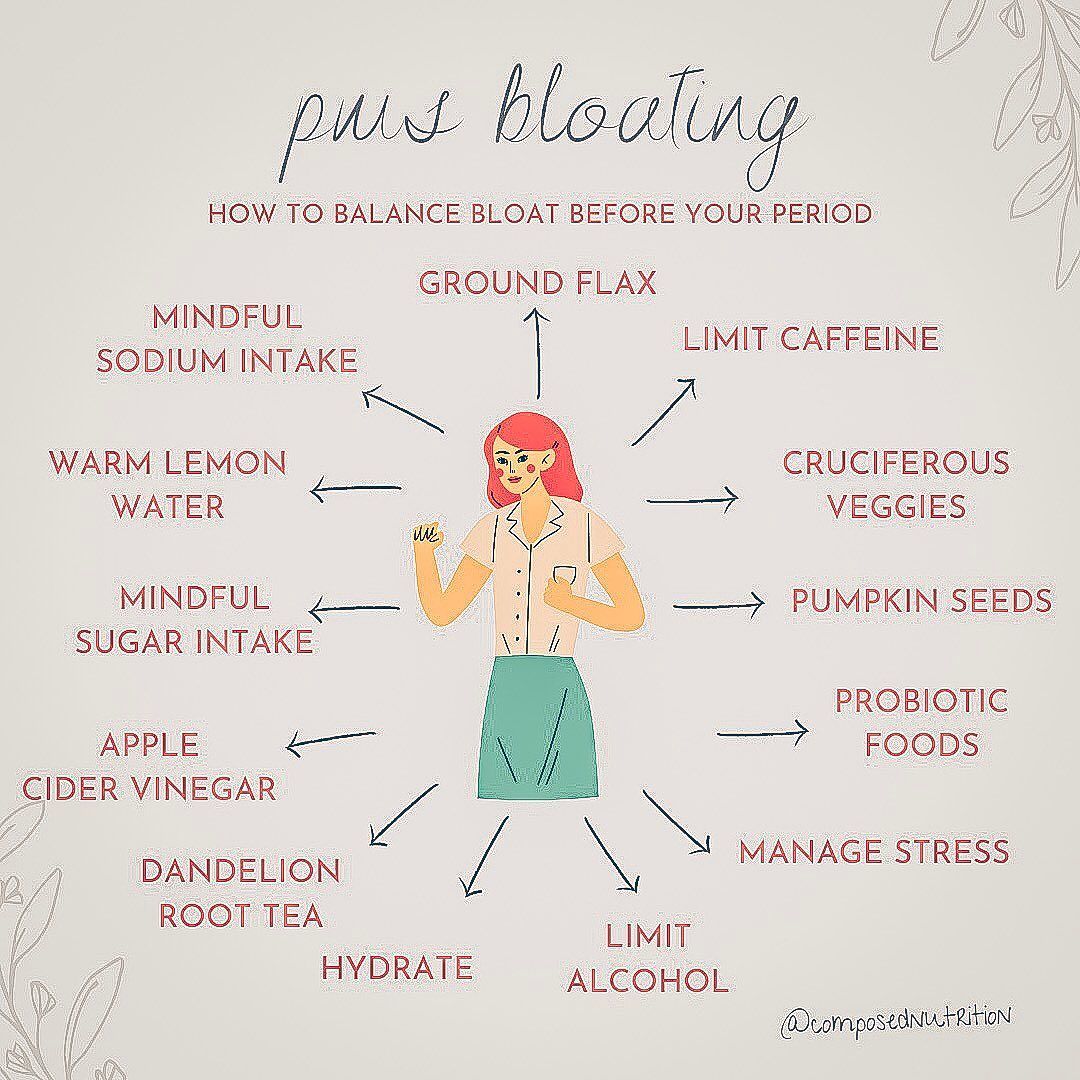 Try eating berries, tomatoes, pineapples and spices like turmeric, ginger or garlic. Leafy green vegetables, almonds, walnuts and fatty fish, like salmon, can also help reduce inflammation.
Try eating berries, tomatoes, pineapples and spices like turmeric, ginger or garlic. Leafy green vegetables, almonds, walnuts and fatty fish, like salmon, can also help reduce inflammation.
4. Skip the treats to avoid extra bloating
While a brownie or french fries might sound delicious, foods high in sugar, trans fat and salt can cause bloating and inflammation, which makes muscle pain and cramps worse. Grab a banana or another piece of fruit to fight sugar cravings, or go for unsalted nuts if you want something more savory.
5. Reach for decaf coffee to improve period pain
Caffeine causes your blood vessels to narrow. This can constrict your uterus, making cramps more painful. If you need your coffee fix, switch to decaf during your period. If you rely on caffeine to beat the afternoon slump, eat a snack high in protein or take a quick 10-minute walk to boost your energy.
