Diseases of the eyes with pictures. Understanding Glaucoma: Symptoms, Causes, and Treatment Options
What are the main types of glaucoma. How is glaucoma diagnosed and treated. Can glaucoma be prevented or slowed down. What are the risk factors for developing glaucoma. How does glaucoma affect daily life and vision.
What is Glaucoma and How Does it Affect Vision?
Glaucoma is a group of eye conditions that damage the optic nerve, which is crucial for good vision. This damage is often caused by abnormally high pressure inside the eye. Glaucoma is one of the leading causes of blindness for people over the age of 60.
The optic nerve is responsible for sending visual information from the eye to the brain. When this nerve is damaged, it can lead to vision loss and blindness. The most common form of glaucoma has no warning signs, and the effect is so gradual that you may not notice a change in vision until the condition is at an advanced stage.
How does glaucoma progress?
Glaucoma typically begins by affecting peripheral or side vision. As it advances, it can lead to tunnel vision and eventually total blindness if left untreated. The progression of glaucoma can be slowed or halted with early detection and proper treatment.

Types of Glaucoma: Understanding the Differences
There are several types of glaucoma, each with its own characteristics and treatment approaches. The two main types are:
- Open-angle glaucoma
- Angle-closure glaucoma
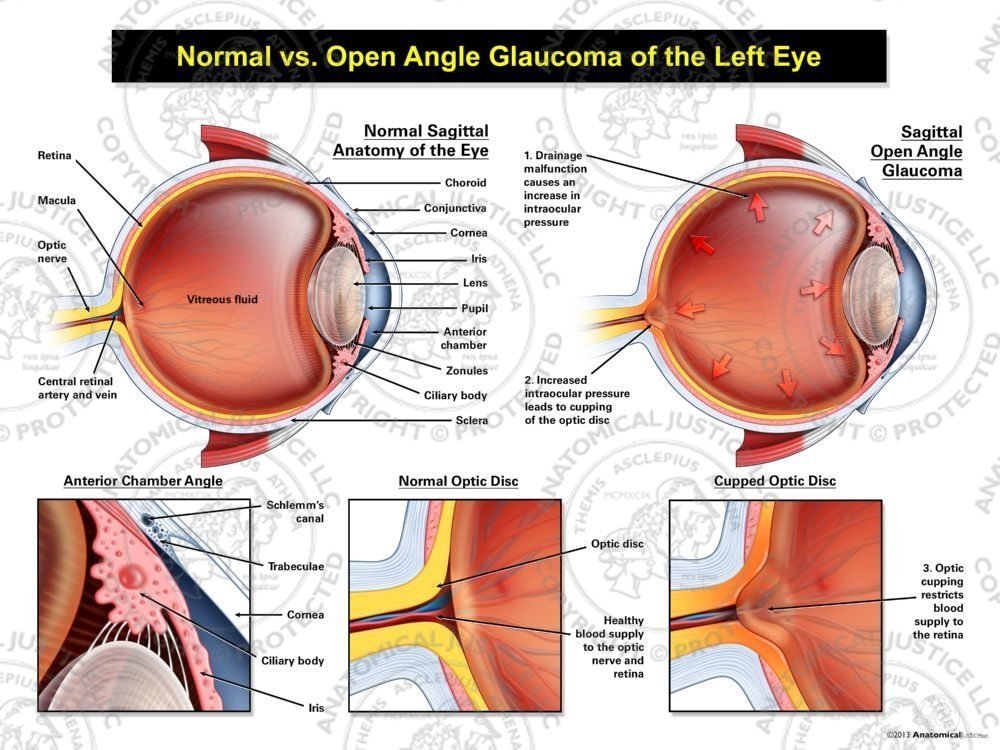
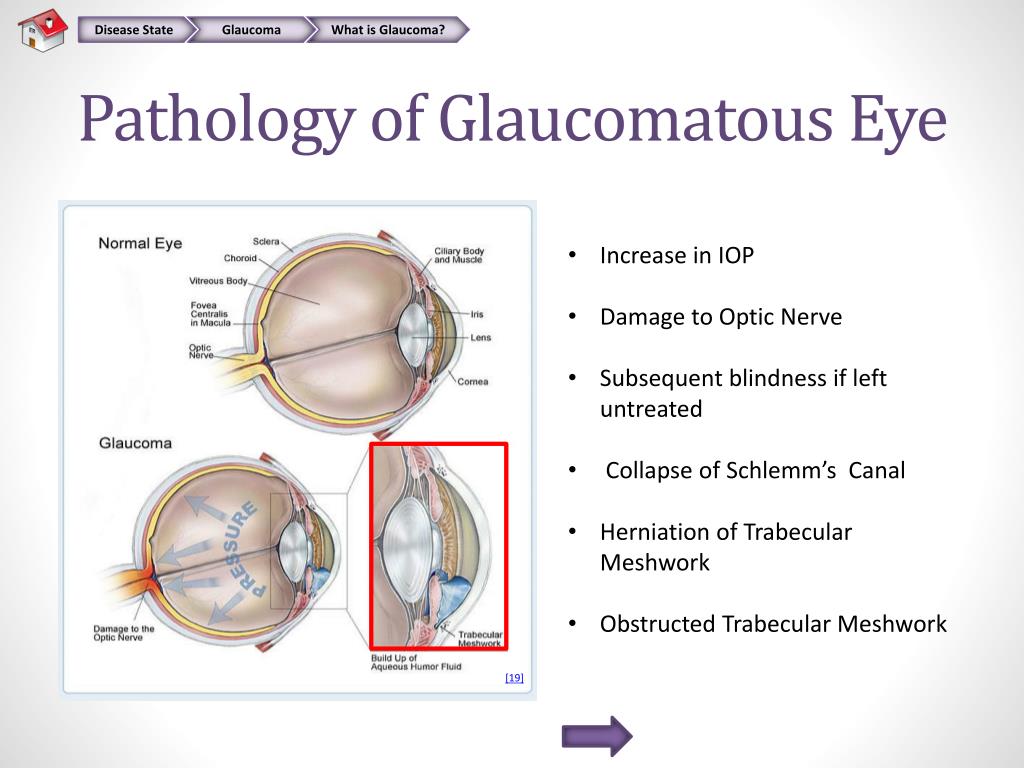
Open-angle glaucoma
Open-angle glaucoma is the most common form, accounting for about 90% of all cases. It occurs when the drainage angle formed by the cornea and iris remains open, but the trabecular meshwork is partially blocked. This causes pressure to build up slowly over time.
Angle-closure glaucoma
Angle-closure glaucoma, also known as closed-angle glaucoma, occurs when the iris bulges forward to narrow or block the drainage angle. This can happen suddenly (acute angle-closure glaucoma) or gradually (chronic angle-closure glaucoma).
Other less common types of glaucoma include normal-tension glaucoma, pigmentary glaucoma, and secondary glaucoma.
Recognizing the Symptoms: Early Warning Signs of Glaucoma
The symptoms of glaucoma can vary depending on the type and stage of the condition. Open-angle glaucoma, the most common form, often has no noticeable symptoms in its early stages.
What are the symptoms of open-angle glaucoma?
As open-angle glaucoma progresses, you may notice:
- Gradual loss of peripheral vision, usually in both eyes
- Tunnel vision in the advanced stages
What are the symptoms of angle-closure glaucoma?
Acute angle-closure glaucoma can present with sudden symptoms, including:
- Severe eye pain
- Nausea and vomiting
- Sudden blurry vision
- Halos around lights
- Red eyes
If you experience these symptoms, seek immediate medical attention as they constitute a medical emergency.
Risk Factors: Who is Most Likely to Develop Glaucoma?
While glaucoma can affect anyone, certain factors increase the risk of developing the condition:
- Age: People over 60 are at higher risk, especially for open-angle glaucoma
- Race: African Americans have a higher risk of glaucoma, and it tends to occur earlier and progress faster
- Family history: Having a family history of glaucoma increases your risk
- Medical conditions: Diabetes, high blood pressure, and heart disease may increase the risk of developing glaucoma
- Eye injuries or certain types of eye surgery
- Long-term use of corticosteroid medications, especially eye drops
Can lifestyle factors influence glaucoma risk?
While some risk factors are beyond our control, certain lifestyle choices may influence glaucoma risk:

- Regular exercise may help reduce eye pressure
- A healthy diet rich in vitamins and minerals may support overall eye health
- Avoiding smoking, which can increase eye pressure
Diagnosing Glaucoma: Tests and Procedures
Early detection of glaucoma is crucial for preventing vision loss. Regular eye exams are essential, especially if you’re at higher risk. During a comprehensive eye exam for glaucoma, your eye doctor may perform several tests:
What tests are used to diagnose glaucoma?
- Tonometry: Measures intraocular pressure
- Ophthalmoscopy: Examines the shape and color of the optic nerve
- Perimetry: Tests peripheral vision
- Gonioscopy: Inspects the drainage angle of the eye
- Pachymetry: Measures the thickness of the cornea
These tests help eye doctors detect glaucoma before significant damage occurs. If glaucoma is suspected, additional tests may be performed to confirm the diagnosis and determine the extent of the condition.
Treatment Options: Managing Glaucoma Effectively
While damage from glaucoma can’t be reversed, treatment can help slow or prevent further vision loss. The goal of glaucoma treatment is to lower intraocular pressure. Depending on the situation, treatment options may include:

What are the main treatment approaches for glaucoma?
- Prescription eye drops: These are usually the first line of treatment. They work by either reducing the production of aqueous humor or increasing its outflow.
- Oral medications: If eye drops alone don’t bring eye pressure down to the desired level, oral medications may be prescribed.
- Laser therapy: Procedures such as laser trabeculoplasty can help increase fluid drainage from the eye.
- Surgery: For cases that don’t respond to other treatments, various surgical procedures can help create new drainage channels.
The choice of treatment depends on several factors, including the type and severity of glaucoma, age, and overall health. Your eye doctor will work with you to determine the best treatment plan.
Living with Glaucoma: Coping Strategies and Lifestyle Adjustments
A diagnosis of glaucoma can be challenging, but with proper management and support, many people with glaucoma lead full and active lives. Here are some strategies for living well with glaucoma:

How can individuals cope with glaucoma in daily life?
- Adhere to your treatment plan: Take medications as prescribed and attend all follow-up appointments
- Protect your eyes: Wear protective eyewear during sports or while working with power tools
- Maintain a healthy lifestyle: Regular exercise and a balanced diet can support overall eye health
- Use visual aids: If you’ve experienced vision loss, various devices and technologies can help you maintain independence
- Seek support: Join a support group or connect with others who have glaucoma
Remember, while glaucoma is a chronic condition, it’s manageable with proper care and treatment. Regular check-ups and open communication with your eye care team are essential for maintaining your vision and quality of life.
Prevention and Early Detection: Safeguarding Your Vision
While not all cases of glaucoma can be prevented, there are steps you can take to protect your vision and detect problems early:
How can you reduce your risk of glaucoma?
- Regular eye exams: The frequency depends on your age and risk factors. Generally, it’s recommended to have a comprehensive eye exam:
- Under 40: Every 2-4 years
- 40-54: Every 1-3 years
- 55-64: Every 1-2 years
- 65 and older: Every 6-12 months
- Know your family history: If glaucoma runs in your family, you may need more frequent screenings
- Exercise regularly: Moderate exercise may help lower intraocular pressure
- Wear eye protection: Prevent eye injuries that could lead to secondary glaucoma
- Manage chronic health conditions: Keep conditions like diabetes and high blood pressure under control
Early detection is key in managing glaucoma effectively. By taking proactive steps and working closely with your eye care professional, you can protect your vision and maintain your quality of life.

Advances in Glaucoma Research: Hope for the Future
The field of glaucoma research is dynamic and rapidly evolving. Scientists and medical professionals are continually working to improve our understanding of the disease and develop new treatments.
What are some promising areas of glaucoma research?
- Neuroprotection: Researchers are exploring ways to protect and even regenerate damaged optic nerve cells
- Gene therapy: Identifying genetic factors that contribute to glaucoma could lead to new targeted treatments
- Improved drug delivery: New methods of delivering medications, such as slow-release implants, could improve treatment efficacy
- Artificial intelligence: AI is being used to improve early detection and predict disease progression
- Stem cell therapy: This could potentially replace damaged cells in the eye
These advancements offer hope for better treatments and potentially even a cure for glaucoma in the future. However, it’s important to remember that research takes time, and many of these approaches are still in early stages.
How can patients stay informed about new developments?
To stay up-to-date on the latest in glaucoma research and treatment:
- Discuss new developments with your eye care professional during regular check-ups
- Follow reputable eye health organizations online
- Consider participating in clinical trials if appropriate
By staying informed and working closely with your healthcare team, you can ensure you’re receiving the most current and effective care for your glaucoma.