6. Try dietary supplements to help with menstrual symptoms
Vitamin D can help your body absorb calcium and reduce inflammation.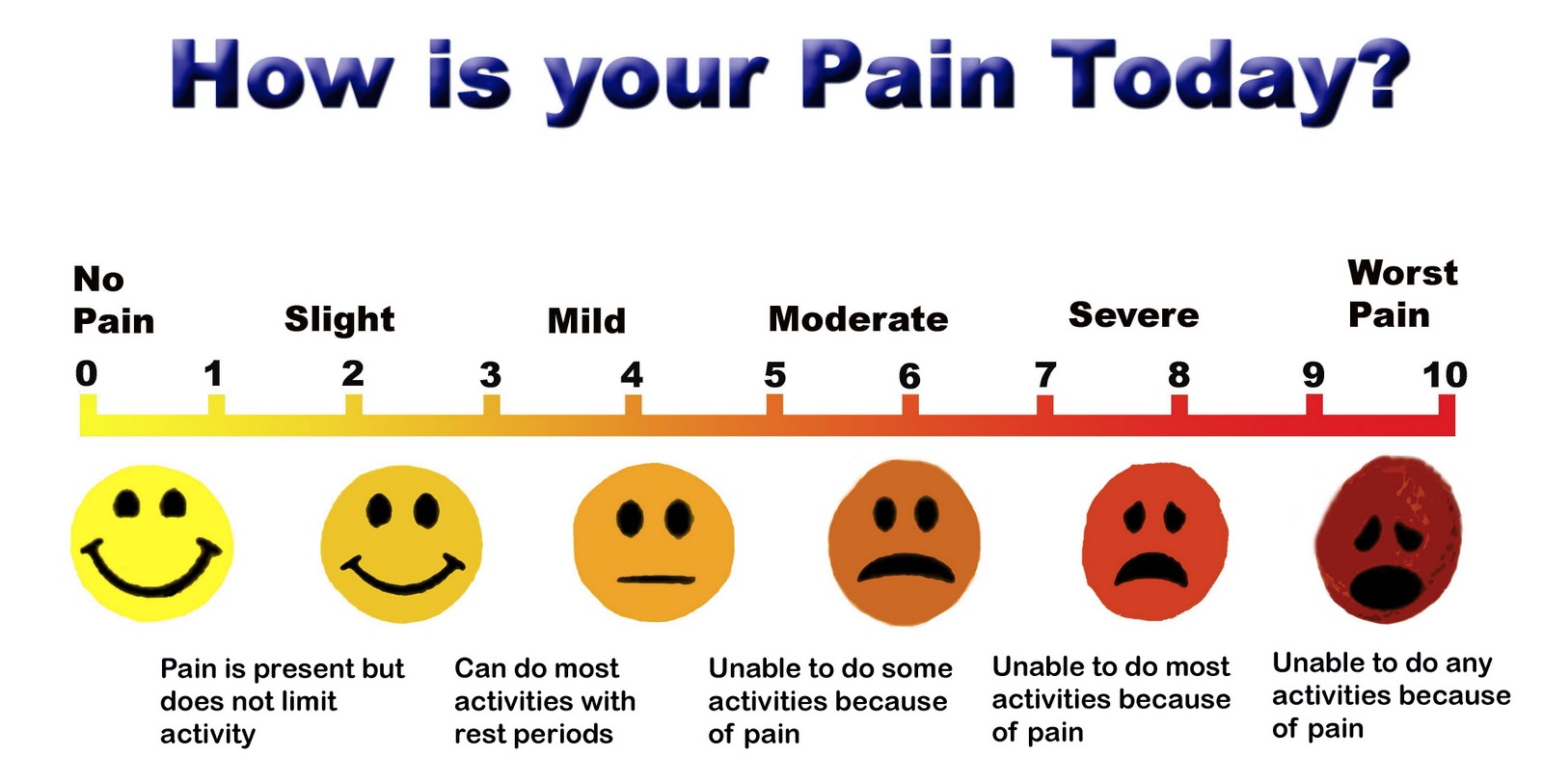 Other supplements, including omega-3, vitamin E and magnesium, can help reduce inflammation and might even make your periods less painful. For best results, take supplements every day, not just during your period. Also, because some supplements interact with medications, be sure to ask your doctor before taking anything new.
Other supplements, including omega-3, vitamin E and magnesium, can help reduce inflammation and might even make your periods less painful. For best results, take supplements every day, not just during your period. Also, because some supplements interact with medications, be sure to ask your doctor before taking anything new.
7. Apply heat to calm cramping
A little heat can help your muscles relax, improve blood flow and relieve tension. Try sitting with a heating pad, taking a hot shower or relaxing in a hot bath.
8. Exercise for muscle relaxation and endorphins
If you’re in pain, exercise might be the last thing on your mind. But even gentle exercise releases endorphins that make you feel happy, reduce pain and relax your muscles. Fifteen minutes of yoga, light stretching or walking might be all you need to feel the physical and mental benefits of exercise. And if exercise is already a part of your routine, did you know that tracking your period can help you improve athletic performance?
9.
 Reduce stress to improve mental and physical period symptoms
Reduce stress to improve mental and physical period symptoms
Stress may make cramps worse. Use stress relief techniques like meditation, deep breathing, yoga or your own favorite way to relieve stress. If you’re not sure how to relieve stress, try guided imagery. Simply close your eyes, take a deep breath and imagine a calm, safe place that’s significant to you. Stay focused on this space for at least a few minutes while you take slow, deep breaths.
10. Try massage therapy to reduce cramping and stress
One study found that massage therapy significantly reduced menstrual pain in women with endometriosis. Massages may reduce uterine spasms by relaxing the uterus. In order to manage period cramps most effectively, massage therapy should focus on the abdominal area. But a full body massage that reduces your overall stress may also help to relieve menstrual cramps.
11. Take over-the-counter (OTC) medicines to get rid of period cramps
The hormone prostaglandin can cause muscle contractions and pain. Anti-inflammatory medicines like ibuprofen can provide fast-acting relief by reducing the amount of prostaglandins in your body. For best results, only take OTC medicines when you start to feel cramps. OTC medicines may not always magically cure menstrual cramps, but they can often improve pain significantly. For best results, only take OTC medicines when you start to feel cramps.
Anti-inflammatory medicines like ibuprofen can provide fast-acting relief by reducing the amount of prostaglandins in your body. For best results, only take OTC medicines when you start to feel cramps. OTC medicines may not always magically cure menstrual cramps, but they can often improve pain significantly. For best results, only take OTC medicines when you start to feel cramps.
12. Try alternative medicine for PMS relief
Some people find relief with alternative medicine practices like acupuncture and acupressure. Acupuncture is a practice that stimulates the body by placing needles in the skin. Acupressure stimulates the body without needles by putting pressure on certain points of the body. These practices can help you relax, release muscle tension and improve blood flow throughout your body.
13. Start hormonal birth control
Birth control can stop period pain if cramps are caused by a hormone imbalance. Balancing your levels of estrogen and progesterone helps thin the uterine lining so it sheds more easily. Hormonal birth control also regulates the length and frequency of your period. Some forms of birth control can completely alleviate period cramps by stopping your period altogether. Talk to your OB-GYN about birth control options, including the pill, birth control shot or hormonal IUD. Then, you’ll be able to choose the type of birth control that works best for you.
Hormonal birth control also regulates the length and frequency of your period. Some forms of birth control can completely alleviate period cramps by stopping your period altogether. Talk to your OB-GYN about birth control options, including the pill, birth control shot or hormonal IUD. Then, you’ll be able to choose the type of birth control that works best for you.
Get help relieving period cramps
If you’ve tried all the menstrual cramp treatments on this list and still have painful periods, or you want to know up front which options will work best for you, talk to your primary care doctor or OB-GYN.
At HealthPartners and Park Nicollet, our women’s health doctors can prescribe stronger treatments for menstrual cramps that can go a long way to improve your quality of life during that time of the month. A little help from a doctor might be the best way to stop dreading your periods.
7 steps for treating pain that will get you feeling better
Chances are you or someone you know has been in some form of physical pain recently.
It’s thought that around 40% of adults in the United States have experienced pain in the last 3 months. A 2013 study found that osteoarthritis, joint and back problems are among the top 3 reasons people go to the doctor. And anecdotally, I can tell you we see a lot of complaints of headaches and jaw pain, too.
Unfortunately, research also shows that most people who have pain for a month will still have it 5 years later – even when they get treatment. The problem is that traditional measures do not work.
For many years, the medical community subscribed to what we thought was compassionate care. We lessened pain with long-term opioid medications. We believed this was safe.
We were wrong.
The fact is that opioids can still be a safe option, but only for short time periods. For example, pain pills for a few days after surgery can ease pain and allow people to get moving again and speed the healing process.
As pain turns chronic, it can become difficult to define an isolated cause behind it. Back pain is one example. Research shows that for about 85 percent of patients with back pain, there is no single cause for the pain that can be identified.
Back pain is one example. Research shows that for about 85 percent of patients with back pain, there is no single cause for the pain that can be identified.
This does not mean that chronic pain is “all in your head.” Human beings are complex. Our bodies, minds, emotions, relationships and environments all interact. If any one of these are out of sync, pain can be produced or worsened.
The reason is that stress, anger and other negative emotions affect the chemicals in our brains, which in turn affects our health. These toxic feelings reduce the chemicals we have that keep our brains functioning healthily, which is what can lead to depression and anxiety. And they bring on the release of chemicals that cause inflammation, which is what can lead to pain.
The good news is that you can rewire your brain with new pathways, which can reduce pain. This is known as “neuroplasticity.” So how do you do it?
I recommend starting with these 7 simple steps to protect yourself against pain:
- Exercise for strength and flexibility.

- Change your habits. Get adequate sleep and establish a healthy diet.
- Make time for things that make you feel joy, happiness and other positive emotions.
- Nurture positive social support systems with family and friends.
- Participate in activities and work that provides you with a sense of purpose.
- Promote healthy thoughts that will give you the ability to bounce back from stress.
- Create a clean and safe environment.
When it comes to chronic pain, there’s no one procedure or medication that’s a cure-all. That’s why HealthPartners provides a holistic approach to treating pain that’s been proven to reduce and control it.
We currently have 4 pain clinic locations. Each offers a variety of services in a single location to address the multiple causes of pain. Services include:
- Medical care to treat underlying physical conditions that cause pain
- Physical Therapy
- Occupational Therapy
- Behavioral Health support
- Relaxation training
- Medication management
Our first clinic opened in 2015 to serve patients who had been taking opioids but still had pain. And I’m pleased to report that more than 1,100 of the patients we’ve seen since report that their pain levels are lower by 50 percent, and that they have been able to stop taking opioids.
And I’m pleased to report that more than 1,100 of the patients we’ve seen since report that their pain levels are lower by 50 percent, and that they have been able to stop taking opioids.
Our organization’s pain clinic locations:
- HealthPartners RiverWay Pain Clinic in Coon Rapids
- HealthPartners Neuroscience Center in St. Paul
- TRIA Orthopaedic Center in Bloomington
- Park Nicollet Pain Management Clinic in St. Louis Park
how to reduce and get rid of pain during menstruation
{{if type === ‘partner-stocks’}}
{{/if}}
{{/if}}
{{each list}}
${this}
{{if isGorzdrav}}
Delete
{{/if}}
{{/each}}
{{/if}}
Search by drug, disease, substance:
Vitamins, Quit smoking, Voltaren, Nurofen, Lymphomyosot
Home
Articles
Painful periods – causes and treatment options
Severe pain during menstruation is not a variant of the norm, despite the high prevalence. This disease is called dysmenorrhea (or algomenorrhea). Gynecologists consider it as one of the violations of the menstrual cycle. From this material you will learn why the stomach hurts on the first day of menstruation, whether it is possible to get rid of this problem.