Common Eye Disorders and Diseases
- More than 4.2 million Americans aged 40 years and older are either legally blind (having best-corrected visual acuity of 6/60 or worse (=20/200) in the better-seeing eye) or are with low vision (having best-corrected visual acuity less than 6/12 (<20/40) in the better-seeing eye, excluding those who were categorized as being blind).
- The leading causes of blindness and low vision in the United States are primarily age-related eye diseases such as age-related macular degeneration, cataract, diabetic retinopathy, and glaucoma. Other common eye disorders include amblyopia and strabismus.
Click here to see the anatomy the eye and how the eyes work.external icon
Refractive Errors
Refractive errors are the most frequent eye problems in the United States. Refractive errors include myopia (near-sightedness), hyperopia (farsightedness), astigmatism (distorted vision at all distances), and presbyopia that occurs between age 40–50 years (loss of the ability to focus up close, inability to read letters of the phone book, need to hold newspaper farther away to see clearly) can be corrected by eyeglasses, contact lenses, or in some cases surgery. The National Eye Institute states that proper refractive correction could improve vision among 150 million Americans.
Learn more about refractive errors.external icon
Age-Related Macular Degeneration
Macular degeneration, often called age-related macular degeneration (AMD), is an eye disorder associated with aging and results in damaging sharp and central vision. Central vision is needed for seeing objects clearly and for common daily tasks such as reading and driving. AMD affects the macula, the central part the retina that allows the eye to see fine details. There are two forms of AMD—wet and dry.
Wet AMD is when abnormal blood vessel behind the retina start to grow under the macula, ultimately leading to blood and fluid leakage. Bleeding, leaking, and scarring from these blood vessels cause damage and lead to rapid central vision loss. An early symptom of wet AMD is that straight lines appear wavy.
Dry AMD is when the macula thins overtime as part of aging process, gradually blurring central vision. The dry form is more common and accounts for 70–90% of cases of AMD and it progresses more slowly than the wet form. Over time, as less of the macula functions, central vision is gradually lost in the affected eye. Dry AMD generally affects both eyes. One of the most common early signs of dry AMD is drusen.
Drusen are tiny yellow or white deposits under the retina. They often are found in people aged 60 years and older. The presence of small drusen is normal and does not cause vision loss. However, the presence of large and more numerous drusen raises the risk of developing advanced dry AMD or wet AMD.
It is estimated that 1.8 million Americans aged 40 years and older are affected by AMD and an additional 7.3 million with large drusen are at substantial risk of developing AMD. The number of people with AMD is estimated to reach 2.95 million in 2020. AMD is the leading cause of permanent impairment of reading and fine or close-up vision among people aged 65 years and older.
Learn more about age-related macular degeneration.external icon
Cataract
Cataract is a clouding of the eye’s lens and is the leading cause of blindness worldwide, and the leading cause of vision loss in the United States. Cataracts can occur at any age because of a variety of causes, and can be present at birth. Although treatment for the removal of cataract is widely available, access barriers such as insurance coverage, treatment costs, patient choice, or lack of awareness prevent many people from receiving the proper treatment.
An estimated 20.5 million (17.2%) Americans aged 40 years and older have cataract in one or both eyes, and 6.1 million (5.1%) have had their lens removed operatively. The total number of people who have cataracts is estimated to increase to 30.1 million by 2020.
Learn more about cataractsexternal icon.
Diabetic Retinopathy
Diabetic retinopathy (DR) is a common complication of diabetes. It is the leading cause of blindness in American adults. It is characterized by progressive damage to the blood vessels of the retina, the light-sensitive tissue at the back of the eye that is necessary for good vision. DR progresses through four stages, mild nonproliferative retinopathy (microaneurysms), moderate nonproliferative retinopathy (blockage in some retinal vessels), severe nonproliferative retinopathy (more vessels are blocked leading to deprived retina from blood supply leading to growing new blood vessels), and proliferative retinopathy (most advanced stage). Diabetic retinopathy usually affects both eyes.
The risks of DR are reduced through disease management that includes good control of blood sugar, blood pressure, and lipid abnormalities. Early diagnosis of DR and timely treatment reduce the risk of vision loss; however, as many as 50% of patients are not getting their eyes examined or are diagnosed too late for treatment to be effective.
It is the leading cause of blindness among U.S. working-aged adults aged 20–74 years. An estimated 4.1 million and 899,000 Americans are affected by retinopathy and vision-threatening retinopathy, respectively.
Learn more about diabetic retinopathy.external icon
Top of Page
Glaucoma
Glaucoma is a group of diseases that can damage the eye’s optic nerve and result in vision loss and blindness. Glaucoma occurs when the normal fluid pressure inside the eyes slowly rises. However, recent findings now show that glaucoma can occur with normal eye pressure. With early treatment, you can often protect your eyes against serious vision loss.
There are two major categories “open angle” and “closed angle” glaucoma. Open angle, is a chronic condition that progress slowly over long period of time without the person noticing vision loss until the disease is very advanced, that is why it is called “sneak thief of sight.” Angle closure can appear suddenly and is painful. Visual loss can progress quickly; however, the pain and discomfort lead patients to seek medical attention before permanent damage occurs.
Learn more about glaucomaexternal icon.
Amblyopia
Amblyopia, also referred to as “lazy eye,” is the most common cause of vision impairment in children. Amblyopia is the medical term used when the vision in one of the eyes is reduced because the eye and the brain are not working together properly. The eye itself looks normal, but it is not being used normally because the brain is favoring the other eye. Conditions leading to amblyopia include strabismus, an imbalance in the positioning of the two eyes; more nearsighted, farsighted, or astigmatic in one eye than the other eye, and rarely other eye conditions such as cataract.
Unless it is successfully treated in early childhood amblyopia usually persists into adulthood, and is the most common cause of permanent one-eye vision impairment among children and young and middle-aged adults. An estimated 2%–3% of the population suffer from amblyopia.
Learn more about amblyopiaexternal icon.
Strabismus
Strabismus involves an imbalance in the positioning of the two eyes. Strabismus can cause the eyes to cross in (esotropia) or turn out (exotropia). Strabismus is caused by a lack of coordination between the eyes. As a result, the eyes look in different directions and do not focus simultaneously on a single point. In most cases of strabismus in children, the cause is unknown. In more than half of these cases, the problem is present at or shortly after birth (congenital strabismus). When the two eyes fail to focus on the same image, there is reduced or absent depth perception and the brain may learn to ignore the input from one eye, causing permanent vision loss in that eye (one type of amblyopia).
Learn more about strabismusexternal icon.
Top of Page
Eye Diseases and Eye Disorders – Symptoms and possible treatments for common eye diseases and disorders : Bausch + Lomb
Many eye diseases have no early symptoms. They may be painless, and you may see no change in your vision until the disease has become quite advanced.
The single best way to protect your vision is through regular professional eye examinations. Of course, between examinations, if you notice a change in your vision – or you think your eye may be injured in any way – contact your eye care professional immediately.
Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is the physical disturbance of the center of the retina called the macula.
Bulging Eyes
Bulging eyes, or proptosis, occurs when one or both eyes protrude from the eye sockets due to space taking lesions such as swelling of the muscles, fat, and tissue behind the eye.
Cataracts
Cataracts are a degenerative form of eye disease in which the lens gradually becomes opaque and vision mists over.
Cataracts in Babies
In rare cases, children develop cataracts in the first few years of their lives.
CMV Retinitis
CMV Retinitis is a serious infection of the retina that often affects people with AIDS (Acquired Immune Deficiency Syndrome) and that may also affect people with other immune disorders.
Color Blindness
Color blindness is not actually blindness in the true sense but rather is a color vision deficiency—people who are affected by it simply do not agree with most other people about color matching.
Crossed Eyes (Strabismus)
Crossed eyes (or strabismus) occur when a person’s eyes are not able to align on the same point at the same time, and appear to be misaligned or pointed in different directions.
Diabetic Macular Edema
Diabetic Macular Edema, DME, is caused by fluid accumulation in the macula. Patients with DME typically experience blurred vision which can be severe.
Eye Floaters and Eye Flashes
Floaters are small specks or clouds that move across your field of vision—especially when you are looking at a bright, plain background, like a blank wall or a cloudless blue sky.
Glaucoma
Glaucoma occurs when a build-up of fluid in the eye creates pressure, damaging the optic nerve.
Keratoconus
When the cornea in the front of the eye, which normally is round, becomes thin and cone shaped.
Lazy Eye
Commonly known as lazy eye, amblyopia is poor vision in an eye that does not receive adequate use during early childhood.
Low Vision
Whenever ordinary glasses or contact lenses don’t produce clear vision, you are considered to have low vision.
Ocular Hypertension
Ocular hypertension is an increase in pressure in the eye that is above the range considered normal.
Retinal Detachment
When the retina detaches, light sensitive membrane in the back of the eye becomes separated from the nerve tissue and blood supply underneath it.
Eyelid Twitching
Sometimes your eyelid simply twitches.
Uveitis
Uveitis is the inflammation of the inside the eye, specifically affecting one or more of the three parts of the eye that make up the uvea.
Eye Problems – Symptoms A to Z
By Gina White; reviewed by Charles Slonim, MD
Is something wrong with your eyes? Find symptoms in the list below, then look to the right for associated eye problems and diseases. To learn more, click on the eye problem or disease for a pop-up window with a definition and links.
Please note: The information on this page is not intended as a diagnosis of your problem, but rather as a helpful guide. Please see your eye doctor for diagnosis and treatment if you suspect you have an eye or vision problem.