This disease is called dysmenorrhea (or algomenorrhea). Gynecologists consider it as one of the violations of the menstrual cycle. From this material you will learn why the stomach hurts on the first day of menstruation, whether it is possible to get rid of this problem.
Nature of menstrual pain
Abdominal pain varies in location. With dysmenorrhea, sensations occur in its lower part as a result of intense contractions of the uterus. The severity of menstrual pain is not the same for all women. Most people endure it “on their feet”, but in 15% of cases it is so strong that their ability to work suffers.
The nature of this phenomenon has not yet been established. A common theory explains dysmenorrhea by high levels of prostaglandins, hormone-like substances in the lipid group. They are secreted by the endometrium during the luteal phase.
Towards the end of the cycle, prostaglandins stimulate the contraction of spiral arterioles (uterine vessels), which provokes a menstrual reaction. If their level is too high, vascular spasms and episodes of local ischemia occur. This causes painful periods.
If their level is too high, vascular spasms and episodes of local ischemia occur. This causes painful periods.
Causes of primary dysmenorrhea
Dysmenorrhea can be primary or secondary. Primary manifests itself within a year after the first menstruation and occurs with each new cycle. In addition to increased levels of prostaglandins, sensations can be enhanced by the following factors:
- low pain threshold;
- abnormal location of the uterus;
- stagnation of blood in the pelvis;
- physiologically narrow cervix;
- psychological mood (anxiety, fear, expectation of illness).
Three forms of the disease are distinguished from this. Spasmodic is more caused by painful uterine contractions. Essential due to the low threshold of sensitivity. Psychogenic is a response to the fear of menstrual pain experienced once.
Increased risk of developing primary dysmenorrhea if there is a family history of it. Early menarche and prolonged menstrual bleeding also worsen the situation.
Early menarche and prolonged menstrual bleeding also worsen the situation.
Causes of secondary dysmenorrhea
Secondary dysmenorrhea can be diagnosed at any age. It is usually caused by other gynecological diseases. Most often it is endometriosis or fibroids, less often – adenomyosis, in which the uterus increases in size due to the presence of endometrioid glands in its muscles.
Menstruation that has suddenly become painful may be due to:
- inflammatory process in the small pelvis;
- intrauterine adhesions;
- blood stasis in the pelvis;
- neoplasms in the ovaries;
- using intrauterine contraceptives;
- traumatic narrowing of the cervical canal.
Dysmenorrhea can also be caused by congenital anomalies in the development of the organs of the reproductive system. Although symptoms appear from an early age, the disease is considered secondary.
Symptoms of algodysmenorrhea
The main symptom of dysmenorrhea is pain in the lower abdomen, which can be either very strong or almost not disturbing. They usually appear on the first day of the cycle, although they can begin before the actual bleeding. The nature of the pain is not the same for all women. It can be spasmodic or pulsating, sharp or dull. Feelings subside after a maximum of three days.
They usually appear on the first day of the cycle, although they can begin before the actual bleeding. The nature of the pain is not the same for all women. It can be spasmodic or pulsating, sharp or dull. Feelings subside after a maximum of three days.
The disease is accompanied by other symptoms:
- frequent urination;
- nausea;
- weakness;
- migraine headache;
- digestive disorders;
- hypersensitivity to odors;
- increased sweating;
- bloating;
- cardiac arrhythmias;
- edema;
- numbness of the extremities.
Although the main attention is focused on painful menstruation, algomenorrhea is considered as a complex of symptoms that accompany a woman with this cycle disorder.
What to do about painful menstruation?
Seeking a doctor in such a situation is mandatory, even if all relatives and friends suffer in the same way. Perhaps there is a disease that needs to be treated. The gynecologist will evaluate the severity of dysmenorrhea to understand how to reduce pain.
The gynecologist will evaluate the severity of dysmenorrhea to understand how to reduce pain.
Degree | Soreness | Associated symptoms | Performance impact | Method of pain relief |
0 | Missing | None | Missing | Not required |
I | Mild | None | Slight drop | Analgesics (as needed) |
II | Expressed | Single | Moderate decline | Analgesics (mandatory) |
III | Strong | Pronounced | Sharp decline up to temporary disability | Non-steroidal anti-inflammatory drugs |
The doctor’s task is not only to alleviate the symptoms, but also to do everything possible so that they do not appear in the future.
Treatment
Pregnancy is the only natural cause of dysmenorrhea. But it will not help to permanently get rid of the disease. Direct elimination of the cause is required, especially when it comes to the secondary form.
In primary dysmenorrhea, when the cause lies only in an increase in the level of prostaglandins, NSAIDs can be limited. In the secondary form, hormonal therapy is often required, within the framework of which it is prescribed:
- for endometriosis – danazol;
- with heavy menstruation and endometrial hyperplasia – levonorgestrel;
- in case of reaction to the uterine coil – etonogestrel;
- with uneven growth of the endometrium – medroxyprogesterone acetate.
Sometimes oral contraceptives help to relieve the disease. Estrogen-progestins in a small dosage weaken the manifestations of algomenorrhea.
What can be done at home?
If for some reason it is not possible to take analgesics or non-steroidal anti-inflammatory drugs, you can use non-drug methods to relieve pain.
The easiest of these is to lie down in the fetal position (with the knees drawn up to the chest). This will reduce the intensity of the spasms. But not every woman has such an opportunity, so it makes sense to consider other methods:
- Drink herbal tea. Mint or chamomile relaxes the abdominal muscles.
- Attach a heating pad with warm water. It will speed up blood circulation and weaken uterine contractions.
- Exercise. While strenuous exercise is best avoided during menstruation, a little stretching of the muscles is beneficial.
It is important to drink plenty of water. On the one hand, when bleeding, the body loses fluid, and it needs to be replenished. On the other hand, the gradually filling bladder presses on the uterus, increasing the pain. However, more frequent emptying of it brings temporary relief.
Is it possible to get rid of algodysmenorrhea forever?
The answer depends on the cause of the menstrual irregularity. If it is caused by secondary factors, everything possible should be done to eliminate them (cure inflammation, remove a cyst, eliminate congestion in the pelvis, etc.). After recovery, it will be possible to get rid of painful periods.
If it is caused by secondary factors, everything possible should be done to eliminate them (cure inflammation, remove a cyst, eliminate congestion in the pelvis, etc.). After recovery, it will be possible to get rid of painful periods.
If algomenorrhea is primary, nothing can be said unequivocally. In some cases, a course of hormone therapy helps, in others it remains only to constantly take measures to alleviate the symptoms.
For example, congenital anatomical anomalies are rarely corrected, respectively, painful menstruation will accompany a woman until the menopause. The only thing that can be done in such cases is to take painkillers and do not forget about prevention.
Prophylaxis
In order to avoid secondary dysmenorrhea, gynecological diseases should be treated in a timely manner.
It is almost impossible to prevent the development of primary algomenorrhea. Here it remains only to take measures to alleviate its manifestations:
- regularly perform exercises to disperse blood stasis in the small pelvis;
- increase intake of foods rich in calcium;
- take vitamins;
- avoid stress.

If the illness is psychogenic, psychotherapy may be helpful. Relieving tension in anticipation of the next menstruation, getting rid of fears of it, changing perceptions – all this reduces the intensity of pain.
Pain during menstruation: why the stomach hurts, how to reduce pain, what not to do
. Trainer’s advice and doctor’s commentary
Gynecologist Ilona Agrba explains the procedure for pain during menstruation
Updated on February 27, 2023, 06:32
Shutterstock
In Spain for the first time approved a law allowing women to take paid leave due to menstrual pain. We find out why they occur, as well as what can and cannot be done to get rid of unpleasant symptoms.
Contents
- Causes of pain
- Normal or not
- How to reduce pain
- What not to do
- Expert comment
Why does the stomach hurt during menstruation
Shutterstock
During the period of menstruation, the uterus rejects the mucous membrane – the endometrium – through the contraction of internal muscles [1]. For many women, this process is noticeable, but does not bring serious discomfort. For others, it causes severe pain that interferes with the usual way of life. Doctors cannot formulate with absolute certainty the reasons why this natural process takes place with different symptoms. One of the versions is an increased concentration of prostaglandins, a group of lipid substances actively secreted by the body during menstruation [2].
For many women, this process is noticeable, but does not bring serious discomfort. For others, it causes severe pain that interferes with the usual way of life. Doctors cannot formulate with absolute certainty the reasons why this natural process takes place with different symptoms. One of the versions is an increased concentration of prostaglandins, a group of lipid substances actively secreted by the body during menstruation [2].
Ilona Agrbavrach obstetrician-gynecologist, candidate of medical sciences, leading specialist of the network of clinics “Semeynaya”
“Painful contractions of the uterus with a feeling of general malaise due to excessive amounts of prostaglandins in the menstrual fluid (inflammatory mediators).”
Painful menstruation is called dysmenorrhea. There are two types of dysmenorrhea – primary and secondary:
- Primary dysmenorrhea occurs in people who experience pain shortly before and then during menstruation.
- Secondary – manifested at some point, if the patient had not previously encountered similar symptoms.
 In this case, it is important to undergo an examination: the causes may be pelvic inflammatory disease, endometriosis, stenosis and benign tumors.
In this case, it is important to undergo an examination: the causes may be pelvic inflammatory disease, endometriosis, stenosis and benign tumors.
Ilona Agrba:
“In physiological (normal) dysmenorrhea, pain in the lower parts appears a few days before menstruation or begins with it at the same time. Pain peaks in intensity 24 hours after the onset of menstruation, after which the symptoms subside and disappear no later than two to three days after the peak condition. The rest of the cycle, the woman does not experience discomfort and leads a normal life.
The pain can be different: pulling, throbbing, dull, can radiate to the lower extremities.
Harmless dysmenorrhea appears most often in adolescence after the establishment of regular menstruation. During the examination, the pathology is not detected, in most cases it disappears with age, sometimes after childbirth.