A, B
Symptom
Possible Eye Problem or Disease
Absence of eye or eyes
anophthalmos
–
Blinking, frequent
blepharospasm, contact lens problem, dry eye syndrome, foreign body, hemifacial spasm, stroke
–
Blinking, infrequent
cranial nerve palsy, Parkinson’s disease
Bloodshot eye (See: red or pink eye)
–
Blurred vision, distance (See also: blurred vision, general myopia)
–
Blurred vision, general
accommodative disorder, albinism, amblyopia, aniridia, asteroid hyalosis, astigmatism, cataract, central serous retinopathy, computer vision syndrome, contact lens problem, corneal abrasion, corneal dystrophy, corneal erosion, cranial nerve palsy, drugs, epiretinal membrane, eye tumor, foreign body, fungal keratitis eye infection, glaucoma, hypotony, keratoconus, lens dislocation, macular degeneration, meibomianitis, migraine, neuroretinitis, nystagmus, ophthalmoplegia, optic nerve problem, orbital cellulitis, photokeratitis, pterygium, retinal detachment, retinitis, retinoschisis, scleritis, surgery,trauma, uveitis, vascular problem, vitreous hemorrhage, white dot syndrome
–
Blurred vision, near
diabetic retinopathy, hyperopia, presbyopia. See also: blurred vision, general
Bulging eye
cavernous sinus problem, eye tumor, glaucoma, Graves’ ophthalmology, histiocytosis, mucormycosis, optic nerve problem, orbital cellulitis, orbital pseudotumor, trauma,vascular problem. See also: small eye
–
Bump on eye (any color)
papilloma, pinguecula, pterygium
–
Bump on eyelid (any color)
chalazion, milia, nevus, eyelid papilloma, skin cancer, sty, xanthelasma
–
Burning
blepharitis, blepharoconjunctivitis, computer vision syndrome,conjunctivitis, contact lens problem, cranial nerve palsy, dry eye syndrome, environmental condition, meibomianitis, rheumatoid arthritis, Sjogren’s syndrome, trauma. See also: eye pain or discomfort
C, D
Symptom
Possible Eye Problem or Disease
Close appearance of
object that is actually farther away
metamorphopsia
–
Cloud shape in vision
See: floater in vision
–
Clouding of the eye’s surface
fungal keratitis eye infection
–
Clump shape in vision
See: floater in vision
–
Color vision problem
cataract, color blindness, drugs, neuroretinitis, optic nerve problem, white dot syndrome
–
Crossed eyes
cranial nerve palsy, strabismus
Crusty eyelid
blepharitis
–
Depth perception problem
anophthalmos, blurred vision (in one eye), cranial nerve palsy, strabismus
–
Differing prescriptions in eyes
anisometropia
–
Discharge
canaliculitis, conjunctivitis, contact lens problem, dacryocystitis, dacryostenosis, foreign body, fungal keratitis eye infection, overflow tearing, rheumatoid arthritis, Sjogren’s syndrome
–
Distorted vision
astigmatism, keratoconus, macular degeneration,metamorphopsia, migraine, ocular migraine
–
Double vision (diplopia)
accommodative disorder, astigmatism, cranial nerve palsy, diabetic retinopathy, eye tumor (orbital), Graves’ ophthalmology, keratoconus, lens dislocation, myasthenia gravis, ophthalmoplegia, pseudotumor cerebri, stroke, trauma,vascular problem, vergence disorder. See also: shadow on letters
–
Droopy eyelid
blepharochalasis, dermatochalasis, ptosis
–
Dry eyelid
blepharitis, dry skin
–
Dry eyes
blepharitis, blepharoconjunctivitis, computer vision syndrome,conjunctivitis, cranial nerve palsy, dacryoadenitis, drugs, dry eye syndrome, environmental condition, meibomianitis, rheumatoid arthritis, sarcoidosis, Sjogren’s syndrome, trauma
–
E, F, G
Symptom
Possible Eye Problem or Disease
Eyelash loss
madarosis, trichotillomania
–
Eyelash particles, atypical
blepharitis, pediculosis
–
Eyelid cleft
coloboma, trauma
–
Eyelid turns in
entropion
–
Eyelid turns out
ectropion
–
Eyes are different colors
heterochromia
–
Eyes don’t point in same direction
cranial nerve palsy, strabismus
–
Eye strain
accommodative disorder, astigmatism, computer vision syndrome, convergence insufficiency, divergence insufficiency, hyperopia, myopia, presbyopia
–
Far appearance of object that is actually closer
metamorphopsia
–
Floater in vision
floater
–
Foreign body sensation (feels like something is in the eye)
band keratopathy, blepharitis, contact lens problem, corneal abrasion, corneal dystrophy, corneal edema, corneal erosion, dry eye syndrome, entropion, eye tumor, foreign body (corneal or conjunctival), keratitis, pterygium (inflamed), Sjogren’s syndrome, surgery, sty, trauma. See also: eye pain or discomfort
–
Glare
See: light sensitivity
–
Grittiness
blepharitis, corneal abrasion, dry eye syndrome, keratitis (including radiation (UV) keratitis)
–
H, I, J, K, L
Symptom
Possible Eye Problem or Disease
Halos around lights
cataract, corneal edema, corneal opacity, drugs, glaucoma,migraine, ocular migraine
–
Iris defect
aniridia, coloboma, eye tumor (iris), surgery, trauma
–
Itchy eyes
allergy, conjunctivitis, contact lens problem, dry eye syndrome, entropion, pterygium (inflamed), Sjogren’s syndrome
–
Large appearance of objects that are actually smaller
metamorphopsia
–
Lazy eye
amblyopia
–
Lesions on the surface of the eye
fungal keratitis eye infection
–
Light flashes
migraine, ocular migraine, retinal detachment, retinal tear, vitreous detachment
–
Light sensitivity
fungal keratitis eye infection, photophobia
–
Lights, halos around
See: halos
–
M, N, O, P, Q
Symptom
Possible Eye Problem or Disease
Movement of eyelid, limited ability
cranial nerve palsy, eye tumor (orbital), trauma (orbital fracture)
–
Movement of eyes, involuntary
nystagmus, opsoclonus
–
Movement of eyes, limited ability
cranial nerve palsy, eye tumor (orbital), Graves’ ophthalmology, ophthalmoplegia, Parinaud dorsal midbrain syndrome, stroke, trauma
–
Night vision problem
myopia, retinitis pigmentosa
–
Pain or discomfort around eyes
blepharoconjunctivitis, eye tumor (orbital), orbital pseudotumor (inflammatory), sinusitis, trauma
–
Pain or discomfort in eye
blepharitis, blepharoconjunctivitis, chalazion, conjunctivitis, contact lens problem, corneal abrasion, corneal dystrophy, corneal edema, corneal erosion, corneal ulcer, dacryocystitis,dry eye syndrome, ectropion, endophthalmitis, entropion, episcleritis, eye tumor, foreign body, fungal keratitis eye infection, glaucoma, Graves’ ophthalmology, hypotony, keratitis,migraine, mucormycosis, neuroretinitis, ophthalmoplegia, optic nerve problem, orbital cellulitis, photokeratitis, scleritis, sinusitis, sty, surgery, trauma, uveitis, vascular problem. See also: burning, foreign body sensation
–
Pain or discomfort, eyelid
blepharitis, chalazion, ectropion, entropion, eye tumor (lid), orbital cellulitis, sty
–
Peripheral vision problem
anophthalmos. See also: vision loss, peripheral
–
Pupil, large (dilated)
cranial nerve palsy, drugs, trauma
–
Pupil, small
Argyll Robertson pupil, drugs, Horner’s syndrome
–
Pupils, different sized
anisocoria. See also: pupil, large and pupil, small
–
Pupil unresponsiveness to light
Argyll Robertson pupil, cranial nerve palsy, drugs, glaucoma, optic nerve problem, Parinaud dorsal midbrain syndrome, tonic pupil, trauma, uveitis
–
Pupil, white
See: spot on eye, white or cloudy
R, S
Symptom
Possible Eye Problem or Disease
Red or pink eye
allergy, blepharoconjunctivitis, canaliculitis, cavernous sinus problem, computer vision syndrome, conjunctivitis, contact lens problem, corneal abrasion, corneal ulcer, dacryocystitis, dry eye syndrome, ectropion, endophthalmitis, entropion, episcleritis, eye tumor, foreign body, fungal keratitis eye infection, glaucoma, Graves’ ophthalmology, meibomianitis, pterygium, scleritis, subconjunctival hemorrhage, surgery, uveitis, vascular problem
–
Red or pink eyelid
blepharitis, blepharoconjunctivitis, contact lens problem, dacryoadenitis, ectropion, lupus erythematosus, meibomianitis,orbital cellulitis, stye, vascular birthmark. See also: spot on eyelid, colored
–
Shadow in vision
macular degeneration, retinal detachment. See also: floater in vision
–
Shadow on letters
astigmatism, macular degeneration. See also: double vision
–
Small appearance of objects that are actually larger
metamorphopsia
–
Small eye
enophthalmos, microphthalmia, ptosis. See also: bulging eye
–
Spasm
See: eye twitching
–
Speck in vision
See: floater in vision
–
Spot in vision
cataract. See also: floater in vision, vision loss
–
Spot on eye, brown
melanosis, nevus, skin cancer
–
Spot on eye, red or pink
See: red or pink eye
–
Spot on eye, white or cloudy
cataract, corneal edema, corneal opacity, corneal ulcer, eye tumor (intraocular), leukocoria, pinguecula, pterygium. See also: white ring/bow around iris
–
Spot on eye, yellow
pinguecula. See also: yellow eyes
–
Spot on eyelid, colored
eye tumor, liver spot, lupus erythematosus, melanosis, nevus, papilloma, pediculosis, skin cancer, xanthelasma. See also: red or pink eyelid
–
Squiggle in vision
metamorphopsia. See also: floater in vision
–
Squinting
accommodation disorder, amblyopia, hyperopia, myopia,photophobia, presbyopia, uveitis, vergence disorder. See also: light sensitivity
–
Sticky eyes
allergy, blepharitis, blepharoconjunctivitis, conjunctivitis,dacryocystitis, dacryostenosis
–
Straight lines appear wavy, curved or bent
metamorphopsia
–
Strand shape in vision
See: floater in vision
–
Swelling, around eyes
dacryoadenitis, dacryocystitis, eye tumor, orbital cellulitis, sinusitis, trauma
–
Swelling, eye
chemosis, fungal keratitis eye infection, trauma
–
Swelling, eyelid
allergy, blepharitis, canaliculitis, chalazion, contact lens problem, dacryoadenitis, eye tumor, meibomianitis, orbital cellulitis, sinusitis, sty, trauma, vascular problem
–
T, U, V
Symptom
Possible Eye Problem or Disease
Tearing
allergy, blepharitis, blepharoconjunctivitis, chalazion, conjunctivitis, corneal abrasion, corneal dystrophy, corneal ulcer, cranial nerve palsy, dacryocystitis, dacryostenosis, dry eye syndrome, entropion, environmental condition, episcleritis, foreign body, fungal keratitis eye infection, keratitis, overflow tearing, scleritis, sty, trauma, uveitis
–
Tired eyes
See: eye strain
–
Tunnel vision
See: vision loss, peripheral
–
Twitching (tic)
blepharospasm, hemifacial spasm, myokymia
–
Vision improvement, temporary
cataract
–
Vision loss, central
central serous retinopathy, choroidal neovascularization,epiretinal membrane, macular degeneration, macular hole, migraine, neuroretinitis, optic nerve problem, vascular problem, white dot syndrome
–
Vision loss, general
albinism, amblyopia, band keratopathy, cavernous sinus problem, corneal dystrophy, corneal edema, corneal opacity,cranial nerve palsy, diabetic retinopathy, drugs, endophthalmitis, entropion, eye tumor, foreign body, fungal keratitis eye infection, Graves’ ophthalmology, lead poisoning, Leber’s congenital amaurosis, lens dislocation, migraine,mucormycosis, neuroretinitis, optic nerve problem, orbital cellulitis, Patau syndrome, photokeratitis, pseudotumor cerebri, retinal detachment, retinitis, stroke, surgery, Tay-Sachs disease, toxocariasis, trauma, vascular problem, vitreous hemorrhage, white dot syndrome
–
Vision loss, peripheral
drugs, glaucoma, migraine, ocular migraine, optic nerve problem, retinitis, retinitis pigmentosa
W, X, Y, Z
Symptom
Possible Eye Problem or Disease
Wall-eyed (eye turned towards ear)
cranial nerve palsy, strabismus
–
Watering eyes
See: tearing
–
Wavy lines in vision
metamorphopsia, migraine, ocular migraine. See also: floater in vision
–
White ring around iris
arcus
–
White spot on eye
See: spot on eye, white or cloudy
–
Yellow eyes
jaundice
–
Yellow spot on eye
See: spot on eye, yellow
–
Zigzag in vision
See: floater in vision, wavy lines in vision
Page published in January 2019
Page updated in October 2021
Most Common Eye Problems – Signs, Symptoms & Treatment
4: Diabetic Retinopathy
Diabetic retinopathy is basically a diabetes complication, which affects eyes by causing damage to the blood vessels spread throughout the light sensitive tissues of the retina (the back of the eye).
Anyone having type 1 or type 2 diabetes can develop this eye condition, especially those who have diabetes for a long time with fluctuating blood sugar levels. Usually, both eyes get affected by diabetic retinopathy.
Signs and Symptoms of Diabetic Retinopathy
There might not be any noticeable symptoms through the early stages of this eye condition. When it progresses to later stages, following symptoms might appear eventually:
- Dark spots or strings floating through your vision (floaters)
- Impaired color recognition
- Fluctuating vision
- Blurred vision
- Vision loss
Treatment Options
There is no reliable way to cure retinopathy once it has progressed to advanced stages. However, photocoagulation (laser treatment for retinopathy) comes really handy in preventing vision loss if chosen before retina being severely damaged.
Another treatment option for diabetic retinopathy in its earlier stages is vitrectomy, a process through which vitreous gel is surgically removed while retina has not been severely damaged.
5: Dry Eyes Syndrome
One of the functions of tears is to keep your eyes lubricated, and when they fail to provide adequate lubrication for the eyes, you are being affected by dry eye syndrome. From your body being unable to produce enough tears to production of low quality tears, there can be a host of reasons behind inadequate lubrication for your eyes.
You can experience stinging or burning sensation when you have dry eyes, which can be experienced under certain situations, such as in an air-conditioned room, while traveling on an airplane or looking at a computer screen for a long time without any breaks.
Signs and Symptoms of Dry Eyes Syndrome
- A burning, scratchy or stinging sensation in eyes
- Eye redness
- Sensitivity to light
- Mucus production in or around the eyes
- Blurred vision
- Eye fatigue
- Issues in wearing contact lenses
Treatment Options
Different treatment options can be used for dry eyes syndrome depending upon the reason behind the eye problem. Some most commonly used treatment options include:
- OTC (Over-the-counter) topical medications: These can be used when your dry eyes syndrome is mild in nature. Artificial tears, gels and ointments can be some of the commonly used OTC medications to treat mild dry eyes.
- Prescription Medications: FDA approves only ‘Lifitegrast’ and ‘Cyclosporine’ as prescription dry eye medications. To deal with eye inflammation, ‘Corticosteroid’ eye drops may also be prescribed as short-term treatment.
- Devices: There are also some FDA-approve devices that serve to temporarily relieve you from dry eyes by stimulation of nerves and glands responsible for tear production.
- Surgical Options: Your eye care professional may resort to insertion of silicone-based punctal plugs to partially or completely plug tear ducts through the inner corners of your eyes to ensure tears aren’t draining from the eye.
- Lifestyle Changes: Lifestyle based enhancements also prove helpful in dealing with dry eyes syndrome. Taking periodic breaks or cutting your screen exposure can be really helpful. Avoiding warmer temperatures also helps in doing so.