Secondary dysmenorrhea, which appears as a result of a disease, occurs some time after the establishment of a regular cycle, is similar in symptoms, but it is accompanied by gynecological diseases (adenomyosis, fibroids, external endometriosis).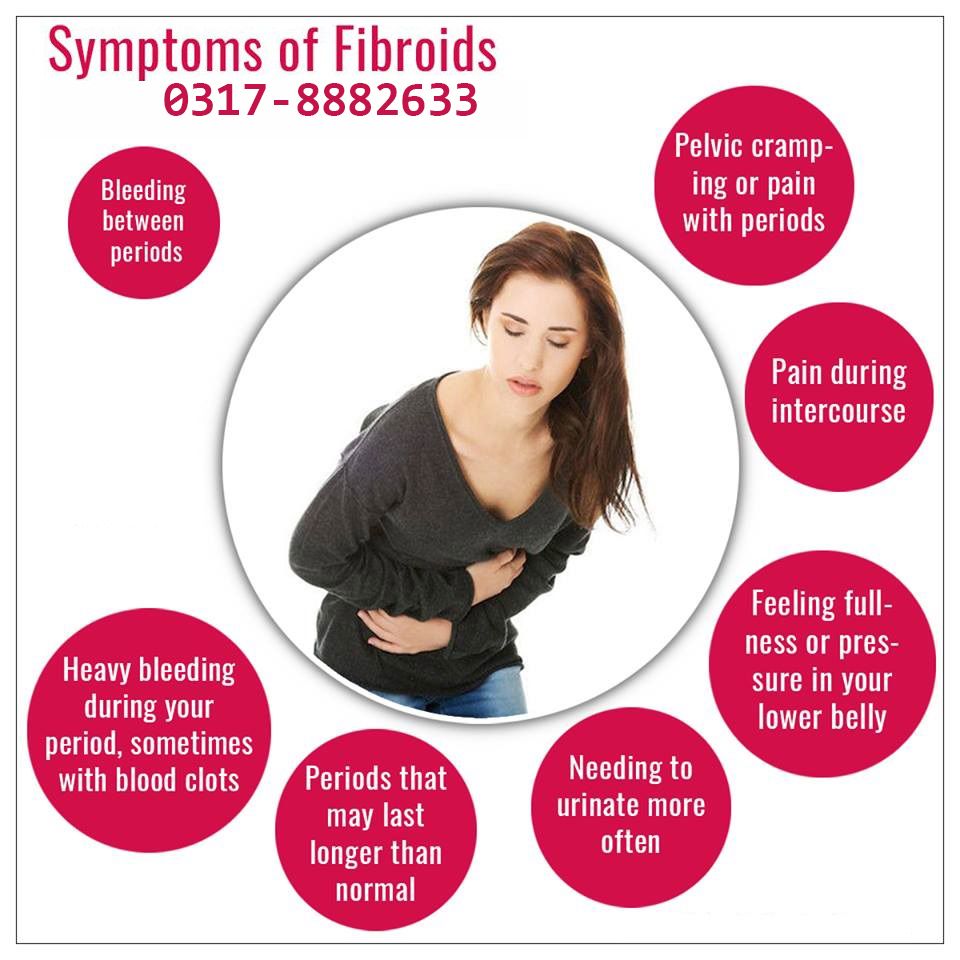 In this case, the pain does not occur on its own, but is a symptom of the disease.
In this case, the pain does not occur on its own, but is a symptom of the disease.
In addition to lower abdominal pain, prostaglandins affect the contraction of the smooth muscles of the gastrointestinal tract. Because of this, women often complain of problems with the gastrointestinal tract during menstruation: nausea, bloating and diarrhea may appear. Ilona Agrba clarifies that headache, constipation, frequent urge to urinate, vomiting can additionally disturb.
Pain during menstruation: normal or not
Shutterstock
Primary dysmenorrhoea is an individual feature of the organism. If you have experienced pain since your first menstrual cycle, it is likely that it will recur every month. Still, you should consult a doctor to rule out other causes of unpleasant symptoms. With secondary dysmenorrhea, a gynecological examination is strictly necessary. This is especially true in cases where the pain increases with each cycle or lasts for several days of menstruation.
The gynecologist will perform an examination, perform an ultrasound of the pelvic organs and, if necessary, prescribe urine and blood tests. Further treatment depends on the identified diseases. Even if serious causes of pain are not found, the doctor will select drugs and methods for getting rid of it.
What to do if the stomach hurts during menstruation: how to reduce pain
Shutterstock
Menstruation is often accompanied by other unpleasant sensations: nausea and headaches against the background of general weakness. Therefore, it makes sense to put things off, take a day off and take care of yourself, ensuring peace. There are several ways to relieve period pain.
1. Pain tablets
If you’re used to dysmenorrhea, make sure you have over-the-counter pain medications in your first aid kit. “Non-steroidal anti-inflammatory drugs are used from medicines. Their action is based on a decrease in the level of prostaglandins, ”says the obstetrician-gynecologist.
If the tablets do not help, contact your doctor and describe the situation in detail. You may need more effective drugs, such as those based on codeine and naproxen. Consider contraindications. So, ibuprofen and acetylsalicylic acid are not prescribed if the patient has a history of diseases of the kidneys, liver and stomach.
2. Hormonal contraceptives
In addition to protecting against unwanted pregnancy, medicated contraception helps correct some other problems in the body. Hormones “turn off” ovulation, and the lining of the uterus becomes thinner. The body produces a smaller amount of prostaglandins, respectively, muscle contractions of the uterus are minimized.
In addition to oral contraceptives, you can use spirals, implants and hormonal patches – the best option is selected by the attending physician, but the choice is up to the patient.
3. Lifestyle
Often the cause of secondary dysmenorrhea is the general condition of the body. Many are familiar with cycle failures and increased unpleasant symptoms after prolonged stressful situations, long trips, physical and psychological fatigue. In order for the body to function normally, it is necessary to adhere to the basic rules: observe a sleep schedule, get rid of stress in time and play sports – at least provide yourself with sufficient daily physical activity. Studies have shown that regular yoga classes relieve unpleasant symptoms during menstruation [3].
Many are familiar with cycle failures and increased unpleasant symptoms after prolonged stressful situations, long trips, physical and psychological fatigue. In order for the body to function normally, it is necessary to adhere to the basic rules: observe a sleep schedule, get rid of stress in time and play sports – at least provide yourself with sufficient daily physical activity. Studies have shown that regular yoga classes relieve unpleasant symptoms during menstruation [3].
4. Nutrition
What you eat affects all life processes and body functions in one way or another. It is important that the diet is complete and varied. Several studies have confirmed the positive impact of proper nutrition and nutritional supplements on the state of menstruation [4]. Talk to your doctor about whether you should take extra B vitamins, magnesium, and omega-3s.
5. Home Methods
Any drug will not work immediately at the time of administration. In anticipation of the effect, you can alleviate the condition in simple and affordable ways.
- Herbal tea. Some plants have an analgesic effect and promote muscle relaxation. Try brewing tea with chamomile or mint, fennel, and ginger.
- Self massage. Light strokes in the lower abdomen help relieve pain and relax the muscles. The method will not help to completely remove the pain, but it will come in handy until painkillers have taken effect [5].
- Heating pad. Ilona Agrba clarifies that this is one of the ways to help yourself with unpleasant symptoms. But be careful not to use too hot a heating pad for a long time: heat promotes vasodilation, which often increases bleeding.
To the question “Is it possible to get rid of menstrual pain forever?” there is no clear answer. For many with primary dysmenorrhea, it becomes less noticeable over the years, sometimes disappears after the birth of a child. But neither case applies to everyone without exception. One thing is certain: there is no point in enduring pain. Therefore, if once a month you consistently fall out of the schedule, seek help from a doctor, select and adjust a program to restore the body.
Therefore, if once a month you consistently fall out of the schedule, seek help from a doctor, select and adjust a program to restore the body.
What not to do during menstruation
Shutterstock
Do not forget about the safety rules that are relevant during the menstrual period. Very important:
- refuse to go to the bathhouse and sauna. Severe fever can cause profuse bleeding;
- abstain from unprotected sex. During this period, the uterus is vulnerable to infections and viruses;
- Do not bathe or swim in open water. Contrary to popular belief, a tampon will not protect the body from bacteria;
- change hygiene products in time in accordance with the manufacturer’s recommendations and individual characteristics (the amount of discharge).
Check out other common questions that cause a lot of controversy.
Is it possible to go in for sports during menstruation
Everything is very individual here. You definitely don’t need to force yourself to go for a run with pain, nausea and weakness. But if you feel good, do not give up training. Choose low-intensity exercise, long walks, yoga, Pilates.
You definitely don’t need to force yourself to go for a run with pain, nausea and weakness. But if you feel good, do not give up training. Choose low-intensity exercise, long walks, yoga, Pilates.
Maria GrudtsovaTrainer of personal training studios Pro Trainer
“If your health allows, there are no acute pains and discomfort, you can go in for sports, but with some restrictions. For example, exclude exercises that use a lot of weight, reduce axial loads and tension in the press. Inverted postures are not recommended in Pilates and yoga. But it all depends on your condition. Cardio training will be useful if you feel normal.”
Is it possible to do douching during menstruation
Washing the vagina during menstruation is strictly contraindicated. Douching can disturb the microflora, cause irritation and lead to infectious diseases.
Is it possible to donate blood during menstruation
Total amount of blood lost during menstruation is 50-150 ml.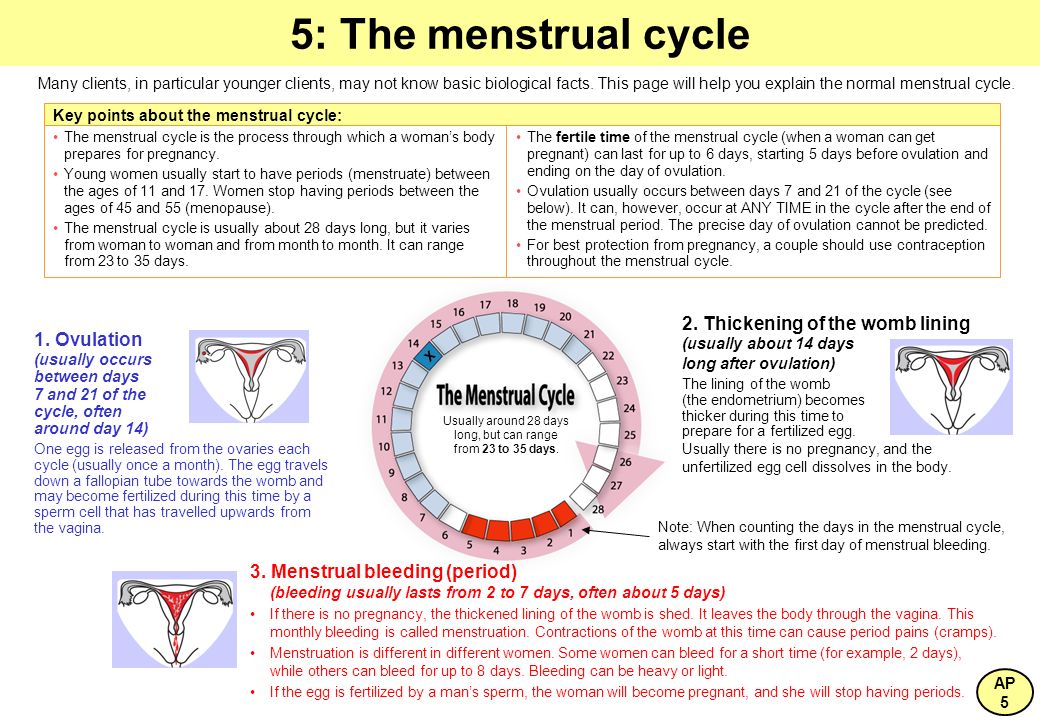 It’s not very much. But when donating blood, up to 500 ml are taken from donors, so even such a small amount can become critical. You should not donate blood during menstruation and another five days after, while the body is recovering. At the same time, menstruation is not a contraindication for surgical interventions [6].
It’s not very much. But when donating blood, up to 500 ml are taken from donors, so even such a small amount can become critical. You should not donate blood during menstruation and another five days after, while the body is recovering. At the same time, menstruation is not a contraindication for surgical interventions [6].