6: Conjunctivitis (Pinkeye)
Conjunctivitis, also known to many as pinkeye is a condition that inflames the tissues lining the back of your eyelids and covering your sclera (conjunctiva). As a result of this, your eyes can turn itchy, red, blurry, teary and discharging, sometimes also giving you a feeling that something is in your eyes. It is also one of the most commonly prevailing eye problems.
Though it is highly contagious (readily affecting children), but rarely serious, quite unlikely to damage your vision, more so when identified and treated early.
Types of Conjunctivitis
Conjunctivitis is categorized into three main types:
1: Allergic Conjunctivitis
- Allergic Conjunctivitis: Mostly affects people already suffering from seasonal allergies, when they contact with something that triggers an allergic reaction within their eyes.
- Giant Papillary Conjunctivitis: Caused due to long term presence of a foreign body in an eye, affecting people wearing hard or rigid contact lenses or the soft ones not being replaced frequently.
2. Infectious Conjunctivitis
- Bacterial Conjunctivitis: This is the type of eye infection caused mostly by streptococcal or staphylococcal bacteria that’s transferred to your eyes via your own respiratory system or skin.
- Viral Conjunctivitis: Contagious viruses thriving in common cold are mostly responsible for spread of this type of conjunctivitis, thus affecting people by exposure to the sneezing or coughing of someone suffering from an upper respiratory tract infection.
- Ophthalmia Neonatorum: One of the most severe forms of bacterial conjunctivitis specifically affecting newborn babies, also capable of causing permanent eye damage if not treated immediately.
3: Chemical Conjunctivitis
This spreads as a result of exposure to noxious chemicals, chlorine in swimming pools or even air pollution.
Signs and Symptoms of Conjunctivitis
- Redness appearing in the eyelid or through the white of the eye
- Swelling in the conjunctiva
- Excessive tearing
- Thick yellowish discharge, mostly covering whole eyelashes, especially after sleep
- Itching and burning eyes
- Blurred vision
- Extra sensitivity to light
Treatment Options
Appropriate treatment options for conjunctivitis vary depending upon the cause of this eye condition.
- Allergic Conjunctivitis: It must start with avoiding exposure to the irritant(s). Artificial tears and cool compresses suffice in case of mild intensity of the disease. Antihistamines or non-steroidal anti-inflammatory drugs may be prescribed in case of severe allergic conjunctivitis. And for people with persistent allergic conjunctivitis, topical steroid eye drops may be the appropriate option.
- Bacterial Conjunctivitis: Antibiotic eye drops or ointments work well for this type of conjunctivitis, mostly requiring 3 to 4 days of treatment for reasonable recovery. However, it’s highly recommended that patients complete the entire course of antibiotics to totally avoid recurrence.
- Viral Conjunctivitis: Viral conjunctivitis cannot be treated with drops, ointments or some antibiotics until the virus runs its course like common cold. This may take up to about 2-3 weeks.
- Chemical Conjunctivitis: The standard treatment for chemical conjunctivitis includes thorough flushing of the eyes using saline water. In some cases, people might need to go for topical steroids.
7: Retinal Detachment
When the retina is separated or detached from its underlying tissues holding it in its place within the eye, the instance is referred as the retinal detachment. Sometimes, it all begins with small areas of the retina being torn (attributed as retinal tears or retinal breaks), eventually leading to retinal detachment. The longer you take in treatment of retinal detachment, the greater your chances of total vision loss in the affected eye are.
Types of Retinal Detachment
Retinal detachment is segregated into three basic types:
- Rhegmatogenous: These are the most common of all retinal detachments whereby a small break or tear appears within the retina, resulting in flow of the fluid underneath the retina, eventually separating it from the retinal pigment epithelium (RPE), which is pigmented cell layer responsible for nourishment of the retina.
- Tractional: In this type, the retina detaches due to the contraction of the scar tissue on surface of retina, resulting in its separation from the PRE. Tractional detachment is not so common.
- Exudative: This sort of detachment takes place due to eye injury/trauma, inflammatory disorders and other such retinal diseases. In exudative detachments, the retina suffers no tears or breaks despite the fluid leaking underneath it.
Signs and Symptoms of Retinal Detachment
Though you don’t suffer any pain through the retinal detachment, but it is almost always followed by certain warning signs, such as:
- Sudden appearance of floaters (tiny specks drifting through your field of vision) in the affected eye
- Sudden appearance of light flashes in one or both eyes
- Blurred vision
- Steadily receding peripheral or side vision
- Presence of a curtain-like shadow through your field of vision
Treatment Options
Cryopexy (a freeze treatment) or laser surgery is used by an ophthalmologist to treat small holes and tears. Tiny burns are made around the damaged area to “weld” the retina back into place, whereas “cryopexy” is used to freeze the area around the weld, helping reattach the retina.
Vitrectomy may also be performed in some cases, during which a tiny incision is made in the white of the eye (the sclera). Sometimes, it also involves removing vitreous (a gel-like substance filled in the center of the eye) by means of a specialized instrument, and injecting gas into the eye to push retina back to its appropriate position.
8: Uveitis
This is the name collectively given to a group of eye diseases causing inflammation in the uvea, eye’s middle layer containing the most blood vessels. Uveitis may also result in destruction of eye tissue, leading to the loss of eye in some cases.
Signs and Symptoms of Uveitis
The symptoms of uveitis may vanish quickly or last a long time. People affected with AIDS, rheumatoid arthritis, ulcerative colitis and other such immune system conditions are highly likely to suffer from uveitis. Some major symptoms include:
- Blurred vision
- Pain in the eye
- Light sensitivity
- Redness of the eye
Types of Uveitis
Uveitis is mostly described by the part of the eye it affects.
- Anterior Uveitis: Affecting the front of the eyes, this is the most widely existing type of uveitis found commonly in young and middle-aged people.
- Intermediate Uveitis: Commonly found in young adults, intermediate uveitis often hits the virteous. It is also linked to a host of disorders like sarcoidosis and multiple sclerosis.
- Posterior Uveitis: Least common of all, posterior uveitis primarily affects the back of the eye, mostly involving the retina as well as the choroid. That is why it is also referred sometimes as choroditis or chorioretinitis.
- Pan-Uveitis: This refers to the instance when inflammation occurs in all three major parts of the eye. One of the most famed forms of pan-uveitis is the Behcet’s disease, severely damaging the retina.
Treatment Options
Uveitis treatment is dependent on the underlying cause and the area of the eye that’s affected, reducing nflammation in your eye being the primary objective here. Several treatment options are available:
1: Medications
- Inflammation Reducing Drugs: Your eye doctor may resort to some anti-inflammatory medication based eye drops, such as corticosteroid. If it is unable to resolve the issue, a corticosteroid pill or injection can be the next options.
- Bacteria/Virus Fighting Drugs: if some sort of infection is the underlying cause of your uveitis, your ophthalmologist can prescribe antibiotics or antiviral medications to control the infection, with or without corticosteroids.
- Immunosuppressive Drugs: Immunosuppressive and cytotoxic drugs are used to treat uveitis if it has affected both eyes, because at this stage, it doesn’t respond well to corticosteroids and can potentially threaten your vision.2: Surgical and Other Options.
2: Surgical and Other Options
- Vitrectomy: A surgical procedure used for removal of excessive vitreous in your eye can be the only way out in some cases.
- Device Implanting Eye Surgery for Slow and Sustained Medication: Posterior uveitis, which is very difficult to treat otherwise, may be treated by implanting a device in eye. The device is introduced in the eye for slowly releasing corticosteroid medications for about two to three years.
Recurrence is also a possibility with uveitis. Consult your eye doctor immediately in case of experiencing any of the associated symptoms.
9: Eyestrain
Another of the most commonly existing eye problems, eyestrain refers to a common condition in which your eyes get tiresome and fatigued due to intense use; for instance, after looking at a computer screen (or other digital screens) for prolonged time period and driving long distances.
Eyestrain can be quite irritating sometimes, but still not capable of seriously inflicting your eyes or vision. It normally fades out after you rest your eyes and follow other ways to sooth your eyes.
Signs and Symptoms of Eyestrain
In some instances, signs and symptoms of eyestrain point out towards other underlying eye condition(s) needing treatment. Some common symptoms of eyestrain include:
- Soreness, tiredness, burning or itching in eyes
- Watery or dry eyes
- Headache
- Blurred or double vision
- High light sensitivity
- Difficulty in keeping your eyes open
Treatment Options
Some methods commonly used by eye doctors to treat eyestrain symptoms include:
- Taking frequent breaks from digital screens and reading activities.
- Improving your home environment, lifestyle and work habits, thus inculcating more breaks for your eyes.
- In case of dry eyes and blinking problem, your doctor might recommend artificial tears.
- Natural treatments like a yoga program, visual cleansing exercises and relaxation routines to lessen stress within your eyes and head.
10: Night Blindness (Nyctalopia)
‘Nyctalopia’ or night blindness is a kind of vision impairment in which people are unable to see rightly at night or in other dimly lit environments. Unlike commonly perceived, night blindness doesn’t totally prevent you from seeing at night. You might only feel increased difficulty in seeing or driving in places not adequately lit.
Night blindness is not considered to be a disease itself; it’s more like a symptom of some other eye problem like untreated nearsightedness.
Signs and Symptoms of Night Blindness
The only symptom associated with night blindness is increased difficulty seeing things in dark. It seems to be effecting more when your eyes undergo a transition from a properly lit environment to a lowly lit environment.
Similarly, you’ll have problems driving at night due to sporadic nature of vehicle’s headlights and streetlights on roads.
Treatment Options
Your eye doctor will be able to diagnose night blindness after thoroughly examining your eyes. Some types of blindness have got a treatment, while others don’t. Once your doctor has determined the underlying cause of your blindness, you can start taking appropriate treatment.
Night blindness caused due to cataracts, nearsightedness or vitamin A deficiency can be treated with corrective lenses like contacts or eyeglasses.
11: Color Blindness
Color blindness, also known as color deficiency is an eye condition when the pigments found in eye cones have some problem and you cannot see the colors in the normal manner.
Red-green colorblindness, the most common form of color blindness, is a type of vision impairment where a person is unable to differentiate between red and green colors.
Similarly, there is blue-yellow color blindness as well and people suffering from it almost always have red-green color blindness as well.
In rare cases, the cones lack any color pigments at all, so the eyes can’t see any color at all, the worst form of color blindness, also known as ‘achromatopsia’.
Color blindness is basically a genetic condition, which seems to be lenient with women than with men, affecting 1 out of every 10 men to some degree.
Signs and Symptoms of Color Blindness
- Trouble distinguishing between different colors
- Failure in seeing differing tones or shades of the same color
Treatment Options
Unfortunately, color blindness still lacks a reliable cure, though glasses and contact lenses with filters are available to assist color deficiencies whenever needed. Luckily, most color blind people enjoy normal vision in all aspects but one, and all they require is certain adaptation methods.
12: Eye Floaters
Strings, black/gray specks or cobwebs drifting around with the movement of your eyes and darting away when trying to look through them, eye floaters are basically spots in your vision.
These are mostly produced due to age-related changes taking place through the jelly-like substance (vitreous) within your eyes, turning into more and more liquid. This vitreous contains microscopic fibers, which tend to cast tiny shadows on your retina when vitreous clump away. These shadows are what floaters are all about.
Signs and Symptoms of Eye Floaters
Some common symptoms associated with eye floaters include:
- Appearance of dark specks or transparent strings floating around within your vision
- Movement of the spots in correspondence with the movement of your eyes, quickly moving out of your visual field when looked upon
- High visibility of the spots when looked at against a plain bright background like a white wall or blue sky
Treatment Options
Rarely, the density and frequency of floaters gets to the point that they start significantly affecting your vision, thus needing vitrectomy. This surgical procedure is used to remove the vitreous gel, also removing the floating debris contained within it and relieving your eye.
13: Nearsightedness (Myopia)
When you can view the objects close to you clearly enough, while getting a blurry vision of the objects far away, this eye condition is referred as myopia or nearsightedness. This happens because of irregular bending of light (refraction) due to the shape of your eye. The resultant images are focused in front of your retina rather than being focused right on it.
Near sightedness seems to be running in families, developing either gradually or rapidly, getting severe mostly during childhood and adolescence.
Signs and Symptoms of Nearsightedness
Major symptoms may include:
- Vision getting blurry when looking at distant objects
- Requiring squinting or partial closing of the eyelids to get a clear vision of something
- Eyestrain leading to headaches
- Difficulty viewing objects while driving a vehicle, particularly at night (night myopia)
Treatment Options
Different options are available as myopia treatment, such as corrective glasses, contact lenses or refractive surgery. You might need to wear your glasses all day long or just when you want to have a sharp distant vision (watching a movie, driving, etc.), depending upon the intensity of your myopia.
14: Farsightedness (Hypermetropia)
Unlike myopia, hypermetropia or farsightedness refers to an eye condition when you have a clear vision looking at far placed things, while getting a blurry vision of nearby objects.