Can I drink alcohol
Although alcoholic beverages may have a slight analgesic effect, they affect the body differently depending on the day of the menstrual cycle. Even small amounts of alcohol can lead to less tolerance during periods.
Is it possible to carry out cosmetic procedures
During menstruation, the level of estrogen in a woman’s body decreases. Because of this, you feel more pain: the usual epilation and injections can feel much more painful and unpleasant. This will not affect the effect, but it is hardly worth giving yourself even more discomfort in this already difficult period.
Expert commentary
Pexels
Ilona Agrba:
“About half of women experience pain during menstruation. Many consider this a variant of the norm, and in most cases it is true, but sometimes pain during or before menstruation can be a symptom of the disease.
Many consider this a variant of the norm, and in most cases it is true, but sometimes pain during or before menstruation can be a symptom of the disease.
It is really possible to relieve and relieve pain without drugs: sports (for example, yoga) and sex (always with an orgasm), dietary changes (restriction of meat and fat, addition of dairy products) and vitamin therapy (group B, omega-3, magnesium).
If secondary dysmenorrhea is not caused by malformations of the uterus and vagina, it appears already in adulthood. Unlike primary, or normal, dysmenorrhea, there is no bloating, nausea, or vomiting. The pain increases during menstruation, may begin 3-10 days before it, often accompanied by additional complaints of painful defecation, blood during urination, pain in the lower back and legs. Often, the nature of menstruation also changes: they can become more scarce or, conversely, abundant, intermenstrual bleeding is diagnosed. In this case, the treatment will depend on the underlying cause.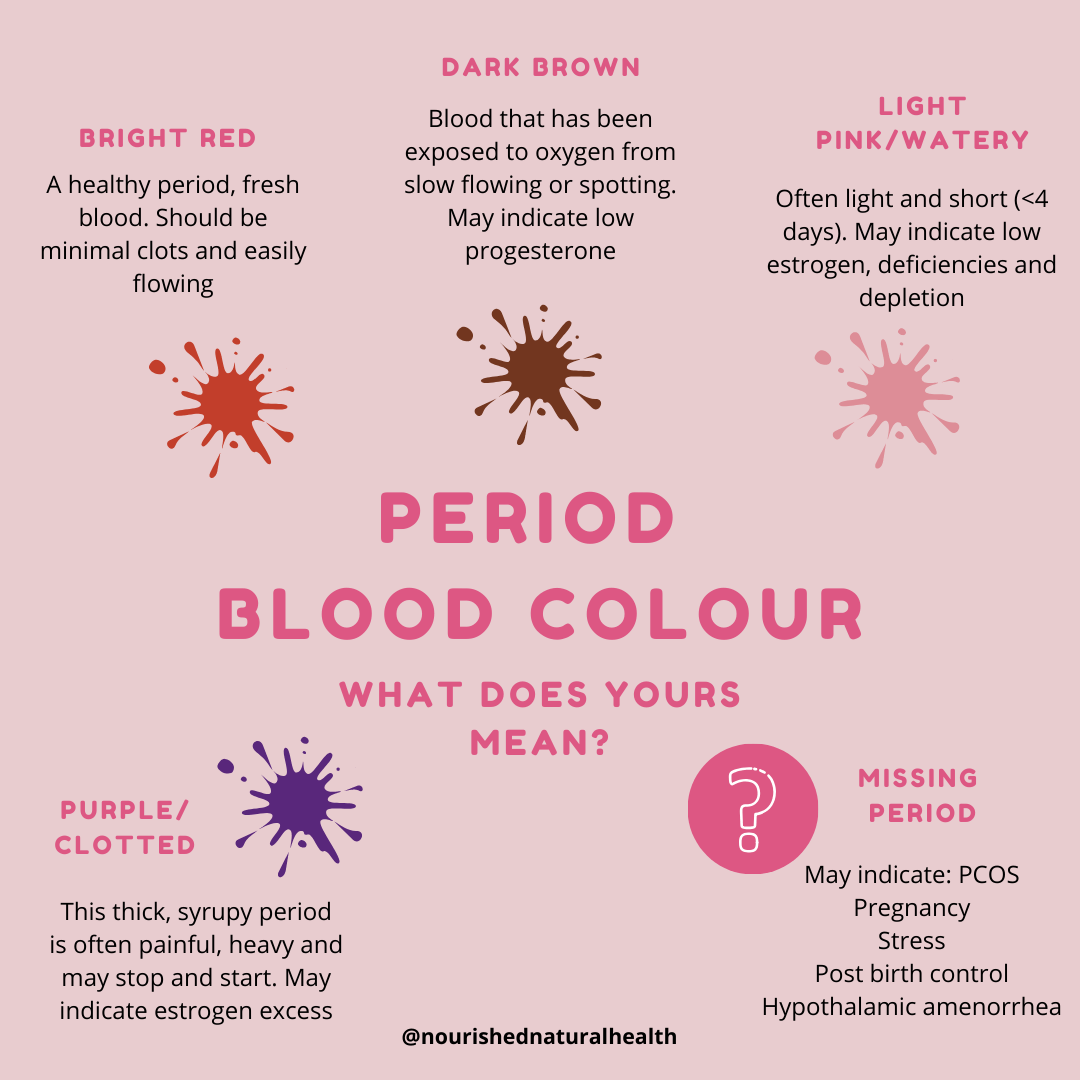


 In this case, it is important to undergo an examination: the causes may be pelvic inflammatory disease, endometriosis, stenosis and benign tumors.
In this case, it is important to undergo an examination: the causes may be pelvic inflammatory disease, endometriosis, stenosis and benign tumors.