If you feel tiredness in your eyes quite often, coupled with problems focusing on close by objects, you might be suffering from hypermetropia.
Signs and Symptoms of Farsightedness
- Vision getting blurry for objects close by
- Need to squint for getting a better vision
- Headache hitting after tasks needing your focus on close by objects
Treatment Options
Corrective glasses and contact lenses are some of the most common ways of treating hypermetropia. Other treatments like LASIK surgery is also advisable for adults suffering from mild to moderate levels of farsightedness.
15: Astigmatism
When your vision gets out of focus due to the abnormally curved cornea (the clear tissue lining the front of the eye), this eye disorder is referred as ‘astigmatism’ or ‘keratoconus’.
People having a family history of acute astigmatism are highly susceptible to this eye problem. Moreover, people using power tools without wearing safety glasses are also prone to the injuries resulting in acquired astigmatism.
Signs and Symptoms of Astigmatism
While astigmatism may exhibit different symptoms for different persons, some might not have any symptoms at all. Some of the symptoms associated with astigmatism include:
- Distorted and blurry vision at close range as well as at a distance
- Difficulty in seeing things at night
- Eyestrain
- Headaches
- Squinting
- Eye irritation
Treatment Options
Astigmatism can be treated in a host of ways including corrective contact lenses, eyeglasses, laser surgery as well as other refractive surgery procedures. LASIK (Laser in Situ Keratomileusis) or PRK (photorefractive keratectomy) are also used to treat astigmatism.
16: Presbyopia
Human eyes’ inability to focus on nearby objects due to gradual loss of vision is referred as “Presbyopia”, an eye disease normally associated with aging. Mostly, it remains unnoticeable until early to mid 40s and continues progression until 65 years of age or so.
Most people become aware of presbyopia only when they feel compelled to hold books, newspapers and other reading materials at arm’s length to be able to read something on them. It can be detected with the help of a basic eye exam.
Signs and Symptoms of Presbyopia
Presbyopia progresses really slowly, first significant symptoms surfacing after 40 years of age and some of them are:
- Blurry vision and inability to read at normal reading distance
- Eyestrain (mostly accompanied with headaches) as a result of activities requiring close-up vision
Treatment Options
Treatments for presbyopia aim at assisting your eyes in focusing nearby objects. Corrective eyeglasses, contact lenses, refractive surgery or lens implantation for presbyopia are some of the mostly sought after treatment options for this eye disease.
17: Proptosis
The phenomenon of protrusion of the eyeball is referred as “Proptosis”, also termed as “Exophthalmos” when such protrusion is caused by the “Graves’ disease”. Orbital mass or inflammation, thrombosis of cavernous sinus, fistulas and expansion of orbital bones are some of the common reasons behind this abnormal protrusion of eyeballs.
Signs and Symptoms of Proptosis
- Eye pain and irritation
- Light sensitivity
- Eye secretions (lacrimation)
- Blurry vision
- Diplopia (double vision resulting from weakened eye muscles)
Treatment Options
In severe cases of proptosis, an ophthalmologist mostly suggests lubrication for corneal protection. When lubrication fails to work, experts resort to surgery, which results in improved coverage of the exposed eye surface. Orbital congestion due to inflammatory orbital pseudotumor or thyroid eye disease is treated with specific systemic corticosteroids. And for cavernous sinus caused by arteriovenous fistulas, selective embolization works best.
18: Strabismus (Crossed Eyes)
Strabismus (or “Crossed Eyes”) represents misaligned eyes pointing in different directions and this misalignment can either be intermittent or constant. Strabismus exists in four common forms, i.e. “esotropia” and “exotropia”, “hypotropia” and “hypertropia”.
Esotropia is when one eye fixates on an object/point of interest, while the other eye turns in; whereas exotropia is when it turns out. Similarly, turning down of the other eye while one fixes at a point is hypotropia and hypertropia is when it turns up.
Strabismus usually occurs because the muscles controlling the movements of the eye and the eyelid, the extraocular muscles, fail to do so in a coordinative manner. Moreover, a disorder in the brain affecting the coordination of the extraocular muscles can also become the cause of strabismus. It can affect children as well as adults and about 4 percent of US population is believed to be suffering from this eye disease.
Signs and Symptoms of Strabismus
- Double vision
- Eyes’ inability to focus on a particular point at the same time
- Uncoordinated eye movements
- Loss of depth perception
Treatment Options
Strabismus is treated differently in kids and adults.
a. Strabismus Treatment Options for Kids
Strabismus in kids is treated preferably with eye patching, eye glasses, and/or atropine drops. If none of these prove effective, then an eye muscle surgery might be advised by your eye doctor, which involves tightening or loosening of the muscles causing the eye to wander. In most cases, kids can go home the same day after receiving surgical treatment.
b. Strabismus Treatment Options for Adults
Adults are treated differently for strabismus depending upon its severity, relying on various options ranging from observation to surgery. For treating minor to mild cases of strabismus, optical approaches including prism correction are preferred. If all such options run out, only then an ophthalmologist would advise for surgery after considering a host of factors and variants.
19: Macular Edema
Macula is the central region of the retina (constituted by the light sensitive tissues located at the back of the eye, wherein macula within the retina serves for sharp, straight-ahead vision) and unwanted buildup of fluids there is referred as the “Macular Edema”. Any accumulation of fluids inside the macula results in swelling and thickening of the macula, which leads to distorted vision.
Since the retina is richly populated with blood vessels, abnormal leakage of blood from damaged blood vessels there can result in fluid accumulation within the macula. Diabetic Retinopathy (DR – an eye disease mostly affecting diabetic people) is considered as one of the most common causes of macular edema. In fact, any eye disease damaging retinal blood vessels can lead to macular edema, such as age-related macular degeneration, an inflammatory disease sometimes, or even a wrongly performed eye surgery.
Signs and Symptoms of Macular Edema
Wavy or blurry vision in or around your central field of vision is considered as the very first symptom of macular edema in most cases. Some people also complain of colors appearing faded or washed. In fact, macular edema symptoms vary anywhere between slightly blurry vision to significant vision loss. If this disease attacks only one of your eyes, you may not even notice blurriness in your vision until the condition is already in advanced stage.
Treatment Options
Treatment options for macular edema also vary according to the underlying cause of the disease and consequential fluid leakage and retinal swelling. Some of them include:
Eye-drops Medication: This serves best in treating cystoid macular edema, a type of macular edema that can potentially damage the macula after cataract surgery and comprises of non-steroidal anti-inflammatory (NSAID) eye-drops. Such treatment can last for a few months.
Steroid Treatment: When inflammation is the reason behind macular edema, your eye doctor may recommend steroid treatment, which can be administered in form of pills, eye-drops or injections.
Laser Treatment: As the name suggests, this surgery is about applying numerous tiny laser pulses to the regions of fluid leakage around the affected macula, so that leaking blood vessels can be sealed and vision can be stabilized.
Anti-VEGF Medication: This treatment is based on anti-VEGF drugs, which are administered to the damaged eye through a very slender needle. Anti-VEGF (anti vascular endothelial growth factor) drugs are meant to curb the growth of abnormal blood vessels in your retina, thus helping prevent unwanted fluid leakage.
Vitrectomy Surgery: Sometimes, macula undergoes vitreous pulling, which results in macular edema (vitreous is the jelly like substance filling the back of the eye). Under such circumstances, seasoned eye doctors resort to “Vitrectomy”, a procedure in which vitreous is removed from the eye using tiny instruments, also peeling off scar tissues damaging the macula due to traction.
Conclusion
Eyes are highly complex and sensitive of body parts requiring extra care preservation if you want them to last you long enough to live a healthy, vibrant and colorful life.
In addition to taking care of them personally, make sure to be observant about any problematic signs and symptoms and respond by consulting an eye doctor, so that your eyes can get professional care and treatment before it’s too late.
20 Rare Eye Conditions That Ophthalmologists Treat
Ophthalmologists regularly care for eye conditions such as near- and farsightedness, cataracts and macular degeneration. But did you know ophthalmologists are uniquely qualified to study and treat uncommon eye diseases as well?
A disease is “rare” if it affects fewer than 200,000 people in the United States. Many rare eye conditions have no treatment or cure. But through innovative research, ophthalmologists are discovering treatments for some of the most challenging eye diseases.
Here are 20 rare diseases that ophthalmologists treat.
Charles Bonnet syndrome:
Up to 30% of people with severe vision loss in both eyes experience hallucinations. They may see geometric patterns or even people, animals or buildings that aren’t really there. Some might worry they’re losing their grip on reality, but that’s not the case. Patients usually know the images aren’t real. These hallucinations may come and go for a year or two, then taper off. There’s no cure or treatment but it can help to switch environments by going from a light to a dark room, for example. It also helps to relax, move around or blink the eyes.
Affects about 500 in 100,000 patients with vision problems.
Hemolacria (bloody tears):
Tears tinged with blood usually signal another underlying problem. Haemolacria may occur after a conjunctival injury, or from an object trapped under or inside the eyelid. Blood disorders like hemophilia, high blood pressure, nosebleeds or tumors in the eye are all possible causes. The exact cause must be narrowed down so that doctors can determine the best treatment.
Extremely rare.
Eye Conditions Passed Down the Family Tree
Retinitis pigmentosa:
People born with this genetic condition slowly lose vision as they age. It starts with trouble seeing at night or difficulty noticing details along the sides, or periphery, of their vision. As rods and cones in the retina slowly die, color vision fades and patients trouble seeing details directly in front of their eyes (central vision). Low vision tools and devices can help. There’s no cure. But ophthalmologists and other researchers are developing promising treatments ranging from gene therapies to retinal implants, sometimes called bionic eyes.
Affects about 25 in 100,000 people.
Usher syndrome:
Retinitis pigmentosa is sometimes part of a broader condition called Usher syndrome that affects vision, hearing and balance. There is no cure for Usher syndrome or retinitis pigmentosa. But genetic therapies show promise for treating these inherited eye diseases.
Affects up to 7 in 100,000 people.
Stargardt disease (juvenile macular degeneration):
Stargardt disease can go undetected until adolescence or adulthood, when people develop blurry or distorted vision. Vision loss can slowly decline to the level of legal blindness. This happens as light-sensing cells in the macula die off. The macula is the part of the retina that gives you central vision. Ophthalmologists and researchers are working hard to produce gene therapies and stem cell therapies for people with this condition.
Affects up to 12 in 100,000 people.
Retinoblastoma:
Children younger than 5 are the group most likely to develop this cancer of the eye. Retinal cells undergo changes that spark uncontrolled cell growth, causing a tumor to form in one or both eyes. The cancer can spread to other parts of the eye and body. Children are at risk for other types of cancers in the bone, muscle, and skin. Because this cancer is inherited, the siblings and children of these patients may also be at risk of retinoblastoma. Early detection and treatment are key to preserving sight and saving the child’s life. Treatments include chemotherapy, laser therapy, cold therapy (cryotherapy) and surgery.
Affects about 6 in 100,000 people.
Best disease:
This condition causes an egg-yolk-like residue to accumulate in the macula. By the time a patient reaches early adulthood, this buildup has damaged cells and distorted central vision. There’s not yet a treatment, but gene therapies and stem cell therapies may alleviate or cure this condition in the future.
Affects about 6 in 100,000 people.
Leber hereditary optic neuropathy:
More men than women develop this eye disease. It often shows up in young adults with a telltale pattern: painless loss of central vision in one eye, followed months or years later by vision loss in the other eye. Ophthalmologists and scientists are evaluating genetic therapies and drugs that may help recover vision in these patients.
Affects up to 7 in 100,000 people.
Leber congenital amaurosis:
Children with this disease can become blind before the age of one. That’s because light-gathering cells in the retina, known as rods and cones, do not work properly. A gene therapy called Luxturna can improve sight in patients with a defect in a gene called RPE65. But the condition can result from defects in more than two dozen other genes, and those defects cannot yet be corrected with gene therapies. Genetic testing can identify parents at risk of passing this condition on to their children.
Affects up to 3 in 100,000 people.
Batten disease (juvenile neuronal ceroid lipofuscinosis):
Infants with Batten disease have a genetic defect that causes fatty substances to build up in cells of the brain, nervous system and retina. Vision loss occurs early, usually between ages five and 10, and ophthalmologists are often the first specialists to suspect a problem. Over time, Batten disease damages the brain and nervous system. There are different forms of the disease, but all are fatal. Doctors are still working on a treatment.
Affects up to 4 in 100,000 people.
Bietti’s crystalline dystrophy:
Crystal deposits build up in the retina and cornea of affected children. These deposits accumulate over time. Eventually, the condition is detected when teens or young adults experience night blindness and trouble with central and side vision. People of Asian descent are most likely to develop this condition. There is not yet a cure or treatment.
Affects about 1.5 in 100,000 people.
Cystinosis:
Multiple organs — including the eyes, brain, kidneys, liver and pancreas — are affected when crystal deposits containing the amino acid cystine accumulate. A medicine called cysteamine helps eliminate these deposits from the body. Cysteamine eye drops can remove crystal deposits from the cornea, improving light sensitivity and vision. Infantile cystinosis is the most common type of cystinosis, but the condition can also surface in children and adults.
Affects fewer than 1 in 100,000 people.
Eye Conditions That Can Be Detected at Birth
Anophthalmia or microphthalmia:
Infants with these conditions are born without an eye (anophthalmia) or with very small eyes (microphthalmia). This usually accompanies other health conditions. There’s no cure, but ophthalmologists can protect the child’s existing vision. An eye specialist called an ocularist can design non-seeing prosthetic eyes to enhance appearance. Patients also work with other eye care professionals, including experts in pediatrics, vitreoretinal disease, orbital and oculoplastic surgery and ophthalmic genetics.
Affects about 10 in 100,000 infants.
Coloboma:
Coloboma means “curtailed” in Greek. When fetal eye development is interrupted during the first three months of pregnancy, infants are born with gaps of tissue missing from the eyelid, lens or other parts of the eye. Sometimes this is part of a broader genetic condition called CHARGE syndrome. Eyeglasses, contacts, eye patching, surgery and low vision devices can help protect sight.
Affects about 10 in 100,000 infants.
Axenfeld-Rieger syndrome:
Various types of eye problems—from a thin iris to an off-center pupil—can affect people with this syndrome. In some cases, extra holes in the iris can give the appearance of multiple pupils. In other cases, the cornea is affected. About half of patients develop glaucoma and are at risk for serious vision loss. Glaucoma can be treated with eyedrops or surgery. Some patients experience glare or light sensitivity, and find relief with special lenses or contacts.
Affects fewer than 1 in 100,000 people.
Polycoria:
People with “true” polycoria have two or more separate pupils in one or both eyes. Each pupil has its own sphincter muscle and they individually constrict and dilate. This can cause poor, dim or double vision. Surgery can help some people with true polycoria. Other patients have so-called “false” polycoria, where holes in the iris appear as two or more pupils, but only one actually works. These holes are usually just a defect of the iris and may cause some glare. Pseudopolycoria can affect patients with Axenfeld-Rieger syndrome, described above.
Extremely rare.
Eye Conditions of the Optic Nerve or Immune System
Optic neuritis:
Your eyes send visual information to the brain by way of the optic nerve. Swelling of this nerve can blur vision and make eye movement painful. Doctors don’t always know why this happens. Sometimes optic neuritis stems from an infection or an autoimmune disease such as neuromyelitis optica, described below. It can also be a side effect of certain medications. Optic neuritis is often treated with steroids.
Affects about 115 in 100,000 people.
Neuromyelitis optica (Devic disease):
Vision loss and paralysis are two early symptoms of this autoimmune disease. Neuromyelitis optica sparks inflammation in the central nervous system, with swelling the optic nerve (known as optic neuritis, described above) and the spinal cord (known as myelitis). In most cases, initial symptoms improve with steroids or immune-suppressing drugs. But relapse can produce lasting vision loss and spinal cord damage, making it difficult to see or walk. More women than men develop this condition.
Affects up to 10 in 100,000 people.
Idiopathic intracranial hypertension:
Pressure buildup in the brain and spinal cord can cause headaches, double vision and even temporary blindness. Doctors don’t always know why this happens. Sometimes it occurs when fluid doesn’t drain properly from the brain. This condition is most likely to affect young, overweight women. It can also be a side effect of certain medications. Treatments include weight loss, a drug called acetazolamide or surgery to relieve pressure on the optic nerve.
Affects up to 2 in 100,000 people.
Behçet’s disease:
This autoimmune disease affects many parts of the body, including the eye. Small blood vessels in the mouth, genitals, skin and eyes become inflamed and damaged. About 1 in 4 patients experience severe vision loss. Steroids and other medications can help calm inflammation and relieve symptoms.
Affects fewer than 1 in 100,000 people in northern Europe and the United States; about 420 in 100,000 people in northern Turkey.
5 Common Eye Diseases You Need to Know About: Health One Family Medicine: Family Medicine
A large percentage of the human population will experience eye problems at some point in their lives. Some of these eye problems are usually minor and will heal on their own, or can be treated at home. Others will require care from an eye specialist.
Here is our list of the 5 most common eye problems you should know about:
1. Macular Degeneration
Over 10 million people in the US will experience macular degeneration, also known as Age-Related Macular Degeneration (AMD). There are more cases of macular degeneration than cataracts and glaucoma combined. Macular degeneration happens when the central portion of the retina, known as the macula, gets damaged over time. At present, macular degeneration is an incurable eye disease.
Common symptoms include partial vision loss, blurry vision, problems seeing in dim light, and things appearing smaller than they actually are.
2. Cataracts
Cataracts are a widely occurring eye problem and usually affect more than half of all Americans over the age of 65. They usually have visually impairing cataract in one or both eyes. It’s when the eye forms clumps that prevent the eye lens from sending information to the retina. Cataracts are usually seen as the formation of a dense, cloudy area in the lens of the eye. When this happens, light is simply unable to pass through to the retina and the victim is unable to clearly see objects in front of them.
3. Glaucoma
Glaucoma occurs when the eye’s optic nerve gets damaged, usually due to fluid buildup and increased pressure from the inside. This restricts the optic nerve from sending images to the brain. The buildup of pressure may lead to permanent loss of vision if it continues for longer without treatment. Glaucoma progresses relatively fast and can render victims blind in just a few years.
The biggest symptoms of glaucoma include tunnel vision, peripheral vision loss, blurry eyes, halos around the eyes, and redness of the eyes.
4. Dry Eyes Syndrome
Dry eye syndrome is caused by a lack of moisture and lubrication on the eye’s surface. Some patients may experience subtle but constant eye irritation, others may undergo significant inflammation leading to scarring of the front surface of the eye.
There is a large variation in the number of people affected by dry eye syndrome, with estimates ranging from as low as 5% to as high as 50% depending on different parts of the world. People who wear contact lenses are at risk of getting dry eyes. It also occurs due to old age.
5. Retinal Detachment
This is a rare condition when the retina gets detached from its place in the eye. It may happen gradually as small areas get torn before the entire retina gets detached. This will affect a person’s vision and the longer you suffer from it, the higher your chances are of complete vision loss in the affected eye. Although the process sounds painful, patients don’t usually feel any pain during retinal detachment.
But there are various warning signs such as blurred vision, a sudden appearance of light flashes, and a curtain-like shadow in one’s field of vision.
Wrapping Up
The human eyes play an important role and are extremely sensitive to diseases and damage. They require extra care and attention if you want them to last long. Part of the care and prevention strategy is to make regular appointments with your eye specialist.
If you require further advice on getting help, you can book an appointment with a physician at Health One Family Medicine.
Visit https://www.healthonemedicine.com or call (469)262-5762 for more information.
Author
Health One Family Medicine
Charleston Cornea and Refractive Surgery
Although you can easily fix red-eye and other photo bloopers with editing tools on your smartphone or computer, you should take note of any eye abnormalities you spot in photos of your children. A strange glow or yellow hue can indicate a number of different eye conditions, some of them more serious than others. At Charleston Cornea, we want you to understand how and why this works.
When the camera flash reflects off the blood-rich retina — the back part of your eye that transmits light cells to your brain — this reflection may result in red-eye in your photos, also called red reflex.
Although a photo with red-eye may be frustrating, it is also a sign that your child’s eyes are healthy. If your child’s eyes appear black, white, or yellow in the photo, it can be a sign of an eye condition.
It may be a minor condition such as myopia or astigmatism, which can be corrected with glasses. In other cases, this eye glow, as it’s sometimes called, may be an indication of something more serious that can eventually rob your child of vision.
If a white glow, also called leukocoria, covers most of your child’s pupil in the photo, it could be a sign of cataracts, retinal detachments, or retinoblastoma, a rare but serious form of childhood cancer. The glow is an indicator of about 16 eye diseases.
Why Photos Are Important
Many serious eye conditions have no symptoms — no pain, irritation, or eyesight issues. Parents tend to take numerous digital photos of their children. Whether they post them online or share them with friends and relatives, these photos provide an opportunity to detect an eye condition early, when it is most treatable. For example, when retinoblastoma is caught early, it has a 95% cure rate.
What to Look for in Photos
There are some things to note if you do, or don’t, spot red-eye, a glow, or abnormal hue in one or both of your child’s eyes in a photo. Was your child looking directly into the camera? If not, the camera’s flash may have captured a side glimpse of the whites of their eyes.
For purposes of eye health evaluation, only use photos in which your child is looking directly at the camera.
Don’t be concerned if your child does not have red-eye in the photo. That is not necessarily an indication that something is wrong. Check to see if your flash is actually on or if you’ve enabled the red-eye reduction setting on your camera.
If you suspect a problem with your child’s eyes, review older photos as well to confirm or alleviate your concerns.
What to Do if You Suspect a Problem
A photo alone is not enough to diagnose your child’s eye condition. It’s a sign, though, that you should seek a professional exam.
If you notice some of these photo eye issues, have your child checked out as soon as possible by a medical professional like Dr. David O’Day of Charleston Cornea at either the Mount Pleasant or North Charleston, South Carolina, office for a diagnosis and treatment plan.
90,000 symptoms, causes, treatment, prevention and hygiene
One of the most dangerous complications of eye disease in dogs is complete loss of visual function. Despite the fact that blind four-legged pets are much more independent than people, you should not bring the situation to such a sad outcome. Unpleasant consequences can be prevented with the help of timely detection of symptoms of eye pathologies and compliance with preventive recommendations.
Causes of eye diseases in dogs
All causes of violations are divided into 3 large groups. These include:
Congenital . Poor genetics or breed predisposition is to blame for the disease.
Infectious . Complication from infection with viruses or bacteria.
Non-infectious . Mechanical damage, neoplasms and allergic reactions that contribute to the ingrowth of eyelashes, eversion of the eyelid and the appearance of tumors.
Treatment of pathologies affecting the eyes is reduced to eliminating the factors that are to blame for their appearance. You can find out the exact cause only with the help of a comprehensive diagnosis in a veterinary clinic. Self-medication attempts based on false conclusions can result in a worsening of the condition.
Classification of diseases, their symptoms and treatment
Symptoms of eye disease in dogs vary by location. The most common pathologies affect the eyeball and its fundus, eyelids, conjunctiva and choroid, retina and cornea.
Diseases of the eyeball
Most cases from this group are congenital.The only exception is strabismus, which develops more often than others due to mechanical damage.
Enophthalm
Enophthalmos, or Horner’s syndrome, is a sinking eyeball. It is easily recognized by the pronounced difference between the organ of vision and the size of its orbit. The eye is located deeply, flattening due to the atrophy that has arisen. A pet with a similar anomaly has frequent blinking and loss of the third eyelid.
The drugs used are aimed at suppressing the symptoms and complications that have arisen.Enophthalmos itself is eliminated only by surgery.
Exophthalmus
Exophthalmos is the opposite of enophthalmos: with it, the apple does not deepen, but goes beyond the orbit. This is due to severe bruising or intraocular pressure, weak muscles, and a shallow orbital cavity. In addition to redness and inflammation of the bulging eye, there is a slight squint and prolapse of the third eyelid.
This anomaly is very frightening and dangerous.In case of complete prolapse, it is necessary to apply a damp cloth soaked in warm water to the affected organ, and urgently take the animal to the veterinary clinic for surgical reduction. Under anesthesia, the eye will be returned to its orbit by suturing the eyelid. Additionally, anti-inflammatory drugs and antibiotics may be prescribed to avoid inflammation and infection of the postoperative wound.
Strabismus
A squinting eye that does not repeat the movement of a fixed one is hard to miss.He can mow towards the nose, away from him or vertically (up or down). Strabismus can be congenital or acquired. In the second case, the violation develops as a complication of an infection (meningitis, distemper, encephalitis) or due to injury (being hit by a car).
If the cause of strabismus lies in concomitant pathology, then for the animal to recover, it is enough to eliminate the root cause. Infections are treated with antibiotics and antivirals, and the effects of trauma are treated with surgery.
Pathology of the eyelids
This group includes diseases that cause inflammation or deformation of the eyelid. Their main causes are infections and breed predisposition.
Ectropion and entropion
Both diseases are characteristic of the canine family, since they practically do not occur in other pets. Symptoms and treatment of these pathologies depends on the direction of the eyelid curvature:
Ectropion, or eversion .It is accompanied by drying out and inflammation of the conjunctiva. The dog constantly rubs his eyes with his paw and blinks often. The disease can be complicated by keratitis or a secondary infection. It is treated with surgery.
Entropion, or volvulus . It is accompanied by similar symptoms, including photophobia and profuse lacrimation. Without timely treatment, it can be complicated by ingrown eyelashes. Entropion is treated by excision of excess skin to form the correct slit for the eyeball.
Diseases often develop in parallel. Their main difference is the possible danger. Entropion is much more dangerous than ectropion, as it can lead to serious pathologies of the cornea.
Blepharitis
Blepharitis is unilateral or bilateral inflammation of the eyelid margins. It can be caused by mechanical damage, staphylococcal infections, demodicosis and allergies.
The affected area is severely swollen, reddened and inflamed. Pus flowing out, forms crusts and ulcers on the eyelid. The skin becomes rough. Fur and eyelashes begin to fall out from the surrounding areas. The development of an ectro- or entropion is possible.
Blepharitis is treated with antibiotics, antihistamines, or acaricidal drugs. Dried crusts are softened with herbal decoctions.
Cherry Eye
An alternative name for this disease is a third century adenoma.The tumor affects the lymph nodes, causing them to swell. Because of the redness, the thickened third eyelid resembles a small cherry. Mucous or transparent outflows appear.
Conservative treatment of “cherry eye” in dogs is ineffective, therefore most often they resort to surgery – the third eyelid is sutured or completely removed. In the second case, the operated pet will have to moisturize the cornea with special preparations.
Conjunctivitis and uveitis
Both diseases are fraught with low vision or blindness, so it is very important not to miss the warning signs. Symptoms and methods of treatment will depend on the type of the affected membrane:
Mucous (conjunctiva) . Inflammation of the mucous membrane of the eye in dogs causes allergic, purulent, or follicular conjunctivitis. All of them are accompanied by swelling and redness of the conjunctiva up to a bright crimson color, as well as lacrimal or purulent discharge. Depending on the type, conjunctivitis is treated with antihistamines or antibiotics.The affected organ is cleansed of pus and moistened with special drops. Excision of the conjunctiva is resorted to only in severe cases characteristic of the follicular type.
Vascular (uveal tract) . Inflammation of the choroid, accompanied by opacity of the iris and photophobia, is called uveitis. An inflamed eye hurts a lot, so the pet constantly covers its eyelids. To save vision, it is important to establish and eliminate the root cause as early as possible.In parallel, symptomatic therapy is prescribed, aimed at relieving inflammation or at least reducing pain.
Uveitis is more dangerous than conjunctivitis. With delayed treatment, you can lose not only vision, but also the eye itself.
Retinal problems
The retina is the thin membrane between the eyeball and the vitreous humor. It is responsible for transmitting images to the brain through nerve impulses, so disturbances in this layer are very dangerous.
Atrophy
This hereditary disease is accompanied by a gradual deterioration in vision at night, and then in the daytime. Over time, the pupil turns pale, and the animal develops blindness. Unfortunately for the owners, retinal atrophy is incurable.
Delamination
The retina can detach due to high blood pressure, neoplasms, trauma, or progressive atrophy.A sick dog has a rapid deterioration in vision or sudden blindness. When diagnosed in a veterinary clinic, hemorrhage in the apple and the absence of a pupil response are revealed.
Treatment is effective only with timely treatment. Detachment is inhibited by taking drugs that eliminate the root cause, or by surgery, returning the retina to its proper place.
Disorders in the fundus and lens
The fundus of the eye is located directly behind the lens – a transparent body responsible for conducting and refracting light.The bottom consists of the optic disc, the central depression, the retina, the macula (macula), and the posterior pole.
Glaucoma
This eye disease in dogs is associated with increased intraocular pressure. The main symptom of glaucoma is a greenish thorn. The sick eye turns red, and the pupil increases significantly, losing its reaction. The animal develops photophobia.
Glaucoma is almost incurable, but its development can be slowed down.To do this, use drugs that improve the outflow of intraocular fluid, and cryotherapy – applying cold to the ciliary body.
Cataract
Cataract is a loss of transparency of the lens, accompanied by visual impairment or blindness. It is easily recognized by the cloudiness of the pupil and iris, as well as their color change to gray-blue.
Pathology is congenital and acquired.In the second case, the cause of the violation lies in injuries, diabetes mellitus and advanced infections.
Cataracts are treated promptly by removing particles of damaged protein. In a more severe course, the lens is excised entirely and replaced with an artificial one.
Lens luxation
Luxation is the displacement of the lens caused by the rupture of the ciliary girdle. The disorder occurs due to genetic predisposition and trauma or as a complication of infection, glaucoma and cataracts.
Because of the pain, the dog constantly squints its reddened eyes and rubs them with its paws. His eyelids swell and there is a clear and bloody discharge from the lacrimal canal. The pupil does not react to light, but its shape changes.
Luxation is treated by removing the lens with the subsequent placement of the implant. If an injury is to blame for the disease, then the affected eye can be removed entirely.
Corneal diseases
The cornea covers the outside of the optic organ and is responsible for refracting light.Its smooth and shiny surface often suffers from external influences, losing its functionality due to inflammatory processes.
Keratitis
Keratitis is inflammation of the cornea caused by infection or injury. It is accompanied by dulling and discoloration of the cornea to gray or blue. A sick pet behaves very restlessly: it blinks often, rubs its muzzle with its paws and avoids bright light. Over time, profuse lacrimation and exudate appear.Protein and mucous membranes turn red.
Inflammation of the cornea is fraught with ulceration and the development of glaucoma or cataracts. Fortunately for the owners, with timely treatment, keratitis responds well to treatment.
Treatment depends on the cause of the keratitis and may include taking glucocorticosteroids, antibiotics, antivirals, and antihistamines. For a quick recovery of the pet, it is necessary to rinse its lacrimal sacs daily with antiseptics. In more severe cases, keratectomy is performed – laser correction of the cornea.
Corneal ulcer
A corneal ulcer is a type of keratitis. It is found more often than others, so it should be distinguished separately.
Ulcerative keratitis affects not only the upper layer of the epithelium, but all the others. The affected tissue gradually becomes thinner and becomes covered with small ulcers. With the aggravation of the pathology, individual foci merge into a single ulcer. In an animal, the cornea becomes cloudy, the contour of the pupil is blurred and the protein turns red.
Treatment of the affected dog’s eye is to eliminate the root cause:
taking antiviral or antibiotics for conjunctivitis;
blepharoplasty with entropion.
In advanced cases, an operation is performed with the removal of pus and excision of dead tissue. After healing, a small scar remains on the cornea.
Animals at risk
The risk group includes animals most vulnerable to the listed violations. These include:
In the first case, vulnerability to external factors is explained by an oversized visual organ. In the second – skin folds on the face, increasing the likelihood of inflammation due to accumulated dirt and dust.In the third – long hair, fraught with frequent irritations and injuries.
Hazards and complications
Timely therapy avoids many complications: atrophy, eye loss, partial or complete blindness. Due to the variability of possible causes, in addition to loss of vision, it is worth considering other dangers associated with the initial pathology or associated infection.
Do not exclude the possibility of disruption of the internal organs and systems, fraught with the death of the pet.It is much safer to try to prevent illness by avoiding its occurrence.
Prevention and hygiene rules
The main preventive measures are aimed at eliminating provoking factors and increasing immunity. This will help you:
Regular and quality food. Avoid vitamin deficiencies and keep your diet balanced.
Safe storage of detergents and cleaning products. To avoid chemical burns, poisoning or an allergic reaction, remove all dangerous items as high as possible.
Hygienic haircut. Get rid of long hairs on your face to avoid irritation.
Periodically check your skin folds for dirt and injury.It is best to check overly active pets after every walk.
Annual preventive examination. If your four-legged pet is at risk, be more attentive to alarming symptoms and immediately contact your veterinarian when they appear.
Correct hygiene. To treat the eye, use herbal extracts of chamomile or calendula. If the sun is too bright or the wind is strong, use eye drops recommended by your doctor.This will help to avoid drying out the mucous membranes. Excessive accumulation of moisture is equally dangerous. If the dog often has tears, wipe them daily, avoiding the formation of paths.
For processing, a cotton pad is suitable, which excludes trauma to the cornea by villi. Move from the outer corner towards the nose. Remember that eye drops are instilled into both eyes strictly after removing all secretions and dried crusts.
It is almost impossible to regain lost vision, so take care of your dogs’ eyes as much as your own.Regular preventive examinations and your own vigilance will help you with this.
This article is for informational purposes only. See your veterinarian!
Like the article?
198
90,000 Diagnosis, treatment and prevention of eye diseases in children
Marina Belashova, an ophthalmologist of the first qualification category, tells how often a child needs to visit an ophthalmologist.
In the first year of life, it is advisable to carry out preventive ophthalmological examinations of a healthy full-term baby twice.
First examination – at the age of one month of life to exclude congenital diseases that may require treatment at an early age. During the examination, the doctor checks the condition of the child’s eye. At this age, the baby must briefly fix objects and monitor them. The accessory apparatus of the eye is assessed, if necessary, the condition of the lacrimal ducts is checked (in children of the first months of life, difficulty in the outflow of tears is often encountered).The eyeball itself is examined to identify congenital and perinatal pathology. The fundus of the child’s eye is examined.
Second examination – at the age of about a year. The doctor will assess visual functions, refraction and control the maturation of the eyeball. This examination is important for diagnosing refractive errors (myopia, hyperopia, astigmatism), preventing the development of amblyopia and strabismus.
In the future, the child needs to visit an ophthalmologist for preventive purposes at least once a year.In childhood, the assessment of the dynamics of visual acuity is relevant. For patients from 3 years old, doctors determine visual acuity according to the table. First, this is a table with pictures, and from 6-7 years old, a table with letters or other symbols is used.
In addition, at present, the age of onset of myopia is rapidly falling, so it is important not to miss the moment of the onset of the disease. Timely diagnosis can prevent the progression of pathology.
You can make an appointment with specialists by phone: +7 (495) 959-88-03, +7 (495) 959-88-00 (around the clock).The ophthalmology department is open seven days a week: Monday – Friday from 8:30 to 20:00, Saturday, Sunday from 9:00 to 15:00.
Yellow plaques around the eyes warn of heart attack
- James Gallagher
- BBC Science Observer
Photo author, SPL
Photo caption,
that there are large deposits of cholesterol in other parts of the body
People with cholesterol formations on their eyelids may be at increased risk of heart attack and other serious illnesses, Danish scientists warn.
Results of a study published on the website of the medical
magazine BMJ, show that patients with yellow patches on the eyes – xanthelasma – are 48% more likely to have a heart attack than people with clean eyelids.
Xanthelasmas are composed primarily of cholesterol, and their presence on the face may indicate that there are extensive deposits in other parts of the body.
Atherosclerosis or the deposition of cholesterol on the inside of the vessel walls can cause strokes and heart attacks.
The study authors believe that their findings should help doctors diagnose serious diseases at an earlier stage.
Competence of a Cardiologist
The study, involving 12,745 people, began in the 1970s at the Herlev Hospital Complex near Copenhagen. At that time, 4.4% of patients had xanthelasma.
33 years later, 1872 study participants suffered a heart attack, 3699 developed cardiovascular disease and 8507 of the patients died.Moreover, those people who had yellow plaques in front of their eyes were in the high-risk category.
Patients with xanthelasmus had 48% more heart attacks, 39% more likely to get heart disease, and during the experiment, 14% more people died among them than among the study participants without deposits on the eyelids.
Currently, most patients with xanthelasma go to beauticians to have them removed.
But first and foremost, these external body fat should serve as a signal to check for cardiovascular disease, the researchers said.
Online vision tests
Online tests may only be used for an REFERENCE self-examination. If the test shows a deviation from the normal state of vision, we recommend that you contact our clinic for an examination of the state of the visual system. Without undergoing a complete diagnosis of vision, it is impossible to diagnose and prescribe methods of correction and treatment.
Amsler Test
This test is used to detect central retinal pathology .
The picture should be approximately 30 cm from your eyes.
Cover one eye with your hand, and with the other, look at the black dot in the center of the picture for a few seconds.
Repeat the same on the other eye.
Are all grid lines straight? Are there gray spots and distortions?
If not, then your macular (central) area of the retina is normal.
If you have curved lines or gray (dark) spots, you should urgently see an ophthalmologist.
The picture must be on the screen of real size!
Astigmatism Test
If some of the lines in this picture seem clearer to you and others are more blurry, you might be presumed to have astigmatism. What is the degree of astigmatism and whether it needs correction? To get answers to these questions, you need to contact an ophthalmologist.
- Close one eye, take 3-5 steps back from the monitor and look at the circle.
- Notice if some of the lines are getting darker than others
- If yes, you may need glasses with astigmatic spectacle lenses or toric soft contact lenses.
Color Test
To check for myopia or hyperopia, click on the picture. If you are better able to distinguish between letters on a red background, you may be suspicious of myopia. If you are better at distinguishing letters on a green background, then there is more data for hyperopia.
To get an accurate answer to the question whether you need a vision correction, you need an ophthalmologist’s opinion, we recommend making an appointment with a doctor if you find a difference in the perception of letters on different backgrounds.
Eyesight Test
When testing your eyesight, refer to the table.
| SCREEN | Monitor distance |
| 640 x 480 | ~ 2.5 m |
| 800 x 600 | ~ 2.0 m |
| 1024 x 768 | ~ 1.5 m |
If in at least one of the tests you have doubts about the state of vision, we recommend that you urgently consult an ophthalmologist.
Tri-Z Eye Clinic – ophthalmology in Krasnodar
Tri-Z is the largest network of modern ophthalmological centers in Russia. These are four clinics in Krasnodar, Perm, Yessentuki, Moscow and 30 diagnostic branches in seven regions of Russia.
We are experts in the treatment of cataracts Cataract Cataract is an eye disease associated with clouding of the lens, due to which light rays stop entering the eye and reaching the retina Retina – the inner lining of the eye, an important part of the visual analyzer.It is she who is responsible for the process of converting light into a nerve impulse, which is transmitted to the brain, which leads to a decrease in vision. – eye disease associated with clouding of the lens, due to which light rays cease to penetrate into the eye and reach the retina Retina – the inner shell of the eye, an important part of the visual analyzer. It is she who is responsible for the process of converting light into a nerve impulse, which is transmitted to the brain, which leads to a decrease in vision. Cataract Cataract – an eye disease associated with clouding of the lens, due to which light rays cease to penetrate into the eye and reach the retina Retina – the inner lining of the eye, an important part of the visual analyzer.It is she who is responsible for the process of converting light into a nerve impulse, which is transmitted to the brain, which leads to a decrease in vision. – eye disease associated with clouding of the lens, due to which light rays cease to penetrate into the eye and reach the retina Retina – the inner shell of the eye, an important part of the visual analyzer. It is she who is responsible for the process of converting light into a nerve impulse, which is transmitted to the brain., Which leads to a decrease in vision., Glaucoma Glaucoma is a disease characterized by a constant or periodic increase in intraocular pressure, which entails atrophy of the optic nerve with specific changes in the field of vision.If untreated, it can lead to blindness., Myopia, hyperopia, astigmatism Astigmatism is a visual defect associated with an uneven curvature of the cornea or a violation of the shape of the lens. As a result, the rays of light hitting the retina are refracted unevenly, and instead of a clear picture, a person sees a blurred double image. and keratoconus Keratoconus is a non-inflammatory disease of the cornea, in which it gradually becomes thinner and takes on an abnormal conical shape.Keratoconus is often confused with myopia and astigmatism Astigmatism is a visual defect associated with an irregular curvature of the cornea or an irregular lens shape. As a result, light rays hitting the retina are refracted unevenly, and instead of a clear picture, a person sees a blurred double image .., as well as diseases of the vitreous body and retina Retina – the inner shell of the eye, an important part of the visual analyzer. It is she who is responsible for the process of converting light into a nerve impulse, which is transmitted to the brain…. We accept patients from the first month of life until old age: we carry out diagnostics, treat and help to choose comfortable glasses and contact lenses.
We use modern equipment from leading manufacturers in Europe, Japan, USA and Russia. Our doctors diagnose eye diseases at an early stage, provide timely treatment and achieve the best result for each patient.
Why double vision, and what to do about it?
Why double vision and what to do about it?
Diplopia or “double vision”
Each of us has two pictures of the surrounding reality, although we usually do not think about it. One is projected onto the retina of the right eye, the other onto the retina of the left. The brain combines these images into a single whole, so that a person sees objects in a single copy. But that’s okay. Often, patients complain that they have “double vision”: they cannot focus their gaze on an object, correctly determine the distance to it, sometimes it is even difficult to orientate in space.The sensation, of course, is not a pleasant one. In addition, it is often accompanied by nausea, visual fatigue, dizziness, and sometimes it comes to severe headaches.
Scientifically, this phenomenon is called diplopia. The visual axis can be displaced in either direction in one or both eyes. In the first situation, we are dealing with monocular diplopia, it does not go away when the second, healthy eye is closed. And in the case of binocular diplopia, vision, on the contrary, is normalized if one eye is closed.
In addition, this defect can be unstable (after injury, poisoning, or excessive alcohol consumption) and permanent (its causes will be discussed below). If you notice that “double vision” has become your companion for a long time and does not go away, you should definitely contact a specialist. Usually, a visit to an ophthalmologist is enough to diagnose diplopia and prescribe treatment. But sometimes a neuropathologist, oncologist, endocrinologist, rheumatologist or even an infectious disease specialist have to be involved in the search for the reasons.Indeed, sometimes diplopia becomes a wake-up call, by which the doctor will identify another disease.
If you notice that “double vision” has become your companion for a long time and does not go away, you should definitely contact a specialist
But there is a special case of double vision, in which anxiety will be unnecessary – volitional diplopia, deliberate defocusing of the gaze. Surely many from childhood remember the stereograms that were printed on the covers of notebooks.It was the ability for strong-willed diplopia that made it possible to see objects woven into the pattern’s canvas. Another example: place a small object in front of the monitor screen, continuing to look at the screen as if through it. The subject will double in front of your eyes, and this is completely normal, there is no reason to panic.
Causes of diplopia
We figured out the varieties of diplopia, now let’s talk in more detail about the reasons. Here are the most basic ones:
- Strabismus. Here we are dealing with binocular diplopia.However, the human body adapts well and the brain can learn to ignore one of the images, especially during childhood. Therefore, paradoxically, people with squint do not always suffer from “double vision.”
- Diseases of the thyroid gland. They can affect the motor function of the eyes.
- Vascular diseases. With them, the blood supply to the eyes is disrupted, which causes problems with focusing.
- Malignant and benign formations.
- Multiple sclerosis or diabetes mellitus. Although these diseases have little in common, they both cause damage to the optic nerves.
- Infectious diseases (such as tetanus and rubella). They interfere with the proper functioning of the eye muscles and nerves.
- Exhaustion of the eye muscles.
- Cataract, corneal injury and other eye diseases. Some of these can occur due to sunburn of the eye. Therefore, it is so important to wear glasses with high-quality lenses that protect against ultraviolet radiation.This will help to avoid not only diplopia, but also many other vision problems. For example, UV rays block Crizal lenses, which will also protect the eyes from blue-violet radiation from the screens that can damage the retina.
Let’s add to this the reasons for temporary double vision, which we wrote about above … And these are not all possible sources of the problem! Therefore, only an experienced ophthalmologist will help to understand and choose the treatment; it will not be possible to cope with the disease on your own.In any case, I recommend to undergo an annual examination, regardless of the state of vision. After all, all diseases are much easier to treat at the initial stage, when they are still invisible to the patient.
Five ways to treat diplopia
There are five main treatments for diplopia in modern medicine:
1. Treatment of the disease that caused diplopia. Most often this is a disease of the nervous system, therefore, therapy should be carried out by a neurologist or neurosurgeon. For orbital causes of double vision, an ophthalmologist is involved in the treatment.
2. Prismatic correction. It is performed using glasses with a prismatic action against the background of active functional treatment (development of fusional ability and reserves). Remember that it is advisable to reduce or completely cancel the prismatic correction, especially in children.
3. Functional treatment. All types of eye exercises aimed at restoring binocular vision help.
4. Surgical treatment. Possible indications for surgery are a high degree of deviation of the eyeball and ineffectiveness of other methods.All types of muscle surgeries are performed no earlier than 6 months after the injury or onset of the disease. This type of treatment is not prescribed for double vision in extreme gaze abductions (lateral, upper, lower and oblique), if there is no double vision in the primary position of the eyes and their symmetrical position is maintained.
5. Suppression of the second image. If functional treatment does not help, you have to temporarily tape one lens of the glasses with adhesive tape or prescribe prisms with a reverse direction of the base to move the double image away from the central part of the visual field.
Rano Ibragimova, ophthalmologist, specialist, Essilor Academy Russia 90,000 Eye research – Medcenter-Zhezkazgan.kz
Computer refracto-keratometry – a method for studying the refraction (refractive power) of the eye and the shape of the cornea. An infrared test mark invisible to the patient is projected onto the fundus of the patient. The degree of its change depends on the refraction of the patient’s eye. A special computer evaluates and recalculates these changes.Keratometry – determination of the radii of curvature and refractive power of the cornea, the study necessary for the selection of contact lenses and the diagnosis of corneal diseases. The built-in printer prints the result in a form convenient for the doctor. The results of computer refractometry are sufficient for the initial assessment of changes in the patient’s vision and further selection of glasses or contact lenses. In most cases, especially in adults, there is no need to dilate the pupils. The autorefractometer has a function that relieves the stress of accommodation.In our clinic, we use an automatic refracto-keratometer Accuref-K Shin-Nippon (Japan), which allows us to determine refraction with a sufficient degree of accuracy and without the use of additional means (for example, ciploplegia). It has the function of automatically measuring the curvature of the cornea at peripheral points, which is especially important when fitting or measuring contact lenses.
Ophthalmoscopy – a research method that allows you to examine the eyeball from the inside, i.e.e. examine the fundus using a special device – an ophthalmoscope. With the help of the method of ophthalmoscopy, it is possible to carefully examine the retina and the structures located in it: the macula region, the central region of the retina, the optic nerve head, the retinal vessels; as well as the choroid.
It is performed on a narrow or wide pupil using electric ophthalmoscopes of various designs, depending on the need.
Perimetry (examination of visual fields)
Perimetry is a method for examining the boundaries of visual fields with their projection onto a spherical surface.The field of view is a part of the space that the eye sees with a certain fixation of the gaze and a motionless head. If you fix an object with your eyes, then in addition to a clear distinction of this object, other objects are visible that are located at different distances from it and fall into the field of vision of a person. Thus, the eye has peripheral vision, which is less clear than the central one.
Indications for perimetry are:
1. Glaucoma.
2.Diseases of the optic nerve (neuritis, trauma, ischemia).
3. Retinal pathology (degeneration, hemorrhage, radiation burn, detachment, tumor).
4. Hypertension.
5. Brain tumors.
6. Traumatic brain injury.
7. Cerebral circulation disorders.
8. Assessment of vision during preventive examinations.
Contraindications to perimetry:
1. Mental illness of the patient.
2. Alcohol or drug intoxication.
When carrying out computer perimetry, the patient also fixes his gaze on a specific mark. At various points of the device, objects of different brightness begin to appear in a chaotic manner with varying speed. As soon as the patient notices such an object, he presses a special button on the device. The device gives out the results of the examination, on the basis of which the doctor makes an accurate diagnosis.
In our arsenal there are automatic computer perimeter
KOWA AP 5000 C (Japan) for static, kinetic, color perimetry and assessment of the threshold sensitivity of the retina.
Ultrasound examination (ultrasound) of the eye – informative diagnostic method This method is becoming more widespread, is simple, safe and highly informative. Eye ultrasound is a diagnostic procedure that allows you to assess the structure of the eye, the condition of the retina, lens and eye muscles. Very often, ultrasound is prescribed after ophthalmic operations, assessing the condition of the fundus or, in particular, when replacing the lens – the location of the lens.Such studies allow not only to identify eye diseases, but also to regularly monitor their dynamics.
Indications for carrying out: high degrees of myopia and hyperopia; retinal disinsertion; cataract; glaucoma; swelling of the eye; pathology of the eye muscles; eye injury; foreign body in the eyeball; vascular diseases of the eyes; diseases of the optic nerve; chronic diseases (hypertension, kidney disease, diabetes mellitus).
There are practically no contraindications for ultrasound of the eyes, with the exception of open eye injuries.
For this study we use ultrasound machine
E-Z scan AB 5500 Sonomed (USA).
Determination of visual acuity is the determination of the eye’s ability to distinguish between two luminous points located at a minimum distance from each other, expressed by a number. Those. visual acuity is the ability to see the structure of an object. Actually, this research method allows you to determine the patient’s level of vision, but, unfortunately, this technique is not applicable in children under 3-4 years of age.
Any appeal to an ophthalmologist is an indication for the determination of visual acuity. There are no contraindications to this procedure. Distinguish between the definition of visual acuity for distance and for near.
Special tables are used to determine visual acuity. For the distance, these are the tables of Sivtsev (with the letters of the Russian alphabet) and Golovin (with Landolt’s rings), and for children – Orlova (with pictures). Opposite each line in these tables is the visual acuity to which this line corresponds.
First, visual acuity is examined without correction, and then with correction, which allows a more detailed assessment of visual function. If the patient wears glasses, then the vision is checked without them and with them.
